Biomarkers of Migraine: An Integrated Evaluation of Preclinical and Clinical Findings
Abstract
1. Introduction
Migraine Pathogenesis
2. Methods
3. The Potential Circulating Biomarkers Described in Migraine Patients and Migraine Animal Models
3.1. Neuropeptides
3.1.1. Calcitonin Gene-Related Peptide (CGRP)
3.1.2. Other Peptides of the CGRP Family
3.1.3. Substance P (SP)
3.1.4. Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP)
3.1.5. Vasoactive Intestinal Polypeptide (VIP)
3.1.6. Neuropeptide Y (NPY)
3.2. Classic Neurotransmitters
3.3. Mediators of Inflammation and Immunity
3.3.1. Cytokines
3.3.2. Adipocytokines
3.3.3. Prostaglandins
3.3.4. Pentraxin-3 (PTX-3)
3.3.5. IgG
3.3.6. Matrix Metalloproteinase-9 (MMP-9)
3.4. Endocannabinoids and Related Lipids
3.5. MicroRNAs
3.6. Mediators of Endothelial/Vascular Functions
3.6.1. Endothelial Progenitor Cells (EPCs)
3.6.2. Endothelin-1 (ET-1)
3.6.3. Homocysteine
3.7. Other Biomarkers
3.7.1. Tryptophan and Kynurenine
3.7.2. Melatonin
3.7.3. Growth Factors
3.7.4. Mediators of Oxidative Stress
3.7.5. Apolipoprotein E
4. Fitting Together the Pieces of a Complex Picture
5. Considerations and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef] [PubMed]
- Olesen, J. International Classification of Headache Disorders. Lancet Neurol. 2018, 17, 396–397. [Google Scholar] [CrossRef]
- Katsarava, Z.; Buse, D.C.; Manack, A.N.; Lipton, R.B. Defining the Differences Between Episodic Migraine and Chronic Migraine. Curr. Pain Headache Rep. 2012, 16, 86–92. [Google Scholar] [CrossRef]
- May, A.; Schulte, L.H. Chronic migraine: Risk factors, mechanisms and treatment. Nat. Rev. Neurol. 2016, 12, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.-P.; May, A. Redefining migraine phases—A suggestion based on clinical, physiological, and functional imaging evidence. Cephalalgia 2020, 40, 866–870. [Google Scholar] [CrossRef] [PubMed]
- Moskowitz, M.A. Neurogenic inflammation in the pathophysiology and treatment of migraine. Neurology 1993, 43, 16–20. [Google Scholar]
- Goadsby, P.; Holland, P.; Martins-Oliveira, M.; Hoffmann, J.; Schankin, C.; Akerman, S. Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiol. Rev. 2017, 97, 553–622. [Google Scholar] [CrossRef]
- Ashina, M.; Hansen, J.M.; Do, T.P.; Melo-Carrillo, A.; Burstein, R.; Moskowitz, M.A. Migraine and the trigeminovascular system—40 years and counting. Lancet Neurol. 2019, 18, 795–804. [Google Scholar] [CrossRef]
- Silberstein, S.D. Migraine. Lancet 2004, 363, 381–391. [Google Scholar] [CrossRef]
- Ashina, M.; Hansen, J.M.; Dunga, B.O.; Olesen, J. Human models of migraine—Short-term pain for long-term gain. Nat. Rev. Neurol. 2017, 13, 713–724. [Google Scholar] [CrossRef]
- Demartini, C.; Greco, R.; Zanaboni, A.M.; Sances, G.; De Icco, R.; Borsook, D.; Tassorelli, C. Nitroglycerin as a comparative experimental model of migraine pain: From animal to human and back. Prog. Neurobiol. 2019, 177, 15–32. [Google Scholar] [CrossRef] [PubMed]
- Greco, R.; DeMartini, C.; De Icco, R.; Martinelli, D.; Putortì, A.; Tassorelli, C. Migraine neuroscience: From experimental models to target therapy. Neurol. Sci. 2020, 41, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Harriott, A.; Strother, L.C.; Vila-Pueyo, M.; Holland, P.R. Animal models of migraine and experimental techniques used to examine trigeminal sensory processing. J. Headache Pain 2019, 20, 91. [Google Scholar] [CrossRef] [PubMed]
- Tardiolo, G.; Bramanti, P.; Mazzon, E. Migraine: Experimental Models and Novel Therapeutic Approaches. Int. J. Mol. Sci. 2019, 20, 2932. [Google Scholar] [CrossRef]
- Ayata, C. Cortical Spreading Depression Triggers Migraine Attack: Pro. Headache 2010, 50, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Nahas, S.J.; Yan, B.M.; Depoy, E.G.; Ahmad, A. Biomarkers in Migraine. Neurol. India 2021, 69, 17–24. [Google Scholar] [CrossRef]
- Ashina, M.; Terwindt, G.M.; Al-Karagholi, M.A.-M.; de Boer, I.; Lee, M.J.; Hay, D.L.; Schulte, L.H.; Hadjikhani, N.; Sinclair, A.J.; Ashina, H.; et al. Migraine: Disease characterisation, biomarkers, and precision medicine. Lancet 2021, 397, 1496–1504. [Google Scholar] [CrossRef]
- Durham, P.; Papapetropoulos, S. Biomarkers Associated With Migraine and Their Potential Role in Migraine Management. Headache 2013, 53, 1262–1277. [Google Scholar] [CrossRef]
- Ferroni, P.; Barbanti, P.; Spila, A.; Fratangeli, F.; Aurilia, C.; Fofi, L.; Egeo, G.; Guadagni, F. Circulating Biomarkers in Migraine: New Opportunities for Precision Medicine. Curr. Med. Chem. 2019, 26, 6191–6206. [Google Scholar] [CrossRef]
- Frederiksen, S.D.; Msc, M.B.D.; Snoer, A.H.; Deen, M.; Edvinsson, L. Serotonin and Neuropeptides in Blood From Episodic and Chronic Migraine and Cluster Headache Patients in Case-Control and Case-Crossover Settings: A Systematic Review and Meta-Analysis. Headache 2020, 60, 1132–1164. [Google Scholar] [CrossRef]
- Ferreira, K.S.; Dhillon, H.; Velly, A.M. The role of a potential biomarker in patients with migraine: Review and new insights. Expert Rev. Neurother. 2021, 21, 817–831. [Google Scholar] [CrossRef]
- Ramadan, N.M. Glutamate and migraine: From Ikeda to the 21st century. Cephalalgia 2013, 34, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Tajti, J.; Szok, D.; Majláth, Z.; Tuka, B.; Csáti, A.; Vécsei, L. Migraine and neuropeptides. Neuropeptides 2015, 52, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Ramadan, N.M. The link between glutamate and migraine. CNS Spectrums 2003, 8, 446–449. [Google Scholar] [CrossRef]
- Russell, F.A.; King, R.; Smillie, S.-J.; Kodji, X.; Brain, S.D.; Pressly, J.D.; Soni, H.; Jiang, S.; Wei, J.; Liu, R.; et al. Calcitonin Gene-Related Peptide: Physiology and Pathophysiology. Physiol. Rev. 2014, 94, 1099–1142. [Google Scholar] [CrossRef] [PubMed]
- Durham, P.L. Calcitonin Gene-Related Peptide (CGRP) and Migraine. Headache 2006, 46 (Suppl. S1), S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Messlinger, K.; Lennerz, J.K.; Eberhardt, M.; Fischer, M.J. CGRP and NO in the Trigeminal System: Mechanisms and Role in Headache Generation. Headache 2012, 52, 1411–1427. [Google Scholar] [CrossRef]
- Ashina, M.; Bendtsen, L.; Jensen, R.; Schifter, S.; Olesen, J. Evidence for increased plasma levels of calcitonin gene-related peptide in migraine outside of attacks. Pain 2000, 86, 133–138. [Google Scholar] [CrossRef]
- Sarchielli, P.; Alberti, A.; Floridi, A.; Gallai, V. Levels of nerve growth factor in cerebrospinal fluid of chronic daily headache patients. Neurology 2001, 57, 132–134. [Google Scholar] [CrossRef]
- Gallai, V.; Alberti, A.; Gallai, B.; Coppola, F.; Floridi, A.; Sarchielli, P. Glutamate and Nitric Oxide Pathway in Chronic Daily Headache: Evidence From Cerebrospinal Fluid. Cephalalgia 2003, 23, 166–174. [Google Scholar] [CrossRef]
- Bellamy, J.L.; Cady, R.K.; Durham, P.L. Salivary Levels of CGRP and VIP in Rhinosinusitis and Migraine Patients. Headache 2006, 46, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Fusayasu, E.; Kowa, H.; Takeshima, T.; Nakaso, K.; Nakashima, K. Increased plasma substance P and CGRP levels, and high ACE activity in migraineurs during headache-free periods. Pain 2007, 128, 209–214. [Google Scholar] [CrossRef]
- Jang, M.-U.; Park, J.-W.; Kho, H.-S.; Chung, S.-C.; Chung, J.-W. Plasma and saliva levels of nerve growth factor and neuropeptides in chronic migraine patients. Oral Dis. 2011, 17, 187–193. [Google Scholar] [CrossRef]
- Rodríguez-Osorio, X.; Sobrino, T.; Brea, D.; Martínez, F.; Castillo, J.; Leira, R. Endothelial progenitor cells: A new key for endothelial dysfunction in migraine. Neurology 2012, 79, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Cernuda-Morollón, E.; Larrosa, D.; Ramón, C.; Vega, J.; Martinez-Camblor, P.; Pascual, J. Interictal increase of CGRP levels in peripheral blood as a biomarker for chronic migraine. Neurology 2013, 81, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Cernuda-Morollón, E.; Martínez-Camblor, P.; Ramón, C.; Larrosa, D.; Serrano-Pertierra, E.; Pascual, J. CGRP and VIP Levels as Predictors of Efficacy of Onabotulinumtoxin Type A in Chronic Migraine. Headache 2014, 54, 987–995. [Google Scholar] [CrossRef]
- Fekrazad, R.; Sardarian, A.; Azma, K.; Karami, M.; Borhani-Haghighi, A.; Gharesi-Fard, B.; Movahedi, B. Interictal levels of calcitonin gene related peptide in gingival crevicular fluid of chronic migraine patients. Neurol. Sci. 2018, 39, 1217–1223. [Google Scholar] [CrossRef]
- Domínguez, C.; López, A.; Ramos-Cabrer, P.; Vieites-Prado, A.; Pérez-Mato, M.; Villalba, C.; Sobrino, T.; Rodriguez-Osorio, X.; Campos, F.; Castillo, J.; et al. Iron deposition in periaqueductal gray matter as a potential biomarker for chronic migraine. Neurology 2019, 92, e1076–e1085. [Google Scholar] [CrossRef]
- Leira, Y.; Ameijeira, P.; Domínguez, C.; López-Arias, E.; Ávila-Gómez, P.; Pérez-Mato, M.; Sobrino, T.; Campos, F.; D’Aiuto, F.; Leira, R.; et al. Periodontal inflammation is related to increased serum calcitonin gene-related peptide levels in patients with chronic migraine. J. Periodontol. 2019, 90, 1088–1095. [Google Scholar] [CrossRef]
- Alpuente, A.; Gallardo, V.J.; Asskour, L.; Caronna, E.; Torres-Ferrus, M.; Pozo-Rosich, P. Salivary CGRP can monitor the different migraine phases: CGRP (in)dependent attacks. Cephalalgia 2022, 42, 186–196. [Google Scholar] [CrossRef]
- Vural, S.; Albayrak, L. Can calcitonin gene-related peptide (CGRP) and pentraxin-3 (PTX-3) be useful in diagnosing acute migraine attack? J. Recept. Signal Transduct. 2022, 42, 562–566. [Google Scholar] [CrossRef]
- Pérez-Pereda, S.; Toriello-Suárez, M.; Ocejo-Vinyals, G.; Guiral-Foz, S.; Castillo-Obeso, J.; Montes-Gómez, S.; Martínez-Nieto, R.M.; Iglesias, F.; González-Quintanilla, V.; Oterino, A. Serum CGRP, VIP, and PACAP usefulness in migraine: A case–control study in chronic migraine patients in real clinical practice. Mol. Biol. Rep. 2020, 47, 7125–7138. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.J.; Lee, S.-Y.; Cho, S.; Kang, E.-S.; Chung, C.-S. Feasibility of serum CGRP measurement as a biomarker of chronic migraine: A critical reappraisal. J. Headache Pain 2018, 19, 53. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Vollesen, A.L.H.; Hansen, Y.B.; Frandsen, E.; Andersen, M.R.; Amin, F.M.; Fahrenkrug, J.; Olesen, J.; Ashina, M. Part II: Biochemical changes after pituitary adenylate cyclase-activating polypeptide-38 infusion in migraine patients. Cephalalgia 2017, 37, 136–147. [Google Scholar] [CrossRef]
