Differential Role of Aldosterone and Transforming Growth Factor Beta-1 in Cardiac Remodeling
Abstract
:1. Introduction
2. Results
2.1. Baseline Characteristics of TGF-β1 Mice
2.2. Effects of Ald and Ep on Cardiac Hypertrophy
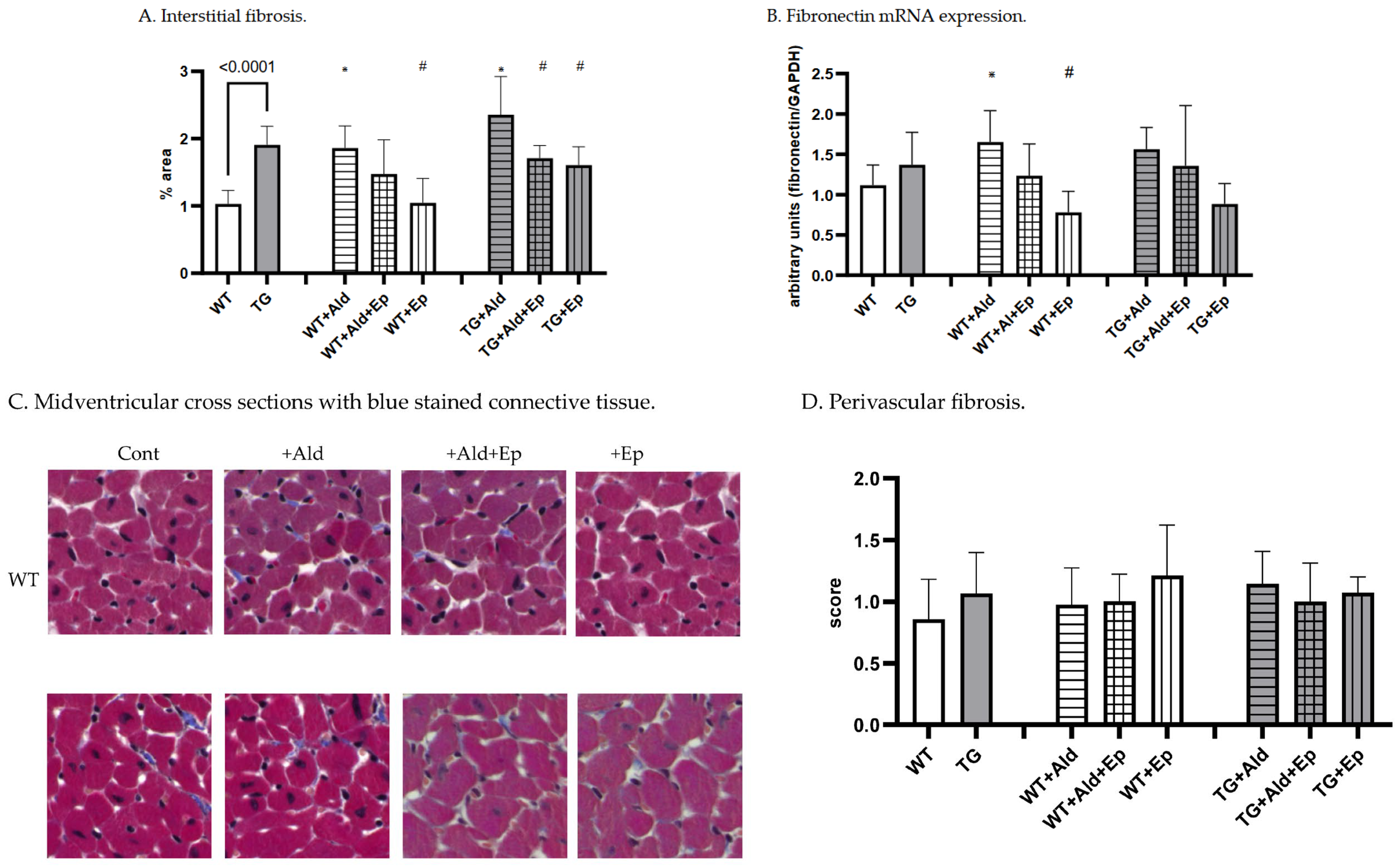
2.3. Effects of Ald and Ep on Cardiac Fibrosis
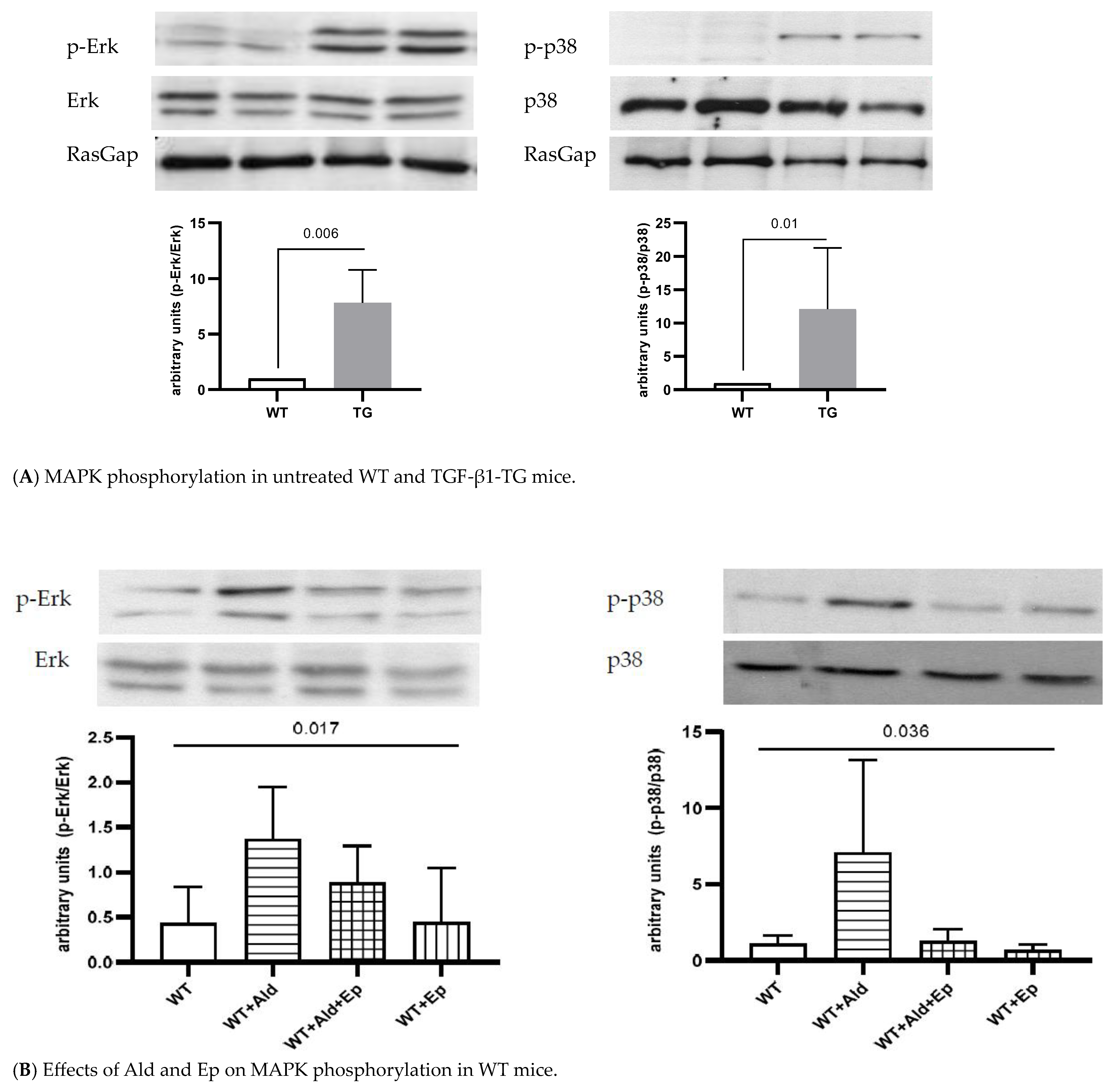
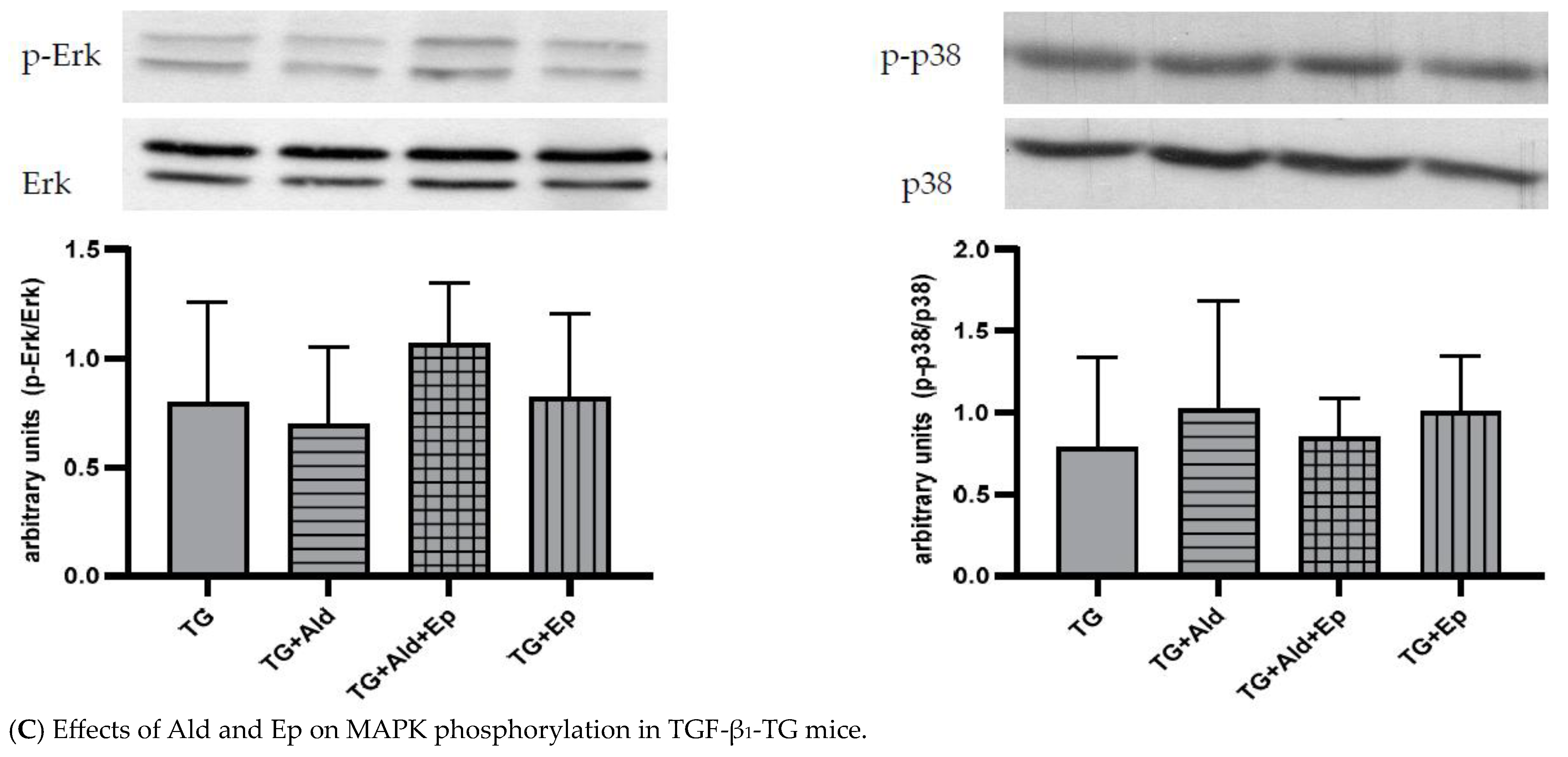
2.4. Effects of Ald and Ep on MAPK Signaling
3. Discussion
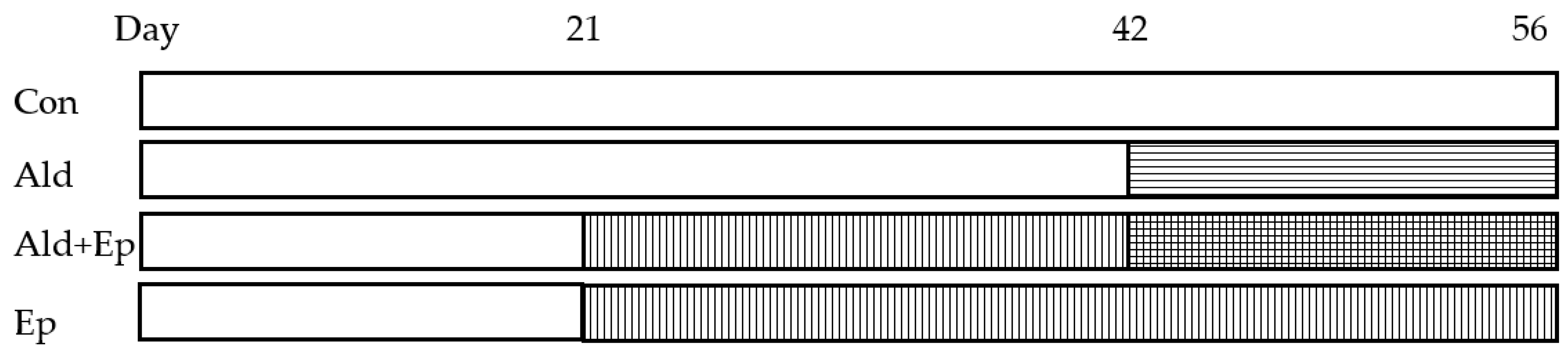
4. Materials and Methods
4.1. Treatment of Animals
4.2. Organ Extraction and Sample Preparation
4.3. Morphometric Analysis
4.4. Western Blotting
4.5. Real-Time qPCR
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shimizu, I.; Minamino, T. Physiological and Pathological Cardiac Hypertrophy. J. Mol. Cell. Cardiol. 2016, 97, 245–262. [Google Scholar] [CrossRef] [PubMed]
- Buffolo, F.; Tetti, M.; Mulatero, P.; Monticone, S. Aldosterone as a Mediator of Cardiovascular Damage. Hypertens. Dallas Tex 1979 2022, 79, 1899–1911. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Zhang, Y.-Y. Understanding the Role of Transforming Growth Factor-Beta Signalling in the Heart: Overview of Studies Using Genetic Mouse Models. Clin. Exp. Pharmacol. Physiol. 2008, 35, 335–341. [Google Scholar] [CrossRef]
- Brown, J.M.; Siddiqui, M.; Calhoun, D.A.; Carey, R.M.; Hopkins, P.N.; Williams, G.H.; Vaidya, A. The Unrecognized Prevalence of Primary Aldosteronism: A Cross-Sectional Study. Ann. Intern. Med. 2020, 173, 10–20. [Google Scholar] [CrossRef]
- Vaidya, A.; Hundemer, G.L.; Nanba, K.; Parksook, W.W.; Brown, J.M. Primary Aldosteronism: State-of-the-Art Review. Am. J. Hypertens. 2022, 35, 967–988. [Google Scholar] [CrossRef]
- Funder, J.W.; Carey, R.M. Primary Aldosteronism: Where Are We Now? Where to From Here? Hypertens. Dallas Tex 1979 2022, 79, 726–735. [Google Scholar] [CrossRef]
- Meng, X.-M.; Nikolic-Paterson, D.J.; Lan, H.Y. TGF-β: The Master Regulator of Fibrosis. Nat. Rev. Nephrol. 2016, 12, 325–338. [Google Scholar] [CrossRef]
- Rosenkranz, S. TGF-Beta1 and Angiotensin Networking in Cardiac Remodeling. Cardiovasc. Res. 2004, 63, 423–432. [Google Scholar] [CrossRef] [Green Version]
- Frangogiannis, N.G. Cardiac Fibrosis. Cardiovasc. Res. 2021, 117, 1450–1488. [Google Scholar] [CrossRef] [PubMed]
