Low Dose of BPA Induces Liver Injury through Oxidative Stress, Inflammation and Apoptosis in Long–Evans Lactating Rats and Its Perinatal Effect on Female PND6 Offspring
Abstract
1. Introduction
2. Results
2.1. Effects of BPA Exposure on Body Weight, Food Consumption, Number of Pregnant Dams and Mortality Rate in PND6 Offspring and Pup Weight
2.2. Effects of BPA Exposure on Antioxidant Enzyme Activities and Glutathione Concentrations in Dams
2.3. Effects of BPA Exposure on Oxidative Damage in Dams and Gene Expression Profile of GSH-Related Enzymes
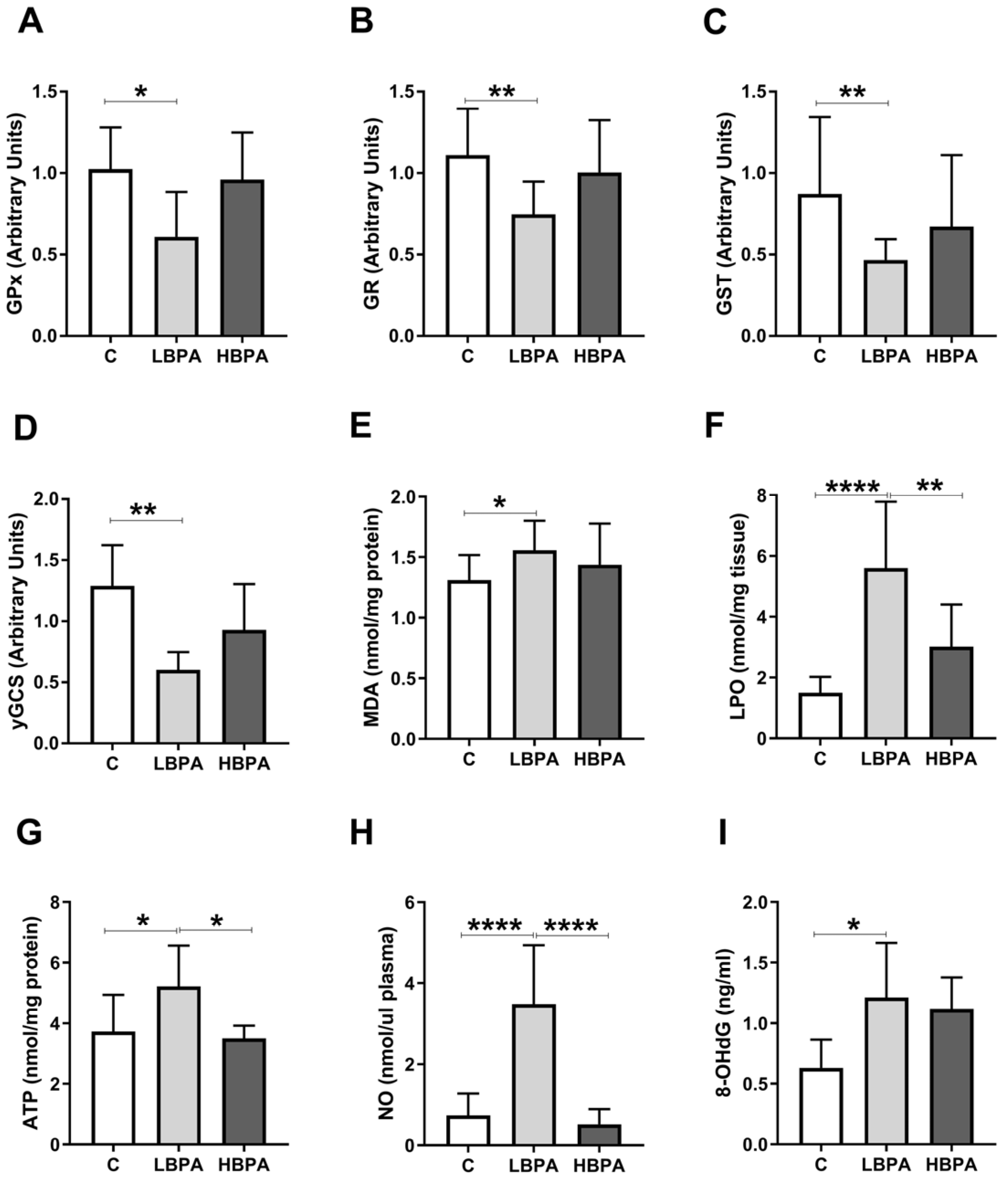
2.4. Effects of BPA Exposure on Oxidative Stress-Inducing Markers in Dams
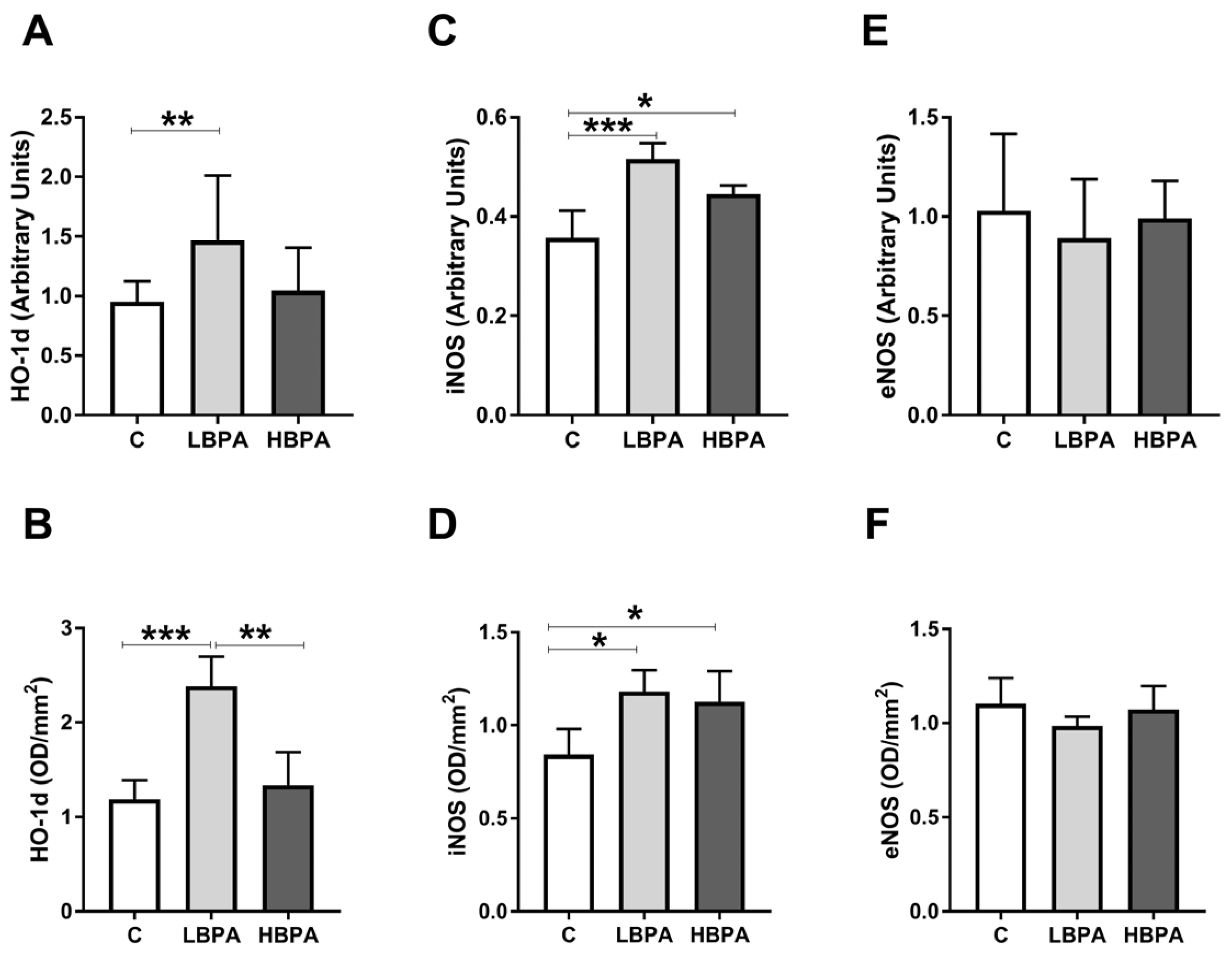
2.5. Effects of BPA Exposure in Dams on Inflammatory and Apoptosis Response in the Liver
2.6. Effects of Perinatal Exposure to BPA on Antioxidant Enzyme Activities and Glutathione Concentrations in Liver of Female PND6 Offspring
2.7. Effects of Perinatal Exposure to BPA on Oxidative Damage and Gene Expression Profile of GSH-Related Enzymes in Liver of PND6 Offspring
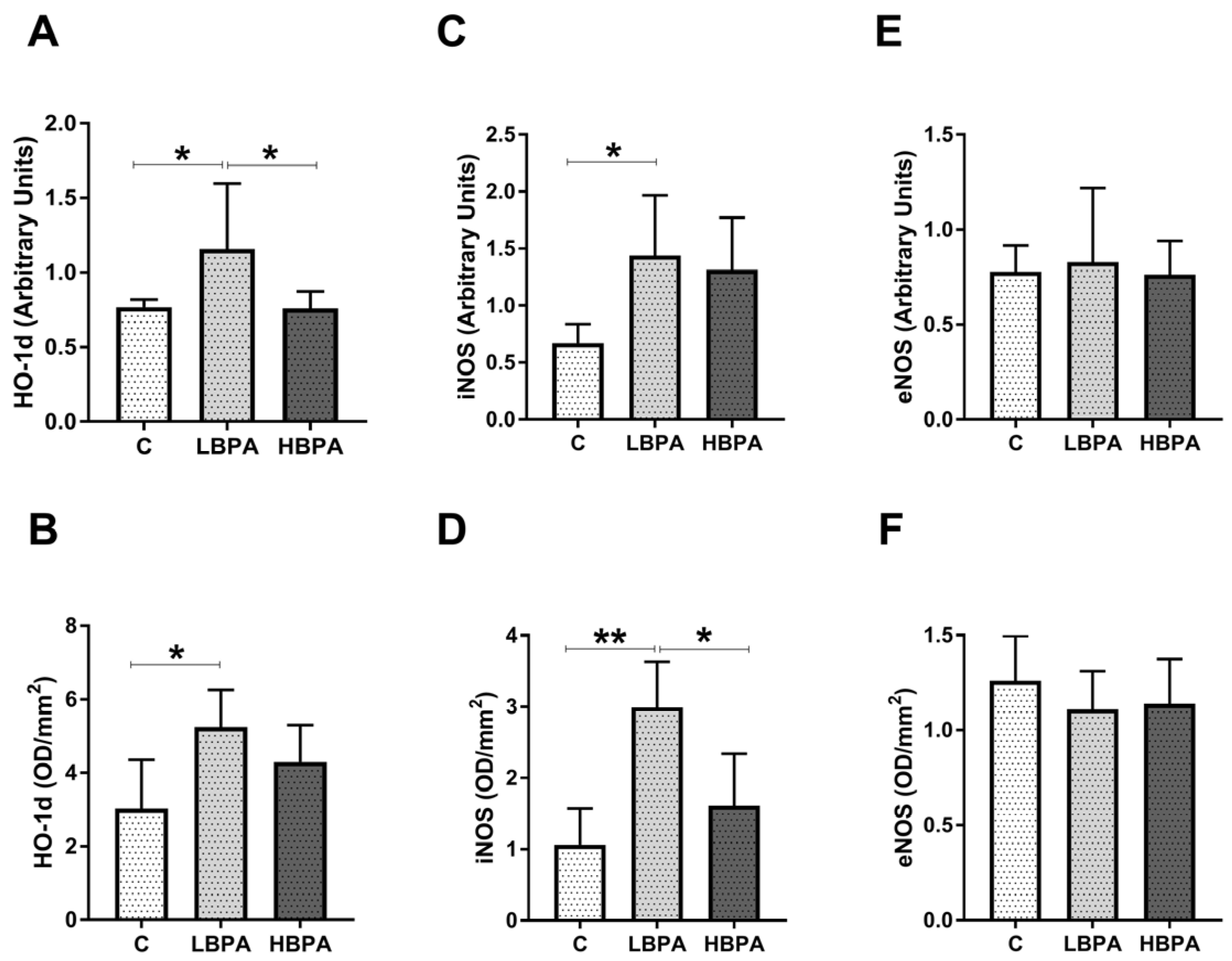
2.8. Effects of Perinatal Exposure to BPA on Oxidative Stress Intermediaries in Liver of PND6 Offspring
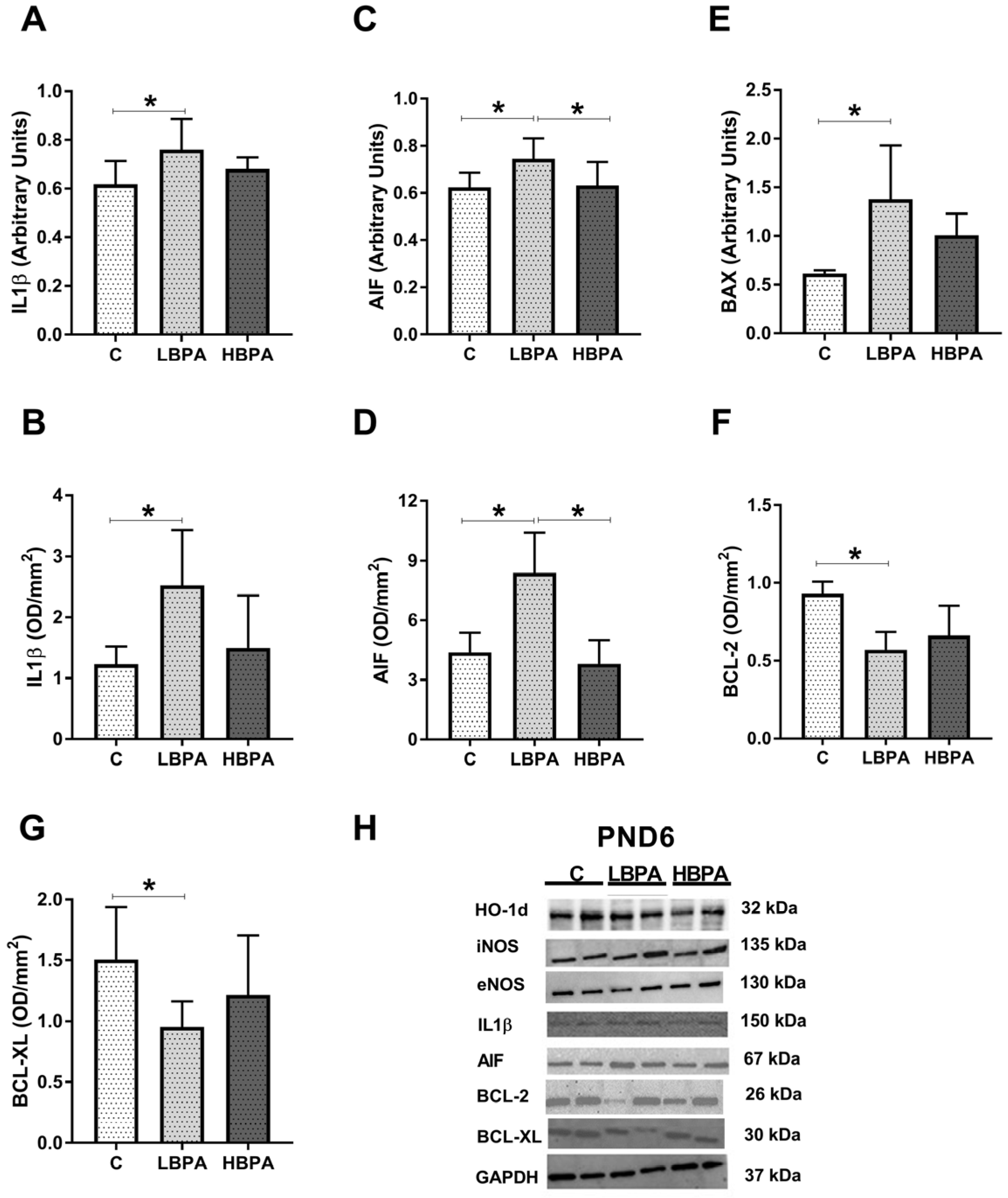
2.9. Effects of Perinatal Exposure to BPA on Inflammatory Mediator and Apoptosis Markers in Liver of PND6 Offspring
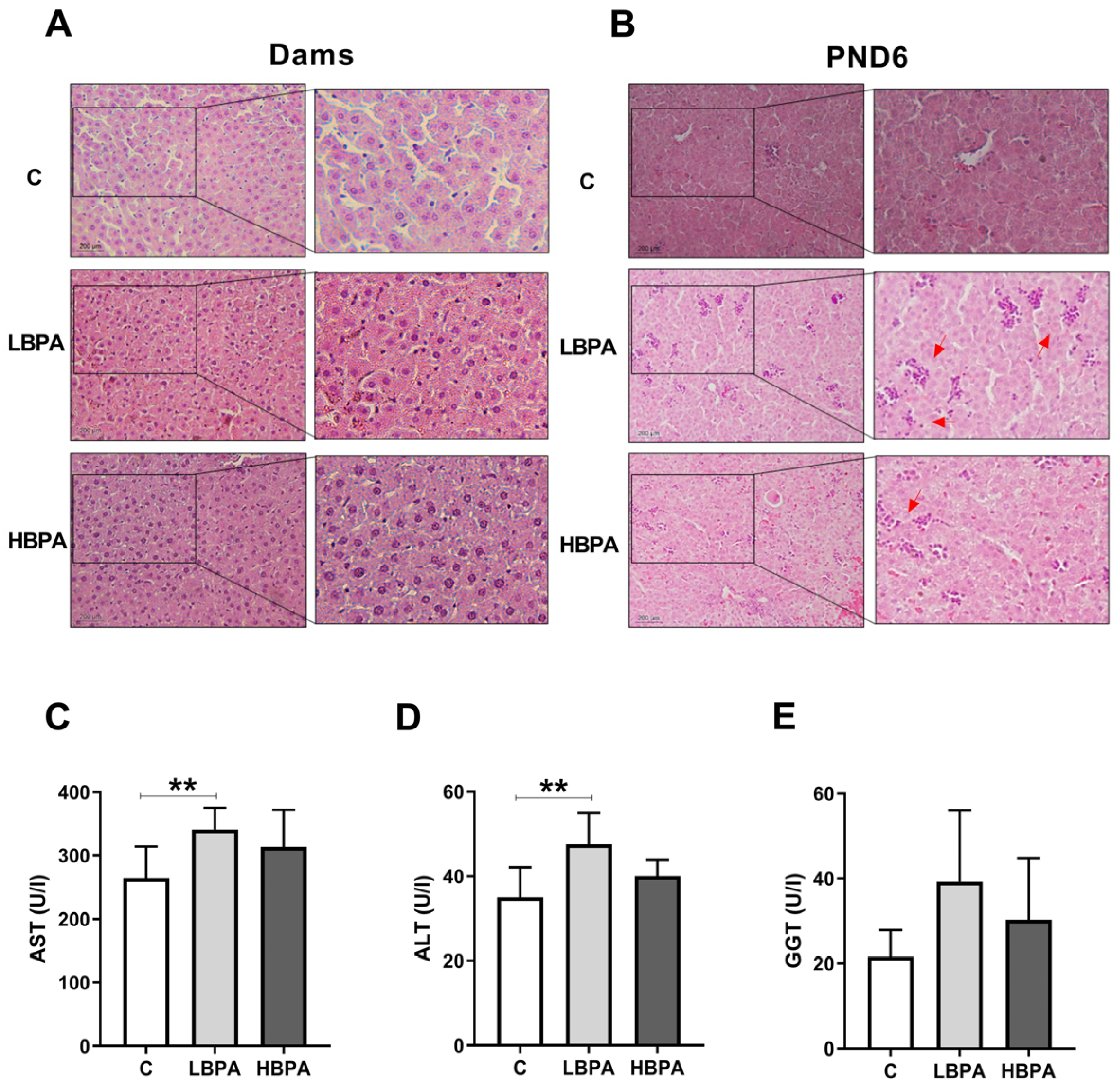
2.10. Effect of BPA on Histopathology and Hepatic Serum Markers
3. Discussion
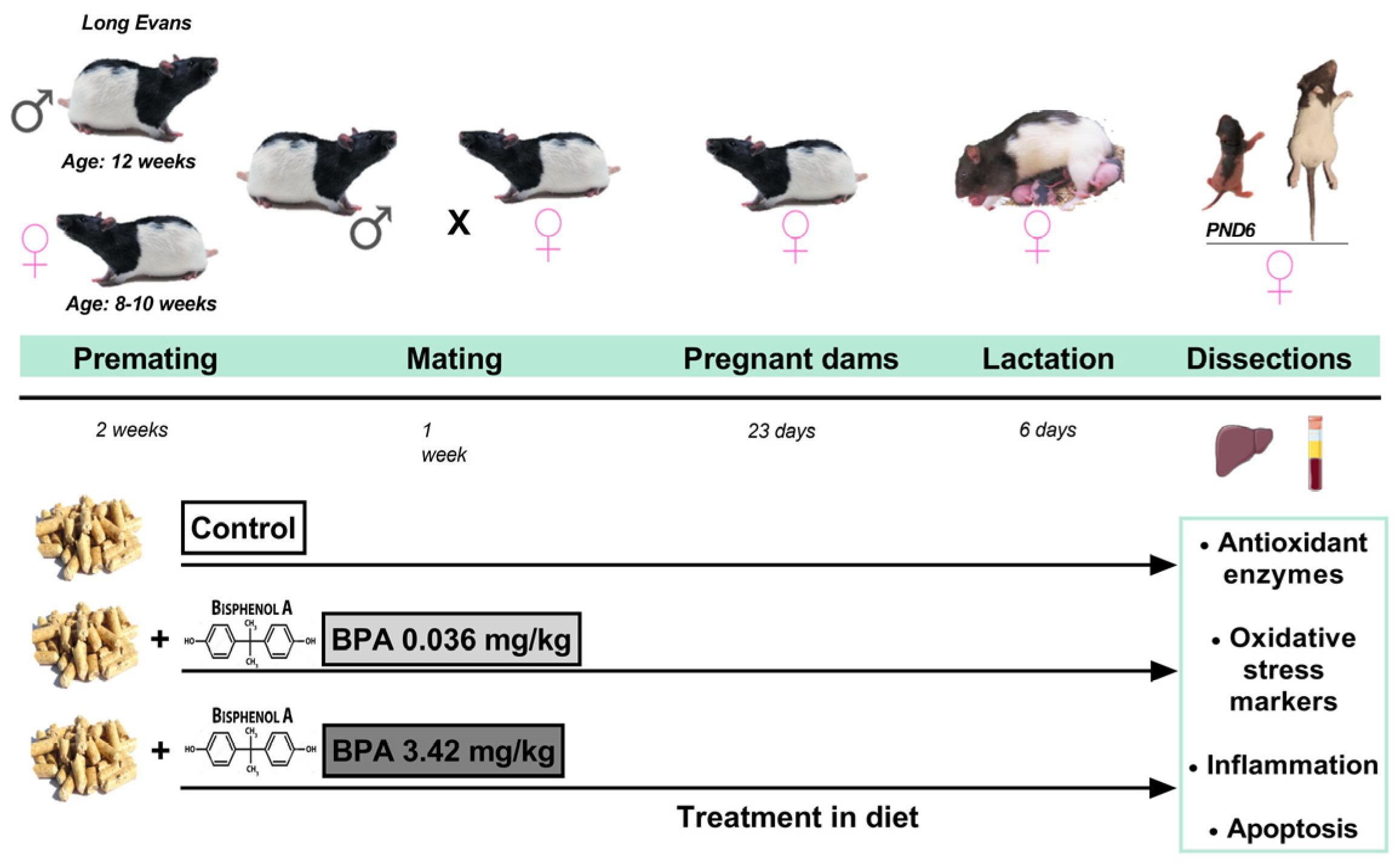
4. Materials and Methods
4.1. Animals
4.2. Treatment and Experimental Design
4.3. Activities of Antioxidant Enzymes and Glutathione Concentrations
4.3.1. Antioxidant Enzymes
4.3.2. Glutathione Concentrations
4.4. Oxidative Stress Markers
4.4.1. Lipid Peroxidation Assay
4.4.2. Thiobarbituric Acid Reactive Substances (TBARS) Assay
4.4.3. Adenosine Triphosphate Determination
4.4.4. Determination of Nitric Oxide Metabolites (NOx)
4.4.5. DNA Oxidative Damage Measurement
4.5. Determination of Protein Concentration
4.6. RNA Isolation and RT-PCR Quantification
4.7. Protein Extraction and Western Blot Analysis
4.8. Histological Staining
4.9. Analysis of Hepatic Serum Markers
4.10. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kazemi, S.; Mousavi, S.N.; Aghapour, F.; Rezaee, B.; Sadeghi, F.; Moghadamnia, A.A. Induction Effect of Bisphenol a on Gene Expression Involving Hepatic Oxidative Stress in Rat. Oxid. Med. Cell. Longev. 2016, 2016, 12–14. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Shi, Y.; Li, Z.; Sun, L.; Zhang, M.; Yu, L.; Wu, S. BPA Disrupts 17-estradiol-mediated Hepatic Protection against Ischemia/Reperfusion Injury in Rat Liver by Upregulating the Ang II/AT1R Signaling Pathway. Mol. Med. Rep. 2020, 22, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Acaroz, U.; Ince, S.; Arslan-Acaroz, D.; Gurler, Z.; Demirel, H.H.; Kucukkurt, I.; Eryavuz, A.; Kara, R.; Varol, N.; Zhu, K. Bisphenol-A