Organophosphorus Poisoning: Acute Respiratory Distress Syndrome (ARDS) and Cardiac Failure as Cause of Death in Hospitalized Patients
Abstract
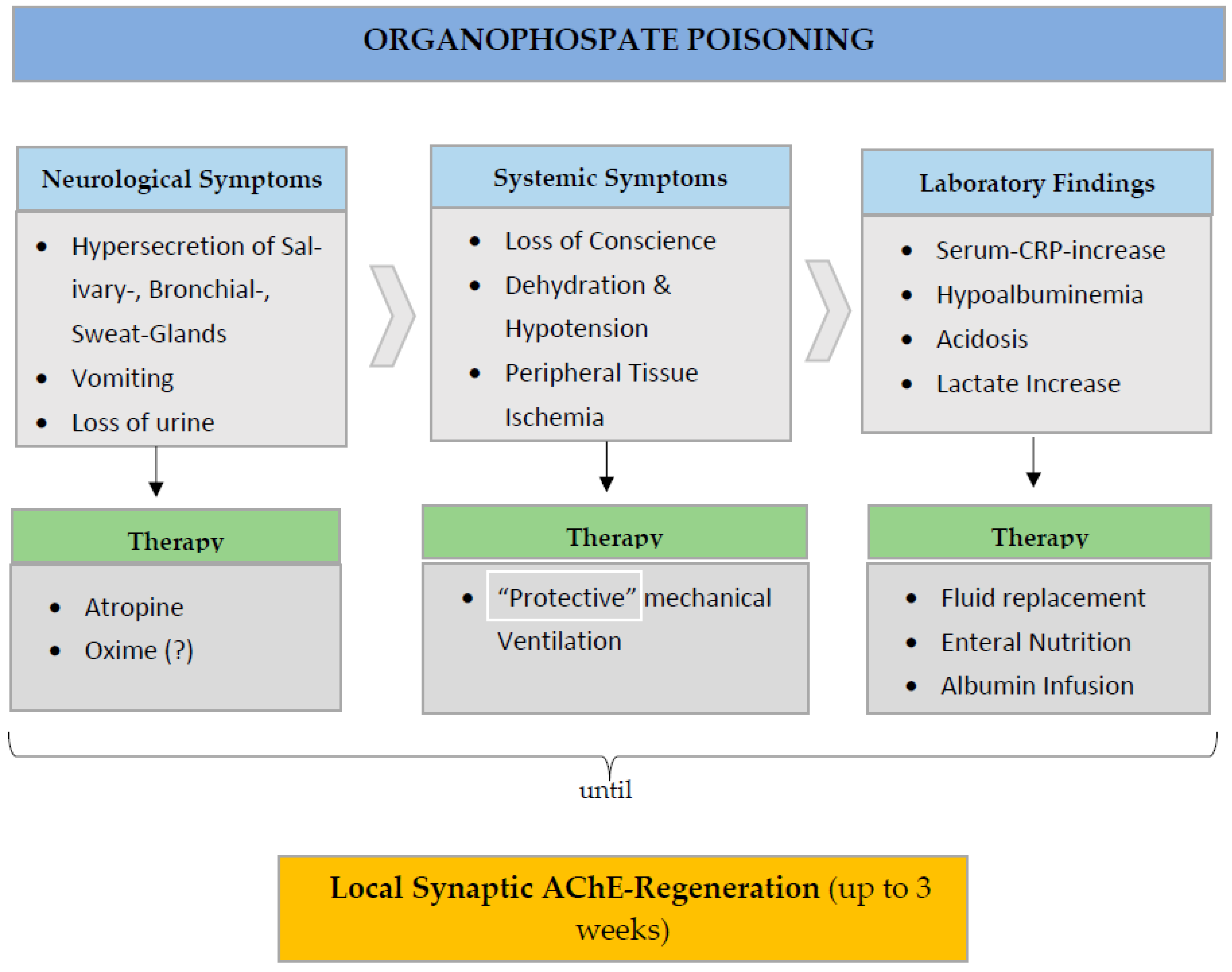
1. Introduction
2. Organophosphorus Compounds as Insecticides and as Nerve Agents
3. Acetylcholinesterase and Albumin Measurement: Importance for Diagnosis and Therapy
3.1. Acetylcholinesterase
3.2. Albumin
3.2.1. Pathophysiology
3.2.2. Albumin, Age, Blood Volume: The Basis for Defense against Homeostasis Disturbances
3.2.3. Hypoalbuminemia and Acute-Phase Reaction Markers in Insecticide Intoxication: Analysis of Possible Therapeutic Consequences
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wagner, D.L.; Grames, E.M.; Forister, M.L.; Berenbaum, M.R.; Stopak, D. Insect decline in the Antropocene:Death by a thousand cuts. Proc. Natl. Acad. Sci. USA 2021, 118, e2023989118. [Google Scholar] [CrossRef]
- Haider, N.; Rothman-Ostrow, P.; Osman, A.Y.; Arruda, L.B.; Macfarlane-Berry, L.; Elton, L.; Thomason, M.J.; Yeboah-Manu, D.; Ansumana, R.; Kapata, N.; et al. COVID-19-zoonosis or emerging infectious disease? Front. Public Health 2020, 8, 596944. [Google Scholar] [CrossRef]
- Mollentze, N.; Streicker, D.G. Viral zoonotic risk is homogenous among taxonomic orders of mammalian and avian reservoir hosts. Proc. Natl. Acad. Sci. USA 2020, 117, 9423–9430. [Google Scholar] [CrossRef]
- Randolph, D.G.; Refisch, J.; McMillan, S.; Wright, C.Y.; Bett, B.; Robinson, D.; Wernecke, B.; Lee, H.S.; Karesh, W.B.; Machalaba, C.; et al. Preventing the Next Pandemic. Zoonotic Diseases and How to Break the Chain of Transmission; UNEP’s Frontiers Report Series; United Nations Environment Programme (UNEP): Nairobi, Kenya, 2020. [Google Scholar]
- Igbedioh, S.O. Effects of agricultural pesticides on humans, animals and higher plants in developing countries. Arch. Environ. Health Int. J. 1991, 46, 218–224. [Google Scholar] [CrossRef]
- Gunnell, D.; Eddleston, M.; Phillips, M.R.; Konradsen, F. The global distribution of fatal pesticides self-poisoning: Systematic review. BMC Public Health 2007, 7, 357. [Google Scholar] [CrossRef]
- Patel, V.; Ramasundarahettige, C.; Vijayakumar, L.; Thakur, J.; Gajalakshmi, V.; Gururaj, G.; Suraweera, W.; Jha, P. Suicide mortality in India: A nationally representative survey. Lancet 2012, 379, 2343–2351. [Google Scholar] [CrossRef] [PubMed]
- Dar, M.A.; Kaushik, G.; Villareal Chiu, J.F. Pollution status and biodegradation of organophosphate pesticides in environment. In Abatement of Environmental Pollutants; Singh, P., Kumar, A., Borthakur, A., Eds.; Elsevier Inc.: Amsterdam, The Netherlands, 2019; pp. 25–66. [Google Scholar]
- The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification, 2019 Edition. Available online: https://www.who.int/publications/i/item/9789240005662 (accessed on 1 May 2020).
