Effects of Metformin Delivery via Biomaterials on Bone and Dental Tissue Engineering
Abstract
:1. Introduction
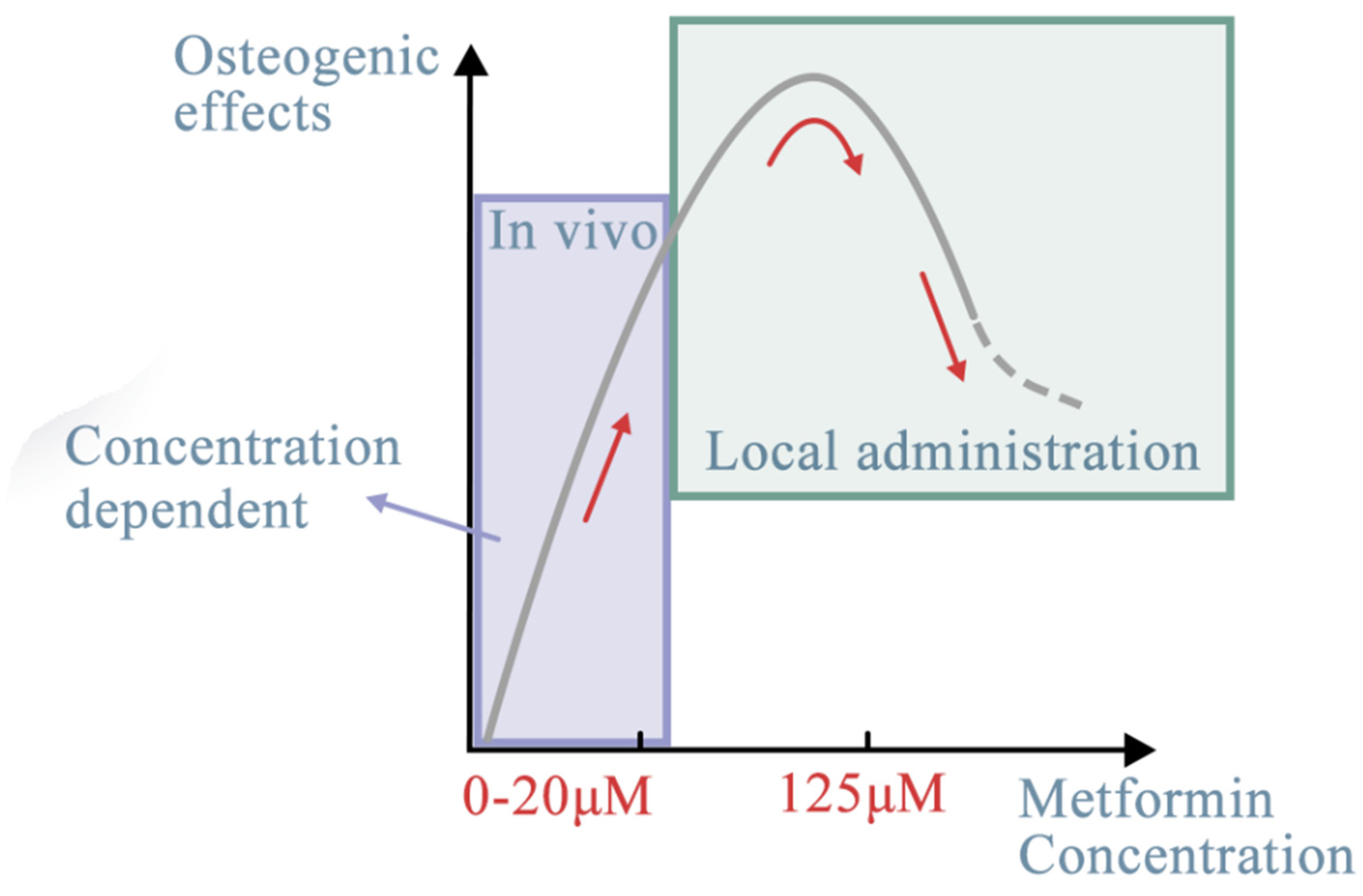
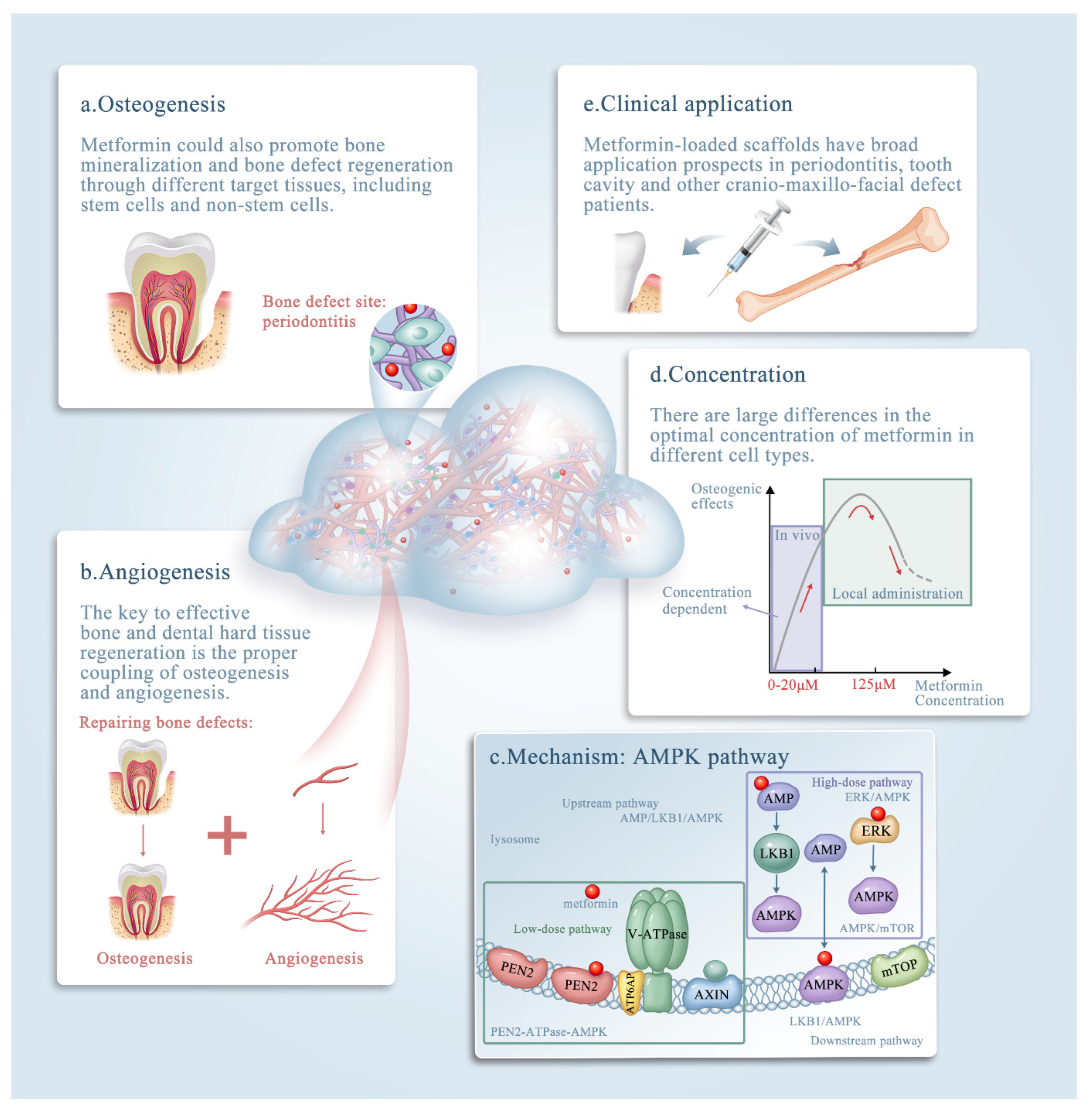
2. Metformin Promotes Bone Repair and Regeneration
| Target Stem Cells | Metformin Concentration | In Vivo/In Vitro (Local Administration) | The Effects of Metformin | References |
|---|---|---|---|---|
| iPSC-MSCs | 0.5-500 μM | In vivo | Promoted osteoblastic differentiation through AMPK signaling | [30] |
| 0–20 μM | In vivo | Increased cell viability in a dose-dependent manner | [31] | |
| BMSCs | 125 μM | In vivo | The optimal concentration | [7] |
| over 200 µM | In vivo | Inhibited the osteogenic differentiation | ||
| Adipose-derived stromal cells | 500 µM | In vitro | Increased the formation of mineralized extracellular matrix | [33] |
| 250 mg/kg/day | In vivo | Accelerated bone healing and facilitated new bone callus formation | ||
| hPDLSCs | 100 µM | In vivo | Positive effect on the osteogenic differentiation Negative effect on the adipogenic differentiation | [34] |
| Human endometrial stem cells | 10 wt% | In vivo | Improve osteogenic capability GBR application | [13] |
| In vitro | ||||
| 10 to 15 wt% | In vivo | Decreased the viability of cell cultured on the surface | ||
| In vitro | ||||
| DPSCs | 20 wt% | In vitro | Restored the tooth cavity, provided protection for dental pulp, | [35] |
| BMSCs | 0, 10, 50, 100, and 200 μM | In vivo | Increase mechanical strength and new bone volume | [36] |
| In vitro |
3. Metformin Enhances Angiogenesis
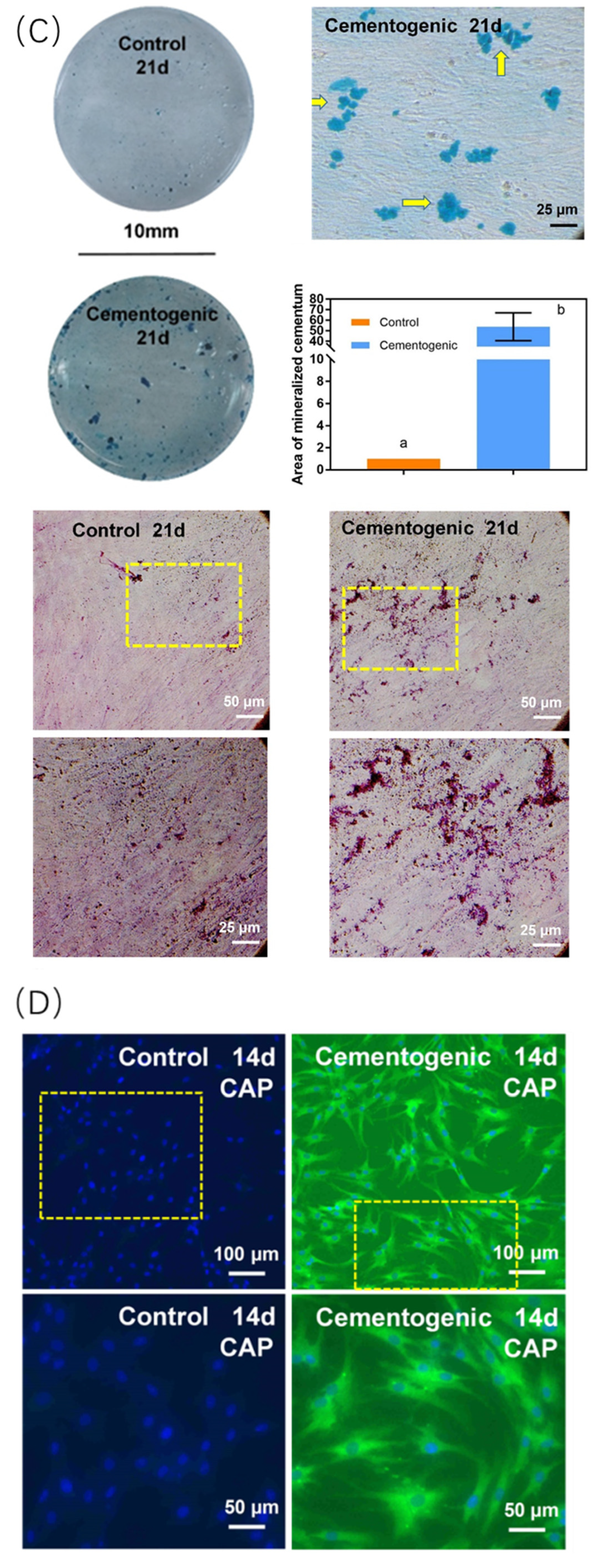
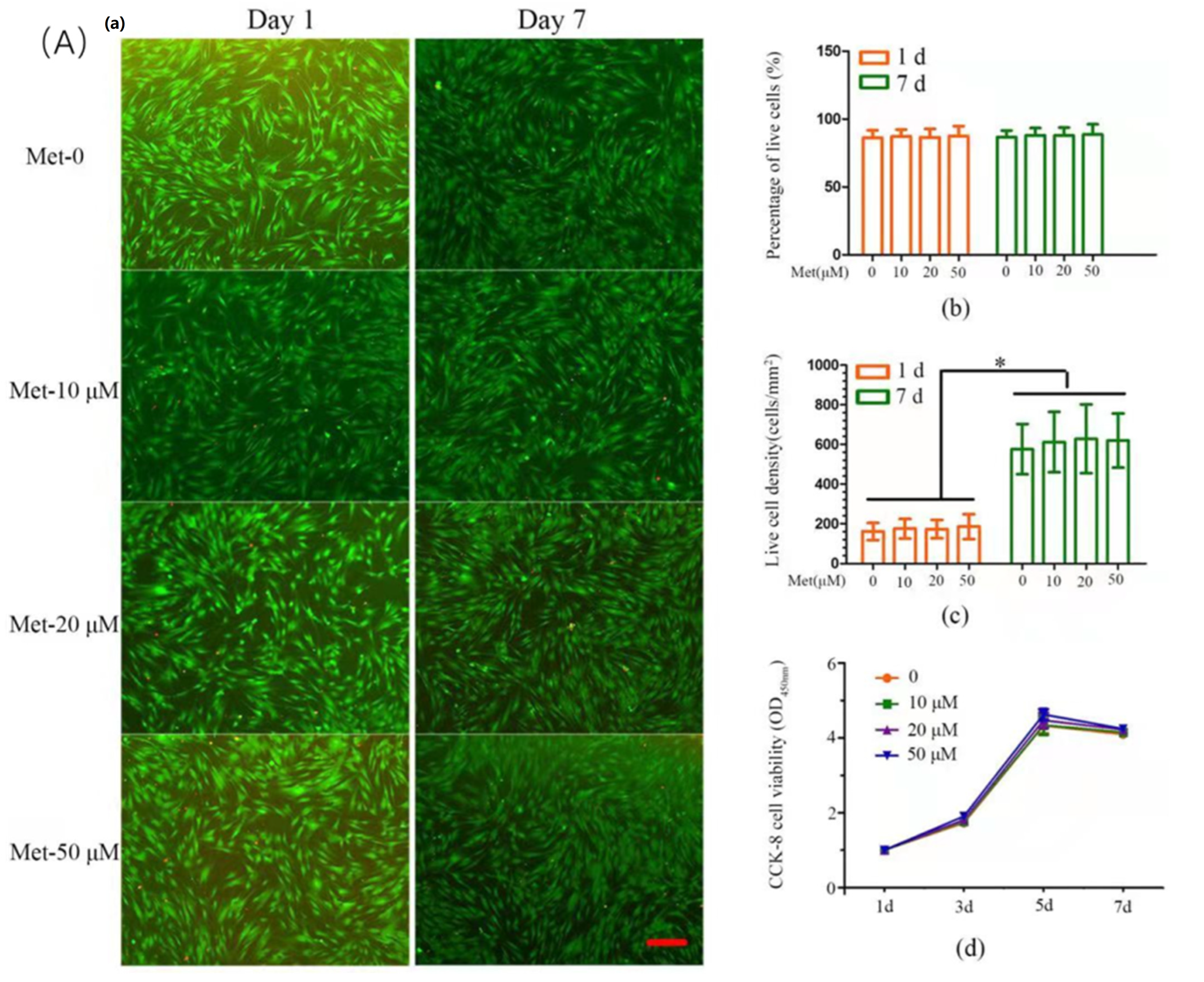
4. Effect of Metformin on Dental-Derived Stem Cells
5. Effect of Metformin in Other Cells and Biomaterials
6. Clinical Application of Metformin in Bone and Dental Tissue Regeneration and Development
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Triggle, C.R.; Mohammed, I.; Bshesh, K.; Marei, I.; Ye, K.; Ding, H.; MacDonald, R.; Hollenberg, M.D.; Hill, M.A. Metformin: Is it a drug for all reasons and diseases? Metabolism 2022, 133, 155223. [Google Scholar] [CrossRef] [PubMed]
- Kawakita, E.; Yang, F.; Kumagai, A.; Takagaki, Y.; Kitada, M.; Yoshitomi, Y.; Ikeda, T.; Nakamura, Y.; Ishigaki, Y.; Kanasaki, K.; et al. Metformin Mitigates DPP-4 Inhibitor-Induced Breast Cancer Metastasis via Suppression of mTOR Signaling. Mol. Cancer Res. 2021, 19, 61–73. [Google Scholar] [CrossRef] [PubMed]