Induced Oxidative Stress, Inflammatory Gene Expression, and Metabolic and Histopathological Changes in Male Wistar Albino Rats: Protective Role of Boron. Toxicol. Res. 2019, 8, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Peerapanyasut, W.; Kobroob, A.; Palee, S.; Chattipakorn, N.; Wongmekiat, O. Activation of Sirtuin 3 and Maintenance of Mitochondrial Integrity by N-Acetylcysteine Protects against Bisphenol A-Induced Kidney and Liver Toxicity in Rats. Int. J. Mol. Sci. 2019, 20, 267. [Google Scholar] [CrossRef]
- Eweda, S.; Newairy, A.; Abdou, H.; Gaber, A. Bisphenol A-induced Oxidative Damage in the Hepatic and Cardiac Tissues of Rats: The Modulatory Role of Sesame Lignans. Exp. Ther. Med. 2019, 2, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Xia, W.; Jiang, Y.; Li, Y.; Wan, Y.; Liu, J.; Ma, Y.; Mao, Z.; Chang, H.; Li, G.; Xu, B.; et al. Early-Life Exposure to Bisphenol a Induces Liver Injury in Rats Involvement of Mitochondria-Mediated Apoptosis. PLoS ONE 2014, 9, e90443. [Google Scholar] [CrossRef] [PubMed]
- Dutta, M.; Paul, G. Gallic Acid Protects Rat Liver Mitochondria Ex Vivo from Bisphenol A Induced Oxidative Stress Mediated Damages. Toxicol. Rep. 2019, 6, 578–589. [Google Scholar] [CrossRef]
- Elswefy, S.E.S.; Abdallah, F.R.; Atteia, H.H.; Wahba, A.S.; Hasan, R.A. Inflammation, Oxidative Stress and Apoptosis Cascade Implications in Bisphenol A-Induced Liver Fibrosis in Male Rats. Int. J. Exp. Pathol. 2016, 97, 369–379. [Google Scholar] [CrossRef]
- Ambreen, S.; Akhtar, T.; Hameed, N.; Ashfaq, I.; Sheikh, N. In Vivo Evaluation of Histopathological Alterations and Trace Metals Estimation of the Small Intestine in Bisphenol A-Intoxicated Rats. Can. J. Gastroenterol. Hepatol. 2019, 2019, 9292316. [Google Scholar] [CrossRef]
- Lin, R.; Jia, Y.; Wu, F.; Meng, Y.; Sun, Q.; Jia, L. Combined Exposure to Fructose and Bisphenol a Exacerbates Abnormal Lipid Metabolism in Liver of Developmental Male Rats. Int. J. Environ. Res. Public Health 2019, 16, 4152. [Google Scholar] [CrossRef]
- Baralić, K.; Djordjevic, A.B.; Živančević, K.; Antonijević, E.; Anđelković, M.; Javorac, D.; Ćurčić, M.; Bulat, Z.; Antonijević, B.; Đukić-ćosić, D. Toxic Effects of the Mixture of Phthalates and Bisphenol a—Subacute Oral Toxicity Study in Wistar Rats. Int. J. Environ. Res. Public Health 2020, 17, 746. [Google Scholar] [CrossRef] [PubMed]
- Mahdavinia, M.; Alizadeh, S.; Raesi Vanani, A.; Dehghani, M.A.; Shirani, M.; Alipour, M.; Shahmohammadi, H.A.; Rafiei Asl, S. Effects of Quercetin on Bisphenol A-Induced Mitochondrial Toxicity in Rat Liver. Iran. J. Basic Med. Sci. 2019, 22, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Moon, M.K.; Kim, M.J.; Jung, I.K.; Koo, Y.D.; Ann, H.Y.; Lee, K.J.; Kim, S.H.; Yoon, Y.C.; Cho, B.J.; Park, K.S.; et al. Bisphenol a Impairs Mitochondrial Function in the Liver at Doses below the No Observed Adverse Effect Level. J. Korean Med. Sci. 2012, 27, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Kovacic, P. How Safe Is Bisphenol A? Fundamentals of Toxicity: Metabolism, Electron Transfer and Oxidative Stress. Med. Hypotheses 2010, 75, 1–4. [Google Scholar] [CrossRef]
