Association between 20% Albumin Use and Acute Kidney Injury in Major Abdominal Surgery with Transfusion
Abstract
1. Introduction
2. Results
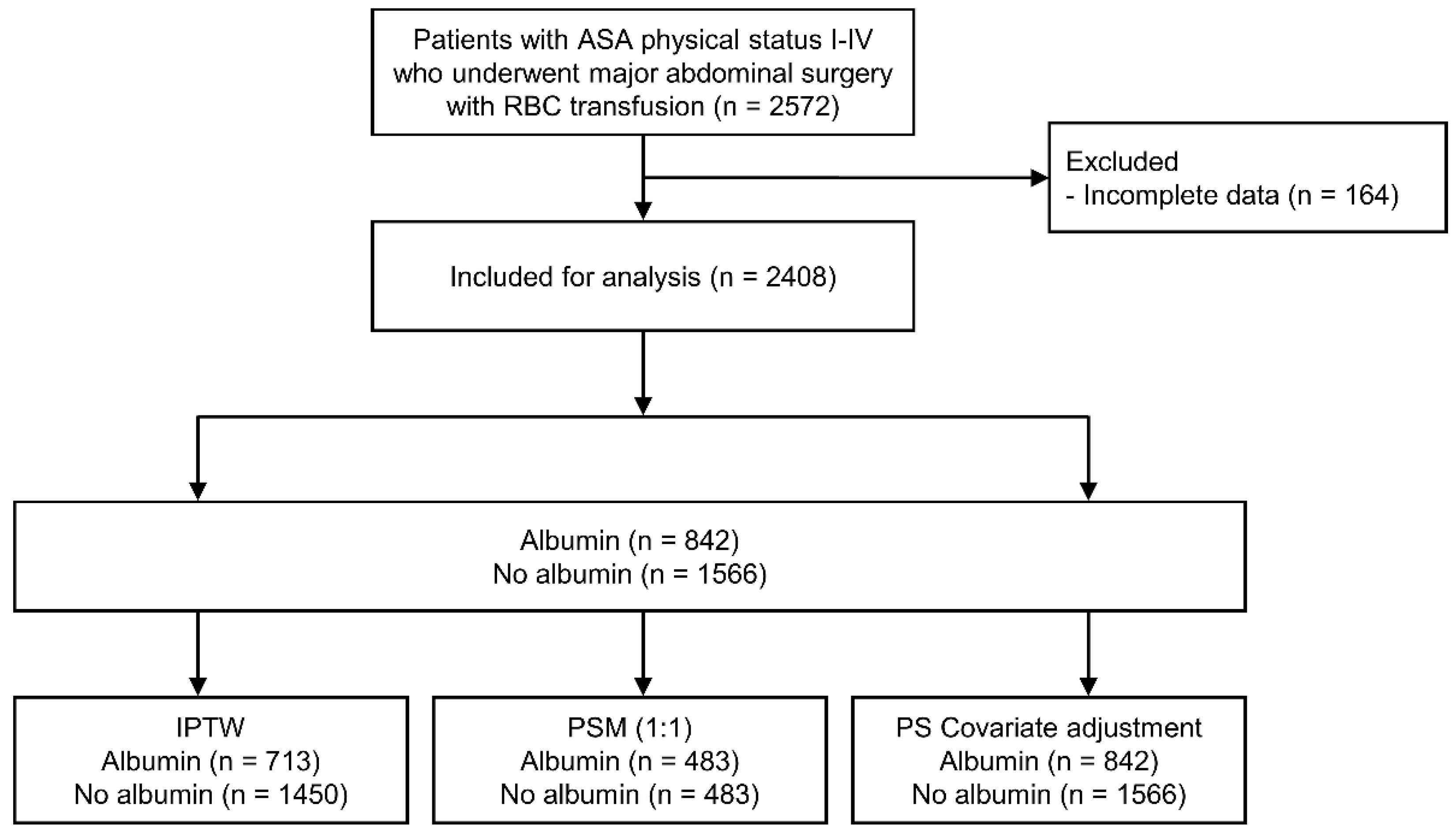
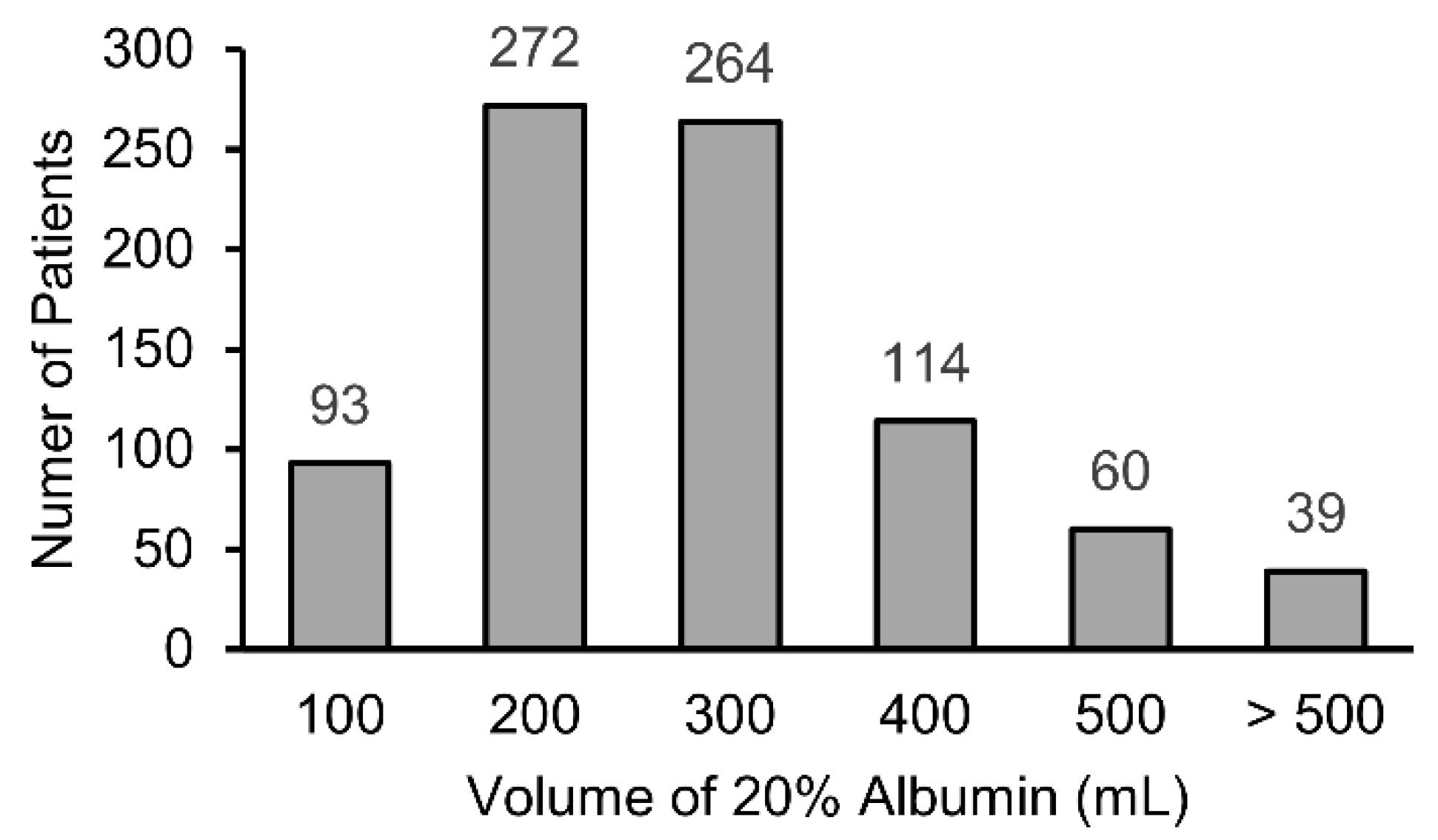
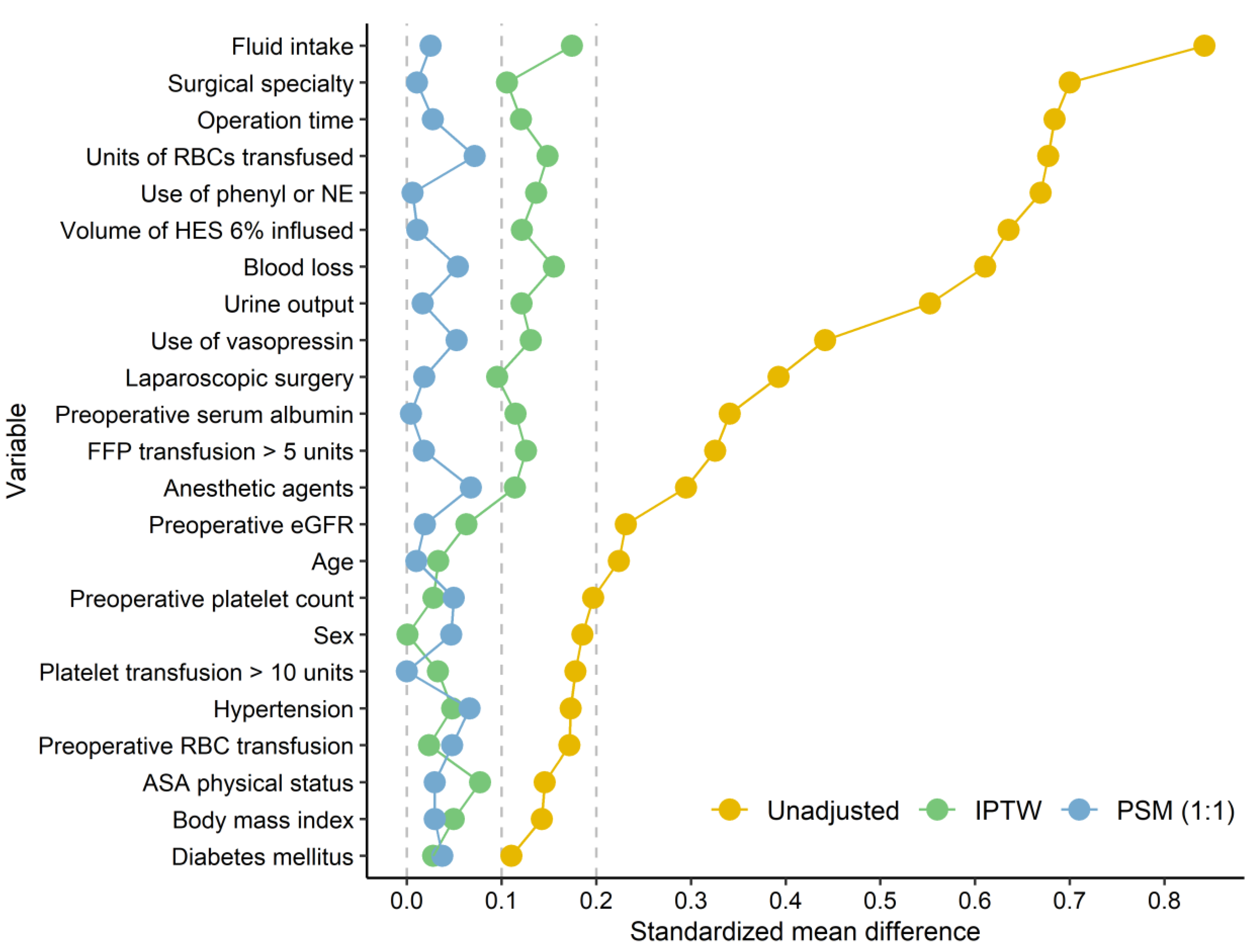
2.1. Study Cohort and Patient Characteristics
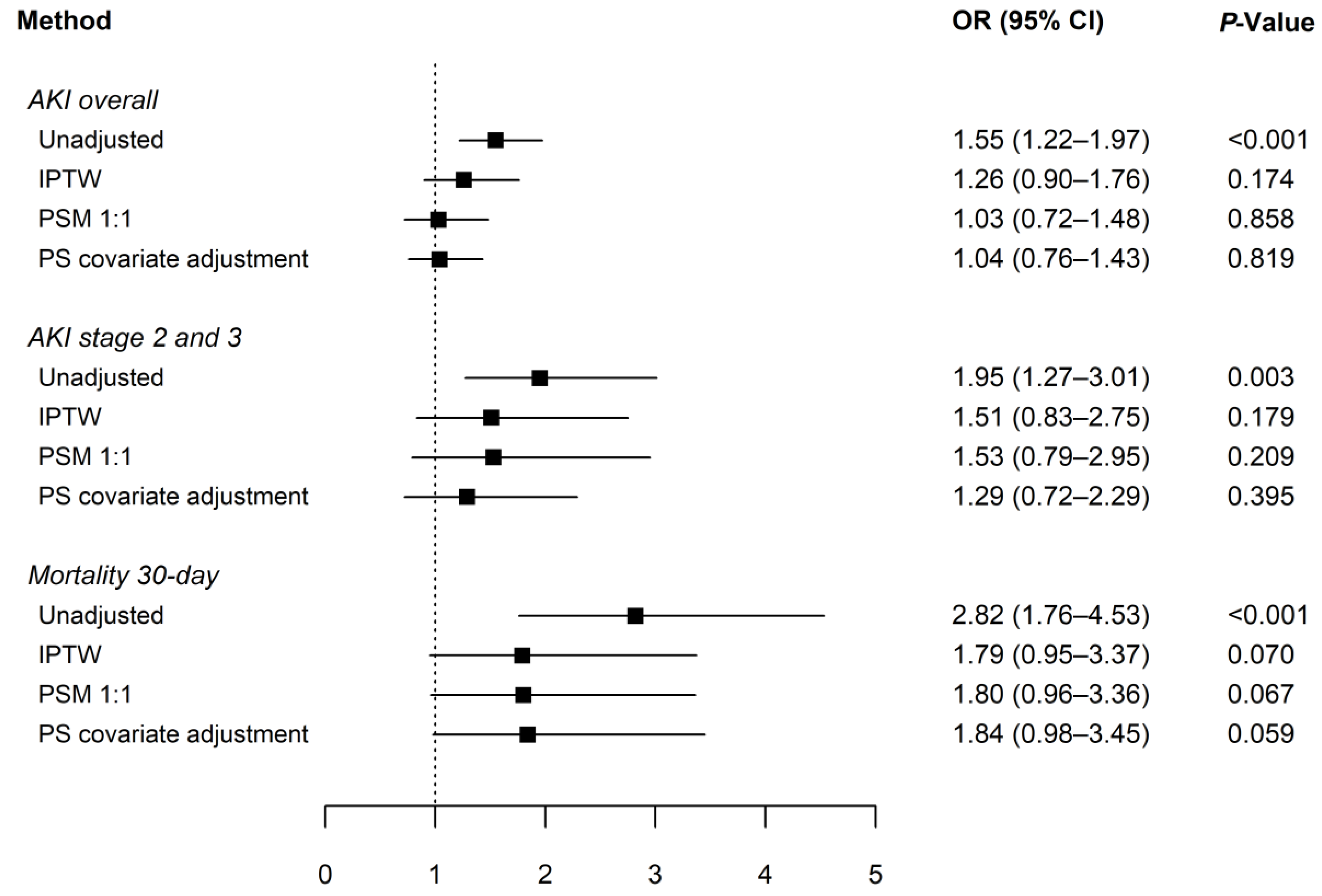
2.2. Primary and Secondary Outcomes
3. Discussion
4. Materials and Methods
4.1. Study Design and Ethical Approval
4.2. Selection and Description of Participants
4.3. Data Collection
4.4. Study Endpoints
4.5. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Norberg, Å.; Rooyackers, O.; Segersvärd, R.; Wernerman, J. Leakage of albumin in major abdominal surgery. Crit. Care 2016, 20, 113. [Google Scholar] [CrossRef] [PubMed]
- Levitt, D.G.; Levitt, M.D. Human serum albumin homeostasis: A new look at the roles of synthesis, catabolism, renal and gastrointestinal excretion, and the clinical value of serum albumin measurements. Int. J. Gen. Med. 2016, 9, 229–255. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, J.P.; Wolmarans, M.R.; Park, G.R. The role of albumin in critical illness. Br. J. Anaesth. 2000, 85, 599–610. [Google Scholar] [CrossRef] [PubMed]
- Pulimood, T.B.; Park, G.R. Debate: Albumin administration should be avoided in the critically ill. Crit. Care 2000, 4, 151–155. [Google Scholar] [CrossRef]
- Wilkes, M.M.; Navickis, R.J. Patient survival after human albumin administration. A meta-analysis of randomized, controlled trials. Ann. Intern. Med. 2001, 135, 149–164. [Google Scholar] [CrossRef]
- Haynes, G.R.; Bassiri, K. Hyper-oncotic vs. Hypo-oncotic albumin solutions: A systematic review of clinical efficacy and safety. SN Compr. Clin. Med. 2021, 3, 1137–1147. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Navickis, R.J.; Wilkes, M.M. Morbidity in hospitalized patients receiving human albumin: A meta-analysis of randomized, controlled trials. Crit. Care Med. 2004, 32, 2029–2038. [Google Scholar] [CrossRef]
