Blue Light—Ocular and Systemic Damaging Effects: A Narrative Review
Abstract
:1. Introduction
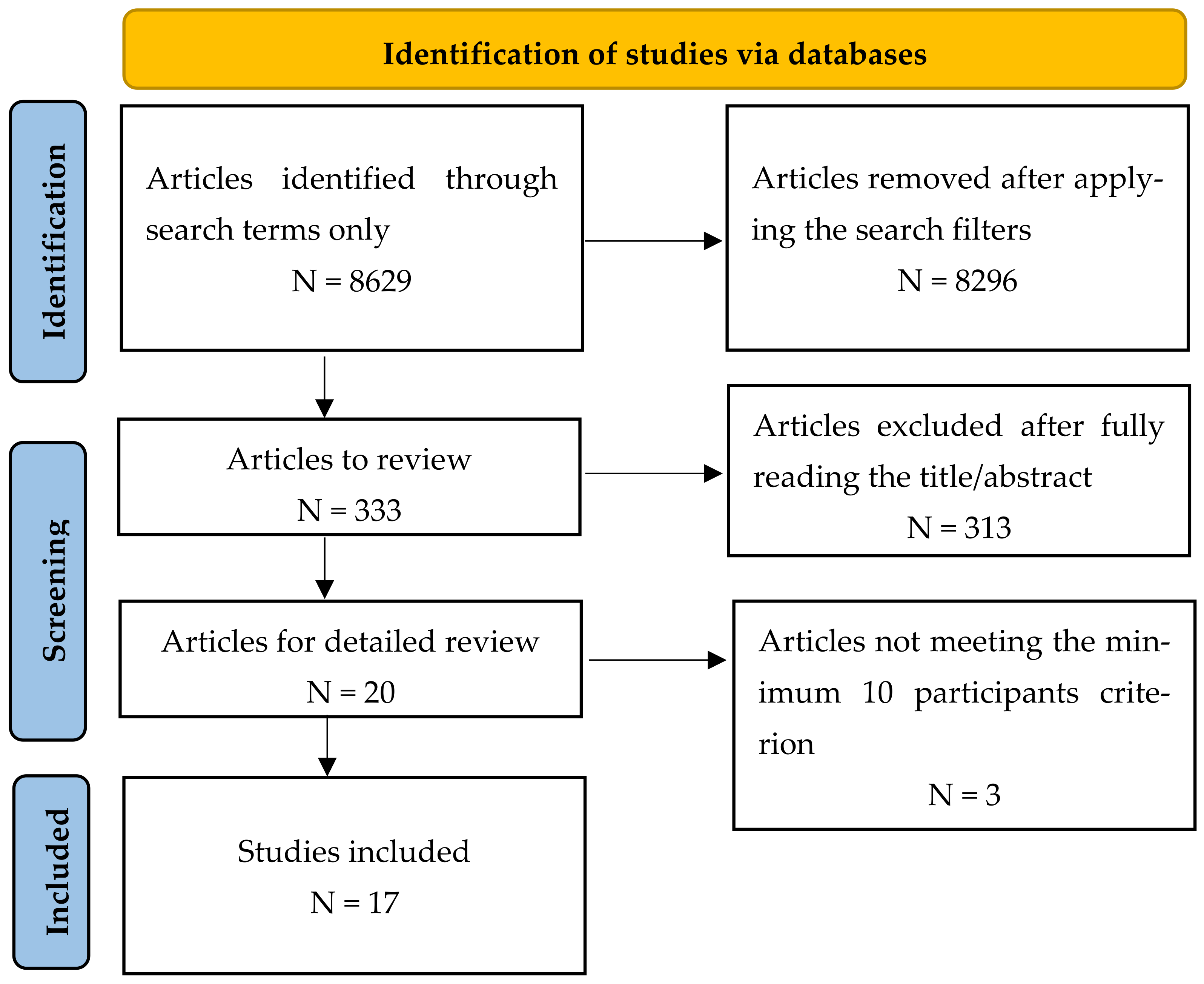
2. Methods
3. Results
4. Discussion
4.1. IOLs and Their Protective Role
4.2. Retinal Electrophysiological Responses to Blue Light
4.3. Systemic Effects of Blue Light
4.3.1. Photophobia and Migraine
4.3.2. Suppression of Vagal Activity Associated with Autonomic and Psychomotor Arousal
5. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Flammer, J.; Mozaffarieh, M.; Bebie, H. Basic Sciences in Ophthalmology: Physics and Chemistry; 2013 Edition; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Gamm, D.M.; Wright, L.S.; Capowski, E.E.; Shearer, R.L.; Meyer, J.S.; Kim, H.J.; Schneider, B.L.; Melvan, J.N.; Svendsen, C.N. Regulation of prenatal human retinal neurosphere growth and cell fate potential by retinal pigment epithelium and Mash1. Stem Cells 2008, 26, 3182–3193. [Google Scholar] [CrossRef] [Green Version]
- Simó, R.; Villarroel, M.; Corraliza, L.; Hernández, C.; Garcia-Ramírez, M. The retinal pigment epithelium: Something more than a constituent of the blood-retinal barrier—Implications for the pathogenesis of diabetic retinopathy. J. Biomed. Biotechnol. 2010, 2010, 190724. [Google Scholar] [CrossRef] [Green Version]
- Roehlecke, C.; Schumann, U.; Ader, M.; Knels, L.; Funk, R.H. Influence of blue light on photoreceptors in a live retinal explant system. Mol. Vis. 2011, 17, 876–884. [Google Scholar]
- Li, X.; Holt, R.R.; Keen, C.L.; Morse, L.S.; You, G.; Hackman, R.M. Goji Berry Intake Increases Macular Pigment Optical Density in Healthy Adults: A Randomized Pilot Trial. Nutrients 2021, 13, 4409. [Google Scholar] [CrossRef]
- Schutt, F.; Bergmann, M.; Holz, F.G.; Kopitz, J. Isolation of intact lysosomes from human RPE cells and effects of A2-E on the integrity of the lysosomal and other cellular membranes. Graefes Arch. Clin. Exp. Ophthalmol. 2002, 240, 983–988. [Google Scholar] [CrossRef] [PubMed]
- Sparrow, J.R.; Vollmer-Snarr, H.R.; Zhou, J.; Jang, Y.P.; Jockusch, S.; Itagaki, Y.; Nakanishi, K. A2E-epoxides damage DNA in retinal pigment epithelial cells. Vitamin E and other antioxidants inhibit A2E-epoxide formation. J. Biol. Chem. 2003, 278, 18207–18213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sparrow, J.R.; Cai, B. Blue light-induced apoptosis of A2E-containing RPE: Involvement of caspase-3 and protection by Bcl-2. Investig. Ophthalmol. Vis. Sci. 2001, 42, 1356–1362. [Google Scholar]
- Sparrow, J.R.; Nakanishi, K.; Parish, C.A. The lipofuscin fluorophore A2E mediates blue light-induced damage to retinal pigmented epithelial cells. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1981–1989. [Google Scholar]
- Leung, T.W.; Li, R.W.; Kee, C.S. Blue-Light Filtering Spectacle Lenses: Optical and Clinical Performances. PLoS ONE 2017, 12, e0169114. [Google Scholar] [CrossRef] [Green Version]
- Yuhas, P.T.; Shorter, P.D.; McDaniel, C.E.; Earley, M.J.; Hartwick, A.T. Blue and Red Light-Evoked Pupil Responses in Photophobic Subjects with TBI. Optom. Vis. Sci. 2017, 94, 108–117. [Google Scholar] [CrossRef]
- Davison, J.A.; Patel, A.S. Light normalizing intraocular lenses. Int. Ophthalmol. Clin. 2005, 45, 55–106. [Google Scholar] [PubMed]
- Pickard, G.E.; Sollars, P.J. Intrinsically photosensitive retinal ganglion cells. Rev. Physiol. Biochem. Pharmacol. 2012, 162, 59–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hattar, S.; Liao, H.W.; Takao, M.; Berson, D.M.; Yau, K.W. Melanopsin-containing retinal ganglion cells: Architecture, projections, and intrinsic photosensitivity. Science 2002, 295, 1065–1070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berson, D.M.; Dunn, F.A.; Takao, M. Phototransduction by retinal ganglion cells that set the circadian clock. Science 2002, 295, 1070–1073. [Google Scholar] [CrossRef] [Green Version]
- Hatori, M.; Panda, S. The emerging roles of melanopsin in behavioral adaptation to light. Trends Mol. Med. 2010, 16, 435–446. [Google Scholar] [CrossRef] [Green Version]
- Bailes, H.J.; Lucas, R.J. Human melanopsin forms a pigment maximally sensitive to blue light (lambda max approximately 479 nm) supporting activation of G(q/11) and G(i/o) signaling cascades. Proc. Biol. Sci. 2013, 280, 20122987. [Google Scholar] [CrossRef] [Green Version]