- Schultz, J.E.J.; Witt, S.A.; Glascock, B.J.; Nieman, M.L.; Reiser, P.J.; Nix, S.L.; Kimball, T.R.; Doetschman, T. TGF-Beta1 Mediates the Hypertrophic Cardiomyocyte Growth Induced by Angiotensin II. J. Clin. Investig. 2002, 109, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Scaglione, R.; Argano, C.; Di Chiara, T.; Parrinello, G.; Colomba, D.; Avellone, G.; Donatelli, M.; Corrao, S.; Licata, G. Effect of Dual Blockade of Renin-Angiotensin System on TGFbeta1 and Left Ventricular Structure and Function in Hypertensive Patients. J. Hum. Hypertens. 2007, 21, 307–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schlüter, K.D.; Zhou, X.J.; Piper, H.M. Induction of Hypertrophic Responsiveness to Isoproterenol by TGF-Beta in Adult Rat Cardiomyocytes. Am. J. Physiol. 1995, 269, C1311–C1316. [Google Scholar] [CrossRef] [PubMed]
- Cannavo, A.; Bencivenga, L.; Liccardo, D.; Elia, A.; Marzano, F.; Gambino, G.; D’Amico, M.L.; Perna, C.; Ferrara, N.; Rengo, G.; et al. Aldosterone and Mineralocorticoid Receptor System in Cardiovascular Physiology and Pathophysiology. Oxid. Med. Cell. Longev. 2018, 2018, 1204598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leask, A.; Abraham, D.J. TGF-Beta Signaling and the Fibrotic Response. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2004, 18, 816–827. [Google Scholar] [CrossRef]
- Schreier, B.; Rabe, S.; Schneider, B.; Ruhs, S.; Grossmann, C.; Hauptmann, S.; Blessing, M.; Neumann, J.; Gekle, M. Aldosterone/NaCl-Induced Renal and Cardiac Fibrosis Is Modulated by TGF-β Responsiveness of T Cells. Hypertens. Res. Off. J. Jpn. Soc. Hypertens. 2011, 34, 623–629. [Google Scholar] [CrossRef]
- Bujak, M.; Frangogiannis, N.G. The Role of TGF-Beta Signaling in Myocardial Infarction and Cardiac Remodeling. Cardiovasc. Res. 2007, 74, 184–195. [Google Scholar] [CrossRef] [Green Version]
- Pollard, C.M.; Desimine, V.L.; Wertz, S.L.; Perez, A.; Parker, B.M.; Maning, J.; McCrink, K.A.; Shehadeh, L.A.; Lymperopoulos, A. Deletion of Osteopontin Enhances Β₂-Adrenergic Receptor-Dependent Anti-Fibrotic Signaling in Cardiomyocytes. Int. J. Mol. Sci. 2019, 20, 1396. [Google Scholar] [CrossRef] [Green Version]
