The Potential Benefits of Quercetin for Brain Health: A Review of Anti-Inflammatory and Neuroprotective Mechanisms
Abstract
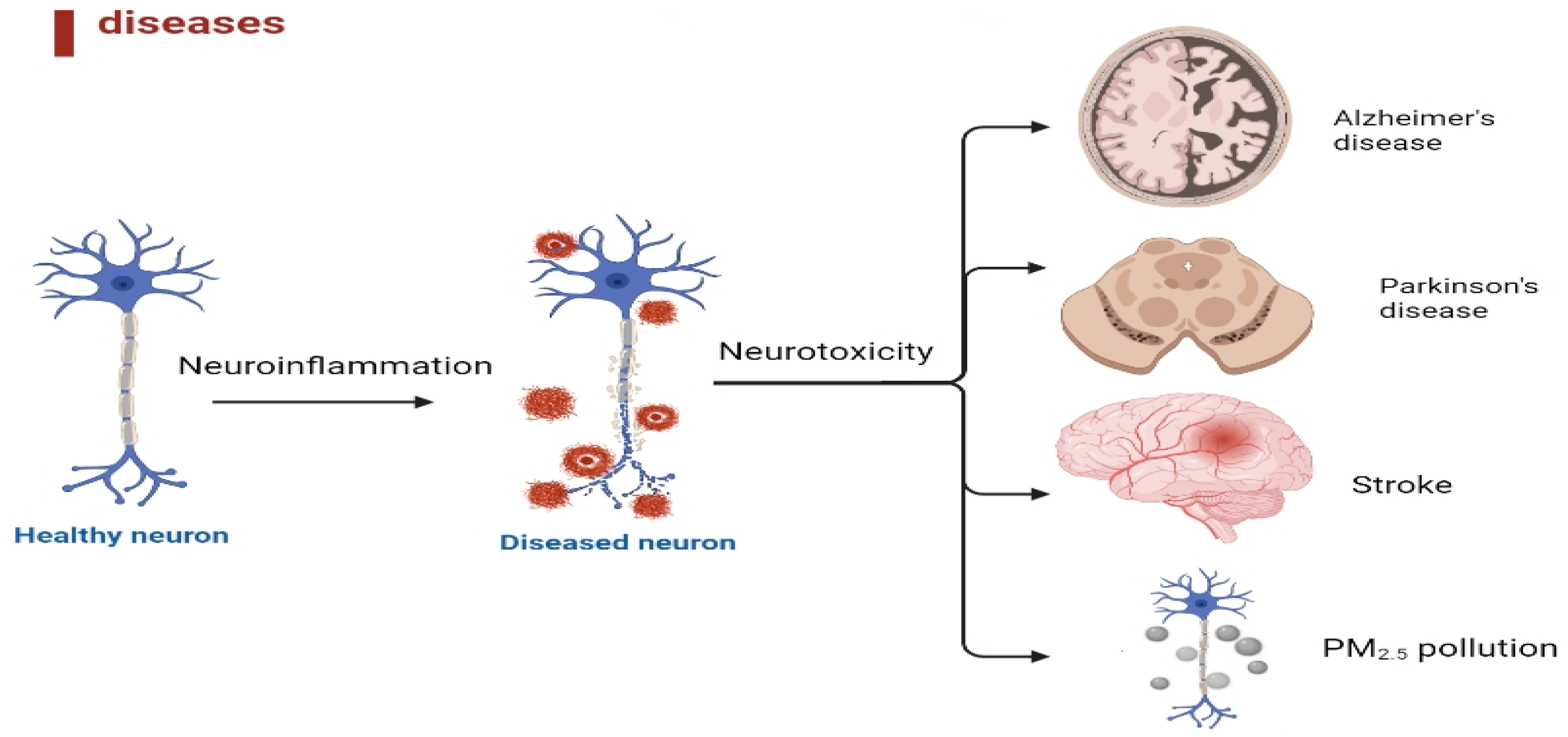
1. Neuroinflammation Toxicity and Neuroprotection
1.1. Neuroinflammation Plays a Crucial Role in the Pathological Processes in the Brain
1.2. Inflammation Can Alter Cellular Functions in a Variety of Ways
1.3. The Pathophysiology of Neuroinflammatory Toxicity in Neurodegenerative Diseases, Stroke, and the Role of PM2.5 Pollution Is a Complex and Multi-Factorial Process
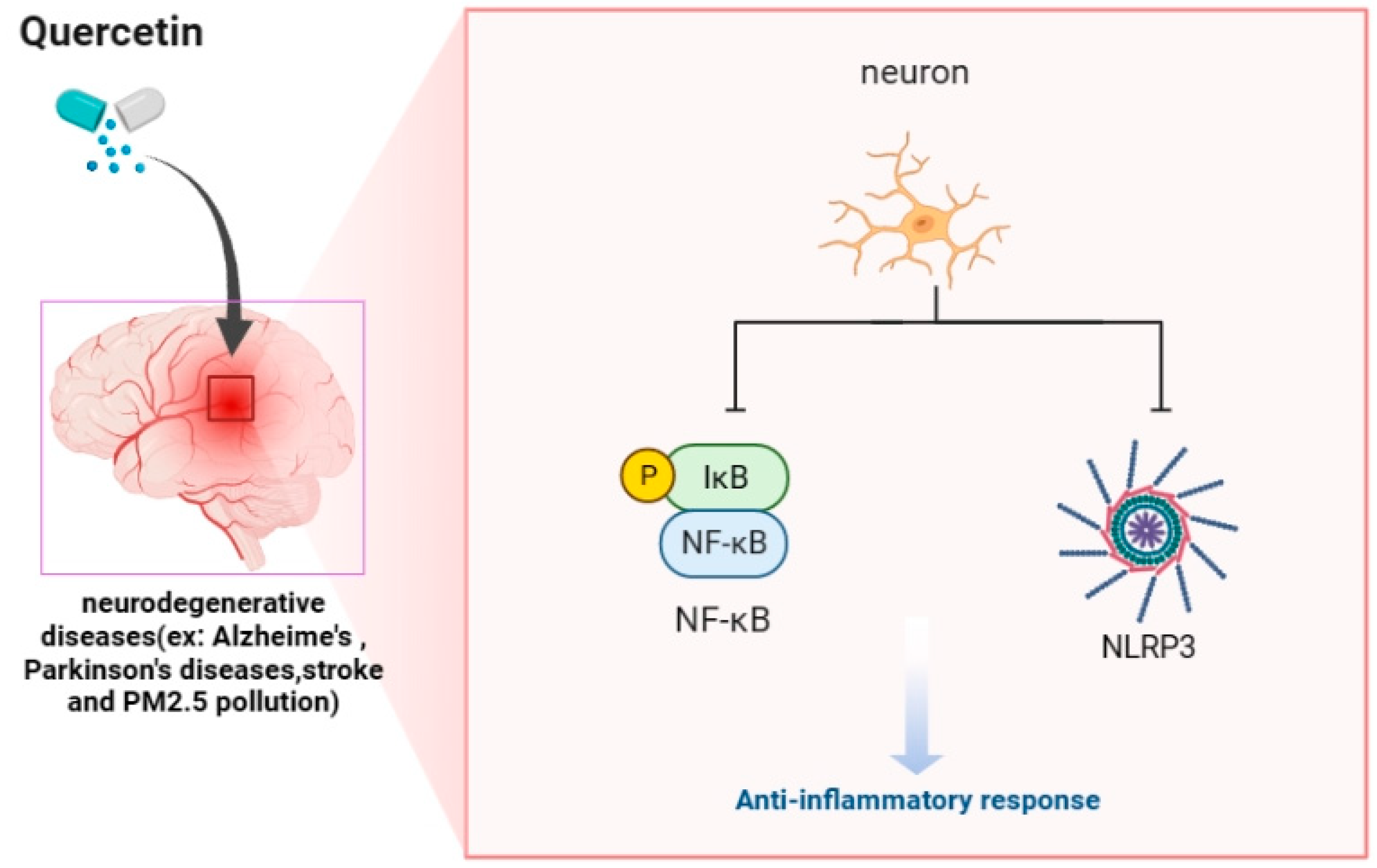
2. Natural Products and Neuroprotection and Neuroinflammation
2.1. Quercetin Is a Natural Anti-Inflammatory Agent That Alters Cellular Functions during Inflammation
2.2. Neuroprotective Role of Quercetin in Neurodegenerative Diseases, Stroke, and PM2.5-Induced Neuroinflammatory Toxicity
2.2.1. The Effect and Molecular Mechanism of Quercetin in AD
2.2.2. Mechanism of Quercetin Therapeutic Targets for PD
2.2.3. Molecular Mechanisms Underlying Protective Role of Quercetin in Stroke
2.2.4. Neuroprotective Effect and Molecular Mechanism of Quercetin on PM2.5
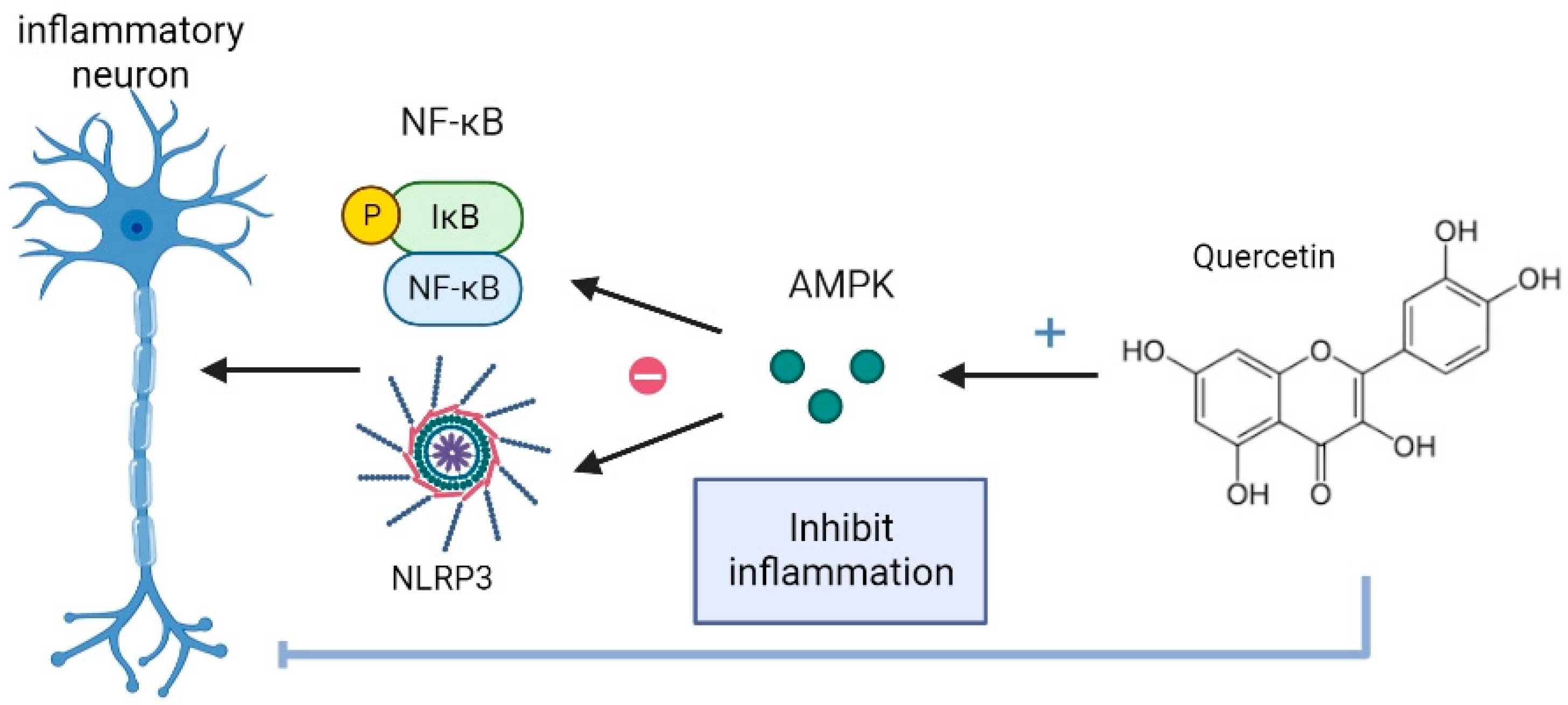
3. Quercetin Is an Anti-Inflammatory Agent via AMPK and Is Neuroprotective for NF-kB and NLRP3 Inflammasome in Neuroinflammatory Toxicity
3.1. Quercetin via AMPK Suppresses NF-κB and NLRP3 Inflammasome Activation in AD and PD
3.2. Quercetin Inhibits NF-κB and NLRP3 Inflammasome in Stroke and PM2.5 by AMPK Signaling Pathway
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Skaper, S.D.; Facci, L.; Zusso, M.; Giusti, P. An Inflammation-Centric View of Neurological Disease: Beyond the Neuron. Front. Cell. Neurosci. 2018, 12, 72. [Google Scholar] [CrossRef] [PubMed]
- Garofalo, S.; Cocozza, G.; Bernardini, G.; Savage, J.; Raspa, M.; Aronica, E.; Tremblay, M.E.; Ransohoff, R.M.; Santoni, A.; Limatola, C. Blocking immune cell infiltration of the central nervous system to tame Neuroinflammation in Amyotrophic lateral sclerosis. Brain Behav. Immun. 2022, 105, 1–14. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, J.A.; Spielman, L.J.; Pointer, C.B.; Lowry, J.R.; Bajwa, E.; Lee, C.W.; Klegeris, A. Neuroinflammation as a Common Mechanism Associated with the Modifiable Risk Factors for Alzheimer’s and Parkinson’s Diseases. Curr. Aging Sci. 2017, 10, 158–176. [Google Scholar] [CrossRef] [PubMed]
- Otani, K.; Shichita, T. Cerebral sterile inflammation in neurodegenerative diseases. Inflamm. Regen. 2020, 40, 28. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, K.; Nakajima, K. Role of the Immune System in the Development of the Central Nervous System. Front. Neurosci. 2019, 13, 916. [Google Scholar] [CrossRef]
- Guzman-Martinez, L.; Maccioni, R.B.; Andrade, V.; Navarrete, L.P.; Pastor, M.G.; Ramos-Escobar, N. Neuroinflammation as a Common Feature of Neurodegenerative Disorders. Front. Pharmacol. 2019, 10, 1008. [Google Scholar] [CrossRef]
- Mohamed, W.; Kumar, J.; Alghamdi, B.S.; Soliman, A.-H.; Toshihide, Y. Neurodegeneration and inflammation crosstalk: Therapeutic targets and perspectives. IBRO Neurosci. Rep. 2023, 14, 95–110. [Google Scholar] [CrossRef]
- Singh, D. Astrocytic and microglial cells as the modulators of neuroinflammation in Alzheimer’s disease. J. Neuroinflammation 2022, 19, 206. [Google Scholar] [CrossRef]
- Picca, A.; Calvani, R.; Coelho-Junior, H.J.; Landi, F.; Bernabei, R.; Marzetti, E. Mitochondrial Dysfunction, Oxidative Stress, and Neuroinflammation: Intertwined Roads to Neurodegeneration. Antioxidants 2020, 9, 647. [Google Scholar] [CrossRef]
- Kany, S.; Vollrath, J.T.; Relja, B. Cytokines in Inflammatory Disease. Int. J. Mol. Sci. 2019, 20, 6008. [Google Scholar] [CrossRef]
