CD40 Ligand–CD40 Interaction Is an Intermediary between Inflammation and Angiogenesis in Proliferative Diabetic Retinopathy
Abstract
1. Introduction
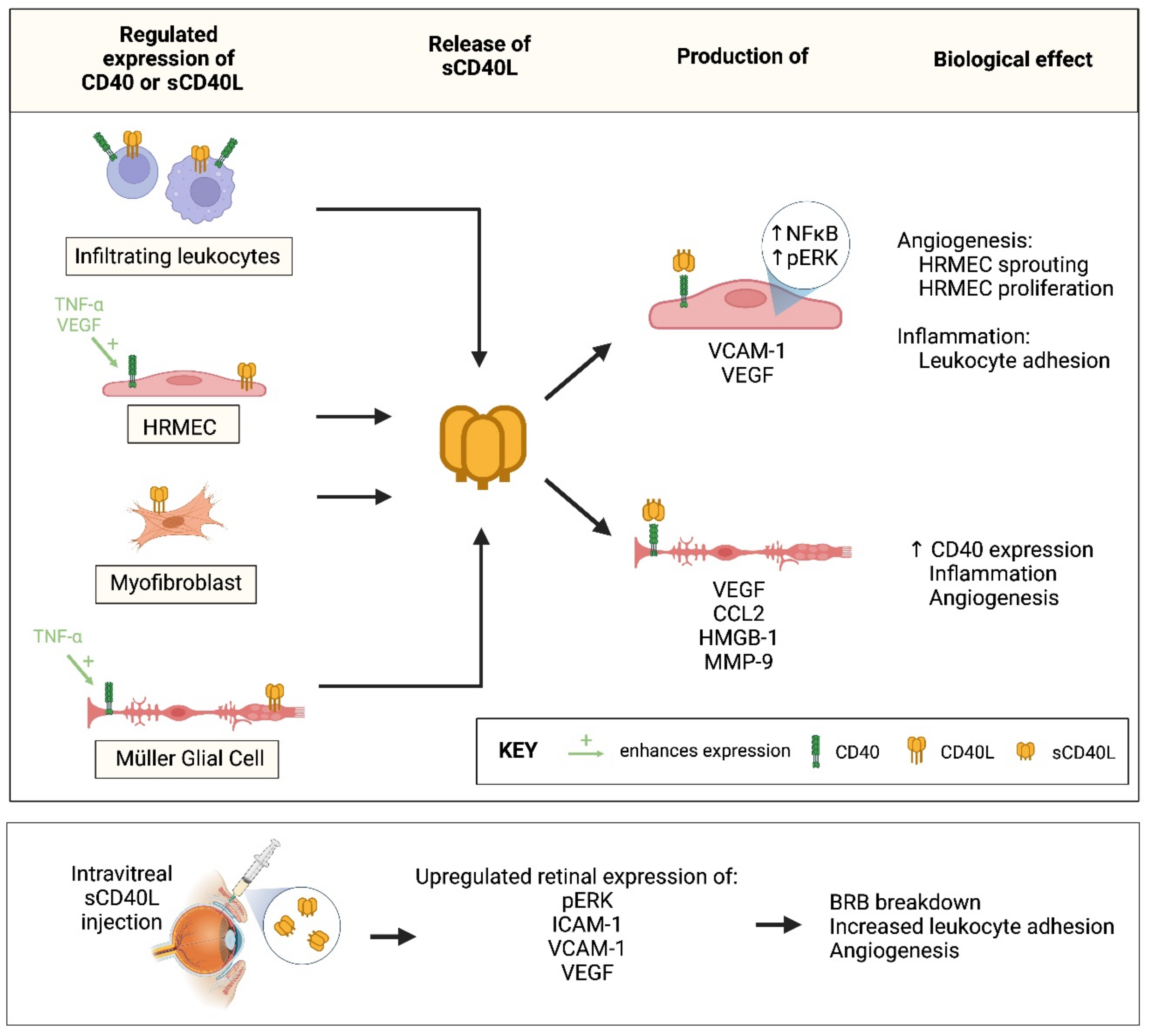
2. Results
2.1. CD40 and CD40L Are Present in Vitreous Samples from Patients with PDR
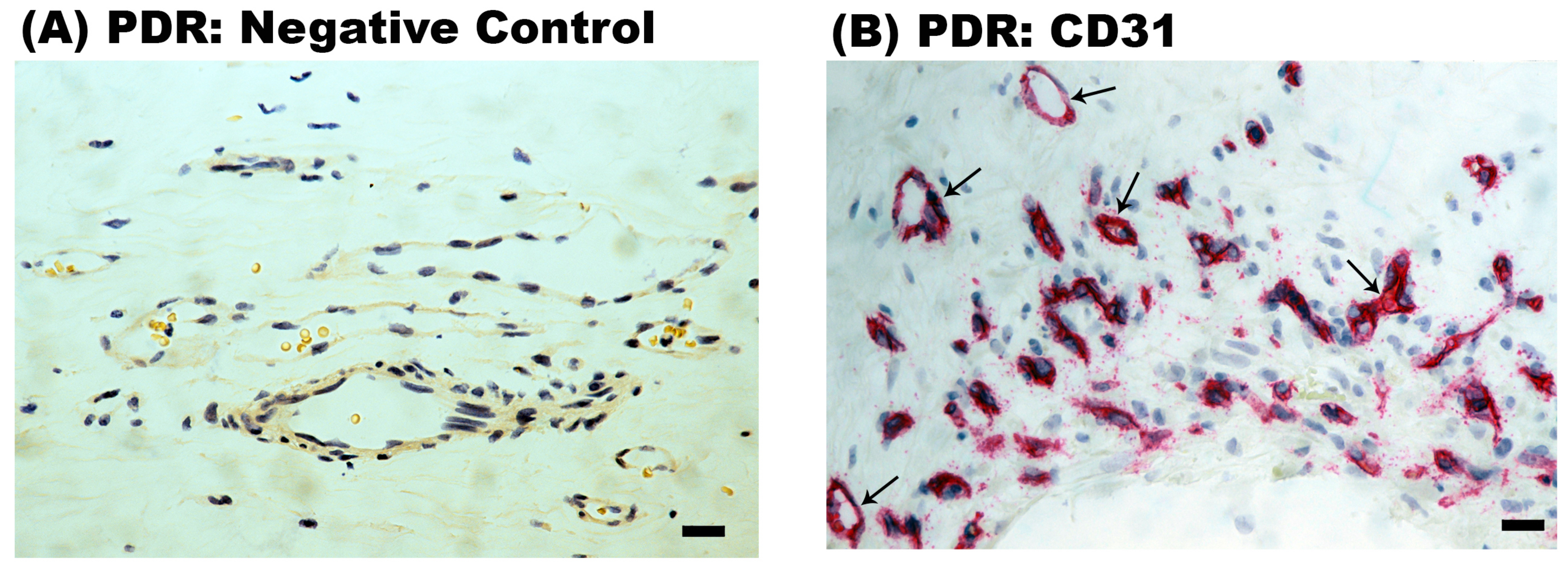
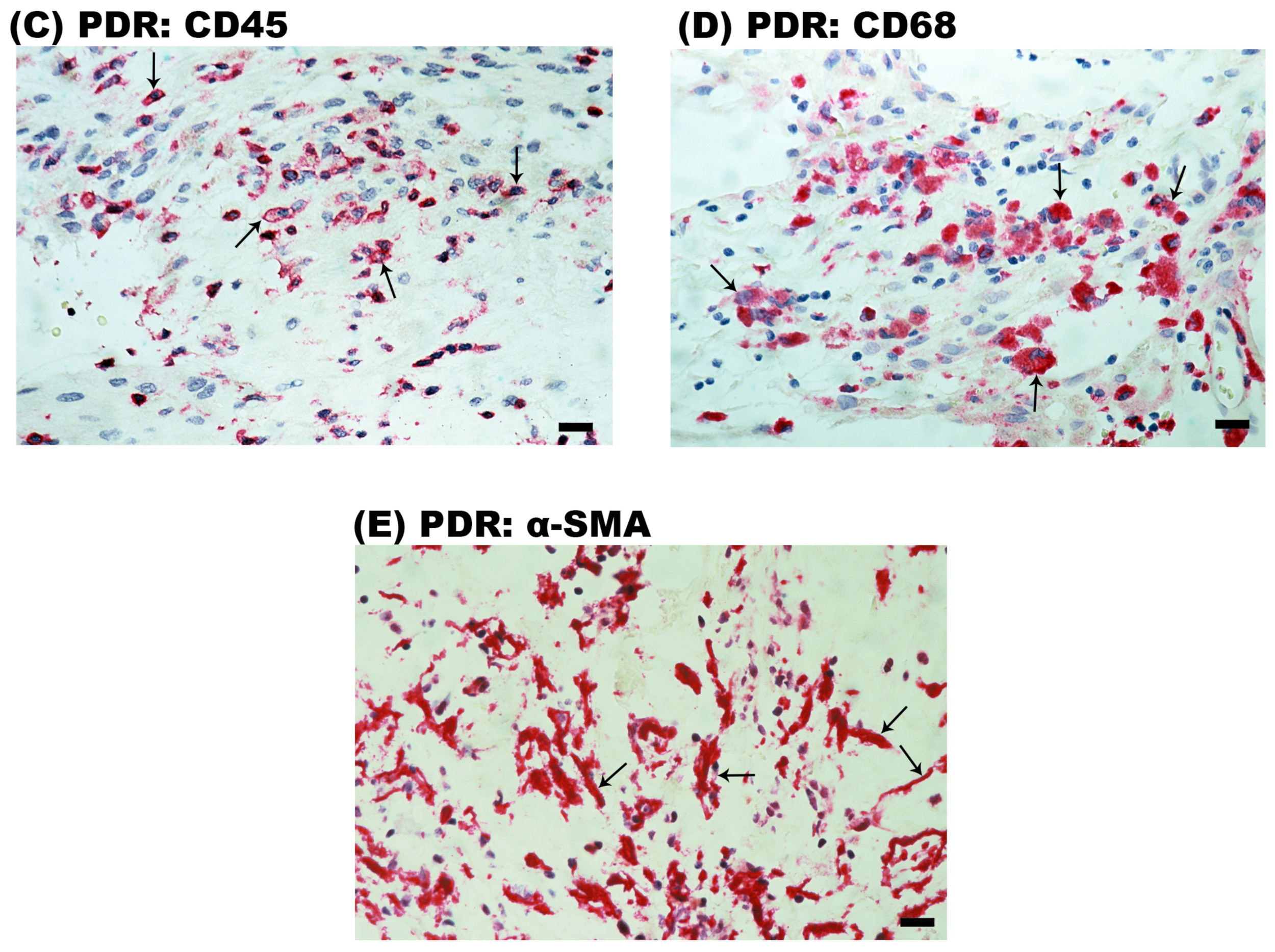
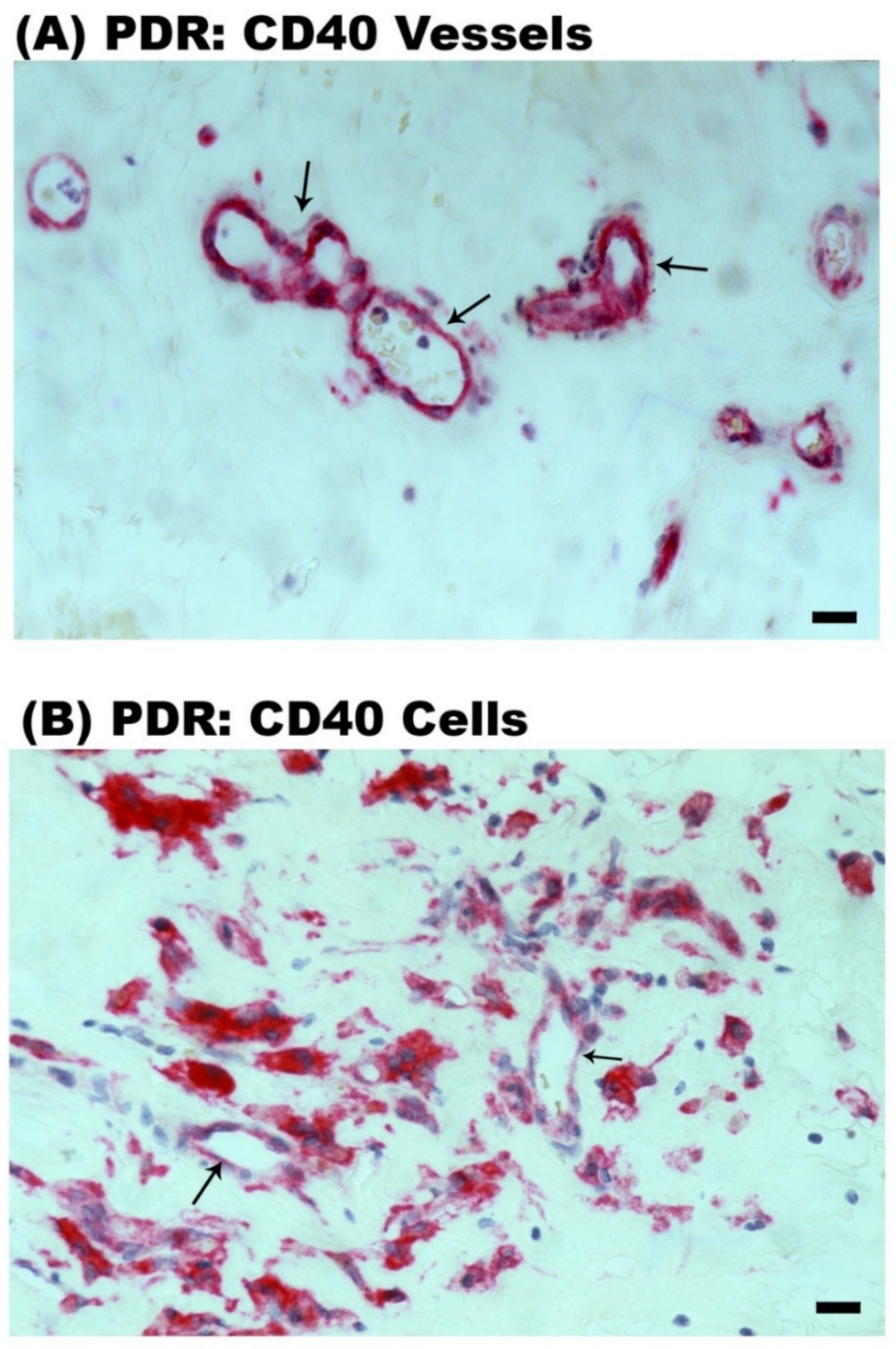
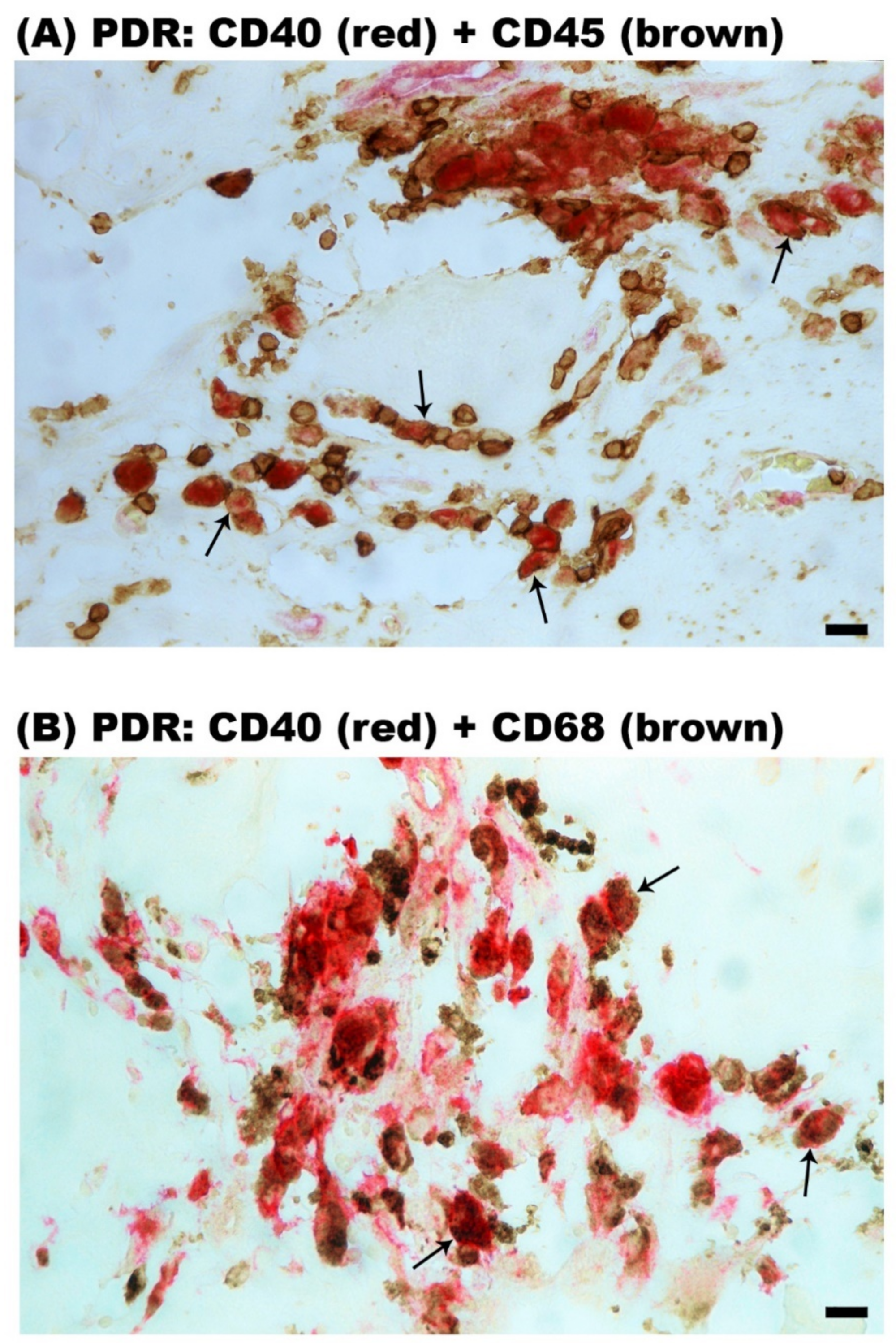
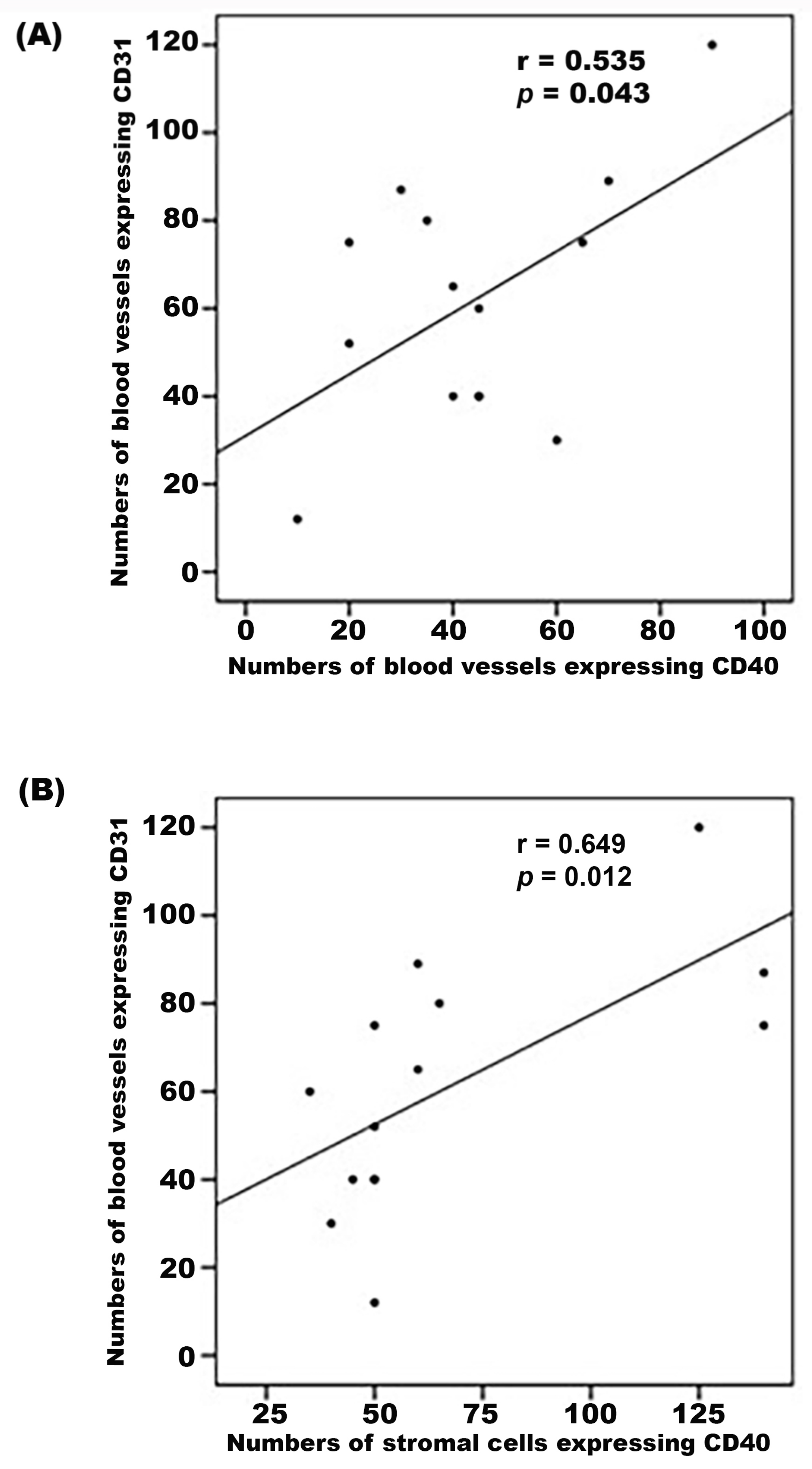
2.2. Expression of CD40L and CD40 in Epiretinal Fibrovascular Membranes from Patients with PDR
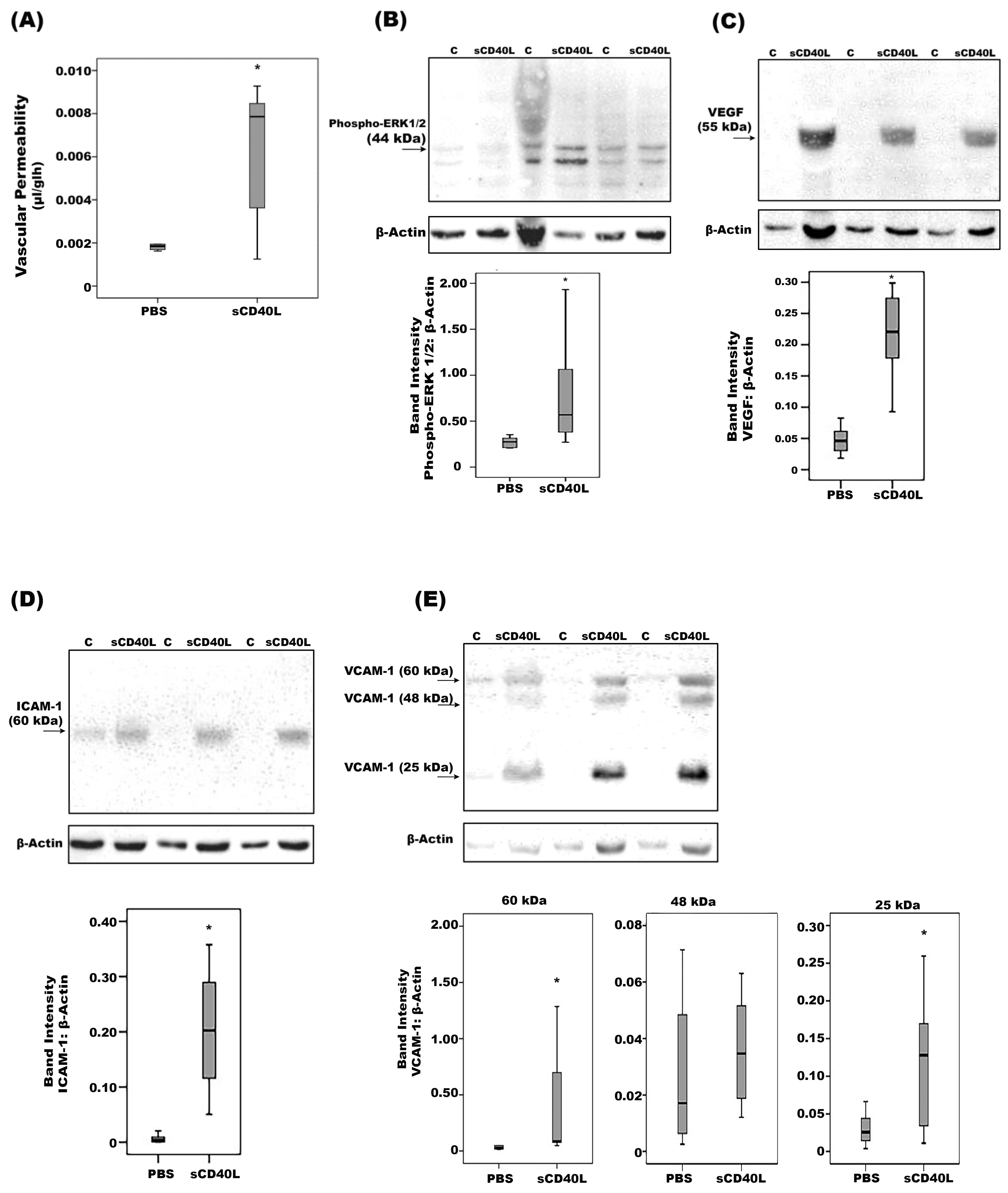
2.3. Effect of Intravitreal Administration of sCD40L in Normal Rats
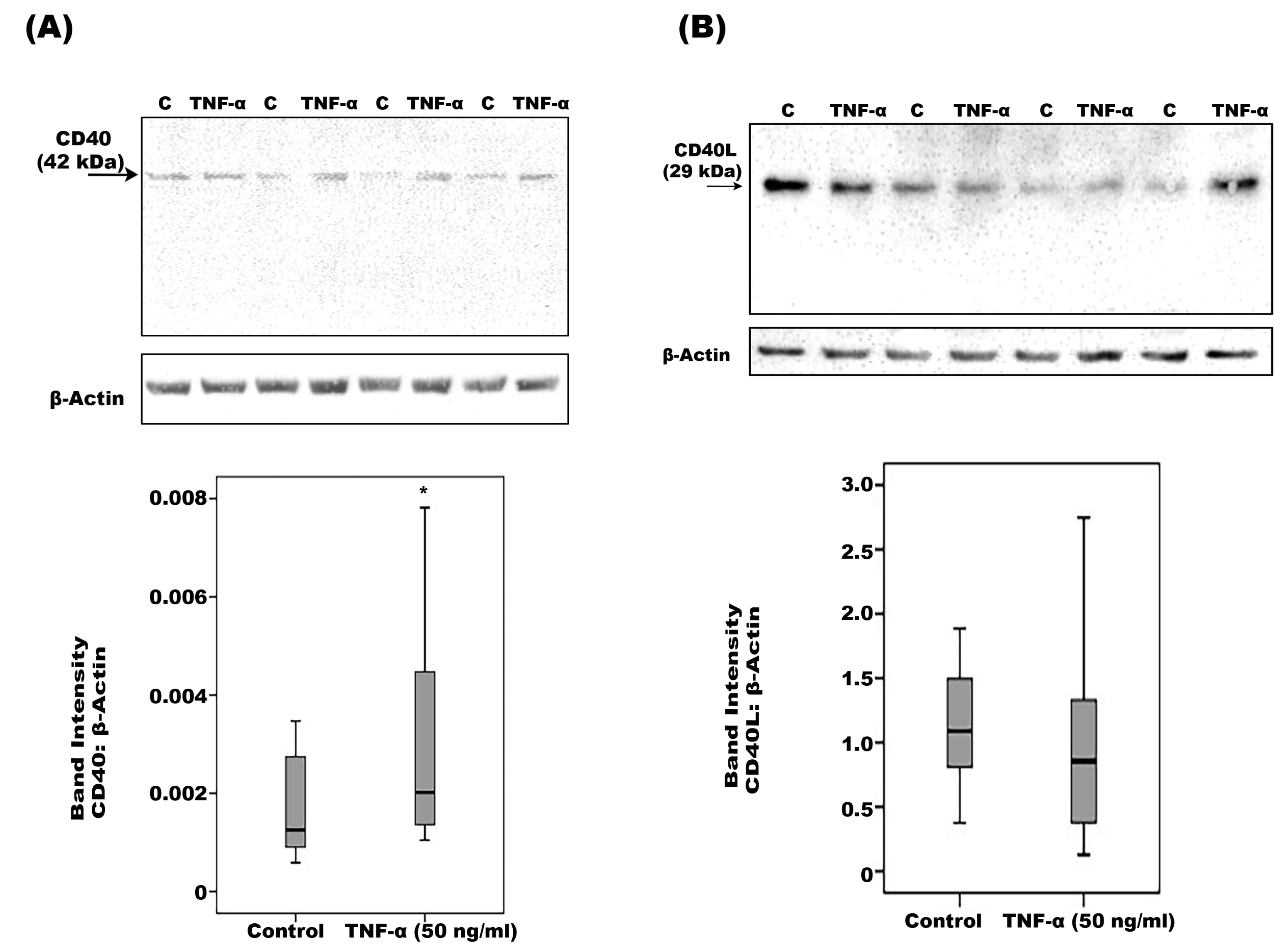
2.4. Effect of Diabetic Retinopathy-Associated Mechanisms on the Expression of CD40 and CD40L in Human Retinal Müller Glial Cells
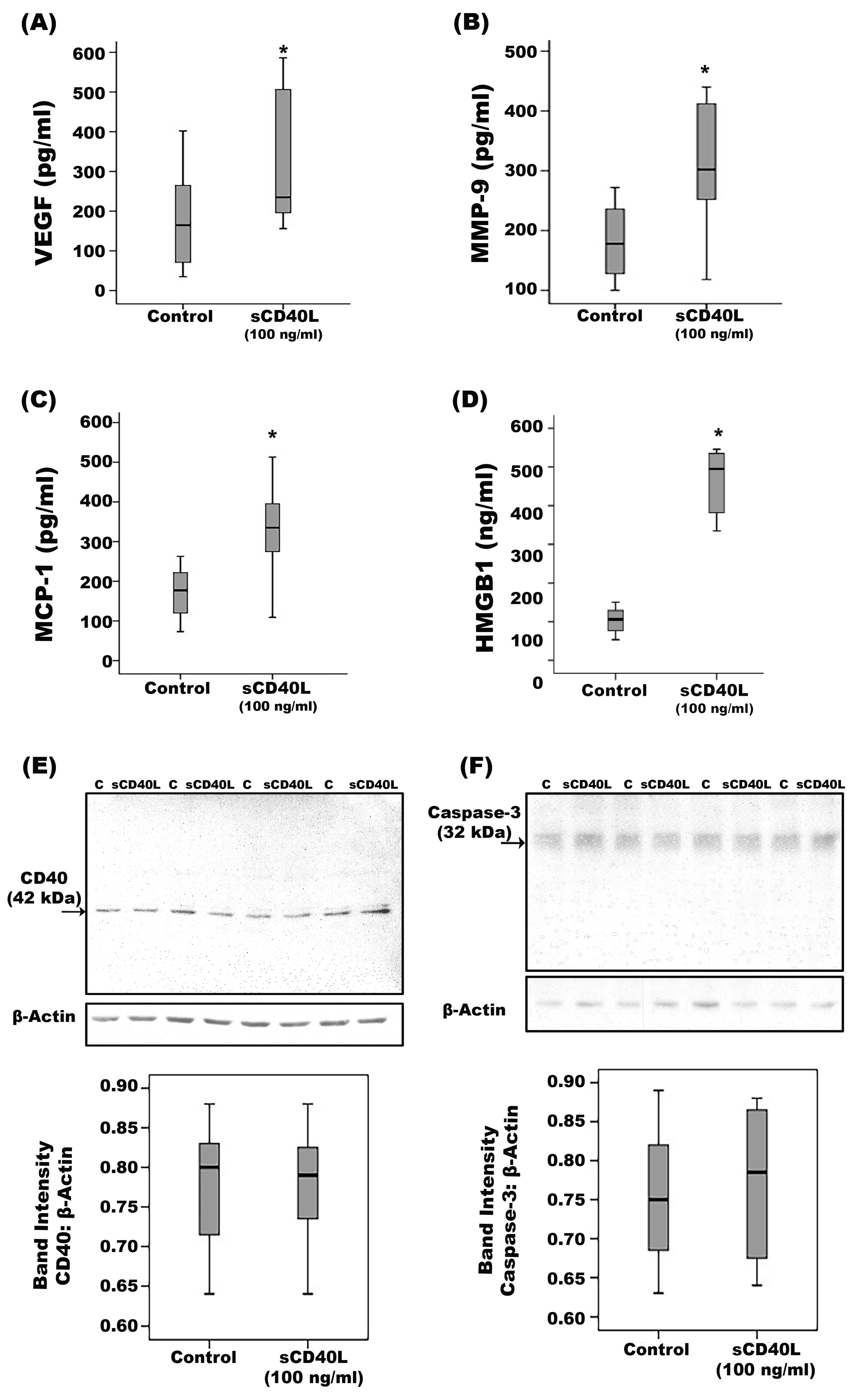
2.5. Effect of CD40 Ligation on Human Retinal Müller Glial Cells
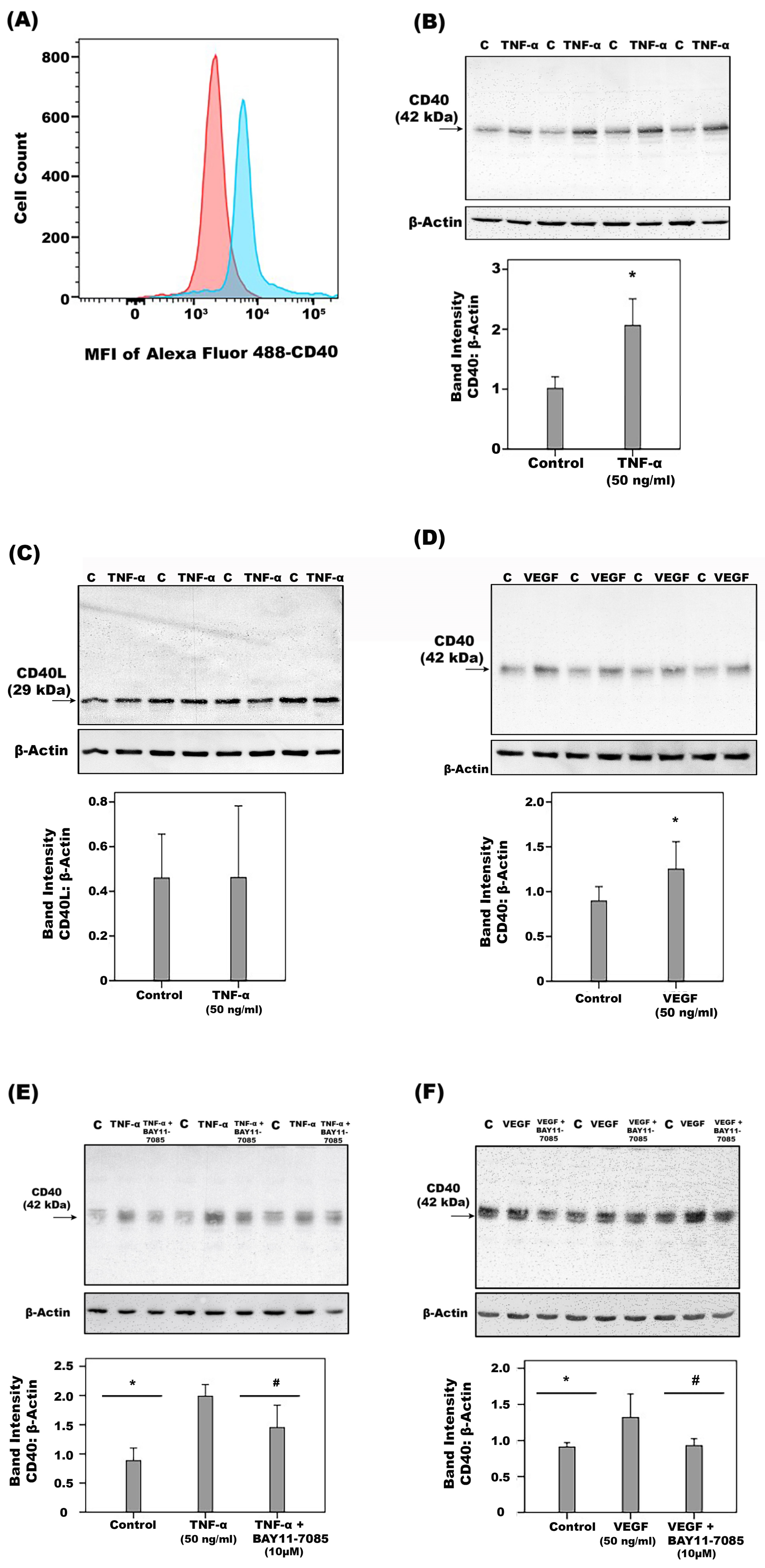
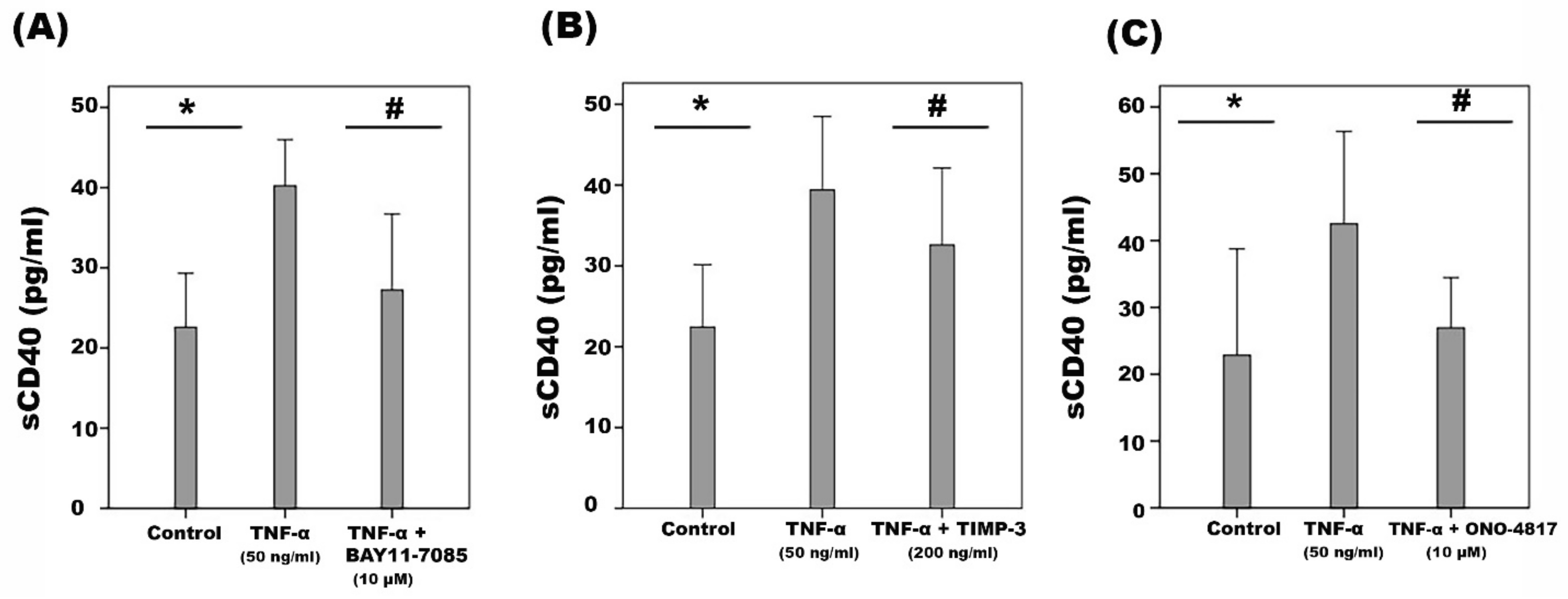
2.6. Effect of Diabetic Retinopathy-Associated Mechanisms on the Expression of CD40 and CD40L in Human Retinal Microvascular Endothelial Cells
2.7. Effect of Ligation of CD40 on Human Retinal Microvascular Endothelial Cells
3. Discussion
4. Materials and Methods
4.1. Patient Samples
4.2. Immunohistochemical Staining of Human Epiretinal Membranes and Quantifications
4.3. Intravitreal Injection of sCD40L in Rats
4.4. Measurement of Blood-Retinal Barrier Breakdown in Rats
4.5. Human retinal Müller Glial Cell and Human Retinal Microvascular Endothelial Cell Cultures
4.6. Enzyme-Linked Immunosorbent Assays of Human Vitreous Fluid and Culture Medium
4.7. Western Blot Analysis of Human Vitreous Fluid, Human Retinal Müller Glial Cell and Human Retinal Microvascular Endothelial Cell Lysates and Rat Retinas
4.8. Cell Adhesion Assay
4.9. Flow Cytometric Detection of CD40 Expression on HRMECs
4.10. Endothelial Cell Proliferation Assay
4.11. Endothelial Cell Spheroid Sprouting Assay
4.12. Müller Glial Cell Proliferation Assay
