Sperm Physiological Response to Female Serum—Potential New Insights into the Reproductive Incompatibility Diagnostics
Abstract
1. Introduction
2. Results
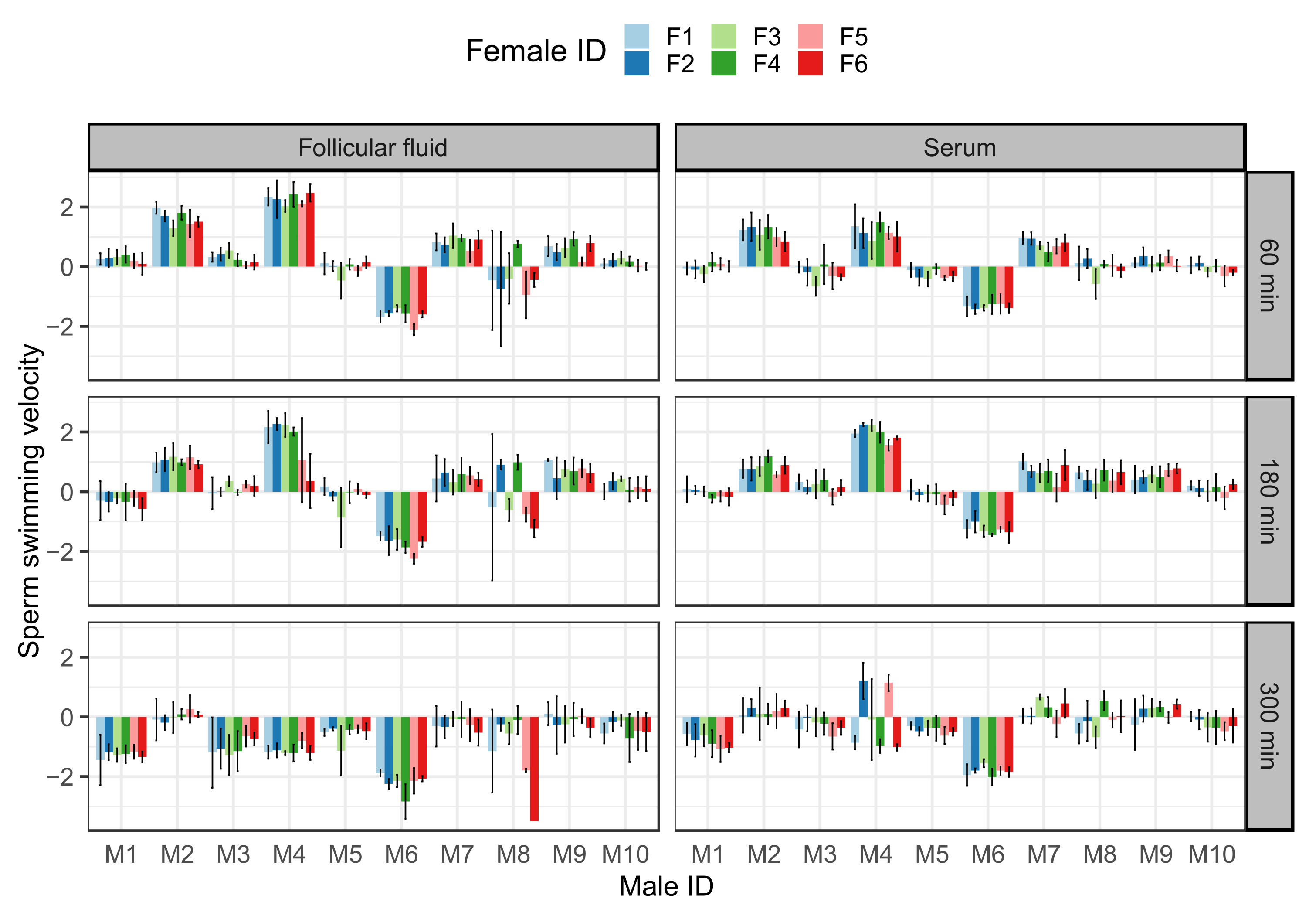
2.1. Effect of Follicular Fluid and Serum on Sperm Motility and Viability
2.2. Serum Treatment Predicts Sperm Performance in Follicular Fluid
2.3. Effect of Allele–Antibody Matches on Sperm Performance
3. Discussion
4. Materials and Methods
4.1. Study Subject and Sample Collection
4.2. Sperm Activation and Measurements for Sperm Performance
4.3. Male HLA Genotyping and Test for Female HLA Antibodies
4.4. Statistical Analysis
4.4.1. Models Testing for the Effect of Time Point and Sperm Treatments on Measured Sperm Traits
4.4.2. Time Point- and Sperm Treatment-Specific Models
4.4.3. Consistency of Gamete Compatibility Effect and Associations between Sperm Treatments
4.4.4. Effect of Allele–Antibody Matches on Sperm Traits
4.4.5. Fitting, Comparison, and Diagnostics of the Models
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kekäläinen, J.; Evans, J.P. Gamete-mediated mate choice: Towards a more inclusive view of sexual selection. Proc. Biol. Sci. 2018, 285, 20180836. [Google Scholar] [CrossRef]
- Eisenbach, M.; Giojalas, L.C. Sperm guidance in mammals—An unpaved road to the egg. Nat. Rev. Mol. Cell Biol. 2006, 7, 276–285. [Google Scholar] [CrossRef]
- Kekäläinen, J.; Larma, I.; Linden, M.; Evans, J.P. Lectin staining and flow cytometry reveals female-induced sperm acrosome reaction and surface carbohydrate reorganization. Sci. Rep. 2015, 5, 15321. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Kawano, N.; Yoshida, K. Control of sperm motility and fertility: Diverse factors and common mechanisms. Cell. Mol. Life Sci. 2008, 65, 3446–3457. [Google Scholar] [CrossRef] [PubMed]
- Cramer, E.R.A.; Stensrud, E.; Marthinsen, G.; Hogner, S.; Johannessen, L.E.; Laskemoen, T.; Eybert, M.-C.; Slagsvold, T.; Lifjeld, J.T.; Johnsen, A. Sperm performance in conspecific and heterospecific female fluid. Ecol. Evol. 2016, 6, 1363–1377. [Google Scholar] [CrossRef] [PubMed]
- Flegel, C.; Vogel, F.; Hofreuter, A.; Schreiner, B.S.P.; Osthold, S.; Veitinger, S.; Becker, C.; Brockmeyer, N.H.; Muschol, M.; Wennemuth, G.; et al. Characterization of the Olfactory Receptors Expressed in Human Spermatozoa. Front. Mol. Biosci. 2016, 2, 73. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.G.; Costello, S.; Kelly, M.C.; Ramalingam, M.; Drew, E.; Publicover, S.J.; Barratt, C.L.R.; Da Silva, S.M. Complex CatSper-dependent and independent [Ca2+]i signalling in human spermatozoa induced by follicular fluid. Hum. Reprod. 2017, 32, 1995–2006. [Google Scholar] [CrossRef]
- Kekäläinen, J.; Evans, J.P. Female-induced remote regulation of sperm physiology may provide opportunities for gamete-level mate choice. Evolution 2017, 71, 238–248. [Google Scholar] [CrossRef] [PubMed]