- Maning, J.; McCrink, K.A.; Pollard, C.M.; Desimine, V.L.; Ghandour, J.; Perez, A.; Cora, N.; Ferraino, K.E.; Parker, B.M.; Brill, A.R.; et al. Antagonistic Roles of GRK2 and GRK5 in Cardiac Aldosterone Signaling Reveal GRK5-Mediated Cardioprotection via Mineralocorticoid Receptor Inhibition. Int. J. Mol. Sci. 2020, 21, 2868. [Google Scholar] [CrossRef] [Green Version]
- Kakoki, M.; Pochynyuk, O.M.; Hathaway, C.M.; Tomita, H.; Hagaman, J.R.; Kim, H.-S.; Zaika, O.L.; Mamenko, M.; Kayashima, Y.; Matsuki, K.; et al. Primary Aldosteronism and Impaired Natriuresis in Mice Underexpressing TGFβ1. Proc. Natl. Acad. Sci. USA 2013, 110, 5600–5605. [Google Scholar] [CrossRef]
- Nishioka, T.; Suzuki, M.; Onishi, K.; Takakura, N.; Inada, H.; Yoshida, T.; Hiroe, M.; Imanaka-Yoshida, K. Eplerenone Attenuates Myocardial Fibrosis in the Angiotensin II-Induced Hypertensive Mouse: Involvement of Tenascin-C Induced by Aldosterone-Mediated Inflammation. J. Cardiovasc. Pharmacol. 2007, 49, 261–268. [Google Scholar] [CrossRef]
- Tsybouleva, N.; Zhang, L.; Chen, S.; Patel, R.; Lutucuta, S.; Nemoto, S.; DeFreitas, G.; Entman, M.; Carabello, B.A.; Roberts, R.; et al. Aldosterone, through Novel Signaling Proteins, Is a Fundamental Molecular Bridge between the Genetic Defect and the Cardiac Phenotype of Hypertrophic Cardiomyopathy. Circulation 2004, 109, 1284–1291. [Google Scholar] [CrossRef]
- Han, J.-S.; Choi, B.-S.; Yang, C.-W.; Kim, Y.-S. Aldosterone-Induced TGF-Beta1 Expression Is Regulated by Mitogen-Activated Protein Kinases and Activator Protein-1 in Mesangial Cells. J. Korean Med. Sci. 2009, 24, S195–S203. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, A.; Takeda, Y.; Karashima, S.; Kometani, M.; Aono, D.; Demura, M.; Higashitani, T.; Konishi, S.; Yoneda, T.; Takeda, Y. Impact of Mineralocorticoid Receptor Blockade with Direct Renin Inhibition in Angiotensin II-Dependent Hypertensive Mice. Hypertens. Res. Off. J. Jpn. Soc. Hypertens. 2020, 43, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Shao, L.; Ma, A.; Guan, G.; Wang, J.; Wang, Y.; Tian, G. Telmisartan Delays Myocardial Fibrosis in Rats with Hypertensive Left Ventricular Hypertrophy by TGF-Β1/Smad Signal Pathway. Hypertens. Res. Off. J. Jpn. Soc. Hypertens. 2014, 37, 43–49. [Google Scholar] [CrossRef]