- Misrani, A.; Tabassum, S.; Yang, L. Mitochondrial Dysfunction and Oxidative Stress in Alzheimer’s Disease. Front. Aging Neurosci. 2021, 13, 617588. [Google Scholar] [CrossRef]
- Dabrowska-Bouta, B.; Sulkowski, G.; Gewartowska, M.; Struzynska, L. Endoplasmic Reticulum Stress Underlies Nanosilver-Induced Neurotoxicity in Immature Rat Brain. Int. J. Mol. Sci. 2022, 23, 13013. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.-Y.; Tan, M.-S.; Yu, J.-T.; Tan, L. Role of pro-inflammatory cytokines released from microglia in Alzheimer’s disease. Ann. Transl. Med. 2015, 3, 136. [Google Scholar] [PubMed]
- Rahman, M.M.; Lendel, C. Extracellular protein components of amyloid plaques and their roles in Alzheimer’s disease pathology. Mol. Neurodegener. 2021, 16, 59. [Google Scholar] [CrossRef]
- Al-Ghraiybah, N.F.; Wang, J.; Alkhalifa, A.E.; Roberts, A.B.; Raj, R.; Yang, E.; Kaddoumi, A. Glial Cell-Mediated Neuroinflammation in Alzheimer’s Disease. Int. J. Mol. Sci. 2022, 23, 10572. [Google Scholar] [CrossRef]
- Maiti, P.; Manna, J.; Dunbar, G.L. Current understanding of the molecular mechanisms in Parkinson’s disease: Targets for potential treatments. Transl. Neurodegener. 2017, 6, 28. [Google Scholar] [CrossRef]
- Tofaris, G.K. Initiation and progression of alpha-synuclein pathology in Parkinson’s disease. Cell. Mol. Life Sci. 2022, 79, 210. [Google Scholar] [CrossRef]
- Araujo, B.; Caridade-Silva, R.; Soares-Guedes, C.; Martins-Macedo, J.; Gomes, E.D.; Monteiro, S.; Teixeira, F.G. Neuroinflammation and Parkinson’s Disease-From Neurodegeneration to Therapeutic Opportunities. Cells 2022, 11, 2908. [Google Scholar] [CrossRef]
- Kuriakose, D.; Xiao, Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int. J. Mol. Sci. 2020, 21, 7609. [Google Scholar] [CrossRef]
- Jurcau, A.; Simion, A. Neuroinflammation in Cerebral Ischemia and Ischemia/Reperfusion Injuries: From Pathophysiology to Therapeutic Strategies. Int. J. Mol. Sci. 2022, 23, 14. [Google Scholar] [CrossRef]
- Peters, A. Ambient air pollution and Alzheimer’s disease: The role of the composition of fine particles. Proc. Natl. Acad. Sci. USA 2023, 120, e2220028120. [Google Scholar] [CrossRef]
- Song, J.; Han, K.; Wang, Y.; Qu, R.; Liu, Y.; Wang, S.; Wang, Y.; An, Z.; Li, J.; Wu, H.; et al. Microglial Activation and Oxidative Stress in PM(2.5)-Induced Neurodegenerative Disorders. Antioxidants 2022, 11, 1482. [Google Scholar] [CrossRef]
- Kang, Y.J.; Tan, H.Y.; Lee, C.Y.; Cho, H. An Air Particulate Pollutant Induces Neuroinflammation and Neurodegeneration in Human Brain Models. Adv. Sci. 2021, 8, e2101251. [Google Scholar] [CrossRef]
- Kwon, H.S.; Koh, S.H. Neuroinflammation in neurodegenerative disorders: The roles of microglia and astrocytes. Transl. Neurodegener. 2020, 9, 42. [Google Scholar] [CrossRef]
- Jayaraj, R.L.; Azimullah, S.; Beiram, R.; Jalal, F.Y.; Rosenberg, G.A. Neuroinflammation: Friend and foe for ischemic stroke. J. Neuroinflammation 2019, 16, 142. [Google Scholar] [CrossRef]
- Armas, F.V.; D’Angiulli, A. Neuroinflammation and Neurodegeneration of the Central Nervous System from Air Pollutants: A Scoping Review. Toxics 2022, 10, 666. [Google Scholar] [CrossRef]
- Mohd Sairazi, N.S.; Sirajudeen, K.N.S. Natural Products and Their Bioactive Compounds: Neuroprotective Potentials against Neurodegenerative Diseases. Evid. Based Complement. Altern. Med. 2020, 2020, 6565396. [Google Scholar] [CrossRef]
- Alghamdi, S.S.; Suliman, R.S.; Aljammaz, N.A.; Kahtani, K.M.; Aljatli, D.A.; Albadrani, G.M. Natural Products as Novel Neuroprotective Agents; Computational Predictions of the Molecular Targets, ADME Properties, and Safety Profile. Plants 2022, 11, 549. [Google Scholar] [CrossRef]
