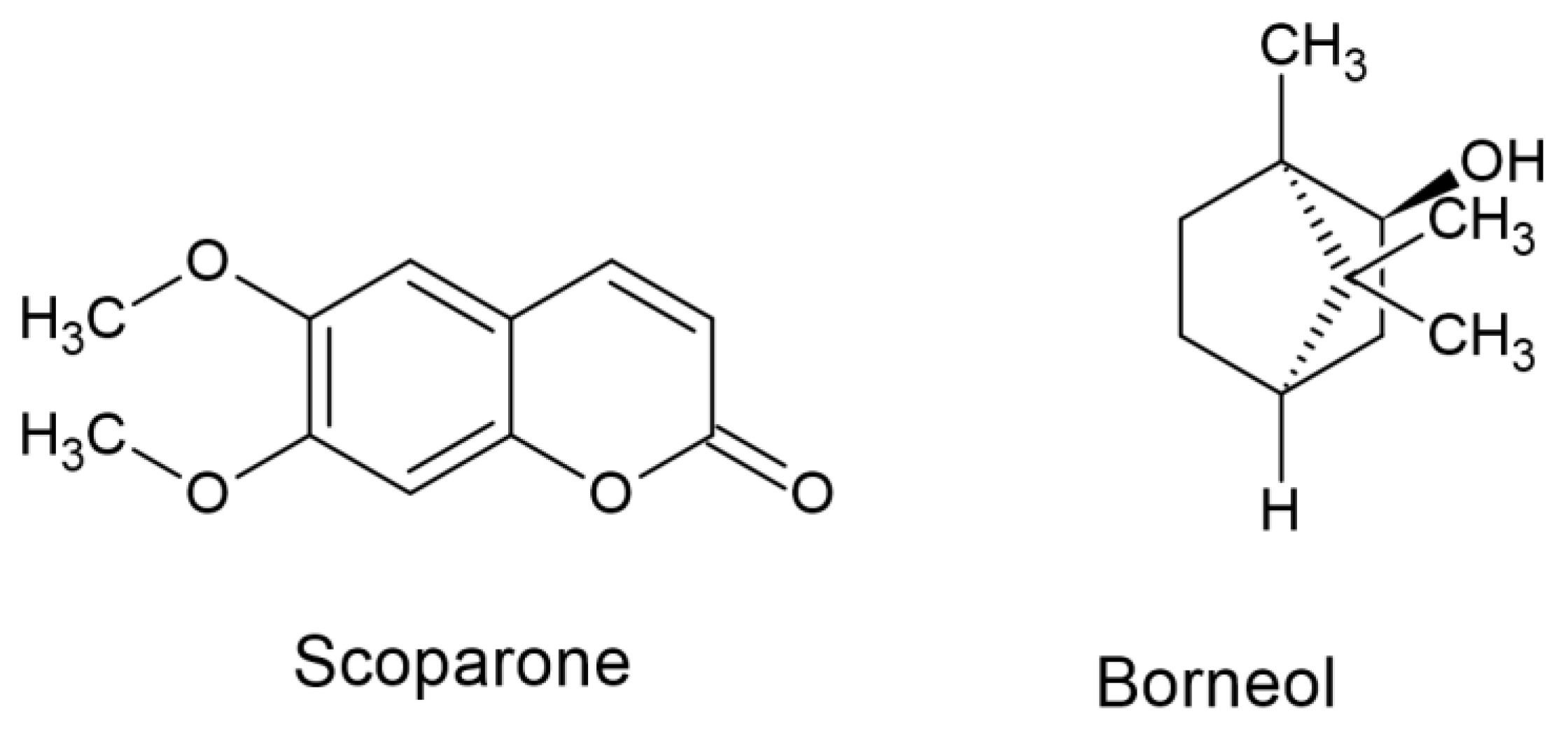
Antiseizure Effects of Scoparone, Borneol and Their Impact on the Anticonvulsant Potency of Four Classic Antiseizure Medications in the Mouse MES Model—An Isobolographic Transformation
Abstract
:1. Introduction
2. Results
2.1. Time Course of the Anticonvulsant Effects of Scoparone and Borneol in the Mouse MES Model
2.2. Effects of Scoparone and Borneol on the Anticonvulsant Potency of Four Classic Antiseizure Medications in the Mouse MES Model
2.3. Isobolographic Analysis of Two-Drug Interaction between Scoparone, Borneol and Four Classic Antiseizure Medications in the Mouse MES Model
2.4. Isobolographic Analysis of Interaction for Three-Drug Mixture Containing Scoparone, Borneol and Four Classic Antiseizure Medications in the Mouse MES Model
2.5. Measurement of Total Brain Concentrations of Phenobarbital and Valproate for the Three-Drug Mixture in Mice
3. Discussion
4. Materials and Methods
4.1. Experimental Animals
4.2. Drugs
4.3. Electrically Evoked Tonic-Clonic Seizures in Animals
4.4. Isobolographic Transformation of Data
4.5. Measurement of Total Brain ASM Concentrations
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Birhan, Y.S. Medicinal Plants Utilized in the Management of Epilepsy in Ethiopia: Ethnobotany, Pharmacology and Phytochemistry. Chin. Med. 2022, 17, 129. [Google Scholar] [CrossRef] [PubMed]
- Perucca, E.; Brodie, M.J.; Kwan, P.; Tomson, T. 30 Years of Second-Generation Antiseizure Medications: Impact and Future Perspectives. Lancet. Neurol. 2020, 19, 544–556. [Google Scholar] [CrossRef] [PubMed]
- Hitiris, N.; Mohanraj, R.; Norrie, J.; Sills, G.J.; Brodie, M.J. Predictors of Pharmacoresistant Epilepsy. Epilepsy Res. 2007, 75, 192–196. [Google Scholar] [CrossRef]
- Ahmad, N.; Hui-Yin, Y.; Makmor-Bakry, M. Mechanisms of Natural Products as Potential Antiepileptic Drugs. Pak. J. Pharm. Sci. 2022, 35, 1043–1053. [Google Scholar] [PubMed]
- Auditeau, E.; Chassagne, F.; Bourdy, G.; Bounlu, M.; Jost, J.; Luna, J.; Ratsimbazafy, V.; Preux, P.M.; Boumediene, F. Herbal medicine for epilepsy seizures in Asia, Africa and Latin America: A systematic review. J. Ethnopharmacol. 2019, 234, 119–153. [Google Scholar] [CrossRef]
- Pattnaik, F.; Nanda, S.; Mohanty, S.; Dalai, A.K.; Kumar, V.; Ponnusamy, S.K.; Naik, S. Cannabis: Chemistry, Extraction and Therapeutic Applications. Chemosphere 2022, 289, 133012. [Google Scholar] [CrossRef]
- Shi, M.-M.; Piao, J.-H.; Xu, X.-L.; Zhu, L.; Yang, L.; Lin, F.-L.; Chen, J.; Jiang, J.-G. Chinese Medicines with Sedative-Hypnotic Effects and Their Active Components. Sleep Med. Rev. 2016, 29, 108–118. [Google Scholar] [CrossRef]
