Abstract
Emerging and re-emerging viruses periodically cause outbreaks and epidemics around the world, which ultimately lead to global events such as the COVID-19 pandemic. Thus, the urgent need for new antiviral drugs is obvious. Over more than a century of antiviral development, nucleoside analogs have proven to be promising agents against diversified DNA and RNA viruses. Here, we present the synthesis and evaluation of the antiviral activity of nucleoside analogs and their deglycosylated derivatives based on a hydroxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one scaffold. The antiviral activity was evaluated against a panel of structurally and phylogenetically diverse RNA and DNA viruses. The leader compound showed micromolar activity against representatives of the family Coronaviridae, including SARS-CoV-2, as well as against respiratory syncytial virus in a submicromolar range without noticeable toxicity for the host cells. Surprisingly, methylation of the aromatic hydroxyl group of the leader compound resulted in micromolar activity against the varicella-zoster virus without any significant impact on cell viability. The leader compound was shown to be a weak inhibitor of the SARS-CoV-2 RNA-dependent RNA polymerase. It also inhibited biocondensate formation important for SARS-CoV-2 replication. The active compounds may be considered as a good starting point for further structure optimization and mechanistic and preclinical studies.
1. Introduction
Over the past two decades, humanity has been afflicted by an increasing number of viral epidemics, including H1N1 influenza, Ebola, and the COVID-19 outbreaks/pandemic [1,2,3,4]. Unfortunately, there is often a lack of effective treatment options for emerging or re-emerging viruses. Developing new antiviral drugs is a time-consuming task, so, when urgent action is required, modifying existing drug scaffolds and repurposing approved drugs is considered the best approach [5].
Nucleoside analogs (NAs) are considered a good choice for quick and efficient development of antiviral therapeutics. Most NAs inhibit viral replication through chain termination or lethal mutagenesis [6,7,8], but they can also affect the efficiency of the binding of a viral nucleic acid to polymerases and inhibit viral methyltransferases and a number of host cell enzymes that are essential for virus replication, such as those involved in nucleotide synthesis and RNA capping [9,10,11]. The efficacy and safety profiles of NAs have been extensively studied, and over 30 NAs have already been approved by the FDA [12,13]. On the other hand, recently discovered features on the mechanism of action and the proposed complex modifications of NAs reveal that, despite their long history, NAs are still prospective for investigation of novel antiviral drugs [14,15].
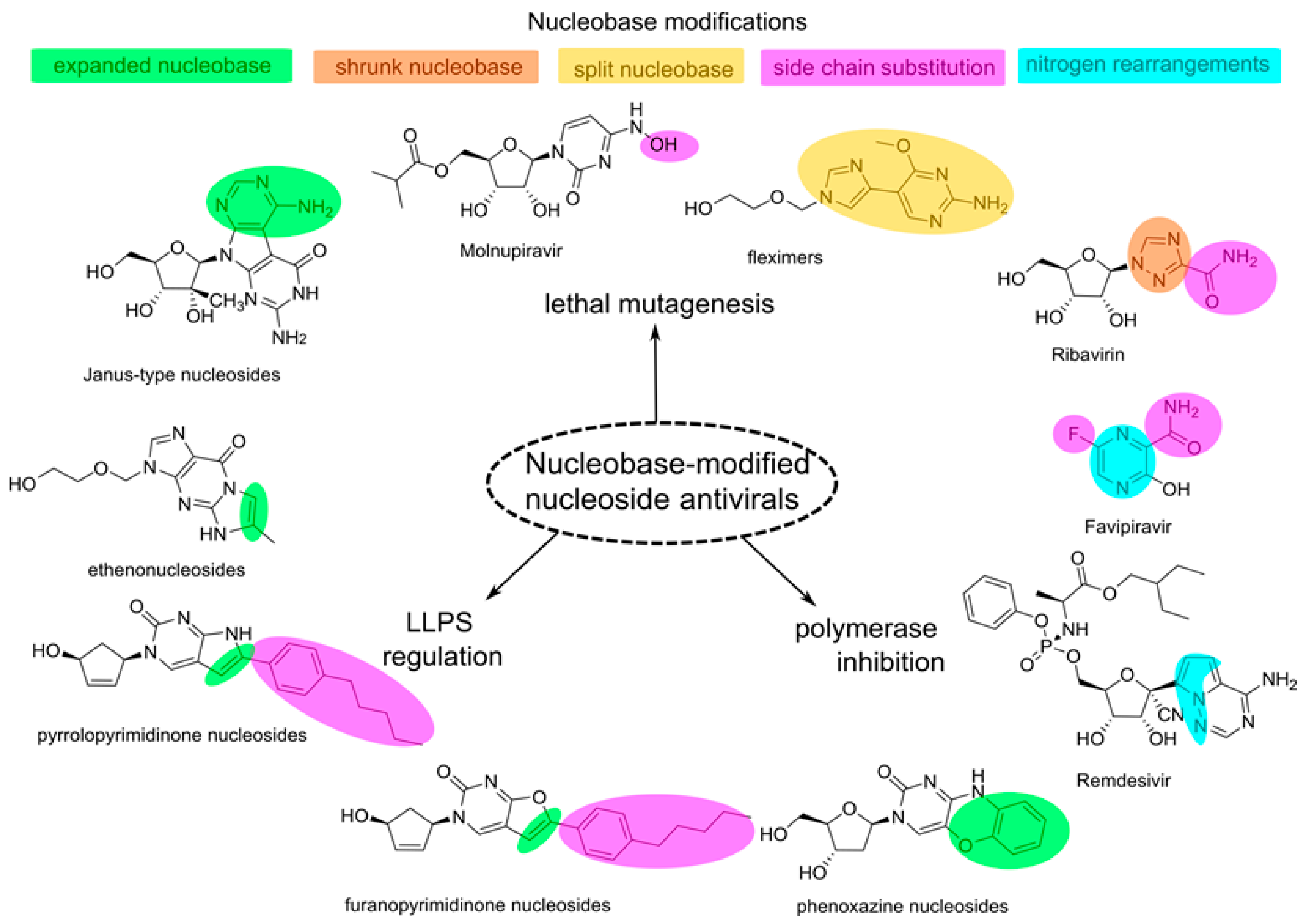
Nucleoside analogs are derivatives of natural nucleosides with a modified sugar residue and/or nucleobase. Sugar modification has been extensively used to obtain viral polymerase inhibitors [7], but the potential of nucleobase modifications has been less explored. Modifications of nucleobases can be classified as follows: (1) nitrogen substitution and rearrangements in the heterocycle (aza and deaza derivatives), (2) side-chain substitution, (3) heterocycle splitting, and (4) nucleobases expansion (Figure 1). Modifications of the first type can be used to increase the stability of the drug, as demonstrated in the case of remdesivir [16]. Many NAs with a modified nucleobase act through lethal mutagenesis, including ribavirin, favipiravir, molnupiravir, and Janus-type nucleosides, however, the latter are less promising due to their high cytotoxicity [6,17]. Fleximers carrying split nucleobases demonstrate mutagenic activity, as well as the ability to inhibit viral polymerases and methyltransferases [18,19]. Etheno derivatives with acyclic sugar residues have demonstrated antiviral activity against viruses from the family Herpesviridae, but they have been shown to be low-effective prodrugs of antivirals with natural nucleobases [20,21]. Phenoxazine derivatives attract attention due to a wide spectrum of activity against RNA and DNA viruses [22]. Their mechanism of action has not been studied, but the incorporation of phenoxazine nucleotides into the growing chain of the viral nucleic acid might lead to a suboptimal secondary structure [22]. Bicyclic NAs, such as furanopyrimidinone and pyrrolopyrimidinone-based derivatives, are a promising class of antivirals [23], including the most effective inhibitor of VZV known to date [24]. A series of furanopyrimidinone derivatives with exclusive activity against VZV can only be phosphorylated by VZV kinases, but their target and further metabolic fate remain unknown [25]. Pyrrolopyrimidinones are capable of inhibiting the activity of coronavirus polymerase without incorporation into the growing chain [26]. At the same time, both pyrrolo- and furanopyrimidinones can influence liquid–liquid phase separation (LLPS) of the viral nucleocapsid protein (N) and viral genomic RNA (vgRNA) [27]. LLPS affects viral packaging and viral genome replication through the recruitment of viral polymerases, thus representing a prospective process to be targeted by antivirals [28].
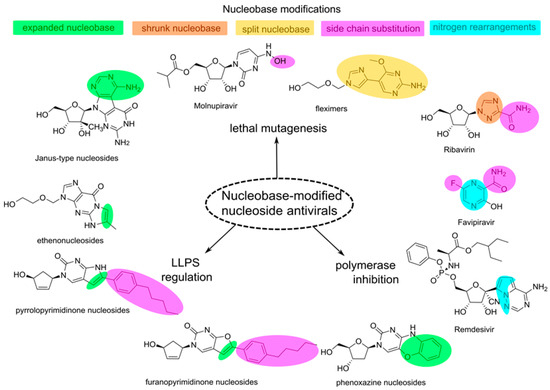
Figure 1.
Examples of nucleobase modifications in various antivirals.
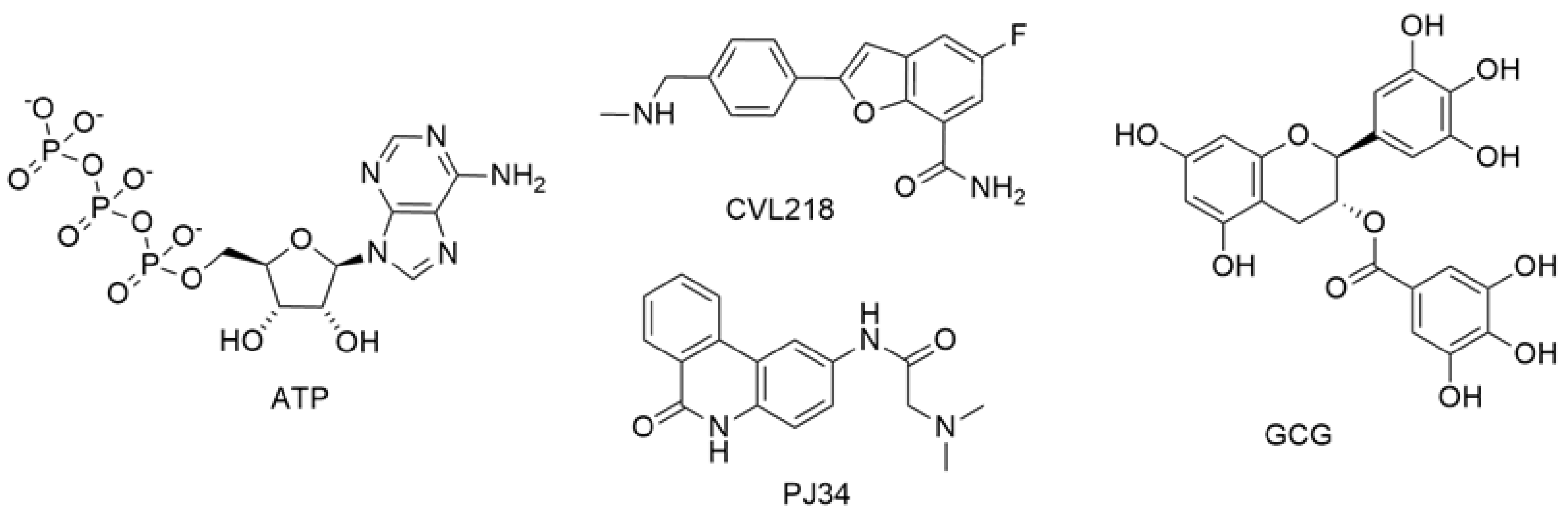
LLPS has been recognized as a new target for antiviral development due to its important role in the viral life cycle [29,30]. LLPS provides the formation of non-membrane organelles, where enrichment in specific biomolecules is achieved to increase the efficiency of biological processes [29,31]. DNA damage foci, promyelocytic leukemia nuclear bodies (PML nuclear bodies), Cajal bodies, processing bodies (P-bodies), and stress granules are prominent examples of host cell biocondensates. Viruses also utilize LLPS to ensure viral genome replication and assembly, as was demonstrated for a number of viruses, including SARS-CoV-2 and HIV-1 [29,30,32,33]. Furthermore, viruses can evade antiviral immune response through LLPS regulation and biocondensate formation [29]. As LLPS is significant for viral replication, small-molecule LLPS modulators are being developed and assessed as antivirals (Figure 2) [33]. Among endogenous molecules, ATP was shown to modulate SARS-CoV-2 N protein condensation with vgRNA [34]. Gallocatechin-3-gallate (GCG) effectively binds to the N protein, disrupts biocondensate formation, and demonstrates moderate antiviral activity [35]. CVL218 and PJ34 decrease the density of SARS-CoV-2 N-protein:vgRNA biocondensates and facilitate access to viral replication machinery for remdesivir [36]. Nucleoside skeletons with modified nucleobases are also promising scaffolds for obtaining LLPS-modulating antivirals, as was demonstrated by pyrrolo- and furanopyrimidinones nucleoside derivatives [27].
