Targeted Large-Volume Lymphocyte Removal Using Magnetic Nanoparticles in Blood Samples of Patients with Chronic Lymphocytic Leukemia: A Proof-of-Concept Study
Abstract
:1. Introduction
2. Results
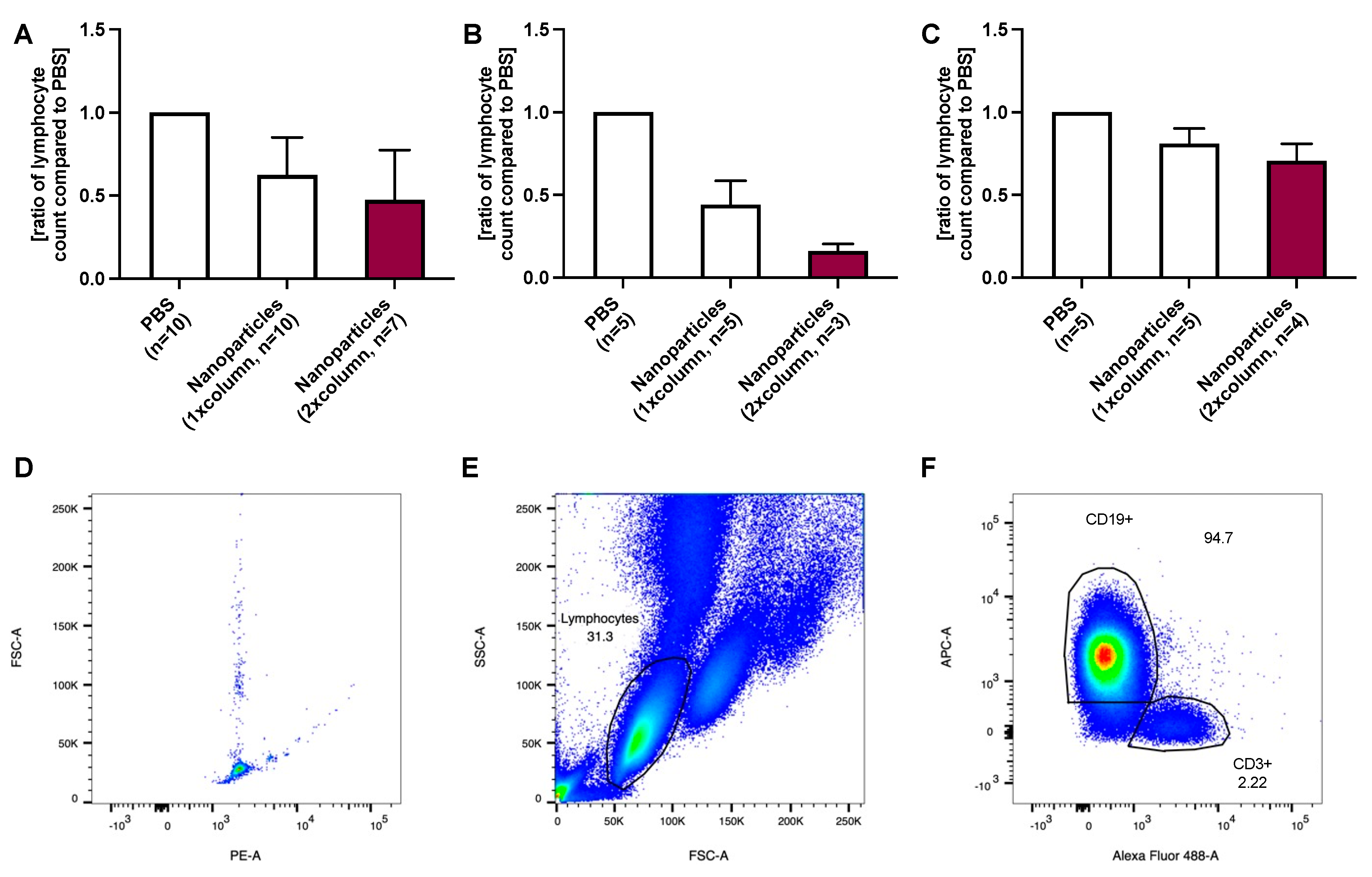
2.1. CD19-Positive B Lymphocyte Removal Using Anti-CD52-Coated Nanoparticles
2.2. CD19-Positive B Lymphocyte Removal Using Anti-CD52-Coated Nanoparticles Adapted to Lymphocyte Count

2.3. CD52-Positive Lymphocyte Removal Using Anti-CD52-Coated Nanoparticles Adapted to Lymphocyte Count

3. Discussion
4. Material and Methods
4.1. Patients
4.2. Nanoparticles
4.3. Ex Vivo Lymphocyte Removal
4.3.1. Experimental Approach
4.3.2. Variation with Nanoparticle Concentration
4.4. Staining of Lymphocytes and Cell Counting
4.5. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alaggio, R.; Amador, C.; Anagnostopoulos, I.; Attygalle, A.D.; Araujo, I.B.d.O.; Berti, E.; Bhagat, G.; Borges, A.M.; Boyer, D.; Calaminici, M.; et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 2022, 36, 1720–1748. [Google Scholar] [CrossRef] [PubMed]
- Hus, I.; Roliński, J. Current concepts in diagnosis and treatment of chronic lymphocytic leukemia. Contemp. Oncol. (Pozn.) 2015, 19, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Merli, F.; Mammi, C.; Ilariucci, F. Integrating Oncogeriatric Tools into the Management of Chronic Lymphocytic Leukemia: Current State of the Art and Challenges for the Future. Curr. Oncol. Rep. 2015, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T. Treatment of older patients with chronic lymphocytic leukemia: Key questions and current answers. Hematol. Am. Soc. Hematol. Educ. Program 2013, 2013, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Doswald, S.; Herzog, A.F.; Zeltner, M.; Zabel, A.; Pregernig, A.; Schläpfer, M.; Siebenhüner, A.; Stark, W.J.; Beck-Schimmer, B. Removal of Circulating Tumor Cells from Blood Samples of Cancer Patients Using Highly Magnetic Nanoparticles: A Translational Research Project. Pharmaceutics 2022, 14, 1397. [Google Scholar] [CrossRef] [PubMed]
- Alinari, L.; Lapalombella, R.; Andritsos, L.; Baiocchi, R.A.; Lin, T.S.; Byrd, J.C. Alemtuzumab (Campath-1H) in the treatment of chronic lymphocytic leukemia. Oncogene 2007, 26, 3644–3653. [Google Scholar] [CrossRef]
- Padmanabhan, A.; Connelly-Smith, L.; Aqui, N.; Balogun, R.A.; Klingel, R.; Meyer, E.; Pham, H.P.; Schneiderman, J.; Witt, V.; Wu, Y.; et al. Guidelines on the Use of Therapeutic Apheresis in Clinical Practice—Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Eighth Special Issue. J. Clin. Apher. 2019, 34, 171–354. [Google Scholar] [CrossRef]
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the clinic: An update. Bioeng. Transl. Med. 2019, 4, e10143. [Google Scholar] [CrossRef]