- Latif, R.; Rafique, N.; Al Asoom, L.; Alsunni, A.A.; Salem, A.M.; AlNoaimi, D.A.; AlHarbi, W.M.; Shaikh, A.Y.; AlRaddadi, S.A.; AlMuhaish, L.A.; et al. Diagnostic Accuracy of Serum Calcitonin Gene-Related Peptide and Apolipoprotein E in Migraine: A Preliminary Study. Int. J. Gen. Med. 2021, 14, 851–856. [Google Scholar] [CrossRef]
- Pellesi, L.; Al-Karagholi, M.A.-M.; De Icco, R.; Chaudhry, B.A.; Lopez, C.L.; Snellman, J.; Hannibal, J.; Amin, F.M.; Ashina, M. Plasma Levels of CGRP During a 2-h Infusion of VIP in Healthy Volunteers and Patients With Migraine: An Exploratory Study. Front. Neurol. 2022, 13, 871176. [Google Scholar] [CrossRef]
- Han, D. Association of serum levels of calcitonin gene-related peptide and cytokines during migraine attacks. Ann. Indian Acad. Neurol. 2019, 22, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Sarchielli, P.; Alberti, A.; Codini, M.; Floridi, A.; Gallai, V. Nitric oxide metabolites, prostaglandins and trigeminal vasoactive peptides in internal jugular vein blood during spontaneous migraine attacks. Cephalalgia 2000, 20, 907–918. [Google Scholar] [CrossRef]
- Cady, R.K.; Vause, C.V.; Ho, T.; Bigal, M.E.; Durham, P.L. Elevated Saliva Calcitonin Gene-Related Peptide Levels During Acute Migraine Predict Therapeutic Response to Rizatriptan. Headache 2009, 49, 1258–1266. [Google Scholar] [CrossRef] [PubMed]
- Sarchielli, P.; Alberti, A.; Coppola, F.; Baldi, A.; Gallai, B.; Floridi, A.; Capocchi, G.; Gallai, V. Platelet-Activating Factor (PAF) in Internal Jugular Venous Blood of Migraine without aura Patients Assessed during Migraine Attacks. Cephalalgia 2004, 24, 623–630. [Google Scholar] [CrossRef]
- Tvedskov, J.F.; Lipka, K.; Ashina, M.; Iversen, H.K.; Schifter, S.; Olesen, J. No increase of calcitonin gene-related peptide in jugular blood during migraine. Ann. Neurol. 2005, 58, 561–568. [Google Scholar] [CrossRef]
- Cady, R.; Turner, I.; Dexter, K.; Beach, M.E.; Cady, R.; Durham, P. An Exploratory Study of Salivary Calcitonin Gene-Related Peptide Levels Relative to Acute Interventions and Preventative Treatment With OnabotulinumtoxinA in Chronic Migraine. Headache 2014, 54, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Hansen, J.M.; Ashina, M. Calcitonin gene-related peptide and migraine with aura: A systematic review. Cephalalgia 2014, 34, 695–707. [Google Scholar] [CrossRef]
- Juhasz, G.; Zsombok, T.; Modos, E.A.; Olajos, S.; Jakab, B.; Nemeth, J.; Szolcsanyi, J.; Vitrai, J.; Bagdy, G. NO-induced migraine attack: Strong increase in plasma calcitonin gene-related peptide (CGRP) concentration and negative correlation with platelet serotonin release. Pain 2003, 106, 461–470. [Google Scholar] [CrossRef]
- Greco, R.; Demartini, C.; Francavilla, M.; Zanaboni, A.M.; Tassorelli, C. Dual Inhibition of FAAH and MAGL Counteracts Migraine-like Pain and Behavior in an Animal Model of Migraine. Cells 2021, 10, 2543. [Google Scholar] [CrossRef]
- Greco, R.; Demartini, C.; Francavilla, M.; Zanaboni, A.M.; Tassorelli, C. Antagonism of CGRP Receptor: Central and Peripheral Mechanisms and Mediators in an Animal Model of Chronic Migraine. Cells 2022, 11, 3092. [Google Scholar] [CrossRef] [PubMed]
- Zagami, A.; Goadsby, P.; Edvinsson, L. Stimulation of the superior sagittal sinus in the cat causes release of vasoactive peptides. Neuropeptides 1990, 16, 69–75. [Google Scholar] [CrossRef]
- Buzzi, M.G.; Carter, W.B.; Shimizu, T.; Heath, H., 3rd; Moskowitz, M.A. Dihydroergotamine and sumatriptan attenuate levels of CGRP in plasma in rat superior sagittal sinus during electrical stimulation of the trigeminal ganglion. Neuropharmacology 1991, 30, 1193–1200. [Google Scholar] [CrossRef] [PubMed]
- Tsujikawa, K.; Yayama, K.; Hayashi, T.; Matsushita, H.; Yamaguchi, T.; Shigeno, T.; Ogitani, Y.; Hirayama, M.; Kato, T.; Fukada, S.-I.; et al. Hypertension and dysregulated proinflammatory cytokine production in receptor activity-modifying protein 1-deficient mice. Proc. Natl. Acad. Sci. USA 2007, 104, 16702–16707. [Google Scholar] [CrossRef]
- Hoffmann, J.; Neeb, L.; Israel, H.; Dannenberg, F.; Triebe, F.; Dirnagl, U.; Reuter, U. Intracisternal Injection of Inflammatory Soup Activates the Trigeminal Nerve System. Cephalalgia 2009, 29, 1212–1217. [Google Scholar] [CrossRef]
- Guo, Y.; Cheng, Y.; An, J.; Qi, Y.; Luo, G. Neuropeptide changes in an improved migraine model with repeat stimulations. Transl. Neurosci. 2021, 12, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Liu, L.; Zhao, L.; Li, B.; Jing, X.; Qu, Z.; Zhu, Y.; Zhang, Y.; Li, Z.; Fisher, M.; et al. Effect of Electroacupuncture on Hyperalgesia and Vasoactive Neurotransmitters in a Rat Model of Conscious Recurrent Migraine. Evid.-Based Complement. Altern. Med. 2019, 2019, 9512875. [Google Scholar] [CrossRef] [PubMed]
- Frank, F.; Kaltseis, K.; Messlinger, K.; Broessner, G. Short Report of Longitudinal CGRP-Measurements in Migraineurs During a Hypoxic Challenge. Front. Neurol. 2022, 13, 925748. [Google Scholar] [CrossRef] [PubMed]
- Juhasz, G.; Zsombok, T.; Jakab, B.; Nemeth, J.; Szolcsanyi, J.; Bagdy, G. Sumatriptan Causes Parallel Decrease in Plasma Calcitonin Gene-Related Peptide (CGRP) Concentration and Migraine Headache During Nitroglycerin Induced Migraine Attack. Cephalalgia 2005, 25, 179–183. [Google Scholar] [CrossRef]
- Cernuda-Morollón, E.; Ramón, C.; Martínez-Camblor, P.; Serrano-Pertierra, E.; Larrosa, D.; Pascual, J. OnabotulinumtoxinA decreases interictal CGRP plasma levels in patients with chronic migraine. Pain 2015, 156, 820–824. [Google Scholar] [CrossRef] [PubMed]
- Greco, R.; De Icco, R.; DeMartini, C.; Zanaboni, A.M.; Tumelero, E.; Sances, G.; Allena, M.; Tassorelli, C. Plasma levels of CGRP and expression of specific microRNAs in blood cells of episodic and chronic migraine subjects: Towards the identification of a panel of peripheral biomarkers of migraine? J. Headache Pain 2020, 21, 122. [Google Scholar] [CrossRef] [PubMed]
- Alpuente, A.; Gallardo, V.J.; Asskour, L.; Caronna, E.; Torres-Ferrus, M.; Pozo-Rosich, P. Salivary CGRP and erenumab treatment response: Towards precision medicine in migraine. Ann. Neurol. 2022, 92, 846–859. [Google Scholar] [CrossRef]
- Domínguez, C.; Vieites-Prado, A.; Pérez-Mato, M.; Sobrino, T.; Rodríguez-Osorio, X.; López, A.; Campos, F.; Martínez, F.; Castillo, J.; Leira, R. CGRP and PTX3 as Predictors of Efficacy of Onabotulinumtoxin Type A in Chronic Migraine: An Observational Study. Headache 2018, 58, 78–87. [Google Scholar] [CrossRef]
- Van Dongen, R.M.; Zielman, R.; Noga, M.; Dekkers, O.; Hankemeier, T.; van den Maagdenberg, A.M.; Terwindt, G.M.; Ferrari, M.D. Migraine biomarkers in cerebrospinal fluid: A systematic review and meta-analysis. Cephalalgia 2017, 37, 49–63. [Google Scholar] [CrossRef]
- Bottiroli, S.; De Icco, R.; Vaghi, G.; Pazzi, S.; Guaschino, E.; Allena, M.; Ghiotto, N.; Martinelli, D.; Tassorelli, C.; Sances, G. Psychological predictors of negative treatment outcome with Erenumab in chronic migraine: Data from an open label long-term prospective study. J. Headache Pain 2021, 22, 114. [Google Scholar] [CrossRef]
- Edvinsson, L.; Edvinsson, J.C.A.; Haanes, K.A. Biological and small molecule strategies in migraine therapy with relation to the calcitonin gene-related peptide family of peptides. Br. J. Pharmacol. 2022, 179, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Turan, H.; Horasanli, B.; Ugur, M.; Arslan, H. Procalcitonin Levels in Migraine Patients. Can. J. Neurol. Sci. 2011, 38, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, N.; Yılmaz, M.; Sirin, B.; Yılmaztekin, S.; Kutlu, G. The relationship between levels of plasma-soluble urokinase plasminogen activator receptor (suPAR) and presence of migraine attack and aura. J. Recept. Signal Transduct. 2017, 37, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Ghanizada, H.; Al-Karagholi, M.A.; Walker, C.S.; Arngrim, N.; Rees, T.; Petersen, J.; Siow, A.; Mørch-Rasmussen, M.; Tan, S.; O’Carroll, S.J.; et al. Amylin Analog Pramlintide Induces Migraine-like Attacks in Patients. Ann. Neurol. 2021, 89, 1157–1171. [Google Scholar] [CrossRef] [PubMed]
- Hay, D.L.; Chen, S.; Lutz, T.A.; Parkes, D.G.; Roth, J.D. Amylin: Pharmacology, Physiology, and Clinical Potential. Pharmacol. Rev. 2015, 67, 564–600. [Google Scholar] [CrossRef]
- Hendrikse, E.R.; Bower, R.L.; Hay, D.L.; Walker, C.S. Molecular studies of CGRP and the CGRP family of peptides in the central nervous system. Cephalalgia 2019, 39, 403–419. [Google Scholar] [CrossRef]
- Irimia, P.; Martínez-Valbuena, I.; Mínguez-Olaondo, A.; Domínguez-Vivero, C.; Sánchez-Arias, J.-A.; Martínez-Vila, E.; Luquin, M.-R.; Leira, R. Interictal amylin levels in chronic migraine patients: A case-control study. Cephalalgia 2021, 41, 604–612. [Google Scholar] [CrossRef]
- Edvinsson, L.; Goadsby, P.J.; Uddman, R. Amylin: Localization, Effects on Cerebral Arteries and on Local Cerebral Blood Flow in the Cat. Sci. World J. 2001, 1, 168–180. [Google Scholar] [CrossRef]
- Nicolodi, M.; Del Bianco, E.; Del, E.B. Sensory Neuropeptides (Substance P, Calcitonin Gene-Related Peptide) and Vasoactive Intestinal Polypeptide in Human Saliva: Their Pattern in Migraine and Cluster Headache. Cephalalgia 1990, 10, 39–50. [Google Scholar] [CrossRef]
- Edvinsson, L.; Goadsby, P.J. Neuropeptides in the Cerebral Circulation: Relevance to Headache. Cephalalgia 1995, 15, 272–276. [Google Scholar] [CrossRef]
- Goadsby, P.J.; Edvinsson, L.; Ekman, R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann. Neurol. 1990, 28, 183–187. [Google Scholar] [CrossRef]
- Goadsby, P.J.; Edvinsson, L.; Ekman, R. Release of vasoactive peptides in the extracerebral circulation of humans and the cat during activation of the trigeminovascular system. Ann. Neurol. 1988, 23, 193–196. [Google Scholar] [CrossRef]
- Diener, H.-C. Rpr100893, A Substance-P Antagonist, is Not Effective in the Treatment of Migraine Attacks. Cephalalgia 2003, 23, 183–185. [Google Scholar] [CrossRef] [PubMed]
- Edvinsson, L.; Tajti, J.; Szalárdy, L.; Vécsei, L. PACAP and its role in primary headaches. J. Headache Pain 2018, 19, 21. [Google Scholar] [CrossRef]
- Cernuda-Morollón, E.; Riesco, N.; Martínez-Camblor, P.; Serrano-Pertierra, E.; García-Cabo, C.; Pascual, J. No Change in Interictal PACAP Levels in Peripheral Blood in Women with Chronic Migraine. Headache 2016, 56, 1448–1454. [Google Scholar] [CrossRef]
- Togha, M.; Ghorbani, Z.; Ramazi, S.; Zavvari, F.; Karimzadeh, F. Evaluation of Serum Levels of Transient Receptor Potential Cation Channel Subfamily V Member 1, Vasoactive Intestinal Polypeptide, and Pituitary Adenylate Cyclase-Activating Polypeptide in Chronic and Episodic Migraine: The Possible Role in Migraine Transformation. Front. Neurol. 2021, 12, 770980. [Google Scholar] [CrossRef] [PubMed]