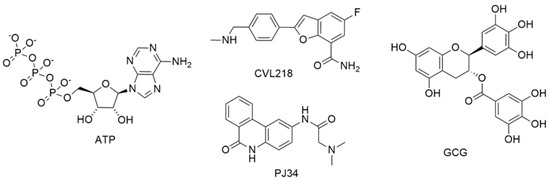
Figure 2.
Examples of LLPS modulators.
Here, we have synthesized a set of nucleoside and non-nucleoside derivatives based on an aromatic system extended in comparison with the parent cytosine nucleobase and tested them for their ability to suppress viral replication in vitro of a large panel of DNA and RNA viruses. In addition, the ability of the leader compound to inhibit the activity of SARS-CoV-2 RNA-dependent RNA polymerase (RdRp) and modulate the formation of biomolecular condensates important for SARS-CoV-2 transcription and replication has been evaluated.
2. Results and Discussion
2.1. Chemistry
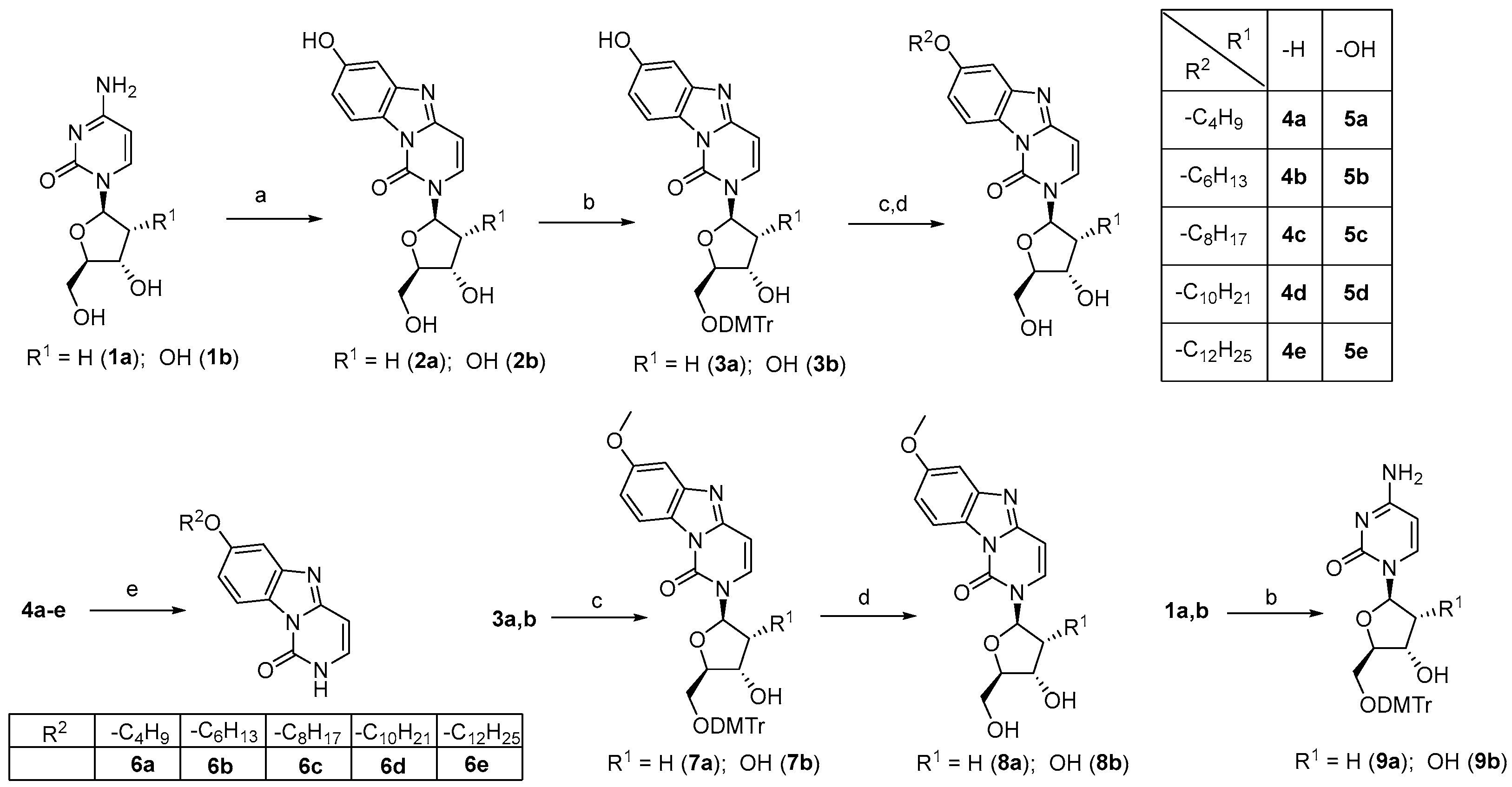
The synthesis began with the extension of the cytosine heteroaromatic system. To create the benzo[4,5]imidazo[1,2-c]pyrimidinonyl system, a reported method for 2′-deoxycytidine as a starting material was used [37]. 2′-Deoxycytidine 1a or cytidine 1b was treated with 1,4-benzoquinone in a sodium acetate buffer (pH 4.5), affording the corresponding tricyclic derivatives 2a and 2b, respectively (Scheme 1). After 5’-O-dimethoxytritylation (DMTr) of 2a,b, the resulting compounds (3a,b) were subjected to Mitsunobu coupling with CnH2n+1OH (n = 4, 6, 8, 10 or 12), followed by DMTr removal in mild acidic conditions (aqueous CH3COOH, 50 °C), yielding the target candidate antivirals 4a–e and 5a–e of the 2′-deoxyribo- and ribonucleoside series, respectively. Finally, to synthesize the tricyclic non-nucleoside derivatives 6a–e, we exploited the instability of the glycosidic bond of the 2′-deoxyribo series and treated 4a–e with hydrochloric acid in CH3OH. Based on activity studies for the above derivatives, an additional set of compounds was prepared. Mitsunobu reaction was applied to condensate 3a,b with CH3OH to prepare 7a,b, and their 5′-O-deblocking provided 8a,b. In addition, 1a,b was also 5′-O-dimethoxytritylated for the preparation of 9a,b, two control compounds for evaluating the role of the tricyclic moiety in the manifestation of antiviral activity.
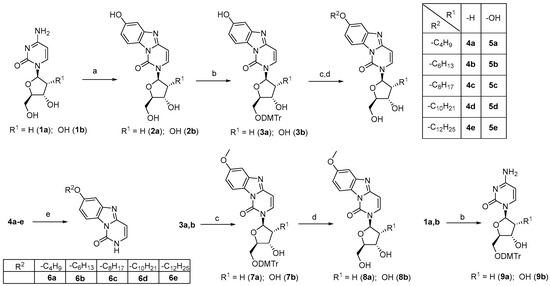
Scheme 1.
The preparation of the benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one derivatives. Reagents and conditions: (a) 1,4-benzoquinone, sodium acetate buffer (pH 4.5), 37 °C; (b) DMTr-Cl, Py, rt; (c) CnH2n+1OH (n = 1 (7a,b), 4 (4a and 5a), 6 (4b and 5b), 8 (4c and 5c), 10 (4d and 5d), 12 (4e and 5e)), PPh3, DIAD, CH2Cl2, 0 °C→rt; (d) CH3COOH, H2O, 50 °C; and (e) 12 N HCl, CH3OH, 50 °C.
2.2. Biological Evaluation
Compounds from the first synthetic round, namely 2a,b, 3a,b, 4a–e, 5a–e, and 6a–e, were evaluated for activity against DNA viruses, including varicella zoster virus (VZV), cytomegalovirus (HCMV), and herpes simplex virus-1 (HSV-1), as well as against RNA viruses, including human coronavirus (HCoV), respiratory syncytial virus (RSV), yellow fever virus (YFV), influenza A virus (IAV), and influenza B virus (IBV) (see Table S1). Ganciclovir, cidofovir, acyclovir, brivudine, remdesivir, ribavirin, zanamivir, and dextran sulfate (molecular weight 10,000, DS.−10,000) were used as reference compounds. Antiviral activity was expressed as EC50, the effective concentration required to reduce virus plaque formation (VZV) by 50% or to reduce the virus-induced cytopathic effect by 50% (other viruses).
All compounds tested can be divided into three groups: (1) 2′-O-deoxyribonucleoside (2a, 3a, 4a–e), (2) ribonucleoside (2b, 3b, 5a–e), and (3) non-nucleoside (6a–e) series. Among them, only two 5′-O-DMTr-substituted compounds (3a and 3b) exhibited activity against two HCoVs, namely 229E and OC43, with EC50 values in the micromolar and submicromolar range, respectively, without any signs of potency against another HCoV strain NL63 (Table 1). These compounds also showed an inhibitory effect on RSV, with 3a having an order of magnitude lower EC50 than 3b. However, the activity was accompanied by cytotoxicity for the Huh7 cell line. The in vitro efficiency of tritylated and 4,4′-dimethoxytritylated pyrimidine and purine nucleoside and non-nucleoside analogs against diverse viruses, including representatives of families Flaviviridae and Herpesviridae, was previously reported [22,38,39]. The results emphasize the importance of the DMTr group in both nucleoside series for their activity, regardless of the sugar moiety. Meanwhile, non-nucleoside derivatives from the third group did not show any noticeable potency. There was no significant activity against VZV, HCMV, HSV-1, YFV, IAV, and IBV.

Table 1.
Activity and cytotoxicity of derivatives from the first synthetic round against HCoV (229E, OC43, and NL63) and RSV (Long) in HEL299/Huh7 cells.
Then, several analogs of the leader compounds 3a,b were synthesized, namely derivatives 7a,b bearing an OCH3 group at the seventh position and their 5′-O-deblocked congeners 8a,b. To evaluate the contribution of the tricyclic system to antiviral activity, 5′-O-DMTr-2′-deoxycytidine 9a and 5′-O-DMTr-cytidine 9b were also synthesized. The compounds were tested against VZV (TK+ and TK− strains) and HCMV (AD-169 and Davis strains) (Table 2). Surprisingly, the methylation of the 7-OH group, which was unsubstituted in the inactive compounds 3a,b, led to anti-VZV activity, whereas there was no activity against HCMV. The inhibitory effect was noticeably greater against the thymidine kinase-deficient TK− VZV strain, suggesting a kinase-independent mechanism of action. Importantly, the activity of 7a was not accompanied by noticeable cytotoxicity, which provides a promising index of selectivity (SI = CC50/EC50) of more than 30 for the TK-deficient VZV strain. The lack of activity of 8a,b and 9a,b emphasizes the importance of the DMTr group and the substituted tricyclic heteroaromatic system.

Table 2.
Activity and cytotoxicity of derivatives from the second synthetic round against VZV in HEL299 cells.
Finally, the set of the second-round compounds was evaluated on a panel of various SARS-CoV-2 strains (Table 3). Only compound 3a from the 2′-O-deoxyribose series had anti-SARS-CoV-2 activity, however, affecting cell morphology at ≥20 μM concentration.

Table 3.
Activity and cytotoxicity of derivatives from the second synthetic round against SARS-CoV-2 in Vero cells.
