Exploring the Structural and Functional Diversity among FGF Signals: A Comparative Study of Human, Mouse, and Xenopus FGF Ligands in Embryonic Development and Cancer Pathogenesis
Abstract
1. Introduction
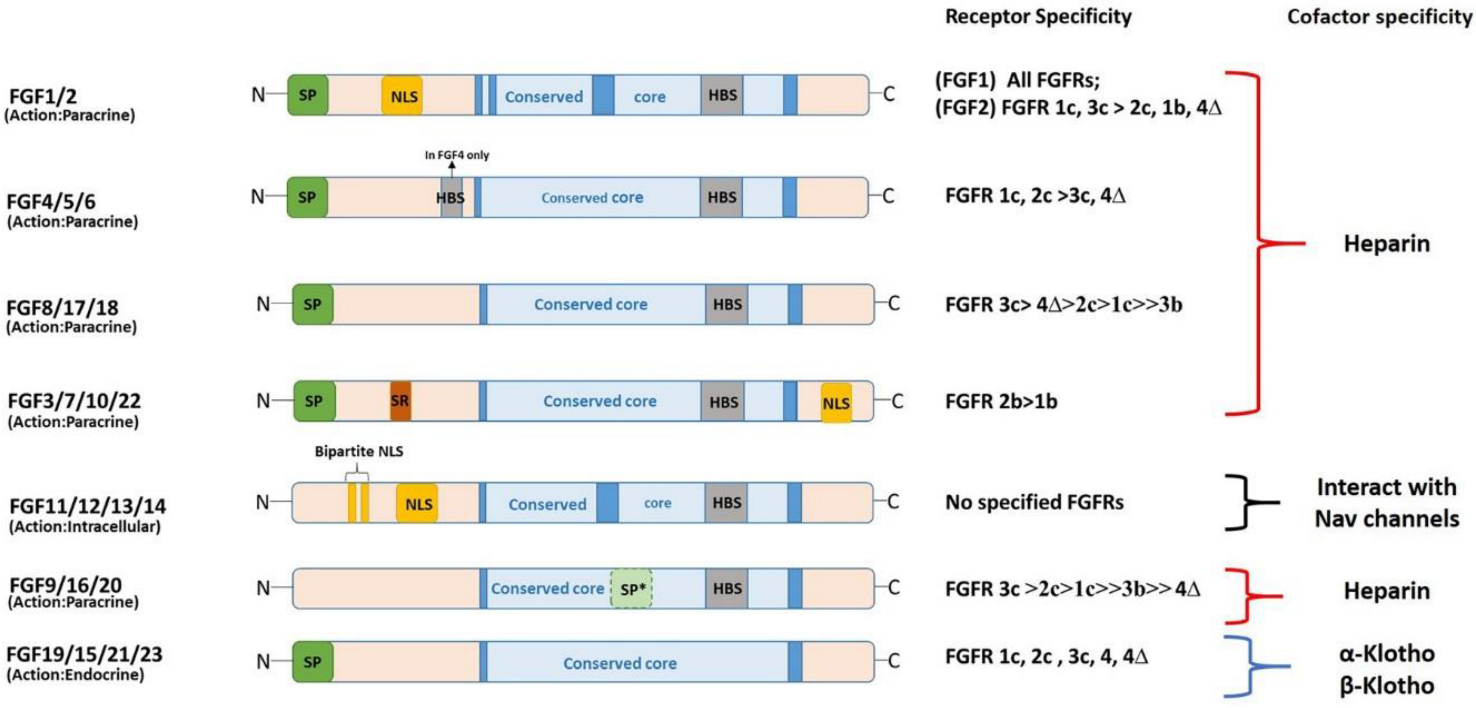
2. Gene Organization and Protein Length
3. Structural and Functional Diversity
4. FGF Signaling in Early Development
4.1. FGF and Mesoderm Specification
4.2. FGF and Neural Specification
4.3. FGF Signaling in Metabolism and Diseases (Cancer)
4.3.1. FGF Signaling in Metabolism
4.3.2. FGF Signaling in Various Types of Cancer
| FGFs | Associated Diseases | References |
|---|---|---|
| FGF1 | Colorectal cancers, breast carcinoma, hepatocellular carcinoma, and esophagus cancer | [139,140,141,142] |
| FGF2 | Rheumatoid arthritis, multiple sclerosis, breast cancer, lung cancer, and glioblastoma | [134,162] |
| FGF3 | Acute rhinitis and chronic sinonasal inflammation | [137,138] |
| FGF4 | Germ cell carcinoma and ovarian cancer | [146,147] |
| FGF5 | Breast cancer | [148] |
| FGF6 | Liver cancer | [149] |
| FGF7 | Gastric adenocarcinoma and gastric inflammation | [150] |
| FGF8 | Prostate cancer | [151,152] |
| FGF9 | Non-small cell lung carcinoma (NSCLC) | [153] |
| FGF10 | Prostate cancer, breast cancer, pancreatic adenocarcinoma, gastric carcinoma, skin cancer and lung squamous cell carcinoma, and acute myeloid leukemia | [154,162] |
| FGF11 | Bladder cancer | [155] |
| FGF12 | Liver fibrosis | [156] |
| FGF13 | Pancreatic cancer, endocrine cancer, and breast cancer | [157] |
| FGF15/19 | Hepatocellular carcinoma | [170] |
| FGF16 | Embryonic carcinoma, ovarian cancer, and liver cancer | [159] |
| FGF17 | Acute myeloid leukemia | [162] |
| FGF18 | Breast cancer | [171] |
| FGF20 | Glioma | [166] |
| FGF21 | Prevents pancreatic ductal adenocarcinoma or hepatocellular carcinoma | [167] |
| FGF14 | Tumor suppressor in colorectal cancer | [158] |
| FGF22 | Pancreatic cancer | [168] |
| FGF23 | Tumor induced ostomalacia | [172] |
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Itoh, N.; Ornitz, D. Functional evolutionary history of the mouseFgf gene family. Dev. Dyn. 2008, 237, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.E.; Williams, L.T. Structural and Functional Diversity in the FGf Receptor Multigene Family. Adv. Cancer Res. 1993, 60, 1–41. [Google Scholar] [CrossRef] [PubMed]
- Morrison, R.S.; Sharma, A.; de Vellis, J.; Bradshaw, R.A. Basic fibroblast growth factor supports the survival of cerebral cortical neurons in primary culture. Proc. Natl. Acad. Sci. USA 1986, 83, 7537–7541. [Google Scholar] [CrossRef]
- Folkman, J.; Klagsbrun, M. Angiogenic factors. Science 1987, 235, 442–447. [Google Scholar] [CrossRef]
