Infection and Persistence of Coxiella burnetii Clinical Isolate in the Placental Environment
Abstract
1. Introduction
2. Results
2.1. Comparative Genomic Analyses of Placental C. burnetii Isolates
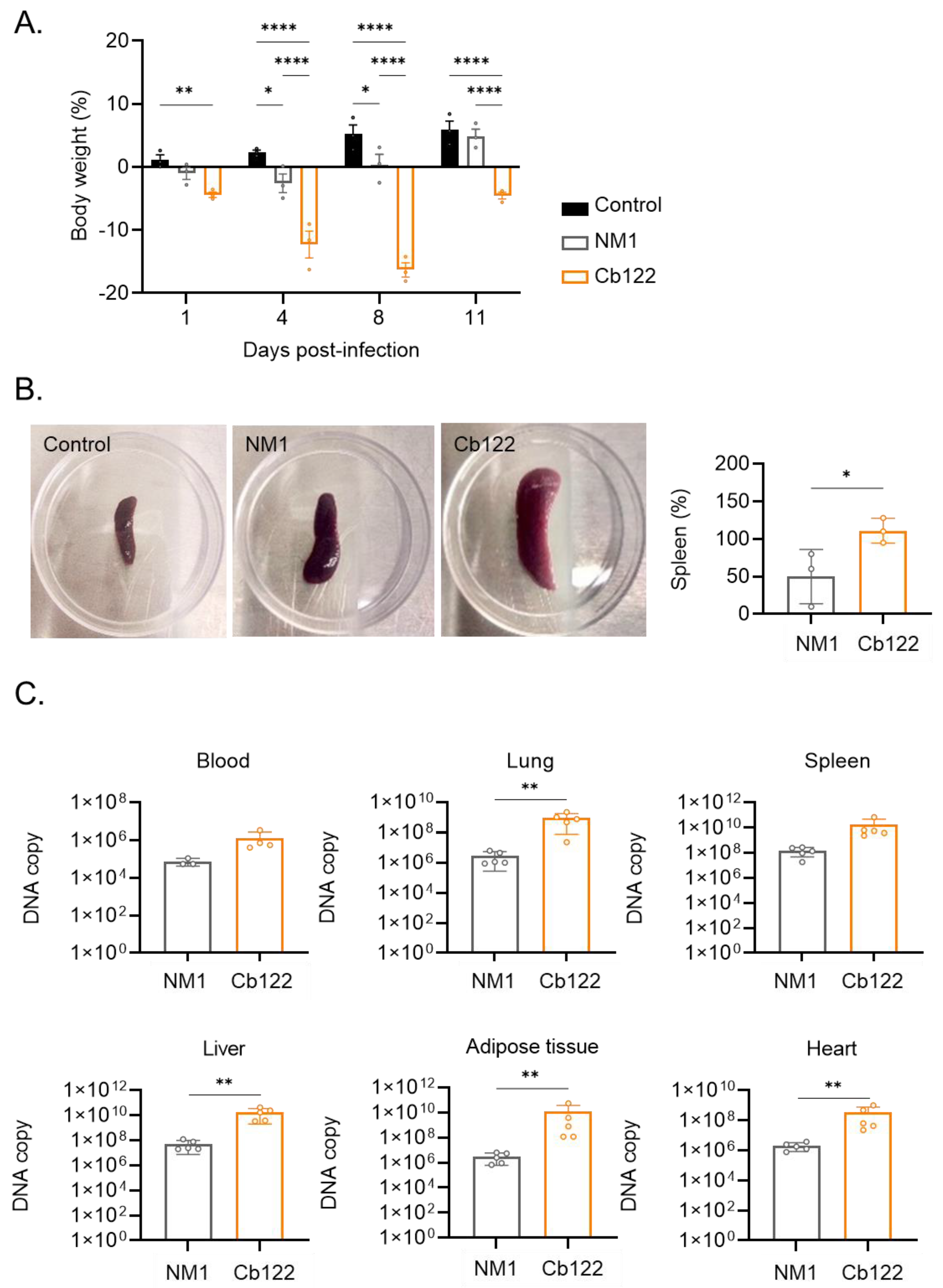
2.2. C. burnetii Placental Isolate Virulence
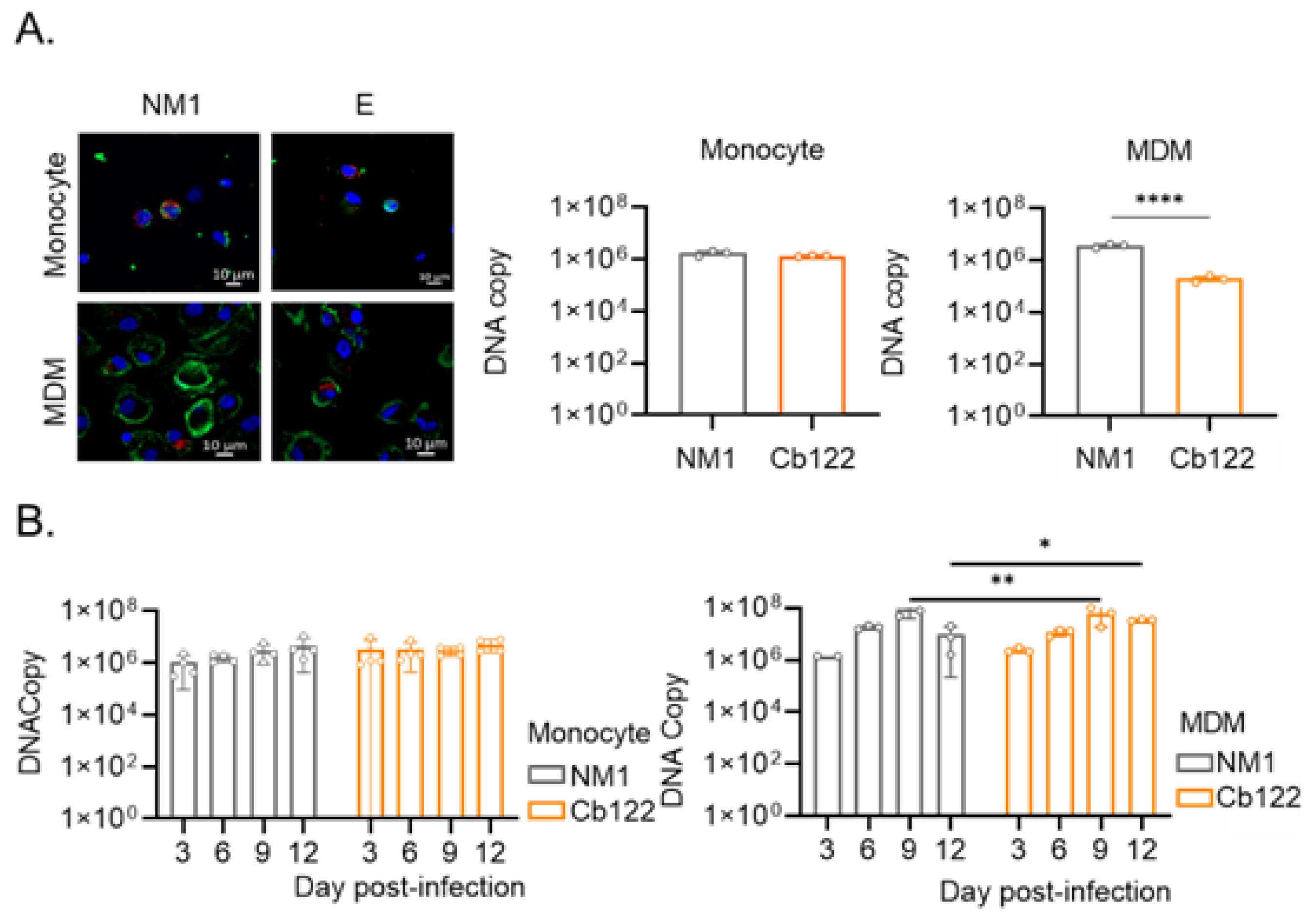
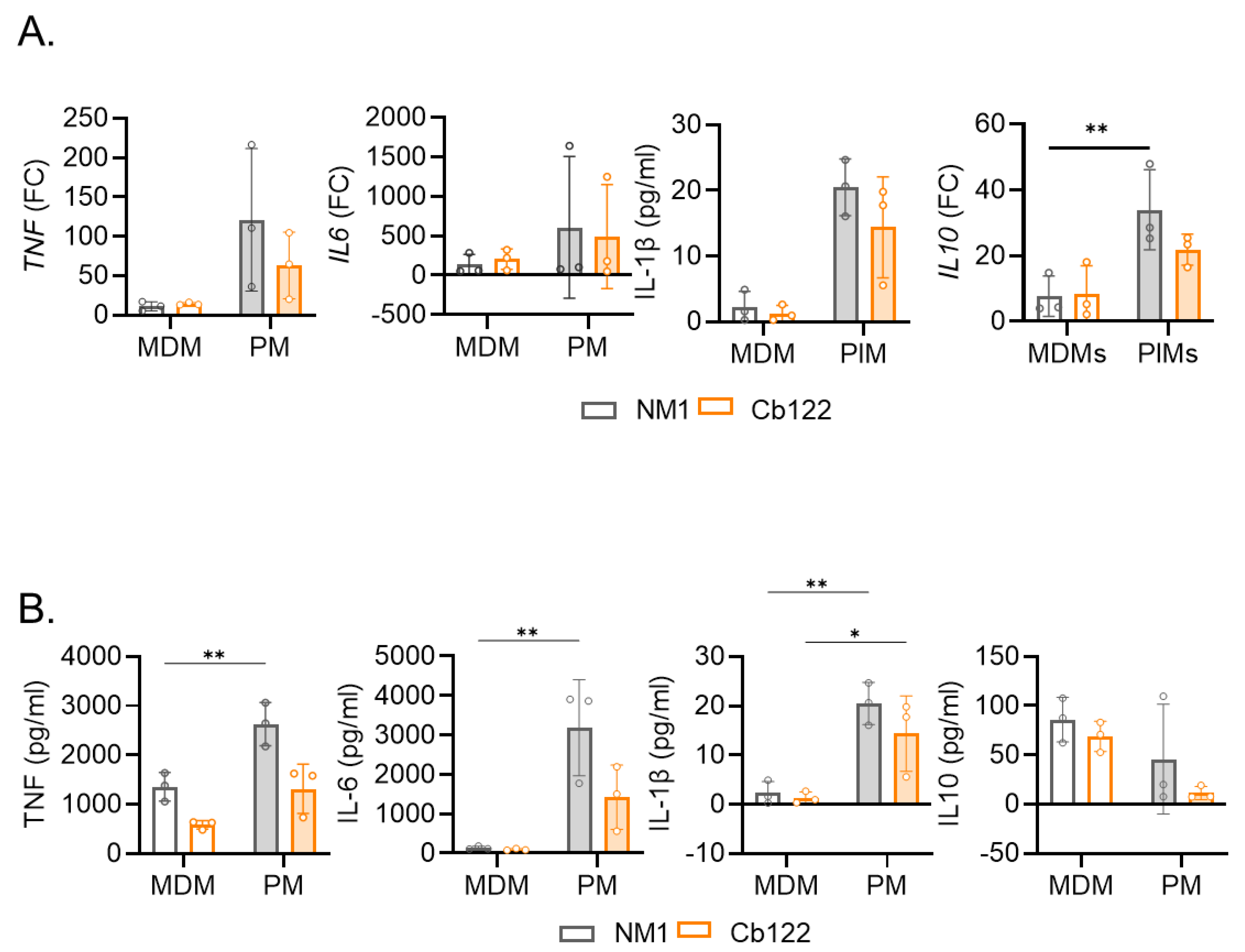
2.3. Macrophage Response to Placental C. burnetii Isolate
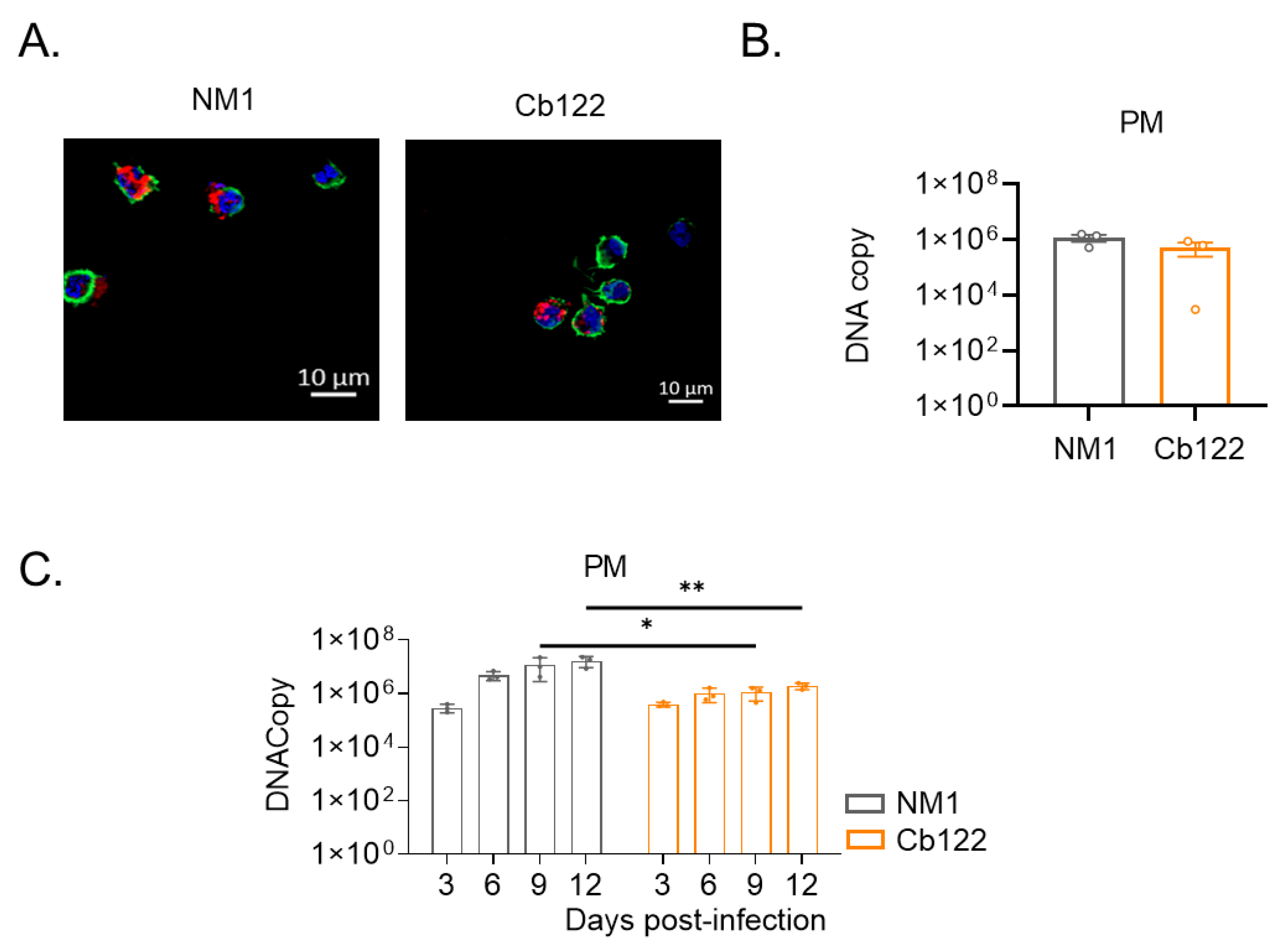
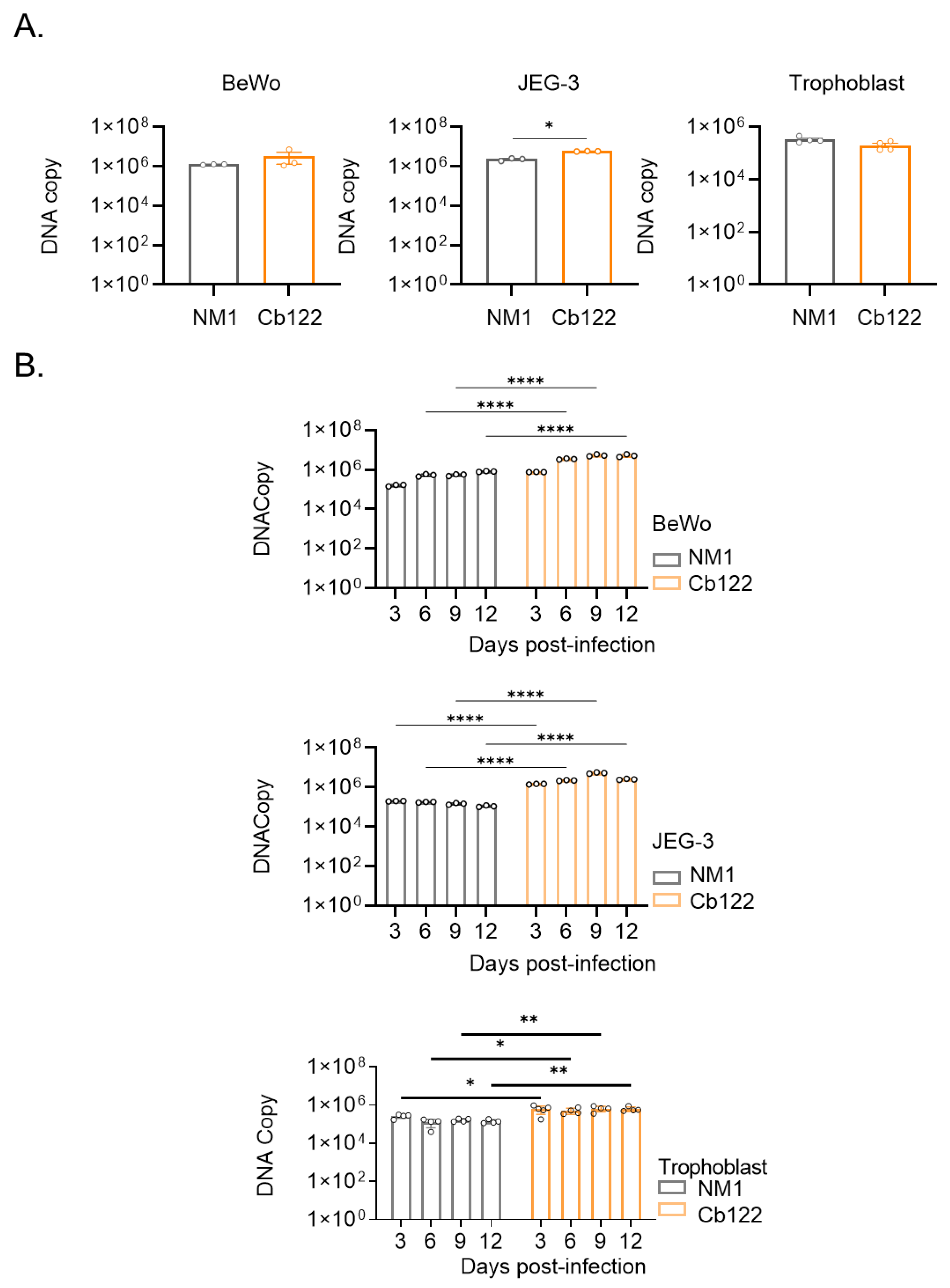
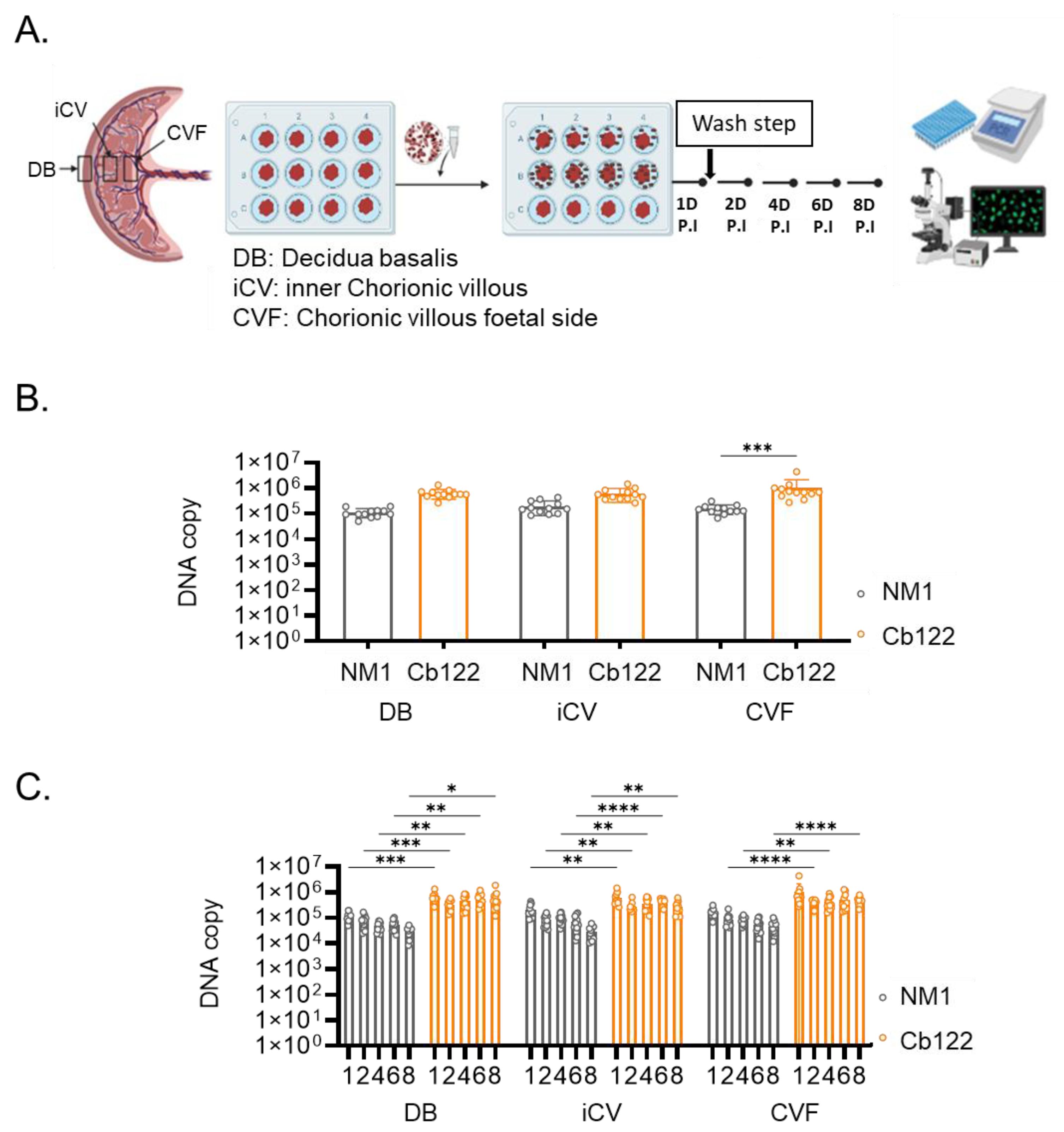
2.4. Placental C. burnetii Isolate Specificity for Placental Tissue
3. Discussion
4. Materials and Methods
4.1. Ethics Statement
4.2. Placenta Collection and Primary Cell Cultures
4.3. C. burnetii Isolation and Cell Infection
4.4. Inflammatory Cytokine Response of Myeloid Cells
4.5. C. burnetii Infection of Placental Explants
4.6. In Vivo Experiments
4.7. Bacteria Quantification
4.8. Genome Sequencing, Comparative Analyses and Phylogeny
4.9. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Raoult, D.; Marrie, T.; Mege, J. Natural History and Pathophysiology of Q Fever. Lancet Infect. Dis. 2005, 5, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Zarza, S.M.; Mezouar, S.; Mege, J.-L. From Coxiella Burnetii Infection to Pregnancy Complications: Key Role of the Immune Response of Placental Cells. Pathogens 2021, 10, 627. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.Y.; Andersen, A.-M.N.; Mølbak, K.; Hjøllund, N.H.; Kantsø, B.; Krogfelt, K.A.; Henriksen, T.B. No Excess Risk of Adverse Pregnancy Outcomes among Women with Serological Markers of Previous Infection with Coxiella Burnetii: Evidence from the Danish National Birth Cohort. BMC Infect. Dis. 2013, 13, 87. [Google Scholar] [CrossRef] [PubMed]
- Eldin, C.; Mélenotte, C.; Mediannikov, O.; Ghigo, E.; Million, M.; Edouard, S.; Mege, J.-L.; Maurin, M.; Raoult, D. From Q Fever to Coxiella Burnetii Infection: A Paradigm Change. Clin. Microbiol. Rev. 2017, 30, 115–190. [Google Scholar] [CrossRef] [PubMed]