- Singh, S.; Nagalakshmi, D.; Sharma, K.K.; Ravichandiran, V. Natural antioxidants for neuroinflammatory disorders and possible involvement of Nrf2 pathway: A review. Heliyon 2021, 7, e06216. [Google Scholar] [CrossRef]
- Sang, A.; Wang, Y.; Wang, S.; Wang, Q.; Wang, X.; Li, X.; Song, X. Quercetin attenuates sepsis-induced acute lung injury via suppressing oxidative stress-mediated ER stress through activation of SIRT1/AMPK pathways. Cell. Signal. 2022, 96, 110363. [Google Scholar] [CrossRef]
- Trefts, E.; Shaw, R.J. AMPK: Restoring metabolic homeostasis over space and time. Mol. Cell 2021, 81, 3677–3690. [Google Scholar] [CrossRef]
- Chiang, M.C.; Nicol, C.J.; Cheng, Y.C. Resveratrol activation of AMPK-dependent pathways is neuroprotective in human neural stem cells against amyloid-beta-induced inflammation and oxidative stress. Neurochem. Int. 2018, 115, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chiang, M.C.; Nicol, C.J.B.; Lo, S.S.; Hung, S.W.; Wang, C.J.; Lin, C.H. Resveratrol Mitigates Oxygen and Glucose Deprivation-Induced Inflammation, NLRP3 Inflammasome, and Oxidative Stress in 3D Neuronal Culture. Int. J. Mol. Sci. 2022, 23, 11678. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.M.; Chen, Y.L.; Pei, D.; Cheng, Y.C.; Sun, B.; Nicol, C.J.; Yen, C.H.; Chen, H.M.; Liang, Y.J.; Chiang, M.C. The neuroprotective role of metformin in advanced glycation end product treated human neural stem cells is AMPK-dependent. Biochim. Biophys. Acta 2015, 1852, 720–731. [Google Scholar] [CrossRef]
- Islam, M.S.; Quispe, C.; Hossain, R.; Islam, M.T.; Al-Harrasi, A.; Al-Rawahi, A.; Martorell, M.; Mamurova, A.; Seilkhan, A.; Altybaeva, N.; et al. Neuropharmacological Effects of Quercetin: A Literature-Based Review. Front. Pharmacol. 2021, 12, 665031. [Google Scholar] [CrossRef]
- Zhang, X.W.; Chen, J.Y.; Ouyang, D.; Lu, J.H. Quercetin in Animal Models of Alzheimer’s Disease: A Systematic Review of Preclinical Studies. Int. J. Mol. Sci. 2020, 21, 493. [Google Scholar] [CrossRef]
- Wrobel-Biedrawa, D.; Grabowska, K.; Galanty, A.; Sobolewska, D.; Podolak, I. A Flavonoid on the Brain: Quercetin as a Potential Therapeutic Agent in Central Nervous System Disorders. Life 2022, 12, 591. [Google Scholar] [CrossRef]
- Sul, O.J.; Ra, S.W. Quercetin Prevents LPS-Induced Oxidative Stress and Inflammation by Modulating NOX2/ROS/NF-kB in Lung Epithelial Cells. Molecules 2021, 26, 6949. [Google Scholar] [CrossRef]
- Salehi, B.; Machin, L.; Monzote, L.; Sharifi-Rad, J.; Ezzat, S.M.; Salem, M.A.; Merghany, R.M.; El Mahdy, N.M.; Kilic, C.S.; Sytar, O.; et al. Therapeutic Potential of Quercetin: New Insights and Perspectives for Human Health. ACS Omega 2020, 5, 11849–11872. [Google Scholar] [CrossRef]
- Cao, B.; Zhang, Y.; Chen, J.; Wu, P.; Dong, Y.; Wang, Y. Neuroprotective effects of liraglutide against inflammation through the AMPK/NF-kappaB pathway in a mouse model of Parkinson’s disease. Metab. Brain Dis. 2022, 37, 451–462. [Google Scholar] [CrossRef]
- Muraleedharan, R.; Dasgupta, B. AMPK in the brain: Its roles in glucose and neural metabolism. FEBS J. 2022, 289, 2247–2262. [Google Scholar] [CrossRef] [PubMed]
- Paskeh, M.D.A.; Asadi, A.; Mirzaei, S.; Hashemi, M.; Entezari, M.; Raesi, R.; Hushmandi, K.; Zarrabi, A.; Ertas, Y.N.; Aref, A.R.; et al. Targeting AMPK signaling in ischemic/reperfusion injury: From molecular mechanism to pharmacological interventions. Cell. Signal. 2022, 94, 110323. [Google Scholar] [CrossRef] [PubMed]
- Bayazid, A.B.; Lim, B.O. Quercetin Is An Active Agent in Berries against Neurodegenerative Diseases Progression through Modulation of Nrf2/HO1. Nutrients 2022, 14, 5132. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.A.; Mendonca, P.; Soliman, K.F.A. Neuroprotective Effects and Therapeutic Potential of the Citrus Flavonoid Hesperetin in Neurodegenerative Diseases. Nutrients 2022, 14, 2228. [Google Scholar] [CrossRef]