- Mårtensson, J.; Bihari, S.; Bannard-Smith, J.; Glassford, N.J.; Lloyd-Donald, P.; Cioccari, L.; Luethi, N.; Tanaka, A.; Crisman, M.; Rey de Castro, N.; et al. Small volume resuscitation with 20% albumin in intensive care: Physiological effects: The swipe randomised clinical trial. Intensive Care Med. 2018, 44, 1797–1806. [Google Scholar] [CrossRef]
- Gameiro, J.; Fonseca, J.A.; Neves, M.; Jorge, S.; Lopes, J.A. Acute kidney injury in major abdominal surgery: Incidence, risk factors, pathogenesis and outcomes. Ann. Intensive Care 2018, 8, 22. [Google Scholar] [CrossRef]
- Kim, C.S.; Oak, C.Y.; Kim, H.Y.; Kang, Y.U.; Choi, J.S.; Bae, E.H.; Ma, S.K.; Kweon, S.S.; Kim, S.W. Incidence, predictive factors, and clinical outcomes of acute kidney injury after gastric surgery for gastric cancer. PLoS ONE 2013, 8, e82289. [Google Scholar] [CrossRef]
- Teixeira, C.; Rosa, R.; Rodrigues, N.; Mendes, I.; Peixoto, L.; Dias, S.; Melo, M.J.; Pereira, M.; Bicha Castelo, H.; Lopes, J.A. Acute kidney injury after major abdominal surgery: A retrospective cohort analysis. Crit. Care Res. Pract. 2014, 2014, 132175. [Google Scholar] [CrossRef] [PubMed]
- Tomozawa, A.; Ishikawa, S.; Shiota, N.; Cholvisudhi, P.; Makita, K. Perioperative risk factors for acute kidney injury after liver resection surgery: An historical cohort study. Can. J. Anesth. 2015, 62, 753–761. [Google Scholar] [CrossRef]
- Frenette, A.J.; Bouchard, J.; Bernier, P.; Charbonneau, A.; Nguyen, L.T.; Rioux, J.P.; Troyanov, S.; Williamson, D.R. Albumin administration is associated with acute kidney injury in cardiac surgery: A propensity score analysis. Crit. Care 2014, 18, 602. [Google Scholar] [CrossRef] [PubMed]
- Schortgen, F.; Girou, E.; Deye, N.; Brochard, L. The risk associated with hyperoncotic colloids in patients with shock. Intensive Care Med. 2008, 34, 2157–2168. [Google Scholar] [CrossRef] [PubMed]
