The Application of Biomaterials in Spinal Cord Injury
Abstract
1. Introduction
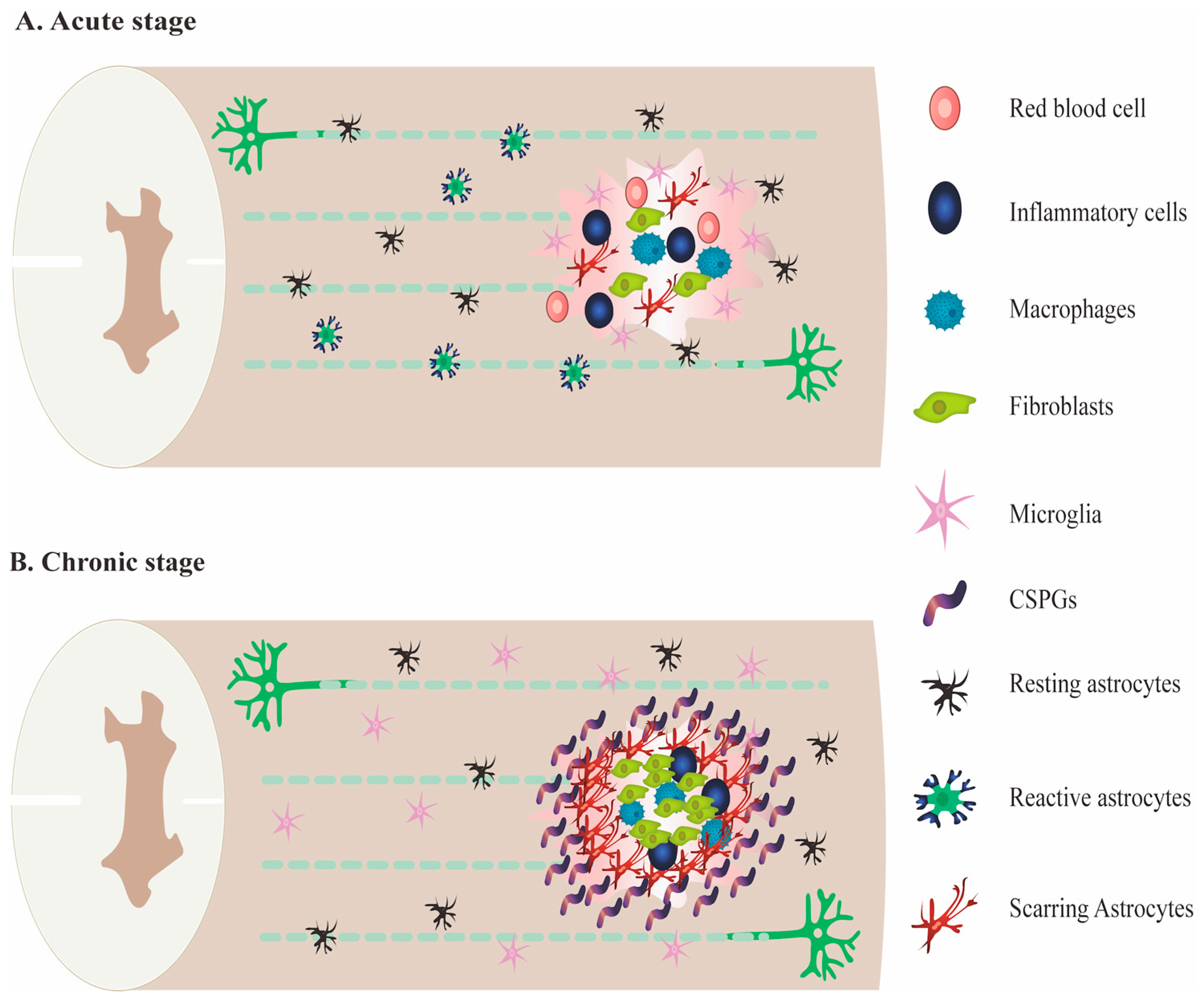
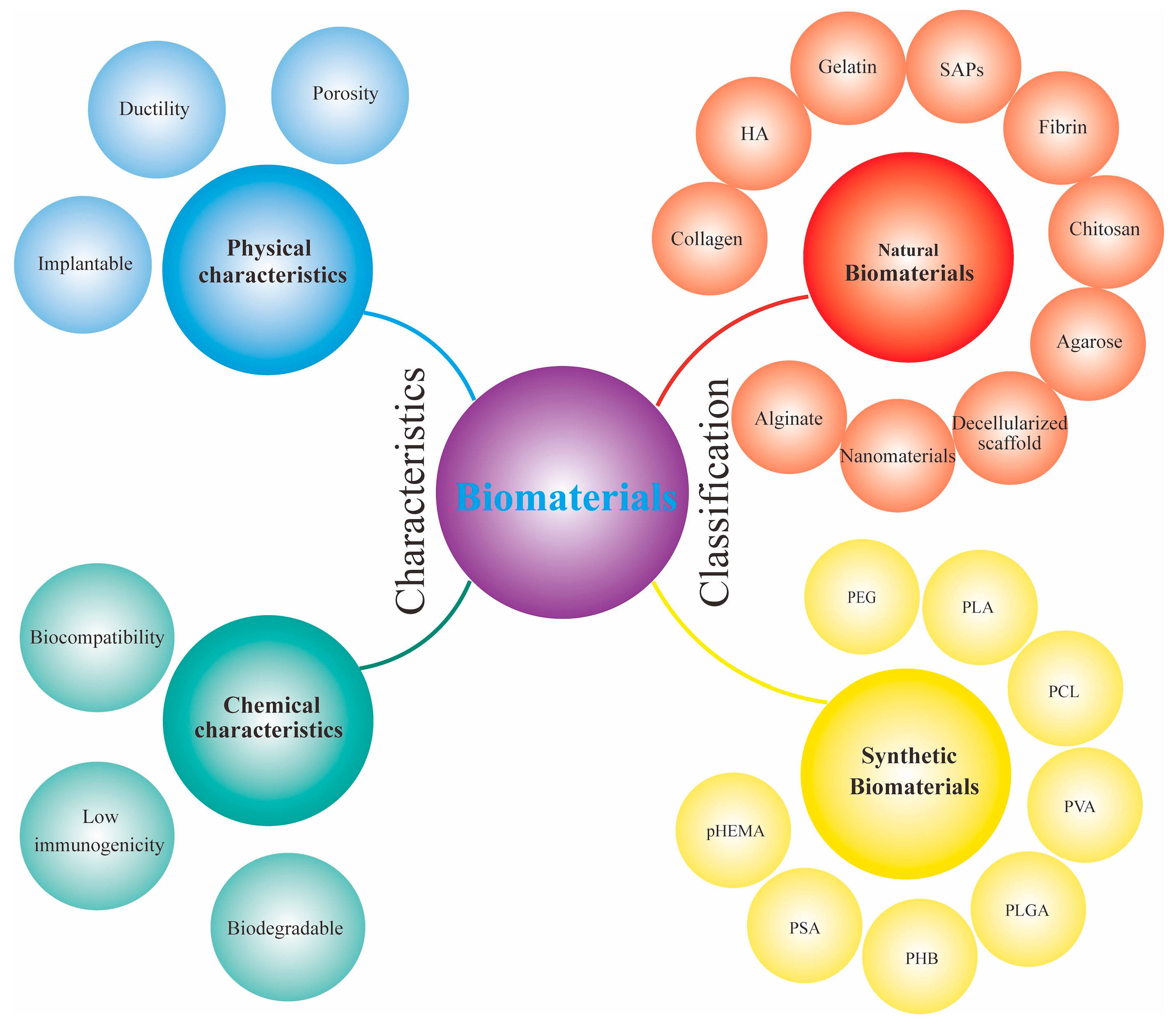
2. Spinal Cord Injury
3. The Application of Biomaterials in SCI
3.1. Natural Materials
3.1.1. Hyaluronic Acid
3.1.2. Collagen
3.1.3. Fibrin
3.1.4. Decellularized Scaffold
3.1.5. Chitosan
3.1.6. Alginate
3.1.7. Agarose
3.1.8. Nanomaterials
3.1.9. Self-Assembled Peptides
3.2. Synthetic Materials
3.2.1. Polyethylene Glycol
3.2.2. Polylactic Acid
3.2.3. Poly(Lactic-Co-Glycolic Acid)
3.2.4. Polycaprolactone
3.2.5. Polyvinyl Alcohol (PVA)
3.2.6. Poly-Beta-Hydroxybutyrate
3.2.7. Polysialic Acid
3.2.8. Poly(2-Hydroxyethyl Methacrylate)
3.3. Titanium Alloys
3.4. 3D Scaffold
4. Clinical Application of Biomaterial Scaffolds
5. Summary and Future Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hachem, L.D.; Ahuja, C.S.; Fehlings, M.G. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J. Spinal Cord Med. 2017, 40, 665–675. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Chen, D.; Chen, C.; Wang, K.; Tang, L.; Yuzhe, L.I.; Aimin, W.U. The epidemiology and disease burden of traumatic spinal cord injury in China: A systematic review. Chin. J. Evid. Based Med. 2018, 18, 143–150. [Google Scholar]
- Ikada, Y. Challenges in tissue engineering. J. R. Soc. Interface 2006, 3, 589–601. [Google Scholar] [CrossRef] [PubMed]
- Thompson, B.C.; Murray, E.; Wallace, G.G. Graphite Oxide to Graphene. Biomaterials to Bionics. Adv. Mater. 2015, 27, 7563–7582. [Google Scholar] [CrossRef] [PubMed]
- Yang Junsong, H.D. Research status and future of stem cell therapy for spinal cord injury. Chin. J. Trauma 2021, 37, 6–10. [Google Scholar] [CrossRef]
- Berg, M.V.D.; Castellote, J.; Mahillo-Fernandez, I.; de Pedro-Cuesta, J. Incidence of Spinal Cord Injury Worldwide: A Systematic Review. Neuroepidemiology 2010, 34, 184–192, discussion 192. [Google Scholar] [CrossRef] [PubMed]
- Hagen, E.M. Acute complications of spinal cord injuries. World J. Orthop. 2015, 6, 17–23. [Google Scholar] [CrossRef]
- Zou, X.; Jing, C.; Yingmei, Q.; Ying, L. Care of a patient with old spinal cord injury causing paraplegia combined with diabetic pressure sores. Jilin Med. 2011, 32, 6963–6964. [Google Scholar]
- Anjum, A.; Yazid, M.; Daud, M.F.; Idris, J.; Lokanathan, Y. Spinal Cord Injury: Pathophysiology, Multimolecular Interactions, and Underlying Recovery Mechanisms. Int. J. Mol. Sci. 2020, 21, 7533. [Google Scholar] [CrossRef]
- Jian, Q.I.; Zhang, J.J.; Meng, Q.X.; Zhao, T.B. Pathology and Treatment of Spinal Cord Injury. Prog. Mod. Biomed. 2017, 17, 4179–4183. [Google Scholar]
- Ahuja, C.S.; Satoshi, N.; Lindsay, T.; Jefferson, W.; Brian, K.; James, H.; David, C.; Fehlings, M.G. Traumatic Spinal Cord Injury—Repair and Regeneration. Neurosurgery 2017, 80, S9–S22. [Google Scholar] [CrossRef]
- Weiner, H.L. A shift from adaptive to innate immunity: A potential mechanism of disease progression in multiple sclerosis. J. Neurol. 2008, 255 (Suppl. S1), 3–11. [Google Scholar] [CrossRef] [PubMed]
- Dimitrijevic, M.R.; Danner, S.M.; Mayr, W. Neurocontrol of Movement in Humans With Spinal Cord Injury. Artif. Organs 2015, 39, 823–833. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Fan, C.; You, Z.; Xiao, Z.; Zhao, Y.; Dai, J. Advances in Biomaterial-Based Spinal Cord Injury Repair. Adv. Funct. Mater. 2022, 32, 2110628. [Google Scholar] [CrossRef]
- Kiyotake, E.A.; Martin, M.D.; Detamore, M.S. Regenerative rehabilitation with conductive biomaterials for spinal cord injury. Acta Biomater. 2022, 139, 43–64. [Google Scholar] [CrossRef]
- Pei, D. Research status of spinal cord injury at home and abroad. Everyone Healthy 2017, 12, 440–444. [Google Scholar]
- Dimar, J.R.; Glassman, S.D.; Raque, G.H.; Zhang, Y.P.; Shields, C.B. The Influence of Spinal Canal Narrowing and Timing of Decompression on Neurologic Recovery After Spinal Cord Contusion in a Rat Model. Spine 1999, 24, 1623. [Google Scholar] [CrossRef]
- Jing-Feng, L.I.; Zhen-Hua, X.U.; Chen, L.B.; Wang, J.P.; Zhang, S.W.; Orthopedics, D.O. Paraspinal approach combined with posterior midline approach in treatment of thoracolumbar fractures with nerve injury. Chin. J. Bone Jt. Inj. 2015, 30, 263–265. [Google Scholar]
- Mallei, A.; Aden, S.A.; Bachis, A.; Brandoli, C.; Ongini, E.; Mocchetti, I. The nitrosteroid NCX 1015, a prednisolone derivative, improves recovery of function in rats after spinal cord injury. Brain Res. 2005, 1062, 16–25. [Google Scholar] [CrossRef]
- Jinchuan, S.; Qingmin, F. Advances in research on neurotrophic factors and spinal cord injury. J. Binzhou Med. Coll. 2013, 36, 136–138. [Google Scholar]
- Marina, G.; Vladislav, V.; Harrell, C.; Crissy, F.; Nemanja, J.; Nebojsa, A.; Miodrag, S. Stem Cells Therapy for Spinal Cord Injury. Int. J. Mol. Ences 2018, 19, 1039. [Google Scholar]
- Haoxian, C.; Lijun, Y.; Yonggang, A. Effects of Exosomes Derived from Adipose-Derived Mesenchymal Stem cells on Macrophage Polarization and Glial Scar Formation in Rats with Spinal Cord Injury. Front. Mol. Neurosci. 2022, 43, 333–338. [Google Scholar] [CrossRef]
- Yamazaki, K.; Kawabori, M.; Seki, T.; Houkin, K. Clinical Trials of Stem Cell Treatment for Spinal Cord Injury. Int. J. Mol. Sci. 2020, 21, 3994. [Google Scholar] [CrossRef] [PubMed]
- Wiliams, R.R.; Bunge, M.B. Schwann cell transplantation: A repair strategy for spinal cord injury? Prog Brain Res. 2012, 201, 295–312. [Google Scholar] [CrossRef]
- Suzuki, H.; Sakai, T. Current Concepts of Stem Cell Therapy for Chronic Spinal Cord Injury. Int. J. Mol. Sci. 2021, 22, 7435. [Google Scholar] [CrossRef]
- Marin, E.; Boschetto, F.; Pezzotti, G. Biomaterials and biocompatibility: An historical overview. J. Biomed. Mater. Res. Part A 2020, 108, 1617–1633. [Google Scholar] [CrossRef]
- Masaeli, R.; Zandsalimi, K.; Tayebi, L. Biomaterials Evaluation: Conceptual Refinements and Practical Reforms. Ther. Innov. Regul. Sci. 2019, 53, 120–127. [Google Scholar] [CrossRef]
- Ratner, B.D.; Zhang, G. A History of Biomaterials. In Biomaterials Science; Academic Press: Cambridge, MA, USA, 2020; pp. 21–34. [Google Scholar]
- Yuan, T.; Zhang, L.; Li, K.; Fan, H.; Fan, Y.; Liang, J.; Zhang, X. Collagen hydrogel as an immunomodulatory scaffold in cartilage tissue engineering. J. Biomed. Mater. Res. Part B Appl. Biomater. 2014, 102, 337–344. [Google Scholar] [CrossRef]
- Masand, S.N.; Chen, J.; Perron, I.J.; Hammerling, B.C.; Loers, G.; Schachner, M.; Shreiber, D.I. The effect of glycomimetic functionalized collagen on peripheral nerve repair. Biomaterials 2012, 33, 8353–8362. [Google Scholar] [CrossRef][Green Version]
- Yang, Y.; Fan, Y.; Zhang, H.; Zhang, Q.; Zhao, Y.; Xiao, Z.; Liu, W.; Chen, B.; Gao, L.; Sun, Z.; et al. Small molecules combined with collagen hydrogel direct neurogenesis and migration of neural stem cells after spinal cord injury. Biomaterials 2021, 269, 120479. [Google Scholar] [CrossRef]
- Kim, B.-S.; Baez, C.E.; Atala, A. Biomaterials for tissue engineering. World J. Urol. 2000, 18, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhai, P.; Chen, X.; Schreyer, D.J.; Sun, X.; Cui, F. Bioengineered Scaffolds for Spinal Cord Repair. Tissue Eng. Part B Rev. 2011, 17, 177–194. [Google Scholar] [CrossRef] [PubMed]
- Joyce, K.; Fabra, G.T.; Bozkurt, Y.; Pandit, A. Bioactive potential of natural biomaterials: Identification, retention and assessment of biological properties. Signal Transduct. Target. Ther. 2021, 6, 122. [Google Scholar] [CrossRef] [PubMed]
- Zarei-Kheirabadi, M.; Sadrosadat, H.; Mohammadshirazi, A.; Jaberi, R.; Sorouri, F.; Khayyatan, F.; Kiani, S. Human embryonic stem cell-derived neural stem cells encapsulated in hyaluronic acid promotes regeneration in a contusion spinal cord injured rat. Int. J. Biol. Macromol. 2020, 148, 1118–1129. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.-T.; He, Y.; Xu, C.-L.; Wang, Y.; Liu, B.-F.; Wang, X.-M.; Sun, X.-D.; Cui, F.-Z.; Xu, Q.-Y. Hyaluronic acid hydrogel modified with nogo-66 receptor antibody and poly-L-lysine to promote axon regrowth after spinal cord injury. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 95B, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Xiao, Z.; Zhang, H.; Chen, B.; Tang, G.; Hou, X.; Ding, W.; Wang, B.; Zhang, P.; Dai, J.; et al. Linear Ordered Collagen Scaffolds Loaded with Collagen-Binding Neurotrophin-3 Promote Axonal Regeneration and Partial Functional Recovery after Complete Spinal Cord Transection. J. Neurotrauma 2010, 27, 1671–1683. [Google Scholar] [CrossRef]
- Breen, B.A.; Kraskiewicz, H.; Ronan, R.; Kshiragar, A.; Patar, A.; Sargeant, T.; Pandit, A.; McMahon, S.S. Therapeutic Effect of Neurotrophin-3 Treatment in an Injectable Collagen Scaffold Following Rat Spinal Cord Hemisection Injury. ACS Biomater. Sci. Eng. 2017, 3, 1287–1295. [Google Scholar] [CrossRef]