- Bindhumol, V.; Chitra, K.C.; Mathur, P.P. Bisphenol A Induces Reactive Oxygen Species Generation in the Liver of Male Rats. Toxicology 2003, 188, 117–124. [Google Scholar] [CrossRef]
- Hanioka, N.; Jinno, H.; Nishimura, T.; Ando, M. Suppression of Male-Specific Cytochrome P450 Isoforms by Bisphenol A in Rat Liver. Arch. Toxicol. 1998, 72, 387–394. [Google Scholar] [CrossRef]
- Ikezuki, Y.; Tsutsumi, O.; Takai, Y.; Kamei, Y.; Taketani, Y. Determination of Bisphenol A Concentrations in Human Biological Fluids Reveals Significant Early Prenatal Exposure. Hum. Reprod. 2002, 17, 2839–2841. [Google Scholar] [CrossRef]
- Jiang, Y.; Xia, W.; Zhu, Y.; Li, X.; Wang, D.; Liu, J.; Chang, H.; Li, G.; Xu, B.; Chen, X.; et al. Mitochondrial Dysfunction in Early Life Resulted from Perinatal Bisphenol A Exposure Contributes to Hepatic Steatosis in Rat Offspring. Toxicol. Lett. 2014, 228, 85–92. [Google Scholar] [CrossRef]
- Weinhouse, C.; Anderson, O.S.; Bergin, I.L.; Vandenbergh, D.J.; Gyekis, J.P.; Dingman, M.A.; Yang, J.; Dolinoy, D.C. Dose-Dependent Incidence of Hepatic Tumors in Adult Mice Following Perinatal Exposure to Bisphenol A. Environ. Health Perspect. 2014, 122, 485–491. [Google Scholar] [CrossRef]
- Wei, J.; Lin, Y.; Li, Y.; Ying, C.; Chen, J.; Song, L.; Zhou, Z.; Lv, Z.; Xia, W.; Chen, X.; et al. Perinatal Exposure to Bisphenol A at Reference Dose Predisposes Offspring to Metabolic Syndrome in Adult Rats on a High-Fat Diet. Endocrinology 2011, 152, 3049–3061. [Google Scholar] [CrossRef]
- Schönfelder, G.; Wittfoht, W.; Hopp, H.; Talsness, C.E.; Paul, M.; Chahoud, I. Parent Bisphenol a Accumulation in the Human Maternal-Fetal-Placental Unit. Environ. Health Perspect. 2002, 110, A703–A707. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Choi, K.; Kim, S.; Ji, K.; Chang, H.; Wiseman, S.; Jones, P.D.; Khim, J.S.; Park, S.; Park, J.; et al. Hydroxylated Polybrominated Diphenyl Ethers and Bisphenol A in Pregnant Women and Their Matching Fetuses: Placental Transfer and Potential Risks. Environ. Sci. Technol. 2010, 44, 5233–5239. [Google Scholar] [CrossRef] [PubMed]
- Yamada, H.; Furuta, I.; Kato, E.H.; Kataoka, S.; Usuki, Y.; Kobashi, G.; Sata, F.; Kishi, R.; Fujimoto, S. Maternal Serum and Amniotic Fluid Bisphenol A Concentrations in the Early Second Trimester. Reprod. Toxicol. 2002, 16, 735–739. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.L.; Zhang, J.; Goodyer, C.G.; Hayward, S.; Cooke, G.M.; Curran, I.H.A. Bisphenol A in Human Placental and Fetal Liver Tissues Collected from Greater Montreal Area (Quebec) during 1998-2008. Chemosphere 2012, 89, 505–511. [Google Scholar] [CrossRef]
- Sun, Y.; Irie, M.; Kishikawa, N.; Wada, M.; Kuroda, N.; Nakashima, K. Determination of Bisphenol A in Human Breast Milk by HPLC with Column-Switching and Fluorescence Detection. Biomed. Chromatogr. 2004, 18, 501–507. [Google Scholar] [CrossRef]
