Proteomic Markers for Mechanobiological Properties of Metastatic Cancer Cells
Abstract
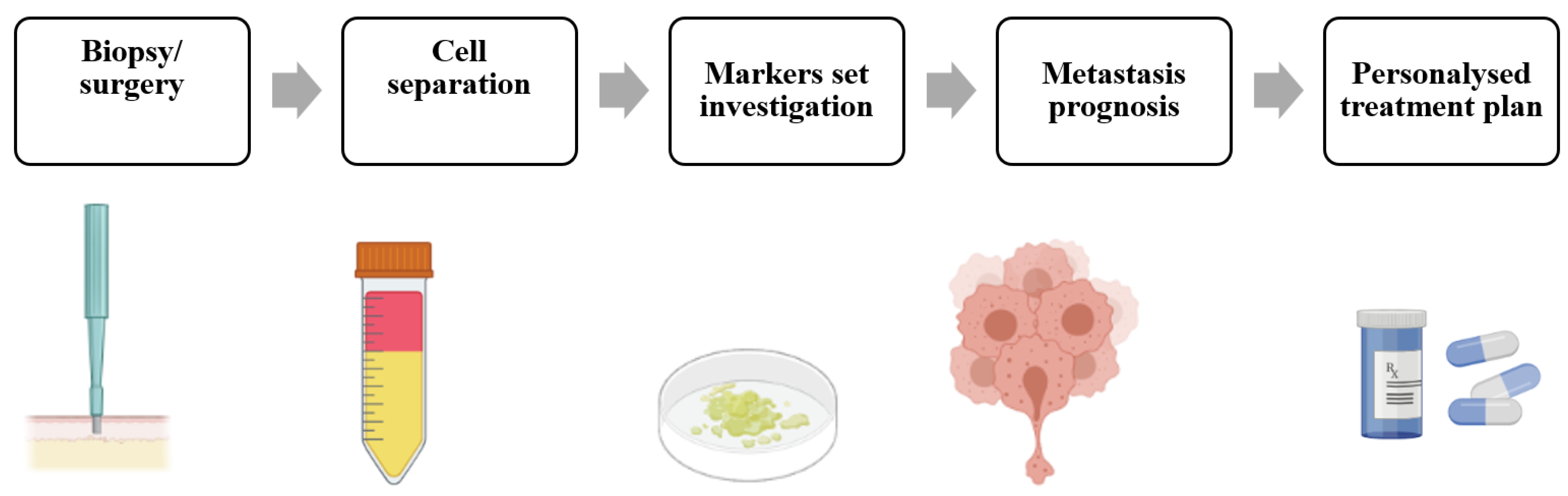
1. A Need for Identification of New Potential Prognostic Markers
2. Tumor Biomarkers
3. Mechanobiology of Metastasis
4. Invasion and Endocytosis
5. Proteins Involved in Actin Cytoskeleton Remodeling
6. Protein Phosphorylation
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yang, J.; Weinberg, R.A. Epithelial-Mesenchymal Transition: At the Crossroads of Development and Tumor Metastasis. Dev. Cell 2008, 14, 818–829. [Google Scholar] [CrossRef]
- Sleeman, J.P.; Nazarenko, I.; Thiele, W. Do All Roads Lead to Rome? Routes to Metastasis Development. Int. J. Cancer 2011, 128, 2511–2526. [Google Scholar] [CrossRef]
- Cairns, R.A.; Khokha, R.; Hill, R.P. Molecular Mechanisms of Tumor Invasion and Metastasis: An Integrated View. Curr. Mol. Med. 2003, 3, 659–671. [Google Scholar] [CrossRef] [PubMed]
- Weigelt, B.; Peterse, J.L.; van ’t Veer, L.J. Breast Cancer Metastasis: Markers and Models. Nat. Rev. Cancer 2005, 5, 591–602. [Google Scholar] [CrossRef]
- Riihimaki, M.; Thomsen, H.; Hemminki, A.; Sundquist, K.; Hemminki, K.; Riihimäki, M.; Thomsen, H.; Hemminki, A.; Sundquist, K.; Hemminki, K.; et al. Comparison of Survival of Patients with Metastases from Known versus Unknown Primaries: Survival in Metastatic Cancer. BMC Cancer 2013, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.A.; Venne, V.; Berse, B. Genetic Tests to Identify Risk for Breast Cancer. Semin. Oncol. Nurs. 2015, 31, 100–107. [Google Scholar] [CrossRef]
- Vaidyanathan, K.; Vasudevan, D.M. Organ Specific Tumor Markers: What’s New? Indian J Clin Biochem 2012, 27, 110–120. [Google Scholar] [CrossRef]
- Gurcan, M.N.; Boucheron, L.E.; Can, A.; Madabhushi, A.; Rajpoot, N.M.; Yener, B. Histopathological Image Analysis: A Review. IEEE Rev. Biomed. Eng. 2009, 2, 147–171. [Google Scholar] [CrossRef]
- Wei, J.W.; Tafe, L.J.; Linnik, Y.A.; Vaickus, L.J.; Tomita, N.; Hassanpour, S. Pathologist-Level Classification of Histologic Patterns on Resected Lung Adenocarcinoma Slides with Deep Neural Networks. Sci. Rep. 2019, 9, 3358. [Google Scholar] [CrossRef]
- Lang, E.V.; Berbaum, K.S.; Lutgendorf, S.K. Large-Core Breast Biopsy: Abnormal Salivary Cortisol Profiles Associated with Uncertainty of Diagnosis. Radiology 2009, 250, 631–637. [Google Scholar] [CrossRef][Green Version]
- Yankaskas, C.L.; Thompson, K.N.; Paul, C.D.; Vitolo, M.I.; Mistriotis, P.; Mahendra, A.; Bajpai, V.K.; Shea, D.J.; Manto, K.M.; Chai, A.C.; et al. A Microfluidic Assay for the Quantification of the Metastatic Propensity of Breast Cancer Specimens. Nat. Biomed. Eng. 2019, 3, 452–465. [Google Scholar] [CrossRef] [PubMed]
- Murugan, A.K. MTOR: Role in Cancer, Metastasis and Drug Resistance. Semin. Cancer Biol. 2019, 59, 92–111. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Qu, X. Cancer Biomarker Detection: Recent Achievements and Challenges. Chem. Soc. Rev. 2015, 44, 2963–2997. [Google Scholar] [CrossRef] [PubMed]
- Narayan Bhatt, A.; Farooque, A.; Verma, A. Cancer Biomarkers-Current Perspectives Role of Tumor Microenvironment in Treatment of Lymphoma and Myeloma View Project Metabolic Signaling Approaches for Anticancer Drug Target Discovery View Project. Artic. Indian J. Med. Res. 2010, 132, 129–149. [Google Scholar]
- Wang, F.; Fang, Q.; Ge, Z.; Yu, N.; Xu, S.; Fan, X. Common BRCA1 and BRCA2 Mutations in Breast Cancer Families: A Meta-Analysis from Systematic Review. Mol. Biol. Rep. 2012, 39, 2109–2118. [Google Scholar] [CrossRef]
- De, P.; Mukhopadhyay, M.J. Study of the Chromosomal Abnormalities and Associated Complex Karyotypes in Hematological Cancer in the Population of West Bengal: A Prospective Observational Study. Indian J. Med. Paediatr. Oncol. 2021, 42, 261–267. [Google Scholar] [CrossRef]
- Wang, C.; Bai, F.; Zhang, L.Z.; Scott, A.; Li, E.; Pei, X.H. Estrogen Promotes Estrogen Receptor Negative BRCA1-Deficient Tumor Initiation and Progression. Breast Cancer Res. 2018, 20, 74. [Google Scholar] [CrossRef]
- Huang, J.; Duran, A.; Reina-Campos, M.; Valencia, T.; Castilla, E.A.; Müller, T.D.; Tschöp, M.H.; Moscat, J.; Diaz-Meco, M.T. Adipocyte P62/SQSTM1 Suppresses Tumorigenesis through Opposite Regulations of Metabolism in Adipose Tissue and Tumor. Cancer Cell 2018, 33, 770–784.e6. [Google Scholar] [CrossRef]
- Szablewski, L. Glucose Transporters as Markers of Diagnosis and Prognosis in Cancer Diseases. Oncol. Rev. 2022, 16, 561. [Google Scholar] [CrossRef]
- Pouliquen, D.; Boissard, A.; Coqueret, O.; Guette, C. Biomarkers of Tumor Invasiveness in Proteomics (Review). Int. J. Oncol. 2020, 57, 409–432. [Google Scholar] [CrossRef]
- Wilt, T.J.; Scardino, P.T.; Carlsson, S.V.; Basch, E. Prostate-Specific Antigen Screening in Prostate Cancer: Perspectives on the Evidence. J. Natl. Cancer Inst. 2014, 106, 10. [Google Scholar] [CrossRef] [PubMed]
- Brufsky, A.M.; Mayer, M.; Rugo, H.S.; Kaufman, P.A.; Tan-Chiu, E.; Tripathy, D.; Tudor, I.C.; Wang, L.I.; Brammer, M.G.; Shing, M.; et al. Central Nervous System Metastases in Patients with HER2-Positive Metastatic Breast Cancer: Incidence, Treatment, and Survival in Patients from RegistHER. Clin. Cancer Res. 2011, 17, 4834–4843. [Google Scholar] [CrossRef] [PubMed]
- Kuba, S.; Ishida, M.; Nakamura, Y.; Yamanouchi, K.; Minami, S.; Taguchi, K.; Eguchi, S.; Ohno, S. Treatment and Prognosis of Breast Cancer Patients with Brain Metastases According to Intrinsic Subtype. Jpn. J. Clin. Oncol. 2014, 44, 1025–1031. [Google Scholar] [CrossRef] [PubMed]
- Molinie, N.; Rubtsova, S.N.; Fokin, A.; Visweshwaran, S.P.; Rocques, N.; Polesskaya, A.; Schnitzler, A.; Vacher, S.; Denisov, E.V.; Tashireva, L.A.; et al. Cortical Branched Actin Determines Cell Cycle Progression. Cell Res. 2019, 29, 432–445. [Google Scholar] [CrossRef]
- Geiger, T.; Cox, J.; Mann, M. Proteomic Changes Resulting from Gene Copy Number Variations in Cancer Cells. PLoS Genet. 2010, 6, e1001090. [Google Scholar] [CrossRef]