- de Lange, M.M.A.; Hukkelhoven, C.W.P.M.; Munster, J.M.; Schneeberger, P.M.; van der Hoek, W. Nationwide Registry-Based Ecological Analysis of Q Fever Incidence and Pregnancy Outcome during an Outbreak in the Netherlands. BMJ Open 2015, 5, e006821. [Google Scholar] [CrossRef]
- Raoult, D.; Fenollar, F.; Stein, A. Q Fever During Pregnancy: Diagnosis, Treatment, and Follow-Up. Arch. Intern. Med. 2002, 162, 701. [Google Scholar] [CrossRef]
- Million, M.; Roblot, F.; Carles, D.; D’Amato, F.; Protopopescu, C.; Carrieri, M.P.; Raoult, D. Reevaluation of the Risk of Fetal Death and Malformation after Q Fever. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2014, 59, 256–260. [Google Scholar] [CrossRef]
- Angelakis, E.; Million, M.; D’Amato, F.; Rouli, L.; Richet, H.; Stein, A.; Rolain, J.-M.; Raoult, D. Q Fever and Pregnancy: Disease, Prevention, and Strain Specificity. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2013, 32, 361–368. [Google Scholar] [CrossRef]
- Carcopino, X.; Raoult, D.; Bretelle, F.; Boubli, L.; Stein, A. Q Fever during Pregnancy: A Cause of Poor Fetal and Maternal Outcome. Ann. N. Y. Acad. Sci. 2009, 1166, 79–89. [Google Scholar] [CrossRef]
- Téllez, A.; Sanz Moreno, J.; Valkova, D.; Domingo, C.; Anda, P.; de Ory, F.; Albarrán, F.; Raoult, D. Q Fever in Pregnancy: Case Report after a 2-Year Follow-Up. J. Infect. 1998, 37, 79–81. [Google Scholar] [CrossRef]
- Russell-Lodrigue, K.E.; Andoh, M.; Poels, M.W.J.; Shive, H.R.; Weeks, B.R.; Zhang, G.Q.; Tersteeg, C.; Masegi, T.; Hotta, A.; Yamaguchi, T.; et al. Coxiella Burnetii Isolates Cause Genogroup-Specific Virulence in Mouse and Guinea Pig Models of Acute Q Fever. Infect. Immun. 2009, 77, 5640–5650. [Google Scholar] [CrossRef] [PubMed]
- Tissot-Dupont, H.; Raoult, D. Q Fever. Infect. Dis. Clin. N. Am. 2008, 22, 505–514, ix. [Google Scholar] [CrossRef] [PubMed]