- Tuka, B.; Helyes, Z.; Markovics, A.; Bagoly, T.; Szolcsányi, J.; Szabó, N.; Tóth, E.; Kincses, Z.T.; Vécsei, L.; Tajti, J. Alterations in PACAP-38-like immunoreactivity in the plasma during ictal and interictal periods of migraine patients. Cephalalgia 2013, 33, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Dong, Z.; Hou, L.; Wan, D.; Chen, M.; Tang, W.; Yu, S. Interictal plasma pituitary adenylate cyclase-activating polypeptide levels are decreased in migraineurs but remain unchanged in patients with tension-type headache. Clin. Chim. Acta 2015, 450, 151–154. [Google Scholar] [CrossRef]
- Zagami, A.S.; Edvinsson, L.; Goadsby, P.J. Pituitary adenylate cyclase activating polypeptide and migraine. Ann. Clin. Transl. Neurol. 2014, 1, 1036–1040. [Google Scholar] [CrossRef]
- Tuka, B.; Helyes, Z.; Markovics, A.; Bagoly, T.; Németh, J.; Márk, L.; Brubel, R.; Reglődi, D.; Párdutz, A.; Szolcsányi, J.; et al. Peripheral and central alterations of pituitary adenylate cyclase activating polypeptide-like immunoreactivity in the rat in response to activation of the trigeminovascular system. Peptides 2012, 33, 307–316. [Google Scholar] [CrossRef]
- Schytz, H.W.; Birk, S.; Wienecke, T.; Kruuse, C.; Olesen, J.; Ashina, M. PACAP38 induces migraine-like attacks in patients with migraine without aura. Brain 2009, 132, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Edvinsson, J.C.A.; Grell, A.-S.; Warfvinge, K.; Sheykhzade, M.; Edvinsson, L.; Haanes, K.A. Differences in pituitary adenylate cyclase-activating peptide and calcitonin gene-related peptide release in the trigeminovascular system. Cephalalgia 2020, 40, 1296–1309. [Google Scholar] [CrossRef] [PubMed]
- Edvinsson, L.; Uddman, R. Neurobiology in primary headaches. Brain Res. Rev. 2005, 48, 438–456. [Google Scholar] [CrossRef] [PubMed]
- Sarchielli, P.; Pini, L.A.; Zanchin, G.; Alberti, A.; Maggioni, F.; Rossi, C.; Floridi, A.; Calabresi, P. Clinical-Biochemical Correlates of Migraine Attacks in Rizatriptan Responders and Non-Responders. Cephalalgia 2006, 26, 257–265. [Google Scholar] [CrossRef]
- Riesco, N.; Cernuda-Morollón, E.; Martínez-Camblor, P.; Pérez-Alvarez, A.; Verano, L.; García-Cabo, C.; Serrano-Pertierra, E.; Pascual, J. Relationship between serum levels of VIP, but not of CGRP, and cranial autonomic parasympathetic symptoms: A study in chronic migraine patients. Cephalalgia 2016, 37, 823–827. [Google Scholar] [CrossRef]
- Riesco, N.; Cernuda-Morollón, E.; Pascual, J. Neuropeptides as a Marker for Chronic Headache. Curr. Pain Headache Rep. 2017, 21, 1–8. [Google Scholar] [CrossRef]
- Pellesi, L.; Al-Karagholi, M.A.-M.; De Icco, R.; Coskun, H.; Elbahi, F.A.; Lopez-Lopez, C.; Snellman, J.; Hannibal, J.; Amin, F.M.; Ashina, M. Effect of Vasoactive Intestinal Polypeptide on Development of Migraine Headaches: A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2118543. [Google Scholar] [CrossRef] [PubMed]
- Boni, L.; Ploug, K.; Olesen, I.; Gupta, S. The in vivo Effect of VIP, PACAP-38 and PACAP-27 and mRNA Expression of Their Receptors in Rat Middle Meningeal Artery. Cephalalgia 2009, 29, 837–847. [Google Scholar] [CrossRef] [PubMed]
- Csati, A.; Tajti, J.; Kuris, A.; Tuka, B.; Edvinsson, L.; Warfvinge, K. Distribution of vasoactive intestinal peptide, pituitary adenylate cyclase-activating peptide, nitric oxide synthase, and their receptors in human and rat sphenopalatine ganglion. Neuroscience 2012, 202, 158–168. [Google Scholar] [CrossRef]
- Valenzuela, R.F.; Donoso, M.; Mellado, P.A.; Huidobro-Toro, J. Migraine, but not subarachnoid hemorrhage, is associated with differentially increased NPY-like immunoreactivity in the CSF. J. Neurol. Sci. 2000, 173, 140–146. [Google Scholar] [CrossRef]
- Vécsei, L.; Widerlöv, E.; Ekman, R.; Kovács, K.; Jelencsik, I.; Bozsik, G.; Kapócs, G. Suboccipital cerebrospinal fluid and plasma concentrations of somatostatin, neuropeptide Y and beta-endorphin in patients with common migraine. Neuropeptides 1992, 22, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Caproni, S.; Corbelli, I.; Pini, L.A.; Cupini, M.L.; Calabresi, P.; Sarchielli, P. Migraine preventive drug-induced weight gain may be mediated by effects on hypothalamic peptides: The results of a pilot study. Cephalalgia 2011, 31, 543–549. [Google Scholar] [CrossRef]
- D’Andrea, G.; Leon, A. Pathogenesis of migraine: From neurotransmitters to neuromodulators and beyond. Neurol. Sci. 2010, 31 (Suppl. S1), S1–S7. [Google Scholar] [CrossRef]
- D’Andrea, G.; Gucciardi, A.; Leon, A. Elusive amines: Migraine depends on biochemical abnormalities. Neurol. Sci. 2022, 43, 6299–6304. [Google Scholar] [CrossRef] [PubMed]
- Rothrock, J.F.; Mar, K.R.; Yaksh, T.L.; Golbeck, A.; Moore, A.C. Cerebrospinal Fluid Analyses in Migraine Patients and Controls. Cephalalgia 1995, 15, 489–493. [Google Scholar] [CrossRef]
- Rajda, C.; Tajti, J.; Komoróczy, R.; Seres, E.; Klivényi, P.; Vécsei, L. Amino acids in the saliva of patients with migraine. Headache 1999, 39, 644–649. [Google Scholar] [CrossRef]
- DaSilva, A.F.; Nascimento, T.D.; Jassar, H.; Heffernan, J.; Toback, R.L.; Lucas, S.; DosSantos, M.F.; Bellile, E.L.; Boonstra, P.S.; Taylor, J.M.; et al. Dopamine D2/D3 imbalance during migraine attack and allodynia in vivo. Neurology 2017, 88, 1634–1641. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Guo, L.; Qiu, F.; Gong, M. Anti-Migraine Effect of the Herbal Combination of Chuanxiong Rhizoma and Cyperi Rhizoma and UPLC-MS/MS Method for the Simultaneous Quantification of the Active Constituents in Rat Serum and Cerebral Cortex. Molecules 2019, 24, 2230. [Google Scholar] [CrossRef] [PubMed]
- Gross, E.C.; Lisicki, M.; Fischer, D.; Sándor, P.S.; Schoenen, J. The metabolic face of migraine—From pathophysiology to treatment. Nat. Rev. Neurol. 2019, 15, 627–643. [Google Scholar] [CrossRef]
- Tuka, B.; Nyári, A.; Cseh, E.K.; Körtési, T.; Veréb, D.; Tömösi, F.; Kecskeméti, G.; Janáky, T.; Tajti, J.; Vécsei, L. Clinical relevance of depressed kynurenine pathway in episodic migraine patients: Potential prognostic markers in the peripheral plasma during the interictal period. J. Headache Pain 2021, 22, 60. [Google Scholar] [CrossRef]
- Tassorelli, C.; Blandini, F.; Costa, A.; Preza, E.; Nappi, G. Nitroglycerin-Induced Activation of Monoaminergic Transmission in the Rat. Cephalalgia 2002, 22, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Edvinsson, L.; Villalón, C.M.; MaassenVanDenBrink, A. Basic mechanisms of migraine and its acute treatment. Pharmacol. Ther. 2012, 136, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Gasparini, C.F.; Griffiths, L.R. The Biology of the Glutamatergic System and Potential Role in Migraine. Int. J. BioMed. Sci. 2013, 9, 1–8. [Google Scholar]
- Ferrari, M.D.; Odink, J.; Bos, K.D.; Malessy, M.; Bruyn, G.W. Neuroexcitatory plasma amino acids are elevated in migraine. Neurology 1990, 40, 1582. [Google Scholar] [CrossRef]
- Cananzi, A.R.; D’Andrea, G.; Perini, F.; Zamberlan, F.; Welch, K. Platelet and Plasma Levels of Glutamate and Glutamine in Migraine with and without Aura. Cephalalgia 1995, 15, 132–135. [Google Scholar] [CrossRef]
- Vaccaro, M.; Riva, C.; Tremolizzo, L.; Longoni, M.; Aliprandi, A.; Agostoni, E.C.; Rigamonti, A.; Leone, M.; Bussone, G.; Ferrarese, C. Platelet Glutamate Uptake and Release in Migraine with and without Aura. Cephalalgia 2007, 27, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.; Spaccalopelo, L.; Pinetti, D.; Tacchi, R.; Bertolini, A. Effective Prophylactic Treatments of Migraine Lower Plasma Glutamate Levels. Cephalalgia 2009, 29, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Nam, J.H.; Lee, H.S.; Kim, J.; Kim, J.; Chu, M.K. Salivary glutamate is elevated in individuals with chronic migraine. Cephalalgia 2018, 38, 1485–1492. [Google Scholar] [CrossRef]
- Park, C.G.; Chu, M.K. Interictal plasma glutamate levels are elevated in individuals with episodic and chronic migraine. Sci. Rep. 2022, 12, 6921. [Google Scholar] [CrossRef] [PubMed]
- Martínez, F.; Castillo, J.; Rodríguez, J.R.; Leira, R.; Noya, M. Neuroexcitatory Amino Acid Levels in Plasma and Cerebrospinal Fluid during Migraine Attacks. Cephalalgia 1993, 13, 89–93. [Google Scholar] [CrossRef]
- Peres, M.; Zukerman, E.; Soares, C.S.; Alonso, E.; Santos, B.; Faulhaber, M. Cerebrospinal Fluid Glutamate Levels in Chronic Migraine. Cephalalgia 2004, 24, 735–739. [Google Scholar] [CrossRef]
- Gao, Z.; Liu, X.; Yu, S.; Zhang, Q.; Chen, Q.; Wu, Q.; Liu, J.; Sun, B.; Fang, L.; Lin, J.; et al. Electroacupuncture at Acupoints Reverses Plasma Glutamate, Lipid, and LDL/VLDL in an Acute Migraine Rat Model: A1H NMR-Based Metabolomic Study. Evid.-Based Complement. Altern. Med. 2014, 2014, 659268. [Google Scholar] [CrossRef] [PubMed]
- Ji, R.-R.; Nackley, A.; Huh, B.Y.; Terrando, N.; Maixner, D.W. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology 2018, 129, 343–366. [Google Scholar] [CrossRef] [PubMed]
- Torres-Ferrús, M.; Ursitti, F.; Alpuente, A.; Brunello, F.; Chiappino, D.; de Vries, T.; Di Marco, S.; Ferlisi, S.; Guerritore, L.; Gonzalez-Garcia, N.; et al. From transformation to chronification of migraine: Pathophysiological and clinical aspects. J. Headache Pain 2020, 21, 42. [Google Scholar] [CrossRef]
- Edvinsson, L.; Haanes, K.A.; Warfvinge, K. Does inflammation have a role in migraine? Nat. Rev. Neurol. 2019, 15, 483–490. [Google Scholar] [CrossRef]
- Cavestro, C.; Ferrero, M.; Mandrino, S.; Di Tavi, M.; Rota, E. Novelty in Inflammation and Immunomodulation in Migraine. Curr. Pharm. Des. 2019, 25, 2919–2936. [Google Scholar] [CrossRef] [PubMed]
- Conti, P.; D’Ovidio, C.; Conti, C.; Gallenga, C.E.; Lauritano, D.; Caraffa, A.; Kritas, S.K.; Ronconi, G. Progression in migraine: Role of mast cells and pro-inflammatory and anti-inflammatory cytokines. Eur. J. Pharmacol. 2019, 844, 87–94. [Google Scholar] [CrossRef]
- Balcziak, L.K.; Russo, A.F. Dural Immune Cells, CGRP, and Migraine. Front. Neurol. 2022, 13, 874193. [Google Scholar] [CrossRef]
- Biscetti, L.; De Vanna, G.; Cresta, E.; Bellotti, A.; Corbelli, I.; Cupini, M.L.; Calabresi, P.; Sarchielli, P. Immunological findings in patients with migraine and other primary headaches: A narrative review. Clin. Exp. Immunol. 2022, 207, 11–26. [Google Scholar] [CrossRef]
- Thuraiaiyah, J.; Erritzøe-Jervild, M.; Al-Khazali, H.M.; Schytz, H.W.; Younis, S. The role of cytokines in migraine: A systematic review. Cephalalgia 2022, 42, 1565–1588. [Google Scholar] [CrossRef]