- Al-Salameh, A.; Wiernsperger, N.; Cariou, B.; Lalau, J.-D. A comment on metformin and COVID-19 with regard to “Metformin use is associated with a decrease in the risk of hospitalization and mortality in COVID-19 patients with diabetes: A population-based study in Lombardy”. Diabetes Obes. Metab. 2022, 24, 1888. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.-K.; Weng, P.-W.; Chang, J.Z.-C.; Lin, Y.-W.; Tsuang, F.-Y.; Lin, F.-H.; Tsai, T.-H.; Sun, J.-S. Metformin-Incorporated Gelatin/Hydroxyapatite Nanofiber Scaffold for Bone Regeneration. Tissue Eng. Part A 2022, 28, 1–12. [Google Scholar] [CrossRef]
- Zhao, X.; Yang, Y.; Yu, J.; Ding, R.; Pei, D.; Zhang, Y.; He, G.; Cheng, Y.; Li, A. Injectable hydrogels with high drug loading through B-N coordination and ROS-triggered drug release for efficient treatment of chronic periodontitis in diabetic rats. Biomaterials 2022, 282, 121387. [Google Scholar] [CrossRef]
- Shen, M.; Yu, H.; Jin, Y.; Mo, J.; Sui, J.; Qian, X.; Chen, T. Metformin Facilitates Osteoblastic Differentiation and M2 Macrophage Polarization by PI3K/AKT/mTOR Pathway in Human Umbilical Cord Mesenchymal Stem Cells. Stem Cells Int. 2022, 2022, 9498876. [Google Scholar] [CrossRef]
- Sun, R.; Liang, C.; Sun, Y.; Xu, Y.; Geng, W.; Li, J. Effects of metformin on the osteogenesis of alveolar BMSCs from diabetic patients and implant osseointegration in rats. Oral Dis. 2022, 28, 1170–1180. [Google Scholar] [CrossRef]
- Leng, T.; Wang, Y.; Cheng, W.; Wang, W.; Qu, X.; Lei, B. Bioactive anti-inflammatory antibacterial metformin-contained hydrogel dressing accelerating wound healing. Biomater. Adv. 2022, 135, 212737. [Google Scholar] [CrossRef]
- Zhao, Z.; Liu, J.; Schneider, A.; Gao, X.; Ren, K.; Weir, M.D.; Zhang, N.; Zhang, K.; Zhang, L.; Bai, Y.; et al. Human periodontal ligament stem cell seeding on calcium phosphate cement scaffold delivering metformin for bone tissue engineering. J. Dent. 2019, 91, 103220. [Google Scholar] [CrossRef]
- Hu, Z.; Qiu, W.; Yu, Y.; Wu, X.; Fang, F.; Zhu, X.; Xu, X.; Tu, Q.; Van Dyke, T.E.; Morgan, E.F.; et al. Identification and Characterization of a Novel Long Noncoding RNA That Regulates Osteogenesis in Diet-Induced Obesity Mice. Front. Cell Dev. Biol. 2022, 10, 832460. [Google Scholar] [CrossRef]
- Bahrambeigi, S.; Yousefi, B.; Rahimi, M.; Shafiei-Irannejad, V. Metformin; an old antidiabetic drug with new potentials in bone disorders. Biomed. Pharmacother. 2019, 109, 1593–1601. [Google Scholar] [CrossRef] [PubMed]
- Shahrezaee, M.; Salehi, M.; Keshtkari, S.; Oryan, A.; Kamali, A.; Shekarchi, B. In vitro and in vivo investigation of PLA/PCL scaffold coated with metformin-loaded gelatin nanocarriers in regeneration of critical-sized bone defects. Nanomedicine 2018, 14, 2061–2073. [Google Scholar] [CrossRef]