- Thakur, M.; Vasudeva, N.; Sharma, S.; Datusalia, A.K. Plants and Their Bioactive Compounds as a Possible Treatment for Traumatic Brain Injury-Induced Multi-Organ Dysfunction Syndrome. CNS Neurol. Disord. Drug Targets 2022. [Google Scholar] [CrossRef]
- Löscher, W. Animal Models of Seizures and Epilepsy: Past, Present, and Future Role for the Discovery of Antiseizure Drugs. Neurochem. Res. 2017, 42, 1873–1888. [Google Scholar] [CrossRef]
- Łuszczki, J.J.; Wojda, E.; Andres-Mach, M.; Cisowski, W.; Glensk, M.; Głowniak, K.; Czuczwar, S.J. Anticonvulsant and Acute Neurotoxic Effects of Imperatorin, Osthole and Valproate in the Maximal Electroshock Seizure and Chimney Tests in Mice: A Comparative Study. Epilepsy Res. 2009, 85, 293–299. [Google Scholar] [CrossRef]
- Łuszczki, J.J.; Andres-Mach, M.; Gleńsk, M.; Skalicka-Woźniak, K. Anticonvulsant Effects of Four Linear Furanocoumarins, Bergapten, Imperatorin, Oxypeucedanin, and Xanthotoxin, in the Mouse Maximal Electroshock-Induced Seizure Model: A Comparative Study. Pharmacol. Rep. 2010, 62, 1231–1236. [Google Scholar] [CrossRef] [PubMed]
- Zagaja, M.; Andres-Mach, M.; Skalicka-Woźniak, K.; Rękas, A.R.; Kondrat-Wróbel, M.W.; Gleńsk, M.; Łuszczki, J.J. Assessment of the Combined Treatment with Umbelliferone and Four Classical Antiepileptic Drugs Against Maximal Electroshock-Induced Seizures in Mice. Pharmacology 2015, 96, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Łuszczki, J.J.; Głowniak, K.; Czuczwar, S.J. Imperatorin Enhances the Protective Activity of Conventional Antiepileptic Drugs against Maximal Electroshock-Induced Seizures in Mice. Eur. J. Pharmacol. 2007, 574, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Zagaja, M.; Pyrka, D.; Skalicka-Wozniak, K.; Głowniak, K.; Florek-Luszczki, M.; Glensk, M.; Łuszczki, J.J. Effect of Xanthotoxin (8-Methoxypsoralen) on the Anticonvulsant Activity of Classical Antiepileptic Drugs against Maximal Electroshock-Induced Seizures in Mice. Fitoterapia 2015, 105, 1–6. [Google Scholar] [CrossRef]
- Łuszczki, J.J.; Rekas, A.; Mazurkiewicz, L.R.; Gleńsk, M.; Ossowska, G. Effect of Osthole on the Protective Activity of Carbamazepine and Phenobarbital against Maximal Electroshock-Induced Seizures in Mice. Ann. Univ. Mariae Curie-Sklodowska Sect. DDD Pharm. 2010, 23, 145–156. [Google Scholar]
- Łuszczki, J.J.; Marczewski, T.; Mazurkiewicz, L.P.; Karwan, S.; Teresińska, M.; Florek-Łuszczki, M.; Gleńsk, M. Influence of Osthole on the Anticonvulsant Activity of Phenytoin and Valproate in the Maximal Electroshock-Induced Seizures in Mice. Ann. Univ. Mariae Curie-Sklodowska Sect. DDD Pharm. 2011, 24, 33–44. [Google Scholar]