- Thangavel, P.; Park, D.; Lee, Y.C. Recent Insights into Particulate Matter (PM(2.5))-Mediated Toxicity in Humans: An Overview. Int. J. Environ. Res. Public Health 2022, 19, 7511. [Google Scholar] [CrossRef]
- Alghamdi, A.; Birch, D.J.S.; Vyshemirsky, V.; Rolinski, O.J. Impact of the Flavonoid Quercetin on beta-Amyloid Aggregation Revealed by Intrinsic Fluorescence. J. Phys. Chem. B 2022, 126, 7229–7237. [Google Scholar] [CrossRef]
- Wang, L.; Sun, J.; Miao, Z.; Jiang, X.; Zheng, Y.; Yang, G. Quercitrin improved cognitive impairment through inhibiting inflammation induced by microglia in Alzheimer’s disease mice. NeuroReport 2022, 33, 327–335. [Google Scholar] [CrossRef]
- Thiruvengadam, M.; Venkidasamy, B.; Subramanian, U.; Samynathan, R.; Ali Shariati, M.; Rebezov, M.; Girish, S.; Thangavel, S.; Dhanapal, A.R.; Fedoseeva, N.; et al. Bioactive Compounds in Oxidative Stress-Mediated Diseases: Targeting the NRF2/ARE Signaling Pathway and Epigenetic Regulation. Antioxidants 2021, 10, 1859. [Google Scholar] [CrossRef]
- Ghafouri-Fard, S.; Shoorei, H.; Khanbabapour Sasi, A.; Taheri, M.; Ayatollahi, S.A. The impact of the phytotherapeutic agent quercetin on expression of genes and activity of signaling pathways. Biomed. Pharmacother. 2021, 141, 111847. [Google Scholar] [CrossRef]
- Zu, G.; Sun, K.; Li, L.; Zu, X.; Han, T.; Huang, H. Mechanism of quercetin therapeutic targets for Alzheimer disease and type 2 diabetes mellitus. Sci. Rep. 2021, 11, 22959. [Google Scholar] [CrossRef]
- Cui, Z.; Zhao, X.; Amevor, F.K.; Du, X.; Wang, Y.; Li, D.; Shu, G.; Tian, Y.; Zhao, X. Therapeutic application of quercetin in aging-related diseases: SIRT1 as a potential mechanism. Front. Immunol. 2022, 13, 943321. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.L.; Kao, N.J.; Lin, C.I.; Cross, T.L.; Lin, S.H. Quercetin Increases Mitochondrial Biogenesis and Reduces Free Radicals in Neuronal SH-SY5Y Cells. Nutrients 2022, 14, 3310. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.J.; Teng, Y.S.; Chen, C.M.; Sun, Y.C.; Hsieh-Li, H.M.; Chang, K.H.; Lee-Chen, G.J. A Neuroprotective Action of Quercetin and Apigenin through Inhibiting Aggregation of Abeta and Activation of TRKB Signaling in a Cellular Experiment. Biomol. Ther. 2023; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Jung, U.J.; Kim, S.R. Beneficial Effects of Flavonoids Against Parkinson’s Disease. J. Med. Food 2018, 21, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Han, S.; Fink, A.L. Oxidized quercetin inhibits alpha-synuclein fibrillization. Biochim. Biophys. Acta 2013, 1830, 2872–2881. [Google Scholar] [CrossRef]
- Sharma, S.; Raj, K.; Singh, S. Neuroprotective Effect of Quercetin in Combination with Piperine Against Rotenone- and Iron Supplement-Induced Parkinson’s Disease in Experimental Rats. Neurotox. Res. 2020, 37, 198–209. [Google Scholar] [CrossRef]
- Jain, J.; Hasan, W.; Biswas, P.; Yadav, R.S.; Jat, D. Neuroprotective effect of quercetin against rotenone-induced neuroinflammation and alterations in mice behavior. J. Biochem. Mol. Toxicol. 2022, 36, e23165. [Google Scholar] [CrossRef]
- Josiah, S.S.; Famusiwa, C.D.; Crown, O.O.; Lawal, A.O.; Olaleye, M.T.; Akindahunsi, A.A.; Akinmoladun, A.C. Neuroprotective effects of catechin and quercetin in experimental Parkinsonism through modulation of dopamine metabolism and expression of IL-1beta, TNF-alpha, NF-kappaB, IkappaKB, and p53 genes in male Wistar rats. Neurotoxicology 2022, 90, 158–171. [Google Scholar] [CrossRef]
