Niclosamide as a Promising Therapeutic Player in Human Cancer and Other Diseases
Abstract
:1. Introduction
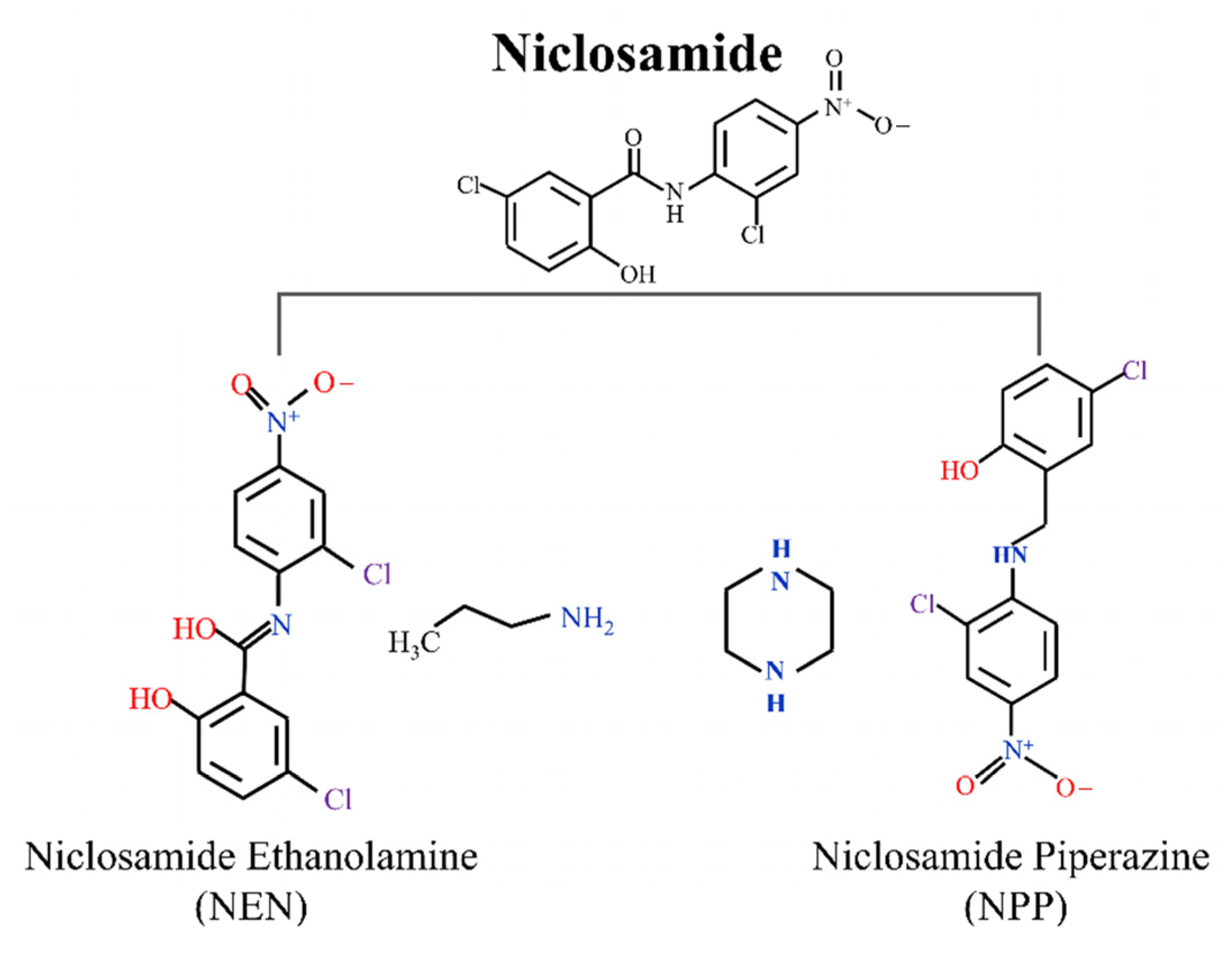
2. NIC and Its Salt Forms
2.1. NIC Ethanolamine Salt (NEN)
2.2. NIC Piperazine (NPP)
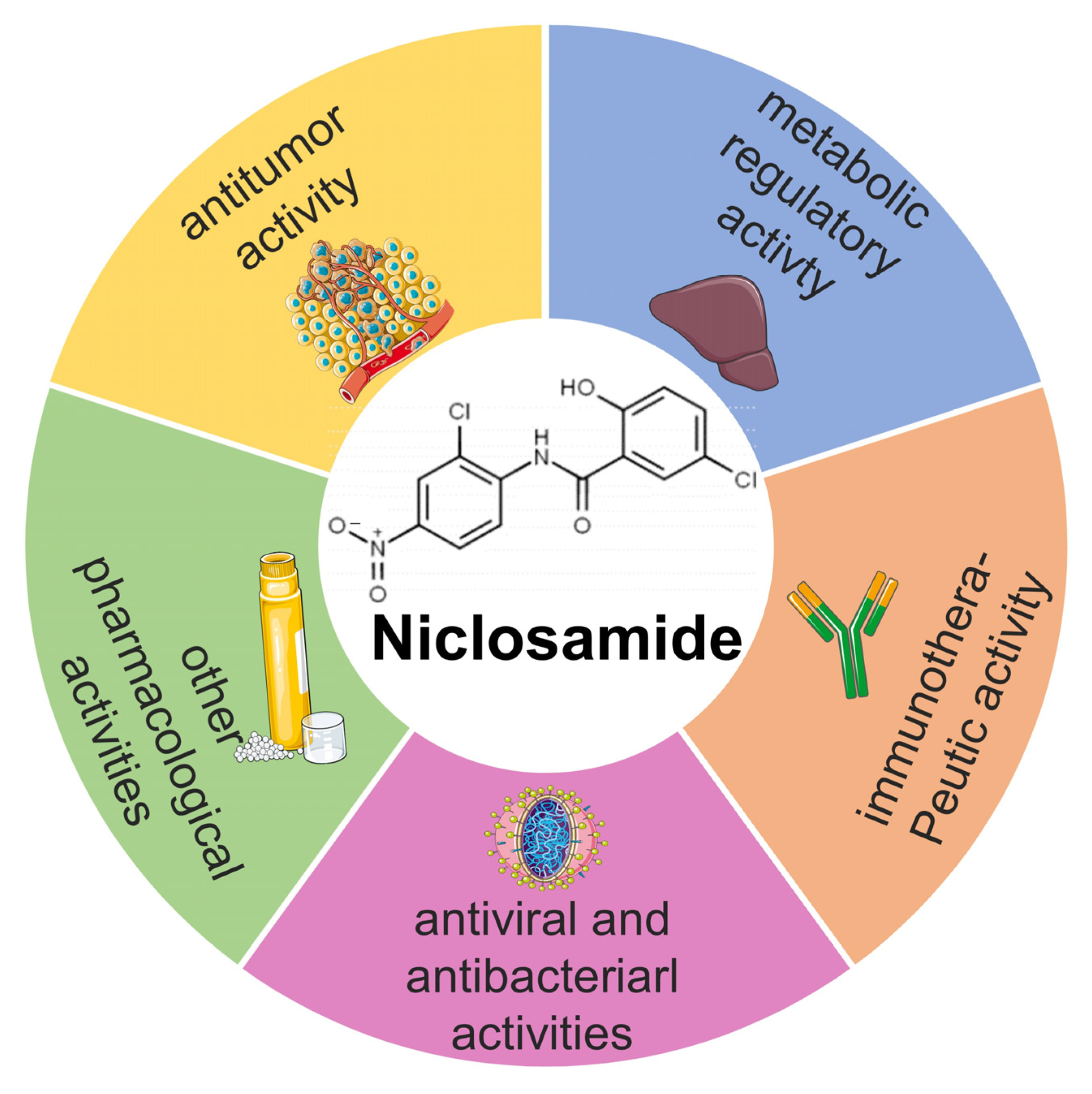
3. The Multifaceted Pharmaceutical Activities of NIC
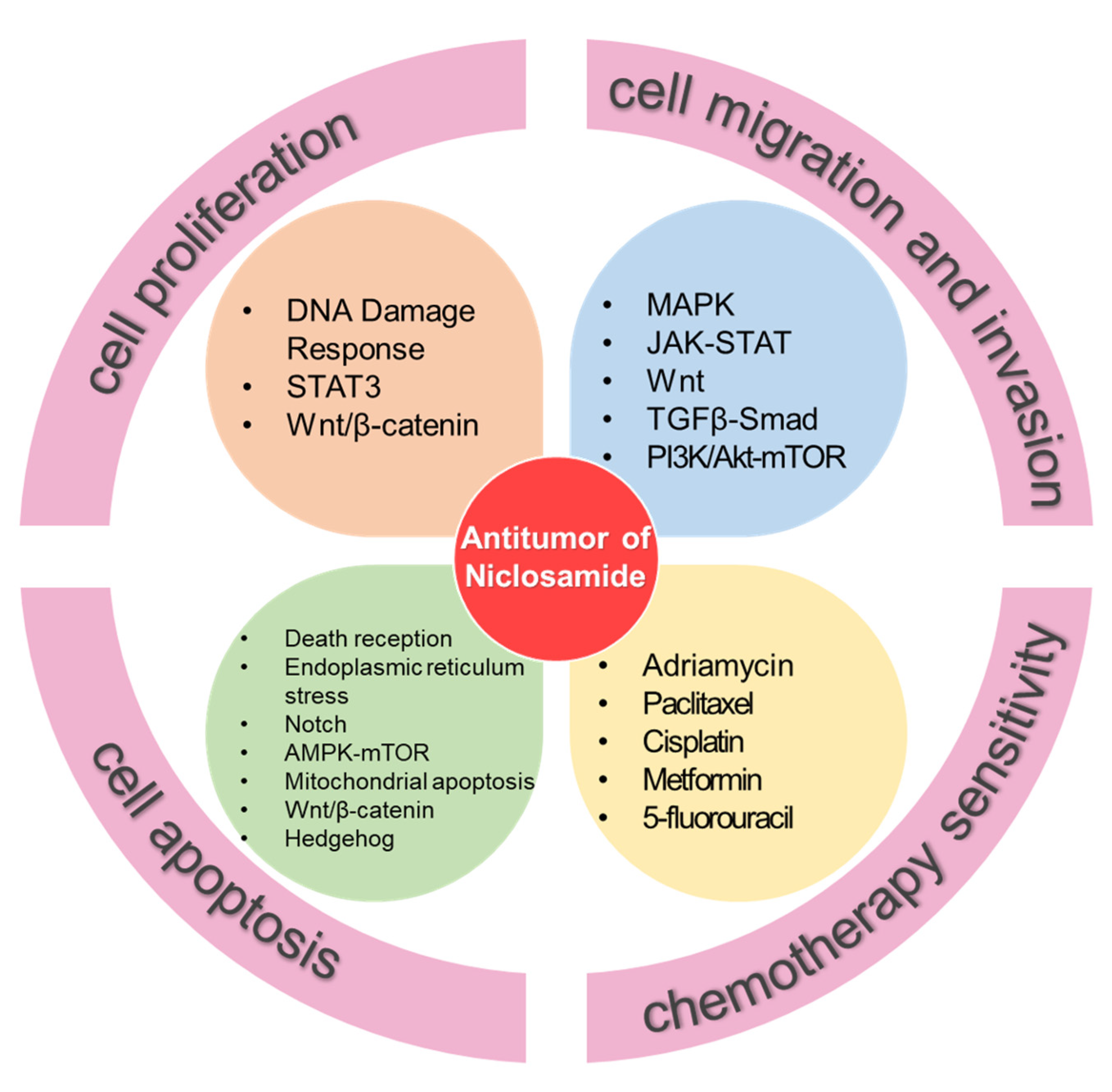
3.1. The Anti-Tumor Activity of NIC
3.1.1. NIC Inhibits Tumor Cell Proliferation
3.1.2. NIC Inhibits Tumor Cell Migration and Invasion
3.1.3. NIC Promotes Tumor Cell Apoptosis
3.1.4. NIC Regulates Cancer Cell Stemness
3.1.5. NIC Sensitizes Tumor Cells to Chemotherapy and Immunotherapy
| Name | Mechanism | References |
|---|---|---|
| Leukemia | Inhibition of proliferation by inhibiting the Wnt/β-catenin signaling pathway and downregulating phosphorylated CREB, STAT5, and Akt expression. Induction of apoptosis by disabling Sp1. | [38,39] |
| Nasopharyngeal carcinoma | Inhibition of proliferation by downregulating ku70/80 expression. | [40] |
| Hepatoma | Inhibition of proliferation by inhibiting the STAT3 signaling pathway. | [41] |
| Colorectal cancer | Inhibition of proliferation by downregulating DCLK1 expression. Induction of apoptosis by reducing DCLK1-B, Mcl-1, and survivin expression; inhibiting the Notch signaling pathway; and upregulating miR-200 family members’ expression. Prevention of chemotherapeutic resistance by inhibiting Wnt, Hippo, and YAP. | [42,62,82] |
| Colon cancer | Inhibition of proliferation by promoting mitochondrial decoupling. | [16,25,43] |
| Prostate cancer | Inhibition of proliferation and induction of apoptosis by inhibiting the FOXM1-mediated DNA damage response. Inhibition of migration and invasion by inhibiting the IL6–STAT3–AR axis. | [44,58] |
| Breast cancer | Inhibition of proliferation by inhibiting STAT3 activation markers pY705 and pS727 and reducing the STAT3 dimerization capacity. Inhibition of migration and invasion by inhibiting the interleukin-6/STAT3 signaling axis. Prevention of chemotherapeutic resistance by targeting ROS and Wnt/β-catenin. | [45,51,79] |
| Osteosarcoma | Inhibition of migration and invasion by inhibiting the Wnt–Axin2–Snail cascade. | [52] |
| Melanoma | Inhibition of migration and invasion by inhibiting p-STAT3 expression. Induction of apoptosis by regulating the AMPK–mTOR pathway. | [53,63] |
| Hepatocellular carcinoma | Inhibition of migration and invasion by inhibiting CD10 expression. | [54] |
| Glioma | Inhibition of migration and invasion by overexpressing ALK4 (NIC). | [55] |
| Oral squamous cell carcinoma | Inhibition of migration and invasion by inhibiting the let-7a/STAT3 axis. | [56] |
| Lung cancer | Inhibition of migration and invasion by blocking S100A4 expression. Induction of apoptosis by activating caspases. Enhances immunotherapy efficiency by enhancing PD-L1 antibodies. | [59,61,90] |
| Chondrosarcoma | Induction of apoptosis by activating the caspase-dependent mitochondrial apoptotic pathway. | [64] |
| Esophageal cancer | Induction of apoptosis by inhibiting the Wnt/β–catenin signaling pathway. | [65] |
| Thyroid cancer | Induction of apoptosis by activating Bax and caspase-3 and suppressing Bcl-2 and mitochondrial membrane potential (ΔYm). | [66] |
| Pancreatic cancer | Induction of apoptosis by targeting the p-GSK3β-mediated non-canonical Hedgehog signaling pathway. | [67] |
3.1.6. NIC’s Formulations for Treating Cancer
3.2. The Metabolic Regulatory Activity of NIC
3.3. The Immune Disease Therapeutic Activity of NIC
3.4. The Anti-Infective Activity of NIC
3.4.1. The Antiviral Activity of NIC
3.4.2. The Antibacterial Activity of NIC
3.5. The Other Pharmacological Activities of NIC
| Diseases | Mechanism | References | |
|---|---|---|---|
| Metabolic Syndrome | Diabetes | Downregulation of the mTOR/4E-BP1 signaling pathway in type 1 diabetes. Inhibition of glucagon signaling in type 2 diabetes. | [15,19,101] |
| Nonalcoholic steatohepatitis | Induction of the AMPK-mediated phosphorylation of p62 (S351). | [25] | |
| Non-alcoholic fatty liver disease | Induction of the AMPK-mediated phosphorylation of p62 at S351 to cause atypical Nrf2 activation. | [25] | |
| Acute lipotoxic stress | Induction of the p62-dependent Keap1–Nrf2 signaling pathway. | [25] | |
| Immune system diseases | Rheumatoid arthritis | Induction of apoptosis by reducing TNF-α-induced cytokine expression, MAP kinase production, and the IKK/NF-κB signaling activity. | [105,106,107,108] |
| Graft-versus-host disease | Inhibition of the STAT3, Wnt/β-catenin, ERK1/2, AKT, and Notch signaling pathway. | [103] | |
| Systemic lupus erythematosus and lupus nephritis | Reduction of urinary protein excretion. Restoring the redox imbalance. Promotion of mitochondrial production. Improvement of renal energy imbalance. | [17] | |
| Swollen lymph nodesand splenomegaly | Reduction of serum anti-dsDNA antibody levels. | [17] | |
| Other types | Athma | Activation of the AMPK pathway. Inhibition of bronchial smooth muscle cell proliferation and migration by inhibiting the STAT3 pathway. | [21] |
| Arterial constriction | Effect on smooth muscle contraction. | [14,126] | |
| Myopia | Inhibition of the Wnt signaling pathway. | [127] | |