- Geng, C.; Yang, Z.; Xu, P.; Zhang, H. Aberrations in peripheral inflammatory cytokine levels in migraine: A systematic review and meta-analysis. J. Clin. Neurosci. 2022, 98, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Güzel, I.; Taşdemir, N.; Çelik, Y. Evaluation of serum transforming growth factor β1 and C-reactive protein levels in migraine patients. Neurol. Neurochir. Polska 2013, 47, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Vanmolkot, F.H.; De Hoon, J.N. Increased C-Reactive Protein in Young Adult Patients with Migraine. Cephalalgia 2007, 27, 843–846. [Google Scholar] [CrossRef] [PubMed]
- Martami, F.; Jahromi, S.R.; Togha, M.; Ghorbani, Z.; Seifishahpar, M.; Saidpour, A. The serum level of inflammatory markers in chronic and episodic migraine: A case-control study. Neurol. Sci. 2018, 39, 1741–1749. [Google Scholar] [CrossRef]
- Gudmundsson, L.; Aspelund, T.; Scher, A.; Thorgeirsson, G.; Johannsson, M.; Launer, L.; Gudnason, V. C-Reactive Protein in Migraine Sufferers Similar to That of Non-Migraineurs: The Reykjavik Study. Cephalalgia 2009, 29, 1301–1310. [Google Scholar] [CrossRef]
- Lassen, L.; Ashina, M.; Christiansen, I.; Ulrich, V.; Olesen, J. Nitric oxide synthase inhibition in migraine. Lancet 1997, 349, 401–402. [Google Scholar] [CrossRef]
- Covelli, V.; Massari, F.; Fallacara, C.; Munno, I.; Pellegrino, N.M.; Jirillo, E.; Savastano, S.; Ghiggi, M.R.; Tommaselli, A.P.; Lombardi, G. Increased Spontaneous Release of Tumor Necrosis Factor-α/Cachectin in Headache Patients. A Possible Correlation with Plasma Endotoxin and Hypothalamic-Pituitary-Adrenal Axis. Int. J. Neurosci. 1991, 61, 53–60. [Google Scholar] [CrossRef]
- Aydın, M.; Demir, C.F.; Arıkanoğlu, A.; Bulut, S.; İlhan, N. Plasma Cytokine Levels in Migraineurs during and Outside of Attacks. Electron. J. Gen. Med. 2015, 12, 307–312. [Google Scholar] [CrossRef]
- Yücel, M.; Kotan, D.; Çiftçi, G.G.; Çiftçi, I.H.; I Cikriklar, H. Serum levels of endocan, claudin-5 and cytokines in migraine. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 930–936. [Google Scholar]
- Ishizaki, K.; Takeshima, T.; Fukuhara, Y.; Araki, H.; Nakaso, K.; Kusumi, M.; Nakashima, K. Increased Plasma Transforming Growth Factor-beta1 in Migraine. Headache 2005, 45, 1224–1228. [Google Scholar] [CrossRef]
- Perini, F.; D’Andrea, G.; Galloni, E.; Pignatelli, F.; Billo, G.; Alba, S.; Bussone, G.; Toso, V. Plasma Cytokine Levels in Migraineurs and Controls. Headache 2005, 45, 926–931. [Google Scholar] [CrossRef]
- Oliveira, A.B.; Bachi, A.L.L.; Ribeiro, R.T.; Mello, M.T.; Tufik, S.; Peres, M.F.P. Unbalanced plasma TNF-α and IL-12/IL-10 profile in women with migraine is associated with psychological and physiological outcomes. J. Neuroimmunol. 2017, 313, 138–144. [Google Scholar] [CrossRef]
- Bowen, R.A.; Remaley, A.T. Interferences from blood collection tube components on clinical chemistry assays. Biochem. Med. 2014, 24, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Togha, M.; Jahromi, S.R.; Ghorbani, Z.; Ghaemi, A.; Rafiee, P. Evaluation of Inflammatory State in Migraineurs: A Case-control Study. Iran. J. Allergy Asthma Immunol. 2020, 19, 83–90. [Google Scholar] [CrossRef]
- Rozen, T.; Swidan, S.Z. Elevation of CSF Tumor Necrosis Factor α Levels in New Daily Persistent Headache and Treatment Refractory Chronic Migraine. Headache 2007, 47, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Kristoffersen, E.S.; Børte, S.; Hagen, K.; Zwart, J.-A.; Winsvold, B.S. Migraine, obesity and body fat distribution—A population-based study. J. Headache Pain 2020, 21, 97. [Google Scholar] [CrossRef]
- Rubino, E.; Vacca, A.; Govone, F.; Gai, A.; Boschi, S.; Zucca, M.; De Martino, P.; Gentile, S.; Pinessi, L.; Rainero, I. Investigating the role of adipokines in chronic migraine. Cephalalgia 2017, 37, 1067–1073. [Google Scholar] [CrossRef] [PubMed]
- Domínguez, C.; Vieites-Prado, A.; Pérez-Mato, M.; Sobrino, T.; Rodríguez-Osorio, X.; López, A.; Campos, F.; Martínez, F.; Castillo, J.; Leira, R. Role of adipocytokines in the pathophysiology of migraine: A cross-sectional study. Cephalalgia 2018, 38, 904–911. [Google Scholar] [CrossRef]
- Duarte, H.; Teixeira, A.L.; Rocha, N.P.; Domingues, R.B. Increased serum levels of adiponectin in migraine. J. Neurol. Sci. 2014, 342, 186–188. [Google Scholar] [CrossRef]
- Chai, N.C.; Gelaye, B.; Tietjen, G.E.; Dash, P.D.; Gower, B.A.; White, L.W.; Ward, T.N.; Scher, A.I.; Peterlin, B.L. Ictal adipokines are associated with pain severity and treatment response in episodic migraine. Neurology 2015, 84, 1409–1418. [Google Scholar] [CrossRef]
- Antonova, M.; Wienecke, T.; Olesen, J.; Ashina, M. Prostaglandins in migraine: Update. Curr. Opin. Neurol. 2013, 26, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Durham, P.L.; Vause, C.V.; Derosier, F.; McDonald, S.; Cady, R.; Martin, V. Changes in Salivary Prostaglandin Levels during Menstrual Migraine with Associated Dysmenorrhea. Headache 2010, 50, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Mannix, L.K. Menstrual-Related Pain Conditions: Dysmenorrhea and Migraine. J. Women’s Health 2008, 17, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Nappi, R.E.; Tiranini, L.; Sacco, S.; De Matteis, E.; De Icco, R.; Tassorelli, C. Role of Estrogens in Menstrual Migraine. Cells 2022, 11, 1355. [Google Scholar] [CrossRef] [PubMed]
- Mozafarihashjin, M.; Togha, M.; Ghorbani, Z.; Farbod, A.; Rafiee, P.; Martami, F. Assessment of peripheral biomarkers potentially involved in episodic and chronic migraine: A case-control study with a focus on NGF, BDNF, VEGF, and PGE2. J. Headache Pain 2022, 23, 3. [Google Scholar] [CrossRef]
- Mohammadian, P.; Hummel, T.; Arora, C.; Carpenter, T. Peripheral levels of inflammatory mediators in migraineurs during headache-free periods. Headache 2001, 41, 867–872. [Google Scholar]
- Tuca, J.O.; Planas, J.; Parellada, R.P. Increase in PGE2 and TXA2 in the Saliva of Common Migraine Patients. Action of Calcium Channel Blockers. Headache 1989, 29, 498–501. [Google Scholar] [CrossRef]
- Takai, E.; Tsukimoto, M.; Kojima, S. TGF-β1 Downregulates COX-2 Expression Leading to Decrease of PGE2 Production in Human Lung Cancer A549 Cells, Which Is Involved in Fibrotic Response to TGF-β1. PLoS ONE 2013, 8, e76346. [Google Scholar] [CrossRef]
- Li, C.; Zhu, Q.; He, Q.; Wang, J.; Wang, F.; Zhang, H. Plasma Levels of Cyclooxygenase-2 (COX-2) and Visfatin during Different Stages and Different Subtypes of Migraine Headaches. Experiment 2017, 23, 24–28. [Google Scholar] [CrossRef]
- Zlibut, A.; Bocsan, I.C.; Agoston-Coldea, L. Pentraxin-3 and endothelial dysfunction. Adv. Clin. Chem. 2019, 91, 163–179. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, H.; Xia, B.; Dong, L. Brief overview of Pentraxin 3. Am. J. Emerg. Med. 2020, 38, 1692. [Google Scholar] [CrossRef]
- Ceylan, M.; Bayraktutan, O.F.; Becel, S.; Atis, Ö.; Yalcin, A.; Kotan, D. Serum levels of pentraxin-3 and other inflammatory biomarkers in migraine: Association with migraine characteristics. Cephalalgia 2016, 36, 518–525. [Google Scholar] [CrossRef] [PubMed]
- Gokdemir, M.T.; Nas, C.; Gokdemir, G.S. Pentraxin 3 level in acute migraine attack with aura: Patient management in the emergency department. Am. J. Emerg. Med. 2020, 38, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Vivero, C.; Leira, Y.; López-Ferreiro, A.; Saavedra, M.; Rodríguez-Osorio, X.; Sobrino, T.; Campos, F.; Castillo, J.; Leira, R. Pentraxin 3 (PTX3): A Molecular Marker of Endothelial Dysfunction in Chronic Migraine. J. Clin. Med. 2020, 9, 849. [Google Scholar] [CrossRef] [PubMed]
- Rees, T.; Watson, D.; Lipscombe, S.; Speight, H.; Cousins, P.; Hardman, G.; Dowson, A. A prospective audit of food intolerance among migraine patients in primary care clinical practice. Headache Care 2005, 2, 105–110. [Google Scholar]
- Alpay, K.; Ertaş, M.; Orhan, E.K.; Üstay, D.K.; Lieners, C.; Baykan, B. Diet restriction in migraine, based on IgG against foods: A clinical double-blind, randomised, cross-over trial. Cephalalgia 2010, 30, 829–837. [Google Scholar] [CrossRef]
- Zhao, Z.; Jin, H.; Yin, Y.; Hou, Y.; Wang, J.; Tang, C.; Fu, J. Association of Migraine with Its Comorbidities and Food Specific Immunoglobulin G Antibodies and Inflammatory Cytokines: Cross-Sectional Clinical Research. J. Pain Res. 2021, 14, 2359–2368. [Google Scholar] [CrossRef]
- Aydinlar, E.I.; Dikmen, P.Y.; Tiftikçi, A.; Saruc, M.; Aksu, M.; Gunsoy, H.G.; Tözün, N. IgG-Based Elimination Diet in Migraine Plus Irritable Bowel Syndrome. Headache 2013, 53, 514–525. [Google Scholar] [CrossRef]
- Xu, J.; Wang, Y.; Han, Y.; Liu, N.; Liu, Z.; Guo, H.; Zou, X.; Zhang, J. A Preliminary Study on Change of Serum Immunoglobulin G Glycosylation in Patients with Migraine. Front. Neurol. 2022, 13, 860555. [Google Scholar] [CrossRef]
- Rempe, R.G.; Hartz, A.M.S.; Bauer, B. Matrix metalloproteinases in the brain and blood–brain barrier: Versatile breakers and makers. J. Cereb. Blood Flow Metab. 2016, 36, 1481–1507. [Google Scholar] [CrossRef] [PubMed]
- Wiggers, A.; Ashina, H.; Hadjikhani, N.; Sagare, A.; Zlokovic, B.V.; Lauritzen, M.; Ashina, M. Brain barriers and their potential role in migraine pathophysiology. J. Headache Pain 2022, 23, 16. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.K. CSD, BBB and MMP-9 elevations: Animal experiments versus clinical phenomena in migraine. Expert Rev. Neurother. 2009, 9, 1595–1614. [Google Scholar] [CrossRef] [PubMed]
- Leira, R.; Sobrino, T.; Rodríguez-Yáñez, M.; Blanco, M.; Arias, S.; Castillo, J. MMP-9 Immunoreactivity in Acute Migraine. Headache 2007, 47, 698–702. [Google Scholar] [CrossRef]
- Imamura, K.; Takeshima, T.; Fusayasu, E.; Nakashima, K. Increased Plasma Matrix Metalloproteinase-9 Levels in Migraineurs. Headache 2008, 48, 135–139. [Google Scholar] [CrossRef]
- Gao, H.-M.; Li, L.; Zhang, K.-L.; Chen, X.-H.; Tian, S.-Q.; Zhang, Z.-L. Impact of migraine attacks on the blood-brain barrier. Chin. Med. J. 2010, 123, 2559–2561. [Google Scholar]
- Ashina, M.; Tvedskov, J.; Lipka, K.; Bilello, J.; Penkowa, M.; Olesen, J. Matrix metalloproteinases during and outside of migraine attacks without aura. Cephalalgia 2010, 30, 303–310. [Google Scholar] [CrossRef]
- Karademir, F.; Ozturk, M.; Altunkaynak, Y.; Doventas, Y.; Mutluay, B.; Koseahmet, F.B.; Baybas, S. Assessment of serum MMP-9, TIMP-1 levels and MMP-9/TIMP-1 ratio in migraine patients with and without aura. Ideggyogy. Szle. 2022, 75, 341–349. [Google Scholar] [CrossRef]