- Daneault, V.; Dumont, M.; Masse, E.; Vandewalle, G.; Carrier, J. Light-sensitive brain pathways and aging. J. Physiol. Anthropol. 2016, 35, 9. [Google Scholar] [CrossRef] [Green Version]
- Kozaki, T.; Hidaka, Y.; Takakura, J.Y.; Kusano, Y. Suppression of salivary melatonin secretion under 100-Hz flickering and non-flickering blue light. J. Physiol. Anthropol. 2018, 37, 23. [Google Scholar] [CrossRef] [Green Version]
- Katsuura, T.; Lee, S. A review of the studies on nonvisual lighting effects in the field of physiological anthropology. J. Physiol. Anthropol. 2019, 38, 2. [Google Scholar] [CrossRef] [Green Version]
- Yasukouchi, A.; Maeda, T.; Hara, K.; Furuune, H. Non-visual effects of diurnal exposure to an artificial skylight, including nocturnal melatonin suppression. J. Physiol. Anthropol. 2019, 38, 10. [Google Scholar] [CrossRef]
- Lebensohn, J.E. Photophobia: Mechanism and implications. Am. J. Ophthalmol. 1951, 34, 1294–1300. [Google Scholar] [CrossRef] [PubMed]
- Gutrecht, J.A.; Lessell, I.M. Photophobia in trigeminal neuralgia. J. Neuroophthalmol. 1994, 14, 122–123. [Google Scholar] [CrossRef]
- Drummond, P. A quantitative assessment of photophobia in migraine and tension headache. Headache 1986, 26, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Hopkinson, R.G. Glare discomfort and pupil diameter. J. Opt. Soc. Am. 1956, 46, 649–656. [Google Scholar] [CrossRef]
- Okamoto, K.; Tashiro, A.; Chang, Z.; Bereiter, D.A. Bright light activates a trigeminal nociceptive pathway. PAIN 2010, 149, 235–242. [Google Scholar] [CrossRef] [Green Version]
- Digre, K.B.; Brennan, K.C. Shedding light on photophobia. J. Neuroophthalmol. 2012, 32, 68–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noseda, R.; Kainz, V.; Jakubowski, M.; Gooley, J.J.; Saper, C.B.; Digre, K.; Burstein, R. A neural mechanism for exacerbation of headache by light. Nat. Neurosci. 2010, 13, 239–245. [Google Scholar] [CrossRef]
- Lucas, R.J.; Hattar, S.; Takao, M.; Berson, D.M.; Foster, R.G.; Yau, K.W. Diminished pupillary light reflex at high irradiances in melanopsin-knockout mice. Science 2003, 299, 245–247. [Google Scholar] [CrossRef] [Green Version]
- Gamlin, P.D.; McDougal, D.H.; Pokorny, J.; Smith, V.C.; Yau, K.W.; Dacey, D.M. Human and macaque pupil responses driven by melanopsin-containing retinal ganglion cells. Vision. Res. 2007, 47, 946–954. [Google Scholar] [CrossRef] [Green Version]
- Stringham, J.M.; Fuld, K.; Wenzel, A.J. Action spectrum for photophobia. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2003, 20, 1852–1858. [Google Scholar] [CrossRef]
- Stringham, J.M.; Snodderly, D.M. Enhancing performance while avoiding damage: A contribution of macular pigment. Investig. Ophthalmol. Vis. Sci. 2013, 54, 6298–6306. [Google Scholar] [CrossRef] [Green Version]
- Stevens, R.G.; Brainard, G.C.; Blask, D.E.; Lockley, S.W.; Motta, M.E. Adverse health effects of nighttime lighting: Comments on American Medical Association policy statement. Am. J. Prev. Med. 2013, 45, 343–346. [Google Scholar] [CrossRef] [PubMed]
- Stevens, R.G.; Brainard, G.C.; Blask, D.E.; Lockley, S.W.; Motta, M.E. Breast cancer and circadian disruption from electric lighting in the modern world. CA Cancer J. Clin. 2014, 64, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Tosini, G.; Ferguson, I.; Tsubota, K. Effects of blue light on the circadian system and eye physiology. Mol. Vis. 2016, 22, 61–72. [Google Scholar] [PubMed]
- Hatori, M.; Gronfier, C.; Van Gelder, R.N.; Bernstein, P.S.; Carreras, J.; Panda, S.; Marks, F.; Sliney, D.; Hunt, C.E.; Hirota, T.; et al. Global rise of potential health hazards caused by blue light-induced circadian disruption in modern aging societies. NPJ Aging Mech. Dis. 2017, 3, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, B.N.; Johnson, C.D.; Adams, A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. J. Chiropr. Med. 2006, 5, 101–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Pautasso, M. Ten simple rules for writing a literature review. PLoS Comput. Biol. 2013, 9, e1003149. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [Green Version]