- Liao, C.; Liu, F.; Alomirah, H.; Loi, V.D.; Mohd, M.A.; Moon, H.B.; Nakata, H.; Kannan, K. Bisphenol S in Urine from the United States and Seven Asian Countries: Occurrence and Human Exposures. Environ. Sci. Technol. 2012, 46, 6860–6866. [Google Scholar] [CrossRef]
- Zhang, T.; Sun, H.; Kannan, K. Blood and Urinary Bisphenol A Concentrations in Children, Adults, and Pregnant Women from China: Partitioning between Blood and Urine and Maternal and Fetal Cord Blood. Environ. Sci. Technol. 2013, 47, 4686–4694. [Google Scholar] [CrossRef]
- Trasande, L.; Attina, T.M.; Trachtman, H. Bisphenol A Exposure Is Associated with Low-Grade Urinary Albumin Excretion in Children of the United States. Kidney Int. 2013, 83, 741–748. [Google Scholar] [CrossRef]
- Hines, C.J.; Jackson, M.V.; Deddens, J.A.; Clark, J.C.; Ye, X.; Christianson, A.L.; Meadows, J.W.; Calafat, A.M. Urinary Bisphenol A (BPA) Concentrations among Workers in Industries That Manufacture and Use BPA in the USA. Ann. Work Expo. Health 2017, 61, 164–182. [Google Scholar] [CrossRef]
- Inoue, H.; Tsuruta, A.; Kudo, S.; Ishii, T.; Fukushima, Y.; Iwano, H.; Yokota, H.; Kato, S. Bisphenol a Glucuronidation and Excretion in Liver of Pregnant and Nonpregnant Female Rats. Drug Metab. Dispos. Biol. Fate Chem. 2005, 33, 55–59. [Google Scholar] [CrossRef]
- Völkel, W.; Colnot, T.; Csanády, G.A.; Filser, J.G.; Dekant, W. Metabolism and Kinetics of Bisphenol a in Humans at Low Doses Following Oral Administration. Chem. Res. Toxicol. 2002, 15, 1281–1287. [Google Scholar] [CrossRef] [PubMed]
- Geens, T.; Aerts, D.; Berthot, C.; Bourguignon, J.-P.; Goeyens, L.; Lecomte, P.; Maghuin-Rogister, G.; Pironnet, A.-M.; Pussemier, L.; Scippo, M.-L.; et al. A Review of Dietary and Non-Dietary Exposure to Bisphenol-A. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2012, 50, 3725–3740. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, A.; Roy, D. In Vitro Conversion of Environmental Estrogenic Chemical Bisphenol A to DNA Binding Metabolite(s). Biochem. Biophys. Res. Commun. 1995, 210, 424–433. [Google Scholar] [CrossRef] [PubMed]
- Sayed-Ahmed, M.M.; Aleisa, A.M.; Al-Rejaie, S.S.; Al-Yahya, A.A.; Al-Shabanah, O.A.; Hafez, M.M.; Nagi, M.N. Thymoquinone Attenuates Diethylnitrosamine Induction of Hepatic Carcinogenesis through Antioxidant Signaling. Oxid. Med. Cell. Longev. 2010, 3, 254–261. [Google Scholar] [CrossRef]
- Sharma, R.; Yang, Y.; Sharma, A.; Awasthi, S.; Awasthi, Y.C. Antioxidant Role of Glutathione S-Transferases: Protection against Oxidant Toxicity and Regulation of Stress-Mediated Apoptosis. Antioxid. Redox Signal. 2004, 6, 289–300. [Google Scholar] [CrossRef]
- Boesten, D.M.P.H.J.; Elie, A.G.I.M.; Drittij-Reijnders, M.-J.; den Hartog, G.J.M.; Bast, A. Effect of Nɛ-Carboxymethyllysine on Oxidative Stress and the Glutathione System in Beta Cells. Toxicol. Rep. 2014, 1, 973–980. [Google Scholar] [CrossRef]