- Gürsoy-Ozdemir, Y.; Qiu, J.; Matsuoka, N.; Bolay, H.; Bermpohl, D.; Jin, H.; Wang, X.; Rosenberg, G.A.; Lo, E.H.; Moskowitz, M.A. Cortical spreading depression activates and upregulates MMP-9. J. Clin. Investig. 2004, 113, 1447–1455. [Google Scholar] [CrossRef]
- Piomelli, D.; Sasso, O. Peripheral gating of pain signals by endogenous lipid mediators. Nat. Neurosci. 2014, 17, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Castor, K.; Dawlaty, J.; Arakaki, X.; Gross, N.; Woldeamanuel, Y.W.; Harrington, M.G.; Cowan, R.P.; Fonteh, A.N. Plasma Lipolysis and Changes in Plasma and Cerebrospinal Fluid Signaling Lipids Reveal Abnormal Lipid Metabolism in Chronic Migraine. Front. Mol. Neurosci. 2021, 14, 691733. [Google Scholar] [CrossRef] [PubMed]
- Di Marzo, V. New approaches and challenges to targeting the endocannabinoid system. Nat. Rev. Drug Discov. 2018, 17, 623–639. [Google Scholar] [CrossRef]
- Russo, E.B. Clinical endocannabinoid deficiency (CECD): Can this concept explain therapeutic benefits of cannabis in migraine, fibromyalgia, irritable bowel syndrome and other treatment-resistant conditions? Neuro Endocrinol. Lett. 2004, 25, 31–39. [Google Scholar]
- Greco, R.; Demartini, C.; Zanaboni, A.M.; Piomelli, D.; Tassorelli, C. Endocannabinoid System and Migraine Pain: An Update. Front. Neurosci. 2018, 12, 172. [Google Scholar] [CrossRef] [PubMed]
- Greco, R.; Demartini, C.; Zanaboni, A.M.; Francavilla, M.; De Icco, R.; Ahmad, L.; Tassorelli, C. The endocannabinoid system and related lipids as potential targets for the treatment of migraine-related pain. Headache 2022, 62, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Rossi, C.; Pini, L.A.; Cupini, M.L.; Calabresi, P.; Sarchielli, P. Endocannabinoids in platelets of chronic migraine patients and medication-overuse headache patients: Relation with serotonin levels. Eur. J. Clin. Pharmacol. 2008, 64, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sarchielli, P.; Pini, L.A.; Coppola, F.; Rossi, C.; Baldi, A.; Mancini, M.L.; Calabresi, P. Endocannabinoids in Chronic Migraine: CSF Findings Suggest a System Failure. Neuropsychopharmacology 2007, 32, 1384–1390. [Google Scholar] [CrossRef] [PubMed]
- Gouveia-Figueira, S.; Goldin, K.; Hashemian, S.A.; Lindberg, A.; Persson, M.; Nording, M.L.; Laurell, K.; Fowler, C.J. Plasma levels of the endocannabinoid anandamide, related N-acylethanolamines and linoleic acid-derived oxylipins in patients with migraine. Prostaglandins Leukot. Essent. Fat. Acids 2017, 120, 15–24. [Google Scholar] [CrossRef]
- De Icco, R.; Greco, R.; Demartini, C.; Vergobbi, P.; Zanaboni, A.; Tumelero, E.; Reggiani, A.; Realini, N.; Sances, G.; Grillo, V.; et al. Spinal nociceptive sensitization and plasma palmitoylethanolamide levels during experimentally induced migraine attacks. Pain 2021, 162, 2376–2385. [Google Scholar] [CrossRef]
- Heiliczer, S.; Wilensky, A.; Gaver, T.; Georgiev, O.; Hamad, S.; Nemirovski, A.; Hadar, R.; Sharav, Y.; Aframian, D.J.; Tam, J.; et al. Salivary Endocannabinoid Profiles in Chronic Orofacial Pain and Headache Disorders: An Observational Study Using a Novel Tool for Diagnosis and Management. Int. J. Mol. Sci. 2022, 23, 13017. [Google Scholar] [CrossRef]
- Cupini, L.; Bari, M.; Battista, N.; Argirò, G.; Finazzi-Agrò, A.; Calabresi, P.; Maccarrone, M. Biochemical Changes in Endocannabinoid System are Expressed in Platelets of Female but not Male Migraineurs. Cephalalgia 2006, 26, 277–281. [Google Scholar] [CrossRef]
- Cupini, L.; Costa, C.; Sarchielli, P.; Bari, M.; Battista, N.; Eusebi, P.; Calabresi, P.; Maccarrone, M. Degradation of endocannabinoids in chronic migraine and medication overuse headache. Neurobiol. Dis. 2008, 30, 186–189. [Google Scholar] [CrossRef]
- Greco, R.; Demartini, C.; Zanaboni, A.M.; Tumelero, E.; De Icco, R.; Sances, G.; Allena, M.; Tassorelli, C. Peripheral changes of endocannabinoid system components in episodic and chronic migraine patients: A pilot study. Cephalalgia 2021, 41, 185–196. [Google Scholar] [CrossRef]
- Greco, R.; Gasperi, V.; Sandrini, G.; Bagetta, G.; Nappi, G.; Maccarrone, M.; Tassorelli, C. Alterations of the endocannabinoid system in an animal model of migraine: Evaluation in cerebral areas of rat. Cephalalgia 2010, 30, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Greco, R.; Mangione, A.S.; Sandrini, G.; Maccarrone, M.; Nappi, G.; Tassorelli, C. Effects of anandamide in migraine: Data from an animal model. J. Headache Pain 2011, 12, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Kilinc, E.; Ankarali, S.; Torun, I.E.; Dagistan, Y. Receptor mechanisms mediating the anti-neuroinflammatory effects of endocannabinoid system modulation in a rat model of migraine. Eur. J. Neurosci. 2022, 55, 1015–1031. [Google Scholar] [CrossRef] [PubMed]
- Akerman, S.; Kaube, H.; Goadsby, P.J. Anandamide acts as a vasodilator of dural blood vessels in vivo by activating TRPV1 receptors. Br. J. Pharmacol. 2004, 142, 1354–1360. [Google Scholar] [CrossRef] [PubMed]
- Akerman, S.; Kaube, H.; Goadsby, P.J. Anandamide Is Able to Inhibit Trigeminal Neurons Using an in Vivo Model of Trigeminovascular-Mediated Nociception. J. Pharmacol. Exp. Ther. 2004, 309, 56–63. [Google Scholar] [CrossRef]
- Gallelli, L.; Cione, E.; Caroleo, M.C.; Carotenuto, M.; Laganà, P.; Siniscalchi, A.; Guidetti, V. microRNAs to Monitor Pain-migraine and Drug Treatment. Microrna 2017, 6, 152–156. [Google Scholar] [CrossRef]
- Gazerani, P. Current Evidence on Potential Uses of MicroRNA Biomarkers for Migraine: From Diagnosis to Treatment. Mol. Diagn. Ther. 2019, 23, 681–694. [Google Scholar] [CrossRef]
- Ahmad, L.; Demartini, C.; Corrado, M.; Vaghi, G.; Piella, E.M.; Allena, M.; Zanaboni, A.M.; Greco, R.; Tassorelli, C.; De Icco, R. Expression of Selected microRNAs in Migraine: A New Class of Possible Biomarkers of Disease? Processes 2021, 9, 2199. [Google Scholar] [CrossRef]
- O’Brien, J.; Hayder, H.; Zayed, Y.; Peng, C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018, 9, 402. [Google Scholar] [CrossRef]
- Velu, V.K.; Ramesh, R.; Srinivasan, A.R. Circulating MicroRNAs as Biomarkers in Health and Disease. J. Clin. Diagn. Res. 2012, 6, 1791–1795. [Google Scholar] [CrossRef] [PubMed]
- Andersen, H.H.; Duroux, M.; Gazerani, P. MicroRNAs as modulators and biomarkers of inflammatory and neuropathic pain conditions. Neurobiol. Dis. 2014, 71, 159–168. [Google Scholar] [CrossRef]
- Andersen, H.H.; Duroux, M.; Gazerani, P. Serum MicroRNA Signatures in Migraineurs during Attacks and in Pain-Free Periods. Mol. Neurobiol. 2016, 53, 1494–1500. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Y.; Zhu, Y.-Y. MiR-30a relieves migraine by degrading CALCA. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 2022–2028. [Google Scholar] [PubMed]
- Cheng, C.-Y.; Chen, S.-P.; Liao, Y.-C.; Fuh, J.-L.; Wang, Y.-F.; Wang, S.-J. Elevated circulating endothelial-specific microRNAs in migraine patients: A pilot study. Cephalalgia 2018, 38, 1585–1591. [Google Scholar] [CrossRef] [PubMed]
- Vila-Pueyo, M.; Fernandez-Morales, J.; Torres-Ferrús, M.; Alvarez-Sabin, J.; Pozo-Rosich, P. EHMTI-0361. Lack of differences in microrna expression profiles of blood cells in migraine. J. Headache Pain 2014, 15, H3. [Google Scholar] [CrossRef]
- Burgos, K.L.; Javaherian, A.; Bomprezzi, R.; Ghaffari, L.; Rhodes, S.; Courtright, A.; Tembe, W.; Kim, S.; Metpally, R.; Van Keuren-Jensen, K. Identification of extracellular miRNA in human cerebrospinal fluid by next-generation sequencing. Rna 2013, 19, 712–722. [Google Scholar] [CrossRef]
- Vanmolkot, F.H.; Van Bortel, L.M.; de Hoon, J.N. Altered arterial function in migraine of recent onset. Neurology 2007, 68, 1563–1570. [Google Scholar] [CrossRef]
- Rossato, A.; Veronese, F.; Maggioni, F.; Vedovetto, V.; Zancan, A.; Biasiolo, M.; Bilora, F. Autonomic dysfunction and endothelial changes in migraine sufferers. Panminerva Med. 2011, 53, 13–18. [Google Scholar]
- Paolucci, M.; Altamura, C.; Vernieri, F. The Role of Endothelial Dysfunction in the Pathophysiology and Cerebrovascular Effects of Migraine: A Narrative Review. J. Clin. Neurol. 2021, 17, 164–175. [Google Scholar] [CrossRef]
- Bigal, M.E.; Kurth, T.; Hu, H.; Santanello, N.; Lipton, R.B. Migraine and cardiovascular disease: Possible mechanisms of interaction. Neurology 2009, 72, 1864–1871. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.M.; Zalos, G.; Halcox, J.P.J.; Schenke, W.H.; Waclawiw, M.A.; Quyyumi, A.A.; Finkel, T. Circulating Endothelial Progenitor Cells, Vascular Function, and Cardiovascular Risk. N. Engl. J. Med. 2003, 348, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Edwards, N.; Langford-Smith, A.W.W.; Wilkinson, F.L.; Alexander, M.Y. Endothelial Progenitor Cells: New Targets for Therapeutics for Inflammatory Conditions with High Cardiovascular Risk. Front. Med. 2018, 5, 200. [Google Scholar] [CrossRef]
- Lee, S.-T.; Chu, K.; Jung, K.-H.; Kim, D.-H.; Choe, V.N.; Im, W.-S.; Kang, L.; Park, J.-E.; Park, H.-J.; Song, E.-C.; et al. Decreased number and function of endothelial progenitor cells in patients with migraine. Neurology 2008, 70, 1510–1517. [Google Scholar] [CrossRef] [PubMed]
- Oterino, A.; Toriello, M.; Palacio, E.; Quintanilla, V.G.; Ruiz-Lavilla, N.; Montes, S.; De La Vega, M.S.; Martinez-Nieto, R.; Castillo, J.; Pascual, J. Analysis of endothelial precursor cells in chronic migraine: A case-control study. Cephalalgia 2013, 33, 236–244. [Google Scholar] [CrossRef]
- Joseph, E.; Levine, J. Role of endothelial cells in antihyperalgesia induced by a triptan and β-blocker. Neuroscience 2013, 232, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, M.; Kurihara, H.; Kimura, S.; Tomobe, Y.; Kobayashi, M.; Mitsui, Y.; Yazaki, Y.; Goto, K.; Masaki, T. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 1988, 332, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Iljazi, A.; Ayata, C.; Ashina, M.; Hougaard, A. The Role of Endothelin in the Pathophysiology of Migraine—A Systematic Review. Curr. Pain Headache Rep. 2018, 22, 27. [Google Scholar] [CrossRef]
- Färkkilä, M.; Palo, J.; Saijonmaa, O.; Fyhrquist, F. Raised Plasma Endothelin during Acute Migraine Attack. Cephalalgia 1992, 12, 383–384. [Google Scholar] [CrossRef]
- Gallai, V.; Sarchielli, P.; Firenze, C.; Trequattrini, A.; Paciaroni, M.; Usai, F.; Palumbo, R. Endothelin 1 in migraine and tension-type headache. Acta Neurol. Scand. 1994, 89, 47–55. [Google Scholar] [CrossRef]
- Bianchi, A.; Pitari, G.; Amenta, V.; Giuliano, F.; Gallina, M.; Costa, R.; Ferlito, S. Endothelial, haemostatic and haemorheological modifications in migraineurs. Artery 1996, 22, 93–100. [Google Scholar]