- Herrmann, I.K.; Urner, M.; Koehler, F.M.; Hasler, M.; Roth-Z’Graggen, B.; Grass, R.N.; Ziegler, U.; Beck-Schimmer, B.; Stark, W.J. Blood Purification Using Functionalized Core/Shell Nanomagnets. Small 2010, 6, 1388–1392. [Google Scholar] [CrossRef]
- Shen, S.; Han, F.; Yuan, A.; Wu, L.; Cao, J.; Qian, J.; Qi, X.; Yan, Y.; Ge, Y. Engineered nanoparticles disguised as macrophages for trapping lipopolysaccharide and preventing endotoxemia. Biomaterials 2019, 189, 60–68. [Google Scholar] [CrossRef]
- Herrmann, I.K.; Urner, M.; Graf, S.; Schumacher, C.M.; Roth-Z’graggen, B.; Hasler, M.; Stark, W.J.; Beck-Schimmer, B. Endotoxin removal by magnetic separation-based blood purification. Adv. Healthc. Mater. 2013, 2, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Bromberg, L.; Chang, E.P.; Alvarez-Lorenzo, C.; Magariños, B.; Concheiro, A.; Hatton, T.A. Binding of functionalized paramagnetic nanoparticles to bacterial lipopolysaccharides and DNA. Langmuir 2010, 26, 8829–8835. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, I.K.; Schlegel, A.; Graf, R.; Schumacher, C.M.; Senn, N.; Hasler, M.; Gschwind, S.; Hirt, A.M.; Günther, D.; Clavien, P.A.; et al. Nanomagnet-based removal of lead and digoxin from living rats. Nanoscale 2013, 5, 8718–8723. [Google Scholar] [CrossRef] [PubMed]
- Ooi, A.T. Single-Cell Protein Analysis Methods and Protocols; Methods in Molecular Biology; Humana Press: New York, NY, USA, 2022. [Google Scholar]
- Choi, M.H.; Choe, Y.H.; Park, Y.; Nah, H.; Kim, S.; Jeong, S.H.; Kim, H.O. The effect of therapeutic leukapheresis on early complications and outcomes in patients with acute leukemia and hyperleukocytosis: A propensity score-matched study. Transfusion 2018, 58, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Zhu, Y.; Jin, Y.; Kaweme, N.M.; Dong, Y. Leukapheresis and Hyperleukocytosis, Past and Future. Int. J. Gen. Med. 2021, 14, 3457–3467. [Google Scholar] [CrossRef]
- Steinberg, M.H.; Charm, S.E. Effect of high concentrations of leukocytes on whole blood viscosity. Blood 1971, 38, 299–301. [Google Scholar] [CrossRef]
- Schulz, A.; Toedt, G.; Zenz, T.; Stilgenbauer, S.; Lichter, P.; Seiffert, M. Inflammatory cytokines and signaling pathways are associated with survival of primary chronic lymphocytic leukemia cells in vitro: A dominant role of CCL2. Haematologica 2011, 96, 408–416. [Google Scholar] [CrossRef]
- Sloop, G.D.; De Mast, Q.; Pop, G.; Weidman, J.J.; St Cyr, J.A. The Role of Blood Viscosity in Infectious Diseases. Cureus 2020, 12, e7090. [Google Scholar] [CrossRef]
- Zheng, Y.; Wen, J.; Nguyen, J.; Cachia, M.A.; Wang, C.; Sun, Y. Decreased deformability of lymphocytes in chronic lymphocytic leukemia. Sci. Rep. 2015, 5, 7613. [Google Scholar] [CrossRef]
- Österborg, A.; Karlsson, C.; Lundin, J.; Kimby, E.; Mellstedt, H. Strategies in the Management of Alemtuzumab-Related Side Effects. Semin. Oncol. 2006, 33, 29–35. [Google Scholar] [CrossRef]