- Neumaier-Ammerer, B.; Felke, S.; Hagen, S.; Haas, P.; Zeiler, F.; Mauler, H.; Binder, S. Comparison of visual performance with blue light-filtering and ultraviolet light-filtering intraocular lenses. J. Cataract Refract. Surg. 2010, 36, 2073–2079. [Google Scholar] [CrossRef]
- Kara-Junior, N.; Espindola, R.F.; Gomes, B.A.; Ventura, B.; Smadja, D.; Santhiago, M.R. Effects of blue light-filtering intraocular lenses on the macula, contrast sensitivity, and color vision after a long-term follow-up. J. Cataract Refract. Surg. 2011, 37, 2115–2119. [Google Scholar] [CrossRef] [PubMed]
- Nagai, H.; Hirano, Y.; Yasukawa, T.; Morita, H.; Nozaki, M.; Wolf-Schnurrbusch, U.; Wolf, S.; Ogura, Y. Prevention of increased abnormal fundus autofluorescence with blue light-filtering intraocular lenses. J. Cataract Refract. Surg. 2015, 41, 1855–1859. [Google Scholar] [CrossRef]
- Ayaki, M.; Negishi, K.; Suzukamo, Y.; Tsubota, K. Color of intra-ocular lens and cataract type are prognostic determinants of health indices after visual and photoreceptive restoration by surgery. Rejuvenation Res. 2015, 18, 145–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokuno, K.; Asami, T.; Nonobe, N.; Ito, H.; Fujiwara, K.; Terasaki, H. Effect of blue light-filtering intraocular lens on color vision in patients with macular diseases after vitrectomy. Int. Ophthalmol. 2016, 36, 829–839. [Google Scholar] [CrossRef]
- Gagné, A.M.; Lévesque, F.; Gagné, P.; Hébert, M. Impact of blue vs red light on retinal response of patients with seasonal affective disorder and healthy controls. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2011, 35, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Morita, Y.; Jounai, K.; Miyake, M.; Inaba, M.; Kanauchi, O. Effect of Heat-Killed Lactobacillus paracasei KW3110 Ingestion on Ocular Disorders Caused by Visual Display Terminal (VDT) Loads: A Randomized, Double-Blind, Placebo-Controlled Parallel-Group Study. Nutrients 2018, 10, 1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.; Zhang, M.; Wang, D.; Dong, G.; Chen, Z.; Li, S.; Sun, X.; Zeng, M.; Liao, H.; Chen, H.; et al. Blue Light from Cell Phones Can Cause Chronic Retinal Light Injury: The Evidence from a Clinical Observational Study and a SD Rat Model. Biomed. Res. Int. 2021, 2021, 3236892. [Google Scholar] [CrossRef]
- Hoggan, R.N.; Subhash, A.; Blair, S.; Digre, K.B.; Baggaley, S.K.; Gordon, J.; Brennan, K.C.; Warner, J.E.; Crum, A.V.; Katz, B.J. Thin-film optical notch filter spectacle coatings for the treatment of migraine and photophobia. J. Clin. Neurosci. 2016, 28, 71–76. [Google Scholar] [CrossRef] [Green Version]
- Yuda, E.; Ogasawara, H.; Yoshida, Y.; Hayano, J. Suppression of vagal cardiac modulation by blue light in healthy subjects. J. Physiol. Anthropol. 2016, 35, 24. [Google Scholar] [CrossRef] [Green Version]
- Yuda, E.; Ogasawara, H.; Yoshida, Y.; Hayano, J. Enhancement of autonomic and psychomotor arousal by exposures to blue wavelength light: Importance of both absolute and relative contents of melanopic component. J. Physiol. Anthropol. 2017, 36, 13. [Google Scholar] [CrossRef] [Green Version]
- Zivcevska, M.; Lei, S.; Blakeman, A.; Goltz, H.C.; Wong, A.M.F. A Novel Visual Psychometric Test for Light-Induced Discomfort Using Red and Blue Light Stimuli Under Binocular and Monocular Viewing Conditions. Investig. Ophthalmol. Vis. Sci. 2018, 59, 1467–1474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vieira, A.; van der Linde, I.; Bright, P.; Wilkins, A. Preference for Lighting Chromaticity in Migraine With Aura. Headache 2020, 60, 1124–1131. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, E.A.; McAdams, H.; Igdalova, A.; Haggerty, E.B.; Cucchiara, B.L.; Brainard, D.H.; Aguirre, G.K. Reflexive Eye Closure in Response to Cone and Melanopsin Stimulation: A Study of Implicit Measures of Light Sensitivity in Migraine. Neurology 2021, 97, e1672–e1680. [Google Scholar] [CrossRef]
- Ali, E.N.; Carle, C.F.; Lueck, C.J.; Kolic, M.; Maddess, T. Assessing migraine patients with multifocal pupillographic objective perimetry. BMC Neurol. 2021, 21, 211. [Google Scholar] [CrossRef]
- Zele, A.J.; Dey, A.; Adhikari, P.; Feigl, B. Melanopsin hypersensitivity dominates interictal photophobia in migraine. Cephalalgia 2021, 41, 217–226. [Google Scholar] [CrossRef]
