The Potential Role of Nitric Oxide as a Therapeutic Agent against SARS-CoV-2 Infection
Abstract
1. Introduction
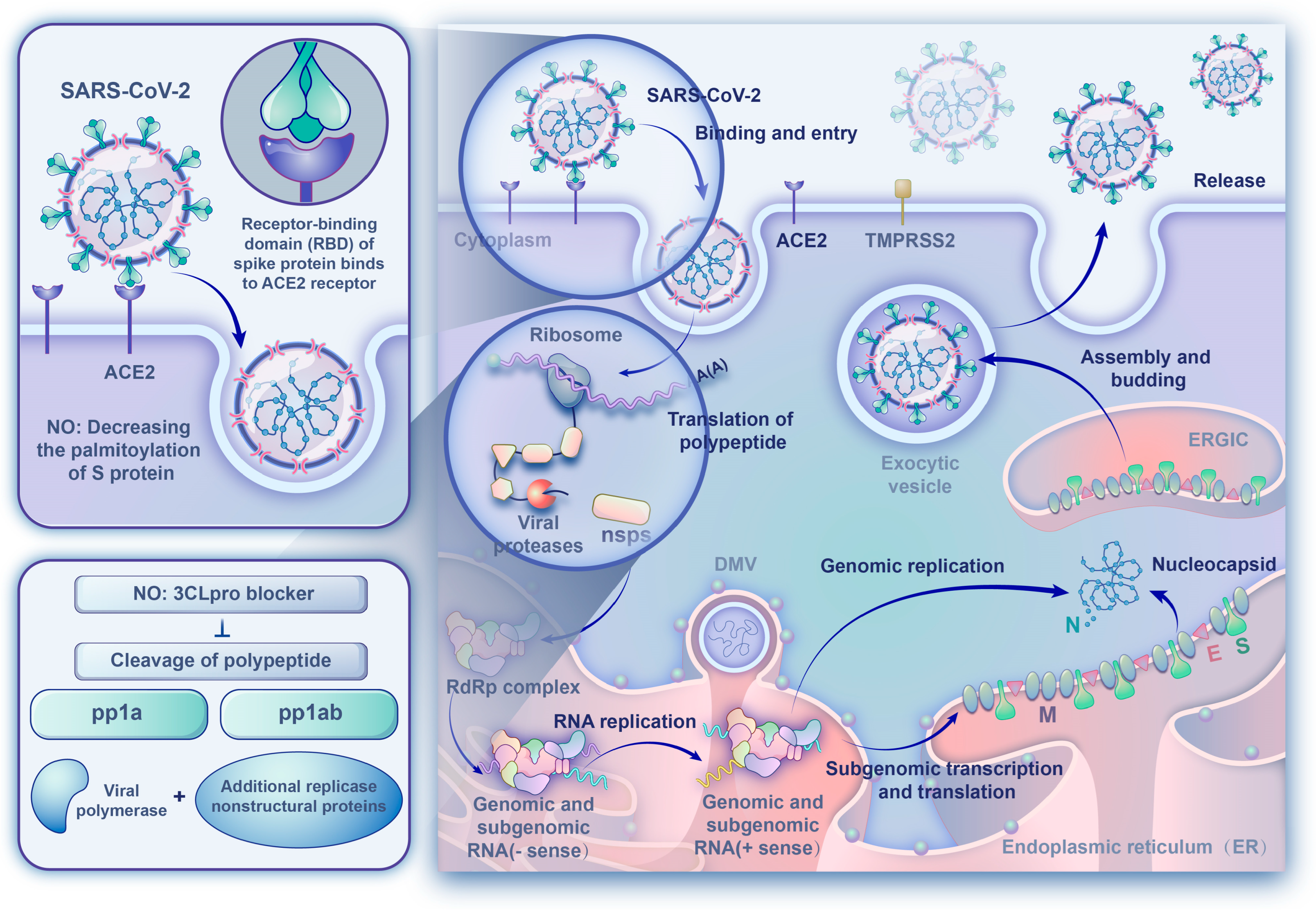
2. SARS-CoV-2 and COVID-19
3. Role of NO in SARS-CoV-2 Infection
3.1. Antiviral Effect
- (1)
- NO decreased the palmitoylation level of S protein, thereby interfering with binding to the target receptor on the host cell. Three different studies demonstrated the potential of NO compounds in the inhibition of SARS-CoV replication in a concentration-dependent manner [30,64,65], and the effect of NO on S protein was also investigated. The results showed that the NO donor-S-nitroso-N-acetylpenicillamine (SNAP) treatment significantly reduced the number of palmitoylated S protein, and the intercellular fusion was significantly decreased. Also, the entry efficiency of the pseudo-type virus was significantly lower after SNAP treatment, and the virus infection rate decreased by about 70% [30].
- (2)
- NO affected replication-related cysteine proteases which directly inhibited viral RNA replication. Similar to the Coxsackievirus 3C cysteine protease, SARS-CoV-2 3CL cysteine protease may be a potential target for S-nitrosation, causing a suppression of the protease activity and a resultant decrease in viral replication [56]. The in vitro study by Akaberi et al. showed that SARS-CoV-2 3CL recombinant protease was covalently inhibited by SNAP through the transfer of nitrosonium ions (NO+s) to the protease cysteine residue, and the observed reduction in SARS-CoV-2 protease activity was consistent with S-nitrosylation of the enzyme active site cysteine. Although the viral replication was not completely abolished, SNAP delayed or completely prevented the development of the viral cytopathic effect in treated cells [31]. In addition, the analysis of proteolytic degradation of the viral polypeptide showed that the content of the nucleocapsid N protein was drastically decreased in the presence of SNAP and that high-molar-mass (non-processed) polypeptide content was increased [30,65].