- Rodolakis, A. Q Fever in Dairy Animals. Ann. N. Y. Acad. Sci. 2009, 1166, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Berri, M.; Rousset, E.; Champion, J.L.; Russo, P.; Rodolakis, A. Goats May Experience Reproductive Failures and Shed Coxiella Burnetii at Two Successive Parturitions after a Q Fever Infection. Res. Vet. Sci. 2007, 83, 47–52. [Google Scholar] [CrossRef]
- Astobiza, I.; Barandika, J.F.; Juste, R.A.; Hurtado, A.; García-Pérez, A.L. Evaluation of the Efficacy of Oxytetracycline Treatment Followed by Vaccination against Q Fever in a Highly Infected Sheep Flock. Vet. J. 2013, 196, 81–85. [Google Scholar] [CrossRef]
- Ben Amara, A.; Ghigo, E.; Le Priol, Y.; Lépolard, C.; Salcedo, S.P.; Lemichez, E.; Bretelle, F.; Capo, C.; Mege, J.-L. Coxiella Burnetii, the Agent of Q Fever, Replicates within Trophoblasts and Induces a Unique Transcriptional Response. PLoS ONE 2010, 5, e15315. [Google Scholar] [CrossRef]
- Howard, Z.P.; Omsland, A. Selective Inhibition of Coxiella Burnetii Replication by the Steroid Hormone Progesterone. Infect. Immun. 2020, 88, e00894-19. [Google Scholar] [CrossRef]
- Gay, L.; Melenotte, C.; Lopez, A.; Desnues, B.; Raoult, D.; Leone, M.; Mezouar, S.; Mege, J.-L. Impact of Sex Hormones on Macrophage Responses to Coxiella Burnetii. Front. Immunol. 2021, 12, 705088. [Google Scholar] [CrossRef]
- Gay, L.; Melenotte, C.; Lakbar, I.; Mezouar, S.; Devaux, C.; Raoult, D.; Bendiane, M.-K.; Leone, M.; Mège, J.-L. Sexual Dimorphism and Gender in Infectious Diseases. Front. Immunol. 2021, 12, 698121. [Google Scholar] [CrossRef]
- Amara, A.B.; Bechah, Y.; Mege, J.-L. Immune Response and Coxiella Burnetii Invasion. Adv. Exp. Med. Biol. 2012, 984, 287–298. [Google Scholar] [CrossRef]
- Mezouar, S.; Ben Amara, A.; Chartier, C.; Gorvel, L.; Mege, J.-L. A Fast and Reliable Method to Isolate Human Placental Macrophages. Curr. Protoc. Immunol. 2019, 125, e77. [Google Scholar] [CrossRef] [PubMed]