- Wang, L.; Shi, Q.; Dai, J.; Gu, Y.; Feng, Y.; Chen, L. Increased vascularization promotes functional recovery in the transected spinal cord rats by implanted vascular endothelial growth factor-targeting collagen scaffold. J. Orthop. Res. 2018, 36, 1024–1034. [Google Scholar] [CrossRef]
- Liu, W.; Xu, B.; Xue, W.; Yang, B.; Fan, Y.; Chen, B.; Xiao, Z.; Xue, X.; Sun, Z.; Shu, M.; et al. A functional scaffold to promote the migration and neuronal differentiation of neural stem/progenitor cells for spinal cord injury repair. Biomaterials 2020, 243, 119941. [Google Scholar] [CrossRef]
- Han, S.; Xiao, Z.; Li, X.; Zhao, H.; Wang, B.; Qiu, Z.; Mei, X.; Xu, B.; Fan, C.; Chen, B.; et al. Human placenta-derived mesenchymal stem cells loaded on linear ordered collagen scaffold improves functional recovery after completely transected spinal cord injury in canine. Sci. China Life Sci. 2018, 61, 2–13. [Google Scholar] [CrossRef]
- Kataoka, K.; Suzuki, Y.; Kitada, M.; Hashimoto, T.; Chou, H.; Bai, H.; Ohta, M.; Wu, S.; Suzuki, K.; Ide, C. Alginate Enhances Elongation of Early Regenerating Axons in Spinal Cord of Young Rats. Tissue Eng. 2004, 10, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Fan, L.; Liu, C.; Chen, X.; Zou, Y.; Zhou, Z.; Lin, C.; Tan, G.; Zhou, L.; Ning, C.; Wang, Q. Directing Induced Pluripotent Stem Cell Derived Neural Stem Cell Fate with a Three-Dimensional Biomimetic Hydrogel for Spinal Cord Injury Repair. ACS Appl. Mater. Interfaces 2018, 10, 17742–17755. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Xu, P.; Guan, J.; Zhang, C.; Chang, J.; Yang, F.; Xiao, H.; Sun, H.; Zhang, Z.; Wang, M.; et al. Promoting 3D neuronal differentiation in hydrogel for spinal cord regeneration. Colloids Surfaces B Biointerfaces 2020, 194, 111214. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yang, H.; Chen, D.; Xie, Y.; Tai, C.; Wang, L.; Wang, P.; Bin Wang, B. Three-dimensional bioprinting sodium alginate/gelatin scaffold combined with neural stem cells and oligodendrocytes markedly promoting nerve regeneration after spinal cord injury. Regen. Biomater. 2022, 9, rbac038. [Google Scholar] [CrossRef] [PubMed]
- Shulman, I.; Ogurcov, S.; Kostennikov, A.; Rogozin, A.; Garanina, E.; Masgutova, G.; Sergeev, M.; Rizvanov, A.; Mukhamedshina, Y. Application of Autologous Peripheral Blood Mononuclear Cells into the Area of Spinal Cord Injury in a Subacute Period: A Feasibility Study in Pigs. Biology 2021, 10, 87. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Yu, S.; Cao, Z.; Yang, Y.; Yu, X.; Mao, H.-Q.; Wang, L.-N.; Sun, X.; Zhao, L.; Wang, X. Hierarchically aligned fibrin nanofiber hydrogel accelerated axonal regrowth and locomotor function recovery in rat spinal cord injury. Int. J. Nanomed. 2018, 13, 2883–2895. [Google Scholar] [CrossRef] [PubMed]
- Monfared, M.J.; Nasirinezhad, F.; Ebrahimi-Barough, S.; Hasanzade, G.; Saberi, H.; Tavangar, S.M.; Asadpour, S.; Aryan, L.; Barabadi, Z.; Ai, J. Transplantation of miR-219 overexpressed human endometrial stem cells encapsulated in fibrin hydrogel in spinal cord injury. J. Cell. Physiol. 2019, 234, 18887–18896. [Google Scholar] [CrossRef]
- Cerqueira, S.R.; Lee, Y.-S.; Cornelison, R.C.; Mertz, M.W.; Wachs, R.A.; Schmidt, C.E.; Bunge, M.B. Decellularized peripheral nerve supports Schwann cell transplants and axon growth following spinal cord injury. Biomaterials 2018, 177, 176–185. [Google Scholar] [CrossRef]
- Liu, J.; Li, K.; Huang, K.; Yang, C.; Huang, Z.; Zhao, X.; Song, S.; Pang, T.; Zhou, J.; Wang, Y.; et al. Acellularized spinal cord scaffolds incorporating bpV(pic)/PLGA microspheres promote axonal regeneration and functional recovery after spinal cord injury. RSC Adv. 2020, 10, 18677–18686. [Google Scholar] [CrossRef]
- Yin, H.; Jiang, T.; Deng, X.; Yu, M.; Xing, H.; Ren, X. A cellular spinal cord scaffold seeded with rat adipose-derived stem cells facilitates functional recovery via enhancing axon regeneration in spinal cord injured rats. Mol. Med. Rep. 2018, 17, 2998–3004. [Google Scholar] [CrossRef]
- Chedly, J.; Soares, S.; Montembault, A.; von Boxberg, Y.; Veron-Ravaille, M.; Mouffle, C.; Benassy, M.-N.; Taxi, J.; David, L.; Nothias, F. Physical chitosan microhydrogels as scaffolds for spinal cord injury restoration and axon regeneration. Biomaterials 2017, 138, 91–107. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.D.; Shao, J.L.; Deng, D.J.; Zhou, Z.G.; Zhou, X.B.; Lin, Y.X.; Li, Z.Z. A chitosan scaffold infused with neurotrophin-3 and human umbilical cord mesenchymal stem cells suppresses inflammation and promotes functional recovery after spinal cord injury in mice. Int. J. Clin. Exp. Med. 2017, 10, 11672–11679. [Google Scholar]
- Hosseini, S.M.; Sharafkhah, A.; Koohi-Hosseinabadi, O.; Semsar-Kazerooni, M. Transplantation of Neural Stem Cells Cultured in Alginate Scaffold for Spinal Cord Injury in Rats. Asian Spine J. 2016, 10, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Schackel, T.; Kumar, P.; Günther, M.; Liu, S.; Brunner, M.; Sandner, B.; Puttagunta, R.; Müller, R.; Weidner, N.; Blesch, A.; et al. Peptides and Astroglia Improve the Regenerative Capacity of Alginate Gels in the Injured Spinal Cord. Tissue Eng. Part A 2019, 25, 522–537. [Google Scholar] [CrossRef]
- Gao, M.; Lu, P.; Lynam, D.; Bednark, B.; Campana, W.M.; Sakamoto, J.; Tuszynski, M. BDNF gene delivery within and beyond templated agarose multi-channel guidance scaffolds enhances peripheral nerve regeneration. J. Neural Eng. 2016, 13, 066011. [Google Scholar] [CrossRef]
- Han, S.; Lee, J.Y.; Heo, E.Y.; Kwon, I.K.; Yune, T.Y.; Youn, I. Implantation of a Matrigel-loaded agarose scaffold promotes functional regeneration of axons after spinal cord injury in rat. Biochem. Biophys. Res. Commun. 2018, 496, 785–791. [Google Scholar] [CrossRef]
- Yang, B.; Liang, C.; Chen, D.; Cheng, F.; Zhang, Y.; Wang, S.; Shu, J.; Huang, X.; Wang, J.; Xia, K.; et al. A conductive supramolecular hydrogel creates ideal endogenous niches to promote spinal cord injury repair. Bioact. Mater. 2022, 15, 103–119. [Google Scholar] [CrossRef]
- Kim, Y.-T.; Caldwell, J.-M.; Bellamkonda, R.V. Nanoparticle-mediated local delivery of methylprednisolone after spinal cord injury. Biomaterials 2009, 30, 2582–2590. [Google Scholar] [CrossRef]
- Cerqueira, S.R.; Oliveira, J.M.; Silva, N.A.; Leite-Almeida, H.; Ribeiro-Samy, S.; Almeida, A.; Mano, J.F.; Sousa, N.; Salgado, A.J.; Reis, R.L. Microglia Response and In Vivo Therapeutic Potential of Methylprednisolone-Loaded Dendrimer Nanoparticles in Spinal Cord Injury. Small 2013, 9, 738–749. [Google Scholar] [CrossRef]
- Park, J.; Zhang, Y.; Saito, E.; Gurczynski, S.J.; Moore, B.B.; Cummings, B.J.; Anderson, A.J.; Shea, L.D. Intravascular innate immune cells reprogrammed via intravenous nanoparticles to promote functional recovery after spinal cord injury. Proc. Natl. Acad. Sci. USA 2019, 116, 14947–14954. [Google Scholar] [CrossRef]
- Yari-Ilkhchi, A.; Ebrahimi-Kalan, A.; Farhoudi, M.; Mahkam, M. Design of graphenic nanocomposites containing chitosan and polyethylene glycol for spinal cord injury improvement. RSC Adv. 2021, 11, 19992–20002. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Yao, G.S.; Liu, Y.; Wang, J.; Satkunendrarajah, K.; Fehlings, M. The role of neural precursor cells and self assembling peptides in nerve regeneration. J. Otolaryngol. Head Neck Surg. 2013, 42, 60. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zheng, J.; Zheng, Q.; Wu, Y.; Wu, B.; Huang, S.; Fang, W.; Guo, X. FGL-functionalized self-assembling nanofiber hydrogel as a scaffold for spinal cord-derived neural stem cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 46, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.A.; Partyka, P.P.; Jin, Y.; Bouyer, J.; Fischer, I.; Galie, P.A. Vascularization of self-assembled peptide scaffolds for spinal cord injury repair. Acta Biomater. 2020, 104, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Song, I.; Dityatev, A. Crosstalk between glia, extracellular matrix and neurons. Brain Res. Bull. 2018, 136, 101–108. [Google Scholar] [CrossRef]
- A Back, S.; Tuohy, T.M.F.; Chen, H.; Wallingford, N.; Craig, A.; Struve, J.; Luo, N.L.; Banine, F.; Liu, Y.; Chang, A.; et al. Hyaluronan accumulates in demyelinated lesions and inhibits oligodendrocyte progenitor maturation. Nat. Med. 2005, 11, 966–972. [Google Scholar] [CrossRef]
- Gupta, R.C.; Lall, R.; Srivastava, A.; Sinha, A. Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front. Vet. Sci. 2019, 6, 192. [Google Scholar] [CrossRef]
- Moshayedi, P.; Carmichael, S.T. Hyaluronan, neural stem cells and tissue reconstruction after acute ischemic stroke. Biomatter 2013, 3, e23863. [Google Scholar] [CrossRef]