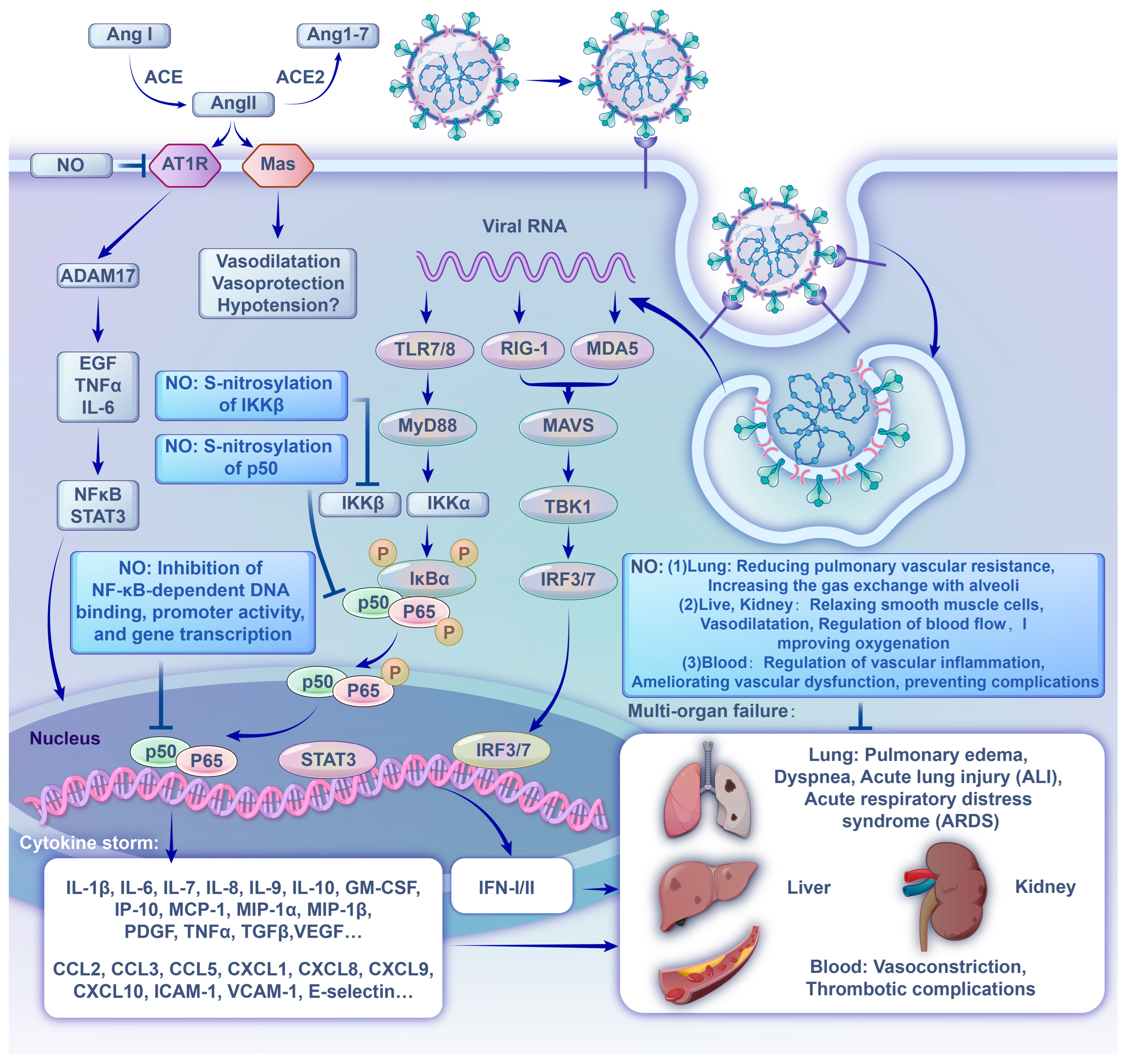
3.2. Effect on Inflammation
3.3. Effects on Vasodilation
4. Application of NO in Clinical Treatment of COVID-19
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abrams, E.M.; Szefler, S.J. COVID-19 and the impact of social determinants of health. Lancet Respir. Med. 2020, 8, 659–661. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. COVID-19 Dashboard. 2023. Available online: https://covid19.who.int/ (accessed on 16 August 2023).
- Wang, Y.; Tian, H.; Zhang, L.; Zhang, M.; Guo, D.; Wu, W.; Zhang, X.; Kan, G.L.; Jia, L.; Huo, D.; et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: A cohort study in Beijing, China. BMJ Glob. Health 2020, 5, e002794. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, J. Lifestyle-mediated nitric oxide boost to prevent SARS-CoV-2 infection: A perspective. Nitric Oxide 2021, 115, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Alkafaas, S.S.; Abdallah, A.M.; Hussien, A.M.; Bedair, H.; Abdo, M.; Ghosh, S.; Elkafas, S.S.; Apollon, W.; Saki, M.; Loutfy, S.A.; et al. A study on the effect of natural products against the transmission of B.1.1.529 Omicron. Virol. J. 2023, 20, 191. [Google Scholar] [CrossRef] [PubMed]
- Kamenshchikov, N.O.; Berra, L.; Carroll, R.W. Therapeutic Effects of Inhaled Nitric Oxide Therapy in COVID-19 Patients. Biomedicines 2022, 10, 369. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Aldhahir, A.M.; Al Ghamdi, S.S.; AlBahrani, S.; AlDraiwiesh, I.A.; Alqarni, A.A.; Latief, K.; Raya, R.P.; Oyelade, T. Inhaled Nitric Oxide for Clinical Management of COVID-19: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 12803. [Google Scholar] [CrossRef] [PubMed]
- Rousseaud, A.; Prot, M.; Loriere, E.S.; Katz, I.; Ramirez-Gil, J.F.; Farjot, G. Gaseous nitric oxide failed to inhibit the replication cycle of SARS-CoV-2 in vitro. Nitric Oxide 2023, 132, 27–33. [Google Scholar] [CrossRef]
- Fehr, A.R.; Perlman, S. Coronaviruses: An overview of their replication and pathogenesis. Methods Mol. Biol. 2015, 1282, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Lu, R.; Zhao, X.; Li, J.; Niu, P.; Yang, B.; Wu, H.; Wang, W.; Song, H.; Huang, B.; Zhu, N.; et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020, 395, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.-M.; Wang, W.; Song, Z.-G.; Hu, Y.; Tao, Z.-W.; Tian, J.-H.; Pei, Y.-Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, Q.; Guo, D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J. Med. Virol. 2020, 92, 2249. [Google Scholar] [CrossRef]
- Bartlam, M.; Xu, Y.; Rao, Z. Structural proteomics of the SARS coronavirus: A model response to emerging infectious diseases. J. Struct. Funct. Genom. 2007, 8, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Ziebuhr, J. Molecular biology of severe acute respiratory syndrome coronavirus. Curr. Opin. Microbiol. 2004, 7, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.C.; Lau, S.K.; Woo, P.C.; Yuen, K.Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin. Microbiol. Rev. 2007, 20, 660–694. [Google Scholar] [CrossRef] [PubMed]
- Zumla, A.; Hui, D.S.; Perlman, S. Middle East respiratory syndrome. Lancet 2015, 386, 995–1007. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Wu, C.; Li, X.; Song, Y.; Yao, X.; Wu, X.; Duan, Y.; Zhang, H.; Wang, Y.; Qian, Z.; et al. On the origin and continuing evolution of SARS-CoV-2. Natl. Sci. Rev. 2020, 7, 1012–1023. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zhou, Q.; Li, Y.; Garner, L.V.; Watkins, S.P.; Carter, L.J.; Smoot, J.; Gregg, A.C.; Daniels, A.D.; Jervey, S.; et al. Research and Development on Therapeutic Agents and Vaccines for COVID-19 and Related Human Coronavirus Diseases. ACS Cent. Sci. 2020, 6, 315–331. [Google Scholar] [CrossRef]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Takahashi, N.; Abe, R.; Hattori, N.; Matsumura, Y.; Oshima, T.; Taniguchi, T.; Igari, H.; Nakada, T.-A. Clinical course of a critically ill patient with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). J. Artif. Organs 2020, 23, 397–400. [Google Scholar] [CrossRef]
- Pascarella, G.; Strumia, A.; Piliego, C.; Bruno, F.; Del Buono, R.; Costa, F.; Scarlata, S.; Agrò, F.E. COVID-19 diagnosis and management: A comprehensive review. J. Intern. Med. 2020, 288, 192–206. [Google Scholar] [CrossRef]
- Callender, L.A.; Curran, M.; Bates, S.M.; Mairesse, M.; Weigandt, J.; Betts, C.J. The Impact of Pre-existing Comorbidities and Therapeutic Interventions on COVID-19. Front. Immunol. 2020, 11, 1991. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhao, Z.; Wang, Y.; Zhou, Y.; Ma, Y.; Zuo, W. Single-Cell RNA Expression Profiling of ACE2, the Receptor of SARS-CoV-2. Am. J. Respir. Crit. Care Med. 2020, 202, 756–759, Erratum in Am. J. Respir. Crit. Care Med. 2021, 203, 782. [Google Scholar] [CrossRef] [PubMed]
- Qi, F.; Qian, S.; Zhang, S.; Zhang, Z. Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem. Biophys. Res. Commun. 2020, 526, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Zhang, Y.; Wu, L.; Niu, S.; Song, C.; Zhang, Z.; Lu, G.; Qiao, C.; Hu, Y.; Yuen, K.Y.; et al. Structural and Functional Basis of SARS-CoV-2 Entry by Using Human ACE2. Cell 2020, 181, 894–904. [Google Scholar] [CrossRef] [PubMed]
- Örd, M.; Faustova, I.; Loog, M. The sequence at Spike S1/S2 site enables cleavage by furin and phospho-regulation in SARS-CoV2 but not in SARS-CoV1 or MERS-CoV. Sci. Rep. 2020, 10, 16944. [Google Scholar] [CrossRef]