4.13. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bhagat, N.; Grigorian, R.A.; Tutela, A.; Zarbin, M.A. Diabetic macular edema: Pathogenesis and treatment. Surv. Ophthalmol. 2009, 54, 1–32. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, K.; Khosrof, S.; Bursell, S.E.; Rohan, R.; Murata, T.; Clermont, A.C.; Aiello, L.P.; Ogura, Y.; Adamis, A.P. Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Proc. Natl. Acad. Sci. USA 1999, 96, 10836–10841. [Google Scholar] [CrossRef] [PubMed]
- Abu El-Asrar, A.M.; Nawaz, M.I.; Ahmad, A.; Siddiquei, M.M.; Allegaert, E.; Gikandi, P.W.; De Hertogh, G.; Opdenakker, G. CD146/Soluble CD146 pathway is a novel biomarker of angiogenesis and inflammation in proliferative diabetic retinopathy. Invest. Ophthalmol. Vis. Sci. 2021, 62, 32. [Google Scholar] [CrossRef] [PubMed]
- Abu El-Asrar, A.M.; Nawaz, M.I.; Ahmad, A.; De Zutter, A.; Siddiquei, M.M.; Blanter, M.; Allegaert, E.; Gikandi, P.W.; De Hertogh, G.; Van Damme, J.; et al. Evaluation of proteoforms of the transmembrane chemokines CXCL16 and CX3CL1, their Receptors, and their processing metalloproteinases ADAM10 and ADAM17 in proliferative diabetic retinopathy. Front. Immunol. 2020, 11, 601639. [Google Scholar] [CrossRef]
- Abu El-Asrar, A.M.; Ahmad, A.; Siddiquei, M.M.; De Zutter, A.; Allegaert, E.; Gikandi, P.W.; De Hertogh, G.; Van Damme, J.; Opdenakker, G.; Struyf, S. The proinflammatory and proangiogenic macrophage migration inhibitory factor is a potential regulator in proliferative diabetic retinopathy. Front. Immunol. 2019, 10, 2752. [Google Scholar] [CrossRef] [PubMed]
- Abu El-Asrar, A.M.; Mohammad, G.; Nawaz, M.I.; Siddiquei, M.M.; Van den Eynde, K.; Mousa, A.; De Hertogh, G.; Opdenakker, G. Relationship between vitreous levels of matrix metalloproteinases and vascular endothelial growth factor in proliferative diabetic retinopathy. PLoS ONE 2013, 8, e85857. [Google Scholar] [CrossRef]
- Wu, G.; Liu, B.; Wu, Q.; Tang, C.; Du, Z.; Fang, Y.; Hu, Y.; Yu, H. Correlations Between Different Angiogenic and Inflammatory Factors in Vitreous Fluid of Eyes With Proliferative Diabetic Retinopathy. Front. Med. 2021, 8, 727407. [Google Scholar] [CrossRef]