- Ebrahimi, L.; Farzin, A.; Ghasemi, Y.; Alizadeh, A.; Goodarzi, A.; Basiri, A.; Zahiri, M.; Monabati, A.; Ai, J. Metformin-Loaded PCL/PVA Fibrous Scaffold Preseeded with Human Endometrial Stem Cells for Effective Guided Bone Regeneration Membranes. ACS Biomater. Sci. Eng. 2021, 7, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Liang, Q.; Kang, W.; Ge, S. Metformin facilitates the proliferation, migration, and osteogenic differentiation of periodontal ligament stem cells in vitro. Cell Biol. Int. 2020, 44, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Qian, H.; Kong, L.; Wang, W.; Wang, X.; Xu, Z.; Chai, Y.; Xu, J.; Kang, Q. Accelerated Bone Regeneration by Astragaloside IV through Stimulating the Coupling of Osteogenesis and Angiogenesis. Int. J. Biol. Sci. 2021, 17, 1821–1836. [Google Scholar] [CrossRef] [PubMed]
- Kusumbe, A.P.; Ramasamy, S.K.; Adams, R.H. Coupling of angiogenesis and osteogenesis by a specific vessel subtype in bone. Nature 2014, 507, 323–328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aghali, A. Craniofacial Bone Tissue Engineering: Current Approaches and Potential Therapy. Cells 2021, 10, 2993. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Liao, L.; Hu, Y.; Xu, Y.; Zhang, Y.; Huo, F.; Tian, W.; Guo, W. Identification of Type H Vessels in Mice Mandibular Condyle. J. Dent. Res. 2021, 100, 983–992. [Google Scholar] [CrossRef]
- Solimando, A.G.; Kalogirou, C.; Krebs, M. Angiogenesis as Therapeutic Target in Metastatic Prostate Cancer—Narrowing the Gap Between Bench and Bedside. Front. Immunol. 2022, 13, 842038. [Google Scholar] [CrossRef]
- Ren, Y.; Luo, H. Metformin: The next angiogenesis panacea? SAGE Open Med. 2021, 9, 20503121211001641. [Google Scholar] [CrossRef]
- Wang, J.; Zhu, L.; Hu, K.; Tang, Y.; Zeng, X.; Liu, J.; Xu, J. Effects of metformin treatment on serum levels of C-reactive protein and interleukin-6 in women with polycystic ovary syndrome: A meta-analysis: A PRISMA-compliant article. Medicine 2017, 96, e8183. [Google Scholar] [CrossRef] [PubMed]
- McCarty, M.F.; Lewis Lujan, L.; Iloki Assanga, S. Targeting Sirt1, AMPK, Nrf2, CK2, and Soluble Guanylate Cyclase with Nutraceuticals: A Practical Strategy for Preserving Bone Mass. Int. J. Mol. Sci. 2022, 23, 4776. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-C.; Peng, D.; Cai, Z.; Lin, H.-K. AMPK signaling and its targeting in cancer progression and treatment. Semin. Cancer Biol. 2022, 85, 52–68. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Tian, X.; Zhang, B.; Li, M.; Wang, Y.; Yang, C.; Wu, J.; Wei, X.; Qu, Q.; Yu, Y.; et al. Low-dose metformin targets the lysosomal AMPK pathway through PEN2. Nature 2022, 603, 159–165. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Jepsen, S.; Jin, L.; Otomo-Corgel, J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J. Clin. Periodontol. 2017, 44, 456–462. [Google Scholar] [CrossRef] [Green Version]