- Calvert, G.M.; Beckman, J.; Prado, J.B.; Bojes, H.; Schwartz, A.; Mulay, P.; Leinenkugel, K.; Higgins, S.; Lackovic, M.; Waltz, J.; et al. Acute occupational Pesticide-related illness and injury-United States, 2007–2011. Morb. Mortal. Wkly. Rep. 2016, 63, 11–16. [Google Scholar] [CrossRef]
- Namulanda, G.; Monti, M.M.; Mulay, P.; Higgins, S.; Lackovic, M.; Schwartz, A.; Prado, J.B.; Waltz, J.; Mitchell, Y.; Calvert, G.M. Acute nonoccupational Pesticide-related illness and injury-United States, 2007–2011. Morb. Mortal. Wkly. Rep. 2016, 63, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Mauer, M.P.; Rosales, R.; Sievert, J.; Thomsen, C. Surveillance for acute insecticide-related illness associated with mosquito-control efforts-Nine States,1999–2002. Morb. Mortal. Wkly. Rep. 2003, 52, 629–634. [Google Scholar]
- Snodgrass, W.R. Diagnosis and Treatment of Poisoning Due to Pesticides. In Hayes’ Handbook of Pesticide Toxicology; Chapter 60; Elsevier Inc.: Amsterdam, The Netherlands, 2015; pp. 1295–1311. [Google Scholar]
- Eddleston, M.; A Buckley, N.; Eyer, P.; Dawson, A.H. Medical management of acute organophosphorus pesticide poisoning. Lancet 2008, 371, 597–607. [Google Scholar] [CrossRef] [PubMed]
- Roberts, D.M.; Aaron, C.K. Managing acute organophosphorus pesticide poisoning. Br. Med. J. 2007, 334, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Dong, N.; Wang, S.; Li, X.; Li, W.; Gao, N.; Pang, L.; Xing, J. Prognostic nomogram for the severity of acute organophosphate insecticide self-poisoning: A retrospective observational cohort study. BMJ Open 2021, 11, e042765. [Google Scholar] [CrossRef] [PubMed]
- Sanjeev, R.K.; Pawar, M.N.; Sharma, D. A retrospective observational study of accidental carbamate poisoning among children referred to a tertiary care center in rural Maharashtra, India. Int. J. Med. Toxicol. Forensic Med. 2019, 9, 141–150. [Google Scholar] [CrossRef]
- Abdel-Satar, M.F.; Magdi, M.M.; Abdel Ghany, E.A.; Galal, D. A case study of neonatal Organophosphate Poisoning presented as acute respiratory distress. Egypt. J. Forensic Sci. Appl. Toxicol. 2022, 22, 27–31. [Google Scholar] [CrossRef]
- Baseer, K.A.A.; Gad, E.F.; Raheem, Y.F.A. Clinical profile and outcome of acute organophosphate poisoning in children of Upper Egypt: A cross-sectional study. BMC Pediatr. 2021, 21, 98. [Google Scholar] [CrossRef]
- Rosane, O. Pesticide Food Poisoning Suspected as 10 Die after Funeral in Peru. EcoWatch, 9 August 2018. [Google Scholar]
- Kwesiga, B.; Ario, A.R.; Bulage, L.; Harris, J.; Zhu, B.-P. Fatal cases associated with eating chapatti contaminated with organophosphate in Tororo District, Eatsern Uganda, 2015: Case series. BMC Public Health 2019, 19, 767. [Google Scholar] [CrossRef]
- Balme, K.H.; Roberts, J.C.; Glasstone, M.; Curling, L.; Rother, H.-A.; London, L.; Zar, H.; Mann, M.D. Pesticide poisoning at a tertiary children’s hospital in South Africa: An increasing problem. Clin. Toxicol. 2010, 48, 928–934. [Google Scholar] [CrossRef]
- Yousef, A.; Albuali, W.; Al Omari, M.; AlMutairi, A.; Albuali, H.W.; AlQurashi, F.O.; Alshaqaq, H.M. Organophosphate Poisoning in a pediatric intensive Care Unit: A retrospective Analysis Based on Ten Years of Experience. Int. J. Gen. Med. 2022, 12, 16513. [Google Scholar] [CrossRef]
- El-Nahhal, Y. Successful management of carbamate poisoning among children: Case report from Gaza Strip. Occup. Dis. Environ. Med. 2018, 6, 95–106. [Google Scholar] [CrossRef]
- McConnell, R.; Hruska, A.J. An epidemic of pesticide poisoning in Nicaragua:Inplications for prevention in developing countries. Am. J. Public Health 1993, 83, 1559–1562. [Google Scholar] [CrossRef]
- Jara, E.A.; Winter, C.K. Safety levels for organophosphate pesticide residues on fruits, vegetables and nuts. Int. J. Food Contam. 2019, 6, 6. [Google Scholar] [CrossRef]
- Boedeker, W.; Watts, M.; Clausing, P.; Marquez, E. The global distribution of acute unintentional pesticide poisoning: Estimations based on a systemic review. BMC Public Health 2020, 20, 1875. [Google Scholar] [CrossRef]
- Sinha, S.N.; Kumpati, R.K.; Ramavath, P.N.; Sangaraju, R.; Gouda, B.; Chougule, P. Investigation of acute organophosphate poisoning in humans based on sociodemographic and role of neurotransmitters with survival study in South India. Sci. Rep. 2022, 12, 16513. [Google Scholar] [CrossRef]
- Calvert, G.M.; Rodriguez, L.; Prado, J.B. Worker illness related to newly marketed pesticides-Douglas County, Washington. Morb. Mortal. Wkly. Rep. 2015, 64, 42–44. [Google Scholar]
- Hrabetz, H.; Thiermann, H.; Felgenhauer, N.; Zilker, T.; Haller, B.; Nährig, J.; Saugel, B.; Eyer, F. Organophosphate poisoning in the developed world. A single center experience from here to the Millenium. Chem. Biol. Interact. 2013, 206, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Ames, R.G.; Steenland, K.; Jenkins, B.; Chrislip, D.; Russo, J. Chronic Neurologic Sequelae to Cholinesterase Inhibition among Agricultural Pesticide Applicators. Arch. Environ. Health Int. J. 1995, 50, 440–444. [Google Scholar] [CrossRef] [PubMed]
- VoPham, T.; Bertrand, K.A.; Hart, J.E.; Laden, F.; Brooks, M.M.; Yuan, J.-M.; Talbott, E.O.; Ruddell, D.; Chang, C.-C.H.; Weissfeld, J.L. Pesticide exposure and liver cancer: A review. Cancer Causes Control 2017, 28, 177–190. [Google Scholar] [CrossRef] [PubMed]
- Saad-Hussein, A.; Beshir, S.; Taha, M.M.; Shahy, E.M.; Shaheen, W.; Abdel-Shafy, E.A.; Thabet, E. Early prediction of liver carcinogenicity due to occupational exposure to pesticides. Mutat. Res. Toxicol. Environ. Mutagen. 2019, 838, 46–53. [Google Scholar] [CrossRef]