| Diseases | Mechanism | References | |
|---|---|---|---|
| Virus | Coronavirus | Inhibition of MERS-CoV and SARS-CoV replication and viral antigen synthesis. | [117,118] |
| Zika virus | Inhibition of Zika virus replication. | [119,120] | |
| Japanese encephalitis virus | Inhibition of proliferation. | [111] | |
| Hepatitis C virus | Inhibition of the replication of HCV host cells. | [121] | |
| Human rhinovirus | Blocks the acidification of the endolysosomal compartment. | [113] | |
| Chikungunya virus | Block the entry of low-pH-dependent CHIKV. | [114] | |
| Human adenovirus | Inhibition of the transport of HADV particles from the endosome to the nuclear membrane. | [122] | |
| Epstein–Barr virus | Inhibition of irreversible cell cycle arrest activated by mTOR. | [116] | |
| Bacteria | Tuberculosis | Effects on the cell-mediated immune response. | [123] |
| Pseudomonas aeruginosa | Not clear | [124] | |
| Staphylococcus aureus | Not clear | [125] | |
4. Conclusions and Future Perspectives
5. Outstanding Questions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NIC | Niclosamide |
| NEN | Niclosamide alcohol amine salt |
| NPP | Niclosamide pipera-zine |
| NASH | Nonalcoholic steatohepatitis |
| AR | Androgen receptor |
| ER | Endoplasmic reticulum |
| CRPC | Castration-resistant prostate cancer |
| NCSLC | Non-small-cell lung cancer |
| OHPP | Octenylsuccinate hydroxypropyl phytoglycogen |
| CPs | Chimeric polypeptides |
| NIC-NCT | Co-crystals of niclosamide-nicotinamide |
| NSPT | Niclosamide stearate prodrug therapeutic |
| Nano-NIC | Nanosuspension of niclosamide |
| NLM-NCs | Niclosamide nanocrystals |
| SARS | Severe acute respiratory syndrome coronavirus |
| MERS-CoV | Middle East respiratory syndrome coronavirus |
| ZIKV | Zika virus |
| JEV | Japanese encephalitis virus |
| HCV | Hepatitis C V |
| EBOV | Ebola virus |
| HRV | Human rhinovirus |
| CHIKV | Chikungunya virus |
| HADV | Human adenovirus |
| EBV | Epstein–Barr virus |
| CPE | Cytopathic effect |
| FDA | Food and Drug Administration |
| WHO | The World Health Organization |
| ROS | Reactive oxygen species |
| T2D | Type 2 diabetes |
| CRC | Colorectal cancer |
| NPC | Nasopharyngeal cancer |
| AML | Acute myeloid leukemia |
| CML | Chronic myeloid leukemia |
| HCC | Hepatocellular carcinoma |
| EMT | Epithelial–mesenchymal transition |
| CSCs | Cancer stem cells |
| d-TPP | Dodecyl-TPP |
| TOS | Tumorospheres |
| CTC | Circulating tumor cell |
| MCTS | Multicellular tumor spheroid |
| SPS | Side population spheres |
| CDKs | Cyclin-dependant kinase |
| TID | Ter in die |
| GVHD | Graft versus host disease |
References
- Andrews, P.; Thyssen, J.; Lorke, D. The biology and toxicology of molluscicides, Bayluscide. Pharmacol. Ther. 1982, 19, 245–295. [Google Scholar] [CrossRef] [PubMed]
- Pearson, R.D.; Hewlett, E.L. Niclosamide therapy for tapeworm infections. Ann. Intern. Med. 1985, 102, 550–551. [Google Scholar] [CrossRef] [PubMed]
- Drugs for parasitic infections. Med. Lett. Drugs Ther. 1986, 28, 9–16.
- Wilkie, M.P.; Hubert, T.D.; Boogaard, M.A.; Birceanu, O. Control of invasive sea lampreys using the piscicides TFM and niclosamide: Toxicology, successes & future prospects. Aquat. Toxicol. 2019, 211, 235–252. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Weiss, A.; Goodman, J.; Fisk, M.; Kulkarni, S.; Lu, I.; Gray, J.; Smith, R.; Sommer, M.; Cheriyan, J. Niclosamide—A promising treatment for COVID-19. Br. J. Pharmacol. 2022, 179, 3250–3267. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Shi, P.Y.; Li, H.; Zhou, J. Broad Spectrum Antiviral Agent Niclosamide and Its Therapeutic Potential. ACS Infect. Dis. 2020, 6, 909–915. [Google Scholar] [CrossRef]
- Jiao, Y.; Chen, C.; Hu, X.; Feng, X.; Shi, Z.; Cao, J.; Li, Q.; Zhu, Y. Niclosamide and its derivative DK-520 inhibit RANKL-induced osteoclastogenesis. FEBS Open Bio 2020, 10, 1685–1697. [Google Scholar] [CrossRef]
- Choi, H.I.; Kim, T.; Lee, S.W.; Woo Kim, J.; Ju Noh, Y.; Kim, G.Y.; Jin Park, H.; Chae, Y.J.; Lee, K.R.; Kim, S.J.; et al. Bioanalysis of niclosamide in plasma using liquid chromatography-tandem mass and application to pharmacokinetics in rats and dogs. J. Chromatogr. B 2021, 1179, 122862. [Google Scholar] [CrossRef]
- Arshad, U.; Pertinez, H.; Box, H.; Tatham, L.; Rajoli, R.K.; Neary, M.; Sharp, J.; Valentijn, A.; Hobson, J.; Unsworth, C.; et al. Optimisation and validation of a sensitive bioanalytical method for niclosamide. bioRxiv 2021. [CrossRef]
- Fan, X.; Li, H.; Ding, X.; Zhang, Q.Y. Contributions of Hepatic and Intestinal Metabolism to the Disposition of Niclosamide, a Repurposed Drug with Poor Bioavailability. Drug Metab. Dispos. 2019, 47, 756–763. [Google Scholar] [CrossRef]
- Bhanushali, J.S.; Dhiman, S.; Nandi, U.; Bharate, S.S. Molecular interactions of niclosamide with hydroxyethyl cellulose in binary and ternary amorphous solid dispersions for synergistic enhancement of water solubility and oral pharmacokinetics in rats. Int. J. Pharm. 2022, 626, 122144. [Google Scholar] [CrossRef] [PubMed]