- Ming, P.; Rao, P.; Wu, T.; Yang, J.; Lu, S.; Yang, B.; Xiao, J.; Tao, G. Biomimetic Design and Fabrication of Sericin-Hydroxyapatite Based Membranes with Osteogenic Activity for Periodontal Tissue Regeneration. Front. Bioeng. Biotechnol. 2022, 10, 899293. [Google Scholar] [CrossRef]
- Uskoković, V.; Graziani, V.; Wu, V.M.; Fadeeva, I.V.; Fomin, A.S.; Presniakov, I.A.; Fosca, M.; Ortenzi, M.; Caminiti, R.; Rau, J.V. Gold is for the mistress, silver for the maid: Enhanced mechanical properties, osteoinduction and antibacterial activity due to iron doping of tricalcium phosphate bone cements. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 94, 798–810. [Google Scholar] [CrossRef]
- Zhao, Z.; Sun, Y.; Qiao, Q.; Zhang, L.; Xie, X.; Weir, M.D.; Schneider, A.; Xu, H.H.K.; Zhang, N.; Zhang, K.; et al. Human Periodontal Ligament Stem Cell and Umbilical Vein Endothelial Cell Co-Culture to Prevascularize Scaffolds for Angiogenic and Osteogenic Tissue Engineering. Int. J. Mol. Sci. 2021, 22, 12363. [Google Scholar] [CrossRef]
- Sanchez-Rangel, E.; Inzucchi, S.E. Metformin: Clinical use in type 2 diabetes. Diabetologia 2017, 60, 1586–1593. [Google Scholar] [CrossRef]
- Wang, P.; Ma, T.; Guo, D.; Hu, K.; Shu, Y.; Xu, H.H.K.; Schneider, A. Metformin induces osteoblastic differentiation of human induced pluripotent stem cell-derived mesenchymal stem cells. J. Tissue Eng. Regen. Med. 2018, 12, 437–446. [Google Scholar] [CrossRef]
- Al Jofi, F.E.; Ma, T.; Guo, D.; Schneider, M.P.; Shu, Y.; Xu, H.H.K.; Schneider, A. Functional organic cation transporters mediate osteogenic response to metformin in human umbilical cord mesenchymal stromal cells. Cytotherapy 2018, 20, 650–659. [Google Scholar] [CrossRef] [PubMed]
- Jang, W.G.; Kim, E.J.; Bae, I.-H.; Lee, K.-N.; Kim, Y.D.; Kim, D.-K.; Kim, S.-H.; Lee, C.-H.; Franceschi, R.T.; Choi, H.-S.; et al. Metformin induces osteoblast differentiation via orphan nuclear receptor SHP-mediated transactivation of Runx2. Bone 2011, 48, 885–893. [Google Scholar] [CrossRef] [PubMed]
- Smieszek, A.; Tomaszewski, K.A.; Kornicka, K.; Marycz, K. Metformin Promotes Osteogenic Differentiation of Adipose-Derived Stromal Cells and Exerts Pro-Osteogenic Effect Stimulating Bone Regeneration. J. Clin. Med. 2018, 7, 482. [Google Scholar] [CrossRef] [Green Version]