- Ungurianu, A.; Șeremet, O.; Grădinaru, D.; Ionescu-Tîrgoviște, C.; Margină, D.; Dănciulescu Miulescu, R. Spectrophotometric versus Spectrofluorometric Assessment in the Study of the Relationships between Lipid Peroxidation and Metabolic Dysregulation. Chem. Biol. Drug Des. 2019, 93, 1026–1035. [Google Scholar] [CrossRef]
- Gassman, N.R. Induction of Oxidative Stress by Bisphenol A and Its Pleiotropic Effects. Environ. Mol. Mutagen. 2017, 58, 60–71. [Google Scholar] [CrossRef]
- Morgan, A.M.; El-Ballal, S.S.; El-Bialy, B.E.; EL-Borai, N.B. Studies on the Potential Protective Effect of Cinnamon against Bisphenol A- and Octylphenol-Induced Oxidative Stress in Male Albino Rats. Toxicol. Rep. 2014, 1, 92–101. [Google Scholar] [CrossRef]
- Hassan, Z.K.; Elobeid, M.A.; Virk, P.; Omer, S.A.; ElAmin, M.; Daghestani, M.H.; AlOlayan, E.M. Bisphenol A Induces Hepatotoxicity through Oxidative Stress in Rat Model. Oxid. Med. Cell. Longev. 2012, 2012, 194829. [Google Scholar] [CrossRef]
- Eid, J.I.; Eissa, S.M.; El-Ghor, A.A. Bisphenol A Induces Oxidative Stress and DNA Damage in Hepatic Tissue of Female Rat Offspring. J. Basic Appl. Zool. 2015, 71, 10–19. [Google Scholar] [CrossRef]
- Choi, A.M.; Alam, J. Heme Oxygenase-1: Function, Regulation, and Implication of a Novel Stress-Inducible Protein in Oxidant-Induced Lung Injury. Am. J. Respir. Cell Mol. Biol. 1996, 15, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Sun, X.; Chen, Y.; Li, Y.; Song, L.; Zhou, Z.; Xu, B.; Lin, Y.; Xu, S. Perinatal Exposure to Bisphenol A Exacerbates Nonalcoholic Steatohepatitis-like Phenotype in Male Rat Offspring Fed on a High-Fat Diet. J. Endocrinol. 2014, 222, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Kazemi, S.; Mousavi Kani, S.N.; Rezazadeh, L.; Pouramir, M.; Ghasemi-Kasman, M.; Moghadamnia, A.A. Low Dose Administration of Bisphenol A Induces Liver Toxicity in Adult Rats. Biochem. Biophys. Res. Commun. 2017, 494, 107–112. [Google Scholar] [CrossRef]
- Ijaz, M.U.; Shahab, M.S.; Samad, A.; Ashraf, A.; Al-Ghanim, K.; Mruthinti, S.S.; Mahboob, S. Tangeretin Ameliorates Bisphenol Induced Hepatocyte Injury by Inhibiting Inflammation and Oxidative Stress. Saudi J. Biol. Sci. 2022, 29, 1375–1379. [Google Scholar] [CrossRef]
- Vagvala, S.H.; O’Connor, S.D. Imaging of Abnormal Liver Function Tests. Clin. Liver Dis. 2018, 11, 128–134. [Google Scholar] [CrossRef]
- Nakagawa, Y.; Tayama, S. Metabolism and Cytotoxicity of Bisphenol A and Other Bisphenols in Isolated Rat Hepatocytes. Arch. Toxicol. 2000, 74, 99–105. [Google Scholar] [CrossRef]
- Liu, R.; Liu, B.; Tian, L.; Jiang, X.; Li, X.; Cai, D.; Sun, J.; Bai, W.; Jin, Y. Exposure to Bisphenol A Caused Hepatoxicity and Intestinal Flora Disorder in Rats. Int. J. Mol. Sci. 2022, 23, 8042. [Google Scholar] [CrossRef]
- Kroemer, G.; Galluzzi, L.; Brenner, C. Mitochondrial Membrane Permeabilization in Cell Death. Physiol. Rev. 2007, 87, 99–163. [Google Scholar] [CrossRef]