- Murakami, T.; Kikuchi, H.; Ishimatsu, H.; Iino, I.; Hirotsu, A.; Matsumoto, T.; Ozaki, Y.; Kawabata, T.; Hiramatsu, Y.; Ohta, M.; et al. Tenascin C in Colorectal Cancer Stroma Is a Predictive Marker for Liver Metastasis and Is a Potent Target of MiR-198 as Identified by MicroRNA Analysis. Br. J. Cancer 2017, 117, 1360–1370. [Google Scholar] [CrossRef]
- Guck, J.; Schinkinger, S.; Lincoln, B.; Wottawah, F.; Ebert, S.; Romeyke, M.; Lenz, D.; Erickson, H.M.; Ananthakrishnan, R.; Mitchell, D.; et al. Optical Deformability as an Inherent Cell Marker for Testing Malignant Transformation and Metastatic Competence. Biophys. J. 2005, 88, 3689–3698. [Google Scholar] [CrossRef]
- Qi, D.; Gill, N.K.; Santiskulvong, C.; Sifuentes, J.; Dorigo, O.; Rao, J.; Taylor-Harding, B.; Wiedemeyer, W.R.; Rowat, A.C. Screening Cell Mechanotype by Parallel Microfiltration. Sci. Rep. 2015, 5, 17595. [Google Scholar] [CrossRef]
- Byun, S.; Son, S.; Amodei, D.; Cermak, N.; Shaw, J.; Kang, J.H.; Hecht, V.C.; Winslow, M.M.; Jacks, T.; Mallick, P.; et al. Characterizing Deformability and Surface Friction of Cancer Cells. Proc. Natl. Acad. Sci. USA 2013, 110, 7580–7585. [Google Scholar] [CrossRef]
- Paszek, M.J.; Zahir, N.; Johnson, K.R.; Lakins, J.N.; Rozenberg, G.I.; Gefen, A.; Reinhart-King, C.A.; Margulies, S.S.; Dembo, M.; Boettiger, D.; et al. Tensional Homeostasis and the Malignant Phenotype. Cancer Cell 2005, 8, 241–254. [Google Scholar] [CrossRef]
- Guck, J.; Ananthakrishnan, R.; Mahmood, H.; Moon, T.J.; Cunningham, C.C.; Käs, J. The Optical Stretcher: A Novel Laser Tool to Micromanipulate Cells. Biophys. J. 2001, 81, 767. [Google Scholar] [CrossRef] [PubMed]
- Gossett, D.R.; Tse, H.T.K.; Lee, S.A.; Ying, Y.; Lindgren, A.G.; Yang, O.O.; Rao, J.; Clark, A.T.; Di Carlo, D. Hydrodynamic Stretching of Single Cells for Large Population Mechanical Phenotyping. Proc. Natl. Acad. Sci. USA 2012, 109, 7630–7635. [Google Scholar] [CrossRef]
- Lekka, M.; Laidler, P.; Gil, D.; Lekki, J.; Stachura, Z.; Hrynkiewicz, A.Z. Elasticity of Normal and Cancerous Human Bladder Cells Studied by Scanning Force Microscopy. Eur. Biophys. J. 1999, 28, 312–316. [Google Scholar] [CrossRef] [PubMed]
- Mak, M.; Spill, F.; Kamm, R.D.; Zaman, M.H. Single-Cell Migration in Complex Microenvironments: Mechanics and Signaling Dynamics. J. Biomech. Eng. 2016, 138, 021004. [Google Scholar] [CrossRef]
- Pachenari, M.; Seyedpour, S.M.; Janmaleki, M.; Shayan, S.B.; Taranejoo, S.; Hosseinkhani, H. Mechanical Properties of Cancer Cytoskeleton Depend on Actin Filaments to Microtubules Content: Investigating Different Grades of Colon Cancer Cell Lines. J. Biomech. 2014, 47, 373–379. [Google Scholar] [CrossRef]
- Ketene, A.N.; Schmelz, E.M.; Roberts, P.C.; Agah, M. The Effects of Cancer Progression on the Viscoelasticity of Ovarian Cell Cytoskeleton Structures. Nanomedicine 2012, 8, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Ochalek, T.; Nordt, F.J.; Tullberg, K.; Burger, M.M. Correlation between Cell Deformability and Metastatic Potential in B16-F1 Melanoma Cell Variants. Cancer Res. 1988, 48, 5124–5128. [Google Scholar]
- Kramer, N.; Walzl, A.; Unger, C.; Rosner, M.; Krupitza, G.; Hengstschläger, M.; Dolznig, H. In Vitro Cell Migration and Invasion Assays. Mutat. Res.—Rev. Mutat. Res. 2013, 752, 10–24. [Google Scholar] [CrossRef]
- Paul, C.D.; Mistriotis, P.; Konstantopoulos, K. Cancer Cell Motility: Lessons from Migration in Confined Spaces. Nat. Rev. Cancer 2017, 17, 131–140. [Google Scholar] [CrossRef]
- Van Golen, K.L.; Wu, Z.F.; Xiao, X.T.; Bao, L.W.; Merajver, S.D. RhoC GTPase, a Novel Transforming Oncogene for Human Mammary Epithelial Cells That Partially Recapitulates the Inflammatory Breast Cancer Phenotype. Cancer Res. 2000, 60, 5832–5838. [Google Scholar]
- Lin, M.; DiVito, M.M.; Merajver, S.D.; Boyanapalli, M.; van Golen, K.L. Regulation of Pancreatic Cancer Cell Migration and Invasion by RhoC GTPase and Caveolin-1. Mol. Cancer 2005, 4, 21. [Google Scholar] [CrossRef] [PubMed]
- Shelby, J.P.; White, J.; Ganesan, K.; Rathod, P.K.; Chiu, D.T. A Microfluidic Model for Single-Cell Capillary Obstruction by Plasmodium Falciparum-Infected Erythrocytes. Proc. Natl. Acad. Sci. USA 2003, 100, 14618–14622. [Google Scholar] [CrossRef] [PubMed]
- Lautscham, L.A.; Kämmerer, C.; Lange, J.R.; Kolb, T.; Mark, C.; Schilling, A.; Strissel, P.L.; Strick, R.; Gluth, C.; Rowat, A.C.; et al. Migration in Confined 3D Environments Is Determined by a Combination of Adhesiveness, Nuclear Volume, Contractility, and Cell Stiffness. Biophys. J. 2015, 109, 900–913. [Google Scholar] [CrossRef]
- Mak, M.; Reinhart-King, C.A.; Erickson, D. Elucidating Mechanical Transition Effects of Invading Cancer Cells with a Subnucleus-Scaled Microfluidic Serial Dimensional Modulation Device. Lab Chip 2013, 13, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Albini, A.; Benelli, R. The Chemoinvasion Assay: A Method to Assess Tumor and Endothelial Cell Invasion and Its Modulation. Nat. Protoc. 2007, 2, 504–511. [Google Scholar] [CrossRef] [PubMed]
- McEwan, R.N.; Kleinman, H.K.; Martin, G.R. A Rapid in Vitro Assay for Quantitating the Invasive Potential of Tumor Cells. Cancer Res. 1987, 47, 3239–3245. [Google Scholar]
- Justus, C.R.; Leffler, N.; Ruiz-Echevarria, M.; Yang, L.V. In Vitro Cell Migration and Invasion Assays. J. Vis. Exp. 2014, 88, 51046. [Google Scholar] [CrossRef]
- Sieuwerts, A.M.; Klijn, J.G.M.; Foekens, J.A. Assessment of the Invasive Potential of Human Gynecological Tumor Cell Lines with the in Vitro Boyden Chamber Assay: Influences of the Ability of Cells to Migrate through the Filter Membrane. Clin. Exp. Metastasis 1997, 15, 53–62. [Google Scholar] [CrossRef]
- Nyström, M.L.; Thomas, G.J.; Stone, M.; Mackenzie, I.C.; Hart, I.R.; Marshall, J.F. Development of a Quantitative Method to Analyse Tumour Cell Invasion in Organotypic Culture. J. Pathol. 2005, 205, 468–475. [Google Scholar] [CrossRef]
- Ayala, I.; Baldassarre, M.; Caldieri, G.; Buccione, R. Invadopodia: A Guided Tour. Eur. J. Cell Biol. 2006, 85, 159–164. [Google Scholar] [CrossRef]