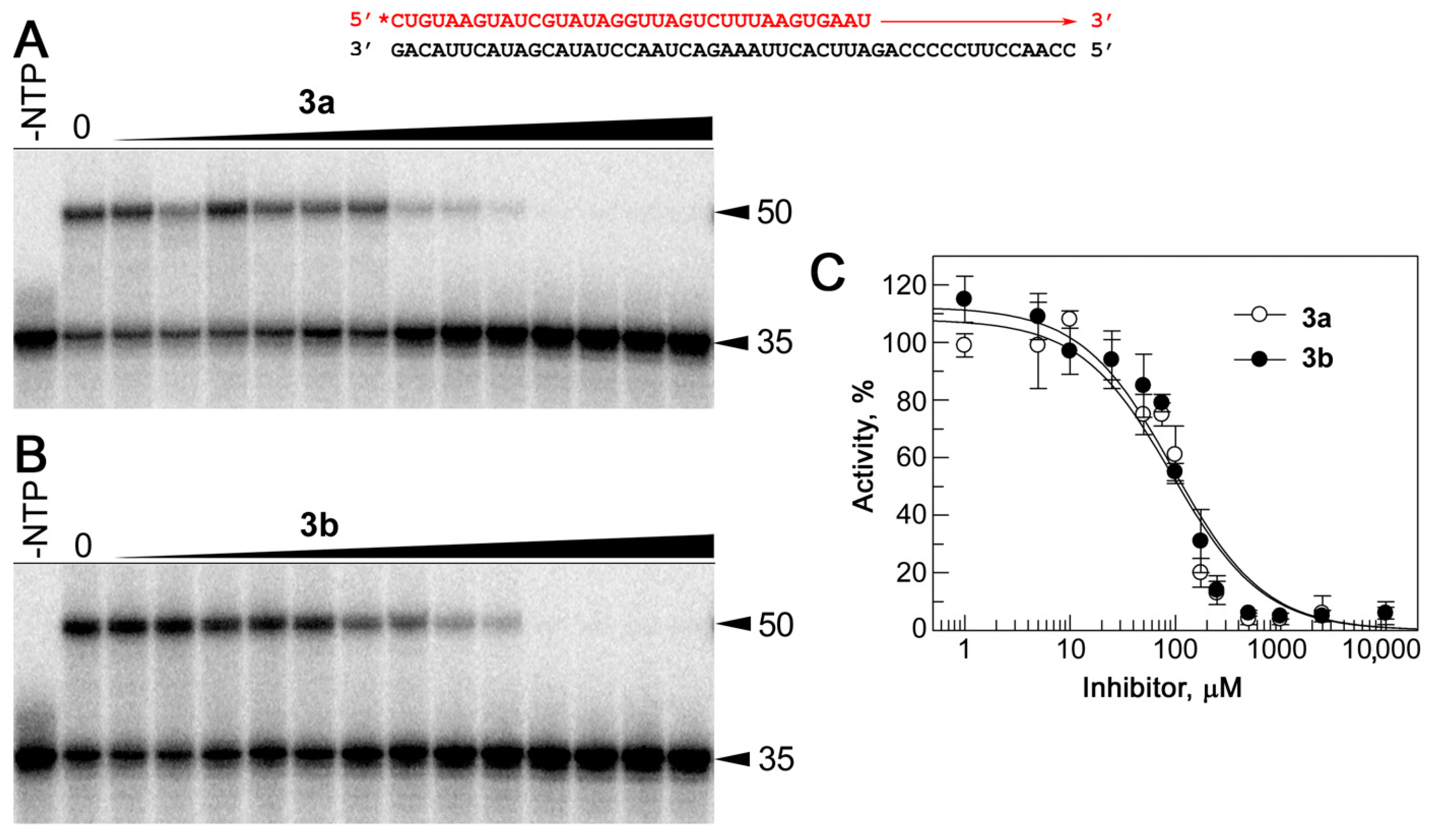
2.3. Inhibition of RdRp Activity In Vitro
Since the leader compound 3a is a 5′-O-dimethoxytrityl nucleoside derivative with activity against various representatives of the family Coronaviridae, viral RNA-dependent RNA polymerase (RdRp) may be considered as its potential target. Indeed, RNA viruses, including coronaviruses, share conserved core sequences and structural features of RdRp [40]. 3′,5′-di-O-trityluridine was shown to inhibit DENV polymerase with IC50 values ranging from 3.1 to 6.9 μM by affecting RNA elongation rather than by the initiation of a DENV-specific “minigenomic” RNA template [38]. To verify this assumption, we analyzed the effects of the leader 3a from the deoxyribose series and its close analog (3b), which is inactive in the CPE reduction assay, on the activity of the SARS-CoV-2 transcription/replication complex in vitro. For this purpose, we purified the RdRp holoenzyme, consisting of the catalytic subunit nsp12 and two accessory subunits (nsp7 and nsp), and tested its activity with a double-stranded RNA substrate containing a radiolabeled primer and the template strand in the presence of various inhibitor concentrations. Previously, we showed that the system could be used as a good model for studying substrate specificity and testing RdRp inhibitors [26,41]. We examined the effect of the inhibitors on RdRp activity in concentrations ranging from 1 µM to 10 mM (Figure 3). To our surprise, the inhibition activity of compounds 3a and 3b was very similar. Both substances were transcriptional inhibitors with almost identical IC50 values, 94 ± 3 μM and 95 ± 4 μM for 3a and 3b, respectively.
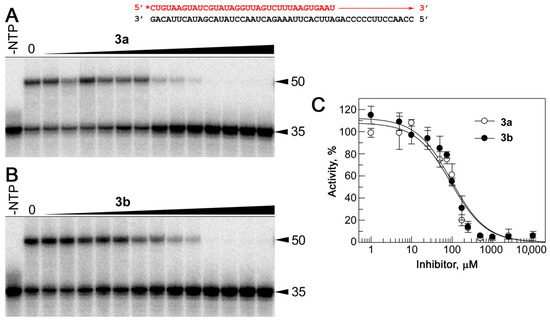
Figure 3.
The effects of compounds 3a and 3b on the activity of RdRp in vitro. The RNA substrate, consisting of an RNA primer 32P-labeled at the 5′-end (red) and the template strand (black), is shown on the top. The direction of primer extension by RdRp is indicated by the red arrow. (A,B) Analysis of RNA products at various concentrations of 3a (A) and 3b (B). Positions of the RNA primer and the extended full-length RNA product are indicated by black arrows. The length of RNA is indicated. (C) Quantitative analysis of the inhibition of RdRp activity by 3a and 3b. Means and standard deviations from three independent measurements are shown. The data were fitted to a hyperbolic equation (see Section 3.3.2 for details).
These values significantly differ from the data on antiviral activity for compound 3a, which has a much lower EC50 value than 3b (by at least one order of magnitude) (Table 3). In contrast to our results, several previously tested nucleoside inhibitors had close values of EC50 and IC50, measured in almost the same in vitro system [26]. Thus, RdRp may not be the primary target for 3a, suggesting the presence of other viral or cellular targets.
2.4. Inhibition of Biocondensate Formation In Vitro
In vivo transcription and replication of SARS-CoV-2 requires the assembly of biomacromolecular condensates on the vgRNA through LLPS [42]. This process is driven by transient interactions of the partly disordered N-protein, which binds stem-loop-rich vgRNA fragments and acts as a condensate “scaffold” [43]. RdRp enters the condensates as a “client” [42]. Its accumulation within the condensates ensures timely vgRNA replication. We assumed the observed anti-SARS-CoV-2 activity of 3a may be associated with the disruption of these condensates.
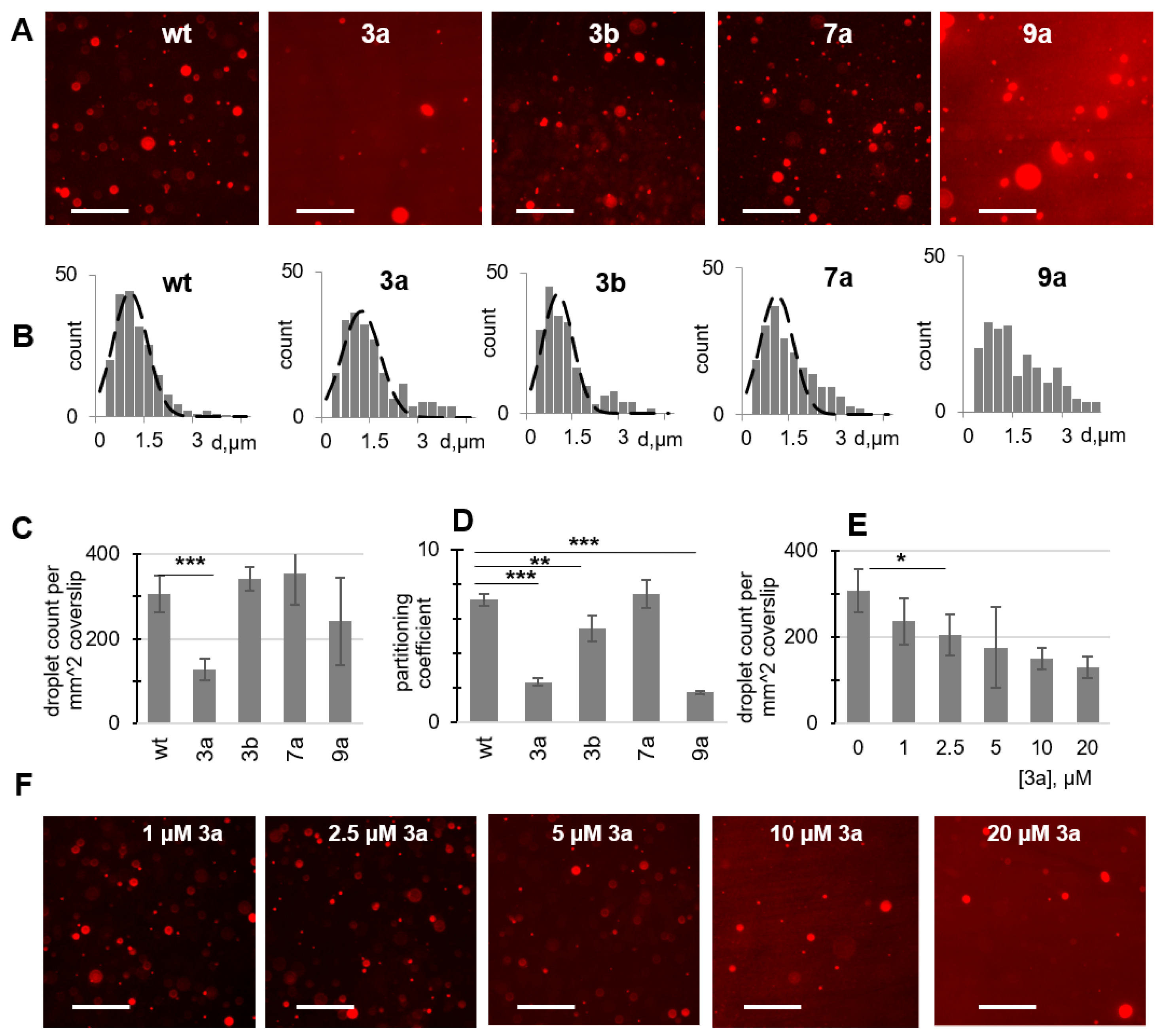
Compound 3a is somewhat similar to previously reported condensate-modulating nucleoside analogs [27], so we verified its activity in LLPS assays. For that, we used model condensates assembled from fluorescently labeled SARS-CoV-2 N-protein and the stem-loop vgRNA fragment, as was described previously [27]. In parallel to the active compound 3a, we tested three inactive derivatives as negative controls, namely 3b with an additional 2′-OH, 7a with an additional methylation of the 7-OH group, and 5′-O-DMTr 2′-deoxycytidine 9a, a derivative without the tricyclic heteroaromatic system. In the absence of the compounds, the condensates were visualized by fluorescence microscopy as droplets of 0.9 ± 0.6 micrometer diameter (Figure 4A,B and Figure S1). They floated and coalesced, consistently with the liquid phase. They were morphologically analogous to previously observed condensates and distinct from reported gel-like structures or solid aggregates [27].
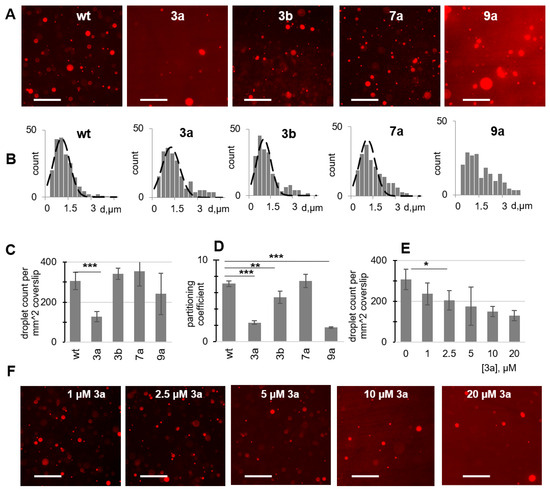
Figure 4.
The effects of the antiviral compounds on biocondensate formation in vitro: cell-free LLPS assays. (A) Fluorescence microscopy images of the condensates assembled from the labeled SARS-CoV-2 N-protein (3 µM) and the gRNA fragment (6 µM) in the absence (wt) and in the presence of the compounds (20 µM). Scale bar: 10 µm. Additional representative large-field images are provided in Supplementary Information. (B) Size distribution of condensates obtained in the absence (wt) and in the presence of the compounds (20 µM). (C) Summary of the compounds’ effects on condensate formation estimated as the average number of droplets per slide (D) Antivirals’ effects on the partitioning coefficient of the N-protein. (E) Dose-dependence of the effects of compound 3a. (F) Representative fluorescence microscopy images illustrating the dose-dependent effects of 3a. Scale bar: 10 µm. Error bars in C-E represent the SD of six repeats. * p < 0.05; ** p < 0.001; *** p < 0.0001 (two-tailed Student’s t-test).