- Robertson, S.A. Seminal plasma and male factor signalling in the female reproductive tract. Cell Tissue Res. 2005, 322, 43–52. [Google Scholar] [CrossRef]
- Holt, W.V.; Fazeli, A. Do sperm possess a molecular passport? Mechanistic insights into sperm selection in the female reproductive tract. Mol. Hum. Reprod. 2015, 21, 491–501. [Google Scholar] [CrossRef]
- Ebenhard, W.G. Female Control: Sexual Selection by Cryptic Female Choice; Princeton University Press: Princeton, NJ, USA, 1996. [Google Scholar]
- Gasparini, C.; Pilastro, A. Cryptic female preference for genetically unrelated males is mediated by ovarian fluid in the guppy. Proc. Biol. Sci. 2011, 278, 2495–2501. [Google Scholar] [CrossRef] [PubMed]
- Alonzo, S.H.; Stiver, K.A.; Marsh-Rollo, S.E. Ovarian fluid allows directional cryptic female choice despite external fertilization. Nat. Commun. 2016, 7, 12452. [Google Scholar] [CrossRef] [PubMed]
- Rosengrave, P.; Montgomerie, R.; Gemmell, N. Cryptic female choice enhances fertilization success and embryo survival in chinook salmon. Proc. Biol. Sci. 2016, 283, 20160001. [Google Scholar] [CrossRef] [PubMed]
- Løvlie, H.; Gillingham, M.A.F.; Worley, K.; Pizzari, T.; Richardson, D.S. Cryptic female choice favours sperm from major histocompatibility complex-dissimilar males. Proc. R. Soc. B 2013, 280, 20131296. [Google Scholar] [CrossRef]
- Gasparini, C.; Congiu, L.; Pilastro, A. Major histocompatibility complex similarity and sexual selection: Different does not always mean attractive. Mol. Ecol. 2015, 24, 4286–4295. [Google Scholar] [CrossRef]
- Lenz, T.L.; Hafer, N.; Samonte, I.E.; Yeates, S.E.; Milinski, M. Cryptic haplotype-specific gamete selection yields offspring with optimal MHC immune genes. Evolution 2018, 72, 2478–2490. [Google Scholar] [CrossRef]
- Firman, R.C.; Gasparini, C.; Manier, M.K.; Pizzari, T. Postmating Female Control: 20 Years of Cryptic Female Choice. Trends Ecol. Evol. 2017, 32, 368–382. [Google Scholar] [CrossRef]
- Winternitz, J.; Abbate, J.L.; Huchard, E.; Havlíček, J.; Garamszegi, L.Z. Patterns of MHC-dependent mate selection in humans and nonhuman primates: A meta-analysis. Mol. Ecol. 2017, 26, 668–688. [Google Scholar] [CrossRef]
- Jokiniemi, A.; Kuusipalo, L.; Ritari, J.; Koskela, S.; Partanen, J.; Kekäläinen, J. Gamete-level immunogenetic incompatibility in humans–towards deeper understanding of fertilization and infertility? Heredity 2020, 125, 281–289. [Google Scholar] [CrossRef]
- Jokiniemi, A.; Magris, M.; Ritari, J.; Kuusipalo, L.; Lundgren, T.; Partanen, J.; Kekäläinen, J. Post-copulatory genetic matchmaking: HLA-dependent effects of cervical mucus on human sperm function. Proc. R. Soc. Lond. B Biol. Sci. 2020, 287, 20201682. [Google Scholar] [CrossRef]
- Kekäläinen, J. Genetic incompatibility of the reproductive partners: An evolutionary perspective on infertility. Hum. Reprod. 2021, 36, 3028–3035. [Google Scholar] [CrossRef] [PubMed]