- Mezouar, S.; Benammar, I.; Boumaza, A.; Diallo, A.B.; Chartier, C.; Buffat, C.; Boudjarane, J.; Halfon, P.; Katsogiannou, M.; Mege, J.-L. Full-Term Human Placental Macrophages Eliminate Coxiella Burnetii Through an IFN-γ Autocrine Loop. Front. Microbiol. 2019, 10, 2434. [Google Scholar] [CrossRef] [PubMed]
- Marchler-Bauer, A.; Bo, Y.; Han, L.; He, J.; Lanczycki, C.J.; Lu, S.; Chitsaz, F.; Derbyshire, M.K.; Geer, R.C.; Gonzales, N.R.; et al. CDD/SPARCLE: Functional Classification of Proteins via Subfamily Domain Architectures. Nucleic Acids Res. 2017, 45, D200–D203. [Google Scholar] [CrossRef] [PubMed]
- Kelley, L.A.; Mezulis, S.; Yates, C.M.; Wass, M.N.; Sternberg, M.J.E. The Phyre2 Web Portal for Protein Modeling, Prediction and Analysis. Nat. Protoc. 2015, 10, 845–858. [Google Scholar] [CrossRef] [PubMed]
- Melenotte, C.; Lepidi, H.; Nappez, C.; Bechah, Y.; Audoly, G.; Terras, J.; Raoult, D.; Brégeon, F. Mouse Model of Coxiella Burnetii Aerosolization. Infect. Immun. 2016, 84, 2116–2123. [Google Scholar] [CrossRef]
- Mezouar, S.; Lepidi, H.; Omar Osman, I.; Gorvel, J.-P.; Raoult, D.; Mege, J.-L.; Bechah, Y. T-Bet Controls Susceptibility of Mice to Coxiella Burnetii Infection. Front. Microbiol. 2020, 11, 1546. [Google Scholar] [CrossRef]
- Capo, C.; Lindberg, F.P.; Meconi, S.; Zaffran, Y.; Tardei, G.; Brown, E.J.; Raoult, D.; Mege, J.-L. Subversion of Monocyte Functions by Coxiella Burnetii: Impairment of the Cross-Talk Between Avβ3 Integrin and CR3. J. Immunol. 1999, 163, 6078–6085. [Google Scholar] [CrossRef]
- Howe, D.; Shannon, J.G.; Winfree, S.; Dorward, D.W.; Heinzen, R.A. Coxiella Burnetii Phase I and II Variants Replicate with Similar Kinetics in Degradative Phagolysosome-Like Compartments of Human Macrophages. Infect. Immun. 2010, 78, 3465–3474. [Google Scholar] [CrossRef]
- Ghanem-Zoubi, N.; Paul, M. Q Fever during Pregnancy: A Narrative Review. Clin. Microbiol. Infect. 2020, 26, 864–870. [Google Scholar] [CrossRef]
- Chauhan, J.S.; Mishra, N.K.; Raghava, G.P. Identification of ATP Binding Residues of a Protein from Its Primary Sequence. BMC Bioinform. 2009, 10, 434. [Google Scholar] [CrossRef]
