The Hypothalamic-Pituitary-Gonadal Axis in Men with Schizophrenia
Abstract
:1. Introduction
2. Material and Methods
3. Neuroendocrinology—The Relationship between the Nervous System and the Endocrine System
4. Hypothalamic-Pituitary-Gonadal (HPG) Axis in Men
5. Pathogenesis of Schizophrenia
5.1. Neurotransmission Disorders in Schizophrenia
5.1.1. Dopamine Hypothesis of Psychosis
5.1.2. Glutamate Hypothesis of Psychosis
5.1.3. Serotonin Hypothesis of Psychosis
6. Sex Hormones and Schizophrenia
7. Schizophrenia and Stress
Effects of Stress on the HPG Axis
8. Pharmacotherapy of Schizophrenia
9. Hyperprolactinemia
9.1. Hyperprolactinemia in Antipsychotic-Naïve Patients
9.2. Hyperprolactinemia Associated with Antipsychotic Use
| High | Moderate | Low or None |
|---|---|---|
| Fluphenazine (FGA) | Flupentixol (FGA) | Chlorpromazine (FGA) |
| Haloperidol (FGA) | Molindone (FGA) | Aripiprazole (SGA) |
| Pimozide (FGA) | Perphenazine (FGA) | Asenapine (SGA) |
| Sulpiride (FGA) | Thioridazine (FGA) | Clozapine (SGA) |
| Zuclopenthixol (FGA) | Trifluoperazine (FGA) | Iloperidone (SGA) |
| Amisulpride (SGA) | Sertindole (SGA) | Lurasidone (SGA) |
| Paliperidone (SGA) | Olanzapine (SGA) | |
| Risperidone (SGA) | Quetiapine (SGA) | |
| Ziprasidone (SGA) |
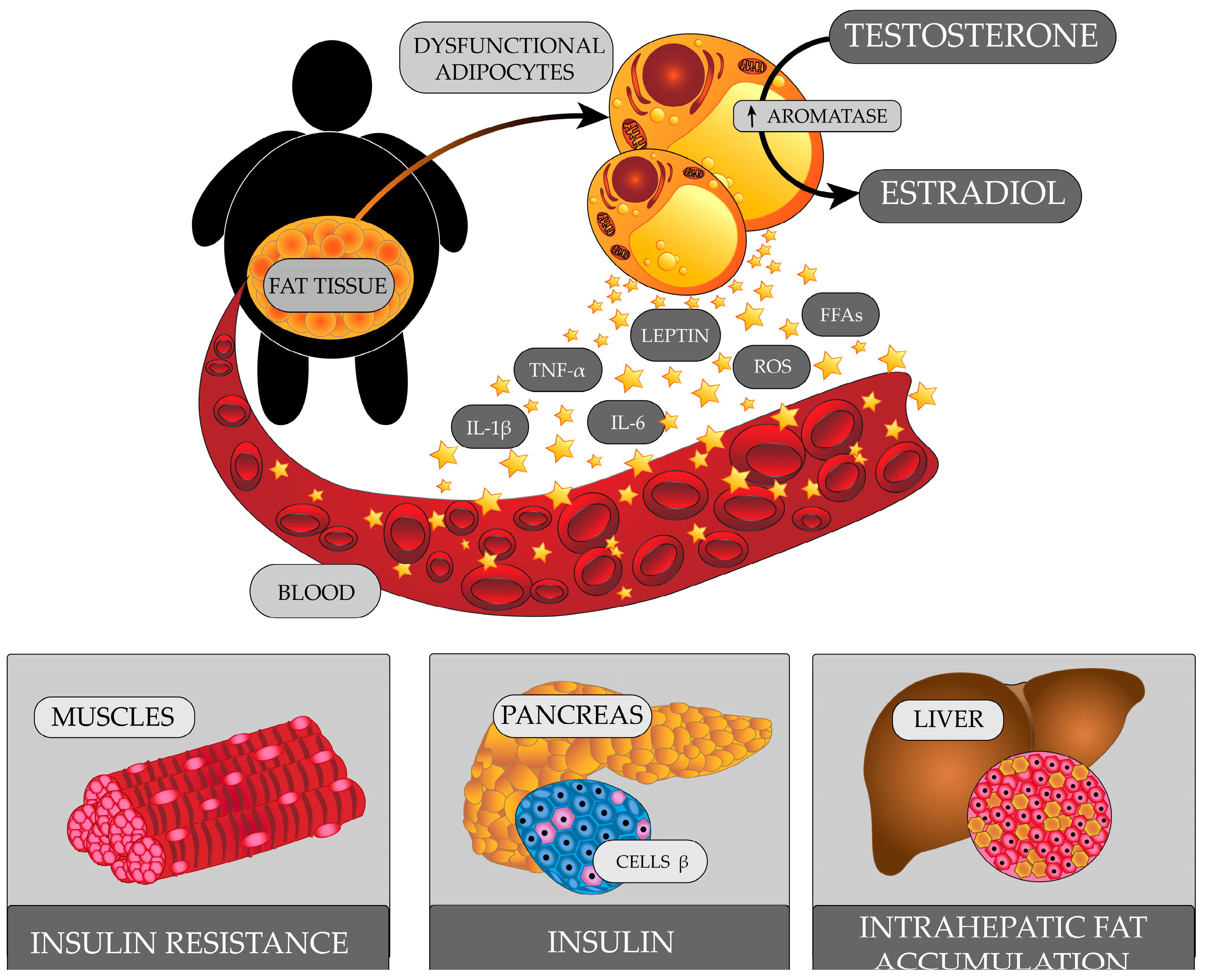
10. Schizophrenia and Obesity
HPG Axis Abnormalities in Obese Men
11. Schizophrenia and Addictions
Effects of Alcohol and Liver Damage on the HPG Axis
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Keshavan, M.S.; Collin, G.; Guimond, S.; Kelly, S.; Prasad, K.M.; Lizano, P. Neuroimaging in Schizophrenia. Neuroimaging Clin. N. Am. 2020, 30, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Owen, M.J.; Sawa, A.; Mortensen, P.B. Schizophrenia. Lancet 2016, 388, 86–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jongsma, H.E.; Turner, C.; Kirkbride, J.B.; Jones, P.B. International incidence of psychotic disorders, 2002–2017: A systematic review and meta-analysis. Lancet Public Health 2019, 4, e229–e244. [Google Scholar] [CrossRef] [Green Version]
- Aleman, A.; Kahn, R.S.; Selten, J.-P. Sex differences in the risk of schizophrenia: Evidence from meta-analysis. Arch. Gen. Psychiatry 2003, 60, 565–571. [Google Scholar] [CrossRef]
- Baandrup, L. Polypharmacy in schizophrenia. Basic Clin. Pharmacol. Toxicol. 2020, 126, 183–192. [Google Scholar] [CrossRef] [Green Version]
- Joyce, E.M.; Roiser, J.P. Cognitive heterogeneity in schizophrenia. Curr. Opin. Psychiatry 2007, 20, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Gogos, A.; Ney, L.J.; Seymour, N.; Van Rheenen, T.E.; Felmingham, K.L. Sex differences in schizophrenia, bipolar disorder, and post-traumatic stress disorder: Are gonadal hormones the link? Br. J. Pharmacol. 2019, 176, 4119–4135. [Google Scholar] [CrossRef]
- Zorkina, Y.; Morozova, A.; Abramova, O.; Reznik, A.; Kostyuk, G. Sex differences in social functioning of patients with schizophrenia depending on the age of onset and severity of the disease. Early Interv. Psychiatry 2021, 15, 1197–1209. [Google Scholar] [CrossRef] [PubMed]
- Fukuta, H.; Ito, I.; Tateno, A.; Nogami, T.; Taiji, Y.; Arakawa, R.; Suhara, T.; Asai, K.; Okubo, Y. Effects of menopause on brain structural changes in schizophrenia. Psychiatry Clin. Neurosci. 2013, 67, 3–11. [Google Scholar] [CrossRef]
- Castle, D.J.; Murray, R.M. The epidemiology of late-onset schizophrenia. Schizophr. Bull. 1993, 19, 691–700. [Google Scholar] [CrossRef] [Green Version]
- Morgan, V.A.; Castle, D.J.; Jablensky, A.V. Do women express and experience psychosis differently from men? Epidemiological evidence from the Australian National Study of Low Prevalence (Psychotic) Disorders. Aust. N. Z. J. Psychiatry 2008, 42, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Brand, B.A.; Haveman, Y.R.A.; de Beer, F.; de Boer, J.N.; Dazzan, P.; Sommer, I.E.C. Antipsychotic medication for women with schizophrenia spectrum disorders. Psychol. Med. 2022, 52, 649–663. [Google Scholar] [CrossRef]
- Li, R.; Ma, X.; Wang, G.; Yang, J.; Wang, C. Why sex differences in schizophrenia? J. Transl. Neurosci. 2016, 1, 37–42. [Google Scholar]
- Salonia, A.; Rastrelli, G.; Hackett, G.; Seminara, S.B.; Huhtaniemi, I.T.; Rey, R.A.; Hellstrom, W.J.G.; Palmert, M.R.; Corona, G.; Dohle, G.R.; et al. Paediatric and adult-onset male hypogonadism. Nat. Rev. Dis. Prim. 2019, 5, 38. [Google Scholar] [CrossRef]
- Zirkin, B.R.; Papadopoulos, V. Leydig cells: Formation, function, and regulation†. Biol. Reprod. 2018, 99, 101–111. [Google Scholar] [CrossRef] [Green Version]
- Barbonetti, A.; D’Andrea, S.; Francavilla, S. Testosterone replacement therapy. Andrology 2020, 8, 1551–1566. [Google Scholar] [CrossRef] [Green Version]
- Corona, G.; Goulis, D.G.; Huhtaniemi, I.; Zitzmann, M.; Toppari, J.; Forti, G.; Vanderschueren, D.; Wu, F.C. European Academy of Andrology (EAA) guidelines on investigation, treatment and monitoring of functional hypogonadism in males. Andrology 2020, 8, 970–987. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giammanco, M.; Tabacchi, G.; Giammanco, S.; Di Majo, D.; La Guardia, M. Testosterone and aggressiveness. Med. Sci. Monit. 2005, 11, RA136–RA145. [Google Scholar] [PubMed]
- Daniel, P.M. Anatomy of the hypothalamus and pituitary gland. J. Clin. Pathol. 1976, 7, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clarke, I.J. Hypothalamus as an endocrine organ. Compr. Physiol. 2015, 5, 217–253. [Google Scholar] [CrossRef]
- Hiller-Sturmhöfel, S.; Bartke, A. The endocrine system—An overview. Alcohol Res. Health 1998, 22, 153–164. [Google Scholar]
- Perez-Castro, C.; Renner, U.; Haedo, M.R.; Stalla, G.K.; Arzt, E. Cellular and molecular specificity of pituitary gland physiology. Physiol. Rev. 2012, 92, 1–38. [Google Scholar] [CrossRef] [Green Version]
- Sladek, C.D.; Michelini, L.C.; Stachenfeld, N.S.; Stern, J.E.; Urban, J.H. Endocrine-autonomic linkages. Compr. Physiol. 2015, 5, 1281–1323. [Google Scholar] [CrossRef] [PubMed]
- Everitt, B.J.; Hökfelt, T. Neuroendocrine anatomy of the hypothalamus. Acta Neurochir. Suppl. 1990, 47, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Kanakis, G.A.; Tsametis, C.P.; Goulis, D.G. Measuring testosterone in women and men. Maturitas 2019, 125, 41–44. [Google Scholar] [CrossRef]
- Stamatiades, G.A.; Kaiser, U.B. Gonadotropin regulation by pulsatile GnRH: Signaling and gene expression. Mol. Cell. Endocrinol. 2018, 463, 131–141. [Google Scholar] [CrossRef]
- Kaprara, A.; Huhtaniemi, I.T. The hypothalamus-pituitary-gonad axis: Tales of mice and men. Metabolism 2018, 86, 3–17. [Google Scholar] [CrossRef]