- Frischknecht, R.; Chang, K.-J.; Rasband, M.N.; Seidenbecher, C.I. Neural ECM molecules in axonal and synaptic homeostatic plasticity. Prog. Brain Res. 2014, 214, 81–100. [Google Scholar] [CrossRef]
- Collins, M.N.; Birkinshaw, C. Hyaluronic acid based scaffolds for tissue engineering—A review. Carbohydr. Polym. 2013, 92, 1262–1279. [Google Scholar] [CrossRef]
- Meng, F.; Modo, M.; Badylak, S.F. Biologic scaffold for CNS repair. Regen. Med. 2014, 9, 367–383. [Google Scholar] [CrossRef] [PubMed]
- Sensharma, P.; Madhumathi, G.; Jayant, R.D.; Jaiswal, A.K. Biomaterials and cells for neural tissue engineering: Current choices. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 77, 1302–1315. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.U.; Kim, D.; Jang, C.H.; Kim, G.H. Highly elastic 3D-printed gelatin/HA/placental-extract scaffolds for bone tissue engineering. Theranostics 2022, 12, 4051–4066. [Google Scholar] [CrossRef] [PubMed]
- Hou, S.; Xu, Q.; Tian, W.; Cui, F.; Cai, Q.; Ma, J.; Lee, I.-S. The repair of brain lesion by implantation of hyaluronic acid hydrogels modified with laminin. J. Neurosci. Methods 2005, 148, 60–70. [Google Scholar] [CrossRef]
- Sabelström, H.; Stenudd, M.; Frisén, J. Neural stem cells in the adult spinal cord. Exp. Neurol. 2014, 260, 44–49. [Google Scholar] [CrossRef]
- Mothe, A.J.; Tam, R.Y.; Zahir, T.; Tator, C.H.; Shoichet, M.S. Repair of the injured spinal cord by transplantation of neural stem cells in a hyaluronan-based hydrogel. Biomaterials 2013, 34, 3775–3783. [Google Scholar] [CrossRef]
- Khaing, Z.Z.; Seidlits, S.K. Hyaluronic acid and neural stem cells: Implications for biomaterial design. J. Mater. Chem. B 2015, 3, 7850–7866. [Google Scholar] [CrossRef]
- Sorushanova, A.; Delgado, L.M.; Wu, Z.; Shologu, N.; Kshirsagar, A.; Raghunath, R.; Mullen, A.M.; Bayon, Y.; Pandit, A.; Raghunath, M.; et al. The Collagen Suprafamily: From Biosynthesis to Advanced Biomaterial Development. Adv. Mater. 2019, 31, e1801651. [Google Scholar] [CrossRef]
- Li, X.; Dai, J. Bridging the gap with functional collagen scaffolds: Tuning endogenous neural stem cells for severe spinal cord injury repair. Biomater. Sci. 2018, 6, 265–271. [Google Scholar] [CrossRef]
- Gu, L.; Shan, T.; Ma, Y.-X.; Tay, F.R.; Niu, L. Novel Biomedical Applications of Crosslinked Collagen. Trends Biotechnol. 2019, 37, 464–491. [Google Scholar] [CrossRef]
- Houweling, D.; Lankhorst, A.; Gispen, W.; Bär, P.; Joosten, E. Collagen Containing Neurotrophin-3 (NT-3) Attracts Regrowing Injured Corticospinal Axons in the Adult Rat Spinal Cord and Promotes Partial Functional Recovery. Exp. Neurol. 1998, 153, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Taheri, A.; Kenari, A.A.; Gildberg, A.; Behnam, S. Extraction and Physicochemical Characterization of Greater Lizardfish (Saurida tumbil) Skin and Bone Gelatin. J. Food Sci. 2009, 74, E160–E165. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Song, S.; Chen, Z.; Gao, C.; Li, Y.; Luo, Y.; Huang, J.; Zhang, Z. Release of O-GlcNAc transferase inhibitor promotes neuronal differentiation of neural stem cells in 3D bioprinted supramolecular hydrogel scaffold for spinal cord injury repair. Acta Biomater. 2022, 151, 148–162. [Google Scholar] [CrossRef]
- Sudhadevi, T.; Vijayakumar, H.S.; Hariharan, E.V.; Sandhyamani, S.; Krishnan, L.K. Optimizing fibrin hydrogel toward effective neural progenitor cell delivery in spinal cord injury. Biomed. Mater. 2021, 17, 014102. [Google Scholar] [CrossRef]
- Mukhamedshina, Y.O.; Akhmetzyanova, E.; Kostennikov, A.; Zakirova, E.Y.; Galieva, L.R.; Garanina, E.E.; Rogozin, A.A.; Kiassov, A.P.; Rizvanov, A. Adipose-Derived Mesenchymal Stem Cell Application Combined With Fibrin Matrix Promotes Structural and Functional Recovery Following Spinal Cord Injury in Rats. Front. Pharmacol. 2018, 9, 343. [Google Scholar] [CrossRef]
- He, X.; Yang, L.; Dong, K.; Zhang, F.; Liu, Y.; Ma, B.; Chen, Y.; Hai, J.; Zhu, R.; Cheng, L. Biocompatible exosome-modified fibrin gel accelerates the recovery of spinal cord injury by VGF-mediated oligodendrogenesis. J. Nanobiotechnol. 2022, 20, 360. [Google Scholar] [CrossRef] [PubMed]
- Lang, B.T.; Cregg, J.M.; DePaul, M.A.; Tran, A.P.; Xu, K.; Dyck, S.M.; Madalena, K.M.; Brown, B.P.; Weng, Y.-L.; Li, S.; et al. Modulation of the proteoglycan receptor PTPσ promotes recovery after spinal cord injury. Nature 2015, 518, 404–408. [Google Scholar] [CrossRef]
- Hu, J.; Shangguan, J.; Askar, P.; Xu, J.; Sun, H.; Zhou, S.; Zhu, C.; Su, W.; Gu, Y. Decellularization alters the unfavorable regenerative adverse microenvironment of the injured spinal cord to support neurite outgrowth. Ann. Transl. Med. 2022, 10, 934. [Google Scholar] [CrossRef]
- Cornelison, R.C.; Gonzalez-Rothi, E.J.; Porvasnik, S.L.; Wellman, S.M.; Park, J.H.; Fuller, D.D.; E Schmidt, C. Injectable hydrogels of optimized acellular nerve for injection in the injured spinal cord. Biomed. Mater. 2018, 13, 034110. [Google Scholar] [CrossRef]
- Li, C.; Song, J.; Wang, Y.; Shi, Y.; Ji, J.; Lin, Q.; Liu, Y. Adhesion and proliferation of bone marrow stromal cells on acellular spinal cord scaffolds. Int. J. Neurosci. 2022, 1–10. [Google Scholar] [CrossRef]
- Baldrick, P. The safety of chitosan as a pharmaceutical excipient. Regul. Toxicol. Pharmacol. 2010, 56, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Muzzarelli, R.A.A.; Mattioli-Belmonte, M.; Pugnaloni, A.; Biagini, G. Biochemistry, histology and clinical uses of chitins and chitosans in wound healing. Exs 1999, 87, 251–264. [Google Scholar] [CrossRef] [PubMed]
- Gan, Q.; Wang, T. Chitosan nanoparticle as protein delivery carrier—Systematic examination of fabrication conditions for efficient loading and release. Colloids Surfaces B Biointerfaces 2007, 59, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Patrulea, V.; Ostafe, V.; Borchard, G.; Jordan, O. Chitosan as a starting material for wound healing applications. Eur. J. Pharm. Biopharm. 2015, 97, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Zuo, Y.Y.; Alolabi, H.; Shafiei, A.; Kang, N.; Policova, Z.; Cox, P.N.; Acosta, E.; Hair, M.L.; Neumann, A.W. Chitosan Enhances the In Vitro Surface Activity of Dilute Lung Surfactant Preparations and Resists Albumin-Induced Inactivation. Pediatr. Res. 2006, 60, 125–130. [Google Scholar] [CrossRef][Green Version]
- Borgens, R.B. Cellular Engineering: Molecular Repair of Membranes to Rescue Cells of the Damaged Nervous System. Neurosurgery 2001, 49, 370–379, discussion 378–379. [Google Scholar] [CrossRef]
- Silva, N.A.; Sousa, N.; Reis, R.L.; Salgado, A.J. From basics to clinical: A comprehensive review on spinal cord injury. Prog. Neurobiol. 2014, 114, 25–57. [Google Scholar] [CrossRef]
- Luo, J.; Shi, R. Acrolein induces axolemmal disruption, oxidative stress, and mitochondrial impairment in spinal cord tissue. Neurochem. Int. 2004, 44, 475–486. [Google Scholar] [CrossRef]
- Tuinstra, H.M.; Aviles, M.O.; Shin, S.; Holland, S.J.; Zelivyanskaya, M.L.; Fast, A.G.; Ko, S.Y.; Margul, D.J.; Bartels, A.K.; Boehler, R.M.; et al. Multifunctional, multichannel bridges that deliver neurotrophin encoding lentivirus for regeneration following spinal cord injury. Biomaterials 2012, 33, 1618–1626. [Google Scholar] [CrossRef]
- Gnavi, S.; Barwig, C.; Freier, T.; Haastert-Talini, K.; Grothe, C.; Geuna, S. The Use of Chitosan-Based Scaffolds to Enhance Regeneration in the Nervous System. Int. Rev. Neurobiol. 2013, 109, 1–62. [Google Scholar] [CrossRef]
- Nomura, H.; Baladie, B.; Katayama, Y.; Morshead, C.M.; Shoichet, M.S.; Tator, C.H. Delayed implantation of intramedullary chitosan channels containing nerve grafts promotes extensive axonal regeneration after spinal cord injury. Neurosurgery 2008, 63, 127–143. [Google Scholar] [CrossRef] [PubMed]
- Guan, S.; Zhang, X.-L.; Lin, X.-M.; Liu, T.-Q.; Ma, X.-H.; Cui, Z.-F. Chitosan/gelatin porous scaffolds containing hyaluronic acid and heparan sulfate for neural tissue engineering. J. Biomater. Sci. Polym. Ed. 2013, 24, 999–1014. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Kim, G. Three-dimensional electrospun polycaprolactone (PCL)/alginate hybrid composite scaffolds. Carbohydr. Polym. 2014, 114, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhao, Y.; Yan, X.; Zhang, L.; Li, G.; Yang, Y. PAM/GO/gel/SA composite hydrogel conduit with bioactivity for repairing peripheral nerve injury. J. Biomed. Mater. Res. Part A 2019, 107, 1273–1283. [Google Scholar] [CrossRef]
- Yazdi, M.K.; Taghizadeh, A.; Taghizadeh, M.; Stadler, F.J.; Farokhi, M.; Mottaghitalab, F.; Zarrintaj, P.; Ramsey, J.D.; Seidi, F.; Saeb, M.R.; et al. Agarose-based biomaterials for advanced drug delivery. J. Control. Release 2020, 326, 523–543. [Google Scholar] [CrossRef]