- Kontogiorgis, C.; Detsi, A.; Hadjipavlou-Litina, D. Coumarin-Based Drugs: A Patent Review (2008—Present). Expert Opin. Ther. Pat. 2012, 22, 437–454. [Google Scholar] [CrossRef]
- Skalicka-Woźniak, K.; Orhan, I.E.; Cordell, G.A.; Nabavi, S.M.; Budzyńska, B. Implication of Coumarins towards Central Nervous System Disorders. Pharmacol. Res. 2016, 103, 188–203. [Google Scholar] [CrossRef]
- Kowalczyk, J.; Budzyńska, B.; Kurach, Ł.; Pellegata, D.; El Sayed, N.S.; Gertsch, J.; Skalicka-Woźniak, K. Neuropsychopharmacological profiling of scoparone in mice. Sci. Rep. 2022, 17, 822. [Google Scholar] [CrossRef]
- Skalicka-Woźniak, K.; Walasek, M.; Aljarba, T.M.; Stapleton, P.; Gibbons, S.; Xiao, J.; Łuszczki, J.J. The anticonvulsant and anti-plasmid conjugation potential of Thymus vulgaris chemistry: An in vivo murine and in vitro study. Food Chem. Toxicol. 2018, 120, 472–478. [Google Scholar] [CrossRef] [Green Version]
- Yu, B.; Ruan, M.; Dong, X.; Yu, Y.; Cheng, H. The Mechanism of the Opening of the Blood-Brain Barrier by Borneol: A Pharmacodynamics and Pharmacokinetics Combination Study. J. Ethnopharmacol. 2013, 150, 1096–1108. [Google Scholar] [CrossRef] [PubMed]
- Cai, Z.; Hou, S.; Li, Y.; Zhao, B.; Yang, Z.; Xu, S.; Pu, J. Effect of Borneol on the Distribution of Gastrodin to the Brain in Mice via Oral Administration. J. Drug Target. 2008, 16, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Yao, Y.; Zhang, X.; Ruan, M.; Zhang, Z.; Xu, L.; Liang, T.; Lu, J. Synergic Neuroprotection Between Ligusticum Chuanxiong Hort and Borneol Against Ischemic Stroke by Neurogenesis via Modulating Reactive Astrogliosis and Maintaining the Blood-Brain Barrier. Front. Pharmacol. 2021, 12, 666790. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Pan, L.; Peng, D.; Bao, Q.; Xiao, L.; Zhou, A.; Wu, H.; Peng, C.; Chen, W. Analysis of the Active Components and Metabolites of Taohong Siwu Decoction by Using Ultra High Performance Liquid Chromatography Quadrupole Time-of-Flight Mass Spectrometry. J. Sep. Sci. 2020, 43, 4131–4147. [Google Scholar] [CrossRef]
- Agnihotri, V.K.; Lattoo, S.K.; Thappa, R.K.; Kaul, P.; Qazi, G.N.; Dhar, A.K.; Saraf, A.; Kapahi, B.K.; Saxena, R.K.; Agarwal, S.G. Chemical Variability in the Essential Oil Components of Achillea Millefolium Agg. from Different Himalayan Habitats (India). Planta Med. 2005, 71, 280–283. [Google Scholar] [CrossRef]
- Skalicka-Woźniak, K.; Zagaja, M.; Głowniak, K.; Łuszczki, J.J. Purification and Anticonvulsant Activity of Xanthotoxin (8-Methoxypsoralen). Cent. Eur. J. Biol. 2014, 9, 431–436. [Google Scholar] [CrossRef] [Green Version]