Unlike the negative controls 3b, 7a, and 9a, compound 3a showed significant (p < 0.0001) inhibition of condensate formation; the average number of droplets decreased by approximately 60% in the presence of 20 µM 3a (Figure 4C). The partitioning coefficient (droplet/solution N-protein concentration ratio) also decreased by 60–70% in the presence of 3a (p < 0.0001), while 3b had a much smaller effect (Figure 4D). Surprisingly, 9a caused a dramatic (approximately 4-fold) decrease in the partitioning coefficient; however, the droplets remained clearly visible, and many of them were enlarged, resulting in a broad and multimodal size distribution (Figure 4B). In the case of 3a (median droplet diameter equal to 1.1 µm) and other compounds (median droplet diameter equal to 0.9 µm), size distribution changes were minor to moderate. To summarize, 9a reduced droplet density but did not prevent LLPS, 7a caused no changes, the effect of 3b was minor, and 3a was the only robust LLPS inhibitor. The effect of 3a was dose-dependent (Figure 4E,F) with EC50 ≤ 10 µM. We conclude that the pronounced antiviral activity of 3a in Vero cells may result, in part, from a combination of LLPS inhibition and direct RdRp inhibition. Importantly, proper orientation of the polar OH groups on the heteroaromatic backbone is essential for LLPS inhibition.
3. Materials and Methods
3.1. Chemistry
3.1.1. General
All reagents were purchased from commercial sources and were used without further purification. Anhydrous CH2Cl2 and pyridine were obtained by distillation over calcium hydride. NMR spectra were recorded on a Bruker Avance III 600 spectrometer (Bruker, Rheinstetten, Germany) at 600 and 150 MHz for 1H and 13C spectra, respectively, or on a Bruker Fourier 300 spectrometer (Bruker, Rheinstetten, Germany) at 300 and 75 MHz for 1H and 13C spectra, respectively. Chemical shifts were reported relative to the residue peaks of DMSO-d6 (2.50 ppm for 1H and 39.5 ppm for 13C) and CDCl3 (7.26 ppm for 1H and 77.0 ppm for 13C). Thin layer chromatography (TLC) was performed on Merck TLC Silica gel 60F254 plates with spot visualization with a UV lamp at 254 nm. Silica gel (silica gel 60, 0.040–0.063 mm) from Merck (Darmstadt, Germany) was used for column chromatography. ESI HR mass spectra were acquired on an LTQ FT Ultra (Thermo Electron Corp., Bremen, Germany) mass spectrometer in negative ion mode.
3.1.2. Synthesis and Characterization of Compounds
General procedure for the preparation of nucleoside derivatives with a tricyclic aromatic system
To a solution of nucleoside 1 (9.50 mmol) in 0.1 M sodium acetate buffer (250 mL, pH 4.5), 1,4-benzoquinone (4.31 g, 40.0 mmol, 4.2 equiv) was added and the reaction mixture was stirred at 37 °C for 24 h. The solvent was removed under reduced pressure and the residue was purified using column chromatography on silica gel (0–13% CH3OH in CH2Cl2), yielding the product as a beige amorphous solid.
7-hydroxy-2-((2R,4S,5R)-4-hydroxy-5-(hydroxymethyl)tetrahydrofuran-2-yl)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 2a
Yield 59%. 1H NMR (600 MHz, DMSO-d6): δ 9.59 (s, 1H), 7.81 (d, J = 7.9 Hz, 1H), 7.75 (s, 1H), 7.53 (d, J = 8.5 Hz, 1H), 6.93 (d, J = 8.3 Hz, 1H), 6.66 (d, J = 7.9 Hz, 1H), 6.46 (t, J = 6.5 Hz, 1H), 5.30 (d, J = 3.3 Hz, 1H), 5.06 (t, J = 4.7 Hz, 1H), 4.34–4.29 (m, 1H), 3.89–3.84 (m, 1H), 3.67–3.58 (m, 2H), 2.26–2.19 (m, 2H). 13C NMR (150 MHz, DMSO-d6): δ 153.97, 146.79, 146.74, 137.18, 130.90, 130.46, 119.03, 114.51, 100.47, 98.12, 87.56, 84.70, 70.35, 61.22, 39.96. HRMS (ESI) m/z: calcd for C15H14N3O5− [M-H]−: 316.0939; found 316.0901.
2-((2R,3R,4S,5R)-3,4-dihydroxy-5-(hydroxymethyl)tetrahydrofuran-2-yl)-7-hydroxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 2b
Yield 57%. 1H NMR (600 MHz, DMSO-d6): δ 9.61 (s, 1H), 7.84 (d, J = 8.1 Hz, 1H), 7.76 (d, J = 2.4 Hz, 1H), 7.54 (d, J = 8.7 Hz, 1H), 6.94 (dd, J = 8.7 Hz, J = 2.4 Hz, 1H), 6.68 (d, J = 8.1 Hz, 1H), 6.10 (d, J = 5.5 Hz, 1H), 5.43 (d, J = 5.6 Hz, 1H), 5.16 (t, J = 5.1 Hz, 1H), 5.13 (d, J = 5.0 Hz, 1H), 4.18–4.15 (m, 1H), 4.07–4.04 (m, 1H), 3.95–3.93 (m, 1H), 3.71–3.67 (m, 1H), 3.64–3.60 (m, 1H). 13C NMR (150 MHz, DMSO-d6): δ 154.03, 147.06, 146.72, 137.15, 131.07, 130.48, 119.08, 114.54, 100.46, 98.12, 88.19, 85.09, 73.95, 69.93, 60.83. HRMS (ESI) m/z: calcd for C15H14N3O6− [M-H]−: 332.0888; found 332.0853.
General procedure for introducing the 5′-O-DMTr group
Compound 1 or 2 (3.00 mmol) was co-evaporated with anhydrous pyridine (20 mL), then dissolved in anhydrous pyridine (80 mL), and 4,4′-dimethoxytrityl chloride (1.22 g, 3.60 mmol, 1.2 equiv) was added. After 5 h at RT, the reaction was stopped by the addition of an aqueous saturated NaHCO3 solution (50 mL), and the organics were extracted with CH2Cl2 (2 × 50 mL). The combined organic layers were concentrated and co-evaporated with toluene (3 × 10 mL). Purification was performed using column chromatography on silica gel (0–4% CH3OH in CH2Cl2 with 0.1% TEA), yielding 3a,b and 9a,b as yellowish and off-white amorphous solids, respectively.
2-((2R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-4-hydroxytetrahydrofuran-2-yl)-7-hydroxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 3a
Yield 80%. 1H NMR (300 MHz, DMSO-d6): δ 9.54 (s, 1H), 7.76 (d, J = 2.4 Hz, 1H), 7.58 (d, J = 8.1 Hz, 1H), 7.53 (d, J = 8.7 Hz, 1H), 7.43–7.38 (m, 2H), 7.35–7.19 (m, 7H), 6.94 (dd, J = 8.7 Hz, J = 2.5 Hz, 1H), 6.92–6.85 (m, 4H), 6.45 (t, J = 6.4 Hz, 1H), 6.39 (d, J = 8.1 Hz, 1H), 5.34 (d, J = 4.7 Hz, 1H), 4.42–4.34 (m, 1H), 4.00–3.94 (m, 1H), 3.73 (s, 3H), 3.73 (s, 3H), 3.32–3.26 (m, 2H), 2.37–2.30 (m, 2H). 13C NMR (75 MHz, DMSO-d6): δ 157.99 (2C), 154.01, 146.61 (2C), 144.56, 137.15, 135.35, 135.16, 130.74, 130.45, 129.63 (4C), 127.73 (2C), 127.63 (2C), 126.61, 119.03, 114.53, 113.10 (4C), 100.45, 97.86, 85.72, 85.47, 84.73, 69.84, 63.27, 54.89 (2C), 39.43 (overlaps with DMSO). HRMS (ESI) m/z: calcd for C36H32N3O7− [M-H]−: 618.2246; found 618.2161.
2-((2R,3R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-3,4-dihydroxytetrahydrofuran-2-yl)-7-hydroxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 3b
Yield 53%. 1H NMR (300 MHz, DMSO-d6): δ 9.58 (s, 1H), 7.77 (d, J = 2.2 Hz, 1H), 7.66 (d, J = 8.1 Hz, 1H), 7.54 (d, J = 8.7 Hz, 1H), 7.45–7.39 (m, 2H), 7.37–7.21 (m, 7H), 6.98–6.87 (m, 5H), 6.34 (d, J = 8.0 Hz, 1H), 6.07 (d, J = 3.5 Hz, 1H), 5.51 (d, J = 4.8 Hz, 1H), 5.15 (d, J = 5.6 Hz, 1H), 4.28–4.17 (m, 2H), 4.09–4.02 (m, 1H), 3.74 (s, 6H), 3.36–3.31 (m, 2H). 13C NMR (75 MHz, DMSO-d6): δ 158.08 (2C), 154.12, 146.83, 146.66, 144.63, 137.16, 135.35, 135.12, 131.00, 130.52, 129.75 (4C), 127.88 (2C), 127.69 (2C), 126.75, 119.14, 114.62, 113.21 (4C), 100.50, 97.81, 89.43, 85.86, 82.60, 73.84, 69.53, 62.84, 54.97, 54.85. HRMS (ESI) m/z: calcd for C36H32N3O8− [M-H]−: 634.2195; found 634.2121.
4-amino-1-((2R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-4-hydroxytetrahydrofuran-2-yl)pyrimidin-2(1H)-one 9a
Yield 89%. 1H NMR (600 MHz, DMSO-d6): δ 7.69 (d, J = 7.5 Hz, 1H), 7.53 (br s, 2H), 7.39–7.36 (m, 2H), 7.33–7.30 (m, 2H), 7.27–7.22 (m, 5H), 6.91–6.88 (m, 4H), 6.15 (t, J = 6.3 Hz, 1H), 5.62 (d, J = 7.5 Hz, 1H), 5.30 (d, J = 4.3 Hz, 1H), 4.27–4.23 (m, 1H), 3.90–3.86 (m, 1H), 3.74 (s, 6H), 3.22 (dd, J = 10.6 Hz, J = 5.0 Hz, 1H), 3.19 (dd, J = 10.6 Hz, J = 3.4 Hz, 1H). 13C NMR (150 MHz, DMSO-d6): δ 164.50, 158.00 (2C), 153.70, 144.57, 140.93, 135.32, 135.21, 129.60 (4C), 127.74 (2C), 127.59 (2C), 126.64, 113.11 (4C), 93.70, 85.64, 85.13, 84.67, 69.80, 63.23, 54.94 (2C), 40.27. HRMS (ESI) m/z: calcd for C30H30N3O6− [M-H]−: 528.2140; found 528.2098.
4-amino-1-((2R,3R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-3,4-dihydroxytetrahydrofuran-2-yl)pyrimidin-2(1H)-one 9b
Yield 79%. 1H NMR (600 MHz, DMSO-d6): δ 7.81 (d, J = 7.5 Hz, 1H), 7.64 (br s, 2H), 7.40–7.37 (m, 2H), 7.34–7.30 (m, 2H), 7.28–7.23 (m, 5H), 6.91–6.88 (m, 4H), 5.77 (d, J = 2.9 Hz, 1H), 5.58 (d, J = 7.5 Hz, 1H), 5.44 (d, J = 3.9 Hz, 1H), 5.06 (d, J = 6.0 Hz, 1H), 4.11–4.06 (m, 1H), 4.00–3.94 (m, 2H), 3.75 (s, 6H), 3.28–3.23 (m, 2H). 13C NMR (150 MHz, DMSO-d6): δ 164.31, 158.01 (2C), 153.56, 144.55, 141.31, 135.33, 135.16, 129.60 (4C), 127.76 (2C), 127.60 (2C), 126.66, 113.13 (4C), 93.59, 89.84, 85.68, 81.66, 73.92, 69.08, 62.54, 54.93 (2C). HRMS (ESI) m/z: calcd for C30H30N3O7− [M-H]−: 544.2089; found 544.2063.