- Zarrintaj, P.; Manouchehri, S.; Ahmadi, Z.; Saeb, M.R.; Urbanska, A.M.; Kaplan, D.L.; Mozafari, M. Agarose-based biomaterials for tissue engineering. Carbohydr. Polym. 2018, 187, 66–84. [Google Scholar] [CrossRef]
- Balgude, A.P.; Yu, X.; Szymanski, A.; Bellamkonda, R.V. Agarose gel stiffness determines rate of DRG neurite extension in 3D cultures. Biomaterials 2001, 22, 1077–1084. [Google Scholar] [CrossRef]
- Luo, Y.; Shoichet, M.S. A photolabile hydrogel for guided three-dimensional cell growth and migration. Nat. Mater. 2004, 3, 249–253. [Google Scholar] [CrossRef]
- Stokols, S.; Tuszynski, M.H. Freeze-dried agarose scaffolds with uniaxial channels stimulate and guide linear axonal growth following spinal cord injury. Biomaterials 2006, 27, 443–451. [Google Scholar] [CrossRef]
- Stokols, S.; Sakamoto, J.; Breckon, C.; Holt, T.; Weiss, J.; Tuszynski, M.H. Templated Agarose Scaffolds Support Linear Axonal Regeneration. Tissue Eng. 2006, 12, 2777–2787. [Google Scholar] [CrossRef]
- Gros, T.; Sakamoto, J.S.; Blesch, A.; Havton, L.A.; Tuszynski, M.H. Regeneration of long-tract axons through sites of spinal cord injury using templated agarose scaffolds. Biomaterials 2010, 31, 6719–6729. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Lu, P.; Bednark, B.; Lynam, D.; Conner, J.M.; Sakamoto, J.; Tuszynski, M.H. Templated agarose scaffolds for the support of motor axon regeneration into sites of complete spinal cord transection. Biomaterials 2013, 34, 1529–1536. [Google Scholar] [CrossRef] [PubMed]
- Lewitus, D.Y.; Smith, K.L.; Landers, J.; Neimark, A.V.; Kohn, J. Bioactive agarose carbon-nanotube composites are capable of manipulating brain-implant interface. J. Appl. Polym. Sci. 2014, 131, 40297. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, K.S.; Husen, A.; Sohrab, S.S.; Yassin, M.O. Recent Status of Nanomaterial Fabrication and Their Potential Applications in Neurological Disease Management. Nanoscale Res. Lett. 2018, 13, 231. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, J.W. Overcoming Inhibition in the Damaged Spinal Cord. J. Neurotrauma 2006, 23, 371–383. [Google Scholar] [CrossRef]
- Bracken, M.B.; Shepard, M.J.; Collins, W.F.; Holford, T.R.; Young, W.; Baskin, D.S.; Eisenberg, H.M.; Flamm, E.; Leo-Summers, L.; Maroon, J.; et al. A Randomized, Controlled Trial of Methylprednisolone or Naloxone in the Treatment of Acute Spinal-Cord Injury: Results of the Second National Acute Spinal Cord Injury Study. N. Engl. J. Med. 1990, 322, 1405–1411. [Google Scholar] [CrossRef]
- Gerndt, S.J.; Rodriguez, J.L.; Pawlik, J.W.; Taheri, P.A.; Wahl, W.L.; Micheals, A.J.; Papadopoulos, S.M. Consequences of High-Dose Steroid Therapy for Acute Spinal Cord Injury. J. Trauma Inj. Infect. Crit. Care 1997, 42, 279–284. [Google Scholar] [CrossRef]
- Song, F.; Li, X.; Wang, Q.; Liao, L.; Zhang, C. Nanocomposite Hydrogels and Their Applications in Drug Delivery and Tissue Engineering. J. Biomed. Nanotechnol. 2015, 11, 40–52. [Google Scholar] [CrossRef]
- Eftekhari, H.; Jahandideh, A.; Asghari, A.; Akbarzadeh, A.; Hesaraki, S. Assessment of polycaprolacton (PCL) nanocomposite scaffold compared with hydroxyapatite (HA) on healing of segmental femur bone defect in rabbits. Artif. Cells Nanomed. Biotechnol. 2017, 45, 961–968. [Google Scholar] [CrossRef]
- Huang, X.; Yin, Z.; Wu, S.; Qi, X.; He, Q.; Zhang, Q.; Yan, Q.; Boey, F.; Zhang, H. Graphene-Based Materials: Synthesis, Characterization, Properties, and Applications. Small 2011, 7, 1876–1902. [Google Scholar] [CrossRef]
- Wang, X.-X.; Wang, S.-X.; Lu, Y.-B.; Wang, Y.; Song, Y.-J.; Wang, X.; Nyamgerelt, M. Graphene and graphene-based materials in axonal repair of spinal cord injury. Neural Regen. Res. 2022, 17, 2117. [Google Scholar] [CrossRef] [PubMed]
- Geim, A.K. Graphene: Status and Prospects. Science 2009, 324, 1530–1534. [Google Scholar] [CrossRef] [PubMed]
- Dan, Y.; Lu, Y.; Kybert, N.J.; Luo, Z.; Johnson, A.T.C. Intrinsic Response of Graphene Vapor Sensors. Nano Lett. 2009, 9, 1472–1475. [Google Scholar] [CrossRef] [PubMed]
- Stoller, M.D.; Park, S.; Zhu, Y.; An, J.; Ruoff, R.S. Graphene-Based Ultracapacitors. Nano Lett. 2008, 8, 3498–3502. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.; Jiang, Z.; Li, N.; Liu, P.; Liu, L.; Tang, M.; Cheng, G. Anti-inflammatory effects of three-dimensional graphene foams cultured with microglial cells. Biomaterials 2014, 35, 6930–6940. [Google Scholar] [CrossRef]
- Ma, Q.; Yang, L.; Jiang, Z.; Song, Q.; Xiao, M.; Zhang, D.; Ma, X.; Wen, T.; Cheng, G. Three-Dimensional Stiff Graphene Scaffold on Neural Stem Cells Behavior. ACS Appl. Mater. Interfaces 2016, 8, 34227–34233. [Google Scholar] [CrossRef]
- Sintov, A.; Velasco-Aguirre, C.; Gallardo-Toledo, E.; Araya, E.; Kogan, M. Metal nanoparticles as targeted carriers circumventing the blood–Brain barrier. Int. Rev. Neurobiol. 2016, 130, 199–227. [Google Scholar]
- Waris, A.; Ali, A.; Khan, A.U.; Asim, M.; Zamel, D.; Fatima, K.; Raziq, A.; Khan, M.A.; Akbar, N.; Baset, A.; et al. Applications of Various Types of Nanomaterials for the Treatment of Neurological Disorders. Nanomaterials 2022, 12, 2140. [Google Scholar] [CrossRef]
- Fang, C.; Ma, Z.; Chen, L.; Li, H.; Jiang, C.; Zhang, W. Biosynthesis of gold nanoparticles, characterization and their loading with zonisamide as a novel drug delivery system for the treatment of acute spinal cord injury. J. Photochem. Photobiol. B Biol. 2019, 190, 72–75. [Google Scholar] [CrossRef]
- Wang, Y.-T.; Lu, X.-M.; Zhu, F.; Huang, P.; Yu, Y.; Zeng, L.; Long, Z.-Y.; Wu, Y.-M. The use of a gold nanoparticle-based adjuvant to improve the therapeutic efficacy of hNgR-Fc protein immunization in spinal cord-injured rats. Biomaterials 2011, 32, 7988–7998. [Google Scholar] [CrossRef]
- Paviolo, C.; Haycock, J.W.; Yong, J.; Yu, A.; Stoddart, P.R.; McArthur, S.L. Laser exposure of gold nanorods can increase neuronal cell outgrowth. Biotechnol. Bioeng. 2013, 110, 2277–2291. [Google Scholar] [CrossRef] [PubMed]
- Naderi, M.S.; Moghadam, T.T.; Khajeh, K.; Ranjbar, B. Improving the stability of chondroitinase ABC I via interaction with gold nanorods. Int. J. Biol. Macromol. 2018, 107, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Liu, Y.; Luo, W.; Liu, S.; Wang, Y.; Gu, R.; Liu, W.; Xiao, C. Minocycline-Loaded Poly(α-Lipoic Acid)–Methylprednisolone Prodrug Nanoparticles for the Combined Anti-Inflammatory Treatment of Spinal Cord Injury. Int. J. Nanomed. 2022, 17, 91–104. [Google Scholar] [CrossRef]
- Shi, H.; Jin, L.; Li, J.; Liang, K.; Li, X.; Ye, Z.; Zhu, X.; Oliveira, J.M.; Reis, R.L.; Mao, Z.; et al. Mesoporous polydopamine nanoparticles for sustained release of rapamycin and reactive oxygen species scavenging to synergistically accelerate neurogenesis after spinal cord injury. J. Mater. Chem. B 2022, 10, 6351–6359. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Trinh, T.H.; Yoo, M.; Shin, J.; Lee, H.; Kim, J.; Hwang, E.; Lim, Y.-B.; Ryou, C. Self-Assembling Peptides and Their Application in the Treatment of Diseases. Int. J. Mol. Sci. 2019, 20, 5850. [Google Scholar] [CrossRef] [PubMed]
- La Manna, S.; Di Natale, C.; Florio, D.; Marasco, D. Peptides as Therapeutic Agents for Inflammatory-Related Diseases. Int. J. Mol. Sci. 2018, 19, 2714. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Leung, G.K.K.; Su, H.; Yuan, Q.; Wang, L.; Chu, T.-H.; Zhang, W.; Pu, J.K.S.; Ng, G.K.P.; Wong, W.M.; et al. Self-assembling peptide nanofiber scaffold promotes the reconstruction of acutely injured brain. Nanomedicine 2009, 5, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.-Y.; Chen, M.-H.; Chang, W.-H.; Huang, M.-Y.; Wang, T.-W. Neural stem cells encapsulated in a functionalized self-assembling peptide hydrogel for brain tissue engineering. Biomaterials 2013, 34, 2005–2016. [Google Scholar] [CrossRef]
- Ando, K.; Imagama, S.; Ito, Z.; Kobayashi, K.; Hida, T.; Nakashima, H.; Ito, K.; Tsushima, M.; Ishikawa, Y.; Matsumoto, A.; et al. Self-assembling Peptide Reduces Glial Scarring, Attenuates Posttraumatic Inflammation, and Promotes Neurite Outgrowth of Spinal Motor Neurons. Spine 2016, 41, E1201–E1207. [Google Scholar] [CrossRef]
- Subramanian, A.; Krishnan, U.M.; Sethuraman, S. Development of biomaterial scaffold for nerve tissue engineering: Biomaterial mediated neural regeneration. J. Biomed. Sci. 2009, 16, 108. [Google Scholar] [CrossRef]