- Ilgin, S. The adverse effects of psychotropic drugs as an endocrine disrupting chemicals on the hypothalamic-pituitary regulation in male. Life Sci. 2020, 253, 117704. [Google Scholar] [CrossRef]
- Santi, D.; Crépieux, P.; Reiter, E.; Spaggiari, G.; Brigante, G.; Casarini, L.; Rochira, V.; Simoni, M. Follicle-stimulating hormone (FSH) action on spermatogenesis: A focus on physiological and therapeutic roles. J. Clin. Med. 2020, 9, 1014. [Google Scholar] [CrossRef] [Green Version]
- Halász, B.; Kiss, J.; Molnár, J. Regulation of the gonadotropin-releasing hormone (GnRH) neuronal system: Morphological aspects. J. Steroid Biochem. 1989, 33, 663–668. [Google Scholar] [CrossRef]
- Tsigos, C.; Chrousos, G.P. Hypothalamic–pituitary–adrenal axis, neuroendocrine factors and stress. J. Psychosom. Res. 2002, 53, 865–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Roux, N.; Genin, E.; Carel, J.-C.; Matsuda, F.; Chaussain, J.-L.; Milgrom, E. Hypogonadotropic hypogonadism due to loss of function of the KiSS1-derived peptide receptor GPR54. Proc. Natl. Acad. Sci. USA 2003, 100, 10972–10976. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gianetti, E.; Seminara, S. Kisspeptin and KISS1R: A critical pathway in the reproductive system. Reproduction 2008, 136, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Sengupta, P.; Dutta, S.; Karkada, I.R.; Chinni, S.V. Endocrinopathies and male infertility. Life 2021, 12, 10. [Google Scholar] [CrossRef]
- Plant, T.M. 60 years of neuroendocrinology: The hypothalamo-pituitary–gonadal axis. J. Endocrinol. 2015, 226, T41–T54. [Google Scholar] [CrossRef] [Green Version]
- Hayes, F.J.; Seminara, S.B.; DeCruz, S.; Boepple, P.A.; Crowley, W.F. Aromatase inhibition in the human male reveals a hypothalamic site of estrogen feedback. J. Clin. Endocrinol. Metab. 2000, 85, 3027–3035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finkelstein, J.S.; O’dea, L.S.L.; Whitcomb, R.W.; Crowley, W.F. Sex steroid control of gonadotropin secretion in the human male. II. Effects of estradiol administration in normal and gonadotropin-releasing hormone-deficient men. J. Clin. Endocrinol. Metab. 1991, 73, 621–628. [Google Scholar] [CrossRef]
- Hayes, F.J.; Pitteloud, N.; DeCruz, S.; Crowley, W.F.; Boepple, P.A. Importance of inhibin B in the regulation of FSH secretion in the human male. J. Clin. Endocrinol. Metab. 2001, 86, 5541–5546. [Google Scholar] [CrossRef]
- Castellano, J.M.; Tena-Sempere, M. Metabolic regulation of kisspeptin. Adv. Exp. Med. Biol. 2013, 784, 363–383. [Google Scholar] [CrossRef]
- Legge, S.E.; Santoro, M.L.; Periyasamy, S.; Okewole, A.; Arsalan, A.; Kowalec, K. Genetic architecture of schizophrenia: A review of major advancements. Psychol. Med. 2021, 51, 2168–2177. [Google Scholar] [CrossRef]
- Sullivan, P.F.; Kendler, K.S.; Neale, M.C. Schizophrenia as a complex trait. Arch. Gen. Psychiatry 2003, 60, 1187. [Google Scholar] [CrossRef] [Green Version]
- Cardno, A.G.; Marshall, E.J.; Coid, B.; Macdonald, A.M.; Ribchester, T.R.; Davies, N.J.; Venturi, P.; Jones, L.A.; Lewis, S.W.; Sham, P.C.; et al. Heritability estimates for psychotic disorders. Arch. Gen. Psychiatry 1999, 56, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trubetskoy, V.; Pardiñas, A.F.; Qi, T.; Panagiotaropoulou, G.; Awasthi, S.; Bigdeli, T.B.; Bryois, J.; Chen, C.-Y.; Dennison, C.A.; Hall, L.S.; et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature 2022, 604, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Insel, T.R. Rethinking schizophrenia. Nature 2010, 468, 187–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomson, P.A.; Parla, J.S.; McRae, A.F.; Kramer, M.; Ramakrishnan, K.; Yao, J.; Soares, D.C.; McCarthy, S.; Morris, S.W.; Cardone, L.; et al. 708 Common and 2010 rare DISC1 locus variants identified in 1542 subjects: Analysis for association with psychiatric disorder and cognitive traits. Mol. Psychiatry 2014, 19, 668–675. [Google Scholar] [CrossRef] [Green Version]
- Tang, S.X.; Gur, R.E. Longitudinal perspectives on the psychosis spectrum in 22q11.2 deletion syndrome. Am. J. Med. Genet. Part A 2018, 176, 2192–2202. [Google Scholar] [CrossRef] [PubMed]
- Cannon, M.; Jones, P.B.; Murray, R.M. Obstetric complications and schizophrenia: Historical and meta-analytic review. Am. J. Psychiatry 2002, 159, 1080–1092. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stilo, S.A.; Murray, R.M. Non-genetic factors in schizophrenia. Curr. Psychiatry Rep. 2019, 21, 100. [Google Scholar] [CrossRef] [Green Version]
- Wahbeh, M.H.; Avramopoulos, D. Gene-Environment Interactions in Schizophrenia: A Literature Review. Genes 2021, 12, 1850. [Google Scholar] [CrossRef]
- Howes, O.D.; McDonald, C.; Cannon, M.; Arseneault, L.; Boydell, J.; Murray, R.M. Pathways to schizophrenia: The impact of environmental factors. Int. J. Neuropsychopharmacol. 2004, 7, S7–S13. [Google Scholar] [CrossRef]
- Rybakowski, J. Etiopathogenesis of schizophrenia—The state of the art for 2021. Psychiatr. Pol. 2021, 55, 261–274. [Google Scholar] [CrossRef]
- Weinberger, D.R. Future of days past: Neurodevelopment and schizophrenia. Schizophr. Bull. 2017, 43, 1164–1168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howes, O.D.; Kapur, S. The dopamine hypothesis of schizophrenia: Version III- the final common pathway. Schizophr. Bull. 2009, 35, 549–562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stahl, S.M. Beyond the dopamine hypothesis of schizophrenia to three neural networks of psychosis: Dopamine, serotonin, and glutamate. CNS Spectr. 2018, 23, 187–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, K.L.; Kahn, R.S.; Ko, G.; Davidson, M. Dopamine in schizophrenia: A review and reconceptualization. Am. J. Psychiatry 1991, 148, 1474–1486. [Google Scholar] [CrossRef] [PubMed]
- Howes, O.D.; Kambeitz, J.; Kim, E.; Stahl, D.; Slifstein, M.; Abi-Dargham, A.; Kapur, S. The nature of dopamine dysfunction in schizophrenia and what this means for treatment. Arch. Gen. Psychiatry 2012, 69, 776–786. [Google Scholar] [CrossRef] [Green Version]
- Nakazawa, K.; Sapkota, K. The origin of NMDA receptor hypofunction in schizophrenia. Pharmacol. Ther. 2020, 205, 107426. [Google Scholar] [CrossRef]
- Moghaddam, B.; Javitt, D. From revolution to evolution: The glutamate hypothesis of schizophrenia and its implication for treatment. Neuropsychopharmacology 2012, 37, 4–15. [Google Scholar] [CrossRef] [Green Version]
- Krystal, J.H. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Arch. Gen. Psychiatry 1994, 51, 199. [Google Scholar] [CrossRef]
- Fogaça, M.V.; Wu, M.; Li, C.; Li, X.-Y.; Picciotto, M.R.; Duman, R.S. Inhibition of GABA interneurons in the mPFC is sufficient and necessary for rapid antidepressant responses. Mol. Psychiatry 2021, 26, 3277–3291. [Google Scholar] [CrossRef]