- Tsai, C.-F.; Yang, S.-F.; Chu, H.-J.; Ueng, K.-C. Cross-Talk between Mineralocorticoid Receptor/Angiotensin II Type 1 Receptor and Mitogen-Activated Protein Kinase Pathways Underlies Aldosterone-Induced Atrial Fibrotic Responses in HL-1 Cardiomyocytes. Int. J. Cardiol. 2013, 169, 17–28. [Google Scholar] [CrossRef]
- Matsuki, K.; Hathaway, C.K.; Chang, A.S.; Smithies, O.; Kakoki, M. Transforming Growth Factor Beta1 and Aldosterone. Curr. Opin. Nephrol. Hypertens. 2015, 24, 139–144. [Google Scholar] [CrossRef] [Green Version]
- Khan, R. Examining Potential Therapies Targeting Myocardial Fibrosis through the Inhibition of Transforming Growth Factor-Beta 1. Cardiology 2007, 108, 368–380. [Google Scholar] [CrossRef]
- Sanderson, N.; Factor, V.; Nagy, P.; Kopp, J.; Kondaiah, P.; Wakefield, L.; Roberts, A.B.; Sporn, M.B.; Thorgeirsson, S.S. Hepatic Expression of Mature Transforming Growth Factor Beta 1 in Transgenic Mice Results in Multiple Tissue Lesions. Proc. Natl. Acad. Sci. USA 1995, 92, 2572–2576. [Google Scholar] [CrossRef]
- Rosenkranz, S.; Flesch, M.; Amann, K.; Haeuseler, C.; Kilter, H.; Seeland, U.; Schlüter, K.-D.; Böhm, M. Alterations of Beta-Adrenergic Signaling and Cardiac Hypertrophy in Transgenic Mice Overexpressing TGF-Beta(1). Am. J. Physiol. Heart Circ. Physiol. 2002, 283, H1253–H1262. [Google Scholar] [CrossRef]
- Seeland, U.; Haeuseler, C.; Hinrichs, R.; Rosenkranz, S.; Pfitzner, T.; Scharffetter-Kochanek, K.; Böhm, M. Myocardial Fibrosis in Transforming Growth Factor-Beta(1) (TGF-Beta(1)) Transgenic Mice Is Associated with Inhibition of Interstitial Collagenase. Eur. J. Clin. Investig. 2002, 32, 295–303. [Google Scholar] [CrossRef]
- Seeland, U.; Schäffer, A.; Selejan, S.; Hohl, M.; Reil, J.-C.; Müller, P.; Rosenkranz, S.; Böhm, M. Effects of AT1- and Beta-Adrenergic Receptor Antagonists on TGF-Beta1-Induced Fibrosis in Transgenic Mice. Eur. J. Clin. Investig. 2009, 39, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, H.; Nakajima, H.O.; Salcher, O.; Dittiè, A.S.; Dembowsky, K.; Jing, S.; Field, L.J. Atrial but Not Ventricular Fibrosis in Mice Expressing a Mutant Transforming Growth Factor-Beta(1) Transgene in the Heart. Circ. Res. 2000, 86, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Brooks, W.W.; Conrad, C.H. Myocardial Fibrosis in Transforming Growth Factor Beta(1)Heterozygous Mice. J. Mol. Cell. Cardiol. 