- Teven, C.M.; Farina, E.M.; Rivas, J.; Reid, R.R. Fibroblast growth factor (FGF) signaling in development and skeletal diseases. Genes Dis. 2014, 1, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Su, N.; Yang, J.; Tan, Q.; Huang, S.; Jin, M.; Ni, Z.; Zhang, B.; Zhang, D.; Luo, F.; et al. FGF/FGFR signaling in health and disease. Signal Transduct. Target. Ther. 2020, 5, 181. [Google Scholar] [CrossRef]
- Ornitz, D.M.; Itoh, N. Fibroblast growth factors. Genome Biol. 2001, 2, REVIEWS3005. [Google Scholar] [CrossRef]
- Ornitz, D.M. FGFs, heparan sulfate and FGFRs: Complex interactions essential for development. Bioessays 2000, 22, 108–112. [Google Scholar] [CrossRef]
- Kuro-O, M. Endocrine FGFs and Klothos: Emerging concepts. Trends Endocrinol. Metab. 2008, 19, 239–245. [Google Scholar] [CrossRef]
- Ornitz, D.M.; Itoh, N. The Fibroblast Growth Factor signaling pathway. Wiley Interdiscip. Rev. Dev. Biol. 2015, 4, 215–266. [Google Scholar] [CrossRef]
- Goetz, R.; Mohammadi, M. Exploring mechanisms of FGF signalling through the lens of structural biology. Nat. Rev. Mol. Cell Biol. 2013, 14, 166–180. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Goutam, R.S.; Park, S.; Lee, U.; Kim, J. Functional Roles of FGF Signaling in Early Development of Vertebrate Embryos. Cells 2021, 10, 2148. [Google Scholar] [CrossRef] [PubMed]
- Itoh, N.; Ornitz, D.M. Evolution of the Fgf and Fgfr gene families. Trends Genet. 2004, 20, 563–569. [Google Scholar] [CrossRef]
- Kiefer, P.; Acland, P.; Pappin, D.; Peters, G.; Dickson, C. Competition between nuclear localization and secretory signals determines the subcellular fate of a single CUG-initiated form of FGF3. EMBO J. 1994, 13, 4126–4136. [Google Scholar] [CrossRef] [PubMed]
- Arnaud, E.; Touriol, C.; Boutonnet, C.; Gensac, M.-C.; Vagner, S.; Prats, H.; Prats, A.-C. A New 34-Kilodalton Isoform of Human Fibroblast Growth Factor 2 Is Cap Dependently Synthesized by Using a Non-AUG Start Codon and Behaves as a Survival Factor. Mol. Cell. Biol. 1999, 19, 505–514. [Google Scholar] [CrossRef]
- Sunmonu, N.A.; Li, K.; Li, J.Y. Numerous isoforms of Fgf8 reflect its multiple roles in the developing brain. J. Cell. Physiol. 2011, 226, 1722–1726. [Google Scholar] [CrossRef]
- Itoh, N.; Ornitz, D.M. Fibroblast growth factors: From molecular evolution to roles in development, metabolism and disease. J. Biochem. 2011, 149, 121–130. [Google Scholar] [CrossRef]
- Powers, C.J.; McLeskey, S.W.; Wellstein, A. Fibroblast growth factors, their receptors and signaling. Endocr.-Relat. Cancer 2000, 7, 165–197. [Google Scholar] [CrossRef]
- Plotnikov, A.N.; Hubbard, S.R.; Schlessinger, J.; Mohammadi, M. Crystal Structures of Two FGF-FGFR Complexes Reveal the Determinants of Ligand-Receptor Specificity. Cell 2000, 101, 413–424. [Google Scholar] [CrossRef]
- Mohammadi, M.; Olsen, S.K.; Ibrahimi, O.A. Structural basis for fibroblast growth factor receptor activation. Cytokine Growth Factor Rev. 2005, 16, 107–137. [Google Scholar] [CrossRef]