- Kim, Y.W.; West, X.Z.; Byzova, T.V. Inflammation and oxidative stress in angiogenesis and vascular disease. J. Mol. Med. 2013, 91, 323–328. [Google Scholar] [CrossRef]
- Ono, M. Molecular links between tumor angiogenesis and inflammation: Inflammatory stimuli of macrophages and cancer cells as targets for therapeutic strategy. Cancer Sci. 2008, 99, 1501–1506. [Google Scholar] [CrossRef]
- Pateras, I.S.; Cooks, T. Determination of polarization of resident macrophages and their effect on the tumor microenvironment. Methods Mol. Biol. 2019, 1928, 101–112. [Google Scholar]
- Umansky, V.; Adema, G.J.; Baran, J.; Brandau, S.; Van Ginderachter, J.A.; Hu, X.; Jablonska, J.; Mojsilovic, S.; Papadaki, H.A.; Pico de Coana, Y.; et al. Interactions among myeloid regulatory cells in cancer. Cancer Immunol. Immunother. 2019, 68, 645–660. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.W.; Le Couter, J.; Strauss, E.C.; Ferrara, N. Vascular endothelial growth factor A in intraocular vascular disease. Ophthalmology 2013, 120, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, M. Differential roles of vascular endothelial growth factor receptor-1 and receptor-2 in angiogenesis. J. Biochem. Mol. Biol. 2006, 39, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Danese, S.; Scaldaferri, F.; Vetrano, S.; Stefanelli, T.; Graziani, C.; Repici, A.; Ricci, R.; Straface, G.; Sgambato, A.; Malesci, A.; et al. Critical role of the CD40-CD40-ligand pathway in regulating mucosal inflammation-driven angiogenesis in inflammatory bowel disease. Gut 2007, 56, 1248–1256. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schönbeck, U.; Libby, P. The CD40/CD154 receptor/ligand dyad. Cell. Mol. Life Sci. 2001, 58, 4–43. [Google Scholar] [PubMed]
- Senhaji, N.; Kojok, K.; Darif, Y.; Fadainia, C.; Zaid, Y. The contribution of CD40/CD40L axis in inflammatory bowel disease: An update. Front. Immunol. 2015, 6, 529. [Google Scholar] [CrossRef]