- Giri, A.K.; Adhikari, N.; Khan, K.A. Comparative genotoxicity of six salicylic acid derivatives in bone marrow cells of mice. Mutat. Res. 1996, 370, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gemmell, M.A.; Johnstone, P.D.; Oudemans, G. The effect of niclosamide on Echinococcus granulosus, Taenia hydatigena and Taenia ovis infections in dogs. Res. Vet. Sci. 1977, 22, 389–391. [Google Scholar] [CrossRef] [PubMed]
- Li, S.L.; Yan, J.; Zhang, Y.Q.; Zhen, C.L.; Liu, M.Y.; Jin, J.; Gao, J.L.; Xiao, X.L.; Shen, X.; Tai, Y.; et al. Niclosamide ethanolamine inhibits artery constriction. Pharm. Res. 2017, 115, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Tao, H.; Zhang, Y.; Zeng, X.; Shulman, G.I.; Jin, S. Niclosamide ethanolamine-induced mild mitochondrial uncoupling improves diabetic symptoms in mice. Nat. Med. 2014, 20, 1263–1269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alasadi, A.; Chen, M.; Swapna, G.V.T.; Tao, H.; Guo, J.; Collantes, J.; Fadhil, N.; Montelione, G.T.; Jin, S. Effect of mitochondrial uncouplers niclosamide ethanolamine (NEN) and oxyclozanide on hepatic metastasis of colon cancer. Cell Death Dis. 2018, 9, 215. [Google Scholar] [CrossRef] [Green Version]
- Han, P.; Weng, W.; Chen, Y.; Cai, Y.; Wang, Y.; Wang, M.; Zhan, H.; Yuan, C.; Yu, X.; Shao, M.; et al. Niclosamide ethanolamine attenuates systemic lupus erythematosus and lupus nephritis in MRL/lpr mice. Am. J. Transl. Res. 2020, 12, 5015–5031. [Google Scholar]
- Chen, B.; Wei, W.; Ma, L.; Yang, B.; Gill, R.M.; Chua, M.S.; Butte, A.J.; So, S. Computational Discovery of Niclosamide Ethanolamine, a Repurposed Drug Candidate That Reduces Growth of Hepatocellular Carcinoma Cells In Vitro and in Mice by Inhibiting Cell Division Cycle 37 Signaling. Gastroenterology 2017, 152, 2022–2036. [Google Scholar] [CrossRef]
- Han, P.; Zhan, H.; Shao, M.; Wang, W.; Song, G.; Yu, X.; Zhang, C.; Ge, N.; Yi, T.; Li, S.; et al. Niclosamide ethanolamine improves kidney injury in db/db mice. Diabetes Res. Clin. Pr. 2018, 144, 25–33. [Google Scholar] [CrossRef]
- Pei, X.; Zheng, F.; Li, Y.; Lin, Z.; Han, X.; Feng, Y.; Tian, Z.; Ren, D.; Cao, K.; Li, C. Niclosamide Ethanolamine Salt Alleviates Idiopathic Pulmonary Fibrosis by Modulating the PI3K-mTORC1 Pathway. Cells 2022, 11, 346. [Google Scholar] [CrossRef]
- Wei, Y.Y.; Xuan, X.C.; Zhang, X.Y.; Guo, T.T.; Dong, D.L. Niclosamide ethanolamine induces trachea relaxation and inhibits proliferation and migration of trachea smooth muscle cells. Eur. J. Pharm. 2019, 853, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Weng, W.; Liu, H.; Sun, Z.; Zhou, P.; Yu, X.; Shao, M.; Han, P.; Sun, H. Combined treatment with niclosamide ethanolamine and artemether combination improves type 1 diabetes via the targeting of liver mitochondria. Exp. Med. 2022, 23, 239. [Google Scholar] [CrossRef]
- Han, P.; Shao, M.; Guo, L.; Wang, W.; Song, G.; Yu, X.; Zhang, C.; Ge, N.; Yi, T.; Li, S.; et al. Niclosamide ethanolamine improves diabetes and diabetic kidney disease in mice. Am. J. Transl. Res. 2018, 10, 1071–1084. [Google Scholar] [PubMed]
- Han, P.; Yuan, C.; Wang, Y.; Wang, M.; Weng, W.; Zhan, H.; Yu, X.; Wang, T.; Li, Y.; Yi, W.; et al. Niclosamide ethanolamine protects kidney in adriamycin nephropathy by regulating mitochondrial redox balance. Am. J. Transl. Res. 2019, 11, 855–864. [Google Scholar] [PubMed]
- Park, J.S.; Lee, Y.S.; Lee, D.H.; Bae, S.H. Repositioning of niclosamide ethanolamine (NEN), an anthelmintic drug, for the treatment of lipotoxicity. Free Radic. Biol. Med. 2019, 137, 143–157. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Tao, H.; Alasadi, A.; Huang, Q.; Jin, S. Niclosamide piperazine prevents high-fat diet-induced obesity and diabetic symptoms in mice. Eat Weight Disord. 2019, 24, 91–96. [Google Scholar] [CrossRef]
- Chen, W.; Mook, R.A., Jr.; Premont, R.T.; Wang, J. Niclosamide: Beyond an antihelminthic drug. Cell. Signal. 2018, 41, 89–96. [Google Scholar] [CrossRef]
- Simsek-Yavuz, S.; Komsuoglu Celikyurt, F.I. An update of anti-viral treatment of COVID-19. Turk. J. Med. Sci. 2021, 51, 3372–3390. [Google Scholar] [CrossRef]
- Khanim, F.L.; Merrick, B.A.; Giles, H.V.; Jankute, M.; Jackson, J.B.; Giles, L.J.; Birtwistle, J.; Bunce, C.M.; Drayson, M.T. Redeployment-based drug screening identifies the anti-helminthic niclosamide as anti-myeloma therapy that also reduces free light chain production. Blood Cancer J. 2011, 1, e39. [Google Scholar] [CrossRef] [Green Version]
- Pan, J.X.; Ding, K.; Wang, C.Y. Niclosamide, an old antihelminthic agent, demonstrates antitumor activity by blocking multiple signaling pathways of cancer stem cells. Chin. J. Cancer 2012, 31, 178–184. [Google Scholar] [CrossRef] [Green Version]