- D’Amato, F.; Eldin, C.; Georgiades, K.; Edouard, S.; Delerce, J.; Labas, N.; Raoult, D. Loss of TSS1 in Hypervirulent Coxiella Burnetii 175, the Causative Agent of Q Fever in French Guiana. Comp. Immunol. Microbiol. Infect. Dis. 2015, 41, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Sobotta, K.; Hillarius, K.; Jiménez, P.H.; Kerner, K.; Heydel, C.; Menge, C. Interaction of Coxiella Burnetii Strains of Different Sources and Genotypes with Bovine and Human Monocyte-Derived Macrophages. Front. Cell. Infect. Microbiol. 2018, 7, 543. [Google Scholar] [CrossRef] [PubMed]
- Dragan, A.L.; Voth, D.E. Coxiella Burnetii: International Pathogen of Mystery. Microbes Infect. 2020, 22, 100–110. [Google Scholar] [CrossRef] [PubMed]
- Roest, H.-J.; van Gelderen, B.; Dinkla, A.; Frangoulidis, D.; van Zijderveld, F.; Rebel, J.; van Keulen, L. Q Fever in Pregnant Goats: Pathogenesis and Excretion of Coxiella Burnetii. PLoS ONE 2012, 7, e48949. [Google Scholar] [CrossRef] [PubMed]
- Capo, C.; Moynault, A.; Collette, Y.; Olive, D.; Brown, E.J.; Raoult, D.; Mege, J.-L. Coxiella Burnetii Avoids Macrophage Phagocytosis by Interfering with Spatial Distribution of Complement Receptor 3. J. Immunol. Baltim. Md 1950 2003, 170, 4217–4225. [Google Scholar] [CrossRef]
- Ghigo, E.; Capo, C.; Raoult, D.; Mege, J.-L. Interleukin-10 Stimulates Coxiella Burnetii Replication in Human Monocytes through Tumor Necrosis Factor Down-Modulation: Role in Microbicidal Defect of Q Fever. Infect. Immun. 2001, 69, 2345–2352. [Google Scholar] [CrossRef]
- Benoit, M.; Barbarat, B.; Bernard, A.; Olive, D.; Mege, J.-L. Coxiella Burnetii, the Agent of Q Fever, Stimulates an Atypical M2 Activation Program in Human Macrophages. Eur. J. Immunol. 2008, 38, 1065–1070. [Google Scholar] [CrossRef]
- Graham, J.G.; MacDonald, L.J.; Hussain, S.K.; Sharma, U.M.; Kurten, R.C.; Voth, D.E. Virulent Coxiella Burnetii Pathotypes Productively Infect Primary Human Alveolar Macrophages: Coxiella Infection of Alveolar Macrophages. Cell. Microbiol. 2013, 15, 1012–1025. [Google Scholar] [CrossRef]