- Artym, V.V.; Yamada, K.M.; Mueller, S.C. ECM Degradation Assays for Analyzing Local Cell Invasion. Methods Mol. Biol. 2009, 522, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Merkher, Y.; Horesh, Y.; Abramov, Z.; Shleifer, G.; Ben-Ishay, O.; Kluger, Y.; Weihs, D. Rapid Cancer Diagnosis and Early Prognosis of Metastatic Risk Based on Mechanical Invasiveness of Sampled Cells. Ann. Biomed. Eng. 2020, 48, 2846–2858. [Google Scholar] [CrossRef] [PubMed]
- Merkher, Y.; Weihs, D. Proximity of Metastatic Cells Enhances Their Mechanobiological Invasiveness. Ann. Biomed. Eng. 2017, 45, 1399–1406. [Google Scholar] [CrossRef] [PubMed]
- Merkher, Y.; Alvarez-Elizondo, M.B.; Weihs, D. Taxol Reduces Synergistic, Mechanobiological Invasiveness of Metastatic Cells. Converg. Sci. Phys. Oncol. 2017, 3, 044002. [Google Scholar] [CrossRef]
- Merkher, Y.; Kontareva, E.; Melekhova, A.; Leonov, S. Abstract PO-042: Nanoparticles Imaging for Cancer Metastasis Diagnosis. Clin. Cancer Res. 2021, 27, PO-042. [Google Scholar] [CrossRef]
- Merkher Yulia; Kontareva Elizaveta; Bogdan Elizaveta; Achkasov Konstantin; Grolman Joshua; Leonov Sergey Nanoparticle Cellular Endocytosis as Potential Prognostic Biomarker for Cancer Progression. FEBS Open Bio 2021, 11, 429–430. [CrossRef]
- Li, Y.; Zhang, H.; Merkher, Y.; Chen, L.; Liu, N.; Leonov, S.; Chen, Y. Recent Advances in Therapeutic Strategies for Triple-Negative Breast Cancer. J. Hematol. Oncol. 2022, 15, 121. [Google Scholar] [CrossRef]
- Ghosh, M.; Song, X.; Mouneimne, G.; Sidani, M.; Lawrence, D.S.; Condeelis, J.S. Cofilin Promotes Actin Polymerization and Defines the Direction of Cell Motility. Science 2004, 304, 743–746. [Google Scholar] [CrossRef]
- Ballestrem, C.; Wehrle-Haller, B.; Hinz, B.; Imhof, B.A. Actin-Dependent Lamellipodia Formation and Microtubule-Dependent Tail Retraction Control-Directed Cell Migration. Mol. Biol. Cell 2000, 11, 2999–3012. [Google Scholar] [CrossRef]
- Campellone, K.G.; Welch, M.D. A Nucleator Arms Race: Cellular Control of Actin Assembly. Nat. Rev. Mol. Cell Biol. 2010, 11, 237–251. [Google Scholar] [CrossRef]
- Yang, Q.; Zhang, X.F.; Pollard, T.D.; Forscher, P. Arp2/3 Complex-Dependent Actin Networks Constrain Myosin II Function in Driving Retrograde Actin Flow. J. Cell Biol. 2012, 197, 939–956. [Google Scholar] [CrossRef]
- Génot, E.; Gligorijevic, B. Invadosomes in Their Natural Habitat. Eur. J. Cell Biol. 2014, 93, 367–379. [Google Scholar] [CrossRef] [PubMed]
- Winograd-Katz, S.E.; Brunner, M.C.; Mirlas, N.; Geiger, B. Analysis of the Signaling Pathways Regulating Src-Dependent Remodeling of the Actin Cytoskeleton. Eur. J. Cell Biol. 2011, 90, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Destaing, O.; Block, M.R.; Planus, E.; Albiges-Rizo, C. Invadosome Regulation by Adhesion Signaling. Curr. Opin. Cell Biol. 2011, 23, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Nakchbandi, I.; Ruppert, R.; Kawelke, N.; Hess, M.W.; Pfaller, K.; Jurdic, P.; Fässler, R.; Moser, M. Kindlin-3-Mediated Signaling from Multiple Integrin Classes Is Required for Osteoclast-Mediated Bone Resorption. J. Cell Biol. 2011, 192, 883–897. [Google Scholar] [CrossRef] [PubMed]
- Mierke, C.T. Mechanical Cues Affect Migration and Invasion of Cells From Three Different Directions. Front. Cell Dev. Biol. 2020, 8, 946. [Google Scholar] [CrossRef]
- Akamatsu, M.; Vasan, R.; Serwas, D.; Ferrin, M.; Rangamani, P.; Drubin, D.G. Principles of Self-Organization and Load Adaptation by the Actin Cytoskeleton during Clathrin-Mediated Endocytosis. Elife 2020, 9, e49840. [Google Scholar] [CrossRef]
- Weston, L.; Coutts, A.S.; La Thangué, N.B. Actin Nucleators in the Nucleus: An Emerging Theme. J. Cell Sci. 2012, 125, 3519–3527. [Google Scholar] [CrossRef]
- Pollard, T.D.; Cooper, J.A. Actin, a Central Player in Cell Shape and Movement. Science 2009, 326, 1208–1212. [Google Scholar] [CrossRef]
- Sirotkin, V. Cell Biology: Actin Keeps Endocytosis on a Short Leash. Curr. Biol. 2011, 21, R552–R554. [Google Scholar] [CrossRef]
- Gheorghe, D.M.; Aghamohammadzadeh, S.; Smaczynska-de Rooij, I.I.; Allwood, E.G.; Winder, S.J.; Ayscough, K.R. Interactions between the Yeast SM22 Homologue Scp1 and Actin Demonstrate the Importance of Actin Bundling in Endocytosis. J. Biol. Chem. 2008, 283, 15037–15046. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Galletta, B.J.; Schmidt, K.O.; Chang, F.S.; Blumer, K.J.; Cooper, J.A. Actin-Based Motility during Endocytosis in Budding Yeast. Mol. Biol. Cell 2006, 17, 1354–1363. [Google Scholar] [CrossRef] [PubMed]
- Kaksonen, M.; Toret, C.P.; Drubin, D.G. A Modular Design for the Clathrin- and Actin-Mediated Endocytosis Machinery. Cell 2005, 123, 305–320. [Google Scholar] [CrossRef]
- Galletta, B.J.; Cooper, J.A. Actin and Endocytosis: Mechanisms and Phylogeny. Curr. Opin. Cell Biol. 2009, 21, 20–27. [Google Scholar] [CrossRef]
- Pishvaee, B.; Costaguta, G.; Yeung, B.G.; Ryazantsev, S.; Greener, T.; Greene, L.E.; Eisenberg, E.; McCaffery, J.M.; Payne, G.S. A Yeast DNA J Protein Required for Uncoating of Clathrin-Coated Vesicles in Vivo. Nat. Cell Biol. 2000, 2, 958–963. [Google Scholar] [CrossRef]
- Toret, C.P.; Lee, L.; Sekiya-Kawasaki, M.; Drubin, D.G. Multiple Pathways Regulate Endocytic Coat Disassembly in Saccharomyces Cerevisiae for Optimal Downstream Trafficking. Traffic 2008, 9, 848–859. [Google Scholar] [CrossRef] [PubMed]
- Galletta, B.J.; Chuang, D.Y.; Cooper, J.A. Distinct Roles for Arp2/3 Regulators in Actin Assembly and Endocytosis. PLoS Biol. 2008, 6, e1. [Google Scholar] [CrossRef]
- Merrifield, C.J.; Qualmann, B.; Kessels, M.M.; Almers, W. Neural Wiskott Aldrich Syndrome Protein (N-WASP) and the Arp 2/3 Complex Are Recruited to Sites of Clathrin-Mediated Endocytosis in Cultured Fibroblasts. Eur. J. Cell Biol. 2004, 83, 13–18. [Google Scholar] [CrossRef]
- Jonas, O.; Mierke, C.T.; Käs, J.A. Invasive Cancer Cell Lines Exhibit Biomechanical Properties That Are Distinct from Their Noninvasive Counterparts. Soft Matter 2011, 7, 11488–11495. [Google Scholar] [CrossRef]
- Smythe, E.; Ayscough, K.R. Actin Regulation in Endocytosis. J. Cell Sci. 2006, 119, 4589–4598. [Google Scholar] [CrossRef]