- Michel, N.A.; Zirlik, A.; Wolf, D. CD40L and its receptors in atherothrombosis-an update. Front. Cardiovasc. Med. 2017, 4, 40. [Google Scholar] [CrossRef]
- Yacoub, D.; Benslimane, N.; Al-Zoobi, L.; Hassan, G.; Nadiri, A.; Mourad, W. CD154 is released from T-cells by a disintegrin and metalloproteinase domain-containing protein 10 (ADAM10) and ADAM17 in a CD40 protein-dependent manner. J. Biol. Chem. 2013, 288, 36083–36093. [Google Scholar] [CrossRef]
- Contin, C.; Pitard, V.; Itai, T.; Nagata, S.; Moreau, J.F.; Dechanet-Merville, J. Membrane-anchored CD40 is processed by the tumor necrosis factor-alpha-converting enzyme. Implications for CD40 signaling. J. Biol. Chem. 2003, 278, 32801–32809. [Google Scholar] [CrossRef]
- Melter, M.; Reinders, M.E.; Sho, M.; Pal, S.; Geehan, C.; Denton, M.D.; Mukhopadhyay, D.; Briscoe, D.M. Ligation of CD40 induces the expression of vascular endothelial growth factor by endothelial cells and monocytes and promotes angiogenesis in vivo. Blood 2000, 96, 3801–3808. [Google Scholar] [CrossRef]
- Reinders, M.E.; Sho, M.; Robertson, S.W.; Geehan, C.S.; Briscoe, D.M. Proangiogenic function of CD40 ligand-CD40 interactions. J. Immunol. 2003, 171, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Deregibus, M.C.; Buttiglieri, S.; Russo, S.; Bussolati, B.; Camussi, G. CD40-dependent activation of phosphatidylinositol 3-kinase/Akt pathway mediates endothelial cell survival and in vitro angiogenesis. J. Biol. Chem. 2003, 278, 18008–18014. [Google Scholar] [CrossRef]
- Portillo, J.A.; Greene, J.A.; Okenka, G.; Miao, Y.; Sheibani, N.; Kern, T.S.; Subauste, C.S. CD40 promotes the development of early diabetic retinopathy in mice. Diabetologia 2014, 57, 2222–2231. [Google Scholar] [CrossRef] [PubMed]
- Dierschke, S.K.; Toro, A.L.; Miller, W.P.; Sunilkumar, S.; Dennis, M.D. Diabetes enhances translation of CD40 mRNA in murine retinal Müller glia via a 4E-BP1/2-dependent mechanism. J. Biol. Chem. 2020, 295, 10831–10841. [Google Scholar] [CrossRef]