- Ay, M.; Luo, J.; Langley, M.; Jin, H.; Anantharam, V.; Kanthasamy, A.; Kanthasamy, A.G. Molecular mechanisms underlying protective effects of quercetin against mitochondrial dysfunction and progressive dopaminergic neurodegeneration in cell culture and MitoPark transgenic mouse models of Parkinson’s Disease. J. Neurochem. 2017, 141, 766–782. [Google Scholar] [CrossRef]
- Zhang, L.; Ma, J.; Yang, F.; Li, S.; Ma, W.; Chang, X.; Yang, L. Neuroprotective Effects of Quercetin on Ischemic Stroke: A Literature Review. Front. Pharmacol. 2022, 13, 854249. [Google Scholar] [CrossRef]
- Guo, C.; Wang, W.J.; Liao, Y.C.; Zhao, C.; Yin, Y.; Yao, M.N.; Ding, Y.; Wang, J.W. Effect and Mechanisms of Quercetin for Experimental Focal Cerebral Ischemia: A Systematic Review and Meta-Analysis. Oxidative Med. Cell. Longev. 2022, 2022, 9749461. [Google Scholar] [CrossRef]
- Wang, Y.Y.; Chang, C.Y.; Lin, S.Y.; Wang, J.D.; Wu, C.C.; Chen, W.Y.; Kuan, Y.H.; Liao, S.L.; Wang, W.Y.; Chen, C.J. Quercetin protects against cerebral ischemia/reperfusion and oxygen glucose deprivation/reoxygenation neurotoxicity. J. Nutr. Biochem. 2020, 83, 108436. [Google Scholar] [CrossRef]
- Park, D.J.; Kang, J.B.; Shah, F.A.; Jin, Y.B.; Koh, P.O. Quercetin Attenuates Decrease of Thioredoxin Expression Following Focal Cerebral Ischemia and Glutamate-induced Neuronal Cell Damage. Neuroscience 2020, 428, 38–49. [Google Scholar] [CrossRef]
- Le, K.; Song, Z.; Deng, J.; Peng, X.; Zhang, J.; Wang, L.; Zhou, L.; Bi, H.; Liao, Z.; Feng, Z. Quercetin alleviates neonatal hypoxic-ischemic brain injury by inhibiting microglia-derived oxidative stress and TLR4-mediated inflammation. Inflamm. Res. 2020, 69, 1201–1213. [Google Scholar] [CrossRef]
- Park, D.J.; Kang, J.B.; Shah, M.A.; Koh, P.O. Quercetin alleviates the injury-induced decrease of protein phosphatase 2A subunit B in cerebral ischemic animal model and glutamate-exposed HT22 cells. J. Vet. Med. Sci. 2019, 81, 1047–1054. [Google Scholar] [CrossRef]
- Li, M.T.; Ke, J.; Guo, S.F.; Wu, Y.; Bian, Y.F.; Shan, L.L.; Liu, Q.Y.; Huo, Y.J.; Guo, C.; Liu, M.Y.; et al. The Protective Effect of Quercetin on Endothelial Cells Injured by Hypoxia and Reoxygenation. Front. Pharmacol. 2021, 12, 732874. [Google Scholar] [CrossRef]
- Fu, P.; Guo, X.; Cheung, F.M.H.; Yung, K.K.L. The association between PM(2.5) exposure and neurological disorders: A systematic review and meta-analysis. Sci. Total Environ. 2019, 655, 1240–1248. [Google Scholar] [CrossRef]
- Liu, W.; Zhang, M.; Feng, J.; Fan, A.; Zhou, Y.; Xu, Y. The Influence of Quercetin on Maternal Immunity, Oxidative Stress, and Inflammation in Mice with Exposure of Fine Particulate Matter during Gestation. Int. J. Environ. Res. Public Health 2017, 14, 592. [Google Scholar] [CrossRef]
- Zhang, M.; Liu, W.; Zhou, Y.; Li, Y.; Qin, Y.; Xu, Y. Neurodevelopmental toxicity induced by maternal PM2.5 exposure and protective effects of quercetin and Vitamin C. Chemosphere 2018, 213, 182–196. [Google Scholar] [CrossRef]
- Jin, X.; Su, R.; Li, R.; Song, L.; Chen, M.; Cheng, L.; Li, Z. Amelioration of particulate matter-induced oxidative damage by vitamin c and quercetin in human bronchial epithelial cells. Chemosphere 2016, 144, 459–466. [Google Scholar] [CrossRef]
- Liu, W.; Zhou, Y.; Qin, Y.; Li, Y.; Yu, L.; Li, R.; Chen, Y.; Xu, Y. Sex-Dependent Effects of PM(2.5) Maternal Exposure and Quercetin Intervention on Offspring’s Short Chain Fatty Acids. Int. J. Environ. Res. Public Health 2019, 16, 4371. [Google Scholar] [CrossRef]
- Chen, T.; Zhang, X.; Zhu, G.; Liu, H.; Chen, J.; Wang, Y.; He, X. Quercetin inhibits TNF-alpha induced HUVECs apoptosis and inflammation via downregulating NF-kB and AP-1 signaling pathway in vitro. Medicine 2020, 99, e22241. [Google Scholar] [CrossRef]