- Alvarez-Elizondo, M.B.M.B.M.B.; Merkher, Y.; Shleifer, G.; Gashri, C.; Weihs, D. Actin as a Target to Reduce Cell Invasiveness in Initial Stages of Metastasis. Ann. Biomed. Eng. 2020, 49, 1342–1352. [Google Scholar] [CrossRef] [PubMed]
- Bearer, E.L. Role of Actin Polymerization in Cell Locomotion: Molecules and Models. Am. J. Respir. Cell Mol. Biol. 1993, 8, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Taunton, J.; Rowning, B.A.; Coughlin, M.L.; Wu, M.; Moon, R.T.; Mitchison, T.J.; Larabell, C.A. Actin-Dependent Propulsion of Endosomes and Lysosomes by Recruitment of N-WASP. J. Cell Biol. 2000, 148, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Grassart, A.; Drubin, D.G. Myosin 1E Coordinates Actin Assembly and Cargo Trafficking during Clathrin-Mediated Endocytosis. Mol. Biol. Cell 2012, 23, 2891–2904. [Google Scholar] [CrossRef]
- Wilkinson, S.; Paterson, H.F.; Marshall, C.J. Cdc42-MRCK and Rho-ROCK Signalling Cooperate in Myosin Phosphorylation and Cell Invasion. Nat. Cell Biol. 2005, 7, 255–261. [Google Scholar] [CrossRef]
- Echarri, A.; Del Pozo, M.A. Caveolae—Mechanosensitive Membrane Invaginations Linked to Actin Filaments. J. Cell Sci. 2015, 128, 2747–2758. [Google Scholar] [CrossRef]
- O’Connor, K.L.; Chen, M. Dynamic Functions of RhoA in Tumor Cell Migration and Invasion. Small GTPases 2013, 4, 141–147. [Google Scholar] [CrossRef]
- Cavallaro, U.; Christofori, G. Cell Adhesion and Signalling by Cadherins and Ig-CAMs in Cancer. Nat. Rev. Cancer 2004, 4, 118–132. [Google Scholar] [CrossRef]
- Shankar, J.; Nabi, I.R. Actin Cytoskeleton Regulation of Epithelial Mesenchymal Transition in Metastatic Cancer Cells. PLoS ONE 2015, 10, e0119954. [Google Scholar] [CrossRef]
- Bor, L.T.; Ee, L.N. Rabs and Cancer Cell Motility. Cell Motil. Cytoskelet. 2009, 66, 365–370. [Google Scholar]
- Caswell, P.T.; Spence, H.J.; Parsons, M.; White, D.P.; Clark, K.; Cheng, K.W.; Mills, G.B.; Humphries, M.J.; Messent, A.J.; Anderson, K.I.; et al. Rab25 Associates with A5β1 Integrin to Promote Invasive Migration in 3D Microenvironments. Dev. Cell 2007, 13, 496–510. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.W.; Lahad, J.P.; Kuo, W.L.; Lapuk, A.; Yamada, K.; Auersperg, N.; Liu, J.; Smith-McCune, K.; Lu, K.H.; Fishman, D.; et al. The RAB25 Small GTPase Determines Aggressiveness of Ovarian and Breast Cancers. Nat. Med. 2004, 10, 1251–1256. [Google Scholar] [CrossRef]
- Jeong, B.Y.; Cho, K.H.; Jeong, K.J.; Park, Y.Y.; Kim, J.M.; Rha, S.Y.; Park, C.G.; Mills, G.B.; Cheong, J.H.; Lee, H.Y. Rab25 Augments Cancer Cell Invasiveness through a Β1 Integrin/EGFR/VEGF-A/Snail Signaling Axis and Expression of Fascin. Exp. Mol. Med. 2018, 50, e435. [Google Scholar] [CrossRef] [PubMed]
- Paul, N.R.; Jacquemet, G.; Caswell, P.T. Endocytic Trafficking of Integrins in Cell Migration. Curr. Biol. 2015, 25, R1092–R1105. [Google Scholar] [CrossRef] [PubMed]
- Caswell, P.T.; Chan, M.; Lindsay, A.J.; McCaffrey, M.W.; Boettiger, D.; Norman, J.C. Rab-Coupling Protein Coordinates Recycling of A5β1 Integrin and EGFR1 to Promote Cell Migration in 3D Microenvironments. J. Cell Biol. 2008, 183, 143–155. [Google Scholar] [CrossRef]
- Jones, M.C.; Caswell, P.T.; Norman, J.C. Endocytic Recycling Pathways: Emerging Regulators of Cell Migration. Curr. Opin. Cell Biol. 2006, 18, 549–557. [Google Scholar] [CrossRef]
- Kawauchi, T. Cell Adhesion and Its Endocytic Regulation in Cell Migration during Neural Development and Cancer Metastasis. Int. J. Mol. Sci. 2012, 13, 4564–4590. [Google Scholar] [CrossRef]
- Weber, G.F. Molecular Mechanisms of Metastasis. Cancer Lett. 2008, 270, 181–190. [Google Scholar] [CrossRef]
- Ponta, H.; Sherman, L.; Herrlich, P.A. CD44: From Adhesion Molecules to Signalling Regulators. Nat. Rev. Mol. Cell Biol. 2003, 4, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Müller, S.; Sindikubwabo, F.; Cañeque, T.; Lafon, A.; Versini, A.; Lombard, B.; Loew, D.; Wu, T.; Wu, T.D.; Ginestier, C.; et al. CD44 Regulates Epigenetic Plasticity by Mediating Iron Endocytosis. Nat. Chem. 2020, 12, 929–938. [Google Scholar] [CrossRef] [PubMed]
- Rim, E.Y.; Kinney, L.K.; Nusse, R. β-Catenin-Mediated Wnt Signal Transduction Proceeds through an Endocytosis-Independent Mechanism. Mol. Biol. Cell 2020, 31, 1425–1436. [Google Scholar] [CrossRef]
- Zhu, W.; Wang, H.; Zhu, D. Wnt/β-Catenin Signaling Pathway in Lung Cancer. Med. Drug Discov. 2022, 13, 100113. [Google Scholar] [CrossRef]
- Garcin, C.; Straube, A. Microtubules in Cell Migration. Essays Biochem. 2019, 63, 509–520. [Google Scholar]
- Palamidessi, A.; Frittoli, E.; Garré, M.; Faretta, M.; Mione, M.; Testa, I.; Diaspro, A.; Lanzetti, L.; Scita, G.; Di Fiore, P.P. Endocytic Trafficking of Rac Is Required for the Spatial Restriction of Signaling in Cell Migration. Cell 2008, 134, 135–147. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, H.; Condeelis, J. Regulation of the Actin Cytoskeleton in Cancer Cell Migration and Invasion. Biochim. Biophys. Acta—Mol. Cell Res. 2007, 1773, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Iwaya, K.; Norio, K.; Mukai, K. Coexpression of Arp2 and WAVE2 Predicts Poor Outcome in Invasive Breast Carcinoma. Mod. Pathol. 2007, 20, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Sah, P.; Sharma, S.; Radhakrishnan, R. Molecular Changes in Invasive Front of Oral Cancer. J. Oral Maxillofac. Pathol. 2013, 17, 240–247. [Google Scholar]
- Clark, E.S.; Brown, B.; Whigham, A.S.; Kochaishvili, A.; Yarbrough, W.G.; Weaver, A.M. Aggressiveness of HNSCC Tumors Depends on Expression Levels of Cortactin, a Gene in the 11q13 Amplicon. Oncogene 2009, 28, 431–444. [Google Scholar] [CrossRef]
- Weaver, A.M.; Karginov, A.V.; Kinley, A.W.; Weed, S.A.; Li, Y.; Parsons, J.T.; Cooper, J.A. Cortactin Promotes and Stabilizes Arp2/3-Induced Actin Filament Network Formation. Curr. Biol. 2001, 11, 370–374. [Google Scholar] [CrossRef]
- Mader, C.C.; Oser, M.; Magalhaes, M.A.O.; Bravo-Cordero, J.J.; Condeelis, J.; Koleske, A.J.; Gil-Henn, H. An EGFR-Src-Arg-Cortactin Pathway Mediates Functional Maturation of Invadopodia and Breast Cancer Cell Invasion. Cancer Res. 2011, 71, 1730–1741. [Google Scholar] [CrossRef]