- Laestander, C.; Engström, W. Role of fibroblast growth factors in elicitation of cell responses. Cell Prolif. 2014, 47, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Kolli, V.; Paul, S.; Sarkar, N. An Overview on Fibroblast Growth Factors: Structural, Functional and Therapeutic Implications. Curr. Proteom. 2015, 12, 144–151. [Google Scholar] [CrossRef]
- Friesel, R.; Maciag, T. Fibroblast growth factor prototype release and fibroblast growth factor receptor signaling. Thromb. Haemost. 1999, 82, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Lea, R.; Papalopulu, N.; Amaya, E.; Dorey, K. Temporal and spatial expression of FGF ligands and receptors during Xenopus development. Dev. Dyn. 2009, 238, 1467–1479. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.K.; Shankar, D.B.; Shackleford, G.M.; Wu, K.; T’Ang, A.; Miller, G.J.; Zheng, J.; Roy-Burman, P. Molecular cloning and characterization of human FGF8 alternative messenger RNA forms. Cell Growth Differ. Mol. Biol. J. Am. Assoc. Cancer Res. 1996, 7, 1425–1434. [Google Scholar] [CrossRef]
- Fletcher, R.B.; Baker, J.C.; Harland, R.M. FGF8 spliceforms mediate early mesoderm and posterior neural tissue formation in Xenopus. Development 2006, 133, 1703–1714. [Google Scholar] [CrossRef]
- Crossley, P.H.; Martin, G.R. The mouse Fgf8 gene encodes a family of polypeptides and is expressed in regions that direct outgrowth and patterning in the developing embryo. Development 1995, 121, 439–451. [Google Scholar] [CrossRef]
- Ron, D.; Bottaro, D.P.; Finch, P.W.; Morris, D.; Rubin, J.S.; Aaronson, S.A. Expression of biologically active recombinant keratinocyte growth factor. Structure/function analysis of amino-terminal truncation mutants. J. Biol. Chem. 1993, 268, 2984–2988. [Google Scholar] [CrossRef]
- Yayon, A.; Klagsbrun, M.; Esko, J.D.; Leder, P.; Ornitz, D.M. Cell surface, heparin-like molecules are required for binding of basic fibroblast growth factor to its high affinity receptor. Cell 1991, 64, 841–848. [Google Scholar] [CrossRef]
- Mohammadi, M.; Olsen, S.K.; Goetz, R. A protein canyon in the FGF–FGF receptor dimer selects from an à la carte menu of heparan sulfate motifs. Curr. Opin. Struct. Biol. 2005, 15, 506–516. [Google Scholar] [CrossRef]
- Sacco, A.; Federico, C.; Giacomini, A.; Caprio, C.; Maccarinelli, F.; Todoerti, K.; Favasuli, V.; Anastasia, A.; Motta, M.; Russo, D.; et al. Halting the FGF/FGFR axis leads to antitumor activity in Waldenström macroglobulinemia by silencing MYD88. Blood 2021, 137, 2495–2508. [Google Scholar] [CrossRef]