- Grewal, A.K.; Singh, T.G.; Sharma, D.; Sharma, V.; Singh, M.; Rahman, M.H.; Najda, A.; Walasek-Janusz, M.; Kamel, M.; Albadrani, G.M.; et al. Mechanistic insights and perspectives involved in neuroprotective action of quercetin. Biomed. Pharmacother. 2021, 140, 111729. [Google Scholar] [CrossRef]
- Han, X.; Xu, T.; Fang, Q.; Zhang, H.; Yue, L.; Hu, G.; Sun, L. Quercetin hinders microglial activation to alleviate neurotoxicity via the interplay between NLRP3 inflammasome and mitophagy. Redox Biol. 2021, 44, 102010. [Google Scholar] [CrossRef] [PubMed]
- Anderson, F.L.; Biggs, K.E.; Rankin, B.E.; Havrda, M.C. NLRP3 inflammasome in neurodegenerative disease. Transl. Res. 2023, 252, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Zhan, X.; Li, Q.; Xu, G.; Xiao, X.; Bai, Z. The mechanism of NLRP3 inflammasome activation and its pharmacological inhibitors. Front. Immunol. 2022, 13, 1109938. [Google Scholar] [CrossRef]
- Chen, Y.; Peng, F.; Xing, Z.; Chen, J.; Peng, C.; Li, D. Beneficial effects of natural flavonoids on neuroinflammation. Front. Immunol. 2022, 13, 1006434. [Google Scholar] [CrossRef] [PubMed]
- Meng-Zhen, S.; Ju, L.; Lan-Chun, Z.; Cai-Feng, D.; Shu-da, Y.; Hao-Fei, Y.; Wei-Yan, H. Potential therapeutic use of plant flavonoids in AD and PD. Heliyon 2022, 8, e11440. [Google Scholar] [CrossRef]
- Yang, Z.; Liu, J.; Wei, S.; Deng, J.; Feng, X.; Liu, S.; Liu, M. A novel strategy for bioactive natural products targeting NLRP3 inflammasome in Alzheimer’s disease. Front. Pharmacol. 2022, 13, 1077222. [Google Scholar] [CrossRef] [PubMed]
- Magalingam, K.B.; Radhakrishnan, A.K.; Haleagrahara, N. Protective Mechanisms of Flavonoids in Parkinson’s Disease. Oxidative Med. Cell. Longev. 2015, 2015, 314560. [Google Scholar] [CrossRef]
- Jiang, W.; Huang, Y.; Han, N.; He, F.; Li, M.; Bian, Z.; Liu, J.; Sun, T.; Zhu, L. Quercetin suppresses NLRP3 inflammasome activation and attenuates histopathology in a rat model of spinal cord injury. Spinal Cord 2016, 54, 592–596. [Google Scholar] [CrossRef]
- Tamtaji, O.R.; Hadinezhad, T.; Fallah, M.; Shahmirzadi, A.R.; Taghizadeh, M.; Behnam, M.; Asemi, Z. The Therapeutic Potential of Quercetin in Parkinson’s Disease: Insights into its Molecular and Cellular Regulation. Curr. Drug Targets 2020, 21, 509–518. [Google Scholar] [CrossRef]
- He, W.; Hu, Z.; Zhong, Y.; Wu, C.; Li, J. The Potential of NLRP3 Inflammasome as a Therapeutic Target in Neurological Diseases. Mol. Neurobiol. 2023, 60, 2520–2538. [Google Scholar] [CrossRef]
- Lin, C.H.; Nicol, C.J.B.; Wan, C.; Chen, S.J.; Huang, R.N.; Chiang, M.C. Exposure to PM(2.5) induces neurotoxicity, mitochondrial dysfunction, oxidative stress and inflammation in human SH-SY5Y neuronal cells. Neurotoxicology 2022, 88, 25–35. [Google Scholar] [CrossRef]
- Zeng, X.; Liu, D.; Wu, W.; Huo, X. PM(2.5) exposure inducing ATP alteration links with NLRP3 inflammasome activation. Environ. Sci. Pollut. Res. Int. 2022, 29, 24445–24456. [Google Scholar] [CrossRef]
- Cao, W.; Wang, X.; Li, J.; Yan, M.; Chang, C.H.; Kim, J.; Jiang, J.; Liao, Y.P.; Tseng, S.; Kusumoputro, S.; et al. NLRP3 inflammasome activation determines the fibrogenic potential of PM(2.5) air pollution particles in the lung. J. Environ. Sci. 2022, 111, 429–441. [Google Scholar] [CrossRef]
- Qi, W.; Qi, W.; Xiong, D.; Long, M. Quercetin: Its Antioxidant Mechanism, Antibacterial Properties and Potential Application in Prevention and Control of Toxipathy. Molecules 2022, 27, 6545. [Google Scholar] [CrossRef]
| Biological Model | Pathways | Targets/Mechanisms | References |
|---|---|---|---|
| Quercetin can simultaneously interfere with AD progression (in vitro) | MAPK signaling | Regulate AKT1, JUN, MAPK, TNF, VEGFA, and EGFR | [50] |