- Zhu, J.; Yu, D.; Zeng, X.C.; Zhou, K.; Zhan, X. Receptor-Mediated Endocytosis Involves Tyrosine Phosphorylation of Cortactin. J. Biol. Chem. 2007, 282, 16086–16094. [Google Scholar] [CrossRef]
- Trochet, D.; Bitoun, M. A Review of Dynamin 2 Involvement in Cancers Highlights a Promising Therapeutic Target. J. Exp. Clin. Cancer Res. 2021, 40, 238. [Google Scholar] [CrossRef]
- Molinie, N.; Gautreau, A. The Arp2/3 Regulatory System and Its Deregulation in Cancer. Physiol. Rev. 2018, 98, 215–238. [Google Scholar] [CrossRef]
- Papalazarou, V.; Machesky, L.M. The Cell Pushes Back: The Arp2/3 Complex Is a Key Orchestrator of Cellular Responses to Environmental Forces. Curr. Opin. Cell Biol. 2021, 68, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Gerashchenko, T.S.; Novikov, N.M.; Krakhmal, N.V.; Zolotaryova, S.Y.; Zavyalova, M.V.; Cherdyntseva, N.V.; Denisov, E.V.; Perelmuter, V.M. Markers of Cancer Cell Invasion: Are They Good Enough? J. Clin. Med. 2019, 8, 1092. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Xie, H.; Dou, Y.; Yuan, J.; Zeng, D.; Xiao, S. Expression and Function of FRA1 Protein in Tumors. Mol. Biol. Rep. 2020, 47, 737–752. [Google Scholar] [CrossRef] [PubMed]
- Llorens, M.C.; Rossi, F.A.; García, I.A.; Cooke, M.; Abba, M.C.; Lopez-Haber, C.; Barrio-Real, L.; Vaglienti, M.V.; Rossi, M.; Bocco, J.L.; et al. PKCα Modulates Epithelial-to-Mesenchymal Transition and Invasiveness of Breast Cancer Cells Through ZEB1. Front. Oncol. 2019, 9, 1323. [Google Scholar] [CrossRef]
- Vuoriluoto, K.; Haugen, H.; Kiviluoto, S.; Mpindi, J.P.; Nevo, J.; Gjerdrum, C.; Tiron, C.; Lorens, J.B.; Ivaska, J. Vimentin Regulates EMT Induction by Slug and Oncogenic H-Ras and Migration by Governing Axl Expression in Breast Cancer. Oncogene 2011, 30, 1436–1448. [Google Scholar] [CrossRef]
- Geletu, M.; Mohan, R.; Arulanandam, R.; Berger-Becvar, A.; Nabi, I.R.; Gunning, P.T.; Raptis, L. Reciprocal Regulation of the Cadherin-11/Stat3 Axis by Caveolin-1 in Mouse Fibroblasts and Lung Carcinoma Cells. Biochim. Biophys. Acta—Mol. Cell Res. 2018, 1865, 794–802. [Google Scholar] [CrossRef]
- Arpaia, E.; Blaser, H.; Quintela-Fandino, M.; Duncan, G.; Leong, H.S.; Ablack, A.; Nambiar, S.C.; Lind, E.F.; Silvester, J.; Fleming, C.K.; et al. The Interaction between Caveolin-1 and Rho-GTPases Promotes Metastasis by Controlling the Expression of Alpha5-Integrin and the Activation of Src, Ras and Erk. Oncogene 2012, 31, 884–896. [Google Scholar] [CrossRef]
- Ni, K.; Wang, C.; Carnino, J.M.; Jin, Y. The Evolving Role of Caveolin-1: A Critical Regulator of Extracellular Vesicles. Med. Sci. 2020, 8, 46. [Google Scholar] [CrossRef] [PubMed]
- Henry, N.L.; Hayes, D.F. Cancer Biomarkers. Mol. Oncol. 2012, 6, 140–146. [Google Scholar] [CrossRef]
- Goicoechea, S.M.; Bednarski, B.; García-Mata, R.; Prentice-Dunn, H.; Kim, H.J.; Otey, C.A. Palladin Contributes to Invasive Motility in Human Breast Cancer Cells. Oncogene 2009, 28, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Layseca, P.; Jäntti, N.Z.; Godbole, R.; Sommer, C.; Jacquemet, G.; Al-Akhrass, H.; Conway, J.R.W.; Kronqvist, P.; Kallionpää, R.E.; Oliveira-Ferrer, L.; et al. Cargo-Specific Recruitment in Clathrin- and Dynamin-Independent Endocytosis. Nat. Cell Biol. 2021, 23, 1073–1084. [Google Scholar] [CrossRef]
- Lee, K.-M.; Nam, K.; Oh, S.; Lim, J.; Kim, Y.P.; Lee, W.W.; Yu, J.H.; Ahn, S.H.; Kim, S.B.; Noh, D.Y.; et al. Extracellular Matrix Protein 1 Regulates Cell Proliferation and Trastuzumab Resistance through Activation of Epidermal Growth Factor Signaling. Breast Cancer Res. 2014, 16, 479. [Google Scholar] [CrossRef]
- Huh, Y.H.; Oh, S.; Yeo, Y.R.; Chae, I.H.; Kim, S.H.; Lee, J.S.; Yun, S.J.; Choi, K.Y.; Ryu, J.H.; Jun, C.D.; et al. Swiprosin-1 Stimulates Cancer Invasion and Metastasis by Increasing the Rho Family of GTPase Signaling. Oncotarget 2015, 6, 13060–13071. [Google Scholar] [CrossRef]
- Qi, H.; Liu, S.; Guo, C.; Wang, J.; Greenaway, F.T.; Sun, M.Z. Role of Annexin A6 in Cancer. Oncol. Lett. 2015, 10, 1947–1952. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.L.; Luo, H.L.; Huang, C.C.; Liu, T.T.; Huang, E.Y.; Sung, M.T.; Lin, J.J.; Chiang, P.H.; Chen, Y.T.; Kang, C.H.; et al. Galectin-1 Overexpression Activates the FAK/PI3K/AKT/MTOR Pathway and Is Correlated with Upper Urinary Urothelial Carcinoma Progression and Survival. Cells 2020, 9, 806. [Google Scholar] [CrossRef]
- Wang, J.F.; Chen, Y.Y.; Zhang, S.W.; Zhao, K.; Qiu, Y.; Wang, Y.; Wang, J.C.; Yu, Z.; Li, B.P.; Wang, Z.; et al. ITGA5 Promotes Tumor Progression through the Activation of the FAK/AKT Signaling Pathway in Human Gastric Cancer. Oxid. Med. Cell. Longev. 2022, 2022, 8611306. [Google Scholar] [CrossRef]
- Chen, J.; Yang, P.; Yang, J.; Wen, Z.; Zhang, B.; Zheng, X. GIT1 Is a Novel Prognostic Biomarker and Facilitates Tumor Progression via Activating ERK/MMP9 Signaling in Hepatocellular Carcinoma. OncoTargets Ther. 2015, 8, 3731. [Google Scholar] [CrossRef]
- Mendoza, M.C.; Vilela, M.; Juarez, J.E.; Blenis, J.; Danuser, G. ERK Reinforces Actin Polymerization to Power Persistent Edge Protrusion during Motility. Sci. Signal. 2015, 8, ra47. [Google Scholar] [CrossRef]
- Taniuchi, K.; Yawata, T.; Tsuboi, M.; Ueba, T.; Saibara, T. Efficient Delivery of Small Interfering RNAs Targeting Particular MRNAs into Pancreatic Cancer Cells Inhibits Invasiveness and Metastasis of Pancreatic Tumors. Oncotarget 2019, 10, 2869. [Google Scholar] [CrossRef]
- Rana, P.S.; Alkrekshi, A.; Wang, W.; Markovic, V.; Sossey-Alaoui, K. The Role of WAVE2 Signaling in Cancer. Biomedicines 2021, 9, 1217. [Google Scholar] [CrossRef]
- Song, F.; Chen, F.Y.; Wu, S.Y.; Hu, B.; Liang, X.L.; Yang, H.Q.; Cheng, J.W.; Wang, P.X.; Guo, W.; Zhou, J.; et al. Mucin 1 Promotes Tumor Progression through Activating WNT/β-Catenin Signaling Pathway in Intrahepatic Cholangiocarcinoma. J. Cancer 2021, 12, 6937–6947. [Google Scholar] [CrossRef] [PubMed]
- Bengoa-Vergniory, N.; Kypta, R.M. Canonical and Noncanonical Wnt Signaling in Neural Stem/Progenitor Cells. Cell. Mol. Life Sci. 2015, 72, 4157–4172. [Google Scholar] [CrossRef] [PubMed]