- Levine, H.; Jørgensen, N.; Martino-Andrade, A.; Mendiola, J.; Weksler-Derri, D.; Mindlis, I.; Pinotti, R.; Swan, S.H. Temporal trends in sperm count: A systematic review and meta-regression analysis. Hum. Reprod. Update 2017, 23, 646–659. [Google Scholar] [CrossRef] [PubMed]
- Pizzol, D. Genetic and molecular diagnostics of male infertility in the clinical practice. Front. Biosci. 2014, 19, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Sakkas, D.; Ramalingam, M.; Garrido, N.; Barratt, C.L.R. Sperm selection in natural conception: What can we learn from Mother Nature to improve assisted reproduction outcomes? Hum. Reprod. Update 2015, 21, 711–726. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.L.; Kao, C.C.; Wei, Y.H. Antithrombin III enhances the motility and chemotaxis of boar sperm. Comp. Biochem. Physiol. Comp. Physiol. 1994, 107, 277–282. [Google Scholar]
- Mandal, M.; Saha, S.; Ghosh, A.K.; Majumder, G.C. Identification and characterization of a sperm motility promoting glycoprotein from buffalo blood serum. J. Cell. Physiol. 2006, 209, 353–362. [Google Scholar] [CrossRef]
- Dungdung, S.R.; Bhoumik, A.; Saha, S.; Ghosh, P.; Das, K.; Mukherjee, S.; Nath, D.; Chakrabarty, J.; Kundu, C.; Jaiswal, B.S.; et al. Sperm Motility Regulatory Proteins: A Tool to Enhance Sperm Quality; IntechOpen: Rijeka, Croatia, 2016; pp. 161–177. [Google Scholar]
- Rodgers, R.J.; Irving-Rodgers, H.F. Morphological classification of bovine ovarian follicles. Reproduction 2010, 139, 309–318. [Google Scholar] [CrossRef]
- Kulin, S.; Bastiaans, B.A.; Hollanders, H.M.G.; Janssen, H.J.G.; Goverde, H.J.M. Human serum and follicular fluid stimulate hyperactivation of human spermatozoa after preincubation. Fertil. Steril. 1994, 62, 1234–1237. [Google Scholar] [CrossRef]
- Hess, K.A.; Chen, L.; Larsen, W.J. The Ovarian Blood Follicle Barrier Is Both Charge- and Size-Selective in Mice1. Biol. Reprod. 1998, 58, 705–711. [Google Scholar] [CrossRef]
- Schweigert, F.J.; Gericke, B.; Wolfram, W.; Kaisers, U.; Dudenhausen, J.W. Peptide and protein profiles in serum and follicular fluid of women undergoing IVF. Hum. Reprod. 2006, 21, 2960–2968. [Google Scholar] [CrossRef]
- Siu, M.K.Y.; Cheng, C.Y. The Blood-Follicle Barrier (BFB) in Disease and in Ovarian Function. In Biology and Regulation of Blood-Tissue Barriers; Cheng, C.Y., Ed.; Springer: New York, NY, USA, 2013; pp. 186–192. [Google Scholar]
- Manarang-Pangan, S.; Menge, A.C. Immunologic studies on human follicular fluid. Fertil. Steril. 1971, 22, 367–372. [Google Scholar] [CrossRef]