- Shulla, A.; Heald-Sargent, T.; Subramanya, G.; Zhao, J.; Perlman, S.; Gallagher, T. A Transmembrane serine protease is linked to the severe acute respiratory syndrome coronavirus receptor and activates virus entry. J. Virol. 2011, 85, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Berardi, M.; Li, W.; Farzan, M.; Dormitzer, P.R.; Harrison, S.C. Conformational states of the severe acute respiratory syndrome coronavirus spike protein ectodomain. J. Virol. 2006, 80, 6794–6800. [Google Scholar] [CrossRef]
- Harrison, A.G.; Lin, T.; Wang, P. Mechanisms of SARS-CoV-2 Transmission and Pathogenesis. Trends Immunol. 2020, 41, 1100–1115. [Google Scholar] [CrossRef]
- Åkerström, S.; Gunalan, V.; Keng, C.T.; Tan, Y.-J.; Mirazimi, A. Dual effect of nitric oxide on SARS-CoV replication: Viral RNA production and palmitoylation of the S protein are affected. Virology 2009, 395, 1–9. [Google Scholar] [CrossRef]
- Akaberi, D.; Krambrich, J.; Ling, J.; Luni, C.; Hedenstierna, G.; Järhult, J.D.; Lennerstrand, J.; Lundkvist, Å. Mitigation of the replication of SARS-CoV-2 by nitric oxide in vitro. Redox Biol. 2020, 37, 101734. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Geng, M.; Peng, Y.; Meng, L.; Lu, S. Molecular immune pathogenesis and diagnosis of COVID-19. J. Pharm. Anal. 2020, 10, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Hunter, C.A.; Jones, S.A. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 2015, 16, 448–457, Erratum in Nat. Immunol. 2017, 18, 1271. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Narazaki, M.; Kishimoto, T. Immunotherapeutic implications of IL-6 blockade for cytokine storm. Immunotherapy 2016, 8, 959–970. [Google Scholar] [CrossRef] [PubMed]
- Rothan, H.A.; Byrareddy, S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020, 109, 102433. [Google Scholar] [CrossRef]
- Blanco-Melo, D.; Nilsson-Payant, B.E.; Liu, W.-C.; Uhl, S.; Hoagland, D.; Møller, R.; Jordan, T.X.; Oishi, K.; Panis, M.; Sachs, D.; et al. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell 2020, 181, 1036–1045. [Google Scholar] [CrossRef] [PubMed]
- England, J.T.; Abdulla, A.; Biggs, C.M.; Lee, A.Y.Y.; Hay, K.A.; Hoiland, R.L.; Wellington, C.L.; Sekhon, M.; Jamal, S.; Shojania, K.; et al. Weathering the COVID-19 storm: Lessons from hematologic cytokine syndromes. Blood Rev. 2021, 45, 100707. [Google Scholar] [CrossRef]
- A Clark, I. The advent of the cytokine storm. Immunol. Cell Biol. 2007, 85, 271–273. [Google Scholar] [CrossRef]
- Hirano, T.; Murakami, M. COVID-19: A New Virus, but a Familiar Receptor and Cytokine Release Syndrome. Immunity 2020, 52, 731–733. [Google Scholar] [CrossRef]
- Shenoy, S. Coronavirus (Covid-19) sepsis: Revisiting mitochondrial dysfunction in pathogenesis, aging, inflammation, and mortality. Inflamm. Res. 2020, 69, 1077–1085. [Google Scholar] [CrossRef]
- Chang, R.; Mamun, A.; Dominic, A.; Le, N.-T. SARS-CoV-2 Mediated Endothelial Dysfunction: The Potential Role of Chronic Oxidative Stress. Front. Physiol. 2021, 11, 605908. [Google Scholar] [CrossRef]
- Croen, K.D. Evidence for antiviral effect of nitric oxide. Inhibition of herpes simplex virus type 1 replication. J. Clin. Investig. 1993, 91, 2446–2452. [Google Scholar] [CrossRef]
- Karupiah, G.; Xie, Q.W.; Buller, R.M.; Nathan, C.; Duarte, C.; MacMicking, J.D. Inhibition of viral replication by interferon-gamma-induced nitric oxide synthase. Science 1993, 261, 1445–1448. [Google Scholar] [CrossRef]
- Akarid, K.; Sinet, M.; Desforges, B.; Gougerot-Pocidalo, M.A. Inhibitory effect of nitric oxide on the replication of a murine retrovirus in vitro and in vivo. J. Virol. 1995, 69, 7001–7005. [Google Scholar] [CrossRef]
- Bi, Z.; Reiss, C.S. Inhibition of vesicular stomatitis virus infection by nitric oxide. J. Virol. 1995, 69, 2208–2213. [Google Scholar] [CrossRef]
- Harris, N.; Buller, R.M.; Karupiah, G. Gamma interferon-induced, nitric oxide-mediated inhibition of vaccinia virus replication. J. Virol. 1995, 69, 910–915. [Google Scholar] [CrossRef] [PubMed]
- Karupiah, G.; Harris, N. Inhibition of viral replication by nitric oxide and its reversal by ferrous sulfate and tricarboxylic acid cycle metabolites. J. Exp. Med. 1995, 181, 2171–2179. [Google Scholar] [CrossRef]
- Mĕlková, Z.; Esteban, M. Inhibition of vaccinia virus DNA replication by inducible expression of nitric oxide synthase. J. Immunol. 1995, 155, 5711–5718. [Google Scholar] [CrossRef]
- Hermann, E.; Idziorek, T.; Kusnierz, J.-P.; Mouton, Y.; Capron, A.; Bahr, G.M. Role of nitric oxide in the regulation of lymphocyte apoptosis and HIV-1 replication. Int. J. Immunopharmacol. 1997, 19, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.L.; Huang, Y.L.; Ma, S.H.; Yeh, C.T.; Chiou, S.Y.; Chen, L.K.; Liao, C.L. Inhibition of Japanese encephalitis virus infection by nitric oxide: Antiviral effect of nitric oxide on RNA virus replication. J. Virol. 1997, 71, 5227–5235. [Google Scholar] [CrossRef] [PubMed]
- Zaragoza, C.; Ocampo, C.J.; Saura, M.; McMillan, A.; Lowenstein, C.J. Nitric oxide inhibition of coxsackievirus replication in vitro. J. Clin. Investig. 1997, 100, 1760–1767. [Google Scholar] [CrossRef]
- Karupiah, G.; Chen, J.-H.; Nathan, C.F.; Mahalingam, S.; MacMicking, J.D. Identification of nitric oxide synthase 2 as an innate resistance locus against ectromelia virus infection. J. Virol. 1998, 72, 7703–7706. [Google Scholar] [CrossRef]
- Persichini, T.; Colasanti, M.; Lauro, G.M.; Ascenzi, P. Cysteine nitrosylation inactivates the HIV-1 protease. Biochem. Biophys. Res. Commun. 1998, 250, 575–576. [Google Scholar] [CrossRef] [PubMed]