| Quercetin (100 mg/kg) exerts neuroprotective effects against chronic aging-related diseases in AD mice model (in vivo) | Oxidative stress, Inflammatory, Mitochondrial damage and Autophagy. | Inhibited SIRT1/Keap1/Nrf2/HO-1 pathway, PI3K/Akt/GSK-3β, SIRT1/NF-Κb pathway, SIRT1/PGC1α/eIF2α/ATF4/CHOP pathway, and SIRT1/FoxO pathway | [51] |
| Quercetin (100 mg/kg) exhibited a synergistic effect with sitagliptin and improved cognitive memory in the rat brain (in vivo) | Decreasing the Aβ1-42 levels, enhancing the antioxidant activity | Increasing the expression of the NRF2/ARE pathway | [48] |
| Aβ and hippocampal tau phosphorylation were reduced during quercetin treatment (in vivo) | Protect neuronal cell death | Modulating Nrf2/HO-1 pathways | [43] |
| Quercitin (50 or 100 mg/kg) improved 5XFAD mice’s cognitive impairment (in vivo) | Anti-inflammatory response | Inhibited IL-1α, IL-6, IL-17A, G-CSF, IL-4, CXCL-1, Eotaxin, G-CSF, MIP-1α and MIP-1β | [47] |
| Quercetin (2.5, 5.0, 7.5, and 10.0 μM) increases mitochondrial biogenesis in hydrogen peroxide (H2O2)-induced oxidative stress neuronal SH-SY5Y cells (in vitro) | ROS production and mitochondrial biogenesis | Elevating the activity of the SIRT1-PGC-1α-TFAM pathway | [52] |
| Quercetin (100 μM) improved neurite outgrowth and reduced caspase-1/AChE activities in Aβ-GFP SH-SY5Y cells (in vitro) | Regulating neuronal survival and oxidative stress | Activating TRKB, enhancing NRF2, and reducing ROS | [53] |
| Biological Model | Pathways | Targets/Mechanisms | References |
|---|---|---|---|
| Quercetin (25 mg/kg) had a neuroprotective effect against rotenone- and iron supplement-induced PD in experimental rats (in vivo) | Anti-inflammatory, antioxidant, and neuroprotective effect | Improve biochemical (LPO, nitrite, GSH, mitochondrial complexes I and IV), neuroinflammatory (TNF-α, IL-1β, and IL-6), and neurotransmitter (dopamine, norepinephrine, serotonin, GABA, glutamate) | [56] |
| Quercetin (30 mg/kg) has a neuroprotective effect against rotenone-induced neuroinflammation and alterations in PD-like symptoms and mice behavior (in vivo) | Anti-neuroinflammation, improved memory, and cognitive function | Regulate the release of inflammatory markers in blood serum, astrocytes activation in substantia nigra and hippocampus, and subsequently decreased density of dopaminergic fibers in the striatum | [57] |
| Quercetin (5–20 mg/kg) has neuroprotective effects in an experimental model of Parkinsonism in male Wistar rats (in vivo) | Modulate dopamine metabolism and decrease neuroinflammation through the downregulation of pro-inflammatory cytokines and genes involved in inflammation and cell death pathways | Attenuating effect on NF-κB mediated inflammation (IL-1β, TNF-α, NF-κB, and IκKB) and the pro-apoptotic gene (p53) | [58] |
| Quercetin (10 and 30 μM; 25 mg/kg)has protective effects against mitochondrial dysfunction and progressive dopaminergic neurodegeneration in MN9D dopaminergic neuronal cells and MitoPark transgenic mouse models of PD (in vivo) | Mediate neuroprotective signaling and mitochondrial bioenergetics capacity | Induced the activation of two major cell survival kinases, protein kinase D1 (PKD1) and Akt; enhanced cAMP response-element binding protein phosphorylation and expression of the cAMP response-element binding protein target gene brain-derived neurotrophic factor | [59] |
| Biological Model | Effects | Targets/Mechanisms | References |
|---|---|---|---|
| Quercetin (25 mg/kg) protects against cerebral ischemia injury and oxygen-glucose deprivation neurotoxicity in SD rats and neuron/glia cultures (in vivo and in vitro) | Neuroprotective, anti-oxidative, anti-inflammatory, and anti-apoptotic effects | Biochemical studies revealed a reduction of ERK and Akt phosphorylation, TNF-α and IL-1β mRNA expression, along with apoptotic caspase 3 activity | [62] |