- Bringmann, A.; Pannicke, T.; Grosche, J.; Francke, M.; Wiedemann, P.; Skatchkov, S.N.; Osborne, N.N.; Reichenbach, A. Müller cells in the healthy and diseased retina. Prog. Retin. Eye Res. 2006, 25, 397–424. [Google Scholar] [CrossRef] [PubMed]
- Portillo, J.A.; Schwartz, I.; Zarini, S.; Bapputty, R.; Kern, T.S.; Gubitosi-Klug, R.A.; Murphy, R.C.; Subauste, M.C.; Subauste, C.S. Proinflammatory responses induced by CD40 in retinal endothelial and Müller cells are inhibited by blocking CD40-Traf2,3 or CD40-Traf6 signaling. Investig. Ophthalmol. Vis. Sci. 2014, 55, 8590–8597. [Google Scholar] [CrossRef]
- D’Aversa, T.G.; Eugenin, E.A.; Berman, J.W. CD40-CD40 ligand interactions in human microglia induce CXCL8 (interleukin-8) secretion by a mechanism dependent on activation of ERK1/2 and nuclear translocation of nuclear factor-ĸB (NFĸB) and activator protein-1 (AP-1). J. Neurosci. Res. 2008, 86, 630–639. [Google Scholar] [CrossRef][Green Version]
- Barbe-Tuana, F.M.; Klein, D.; Ichii, H.; Berman, D.M.; Coffey, L.; Kenyon, N.S.; Ricordi, C.; Pastori, R.L. CD40-CD40 ligand interaction activates proinflammatory pathways in pancreatic islets. Diabetes 2006, 55, 2437–2445. [Google Scholar] [CrossRef]
- Saito, M.; Ota, Y.; Ohashi, H.; Dei, Y.; Shimoyama, K.; Suzuki, D.; Hayashi, H.; Ogawa, N. CD40-CD40 ligand signal induces the intercellular adhesion molecule-1 expression through nuclear factor-ĸB p50 in cultured salivary gland epithelial cells from patients with Sjögren’s syndrome. Mod. Rheumatol. 2007, 17, 45–53. [Google Scholar] [CrossRef]
- Zhao, L.Q.; Wei, R.L.; Cheng, J.W.; Cai, J.P.; Li, Y. The expression of intercellular adhesion molecule-1 induced by CD40-CD40L ligand signaling in orbital fibroblasts in patients with Graves’ ophthalmopathy. Invest. Ophthalmol. Vis. Sci. 2010, 51, 4652–4660. [Google Scholar] [CrossRef]
- Gillespie, E.F.; Raychaudhuri, N.; Papageorgiou, K.I.; Atkins, S.J.; Lu, Y.; Charara, L.K.; Mester, T.; Smith, T.J.; Douglas, R.S. Interleukin-6 production in CD40-engaged fibrocytes in thyroid-associated ophthalmopathy: Involvement of Akt and NF-ĸB. Investig. Ophthalmol. Vis. Sci. 2012, 53, 7746–7753. [Google Scholar] [CrossRef]