- Ding, J.; Yang, C.; Zhang, Y.; Wang, J.; Zhang, S.; Guo, D.; Yin, T.; Yang, J. M2 Macrophage-derived G-CSF Promotes Trophoblasts EMT, Invasion and Migration via Activating PI3K/Akt/Erk1/2 Pathway to Mediate Normal Pregnancy. J. Cell. Mol. Med. 2021, 25, 2136–2147. [Google Scholar] [CrossRef]
- Yang, F.; Zheng, Q.; Jin, L. Dynamic Function and Composition Changes of Immune Cells During Normal and Pathological Pregnancy at the Maternal-Fetal Interface. Front. Immunol. 2019, 10, 2317. [Google Scholar] [CrossRef]
- Fahmi, A.; Brügger, M.; Démoulins, T.; Zumkehr, B.; Oliveira Esteves, B.I.; Bracher, L.; Wotzkow, C.; Blank, F.; Thiel, V.; Baud, D.; et al. SARS-CoV-2 Can Infect and Propagate in Human Placenta Explants. Cell Rep. Med. 2021, 2, 100456. [Google Scholar] [CrossRef] [PubMed]
- Platt, D.J.; Smith, A.M.; Arora, N.; Diamond, M.S.; Coyne, C.B.; Miner, J.J. Zika Virus–Related Neurotropic Flaviviruses Infect Human Placental Explants and Cause Fetal Demise in Mice. Sci. Transl. Med. 2018, 10, eaao7090. [Google Scholar] [CrossRef] [PubMed]
- Pereira, L.; Tabata, T.; Petitt, M.; Fang-Hoover, J. Congenital Cytomegalovirus Infection Undermines Early Development and Functions of the Human Placenta. Placenta 2017, 59, S8–S16. [Google Scholar] [CrossRef] [PubMed]
- Melenotte, C.; Gay, L.; Mezouar, S.; Bardin, N.; Raoult, D.; Mège, J.-L. The Sexual Dimorphism of Anticardiolipin Autoantibodies in Acute Q Fever Patients. Clin. Microbiol. Infect. 2019, 25, 763.e1–763.e3. [Google Scholar] [CrossRef]
- Kersh, G.J.; Wolfe, T.M.; Fitzpatrick, K.A.; Candee, A.J.; Oliver, L.D.; Patterson, N.E.; Self, J.S.; Priestley, R.A.; Loftis, A.D.; Massung, R.F. Presence of Coxiella Burnetii DNA in the Environment of the United States, 2006 to 2008. Appl. Environ. Microbiol. 2010, 76, 4469–4475. [Google Scholar] [CrossRef]