- Dalmau, J.; Gleichman, A.J.; Hughes, E.G.; Rossi, J.E.; Peng, X.; Lai, M.; Dessain, S.K.; Rosenfeld, M.R.; Balice-Gordon, R.; Lynch, D.R. Anti-NMDA-receptor encephalitis: Case series and analysis of the effects of antibodies. Lancet Neurol. 2008, 7, 1091–1098. [Google Scholar] [CrossRef] [Green Version]
- Aghajanian, G. Serotonin model of schizophrenia: Emerging role of glutamate mechanisms. Brain Res. Rev. 2000, 31, 302–312. [Google Scholar] [CrossRef]
- Igbal, N.; van Praag, H.M. The role of serotonin in schizophrenia. Eur. Neuropsychopharmacol. 1995, 5, 11–23. [Google Scholar] [CrossRef]
- De Gregorio, D.; Comai, S.; Posa, L.; Gobbi, G. D-Lysergic Acid Diethylamide (LSD) as a model of psychosis: Mechanism of action and pharmacology. Int. J. Mol. Sci. 2016, 17, 1953. [Google Scholar] [CrossRef] [Green Version]
- Marek, G.J.; Aghajanian, G.K. The electrophysiology of prefrontal serotonin systems: Therapeutic implications for mood and psychosis. Biol. Psychiatry 1998, 44, 1118–1127. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, H.Y.; Gadaleta, E. Contrasting typical and atypical antipsychotic drugs. Focus 2021, 19, 3–13. [Google Scholar] [CrossRef]
- Cummings, J.; Ballard, C.; Tariot, P.; Owen, R.; Foff, E.; Youakim, J.; Norton, J.; Stankovic, S. Pimavanserin: Potential treatment for dementia-related psychosis. J. Prev. Alzheimer’s Dis. 2018, 5, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Cosgrove, K.P.; Mazure, C.M.; Staley, J.K. Evolving knowledge of sex differences in brain structure, function, and chemistry. Biol. Psychiatry 2007, 62, 847–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pallier, P.N.; Ferrara, M.; Romagnolo, F.; Ferretti, M.T.; Soreq, H.; Cerase, A. Chromosomal and environmental contributions to sex differences in the vulnerability to neurological and neuropsychiatric disorders: Implications for therapeutic interventions. Prog. Neurobiol. 2022, 219, 102353. [Google Scholar] [CrossRef]
- Shobeiri, P.; Kalantari, A.; Teixeira, A.L.; Rezaei, N. Shedding light on biological sex differences and microbiota–gut–brain axis: A comprehensive review of its roles in neuropsychiatric disorders. Biol. Sex Differ. 2022, 13, 12. [Google Scholar] [CrossRef]
- Nelson, L.H.; Saulsbery, A.I.; Lenz, K.M. Small cells with big implications: Microglia and sex differences in brain development, plasticity and behavioral health. Prog. Neurobiol. 2019, 176, 103–119. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.M. Normal sexual dimorphism of the adult human brain assessed by in vivo magnetic resonance imaging. Cereb. Cortex 2001, 11, 490–497. [Google Scholar] [CrossRef]
- Goldstein, J.M. Sex, hormones and affective arousal circuitry dysfunction in schizophrenia. Horm. Behav. 2006, 50, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.M.; Seidman, L.J.; O’Brien, L.M.; Horton, N.J.; Kennedy, D.N.; Makris, N.; Caviness, V.S.; Faraone, S.V.; Tsuang, M.T. Impact of normal sexual dimorphisms on sex differences in structural brain abnormalities in schizophrenia assessed by magnetic resonance imaging. Arch. Gen. Psychiatry 2002, 59, 154. [Google Scholar] [CrossRef] [Green Version]
- Ellman, L.M.; Murphy, S.K.; Maxwell, S.D.; Calvo, E.M.; Cooper, T.; Schaefer, C.A.; Bresnahan, M.A.; Susser, E.S.; Brown, A.S. Maternal cortisol during pregnancy and offspring schizophrenia: Influence of fetal sex and timing of exposure. Schizophr. Res. 2019, 213, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Pinares-Garcia, P.; Stratikopoulos, M.; Zagato, A.; Loke, H.; Lee, J. Sex: A significant risk factor for neurodevelopmental and neurodegenerative disorders. Brain Sci. 2018, 8, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misiak, B.; Frydecka, D.; Loska, O.; Moustafa, A.A.; Samochowiec, J.; Kasznia, J.; Stańczykiewicz, B. Testosterone, DHEA and DHEA-S in patients with schizophrenia: A systematic review and meta-analysis. Psychoneuroendocrinology 2018, 89, 92–102. [Google Scholar] [CrossRef]
- Tharoor, H.; Mohan, G.; Gopal, S. Sex hormones and psychopathology in drug naïve schizophrenia. Asian J. Psychiatr. 2020, 52, 102042. [Google Scholar] [CrossRef]
- Doğan Bulut, S.; Bulut, S.; Güriz, O. The relationship between sex hormone profiles and symptoms of schizophrenia in men. Compr. Psychiatry 2016, 69, 186–192. [Google Scholar] [CrossRef]
- Olsen, L.; Hansen, T.; Jakobsen, K.D.; Djurovic, S.; Melle, I.; Agartz, I.; Hall, H.; Ullum, H.; Timm, S.; Wang, A.G.; et al. The estrogen hypothesis of schizophrenia implicates glucose metabolism: Association study in three independent samples. BMC Med. Genet. 2008, 9, 39. [Google Scholar] [CrossRef] [Green Version]
- Kulkarni, J.; Gavrilidis, E.; Worsley, R.; Hayes, E. Role of estrogen treatment in the management of schizophrenia. CNS Drugs 2012, 26, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Grigoriadis, S.; Seeman, M.V. The role of estrogen in schizophrenia: Implications for Schizophrenia Practice Guidelines for women. Can. J. Psychiatry 2002, 47, 437–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulkarni, J.; Hayes, E.; Gavrilidis, E. Hormones and schizophrenia. Curr. Opin. Psychiatry 2012, 25, 89–95. [Google Scholar] [CrossRef]
- Markham, J.A. Sex steroids and schizophrenia. Rev. Endocr. Metab. Disord. 2012, 13, 187–207. [Google Scholar] [CrossRef]
- Kulkarni, J.; Riedel, A.; de Castella, A.R.; Fitzgerald, P.B.; Rolfe, T.J.; Taffe, J.; Burger, H. A clinical trial of adjunctive oestrogen treatment in women with schizophrenia. Arch. Women’s Ment. Health 2002, 5, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Akhondzadeh, S.; Nejatisafa, A.A.; Amini, H.; Mohammadi, M.R.; Larijani, B.; Kashani, L.; Raisi, F.; Kamalipour, A. Adjunctive estrogen treatment in women with chronic schizophrenia: A double-blind, randomized, and placebo-controlled trial. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2003, 27, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, J.; Gavrilidis, E.; Worsley, R.; Van Rheenen, T.; Hayes, E. The role of estrogen in the treatment of men with schizophrenia. Int. J. Endocrinol. Metab. 2013, 11, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Owens, S.J.; Weickert, T.W.; Purves-Tyson, T.D.; Ji, E.; White, C.; Galletly, C.; Liu, D.; O’Donnell, M.; Shannon Weickert, C. Sex-specific associations of androgen receptor CAG trinucleotide repeat length and of raloxifene treatment with testosterone levels and perceived stress in schizophrenia. Complex Psychiatry 2019, 5, 28–41. [Google Scholar] [CrossRef]