2000, 32, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Kuwahara, F.; Kai, H.; Tokuda, K.; Kai, M.; Takeshita, A.; Egashira, K.; Imaizumi, T. Transforming Growth Factor-Beta Function Blocking Prevents Myocardial Fibrosis and Diastolic Dysfunction in Pressure-Overloaded Rats. Circulation 2002, 106, 130–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burch, M.L.; Yang, S.N.Y.; Ballinger, M.L.; Getachew, R.; Osman, N.; Little, P.J. TGF-Beta Stimulates Biglycan Synthesis via P38 and ERK Phosphorylation of the Linker Region of Smad2. Cell. Mol. Life Sci. CMLS 2010, 67, 2077–2090. [Google Scholar] [CrossRef] [PubMed]
- Derynck, R.; Zhang, Y.E. Smad-Dependent and Smad-Independent Pathways in TGF-Beta Family Signalling. Nature 2003, 425, 577–584. [Google Scholar] [CrossRef]
- Liu, X.; Sun, S.Q.; Hassid, A.; Ostrom, R.S. CAMP Inhibits Transforming Growth Factor-Beta-Stimulated Collagen Synthesis via Inhibition of Extracellular Signal-Regulated Kinase 1/2 and Smad Signaling in Cardiac Fibroblasts. Mol. Pharmacol. 2006, 70, 1992–2003. [Google Scholar] [CrossRef] [Green Version]
- Muslin, A.J. MAPK Signalling in Cardiovascular Health and Disease: Molecular Mechanisms and Therapeutic Targets. Clin. Sci. 2008, 115, 203–218. [Google Scholar] [CrossRef] [Green Version]
- Zhang, D.; Gaussin, V.; Taffet, G.E.; Belaguli, N.S.; Yamada, M.; Schwartz, R.J.; Michael, L.H.; Overbeek, P.A.; Schneider, M.D. TAK1 Is Activated in the Myocardium after Pressure Overload and Is Sufficient to Provoke Heart Failure in Transgenic Mice. Nat. Med. 2000, 6, 556–563. [Google Scholar] [CrossRef]
- Romero-Becerra, R.; Santamans, A.M.; Folgueira, C.; Sabio, G. P38 MAPK Pathway in the Heart: New Insights in Health and Disease. Int. J. Mol. Sci. 2020, 21, 7412. [Google Scholar] [CrossRef]
- Gallo, S.; Vitacolonna, A.; Bonzano, A.; Comoglio, P.; Crepaldi, T. ERK: A Key Player in the Pathophysiology of Cardiac Hypertrophy. Int. J. Mol. Sci. 2019, 20, 2164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duangrat, R.; Parichatikanond, W.; Morales, N.P.; Pinthong, D.; Mangmool, S. Sustained AT1R Stimulation Induces Upregulation of Growth Factors in Human Cardiac Fibroblasts via Gαq/TGF-β/ERK Signaling That Influences Myocyte Hypertrophy. Eur. J. Pharmacol. 2022, 937, 175384. [Google Scholar] [CrossRef] [PubMed]