- Ratheesh, G.; Venugopal, J.R.; Chinappan, A.; Ezhilarasu, H.; Sadiq, A.; Ramakrishna, S. 3D Fabrication of Polymeric Scaffolds for Regenerative Therapy. ACS Biomater. Sci. Eng. 2017, 3, 1175–1194. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Slamovich, E.B.; Webster, T.J. Less harmful acidic degradation of poly(lactic-co-glycolic acid) bone tissue engineering scaffolds through titania nanoparticle addition. Int. J. Nanomed. 2006, 1, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Shalumon, K.T.; Anulekha, K.H.; Nair, S.V.; Nair, S.V.; Chennazhi, K.P.; Jayakumar, R. Sodium alginate/poly(vinyl alcohol)/nano ZnO composite nanofibers for antibacterial wound dressings. Int. J. Biol. Macromol. 2011, 49, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Gunatillake, P.A.; Adhikari, R. Biodegradable synthetic polymers for tissue engineering. Eur. Cells Mater. 2003, 5, 1–16, discussion 16. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Wang, H.; Ma, K.; Wang, S.; Yang, C.; Mu, N.; Yang, F.; Feng, H.; Chen, T. Novel cytokine-loaded PCL-PEG scaffold composites for spinal cord injury repair. RSC Adv. 2020, 10, 6306–6314. [Google Scholar] [CrossRef]
- Luo, J.; Shi, R. Diffusive oxidative stress following acute spinal cord injury in guinea pigs and its inhibition by polyethylene glycol. Neurosci. Lett. 2004, 359, 167–170. [Google Scholar] [CrossRef]
- Shi, R. Polyethylene glycol repairs membrane damage and enhances functional recovery: A tissue engineering approach to spinal cord injury. Neurosci. Bull. 2013, 29, 460–466. [Google Scholar] [CrossRef]
- Wang, A.; Huo, X.; Zhang, G.; Wang, X.; Zhang, C.; Wu, C.; Rong, W.; Xu, J.; Song, T. Effect of DSPE-PEG on compound action potential, injury potential and ion concentration following compression in ex vivo spinal cord. Neurosci. Lett. 2016, 620, 50–56. [Google Scholar] [CrossRef]
- Raynald; Shu, B.; Liu, X.; Zhou, J.; Huang, H.; Wang, J.; Sun, X.; Qin, C.; An, Y. Polypyrrole/polylactic acid nanofibrous scaffold cotransplanted with bone marrow stromal cells promotes the functional recovery of spinal cord injury in rats. CNS Neurosci. Ther. 2019, 25, 951–964. [Google Scholar] [CrossRef]
- Liu, Z.-H.; Huang, Y.-C.; Kuo, C.-Y.; Kuo, C.-Y.; Chin, C.-Y.; Yip, P.K.; Chen, J.-P. Docosahexaenoic Acid-Loaded Polylactic Acid Core-Shell Nanofiber Membranes for Regenerative Medicine after Spinal Cord Injury: In Vitro and In Vivo Study. Int. J. Mol. Sci. 2020, 21, 7031. [Google Scholar] [CrossRef]
- Hurtado, A.; Cregg, J.; Wang, H.B.; Wendell, D.F.; Oudega, M.; Gilbert, R.J.; McDonald, J.W. Robust CNS regeneration after complete spinal cord transection using aligned poly-l-lactic acid microfibers. Biomaterials 2011, 32, 6068–6079. [Google Scholar] [CrossRef] [PubMed]
- Gwak, S.-J.; Yun, Y.; Yoon, D.H.; Kim, K.N.; Ha, Y. Therapeutic Use of 3β-[N-(N′,N′-Dimethylaminoethane) Carbamoyl] Cholesterol-Modified PLGA Nanospheres as Gene Delivery Vehicles for Spinal Cord Injury. PLoS ONE 2016, 11, e0147389. [Google Scholar] [CrossRef] [PubMed]
- Ganz, J.; Shor, E.; Guo, S.; Sheinin, A.; Arie, I.; Michaelevski, I.; Pitaru, S.; Offen, D.; Levenberg, S. Implantation of 3D Constructs Embedded with Oral Mucosa-Derived Cells Induces Functional Recovery in Rats with Complete Spinal Cord Transection. Front. Neurosci. 2017, 11, 589. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Redenski, I.; Landau, S.; Szklanny, A.; Merdler, U.; Levenberg, S. Prevascularized Scaffolds Bearing Human Dental Pulp Stem Cells for Treating Complete Spinal Cord Injury. Adv. Health Mater. 2020, 9, e2000974. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.; Yu, S.; Wu, Y.; Ju, R.; Wang, H.; Liu, Y.; Wang, Y.; Xu, Q. Spinal cord injury repair by implantation of structured hyaluronic acid scaffold with PLGA microspheres in the rat. Cell Tissue Res. 2016, 364, 17–28. [Google Scholar] [CrossRef]
- Babaloo, H.; Ebrahimi-Barough, S.; Derakhshan, M.A.; Yazdankhah, M.; Lotfibakhshaiesh, N.; Soleimani, M.; Joghataei, M.; Ai, J. PCL/gelatin nanofibrous scaffolds with human endometrial stem cells/Schwann cells facilitate axon regeneration in spinal cord injury. J. Cell. Physiol. 2019, 234, 11060–11069. [Google Scholar] [CrossRef]
- Novikova, L.N.; Kolar, M.K.; Kingham, P.J.; Ullrich, A.; Oberhoffner, S.; Renardy, M.; Doser, M.; Müller, E.; Wiberg, M.; Novikov, L.N. Trimethylene carbonate-caprolactone conduit with poly-p-dioxanone microfilaments to promote regeneration after spinal cord injury. Acta Biomater. 2018, 66, 177–191. [Google Scholar] [CrossRef]
- Shahriari, D.; Koffler, J.Y.; Tuszynski, M.H.; Campana, W.M.; Sakamoto, J.S. Hierarchically Ordered Porous and High-Volume Polycaprolactone Microchannel Scaffolds Enhanced Axon Growth in Transected Spinal Cords. Tissue Eng. Part A 2017, 23, 415–425. [Google Scholar] [CrossRef]
- Comolli, N.; Donaldson, O.; Grantier, N.; Zhukareva, V.; Tom, V.J. Polyvinyl alcohol-polyvinyl pyrrolidone thin films provide local short-term release of anti-inflammatory agents post spinal cord injury. J. Biomed. Mater. Res. Part B Appl. Biomater. 2012, 100, 1867–1873. [Google Scholar] [CrossRef]
- Chen, L.; Wang, W.; Lin, Z.; Lu, Y.; Chen, H.; Li, B.; Li, Z.; Xia, H.; Li, L.; Zhang, T. Conducting molybdenum sulfide/graphene oxide/polyvinyl alcohol nanocomposite hydrogel for repairing spinal cord injury. J. Nanobiotechnol. 2022, 20, 210. [Google Scholar] [CrossRef]
- Zhao, T.; Jing, Y.; Zhou, X.; Wang, J.; Huang, X.; Gao, L.; Zhu, Y.; Wang, L.; Gou, Z.; Liang, C.; et al. PHBV/PLA/Col-Based Nanofibrous Scaffolds Promote Recovery of Locomotor Function by Decreasing Reactive Astrogliosis in a Hemisection Spinal Cord Injury Rat Model. J. Biomed. Nanotechnol. 2018, 14, 1921–1933. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Xu, K.; Wu, Q.; Wang, C.; Xiao, S.; Li, H.; He, T.; Wang, L.; Li, F.; Chen, Q. Duraplasty of PHBV/PLA/Col membranes promotes axonal regeneration by inhibiting NLRP3 complex and M1 macrophage polarization in rats with spinal cord injury. FASEB J. 2020, 34, 12147–12162. [Google Scholar] [CrossRef] [PubMed]
- Kong, G.; Liu, J.; Li, R.; Lin, J.; Huang, Z.; Yang, Z.; Wu, X.; Huang, Z.; Zhu, Q.; Wu, X. Ketone Metabolite β-Hydroxybutyrate Ameliorates Inflammation After Spinal Cord Injury by Inhibiting the NLRP3 Inflammasome. Neurochem. Res. 2021, 46, 213–229. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, X.-J.; Li, W.-S.; Xu, X.-L.; Hu, J.-B.; Kang, X.-Q.; Qi, J.; Ying, X.-Y.; You, J.; Du, Y.-Z. Polycaprolactone/polysialic acid hybrid, multifunctional nanofiber scaffolds for treatment of spinal cord injury. Acta Biomater. 2018, 77, 15–27. [Google Scholar] [CrossRef]
- Mehanna, A.; Jakovcevski, I.; Acar, A.; Xiao, M.; Loers, G.; Rougon, G.; Irintchev, A.; Schachner, M. Polysialic Acid Glycomimetic Promotes Functional Recovery and Plasticity After Spinal Cord Injury in Mice. Mol. Ther. 2010, 18, 34–43. [Google Scholar] [CrossRef]
- Kalotra, S.; Saini, V.; Singh, H.; Sharma, A.; Kaur, G. 5-Nonyloxytryptamine oxalate–embedded collagen–laminin scaffolds augment functional recovery after spinal cord injury in mice. Ann. New York Acad. Sci. 2020, 1465, 99–116. [Google Scholar] [CrossRef]
- Tsai, E.; Dalton, P.D.; Shoichet, M.S.; Tator, C.H. Matrix inclusion within synthetic hydrogel guidance channels improves specific supraspinal and local axonal regeneration after complete spinal cord transection. Biomaterials 2006, 27, 519–533. [Google Scholar] [CrossRef]
- Kubinová, Š.; Horák, D.; Hejčl, A.; Plichta, Z.; Kotek, J.; Proks, V.; Forostyak, S.; Syková, E. SIKVAV-modified highly superporous PHEMA scaffolds with oriented pores for spinal cord injury repair. J. Tissue Eng. Regen. Med. 2013, 9, 1298–1309. [Google Scholar] [CrossRef]
- Tsai, E.; Dalton, P.D.; Shoichet, M.S.; Tator, C.H. Synthetic Hydrogel Guidance Channels Facilitate Regeneration of Adult Rat Brainstem Motor Axons after Complete Spinal Cord Transection. J. Neurotrauma 2004, 21, 789–804. [Google Scholar] [CrossRef]
- D’Souza, A.A.; Shegokar, R. Polyethylene glycol (PEG): A versatile polymer for pharmaceutical applications. Expert Opin. Drug Deliv. 2016, 13, 1257–1275. [Google Scholar] [CrossRef]
- Pape, A.C.H.; Ippel, B.D.; Dankers, P.Y.W. Cell and Protein Fouling Properties of Polymeric Mixtures Containing Supramolecular Poly(ethylene glycol) Additives. Langmuir 2017, 33, 4076–4082. [Google Scholar] [CrossRef] [PubMed]
- Knop, K.; Hoogenboom, R.; Fischer, D.; Schubert, U.S. Poly(ethylene glycol) in Drug Delivery: Pros and Cons as Well as Potential Alternatives. Angew. Chem. Int. Ed. 2010, 49, 6288–6308. [Google Scholar] [CrossRef] [PubMed]
- Padín-González, E.; Lancaster, P.; Bottini, M.; Gasco, P.; Tran, L.; Fadeel, B.; Wilkins, T.; Monopoli, M.P. Understanding the Role and Impact of Poly (Ethylene Glycol) (PEG) on Nanoparticle Formulation: Implications for COVID-19 Vaccines. Front. Bioeng. Biotechnol. 2022, 10, 882363. [Google Scholar] [CrossRef] [PubMed]
- Tyler, J.Y.; Xu, X.-M.; Cheng, J.-X. Nanomedicine for treating spinal cord injury. Nanoscale 2013, 5, 8821–8836. [Google Scholar] [CrossRef]