- Balgi, A.D.; Fonseca, B.D.; Donohue, E.; Tsang, T.C.; Lajoie, P.; Proud, C.G.; Nabi, I.R.; Roberge, M. Screen for chemical modulators of autophagy reveals novel therapeutic inhibitors of mTORC1 signaling. PLoS ONE 2009, 4, e7124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ren, X.; Duan, L.; He, Q.; Zhang, Z.; Zhou, Y.; Wu, D.; Pan, J.; Pei, D.; Ding, K. Identification of Niclosamide as a New Small-Molecule Inhibitor of the STAT3 Signaling Pathway. ACS Med. Chem. Lett. 2010, 1, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Lu, Z.; Ding, K.; Li, J.; Du, X.; Chen, C.; Sun, X.; Wu, Y.; Zhou, J.; Pan, J. Antineoplastic mechanisms of niclosamide in acute myelogenous leukemia stem cells: Inactivation of the NF-κB pathway and generation of reactive oxygen species. Cancer Res. 2010, 70, 2516–2527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, A.M.; Ku, H.H.; Liang, Y.C.; Chen, Y.C.; Hwu, Y.M.; Yeh, T.S. The autonomous notch signal pathway is activated by baicalin and baicalein but is suppressed by niclosamide in K562 cells. J. Cell. Biochem. 2009, 106, 682–692. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Wang, J.; Lu, J.; Bond, M.C.; Ren, X.R.; Lyerly, H.K.; Barak, L.S.; Chen, W. The anti-helminthic niclosamide inhibits Wnt/Frizzled1 signaling. Biochemistry 2009, 48, 10267–10274. [Google Scholar] [CrossRef] [Green Version]
- Barbosa, E.J.; Lobenberg, R.; de Araujo, G.L.B.; Bou-Chacra, N.A. Niclosamide repositioning for treating cancer: Challenges and nano-based drug delivery opportunities. Eur. J. Pharm. Biopharm. 2019, 141, 58–69. [Google Scholar] [CrossRef]
- Fong, D.; Christensen, C.T.; Chan, M.M. Targeting Cancer Stem Cells with Repurposed Drugs to Improve Current Therapies. Recent Pat. Anti-Cancer Drug Discov. 2021, 16, 136–160. [Google Scholar] [CrossRef]
- Chae, H.D.; Cox, N.; Dahl, G.V.; Lacayo, N.J.; Davis, K.L.; Capolicchio, S.; Smith, M.; Sakamoto, K.M. Niclosamide suppresses acute myeloid leukemia cell proliferation through inhibition of CREB-dependent signaling pathways. Oncotarget 2018, 9, 4301–4317. [Google Scholar] [CrossRef]
- Jin, B.; Wang, C.; Shen, Y.; Pan, J. Anthelmintic niclosamide suppresses transcription of BCR-ABL fusion oncogene via disabling Sp1 and induces apoptosis in imatinib-resistant CML cells harboring T315I mutant. Cell Death Dis. 2018, 9, 68. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Li, H.; Zhan, D.; Xiang, M.; Yang, J.; Zuo, Y.; Yu, Y.; Zhou, H.; Jiang, D.; Luo, H.; et al. Niclosamide sensitizes nasopharyngeal carcinoma to radiation by downregulating Ku70/80 expression. J. Cancer 2018, 9, 736–744. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Zhou, X.; Xu, H.; Shi, X.; Zhao, J.; Yang, M.; Zhang, L.; Jin, X.; Hu, Y.; Li, X.; et al. Niclosamide Inhibits Cell Growth and Enhances Drug Sensitivity of Hepatocellular Carcinoma Cells via STAT3 Signaling Pathway. J. Cancer 2018, 9, 4150–4155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.Y.; Kim, J.Y.; Choi, J.H.; Kim, J.H.; Lee, C.J.; Singh, P.; Sarkar, S.; Baek, J.H.; Nam, J.S. Inhibition of LEF1-Mediated DCLK1 by Niclosamide Attenuates Colorectal Cancer Stemness. Clin. Cancer Res. 2019, 25, 1415–1429. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.; Yucel, N.; Kim, B.; Arany, Z. Local Mitochondrial ATP Production Regulates Endothelial Fatty Acid Uptake and Transport. Cell Metab. 2020, 32, 309–319.e307. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.Y.; Jung, A.R.; Shin, D.; Kwon, H.; Cho, H.J.; Ha, U.S.; Hong, S.H.; Lee, J.Y.; Kim, S.W.; Park, Y.H. Niclosamide exerts anticancer effects through inhibition of the FOXM1-mediated DNA damage response in prostate cancer. Am. J. Cancer Res. 2021, 11, 2944–2959. [Google Scholar] [PubMed]
- Dimri, S.; Malhotra, R.; Shet, T.; Mokal, S.; Gupta, S.; De, A. Noncanonical pS727 post translational modification dictates major STAT3 activation and downstream functions in breast cancer. Exp. Cell Res. 2020, 396, 112313. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.Y.; Richardson, B.C. The MAPK signalling pathways and colorectal cancer. Lancet Oncol. 2005, 6, 322–327. [Google Scholar] [CrossRef]
- Wagner, E.F.; Nebreda, A.R. Signal integration by JNK and p38 MAPK pathways in cancer development. Nat. Rev. Cancer 2009, 9, 537–549. [Google Scholar] [CrossRef]
- Taciak, B.; Pruszynska, I.; Kiraga, L.; Bialasek, M.; Krol, M. Wnt signaling pathway in development and cancer. J. Physiol. Pharmacol. 2018, 69, 185–196. [Google Scholar] [CrossRef]
- Hua, H.; Kong, Q.; Zhang, H.; Wang, J.; Luo, T.; Jiang, Y. Targeting mTOR for cancer therapy. J. Hematol. Oncol. 2019, 12, 71. [Google Scholar] [CrossRef]
- Newton, P.T. New insights into niclosamide action: Autophagy activation in colorectal cancer. Biochem. J. 2019, 476, 779–781. [Google Scholar] [CrossRef]
- Gyamfi, J.; Lee, Y.H.; Min, B.S.; Choi, J. Niclosamide reverses adipocyte induced epithelial-mesenchymal transition in breast cancer cells via suppression of the interleukin-6/STAT3 signalling axis. Sci. Rep. 2019, 9, 11336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yi, Y.; Woo, Y.M.; Hwang, K.H.; Kim, H.S.; Lee, S.H. Niclosamide and Pyrvinium Are Both Potential Therapeutics for Osteosarcoma, Inhibiting Wnt-Axin2-Snail Cascade. Cancers 2021, 13, 4630. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Zuo, W.; Chen, L.; Bian, S.; Jing, J.; Gan, C.; Wu, X.; Liu, H.; Su, X.; Hu, W.; et al. Repurposing of the anti-helminthic drug niclosamide to treat melanoma and pulmonary metastasis via the STAT3 signaling pathway. Biochem. Pharm. 2019, 169, 113610. [Google Scholar] [CrossRef]