- Planque, N. Nuclear trafficking of secreted factors and cell-surface receptors: New pathways to regulate cell proliferation and differentiation, and involvement in cancers. Cell Commun. Signal. 2006, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Olsnes, S.; Klingenberg, O.; Wie˛dłocha, A. Transport of Exogenous Growth Factors and Cytokines to the Cytosol and to the Nucleus. Physiol. Rev. 2003, 83, 163–182. [Google Scholar] [CrossRef]
- Rodriguez-Enfedaque, A.; Bouleau, S.; Laurent, M.; Courtois, Y.; Mignotte, B.; Vayssière, J.-L.; Renaud, F. FGF1 nuclear translocation is required for both its neurotrophic activity and its p53-dependent apoptosis protection. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2009, 1793, 1719–1727. [Google Scholar] [CrossRef] [PubMed]
- Bouleau, S.; Grimal, H.; Rincheval, V.; Godefroy, N.; Mignotte, B.; Vayssière, J.-L.; Renaud, F. FGF1 inhibits p53-dependent apoptosis and cell cycle arrest via an intracrine pathway. Oncogene 2005, 24, 7839–7849. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, D.; Janick, L.; Reh, T. Basic fibroblast growth factor (FGF-2) induced transdifferentiation of retinal pigment epithelium: Generation of retinal neurons and glia. Dev. Dyn. 1997, 209, 387–398. [Google Scholar] [CrossRef]
- Fukui, L.; Henry, J.J. FGF Signaling Is Required for Lens Regeneration in Xenopus laevis. Biol. Bull. 2011, 221, 137–145. [Google Scholar] [CrossRef]
- Cailliau, K.; Browaeys-Poly, E.; Vilain, J.P. Fibroblast growth factors 1 and 2 differently activate MAP kinase in Xenopus oocytes expressing fibroblast growth factor receptors 1 and 4. Biochim. Biophys. Acta 2001, 1538, 228–233. [Google Scholar] [CrossRef]
- Zhang, X.; Ibrahimi, O.A.; Olsen, S.; Umemori, H.; Mohammadi, M.; Ornitz, D.M. Receptor Specificity of the Fibroblast Growth Factor Family. J. Biol. Chem. 2006, 281, 15694–15700. [Google Scholar] [CrossRef]
- Ornitz, D.M.; Xu, J.; Colvin, J.S.; McEwen, D.G.; MacArthur, C.A.; Coulier, F.; Gao, G.; Goldfarb, M. Receptor Specificity of the Fibroblast Growth Factor Family. J. Biol. Chem. 1996, 271, 15292–15297. [Google Scholar] [CrossRef]
- Oulion, S.; Bertrand, S.; Escriva, H. Evolution of the FGF Gene Family. Int. J. Evol. Biol. 2012, 2012, 298147. [Google Scholar] [CrossRef]
- Miyakawa, K.; Imamura, T. Secretion of FGF-16 Requires an Uncleaved Bipartite Signal Sequence. J. Biol. Chem. 2003, 278, 35718–35724. [Google Scholar] [CrossRef] [PubMed]
- Miyakawa, K.; Hatsuzawa, K.; Kurokawa, T.; Asada, M.; Kuroiwa, T.; Imamura, T. A Hydrophobic Region Locating at the Center of Fibroblast Growth Factor-9 Is Crucial for Its Secretion. J. Biol. Chem. 1999, 274, 29352–29357. [Google Scholar] [CrossRef]
- Goetz, R.; Beenken, A.; Ibrahimi, O.A.; Kalinina, J.; Olsen, S.K.; Eliseenkova, A.V.; Xu, C.; Neubert, T.A.; Zhang, F.; Linhardt, R.J.; et al. Molecular Insights into the Klotho-Dependent, Endocrine Mode of Action of Fibroblast Growth Factor 19 Subfamily Members. Mol. Cell. Biol. 2007, 27, 3417–3428. [Google Scholar] [CrossRef]