- Wu, Z.; Zhao, G.; Peng, L.; Du, J.; Wang, S.; Huang, Y.; Ou, J.; Jian, Z. Protein kinase C beta mediates CD40 ligand-induced adhesion of monocytes to endothelial cells. PLoS ONE 2013, 8, e72593. [Google Scholar] [CrossRef] [PubMed]
- Flaxenburg, J.A.; Melter, M.; Lapchak, P.H.; Briscoe, D.M.; Pal, S. The CD40-induced signaling pathway in endothelial cells resulting in the overexpression of vascular endothelial growth factor involves Ras and phosphatidylinositol 3-kinase. J. Immunol. 2004, 172, 7503–7509. [Google Scholar] [CrossRef] [PubMed]
- Dormond, O.; Contreras, A.G.; Meijer, E.; Datta, D.; Flynn, E.; Pal, S.; Briscoe, D.M. CD40-induced signaling in human endothelial cells results in mTORC2- and Akt-dependent expression of vascular endothelial growth factor in vitro and in vivo. J. Immunol. 2008, 181, 8088–8095. [Google Scholar] [CrossRef]
- Cho, C.S.; Cho, M.L.; Min, S.Y.; Kim, W.U.; Min, D.J.; Lee, S.S.; Park, S.H.; Choe, J.; Kim, H.Y. CD40 engagement on synovial fibroblast up-regulates production of vascular endothelial growth factor. J. Immunol. 2000, 164, 5055–5061. [Google Scholar] [CrossRef] [PubMed]
- Futagami, S.; Tatsuguchi, A.; Hiratsuka, T.; Shindo, T.; Horie, A.; Hamamoto, T.; Ueki, N.; Kusunoki, M.; Miyake, K.; Gudis, K.; et al. Monocyte chemoattractant protein 1 and CD40 ligation have a synergistic effect on vascular endothelial growth factor production through cyclooxygenase 2 upregulation in gastric cancer. J. Gastroenterol. 2008, 43, 216–224. [Google Scholar] [CrossRef]
- Mach, F.; Schönbeck, U.; Fabunmi, R.P.; Murphy, C.; Atkinson, E.; Bonnefoy, J.Y.; Graber, P.; Libby, P. T lymphocytes induce endothelial cell matrix metalloproteinase expression by a CD40L-dependent mechanism: Implications for tubule formation. Am. J. Pathol. 1999, 154, 229–238. [Google Scholar] [CrossRef]
- Greene, J.A.; Portillo, J.A.; Lopez Corcino, Y.; Subauste, C.S. CD40-TRAF signaling upregulates CX3CL1 and TNF-alpha in human aortic endothelial cells but not in retinal endothelial cells. PLoS ONE 2015, 10, e0144133. [Google Scholar] [CrossRef]