- Kulkarni, J.; Gurvich, C.; Lee, S.J.; Gilbert, H.; Gavrilidis, E.; de Castella, A.; Berk, M.; Dodd, S.; Fitzgerald, P.B.; Davis, S.R. Piloting the effective therapeutic dose of adjunctive selective estrogen receptor modulator treatment in postmenopausal women with schizophrenia. Psychoneuroendocrinology 2010, 35, 1142–1147. [Google Scholar] [CrossRef]
- Trifu, S.; Istrate, D.; Miruna, D. Gaps or links between hormonal therapy and schizophrenia? Exp. Ther. Med. 2020, 20, 3508–3512. [Google Scholar] [CrossRef]
- Weiser, M.; Levi, L.; Burshtein, S.; Hagin, M.; Matei, V.P.; Podea, D.; Micluția, I.; Tiugan, A.; Păcală, B.; Grecu, I.G.; et al. Raloxifene plus antipsychotics versus placebo plus antipsychotics in severely ill decompensated postmenopausal women with schizophrenia or schizoaffective disorder. J. Clin. Psychiatry 2017, 78, e758–e765. [Google Scholar] [CrossRef] [PubMed]
- Creutz, L.M.; Kritzer, M.F. Mesostriatal and mesolimbic projections of midbrain neurons immunoreactive for estrogen receptor beta or androgen receptors in rats. J. Comp. Neurol. 2004, 476, 348–362. [Google Scholar] [CrossRef] [PubMed]
- Eck, S.R.; Bangasser, D.A. The effects of early life stress on motivated behaviors: A role for gonadal hormones. Neurosci. Biobehav. Rev. 2020, 119, 86–100. [Google Scholar] [CrossRef] [PubMed]
- Tobiansky, D.J.; Korol, A.M.; Ma, C.; Hamden, J.E.; Jalabert, C.; Tomm, R.J.; Soma, K.K. Testosterone and corticosterone in the mesocorticolimbic system of male rats: Effects of gonadectomy and caloric restriction. Endocrinology 2018, 159, 450–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huber, T.J.; Tettenborn, C.; Leifke, E.; Emrich, H.M. Sex hormones in psychotic men. Psychoneuroendocrinology 2005, 30, 111–114. [Google Scholar] [CrossRef]
- Taherianfard, M.; Shariaty, M. Evaluation of serum steroid hormones in schizophrenic patients. Indian J. Med. Sci. 2004, 58, 3–9. [Google Scholar] [PubMed]
- Redman, B.; Kitchen, C.; Johnson, K.W.; Bezwada, P.; Kelly, D.L. Levels of prolactin and testosterone and associated sexual dysfunction and breast abnormalities in men with schizophrenia treated with antipsychotic medications. J. Psychiatr. Res. 2021, 143, 50–53. [Google Scholar] [CrossRef]
- Moore, L.; Kyaw, M.; Vercammen, A.; Lenroot, R.; Kulkarni, J.; Curtis, J.; O’Donnell, M.; Carr, V.J.; Shannon Weickert, C.; Weickert, T.W. Serum testosterone levels are related to cognitive function in men with schizophrenia. Psychoneuroendocrinology 2013, 38, 1717–1728. [Google Scholar] [CrossRef]
- Allimuthu, P.; Nandeesha, H.; Chinniyappan, R.; Bhardwaz, B.; Blessed raj, J. Relationship of brain-derived neurotrophic factor with interleukin-23, testosterone and oisease severity in schizophrenia. Indian J. Clin. Biochem. 2021, 36, 365–369. [Google Scholar] [CrossRef]
- Riahi, F.; Izadi-Mazidi, M.; Ghaffari, A.; Yousefi, E.; Khademvatan, S. Comparison of plasma neurosteroid and prolactin levels in patients with schizophrenia and healthy individuals. Scientifica 2016, 2016, 3108689. [Google Scholar] [CrossRef] [Green Version]
- Goyal, R.O.; Sagar, R.; Ammini, A.C.; Khurana, M.L.; Alias, A.G. Negative correlation between negative symptoms of schizophrenia and testosterone levels. Ann. N. Y. Acad. Sci. 2004, 1032, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Sisek-Šprem, M.; Križaj, A.; Jukić, V.; Milošević, M.; Petrović, Z.; Herceg, M. Testosterone levels and clinical features of schizophrenia with emphasis on negative symptoms and aggression. Nord. J. Psychiatry 2015, 69, 102–109. [Google Scholar] [CrossRef]
- Albayrak, Y.; Beyazyuz, M.; Beyazyüz, E.; Unsal, C.; Göka, E. Increased serum dehydroepiandrosterone sulfate in the first episode but not in subsequent episodes in male patients with schizophrenia. Neuropsychiatr. Dis. Treat. 2014, 10, 687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nenezic, N.; Kostic, S.; Strac, D.S.; Grunauer, M.; Nenezic, D.; Radosavljevic, M.; Jancic, J.; Jancic, J. Dehydroepiandrosterone (DHEA): Pharmacological effects and potential therapeutic application. Mini-Rev. Med. Chem. 2022, 22. [Google Scholar] [CrossRef]
- Peng, R.; Li, Y. Association among serum cortisol, dehydroepiandrosterone-sulfate levels and psychiatric symptoms in men with chronic schizophrenia. Compr. Psychiatry 2017, 76, 113–118. [Google Scholar] [CrossRef]
- Strous, R.D. Dehydroepiandrosterone (DHEA) augmentation in the management of schizophrenia symptomatology. Essent. Psychopharmacol. 2005, 6, 141–147. [Google Scholar] [CrossRef]
- Avdibegović, E.; Hasanović, M. The stigma of mental illness and recovery. Psychiatr. Danub. 2017, 29, 900–905. [Google Scholar]
- Oexle, N.; Waldmann, T.; Staiger, T.; Xu, Z.; Rüsch, N. Mental illness stigma and suicidality: The role of public and individual stigma. Epidemiol. Psychiatr. Sci. 2018, 27, 169–175. [Google Scholar] [CrossRef]
- Bradbury, A. Mental health stigma: The impact of age and gender on attitudes. Community Ment. Health J. 2020, 56, 933–938. [Google Scholar] [CrossRef]
- Zahid, A.; Best, M.W. Stigma towards individuals with schizophrenia: Examining the effects of negative symptoms and diagnosis awareness on preference for social distance. Psychiatry Res. 2021, 297, 113724. [Google Scholar] [CrossRef]
- Dubreucq, J.; Plasse, J.; Franck, N. Self-stigma in Serious Mental Illness: A Systematic Review of Frequency, Correlates, and Consequences. Schizophr. Bull. 2021, 47, 1261–1287. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, K.; Millier, A.; Amri, I.; Aballéa, S.; Toumi, M. Association between social contact frequency and negative symptoms, psychosocial functioning and quality of life in patients with schizophrenia. Psychiatry Res. 2015, 230, 860–866. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nicolaides, N.C.; Kyratzi, E.; Lamprokostopoulou, A.; Chrousos, G.P.; Charmandari, E. Stress, the stress system and the role of glucocorticoids. Neuroimmunomodulation 2015, 22, 6–19. [Google Scholar] [CrossRef]
- Handa, R.J.; Weiser, M.J. Gonadal steroid hormones and the hypothalamo–pituitary–adrenal axis. Front. Neuroendocrinol. 2014, 35, 197–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zefferino, R.; Di Gioia, S.; Conese, M. Molecular links between endocrine, nervous and immune system during chronic stress. Brain Behav. 2021, 11, e01960. [Google Scholar] [CrossRef]
- Rivier, C.; Rivest, S. Effect of stress on the activity of the hypothalamic-pituitary-gonadal axis: Peripheral and central mechanisms. Biol. Reprod. 1991, 45, 523–532. [Google Scholar] [CrossRef]
- Barbarino, A.; Marinis, L.D.; Tofani, A.; Casa, S.D.; D’Amico, C.; Mancini, A.; Corsello, S.M.; Sciuto, R.; Barini, A. Corticotropin-releasing hormone inhibition of gonadotropin release and the effect of opioid blockade. J. Clin. Endocrinol. Metab. 1989, 68, 523–528. [Google Scholar] [CrossRef]