- Potthoff, M.J.; Kliewer, S.A.; Mangelsdorf, D.J. Endocrine fibroblast growth factors 15/19 and 21: From feast to famine. Genes Dev. 2012, 26, 312–324. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Ge, H.; Lemon, B.; Vonderfecht, S.; Weiszmann, J.; Hecht, R.; Gupte, J.; Hager, T.; Wang, Z.; Lindberg, R.; et al. FGF19-induced Hepatocyte Proliferation Is Mediated through FGFR4 Activation. J. Biol. Chem. 2010, 285, 5165–5170. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.-L.; Kolumam, G.; Stawicki, S.; Chen, Y.; Li, J.; Zavala-Solorio, J.; Phamluong, K.; Feng, B.; Li, L.; Marsters, S.; et al. Amelioration of Type 2 Diabetes by Antibody-Mediated Activation of Fibroblast Growth Factor Receptor 1. Sci. Transl. Med. 2011, 3, 113ra126. [Google Scholar] [CrossRef]
- Ding, X.; Boney-Montoya, J.; Owen, B.M.; Bookout, A.L.; Coate, K.C.; Mangelsdorf, D.J.; Kliewer, S.A. betaKlotho is required for fibroblast growth factor 21 effects on growth and metabolism. Cell Metab. 2012, 16, 387–393. [Google Scholar] [CrossRef]
- Yu, C.; Wang, F.; Kan, M.; Jin, C.; Jones, R.B.; Weinstein, M.; Deng, C.-X.; McKeehan, W.L. Elevated Cholesterol Metabolism and Bile Acid Synthesis in Mice Lacking Membrane Tyrosine Kinase Receptor FGFR4. J. Biol. Chem. 2000, 275, 15482–15489. [Google Scholar] [CrossRef]
- French, D.M.; Lin, B.C.; Wang, M.; Adams, C.; Shek, T.; Hötzel, K.; Bolon, B.; Ferrando, R.; Blackmore, C.; Schroeder, K.; et al. Targeting FGFR4 Inhibits Hepatocellular Carcinoma in Preclinical Mouse Models. PLoS ONE 2012, 7, e36713. [Google Scholar] [CrossRef]
- Gattineni, J.; Alphonse, P.; Zhang, Q.; Mathews, N.; Bates, C.M.; Baum, M. Regulation of renal phosphate transport by FGF23 is mediated by FGFR1 and FGFR4. Am. J. Physiol. Physiol. 2014, 306, F351–F358. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, S.; Combet, E.; Stenvinkel, P.; Shiels, P.G. Klotho, Aging, and the Failing Kidney. Front. Endocrinol. 2020, 11, 560. [Google Scholar] [CrossRef] [PubMed]
- Smallwood, P.M.; Munoz-Sanjuan, I.; Tong, P.; Macke, J.P.; Hendry, S.H.; Gilbert, D.J.; Copeland, N.G.; A Jenkins, N.; Nathans, J. Fibroblast growth factor (FGF) homologous factors: New members of the FGF family implicated in nervous system development. Proc. Natl. Acad. Sci. USA 1996, 93, 9850–9857. [Google Scholar] [CrossRef] [PubMed]
- Olsen, S.K.; Garbi, M.; Zampieri, N.; Eliseenkova, A.V.; Ornitz, D.M.; Goldfarb, M.; Mohammadi, M. Fibroblast Growth Factor (FGF) Homologous Factors Share Structural but Not Functional Homology with FGFs. J. Biol. Chem. 2003, 278, 34226–34236. [Google Scholar] [CrossRef]
- Goldfarb, M. Fibroblast growth factor homologous factors: Evolution, structure, and function. Cytokine Growth Factor Rev. 2005, 16, 215–220. [Google Scholar] [CrossRef]