- Downie, L.E.; Busija, L.; Keller, P.R. Blue-light filtering intraocular lenses (IOLs) for protecting macular health. Cochrane Database Syst. Rev. 2018, 5, CD011977. [Google Scholar] [CrossRef] [PubMed]
- Mainster, M.A.; Turner, P.L. Blue-blocking IOLs decrease photoreception without providing significant photoprotection. Surv. Ophthalmol. 2010, 55, 272–289. [Google Scholar] [CrossRef] [PubMed]
- Algvere, P.V.; Marshall, J.; Seregard, S. Age-related maculopathy and the impact of blue light hazard. Acta Ophthalmol. Scand. 2006, 84, 4–15. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1600-0420.2005.00627.x?sid=nlm%3Apubmed (accessed on 10 February 2023). [CrossRef] [PubMed]
- Sparrow, J.R.; Miller, A.S.; Zhou, J. Blue light-absorbing intraocular lens and retinal pigment epithelium protection in vitro. J. Cataract Refract. Surg. 2004, 30, 873–878. [Google Scholar] [CrossRef]
- Boulton, M.; Dontsov, A.; Jarvis-Evans, J.; Ostrovsky, M.; Svistunenko, D. Lipofuscin is a photoinducible free radical generator. J. Photochem. Photobiol. B Biol. 1993, 19, 201–204. [Google Scholar] [CrossRef]
- Rózanowska, M.; Wessels, J.; Boulton, M.; Burke, J.M.; Rodgers, M.A.; Truscott, T.G.; Sarna, T. Blue light-induced singlet oxygen generation by retinal lipofuscin in non-polar media. Free Radic. Biol. Med. 1998, 24, 1107–1112. [Google Scholar] [CrossRef] [PubMed]
- Yanagi, Y.; Inoue, Y.; Iriyama, A.; Jang, W.-D. Effects of yellow intraocular lenses on light-induced upregulation of vascular endothelial growth factor. J. Cataract Refract. Surg. 2006, 32, 1540–1544. [Google Scholar] [CrossRef] [PubMed]
- Obana, A.; Tanito, M.; Gohto, Y.; Gellermann, W.; Okazaki, S.; Ohira, A. Macular pigment changes in pseudophakic eyes quantified with resonance Raman spectroscopy. Ophthalmology 2011, 118, 1852–1858. [Google Scholar] [CrossRef] [PubMed]
- Chew, E.Y.; Sperduto, R.D.; Milton, R.C.; Clemons, T.E.; Gensler, G.R.; Bressler, S.B.; Klein, R.; Klein, B.E.; Ferris, F.L., 3rd. Risk of advanced age-related macular degeneration after cataract surgery in the Age-Related Eye Disease Study: AREDS report 25. Ophthalmology 2009, 116, 297–303. [Google Scholar] [CrossRef] [Green Version]
- Murata, K.; Araki, S.; Kawakami, N.; Saito, Y.; Hino, E. Central nervous system effects and visual fatigue in VDT workers. Int. Arch. Occup. Environ. Health 1991, 63, 109–113. [Google Scholar] [CrossRef]
- Murata, K.; Araki, S.; Yokoyama, K.; Yamashita, K.; Okumatsu, T.; Sakou, S. Accumulation of VDT work-related visual fatigue assessed by visual evoked potential, near point distance and critical flicker fusion. Ind. Health 1996, 34, 61–69. [Google Scholar] [CrossRef] [Green Version]
- Mankowska, N.D.; Marcinkowska, A.B.; Waskow, M.; Sharma, R.I.; Kot, J.; Winklewski, P.J. Critical Flicker Fusion Frequency: A Narrative Review. Medicina 2021, 57, 1096. [Google Scholar] [CrossRef]
- Krigel, A.; Berdugo, M.; Picard, E.; Levy-Boukris, R.; Jaadane, I.; Jonet, L.; Dernigoghossian, M.; Andrieu-Soler, C.; Torriglia, A.; Behar-Cohen, F. Light-induced retinal damage using different light sources, protocols and rat strains reveals LED phototoxicity. Neuroscience 2016, 339, 296–307. [Google Scholar] [CrossRef] [Green Version]
- Vicente-Tejedor, J.; Marchena, M.; Ramírez, L.; García-Ayuso, D.; Gómez-Vicente, V.; Sánchez-Ramos, C.; de la Villa, P.; Germain, F. Removal of the blue component of light significantly decreases retinal damage after high intensity exposure. PLoS ONE 2018, 13, e0194218. [Google Scholar] [CrossRef]
- Yuan, D.; Collage, R.D.; Huang, H.; Zhang, X.; Kautza, B.C.; Lewis, A.J.; Zuckerbraun, B.S.; Tsung, A.; Angus, D.C.; Rosengart, M.R. Blue light reduces organ injury from ischemia and reperfusion. Proc. Natl. Acad. Sci. USA 2016, 113, 5239–5244. [Google Scholar] [CrossRef] [Green Version]
- Perenboom, M.J.L.; Zamanipoor Najafabadi, A.H.; Zielman, R.; Carpay, J.A.; Ferrari, M.D. Quantifying visual allodynia across migraine subtypes: The Leiden visual sensitivity scale. PAIN 2018, 159, 2375–2382. [Google Scholar] [CrossRef] [PubMed]
- Mulleners, W.M.; Aurora, S.K.; Chronicle, E.P.; Stewart, R.; Gopal, S.; Koehler, P.J. Self-reported photophobic symptoms in migraineurs and controls are reliable and predict diagnostic category accurately. Headache 2001, 41, 31–39. [Google Scholar] [CrossRef]