- Sanders, S.P.; Siekierski, E.S.; Porter, J.D.; Richards, S.M.; Proud, D. Nitric oxide inhibits rhinovirus-induced cytokine production and viral replication in a human respiratory epithelial cell line. J. Virol. 1998, 72, 934–942. [Google Scholar] [CrossRef]
- Rimmelzwaan, G.F.; Baars, M.M.; de Lijster, P.; Fouchier, R.A.; Osterhaus, A.D. Inhibition of influenza virus replication by nitric oxide. J. Virol. 1999, 73, 8880–8883. [Google Scholar] [CrossRef]
- Saura, M.; Zaragoza, C.; McMillan, A.; Quick, R.A.; Hohenadl, C.; Lowenstein, J.M.; Lowenstein, C.J. An antiviral mechanism of nitric oxide: Inhibition of a viral protease. Immunity 1999, 10, 21–28. [Google Scholar] [CrossRef]
- Flodström, M.; Horwitz, M.S.; Maday, A.; Balakrishna, D.; Rodriguez, E.; Sarvetnick, N. A critical role for inducible nitric oxide synthase in host survival following coxsackievirus B4 infection. Virology 2001, 281, 205–215. [Google Scholar] [CrossRef]
- Noda, S.; Tanaka, K.; Sawamura, S.-A.; Sasaki, M.; Matsumoto, T.; Mikami, K.; Aiba, Y.; Hasegawa, H.; Kawabe, N.; Koga, Y. Role of nitric oxide synthase type 2 in acute infection with murine cytomegalovirus. J. Immunol. 2001, 166, 3533–3541. [Google Scholar] [CrossRef]
- Sanders, S.P.; Kim, J.; Connolly, K.R.; Porter, J.D.; Siekierski, E.S.; Proud, D. Nitric oxide inhibits rhinovirus-induced granulocyte macrophage colony-stimulating factor production in bronchial epithelial cells. Am. J. Respir. Cell Mol. Biol. 2001, 24, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Baniecki, M.L.; McGrath, W.J.; Bao, C.; Deming, C.B.; Rade, J.J.; Lowenstein, C.J.; Mangel, W.F. Nitric oxide inhibits the adenovirus proteinase in vitro and viral infectivity in vivo. FASEB J. 2003, 17, 2345–2346. [Google Scholar] [CrossRef]
- Klingström, J.; Åkerström, S.; Hardestam, J.; Stoltz, M.; Simon, M.; Falk, K.I.; Mirazimi, A.; Rottenberg, M.; Lundkvist, A. Nitric oxide and peroxynitrite have different antiviral effects against hantavirus replication and free mature virions. Eur. J. Immunol. 2006, 36, 2649–2657. [Google Scholar] [CrossRef] [PubMed]
- Regev-Shoshani, G.; Vimalanathan, S.; McMullin, B.; Road, J.; Av-Gay, Y.; Miller, C. Gaseous nitric oxide reduces influenza infectivity in vitro. Nitric Oxide 2013, 31, 48–53. [Google Scholar] [CrossRef]
- Jung, K.; Gurnani, A.; Renukaradhya, G.J.; Saif, L.J. Nitric oxide is elicited and inhibits viral replication in pigs infected with porcine respiratory coronavirus but not porcine reproductive and respiratory syndrome virus. Vet. Immunol. Immunopathol. 2010, 136, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Keyaerts, E.; Vijgen, L.; Chen, L.; Maes, P.; Hedenstierna, G.; Van Ranst, M. Inhibition of SARS-coronavirus infection in vitro by S-nitroso-N-acetylpenicillamine, a nitric oxide donor compound. Int. J. Infect. Dis. 2004, 8, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Åkerström, S.; Mousavi-Jazi, M.; Klingström, J.; Leijon, M.; Lundkvist, A.; Mirazimi, A. Nitric oxide inhibits the replication cycle of severe acute respiratory syndrome coronavirus. J. Virol. 2005, 79, 1966–1969. [Google Scholar] [CrossRef]
- Alberty, J.; Stoll, W.; Rudack, C. The effect of endogenous nitric oxide on mechanical ciliostimulation of human nasal mucosa. Clin. Exp. Allergy 2006, 36, 1254–1259. [Google Scholar] [CrossRef]
- Moilanen, E.; Vapaatalo, H. Nitric oxide in inflammation and immune response. Ann. Med. 1995, 27, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Koetzler, R.; Zaheer, R.S.; Wiehler, S.; Holden, N.S.; Giembycz, M.A.; Proud, D. Nitric oxide inhibits human rhinovirus-induced transcriptional activation of CXCL10 in airway epithelial cells. J. Allergy Clin. Immunol. 2009, 123, 201–208.e9. [Google Scholar] [CrossRef] [PubMed]
- Guzik, T.J.; Korbut, R.; Adamek-Guzik, T. Nitric oxide and superoxide in inflammation and immune regulation. J. Physiol. Pharmacol. 2003, 54, 469–487. [Google Scholar]
- Kircheis, R.; Haasbach, E.; Lueftenegger, D.; Heyken, W.T.; Ocker, M.; Planz, O. NF-κB Pathway as a Potential Target for Treatment of Critical Stage COVID-19 Patients. Front. Immunol. 2020, 11, 598444. [Google Scholar] [CrossRef]
- Hess, D.T.; Matsumoto, A.; Kim, S.-O.; Marshall, H.E.; Stamler, J.S. Protein S-nitrosylation: Purview and parameters. Nat. Rev. Mol. Cell Biol. 2005, 6, 150–166. [Google Scholar] [CrossRef]
- Reynaert, N.L.; Ckless, K.; Korn, S.H.; Vos, N.; Guala, A.S.; Wouters, E.F.; van der Vliet, A.; Janssen-Heininger, Y.M. Nitric oxide represses inhibitory κB kinase through S-nitrosylation. Proc. Natl. Acad. Sci. USA 2004, 101, 8945–8950. [Google Scholar] [CrossRef] [PubMed]
- Coleman, J.W. Nitric oxide in immunity and inflammation. Int. Immunopharmacol. 2001, 1, 1397–1406. [Google Scholar] [CrossRef] [PubMed]
- Mannick, J.B. Immunoregulatory and antimicrobial effects of nitrogen oxides. Proc. Am. Thorac. Soc. 2006, 3, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Tejero, J.; Shiva, S.; Gladwin, M.T. Sources of Vascular Nitric Oxide and Reactive Oxygen Species and Their Regulation. Physiol. Rev. 2019, 99, 311–379. [Google Scholar] [CrossRef] [PubMed]
- Leclerc, P.C.; Lanctot, P.M.; Auger-Messier, M.; Escher, E.; Leduc, R.; Guillemette, G. S-nitrosylation of cysteine 289 of the AT1 receptor decreases its binding affinity for angiotensin II. Br. J. Pharmacol. 2006, 148, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, L.C.; Oliveira-Paula, G.H.; Ferreira, G.C.; Dal-Cin de Paula, T.; Duarte, D.A.; Costa-Neto, C.M.; Tanus-Santos, J.E. Oral nitrite treatment increases S-nitrosylation of vascular protein kinase C and attenuates the responses to angiotensin II. Redox Biol. 2021, 38, 101769. [Google Scholar] [CrossRef]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal Coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef]