- Schoorlemmer, J.; Goldfarb, M. Fibroblast Growth Factor Homologous Factors and the Islet Brain-2 Scaffold Protein Regulate Activation of a Stress-activated Protein Kinase. J. Biol. Chem. 2002, 277, 49111–49119. [Google Scholar] [CrossRef]
- Wu, Q.-F.; Yang, L.; Li, S.; Wang, Q.; Yuan, X.-B.; Gao, X.; Bao, L.; Zhang, X. Fibroblast Growth Factor 13 Is a Microtubule-Stabilizing Protein Regulating Neuronal Polarization and Migration. Cell 2012, 149, 1549–1564. [Google Scholar] [CrossRef]
- König, H.G.; Fenner, B.J.; Byrne, J.C.; Schwamborn, R.F.; Bernas, T.; Jefferies, C.A.; Prehn, J.H. Fibroblast growth factor homologous factor 1 interacts with NEMO to regulate NF-kappaB signaling in neurons. J. Cell Sci. 2012, 125 Pt 24, 6058–6070. [Google Scholar] [CrossRef]
- Goldfarb, M.; Schoorlemmer, J.; Williams, A.; Diwakar, S.; Wang, Q.; Huang, X.; Giza, J.; Tchetchik, D.; Kelley, K.; Vega, A.; et al. Fibroblast Growth Factor Homologous Factors Control Neuronal Excitability through Modulation of Voltage-Gated Sodium Channels. Neuron 2007, 55, 449–463. [Google Scholar] [CrossRef]
- Amaya, E.; Musci, T.J.; Kirschner, M.W. Expression of a dominant negative mutant of the FGF receptor disrupts mesoderm formation in xenopus embryos. Cell 1991, 66, 257–270. [Google Scholar] [CrossRef]
- Partanen, J.; Schwartz, L.; Rossant, J. Opposite phenotypes of hypomorphic and Y766 phosphorylation site mutations reveal a function for Fgfr1 in anteroposterior patterning of mouse embryos. Genes Dev. 1998, 12, 2332–2344. [Google Scholar] [CrossRef] [PubMed]
- Thisse, B.; Thisse, C. Functions and regulations of fibroblast growth factor signaling during embryonic development. Dev. Biol. 2005, 287, 390–402. [Google Scholar] [CrossRef]
- Stavridis, M.P.; Lunn, J.S.; Collins, B.J.; Storey, K.G. A discrete period of FGF-induced Erk1/2 signalling is required for vertebrate neural specification. Development 2007, 134, 2889–2894. [Google Scholar] [CrossRef]
- Amaya, E.; A Stein, P.; Musci, T.J.; Kirschner, M.W. FGF signalling in the early specification of mesoderm in Xenopus. Development 1993, 118, 477–487. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, R.B.; Harland, R.M. The role of FGF signaling in the establishment and maintenance of mesodermal gene expression in Xenopus. Dev. Dyn. 2008, 237, 1243–1254. [Google Scholar] [CrossRef] [PubMed]
- Fan, T.-P.; Ting, H.-C.; Yu, J.-K.; Su, Y.-H. Reiterative use of FGF signaling in mesoderm development during embryogenesis and metamorphosis in the hemichordate Ptychodera flava. BMC Evol. Biol. 2018, 18, 120. [Google Scholar] [CrossRef]
- Slack, J.M.W.; Darlington, B.G.; Heath, J.K.; Godsave, S.F. Mesoderm induction in early Xenopus embryos by heparin-binding growth factors. Nature 1987, 326, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Cha, S.-W.; Hwang, Y.-S.; Chae, J.-P.; Lee, S.-Y.; Lee, H.-S.; Daar, I.; Park, M.J.; Kim, J. Inhibition of FGF signaling causes expansion of the endoderm in Xenopus. Biochem. Biophys. Res. Commun. 2004, 315, 100–106. [Google Scholar] [CrossRef]