- Zagaja, M.; Andres-Mach, M.; Patrzylas, P.; Pyrka, D.; Szpringer, M.; Florek-Łuszczki, M.; Żółkowska, D.; Skalicka-Woźniak, K.; Łuszczki, J.J. Influence of Xanthotoxin (8-Methoxypsoralen) on the Anticonvulsant Activity of Various Novel Antiepileptic Drugs against Maximal Electroshock-Induced Seizures in Mice. Fitoterapia 2016, 115, 86–91. [Google Scholar] [CrossRef]
- Łuszczki, J.J.; Danysz, W.; Czuczwar, S.J. Interactions of MRZ 2/576 with Felbamate, Lamotrigine, Oxcarbazepine and Topiramate in the Mouse Maximal Electroshock-Induced Seizure Model. Pharmacology 2008, 81, 259–265. [Google Scholar] [CrossRef]
- Łuszczki, J.J.; Marzeda, P.; Gut-Lepiech, A.; Kondrat-Wróbel, M.W.; Wróblewska-Łuczka, P.; Karwan, S.; Plech, T. New Derivative of 1,2,4-Triazole-3-Thione (TP427) Potentiates the Anticonvulsant Action of Valproate, but Not That of Carbamazepine, Phenytoin or Phenobarbital in the Mouse Tonic-Clonic Seizure Model. Pharmacol. Rep. 2019, 71, 299–305. [Google Scholar] [CrossRef]
- Łuszczki, J.; Świa̧der, M.; Czuczwar, M.; Kiś, J.; Czuczwar, S.J. Interactions of Tiagabine with Some Antiepileptics in the Maximal Electroshock in Mice. Pharmacol. Biochem. Behav. 2003, 75, 319–327. [Google Scholar] [CrossRef]
- Cadart, M.; Marchand, S.; Pariat, C.; Bouquet, S.; Couet, W. Ignoring Pharmacokinetics May Lead to Isoboles Misinterpretation: Illustration with the Norfloxacin-Theophylline Convulsant Interaction in Rats. Pharm. Res. 2002, 19, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Łuszczki, J.J.; Ratnaraj, N.; Patsalos, P.N.; Czuczwar, S.J. Isobolographic Analysis of Interactions between Loreclezole and Conventional Antiepileptic Drugs in the Mouse Maximal Electroshock-Induced Seizure Model. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2006, 373, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Chai, L.; Zhang, H.; Wang, Y.; Zhang, B.; Gao, X. Borneol Depresses P-Glycoprotein Function by a NF-ΚB Signaling Mediated Mechanism in a Blood Brain Barrier in Vitro Model. Int. J. Mol. Sci. 2015, 16, 27576–27588. [Google Scholar] [CrossRef] [Green Version]
- Luo, D.-D.; Chen, X.-Y.; Zhang, Z.-B.; Sun, C.-Y.; Zheng, Y.-F.; Liu, Y.-H.; Wang, X.-F.; Wang, Q.; Zhan, J.Y.-X.; Su, Z.-R. Different Effects of (+)-borneol and (-)-borneol on the Pharmacokinetics of Osthole in Rats Following Oral Administration. Mol. Med. Rep. 2017, 15, 4239–4246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.Y.; Huang, X.T.; Wang, J.J.; Chen, Y. In vivo effect of borneol on rat hepatic CYP2B expression and activity. Chem Biol. Interact. 2017, 261, 96–102. [Google Scholar] [CrossRef]