- Jia, L.; Xiong, Y.; Zhang, W.; Ma, X.; Xu, X. Metformin promotes osteogenic differentiation and protects against oxidative stress-induced damage in periodontal ligament stem cells via activation of the Akt/Nrf2 signaling pathway. Exp. Cell Res. 2020, 386, 111717. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Xia, Y.; Ma, T.; Weir, M.D.; Ren, K.; Reynolds, M.A.; Shu, Y.; Cheng, L.; Schneider, A.; Xu, H.H.K. Novel metformin-containing resin promotes odontogenic differentiation and mineral synthesis of dental pulp stem cells. Drug Deliv. Transl. Res. 2019, 9, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Zhang, T.; Chen, Y.; Xu, Y.; Deng, Z.; Xu, D. Local Administration of Metformin Improves Bone Microarchitecture and Biomechanical Properties During Ruptured Canine Achilles Tendon-Calcaneus Interface Healing. Am. J. Sport. Med. 2022, 50, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Hu, K.; Liu, X.; Reynolds, M.A.; Bao, C.; Wang, P.; Zhao, L.; Xu, H.H.K. Novel hiPSC-based tri-culture for pre-vascularization of calcium phosphate scaffold to enhance bone and vessel formation. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 79, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Xu, T.; Huang, G.; Jiang, S.; Gu, Y.; Chen, F. Oral microbiomes: More and more importance in oral cavity and whole body. Protein Cell 2018, 9, 488–500. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Zhao, Z.; Ruan, J.; Weir, M.D.; Ma, T.; Ren, K.; Schneider, A.; Oates, T.W.; Li, A.; Zhao, L.; et al. Stem cells in the periodontal ligament differentiated into osteogenic, fibrogenic and cementogenic lineages for the regeneration of the periodontal complex. J. Dent. 2020, 92, 103259. [Google Scholar] [CrossRef]
- Qing, L.; Fu, J.; Wu, P.; Zhou, Z.; Yu, F.; Tang, J. Metformin induces the M2 macrophage polarization to accelerate the wound healing via regulating AMPK/mTOR/NLRP3 inflammasome singling pathway. Am. J. Transl. Res. 2019, 11, 655–668. [Google Scholar]
- Takahashi, N.; Shibata, R.; Ouchi, N.; Sugimoto, M.; Murohara, T.; Komori, K. Metformin stimulates ischemia-induced revascularization through an eNOS dependent pathway in the ischemic hindlimb mice model. J. Vasc. Surg. 2015, 61, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Xu, J.; Zhao, M.; Luo, H.; Lin, M.; Luo, Y.; Li, Y.; He, H.; Wu, J. Adhesive, injectable, and ROS-responsive hybrid polyvinyl alcohol (PVA) hydrogel co-delivers metformin and fibroblast growth factor 21 (FGF21) for enhanced diabetic wound repair. Front. Bioeng. Biotechnol. 2022, 10, 968078. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Lin, F.; Wan, Q.; Wu, J.; Luo, M. Mechanisms of action of metformin and its regulatory effect on microRNAs related to angiogenesis. Pharmacol. Res. 2021, 164, 105390. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Qin, Y.; Wang, Y.; Meng, S.; Xian, H.; Che, H.; Lv, J.; Li, Y.; Yu, Y.; Bai, Y.; et al. Metformin Inhibits the NLRP3 Inflammasome via AMPK/mTOR-dependent Effects in Diabetic Cardiomyopathy. Int. J. Biol. Sci. 2019, 15, 1010–1019. [Google Scholar] [CrossRef] [Green Version]