- Green, S.J. Covid-19 accelerates endothelial dysfunction and nitric oxide deficiency. Microbes Infect. 2020, 22, 149–150. [Google Scholar] [CrossRef]
- Hottz, E.D.; Azevedo-Quintanilha, I.G.; Palhinha, L.; Teixeira, L.; Barreto, E.A.; Pão, C.R.R.; Righy, C.; Franco, S.; Souza, T.M.L.; Kurtz, P.; et al. Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood 2020, 136, 1330–1341. [Google Scholar] [CrossRef]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020, 97, 829–838. [Google Scholar] [CrossRef]
- Akter, F.; Coghlan, G.; de Mel, A. Nitric oxide in paediatric respiratory disorders: Novel interventions to address associated vascular phenomena? Ther. Adv. Cardiovasc. Dis. 2016, 10, 256–270. [Google Scholar] [CrossRef]
- Friebe, A.; Sandner, P.; Schmidtko, A. cGMP: A unique 2nd messenger molecule—Recent developments in cGMP research and development. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2020, 393, 287–302. [Google Scholar] [CrossRef] [PubMed]
- Ricciardolo, F.L. Multiple roles of nitric oxide in the airways. Thorax 2003, 58, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Dattilo, J.B.; Makhoul, R.G. The role of nitric oxide in vascular biology and pathobiology. Ann. Vasc. Surg. 1997, 11, 307–314. [Google Scholar] [CrossRef]
- Cabrales, P.; Tsai, A.G.; Frangos, J.A.; Intaglietta, M. Role of endothelial nitric oxide in microvascular oxygen delivery and consumption. Free Radic. Biol. Med. 2005, 39, 1229–1237. [Google Scholar] [CrossRef]
- Kvietys, P.R.; Granger, D.N. Role of reactive oxygen and nitrogen species in the vascular responses to inflammation. Free Radic. Biol. Med. 2012, 52, 556–592. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Liu, P.; Gao, H.; Sun, B.; Chao, D.; Wang, F.; Zhu, Y.; Hedenstierna, G.; Wang, C.G. Inhalation of nitric oxide in the treatment of severe acute respiratory syndrome: A rescue trial in Beijing. Clin. Infect. Dis. 2004, 39, 1531–1535. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Winchester, S.; John, S.; Jabbar, K.; John, I. Clinical efficacy of nitric oxide nasal spray (NONS) for the treatment of mild COVID-19 infection. J. Infect. 2021, 83, 237–279. [Google Scholar] [CrossRef]
- Cardinale, M.; Esnault, P.; Cotte, J.; Cungi, P.J.; Goutorbe, P. Effect of almitrine bismesylate and inhaled nitric oxide on oxygenation in COVID-19 acute respiratory distress syndrome. Anaesth. Crit. Care Pain Med. 2020, 39, 471–472. [Google Scholar] [CrossRef]
- Lotz, C.; Muellenbach, R.M.; Meybohm, P.; Mutlak, H.; Lepper, P.M.; Rolfes, C.B.; Peivandi, A.; Stumpner, J.; Kredel, M.; Kranke, P.; et al. Effects of inhaled nitric oxide in COVID-19–induced ARDS—Is it worthwhile? Acta Anaesthesiol. Scand. 2021, 65, 629–632. [Google Scholar] [CrossRef]
- Al Sulaiman, K.; Korayem, G.B.; Altebainawi, A.F.; Al Harbi, S.; Alissa, A.; Alharthi, A.; Kensara, R.; Alfahed, A.; Vishwakarma, R.; Al Haji, H.; et al. Evaluation of inhaled nitric oxide (iNO) treatment for moderate-to-severe ARDS in critically ill patients with COVID-19: A multicenter cohort study. Crit. Care 2022, 26, 304. [Google Scholar] [CrossRef]
- Safaee Fakhr, B.; Wiegand, S.B.; Pinciroli, R.; Gianni, S.; Morais, C.C.A.; Ikeda, T.; Miyazaki, Y.; Marutani, E.; Di Fenza, R.; Larson, G.M.; et al. High Concentrations of Nitric Oxide Inhalation Therapy in Pregnant Patients with Severe Coronavirus Disease 2019 (COVID-19). Obstet. Gynecol. 2020, 136, 1109–1113. [Google Scholar] [CrossRef]
- Valsecchi, C.; Winterton, D.; Safaee Fakhr, B.; Collier, A.Y.; Nozari, A.; Ortoleva, J.; Mukerji, S.; Gibson, L.E.; Carroll, R.W.; Shaefi, S.; et al. High-Dose Inhaled Nitric Oxide for the Treatment of Spontaneously Breathing Pregnant Patients with Severe Coronavirus Disease 2019 (COVID-19) Pneumonia. Obstet. Gynecol. 2022, 140, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Bobot, M.; Tonon, D.; Peres, N.; Guervilly, C.; Lefèvre, F.; Max, H.; Bommel, Y.; Volff, M.; Leone, M.; Lopez, A.; et al. Impact of Dexamethasone and Inhaled Nitric Oxide on Severe Acute Kidney Injury in Critically Ill Patients with COVID-19. J. Clin. Med. 2022, 11, 6130. [Google Scholar] [CrossRef] [PubMed]
- Feng, W.X.; Yang, Y.; Wen, J.; Liu, Y.X.; Liu, L.; Feng, C. Implication of inhaled nitric oxide for the treatment of critically ill COVID-19 patients with pulmonary hypertension. ESC Heart Fail. 2021, 8, 714–718. [Google Scholar] [CrossRef]
- Bonizzoli, M.; Lazzeri, C.; Cianchi, G.; Guetti, C.; Fulceri, G.E.; Socci, F.; Peris, A. Effects of rescue inhaled nitric oxide on right ventricle and pulmonary circulation in severe COVID-related acute respiratory distress syndrome. J. Crit. Care 2022, 72, 153987. [Google Scholar] [CrossRef]
- Caplan, M.; Goutay, J.; Bignon, A.; Jaillette, E.; Favory, R.; Mathieu, D.; Parmentier-Decrucq, E.; Poissy, J.; Duburcq, T.; Lille Intensive Care COVID-19 Group. Almitrine Infusion in Severe Acute Respiratory Syndrome Coronavirus 2-Induced Acute Respiratory Distress Syndrome: A Single-Center Observational Study. Crit. Care Med. 2020, 49, e191–e198. [Google Scholar] [CrossRef] [PubMed]
- Abou-Arab, O.; Huette, P.; Debouvries, F.; Dupont, H.; Jounieaux, V.; Mahjoub, Y. Inhaled nitric oxide for critically ill Covid-19 patients: A prospective study. Crit. Care 2020, 24, 645. [Google Scholar] [CrossRef]