- Chien, M.H.; Ho, Y.C.; Yang, S.F.; Yang, Y.C.; Lai, S.Y.; Chen, W.S.; Chen, M.J.; Yeh, C.B. Niclosamide, an oral antihelmintic drug, exhibits antimetastatic activity in hepatocellular carcinoma cells through downregulating twist-mediated CD10 expression. Environ. Toxicol. 2018, 33, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Fan, B.; Xiao, Z. Overexpression of ALK4 inhibits cell proliferation and migration through the inactivation of JAK/STAT3 signaling pathway in glioma. Biomed. Pharmacother. 2018, 98, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Ding, R.; Han, Z.; Ma, Z.; Wang, Y. Targeting of cell cycle and let-7a/STAT3 pathway by niclosamide inhibits proliferation, migration and invasion in oral squamous cell carcinoma cells. Biomed. Pharmacother. 2017, 96, 434–442. [Google Scholar] [CrossRef]
- Culig, Z.; Santer, F.R. Androgen receptor signaling in prostate cancer. Cancer Metastasis Rev. 2014, 33, 413–427. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Lou, W.; Armstrong, C.; Zhu, Y.; Evans, C.P.; Gao, A.C. Niclosamide suppresses cell migration and invasion in enzalutamide resistant prostate cancer cells via Stat3-AR axis inhibition. Prostate 2015, 75, 1341–1353. [Google Scholar] [CrossRef] [Green Version]
- Stewart, R.L.; Carpenter, B.L.; West, D.S.; Knifley, T.; Liu, L.; Wang, C.; Weiss, H.L.; Gal, T.S.; Durbin, E.B.; Arnold, S.M.; et al. S100A4 drives non-small cell lung cancer invasion, associates with poor prognosis, and is effectively targeted by the FDA-approved anti-helminthic agent niclosamide. Oncotarget 2016, 7, 34630–34642. [Google Scholar] [CrossRef] [Green Version]
- Moskaleva, E.Y.; Perevozchikova, V.G.; Zhirnik, A.S.; Severin, S.E. Molecular mechanisms of niclosamide antitumor activity. Biomeditsinskaya Khimiya 2015, 61, 680–693. [Google Scholar] [CrossRef] [Green Version]
- Akgun, O.; Erkisa, M.; Ari, F. Effective and new potent drug combination: Histone deacetylase and Wnt/beta-catenin pathway inhibitors in lung carcinoma cells. J. Cell. Biochem. 2019, 120, 15467–15482. [Google Scholar] [CrossRef] [PubMed]
- Suliman, M.A.; Zhang, Z.; Na, H.; Ribeiro, A.L.; Zhang, Y.; Niang, B.; Hamid, A.S.; Zhang, H.; Xu, L.; Zuo, Y. Niclosamide inhibits colon cancer progression through downregulation of the Notch pathway and upregulation of the tumor suppressor miR-200 family. Int. J. Mol. Med. 2016, 38, 776–784. [Google Scholar] [CrossRef] [PubMed]
- Figarola, J.L.; Singhal, J.; Singhal, S.; Kusari, J.; Riggs, A. Bioenergetic modulation with the mitochondria uncouplers SR4 and niclosamide prevents proliferation and growth of treatment-naive and vemurafenib-resistant melanomas. Oncotarget 2018, 9, 36945–36965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Q.S.; Xin, H.R.; Qiu, R.L.; Deng, Z.L.; Deng, F.; Yan, Z.J. Niclosamide: Drug repurposing for human chondrosarcoma treatment via the caspase-dependent mitochondrial apoptotic pathway. Am. J. Transl. Res. 2020, 12, 3688–3701. [Google Scholar] [PubMed]
- Lee, M.C.; Chen, Y.K.; Hsu, Y.J.; Lin, B.R. Niclosamide inhibits the cell proliferation and enhances the responsiveness of esophageal cancer cells to chemotherapeutic agents. Oncol. Rep. 2020, 43, 549–561. [Google Scholar] [CrossRef] [PubMed]
- Yu, K.; Wang, T.; Li, Y.; Wang, C.; Wang, X.; Zhang, M.; Xie, Y.; Li, S.; An, Z.; Ye, T. Niclosamide induces apoptosis through mitochondrial intrinsic pathway and inhibits migration and invasion in human thyroid cancer in vitro. Biomed. Pharmacother. 2017, 92, 403–411. [Google Scholar] [CrossRef]
- Kaushal, J.B.; Bhatia, R.; Kanchan, R.K.; Raut, P.; Mallapragada, S.; Ly, Q.P.; Batra, S.K.; Rachagani, S. Repurposing Niclosamide for Targeting Pancreatic Cancer by Inhibiting Hh/Gli Non-Canonical Axis of Gsk3beta. Cancers 2021, 13, 3105. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.K.; Cheong, J.H. Mitochondria-centric bioenergetic characteristics in cancer stem-like cells. Arch. Pharmacal Res. 2019, 42, 113–127. [Google Scholar] [CrossRef] [Green Version]
- Altieri, D.C. Mitochondrial dynamics and metastasis. Cell. Mol. Life Sci. 2019, 76, 827–835. [Google Scholar] [CrossRef]
- De Francesco, E.M.; Ozsvari, B.; Sotgia, F.; Lisanti, M.P. Dodecyl-TPP Targets Mitochondria and Potently Eradicates Cancer Stem Cells (CSCs): Synergy With FDA-Approved Drugs and Natural Compounds (Vitamin C and Berberine). Front. Oncol. 2019, 9, 615. [Google Scholar] [CrossRef] [Green Version]
- Hilfenhaus, G.; Mompeon, A.; Freshman, J.; Prajapati, D.P.; Hernandez, G.; Freitas, V.M.; Ma, F.; Langenbacher, A.D.; Mirkov, S.; Song, D.; et al. A High-Content Screen Identifies Drugs That Restrict Tumor Cell Extravasation across the Endothelial Barrier. Cancer Res. 2021, 81, 619–633. [Google Scholar] [CrossRef] [PubMed]
- Hochmair, M.; Rath, B.; Klameth, L.; Ulsperger, E.; Weinlinger, C.; Fazekas, A.; Plangger, A.; Zeillinger, R.; Hamilton, G. Effects of salinomycin and niclosamide on small cell lung cancer and small cell lung cancer circulating tumor cell lines. Investig. New Drugs 2020, 38, 946–955. [Google Scholar] [CrossRef] [PubMed]