- Niu, J.; Lin, Y.; Guo, Z.; Niu, M.; Su, C. The epidemiological investigation on the risk factors of hepatocellular carcinoma. A case control study in sudest China. Medicine 2016, 95, e2758. [Google Scholar] [CrossRef]
- Lodovici, M.; Casalini, C.; Briani, C.; Dolara, P. Oxidative liver DNA damage in rats treated with pesticide mixture. Toxicology 1997, 117, 55–60. [Google Scholar] [CrossRef]
- Lake, B.G.; Price, R.J.; Osimitz, T.G. Mode of action analysis for pesticide-induced rodent liver tumors involving activation of the constitutive androstone receptor: Relevance to human cancer risk. Pest Manag. Sci. 2014, 71, 829–834. [Google Scholar] [CrossRef]
- Banday, T.H.; Desai, M.S.; Naik, V.; Tathineni, B. Predictors of morbidity and mortality in organophosphorus poisoning: A Case study in rural Hospital in Karnataka, India. N. Am. J. Med. Sci. 2015, 7, 259–265. [Google Scholar] [CrossRef]
- Eddleston, M. Novel clinical toxicology and pharmacology of organophosphorus insecticide self-poisoning. Annu. Rev. Pharmacol. Toxicol. 2019, 59, 341–360. [Google Scholar] [CrossRef] [PubMed]
- Senanayake, N.; de Silva, H.J.; Narang, U.; Narang, P.; Gupta, O.P. Organophosphorus poisoning: A social calamity. J. Mahatma Gandhi Inst. Med. Sci. 2015, 20, 46–51. [Google Scholar] [CrossRef]
- Senanayake, N.; De Silva, H.; Karalliedde, L. A scale to assess severity in organophosphorus intoxication: POP Scale. Hum. Exp. Toxicol. 1993, 12, 297–299. [Google Scholar] [CrossRef]
- Lockridge, O.; Schopfer, L.M.; Masson, P. Biomarker of exposure to organophosphorus poisons: A new motif for covalent binding to tyrosine in proteins that have no active site serine. In Enciclopedia of Food and Health; Chapter 64; Elsevier Inc.: Amsterdam, The Netherlands, 2016; pp. 953–965. [Google Scholar]
- Pope, C.N.; Brimijoin, S. Cholinesterase and the fine line between poison and remedy. Biochem. Pharmacol. 2018, 153, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, J.N.; Keifer, M.C.; De Roos, A.J.; A Fenske, R.; E Furlong, C.; Van Belle, G.; Checkoway, H. Occupational determinants of serum cholinesterase inhibition among organophosphate-exposed agricultural pesticide handlers in Washington State. Occup. Environ. Med. 2009, 67, 375–386. [Google Scholar] [CrossRef]
- Thiermann, H.; Mast, U.; Klimmek, R.; Eyer, P.; Hibler, A.; Pfab, R.; Felgenhauer, N.; Zilker, T. Cholinesterase status, pharmacokinetics and laboratory findings during obidoxime therapy in organophosphate poisoned patients. Hum. Exp. Toxicol. 1997, 16, 473–480. [Google Scholar] [CrossRef]
- Strelitz, J.; Engel, L.; Keifer, M.C. Blood acethylcholinesterase and buthyrylcholinesterase as biomarker of cholinesterase depression among pesticide handlers. Occup. Environ. Med. 2014, 71, 842–847. [Google Scholar] [CrossRef] [PubMed]
- Eddleston, M. The pathophysiology of organophosphorus pesticide self-poisoning is not so simple. Neth. J. Med. 2008, 66, 146–148. [Google Scholar]
- Assis, C.R.D.; Linhares, A.G.; Cabrera, M.P.; Oliveira, V.M.; Silva, K.C.C.; Marcuschi, M.; Carvalho, E.V.M.M.; Bezerra, R.S.; Carvalho, L.B. Erythrocyte acetylcholinesterase as biomarker of pesticide exposure: New and forgotten insights. Environ. Sci. Pollut. Res. 2018, 25, 18364–18376. [Google Scholar] [CrossRef]
- Gagarin, P.Y.; Rajagopal, R.L. Clinical profile and outcome of organophosphorus poisoning in a tertiary care center, a prospective observational study. Int. J. Med. Res. Rev. 2020, 8, 148–153. [Google Scholar] [CrossRef]
- Sidell, F.R. Soman and Sarin: Clinical Manifestations and Treatment of Accidental Poisoning by Organophosphates. Clin. Toxicol. 1974, 7, 1–17. [Google Scholar] [CrossRef]
- Grob, D.; Harvey, J.C. Effects in man of the compound anticholinesterase sarin (isopropyl methyl phosphorofluoridate). J. Clin. Investig. 1958, 37, 350–368. [Google Scholar] [CrossRef]
- Namba, T.; Nolte, C.T.; Jackrel, J.; Grob, D. Poisoning due to organophosphate insecticide. Acute and chronic manifestations. Am. J. Med. 1971, 50, 475–492. [Google Scholar] [CrossRef] [PubMed]
- Morita, H.; Yanagisawa, N.; Narajima, T.; Okudera, H.; Shimizu, M.; Hirabayashi, H.; Nohara, M.; Midorikawa, Y.; Mimura, S. Sarin poisoning in Matsumoto, Japan. Lancet 1995, 346, 290–293. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Morita, H.; Ono, K.; Maekawa, K.; Nagai, R.; Yazaki, Y.; Nozaki, H.; Aikawa, N.; Shinozawa, Y.; Hori, S.; et al. Sarin poisoning in Tokyo subway. Lancet 1995, 345, 980–981. [Google Scholar] [CrossRef]
- Nozaki, H.; Hori, S.; Shinozawa, Y.; Fujishima, S.; Takuma, K.; Sagoh, M.; Kimura, H.; Ohki, T.; Suzuki, M.; Aikawa, N. Secondary exposure of medical staff to sarin vapor in the emergency room. Intensive Care Med. 1995, 21, 1032–1035. Available online: https://link.springer.com/article/10.1007/BF01700667 (accessed on 15 January 2023). [CrossRef] [PubMed]
- Okumura, T.; Takasu, N.; Ishimatsu, S.; Miyanoki, S.; Mitsuhashi, A.; Kumada, K.; Tanaka, K.; Hinohara, S. Report of 640 victims of the Tokyo subway sarin attack. Ann. Emerg. Med. 1996, 28, 129–135. [Google Scholar] [CrossRef]
- Nozaki, H.; Hori, S.; Shinozawa, Y.; Fujishima, S.; Takuma, K.; Kimura, H.; Suzuki, M.; Aikawa, N. Relationship between pupil size and acetylcholinesterase activity in patients exposed to sarin vapor. Intensive Care Med. 1997, 23, 1005–1007. [Google Scholar] [CrossRef]