- Udeh, C.I.; You, J.; Wanek, M.R.; Dalton, J.; Udeh, B.L.; Demirjian, S.; Rahman, N.; Hata, J.S. Acute kidney injury in postoperative shock: Is hyperoncotic albumin administration an unrecognized resuscitation risk factor? Perioper. Med. 2018, 7, 29. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.H.; Kim, W.J.; Kim, J.Y.; Chin, J.H.; Choi, D.K.; Sim, J.Y.; Choo, S.J.; Chung, C.H.; Lee, J.W.; Choi, I.C. Effect of exogenous albumin on the incidence of postoperative acute kidney injury in patients undergoing off-pump coronary artery bypass surgery with a preoperative albumin level of less than 4.0 g/dL. Anesthesiology 2016, 124, 1001–1011. [Google Scholar] [CrossRef] [PubMed]
- Wiedermann, C.J.; Dunzendorfer, S.; Gaioni, L.U.; Zaraca, F.; Joannidis, M. Hyperoncotic colloids and acute kidney injury: A meta-analysis of randomized trials. Crit. Care 2010, 14, R191. [Google Scholar] [CrossRef] [PubMed]
- Dubois, M.J.; Orellana-Jimenez, C.; Melot, C.; De Backer, D.; Berre, J.; Leeman, M.; Brimioulle, S.; Appoloni, O.; Creteur, J.; Vincent, J.L. Albumin administration improves organ function in critically ill hypoalbuminemic patients: A prospective, randomized, controlled, pilot study. Crit. Care Med. 2006, 34, 2536–2540. [Google Scholar] [CrossRef]
- Hanley, C.; Callum, J.; McCluskey, S.; Karkouti, K.; Bartoszko, J. Albumin use in bleeding cardiac surgical patients and associated patient outcomes. Can. J. Anesth. 2021, 68, 1514–1526. [Google Scholar] [CrossRef]
- Causey, M.W.; Maykel, J.A.; Hatch, Q.; Miller, S.; Steele, S.R. Identifying risk factors for renal failure and myocardial infarction following colorectal surgery. J. Surg. Res. 2011, 170, 32–37. [Google Scholar] [CrossRef]
- Zetterström, H.; Hedstrand, U. Albumin treatment following major surgery. I. Effects on plasma oncotic pressure, renal function and peripheral oedema. Acta Anaesthesiol. Scand. 1981, 25, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.Y.; Zhang, C.H.; He, Y.L.; Yuan, Y.X.; Cai, S.R.; Luo, N.X.; Zhan, W.H.; Cui, J. Is albumin administration beneficial in early stage of postoperative hypoalbuminemia following gastrointestinal surgery?: A prospective randomized controlled trial. Am. J. Surg. 2008, 196, 751–755. [Google Scholar] [CrossRef] [PubMed]