- Bueno, O.F.; De Windt, L.J.; Tymitz, K.M.; Witt, S.A.; Kimball, T.R.; Klevitsky, R.; Hewett, T.E.; Jones, S.P.; Lefer, D.J.; Peng, C.F.; et al. The MEK1-ERK1/2 Signaling Pathway Promotes Compensated Cardiac Hypertrophy in Transgenic Mice. EMBO J. 2000, 19, 6341–6350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshida, K.; Kim-Mitsuyama, S.; Wake, R.; Izumiya, Y.; Izumi, Y.; Yukimura, T.; Ueda, M.; Yoshiyama, M.; Iwao, H. Excess Aldosterone under Normal Salt Diet Induces Cardiac Hypertrophy and Infiltration via Oxidative Stress. Hypertens. Res. 2005, 28, 447–455. [Google Scholar] [CrossRef] [Green Version]
- Nakano, S.; Kobayashi, N.; Yoshida, K.; Ohno, T.; Matsuoka, H. Cardioprotective Mechanisms of Spironolactone Associated with the Angiotensin-Converting Enzyme/Epidermal Growth Factor Receptor/Extracellular Signal-Regulated Kinases, NAD(P)H Oxidase/Lectin-Like Oxidized Low-Density Lipoprotein Receptor-1, and Rho-Kinase Pathways in Aldosterone/Salt-Induced Hypertensive Rats. Hypertens. Res. 2005, 28, 925–936. [Google Scholar] [CrossRef] [Green Version]
- Qin, W.; Rudolph, A.E.; Bond, B.R.; Rocha, R.; Blomme, E.A.G.; Goellner, J.J.; Funder, J.W.; McMahon, E.G. Transgenic Model of Aldosterone-Driven Cardiac Hypertrophy and Heart Failure. Circ. Res. 2003, 93, 69–76. [Google Scholar] [CrossRef]
- Iglarz, M.; Touyz, R.M.; Viel, E.C.; Amiri, F.; Schiffrin, E.L. Involvement of Oxidative Stress in the Profibrotic Action of Aldosterone. Interaction Wtih the Renin-Angiotension System. Am. J. Hypertens. 2004, 17, 597–603. [Google Scholar] [CrossRef]
- Johar, S.; Cave, A.C.; Narayanapanicker, A.; Grieve, D.J.; Shah, A.M. Aldosterone Mediates Angiotensin II-Induced Interstitial Cardiac Fibrosis via a Nox2-Containing NADPH Oxidase. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2006, 20, 1546–1548. [Google Scholar] [CrossRef] [Green Version]
- Brilla, C.G. Aldosterone and Myocardial Fibrosis in Heart Failure. Herz 2000, 25, 299–306. [Google Scholar] [CrossRef]
- Tsukamoto, O.; Minamino, T.; Sanada, S.; Okada, K.; Hirata, A.; Fujita, M.; Shintani, Y.; Yulin, L.; Asano, Y.; Takashima, S.; et al. The Antagonism of Aldosterone Receptor Prevents the Development of Hypertensive Heart Failure Induced by Chronic Inhibition of Nitric Oxide Synthesis in Rats. Cardiovasc. Drugs Ther. 2006, 20, 93–102. [Google Scholar] [CrossRef]