| Quercetin (10 mg/kg) has the potential as a neuroprotective agent and protects against oxidative stress and neuronal damage in cerebral ischemia SD rats and primary cultures of neurons (in vivo and in vitro) | Neuroprotective against oxidative stress and neuronal damage. | Regulate thioredoxin expression and maintain interaction between ASK1 and thioredoxin | [63] |
| Quercetin (50 mg/kg) inhibited oxygen-glucose deprivation-induced expression of inflammatory factors in BV2 cells and suppressed cerebral infarct volume in oxygen-glucose deprivation mice (in vivo and in vitro) | Anti-inflammatory and anti-oxidative effects | Inhibition of TLR4-mediated inflammatory responses and oxidative stress in activated microglia | [64] |
| Quercetin (10 mg/kg) has the potential as a neuroprotective agent by alleviates cerebral ischemic animal models and glutamate-exposed HT22 cells (in vivo and in vitro) | Neuroprotective function in ischemic brain injury | Increase the expression of PP2A-B and protect against neuronal injury and cell death | [65] |
| Protective Effect of Quercetin (1 μM) on human brain microvascular endothelial cells injured by hypoxia damage (in vitro) | Inhibition of endoplasmic reticulum stress and antioxidation | Promote the Keap1/Nrf2 signaling pathway, and reduce ATF6/GRP78 protein expression | [66] |
| Biological Model | Effects | Targets/Mechanisms | References |
|---|---|---|---|
| Quercetin protects against PM2.5-induced neurodevelopmental toxicity in animal models (in vivo) | Oxidative stress, inflammatory response, and modulation of the CREB/BDNF signaling pathway | Improve BDNF, TrkB, p-CREB/CREB, p-Akt/Akt, p-ERK1/2/ERK1/2 expression | [69] |
| Quercetin has an inhibitory effect on PM2.5-induced respiratory oxidative damage and inflammation in human bronchial epithelial cells (in vitro) | Antioxidant and anti-inflammation properties | Regulates NADPH oxidase, inflammation cytokines, SIRT1, p53R2, NDUFS2, and UQCRI1 levels | [70] |
| Quercetin (100 mg/kg) has protective effects against the adverse effects of PM2.5 exposure in Pregnant mice (in vivo) | Anti-inflammatory and antioxidant properties | Inhibit biomarkers of systemic inflammation injuries (IL-2, IL-6, IL-8, and TNF-α) and oxidative stress indicators (CAT, GSH, and HO-1) | [68] |
| Quercetin (100 mg/kg) intervention during gestation protects against the adverse effects of PM2.5 exposure (in vivo) | Anti-inflammatory and antioxidant properties | Quercetin administration during gestation has been shown to have the potential to offset the effects of maternal PM2.5 exposure on short-chain fatty acids in offspring | [71] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiang, M.-C.; Tsai, T.-Y.; Wang, C.-J. The Potential Benefits of Quercetin for Brain Health: A Review of Anti-Inflammatory and Neuroprotective Mechanisms. Int. J. Mol. Sci. 2023, 24, 6328. https://doi.org/10.3390/ijms24076328
Chiang M-C, Tsai T-Y, Wang C-J. The Potential Benefits of Quercetin for Brain Health: A Review of Anti-Inflammatory and Neuroprotective Mechanisms. International Journal of Molecular Sciences. 2023; 24(7):6328. https://doi.org/10.3390/ijms24076328
Chicago/Turabian StyleChiang, Ming-Chang, Tsung-Yu Tsai, and Chieh-Ju Wang. 2023. "The Potential Benefits of Quercetin for Brain Health: A Review of Anti-Inflammatory and Neuroprotective Mechanisms" International Journal of Molecular Sciences 24, no. 7: 6328. https://doi.org/10.3390/ijms24076328
APA StyleChiang, M.-C., Tsai, T.-Y., & Wang, C.-J. (2023). The Potential Benefits of Quercetin for Brain Health: A Review of Anti-Inflammatory and Neuroprotective Mechanisms. International Journal of Molecular Sciences, 24(7), 6328. https://doi.org/10.3390/ijms24076328