- Negro-Vilar, A. Stress and other environmental factors affecting fertility in men and women: Overview. Environ. Health Perspect. 1993, 101, 59–64. [Google Scholar] [CrossRef]
- Robinson, D.; Woerner, M.G.; Alvir, J.M.J.; Bilder, R.; Goldman, R.; Geisler, S.; Koreen, A.; Sheitman, B.; Chakos, M.; Mayerhoff, D.; et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch. Gen. Psychiatry 1999, 56, 241. [Google Scholar] [CrossRef]
- Hasan, A.; Falkai, P.; Wobrock, T.; Lieberman, J.; Glenthoj, B.; Gattaz, W.F.; Thibaut, F.; Möller, H.J.; Altamura, A.C.; Andreasen, N.; et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for biological treatment of schizophrenia, Part 2: Update 2012 on the long-term treatment of schizophrenia and management of antipsychotic-induced side effects. World J. Biol. Psychiatry 2013, 14, 2–44. [Google Scholar] [CrossRef]
- Leucht, S.; Huhn, M.; Davis, J.M. Should “typical”, first-generation antipsychotics no longer be generally used in the treatment of schizophrenia? Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 1411–1413. [Google Scholar] [CrossRef]
- Leucht, S.; Davis, J.M. Which first-generation antipsychotics should be “repurposed” for the treatment of schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 272, 1–3. [Google Scholar] [CrossRef]
- Nucifora, F.C.; Mihaljevic, M.; Lee, B.J.; Sawa, A. Clozapine as a model for antipsychotic development. Neurotherapeutics 2017, 14, 750–761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasan, A.; Falkai, P.; Wobrock, T.; Lieberman, J.; Glenthoj, B.; Gattaz, W.F.; Thibaut, F.; Möller, H.-J. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for biological treatment of schizophrenia, Part 1: Update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J. Biol. Psychiatry 2012, 13, 318–378. [Google Scholar] [CrossRef] [PubMed]
- Atkin, K.; Kendall, F.; Gould, D.; Freeman, H.; Lieberman, J.; O’Sullivan, D. Neutropenia and agranulocytosis in patients receiving clozapine in the UK and Ireland. Br. J. Psychiatry 1996, 169, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Albayrak, Y.; Beyazyüz, M.; Beyazyüz, E.; Kuloğlu, M. Increased serum prolactin levels in drug-naive first-episode male patients with schizophrenia. Nord. J. Psychiatry 2014, 68, 341–346. [Google Scholar] [CrossRef]
- Rizzo, L.F.L.; Mana, D.L.; Serra, H.A.; Danilowicz, K. Hyperprolactinemia associated with psychiatric disorders. Medicina 2020, 80, 670–680. [Google Scholar]
- Tasaki, M.; Yasui-Furukori, N.; Yokoyama, S.; Shinozaki, M.; Sugawara, N.; Shimoda, K. Hypoprolactinemia and hyperprolactinemia in male schizophrenia patients treated with aripiprazole and risperidone and their relationships with testosterone levels. Neuropsychopharmacol. Rep. 2021, 41, 379–384. [Google Scholar] [CrossRef]
- Capozzi, A.; Scambia, G.; Pontecorvi, A.; Lello, S. Hyperprolactinemia: Pathophysiology and therapeutic approach. Gynecol. Endocrinol. 2015, 31, 506–510. [Google Scholar] [CrossRef]
- di Filippo, L.; Doga, M.; Resmini, E.; Giustina, A. Hyperprolactinemia and bone. Pituitary 2020, 23, 314–321. [Google Scholar] [CrossRef]
- Dabbous, Z.; Atkin, S.L. Hyperprolactinaemia in male infertility: Clinical case scenarios. Arab J. Urol. 2018, 16, 44–52. [Google Scholar] [CrossRef] [Green Version]
- Segal, M.; Avital, A.; Rojas, M.; Hausvater, N.; Sandbank, S.; Liba, D.; Moguillansky, L.; Tal, I.; Weizman, A. Serum prolactin levels in unmedicated first-episode and recurrent schizophrenia patients: A possible marker for the disease’s subtypes. Psychiatry Res. 2004, 127, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Kuruvilla, A.; Peedicayil, J.; Srikrishna, G.; Kuruvilla, K.; Kanagasabapathy, A.S. A study of serum prolactin levels in schizophrenia: Comparison of males and females. Clin. Exp. Pharmacol. Physiol. 1992, 19, 603–606. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, A.; Johnston, M.; Bureau, Y.; Shah, N. Baseline serum prolactin in drug-naive, first-episode schizophrenia and outcome at five years: Is it a predictive factor? Innov. Clin. Neurosci. 2012, 9, 17–21. [Google Scholar] [PubMed]
- Riecher-Rössler, A.; Rybakowski, J.K.; Pflueger, M.O.; Beyrau, R.; Kahn, R.S.; Malik, P.; Fleischhacker, W.W. Hyperprolactinemia in antipsychotic-naive patients with first-episode psychosis. Psychol. Med. 2013, 43, 2571–2582. [Google Scholar] [CrossRef]
- Petruzzelli, M.G.; Margari, M.; Peschechera, A.; de Giambattista, C.; De Giacomo, A.; Matera, E.; Margari, F. Hyperprolactinemia and insulin resistance in drug naive patients with early onset first episode psychosis. BMC Psychiatry 2018, 18, 246. [Google Scholar] [CrossRef] [Green Version]
- González-Blanco, L.; Greenhalgh, A.M.D.; Garcia-Rizo, C.; Fernandez-Egea, E.; Miller, B.J.; Kirkpatrick, B. Prolactin concentrations in antipsychotic-naïve patients with schizophrenia and related disorders: A meta-analysis. Schizophr. Res. 2016, 174, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Del Cacho, N.; Butjosa, A.; Vila-Badia, R.; Cuadras, D.; Kaplan, M.; Rubio-Abadal, E.; Pardo, M.; Muñoz-Samons, D.; Cuevas-Esteban, J.; Saenz-Navarrete, G.; et al. Prolactin levels in drug-naïve first episode nonaffective psychosis patients compared with healthy controls. Sex differences. Psychiatry Res. 2019, 276, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Walter, A.; Studerus, E.; Smieskova, R.; Tamagni, C.; Rapp, C.; Borgwardt, S.J.; Riecher-Rössler, A. Pituitary gland volume in at-risk mental state for psychosis: A longitudinal MRI analysis. CNS Spectr. 2015, 20, 122–129. [Google Scholar] [CrossRef] [Green Version]
- Stahl, S.M. Psychosis and schizophrenia. In Stahl’s Essential Psychopharmacology: Neuroscientific Basis and Practical Applications; Cambridge University Press & Assessment: Cambridge, UK, 2013; pp. 79–128. ISBN 1107025982. [Google Scholar]
- Peuskens, J.; Pani, L.; Detraux, J.; De Hert, M. The effects of novel and newly approved antipsychotics on serum prolactin levels: A comprehensive review. CNS Drugs 2014, 28, 421–453. [Google Scholar] [CrossRef]
- Tsuboi, T.; Bies, R.R.; Suzuki, T.; Mamo, D.C.; Pollock, B.G.; Graff-Guerrero, A.; Mimura, M.; Uchida, H. Hyperprolactinemia and estimated dopamine D2 receptor occupancy in patients with schizophrenia: Analysis of the CATIE data. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2013, 45, 178–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tewksbury, A.; Olander, A. Management of antipsychotic-induced hyperprolactinemia. Ment. Health Clin. 2016, 6, 185–190. [Google Scholar] [CrossRef]