- Datta, R.; Aguirre, G.K.; Hu, S.; Detre, J.A.; Cucchiara, B. Interictal cortical hyperresponsiveness in migraine is directly related to the presence of aura. Cephalalgia 2013, 33, 365–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chong, C.D.; Starling, A.J.; Schwedt, T.J. Interictal photosensitivity associates with altered brain structure in patients with episodic migraine. Cephalalgia 2016, 36, 526–533. [Google Scholar] [CrossRef] [PubMed]
- Drummond, P.D.; Woodhouse, A. Painful stimulation of the forehead increases photophobia in migraine sufferers. Cephalalgia 1993, 13, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Vanagaite, J.; Pareja, J.A.; Storen, O.; White, L.R.; Sand, T.; Stovner, L.J. Light-induced discomfort and pain in migraine. Cephalalgia 1997, 17, 733–741. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, A.J.; Nimmo-Smith, I.; Slater, A.I.; Bedocs, L. Fluorescent lighting, headaches and eyestrain. Light. Res. Technol. 1989, 21, 11–18. [Google Scholar] [CrossRef]
- Goadsby, P.J.; Lipton, R.B.; Ferrari, M.D. Migraine-current understanding and treatment. N. Engl. J. Med. 2002, 346, 257–270. [Google Scholar] [CrossRef] [Green Version]
- Cajochen, C.; Munch, M.; Kobialka, S.; Krauchi, K.; Steiner, R.; Oelhafen, P.; Orgul, S.; Wirz-Justice, A. High sensitivity of human melatonin, alertness, thermoregulation, and heart rate to short wavelength light. J. Clin. Endocrinol. Metab. 2005, 90, 1311–1316. [Google Scholar] [CrossRef] [Green Version]
- Chellappa, S.L.; Steiner, R.; Blattner, P.; Oelhafen, P.; Gotz, T.; Cajochen, C. Non-visual effects of light on melatonin, alertness and cognitive performance: Can blue-enriched light keep us alert? PLoS ONE 2011, 6, e16429. [Google Scholar] [CrossRef]
- Drummond, P.D. Photophobia and autonomic responses to facial pain in migraine. Brain 1997, 120, 1857–1864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boulloche, N.; Denuelle, M.; Payoux, P.; Fabre, N.; Trotter, Y.; Geraud, G. Photophobia in migraine: An interictal PET study of cortical hyperexcitability and its modulation by pain. J. Neurol. Neurosurg. Psychiatry 2010, 81, 978–984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kowacs, P.A.; Piovesan, E.J.; Werneck, L.C.; Tatsui, C.E.; Lange, M.C.; Ribas, L.C.; da Silva, H.P. Influence of intense light stimulation on trigeminal and cervical pain perception thresholds. Cephalalgia 2001, 21, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Matynia, A.; Nguyen, E.; Sun, X.; Blixt, F.W.; Parikh, S.; Kessler, J.; Pérez de Sevilla Müller, L.; Habib, S.; Kim, P.; Wang, Z.Z.; et al. Peripheral sensory neurons expressing melanopsin respond to light. Front. Neural Circuits 2016, 10, 60. [Google Scholar] [CrossRef] [Green Version]
- Delwig, A.; Chaney, S.Y.; Bertke, A.S.; Verweij, J.; Quirce, S.; Larsen, D.D.; Yang, C.; Buhr, E.; VAN Gelder, R.; Gallar, J.; et al. Melanopsin expression in the cornea. Vis. Neurosci. 2018, 35, E004. [Google Scholar] [CrossRef]
- Lei, S.; Zivcevska, M.; Goltz, H.C.; Chen, X.; Wong, A.M.F. Ocular Topical Anesthesia Does Not Attenuate Light-Induced Discomfort Using Blue and Red Light Stimuli. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4714–4719. [Google Scholar] [CrossRef] [Green Version]
- Good, P.A.; Taylor, R.H.; Mortimer, M.J. The use of tinted glasses in childhood migraine. Headache 1991, 31, 533–536. [Google Scholar] [CrossRef]
- Waddell, P.A.; Gronwall, D.M. Sensitivity to light and sound following minor head injury. Acta Neurol. Scand. 1984, 69, 270–276. [Google Scholar] [CrossRef]
- Jonsson, C.O.; Lidvall, H.; Ma¨lhammar, G. An exploratory psychological study of the post-traumatic cerebral syndrome. Acta Neurol. Scand. 1967, 43, 158–166. [Google Scholar] [CrossRef]
- Kapoor, N.; Ciuffreda, K.J. Vision disturbances following traumatic brain Injury. Curr. Treat. Options Neurol. 2002, 4, 271–280. [Google Scholar] [CrossRef]
- Alvarez, T.L.; Kim, E.H.; Vicci, V.R.; Dhar, S.K.; Biswal, B.B.; Barrett, A.M. Concurrent vision dysfunctions in convergence insufficiency with traumatic brain injury. Optom. Vis. Sci. 2012, 89, 1740–1751. [Google Scholar] [CrossRef] [PubMed]