- Lei, T.; Deng, S.; Chen, P.; Xiao, Z.; Cai, S.; Hang, Z.; Yang, Y.; Zhang, X.; Li, Q.; Du, H. Metformin enhances the osteogenesis and angiogenesis of human umbilical cord mesenchymal stem cells for tissue regeneration engineering. Int. J. Biochem. Cell Biol. 2021, 141, 106086. [Google Scholar] [CrossRef]
- Deng, S.; Lei, T.; Chen, H.; Zheng, H.; Xiao, Z.; Cai, S.; Hang, Z.; Xiong, W.; Yu, Y.; Zhang, X.; et al. Metformin pre-treatment of stem cells from human exfoliated deciduous teeth promotes migration and angiogenesis of human umbilical vein endothelial cells for tissue engineering. Cytotherapy 2022, 24, 1095–1104. [Google Scholar] [CrossRef]
- Yang, Z.; Gao, X.; Zhou, M.; Kuang, Y.; Xiang, M.; Li, J.; Song, J. Effect of metformin on human periodontal ligament stem cells cultured with polydopamine-templated hydroxyapatite. Eur. J. Oral Sci. 2019, 127, 210–221. [Google Scholar] [CrossRef]
- Han, H.; Hou, Y.; Chen, X.; Zhang, P.; Kang, M.; Jin, Q.; Ji, J.; Gao, M. Metformin-Induced Stromal Depletion to Enhance the Penetration of Gemcitabine-Loaded Magnetic Nanoparticles for Pancreatic Cancer Targeted Therapy. J. Am. Chem. Soc. 2020, 142, 4944–4954. [Google Scholar] [CrossRef]
- Chen, P.; Cao, Y.; Chen, S.; Liu, Z.; Chen, S.; Guo, Y. Association of and Polymorphisms with Metformin Efficacy in Type 2 Diabetic Patients. Biomedicines 2022, 10, 2546. [Google Scholar] [CrossRef]
- Li, S.; Xu, B.; Fan, S.; Kang, B.; Deng, L.; Chen, D.; Yang, B.; Tang, F.; He, Z.; Xue, Y.; et al. Effects of single-nucleotide polymorphism on the pharmacokinetics and pharmacodynamics of metformin. Expert Rev. Clin. Pharmacol. 2022, 15, 1107–1117. [Google Scholar] [CrossRef]
- Qin, W.; Gao, X.; Ma, T.; Weir, M.D.; Zou, J.; Song, B.; Lin, Z.; Schneider, A.; Xu, H.H.K. Metformin Enhances the Differentiation of Dental Pulp Cells into Odontoblasts by Activating AMPK Signaling. J. Endod. 2018, 44, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Jia, X.; Fang, D.; Cheng, Y.; Zhai, Z.; Deng, W.; Du, B.; Lu, T.; Wang, L.; Yang, C.; et al. Metformin Inhibits Lipid Droplets Fusion and Growth via Reduction in Cidec and Its Regulatory Factors in Rat Adipose-Derived Stem Cells. Int. J. Mol. Sci. 2022, 23, 5986. [Google Scholar] [CrossRef]
- Zhang, M.; Yang, B.; Peng, S.; Xiao, J. Metformin Rescues the Impaired Osteogenesis Differentiation Ability of Rat Adipose-Derived Stem Cells in High Glucose by Activating Autophagy. Stem Cells Dev. 2021, 30, 1017–1027. [Google Scholar] [CrossRef] [PubMed]