- Kapur, S. Relationship between dopamine D2 occupancy, clinical response, and side effects: A double-blind PET study of first-episode schizophrenia. Am. J. Psychiatry 2000, 157, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Kapur, S.; Seeman, P. Antipsychotic agents differ in how fast they come off the dopamine D2 receptors. Implications for atypical antipsychotic action. J. Psychiatry Neurosci. 2000, 25, 161–166. [Google Scholar]
- Kapur, S.; Seeman, P. Does fast dissociation from the dopamine D2 receptor explain the action of atypical antipsychotics?: A new hypothesis. Am. J. Psychiatry 2001, 158, 360–369. [Google Scholar] [CrossRef]
- Sykes, D.A.; Moore, H.; Stott, L.; Holliday, N.; Javitch, J.A.; Lane, J.R.; Charlton, S.J. Extrapyramidal side effects of antipsychotics are linked to their association kinetics at dopamine D2 receptors. Nat. Commun. 2017, 8, 763. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kato, Y.; Nakai, Y.; Imura, H.; Chihara, K.; Ohgo, S. Effect of 5-hydroxytryptophan (5-HTP) on plasma prolactin levels in man. J. Clin. Endocrinol. Metab. 1974, 38, 695–697. [Google Scholar] [CrossRef]
- Divac, N.; Prostran, M.; Jakovcevski, I.; Cerovac, N. Second-generation antipsychotics and extrapyramidal adverse effects. Biomed Res. Int. 2014, 2014, 656370. [Google Scholar] [CrossRef] [Green Version]
- Shim, J.-C.; Shin, J.-G.K.; Kelly, D.L.; Jung, D.-U.; Seo, Y.-S.; Liu, K.-H.; Shon, J.-H.; Conley, R.R. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: A placebo-controlled trial. Am. J. Psychiatry 2007, 164, 1404–1410. [Google Scholar] [CrossRef]
- Kusumi, I.; Boku, S.; Takahashi, Y. Psychopharmacology of atypical antipsychotic drugs: From the receptor binding profile to neuroprotection and neurogenesis. Psychiatry Clin. Neurosci. 2015, 69, 243–258. [Google Scholar] [CrossRef]
- Bushe, C.; Shaw, M.; Peveler, R.C. A review of the association between antipsychotic use and hyperprolactinaemia. J. Psychopharmacol. 2008, 22, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.-H.; Kang, S.-G.; Kim, T.-W.; Lee, H.-J.; Yoon, H.-K.; Park, Y.-M. Hyperprolactinemia induced by low-dosage amisulpride in Korean psychiatric patients. Psychiatry Clin. Neurosci. 2012, 66, 69–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corena-McLeod, M. Comparative pharmacology of risperidone and paliperidone. Drugs R & D 2015, 15, 163–174. [Google Scholar] [CrossRef] [Green Version]
- Kearns, A.E.; Goff, D.C.; Hayden, D.L.; Daniels, G.H. Risperidone-associated hyperprolactinemia. Endocr. Pract. 2000, 6, 425–429. [Google Scholar] [CrossRef]
- Paparrigopoulos, T.; Liappas, J.; Tzavellas, E.; Mourikis, I.; Soldatos, C. Amisulpride-induced hyperprolactinemia is reversible following discontinuation. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2007, 31, 92–96. [Google Scholar] [CrossRef]
- Wang, J.-S.; Ruan, Y.; Taylor, R.M.; Donovan, J.L.; Markowitz, J.S.; DeVane, C.L. The brain entry of risperidone and 9-hydroxyrisperidone is greatly limited by P-glycoprotein. Int. J. Neuropsychopharmacol. 2004, 7, 415–419. [Google Scholar] [CrossRef] [Green Version]
- Leucht, S.; Cipriani, A.; Spineli, L.; Mavridis, D.; Örey, D.; Richter, F.; Samara, M.; Barbui, C.; Engel, R.R.; Geddes, J.R.; et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. Lancet 2013, 382, 951–962. [Google Scholar] [CrossRef]
- Ajmal, A.; Joffe, H.; Nachtigall, L.B. Psychotropic-induced hyperprolactinemia: A clinical review. Psychosomatics 2014, 55, 29–36. [Google Scholar] [CrossRef]
- The American Psychiatric Association Practice Guideline for the Treatment of Patients with Schizophrenia; American Psychiatric Association Publishing: Washington, DC, USA, 2020; ISBN 0-89042-484-5.
- Allison, D.B.; Fontaine, K.R.; Heo, M.; Mentore, J.L.; Cappelleri, J.C.; Chandler, L.P.; Weiden, P.J.; Cheskin, L.J. The distribution of body mass index among individuals with and without schizophrenia. J. Clin. Psychiatry 1999, 60, 215–220. [Google Scholar] [CrossRef]
- Elman, I.; Borsook, D.; Lukas, S.E. Food intake and reward mechanisms in patients with schizophrenia: Implications for metabolic disturbances and treatment with second-generation antipsychotic agents. Neuropsychopharmacology 2006, 31, 2091–2120. [Google Scholar] [CrossRef] [Green Version]
- Jonikas, J.A.; Cook, J.A.; Razzano, L.A.; Steigman, P.J.; Hamilton, M.M.; Swarbrick, M.A.; Santos, A. Associations between gender and obesity among adults with mental illnesses in a Community Health Screening Study. Community Ment. Health J. 2016, 52, 406–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coodin, S. Body mass index in persons with schizophrenia. Can. J. Psychiatry 2001, 46, 549–555. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Werneck, A.O.; Vancampfort, D.; Oyeyemi, A.L.; Szwarcwald, C.L.; Stubbs, B.; Silva, D.R. Lifestyle behaviors among 4343 Brazilian adults with severe mental illness and 55,859 general population controls: Data from the Brazilian National Health Survey. Braz. J. Psychiatry 2020, 42, 245–249. [Google Scholar] [CrossRef] [Green Version]
- Porcelli, S.; Van Der Wee, N.; van der Werff, S.; Aghajani, M.; Glennon, J.C.; van Heukelum, S.; Mogavero, F.; Lobo, A.; Olivera, F.J.; Lobo, E.; et al. Social brain, social dysfunction and social withdrawal. Neurosci. Biobehav. Rev. 2019, 97, 10–33. [Google Scholar] [CrossRef]
- Vancampfort, D.; Firth, J.; Schuch, F.B.; Rosenbaum, S.; Mugisha, J.; Hallgren, M.; Probst, M.; Ward, P.B.; Gaughran, F.; De Hert, M.; et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: A global systematic review and meta-analysis. World Psychiatry 2017, 16, 308–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dipasquale, S.; Pariante, C.M.; Dazzan, P.; Aguglia, E.; McGuire, P.; Mondelli, V. The dietary pattern of patients with schizophrenia: A systematic review. J. Psychiatr. Res. 2013, 47, 197–207. [Google Scholar] [CrossRef] [Green Version]
- Kalinowska, S.; Trześniowska-Drukała, B.; Kłoda, K.; Safranow, K.; Misiak, B.; Cyran, A.; Samochowiec, J. The association between lifestyle choices and schizophrenia symptoms. J. Clin. Med. 2021, 10, 165. [Google Scholar] [CrossRef]
- Baptista, T.; Lacruz, A.; Angeles, F.; Silvera, R.; de Mendoza, S.; Mendoza, M.; Hernández, L. Endocrine and metabolic abnormalities involved in obesity associated with typical antipsychotic drug administration. Pharmacopsychiatry 2001, 34, 223–231. [Google Scholar] [CrossRef]
- Wetterling, T.; Müssigbrodt, H.E. Weight gain: Side effect of atypical neuroleptics? J. Clin. Psychopharmacol. 1999, 19, 316–321. [Google Scholar] [CrossRef]