- Zhang, R.; Mi, S.Q.; Wang, N.S. Effect of borneol on cytochrome P450 3A enzyme and midazolam pharmacokinetics in rats. Eur. J. Drug Metab. Pharmacokinet. 2013, 38, 159–169. [Google Scholar] [CrossRef]
- Boissier, J.R.; Tardy, J.; Diverres, J.C. Une nouvelle méthode simple pour explorer l’action «tranquillisante»: Le test de la cheminée. Pharmacology 1960, 3, 81–84. [Google Scholar] [CrossRef]
- Meyer, O.A.; Tilson, H.A.; Byrd, W.C.; Riley, M.T. A method for the routine assessment of fore- and hindlimb grip strength of rats and mice. Neurobehav. Toxicol. 1979, 1, 233–236. [Google Scholar]
- Sawicka, K.M.; Wawryniuk, A.; Daniluk, J.; Karwan, S.; Florek-Łuszczki, M.; Chmielewski, J.; Łuszczki, J.J. Influence of Dronedarone (a Class III Antiarrhythmic Drug) on the Anticonvulsant Potency of Four Classical Antiepileptic Drugs in the Tonic–Clonic Seizure Model in Mice. J. Neural Transm. 2019, 126, 115–122. [Google Scholar] [CrossRef] [Green Version]
- Sawicka, K.M.; Florek-Łuszczki, M.; Wawryniuk, A.; Daniluk, J.; Wróblewska-Łuczka, P.; Chmielewski, J.; Karwan, S.; Łuszczki, J.J. Dronedarone (a Multichannel Blocker) Enhances the Anticonvulsant Potency of Lamotrigine, but Not That of Lacosamide, Pregabalin and Topiramate in the Tonic-Clonic Seizure Model in Mice. Epilepsy Res. 2019, 154, 62–68. [Google Scholar] [CrossRef]
- Litchfield, J.T.; Wilcoxon, F. A Simplified Method of Evaluating Dose-Effect Experiments. J. Pharmacol. Exp. Ther. 1949, 96, 99–113. [Google Scholar]
- Loewe, S. The Problem of Synergism and Antagonism of Combined Drugs. Arzneimittelforschung 1953, 3, 285–290. [Google Scholar] [PubMed]
- Łuszczki, J.J.; Panasiuk, A.; Zagaja, M.; Karwan, S.; Bojar, H.; Plewa, Z.; Florek-Łuszczki, M. Polygonogram and Isobolographic Analysis of Interactions between Various Novel Antiepileptic Drugs in the 6-Hz Corneal Stimulation-Induced Seizure Model in Mice. PLoS ONE 2020, 15, e0234070. [Google Scholar] [CrossRef] [PubMed]
- Łuszczki, J.J.; Podgórska, D.; Kozińska, J.; Jankiewicz, M.; Plewa, Z.; Kominek, M.; Żółkowska, D.; Florek-Łuszczki, M. Polygonogram with Isobolographic Synergy for Three-Drug Combinations of Phenobarbital with Second-Generation Antiepileptic Drugs in the Tonic–Clonic Seizure Model in Mice. Pharmacol. Rep. 2021, 73, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Chou, T.-C. Preclinical versus Clinical Drug Combination Studies. Leuk. Lymphoma 2008, 49, 2059–2080. [Google Scholar] [CrossRef]
- Tomaszewski, M.; Zolkowska, D.; Plewa, Z.; Czuczwar, S.J.; Łuszczki, J.J. Effect of acute and chronic exposure to lovastatin on the anticonvulsant action of classical antiepileptic drugs in the mouse maximal electroshock-induced seizure model. Eur. J. Pharmacol. 2021, 907, 174290. [Google Scholar] [CrossRef]