General procedure for the preparation of 7-O-alkylated nucleoside derivatives
To a stirred mixture of compound 3 (0.11 mmol), PPh3 (58 mg, 0.22 mmol, 2 equiv) and the corresponding CnH2n+1OH alcohol (n = 4, 6, 8, 10, 12) (0.15 mmol, 1.3 equiv) in dry CH2Cl2 (5 mL) DIAD (43 μL, 0.22 mmol, 2 equiv) was added at 0 °C. The reaction mixture was stirred at RT overnight and concentrated under reduced pressure. The residue was dissolved in a mixture of CH3COOH/H2O (2 mL, 1:9, v:v) and kept at 50 °C for 8 h. After concentration and co-evaporation with toluene (3 × 10 mL), the residue was purified using column chromatography on silica gel (0–6% CH3OH in CH2Cl2), yielding 4a–e and 5a–e as a yellowish amorphous solid.
2-((2R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-4-hydroxytetrahydrofuran-2-yl)-7-butoxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 4a
Yield 82%. 1H NMR (300 MHz, DMSO-d6): δ 7.87(d, J = 8.0 Hz, 1H), 7.85 (dd, J = 2.6 Hz, 1H), 7.62 (d, J = 8.8 Hz, 1H), 7.09 (dd, J = 8.8 Hz, J = 2.6 Hz, 1H), 6.68 (d, J = 8.0 Hz, 1H), 6.46 (t, J = 6.7 Hz, 1H), 4.35–4.30 (m, 1H), 4.05 (t, J = 6.5 Hz, 2H), 3.91–3.86 (m, 1H), 3.67 (dd, J = 11.9 Hz, J = 3.6 3.62 (dd, J = 11.9 Hz, J = 4.0 2.29–2.21 (m, 2H), 1.81–1.69 (m, 2H), 1.55–1.41 (m, 2H), 0.96 (t, J = 7.4 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 155.25, 147.36, 146.65, 137.96, 131.33, 130.31, 119.05, 114.59, 99.12, 97.92, 87.62, 84.87, 70.20, 67.77, 61.12, 40.10, 30.65, 18.61, 13.56. HRMS (ESI) m/z: calcd for C40H40N3O7− [M-H]−: 674.2872; found 674.2856.
2-((2R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-4-hydroxytetrahydrofuran-2-yl)-7-(hexyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 4b
Yield 82%. 1H NMR (600 MHz, DMSO-d6): δ 7.87(d, J = 8.1 Hz, 1H), 7.84 (d, J = 2.5 Hz, 1H), 7.62 (d, J = 8.8 Hz, 1H), 7.08 (dd, J = 8.8 Hz, J = 2.5 Hz, 1H), 6.69 (d, J = 8.1 Hz, 1H), 6.46 (t, J = 6.7 Hz, 1H), 5.30 (br s, 1H), 5.07 (br s, 1H), 4.34–4.30 (m, 1H), 4.03 (t, J = 6.4 Hz, 2H), 3.90–3.86 (m, 1H), 3.66 (dd, J = 11.8 Hz, J = 3.6 3.62 (dd, J = 11.8 Hz, J = 3.8 2.28–2.20 (m, 2H), 1.78–1.72 (m, 2H), 1.48–1.41 (m, 2H), 1.35–1.28 (m, 4H), 0.88 (t, J = 7.0 Hz, 3H). 13C NMR (150 MHz, DMSO-d6): δ 155.25, 147.37, 146.68, 138.05, 131.29, 130.33, 119.09, 114.58, 99.09, 97.98, 87.62, 84.86, 70.22, 68.07, 61.13, 40.11, 30.89, 28.56, 25.07, 21.94, 13.77. HRMS (ESI) m/z: calcd for C42H44N3O7− [M-H]−: 702.3185; found 702.3150.
2-((2R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-4-hydroxytetrahydrofuran-2-yl)-7-(octyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 4c
Yield 73%. 1H NMR (600 MHz, DMSO-d6): δ 7.87(d, J = 8.1 Hz, 1H), 7.84 (d, J = 2.4 Hz, 1H), 7.62 (d, J = 8.8 Hz, 1H), 7.07 (dd, J = 8.8 Hz, J = 2.4 Hz, 1H), 6.69 (d, J = 8.1 Hz, 1H), 6.46 (t, J = 6.7 Hz, 1H), 5.31 (br s, 1H), 5.08 (br s, 1H), 4.33–4.30 (m, 1H), 4.03 (t, J = 6.4 Hz, 2H), 3.89–3.87 (m, 1H), 3.66 (dd, J = 11.8 Hz, J = 3.6 3.62 (dd, J = 11.8 Hz, J = 3.7 2.28–2.19 (m, 2H), 1.78–1.71 (m, 2H), 1.47–1.40 (m, 2H), 1.36–1.21 (m, 8H), 0.86 (t, J = 6.9 Hz, 3H). 13C NMR (150 MHz, DMSO-d6): δ 155.24, 147.37, 146.69, 138.09, 131.26, 130.34, 119.11, 114.57, 99.10, 98.00, 87.62, 84.86, 70.23, 68.06, 61.14, 40.11, 31.10, 28.63, 28.59, 28.53, 25.40, 21.95, 13.80. HRMS (ESI) m/z: calcd for C44H48N3O7− [M-H]−: 730.3498; found 730.3487.
2-((2R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-4-hydroxytetrahydrofuran-2-yl)-7-(decyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 4d
Yield 79%. 1H NMR (300 MHz, DMSO-d6): δ 7.86 (d, J = 8.1 Hz, 1H), 7.84 (dd, J = 2.5 Hz, 1H), 7.61 (d, J = 8.8 Hz, 1H), 7.08 (dd, J = 8.8 Hz, J = 2.5 Hz, 1H), 6.68 (d, J = 8.1 Hz, 1H), 6.46 (t, J = 6.7 Hz, 1H), 4.36–4.29 (m, 1H), 4.04 (t, J = 6.5 Hz, 2H), 3.91–3.86 (m, 1H), 3.67 (dd, J = 11.9 Hz, J = 3.8 3.62 (dd, J = 11.9 Hz, J = 4.0 2.30–2.19 (m, 2H), 1.81–1.69 (m, 2H), 1.50–1.37 (m, 2H), 1.37–1.18 (m, 12H), 0.85 (t, J = 6.7 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 155.24, 147.36, 146.67, 138.06, 131.27, 130.33, 119.08, 114.56, 99.11, 97.98, 87.62, 84.86, 70.22, 68.05, 61.13, 40.11, 31.15, 28.86, 28.81, 28.64, 28.56 (2C), 25.37, 21.94, 13.79. HRMS (ESI) m/z: calcd for C46H52N3O7− [M-H]−: 758.3811; found 758.3777.
2-((2R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-4-hydroxytetrahydrofuran-2-yl)-7-(dodecyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 4e
Yield 88%. 1H NMR (600 MHz, DMSO-d6): δ 7.87 (d, J = 8.0 Hz, 1H), 7.84 (d, J = 2.0 Hz, 1H), 7.62 (d, J = 8.7 Hz, 1H), 7.07 (dd, J = 8.7 Hz, J = 2.0 Hz, 1H), 6.69 (d, J = 8.0 Hz, 1H), 6.46 (t, J = 6.5 Hz, 1H), 5.31 (br s, 1H), 5.08 (br s, 1H), 4.35–4.29 (m, 1H), 4.03 (t, J = 5.9 Hz, 2H), 3.91–3.86 (m, 1H), 3.65 (dd, J = 11.1 Hz, J = 2.9 3.61 (dd, J = 11.9 Hz, J = 3.1 2.29–2.19 (m, 2H), 1.80–1.70 (m, 2H), 1.48–1.39 (m, 2H), 1.37–1.17 (m, 16H), 0.84 (t, J = 6.6 Hz, 3H). 13C NMR (150 MHz, DMSO-d6): δ 155.24, 147.37, 146.69, 138.12, 131.25, 130.35, 119.12, 114.57, 99.11, 98.02, 87.62, 84.85, 70.23, 68.05, 61.14, 40.12, 31.16, 28.90, 28.87, 28.84 (2C), 28.62, 28.57 (2C), 25.37, 21.96, 13.80. HRMS (ESI) m/z: calcd for C48H56N3O7− [M-H]−: 786.4124; found 786.4194.
2-((2R,3R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-3,4-dihydroxytetrahydrofuran-2-yl)-7-butoxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 5a
Yield 69%. 1H NMR (300 MHz, DMSO-d6): δ 7.92 (d, J = 8.1 Hz, 1H), 7.87 (d, J = 2.5 Hz, 1H), 7.64 (d, J = 8.8 Hz, 1H), 7.10 (dd, J = 8.8 Hz, J = 2.5 Hz, 1H), 6.71 (d, J = 8.1 Hz, 1H), 6.10 (d, J = 5.1 Hz, 1H), 4.18 (t, J = 5.2 Hz, 1H), 4.10–4.03 (m, 3H), 3.98–3.94 (m, 1H), 3.72 (dd, J = 12.0 Hz, J = 3.0 3.64 (dd, J = 12.0 Hz, J = 3.3 1.81–1.70 (m, 2H), 1.55–1.42 (m, 2H), 0.96 (t, J = 7.4 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 155.39, 147.36, 146.98, 137.63, 131.78, 130.33, 119.07, 114.78, 99.06, 97.84, 88.55, 85.05, 74.20, 69.74, 67.78, 60.65, 30.71, 18.70, 13.67. HRMS (ESI) m/z: calcd for C40H40N3O8− [M-H]−: 690.2821; found 690.2790.
2-((2R,3R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-3,4-dihydroxytetrahydrofuran-2-yl)-7-(hexyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 5b
Yield 71%. 1H NMR (300 MHz, DMSO-d6): δ 7.91 (d, J = 8.1 Hz, 1H), 7.86 (d, J = 2.4 Hz, 1H), 7.63 (d, J = 8.8 Hz, 1H), 7.09 (dd, J = 8.8 Hz, J = 2.4 Hz, 1H), 6.71 (d, J = 8.1 Hz, 1H), 6.10 (d, J = 5.1 Hz, 1H), 4.17 (t, J = 5.0 Hz, 1H), 4.09–4.01 (m, 3H), 3.97–3.93 (m, 1H), 3.72 (dd, J = 12.2 Hz, J = 3.1 3.63 (dd, J = 12.2 Hz, J = 3.1 1.82–1.70 (m, 2H), 1.51–1.40 (m, 2H), 1.39–1.27 (m, 4H), 0.89 (t, J = 7.0 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 155.33, 147.38, 147.06, 138.10, 131.49, 130.41, 119.24, 114.68, 99.04, 98.06, 88.46, 85.07, 74.17, 69.80, 68.07, 60.70, 30.96, 28.61, 25.14, 22.02, 13.86. HRMS (ESI) m/z: calcd for C42H44N3O8− [M-H]−: 718.3134; found 718.3129.
2-((2R,3R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-3,4-dihydroxytetrahydrofuran-2-yl)-7-(octyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 5c
Yield 78%. 1H NMR (300 MHz, DMSO-d6): δ 7.93 (d, J = 8.1 Hz, 1H), 7.87 (d, J = 2.1 Hz, 1H), 7.64 (d, J = 8.9 Hz, 1H), 7.10 (dd, J = 8.9 Hz, J = 2.1 Hz, 1H), 6.72 (d, J = 8.1 Hz, 1H), 6.10 (d, J = 5.1 Hz, 1H), 4.18 (t, J = 5.2 Hz, 1H), 4.10–4.01 (m, 3H), 3.99–3.93 (m, 1H), 3.72 (dd, J = 11.9 Hz, J = 2.7 3.64 (dd, J = 11.9 Hz, J = 3.0 1.82–1.70 (m, 2H), 1.52–1.38 (m, 2H), 1.37–1.16 (m, 8H), 0.87 (t, J = 6.5 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 155.41, 147.35, 146.95, 137.49, 131.87, 130.30, 119.02, 114.79, 99.07, 97.77, 88.57, 85.06, 74.20, 69.73, 68.08, 60.64, 31.17, 28.70, 28.61 (2C), 25.47, 22.02, 13.90. HRMS (ESI) m/z: calcd for C44H48N3O8− [M-H]−: 746.3447; found 746.3387.
2-((2R,3R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-3,4-dihydroxytetrahydrofuran-2-yl)-7-(decyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 5d
Yield 75%. 1H NMR (300 MHz, DMSO-d6): δ 7.92 (d, J = 8.1 Hz, 1H), 7.86 (d, J = 2.5 Hz, 1H), 7.63 (d, J = 8.9 Hz, 1H), 7.09 (dd, J = 8.9 Hz, J = 2.5 Hz, 1H), 6.71 (d, J = 8.1 Hz, 1H), 6.10 (d, J = 5.1 Hz, 1H), 4.18 (t, J = 5.0 Hz, 1H), 4.10–4.02 (m, 3H), 3.98–3.94 (m, 1H), 3.72 (dd, J = 12.0 Hz, J = 3.0 3.63 (dd, J = 12.0 Hz, J = 3.2 1.81–1.71 (m, 2H), 1.51–1.39 (m, 2H), 1.34–1.21 (m, 12H), 0.85 (t, J = 6.8 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 155.39, 147.35, 146.97, 137.64, 131.77, 130.33, 119.07, 114.75, 99.07, 97.84, 88.54, 85.05, 74.19, 69.74, 68.07, 60.65, 31.22, 28.94, 28.89, 28.72, 28.63 (2C), 25.45, 22.02, 13.88. HRMS (ESI) m/z: calcd for C46H52N3O8− [M-H]−: 774.3760; found 774.3751.