- Senkowski, W.; Zhang, X.; Olofsson, M.H.; Isacson, R.; Hoglund, U.; Gustafsson, M.; Nygren, P.; Linder, S.; Larsson, R.; Fryknas, M. Three-Dimensional Cell Culture-Based Screening Identifies the Anthelmintic Drug Nitazoxanide as a Candidate for Treatment of Colorectal Cancer. Mol. Cancer Ther. 2015, 14, 1504–1516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.C.; Chao, T.K.; Chang, C.C.; Yo, Y.T.; Yu, M.H.; Lai, H.C. Drug screening identifies niclosamide as an inhibitor of breast cancer stem-like cells. PLoS ONE 2013, 8, e74538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asano, T. Drug Resistance in Cancer Therapy and the Role of Epigenetics. J. Nippon. Med. Sch. 2020, 87, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Robey, R.W.; Pluchino, K.M.; Hall, M.D.; Fojo, A.T.; Bates, S.E.; Gottesman, M.M. Revisiting the role of ABC transporters in multidrug-resistant cancer. Nat. Rev. Cancer 2018, 18, 452–464. [Google Scholar] [CrossRef] [PubMed]
- Hamdoun, S.; Jung, P.; Efferth, T. Drug Repurposing of the Anthelmintic Niclosamide to Treat Multidrug-Resistant Leukemia. Front. Pharm. 2017, 8, 110. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Li, P.K.; Roberts, M.J.; Arend, R.C.; Samant, R.S.; Buchsbaum, D.J. Multi-targeted therapy of cancer by niclosamide: A new application for an old drug. Cancer Lett. 2014, 349, 8–14. [Google Scholar] [CrossRef] [Green Version]
- Lohiya, G.; Katti, D.S. A Synergistic Combination of Niclosamide and Doxorubicin as an Efficacious Therapy for All Clinical Subtypes of Breast Cancer. Cancers 2021, 13, 3299. [Google Scholar] [CrossRef]
- Zhao, D.; Hu, C.; Fu, Q.; Lv, H. Combined chemotherapy for triple negative breast cancer treatment by paclitaxel and niclosamide nanocrystals loaded thermosensitive hydrogel. Eur. J. Pharm. Sci. 2021, 167, 105992. [Google Scholar] [CrossRef]
- Liu, J.; Ding, H.; Quan, H.; Han, J. Anthelminthic niclosamide inhibits tumor growth and invasion in cisplatin-resistant human epidermal growth factor receptor 2-positive breast cancer. Oncol. Lett. 2021, 22, 666. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.E.; Seo, Y.; Yun, J.S.; Song, S.H.; Han, D.; Cho, E.S.; Cho, S.B.; Jeon, Y.; Lee, H.; Kim, H.S.; et al. Metformin and Niclosamide Synergistically Suppress Wnt and YAP in APC-Mutated Colorectal Cancer. Cancers 2021, 13, 3437. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.H.; Hsiang, J.; Rosen, S.T. Flavopiridol (Alvocidib), a Cyclin-dependent Kinases (CDKs) Inhibitor, Found Synergy Effects with Niclosamide in Cutaneous T-cell Lymphoma. J. Clin. Haematol. 2021, 2, 48–61. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Armstrong, C.M.; Lou, W.; Lombard, A.P.; Cucchiara, V.; Gu, X.; Yang, J.C.; Nadiminty, N.; Pan, C.X.; Evans, C.P.; et al. Niclosamide and Bicalutamide Combination Treatment Overcomes Enzalutamide- and Bicalutamide-Resistant Prostate Cancer. Mol. Cancer Ther. 2017, 16, 1521–1530. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Lou, W.; Zhu, Y.; Nadiminty, N.; Schwartz, C.T.; Evans, C.P.; Gao, A.C. Niclosamide inhibits androgen receptor variants expression and overcomes enzalutamide resistance in castration-resistant prostate cancer. Clin. Cancer Res. 2014, 20, 3198–3210. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Armstrong, C.; Zhu, Y.; Lou, W.; Gao, A.C. Niclosamide enhances abiraterone treatment via inhibition of androgen receptor variants in castration resistant prostate cancer. Oncotarget 2016, 7, 32210–32220. [Google Scholar] [CrossRef] [Green Version]
- Schweizer, M.T.; Haugk, K.; McKiernan, J.S.; Gulati, R.; Cheng, H.H.; Maes, J.L.; Dumpit, R.F.; Nelson, P.S.; Montgomery, B.; McCune, J.S.; et al. A phase I study of niclosamide in combination with enzalutamide in men with castration-resistant prostate cancer. PLoS ONE 2018, 13, e0198389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parikh, M.; Liu, C.; Wu, C.Y.; Evans, C.P.; Dall’Era, M.; Robles, D.; Lara, P.N.; Agarwal, N.; Gao, A.C.; Pan, C.X. Phase Ib trial of reformulated niclosamide with abiraterone/prednisone in men with castration-resistant prostate cancer. Sci. Rep. 2021, 11, 6377. [Google Scholar] [CrossRef]
- Abbott, M.; Ustoyev, Y. Cancer and the Immune System: The History and Background of Immunotherapy. Semin. Oncol. Nurs. 2019, 35, 150923. [Google Scholar] [CrossRef]
- Luo, F.; Luo, M.; Rong, Q.X.; Zhang, H.; Chen, Z.; Wang, F.; Zhao, H.Y.; Fu, L.W. Niclosamide, an antihelmintic drug, enhances efficacy of PD-1/PD-L1 immune checkpoint blockade in non-small cell lung cancer. J. Immunother. Cancer 2019, 7, 245. [Google Scholar] [CrossRef]
- Ma, R.; Ma, Z.G.; Gao, J.L.; Tai, Y.; Li, L.J.; Zhu, H.B.; Li, L.; Dong, D.L.; Sun, Z.J. Injectable pegylated niclosamide (polyethylene glycol-modified niclosamide) for cancer therapy. J. Biomed. Mater. Res. A 2020, 108, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Yao, Y. Octenylsuccinate hydroxypropyl phytoglycogen enhances the solubility and in-vitro antitumor efficacy of niclosamide. Int. J. Pharm. 2018, 535, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Hatamipour, M.; Jaafari, M.R.; Momtazi-Borojeni, A.A.; Ramezani, M.; Sahebkar, A. Nanoliposomal Encapsulation Enhances In Vivo Anti-Tumor Activity of Niclosamide against Melanoma. Anti-Cancer Agents Med. Chem. 2019, 19, 1618–1626. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, J.; Ren, X.R.; Mook, R.A.; Wang, J.; Spasojevic, I.; Premont, R.T.; Li, X.; Chilkoti, A.; Chen, W. Niclosamide-conjugated polypeptide nanoparticles inhibit Wnt signaling and colon cancer growth. Nanoscale 2017, 9, 12709–12717. [Google Scholar] [CrossRef]