- Goodrich, G.L.; Flyg, H.M.; Kirby, J.E.; Chang, C.Y.; Martinsen, G.L. Mechanisms of TBI and visual consequences in military and veteran populations. Optom. Vis. Sci. 2013, 90, 105–112. [Google Scholar] [CrossRef] [Green Version]
- Capo’-Aponte, J.E.; Urosevich, T.G.; Temme, L.A.; Tarbett, A.K.; Sanghera, N.K. Visual dysfunctions and symptoms during the subacute stage of blast-induced mild traumatic brain injury. Mil. Med. 2012, 177, 804–813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lei, S.; Goltz, H.C.; Chandrakumar, M.; Wong, A.M. Full-field chromatic pupillometry for the assessment of the postillumination pupil response driven by melanopsin-containing retinal ganglion cells. Investig. Ophthalmol. Vis. Sci. 2014, 55, 4496–4503. [Google Scholar] [CrossRef] [Green Version]
- Lei, S.; Goltz, H.C.; Chandrakumar, M.; Wong, A.M. Test–retest reliability of hemifield, central-field, and full-field chromatic pupillometry for assessing the function of melanopsin-containing retinal ganglion cells. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1267–1273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flannagan, M.J.; Sivak, M.; Ensing, M.; Simmons, C. Effect of wavelength on discomfort glare from monochromatic sources. In Technical Report UMTRI-89-30; University of Michigan Transportation Research Institute: Ann Arbor, MI, USA, 1989; pp. 1–20. Available online: https://deepblue.lib.umich.edu/bitstream/handle/2027.42/64064/78939.pdf?sequence=1&isAllowed=y (accessed on 10 February 2023).
- Aldrich, A.; Hibbard, P.B.; Wilkins, A.J. Vision and hyper-responsiveness in migraine. Vision 2019, 3, 62. [Google Scholar] [CrossRef] [Green Version]
- Hackley, S.A.; Johnson, L.N. Distinct early and late subcomponents of the photic blink reflex: Response characteristics in patients with retrogeniculate lesions. Psychophysiology 1996, 33, 239–251. [Google Scholar] [CrossRef]
- Rimpel, J.; Geyer, D.; Hopf, H.C. Changes in the blink responses to combined trigeminal, acoustic and visual repetitive stimulation, studied in the human subject. Electroencephalogr. Clin. Neurophysiol. 1982, 54, 552–560. [Google Scholar] [CrossRef]
- Zele, A.J.; Dey, A.; Adhikari, P.; Feigl, B. Rhodopsin and melanopsin contributions to human brightness estimation. J. Opt. Soc. Am. A 2020, 37, A145–A153. [Google Scholar] [CrossRef]
- Park, J.C.; Moura, A.L.; Raza, A.S.; Rhee, D.W.; Kardon, R.H.; Hood, D.C. Toward a clinical protocol for assessing rod, cone, and melanopsin contributions to the human pupil response. Investig. Ophthalmol. Vis. Sci. 2011, 52, 6624–6635. [Google Scholar] [CrossRef] [Green Version]
- McDougal, D.H.; Gamlin, P.D. The influence of intrinsically-photosensitive retinal ganglion cells on the spectral sensitivity and response dynamics of the human pupillary light reflex. Vis. Res. 2010, 50, 72–87. [Google Scholar] [CrossRef] [Green Version]
- Herbst, K.; Sander, B.; Lund-Andersen, H.; Broendsted, A.E.; Kessel, L.; Hansen, M.S.; Kawasaki, A. Intrinsically photosensitive retinal ganglion cell function in relation to age: A pupillometric study in humans with special reference to the age-related optic properties of the lens. BMC Ophthalmol. 2012, 12, 4. [Google Scholar] [CrossRef] [Green Version]
- McKendrick, A.M.; Badcock, D.R. Decreased visual field sensitivity measured 1 day, then 1 week, after migraine. Investig. Ophthalmol. Vis. Sci. 2004, 45, 1061–1070. [Google Scholar] [CrossRef] [Green Version]
- McKendrick, A.M.; Badcock, D.R. An analysis of the factors associated with visual field deficits measured with flickering stimuli in-between migraine. Cephalalgia 2004, 24, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.F.; Guo, H.; Huang, J.H.; Yu, J.G.; Yuan, F. Retinal nerve fiber layer thickness changes in migraine: A meta-analysis of case-control studies. Curr. Eye Res. 2016, 41, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Cambron, M.; Maertens, H.; Paemeleire, K.; Crevits, L. Autonomic function in migraine patients: Ictal and interictal pupillometry. Headache 2013, 54, 655–662. [Google Scholar] [CrossRef] [PubMed]
- Marcus, D.A.; Soso, M.J. Migraine and stripe-induced visual discomfort. Arch. Neurol. 1989, 46, 1129–1132. [Google Scholar] [CrossRef] [PubMed]