- Burdsal, C.A.; Flannery, M.L.; Pedersen, R.A. FGF-2 alters the fate of mouse epiblast from ectoderm to mesoderm in vitro. Dev. Biol. 1998, 198, 231–244. [Google Scholar] [CrossRef]
- Dvorak, P.; Flechon, J.; Thompson, E.; Horak, V.; Adenot, P.; Renard, J. Embryoglycans regulate FGF-2-mediated mesoderm induction in the rabbit embryo. J. Cell Sci. 1997, 110 Pt 1, 1–10. [Google Scholar] [CrossRef]
- Mossahebi-Mohammadi, M.; Quan, M.; Zhang, J.-S.; Li, X. FGF Signaling Pathway: A Key Regulator of Stem Cell Pluripotency. Front. Cell Dev. Biol. 2020, 8, 79. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, V.; Hudson, C.; Caillol, D.; Popovici, C.; Lemaire, P. Neural Tissue in Ascidian Embryos Is Induced by FGF9/16/20, Acting via a Combination of Maternal GATA and Ets Transcription Factors. Cell 2003, 115, 615–627. [Google Scholar] [CrossRef]
- Henrique, D.; Abranches, E.; Verrier, L.; Storey, K.G. Neuromesodermal progenitors and the making of the spinal cord. Development 2015, 142, 2864–2875. [Google Scholar] [CrossRef]
- Wilson, V.I. Olivera-Martinez, and K.G. Storey, Stem cells, signals and vertebrate body axis extension. Development 2009, 136, 1591–1604. [Google Scholar] [CrossRef]
- del Corral, R.D.; Morales, A.V. The Multiple Roles of FGF Signaling in the Developing Spinal Cord. Front. Cell Dev. Biol. 2017, 5, 58. [Google Scholar] [CrossRef]
- Delfino-Machín, M.; Lunn, J.S.; Breitkreuz, D.N.; Akai, J.; Storey, K. Specification and maintenance of the spinal cord stem zone. Development 2005, 132, 4273–4283. [Google Scholar] [CrossRef]
- Karabagli, H.; Karabagli, P.; Ladher, R.K.; Schoenwolf, G.C. Comparison of the expression patterns of several fibroblast growth factors during chick gastrulation and neurulation. Anat. Embryol. 2002, 205, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Wahl, M.B.; Deng, C.; Lewandoski, M.; Pourquie, O. FGF signaling acts upstream of the NOTCH and WNT signaling pathways to control segmentation clock oscillations in mouse somitogenesis. Development 2007, 134, 4033–4041. [Google Scholar] [CrossRef] [PubMed]
- Gofflot, F.; Hall, M.; Morriss-Kay, G. Genetic patterning of the developing mouse tail at the time of posterior neuropore closure. Dev. Dyn. 1997, 210, 431–445. [Google Scholar] [CrossRef]
- Anderson, M.J.; Schimmang, T.; Lewandoski, M. An FGF3-BMP Signaling Axis Regulates Caudal Neural Tube Closure, Neural Crest Specification and Anterior-Posterior Axis Extension. PLoS Genet. 2016, 12, e1006018. [Google Scholar] [CrossRef]