2-((2R,3R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-3,4-dihydroxytetrahydrofuran-2-yl)-7-(dodecyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 5e
Yield 76%. 1H NMR (300 MHz, DMSO-d6): δ 7.90 (d, J = 8.0 Hz, 1H), 7.86 (d, J = 2.4 Hz, 1H), 7.63 (d, J = 9.0 Hz, 1H), 7.09 (dd, J = 8.9 Hz, J = 2.4 Hz, 1H), 6.70 (d, J = 8.0 Hz, 1H), 6.10 (d, J = 4.9 Hz, 1H), 4.17 (t, J = 5.1 Hz, 1H), 4.11–4.00 (m, 3H), 3.98–3.93 (m, 1H), 3.72 (dd, J = 12.0 Hz, J = 3.2 3.63 (dd, J = 12.0 Hz, J = 3.2 1.82–1.69 (m, 2H), 1.52–1.36 (m, 2H), 1.38–1.13 (m, 16H), 0.85 (t, J = 6.5 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 155.36, 147.37, 147.01, 137.85, 131.65, 130.37, 119.15, 114.72, 99.07, 97.95, 88.50, 85.06, 74.18, 69.76, 68.06, 60.67, 31.22, 28.92 (4C), 28.69, 28.63 (2C), 25.43, 22.02, 13.88. HRMS (ESI) m/z: calcd for C48H56N3O8− [M-H]−: 802.4073; found 802.4049.
General procedure for the preparation of 7-O-alkylated non-nucleoside derivatives
Compound 4 (0.07 mmol) was dissolved in a mixture of CH3OH/12 N HCl (5 mL, 1:20, v:v) and kept at 50 °C for 72 h. The reaction mixture was concentrated, and the residue was purified using column chromatography on silica gel (0–5% CH3OH in CH2Cl2), yielding 6a–e as a beige amorphous solid.
7-butoxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 6a
Yield 89%. 1H NMR (300 MHz, DMSO-d6): δ 12.59 (br s, 1H), 7.90 (d, J = 2.4 Hz, 1H), 7.80 (d, J = 7.4 Hz, 1H), 7.72 (d, J = 8.9 Hz, 1H), 7.24 (dd, J = 8.9 Hz, J = 2.4 Hz, 1H), 6.79 (d, J = 7.4 Hz, 1H), 4.08 (t, J = 6.4 Hz, 1H), 1.81–1.70 (m, 2H), 1.55–1.41 (m, 2H), 0.95 (t, J = 7.4 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 156.14, 148.07, 146.03, 138.55, 129.26, 128.75, 116.06, 115.88, 99.53, 93.15, 68.00, 30.50, 18.52, 13.48. HRMS (ESI) m/z: calcd for C14H14N3O2− [M-H]−: 256.1092; found 256.1075.
7-(hexyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 6b
Yield 86%. 1H NMR (300 MHz, DMSO-d6): δ 12.55 (br s, 1H), 7.90 (d, J = 2.4 Hz, 1H), 7.78 (d, J = 7.4 Hz, 1H), 7.72 (d, J = 8.9 Hz, 1H), 7.23 (dd, J = 8.9 Hz, J = 2.4 Hz, 1H), 6.78 (d, J = 7.4 Hz, 1H), 4.07 (t, J = 6.4 Hz, 1H), 1.82–1.71 (m, 2H), 1.51–1.40 (m, 2H), 1.40–1.27 (m, 4H), 0.89 (t, J = 6.9 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 156.13, 148.09, 146.06, 138.49, 129.36, 128.77, 116.05, 115.92, 99.52, 93.20, 68.30, 30.79, 28.39, 24.94, 21.84, 13.68. HRMS (ESI) m/z: calcd for C16H18N3O2− [M-H]−: 284.1405; found 284.1388.
7-(octyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 6c
Yield 94%. 1H NMR (600 MHz, DMSO-d6): δ 12.52 (br s, 1H), 7.89 (d, J = 2.4 Hz, 1H), 7.78 (d, J = 7.4 Hz, 1H), 7.72 (d, J = 8.9 Hz, 1H), 7.23 (dd, J = 8.9 Hz, J = 2.4 Hz, 1H), 6.78 (d, J = 7.4 Hz, 1H), 4.06 (t, J = 6.4 Hz, 1H), 1.79–1.73 (m, 2H), 1.48–1.41 (m, 2H), 1.35–1.23 (m, 8H), 0.86 (t, J = 6.9 Hz, 3H). 13C NMR (150 MHz, DMSO-d6): δ 156.11, 148.15, 146.19, 138.30, 129.73, 128.86, 116.11, 116.03, 99.46, 93.42, 68.28, 31.09, 28.60, 28.51, 28.48, 25.35, 21.93, 13.80. HRMS (ESI) m/z: calcd for C18H22N3O2− [M-H]−: 312.1718; found 312.1701.
7-(decyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 6d
Yield 94%. 1H NMR (300 MHz, DMSO-d6): δ 12.18 (br s, 1H), 7.89 (d, J = 2.4 Hz, 1H), 7.69 (d, J = 8.9 Hz, 1H), 7.66 (d, J = 7.6 Hz, 1H), 7.19 (dd, J = 8.9 Hz, J = 2.4 Hz, 1H), 6.72 (d, J = 7.6 Hz, 1H), 4.07 (t, J = 6.5 Hz, 1H), 1.82–1.71 (m, 2H), 1.51–1.39 (m, 2H), 1.37–1.21 (m, 12H), 0.86 (t, J = 6.8 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 156.04, 148.19, 146.28, 137.81, 130.45, 128.96, 116.35, 115.90, 99.49, 93.71, 68.29, 31.09, 28.79, 28.74, 28.56, 28.48, 28.45, 25.29, 21.89, 13.74. HRMS (ESI) m/z: calcd for C20H26N3O2− [M-H]−: 340.2031; found 340.1987.
7-(dodecyloxy)benzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 6e
Yield 91%. 1H NMR (300 MHz, DMSO-d6): δ 12.58 (br s, 1H), 7.90 (d, J = 1.7 Hz, 1H), 7.82 (d, J = 7.2 Hz, 1H), 7.73 (d, J = 8.9 Hz, 1H), 7.24 (dd, J = 8.9 Hz, J = 1.7 Hz, 1H), 6.81 (d, J = 7.2 Hz, 1H), 4.07 (t, J = 6.3 Hz, 1H), 1.79–1.73 (m, 2H), 1.47–1.41 (m, 2H), 1.35–1.20 (m, 4H), 0.85 (t, J = 6.8 Hz, 3H). 13C NMR (75 MHz, DMSO-d6): δ 219.47, 156.29, 148.15, 146.09, 139.04, 139.00, 128.77, 116.27, 115.85, 99.56, 93.08, 68.34, 31.17, 28.91, 28.88, 28.85, 28.63, 28.58, 28.47, 25.34, 21.97, 13.83. HRMS (ESI) m/z: calcd for C22H30N3O2− [M-H]−: 368.2344; found 368.2339.
General procedure for the preparation of 7-O-methyl 5′-O-DMTr nucleoside derivatives
To a stirred mixture of compound 3 (0.11 mmol), PPh3 (58 mg, 0.22 mmol, 2 equiv) and CH3OH (6 μL, 0.15 mmol, 1.3 equiv) in dry CH2Cl2 (5 mL) DIAD (43 μL, 0.22 mmol, 2 equiv) was added at 0 °C. The reaction mixture was stirred at RT overnight and concentrated under reduced pressure. The residue was purified using column chromatography on silica gel (0–1% CH3OH in CH2Cl2 with 0.1% TEA), yielding 7a,b as a yellowish amorphous solid.
2-((2R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-4-hydroxytetrahydrofuran-2-yl)-7-methoxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 7a
Yield 83%. 1H NMR (600 MHz, DMSO-d6): δ 7.86 (d, J = 2.5 Hz, 1H), 7.65 (d, J = 8.0 Hz, 1H), 7.64 (d, J = 8.8 Hz, 1H), 7.42–7.39 (m, 2H), 7.33–7.21 (m, 7H), 7.10 (dd, J = 8.8 Hz, J = 2.5 Hz, 1H), 6.91–6.87 (m, 4H), 6.45 (t, J = 6.4 Hz, 1H), 6.42 (d, J = 8.0 Hz, 1H), 5.43 (br s, 1H), 4.41–4.36 (m, 1H), 3.99–3.96 (m, 1H), 3.85 (s, 3H), 3.72 (s, 3H), 3.72 (s, 3H), 3.31 (dd, J = 10.4 Hz, J = 4.9 Hz, 1H), 3.27 (dd, J = 10.4 Hz, J = 3.0 Hz, 1H), 2.39–2.30 (m 2H). 13C NMR (150 MHz, DMSO-d6): δ 158.00 (2C), 155.90, 147.27, 146.58, 144.57, 138.20, 135.34, 135.15, 131.16, 130.38, 129.65 (4C), 127.75 (2C), 127.63 (2C), 126.63, 119.19, 114.16, 113.11 (4C), 98.36, 97.79, 85.74, 85.54, 84.98, 69.74, 63.21, 55.54, 54.90 (2C), 39.94. HRMS (ESI) m/z: calcd for C37H34N3O7− [M-H]−: 632.2402; found 632.2157.
2-((2R,3R,4S,5R)-5-((bis(4-methoxyphenyl)(phenyl)methoxy)methyl)-3,4-dihydroxytetrahydrofuran-2-yl)-7-methoxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 7b
Yield 80%. 1H NMR (600 MHz, DMSO-d6): δ 7.87 (d, J = 2.5 Hz, 1H), 7.74 (d, J = 8.0 Hz, 1H), 7.65 (d, J = 8.8 Hz, 1H), 7.44–7.41 (m, 2H), 7.35–7.23 (m, 7H), 7.11 (dd, J = 8.8 Hz, J = 2.5 Hz, 1H), 6.93–6.89 (m, 4H), 6.34 (d, J = 8.0 Hz, 1H), 6.07 (d, J = 3.5 Hz, 1H), 5.60 (d, J = 4.6 Hz, 1H), 5.22 (d, J = 5.7 Hz, 1H), 4.27–4.23 (m, 1H), 4.24–4.20 (m, 1H), 4.09–4.06 (m, 1H), 3.85 (s, 3H), 3.74 (s, 6H), 3.37–3.31 (m, 2H). 13C NMR (150 MHz, DMSO-d6): δ 158.05 (2C), 155.94, 147.23, 146.73, 144.56, 138.17, 135.31, 135.08, 132.96, 132.28, 129.69 (4C), 127.80 (2C), 127.65 (2C), 126.69, 119.22, 114.20, 113.16 (4C), 98.35, 97.65, 89.72, 85.84, 82.53, 73.89, 69.38, 62.69, 55.53, 54.93, 54.76. HRMS (ESI) m/z: calcd for C37H34N3O8− [M-H]−: 648.2351; found 648.2302.
General procedure for the preparation of 7-O-methyl nucleoside derivatives
Compound 7 (0.6 mmol) was dissolved in a mixture of CH3COOH/H2O (2 mL, 1:9, v:v) and kept at 50 °C for 8 h. After concentration and co-evaporation with toluene (3 × 10 mL), the residue was purified using column chromatography on silica gel (0–6% CH3OH in CH2Cl2), yielding 8a,b as a beige amorphous solid.
2-((2R,4S,5R)-4-hydroxy-5-(hydroxymethyl)tetrahydrofuran-2-yl)-7-methoxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 8a
Yield 91%. 1H NMR (300 MHz, DMSO-d6): δ 7.88 (s, 1H), 7.85 (d, J = 2.4 Hz, 1H), 7.63 (d, J = 8.8 Hz, 1H), 7.08 (dd, J = 8.8 Hz, J = 2.4 Hz, 1H), 6.70 (d, J = 8.0 Hz, 1H), 6.46 (t, J = 6.4 Hz, 1H), 5.35 (d, J = 3.6 Hz, 1H), 5.13 (t, J = 4.6 Hz, 1H), 4.36–4.27 (m, 1H), 3.91–3.83 (m, 1H), 3.84 (s, 3H), 3.70–3.57 (m, 2H), 2.30–2.18 (m, 2H). 13C NMR (75 MHz, DMSO-d6): δ 155.90, 147.49, 146.78, 138.24, 131.35, 130.43, 119.26, 114.23, 98.35, 98.13, 87.68, 84.92, 70.29, 61.19, 55.58, 40.26. HRMS (ESI) m/z: calcd for C16H16N3O5− [M-H]−: 330.1095; found 330.1074.