- Carballo-Molina, O.A.; Velasco, I. Hydrogels as scaffolds and delivery systems to enhance axonal regeneration after injuries. Front. Cell. Neurosci. 2015, 9, 13. [Google Scholar] [CrossRef]
- Peppas, N.A.; Bures, P.; Leobandung, W.; Ichikawa, H. Hydrogels in pharmaceutical formulations. Eur. J. Pharm. Biopharm. 2000, 50, 27–46. [Google Scholar] [CrossRef]
- Rizzi, S.C.; Ehrbar, M.; Halstenberg, S.; Raeber, G.P.; Schmoekel, H.G.; Hagenmüller, H.; Müller, R.; Weber, F.E.; Hubbell, J.A. Recombinant Protein-co-PEG Networks as Cell-Adhesive and Proteolytically Degradable Hydrogel Matrixes. Part II: Biofunctional Characteristics. Biomacromolecules 2006, 7, 3019–3029. [Google Scholar] [CrossRef]
- Benoit, D.; Schwartz, M.; Durney, A.R.; Anseth, K.S. Small functional groups for controlled differentiation of hydrogel-encapsulated human mesenchymal stem cells. Nat. Mater. 2008, 7, 816–823. [Google Scholar] [CrossRef]
- Luo, J.; Borgens, R.; Shi, R. Polyethylene glycol immediately repairs neuronal membranes and inhibits free radical production after acute spinal cord injury. J. Neurochem. 2002, 83, 471–480. [Google Scholar] [CrossRef]
- Lopes, M.S.; Jardini, A.; Filho, R.M. Poly (Lactic Acid) Production for Tissue Engineering Applications. Procedia Eng. 2012, 42, 1402–1413. [Google Scholar] [CrossRef]
- Gupta, B.; Revagade, N.; Hilborn, J. Poly(lactic acid) fiber: An overview. Prog. Polym. Sci. 2007, 32, 455–482. [Google Scholar] [CrossRef]
- Gautier, S.E.; Oudega, M.; Fragoso, M.; Chapon, P.; Plant, G.W.; Bunge, M.B.; Parel, J.M. Poly(alpha-hydroxyacids) for application in the spinal cord: Resorbability and biocompatibility with adult rat Schwann cells and spinal cord. J. Biomed. Mater. Res. 1998, 42, 642–654. [Google Scholar] [CrossRef]
- Lasprilla, A.J.R.; Martinez, G.A.R.; Lunelli, B.H.; Jardini, A.L.; Filho, R.M. Poly-lactic acid synthesis for application in biomedical devices—A review. Biotechnol. Adv. 2012, 30, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Rasal, R.M.; Janorkar, A.V.; Hirt, D.E. Poly(lactic acid) modifications. Prog. Polym. Sci. 2010, 35, 338–356. [Google Scholar] [CrossRef]
- Burg, K.J.L.; Holder, W.D.; Culberson, C.R.; Beiler, R.J.; Greene, K.G.; Loebsack, A.B.; Roland, W.D.; Mooney, D.J.; Halberstadt, C.R. Parameters affecting cellular adhesion to polylactide films. J. Biomater. Sci. Polym. Ed. 1999, 10, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Rasal, R.M.; Hirt, D.E. Toughness decrease of PLA-PHBHHx blend films upon surface-confined photopolymerization. J. Biomed. Mater. Res. Part A 2009, 88, 1079–1086. [Google Scholar] [CrossRef] [PubMed]
- Danhier, F.; Ansorena, E.; Silva, J.M.; Coco, R.; Le Breton, A.; Préat, V. PLGA-based nanoparticles: An overview of biomedical applications. J. Control. Release 2012, 161, 505–522. [Google Scholar] [CrossRef]
- Rocha, C.V.; Gonçalves, V.; da Silva, M.C.; Bañobre-López, M.; Gallo, J. PLGA-Based Composites for Various Biomedical Applications. Int. J. Mol. Sci. 2022, 23, 2034. [Google Scholar] [CrossRef]
- Mirakabad, F.S.T.; Nejati-Koshki, K.; Akbarzadeh, A.; Yamchi, M.R.; Milani, M.; Zarghami, N.; Zeighamian, V.; Rahimzadeh, A.; Alimohammadi, S.; Hanifehpour, Y.; et al. PLGA-Based Nanoparticles as Cancer Drug Delivery Systems. Asian Pac. J. Cancer Prev. 2014, 15, 517–535. [Google Scholar] [CrossRef]
- Makadia, H.K.; Siegel, S.J. Poly lactic-co-glycolic acid (PLGA) As biodegradable controlled drug delivery carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef]
- Han, F.Y.; Thurecht, K.J.; Whittaker, A.K.; Smith, M.T. Bioerodable PLGA-Based Microparticles for Producing Sustained-Release Drug Formulations and Strategies for Improving Drug Loading. Front. Pharmacol. 2016, 7, 185. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Zhu, Q. Recent advances of PLGA micro/nanoparticles for the delivery of biomacromolecular therapeutics. Mater. Sci. Eng. C 2018, 92, 1041–1060. [Google Scholar] [CrossRef] [PubMed]
- Krych, A.J.; Rooney, G.E.; Chen, B.; Schermerhorn, T.C.; Ameenuddin, S.; Gross, L.; Moore, M.J.; Currier, B.L.; Spinner, R.J.; Friedman, J.A.; et al. Relationship between scaffold channel diameter and number of regenerating axons in the transected rat spinal cord. Acta Biomater. 2009, 5, 2551–2559. [Google Scholar] [CrossRef] [PubMed]
- Mohtaram, N.K.; Ko, J.; King, C.; Sun, L.; Muller, N.; Jun, M.B.-G.; Willerth, S.M. Electrospun biomaterial scaffolds with varied topographies for neuronal differentiation of human-induced pluripotent stem cells. J. Biomed. Mater. Res. Part A 2014, 103, 2591–2601. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Zhang, Y.; Zeng, C.; Ngiam, M.; Liao, S.; Quan, D.; Zeng, Y.; Lu, J.; Ramakrishna, S. Manufacture of PLGA Multiple-Channel Conduits with Precise Hierarchical Pore Architectures and In Vitro/Vivo Evaluation for Spinal Cord Injury. Tissue Eng. Part C Methods 2009, 15, 243–255. [Google Scholar] [CrossRef]
- Sonomoto, K.; Yamaoka, K.; Kaneko, H.; Yamagata, K.; Sakata, K.; Zhang, X.; Kondo, M.; Zenke, Y.; Sabanai, K.; Nakayamada, S.; et al. Spontaneous Differentiation of Human Mesenchymal Stem Cells on Poly-Lactic-Co-Glycolic Acid Nano-Fiber Scaffold. PLoS ONE 2016, 11, e0153231. [Google Scholar] [CrossRef]
- Kim, B.G.; Kang, Y.M.; Phi, J.H.; Kim, Y.-H.; Hwang, D.H.; Choi, J.Y.; Ryu, S.; Elastal, A.-E.; Paek, S.H.; Wang, K.-C.; et al. Implantation of polymer scaffolds seeded with neural stem cells in a canine spinal cord injury model. Cytotherapy 2010, 12, 841–845. [Google Scholar] [CrossRef]
- Liu, C.; Huang, Y.; Pang, M.; Yang, Y.; Linshan, L.; Liu, L.; Shu, T.; Zhou, W.; Wang, X.; Rong, L.; et al. Tissue-Engineered Regeneration of Completely Transected Spinal Cord Using Induced Neural Stem Cells and Gelatin-Electrospun Poly (Lactide-Co-Glycolide)/Polyethylene Glycol Scaffolds. PLoS ONE 2015, 10, e0117709. [Google Scholar] [CrossRef]
- Sawadkar, P.; Mohanakrishnan, J.; Rajasekar, P.; Rahmani, B.; Kohli, N.; Bozec, L.; Garcia-Gareta, E. A Synergistic Relationship between Polycaprolactone and Natural Polymers Enhances the Physical Properties and Biological Activity of Scaffolds. ACS Appl. Mater. Interfaces 2020, 12, 13587–13597. [Google Scholar] [CrossRef]
- Lim, W.; Chowdhury, S.; Ng, M.; Law, J. Physicochemical Properties and Biocompatibility of Electrospun Polycaprolactone/Gelatin Nanofibers. Int. J. Environ. Res. Public Health 2021, 18, 4764. [Google Scholar] [CrossRef]
- Patel, B.B.; Sharifi, F.; Stroud, D.P.; Montazami, R.; Hashemi, N.N.; Sakaguchi, D.S. 3D Microfibrous Scaffolds Selectively Promotes Proliferation and Glial Differentiation of Adult Neural Stem Cells: A Platform to Tune Cellular Behavior in Neural Tissue Engineering. Macromol. Biosci. 2019, 19, e1800236. [Google Scholar] [CrossRef] [PubMed]
- Gelain, F.; Panseri, S.; Antonini, S.; Cunha, C.; Donega, M.; Lowery, J.; Taraballi, F.; Cerri, G.; Montagna, M.; Baldissera, F.; et al. Transplantation of Nanostructured Composite Scaffolds Results in the Regeneration of Chronically Injured Spinal Cords. ACS Nano 2011, 5, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Hiraizumi, Y.; Transfeldt, E.E.; Fujimaki, E.; Nambu, M. Application of Polyvinyl Alcohol Hydrogel Membrane as Anti-adhesive Interposition After Spinal Surgery. Spine 1995, 20, 2272–2277. [Google Scholar] [CrossRef] [PubMed]
- Lebugle, A.; Rodrigues, A.; Bonnevialle, P.; Voigt, J.; Canal, P.; Rodriguez, F. Study of implantable calcium phosphate systems for the slow release of methotrexate. Biomaterials 2002, 23, 3517–3522. [Google Scholar] [CrossRef]
- Novikova, L.N.; Pettersson, J.; Brohlin, M.; Wiberg, M.; Novikov, L.N. Biodegradable poly-β-hydroxybutyrate scaffold seeded with Schwann cells to promote spinal cord repair. Biomaterials 2008, 29, 1198–1206. [Google Scholar] [CrossRef]
- Doncel-Pérez, E.; Ellis, G.; Sandt, C.; Shuttleworth, P.S.; Bastida, A.; Revuelta, J.; García-Junceda, E.; Fernández-Mayoralas, A.; Garrido, L. Biochemical profiling of rat embryonic stem cells grown on electrospun polyester fibers using synchrotron infrared microspectroscopy. Anal. Bioanal. Chem. 2018, 410, 3649–3660. [Google Scholar] [CrossRef]
- Agrawal, L.; Vimal, S.K.; Barzaghi, P.; Shiga, T.; Terenzio, M. Biodegradable and Electrically Conductive Melanin-Poly (3-Hydroxybutyrate) 3D Fibrous Scaffolds for Neural Tissue Engineering Applications. Macromol. Biosci. 2022, 22, e2200315. [Google Scholar] [CrossRef]
- Wu, J.; Zhan, X.; Liu, L.; Xia, X. Bioproduction, purification, and application of polysialic acid. Appl. Microbiol. Biotechnol. 2018, 102, 9403–9409. [Google Scholar] [CrossRef]
- Mindler, K.; Ostertag, E.; Stehle, T. The polyfunctional polysialic acid: A structural view. Carbohydr. Res. 2021, 507, 108376. [Google Scholar] [CrossRef]