- Torchia, M.G.; Danzinger, R.G. Perioperative blood transfusion and albumin administration are independent risk factors for the development of postoperative infections after colorectal surgery. Can. J. Surg. 2000, 43, 212–216. [Google Scholar]
- Zhang, F.; Liu, X.; Tan, Z.; Li, J.; Fu, D.; Zhu, L. Effect of postoperative hypoalbuminemia and supplement of human serum albumin on the development of surgical site infection following spinal fusion surgery: A retrospective study. Eur. Spine J. 2020, 29, 1483–1489. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, N.N.; Turpin, R.S.; Yang, G.; Saunders, W.B. Impact of surgical site infections on length of stay and costs in selected colorectal procedures. Surg. Infect. 2009, 10, 539–544. [Google Scholar] [CrossRef]
- Kusachi, S.; Kashimura, N.; Konishi, T.; Shimizu, J.; Kusunoki, M.; Oka, M.; Wakatsuki, T.; Kobayashi, J.; Sawa, Y.; Imoto, H.; et al. Length of stay and cost for surgical site infection after abdominal and cardiac surgery in japanese hospitals: Multi-center surveillance. Surg. Infect. 2012, 13, 257–265. [Google Scholar] [CrossRef]
- GlobalSurg Collaborative. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: A prospective, international, multicentre cohort study. Lancet Infect. Dis. 2018, 18, 516–525. [Google Scholar] [CrossRef]
- Grams, M.E.; Sang, Y.; Coresh, J.; Ballew, S.; Matsushita, K.; Molnar, M.Z.; Szabo, Z.; Kalantar-Zadeh, K.; Kovesdy, C.P. Acute kidney injury after major surgery: A retrospective analysis of veterans health administration data. Am. J. Kidney Dis. 2016, 67, 872–880. [Google Scholar] [CrossRef]