2-((2R,3R,4S,5R)-3,4-dihydroxy-5-(hydroxymethyl)tetrahydrofuran-2-yl)-7-methoxybenzo[4,5]imidazo[1,2-c]pyrimidin-1(2H)-one 8b
Yield 92%. 1H NMR (300 MHz, DMSO-d6): δ 7.93 (d, J = 7.9 Hz, 1H), 7.86 (s, 1H), 7.65 (d, J = 7.9 Hz, 1H), 7.10 (d, J = 7.9 Hz, 1H), 6.72 (d, J = 7.9 Hz, 1H), 6.10 (d, J = 4.1 Hz, 1H), 5.50 (d, J = 4.6 Hz, 1H), 5.23 (t, J = 4.2 Hz, 1H), 5.19 (d, J = 4.0 Hz, 1H), 4.22–4.10 (m, 1H), 4.11–4.06 (m, 1H), 3.99–3.89 (m, 1H), 3.85 (s, 3H), 3.76–3.57 (m, 2H). 13C NMR (75 MHz, DMSO-d6): δ 155.94, 147.44, 147.08, 138.22, 131.50, 130.45, 119.30, 114.25, 98.33, 98.10, 88.50, 85.08, 74.22, 69.80, 60.70, 55.57. HRMS (ESI) m/z: calcd for C16H16N3O6− [M-H]−: 346.1045; found 346.1012.
3.2. Biology
3.2.1. Cells and Viruses
Human embryonic lung fibroblasts (HEL299), human hepatoma (Huh7), green monkey kidney (Vero), and Madin-Darby canine kidney (MDCK) cell lines were obtained from the American Type Culture Collection (ATCC). Viruses and strains used in the present work, with the exception of SARS-CoV-2 strains, as well as the specific cell type for each virus, are specified in Table S1.
A variant of SARS-CoV-2, designated UC-1074, was isolated in Vero cells in 2020 from a nasopharyngeal swab of a COVID-19 patient who had a Ct of 19 from the detection of SARS-CoV-2 E protein using RT-qPCR. UC-1074 has a genome sequence matching the early A lineage (Wuhan/WH04/2020). The following four strains were kindly provided by Piet Maes (Laboratory of Clinical and Epidemiological Virology, Rega Institute, KU Leuven, Belgium): NVDBB-2220 (Alpha variant), RG-2674 (Beta variant), 860-J1 (Delta variant), and B1.1.529 BA.1 (Omicron). All studies on SARS-CoV-2 were conducted in the BSL3 facilities of the KU Leuven Rega Institute (3CAPS) under licenses AMV 30112018 SBB 219 2018 0892 and AMV 23102017 SBB 219 2017 0589 according to institutional guidelines.
3.2.2. Methods
Cell Toxicity Evaluation in HEL299, Vero, Huh7 and MDCK Cells
Cells were seeded at a rate of 5 × 103 cells/well into 96-well plates and allowed to proliferate for 24 h. Then, a medium containing different concentrations of the test compounds, starting at 100 mM, was added. After 3 days of incubation at 37 °C, the cell count was determined with a Beckman Coulter counter or, alternatively, cell viability was determined with the colorimetric formazan-based MTS assay. The compound concentration required to reduce cell growth by 50% (CC50) was estimated from graphical plots of the number of cells (percentage of control) as a function of the concentration of the test compounds. The cytotoxic effects of the compounds were also assessed by evaluating the MCC (minimum cytotoxic concentration that causes a microscopically detectable alteration of cell morphology).
Cytopathicity or Plaque Reduction Test
Confluent cell cultures in microtiter 96-well plates were inoculated with 100 CCID50 of virus (1 CCID50 being the virus dose to infect 50% of the cell cultures) or with 20 or 100 plaque-forming units (PFU) for VZV and HCMV, respectively. Following a 2 h adsorption period, viral inoculum was removed and the cell cultures were incubated in the presence of varying concentrations of the test compounds. Viral cytopathicity, or plaque formation, was recorded as soon as it reached completion in the control virus-infected cell cultures that were not treated with the test compounds. Antiviral activity was expressed as EC50 (the compound concentration required to reduce virus-induced cytopathicity or viral plaque formation by 50%).
3.3. Biochemical Assays
3.3.1. RdRp and Reagents
SARS-CoV-2 RdRp containing the catalytic subunit nsp12 and fused nsp7-nsp8 subunits (separated by a His6-tag) was expressed in Escherichia coli BL-21(DE3) and purified using Ni-affinity and HiTrap Q HP columns as described previously [41]. RNA oligonucleotides for in vitro reactions were synthesized and purified by DNA Synthesis (Moscow, Russia). All reagents for protein purification and in vitro experiments were from Sigma-Aldrich (St. Louis, MO, USA) unless otherwise specified. The inhibitors were diluted in DMSO (VWR International LLC, Radnor, PA, USA) and stored at −20 °C.
3.3.2. In Vitro Transcription Assay
The primer RNA oligonucleotide was 5′-labeled with γ-[32P]-ATP by T4 polynucleotide kinase (NEB, Ipswich, MA, USA). The RNA substrate was prepared by annealing the labeled primer with the template RNA oligonucleotide as described previously [41]. To test the effects of the studied compounds on RdRp activity, RdRp (1 µM) was incubated with increasing concentrations of the inhibitors (1–10,000 μM, or the same volume of DMSO in control samples) in a reaction buffer (10 mM Tris-HCl, pH 7.9, 10 mM KCl, 2 mM MgCl2, and 1 mM DTT) for 10 min at 30 °C. Then, the RNA substrate (25 nM) was added and the samples were incubated for 10 min at 30 °C. RNA synthesis was initiated by adding 100 µM of all 4 NTPs (Thermo Fisher Scientific, Waltham, MA, USA) and was quenched after 10 min with a 1.2 volume of the stop solution containing 95% formamide, 10 mM EDTA, heparin 100 μg/mL. The samples were heated at 98 °C for 3 min. The reaction products were separated by 15% denaturing PAGE (acrylamide:bisacrylaimde 19:1, 8 M urea) and visualized by phosphor imaging using a Typhoon 9500 scanner (GE Healthcare, Chicago, IL, USA). The efficiency of primer extension was calculated in every sample and normalized to activity in the absence of the inhibitors. The data were fitted to the hyperbolic equation A = Amax × (1 − [Inhibitor]/(IC50 + [Inhibitor])), where A is the efficiency of the RNA extension at a given concentration of the inhibitor and Amax is the maximal activity, using GraFit software version 4 (Erithacus). All experiments were independently reproduced 3 times.
3.3.3. LLPS Assays
Recombinant SARS-CoV-2 N-protein with His-tag, obtained as described previously [27] (purity: ≥90%), was a kind gift of the group of Prof. V. N. Lazarev. The protein was labeled with a far-red-emitting RED dye using the RED-NHS 2nd Generation Protein Labeling Kit (Nanotemper, Munich, Germany). The stem-loop fragment of SARS-CoV-2 gRNA (SL5 in [43]) was obtained by in vitro transcription from the T7-promoter-containing dsDNA template according to the published procedure [27].
- Template sense strand:
- TAATACGACTCACTATAGGGAGAACTAATTACTGTCGTTGACAGGACACGAGTAACTCGTCTATCTTCTGCAGGCTGCTTACGGTTTCGTCCGTGTTGCAGCCGATCATCAGCACATCTAGGTTTCGTCCGGGTGTGACCGAAAGGTAAGATGGAGAGCCTTGTCCCTGGTTTCAACGACAGTAATTAGT
The labeled N-protein (3 µM final concentration) was mixed with RNA (6 µM final concentration) in the RNAse-free 20 mM sodium phosphate buffer (pH 6) supplemented with 150 mM NaCl. Compound 3a/3b/7a/9a was added to a final concentration of 20 µM. The mixture was incubated at 37 °C for 2 h. Then, 3 μL of the mixture was placed between glass slides and analyzed using a Nikon Eclipse Ti2 microscope (Nikon, Tokyo, Japan) in the red channel. All experiments were performed in 6 repeats. Droplets were counted in ImageJ software, version 1.53a, and the partitioning coefficient (PC = [N-protein]droplet/[N-protein]solution) was calculated based on the average fluorescence intensity values in droplets and bulk solution.
4. Conclusions
Using the reaction between cytosine and 1,4-benzoquinone to assemble a tricyclic heteroaromatic backbone, a set of nucleoside and non-nucleoside derivatives substituted at the 7-hydroxyl position with alkyl groups of varying length was obtained and then tested for their ability to inhibit the replication of a wide range of DNA and RNA viruses. Among the synthesized compounds, only 5′-O-DMTr-substituted intermediates (3a and 3b) showed micromolar to submicromolar activity against human coronavirus and respiratory syncytial virus without any noticeable cytotoxicity for the host cells (HEL299) (Table 1). Then, a few analogs of 3a,b were synthesized, among which derivatives 7a,b which additionally contained a methyl group at the seventh position of the heteroaromatic scaffold exhibited micromolar anti-VZV activity, with SI being more than 30 for 7a (Table 2). Finally, 3a,b and their analogs were tested against various SARS-CoV-2 strains, with 3a showing an EC50 of about 10 μM against all strains, however, with a moderate effect on Vero cell morphology. Since 3a belongs to nucleoside analogs, which often exhibit their activity by the inhibition of viral polymerases, we tested its ability to inhibit SARS-CoV-2 RdRp in vitro. The compound was a transcription inhibitor with an IC50 value of 94 ± 3 μM, which, however, was one order of magnitude higher than the EC50 value for the same compound, suggesting RdRp may not be the primary target. One possible additional pathway, namely interference with the replication-promoting biocondensate assembly, was verified for 3a and its structurally related inactive analogs in LLPS assays. Of all tested compounds, only 3a decreased condensate formation in a dose-dependent manner with EC50 ≤ 10 µM. The results confirm the promise and pave the way for further development of LLPS inhibitors as antiviral compounds.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms241914540/s1.
Author Contributions
Conceptualization, A.A.; methodology, R.S., A.K., A.V., G.A. and A.A.; investigation, P.K., I.P., E.K., Y.K., E.R., V.A., A.E.-S., E.B., J.S. and T.V.; writing—original draft preparation, P.K., I.P., A.V. and A.A.; writing—review and editing, P.K., A.K., A.V. and A.A.; visualization, P.K., I.P., A.V. and A.A.; funding acquisition, A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Russian Science Foundation (grant 22-25-00161).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in the article and Supplementary Materials.