- Wichniak, A.; Dudek, D.; Heitzman, J.; Kapłon-Cieślicka, A.; Mamcarz, A.; Samochowiec, J.; Szulc, A.; Bieńkowski, P. Metabolic risk reduction in patients with schizophrenia treated with antipsychotics: Recommendations of the Polish Psychiatric Association. Psychiatr. Pol. 2019, 53, 1191–1218. [Google Scholar] [CrossRef]
- Lech, M.; Ostrowska, L. Obesity in patients with schizophrenia. Forum Zaburzeń Metab. 2015, 6, 103–111. [Google Scholar]
- Vermeulen, A.; Kaufman, J.M.; Deslypere, J.P.; Thomas, G. Attenuated luteinizing hormone (LH) pulse amplitude but normal LH pulse frequency, and its relation to plasma androgens in hypogonadism of obese men. J. Clin. Endocrinol. Metab. 1993, 76, 1140–1146. [Google Scholar] [CrossRef] [PubMed]
- Glass, A.R.; Swerdloff, R.S.; Bray, G.A.; Dahms, W.T.; Atkinson, R.L. Low serum testosterone and sex-hormone-binding-globulin in massively obese men. J. Clin. Endocrinol. Metab. 1977, 45, 1211–1219. [Google Scholar] [CrossRef] [PubMed]
- Stárka, L.; Hill, M.; Pospíšilová, H.; Dušková, M. Estradiol, obesity and hypogonadism. Physiol. Res. 2020, 69, S273–S278. [Google Scholar] [CrossRef] [PubMed]
- Oztekin, U.; Caniklioglu, M.; Sari, S.; Gurel, A.; Selmi, V.; Isikay, L. The impact of body mass index on reproductive hormones, testosterone/estradiol ratio and semen parameters. Cent. Eur. J. Urol. 2020, 73, 226–230. [Google Scholar] [CrossRef]
- Fejes, I.; Koloszár, S.; Závaczki, Z.; Daru, J.; Szöllösi, J.; Pál, A. Effect of body weight on testosterone/estradiol ratio in oligozoospermic patients. Arch. Androl. 2006, 52, 97–102. [Google Scholar] [CrossRef] [Green Version]
- Clavijo, R.I.; Hsiao, W. Update on male reproductive endocrinology. Transl. Androl. Urol. 2018, 7, S367–S372. [Google Scholar] [CrossRef]
- Kelly, D.M.; Jones, T.H. Testosterone and obesity. Obes. Rev. 2015, 16, 581–606. [Google Scholar] [CrossRef]
- Al-Harithy, R.N. Relationship of leptin concentration to gender, body mass index and age in Saudi adults. Saudi Med. J. 2004, 25, 1086–1090. [Google Scholar]
- Leisegang, K.; Bouic, P.J.; Menkveld, R.; Henkel, R.R. Obesity is associated with increased seminal insulin and leptin alongside reduced fertility parameters in a controlled male cohort. Reprod. Biol. Endocrinol. 2014, 12, 34. [Google Scholar] [CrossRef] [Green Version]
- Childs, G.V.; Odle, A.K.; MacNicol, M.C.; MacNicol, A.M. The importance of leptin to reproduction. Endocrinology 2021, 162, bqaa204. [Google Scholar] [CrossRef]
- Barber, T.M.; Kyrou, I.; Kaltsas, G.; Grossman, A.B.; Randeva, H.S.; Weickert, M.O. Mechanisms of central hypogonadism. Int. J. Mol. Sci. 2021, 22, 8217. [Google Scholar] [CrossRef] [PubMed]
- Kahn, B.E.; Brannigan, R.E. Obesity and male infertility. Curr. Opin. Urol. 2017, 27, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Kozakowski, J.; Dudek, P. Impairment of male fertility—A consequential problem of our time. The impact of obesity and related metabolic disorders. Postępy Nauk Med. 2017, 30, 674–678. [Google Scholar] [CrossRef]
- Caprio, M.; Isidori, A.M.; Carta, A.R.; Moretti, C.; Dufau, M.L.; Fabbri, A. Expression of functional leptin receptors in rodent Leydig cells. Endocrinology 1999, 140, 4939–4947. [Google Scholar] [CrossRef]
- Landry, D.A.; Sormany, F.; Haché, J.; Roumaud, P.; Martin, L.J. Steroidogenic genes expressions are repressed by high levels of leptin and the JAK/STAT signaling pathway in MA-10 Leydig cells. Mol. Cell. Biochem. 2017, 433, 79–95. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Vancampfort, D.; De Herdt, A.; Yu, W.; De Hert, M. Is the prevalence of metabolic syndrome and metabolic abnormalities increased in early schizophrenia? A comparative meta-analysis of first episode, untreated and treated patients. Schizophr. Bull. 2013, 39, 295–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guest, P.C. Insulin resistance in schizophrenia. In Reviews on Biomarker Studies of Metabolic and Metabolism-Related Disorders. Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2019; Volume 1134, pp. 1–16. ISBN 978-3-030-12668-1. [Google Scholar]
- Ahmed, B.; Sultana, R.; Greene, M.W. Adipose tissue and insulin resistance in obese. Biomed. Pharmacother. 2021, 137, 111315. [Google Scholar] [CrossRef]
- Ebbert, J.; Jensen, M. Fat depots, free fatty acids, and dyslipidemia. Nutrients 2013, 5, 498–508. [Google Scholar] [CrossRef] [Green Version]
- Polyzos, S.A.; Kountouras, J.; Mantzoros, C.S. Obesity and nonalcoholic fatty liver disease: From pathophysiology to therapeutics. Metabolism 2019, 92, 82–97. [Google Scholar] [CrossRef]
- Winters, S.J.; Scoggins, C.R.; Appiah, D.; Ghooray, D.T. The hepatic lipidome and HNF4α and SHBG expression in human liver. Endocr. Connect. 2020, 9, 1009–1018. [Google Scholar] [CrossRef] [PubMed]
- Kotronen, A.; Yki-Järvinen, H. Fatty liver. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Simó, R.; Sáez-López, C.; Barbosa-Desongles, A.; Hernández, C.; Selva, D.M. Novel insights in SHBG regulation and clinical implications. Trends Endocrinol. Metab. 2015, 26, 376–383. [Google Scholar] [CrossRef]
- Tekin Uludag, Y.; Gulenc, G. Prevalence of substance use in patients diagnosed with schizophrenia. Noro Psikiyatr. Ars. 2016, 53, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Thoma, P.; Daum, I. Comorbid substance use disorder in schizophrenia: A selective overview of neurobiological and cognitive underpinnings. Psychiatry Clin. Neurosci. 2013, 67, 367–383. [Google Scholar] [CrossRef]
- Hunt, G.E.; Large, M.M.; Cleary, M.; Lai, H.M.X.; Saunders, J.B. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990–2017: Systematic review and meta-analysis. Drug Alcohol Depend. 2018, 191, 234–258. [Google Scholar] [CrossRef] [PubMed]
- Drake, R.E.; Mueser, K.T. Co-occurring alcohol use disorder and schizophrenia. Alcohol Res. Health 2002, 26, 99–101. [Google Scholar]
- Archibald, L. Alcohol use disorder and schizophrenia and schizoaffective disorders. Alcohol Res. Curr. Rev. 2019, 40, e1–e9. [Google Scholar] [CrossRef]
- Batel, P. Addiction and schizophrenia. Eur. Psychiatry 2000, 15, 115–122. [Google Scholar] [CrossRef]
- Carney, C.P.; Jones, L.; Woolson, R.F. Medical comorbidity in women and men with schizophrenia. J. Gen. Intern. Med. 2006, 21, 1133–1137. [Google Scholar] [CrossRef]
- Fuller, B.E.; Rodriguez, V.L.; Linke, A.; Sikirica, M.; Dirani, R.; Hauser, P. Prevalence of liver disease in veterans with bipolar disorder or schizophrenia. Gen. Hosp. Psychiatry 2011, 33, 232–237. [Google Scholar] [CrossRef] [Green Version]