- Ferrari, M.; Santini, A.; Protti, A.; Andreis, D.T.; Iapichino, G.; Castellani, G.; Rendiniello, V.; Costantini, E.; Cecconi, M. Inhaled nitric oxide in mechanically ventilated patients with COVID-19. J. Crit. Care 2020, 60, 159–160. [Google Scholar] [CrossRef]
- Tavazzi, G.; Pozzi, M.; Mongodi, S.; Dammassa, V.; Romito, G.; Mojoli, F. Inhaled nitric oxide in patients admitted to intensive care unit with COVID-19 pneumonia. Crit. Care 2020, 24, 665. [Google Scholar] [CrossRef]
- Herranz, L.; da Silveira, J.G.; Trocado, L.F.L.; Alvaraes, A.L.; Fittipaldi, J. Inhaled Nitric Oxide in Patients with Severe COVID-19 Infection at Intensive Care Unit—A Cross Sectional Study. J. Crit. Care Med. 2021, 7, 318–319. [Google Scholar] [CrossRef]
- Parikh, R.; Wilson, C.; Weinberg, J.; Gavin, D.; Murphy, J.; Reardon, C.C. Inhaled nitric oxide treatment in spontaneously breathing COVID-19 patients. Ther. Adv. Respir. Dis. 2020, 14, 1753466620933510. [Google Scholar] [CrossRef] [PubMed]
- Chandel, A.; Patolia, S.; Ahmad, K.; Aryal, S.; Brown, A.W.; Sahjwani, D.; Khangoora, V.; Shlobin, O.A.; Cameron, P.C.; Singhal, A.; et al. Inhaled Nitric Oxide via High-Flow Nasal Cannula in Patients with Acute Respiratory Failure Related to COVID-19. Clin. Med. Insights Circ. Respir. Pulm. Med. 2021, 15, 11795484211047065. [Google Scholar] [CrossRef] [PubMed]
- Lubinsky, A.S.; Brosnahan, S.B.; Lehr, A.; Elnadoury, O.; Hagedorn, J.; Garimella, B.; Bender, M.T.; Amoroso, N.; Artigas, A.; Bos, L.D.J.; et al. Inhaled pulmonary vasodilators are not associated with improved gas exchange in mechanically ventilated patients with COVID-19: A retrospective cohort study. J. Crit. Care 2022, 69, 153990. [Google Scholar] [CrossRef] [PubMed]
- DeGrado, J.R.; Szumita, P.M.; Schuler, B.R.; Dube, K.M.; Lenox, J.; Kim, E.Y.; Weinhouse, G.L.; Massaro, A.F. Evaluation of the Efficacy and Safety of Inhaled Epoprostenol and Inhaled Nitric Oxide for Refractory Hypoxemia in Patients with Coronavirus Disease 2019. Crit. Care Explor. 2020, 2, e0259. [Google Scholar] [CrossRef]
- Longobardo, A.; Montanari, C.; Shulman, R.; Benhalim, S.; Singer, M.; Arulkumaran, N. Inhaled nitric oxide minimally improves oxygenation in COVID-19 related acute respiratory distress syndrome. Br. J. Anaesth. 2021, 126, e44–e46. [Google Scholar] [CrossRef] [PubMed]
- Robba, C.; Ball, L.; Battaglini, D.; Cardim, D.; Moncalvo, E.; Brunetti, I.; Bassetti, M.; Giacobbe, D.R.; Vena, A.; Patroniti, N.; et al. Early effects of ventilatory rescue therapies on systemic and cerebral oxygenation in mechanically ventilated COVID-19 patients with acute respiratory distress syndrome: A prospective observational study. Crit. Care 2021, 25, 111. [Google Scholar] [CrossRef] [PubMed]
- Matthews, L.; Baker, L.; Ferrari, M.; Sanchez, W.; Pappachan, J.; Grocott, M.P.; Dushianthan, A.; The REACT COVID-19 Investigators. Compassionate use of Pulmonary Vasodilators in Acute Severe Hypoxic Respiratory Failure due to COVID-19. J. Intensiv. Care Med. 2022, 37, 1101–1111. [Google Scholar] [CrossRef]
- Safaee Fakhr, B.; Di Fenza, R.; Gianni, S.; Wiegand, S.B.; Miyazaki, Y.; Araujo Morais, C.C.; Gibson, L.E.; Chang, M.G.; Mueller, A.L.; Rodriguez-Lopez, J.M.; et al. Inhaled high dose nitric oxide is a safe and effective respiratory treatment in spontaneous breathing hospitalized patients with COVID-19 pneumonia. Nitric Oxide 2021, 116, 7–13. [Google Scholar] [CrossRef]
- Heuts, S.; Ubben, J.F.; Banks-Gonzales, V.; Sels, J.-W.; Lorusso, R.; van Mook, W.N.; Delnoij, T.S. Nitric Oxide Ventilation Improves Recirculation and Right Ventricular Function During Veno-Venous Extracorporeal Membrane Oxygenation in a COVID-19 Patient. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2763–2767. [Google Scholar] [CrossRef]
- Garfield, B.; McFadyen, C.; Briar, C.; Bleakley, C.; Vlachou, A.; Baldwin, M.; Lees, N.; Price, S.; Ledot, S.; McCabe, C.; et al. Potential for personalised application of inhaled nitric oxide in COVID-19 pneumonia. Br. J. Anaesth. 2021, 126, e72–e75. [Google Scholar] [CrossRef] [PubMed]
- Lei, C.; Su, B.; Dong, H.; Fakhr, B.S.; Grassi, L.G.; Di Fenza, R.; Gianni, S.; Pinciroli, R.; Vassena, E.; Morais, C.C.A.; et al. Protocol for a randomized controlled trial testing inhaled nitric oxide therapy in spontaneously breathing patients with COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Abman, S.H.; Fox, N.R.; Malik, M.I.; Kelkar, S.S.; Corman, S.L.; Rege, S.; Bhaloo, J.; Shah, R.; Shei, R.-J.; Saporito, D.; et al. Real-world use of inhaled nitric oxide therapy in patients with COVID-19 and mild-to-moderate acute respiratory distress syndrome. Drugs Context 2022, 11, 1–4. [Google Scholar] [CrossRef]
- Bagate, F.; Tuffet, S.; Masi, P.; Perier, F.; Razazi, K.; de Prost, N.; Carteaux, G.; Payen, D.; Mekontso Dessap, A. Rescue therapy with inhaled nitric oxide and almitrine in COVID-19 patients with severe acute respiratory distress syndrome. Ann. Intensiv. Care 2020, 10, 151. [Google Scholar] [CrossRef] [PubMed]
- Ziehr, D.R.; Alladina, J.; Wolf, M.E.; Brait, K.L.; Malhotra, A.; La Vita, C.; Berra, L.; Hibbert, K.A.; Hardin, C.C. Respiratory Physiology of Prone Positioning with and without Inhaled Nitric Oxide Across the Coronavirus Disease 2019 Acute Respiratory Distress Syndrome Severity Spectrum. Crit. Care Explor. 2021, 3, e0471. [Google Scholar] [CrossRef] [PubMed]