- Rönn, M.; Kullberg, J.; Karlsson, H.; Berglund, J.; Malmberg, F.; Örberg, J.; Lind, L.; Ahlström, H.; Lind, P.M. Bisphenol A Exposure Increases Liver Fat in Juvenile Fructose-Fed Fischer 344 Rats. Toxicology 2013, 303, 125–132. [Google Scholar] [CrossRef]
- Vaux, D.L. Apoptogenic Factors Released from Mitochondria. Biochim. Biophys. Acta 2011, 1813, 546–550. [Google Scholar] [CrossRef] [PubMed]
- Muntané, J.; González, R.; Ranchal, I.; Collado, J.A.; López-Sánchez, L.M.; Herencia, C.; Rodríguez-Ariza, A.; Muñoz-Castañeda, J.R.; de la Mata, M. Mecanismos de Lesión Hepatocelular. Rev. Esp. Enferm. Dig. 2007, 99, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Kluck, R.M.; Bossy-Wetzel, E.; Green, D.R.; Newmeyer, D.D. The Release of Cytochrome c from Mitochondria: A Primary Site for Bcl-2 Regulation of Apoptosis. Science 1997, 275, 1132–1136. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Osuga, Y.; Yano, T.; Morita, Y.; Tang, X.; Fujiwara, T.; Takai, Y.; Matsumi, H.; Koga, K.; Taketani, Y.; et al. Bisphenol A Induces Apoptosis and G2-to-M Arrest of Ovarian Granulosa Cells. Biochem. Biophys. Res. Commun. 2002, 292, 456–462. [Google Scholar] [CrossRef]
- Pottenger, L.H.; Domoradzki, J.Y.; Markham, D.A.; Hansen, S.C.; Cagen, S.Z.; Waechter, J.M., Jr. The Relative Bioavailability and Metabolism of Bisphenol A in Rats Is Dependent upon the Route of Administration. Toxicol. Sci. 2000, 54, 3–18. [Google Scholar] [CrossRef]
- Gould, J.C.; Leonard, L.S.; Maness, S.C.; Wagner, B.L.; Conner, K.; Zacharewski, T.; Safe, S.; McDonnell, D.P.; Gaido, K.W. Bisphenol A Interacts with the Estrogen Receptor α in a Distinct Manner from Estradiol. Mol. Cell. Endocrinol. 1998, 142, 203–214. [Google Scholar] [CrossRef]
- Vandenberg, L.N.; Maffini, M.V.; Sonnenschein, C.; Rubin, B.S.; Soto, A.M. Bisphenol-A and the Great Divide: A Review of Controversies in the Field of Endocrine Disruption. Endocr. Rev. 2009, 30, 75–95. [Google Scholar] [CrossRef]
- Kuiper, G.G.; Lemmen, J.G.; Carlsson, B.; Corton, J.C.; Safe, S.H.; van der Saag, P.T.; van der Burg, B.; Gustafsson, J.A. Interaction of Estrogenic Chemicals and Phytoestrogens with Estrogen Receptor Beta. Endocrinology 1998, 139, 4252–4263. [Google Scholar] [CrossRef]
- Alonso-Magdalena, P.; Ropero, A.B.; Soriano, S.; García-Arévalo, M.; Ripoll, C.; Fuentes, E.; Quesada, I.; Nadal, Á. Bisphenol-A Acts as a Potent Estrogen via Non-Classical Estrogen Triggered Pathways. Mol. Cell. Endocrinol. 2012, 355, 201–207. [Google Scholar] [CrossRef]
- Thomas, P.; Dong, J. Binding and Activation of the Seven-Transmembrane Estrogen Receptor GPR30 by Environmental Estrogens: A Potential Novel Mechanism of Endocrine Disruption. J. Steroid Biochem. Mol. Biol. 2006, 102, 175–179. [Google Scholar] [CrossRef]