- Hsu, J.-H.; Chien, I.-C.; Lin, C.-H.; Chou, Y.-J.; Chou, P. Increased risk of chronic liver disease in patients with schizophrenia: A population-based cohort study. Psychosomatics 2014, 55, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Grant, R.K.; Brindle, W.M.; Donnelly, M.C.; McConville, P.M.; Stroud, T.G.; Bandieri, L.; Plevris, J.N. Gastrointestinal and liver disease in patients with schizophrenia: A narrative review. World J. Gastroenterol. 2022, 28, 5515–5529. [Google Scholar] [CrossRef]
- Emanuele, N.V.; LaPaglia, N.; Steiner, J.; Colantoni, A.; Van Thiel, D.H.; Emanuele, M.A. Peripubertal paternal EtOH exposure: Testicular oxidative injury, fecundity, and offspring. Endocrine 2001, 14, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Emanuele, M.A.; Emanuele, N.V. Alcohols effects on male reproduction. Alcohol Res. Health 1998, 22, 195–201. [Google Scholar]
- Duca, Y.; Aversa, A.; Condorelli, R.A.; Calogero, A.E.; La Vignera, S. Substance abuse and male hypogonadism. J. Clin. Med. 2019, 8, 732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ceni, E.; Mello, T.; Galli, A. Pathogenesis of alcoholic liver disease: Role of oxidative metabolism. World J. Gastroenterol. 2014, 20, 17756–17772. [Google Scholar] [CrossRef]
- Cederbaum, A.I.; Lu, Y.; Wu, D. Role of oxidative stress in alcohol-induced liver injury. Arch. Toxicol. 2009, 83, 519–548. [Google Scholar] [CrossRef]
- Li, S.; Tan, H.-Y.; Wang, N.; Zhang, Z.-J.; Lao, L.; Wong, C.-W.; Feng, Y. The role of oxidative stress and antioxidants in liver diseases. Int. J. Mol. Sci. 2015, 16, 26087–26124. [Google Scholar] [CrossRef] [Green Version]
- Siervo, G.E.M.L.; Vieira, H.R.; Ogo, F.M.; Fernandez, C.D.B.; Gonçalves, G.D.; Mesquita, S.F.P.; Anselmo-Franci, J.A.; Cecchini, R.; Guarnier, F.A.; Fernandes, G.S.A. Spermatic and testicular damages in rats exposed to ethanol: Influence of lipid peroxidation but not testosterone. Toxicology 2015, 330, 1–8. [Google Scholar] [CrossRef]
- Reddy, V.D.; Padmavathi, P.; Kavitha, G.; Saradamma, B.; Varadacharyulu, N. Alcohol-induced oxidative/nitrosative stress alters brain mitochondrial membrane properties. Mol. Cell. Biochem. 2012, 375, 39–47. [Google Scholar] [CrossRef]
- Adams, M.L.; Cicero, T.J. Effects of alcohol on beta-endorphin and reproductive hormones in the male rat. Alcohol. Clin. Exp. Res. 1991, 15, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Gianoulakis, C. Characterization of the effects of acute ethanol administration on the release of β-endorphin peptides by the rat hypothalamus. Eur. J. Pharmacol. 1990, 180, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Emanuele, M.A.; Emanuele, N. Alcohol and the male reproductive system. Alcohol Res. Health 2001, 25, 282–287. [Google Scholar] [PubMed]
- Chiao, Y.-B.; Van Thiel, D.H. Biochemical mechanisms that contribute to alcohol-induced hypogonadism in the male. Alcohol. Clin. Exp. Res. 1983, 7, 131–134. [Google Scholar] [CrossRef]
- Jana, K.; Jana, N.; De, D.K.; Guha, S.K. Ethanol induces mouse spermatogenic cell apoptosis in vivo through over-expression of Fas/Fas-L, p53, and caspase-3 along with cytochrome C translocation and glutathione depletion. Mol. Reprod. Dev. 2010, 77, 820–833. [Google Scholar] [CrossRef]
- Bhasin, S.; Brito, J.P.; Cunningham, G.R.; Hayes, F.J.; Hodis, H.N.; Matsumoto, A.M.; Snyder, P.J.; Swerdloff, R.S.; Wu, F.C.; Yialamas, M.A. Testosterone therapy in men with hypogonadism: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2018, 103, 1715–1744. [Google Scholar] [CrossRef] [Green Version]
- Rachdaoui, N.; Sarkar, D.K. Pathophysiology of the effects of alcohol abuse on the endocrine system. Alcohol Res. Curr. Rev. 2017, 38, 255–276. [Google Scholar]
- Karagiannis, A.; Harsoulis, F. Gonadal dysfunction in systemic diseases. Eur. J. Endocrinol. 2005, 152, 501–513. [Google Scholar] [CrossRef] [Green Version]
- Sinclair, M.; Grossmann, M.; Gow, P.J.; Angus, P.W. Testosterone in men with advanced liver disease: Abnormalities and implications. J. Gastroenterol. Hepatol. 2015, 30, 244–251. [Google Scholar] [CrossRef]
- Kim, S.M.; Yalamanchi, S.; Dobs, A.S. Male hypogonadism and liver disease. In Male Hypogonadism; Springer International Publishing: Cham, Switzerland, 2017; pp. 219–234. ISBN 978-3-319-53298-1. [Google Scholar]
- Ray, G.; Bhargav, P.M. A study of hormonal abnormalities in chronic liver disease. J. Assoc. Physicians India 2019, 67, 47–52. [Google Scholar] [PubMed]
- Zietz, B.; Lock, G.; Plach, B.; Drobnik, W.; Grossmann, J.; Schölmerich, J.; Straub, R.H. Dysfunction of the hypothalamic-pituitary-glandular axes and relation to Child-Pugh classification in male patients with alcoholic and virus-related cirrhosis. Eur. J. Gastroenterol. Hepatol. 2003, 15, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Handelsman, D.J.; Strasser, S.; McDonald, J.A.; Conway, A.J.; McCaughan, G.W. Hypothalamic-pituitary-testicular function in end-stage non-alcoholic liver disease before and after liver transplantation. Clin. Endocrinol. 1995, 43, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Burke, C.W.; Anderson, D.C. Sex-hormone-binding globulin is an oestrogen amplifier. Nature 1972, 240, 38–40. [Google Scholar] [CrossRef]


| First-Generation Antipsychotics (FGAs) (Selected) | Second-Generation Antipsychotics (SGAs) (Selected) |
|---|---|
| Chlorpromazine | Amisulpride |
| Clopenthixol | Aripiprazole |
| Flupentixol | Asenapine |
| Fluphenazine | Clozapine |
| Haloperidol | Iloperidone |
| Levomepromazine | Lurasidone |
| Loxapine | Olanzapine |
| Molindone | Paliperidone |
| Perazine | Quetiapine |
| Perphenazine | Risperidone |
| Pimozide | Sertindole |
| Sulpiride | Ziprasidone |
| Thioridazine | |
| Trifluoperazine | |
| Zuclopenthixol |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matuszewska, A.; Kowalski, K.; Jawień, P.; Tomkalski, T.; Gaweł-Dąbrowska, D.; Merwid-Ląd, A.; Szeląg, E.; Błaszczak, K.; Wiatrak, B.; Danielewski, M.; et al. The Hypothalamic-Pituitary-Gonadal Axis in Men with Schizophrenia. Int. J. Mol. Sci. 2023, 24, 6492. https://doi.org/10.3390/ijms24076492
Matuszewska A, Kowalski K, Jawień P, Tomkalski T, Gaweł-Dąbrowska D, Merwid-Ląd A, Szeląg E, Błaszczak K, Wiatrak B, Danielewski M, et al. The Hypothalamic-Pituitary-Gonadal Axis in Men with Schizophrenia. International Journal of Molecular Sciences. 2023; 24(7):6492. https://doi.org/10.3390/ijms24076492
Chicago/Turabian StyleMatuszewska, Agnieszka, Krzysztof Kowalski, Paulina Jawień, Tomasz Tomkalski, Dagmara Gaweł-Dąbrowska, Anna Merwid-Ląd, Ewa Szeląg, Karolina Błaszczak, Benita Wiatrak, Maciej Danielewski, and et al. 2023. "The Hypothalamic-Pituitary-Gonadal Axis in Men with Schizophrenia" International Journal of Molecular Sciences 24, no. 7: 6492. https://doi.org/10.3390/ijms24076492