- Nagao, M.; Takatori, T.; Matsuda, Y.; Nakajima, M.; Iwase, H.; Iwadate, K. Definitive evidence for the acute sarin poisoning diagnosis in the Tokyo subway. Toxicol. Appl. Pharmacol. 1997, 144, 198–203. [Google Scholar] [CrossRef]
- Lee, E.C. Clinical Manifestations of sarin nerve gas exposure. JAMA 2003, 290, 659. [Google Scholar] [CrossRef]
- Ciottone, G.R. Toxidrome recognition in clinical weapons attacks. N. Engl. J. Med. 2018, 378, 1611–1620. [Google Scholar] [CrossRef]
- Balali-Mood, M.; Saber, H. Recent advances in the treatment of organophosphorus poisoning. Iran. J. Med. Sci. 2012, 37, 74–91. [Google Scholar]
- Hulse, E.J.; Haslam, J.; Emmett, S.R.; Woolley, T. Organophosphorus nerve agent poisoning: Managing the poisoned patient. Br. J. Anaesth. 2019, 123, 457–463. [Google Scholar] [CrossRef]
- Vale, J.A.; Marrs, T.C.; Maynard, R.L. Novichok: A murderous nerve agent attack in the UK. Clin. Toxicol. 2018, 56, 1093–1097. [Google Scholar] [CrossRef]
- Carlsen, L. After Salisbury nerve agents revisited. Mol. Inform. 2018, 37, 1800106. [Google Scholar] [CrossRef] [PubMed]
- Thiermann, H.; Zilker, T.; Eyer, F.; Felgenhauer, N.; Eyer, P.; Worek, F. Monitoring of neuromuscular transmission in organophosphate pesticide-poisoned patients. Toxicol. Lett. 2009, 191, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Chuang, M.-C.; Chang, C.-H.; Lee, C.S.; Li, S.-H.; Hsiao, C.-C.; Fang, Y.-F.; Hsieh, M.-J. One year mortality among hospital survivors of cholinesterase inhibitor poisoning based on Taiwan national health insurance research database from 2003 to 2012. BMC Pharmacol. Toxicol. 2018, 19, 72. [Google Scholar] [CrossRef] [PubMed]
- Bajracharya, S.R.; Prasa, P.N.; Chimire, R. Management of organophosphorus poisoning. J. Nepal Health Res. Counc. 2016, 14, 131–138. [Google Scholar] [PubMed]
- Bledsoe, F.H.; Seymour, E.Q. Acute pulmonary edema associated with parathion poisoning. Radiology 1972, 103, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Kass, J.B.; Khamapirad, T.; Wagner, M.L. Pulmonary edema following absorption of organophosphate insecticide. Pediatr. Radiol. 1978, 7, 113–114. [Google Scholar] [CrossRef]
- Li, C.; Miller, W.; Jiang, J. Pulmonary edema due to ingestion of organophosphate insecticide. Am. J. Roentgenol. 1989, 152, 265–266. [Google Scholar] [CrossRef]
- Patil, G.; Murthy, N.; Nikhil, M. Contributing factors for morbidity and mortality in patients with organophosphate poisoning on mechanical ventilation: A retrospective study in teaching hospital. J. Clin. Diagn. Res. 2016, 10, UC18–UC20. [Google Scholar] [CrossRef]
- Kamat, S.R.; Heera, S.; Potdar, P.V.; Shah, S.V.; Bhambure, N.M.; Mahashur, A.A. Bombay experience in intensive respiratory care over 6 years. J. Postgrad. Med. 1989, 35, 123–134. [Google Scholar]
- Giyanwani, P.R.; Zubair, U.; Salam, O.; Zubair, Z. Respiratory failure following organophosphate poisoning: A literature review. Cureus 2017, 9, e1651. [Google Scholar] [CrossRef]
- Yu, J.-R.; Hou, Y.-C.; Fu, J.-F.; Wang, I.-K.; Chan, M.; Chen, C.-Y.; Weng, C.-H.; Huang, W.-H.; Yang, H.-Y.; Hsu, C.-W.; et al. Outcomes of elderly patients with organophosphate intoxication. Sci. Rep. 2021, 11, 11615. [Google Scholar] [CrossRef] [PubMed]
- Hulse, E.J.; Davies, J.O.J.; Simpson, A.J.; Sciuto, A.M.; Eddleston, M. Respiratory complications of organophosphorus nerve agent and insecticide poisoning. Am. J. Respir. Crit. Care Med. 2014, 190, 1342–1354. [Google Scholar] [CrossRef]
- Sharma, B.R.; Relhan, N.; Gupta, N.; Singh, H. Trends in fatal poisoning in Northern India: A ten-year Autopsy Analysis. J. Pharmacol. Toxicol. 2007, 2, 350–358. [Google Scholar] [CrossRef]
- Viswanathan, K.G.; Srijith Santhosh, C.S.; Siddesh, R.C. Pattern of histopathological Changes in Lungs, Liver and Kidneys in Cases of Organophosphate Insecticide Poisoning. JKAMLS 2015, 24, 12–17. [Google Scholar]
- Sobolev, V.E.; Sokolova, M.O.; Jenkins, R.O.; Goncharov, N.V. Molecular Mechanisms of Acute Organophosphate Nephrotoxicity. Int. J. Mol. Sci. 2022, 23, 8855. [Google Scholar] [CrossRef] [PubMed]
- Aghera, V.J.; Pipaliya, K.N.; Dabhi, D.M.; Mangal, H.M.; Varu, P.R.; Manvar, P.J. Study of gross mucosal findings of stomach in cases of fatal poisoning. An autopsy study. Indian J. Forensic Community Med. 2015, 2, 229–233. [Google Scholar] [CrossRef]
- Atanda, A.T.; Yusuf, A.T.; Faro, R.O. Autopsy Findings in Pediatric Poisoning with Otapiapia. Niger. J. Basic Clin. Sci. 2018, 15, 98–100. [Google Scholar] [CrossRef]
- Jinu, M.; George, T.P.; Balaram, N.A.; Sujisha, S.S. Carbamate poisoning-An Autopsy study. Med. Leg. Update 2020, 20, 1–7. [Google Scholar]
- Mlayeh, S.; Annabi, K.; Ben Daly, A.; Jedidi, M.; Ben Dhiab, M. Pesticide poisoning deaths: A 19-year retrospective study of medicolegal autopsies in center Tunisia. Egypt. J. Forensic Sci. 2020, 10, 26. [Google Scholar] [CrossRef]
- Saha, A.; Amonkar, G.; Desai, H.; Baro, B.; Agrawal, R. Acute respiratory distress syndrome: A study of autopsy findings. Lung India 2021, 38, 442–447. [Google Scholar] [CrossRef] [PubMed]
- AL Ajeli, M.H.; Shukr, M.; Abd AL-Hassin Hachim, B. Prevalence and Etiology of Respiratory Distress in Newborns in the Fallujah Teaching Hospital for Women and Children. Karbala J. Md. 2019, 12, 2199–2202. [Google Scholar]
- Chhabra, S.; Dalal, N.; Verma, R.; Dahiya, J.; Singh, S. Histopathological Findings in a Autopsy of Covid-19 Positive Young Male. Open Access J. Biomed. Sci. 2021, 3, 1122–1124. [Google Scholar] [CrossRef]