- Walsh, M.; Devereaux, P.J.; Garg, A.X.; Kurz, A.; Turan, A.; Rodseth, R.N.; Cywinski, J.; Thabane, L.; Sessler, D.I. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: Toward an empirical definition of hypotension. Anesthesiology 2013, 119, 507–515. [Google Scholar] [CrossRef]
- Rule, A.D. The ckd-epi equation for estimating gfr from serum creatinine: Real improvement or more of the same? Clin. J. Am. Soc. Nephrol. 2010, 5, 951. [Google Scholar] [CrossRef]
- Khwaja, A. Kdigo clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Ross, C.; Raebel, M.A.; Shetterly, S.; Blanchette, C.; Smith, D. Use of stabilized inverse propensity scores as weights to directly estimate relative risk and its confidence intervals. Value Health 2010, 13, 273–277. [Google Scholar] [CrossRef] [PubMed]

| Variables | Unadjusted | Adjusted Using IPTW | Adjusted Using PSM | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Albumin (n = 842) | No Albumin (n = 1566) | SMD | ALBUMIN (n = 713) | No Albumin (n = 1450) | SMD | Albumin (n = 483) | No Albumin (n = 483) | SMD | |
| Age (years) | 59 [50–69] | 64 [52–73] | 0.224 | 60 [51–71] | 62 [50–72] | 0.033 | 60 [50–71] | 61 [50–72] | 0.010 |
| Male sex | 294 (34.9%) | 688 (43.9%) | 0.185 | 298 (41.8%) | 607 (41.9%) | 0.001 | 183 (37.9%) | 194 (40.2%) | 0.047 |
| Body mass index (kg·m−2) | 22.5 [20.2–24.7] | 23.0 [20.8–25.2] | 0.143 | 22.6 [20.5–25.1] | 22.8 [20.5–25.2] | 0.049 | 22.5 [20.3–24.8] | 22.4 [20.0–24.7] | 0.029 |
| ASA physical status | 0.145 | 0.077 | 0.030 | ||||||
| I | 30 (3.6%) | 96 (6.1%) | 28 (3.9%) | 79 (5.4%) | 21 (4.4%) | 22 (4.6%) | |||
| II | 315 (37.4%) | 609 (38.9%) | 287 (40.2%) | 558 (38.5%) | 191 (39.5%) | 188 (38.9%) | |||
| III | 424 (50.4%) | 759 (48.5%) | 345 (48.4%) | 708 (48.8%) | 229 (47.4%) | 234 (48.5%) | |||
| IV | 73 (8.7%) | 102 (6.5%) | 54 (7.6%) | 106 (7.3%) | 42 (8.7%) | 39 (8.1%) | |||
| Comorbidities | |||||||||
| Hypertension | 392 (46.6%) | 864 (55.2%) | 0.173 | 344 (48.2%) | 733 (50.6%) | 0.048 | 226 (46.8%) | 242 (50.1%) | 0.066 |