- Łuszczki, J.J.; Czuczwar, S.J. Isobolographic and Subthreshold Methods in the Detection of Interactions between Oxcarbazepine and Conventional Antiepileptics—A Comparative Study. Epilepsy Res. 2003, 56, 27–42. [Google Scholar] [CrossRef]





| ASM | ED50 | n | ANOVA Statistics | Fraction of ASM |
|---|---|---|---|---|
| CBZ + vehicle | 9.52 ± 0.76 | 16 | 1.00 | |
| CBZ + scoparone (25) | 8.44 ± 0.84 | 16 | 0.89 | |
| CBZ + scoparone (50) | 6.84 ± 0.85 | 16 | F(2;45) = 2.719; p = 0.077 | 0.72 |
| PHT + vehicle | 8.71 ± 0.95 | 16 | 1.00 | |
| PHT + scoparone (25) | 8.18 ± 0.80 | 16 | 0.94 | |
| PHT + scoparone (50) | 7.27 ± 0.72 | 16 | F(2;45) = 0.772; p = 0.468 | 0.84 |
| PB + vehicle | 28.85 ± 1.89 | 16 | 1.00 | |
| PB + scoparone (25) | 23.17 ± 2.18 | 16 | 0.80 | |
| PB + scoparone (50) | 18.71 ± 1.88 ** | 16 | F(2;45) = 6.534; p = 0.003 | 0.65 |
| VPA + vehicle | 292.0 ± 12.6 | 24 | 1.00 | |
| VPA + scoparone (12.5) | 269.7 ± 12.9 | 24 | 0.92 | |
| VPA + scoparone (25) | 241.5 ± 12.5 * | 24 | 0.83 | |
| VPA + scoparone (50) | 219.4 ± 13.0 *** | 24 | F(3;92) = 6.234; p = 0.0007 | 0.75 |
| CBZ + vehicle | 9.52 ± 0.76 | 16 | 1.00 | |
| CBZ + borneol (25) | 7.83 ± 0.86 | 24 | 0.82 | |
| CBZ + borneol (50) | 7.27 ± 0.72 | 16 | F(2;53) = 1.772; p = 0.180 | 0.76 |
| PHT + vehicle | 8.71 ± 0.95 | 16 | 1.00 | |
| PHT + borneol (25) | 7.82 ± 0.85 | 24 | 0.90 | |
| PHT + borneol (50) | 6.84 ± 0.85 | 16 | F(2;53) = 0.941; p = 0.397 | 0.79 |
| PB + vehicle | 28.85 ± 1.89 | 16 | 1.00 | |
| PB + borneol (25) | 22.35 ± 2.09 | 24 | 0.78 | |
| PB + borneol (50) | 19.57 ± 2.15 * | 24 | F(2;61) = 4.401; p = 0.016 | 0.68 |
| VPA + vehicle | 292.0 ± 12.6 | 24 | 1.00 | |
| VPA + borneol (12.5) | 230.4 ± 11.3 | 16 | 0.79 | |
| VPA + borneol (25) | 205.2 ± 11.7 ** | 16 | 0.70 | |
| VPA + borneol (50) | 188.3 ± 11.5 *** | 16 | F(3;68) = 15.80; p < 0.0001 | 0.65 |
| Combination | ED50exp | nexp | ED50add | nadd | t-Test Statistics | Sum of Fractions |
|---|---|---|---|---|---|---|
| CBZ + scoparone (50) | 56.84 ± 0.85 | 16 | 57.14 ± 2.01 | 28 | t = 0.138; df = 35.48; p = 0.891 | 0.72 + 0.25 = 0.97 |
| PHT + scoparone (50) | 57.27 ± 0.72 | 16 | 56.53 ± 2.08 | 28 | t = 0.336; df = 33.01; p = 0.739 | 0.84 + 0.25 = 1.09 |
| PB + scoparone (50) | 68.71 ± 1.88 | 16 | 71.63 ± 2.44 | 28 | t = 0.948; df = 41.96; p = 0.349 | 0.65 + 0.25 = 0.90 |
| VPA + scoparone (50) | 269.4 ± 12.96 | 24 | 268.9 ± 6.44 | 36 | t = 0.035; df = 34.38; p = 0.973 | 0.75 + 0.25 = 1.00 |
| CBZ + borneol (50) | 57.27 ± 0.72 | 16 | 57.66 ± 2.26 | 28 | t = 0.164; df = 32.16; p = 0.870 | 0.76 + 0.20 = 0.96 |