- Ogrinc, G.; Davies, L.; Goodman, D.; Batalden, P.; Davidoff, F.; Stevens, D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Qual. Saf. 2016, 25, 986–992. [Google Scholar] [CrossRef] [PubMed]
- Grass, R.N.; Athanassiou, E.K.; Stark, W.J. Covalently functionalized cobalt nanoparticles as a platform for magnetic separations in organic synthesis. Angew. Chem. Int. Ed. Engl. 2007, 46, 4909–4912. [Google Scholar] [CrossRef] [PubMed]
- Doswald, S.; Stark, W.J.; Beck-Schimmer, B. Biochemical functionality of magnetic particles as nanosensors: How far away are we to implement them into clinical practice? J. Nanobiotechnol. 2019, 17, 73. [Google Scholar] [CrossRef] [PubMed]
| ≤20 G Lymphocytes/L Blood (n = 4) | >20 G Lymphocytes/L Blood (n = 6) | |
|---|---|---|
| Age [years] (mean ± SD) | 71 ± 8.79 | 61 ± 10.39 |
| Sex Female (n) Male (n) | 3 1 | 2 4 |
| Chronic lymphocytic leukemia (n) | 4 | 6 |
| Patients under watch-and-wait strategy (n) | 3 | 5 |
| Patients under first-line treatment (n) | 1 | 0 |
| Patients under second-line treatment (n) | 0 | 1 |
| Lymphocyte count [G/L] (mean ± SD) | 9.14 ± 5.10 | 65.57 ± 26.14 |
| ≤20 G Lymphocytes/L Blood (n = 4) | >20 G Lymphocytes/L Blood (n = 6) | |
|---|---|---|
| Age [years] (mean ± SD) | 76 ± 7.44 | 62 ± 8.23 |
| Sex Female (n) Male (n) | 2 3 | 4 2 |
| Chronic lymphocytic leukemia (n) | 5 | 6 |
| Patients under watch-and-wait strategy (n) | 4 | 5 |
| Patients under first-line treatment (n) | 1 | 0 |
| Patients under second-line treatment (n) | 0 | 1 |
| Lymphocyte count [G/L] (mean ± SD) | 11.87 ± 4.22 | 71.12 ± 20.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Janker, S.; Doswald, S.; Schimmer, R.R.; Schanz, U.; Stark, W.J.; Schläpfer, M.; Beck-Schimmer, B. Targeted Large-Volume Lymphocyte Removal Using Magnetic Nanoparticles in Blood Samples of Patients with Chronic Lymphocytic Leukemia: A Proof-of-Concept Study. Int. J. Mol. Sci. 2023, 24, 7523. https://doi.org/10.3390/ijms24087523
Janker S, Doswald S, Schimmer RR, Schanz U, Stark WJ, Schläpfer M, Beck-Schimmer B. Targeted Large-Volume Lymphocyte Removal Using Magnetic Nanoparticles in Blood Samples of Patients with Chronic Lymphocytic Leukemia: A Proof-of-Concept Study. International Journal of Molecular Sciences. 2023; 24(8):7523. https://doi.org/10.3390/ijms24087523
Chicago/Turabian StyleJanker, Stefanie, Simon Doswald, Roman R. Schimmer, Urs Schanz, Wendelin J. Stark, Martin Schläpfer, and Beatrice Beck-Schimmer. 2023. "Targeted Large-Volume Lymphocyte Removal Using Magnetic Nanoparticles in Blood Samples of Patients with Chronic Lymphocytic Leukemia: A Proof-of-Concept Study" International Journal of Molecular Sciences 24, no. 8: 7523. https://doi.org/10.3390/ijms24087523