- Marx, N.; Imhof, A.; Froehlich, J.; Siam, L.; Ittner, J.; Wierse, G.; Schmidt, A.; Maerz, W.; Hombach, V.; Koenig, W. Effect of rosiglitazone treatment on soluble CD40L in patients with type 2 diabetes and coronary artery disease. Circulation 2003, 107, 1954–1957. [Google Scholar] [CrossRef]
- Jinchuan, Y.; Zonggui, W.; Jinming, C.; Li, L.; Xiantao, K. Upregulation of CD40--CD40 ligand system in patients with diabetes mellitus. Clin. Chim. Acta 2004, 339, 85–90. [Google Scholar] [CrossRef]
- Cipollone, F.; Chiarelli, F.; Davi, G.; Ferri, C.; Desideri, G.; Fazia, M.; Iezzi, A.; Santilli, F.; Pini, B.; Cuccurullo, C.; et al. Enhanced soluble CD40 ligand contributes to endothelial cell dysfunction in vitro and monocyte activation in patients with diabetes mellitus: Effect of improved metabolic control. Diabetologia 2005, 48, 1216–1224. [Google Scholar] [CrossRef] [PubMed]
- Neubauer, H.; Setiadi, P.; Gunesdogan, B.; Pinto, A.; Borgel, J.; Mugge, A. Influence of glycaemic control on platelet bound CD40-CD40L system, P-selectin and soluble CD40 ligand in Type 2 diabetes. Diabet. Med. 2010, 27, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Krzesz, R.; Wagner, A.H.; Cattaruzza, M.; Hecker, M. Cytokine-inducible CD40 gene expression in vascular smooth muscle cells is mediated by nuclear factor kappaB and signal transducer and activation of transcription-1. FEBS Lett. 1999, 453, 191–196. [Google Scholar] [CrossRef]
- De Zutter, A.; Crijns, H.; Berghmans, N.; Garcia-Caballero, M.; Vanbrabant, L.; Pörtner, N.; Vanheule, V.; Verscheure, P.; Siddiquei, M.M.; Abu El-Asrar, A.M.; et al. The Chemokine-Based Peptide, CXCL9(74-103), Inhibits Angiogenesis by Blocking Heparan Sulfate Proteoglycan-Mediated Signaling of Multiple Endothelial Growth Factors. Cancers 2021, 13, 5090. [Google Scholar] [CrossRef] [PubMed]
- De Zutter, A.; Dillemans, L.; Berghmans, N.; Noppen, S.; Crijns, H.; Verscheure, P.; Verhaegen, J.; Martens, E.; Vanbrabant, L.; Pörtner, N.; et al. A stabilized CXCL9(74-103)-derived peptide selectively inhibits proliferation, adhesion and metastasis of tumor cells that express high levels of heparan sulfate. Int. J. Biol. Macromol. 2022, 222 Pt B, 2808–2822. [Google Scholar] [CrossRef]