- Bösmüller, H.; Traxler, S.; Bitzer, M.; Häberle, H.; Raiser, W.; Nann, D.; Frauenfeld, L.; Vogelsberg, A.; Klingel, K.; Fend, F. The evolution of pulmonary pathology in fatal COVID-19 disease: An autopsy study with clinical correlation. Virchows Arch. 2020, 477, 349–357. [Google Scholar] [CrossRef]
- Lu, S.; Huang, X.; Liu, R.; Lan, Y.; Lei, Y.; Zeng, F.; Tang, X.; He, H. Comparison of COVID-19 Induced Respiratory Failure and Typical ARDS: Similarities and Differences. Front. Med. 2022, 9, 829771. [Google Scholar] [CrossRef]
- Kumar, S.; Gupta, S.; Bansal, Y.S.; Bal, A.; Rastogi, P.; Muthu, V.; Arora, V. Pulmonary histopathology in fatal paraquat poisoning. Autops. Case Rep. 2021, 11, e2021342. [Google Scholar] [CrossRef] [PubMed]
- Hulse, E.J.; Clutton, R.E.; Drummond, G.; Thompson, A.P.; van Beek, E.J.R.; Smith, S.H.; Eddleston, M. Lung Injury caused by aspiration of organophosphorus insecticide and gastric contents in pigs. Clin. Toxicol. 2022, 60, 725–736. [Google Scholar] [CrossRef] [PubMed]
- Masson, P.; Carletti, E.; Nachon, F. Structure activities and biomedical applications of human buthyrylcholinesterase. Protein Pept. Lett. 2009, 16, 1215–1224. [Google Scholar] [CrossRef]
- Mccance, R.A.; Widdowson, E.M.; Hutchinson, A.O. Effect of under-nutrition and alterations in diet on the cholinesterase activity of serum. Nature 1948, 161, 56–57. [Google Scholar] [CrossRef]
- Iwasaki, T.; Yoneda, M.; Nakajima, A.; Terauchi, Y. Serum buthyrylcholinesterase is strongly associated with adiposity, the serum and lipid profile and insulin resistance. Intern. Med. 2007, 46, 1633–1639. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.; Moore, S.W. Why has buthyrylcholinesterase been retained? Structural and functional diversification in a duplicate gene. Neurochem. Int. 2012, 61, 783–797. [Google Scholar] [CrossRef]
- Andersson, M.L.; Møller, A.M.; Wildgaard, K. Buthyrylcholinesterase deficiency and ist clinical importance in Anesthesia systematic review. Anaesthesia 2019, 74, 518–528. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Guo, Y.; Dan, Y.; Tan, W.; Mao, Q.; Deng, G. A novel mutation in the BCE gene and phenotype identified in a child with low buthyrylcholinesterase activity: A case report. BMC Med. Genet. 2018, 19, 58. [Google Scholar] [CrossRef]
- Worek, F.; Mast, U.; Kiderlen, D.; Diepold, C.; Eyer, P. Improved determination of acetylcholinesterase activity in human whole blood. Clin. Chim. Acta 1999, 288, 73–90. [Google Scholar] [CrossRef]
- Lotti, M. Cholinesterase inhibition: Complexities in interpretation. Clin. Chem. 1995, 41, 1814–1818. [Google Scholar] [CrossRef]
- Ellman, G.L.; Courtney, K.D.; Andres, V., Jr.; Featherstone, R.M. A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem. Pharmacol. 1961, 7, 88–95. [Google Scholar] [CrossRef]
- Worek, F.; Schilha, M.; Neumaier, K.; Aurbek, N.; Wille, T.; Thiermann, H.; Kehe, K. On-site analysis of acetylcholinesterase and butyrylcholines rase activity with the ChE check mobile test kit-Determination of reference values and their relevance for diagnosis of exposure to organophosphorus compounds. Toxicol. Lett. 2016, 249, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Bozzetti, F.; Migliavacca, S.; Gallus, G.; Radaelli, G.; Scotti, A.; Bonalumi, M.G.; Ammatuna, M.; Sequeira, C.; Terno, G. Nutritional markers as Prognostic Indicators of Postoperative Sepsis in Cancer Patients. J. Parenter. Enter. Nutr. 1985, 9, 464–470. [Google Scholar] [CrossRef]
- Fanali, G.; di Masi, A.; Trezza, V.; Marino, M.; Fasano, M.; Ascenzi, P. Human serum Albumin: From the bench to the bedside. Mol. Asp. Med. 2012, 33, 209–290. [Google Scholar] [CrossRef] [PubMed]
- Levitt, D.; Levitt, M. Human serum albumin homeostasis: A new look at the roles of synthesis, catabolism, renal and gastrointestinal excretion, and the clinical value of serum albumin measurements. Int. J. Gen. Med. 2016, 9, 229–255. [Google Scholar] [CrossRef]
- De Feo, P.; Horber, F.F.; Haymond, M.W. Meal stimulation of albumin synthesis: A significant contributor to whole body protein synthesis in human. Am. J. Physiol. Endocrinol. Metab. 1992, 263, E794–E799. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.R.; Robinson, M.J.; Fry, J.L.; Tang, J.E.; Glover, E.I.; Wilkinson, S.B.; Prior, T.; Tarnopolsky, M.A.; Phillips, S.M. Ingested protein dose response of muscle and albumin protein synthesis after resistance exercise in young men. Am. J. Clin. Nutr. 2009, 89, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Onen, K.; Wade, O.; Blainey, J. Amino-acids in hepatic venous and arterial blood investigated by paper chromatography. Lancet 1956, 268, 1075–1076. [Google Scholar] [CrossRef]
- Rothschild, M.A.; Oratz, M.; Mongelli, J.; Schreiber, S.S. Effects of a short-term fast on albumin synthesis studied in vivo, in the perfused liver, and on amino acid incorporation by hepatic microsomes. J. Clin. Investig. 1968, 47, 2591–2599. [Google Scholar] [CrossRef]
- Caso, G.; Scalfi, L.; Marra, M.; Covino, A.; Muscaritoli, M.; McNurlan, M.A.; Garlick, P.J.; Contaldo, F. Albumin synthesis is diminished in Man consuming a predominantly vegetarian diet. J. Nutr. 2000, 130, 528–533. [Google Scholar] [CrossRef]
- Imoberdorf, R.; Garlick, P.J.; McNurlan, M.A.; Casella, G.A.; Peheim, E.; Turgay, M.; Bärtsch, P.; Ballmer, P.E. EEnhanced synthesis of albumin and fibrinogen at high altitude. J. Appl. Physiol. 2001, 90, 528–537. [Google Scholar] [CrossRef] [PubMed]