- Strickland, B.; Albala, L.; Coffey, E.C.; Carroll, R.W.; Zapol, W.M.; Ichinose, F.; Berra, L.; Harris, N.S. Safety and practicality of high dose inhaled nitric oxide in emergency department COVID-19 patients. Am. J. Emerg. Med. 2022, 58, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Tandon, M.; Wu, W.; Moore, K.; Winchester, S.; Tu, Y.-P.; Miller, C.; Kodgule, R.; Pendse, A.; Rangwala, S.; Joshi, S.; et al. SARS-CoV-2 accelerated clearance using a novel nitric oxide nasal spray (NONS) treatment: A randomized trial. Lancet Reg. Health Southeast Asia 2022, 3, 100036, Erratum in Lancet Reg. Health Southeast Asia 2022, 7, 100110. [Google Scholar] [CrossRef]
- Laghlam, D.; Rahoual, G.; Malvy, J.; Estagnasié, P.; Brusset, A.; Squara, P. Use of Almitrine and Inhaled Nitric Oxide in ARDS Due to COVID-19. Front. Med. 2021, 8, 655763. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, S.B.; Safaee Fakhr, B.; Carroll, R.W.; Zapol, W.M.; Kacmarek, R.M.; Berra, L. Rescue Treatment with High-Dose Gaseous Nitric Oxide in Spontaneously Breathing Patients with Severe Coronavirus Disease 2019. Crit. Care Explor. 2020, 2, e0277. [Google Scholar] [CrossRef] [PubMed]
- Gianni, S.; Fakhr, B.S.; Araujo Morais, C.C.; Raffaele, D.F.; Grant, L.; Riccardo, P.; Timothy, H.; Ariel, L.M.; Andrea, B.; Robert, K.; et al. Nitric oxide gas inhalation to prevent COVID-2019 in healthcare providers. medRxiv 2020. [Google Scholar] [CrossRef]
- Zamanian, R.T.; Pollack, C.V., Jr.; Gentile, M.A.; Rashid, M.; Fox, J.C.; Mahaffey, K.W.; de Jesus Perez, V. Outpatient Inhaled Nitric Oxide in a Patient with Vasoreactive Idiopathic Pulmonary Arterial Hypertension and COVID-19 Infection. Am. J. Respir. Crit. Care Med. 2020, 202, 130–132. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, R.A.; Berra, L.; Gladwin, M.T. Home Nitric Oxide Therapy for COVID-19. Am. J. Respir. Crit. Care Med. 2020, 202, 16–20. [Google Scholar] [CrossRef]
- Lee, H.-Y.; Zeeshan, H.M.A.; Kim, H.-R.; Chae, H.-J. Nox4 regulates the eNOS uncoupling process in aging endothelial cells. Free Radic. Biol. Med. 2017, 113, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Csoma, B.; Bikov, A.; Nagy, L.; Tóth, B.; Tábi, T.; Szűcs, G.; Komlósi, Z.I.; Müller, V.; Losonczy, G.; Lázár, Z. Dysregulation of the endothelial nitric oxide pathway is associated with airway inflammation in COPD. Respir. Res. 2019, 20, 156. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, B.; Yazici, A. Could the decrease in the endothelial nitric oxide (NO) production and NO bioavailability be the crucial cause of COVID-19 related deaths? Med. Hypotheses 2020, 144, 109970. [Google Scholar] [CrossRef] [PubMed]
- Bohlen, H.G. Nitric oxide and the cardiovascular system. Compr. Physiol. 2015, 5, 808–823. [Google Scholar] [CrossRef]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481, Erratum in Lancet Respir. Med. 2020, 8, e26. [Google Scholar] [CrossRef]
- Banerjee, A.; Pasea, L.; Harris, S.; Gonzalez-Izquierdo, A.; Torralbo, A.; Shallcross, L.; Noursadeghi, M.; Pillay, D.; Sebire, N.; Holmes, C.; et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: A population-based cohort study. Lancet 2020, 395, 1715–1725. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, R.T.; Lynch, J.B.; Del Rio, C. Mild or Moderate Covid-19. N. Engl. J. Med. 2020, 383, 1757–1766. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Tian, S.; Chen, T.; Cui, Z.; Shi, N.; Zhong, X.; Qiu, K.; Zhang, J.; Zeng, T.; Chen, L.; et al. Newly diagnosed diabetes is associated with a higher risk of mortality than known diabetes in hospitalized patients with COVID-19. Diabetes Obes. Metab. 2020, 22, 1897–1906. [Google Scholar] [CrossRef]
- Ignarro, L.J. Inhaled NO and COVID-19. Br. J. Pharmacol. 2020, 177, 3848–3849. [Google Scholar] [CrossRef] [PubMed]
| Experimental Design | Dose | Duration | Sample Size | Finding | Reference | |
|---|---|---|---|---|---|---|
| 1 | Double-blind randomized study | 120–140 μL of solution/spray | 24 h/72 h | 80 | NONS accelerated the reduction in SARS-CoV-2 RNA load versus a control with saline spray. | [89] |
| 2 | Retrospective study | 10–20 ppm (parts per million) | 5–13 days | 20 | The use of NO or almitrine bismesylate or both did not improve oxygenation in moderate to severe COVID-19 ARDS, but the result remains to be confirmed by a study on a larger cohort of patients. | [90] |
| 3 | Retrospective observational study | 20 ppm | 15–30 min | 7 | iNO provided immediate help and delayed respiratory deterioration in COVID-19-induced moderate to severe ARDS. | [91] |
| 4 | Multicenter, retrospective cohort study | 20–40.0 ppm | 24 h–30 days | 1598 | In critically ill COVID-19 patients with moderate-to-severe ARDS, iNO rescue therapy is related to improved oxygenation parameters but no mortality benefits. | [92] |
| 5 | Retrospective observational study | 160–200 ppm | 30 min–1 h | 6 | High-dose iNO was well tolerated and improved oxygenation and respiratory rate for pregnant patients with severe or critical COVID-19. | [93] |
| 6 | Retrospective cohort study | 200 ppm, 30 min | twice daily, 23–26 days | 71 | iNO treatment improves respiratory function and outcomes among pregnant patients hospitalized with severe COVID-19 pneumonia. | [94] |
| 7 | Multicentric cohort study | 5–30 ppm | 2–11 days | 164 | iNO was related to severe AKI and RRT in critically ill patients with COVID-19. | [95] |
| 8 | Retrospective observational study | 10–20 ppm | 24–30 days | 5 | iNO treatment was beneficial in reducing and stabilizing the PASP and reduced the risk of right heart failure in patients with COVID-19 with pulmonary hypertension. | [96] |