- Okoshi, M.P.; Yan, X.; Okoshi, K.; Nakayama, M.; Schuldt, A.J.T.; O’Connell, T.D.; Simpson, P.C.; Lorell, B.H. Aldosterone Directly Stimulates Cardiac Myocyte Hypertrophy. J. Card. Fail. 2004, 10, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Nehme, J.; Mercier, N.; Labat, C.; Benetos, A.; Safar, M.E.; Delcayre, C.; Lacolley, P. Differences between Cardiac and Arterial Fibrosis and Stiffness in Aldosterone-Salt Rats: Effect of Eplerenone. J. Renin-Angiotensin-Aldosterone Syst. JRAAS 2006, 7, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Samuel, S.K.; Hurta, R.A.; Kondaiah, P.; Khalil, N.; Turley, E.A.; Wright, J.A.; Greenberg, A.H. Autocrine Induction of Tumor Protease Production and Invasion by a Metallothionein-Regulated TGF-Beta 1 (Ser223, 225). EMBO J. 1992, 11, 1599–1605. [Google Scholar] [CrossRef] [PubMed]
- Bruder-Nascimento, T.; Ferreira, N.S.; Zanotto, C.Z.; Ramalho, F.; Pequeno, I.O.; Olivon, V.C.; Neves, K.B.; Alves-Lopes, R.; Campos, E.; Silva, C.A.A.; et al. NLRP3 Inflammasome Mediates Aldosterone-Induced Vascular Damage. Circulation 2016, 134, 1866–1880. [Google Scholar] [CrossRef]
- Ikuno, Y.; Kazlauskas, A. TGFbeta1-Dependent Contraction of Fibroblasts Is Mediated by the PDGFalpha Receptor. Investig. Ophthalmol. Vis. Sci. 2002, 43, 41–46. [Google Scholar]
- Stael, S.; Miller, L.P.; Fernández-Fernández, Á.D.; Van Breusegem, F. Detection of Damage-Activated Metacaspase Activity by Western Blot in Plants. In Plant Proteases and Plant Cell Death; Klemenčič, M., Stael, S., Huesgen, P.F., Eds.; Methods in Molecular Biology; Springer US: New York, NY, USA, 2022; Volume 2447, pp. 127–137. ISBN 978-1-07-162078-6. [Google Scholar]
- Rio, D.C.; Ares, M.; Hannon, G.J.; Nilsen, T.W. Purification of RNA Using TRIzol (TRI Reagent). Cold Spring Harb. Protoc. 2010, 2010, pdb-prot5439. [Google Scholar] [CrossRef]
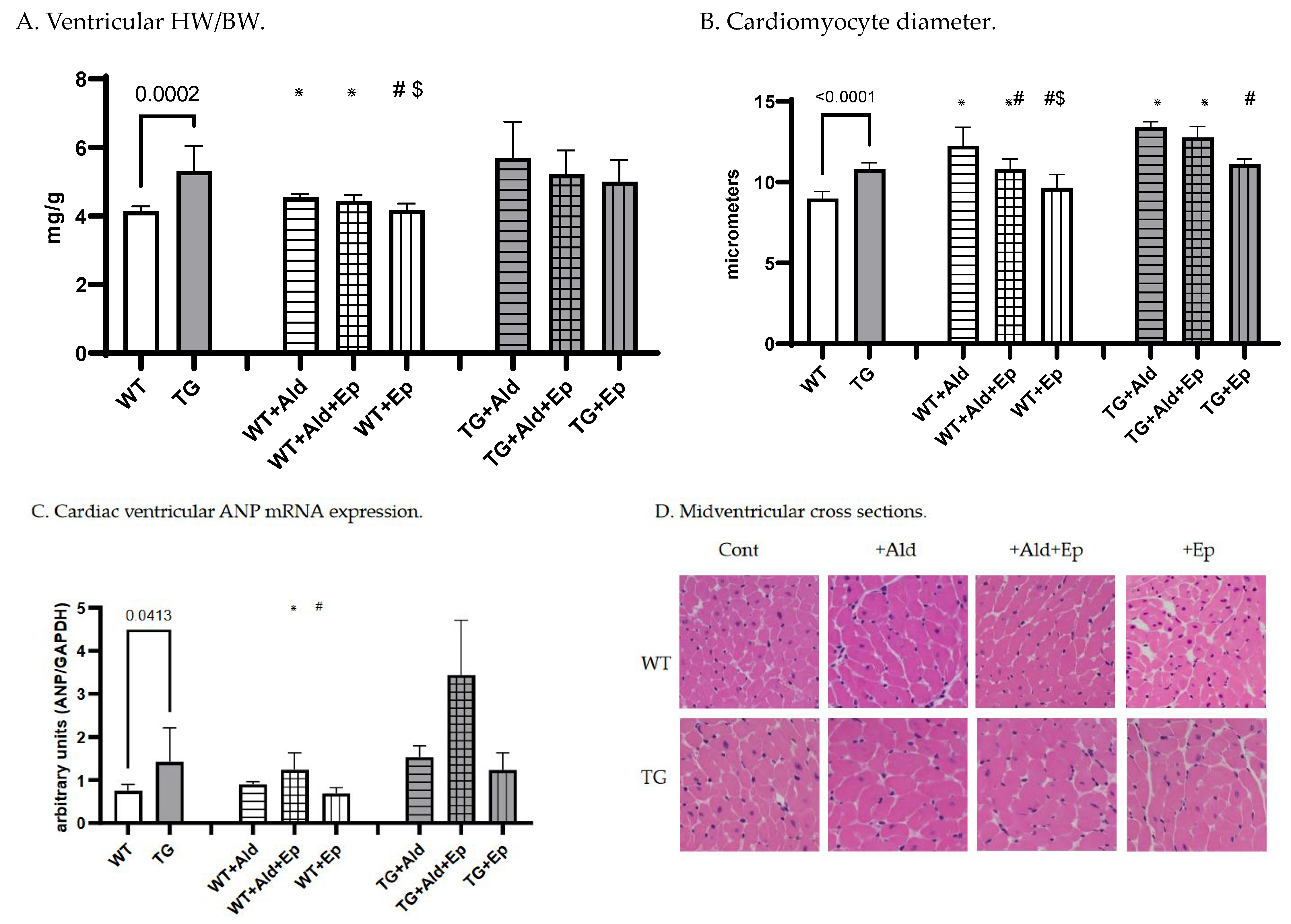
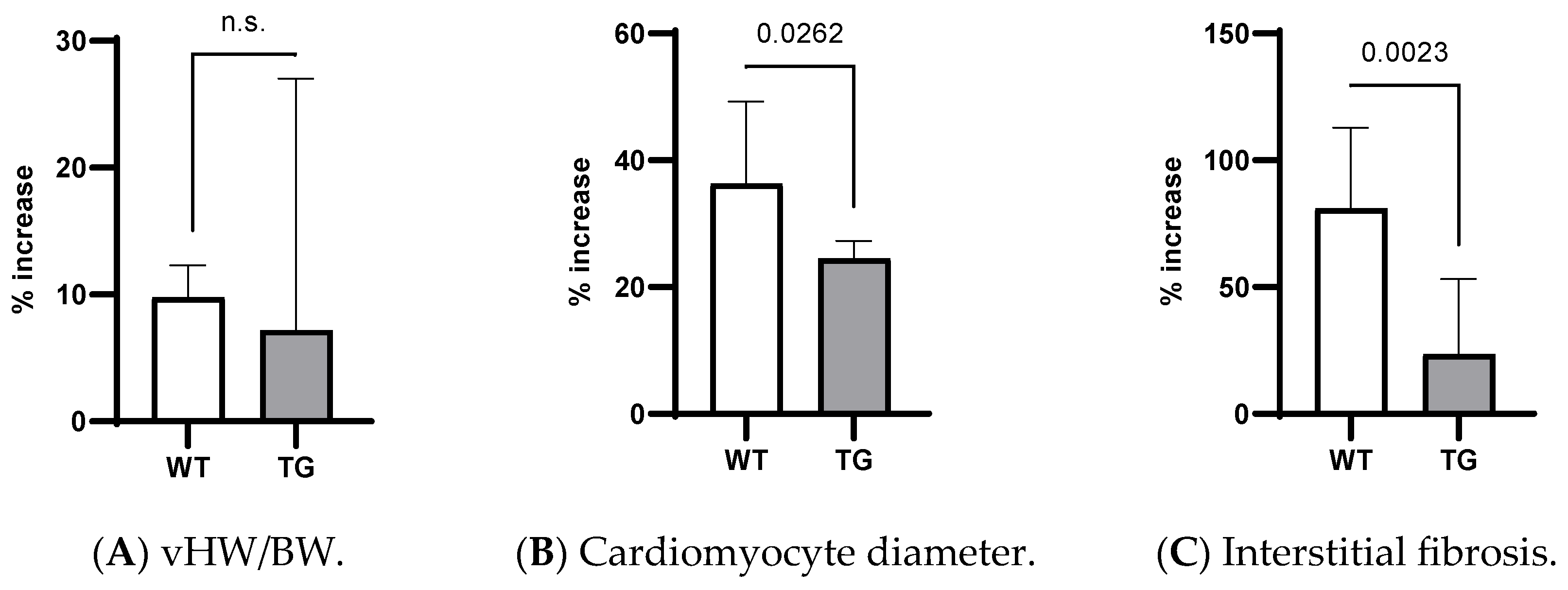
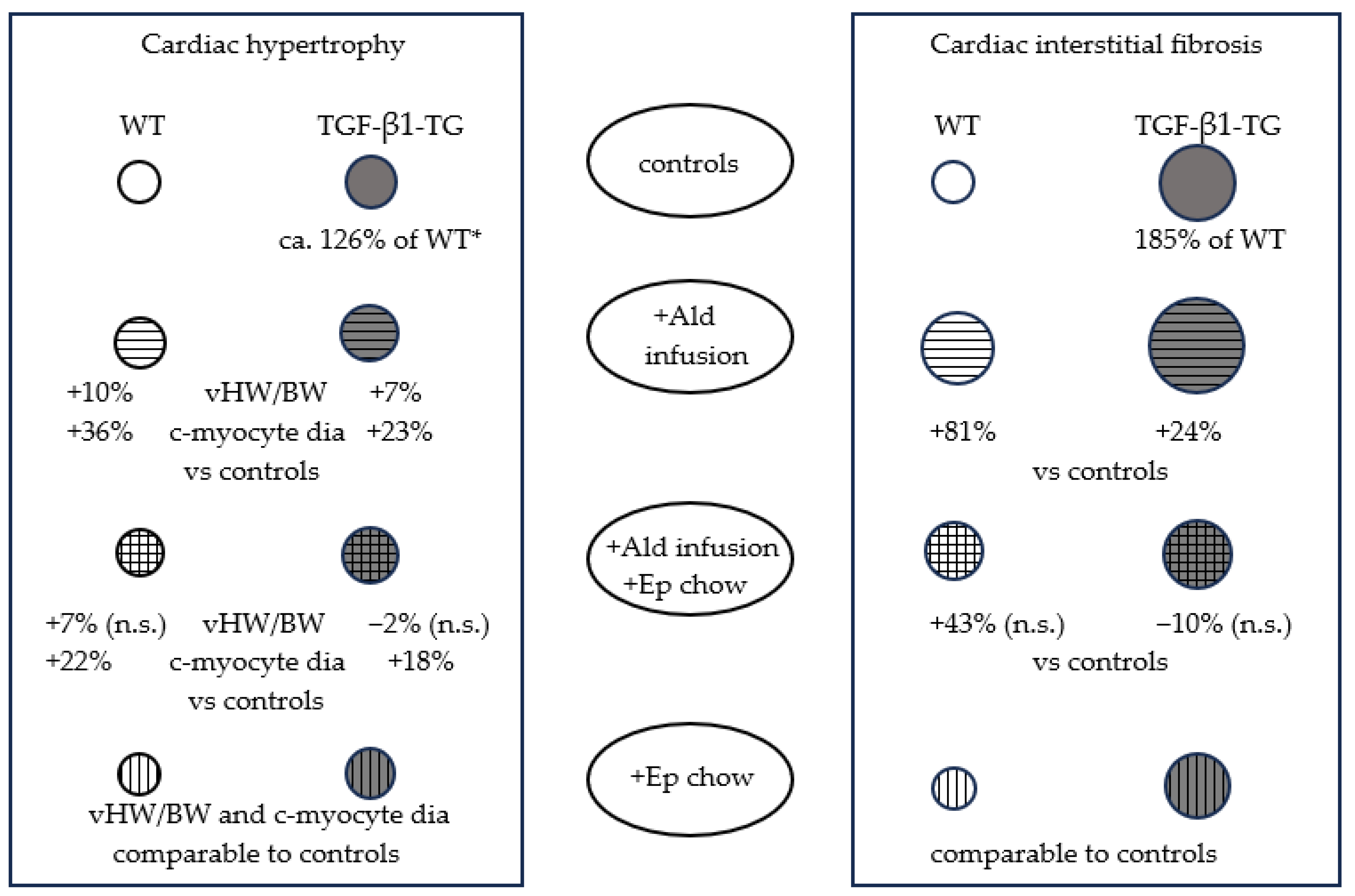
| WT | TG | p | WT + Ald | WT + Ald + Ep | WT + Ep | p (WT) | TG + Ald | TG + Ald + Ep | TG + Ep | p (TG) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ventricular HW /BW | n | 8 | 14 | 7 | 7 | 8 | 9 | 9 | 9 | |||
| mg/g | 4.1 ± 0.1 | 5.3 ± 0.7 | <10−3 | 4.5 ± 0.1 * | 4.4 ± 0.2 * | 4.2 ± 0.2 #$ | <10−4 | 5.7 ± 1.1 | 5.2 ± 0.7 | 5 ± 0.6 | 0.31 | |