- Clarke, G.N.; Hsieh, C.; Koh, S.H.; Cauchi, M.N. Sperm Antibodies, Immunoglobulins, and Complement in Human Follicular Fluid. Am. J. Reprod. Immunol. 1984, 5, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Schweigert, F.J.; Steinhagen, B.; Raila, J.; Siemann, A.; Peet, D.; Buscher, U. Concentrations of carotenoids, retinol and α-tocopherol in plasma and follicular fluid of women undergoing IVF. Hum. Reprod. 2003, 18, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- Anifandis, G.; Koutselini, E.; Stefanidis, I.; Liakopoulos, V.; Leivaditis, C.; Mantzavinos, T.; Vamvakopoulos, N. Serum and follicular fluid leptin levels are correlated with human embryo quality. Reproduction 2005, 130, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Buckingham, K.L.; Stone, P.R.; Smith, J.F.; Chamley, L.W. Antiphospholipid antibodies in serum and follicular fluid—Is there a correlation with IVF implantation failure? Hum. Reprod. 2006, 21, 728–734. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cai, Y.Y.; Lin, N.; Zhong, L.P.; Duan, H.J.; Dong, Y.H.; Wu, Z.; Su, H. Serum and follicular fluid thyroid hormone levels and assisted reproductive technology outcomes. Reprod. Biol. Endocrinol. 2019, 17, 90. [Google Scholar] [CrossRef] [PubMed]
- Nagy, R.A.; Hollema, H.; Andrei, D.; Jurdzinski, A.; Kuipers, F.; Hoek, A.; Tietge, U.J.F. The Origin of Follicular Bile Acids in the Human Ovary. Am. J. Pathol. 2019, 189, 2036–2045. [Google Scholar] [CrossRef]
- Silva, A.F.; Ramalho-Santos, J.; Amaral, S. The impact of antisperm antibodies on human male reproductive function: An update. Reproduction 2021, 162, R55–R71. [Google Scholar] [CrossRef]
- Choudhury, S.R. Human reproductive failure I: Immunological factors. Hum. Reprod. Update 2001, 7, 113–134. [Google Scholar] [CrossRef]
- Nielsen, H.S.; Witvliet, M.D.; Steffensen, R.; Haasnoot, G.W.; Goulmy, E.; Christiansen, O.B.; Claas, F. The presence of HLA-antibodies in recurrent miscarriage patients is associated with a reduced chance of a live birth. J. Reprod. Immunol. 2010, 87, 67–73. [Google Scholar] [CrossRef]
- Martín-Villa, J.M.; Luque, I.; Martínez-Quiles, N.; Corell, A.; Regueiro, J.R.; Timón, M.; Arnaiz-Villena, A. Diploid Expression of Human Leukocyte Antigen Class I and Class II Molecules on Spermatozoa and their Cyclic Inverse Correlation with Inhibin Concentration1. Biol. Reprod. 1996, 55, 620–629. [Google Scholar] [CrossRef] [PubMed]
- Paradisi, R.; Neri, S.; Pession, A.; Magrini, E.; Bellavia, E.; Ceccardi, S.; Flamigni, C. Human Leukocyte Antigen Ii Expression in Sperm Cells: Comparison Between Fertile and Infertile Men. Arch. Androl. 2000, 45, 203–213. [Google Scholar] [PubMed]
- Sereshki, N.; Andalib, A.; Ghahiri, A.; Mehrabian, F.; Sherkat, R.; Rezaei, A.; Wilkinson, D. The expression of human leukocyte antigen by human ejaculated spermatozoa. Mol. Genet. Genom. Med. 2019, 7, e1005. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Wan, Q.-H.; Zhang, H.-M.; Fang, S.-G. Reproductive Strategy Inferred from Major Histocompatibility Complex-Based Inter-Individual, Sperm-Egg, and Mother-Fetus Recognitions in Giant Pandas (Ailuropoda melanoleuca). Cells 2019, 8, 257. [Google Scholar] [CrossRef]