| 9 | Observational study | 40 ppm | 24 h | 12 | COVID-19-related severe ARDS iNO administrated as rescue therapy cannot ameliorate oxygenation nor pulmonary hypertension. | [97] |
| 10 | Single-center retrospective observational study | 10 ppm | 2–5 days | 32 | Almitrine often used in combination with iNO improves oxygenation in patients with SARS-CoV-2-induced ARDS without side effects, and in the case of life-threatening refractory hypoxemia, almitrine alone or in combination with iNO could be a good time saver. | [98] |
| 11 | Single-center prospective study | 10 ppm | 15–30 min | 34 | iNO improves PaO2/FiO2 ventilation/perfusion in the majority of patients with COVID-19 and severe pneumonia. | [99] |
| 12 | Observational study | 20 ppm | 30 min | 10 | iNO relieves hypoxemia in mechanically ventilated COVID-19 patients. | [100] |
| 13 | Single-center, observational study | 20–30 ppm | 15–30 min | 72 | iNO induced an improvement in oxygenation and cardiac output. | [101] |
| 14 | Retrospective cross-sectional study | 20–40 ppm | 2–7 days | 34 | iNO is an auxiliary therapy that can increase the PaO2/FiO2 ratio in SARS-COV-2 mechanical ventilated critically ill patients without major side effects. | [102] |
| 15 | Single-center observational study | 30 ppm | 2.1 days | 39 | iNO therapy prevents the progression of hypoxic respiratory failure in patients with COVID-19. | [103] |
| 16 | Multicenter cohort study | 20–40 ppm | 44–135 h | 272 | iNO therapy improved oxygenation in spontaneously breathing patients with COVID-19. | [104] |
| 17 | Retrospective cohort study | 10–40 ppm | 6 days | 84 | iNOs are not associated with improved gas exchange in mechanically ventilated patients with COVID-19. | [105] |
| 18 | Single-center retrospective study | 20–30 ppm | 18–72 h | 38 | A group of patients showed a significant improvement with inhaled nitric oxide. The administration of inhaled nitric oxide may be considered in patients with severe respiratory failure secondary to COVID-19. | [106] |
| 19 | Single-center retrospective case–control study | 10–20 ppm | 24 h | 154 | iNO improves oxygenation in COVID-19-related acute respiratory distress syndrome. | [107] |
| 20 | Prospective observational study | 20 ppm | 1 h | 22 | iNO and prone positioning improved systemic and cerebral oxygenation. | [108] |
| 21 | Retrospective study | 20–40 ppm | 2–72 h | 59 | Both iNO and prostaglandins can be used in patients with COVID-19 with severe refractory hypoxaemia. | [109] |
| 22 | Multicenter interventional study | 160 ppm, 30 min | twice daily, 4–8 days | 29 | A high dose of iNO is helpful in spontaneously breathing patients with COVID-19. | [110] |
| 23 | Observational study | 20–30 ppm | 24 h | 1 | Continuous iNO-enriched ventilation was effective in a patient with COVID-19 on veno-venous ECMO. | [111] |
| 24 | Retrospective observational study | 20 ppm | 5 days | 35 | iNO can be used in patients with COVID-19 with refractory hypoxaemia. | [112] |
| 25 | Multicenter randomized study | 140–180 ppm for 30 min | 2 sessions every day for 14 days | 1260 | A protocol was developed to treat patients with COVID-19 with NO in RCTs. | [113] |
| 26 | Retrospective observational study | 9–40 ppm, ≥24 h | 3–9 days | 37 | iNO is helpful for the treatment of mild-to-moderate ARDS in patients with COVID-19. | [114] |
| 27 | Monocentric prospective study | 10 ppm, 30 min | 5–15 days | 10 | The iNO-almitrine combination is effective in oxygenation improvement. | [115] |
| 28 | Single-center, retrospective cohort study | 20–80 ppm | 2–36 h | 122 | Prone positioning is helpful in oxygenation among patients treated with iNO. | [116] |
| 29 | Randomized study | 250 ppm, 30 min | 28 days | 47 | Single high-dose iNO is effective in patients with acute respiratory symptoms. | [117] |
| 30 | Multicenter randomized study | 0.45 mL/dose | six time daily, 7 days | 306 | NONS accelerates nasal virus clearance in patients with COVID-19. | [118] |
| 31 | Single-center, open- label, observational study | 10 ppm, 30 min | 3–19 days | 12 | The combination of iNO and almitrine improved short-term oxygenation in patients with COVID-19. | [119] |
| 32 | Single-center, retrospective observational study | 160 ppm, 30 min | twice daily, 1–9 days | 5 | Gaseous NO is a useful adjuvant rescue therapy for patients with COVID-19. | [120] |
| 33 | Single-center, randomized study | 160 ppm, 15 min | twice daily, 14 days | 470 | Inhalation of NO can prevent COVID-19 among healthcare workers. | [121] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiao, S.; Yuan, Z.; Huang, Y. The Potential Role of Nitric Oxide as a Therapeutic Agent against SARS-CoV-2 Infection. Int. J. Mol. Sci. 2023, 24, 17162. https://doi.org/10.3390/ijms242417162
Xiao S, Yuan Z, Huang Y. The Potential Role of Nitric Oxide as a Therapeutic Agent against SARS-CoV-2 Infection. International Journal of Molecular Sciences. 2023; 24(24):17162. https://doi.org/10.3390/ijms242417162
Chicago/Turabian StyleXiao, Shuqi, Zhiming Yuan, and Yi Huang. 2023. "The Potential Role of Nitric Oxide as a Therapeutic Agent against SARS-CoV-2 Infection" International Journal of Molecular Sciences 24, no. 24: 17162. https://doi.org/10.3390/ijms242417162
APA StyleXiao, S., Yuan, Z., & Huang, Y. (2023). The Potential Role of Nitric Oxide as a Therapeutic Agent against SARS-CoV-2 Infection. International Journal of Molecular Sciences, 24(24), 17162. https://doi.org/10.3390/ijms242417162