| Diabetes mellitus | 224 (26.6%) | 495 (31.6%) | 0.110 | 197 (27.6%) | 418 (28.9%) | 0.028 | 126 (26.1%) | 134 (27.7%) | 0.037 |
| Cerebrovascular disease | 49 (5.8%) | 116 (7.4%) | 0.064 | 42 (5.9%) | 96 (6.6%) | 0.031 | 32 (6.6%) | 29 (6.0%) | 0.026 |
| Asthma | 18 (2.1%) | 43 (2.8%) | 0.039 | 12 (1.7%) | 41 (2.8%) | 0.072 | 11 (2.3%) | 16 (3.3%) | 0.063 |
| Coronary artery disease | 23 (2.7%) | 72 (4.6%) | 0.099 | 22 (3.1%) | 68 (4.7%) | 0.082 | 16 (3.3%) | 21 (4.4%) | 0.054 |
| Valvular heart disease | 16 (1.9%) | 36 (2.3%) | 0.028 | 11 (1.5%) | 39 (2.7%) | 0.082 | 9 (1.9%) | 16 (3.3%) | 0.091 |
| Atrial fibrillation | 18 (2.1%) | 44 (2.8%) | 0.043 | 23 (3.3%) | 35 (2.4%) | 0.051 | 9 (1.9%) | 10 (2.1%) | 0.015 |
| Chronic kidney disease | 11 (1.3%) | 39 (2.5%) | 0.087 | 11 (1.6%) | 31 (2.1%) | 0.039 | 8 (1.7%) | 10 (2.1%) | 0.031 |
| Preoperative RBC transfusion | 77 (9.1%) | 75 (4.8%) | 0.172 | 47 (6.6%) | 87 (6.0%) | 0.023 | 38 (7.9%) | 32 (6.6%) | 0.048 |
| Preoperative laboratory values | |||||||||
| Hematocrit (%) | 32.9 [29.3–37.0] | 33.0 [28.9–37.4] | 0.020 | 33.0 [29.1–37.5] | 32.9 [28.8–37.3] | 0.055 | 33.0 [29.3–37.6] | 32.7 [28.6–36.9] | 0.125 |
| Platelet count (×103·μL−1) | 275 [201–369] | 252 [190–323] | 0.197 | 260 [184–344] | 256 [191–332] | 0.028 | 275 [200–359] | 265 [201–343] | 0.050 |
| Serum albumin (g·dL−1) | 3.6 [2.9–4.3] | 4.0 [3.4–4.3] | 0.341 | 3.8 [3.0–4.4] | 3.9 [3.3–4.3] | 0.115 | 3.7 [3.0–4.4] | 3.7 [3.1–4.2] | 0.004 |
| eGFR (mL·min−1·1.73 m−2) | 98 [85–108] | 92 [78–104] | 0.231 | 97 [84–107] | 94 [80–106] | 0.063 | 97 [83–108] | 97 [83–109] | 0.019 |
| Variables | Unadjusted | Adjusted Using IPTW | Adjusted Using PSM | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Albumin (n = 842) | No Albumin (n = 1566) | SMD | Albumin (n = 713) | No Albumin (n = 1450) | SMD | Albumin (n = 483) | No Albumin (n = 483) | SMD | |
| Operation time (min) | 411 [264–588] | 275 [191–396] | 0.684 | 347 [207–505] | 311 [214–467] | 0.121 | 356 [216–502] | 344 [235–494] | 0.027 |