- Kallela, M.; Färkkilä, M.; Saijonmaa, O.; Fyhrquist, F. Endothelin in Migraine Patients. Cephalalgia 1998, 18, 329–332. [Google Scholar] [CrossRef]
- Hasselblatt, M.; Köhler, J.; Volles, E.; Ehrenreich, H. Simultaneous monitoring of endothelin-1 and vasopressin plasma levels in migraine. Neuroreport 1999, 10, 423–425. [Google Scholar] [CrossRef]
- Eftedal, O.; Lydersen, S.; Helde, G.; White, L.; Brubakk, A.; Stovner, L. A Randomized, Double Blind Study of the Prophylactic Effect of Hyperbaric Oxygen Therapy on Migraine. Cephalalgia 2004, 24, 639–644. [Google Scholar] [CrossRef]
- Hamed, S.A.; Hamed, E.A.; Eldin, A.M.E.; Mahmoud, N.M. Vascular Risk Factors, Endothelial Function, and Carotid Thickness in Patients with Migraine: Relationship to Atherosclerosis. J. Stroke Cerebrovasc. Dis. 2010, 19, 92–103. [Google Scholar] [CrossRef]
- Kim, J.; Park, C.G.; Chu, M.K. Interictal plasma endothelin-1 levels do not change in individuals with episodic and chronic migraine. Cephalalgia 2022, 42, 761–768. [Google Scholar] [CrossRef] [PubMed]
- Vong, C.T.; Chen, Y.; Chen, Z.; Gao, C.; Yang, F.; Wang, S.; Wang, Y. Classical prescription Dachuanxiong Formula delays nitroglycerin-induced pain response in migraine mice through reducing endothelin-1 level and regulating fatty acid biosynthesis. J. Ethnopharmacol. 2022, 288, 114992. [Google Scholar] [CrossRef] [PubMed]
- Dreier, J.P.; Kleeberg, J.; Petzold, G.; Priller, J.; Windmüller, O.; Orzechowski, H.; Lindauer, U.; Heinemann, U.; Einhäupl, K.M.; Dirnagl, U. Endothelin-1 potently induces Leão’s cortical spreading depression in vivo in the rat: A model for an endothelial trigger of migrainous aura? Brain 2002, 125, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Kleeberg, J.; Petzold, G.C.; Major, S.; Dirnagl, U.; Dreier, J.P. ET-1 induces cortical spreading depression via activation of the ETA receptor/phospholipase C pathway in vivo. Am. J. Physiol. Heart Circ. Physiol. 2004, 286, H1339–H1346. [Google Scholar] [CrossRef]
- Hougaard, A.; Younis, S.; Iljazi, A.; Sugimoto, K.; Ayata, C.; Ashina, M. Intravenous Endothelin-1 Infusion Does Not Induce Aura or Headache in Migraine Patients with Aura. Headache 2020, 60, 724–734. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Mattiuzzi, C.; Meschi, T.; Cervellin, G.; Borghi, L. Homocysteine and migraine. A narrative review. Clin. Chim. Acta 2014, 433, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Cupini, L.; Stipa, E. Migraine Aura Status and Hyperhomocysteinaemia. Cephalalgia 2007, 27, 847–849. [Google Scholar] [CrossRef]
- Gerasimova, E.; Burkhanova, G.; Chernova, K.; Zakharov, A.; Enikeev, D.; Khaertdinov, N.; Giniatullin, R.; Sitdikova, G. Hyperhomocysteinemia increases susceptibility to cortical spreading depression associated with photophobia, mechanical allodynia, and anxiety in rats. Behav. Brain Res. 2021, 409, 113324. [Google Scholar] [CrossRef]
- Liampas, I.; Siokas, V.; Mentis, A.A.; Aloizou, A.M.; Dastamani, M.; Tsouris, Z.; Aslanidou, P.; Brotis, A.; Dardiotis, E. Serum Homocysteine, Pyridoxine, Folate, and Vitamin B12 Levels in Migraine: Systematic Review and Meta-Analysis. Headache 2020, 60, 1508–1534. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y. Change and significance of plasma homocysteine in patients with migraine. Chin. J. Clin. Rehabil. 2004, 8, 92–93. [Google Scholar]
- Moschiano, F.; D’Amico, D.; Usai, S.; Grazzi, L.; Di Stefano, M.; Ciusani, E.; Erba, N.; Bussone, G. Homocysteine plasma levels in patients with migraine with aura. Neurol. Sci. 2008, 29 (Suppl. S1), S173–S175. [Google Scholar] [CrossRef]
- Ipçioǧlu, O.M.; Özcan, Ö.; Gültepe, M.; Tekeli, H.; Şenol, M.G. Functional Vitamin B12 Deficiency Represented by Elevated Urine Methylmalonic Acid Levels in Patients with Migraine. Turk. J. Med. Sci. 2008, 38, 409–414. [Google Scholar]
- Bahadir, A.; Eroz, R.; Dikici, S. Investigation of MTHFR C677T Gene Polymorphism, Biochemical and Clinical Parameters in Turkish Migraine Patients: Association with Allodynia and Fatigue. Cell. Mol. Neurobiol. 2013, 33, 1055–1063. [Google Scholar] [CrossRef] [PubMed]
- Gavgani, S.C. Comparative study on homocysteine levels in migraine patients and normal peoples. Ann. Biol. Res. 2012, 3, 1804–1807. [Google Scholar]
- Hering-Hanit, R.; Gadoth, N.; Yavetz, A.; Gavendo, S.; Sela, B. Is Blood Homocysteine Elevated in Migraine? Headache 2001, 41, 779–781. [Google Scholar] [CrossRef] [PubMed]
- Bokhari, F.A.; Shakoori, T.A.; Hassan SA, A.; Qureshi, H.J.; Qureshi, G.A. Plasma homocysteine in patients of migraine without aura. J. Ayub Med. Coll. Abbottabad 2011, 22, 52–55. [Google Scholar]
- Oterino, A.; Toriello, M.; Valle, N.; Castillo, J.; Alonso-Arranz, A.; Bravo, Y.; Ruiz-Alegria, C.; Quintela, E.; Pascual, J. The Relationship between Homocysteine and Genes of Folate-Related Enzymes in Migraine Patients. Headache 2010, 50, 99–168. [Google Scholar] [CrossRef] [PubMed]
- Kurth, T.; Ridker, P.; Buring, J. Migraine and Biomarkers of Cardiovascular Disease in Women. Cephalalgia 2008, 28, 49–56. [Google Scholar] [CrossRef]
- Tietjen, G.E.; Herial, N.A.; White, L.; Utley, C.; Kosmyna, J.M.; Khuder, S.A. Migraine and Biomarkers of Endothelial Activation in Young Women. Stroke 2009, 40, 2977–2982. [Google Scholar] [CrossRef] [PubMed]
- Isobe, C.; Terayama, Y. A Remarkable Increase in Total Homocysteine Concentrations in the CSF of Migraine Patients with Aura. Headache 2010, 50, 1561–1569. [Google Scholar] [CrossRef]
- Gerasimova, E.; Yakovleva, O.; Enikeev, D.; Bogatova, K.; Hermann, A.; Giniatullin, R.; Sitdikova, G. Hyperhomocysteinemia Increases Cortical Excitability and Aggravates Mechanical Hyperalgesia and Anxiety in a Nitroglycerine-Induced Migraine Model in Rats. Biomolecules 2022, 12, 735. [Google Scholar] [CrossRef]
- Schwarcz, R.; Bruno, J.P.; Muchowski, P.J.; Wu, H.-Q. Kynurenines in the mammalian brain: When physiology meets pathology. Nat. Rev. Neurosci. 2012, 13, 465–477. [Google Scholar] [CrossRef] [PubMed]
- Curto, M.; Lionetto, L.; Fazio, F.; Mitsikostas, D.-D.; Martelletti, P. Fathoming the kynurenine pathway in migraine: Why understanding the enzymatic cascades is still critically important. Intern. Emerg. Med. 2015, 10, 413–421. [Google Scholar] [CrossRef]
- Nagy-Grócz, G.; Laborc, K.F.; Veres, G.; Bajtai, A.; Bohár, Z.; Zádori, D.; Fejes-Szabó, A.; Spekker, E.; Vécsei, L.; Párdutz, Á. The Effect of Systemic Nitroglycerin Administration on the Kynurenine Pathway in the Rat. Front. Neurol. 2017, 8, 278. [Google Scholar] [CrossRef]
- Cseh, E.K.; Veres, G.; Körtési, T.; Polyák, H.; Nánási, N.; Tajti, J.; Párdutz, Á.; Klivényi, P.; Vécsei, L.; Zádori, D. Neurotransmitter and tryptophan metabolite concentration changes in the complete Freund’s adjuvant model of orofacial pain. J. Headache Pain 2020, 21, 35. [Google Scholar] [CrossRef]
- Ren, C.; Liu, J.; Zhou, J.; Liang, H.; Wang, Y.; Sun, Y.; Ma, B.; Yin, Y. Low levels of serum serotonin and amino acids identified in migraine patients. Biochem. Biophys. Res. Commun. 2018, 496, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Nagata, E.; Shibata, M.; Hamada, J.; Shimizu, T.; Katoh, Y.; Gotoh, K.; Suzuki, N. Plasma 5-Hydroxytryptamine (5-HT) in Migraine during an Attack-Free Period. Headache 2006, 46, 592–596. [Google Scholar] [CrossRef] [PubMed]
- Curto, M.; Lionetto, L.; Negro, A.; Capi, M.; Fazio, F.; Giamberardino, M.A.; Simmaco, M.; Nicoletti, F.; Martelletti, P. Altered kynurenine pathway metabolites in serum of chronic migraine patients. J. Headache Pain 2015, 17, 47. [Google Scholar] [CrossRef] [PubMed]
- Gecse, K.; Édes, A.E.; Nagy, T.; Demeter, A.K.; Virág, D.; Király, M.; Kiss, B.D.; Ludányi, K.; Környei, Z.; Denes, A.; et al. Citalopram Neuroendocrine Challenge Shows Altered Tryptophan and Kynurenine Metabolism in Migraine. Cells 2022, 11, 2258. [Google Scholar] [CrossRef] [PubMed]
- Zduńska, A.; Cegielska, J.; Domitrz, I. The Pathogenetic Role of Melatonin in Migraine and Its Theoretic Implications for Pharmacotherapy: A Brief Overview of the Research. Nutrients 2022, 14, 3335. [Google Scholar] [CrossRef] [PubMed]
- Alstadhaug, K.B.; Odeh, F.; Salvesen, R.; Bekkelund, S.I. Prophylaxis of migraine with melatonin: A randomized controlled trial. Neurology 2010, 75, 1527–1532. [Google Scholar] [CrossRef]
- Ebrahimi-Monfared, M.; Sharafkhah, M.; Abdolrazaghnejad, A.; Mohammadbeigi, A.; Faraji, F. Use of melatonin versus valproic acid in prophylaxis of migraine patients: A double-blind randomized clinical trial. Restor. Neurol. Neurosci. 2017, 35, 385–393. [Google Scholar] [CrossRef]
- Liampas, I.; Siokas, V.; Brotis, A.; Vikelis, M.; Dardiotis, E. Endogenous Melatonin Levels and Therapeutic Use of Exogenous Melatonin in Migraine: Systematic Review and Meta-Analysis. Headache 2020, 60, 1273–1299. [Google Scholar] [CrossRef]
- Tseng, P.; Yang, C.; Su, K.; Chen, T.; Wu, Y.; Tu, Y.; Lin, P.; Stubbs, B.; Carvalho, A.F.; Matsuoka, Y.J.; et al. The association between melatonin and episodic migraine: A pilot network meta-analysis of randomized controlled trials to compare the prophylactic effects with exogenous melatonin supplementation and pharmacotherapy. J. Pineal Res. 2020, 69, e12663. [Google Scholar] [CrossRef]
- Barker, P.A.; Mantyh, P.; Arendt-Nielsen, L.; Viktrup, L.; Tive, L. Nerve Growth Factor Signaling and Its Contribution to Pain. J. Pain Res. 2020, 13, 1223–1241. [Google Scholar] [CrossRef] [PubMed]
- Merighi, A.; Salio, C.; Ghirri, A.; Lossi, L.; Ferrini, F.; Betelli, C.; Bardoni, R. BDNF as a pain modulator. Prog. Neurobiol. 2008, 85, 297–317. [Google Scholar] [CrossRef] [PubMed]
- Shu, X.-Q.; Llinas, A.; Mendell, L.M. Effects of trkB and trkC neurotrophin receptor agonists on thermal nociception: A behavioral and electrophysiological study. Pain 1999, 80, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Martins, L.B.; Duarte, H.; Ferreira, A.V.; Rocha, N.P.; Teixeira, A.L.; Domingues, R.B. Migraine is associated with altered levels of neurotrophins. Neurosci. Lett. 2015, 587, 6–10. [Google Scholar] [CrossRef]
- Sarchielli, P.; Alberti, A.; Candeliere, A.; Floridi, A.; Capocchi, G.; Calabresi, P. Glial Cell Line-Derived Neurotrophic Factor and Somatostatin Levels in Cerebrospinal Fluid of Patients Affected by Chronic Migraine and Fibromyalgia. Cephalalgia 2006, 26, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Blandini, F.; Rinaldi, L.; Tassorelli, C.; Sances, G.; Motta, M.; Samuele, A.; Fancellu, R.; Nappi, G.; Leon, A. Peripheral Levels of BDNF and NGF in Primary Headaches. Cephalalgia 2006, 26, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Sarchielli, P.; Mancini, M.L.; Floridi, A.; Coppola, F.; Rossi, C.; Nardi, K.; Acciarresi, M.; Pini, L.A.; Calabresi, P. Increased Levels of Neurotrophins Are Not Specific for Chronic Migraine: Evidence from Primary Fibromyalgia Syndrome. J. Pain 2007, 8, 737–745. [Google Scholar] [CrossRef]