- Ropero, A.B.; Alonso-Magdalena, P.; Ripoll, C.; Fuentes, E.; Nadal, A. Rapid Endocrine Disruption: Environmental Estrogen Actions Triggered Outside the Nucleus. J. Steroid Biochem. Mol. Biol. 2006, 102, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Rochester, J.R. Bisphenol A and Human Health: A Review of the Literature. Reprod. Toxicol. 2013, 42, 132–155. [Google Scholar] [CrossRef] [PubMed]
- Vandenberg, L.N.; Colborn, T.; Hayes, T.B.; Heindel, J.J.; Jacobs, D.R.; Lee, D.-H.; Shioda, T.; Soto, A.M.; vom Saal, F.S.; Welshons, W.V.; et al. Hormones and Endocrine-Disrupting Chemicals: Low-Dose Effects and Nonmonotonic Dose Responses. Endocr. Rev. 2012, 33, 378–455. [Google Scholar] [CrossRef] [PubMed]
- Sewelam, A.S.; Mokhtar, H. Effect of Perinatal Exposure to Low Dose Bisphenol A on Hepatic and Renal Tissues of Male Albino Rat Offspring: Histological, Immunohistochemical and Morphometric Studies. Egypt. J. Histol. 2019, 42, 974–1000. [Google Scholar] [CrossRef]
- Ginsberg, G.; Rice, D.C. Does Rapid Metabolism Ensure Negligible Risk from Bisphenol A? Environ. Health Perspect. 2009, 117, 1639–1643. [Google Scholar] [CrossRef] [PubMed]
- Fouyet, S.; Olivier, E.; Leproux, P.; Dutot, M.; Rat, P. Bisphenol A, Bisphenol F, and Bisphenol S: The Bad and the Ugly. Where Is the Good? Life 2021, 11, 314. [Google Scholar] [CrossRef]
- Nishikawa, M.; Iwano, H.; Yanagisawa, R.; Koike, N.; Inoue, H.; Yokota, H. Placental Transfer of Conjugated Bisphenol A and Subsequent Reactivation in the Rat Fetus. Environ. Health Perspect. 2010, 118, 1196–1203. [Google Scholar] [CrossRef]
- Meng, Z.; Tian, S.; Yan, J.; Jia, M.; Yan, S.; Li, R.; Zhang, R.; Zhu, W.; Zhou, Z. Effects of Perinatal Exposure to BPA, BPF and BPAF on Liver Function in Male Mouse Offspring Involving in Oxidative Damage and Metabolic Disorder. Environ. Pollut. 2019, 247, 935–943. [Google Scholar] [CrossRef]
- Lin, R.; Wu, D.; Wu, F.-J.; Meng, Y.; Zhang, J.-H.; Wang, X.-G.; Jia, L.-H. Non-Alcoholic Fatty Liver Disease Induced by Perinatal Exposure to Bisphenol a Is Associated With Activated MTOR and TLR4/NF-ΚB Signaling Pathways in Offspring Rats. Front. Endocrinol. 2019, 10, 620. [Google Scholar] [CrossRef]
- Santoro, A.; Scafuro, M.; Troisi, J.; Piegari, G.; Di Pietro, P.; Mele, E.; Cappetta, D.; Marino, M.; De Angelis, A.; Vecchione, C.; et al. Multi-Systemic Alterations by Chronic Exposure to a Low Dose of Bisphenol A in Drinking Water: Effects on Inflammation and NAD+-Dependent Deacetylase Sirtuin1 in Lactating and Weaned Rats. Int. J. Mol. Sci. 2021, 22, 9666. [Google Scholar] [CrossRef]
- Crain, D.A.; Janssen, S.J.; Edwards, T.M.; Heindel, J.; Ho, S.; Hunt, P.; Iguchi, T.; Juul, A.; McLachlan, J.A.; Schwartz, J.; et al. Female Reproductive Disorders: The Roles of Endocrine-Disrupting Compounds and Developmental Timing. Fertil. Steril. 2008, 90, 911–940. [Google Scholar] [CrossRef] [PubMed]
- Chomczynski, P.; Sacchi, N. Single-Step Method of RNA Isolation by Acid Guanidinium Thiocyanate-Phenol-Chloroform Extraction. Anal. Biochem. 1987, 162, 156–159. [Google Scholar] [CrossRef] [PubMed]