- Pearse, D.D.; Rao, S.N.; Morales, A.A.; Wakarchuk, W.; Rutishauser, U.; El-Maarouf, A.; Ghosh, M. Engineering polysialic acid on Schwann cells using polysialyltransferase gene transfer or purified enzyme exposure for spinal cord injury transplantation. Neurosci. Lett. 2021, 748, 135690. [Google Scholar] [CrossRef]
- Wang, X.-J.; Peng, C.-H.; Zhang, S.; Xu, X.-L.; Shu, G.-F.; Qi, J.; Zhu, Y.-F.; Xu, D.-M.; Kang, X.-Q.; Lu, K.-J.; et al. Polysialic-Acid-Based Micelles Promote Neural Regeneration in Spinal Cord Injury Therapy. Nano Lett. 2019, 19, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Marino, P.; Norreel, J.-C.; Schachner, M.; Rougon, G.; Amoureux, M.-C. A polysialic acid mimetic peptide promotes functional recovery in a mouse model of spinal cord injury. Exp. Neurol. 2009, 219, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Giannetti, S.; Lauretti, L.; Fernandez, E.; Salvinelli, F.; Tamburrini, G.; Pallini, R. Acrylic hydrogel implants after spinal cord lesion in the adult rat. Neurol. Res. 2001, 23, 405–409. [Google Scholar] [CrossRef]
- Bakshi, A.; Fisher, O.; Dagci, T.; Himes, B.T.; Fischer, I.; Lowman, A. Mechanically engineered hydrogel scaffolds for axonal growth and angiogenesis after transplantation in spinal cord injury. J. Neurosurg. Spine 2004, 1, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Hejčl, A.; Lesný, P.; Přádný, M.; Šedý, J.; Zámečník, J.; Jendelová, P.; Michálek, J.; Syková, E. Macroporous hydrogels based on 2-hydroxyethyl methacrylate. Part 6: 3D hydrogels with positive and negative surface charges and polyelectrolyte complexes in spinal cord injury repair. J. Mater. Sci. Mater. Med. 2009, 20, 1571–1577. [Google Scholar] [CrossRef] [PubMed]
- Kubinová, Š.; Horák, D.; Vaněček, V.; Plichta, Z.; Proks, V.; Syková, E. The use of new surface-modified poly(2-hydroxyethyl methacrylate) hydrogels in tissue engineering: Treatment of the surface with fibronectin subunits versus Ac-CGGASIKVAVS-OH, cysteine, and 2-mercaptoethanol modification. J. Biomed. Mater. Res. Part A 2013, 102, 2315–2323. [Google Scholar] [CrossRef] [PubMed]
- Carone, T.W.; Hasenwinkel, J.M. Mechanical and morphological characterization of homogeneous and bilayered poly(2-hydroxyethyl methacrylate) scaffolds for use in CNS nerve regeneration. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 78, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Valdes-Sánchez, T.; Rodriguez-Jimenez, F.J.; García-Cruz, D.M.; Escobar-Ivirico, J.L.; Alastrue-Agudo, A.; Erceg, S.; Monleón, M.; Moreno-Manzano, V. Methacrylate-endcapped caprolactone and FM19G11 provide a proper niche for spinal cord-derived neural cells. J. Tissue Eng. Regen. Med. 2013, 9, 734–739. [Google Scholar] [CrossRef]
- Hejčl, A.; Růžička, J.; Proks, V.; Macková, H.; Kubinová, Š.; Tukmachev, D.; Cihlář, J.; Horák, D.; Jendelová, P. Dynamics of tissue ingrowth in SIKVAV-modified highly superporous PHEMA scaffolds with oriented pores after bridging a spinal cord transection. J. Mater. Sci. Mater. Med. 2018, 29, 89. [Google Scholar] [CrossRef]
- Geetha, M.; Singh, A.K.; Asokamani, R.; Gogia, A.K. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog. Mater. Sci. 2009, 54, 397–425. [Google Scholar] [CrossRef]
- Chen, Q.; Thouas, G.A. Metallic implant biomaterials. Mater. Sci. Eng. R Rep. 2015, 87, 1–57. [Google Scholar] [CrossRef]
- Spataru, M.-C.; Cojocaru, F.D.; Sandu, A.V.; Solcan, C.; Duceac, I.A.; Baltatu, M.S.; Voiculescu, I.; Geanta, V.; Vizureanu, P. Assessment of the Effects of Si Addition to a New TiMoZrTa System. Materials 2021, 14, 7610. [Google Scholar] [CrossRef] [PubMed]
- Che Lah, N.A.; Hussin, M.H. Titanium and Titanium Based Alloys as Metallic Biomaterials in Medical Applications-Spine Implant Case Study. Pertanika J. Sci. Technol. 2019, 27, 459–472. [Google Scholar]
- Liu, X.; Hao, M.; Chen, Z.; Zhang, T.; Huang, J.; Dai, J.; Zhang, Z. 3D bioprinted neural tissue constructs for spinal cord injury repair. Biomaterials 2021, 272, 120771. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Kong, X.; Li, Q.; Li, C.; Yu, H.; Ning, G.; Xiang, Z.; Liu, Y.; Feng, S. The spatial arrangement of cells in a 3D-printed biomimetic spinal cord promotes directional differentiation and repairs the motor function after spinal cord injury. Biofabrication 2021, 13, 045016. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.-Y.; Chen, C.; Xu, H.-H.; Zhang, Y.-S.; Zhong, L.; Hu, N.; Jia, X.-L.; Wang, Y.-W.; Zhong, K.-H.; Liu, C.; et al. Integrated printed BDNF/collagen/chitosan scaffolds with low temperature extrusion 3D printer accelerated neural regeneration after spinal cord injury. Regen. Biomater. 2021, 8, rbab047. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-H.; Zhu, X.; Liu, X.-Y.; Xu, H.-H.; Jiang, W.; Wang, J.-J.; Chen, F.; Zhang, S.; Li, R.-X.; Chen, X.-Y.; et al. The corticospinal tract structure of collagen/silk fibroin scaffold implants using 3D printing promotes functional recovery after complete spinal cord transection in rats. J. Mater. Sci. Mater. Med. 2021, 32, 31. [Google Scholar] [CrossRef]
- Joung, D.; Truong, V.; Neitzke, C.C.; Guo, S.-Z.; Walsh, P.J.; Monat, J.R.; Meng, F.; Park, S.H.; Dutton, J.R.; Parr, A.M.; et al. 3D Printed Stem-Cell Derived Neural Progenitors Generate Spinal Cord Scaffolds. Adv. Funct. Mater. 2018, 28. [Google Scholar] [CrossRef]
- Koffler, J.; Zhu, W.; Qu, X.; Platoshyn, O.; Dulin, J.N.; Brock, J.; Graham, L.; Lu, P.; Sakamoto, J.; Marsala, M.; et al. Biomimetic 3D-printed scaffolds for spinal cord injury repair. Nat. Med. 2019, 25, 263–269. [Google Scholar] [CrossRef]
- Amr, S.M.; Gouda, A.; Koptan, W.T.; Galal, A.A.; Abdel-Fattah, D.S.; Rashed, L.A.; Atta, H.M.; Abdel-Aziz, M.T. Bridging defects in chronic spinal cord injury using peripheral nerve grafts combined with a chitosan-laminin scaffold and enhancing regeneration through them by co-transplantation with bone-marrow-derived mesenchymal stem cells: Case series of 14 patients. J. Spinal Cord Med. 2014, 37, 54–71. [Google Scholar] [CrossRef]
- Xiao, Z.; Tang, F.; Tang, J.; Yang, H.; Zhao, Y.; Chen, B.; Han, S.; Wang, N.; Li, X.; Cheng, S.; et al. One-year clinical study of NeuroRegen scaffold implantation following scar resection in complete chronic spinal cord injury patients. Sci. China Life Sci. 2016, 59, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Tang, F.; Zhao, Y.; Han, G.; Yin, N.; Li, X.; Chen, B.; Han, S.; Jiang, X.; Yun, C.; et al. Significant Improvement of Acute Complete Spinal Cord Injury Patients Diagnosed by a Combined Criteria Implanted with NeuroRegen Scaffolds and Mesenchymal Stem Cells. Cell Transplant. 2018, 27, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zhang, Y.; Yang, S.; Sun, J.; Qiu, H.; Hu, X.; Niu, X.; Xiao, Z.; Zhao, Y.; Zhou, Y.; et al. NeuroRegen Scaffolds Combined with Autologous Bone Marrow Mononuclear Cells for the Repair of Acute Complete Spinal Cord Injury: A 3-Year Clinical Study. Cell Transplant. 2020, 29, 963689720950637. [Google Scholar] [CrossRef] [PubMed]
- Theodore, N.; Hlubek, R.; Danielson, J.; Neff, K.; Vaickus, L.; Ulich, T.R.; Ropper, A.E. First Human Implantation of a Bioresorbable Polymer Scaffold for Acute Traumatic Spinal Cord Injury: A Clinical Pilot Study for Safety and Feasibility. Neurosurgery 2016, 79, E305–E312. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.-Y.; Zhang, S.; Deng, W.-S.; Ma, K.; Liang, B.; Liu, X.-Y.; Xu, H.-Y.; Zhang, J.; Shi, H.-Y.; Sun, H.-T. Collagen scaffold combined with human umbilical cord-mesenchymal stem cells transplantation for acute complete spinal cord injury. Neural Regen. Res. 2020, 15, 1686–1700. [Google Scholar] [CrossRef]

| Natural Biomaterials | Implanted Substance | Animals and SCI Model | Effect | Ref. |
|---|---|---|---|---|
| Hyaluronic Acid | Human embryonic stem cell-derived neural stem cells | Wister rats with spinal cord injury | Increasing cell differentiation and improving motor function | [35] |
| Hyaluronic Acid | Nogo-66 receptor antibody and poly-L-lysine | Wister rats with spinal cord hemisection | Promoting vascular regeneration, and inhibiting the formation of glial scar | [36] |
| Collagen | Linear ordered collagen scaffolds loaded with collagen-binding neurotrophin-3 | Wister rats with spinal cord transection | Promoting axonal regeneration and restoring some motor function | [37] |
| Collagen | Neurotrophin-3 | Dawley rats with spinal cord hemisection | Inhibiting inflammation and scar; promoting neuronal regeneration | [38] |
| Collagen | Implanted vascular endothelial growth factor | Sprague–Dawley (SD) rats with spinal cord transection | Improving the microenvironment and promoting angiogenesis | [39] |