| Anesthetic agents | 0.295 | 0.114 | 0.068 | ||||||
| Desflurane | 414 (49.2%) | 952 (60.8%) | 380 (53.3%) | 843 (58.1%) | 250 (51.8%) | 266 (55.1%) | |||
| Sevoflurane | 418 (49.6%) | 565 (36.1%) | 321 (44.9%) | 573 (39.5%) | 227 (47.0%) | 212 (43.9%) | |||
| Propofol for TIVA | 10 (1.2%) | 49 (3.1%) | 13 (1.8%) | 35 (2.4%) | 6 (1.2%) | 5 (1.0%) | |||
| Vasopressor use | |||||||||
| Phenyl or NE | 771 (91.6%) | 1026 (65.5%) | 0.669 | 569 (79.8%) | 1074 (74.0) | 0.137 | 419 (86.8%) | 418 (86.5%) | 0.006 |
| Vasopressin | 159 (18.9%) | 77 (4.9%) | 0.442 | 86 (12.1%) | 118 (8.1%) | 0.131 | 58 (12.0%) | 50 (10.4%) | 0.053 |
| Fluid intake (mL) | 5250 [3513–7300] | 3000 [2085–4388] | 0.842 | 4200 [2500–5900] | 3550 [2450–5200] | 0.174 | 4300 [2700–5900] | 3950 [2750–5600] | 0.025 |
| HES 6% infused (mL) | 1000 [1000–1500] | 1000 [500–1000] | 0.636 | 1000 [500–1000] | 1000 [500–1000] | 0.121 | 1000 [500–1000] | 1000 [500–1000] | 0.011 |
| Urine output (mL) | 745 [390–1360] | 455 [240–780] | 0.552 | 590 [279–1075] | 515 [260–960] | 0.121 | 600 [308–1053] | 580 [310–1053] | 0.017 |
| Blood loss (mL) | 1250 [650–2250] | 650 [300–1100] | 0.611 | 900 [400–1700] | 800 [400–1400] | 0.155 | 900 [500–1695] | 850 [500–1500] | 0.054 |
| Transfusion | |||||||||
| RBCs (U) | 3 [2–5] | 1 [1–2] | 0.677 | 2 [1–3] | 2 [1–2] | 0.149 | 2 [1–3] | 2 [1–3] | 0.072 |
| FFP > 5 U | 51 (6.1%) | 6 (0.4%) | 0.326 | 20 (2.8%) | 15 (1.0%) | 0.126 | 7 (1.5%) | 6 (1.2%) | 0.018 |
| Platelets > 10 U | 21 (2.5%) | 6 (0.4%) | 0.178 | 9 (1.3%) | 14 (0.9%) | 0.033 | 4 (0.8%) | 4 (0.8%) | <0.001 |
| Laparoscopic surgery | 84 (10.0%) | 384 (24.5%) | 0.392 | 106 (14.9%) | 267 (18.4%) | 0.096 | 66 (13.7%) | 63 (13.0%) | 0.018 |
| Cancer surgery | 672 (79.8%) | 1252 (80.0%) | 0.004 | 572 (80.2%) | 1142 (78.7%) | 0.037 | 376 (77.9%) | 371 (76.8%) | 0.025 |
| Emergency surgery | 147 (17.5%) | 232 (14.8%) | 0.072 | 130 (18.2%) | 242 (16.7%) | 0.040 | 95 (19.7%) | 92 (19.1%) | 0.016 |