- Srichai, M.B.; Zent, R. Integrin Structure and Function. In Cell-Extracellular Matrix Interactions in Cancer; Springer: New York, NY, USA, 2010; pp. 19–41. [Google Scholar] [CrossRef]
- Wozniak, M.A.; Modzelewska, K.; Kwong, L.; Keely, P.J. Focal Adhesion Regulation of Cell Behavior. Biochim. Biophys. Acta—Mol. Cell Res. 2004, 1692, 103–119. [Google Scholar] [CrossRef]
- Ginestier, C.; Liu, S.; Diebel, M.E.; Korkaya, H.; Luo, M.; Brown, M.; Wicinski, J.; Cabaud, O.; Charafe-Jauffret, E.; Birnbaum, D.; et al. CXCR1 Blockade Selectively Targets Human Breast Cancer Stem Cells in Vitro and in Xenografts. J. Clin. Investig. 2010, 120, 485–497. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Bauden, M.; Andersson, R.; Hu, D.; Marko-Varga, G.; Xu, J.; Sasor, A.; Dai, H.; Pawłowski, K.; Said Hilmersson, K.; et al. YAP1 Is an Independent Prognostic Marker in Pancreatic Cancer and Associated with Extracellular Matrix Remodeling. J. Transl. Med. 2020, 18, 77. [Google Scholar] [CrossRef]
- Wei, C.; Wang, Y.; Li, X. The Role of Hippo Signal Pathway in Breast Cancer Metastasis. OncoTargets Ther. 2018, 11, 2185. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, P.; Tapon, N. Sensing the Local Environment: Actin Architecture and Hippo Signalling. Curr. Opin. Cell Biol. 2014, 31, 74–83. [Google Scholar] [CrossRef]
- Lavado, A.; Park, J.Y.; Paré, J.; Finkelstein, D.; Pan, H.; Xu, B.; Fan, Y.; Kumar, R.P.; Neale, G.; Kwak, Y.D.; et al. The Hippo Pathway Prevents YAP/TAZ-Driven Hypertranscription and Controls Neural Progenitor Number. Dev. Cell 2018, 47, 576–591.e8. [Google Scholar] [CrossRef]
- Edwards, A.; Brennan, K. Notch Signalling in Breast Development and Cancer. Front. Cell Dev. Biol. 2021, 9, 692173. [Google Scholar] [CrossRef]
- Wang, X.; Bo, J.; Bridges, T.; Dugan, K.D.; Pan, T.C.; Chodosh, L.A.; Montell, D.J. Analysis of Cell Migration Using Whole-Genome Expression Profiling of Migratory Cells in the Drosophila Ovary. Dev. Cell 2006, 10, 483–495. [Google Scholar] [CrossRef]
- Hofseth, L.J.; Hussain, S.P.; Harris, C.C. P53: 25 Years after Its Discovery. Trends Pharmacol. Sci. 2004, 25, 177–181. [Google Scholar] [CrossRef]
- Mellman, I.; Yarden, Y. Endocytosis and Cancer. Cold Spring Harb. Perspect. Biol. 2013, 5, a016949. [Google Scholar] [CrossRef] [PubMed]
- Hoque, M.; Elmaghrabi, Y.A.; Köse, M.; Beevi, S.S.; Jose, J.; Meneses-Salas, E.; Blanco-Muñoz, P.; Conway, J.R.W.; Swarbrick, A.; Timpson, P.; et al. Annexin A6 Improves Anti-Migratory and Anti-Invasive Properties of Tyrosine Kinase Inhibitors in EGFR Overexpressing Human Squamous Epithelial Cells. FEBS J. 2020, 287, 2961–2978. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.Y.; Lin, C.F. Annexin A2: Its Molecular Regulation and Cellular Expression in Cancer Development. Dis. Markers 2014, 2014, 308976. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.M.; Nam, K.; Oh, S.; Lim, J.; Kim, R.K.; Shim, D.; Choi, J.H.; Lee, S.J.; Yu, J.H.; Lee, J.W.; et al. ECM1 Regulates Tumor Metastasis and CSC-like Property through Stabilization of β-Catenin. Oncogene 2015, 34, 6055–6065. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Königshoff, M.; Jayachandran, A.; Handley, D.; Seeger, W.; Kaminski, N.; Eickelberg, O. Transgelin Is a Direct Target of TGF-β/Smad3-dependent Epithelial Cell Migration in Lung Fibrosis. FASEB J. 2008, 22, 1778–1789. [Google Scholar] [CrossRef]
- Lin, Y.; Buckhaults, P.J.; Lee, J.R.; Xiong, H.; Farrell, C.; Podolsky, R.H.; Schade, R.R.; Dynan, W.S. Association of the Actin-Binding Protein Transgelin with Lymph Node Metastasis in Human Colorectal Cancer. Neoplasia 2009, 11, 864–873. [Google Scholar] [CrossRef] [PubMed]
- Gimona, M.; Kaverina, I.; Resch, G.P.; Vignal, E.; Burgstaller, G. Calponin Repeats Regulate Actin Filament Stability and Formation of Podosomes in Smooth Muscle Cells. Mol. Biol. Cell 2003, 14, 2482–2491. [Google Scholar] [CrossRef]
- Lee, K.C.; Kuo, H.C.; Shen, C.H.; Lu, C.C.; Huang, W.S.; Hsieh, M.C.; Huang, C.Y.; Kuo, Y.H.; Hsieh, Y.Y.; Teng, C.C.; et al. A Proteomics Approach to Identifying Novel Protein Targets Involved in Erinacine A–Mediated Inhibition of Colorectal Cancer Cells’ Aggressiveness. J. Cell. Mol. Med. 2017, 21, 588–599. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, S.; Zhang, Y.; Yang, J. Myosin Heavy Chain 9: Oncogene or Tumor Suppressor Gene? Med. Sci. Monit. 2019, 25, 888–892. [Google Scholar] [CrossRef]
- Mousavi, S.; Safaralizadeh, R.; Hosseinpour-Feizi, M.; Azimzadeh-Isfanjani, A.; Hashemzadeh, S. Study of Cofilin 1 Gene Expression in Colorectal Cancer. J. Gastrointest. Oncol. 2018, 9, 791–796. [Google Scholar] [CrossRef]
- Song, Y.; Ma, X.; Zhang, M.; Wang, M.; Wang, G.; Ye, Y.; Xia, W. Ezrin Mediates Invasion and Metastasis in Tumorigenesis: A Review. Front. Cell Dev. Biol. 2020, 8, 588801. [Google Scholar] [CrossRef] [PubMed]
- Tentler, D.; Lomert, E.; Novitskaya, K.; Barlev, N.A. Role of ACTN4 in Tumorigenesis, Metastasis, and EMT. Cells 2019, 8, 1427. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Luo, X.; Lin, J.; Fu, S.; Feng, P.; Su, H.; He, X.; Liang, X.; Liu, K.; Deng, W. Gelsolin Promotes Cancer Progression by Regulating Epithelial-Mesenchymal Transition in Hepatocellular Carcinoma and Correlates with a Poor Prognosis. J. Oncol. 2020, 2020, 1980368. [Google Scholar] [CrossRef]
- Barnawi, R.; Al-Khaldi, S.; Bakheet, T.; Fallatah, M.; Alaiya, A.; Ghebeh, H.; Al-Alwan, M. Fascin Activates β-Catenin Signaling and Promotes Breast Cancer Stem Cell Function Mainly Through Focal Adhesion Kinase (FAK): Relation With Disease Progression. Front. Oncol. 2020, 10, 440. [Google Scholar] [CrossRef] [PubMed]
- Beghein, E.; Devriese, D.; Van Hoey, E.; Gettemans, J. Cortactin and Fascin-1 Regulate Extracellular Vesicle Release by Controlling Endosomal Trafficking or Invadopodia Formation and Function. Sci. Rep. 2018, 8, 15606. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Ning, G.; Xu, R.; Cao, Y.; Meng, A.; Wang, Q. Fscn1 Is Required for the Trafficking of TGF-β Family Type i Receptors during Endoderm Formation. Nat. Commun. 2016, 7, 12603. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, Y.; Li, L.; Cao, J.; Guo, Y.; Wu, Y.; Gao, W. Fascin Actin-Bundling Protein 1 in Human Cancer: Promising Biomarker or Therapeutic Target? Mol. Ther.—Oncolytics 2021, 20, 240–264. [Google Scholar] [CrossRef] [PubMed]