- Nagashima, K.; Mack, G.W.; Haskell, A.; Nishiyasu, T.; Nadel, E.R. Mechanisms for the posture-specific plasma volume increase after a single intense exercise protocol. J. Appl. Physiol. 1999, 86, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Nagashima, K.; Cline, G.W.; Mack, G.W.; Shulman, G.I.; Nadel, E.R. Intense exercise stimulates albumin synthesis in the upright posture. J. Appl. Physiol. 2000, 88, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Rothschild, M.A.; Oratz, M.; Schreiber, S.S. Albumin synthesis. N. Engl. J. Med. 1972, 286, 816–821. [Google Scholar] [CrossRef]
- Hülshoff, A.; Schricker, T.; Elgendy, H.; Hatzakorzian, R.; Lattermann, R. Albumin synthesis in surgical patients. Nutrition 2013, 29, 703–707. [Google Scholar] [CrossRef]
- Schomerus, H.; Mayer, G. Synthesis rates of albumin and fibrinogen in patients with protein-losing enteropathy and in a patient recovering from protein malnutrition. Digestion 1975, 13, 201–208. [Google Scholar] [CrossRef]
- Ballmer, P.E.; Weber, B.K.; Roy-Chaudhury, P.; Mcnurlan, M.A.; Watson, H.; Power, D.A.; Garlick, P.J. Elevation of albumin synthesis rates in nephrotic patients measured with (1-13C) leucine. Kidney Int. 1992, 41, 132–138. [Google Scholar] [CrossRef]
- Caso, G.; Feiner, J.; Mileva, I.; Bryan, L.J.; Kelly, P.; Autio, K.; Gelato, M.C.; McNurlan, A.M. Response of albumin synthesis to oral nutrients in young and elderly subjects. Am. J. Clin. Nutr. 2007, 85, 446–451. [Google Scholar] [CrossRef]
- Weaving, G.; Batstone, G.F.; Jones, R.G. Age and sex variation in serum albumin concentration: An observational study. Ann. Clin. Biochem. 2015, 53, 106–111. [Google Scholar] [CrossRef]
- Fu, A.; Nair, K.S. Age effect on fibrinogen and albumin synthesis in humans. Am. J. Physiol. Endocrinol. Metab. 1998, 275, E1023–E1030. [Google Scholar] [CrossRef]
- Devi, R.; Kumar, M.P. Effect of aging and sex on the ceruloplasmin(Cp) and the plasma protein levels. J. Clin. Diagn. Res. 2012, 6 (Suppl. S2), 577–580. [Google Scholar]
- Shetty, P.; Jung, R.; Watrasiewicz, K.; James, W. Rapid turnover transport proteins: An index of subclinical protein-energy malnutrition. Lancet 1979, 314, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Salive, M.E.; Cornoni-Huntley, J.; Phillips, C.L.; Guralnik, J.M.; Cohen, H.J.; Ostfeld, A.M.; Wallace, R.B. Serum albumin in older persons: Relationship with age and health status. J. Clin. Epidemiol. 1992, 45, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.K.; Gardner, C. Effect of aging on serum albumin. J. Am. Geriatr. Soc. 1989, 37, 1039–1142. [Google Scholar] [CrossRef]
- Cabrerizo, S.; Cuadras, D.; Gomez-Busto, F.; Artaza-Artabe, I.; Marín-Ciancas, F.; Malafarina, V. Serum albumin and health in older people. Maturitas 2015, 81, 17–27. [Google Scholar] [CrossRef]
- Haydock, D.A.; Hill, G.L. Wound healing in surgical patients with varying degree of malnutrition. J. Parenter. Enter. Nutr. 1986, 10, 550–554. [Google Scholar] [CrossRef]
- Volpi, E.; Lucidi, P.; Cruciani, G.; Monacchia, F.; Reboldi, G.; Brunetti, P.; Bolli, G.B.; De Feo, P. Nicotinamide counteracts alcohol-induced impairment of hepatic protein metabolism in humans. J. Nutr. 1997, 127, 2199–2204. [Google Scholar] [CrossRef]
- Soeters, P.B.; Wolfe, R.R.; Shenkin, A. Hypoalbuminemia:pathogenesis and clinical significance. J. Parenter. Enter. Nutr. 2019, 43, 181–193. [Google Scholar] [CrossRef]
- Corti, M.C.; Guralnik, J.M.; Salive, M.E.; Sorkin, J.D. Serum albumin level and physical disability as predictors of mortality in older persons. JAMA 1994, 272, 1036–1042. [Google Scholar] [CrossRef]
- Iwata, M.; Kuzuya, M.; Kitagawa, Y.; Iguchi, A. Prognostic value of serum albumin combined with serum C-reactive protein levels in older hospitalized patients: Continuing importance of serum albumin. Aging Clin. Exp. Res. 2006, 18, 307–311. [Google Scholar] [CrossRef]
- Harris, T.B.; Ferrucci, L.; Tracy, R.P.; Corti, M.C.; Wacholder, S.; Ettinger, W.H., Jr.; Heimovitz, H.; Cohen, H.J.; Wallace, R. Association of elevated Interleukin-6 and C-Reactive Protein levels. Am. J. Med. 1999, 106, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Lyons, O.; Whelan, B.; Bennett, K.; O‘Riordan, D.; Silke, B. Serum albumin as an outcome predictor in hospital emergency medical admissions. Eur. J. Intern. Med. 2010, 21, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Nakazato, Y.; Kurane, R.; Hirose, S.; Watanabe, A.; Shimoyama, H. Aging and death-associated changes in serum albumin variability over the course of chronic hemodialysis treatment. PLoS ONE 2017, 12, e0185216. [Google Scholar] [CrossRef]
- Gupta, D.; Lis, C.G. Pretreatment serum albumin as a predictor of cancer survival: A systematic review oft he epidemiological literature. Nutr. J. 2010, 9, 69. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, S.; Yoshioka, H.; Ikeo, S.; Morita, M.; Sone, N.; Niwa, T.; Nishiyama, A.; Yokoyama, T.; Sekine, A.; Ogura, T.; et al. Serum albumin level as a potential marker for deciding chemotherapy or best supportive care in elderly, advanced non-small cell lung cancer patients with poor performance status. BMC Cancer 2017, 17, 797. [Google Scholar] [CrossRef]
- Johnson, P.J.; Berhane, S.; Kagebayashi, C.; Satomura, S.; Teng, M.; Reeves, H.L.; O’Beirne, J.; Fox, R.; Skowronska, A.; Palmer, D.; et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-The ALBI Grade. J. Clin. Oncol. 2015, 33, 550–558. [Google Scholar] [CrossRef]
- Yamamoto, M.; Saito, H.; Uejima, C.; Tanio, A.; Tada, Y.; Matsunaga, T.; Sakamoto, T.; Honjo, S.; Ashida, K.; Fujiwara, Y. Combination of serum albumin and cholinesterase levels as prognostic indicator in patients with colorectal cancer. Anticancer Res. 2019, 39, 1085–1090. [Google Scholar] [CrossRef]