- Diop, A.; Khelaifia, S.; Armstrong, N.; Labas, N.; Fournier, P.-E.; Raoult, D.; Million, M. Microbial Culturomics Unravels the Halophilic Microbiota Repertoire of Table Salt: Description of Gracilibacillus Massiliensis sp. Nov. Microb. Ecol. Health Dis. 2016, 27, 32049. [Google Scholar] [CrossRef]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A New Genome Assembly Algorithm and Its Applications to Single-Cell Sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A Flexible Trimmer for Illumina Sequence Data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef]
- Seemann, T. Prokka: Rapid Prokaryotic Genome Annotation. Bioinform. Oxf. Engl. 2014, 30, 2068–2069. [Google Scholar] [CrossRef]
- Page, A.J.; Cummins, C.A.; Hunt, M.; Wong, V.K.; Reuter, S.; Holden, M.T.G.; Fookes, M.; Falush, D.; Keane, J.A.; Parkhill, J. Roary: Rapid Large-Scale Prokaryote Pan Genome Analysis. Bioinformatics 2015, 31, 3691–3693. [Google Scholar] [CrossRef]
- Price, M.N.; Dehal, P.S.; Arkin, A.P. FastTree 2—Approximately Maximum-Likelihood Trees for Large Alignments. PLoS ONE 2010, 5, e9490. [Google Scholar] [CrossRef] [PubMed]

| Name | Genome Size (bp) | Elements | Genes (Number) | |||
|---|---|---|---|---|---|---|
| Core | Accessory | Unique | Missed | |||
| Cb48 | 2,000,491 | 2012 | 1379 | 1974 | 38 | 1429 |
| Cb51 | 2,035,629 | 1960 | 1379 | 1939 | 21 | 1481 |
| Cb87 | 2,029,231 | 1950 | 1379 | 1930 | 20 | 1491 |
| Cb93 | 2,048,785 | 1975 | 1379 | 1882 | 93 | 1466 |
| Cb122 | 1,999,784 | 1997 | 1379 | 1953 | 44 | 1444 |
| Cb175 | 1,995,488 | 2384 | 1379 | 2016 | 368 | 1057 |
| NL3262 | 1,995,457 | 2200 | 1379 | 1947 | 253 | 1241 |
| RSA493 | 2,093,477 | 2003 | 1379 | 1962 | 41 | 1438 |
| Z3055 | 1,989,565 | 2042 | 1379 | 1981 | 61 | 1399 |
| C. burnetii | Source (Species) | Isolation (Country/Year) | MST |
|---|---|---|---|
| Cb48 | human placenta | France/2012 | 20 |
| Cb51 | human placenta | Spain/2012 | 4 |
| Cb87 | human placenta | France/2012 | 1 |
| Cb93 | human placenta | France/2012 | 8 |