- Schmittgen, T.D.; Livak, K.J. Analyzing Real-Time PCR Data by the Comparative C(T) Method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef] [PubMed]





| Target Gen | Forward (5′-3′) | Reverse (5′-3′) |
|---|---|---|
| GPx | CAGTTCGGACATCAGGAGAAT | AGAGCGGGTGAGCCTTCT |
| GR | GGGCAAAGAAGATTCCAGGTT | GGACGGCTTCATCTTCAGTGA |
| GST | TTGAGGCACCTGGGTCGCTCTTTAG | GGTTCTGGGACAGCAGGGTCTCAAA |
| γ-GCS | ATCTGGATGATGCCAACGAGTC | CCTCCATTGGTCGGAACTCTACT |
| HO-1d | GTCAAGCACAGGGTGACAGA | ATCACCTGCAGCTCCTCAAA |
| iNOS | CTTTGCCACGGACGAGAC | TCATTGTACTCTGAGGGCTGAC |
| eNOS | CCAGTGCCCTGCTTCATC | GCAGGGCAAGTTAGGATCAG |
| IL-1β | TGTGATGAAAGACGGCACAC | CTTCTTCTTTGGGTATTGTTTGG |
| AIF | AGTCGTTATTGTGGGGTTATCAAC | TTGGTCTTATTTAATAGTCTTGTAGGC |
| BAX | GTGAGCGGCTGCTTGTCT | GTCCCGAAGTAGGAGAGGA |
| 18S | GGTGCATGGCCGTTCTTA | TCGTTCGTTATCGGAATTAAC |
| Antibody | Catalog Number | Company |
|---|---|---|
| HO-1d | AB1284 | Chemicon International, Temecula, CA, USA |
| iNOS | AB16311 | Chemicon International, Temecula, CA, USA |
| eNOS | AB16301 | Chemicon International, Temecula, CA, USA |
| IL-1β | 500-P80 | PeproTech EC, Ltd., London, UK |
| AIF | 5318 | Cell Signaling Technology, Beverly, MA, USA |
| BCL-2 | 2870 | Cell Signaling Technology, Beverly, MA, USA |
| BCL-XL | 21061 | Signalway antibody, College Park, MD, USA |
| GAPDH | 2118 | Cell Signaling Technology, Beverly, MA, USA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Linillos-Pradillo, B.; Rancan, L.; Paredes, S.D.; Schlumpf, M.; Lichtensteiger, W.; Vara, E.; Tresguerres, J.Á.F. Low Dose of BPA Induces Liver Injury through Oxidative Stress, Inflammation and Apoptosis in Long–Evans Lactating Rats and Its Perinatal Effect on Female PND6 Offspring. Int. J. Mol. Sci. 2023, 24, 4585. https://doi.org/10.3390/ijms24054585
Linillos-Pradillo B, Rancan L, Paredes SD, Schlumpf M, Lichtensteiger W, Vara E, Tresguerres JÁF. Low Dose of BPA Induces Liver Injury through Oxidative Stress, Inflammation and Apoptosis in Long–Evans Lactating Rats and Its Perinatal Effect on Female PND6 Offspring. International Journal of Molecular Sciences. 2023; 24(5):4585. https://doi.org/10.3390/ijms24054585
Chicago/Turabian StyleLinillos-Pradillo, Beatriz, Lisa Rancan, Sergio D. Paredes, Margret Schlumpf, Walter Lichtensteiger, Elena Vara, and Jesús Á. F. Tresguerres. 2023. "Low Dose of BPA Induces Liver Injury through Oxidative Stress, Inflammation and Apoptosis in Long–Evans Lactating Rats and Its Perinatal Effect on Female PND6 Offspring" International Journal of Molecular Sciences 24, no. 5: 4585. https://doi.org/10.3390/ijms24054585
APA StyleLinillos-Pradillo, B., Rancan, L., Paredes, S. D., Schlumpf, M., Lichtensteiger, W., Vara, E., & Tresguerres, J. Á. F. (2023). Low Dose of BPA Induces Liver Injury through Oxidative Stress, Inflammation and Apoptosis in Long–Evans Lactating Rats and Its Perinatal Effect on Female PND6 Offspring. International Journal of Molecular Sciences, 24(5), 4585. https://doi.org/10.3390/ijms24054585