- Tanure, M.T.A.; Gomez, R.S.; Hurtado, R.C.L.; Teixeira, A.L.; Domingues, R.B. Increased serum levels of brain-derived neurotropic factor during migraine attacks: A pilot study. J. Headache Pain 2010, 11, 427–430. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.; Wille, G.; Klien, S.; Shanib, H.; Holle, D.; Gaul, C.; Broessner, G. Brain-derived neurotrophic factor in primary headaches. J. Headache Pain 2012, 13, 469–475. [Google Scholar] [CrossRef]
- Ghavami, A.; Khorvash, F.; Khalesi, S.; Heidari, Z.; Askari, G. The effects of synbiotic supplementation on oxidative stress and clinical symptoms in women with migraine: A double-blind, placebo-controlled, randomized trial. J. Funct. Foods 2021, 86, 104738. [Google Scholar] [CrossRef]
- Khosravi, A.; Nakhaee, A.; Ghoreishi, A.; Arefpoor, Z.; Sadeghi, M. Impaired oxidative-antioxidative balance during migraine attack. BioMed. Res. Ther. 2019, 6, 2996–3002. [Google Scholar] [CrossRef]
- Borkum, J.M. Migraine Triggers and Oxidative Stress: A Narrative Review and Synthesis. Headache 2016, 56, 12–35. [Google Scholar] [CrossRef] [PubMed]
- Xiong, S.; Markesbery, W.R.; Shao, C.; Lovell, M.A. Seleno-L-Methionine Protects against β-Amyloid and Iron/Hydrogen Peroxide-Mediated Neuron Death. Antioxid. Redox Signal. 2007, 9, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Draper, H.H.; Hadley, M. [43] Malondialdehyde determination as index of lipid Peroxidation. In Methods in Enzymology; Academic press: Cambridge, MA, USA, 1990; Volume 186, pp. 421–431. [Google Scholar] [CrossRef]
- Hageman, J.; Bast, A.; Vermeulen, N. Monitoring of oxidative free radical damage in vivo: Analytical aspects. Chem. Biol. Interact. 1992, 82, 243–293. [Google Scholar] [CrossRef] [PubMed]
- Neri, M.; Frustaci, A.; Milic, M.; Valdiglesias, V.; Fini, M.; Bonassi, S.; Barbanti, P. A meta-analysis of biomarkers related to oxidative stress and nitric oxide pathway in migraine. Cephalalgia 2015, 35, 931–937. [Google Scholar] [CrossRef]
- Talaie, A.; Jafary, H.; Faraji, F.; Malekirad, A.A. The Serum Oxidative Stress Biomarkers and Selenium Levels in a Group of Migraine Patients Compared with Healthy Controls: A Case-Control Study. Biol. Trace Elem. Res. 2022, 200, 4250–4255. [Google Scholar] [CrossRef]
- Togha, M.; Jahromi, S.R.; Ghorbani, Z.; Ghaemi, A.; Rafiee, P. An investigation of oxidant/antioxidant balance in patients with migraine: A case-control study. BMC Neurol. 2019, 19, 323. [Google Scholar] [CrossRef]
- Tripathi, G.M.; Kalita, J.; Misra, U.K. A study of oxidative stress in migraine with special reference to prophylactic therapy. Int. J. Neurosci. 2018, 128, 318–324. [Google Scholar] [CrossRef]
- Yamazaki, Y.; Zhao, N.; Caulfield, T.R.; Liu, C.-C.; Bu, G. Apolipoprotein E and Alzheimer disease: Pathobiology and targeting strategies. Nat. Rev. Neurol. 2019, 15, 501–518. [Google Scholar] [CrossRef]
- Lagging, C.; Lorentzen, E.; Stanne, T.M.; Pedersen, A.; Söderholm, M.; Cole, J.W.; Jood, K.; Lemmens, R.; Phuah, C.-L.; Rost, N.S.; et al. APOE ε4 is associated with younger age at ischemic stroke onset but not with stroke outcome. Neurology 2019, 93, 849–853. [Google Scholar] [CrossRef]
- Yuasa, N.; Nagata, E.; Fujii, N.; Ito, M.; Tsukamoto, H.; Takizawa, S. Serum apolipoprotein E may be a novel biomarker of migraine. PLoS ONE 2018, 13, e0190620. [Google Scholar] [CrossRef] [PubMed]
- Miao, J.; Wang, F.; Zheng, W.; Zhuang, X. Association of the Apolipoprotein E polymorphism with migraine: A meta-analysis. BMC Neurol. 2015, 15, 138. [Google Scholar] [CrossRef]
- Gupta, R.; Kumar, V.; Luthra, K.; Banerjee, B.; Bhatia, M.S. Polymorphism in apolipoprotein E among migraineurs and tension-type headache subjects. J. Headache Pain 2009, 10, 115–120. [Google Scholar] [CrossRef]
- Bhatt, D.K.; Gupta, S.; Olesen, J.; Jansen-Olesen, I. PACAP-38 infusion causes sustained vasodilation of the middle meningeal artery in the rat: Possible involvement of mast cells. Cephalalgia 2014, 34, 877–886. [Google Scholar] [CrossRef]
- Iyengar, S.; Ossipov, M.H.; Johnson, K.W. The role of calcitonin gene–related peptide in peripheral and central pain mechanisms including migraine. Pain 2017, 158, 543–559. [Google Scholar] [CrossRef]
- Moriarty, M.; Mallick-Searle, T.; Barch, C.A.; Oas, K. Monoclonal Antibodies to CGRP or Its Receptor for Migraine Prevention. J. Nurse Pract. 2019, 15, 717–724.e1. [Google Scholar] [CrossRef]
- Sevivas, H.; Fresco, P. Treatment of resistant chronic migraine with anti-CGRP monoclonal antibodies: A systematic review. Eur. J. Med. Res. 2022, 27, 86. [Google Scholar] [CrossRef] [PubMed]
- De Icco, R.; Fiamingo, G.; Greco, R.; Bottiroli, S.; Demartini, C.; Zanaboni, A.M.; Allena, M.; Guaschino, E.; Martinelli, D.; Putortì, A.; et al. Neurophysiological and biomolecular effects of erenumab in chronic migraine: An open label study. Cephalalgia 2020, 40, 1336–1345. [Google Scholar] [CrossRef] [PubMed]
- Iannone, L.F.; De Cesaris, F.; Ferrari, A.; Benemei, S.; Fattori, D.; Chiarugi, A. Effectiveness of anti-CGRP monoclonal antibodies on central symptoms of migraine. Cephalalgia 2022, 42, 1323–1330. [Google Scholar] [CrossRef]
- Akerman, S.; Williamson, D.J.; Kaube, H.; Goadsby, P.J. Nitric oxide synthase inhibitors can antagonize neurogenic and calcitonin gene-related peptide induced dilation of dural meningeal vessels. Br. J. Pharmacol. 2002, 137, 62–68. [Google Scholar] [CrossRef]
- D’Amico, D.; Ferraris, A.; Leone, M.; Catania, A.; Carlin, A.; Grazzi, L.; Bussone, G. Increased Plasma Nitrites in Migraine and Cluster Headache Patients in Interictal Period: Basal Hyperactivity of L-Arginine-No Pathway? Cephalalgia 2002, 22, 33–36. [Google Scholar] [CrossRef]
- Uzar, E.; Evliyaoglu, O.; Toprak, G.; Acar, A.; Yucel, Y.; Calisir, T.; Cevik, M.U.; Tasdemir, N. Increased asymmetric dimethylarginine and nitric oxide levels in patients with migraine. J. Headache Pain 2011, 12, 239–243. [Google Scholar] [CrossRef]
- Li, J.; Vause, C.V.; Durham, P.L. Calcitonin gene-related peptide stimulation of nitric oxide synthesis and release from trigeminal ganglion glial cells. Brain Res. 2008, 1196, 22–32. [Google Scholar] [CrossRef]
- Vause, C.V.; Durham, P.L. CGRP stimulation of iNOS and NO release from trigeminal ganglion glial cells involves mitogen-activated protein kinase pathways. J. Neurochem. 2009, 110, 811–821. [Google Scholar] [CrossRef]
- Reuter, U.; Bolay, H.; Jansen-Olesen, I.; Chiarugi, A.; Del Rio, M.S.; Letourneau, R.; Theoharides, T.C.; Waeber, C.; Moskowitz, M.A. Delayed inflammation in rat meninges: Implications for migraine pathophysiology. Brain 2001, 124, 2490–2502. [Google Scholar] [CrossRef] [PubMed]
- Pardutz, A.; Krizbai, I.; Multon, S.; Vécsei, L.; Schoenen, J. Systemic nitroglycerin increases nNOS levels in rat trigeminal nucleus caudalis. Neuroreport 2000, 11, 3071–3075. [Google Scholar] [CrossRef] [PubMed]
- Nagy-Grócz, G.; Tar, L.; Bohár, Z.; Fejes-Szabó, A.; Laborc, K.F.; Spekker, E.; Vécsei, L.; Párdutz, Á. The modulatory effect of anandamide on nitroglycerin-induced sensitization in the trigeminal system of the rat. Cephalalgia 2016, 36, 849–861. [Google Scholar] [CrossRef] [PubMed]
- Greco, R.; Ferrigno, A.; DeMartini, C.; Zanaboni, A.; Mangione, A.S.; Blandini, F.; Nappi, G.; Vairetti, M.; Tassorelli, C. Evaluation of ADMA-DDAH-NOS axis in specific brain areas following nitroglycerin administration: Study in an animal model of migraine. J. Headache Pain 2015, 16, 560. [Google Scholar] [CrossRef] [PubMed]
- Greco, R.; Demartini, C.; Zanaboni, A.M.; Redavide, E.; Pampalone, S.; Toldi, J.; Fülöp, F.; Blandini, F.; Nappi, G.; Sandrini, G.; et al. Effects of kynurenic acid analogue 1 (KYNA-A1) in nitroglycerin-induced hyperalgesia: Targets and anti-migraine mechanisms. Cephalalgia 2017, 37, 1272–1284. [Google Scholar] [CrossRef] [PubMed]
- Kurul, S.H.; Demirpence, S.; Kiray, M.; Tugyan, K.; Yilmaz, O.; Kose, G. Investigation of the immunoreactivities of NOS enzymes and the effect of sumatriptan in adolescent rats using an experimental model of migraine. J. Headache Pain 2008, 9, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Hou, M.; Tang, Q.; Xue, Q.; Zhang, X.; Liu, Y.; Yang, S.; Chen, L.; Xu, X. Pharmacodynamic action and mechanism of Du Liang soft capsule, a traditional Chinese medicine capsule, on treating nitroglycerin-induced migraine. J. Ethnopharmacol. 2017, 195, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Colton, C.A.; Brown, C.M.; Cook, D.; Needham, L.K.; Xu, Q.; Czapiga, M.; Saunders, A.M.; Schmechel, D.E.; Rasheed, K.; Vitek, M.P. APOE and the regulation of microglial nitric oxide production: A link between genetic risk and oxidative stress. Neurobiol. Aging 2002, 23, 777–785. [Google Scholar] [CrossRef]
- Czapiga, M.; Colton, C.A. Microglial function in human APOE3 and APOE4 transgenic mice: Altered arginine transport. J. Neuroimmunol. 2003, 134, 44–51. [Google Scholar] [CrossRef]
- Tsoi, L.-M.; Wong, K.-Y.; Liu, Y.-M.; Ho, Y.-Y. Apoprotein E isoform-dependent expression and secretion of pro-inflammatory cytokines TNF-α and IL-6 in macrophages. Arch. Biochem. Biophys. 2007, 460, 33–40. [Google Scholar] [CrossRef]
- Afroz, S.; Arakaki, R.; Iwasa, T.; Oshima, M.; Hosoki, M.; Inoue, M.; Baba, O.; Okayama, Y.; Matsuka, Y. CGRP Induces Differential Regulation of Cytokines from Satellite Glial Cells in Trigeminal Ganglia and Orofacial Nociception. Int. J. Mol. Sci. 2019, 20, 711. [Google Scholar] [CrossRef]
- Demartini, C.; Greco, R.; Magni, G.; Zanaboni, A.M.; Riboldi, B.; Francavilla, M.; Nativi, C.; Ceruti, S.; Tassorelli, C. Modulation of Glia Activation by TRPA1 Antagonism in Preclinical Models of Migraine. Int. J. Mol. Sci. 2022, 23, 14085. [Google Scholar] [CrossRef] [PubMed]
- Ye, S.; Li, S.; Ma, Y.; Wei, L.; Zeng, Y.; Hu, D.; Xiao, F. Ambient NO2 exposure induces migraine in rats: Evidence, mechanisms and interventions. Sci. Total Environ. 2022, 844, 157102. [Google Scholar] [CrossRef] [PubMed]
- Naya, M.; Tsukamoto, T.; Morita, K.; Katoh, C.; Furumoto, T.; Fujii, S.; Tamaki, N.; Tsutsui, H. Plasma Interleukin-6 and Tumor Necrosis Factor-.ALPHA. Can Predict Coronary Endothelial Dysfunction in Hypertensive Patients. Hypertens. Res. 2007, 30, 541–548. [Google Scholar] [CrossRef]