- Phung, S.; Lee, C.; Hong, C.; Song, M.; Yi, J.K.; Stevenson, R.G.; Kang, M.K.; Shin, K.H.; Park, N.H.; Kim, R.H. Effects of Bioactive Compounds on Odontogenic Differentiation and Mineralization. J. Dent. Res. 2017, 96, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Qin, W.; Chen, J.-Y.; Guo, J.; Ma, T.; Weir, M.D.; Guo, D.; Shu, Y.; Lin, Z.-M.; Schneider, A.; Xu, H.H.K. Novel Calcium Phosphate Cement with Metformin-Loaded Chitosan for Odontogenic Differentiation of Human Dental Pulp Cells. Stem Cells Int. 2018, 2018, 7173481. [Google Scholar] [CrossRef]
- Zhao, X.; Pathak, J.L.; Huang, W.; Zhu, C.; Li, Y.; Guan, H.; Zeng, S.; Ge, L.; Shu, Y. Metformin enhances osteogenic differentiation of stem cells from human exfoliated deciduous teeth through AMPK pathway. J. Tissue Eng. Regen. Med. 2020, 14, 1869–1879. [Google Scholar] [CrossRef]
- Qu, L.; Dubey, N.; Ribeiro, J.S.; Bordini, E.A.F.; Ferreira, J.A.; Xu, J.; Castilho, R.M.; Bottino, M.C. Metformin-loaded nanospheres-laden photocrosslinkable gelatin hydrogel for bone tissue engineering. J. Mech. Behav. Biomed. Mater. 2021, 116, 104293. [Google Scholar] [CrossRef]
- Tao, L.Y.; Łagosz-Ćwik, K.B.; Hogervorst, J.M.A.; Schoenmaker, T.; Grabiec, A.M.; Forouzanfar, T.; van der Weijden, F.A.; de Vries, T.J. Diabetes Medication Metformin Inhibits Osteoclast Formation and Activity in Models for Periodontitis. Front. Cell Dev. Biol. 2021, 9, 777450. [Google Scholar] [CrossRef]
- Codispoti, B.; Marrelli, M.; Paduano, F.; Tatullo, M. NANOmetric BIO-Banked MSC-Derived Exosome (NANOBIOME) as a Novel Approach to Regenerative Medicine. J. Clin. Med. 2018, 7, 357. [Google Scholar] [CrossRef] [Green Version]
- Śmieszek, A.; Czyrek, A.; Basinska, K.; Trynda, J.; Skaradzińska, A.; Siudzińska, A.; Marędziak, M.; Marycz, K. Effect of Metformin on Viability, Morphology, and Ultrastructure of Mouse Bone Marrow-Derived Multipotent Mesenchymal Stromal Cells and Balb/3T3 Embryonic Fibroblast Cell Line. Biomed. Res. Int. 2015, 2015, 769402. [Google Scholar] [CrossRef] [Green Version]
- Tao, T.; Deng, P.; Wang, Y.; Zhang, X.; Guo, Y.; Chen, W.; Qin, J. Microengineered Multi-Organoid System from hiPSCs to Recapitulate Human Liver-Islet Axis in Normal and Type 2 Diabetes. Adv. Sci. 2022, 9, e2103495. [Google Scholar] [CrossRef]
- Mannix, A.J.; Zhang, Z.; Guisinger, N.P.; Yakobson, B.I.; Hersam, M.C. Borophene as a prototype for synthetic 2D materials development. Nat. Nanotechnol. 2018, 13, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Tatullo, M.; Genovese, F.; Aiello, E.; Amantea, M.; Makeeva, I.; Zavan, B.; Rengo, S.; Fortunato, L. Phosphorene Is the New Graphene in Biomedical Applications. Materials 2019, 12, 2301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tatullo, M.; Zavan, B.; Genovese, F.; Codispoti, B.; Makeeva, I.; Rengo, S.; Fortunato, L.; Spagnuolo, G. Borophene Is a Promising 2D Allotropic Material for Biomedical Devices. Appl. Sci. 2019, 9, 3446. [Google Scholar] [CrossRef] [Green Version]