| PHT + borneol (50) | 56.84 ± 0.85 | 16 | 57.00 ± 2.33 | 28 | t = 0.065; df = 33.59; p = 0.949 | 0.79 + 0.20 = 0.99 |
| PB + borneol (50) | 69.57 ± 2.15 | 24 | 73.20 ± 2.71 | 28 | t = 1.049; df = 48.93; p = 0.299 | 0.68 + 0.20 = 0.88 |
| VPA + borneol (50) | 238.3 ± 11.48 ** | 16 | 284.8 ± 7.01 | 36 | t = 3.457; df = 26.68; p = 0.002 | 0.65 + 0.20 = 0.85 |
| Combination | ED50exp | nexp | ED50add | nadd | t-Test Statistics | Sum of Fractions |
|---|---|---|---|---|---|---|
| CBZ + scoparone (25) + borneol (25) | 56.40 ± 0.87 | 16 | 58.46 ± 2.26 | 28 | t = 0.851; df = 34.24; p = 0.401 | 0.67 + 0.13 + 0.10 = 0.90 |
| PHT + scoparone (25) + borneol (25) | 55.21 ± 0.70 | 16 | 57.74 ± 2.34 | 28 | t = 1.036; df = 31.59; p = 0.308 | 0.60 + 0.13 + 0.10 = 0.83 |
| PB + scoparone (25) + borneol (25) | 66.55 ± 2.40 * | 16 | 75.64 ± 2.76 | 28 | t = 2.485; df = 41.04; p = 0.017 | 0.57 + 0.13 + 0.10 = 0.80 |
| VPA + scoparone (25) + borneol (25) | 224.1 ± 11.01 *** | 24 | 288.4 ± 7.51 | 36 | t = 4.825; df = 43.23; p < 0.0001 | 0.60 + 0.13 + 0.10 = 0.83 |
| Compound | Pretreatment Time (min) | Ref. | |||
|---|---|---|---|---|---|
| 15 | 30 | 60 | 120 | ||
| Imperatorin | 185 (0.684) | 167 (0.618) | 206 (0.762) | 290 (1.073) | [10] |
| Xanthotoxin | 227.7 (0.910) | 225.1 (0.899) | 219.1 (0.875) | 252.4 (1.008) | [26] |
| Scoparone | 199.8 (0.969) | 277.7 (1.347) | 256.5 (1.244) | 320.1 (1.552) | this study |
| Osthole | 266 (1.089) | 253 (1.036) | 472 (1.932) | 639 (2.616) | [10] |
| Borneol | 255.4 (1.656) | 315.0 (2.042) | 370.8 (2.404) | 448.1 (2.905) | this study |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Łuszczki, J.J.; Bojar, H.; Góralczyk, A.; Skalicka-Woźniak, K. Antiseizure Effects of Scoparone, Borneol and Their Impact on the Anticonvulsant Potency of Four Classic Antiseizure Medications in the Mouse MES Model—An Isobolographic Transformation. Int. J. Mol. Sci. 2023, 24, 1395. https://doi.org/10.3390/ijms24021395
Łuszczki JJ, Bojar H, Góralczyk A, Skalicka-Woźniak K. Antiseizure Effects of Scoparone, Borneol and Their Impact on the Anticonvulsant Potency of Four Classic Antiseizure Medications in the Mouse MES Model—An Isobolographic Transformation. International Journal of Molecular Sciences. 2023; 24(2):1395. https://doi.org/10.3390/ijms24021395
Chicago/Turabian StyleŁuszczki, Jarogniew J., Hubert Bojar, Agnieszka Góralczyk, and Krystyna Skalicka-Woźniak. 2023. "Antiseizure Effects of Scoparone, Borneol and Their Impact on the Anticonvulsant Potency of Four Classic Antiseizure Medications in the Mouse MES Model—An Isobolographic Transformation" International Journal of Molecular Sciences 24, no. 2: 1395. https://doi.org/10.3390/ijms24021395