- Frame, M.C.; Patel, H.; Serrels, B.; Lietha, D.; Eck, M.J. The FERM Domain: Organizing the Structure and Function of FAK. Nat. Rev. Mol. Cell Biol. 2010, 11, 802–814. [Google Scholar] [CrossRef]
- Wu, J.C.; Chen, Y.C.; Kuo, C.T.; Yu, H.W.; Chen, Y.Q.; Chiou, A.; Kuo, J.C. Focal Adhesion Kinase-Dependent Focal Adhesion Recruitment of SH2 Domains Directs SRC into Focal Adhesions to Regulate Cell Adhesion and Migration. Sci. Rep. 2015, 5, 18476. [Google Scholar] [CrossRef] [PubMed]
- Schlaepfer, D.D.; Hanks, S.K.; Hunter, T.; Geer, P. Van Der Integrin-Mediated Signal Transduction Linked to Ras Pathway by GRB2 Binding to Focal Adhesion Kinase. Nature 1994, 372, 786–791. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.T.S. Nuclear FAK: A New Mode of Gene Regulation from Cellular Adhesions. Mol. Cells 2013, 36, 1–6. [Google Scholar] [CrossRef]
- Mizuno, K. Signaling Mechanisms and Functional Roles of Cofilin Phosphorylation and Dephosphorylation. Cell. Signal. 2013, 25, 457–469. [Google Scholar] [CrossRef]
- Garrido-Casado, M.; Asensio-Juárez, G.; Vicente-Manzanares, M. Nonmuscle Myosin II Regulation Directs Its Multiple Roles in Cell Migration and Division. Annu. Rev. Cell Dev. Biol. 2021, 37, 285–310. [Google Scholar] [CrossRef]
- Schaller, M.D.; Hildebrand, J.D.; Shannon, J.D.; Fox, J.W.; Vines, R.R.; Parsons, J.T. Autophosphorylation of the Focal Adhesion Kinase, Pp125FAK, Directs SH2-Dependent Binding of Pp60src. Mol. Cell. Biol. 1994, 14, 1680–1688. [Google Scholar] [CrossRef]
- Polte, T.R.; Hanks, S.K. Interaction between Focal Adhesion Kinase and Crk-Associated Tyrosine Kinase Substrate P130Cas. Proc. Natl. Acad. Sci. USA 1995, 92, 10678–10682. [Google Scholar] [CrossRef]
- Chen, H.C.; Appeddu, P.A.; Isoda, H.; Guan, J.L. Phosphorylation of Tyrosine 397 in Focal Adhesion Kinase Is Required for Binding Phosphatidylinositol 3-Kinase. J. Biol. Chem. 1996, 271, 26329–26334. [Google Scholar] [CrossRef]
- Calalb, M.B.; Polte, T.R.; Hanks, S.K. Tyrosine Phosphorylation of Focal Adhesion Kinase at Sites in the Catalytic Domain Regulates Kinase Activity: A Role for Src Family Kinases. Mol. Cell. Biol. 1995, 15, 954–963. [Google Scholar] [CrossRef] [PubMed]
- Calalb, M.B.; Zhang, X.; Polte, T.R.; Hanks, S.K. Focal Ahdhesion Kinase Tyrosine-861 Is a Major Site of Phosphorylation by Src. Biochem. Biophys. Res. Commun. 1996, 228, 662–668. [Google Scholar] [CrossRef]
- Thomas, J.W.; Ellis, B.; Boerner, R.J.; Knight, W.B.; White, G.C.; Schaller, M.D. SH2- and SH3-Mediated Interactions between Focal Adhesion Kinase and Src. J. Biol. Chem. 1998, 273, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, K.; Iida, K.; Yahara, I. Phosphorylation of Ser-3 of Cofilin Regulates Its Essential Function on Actin. Genes Cells 1996, 1, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Bamburg, J.R. Proteins of the ADF/Cofilin Family: Essential Regulators of Actin Dynamics. Annu. Rev. Cell Dev. Biol. 1999, 15, 185–230. [Google Scholar] [CrossRef]
- Wendt, T.; Taylor, D.; Trybus, K.M.; Taylor, K. Three-Dimensional Image Reconstruction of Dephosphorylated Smooth Muscle Heavy Meromyosin Reveals Asymmetry in the Interaction between Myosin Heads and Placement of Subfragment 2. Proc. Natl. Acad. Sci. USA 2001, 98, 4361–4366. [Google Scholar] [CrossRef]
- Dulyaninova, N.G.; House, R.P.; Betapudi, V.; Bresnick, A.R. Myosin-IIA Heavy-Chain Phosphorylation Regulates the Motility of MDA-MB-231 Carcinoma Cells. Mol. Biol. Cell 2007, 18, 3144–3155. [Google Scholar] [CrossRef]
- Beausoleil, S.A.; Villén, J.; Gerber, S.A.; Rush, J.; Gygi, S.P. A Probability-Based Approach for High-Throughput Protein Phosphorylation Analysis and Site Localization. Nat. Biotechnol. 2006, 24, 1285–1292. [Google Scholar] [CrossRef]


| Intracellular Process/Compartment | Invasion | Endocytosis | Reference |
|---|---|---|---|
| Actin polymerization | Actin polymerization occurs in cells at the leading edge of the invadosome during invasion | Actin polymerization promotes the movement of the nascent endocytic vesicles into the cytoplasmic milieu, forming a comet tail | [82,83] |
| Myosin | Myosin phosphorylation by Cdc42-MRCK and Rho-ROCK signaling coordinates cell invasion | Myosin coordinates actin assembly and cargo trafficking during clathrin-mediated endocytosis | [84,85] |
| Formation of stress fibers | RhoA and RhoC are major GTpases capable of mediating stress fiber formation and generating the contractile force needed for retraction of the trailing edge during migration and invasion | The endocytotic protein Caveolin-1 regulates tension from stress fibers via RhoA signaling | [86,87] |
| EMT | Loss of E-cadherin is leading to acquisition of migration characteristics through loss of adhesive junctions | E-cadherin internalization is mediated by clathrin-mediated endocytosis, caveolin-mediated endocytosis, and macropinocytosis | [88,89] |
| Integrin trafficking | It promotes invasion, Rab 25 gene delivers α5b1, an integrin influences invasion to pseudopod tips at the plasma membrane | Integrins trafficking is driven by Rab which mediates clathrin-dependent and -independent endocytosis. | [90,91,92,93,94] |
| Integrin recycling | Integrin recycling is coordinated by Rab-coupling protein pathway and RTK, this drives invasion into fibronectin-rich 3D ECM. | The integrin is recycled through Rab11- and/or Arf6-dependent mechanisms in the endosomal system. | [95,96] |
| Cell adhesion | Many adhesion and signaling molecules are involved in cell migration and tumor invasion, including integrins, CD44, and several (IgCAMs). | CD44 mediates the endocytosis | [97,98,99,100] |
| Catenin signaling | The Wnt/β-catenin signaling pathway is a receptor-dependent mechanism coordinated by the Fzd receptor to facilitate cell invasion. | Β-catenin-dependent Wnt ligands require endocytosis for signal activation and to regulate gene transcription in the responding cells | [101,102] |