- Yasukouchi, A.; Ishibashi, K. Non-visual effects of the color temperature of fluorescent lamps on physiological aspects in humans. J. Physiol. Anthropol. Appl. Hum. Sci. 2005, 24, 41–43. [Google Scholar] [CrossRef] [Green Version]
- Litscher, D.; Wang, L.; Gaischek, I.; Litscher, G. The influence of new colored light stimulation methods on heart rate variability, temperature, and wellbeing: Results of a pilot study in humans. Evid.-Based Complement. Altern. Med. 2013, 2013, 674183. [Google Scholar] [CrossRef] [Green Version]
- Hayano, J.; Sakakibara, Y.; Yamada, A.; Yamada, M.; Mukai, S.; Fujinami, T.; Yokoyama, K.; Watanabe, Y.; Takata, K. Accuracy of assessment of cardiac vagal tone by heart rate variability in normal subjects. Am. J. Cardiol. 1991, 67, 199–204. [Google Scholar] [CrossRef]
- Pomeranz, B.; Macaulay, R.J.B.; Caudill, M.A.; Kutz, I.; Adam, D.; Gordon, D.; Kilborn, K.M.; Barger, A.C.; Shannon, D.C.; Cohen, R.J.; et al. Assessment of autonomic function in humans by heart rate spectral analysis. Am. J. Physiol. 1985, 248, H151-3. [Google Scholar] [CrossRef] [PubMed]
- Hayano, J.; Yasuma, F.; Okada, A.; Mukai, S.; Fujinami, T. Respiratory sinus arrhythmia. A phenomenon improving pulmonary gas exchange and circulatory efficiency. Circulation 1996, 94, 842–847. [Google Scholar] [CrossRef] [PubMed]
- Yuda, E.; Yoshida, Y.; Ueda, N.; Hayano, J. Difference in autonomic nervous effect of blue light depending on the angle of incidence on the eye. BMC Res. Notes 2020, 13, 141. [Google Scholar] [CrossRef] [PubMed]
- Lasko, T.A.; Kripke, D.F.; Elliot, J.A. Melatonin suppression by illumination of upper and lower visual fields. J. Biol. Rhythms 1999, 14, 122–125. [Google Scholar] [CrossRef]
- Glickman, G.; Hanifin, J.P.; Rollag, M.D.; Wang, J.; Cooper, H.; Brainard, G.C. Inferior retinal light exposure is more effective than superior retinal exposure in suppressing melatonin in humans. J. Biol. Rhythms 2003, 18, 71–79. [Google Scholar] [CrossRef]
| Year | Title | Authors | Subjects (Eyes with Yellow/Clear IOL) | Element of Study | Primary Endpoint | Type of Study | Maximum Follow-Up | Outcome |
|---|---|---|---|---|---|---|---|---|
| 2010 | Comparison of visual performance with blue light-filtering and ultraviolet light-filtering intraocular lenses | Neumaier-Ammerer et al. [41] | 76 (37/39) | Cones and rods | VA, CS, Color vision | Prospective, randomized, double-blind control trial | 2 months | Negative: no difference between tested parameters (except for color vision) |
| 2011 | Effects of blue light-filtering intraocular lenses on the macula, contrast sensitivity, and color vision after a long-term follow-up | Kara-Junior et al. [42] | 25 (25/25) | Cones and rods | CS, Color vision, OCT Ophthalmoscopy | Prospective randomized control trial | 5 years | Negative: no differences between tested parameters |
| 2015 | Prevention of increased abnormal fundus autofluorescence with blue light-filtering intraocular lenses | Nagai et al. [43] | 131 (52/79) | RPE cells | FAF | Prospective comparative observational study | 2 years | Positive: Lower FAF abnormalities and AMD incidence in the yellow-tinted IOL group |
| 2015 | Color of Intra-Ocular Lens and Cataract Type Are Prognostic Determinants of Health Indices After Visual and Photoreceptive Restoration by Surgery | Ayaki et al. [44] | 206 (135/71) | Cones and rods | Japanese versions of: VFQ-25 PSQI | Prospective comparative observational study | 7 months | Positive: improvement of VFQ-25 (yellow-tinted IOL) and PSQI (clear IOL) |
| 2016 | Effect of blue light-filtering intraocular lens on color vision in patients with macular diseases after vitrectomy | Mokuno et al. [45] | 67 (27/40) | Cones and rods | Color vision | Prospective comparative observational study | 16 months | Negative: no differences between study groups |
| Year | Title | Authors | Subjects | Element of Study | Primary Endpoint | Type of Study | Outcome |
|---|---|---|---|---|---|---|---|
| 2011 | Impact of blue vs. red light on retinal response of patients with seasonal affective disorder and healthy controls | Gagné et al. [46] | 20 | Cones and rods | ERG | Prospective controlled study | Positive: blue light decreases maximal ERG response |