- Yagci, B.S.; Odabas, S.; Aksoy, E.A. Development of metformin chain extended polyurethane elastomers as bone regenerative films. Eur. J. Pharm. Sci. 2019, 131, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Moraschini, V.; Fujioka-Kobayashi, M.; Zhang, Y.; Kawase, T.; Cosgarea, R.; Jepsen, S.; Bishara, M.; Canullo, L.; Shirakata, Y.; et al. Use of platelet-rich fibrin for the treatment of periodontal intrabony defects: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 2461–2478. [Google Scholar] [CrossRef]
- Tan, W.; Gao, C.; Feng, P.; Liu, Q.; Liu, C.; Wang, Z.; Deng, Y.; Shuai, C. Dual-functional scaffolds of poly(L-lactic acid)/nanohydroxyapatite encapsulated with metformin: Simultaneous enhancement of bone repair and bone tumor inhibition. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 120, 111592. [Google Scholar] [CrossRef]
- Fang, C.-H.; Sun, C.-K.; Lin, Y.-W.; Hung, M.-C.; Lin, H.-Y.; Li, C.-H.; Lin, I.P.; Chang, H.-C.; Sun, J.-S.; Chang, J.Z.-C. Metformin-Incorporated Gelatin/Nano-Hydroxyapatite Scaffolds Promotes Bone Regeneration in Critical Size Rat Alveolar Bone Defect Model. Int. J. Mol. Sci. 2022, 23, 558. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, M.; Zhao, Z.; Xu, H.H.K.; Dai, Z.; Yu, K.; Xiao, L.; Schneider, A.; Weir, M.D.; Oates, T.W.; Bai, Y.; et al. Effects of Metformin Delivery via Biomaterials on Bone and Dental Tissue Engineering. Int. J. Mol. Sci. 2022, 23, 15905. https://doi.org/10.3390/ijms232415905
Zhu M, Zhao Z, Xu HHK, Dai Z, Yu K, Xiao L, Schneider A, Weir MD, Oates TW, Bai Y, et al. Effects of Metformin Delivery via Biomaterials on Bone and Dental Tissue Engineering. International Journal of Molecular Sciences. 2022; 23(24):15905. https://doi.org/10.3390/ijms232415905
Chicago/Turabian StyleZhu, Minjia, Zeqing Zhao, Hockin H. K. Xu, Zixiang Dai, Kan Yu, Le Xiao, Abraham Schneider, Michael D. Weir, Thomas W. Oates, Yuxing Bai, and et al. 2022. "Effects of Metformin Delivery via Biomaterials on Bone and Dental Tissue Engineering" International Journal of Molecular Sciences 23, no. 24: 15905. https://doi.org/10.3390/ijms232415905
APA StyleZhu, M., Zhao, Z., Xu, H. H. K., Dai, Z., Yu, K., Xiao, L., Schneider, A., Weir, M. D., Oates, T. W., Bai, Y., & Zhang, K. (2022). Effects of Metformin Delivery via Biomaterials on Bone and Dental Tissue Engineering. International Journal of Molecular Sciences, 23(24), 15905. https://doi.org/10.3390/ijms232415905