| Collagen | N-cadherin | SD rats with spinal cord transection | Promoting the regeneration of neurons and improving motor function | [40] |
| Collagen | Human placenta-derived mesenchymal stem cells | Beagle dog with spinal cord transection | Improving the regeneration of neurons and exercise capacity | [41] |
| Collagen | Freeze-dried alginate sponge cross-linked with covalent bonds | Rats with spinal cord transection | Enhancing nerve regeneration of spinal cord | [42] |
| Gelatin | iNSCs | C57BL/6N mice with spinal cord transection | Promoting the proliferation of neural stem cells and significantly promoting functional recovery | [43] |
| Gelatin | BMSC and NSC | SD rats with spinal cord hemisection | Significantly promoting motor function recovery and neuronal differentiation | [44] |
| Gelatin | NSC | SD rats with spinal cord transection | Significantly improving hindlimb movement and nerve regeneration | [45] |
| Fibrin | – | Pot-bellied pigs with spinal cord dorsal column removed | Promoting tissue repair in areas near the injury and restoration of conduction function in the posterior column of the spinal cord | [46] |
| Fibrin | – | SD rats with spinal cord hemisection | Promoting directed host cell invasion, vasculature remodeling and axonal regeneration | [47] |
| Fibrin | Human endometrial stem cells (hEnSCs) | Wister rats with spinal cord aneurysm clip | Significantly promoting the recovery of motor function in injured rats | [48] |
| Decellularized scaffold | iPN and SC | Fischer rats with Moderate thoracic contusion injury | Promoting Schwann cell survival and neurite outgrowth in grafts | [49] |
| Decellularized scaffold | bpV (pic) | SD rats with spinal cord hemisection | Promoting NSC activity and axon outgrowth | [50] |
| Decellularized scaffold | ADSC | SD rats with spinal cord hemisecion | Enhancing the ability of axonal regeneration and promoting functional recovery | [51] |
| Chitosan | – | Wister rats with spinal cord hemisection | Reducing glial scar; improving the inflammatory response | [52] |
| Chitosan | Neurotrophin-3 and human umbilical cord mesenchymal stem cells | C57BL/6 Mice with spinal cord transection | Promoting the recovery of neurological function and reducing inflammation | [53] |
| Alginate | Neural stem cells | SD rats with spinal cord Aneurysmal clip | Reducing inflammation and lesion size | [54] |
| Alginate | Peptides and astroglia | GFP-transgenic F344 rats with spinal cord hemisection | Promoting cell migration and slight axon growth | [55] |
| Agarose | BDNF | F344 rats with spinal cord transection | Promoting nerve regeneration and axon growth | [56] |
| Agarose | Matrigel | Sprague–Dawley rats with spinal cord dorsal column removed | Improving motor function and promoting cell proliferation | [57] |
| Agarose | Gelatin and polypyrrole | Rats with spinal cord hemisection | Inhibiting the formation of astrocytes and activating endogenous nerve regeneration of spinal cord | [58] |
| Nanomaterial | MP | SD rats with spinal cord hemisection | Reducing lesion volume and improving drug transport efficiency | [59] |
| Nanomaterial | MP | Wister rats with spinal cord hemisection | Reducing the secondary reaction after SCI | [60] |
| Nanomaterial | Poly(lactide-coglycolide) | C57/BL6 mice with spinal cord hemisection | Enhancing the expression of anti-inflammatory and regeneration genes and increasing axon regeneration | [61] |
| Nanomaterial | Chitosan and polyethylene glycol | BALB/c mice with compression injury of spinal cord | Promoting cell growth and reducing inflammatory response | [62] |
| Self-loading peptide | Neural precursor cells | Wister rats with spinal cord aneurysm clip | Enhancing nerve repair and regeneration | [63] |
| Self-loading peptide | – | Sprague–Dawley rats with thoracic spinal cord tissues | Promoting the proliferation and migration of neural stem cells | [64] |
| Self-loading peptide | – | SD rats with injury spinal cord | Reducing inflammation and glial scar formation, and increaseing axonal growth | [65] |
| Synthetic Biomaterials | Implantted Substance | Animals and SCI Model | Effect | Ref. |
|---|---|---|---|---|
| PEG | FGF2, EGF, GDNF | SD Rats with spinal cord transection | Improving motor function and increasing axonal regeneration | [146] |
| PEG | – | Guinea pig with compression injury of spinal cord | Inhibiting the formation of free radicals, and resistancing lipid peroxidation | [147] |
| PEG | – | Guinea pig with spinal cord transection | Repairing cell membrane, and reducing oxidative stress | [148] |
| PEG | DSPE | SD rats with compression injury of spinal cord | Reducing material concentration and improving dysfunction after injury | [149] |
| PLA | Bone marrow stromal cells | SD rats with spinal cord transection | Promoting nerve regeneration as well as restoration of conduction, and providing a better microenvironment | [150] |
| PLA | DHA | SD rats with spinal cord hemisection | Promoting axon regeneration with strong mechanical properties | [151] |
| PLA | Aligned microfiber-based grafts | SD rats with spinal cord transection | Reducing cyst volume in SCI | [152] |
| PLGA | DC-Chol | SD rats with spinal cord injury | Promoting the regeneration of blood vessels and tissues and improving exercise capacity | [153] |
| PLGA | HOMSC | SD rats with spinal cord transection | Promoting endogenous repair, thereby restoring exercise capacity | [154] |
| PLGA | DPSCs | Rats with spinal cord transection | Enhancing the regeneration of blood vessels and axons | [155] |
| PLGA | AntiNgR | SD rats with spinal cord hemisection | Inhibiting inflammation and promoting angiogenesis | [156] |
| PCL | HEnSCs and hSC | SD rats with spinal cord hemisection | Limiting secondary reactions and restoring motor function | [157] |
| PCL | PDO | SD rats with spinal cord hemisection | Promoting axonal regeneration and inhibiting the activity of astrocytes | [158] |
| PCL | – | Fischer 344 rats with spinal cord transection | Promoting axonal growth as well as reducing scar tissue | [159] |
| PVA | – | SD rats with spinal cord cervical contusion | Reducing inflammation and reducing the number of cell death—promoting proteins | [160] |
| PVA | MoS 2/GO | C57BL/6 N mice with spinal cord hemisection | Inhibiting inflammatory and the activation of glial cells at the site of injury | [161] |
| PHB | – | SD rats with spinal cord hemisection | Promoting differentiation of astrocytes but inhibits their activation | [162] |
| PHB | – | SD rats with spinal cord contusion | Inhibiting inflammatory bodies, reducing glial scar formation and promoting axonal growth | [163] |
| PHB | – | SD Rats with spinal cord hemi-contusion | Reducing neuroinflammatory reaction and improving exercise ability | [164] |
| PSA | MP | SD Rats with spinal cord transection | Inhibiting acute tissue inflammation and apoptosis, and promoting axon regeneration | [165] |
| PSA | HNK-1 | C57BL/6J mice with spinal cord compression injury | Promoting the formation of axonal myelin sheath and improving the recovery of function | [166] |
| PSA | 5-NOT | C57BL/6J mice with spinal cord compression injury | Promoting survival and neurite length of cortical neurons, and improving motor function | [167] |
| pHEMA | Various substrates and nutritional | Sprague–Dawley rats with spinal cord transection | Increasing the regeneration of the damaged spinal cord and improving motor ability | [168] |
| pHEMA | – | Wister rats with spinal cord hemisection or transection | Promoting regeneration of axons as well as blood vessels | [169] |
| pHEMA | – | Sprague–Dawley rats with spinal cord transection | Promoting axonal growth and reducing scar formation | [170] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, C.; Deng, L.; Yong, Y.-Y.; Wu, J.-M.; Qin, D.-L.; Yu, L.; Zhou, X.-G.; Wu, A.-G. The Application of Biomaterials in Spinal Cord Injury. Int. J. Mol. Sci. 2023, 24, 816. https://doi.org/10.3390/ijms24010816
Feng C, Deng L, Yong Y-Y, Wu J-M, Qin D-L, Yu L, Zhou X-G, Wu A-G. The Application of Biomaterials in Spinal Cord Injury. International Journal of Molecular Sciences. 2023; 24(1):816. https://doi.org/10.3390/ijms24010816
Chicago/Turabian StyleFeng, Chi, Lan Deng, Yuan-Yuan Yong, Jian-Ming Wu, Da-Lian Qin, Lu Yu, Xiao-Gang Zhou, and An-Guo Wu. 2023. "The Application of Biomaterials in Spinal Cord Injury" International Journal of Molecular Sciences 24, no. 1: 816. https://doi.org/10.3390/ijms24010816
APA StyleFeng, C., Deng, L., Yong, Y.-Y., Wu, J.-M., Qin, D.-L., Yu, L., Zhou, X.-G., & Wu, A.-G. (2023). The Application of Biomaterials in Spinal Cord Injury. International Journal of Molecular Sciences, 24(1), 816. https://doi.org/10.3390/ijms24010816