| Cardiomyocyte diameter | n | 8 | 9 | 7 | 7 | 8 | 9 | 9 | 9 | |||
| µm | 8.8 (0.8) | 10.9 (0.3) | <10−4 | 12.3 ± 1.2 * | 10.8 ± 0.6 *# | 9.6 ± 0.8 #$ | <10−4 | 13.4 (0.5) * | 12.8 (1.1) * | 11 (0.5) # | <10−4 | |
| ANP/GAPDH mRNA | n | 7 | 14 | 6 | 7 | 6 | 7 | 7 | 6 | |||
| - | 0.8 ± 0.2 | 1.4 ± 0.8 | 0.041 | 0.9 ± 0.06 | 1.2 ± 0.4 * | 0.7 ± 0.1 $ | 10−3 | 1.5 ± 0.3 | 3.4 ± 1.3 *# | 1.2 ± 0.4 $ | <10−4 | |
| Interstitial fibrosis | n | 8 | 9 | 7 | 7 | 8 | 9 | 9 | 10 | |||
| % | 1 ± 0.1 | 1.9 ± 0.1 | <10−4 | 1.9 ± 0.1 * | 1.5 ± 0.2 | 1.05 ± 0.1 # | <10−3 | 2.4 ± 0.2 * | 1.7 ± 0.1 # | 1.61 ± 0.1 # | <10−3 | |
| Perivascular fibrosis | n | 8 | 9 | 7 | 6 | 6 | 9 | 9 | 10 | |||
| score | 0.9 ± 0.3 | 1.1 ± 0.3 | 0.21 | 1 ± 0.3 | 1 ± 0.22 | 1.2 ± 0.4 | 0.27 | 1.2 ± 0.26 | 1 ± 0.3 | 1.1 ± 0.1 | 0.73 | |
| FBN/GAPDH mRNA | n | 7 | 15 | 7 | 7 | 7 | 7 | 9 | 7 | |||
| - | 1.1 ± 0.3 | 1.4 ± 0.4 | 0.15 | 1.7 ± 0.4 * | 1.2 ± 0.4 | 0.8 ± 0.3 # | <10−3 | 1.6 ± 0.3 | 1.4 ± 0.8 | 0.9 ± 0.3 | 0.06 | |
| Kidney W /BW | n | 8 | 14 | 7 | 10 | 8 | 9 | 9 | 9 | |||
| mg/g | 11.9 ± 0.3 | 12.8 ± 1.6 | 0.15 | 14.9 ± 1.6 * | 13.7 ± 1.2 * | 11.4 ± 1.5 #$ | <10−4 | 15.9 ± 1.5 * | 13 ± 0.8 # | 12.3 ± 1.8 # | <10−4 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kmieć, P.; Rosenkranz, S.; Odenthal, M.; Caglayan, E. Differential Role of Aldosterone and Transforming Growth Factor Beta-1 in Cardiac Remodeling. Int. J. Mol. Sci. 2023, 24, 12237. https://doi.org/10.3390/ijms241512237
Kmieć P, Rosenkranz S, Odenthal M, Caglayan E. Differential Role of Aldosterone and Transforming Growth Factor Beta-1 in Cardiac Remodeling. International Journal of Molecular Sciences. 2023; 24(15):12237. https://doi.org/10.3390/ijms241512237
Chicago/Turabian StyleKmieć, Piotr, Stephan Rosenkranz, Margarete Odenthal, and Evren Caglayan. 2023. "Differential Role of Aldosterone and Transforming Growth Factor Beta-1 in Cardiac Remodeling" International Journal of Molecular Sciences 24, no. 15: 12237. https://doi.org/10.3390/ijms241512237
APA StyleKmieć, P., Rosenkranz, S., Odenthal, M., & Caglayan, E. (2023). Differential Role of Aldosterone and Transforming Growth Factor Beta-1 in Cardiac Remodeling. International Journal of Molecular Sciences, 24(15), 12237. https://doi.org/10.3390/ijms241512237