- Ray, E.; Vaghasiya, K.; Sharma, A.; Shukla, R.; Khan, R.; Kumar, A.; Verma, R.K. Autophagy-Inducing Inhalable Co-crystal Formulation of Niclosamide-Nicotinamide for Lung Cancer Therapy. AAPS PharmSciTech 2020, 21, 260. [Google Scholar] [CrossRef]
- Reddy, G.B.; Kerr, D.L.; Spasojevic, I.; Tovmasyan, A.; Hsu, D.S.; Brigman, B.E.; Somarelli, J.A.; Needham, D.; Eward, W.C. Preclinical Testing of a Novel Niclosamide Stearate Prodrug Therapeutic (NSPT) Shows Efficacy Against Osteosarcoma. Mol. Cancer Ther. 2020, 19, 1448–1461. [Google Scholar] [CrossRef]
- Ye, Y.; Zhang, X.; Zhang, T.; Wang, H.; Wu, B. Design and evaluation of injectable niclosamide nanocrystals prepared by wet media milling technique. Drug Dev. Ind. Pharm. 2015, 41, 1416–1424. [Google Scholar] [CrossRef]
- Lodagekar, A.; Borkar, R.M.; Thatikonda, S.; Chavan, R.B.; Naidu, V.G.M.; Shastri, N.R.; Srinivas, R.; Chella, N. Formulation and evaluation of cyclodextrin complexes for improved anticancer activity of repurposed drug: Niclosamide. Carbohydr. Polym. 2019, 212, 252–259. [Google Scholar] [CrossRef]
- Lin, C.K.; Bai, M.Y.; Hu, T.M.; Wang, Y.C.; Chao, T.K.; Weng, S.J.; Huang, R.L.; Su, P.H.; Lai, H.C. Preclinical evaluation of a nanoformulated antihelminthic, niclosamide, in ovarian cancer. Oncotarget 2016, 7, 8993–9006. [Google Scholar] [CrossRef] [Green Version]
- Fu, Q.; Jin, X.; Zhang, Z.; Lv, H. Preparation and in vitro antitumor effects on MDA-MB-231 cells of niclosamide nanocrystals stabilized by poloxamer188 and PBS. Int. J. Pharm. 2020, 584, 119432. [Google Scholar] [CrossRef]
- Chowdhury, M.K.; Turner, N.; Bentley, N.L.; Das, A.; Wu, L.E.; Richani, D.; Bustamante, S.; Gilchrist, R.B.; Morris, M.J.; Shepherd, P.R.; et al. Niclosamide reduces glucagon sensitivity via hepatic PKA inhibition in obese mice: Implications for glucose metabolism improvements in type 2 diabetes. Sci. Rep. 2017, 7, 40159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, M.; Zeng, S.; Qiu, Q.; Xiao, Y.; Shi, M.; Zou, Y.; Yang, X.; Xu, H.; Liang, L. Niclosamide induces apoptosis in human rheumatoid arthritis fibroblast-like synoviocytes. Int. Immunopharmacol. 2016, 31, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Morin, F.; Kavian, N.; Nicco, C.; Cerles, O.; Chereau, C.; Batteux, F. Improvement of Sclerodermatous Graft-Versus-Host Disease in Mice by Niclosamide. J. Investig. Dermatol. 2016, 136, 2158–2167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morin, F.; Kavian, N.; Nicco, C.; Cerles, O.; Chereau, C.; Batteux, F. Niclosamide Prevents Systemic Sclerosis in a Reactive Oxygen Species-Induced Mouse Model. J. Immunol. 2016, 197, 3018–3028. [Google Scholar] [CrossRef]
- Liang, L.; Huang, M.; Xiao, Y.; Zen, S.; Lao, M.; Zou, Y.; Shi, M.; Yang, X.; Xu, H. Inhibitory effects of niclosamide on inflammation and migration of fibroblast-like synoviocytes from patients with rheumatoid arthritis. Inflamm. Res. 2015, 64, 225–233. [Google Scholar] [CrossRef]
- Huang, M.; Qiu, Q.; Zeng, S.; Xiao, Y.; Shi, M.; Zou, Y.; Ye, Y.; Liang, L.; Yang, X.; Xu, H. Niclosamide inhibits the inflammatory and angiogenic activation of human umbilical vein endothelial cells. Inflamm. Res. 2015, 64, 1023–1032. [Google Scholar] [CrossRef]
- Al-Gareeb, A.; Gorial, F.; Mahmood, A. The Anti-Rheumatoid Activity of Niclosamide in Collagen-Induced Arthritis in Rats. Arch. Rheumatol. 2019, 34, 426–433. [Google Scholar] [CrossRef] [Green Version]
- Walker, J.U.; Ram, J.L. Effects of deionized water on sensitivity of zebra mussels (Dreissena polymorpha) to toxic chemicals. Comp. Biochem. Physiol. Part C Pharmacol. Toxicol. Endocrinol. 1994, 107, 353–358. [Google Scholar] [CrossRef]
- Mostafa, A.; Kandeil, A.; Elshaier, Y.A.M.M.; Kutkat, O.; Moatasim, Y.; Rashad, A.A.; Shehata, M.; Gomaa, M.R.; Mahrous, N.; Mahmoud, S.H.; et al. FDA-Approved Drugs with Potent In Vitro Antiviral Activity against Severe Acute Respiratory Syndrome Coronavirus 2. Pharmaceuticals 2020, 13, 443. [Google Scholar] [CrossRef]
- Li, Z.; Xu, J.; Lang, Y.; Fan, X.; Kuo, L.; D’Brant, L.; Hu, S.; Samrat, S.K.; Trudeau, N.; Tharappel, A.M.; et al. JMX0207, a Niclosamide Derivative with Improved Pharmacokinetics, Suppresses Zika Virus Infection Both In Vitro and In Vivo. ACS Infect. Dis. 2020, 6, 2616–2628. [Google Scholar] [CrossRef]
- Fang, J.; Sun, L.; Peng, G.; Xu, J.; Zhou, R.; Cao, S.; Chen, H.; Song, Y. Identification of three antiviral inhibitors against Japanese encephalitis virus from library of pharmacologically active compounds 1280. PLoS ONE 2013, 8, e78425. [Google Scholar] [CrossRef] [PubMed]
- Herring, S.; Oda, J.M.; Wagoner, J.; Kirchmeier, D.; O’Connor, A.; Nelson, E.A.; Huang, Q.; Liang, Y.; DeWald, L.E.; Johansen, L.M.; et al. Inhibition of Arenaviruses by Combinations of Orally Available Approved Drugs. Antimicrob. Agents Chemother. 2021, 65, e01146-20. [Google Scholar] [CrossRef] [PubMed]