- Fitzpatrick, J.L.; Willis, C.; Devigili, A.; Young, A.; Carroll, M.; Hunter, H.R.; Brison, D.R. Chemical signals from eggs facilitate cryptic female choice in humans. Proc. R. Soc. Lond. B Biol. Sci. 2020, 287, 20200805. [Google Scholar] [CrossRef] [PubMed]
- Gardner, D.K.; Weissman, A.; Howles, C.M.; Shoham, Z. (Eds.) Textbook of Assisted Reproductive Techniques: Volume 2: Clinical Perspectives, 5th ed.; CRC Press: Boca Raton, FL, USA, 2018. [Google Scholar]
- Ray, A.; Shah, A.; Gudi, A.; Homburg, R. Unexplained infertility: An update and review of practice. Reprod. Biomed. Online 2012, 24, 591–602. [Google Scholar] [CrossRef]
- Magris, M.; Jokiniemi, A.; Kuusipalo, L.; Ritari, J.; Koskela, S.; Partanen, J.; Kekäläinen, J. Structural dissimilarity of partners’ immune genes increases sperm viability in women’s reproductive tract. J. Evol. Biol. 2021, 34, 1125–1132. [Google Scholar] [CrossRef]
- Aguilar, J.; Reyley, M. The uterine tubal fluid: Secretion, composition and biological effects. Anim. Reprod. 2005, 2, 91–105. [Google Scholar]
- Sun, F.; Bahat, A.; Gakamsky, A.; Girsh, E.; Katz, N.; Giojalas, L.C.; Tur-Kaspa, I.; Eisenbach, M. Human sperm chemotaxis: Both the oocyte and its surrounding cumulus cells secrete sperm chemoattractants. Hum. Reprod. 2005, 20, 761–767. [Google Scholar] [CrossRef]
- Ralt, D.; Goldenberg, M.; Fetterolf, P.; Thompson, D.; Dor, J.; Mashiach, S.; Garbers, D.L.; Eisenbach, M. Sperm attraction to a follicular factor(s) correlates with human egg fertilizability. Proc. Natl. Acad. Sci. USA 1991, 88, 2840–2844. [Google Scholar] [CrossRef]
- Vieira, L.A.; Diana, A.; Soriano-Úbeda, C.; Matás, C. Selection of Boar Sperm by Reproductive Biofluids as Chemoattractants. Animals 2021, 11, 53. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.Z.; Wu, J.Z.; Chen, C.Q.; Dorfmann, A.D. Human follicular fluid-induced acrosome reaction predicts sperm fertilizing ability in vitro. Fertil. Steril. 2007, 88, S138. [Google Scholar] [CrossRef]
- Wedekind, C.; Chapuisat, M.; Macas, E.; Rülicke, T. Non-random fertilization in mice correlates with the MHC and something else. Heredity 1996, 77, 400–409. [Google Scholar] [CrossRef][Green Version]
- Castilla, J.A.; Gil, T.; Rodriguez, F.; Molina, J.; Samaniego, F.; Vergara, F.; Herruzo, A.J. Lack of Expression of HLA Antigens on Immature Germ Cells from Ejaculates with Antisperm Antibodies. Am. J. Reprod. Immunol. 1993, 30, 9–14. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen, 6th ed.; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Kay, V.; Robertson, L. Hyperactivated motility of human spermatozoa: A review of physiological function and application in assisted reproduction. Hum. Reprod. Update 1998, 4, 776–786. [Google Scholar] [CrossRef]