- Arrieta, O.; Ortega, R.M.M.; Villanueva-Rodríguez, G.; Serna-Thomé, M.G.; Flores-Estrada, D.; Diaz-Romero, C.; Rodríguez, C.M.; Martínez, L.; Sánchez-Lara, K. Association of nutritional status and serum albumin levels with development of toxicity in patients with advanced non-small cell lung cancer treated with paclitaxel-cisplatin chemotherapy: A prospective study. BMC Cancer 2010, 10, 50. [Google Scholar] [CrossRef]
- Gibbs, J.; Cull, W.; Henderson, W.; Daley, J.; Hur, K.; Khuri, S.F. Preoperative serum albumin level as predictor of operative mortality and morbidity. Results from the national VA surgical Risk Study. Arch. Surg. 1999, 134, 36–42. [Google Scholar] [CrossRef]
- Kamath, P.S.; Wiesner, R.H.; Malinchoc, M.; Kremers, W.; Therneau, T.M.; Kosberg, C.L.; D‘Amico, G.; Dickson, E.R.; Kim, W.R. A model to predict survival in patients with end-stage liver disease. Hepatology 2001, 33, 464–470. [Google Scholar] [CrossRef]
- Cholongitas, E.; Marelli, L.; Shusang, V.; Senzolo, M.; Rolles, K.; Patch, D.; Burroughs, A.K. A systematic review of the performance of the model for end-stage liver disease (MELD) in the setting of liver transplantation. Liver Transplant. 2006, 12, 1049–1061. [Google Scholar] [CrossRef] [PubMed]
- Gotthardt, D.; Weiss, K.H.; Baumgärtner, M.; Zahn, A.; Stremmel, W.; Schmidt, J.; Bruckner, T.; Sauer, P. Limitations of the MELD score in predicting mortality or need for removal from waiting list in patients awaiting liver transplantation. BMC Gastroenterol. 2009, 9, 72. [Google Scholar] [CrossRef]
- Rahimi-Dehkordi, N.; Nourijelyani, K.; NASIRI-Tousi, M.; Ghodssi-Ghassemabadi, R.; Azmoudeh-Ardalan, F.; Nedjat, S. Model for End Stage liver Disease (MELD) and Child-Turcotte-Pugh(CTP) scores: Ability to predict mortality and removal from liver transplantation waiting list due to poor medical conditions. Arch. Iran. Med. 2014, 17, 118–121. [Google Scholar]
- Ghabril, M.; Charlton, M. Lack of survival benefit following liver transplantation with MELD exception points for hepatocellular carcinoma: Beyond the unblinding of lady justice. Gastroenterology 2015, 149, 531–533. [Google Scholar] [CrossRef]
- Taverna, M.; Marie, A.-L.; Mira, J.-P.; Guidet, B. Specific antioxidant properties of human serum albumin. Ann. Intensive Care 2013, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- Goncharov, N.V.; Belinskaia, D.A.; Shmurak, V.I.; Terpilowski, M.A.; Jenkins, R.O.; Avdonin, P.V. Serum albumin binding and esterase activity: Mechanistic interactions with Organophosphates. Molecules 2017, 22, 1201. [Google Scholar] [CrossRef] [PubMed]
- Sogorb, M.A.; Vilanova, E. Serum albumins and detoxification of anti- cholinesterase agents. Chem. Biol. Interact. 2010, 187, 325–329. [Google Scholar] [CrossRef]
- Sogorb, M.A.; García-Argüelles, S.; Carrera, V.; Vilanova, E. Serum albumin is as efficient as paraxonase at toxicologically relevant concentrations. Chem. Res. Toxicol. 2008, 21, 1524–1529. [Google Scholar] [CrossRef]
- Li, B.; Nachon, F.; Froment, M.-T.; Verdier, L.; Debouzy, J.-C.; Brasme, B.; Gillon, E.; Schopfer, L.M.; Lockridge, O.; Masson, P. Binding and hydrolysis of Soman by human serum albumin. Chem. Res. Toxicol. 2008, 21, 421–431. [Google Scholar] [CrossRef]
- Noh, E.; Moon, J.M.; Chun, B.J.; Cho, Y.S.; Ryu, S.; Kim, D. The clinical role of serum albumin in OP poisoning. Basic Clin. Pharmacol. Toxicol. 2020, 128, 605–614. [Google Scholar] [CrossRef]
- Peeples, E.S.; Schopfer, L.M.; Duysen, E.G.; Spaulding, R.; Voelker, T.; Thompson, C.M.; Lockridge, O. Albumin, a new Biomarker of Organophosphorus Toxicant Exposure, Identified by Mass Spectrometry. Toxicol. Sci. 2004, 83, 303–312. [Google Scholar] [CrossRef]
- Wu, X.; Xie, W.; Cheng, Y.; Guan, Q. Severity and prognosis of acute organophosphorus pesticide poisoning are indicated by C-Reactive Protein and Copeptin levels and APACHE II score. Exp. Ther. Med. 2016, 11, 806–810. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, Y.H.; Park, Y.H.; Kim, Y.H.; Hong, C.K.; Cho, K.W.; Hwang, S.Y. The difference in C-reactive protein value between initial and 24 hours follow-up (D-CRP) data as predictor of mortality in organophosphate poisoned patients. Clin. Toxicol. 2013, 51, 29–34. [Google Scholar] [CrossRef]
- Lee, S.B.; Kang, C.; Kim, D.H.; Kim, T.; Lee, S.H.; Jeong, J.H.; Kim, S.C.; Rhee, D.Y.; Lim, D. Base deficit is a predictor of mortality in organophosphate insecticide poisoning. Hum. Exp. Toxicol. 2018, 37, 118–124. [Google Scholar] [CrossRef]
- Tang, W.; Ruan, F.; Chen, Q.; Chen, S.; Shao, X.; Gao, J.; Zhang, M. Independent prognostic factors for acute organophosphorus pesticide poisoning. Respir. Care 2016, 61, 965–970. [Google Scholar] [CrossRef]
- Liu, H.-F.; Ku, C.-H.; Chang, S.-S.; Chang, C.-M.; Wang, I.-K.; Yang, H.-Y.; Weng, C.-H.; Huang, W.-H.; Hsu, C.-W.; Yen, T.-H. Outcome of patients with chlorpyrifos intoxication. Hum. Exp. Toxicol. 2020, 39, 1291–1300. [Google Scholar] [CrossRef]
- Güven, M.; Sungur, M.; Eser, B.; Sarı, I.; Altuntas, F. The effects of fresh frozen Plasma of Cholinesterase levels and Outcomes in Patients with organophosphate Poisoning. J. Toxicol. Clin. Toxicol. 2004, 42, 617–623. [Google Scholar] [CrossRef]
- Pazooki, S.; Solhi, H.; Vishteh, H.R.K.; Shadnia, S.; Beigi, M.J.B. Effectiveness of fresh frozen plasma as supplementary treatment in organophosphate poisoning. Med. J. Malays. 2011, 66, 342–345. [Google Scholar]