- Jurgeit, A.; McDowell, R.; Moese, S.; Meldrum, E.; Schwendener, R.; Greber, U.F. Niclosamide is a proton carrier and targets acidic endosomes with broad antiviral effects. PLoS Pathog. 2012, 8, e1002976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.M.; Lu, J.W.; Lin, C.C.; Chin, Y.F.; Wu, T.Y.; Lin, L.I.; Lai, Z.Z.; Kuo, S.C.; Ho, Y.J. Antiviral activities of niclosamide and nitazoxanide against chikungunya virus entry and transmission. Antivir. Res. 2016, 135, 81–90. [Google Scholar] [CrossRef]
- Xu, J.; Berastegui-Cabrera, J.; Carretero-Ledesma, M.; Chen, H.; Xue, Y.; Wold, E.A.; Pachon, J.; Zhou, J.; Sanchez-Cespedes, J. Discovery of a Small Molecule Inhibitor of Human Adenovirus Capable of Preventing Escape from the Endosome. Int. J. Mol. Sci. 2021, 22, 1617. [Google Scholar] [CrossRef]
- Huang, L.; Yang, M.; Yuan, Y.; Li, X.; Kuang, E. Niclosamide inhibits lytic replication of Epstein-Barr virus by disrupting mTOR activation. Antivir. Res. 2017, 138, 68–78. [Google Scholar] [CrossRef]
- Wu, C.J.; Jan, J.T.; Chen, C.M.; Hsieh, H.P.; Hwang, D.R.; Liu, H.W.; Liu, C.Y.; Huang, H.W.; Chen, S.C.; Hong, C.F.; et al. Inhibition of severe acute respiratory syndrome coronavirus replication by niclosamide. Antimicrob. Agents Chemother. 2004, 48, 2693–2696. [Google Scholar] [CrossRef] [Green Version]
- Brunaugh, A.D.; Seo, H.; Warnken, Z.; Ding, L.; Seo, S.H.; Smyth, H.D.C. Development and evaluation of inhalable composite niclosamide-lysozyme particles: A broad-spectrum, patient-adaptable treatment for coronavirus infections and sequalae. PLoS ONE 2021, 16, e0246803. [Google Scholar] [CrossRef]
- Cairns, D.M.; Boorgu, D.; Levin, M.; Kaplan, D.L. Niclosamide rescues microcephaly in a humanized in vivo model of Zika infection using human induced neural stem cells. Biol. Open 2018, 7, bio031807. [Google Scholar] [CrossRef] [Green Version]
- Xu, M.; Lee, E.M.; Wen, Z.; Cheng, Y.; Huang, W.K.; Qian, X.; Tcw, J.; Kouznetsova, J.; Ogden, S.C.; Hammack, C.; et al. Identification of small-molecule inhibitors of Zika virus infection and induced neural cell death via a drug repurposing screen. Nat. Med. 2016, 22, 1101–1107. [Google Scholar] [CrossRef]
- Stachulski, A.V.; Pidathala, C.; Row, E.C.; Sharma, R.; Berry, N.G.; Iqbal, M.; Bentley, J.; Allman, S.A.; Edwards, G.; Helm, A.; et al. Thiazolides as novel antiviral agents. 1. Inhibition of hepatitis B virus replication. J. Med. Chem. 2011, 54, 4119–4132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, J.; Berastegui-Cabrera, J.; Chen, H.; Pachon, J.; Zhou, J.; Sanchez-Cespedes, J. Structure-Activity Relationship Studies on Diversified Salicylamide Derivatives as Potent Inhibitors of Human Adenovirus Infection. J. Med. Chem. 2020, 63, 3142–3160. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Xu, J.; Files, M.; Cirillo, J.D.; Endsley, J.J.; Zhou, J.; Endsley, M.A. Dual activity of niclosamide to suppress replication of integrated HIV-1 and Mycobacterium tuberculosis (Beijing). Tuberculosis 2019, 116S, S28–S33. [Google Scholar] [CrossRef] [PubMed]
- Zhu, P.J.; Hobson, J.P.; Southall, N.; Qiu, C.; Thomas, C.J.; Lu, J.; Inglese, J.; Zheng, W.; Leppla, S.H.; Bugge, T.H.; et al. Quantitative high-throughput screening identifies inhibitors of anthrax-induced cell death. Bioorganic Med. Chem. 2009, 17, 5139–5145. [Google Scholar] [CrossRef]
- Rajamuthiah, R.; Fuchs, B.B.; Conery, A.L.; Kim, W.; Jayamani, E.; Kwon, B.; Ausubel, F.M.; Mylonakis, E. Repurposing salicylanilide anthelmintic drugs to combat drug resistant Staphylococcus aureus. PLoS ONE 2015, 10, e0124595. [Google Scholar] [CrossRef] [Green Version]
- Ma, R.; Ma, Z.G.; Zhen, C.L.; Shen, X.; Li, S.L.; Li, L.; Zheng, Y.F.; Dong, D.L.; Sun, Z.J. Design, synthesis and characterization of poly (methacrylic acid-niclosamide) and its effect on arterial function. Mater. Sci. Eng. C 2017, 77, 352–359. [Google Scholar] [CrossRef]
- Liu, Z.; Xiu, Y.; Qiu, F.; Zhu, Z.; Zong, R.; Zhou, X.; An, J.; Wang, Q.; Reinach, P.S.; Li, W.; et al. Canonical Wnt Signaling Drives Myopia Development and Can Be Pharmacologically Modulated. Investig. Opthalmology Vis. Sci. 2021, 62, 21. [Google Scholar] [CrossRef]
- Xu, Y.; Dai, J.R. Researches on mechanism of cell toxicity caused by niclosamide. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi = Chin. J. Schistosomiasis Control 2015, 27, 104–107. [Google Scholar]
- Lu, D.; Ma, Z.; Zhang, T.; Zhang, X.; Wu, B. Metabolism of the anthelmintic drug niclosamide by cytochrome P450 enzymes and UDP-glucuronosyltransferases: Metabolite elucidation and main contributions from CYP1A2 and UGT1A1. Xenobiotica 2016, 46, 1–13. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Z.; Ren, J.; Du, J.; Wang, H.; Liu, J.; Wang, G. Niclosamide as a Promising Therapeutic Player in Human Cancer and Other Diseases. Int. J. Mol. Sci. 2022, 23, 16116. https://doi.org/10.3390/ijms232416116
Wang Z, Ren J, Du J, Wang H, Liu J, Wang G. Niclosamide as a Promising Therapeutic Player in Human Cancer and Other Diseases. International Journal of Molecular Sciences. 2022; 23(24):16116. https://doi.org/10.3390/ijms232416116
Chicago/Turabian StyleWang, Zhan, Junyi Ren, Jinxiu Du, Huan Wang, Jia Liu, and Guiling Wang. 2022. "Niclosamide as a Promising Therapeutic Player in Human Cancer and Other Diseases" International Journal of Molecular Sciences 23, no. 24: 16116. https://doi.org/10.3390/ijms232416116