Acknowledgments
We thank V.A. Manuvera and the Center for Precision Genome Editing and Genetic Technologies for Biomedicine and the Lopukhin Federal Research and Clinical Center of Physical-Chemical Medicine of Federal Medical Biological Agency for the recombinant SARS-CoV2 protein expression and purification. The authors are also in debt to Leentje Perssons and Brecht Dirix for excellent assistance in performing the antiviral assays.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chowell, G.; Echevarría-Zuno, S.; Viboud, C.; Simonsen, L.; Tamerius, J.; Miller, M.A.; Borja-Aburto, V.H. Characterizing the Epidemiology of the 2009 Influenza A/H1N1 Pandemic in Mexico. PLoS Med. 2011, 8, e1000436. [Google Scholar] [CrossRef] [PubMed]
- Cenciarelli, O.; Pietropaoli, S.; Malizia, A.; Carestia, M.; D’Amico, F.; Sassolini, A.; Di Giovanni, D.; Rea, S.; Gabbarini, V.; Tamburrini, A.; et al. Ebola Virus Disease 2013-2014 Outbreak in West Africa: An Analysis of the Epidemic Spread and Response. Int. J. Microbiol. 2015, 2015, 769121. [Google Scholar] [CrossRef] [PubMed]
- Mackay, I.M.; Arden, K.E. MERS Coronavirus: Diagnostics, Epidemiology and Transmission. Virol. J. 2015, 12, 222. [Google Scholar] [CrossRef] [PubMed]
- Walsh, D.; Mohr, I. Viral Subversion of the Host Protein Synthesis Machinery. Nat. Rev. Microbiol. 2011, 9, 860–875. [Google Scholar] [CrossRef] [PubMed]
- Mercorelli, B.; Palù, G.; Loregian, A. Drug Repurposing for Viral Infectious Diseases: How Far Are We? Trends Microbiol. 2018, 26, 865–876. [Google Scholar] [CrossRef] [PubMed]
- Hadj Hassine, I.; Ben M’hadheb, M.; Menéndez-Arias, L. Lethal Mutagenesis of RNA Viruses and Approved Drugs with Antiviral Mutagenic Activity. Viruses 2022, 14, 841. [Google Scholar] [CrossRef]
- Thames, J.E.; Seley-Radtke, K.L. Comparison of the Old and New—Novel Mechanisms of Action for Anti-Coronavirus Nucleoside Analogues. Chimia 2022, 76, 409. [Google Scholar] [CrossRef]
- Zenchenko, A.A.; Drenichev, M.S.; Il’icheva, I.A.; Mikhailov, S.N. Antiviral and Antimicrobial Nucleoside Derivatives: Structural Features and Mechanisms of Action. Mol. Biol. 2021, 55, 786–812. [Google Scholar] [CrossRef]
- Ramdhan, P.; Li, C. Targeting Viral Methyltransferases: An Approach to Antiviral Treatment for SsRNA Viruses. Viruses 2022, 14, 379. [Google Scholar] [CrossRef]
- Takizawa, N.; Takada, H.; Umekita, M.; Igarashi, M.; Takahashi, Y. Anti-Influenza Virus Activity of Methylthio-Formycin Distinct From That of T-705. Front. Microbiol. 2022, 13, 802671. [Google Scholar] [CrossRef]
- Geraghty, R.; Aliota, M.; Bonnac, L. Broad-Spectrum Antiviral Strategies and Nucleoside Analogues. Viruses 2021, 13, 667. [Google Scholar] [CrossRef]
- Jordheim, L.P.; Durantel, D.; Zoulim, F.; Dumontet, C. Advances in the Development of Nucleoside and Nucleotide Analogues for Cancer and Viral Diseases. Nat. Rev. Drug Discov. 2013, 12, 447–464. [Google Scholar] [CrossRef] [PubMed]
- Nijhuis, M.; Van Maarseveen, N.M.; Boucher, C.A.B. Antiviral Resistance and Impact on Viral Replication Capacity: Evolution of Viruses Under Antiviral Pressure Occurs in Three Phases. In Antiviral Strategies; Kräusslich, H.-G., Bartenschlager, R., Eds.; Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2009; Volume 189, pp. 299–320. ISBN 978-3-540-79085-3. [Google Scholar]
- Seley-Radtke, K.L.; Yates, M.K. The Evolution of Nucleoside Analogue Antivirals: A Review for Chemists and Non-Chemists. Part 1: Early Structural Modifications to the Nucleoside Scaffold. Antivir. Res. 2018, 154, 66–86. [Google Scholar] [CrossRef] [PubMed]
- Yates, M.K.; Seley-Radtke, K.L. The Evolution of Antiviral Nucleoside Analogues: A Review for Chemists and Non-Chemists. Part II: Complex Modifications to the Nucleoside Scaffold. Antivir. Res. 2019, 162, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Cho, A.; Saunders, O.L.; Butler, T.; Zhang, L.; Xu, J.; Vela, J.E.; Feng, J.Y.; Ray, A.S.; Kim, C.U. Synthesis and Antiviral Activity of a Series of 1′-Substituted 4-Aza-7,9-Dideazaadenosine C-Nucleosides. Bioorg. Med. Chem. Lett. 2012, 22, 2705–2707. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Amblard, F.; Zhang, H.; McBrayer, T.R.; Detorio, M.A.; Whitaker, T.; Coats, S.J.; Schinazi, R.F. Synthesis and Evaluation of Janus Type Nucleosides as Potential HCV NS5B Polymerase Inhibitors. Bioorg. Med. Chem. Lett. 2013, 23, 3385–3388. [Google Scholar] [CrossRef]
- Chudinov, M.V. Nucleoside Analogs with Fleximer Nucleobase. Chem. Heterocycl. Compd. 2020, 56, 636–643. [Google Scholar] [CrossRef]
- Thames, J.E.; Waters, C.D.; Valle, C.; Bassetto, M.; Aouadi, W.; Martin, B.; Selisko, B.; Falat, A.; Coutard, B.; Brancale, A.; et al. Synthesis and Biological Evaluation of Novel Flexible Nucleoside Analogues That Inhibit Flavivirus Replication in Vitro. Bioorg. Med. Chem. 2020, 28, 115713. [Google Scholar] [CrossRef] [PubMed]
- Jahnz-Wechmann, Z.; Framski, G.R.; Januszczyk, P.A.; Boryski, J. Base-Modified Nucleosides: Etheno Derivatives. Front. Chem. 2016, 4, 19. [Google Scholar] [CrossRef] [PubMed]
- Jahnz-Wechmann, Z.; Framski, G.; Januszczyk, P.; Boryski, J. Bioactive Fused Heterocycles: Nucleoside Analogs with an Additional Ring. Eur. J. Med. Chem. 2015, 97, 388–396. [Google Scholar] [CrossRef]
- Kozlovskaya, L.I.; Andrei, G.; Orlov, A.A.; Khvatov, E.V.; Koruchekov, A.A.; Belyaev, E.S.; Nikolaev, E.N.; Korshun, V.A.; Snoeck, R.; Osolodkin, D.I.; et al. Antiviral Activity Spectrum of Phenoxazine Nucleoside Derivatives. Antivir. Res. 2019, 163, 117–124. [Google Scholar] [CrossRef] [PubMed]
- McGuigan, C.; Brancale, A.; Andrei, G.; Snoeck, R.; De Clercq, E.; Balzarini, J. Novel Bicyclic Furanopyrimidines with Dual Anti-VZV and -HCMV Activity. Bioorg. Med. Chem. Lett. 2003, 13, 4511–4513. [Google Scholar] [CrossRef] [PubMed]
- McGuigan, C.; Barucki, H.; Blewett, S.; Carangio, A.; Erichsen, J.T.; Andrei, G.; Snoeck, R.; De Clercq, E.; Balzarini, J. Highly Potent and Selective Inhibition of Varicella-Zoster Virus by Bicyclic Furopyrimidine Nucleosides Bearing an Aryl Side Chain. J. Med. Chem. 2000, 43, 4993–4997. [Google Scholar] [CrossRef] [PubMed]
- De Clercq, E. FV-100 for the Treatment of Varicella-Virus (VZV) Infections: Quo Vadis? Viruses 2022, 14, 770. [Google Scholar] [CrossRef] [PubMed]
- Matyugina, E.; Petushkov, I.; Surzhikov, S.; Kezin, V.; Maslova, A.; Ivanova, O.; Smirnova, O.; Kirillov, I.; Fedyakina, I.; Kulbachinskiy, A.; et al. Nucleoside Analogs That Inhibit SARS-CoV-2 Replication by Blocking Interaction of Virus Polymerase with RNA. Int. J. Mol. Sci. 2023, 24, 3361. [Google Scholar] [CrossRef]
- Svetlova, J.; Knizhnik, E.; Manuvera, V.; Severov, V.; Shirokov, D.; Grafskaia, E.; Bobrovsky, P.; Matyugina, E.; Khandazhinskaya, A.; Kozlovskaya, L.; et al. Nucleoside Analogs and Perylene Derivatives Modulate Phase Separation of SARS-CoV-2 N Protein and Genomic RNA In Vitro. Int. J. Mol. Sci. 2022, 23, 15281. [Google Scholar] [CrossRef]
- Cascarina, S.M.; Ross, E.D. Phase Separation by the SARS-CoV-2 Nucleocapsid Protein: Consensus and Open Questions. J. Biol. Chem. 2022, 298, 101677. [Google Scholar] [CrossRef]
- Yang, S.; Shen, W.; Hu, J.; Cai, S.; Zhang, C.; Jin, S.; Guan, X.; Wu, J.; Wu, Y.; Cui, J. Molecular Mechanisms and Cellular Functions of Liquid-Liquid Phase Separation during Antiviral Immune Responses. Front. Immunol. 2023, 14, 1162211. [Google Scholar] [CrossRef]
- Wei, W.; Bai, L.; Yan, B.; Meng, W.; Wang, H.; Zhai, J.; Si, F.; Zheng, C. When Liquid-Liquid Phase Separation Meets Viral Infections. Front. Immunol. 2022, 13, 985622. [Google Scholar] [CrossRef]
- Banani, S.F.; Lee, H.O.; Hyman, A.A.; Rosen, M.K. Biomolecular Condensates: Organizers of Cellular Biochemistry. Nat. Rev. Mol. Cell Biol. 2017, 18, 285–298. [Google Scholar] [CrossRef]
- Di Nunzio, F.; Uversky, V.N.; Mouland, A.J. Biomolecular Condensates: Insights into Early and Late Steps of the HIV-1 Replication Cycle. Retrovirology 2023, 20, 4. [Google Scholar] [CrossRef]
- Svetlova, Y.I.; Pavlova, Y.I.; Aralov, A.V.; Varizhuk, A.M. Condensates of SARS-CoV-2 Nucleoprotein on Viral RNA and Their Small Molecule Modulators (A Review). Russ. J. Bioorganic Chem. 2023, 49, 917–929. [Google Scholar] [CrossRef]
- Dang, M.; Li, Y.; Song, J. ATP Biphasically Modulates LLPS of SARS-CoV-2 Nucleocapsid Protein and Specifically Binds Its RNA-Binding Domain. Biochem. Biophys. Res. Commun. 2021, 541, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Yu, Y.; Sun, L.-M.; Xing, J.-Q.; Li, T.; Zhu, Y.; Wang, M.; Yu, Y.; Xue, W.; Xia, T.; et al. GCG Inhibits SARS-CoV-2 Replication by Disrupting the Liquid Phase Condensation of Its Nucleocapsid Protein. Nat. Commun. 2021, 12, 2114. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Xu, W.; Zhang, X.; Wang, X.; Ge, Y.; Yuan, E.; Xiong, Y.; Wu, S.; Li, S.; Wu, N.; et al. Understanding the Phase Separation Characteristics of Nucleocapsid Protein Provides a New Therapeutic Opportunity against SARS-CoV-2. Protein Cell 2021, 12, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Chenna, A.; Singer, B. Large Scale Synthesis of P-Benzoquinone-2′-Deoxycytidine and p-Benzoquinone-2′-Deoxyadenosine Adducts and Their Site-Specific Incorporation into DNA Oligodeoxyribonucleotides. Chem. Res. Toxicol. 1995, 8, 865–874. [Google Scholar] [CrossRef]
- De Burghgraeve, T.; Selisko, B.; Kaptein, S.; Chatelain, G.; Leyssen, P.; Debing, Y.; Jacobs, M.; Van Aerschot, A.; Canard, B.; Neyts, J. 3′,5′Di-O-Trityluridine Inhibits in Vitro Flavivirus Replication. Antivir. Res. 2013, 98, 242–247. [Google Scholar] [CrossRef]
- McGuigan, C.; Serpi, M.; Slusarczyk, M.; Ferrari, V.; Pertusati, F.; Meneghesso, S.; Derudas, M.; Farleigh, L.; Zanetta, P.; Bugert, J. Anti-Flavivirus Activity of Different Tritylated Pyrimidine and Purine Nucleoside Analogues. ChemistryOpen 2016, 5, 227–235. [Google Scholar] [CrossRef]
- De Farias, S.T.; Dos Santos Junior, A.P.; Rêgo, T.G.; José, M.V. Origin and Evolution of RNA-Dependent RNA Polymerase. Front. Genet. 2017, 8, 125. [Google Scholar] [CrossRef]
- Petushkov, I.; Esyunina, D.; Kulbachinskiy, A. Effects of Natural RNA Modifications on the Activity of SARS-CoV-2 RNA-dependent RNA Polymerase. FEBS J. 2023, 290, 80–92. [Google Scholar] [CrossRef]
- Savastano, A.; Ibáñez De Opakua, A.; Rankovic, M.; Zweckstetter, M. Nucleocapsid Protein of SARS-CoV-2 Phase Separates into RNA-Rich Polymerase-Containing Condensates. Nat. Commun. 2020, 11, 6041. [Google Scholar] [CrossRef] [PubMed]
- Roden, C.A.; Dai, Y.; Giannetti, C.A.; Seim, I.; Lee, M.; Sealfon, R.; McLaughlin, G.A.; Boerneke, M.A.; Iserman, C.; Wey, S.A.; et al. Double-Stranded RNA Drives SARS-CoV-2 Nucleocapsid Protein to Undergo Phase Separation at Specific Temperatures. Nucleic Acids Res. 2022, 50, 8168–8192. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).