- Pichamuthu, K.; Jerobin, J.; Nair, A.; John, G.; Kamalesh, J.; Thomas, K.; Jose, A.; Fleming, J.J.; Zachariah, A.; David, S.S.; et al. Bioscavenger therapy for organophosphate poisoning-an open-labeled pilot randomized trial comparing fresh froze plasma or albumin with saline in acute organophosphate poisoning in humans. Clin. Toxicol. 2010, 48, 813–819. [Google Scholar] [CrossRef]
- Dayananda, V.; Bhaskara, B.; Pateel, G. A study of effectiveness of fresh frozen plasma in organophosphorus compound poisoning in reducing length of intensive care unit stay and in reducing need of tracheostomy. Anesth. Essays Res. 2016, 10, 268–272. [Google Scholar] [CrossRef]
- Amend, N.; Langgartner, J.; Siegert, M.; Kranawetvogl, T.; Koller, M.; John, H.; Pflügler, C.; Mögele-Schmid, C.; Worek, F.; Thiermann, H.; et al. A case report of cholinesterase inhibitor poisoning: Cholinesterase activities and analytical methods for diagnosis and clinical decision making. Arch. Toxicol. 2020, 94, 2239–2247. [Google Scholar] [CrossRef]
- Fulton, J.A.; Bouchard, N.C.; Becker, M.L.; Gertz, S.; Hoffman, R.S. FFP in Organophosphate Poisoning: What’s the secret Ingredient? Clin. Toxicol. 2005, 43, 215. [Google Scholar] [CrossRef]
- Bao, H.-X.; Tong, P.-J.; Li, C.-X.; Du, J.; Chen, B.-Y.; Huang, Z.-H.; Wang, Y. Efficacy of fresh packed red blood transfusion in organophosphate poisoning. Medicine 2017, 96, e6375. [Google Scholar] [CrossRef]
- Ghayyor, A. Modulation of Gene Expression of Iron Regulatory Proteins, Hemoxigenase-1 and Lactoferrin, in Mice ‘Liver and Muscle by Different Cytokines, in Two Models of Acute-Phase Reaction. Ph.D. Thesis, Faculty of Biology, University of Göttingen, Göttingen, Germany, 2010. [Google Scholar]
- Rooyackers, O.E.; Saris, W.H.M.; Soeters, P.B.; Wagenmakers, A. Prolonged changes in protein and amino acid metabolism after zymosan treatment in rats. Clin. Sci. 1994, 87, 619–626. [Google Scholar] [CrossRef]
- Moriconi, F.; Ahmad, G.; Ramadori, P.; Malik, I.; Sheikh, N.; Merli, M.; Riggio, O.; Dudas, J.; Ramadori, G. Phagocytosis of gadolinium chloride or zymosan induces simultaneous upregulation of hepcidin and downregulation of hemojuvelin and ferroportin-1-gene-expression in murine liver. Lab. Investig. 2009, 89, 1252–1260. [Google Scholar] [CrossRef]
- Liu, K.D.; Matthay, M.A. Advances in Critical Care for the Nephrologist: Acute Lung Injury/ARDS. Clin. J. Am. Soc. Nephrol. 2008, 3, 578–586. [Google Scholar] [CrossRef]
- Steindl, D.; Boehmerle, W.; Körner, R.; Praeger, D.; Haug, M.; Nee, J.; Schreiber, A.; Scheibe, F.; Demin, K.; Jacoby, P.; et al. Novichock nerve agent poisoning. Lancet 2021, 397, 249–252. [Google Scholar] [CrossRef]
- Singh, S.; Bhardwaj, U.; Verma, S.K.; Bhalla, A.; Gill, K. Hyperamylasemia and acute pancreatitis following anticholinesterase poisoning. Hum. Exp. Toxicol. 2007, 26, 467–471. [Google Scholar] [CrossRef]
- Chen, K.-X.; Zhou, X.-H.; Sun, C.-A.; Yan, P.-X. Manifestation of and risk factors for acute myocardial injury after organophosphorus pesticide poisoning. Medicine 2019, 98, e14371. [Google Scholar] [CrossRef]
- Pereska, Z.; Chaparoska, D.; Bekarovski, N.; Jurukov, I.; Simonovska, N.; Babulovska, A. Pulmonary thrombosis in acute organophosphate poisoning-Case report and literature overview of prothrombotic preconditioning in organophosphate toxicity. Toxicol. Rep. 2019, 6, 550–555. [Google Scholar] [CrossRef]
- Bereda, G. Poisoning by Organophosphate Pesticides: A case Report. Cureus 2022, 14, e29842. [Google Scholar] [CrossRef]
- Ibrahim, A.E.; Ghantarchyan, H.; Le, T.; Bhagat, A.; Maknouni, B.; Arabian, S. A rare Presentation of Severe Organophosphate Poisoning: A Case Report and Review of Literature. Cureus 2022, 14, e31497. [Google Scholar] [CrossRef]
- Faluomi, M.; Cialini, M.; Naviganti, M.; Mastromauro, A.; Marinangeli, F.; Angeletti, C. Organophosphates pesticide poisoning: A peculiar case report. J. Emerg. Crit. Care Med. 2022, 6, 30. [Google Scholar] [CrossRef]
- Lockridge, O. Nocholinesterase Protein Targets of Organophosphorus Pesticides. Adv. Mol. Toxicol. 2013, 7, 179–205. [Google Scholar] [CrossRef]
- Eddleston, M. Are oximes still indicated for acute organophosphorus insecticide self-poisoning? J. Med. Toxicol. 2018, 14, 1–2. [Google Scholar] [CrossRef]
- Kharel, H.; Pokhrel, N.B.; Ghimire, R.; Kharel, Z. The Efficacy of Pralidoxime in the Treatment of Organophosphate Poisoning in Humans: A Systematic Review and Meta-analysis of Randomized Trials. Cureus 2020, 12, e7174. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramadori, G.P. Organophosphorus Poisoning: Acute Respiratory Distress Syndrome (ARDS) and Cardiac Failure as Cause of Death in Hospitalized Patients. Int. J. Mol. Sci. 2023, 24, 6658. https://doi.org/10.3390/ijms24076658
Ramadori GP. Organophosphorus Poisoning: Acute Respiratory Distress Syndrome (ARDS) and Cardiac Failure as Cause of Death in Hospitalized Patients. International Journal of Molecular Sciences. 2023; 24(7):6658. https://doi.org/10.3390/ijms24076658
Chicago/Turabian StyleRamadori, Giuliano Pasquale. 2023. "Organophosphorus Poisoning: Acute Respiratory Distress Syndrome (ARDS) and Cardiac Failure as Cause of Death in Hospitalized Patients" International Journal of Molecular Sciences 24, no. 7: 6658. https://doi.org/10.3390/ijms24076658
APA StyleRamadori, G. P. (2023). Organophosphorus Poisoning: Acute Respiratory Distress Syndrome (ARDS) and Cardiac Failure as Cause of Death in Hospitalized Patients. International Journal of Molecular Sciences, 24(7), 6658. https://doi.org/10.3390/ijms24076658