| Microtubule network | Microtubules help to form and maintain membrane protrusions by their ability to withstand high compressive loads and generate pushing forces employed by migrating cells. | Microtubules can transport recycling endosomes containing membrane-associated signaling molecules which are required for cell migration. | [103,104] |
| Signalling Pathway | Function during Cell Invasion and/or Migration | Potential Clinically Relevant Biomarker | Reference |
|---|---|---|---|
| EGF | Promotes epithelial-mesenchymal transition (EMT) through the B-catenin stabilization | ECM1 | [125,126] |
| Ras | Participates in membrane and cytoskeletal remodeling during endocytic transport | Annexin A6 | [127] |
| FAK/PI3K | Participates in the phenotype changes in focal adhesion and cytoskeletal dynamics and alteration in the activation of MMPs | Galectin-1, ITGA5 | [128,129] |
| ERK | Dissembles adhesion process to facilitate lamellipodium protrusion | GIT1 | [130,131] |
| WAVE | Helps actin polymerization for the formation of lamellipodia and amoeboid movement | WAVE2 | [132,133] |
| Wnt/β-catenin | Allows cytoskeleton reorganization by the activation of small GTpases Rho or Rac, triggering ROCK downstream | Mucin 1 | [102,134,135] |
| FAK | Participates in cell migration, activation of Rho-GTpases, integrin signalling | Rho GTPase, MMPs, CXCR1 | [136,137,138] |
| Hippo | Promotes the downregulation of EMT machinery (E-cadherin and Laminin), cell proliferation and apoptosis, tumorigenesis | Yap-1, YAP-TAZ | [139,140,141,142] |
| Notch | Induces EMT via the activation of transcriptional repressor proteins leading to E-cadherin downregulation | Notch 3 | [143,144] |
| P53 | Regulates DNA repair, control of the cell cycle, apoptosis, and differentiation | p53 protein | [145,146] |
| Marker | Cancer Type | Involvement | Reference |
|---|---|---|---|
| Annexin A6 and A2 | Melanoma, cervical cancer, epithelial carcinoma, breast cancer, gastric cancer, prostate cancer, acute lymphoblastic leukemia, chronic myeloid leukemia, large-cell lymphoma myeloma | Formation of reversible, membrane-cytoskeleton complexes through interactions with actin and α-actinin | [147,148] |
| ECM1 | Epithelial tumors, invasive breast cancer | Regulates cell proliferation, enhances MUC1 expression and stabilizes EGFR/HER3 proteins via a galectin-3/MUC1-dependent mechanism stabilization of β-catenin | [125,149] |
| Transgelin | Colorectal cancer | Stabilization of actin filaments promotes actin gelling is involved in podosome formation in smooth muscle cells, thus predisposing the cells toward migration and invasion. It is associated with Ca2+-independent vascular contractility and is also a direct target of transforming growth factor β (TGF-β)/Smad3-dependent epithelial cell migration in idiopathic pulmonary fibrosis | [150,151,152] |
| PROF1 | Human colon cancer | Actin-monomer binding protein regulates actin dynamics and cell motility and plays an important role in the migration of cancer cells | [153] |
| Myosin 9 | Lung cancer, breast cancer, leukemia, gastric cancer, esophageal cancer, and other malignant tumors | A cytokine, involved in cytoskeletal reorganization; plays an important role in the formation of cellular pseudopodia | [154] |
| Cofilin-1 | Colorectal cancer | Actin-depolymerizing protein increases in relation to cell cycle progression, migration, intravasation and the invasion | [155] |
| Ezrin | Osteosarcoma, pancreatic cancer, lung cancer, and others | Actin filament binding proteinfacilitates numerous signal transductions in tumorigenesis and mediates diverse essential functions through interactions with a variety of growth factor receptors and adhesion molecules | [156] |
| ACTN4 | Carcinoma tongue cancer, pancreatic cancer, lung cancers | Highly concentrated in actin-rich protrusions and invadopodias at the peripheries of cell clusters, induces cancer invasion | [157] |
| Gelsolin | Hepatocellular carcinoma | A cytoskeletal protein, frequently overexpressed in different cancers and promotes cell motility | [158] |
| Fascin | Breast cancer | A promoter of directed cell migration supporting the development of membrane protrusions | [159,160,161,162] |
| Protein | Phosphorylation Site | Function | Reference |
|---|---|---|---|
| FAK | Y397, | Autophosphorylation; binding site for Src family kinase (SFKs), p85 | [165,169,170,171] |
| Y576, Y577 | Regulate the catalytic activity | [172] | |
| Y861, Y925 | Serve as a docking site for SH2 domain-containing proteins | [165,173,174] | |
| Cofilin | Ser3 | Inhibit its binding to G-actin and F-actin, inactivate itself | [175,176] |
| MyosinⅡ | Ser19, Thr18 | Increase the Mg2+-ATPase activity of myosin | [168,177] |
| Ser1943 | Regulates the motility of breast cancer cells | [178] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leonov, S.; Inyang, O.; Achkasov, K.; Bogdan, E.; Kontareva, E.; Chen, Y.; Fu, Y.; Osipov, A.N.; Pustovalova, M.; Merkher, Y. Proteomic Markers for Mechanobiological Properties of Metastatic Cancer Cells. Int. J. Mol. Sci. 2023, 24, 4773. https://doi.org/10.3390/ijms24054773
Leonov S, Inyang O, Achkasov K, Bogdan E, Kontareva E, Chen Y, Fu Y, Osipov AN, Pustovalova M, Merkher Y. Proteomic Markers for Mechanobiological Properties of Metastatic Cancer Cells. International Journal of Molecular Sciences. 2023; 24(5):4773. https://doi.org/10.3390/ijms24054773
Chicago/Turabian StyleLeonov, Sergey, Olumide Inyang, Konstantin Achkasov, Elizaveta Bogdan, Elizaveta Kontareva, Yongheng Chen, Ying Fu, Andreyan N. Osipov, Margarita Pustovalova, and Yulia Merkher. 2023. "Proteomic Markers for Mechanobiological Properties of Metastatic Cancer Cells" International Journal of Molecular Sciences 24, no. 5: 4773. https://doi.org/10.3390/ijms24054773
APA StyleLeonov, S., Inyang, O., Achkasov, K., Bogdan, E., Kontareva, E., Chen, Y., Fu, Y., Osipov, A. N., Pustovalova, M., & Merkher, Y. (2023). Proteomic Markers for Mechanobiological Properties of Metastatic Cancer Cells. International Journal of Molecular Sciences, 24(5), 4773. https://doi.org/10.3390/ijms24054773