- Picchi, A.; Gao, X.; Belmadani, S.; Potter, B.J.; Focardi, M.; Chilian, W.M.; Zhang, C. Tumor Necrosis Factor-α Induces Endothelial Dysfunction in the Prediabetic Metabolic Syndrome. Circ. Res. 2006, 99, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, D.H. Prevention of endothelin-1-induced increases in blood pressure: Role of endogenous CGRP. Am. J. Physiol. Heart Circ. Physiol. 2004, 287, H1868–H1874. [Google Scholar] [CrossRef]
- Bourque, S.L.; Davidge, S.T.; Adams, M.A. The interaction between endothelin-1 and nitric oxide in the vasculature: New perspectives. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2011, 300, R1288–R1295. [Google Scholar] [CrossRef]
- Miura, K.; Yukimura, T.; Yamashita, Y.; Shimmen, T.; Okumura, M.; Imanishi, M.; Yamamoto, K. Endothelin stimulates the renal production of prostaglandin E2 and I2 in anesthetized dogs. Eur. J. Pharmacol. 1989, 170, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Edvinsson, L. Role of VIP/PACAP in primary headaches. Cephalalgia 2013, 33, 1070–1072. [Google Scholar] [CrossRef]
- Donnerer, J.; Schuligoi, R.; Stein, C. Increased content and transport of substance P and calcitonin gene-related peptide in sensory nerves innervating inflamed tissue: Evidence for a regulatory function of nerve growth factor in vivo. Neuroscience 1992, 49, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Huang, J.; McNaughton, P.A. NGF rapidly increases membrane expression of TRPV1 heat-gated ion channels. EMBO J. 2005, 24, 4211–4223. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhang, X.M.; Zong, D.D.; Ji, X.Y.; Jiang, H.; Zhang, F.Z.; He, S.D. miR-34a-5p up-regulates the IL-1β/COX2/PGE2 inflammation pathway and induces the release of CGRP via inhibition of SIRT1 in rat trigeminal ganglion neurons. FEBS Open Bio. 2021, 11, 300–311. [Google Scholar] [CrossRef]
- Abouheif, M.M.; Nakasa, T.; Shibuya, H.; Niimoto, T.; Kongcharoensombat, W.; Ochi, M. Silencing microRNA-34a inhibits chondrocyte apoptosis in a rat osteoarthritis model in vitro. Rheumatology 2010, 49, 2054–2060. [Google Scholar] [CrossRef]
- Kriegel, A.J.; Fang, Y.; Liu, Y.; Tian, Z.; Mladinov, D.; Matus, I.R.; Ding, X.; Greene, A.S.; Liang, M. MicroRNA-target pairs in human renal epithelial cells treated with transforming growth factor β1: A novel role of miR-382. Nucleic Acids Res. 2010, 38, 8338–8347. [Google Scholar] [CrossRef]
- Tafuri, E.; Santovito, D.; De Nardis, V.; Marcantonio, P.; Paganelli, C.; Affaitati, G.; Bucci, M.; Mezzetti, A.; Giamberardino, M.A.; Cipollone, F. MicroRNA profiling in migraine without aura: Pilot study. Ann. Med. 2015, 47, 468–473. [Google Scholar] [CrossRef]
- Vikelis, M.; Mitsikostas, D.D. The role of glutamate and its receptors in migraine. CNS Neurol. Disord. Drug Targets 2007, 6, 251–257. [Google Scholar] [CrossRef]
- Tajti, J.; Szok, D.; Nagy-Grocz, G.; Tuka, B.; Petrovics-Balog, A.; Toldi, J.; Vecsei, L. Kynurenines and PACAP in Migraine: Medicinal Chemistry and Pathogenetic Aspects. Curr. Med. Chem. 2017, 24, 1332–1349. [Google Scholar] [CrossRef] [PubMed]
- Colín-González, A.L.; Aguilera, G.; Santamaría, A. Cannabinoids: Glutamatergic Transmission and Kynurenines. Adv. Neurobiol. 2016, 12, 173–198. [Google Scholar] [CrossRef]
- Nagy-Grócz, G.; Zádor, F.; Dvorácskó, S.; Bohár, Z.; Benyhe, S.; Tömböly, C.; Párdutz, Á.; Vécsei, L. Interactions between the Kynurenine and the Endocannabinoid System with Special Emphasis on Migraine. Int. J. Mol. Sci. 2017, 18, 1617. [Google Scholar] [CrossRef] [PubMed]
- Zubrzycki, M.; Stasiolek, M.; Zubrzycka, M. Opioid and Endocannabinoid System in Orofacial Pain. Physiol. Res. 2019, 68, 705–715. [Google Scholar] [CrossRef]
- Di Marzo, V.; Piscitelli, F. The Endocannabinoid System and its Modulation by Phytocannabinoids. Neurotherapeutics 2015, 12, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Ovsepian, S.V.; Wang, J.; Pickering, M.; Sasse, A.; Aoki, K.R.; Lawrence, G.W.; Dolly, J.O. Activation of TRPV1 Mediates Calcitonin Gene-Related Peptide Release, Which Excites Trigeminal Sensory Neurons and Is Attenuated by a Retargeted Botulinum Toxin with Anti-Nociceptive Potential. J. Neurosci. 2009, 29, 4981–4992. [Google Scholar] [CrossRef]
- Berghe, W.V.; Vermeulen, L.; Delerive, P.; De Bosscher, K.; Staels, B.; Haegeman, G. A Paradigm for Gene Regulation: Inflammation, NF-κB and PPAR. Adv. Exp. Med. Biol. 2003, 544, 181–196. [Google Scholar] [CrossRef]
- Nie, L.; Sun, K.; Gong, Z.; Li, H.; Quinn, J.P.; Wang, M. Src Family Kinases Facilitate the Crosstalk between CGRP and Cytokines in Sensitizing Trigeminal Ganglion via Transmitting CGRP Receptor/PKA Pathway. Cells 2022, 11, 3498. [Google Scholar] [CrossRef]
- Krause, D.N.; Warfvinge, K.; Haanes, K.A.; Edvinsson, L. Hormonal influences in migraine—Interactions of oestrogen, oxytocin and CGRP. Nat. Rev. Neurol. 2021, 17, 621–633. [Google Scholar] [CrossRef]
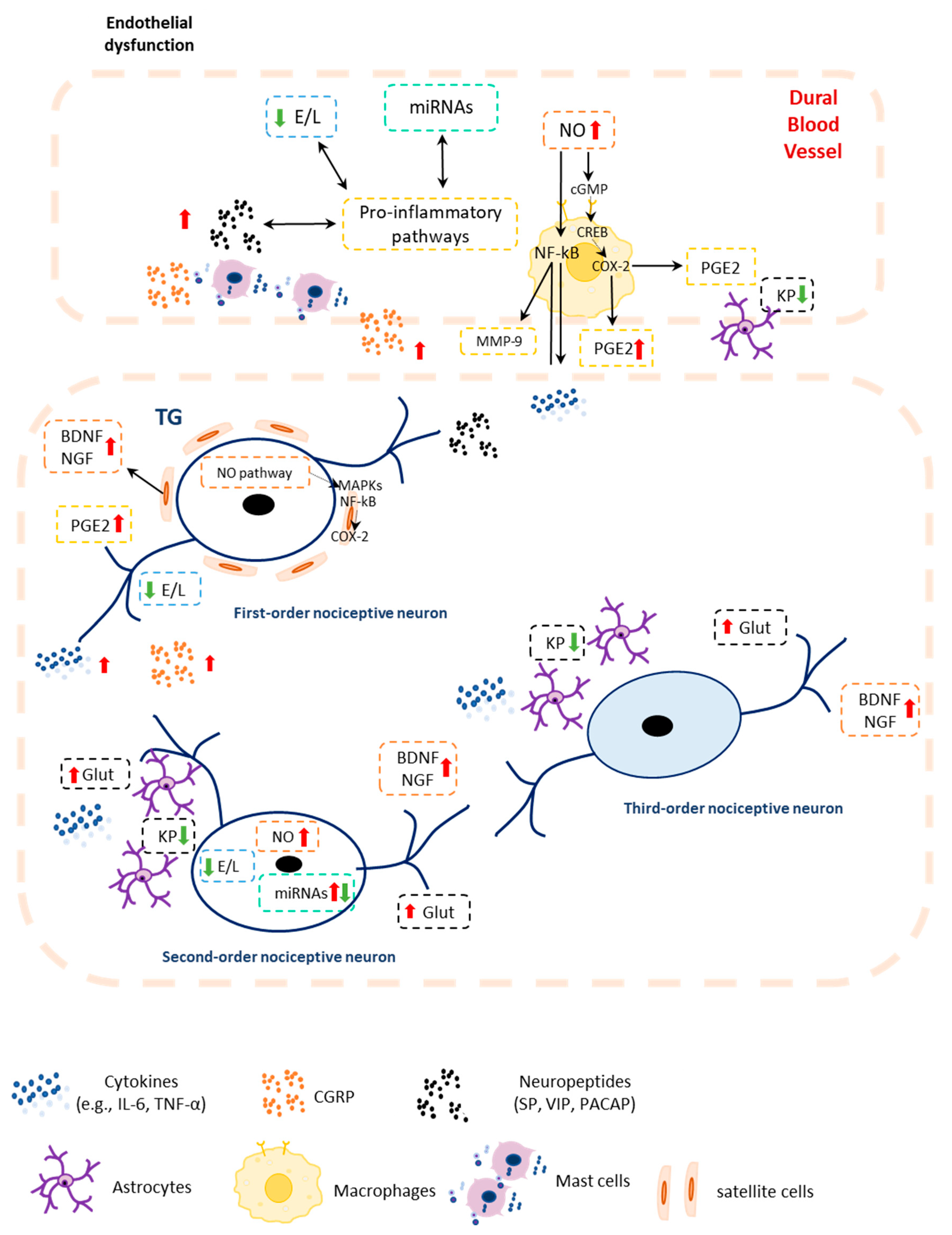
| Biomarkers | Clinical Sample | Preclinical Sample | Clinical Findings | Preclinical Findings | Key Conclusions |
|---|---|---|---|---|---|
| Neuropeptides | |||||
| CGRP | Blood (plasma, serum), Saliva, CSF | Blood (plasma, serum) | ↑ Levels in EM and CM patients during interictal and ictal phases [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,47,48,49,54]; Index of good response to onabotulinumtoxinA treatment and detoxification in CM or MO-CM patients [36,52,65,66,68]; Unchanged levels in EM and CM patients during interictal and ictal phases [42,43,44,45,46,52,63] | ↑ in rodents and cat [55,56,57,58,59,60,61,62] | Potential diagnostic biomarker and potential biomarker for prediction of response to treatments |
| Substance P | Blood (plasma, serum) | Blood (plasma, serum) | ↑ Levels in EM patients during interictal and ictal phases and interictal CM [32,33,79] Unchanged levels in EM patients and HC [80,81] | ↑ levels in rat [62] | |
| PACAP | Blood (plasma, serum) | Blood (plasma) | ↑ Levels in EM patients during interictal and ictal phases [42,86,87,89] or ↓levels in EM patients during interictal phase [87,88]↑ levels in CM patients during interictal phase [42] Unchanged in EM or CM during interictal or vs. HC [42,85] | ↑ levels in rat and cat [57,61,62,90] | Potential Therapeutic Biomarker |
| VIP | Blood (plasma) | Blood (plasma) | ↑Levels EM and CM patients during interictal and ictal phases [31,36,42,65,81,85,86] Correlation with autonomic symptoms [81,94] and cranial parasympathetic symptoms [95] Index of good response to triptan treatment in EM [94] | ↑ levels in rat [61,62] | |
| NPY | Blood (plasma) CSF | Blood (plasma) | ↑ Levels in CSF [100] or ↓ levels in plasma in CM and EM patients during ictal phase migraine patients [102] Unchanged levels in EM patients during ictal and interictal phases and vs. HC [81,101] | ↑ levels in rat [61] | |
| Classic Neurotransmitters | |||||
| Glutamate | Blood (plasma) Saliva CSF | Blood (serum) | ↑ Plasma and salivary levels in EM and CM patients vs. HC during interictal and ictal phase [106,114,115,116,117,118,119] ↑ CSF levels in EM and CM vs. HC during ictal phase [30,120,121] | ↑ levels in rat [122] | |
| Inflammatory Mediators | |||||
| Cytokines | Blood (plasma, serum), CSF | Blood (serum) | ↑ IL-6, TNF-α, IL-1β, TGF-β1 levels in EM patients during interictal phase [132,138,139,140] ↑ IL-6, TNF-α levels in CM patients during ictal and interictal phase [134,144,145] | ↑ IL-6, TNF-α, IL-1β levels in rat [56] | |
| Other Potential Biomarkers | |||||
| Endocannabinoids and related lipids | Blood (platelets, plasma), Saliva, CSF | Data available only for brain areas | ↑ PEA levels in EM patients during ictal phase induced by nitroglycerin [188] ↓ Salivary PEA levels in migraine patients [189] ↓ AEA, 2-AG, and PEA levels in CM and MOH patients [185,186] AEA and related lipid levels unchanged during the interictal phase in EM patients vs. HC [187,188] ↑FAAH and AEA transporter activities in woman EM patients [190] ↓FAAH and the AEA transporter activity in CM and MOH patients [191] | Increased levels of the degrading enzymes FAAH and MAGL [193] | |
| MicroRNAs | Blood (plasma, serum) | Data available only for brain areas | ↑ miR-34a-5p levels in CM during ictal phase and in CM and MOH patients during interictal phase [66,204] ↑miR-382-5p levels CM during ictal phase and CM and MOH patients during interictal phase [66,204] ↓ miR-30 in EM patients [205] ↑ miR-155 in EM patients in interictal phase [206] | ↑ miR-155-5p, miR-34a-5p, and miR-382-5p in several brain areas. Inhibitory effect of a CGRP antagonist [56] | |
| ET-1 | Blood (plasma) | Blood (plasma) | ↑ levels in EM patients in the early stages of the attack [220,221,222,223,224] Conflicting results in interictal phase [221,222,225,226,227] | ↑ or ↓ levels in rodents [108,228] | |
| Tryptophan and Kynurenine Metabolism | Blood (plasma, serum) | CSF | ↓ Levels in EM patients during interictal and ictal phases [110,252] ↓ levels only of kynurenine metabolites in CM patients during interictal phase [254] ↑ levels in EM and CM patients vs. HC during interictal phase [254,255] Unchanged levels in EM patients during interictal phase [253] | ↓ levels in rat [251] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demartini, C.; Francavilla, M.; Zanaboni, A.M.; Facchetti, S.; De Icco, R.; Martinelli, D.; Allena, M.; Greco, R.; Tassorelli, C. Biomarkers of Migraine: An Integrated Evaluation of Preclinical and Clinical Findings. Int. J. Mol. Sci. 2023, 24, 5334. https://doi.org/10.3390/ijms24065334
Demartini C, Francavilla M, Zanaboni AM, Facchetti S, De Icco R, Martinelli D, Allena M, Greco R, Tassorelli C. Biomarkers of Migraine: An Integrated Evaluation of Preclinical and Clinical Findings. International Journal of Molecular Sciences. 2023; 24(6):5334. https://doi.org/10.3390/ijms24065334
Chicago/Turabian StyleDemartini, Chiara, Miriam Francavilla, Anna Maria Zanaboni, Sara Facchetti, Roberto De Icco, Daniele Martinelli, Marta Allena, Rosaria Greco, and Cristina Tassorelli. 2023. "Biomarkers of Migraine: An Integrated Evaluation of Preclinical and Clinical Findings" International Journal of Molecular Sciences 24, no. 6: 5334. https://doi.org/10.3390/ijms24065334
APA StyleDemartini, C., Francavilla, M., Zanaboni, A. M., Facchetti, S., De Icco, R., Martinelli, D., Allena, M., Greco, R., & Tassorelli, C. (2023). Biomarkers of Migraine: An Integrated Evaluation of Preclinical and Clinical Findings. International Journal of Molecular Sciences, 24(6), 5334. https://doi.org/10.3390/ijms24065334