| Cb122 | human placenta | France/2012 | 22 |
| Nine Mile RSA493 (NMI) | Tick | USA/1935 | 16 |
| Gene | Forward Primer (5′-3′) | Reverse Primer (5′-3′) |
|---|---|---|
| ACTB | GGAAATCGTGCGTGACATTA | AGGAAGGAAGGCTGGAAGAG |
| TNF | AGGAGAAGAGGCTGAGGAACAAG | GAGGGAGAGAAGCAACTACAGACC |
| IL1B | CAGCACCTCTCAAGCAGAAAAC | GTTGGGCATTGGTGTAGACAAC |
| IL10 | GGGGGTTGAGGTATCAGAGGTAA | GCTCCAAGAGAAAGGCATCTACA |
| IL6 | CCAGGAGAAGATTCCAAAGATG | GGAAGGTTCAGGTTGTTTTCTG |
| Gene | Forward Primer (5′-3′) | Reverse Primer (5′-3′) |
|---|---|---|
| Com-1 | GCACTATTTTTAGCCG-GAACCTT | TTGAGGAGAAAAACTGGATTGAGA |
| C. burnetii 16S | ACGGGTGAGTAATGCGTAGG | GCTGATCGTCCTCTCA-GACC |
| Probes | 6-FAMGCAAAGCGGGGGATCTTCGG-TAMR | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zarza, S.M.; Militello, M.; Gay, L.; Levasseur, A.; Lepidi, H.; Bechah, Y.; Mezouar, S.; Mege, J.-L. Infection and Persistence of Coxiella burnetii Clinical Isolate in the Placental Environment. Int. J. Mol. Sci. 2023, 24, 1209. https://doi.org/10.3390/ijms24021209
Zarza SM, Militello M, Gay L, Levasseur A, Lepidi H, Bechah Y, Mezouar S, Mege J-L. Infection and Persistence of Coxiella burnetii Clinical Isolate in the Placental Environment. International Journal of Molecular Sciences. 2023; 24(2):1209. https://doi.org/10.3390/ijms24021209
Chicago/Turabian StyleZarza, Sandra Madariaga, Muriel Militello, Laetitia Gay, Anthony Levasseur, Hubert Lepidi, Yassina Bechah, Soraya Mezouar, and Jean-Louis Mege. 2023. "Infection and Persistence of Coxiella burnetii Clinical Isolate in the Placental Environment" International Journal of Molecular Sciences 24, no. 2: 1209. https://doi.org/10.3390/ijms24021209
APA StyleZarza, S. M., Militello, M., Gay, L., Levasseur, A., Lepidi, H., Bechah, Y., Mezouar, S., & Mege, J.-L. (2023). Infection and Persistence of Coxiella burnetii Clinical Isolate in the Placental Environment. International Journal of Molecular Sciences, 24(2), 1209. https://doi.org/10.3390/ijms24021209