| 2018 | Effect of Heat-Killed Lactobacillus paracasei KW3110 Ingestion on Ocular Disorders Caused by Visual Display Terminal (VDT) Loads: A Randomized, Double-Blind, Placebo-Controlled Parallel-Group Study | Morita et al. [47] | 62 | Cones and rods | CFF, VAS, CS | Prospective, randomized, controlled study | Neutral: significant improvement 4 weeks after intake, but not during the 8th week |
| 2021 | Blue Light from Cell Phones Can Cause Chronic Retinal Light Injury: The Evidence from a Clinical Observational Study and a SD Rat Model | Li et al. [48] | 25 | Cones and rods | mfERG | Prospective, randomized, controlled study | Positive: reduced amplitude of parafoveal regions |
| Year | Title | Authors | Subjects | Element of Study | Primary Endpoint | Type of Study | Outcome |
|---|---|---|---|---|---|---|---|
| 2016 | Thin-film optical notch filter spectacle coatings for the treatment of migraine and photophobia | Hoggan et al. [49] | 48 | ipRGC | Headache impact using HIT-6 | Randomized, double-masked, crossover | Positive: Reduction in HIT-6 score + Unexpected result for the 620 nm lenses |
| 2016 | Suppression of vagal cardiac modulation by blue light in healthy subjects | Yuda et al. [50] | 12 | ipRGC | HRV indices—HF, LF/HF | Open-label, Non-Controlled Trial | Positive: Lower HF (greatest with blue light) and increased LF/HF |
| 2017 | Enhancement of autonomic and psychomotor arousal by exposures to blue wavelength light: importance of both absolute and relative contents of melanopic component | Yuda et al. [51] | 10 | ipRGC | Heart rate, HRV indices (HF, LF/HF) + performance of PVT | Open-label, Non-Controlled Trial |
Positive: lower heart rate, HF, and reaction time, but no difference in LF/HF |
| 2017 | Blue and Red Light-Evoked Pupil Responses in Photophobic Subjects with TBI | Yuhas et al. [11] | 36 | ipRGC | Pupil fluctuation | Open-label, Non-Controlled Trial | Negative: no differences between groups regarding blue light |
| 2018 | A Novel Visual Psychometric Test for Light-Induced Discomfort Using Red and Blue Light Stimuli Under Binocular and Monocular Viewing Conditions | Zivcevska et al. [52] | 11 | ipRGC | Light discomfort thresholds | Open-label, Non-Controlled Trial | Positive: greater discomfort for blue light under both monocular and binocular stimulation |
| 2020 | Preference for Lighting Chromaticity in Migraine with Aura | Vieira et al. [53] | 54 | ipRGC | Visual search task | Cross-sectional laboratory study | Positive: visual search time decreased |
| 2021 | Reflexive Eye Closure in Response to Cone and Melanopsin Stimulation: A Study of Implicit Measures of Light Sensitivity in Migraine | Kaiser et al. [54] | 60 | ipRGC | OO-EMG, VDS | Non-Randomized Controlled Trial | Positive: greater OO-EMG activity and visual discomfort for migraineurs |
| 2021 | Assessing migraine patients with multifocal pupillographic objective perimetry | Ali et al. [55] | 62 | ipRGC | Migraine headache diary, mfPOP | Randomized, open-label, crossover | Negative: no differences between used protocols and study groups for the first two aims. Moderate changes for the yellow protocol about their third aim |
| 2021 | Melanopsin hypersensitivity dominates interictal photophobia in migraine | Zele et al. [56] | 23 | ipRGC | EMG, Pupillometry | Non-Randomized Controlled Trial | Positive: lower EMG thresholds and higher PIPR in blue and green light settings |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antemie, R.-G.; Samoilă, O.C.; Clichici, S.V. Blue Light—Ocular and Systemic Damaging Effects: A Narrative Review. Int. J. Mol. Sci. 2023, 24, 5998. https://doi.org/10.3390/ijms24065998
Antemie R-G, Samoilă OC, Clichici SV. Blue Light—Ocular and Systemic Damaging Effects: A Narrative Review. International Journal of Molecular Sciences. 2023; 24(6):5998. https://doi.org/10.3390/ijms24065998
Chicago/Turabian StyleAntemie, Răzvan-Geo, Ovidiu Ciprian Samoilă, and Simona Valeria Clichici. 2023. "Blue Light—Ocular and Systemic Damaging Effects: A Narrative Review" International Journal of Molecular Sciences 24, no. 6: 5998. https://doi.org/10.3390/ijms24065998
APA StyleAntemie, R.-G., Samoilă, O. C., & Clichici, S. V. (2023). Blue Light—Ocular and Systemic Damaging Effects: A Narrative Review. International Journal of Molecular Sciences, 24(6), 5998. https://doi.org/10.3390/ijms24065998