- Ritari, J.; Hyvärinen, K.; Clancy, J.; FinnGen Partanen, J.; Koskela, S. Increasing accuracy of HLA imputation by a population-specific reference panel in a FinnGen biobank cohort. NAR Genom. Bioinform. 2020, 2, lqaa030. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Shen, J.; Cox, C.; Wakefield, J.C.; Ehm, M.G.; Nelson, M.R.; Weir, B.S. HIBAG—HLA genotype imputation with attribute bagging. Pharm. J. 2014, 14, 192–200. [Google Scholar] [CrossRef]
- Crawley, M.J. The R Book; Hoboken, N.J., Ed.; Wiley: Chichester, UK, 2007. [Google Scholar]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Kuznetsova, A.; Brockhoff, P.B.; Christensen, R.H.B. lmerTest Package: Tests in Linear Mixed Effects Models. J. Stat. Softw. 2017, 82, 1–26. [Google Scholar] [CrossRef]
- Brooks, M.E.; Kristensen, K.; van Benthem, K.J.; Magnusson, A.; Berg, C.W.; Nielsen, A.; Skaug, H.J.; Mächler, M.; Bolker, B.M. Glmm TMB Balances Speed and Flexibility Among Packages for Zero-inflated Generalized Linear Mixed Modeling. R J. 2017, 9, 378–400. [Google Scholar] [CrossRef]
- Harrison, X.A. A comparison of observation-level random effect and Beta-Binomial models for modelling overdispersion in Binomial data in ecology & evolution. PeerJ 2015, 3, e1114. [Google Scholar] [PubMed]
- Nakagawa, S.; Schielzeth, H. A general and simple method for obtainingR2 from generalized linear mixed-effects models. Methods Ecol. Evol. 2013, 4, 133–142. [Google Scholar] [CrossRef]
- Fox, J.; Weisberg, S. An R Companion to Applied Regression, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2019. [Google Scholar]
| Time Point | 60 Min | 180 Min | 300 Min | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment | Follicular Fluid | Serum | Follicular Fluid | Serum | Follicular Fluid | Serum | ||||||||||||
| Fixed effect | F-value | df | p-value | F-value | df | p-value | F-value | df | p-value | F-value | df | p-value | F-value | df | p-value | F-value | df | p-value |
| Replicate tube | 10.895 | 1 | 0.001 | 34.155 | 1 | 0.028 | 11.016 | 1 | 0.001 | 0.081 | 1 | 0.803 | 80.422 | 1 | <0.001 | 45.576 | 1 | <0.001 |
| Random effects: | χ2 | df | p-value | χ2 | df | p-value | χ2 | df | p-value | χ2 | df | p-value | χ2 | df | p-value | χ2 | df | p-value |
| 1|Male | 128.587 | 1 | <0.001 | 131.190 | 1 | <0.001 | 72.455 | 1 | <0.001 | 131.285 | 1 | <0.001 | 64.600 | 1 | <0.001 | 41.918 | 1 | <0.001 |
| 1|Female | 8.098 | 1 | 0.004 | 13.668 | 1 | <0.001 | 0.350 | 1 | 0.554 | 6.895 | 1 | 0.009 | 0.000 | 1 | 1.000 | 0.000 | 1 | 1.000 |
| 1|Male:Female | 0.827 | 1 | 0.363 | 0.535 | 1 | 0.465 | 11.528 | 1 | <0.001 | 2.631 | 1 | 0.105 | 2.023 | 1 | 0.155 | 47.970 | 1 | <0.001 |
| 1|Sample | 0.000 | 1 | 1.000 | 0.352 | 1 | 0.553 | 0.000 | 1 | 1.000 | 7.043 | 1 | 0.008 | 0.000 | 1 | 1.000 | 0.000 | 1 | 1.000 |
| R2m = 0.006; R2c = 0.875 | R2m = 0.023; R2c = 0.883 | R2m = 0.011; R2c = 0.786 | R2m = 0.000; R2c = 0.898 | R2m = 0.093; R2c = 0.744 | R2m = 0.044; R2c = 0.744 | |||||||||||||