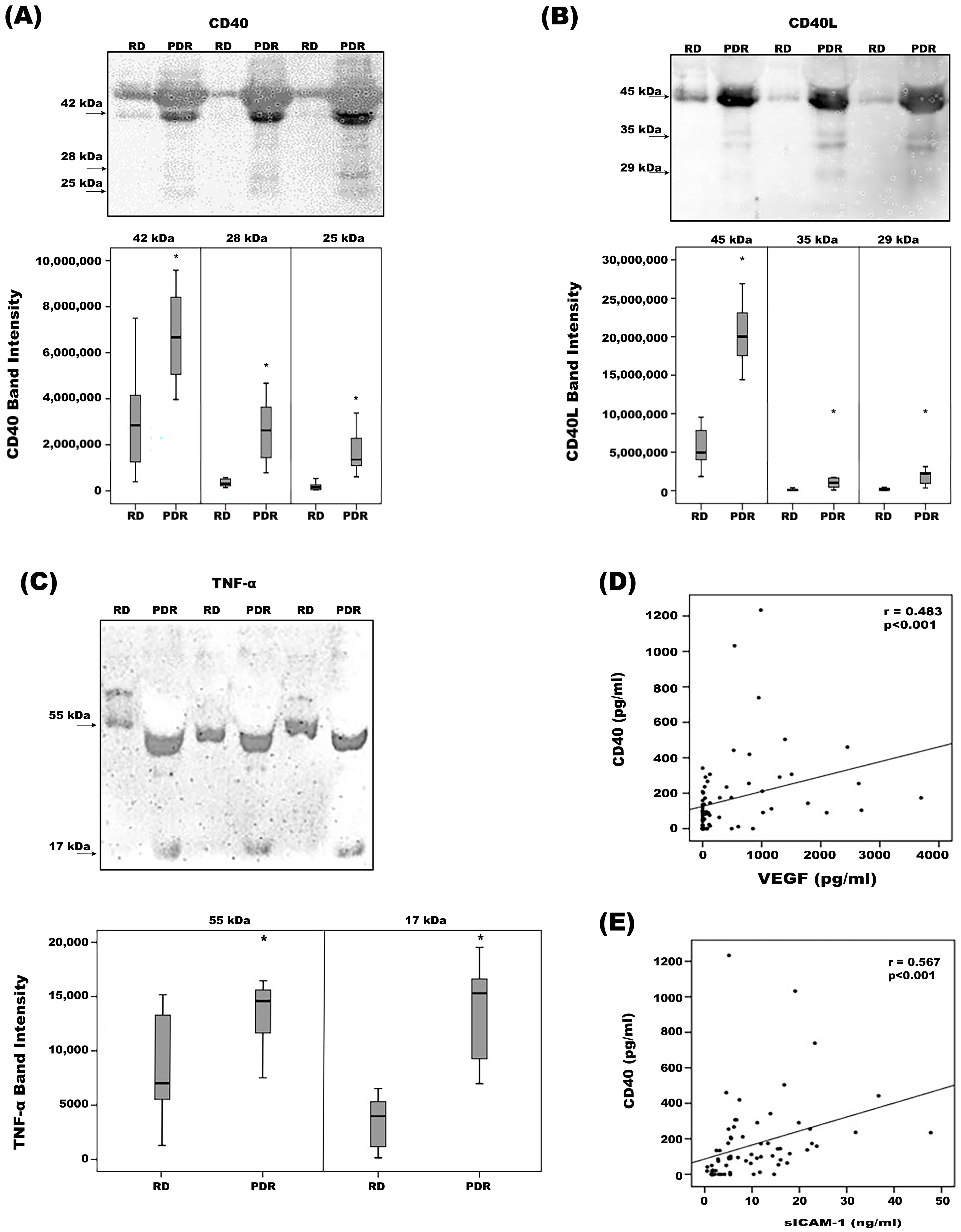





| PDR (n = 38) Median (IQR) | RD (n = 32) Median (IQR) | p-Value (Mann–Whitney Test) | |
|---|---|---|---|
| CD40 | 173.00 (90.4–290.63) | 21.65 (<DL–97.38) | <0.001 * |
| (pg/mL) | |||
| VEGF | 446.25 (47.7–1013.02) | <DL (<DL–56.6) | <0.001 * |
| (pg/mL) | |||
| sICAM-1 | 11.07 (5.29–17.56) | 3.07 (1.67–9.48) | <0.001 * |
| (ng/mL) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abu El-Asrar, A.M.; Nawaz, M.I.; Ahmad, A.; Dillemans, L.; Siddiquei, M.; Allegaert, E.; Gikandi, P.W.; De Hertogh, G.; Opdenakker, G.; Struyf, S. CD40 Ligand–CD40 Interaction Is an Intermediary between Inflammation and Angiogenesis in Proliferative Diabetic Retinopathy. Int. J. Mol. Sci. 2023, 24, 15582. https://doi.org/10.3390/ijms242115582
Abu El-Asrar AM, Nawaz MI, Ahmad A, Dillemans L, Siddiquei M, Allegaert E, Gikandi PW, De Hertogh G, Opdenakker G, Struyf S. CD40 Ligand–CD40 Interaction Is an Intermediary between Inflammation and Angiogenesis in Proliferative Diabetic Retinopathy. International Journal of Molecular Sciences. 2023; 24(21):15582. https://doi.org/10.3390/ijms242115582
Chicago/Turabian StyleAbu El-Asrar, Ahmed M., Mohd I. Nawaz, Ajmal Ahmad, Luna Dillemans, Mairaj Siddiquei, Eef Allegaert, Priscilla W. Gikandi, Gert De Hertogh, Ghislain Opdenakker, and Sofie Struyf. 2023. "CD40 Ligand–CD40 Interaction Is an Intermediary between Inflammation and Angiogenesis in Proliferative Diabetic Retinopathy" International Journal of Molecular Sciences 24, no. 21: 15582. https://doi.org/10.3390/ijms242115582
APA StyleAbu El-Asrar, A. M., Nawaz, M. I., Ahmad, A., Dillemans, L., Siddiquei, M., Allegaert, E., Gikandi, P. W., De Hertogh, G., Opdenakker, G., & Struyf, S. (2023). CD40 Ligand–CD40 Interaction Is an Intermediary between Inflammation and Angiogenesis in Proliferative Diabetic Retinopathy. International Journal of Molecular Sciences, 24(21), 15582. https://doi.org/10.3390/ijms242115582