| Surgical specialty | 0.700 | 0.106 | 0.011 | ||||||
| Upper GI | 66 (7.8%) | 304 (19.4%) | 107 (15.0%) | 229 (15.8%) | 57 (11.8%) | 58 (12.0%) | |||
| Hepatobiliary | 42 (5.0%) | 349 (22.3%) | 95 (13.3%) | 243 (16.8%) | 36 (7.5%) | 35 (7.3%) | |||
| Colorectal | 425 (50.5%) | 564 (36.0%) | 305 (42.7%) | 580 (40.0%) | 233 (48.2%) | 234 (48.5%) | |||
| Gynecological | 309 (36.7%) | 349 (22.3%) | 207 (29.0%) | 397 (27.4%) | 157 (32.5%) | 156 (32.3%) | |||
| Analysis Method | β (95% CI) | p-Value |
|---|---|---|
| Unadjusted | 6.15 (4.96 to 7.35) | <0.001 |
| Adjustment with IPTW | 4.01 (1.93 to 6.09) | <0.001 |
| Adjustment with PSM | 3.18 (1.32 to 5.04) | <0.001 |
| PS covariate adjustment | 3.11 (1.53 to 4.68) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.J.; Kim, H.J.; Park, J.H.; Shin, H.J.; Yu, S.K.; Roh, Y.H.; Jeon, S.Y.; Kim, S.Y. Association between 20% Albumin Use and Acute Kidney Injury in Major Abdominal Surgery with Transfusion. Int. J. Mol. Sci. 2023, 24, 2333. https://doi.org/10.3390/ijms24032333
Kim HJ, Kim HJ, Park JH, Shin HJ, Yu SK, Roh YH, Jeon SY, Kim SY. Association between 20% Albumin Use and Acute Kidney Injury in Major Abdominal Surgery with Transfusion. International Journal of Molecular Sciences. 2023; 24(3):2333. https://doi.org/10.3390/ijms24032333
Chicago/Turabian StyleKim, Hye Jin, Hyun Joo Kim, Jin Ha Park, Hye Jung Shin, Sung Kyung Yu, Yun Ho Roh, Soo Yeon Jeon, and So Yeon Kim. 2023. "Association between 20% Albumin Use and Acute Kidney Injury in Major Abdominal Surgery with Transfusion" International Journal of Molecular Sciences 24, no. 3: 2333. https://doi.org/10.3390/ijms24032333
APA StyleKim, H. J., Kim, H. J., Park, J. H., Shin, H. J., Yu, S. K., Roh, Y. H., Jeon, S. Y., & Kim, S. Y. (2023). Association between 20% Albumin Use and Acute Kidney Injury in Major Abdominal Surgery with Transfusion. International Journal of Molecular Sciences, 24(3), 2333. https://doi.org/10.3390/ijms24032333