| Time Point | 60 Min | 180 Min | 300 Min | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Fixed Effects: | F-value | df | p-value | F-value | df | p-value | F-value | df | p-value |
| VCL in Serum | 5.391 | 1 | 0.021 | 9.402 | 1 | 0.003 | 9.804 | 1 | 0.002 |
| Replicate Tube | 3.668 | 1 | 0.057 | 18.692 | 1 | 0.043 | 71.175 | 1 | <0.001 |
| Random Effects: | χ2 | df | p-value | χ2 | df | p-value | χ2 | df | p-value |
| 1|Male | 84.694 | 1 | <0.001 | 24.468 | 1 | <0.001 | 30.020 | 1 | <0.001 |
| 1|Female | 5.978 | 1 | 0.014 | 0.524 | 1 | 0.469 | 0.0000 | 1 | 0.999 |
| 1|Male:Female | 1.579 | 1 | 0.209 | 25.336 | 1 | <0.001 | 8.6606 | 1 | 0.003 |
| 1|Sample | 0.000 | 1 | 1.000 | 0.004 | 1 | 0.951 | 0.0000 | 1 | 0.999 |
| R2m = 0.034; R2c = 0.846 | R2m = 0.103; R2c = 0.786 | R2m = 0.158; R2c = 0.775 | |||||||
| Response Variable | VCL | Hyperactivation | ||||
|---|---|---|---|---|---|---|
| Fixed Effects: | F-value | df | p-value | χ2 | df | p-value |
| Treatment | 2.143 | 1 | 0.160 | 1.870 | 1 | 0.171 |
| Replicate Tube | 44.988 | 1 | <0.001 | 59.141 | 1 | <0.001 |
| Random Effects: | χ2 | df | p-value | χ2 | df | p-value |
| 1|Treatment:Male | 118.825 | 1 | <0.001 | 124.81 | 1 | <0.001 |
| 1|Treatment:Female | 0.035 | 1 | 0.851 | 0.000 | 1 | 1.000 |
| 1|Treatment:Male:Female | 49.487 | 1 | <0.001 | 44.413 | 1 | <0.001 |
| 1|Sample | 0.000 | 1 | 1.000 | 0.000 | 1 | 1.000 |
| R2m = 0.088; R2c = 0.797 | R2m = 0.040; R2c = 0.384 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Łukasiewicz, A.; Huhta, K.; Ritari, J.; Peräsaari, J.; Allinen, P.; Malinen, M.; Jokiniemi, A.; Turunen, T.; Partanen, J.; Kekäläinen, J. Sperm Physiological Response to Female Serum—Potential New Insights into the Reproductive Incompatibility Diagnostics. Int. J. Mol. Sci. 2022, 23, 3428. https://doi.org/10.3390/ijms23073428
Łukasiewicz A, Huhta K, Ritari J, Peräsaari J, Allinen P, Malinen M, Jokiniemi A, Turunen T, Partanen J, Kekäläinen J. Sperm Physiological Response to Female Serum—Potential New Insights into the Reproductive Incompatibility Diagnostics. International Journal of Molecular Sciences. 2022; 23(7):3428. https://doi.org/10.3390/ijms23073428
Chicago/Turabian StyleŁukasiewicz, Aleksandra, Kari Huhta, Jarmo Ritari, Juha Peräsaari, Pia Allinen, Marjo Malinen, Annalaura Jokiniemi, Tanja Turunen, Jukka Partanen, and Jukka Kekäläinen. 2022. "Sperm Physiological Response to Female Serum—Potential New Insights into the Reproductive Incompatibility Diagnostics" International Journal of Molecular Sciences 23, no. 7: 3428. https://doi.org/10.3390/ijms23073428
APA StyleŁukasiewicz, A., Huhta, K., Ritari, J., Peräsaari, J., Allinen, P., Malinen, M., Jokiniemi, A., Turunen, T., Partanen, J., & Kekäläinen, J. (2022). Sperm Physiological Response to Female Serum—Potential New Insights into the Reproductive Incompatibility Diagnostics. International Journal of Molecular Sciences, 23(7), 3428. https://doi.org/10.3390/ijms23073428