- Miya, T.; Nishida, H. An Ets transcription factor, HrEts, is target of FGF signaling and involved in induction of notochord, mesenchyme, and brain in ascidian embryos. Dev. Biol. 2003, 261, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Spemann, H.; Mangold, H. über Induktion von Embryonalanlagen durch Implantation artfremder Organisatoren. Dev. Genes Evol. 1924, 100, 599–638. [Google Scholar] [CrossRef]
- Wilson, S.I.; Edlund, T. Neural induction: Toward a unifying mechanism. Nat. Neurosci. 2001, 4, 1161–1168. [Google Scholar] [CrossRef] [PubMed]
- Stern, C.D. Neural induction: Old problem, new findings, yet more questions. Development 2005, 132, 2007–2021. [Google Scholar] [CrossRef]
- Yoon, J.; Kim, J.-H.; Lee, S.-Y.; Kim, S.; Park, J.-B.; Lee, J.-Y.; Kim, J. PV.1 induced by FGF-Xbra functions as a repressor of neurogenesis in Xenopus embryos. BMB Rep. 2014, 47, 673–678. [Google Scholar] [CrossRef]
- Marchal, L.; Luxardi, G.; Thomé, V.; Kodjabachian, L. BMP inhibition initiates neural induction via FGF signaling and Zic genes. Proc. Natl. Acad. Sci. USA 2009, 106, 17437–17442. [Google Scholar] [CrossRef]
- Nichols, J.; Zevnik, B.; Anastassiadis, K.; Niwa, H.; Klewe-Nebenius, D.; Chambers, I.; Schöler, H.; Smith, A. Formation of Pluripotent Stem Cells in the Mammalian Embryo Depends on the POU Transcription Factor Oct4. Cell 1998, 95, 379–391. [Google Scholar] [CrossRef]
- Mayshar, Y.; Rom, E.; Chumakov, I.; Kronman, A.; Yayon, A.; Benvenisty, N. Fibroblast Growth Factor 4 and Its Novel Splice Isoform Have Opposing Effects on the Maintenance of Human Embryonic Stem Cell Self-Renewal. Stem Cells 2008, 26, 767–774. [Google Scholar] [CrossRef]
- Crossley, P.H.; Martinez, S.; Martin, G.R. Midbrain development induced by FGF8 in the chick embryo. Nature 1996, 380, 66–68. [Google Scholar] [CrossRef]
- Hongo, I.; Okamoto, H. FGF/MAPK/Ets signaling in Xenopus ectoderm contributes to neural induction and patterning in an autonomous and paracrine manner, respectively. Cells Dev. 2022, 170, 203769. [Google Scholar] [CrossRef]
- Kang, W.; Hébert, J.M. FGF Signaling Is Necessary for Neurogenesis in Young Mice and Sufficient to Reverse Its Decline in Old Mice. J. Neurosci. 2015, 35, 10217–10223. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Davis, A.A.; Goderie, S.K.; Temple, S. FGF2 Concentration Regulates the Generation of Neurons and Glia from Multipotent Cortical Stem Cells. Neuron 1997, 18, 81–93. [Google Scholar] [CrossRef]
- Nelson, A.D.; Svendsen, C.N. Low concentrations of extracellular FGF-2 are sufficient but not essential for neurogenesis from human neural progenitor cells. Mol. Cell. Neurosci. 2006, 33, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Kilpatrick, T.; Bartlett, P. Cloning and growth of multipotential neural precursors: Requirements for proliferation and differentiation. Neuron 1993, 10, 255–265. [Google Scholar] [CrossRef]
- Gritti, A.; Parati, E.; Cova, L.; Frolichsthal, P.; Galli, R.; Wanke, E.; Faravelli, L.; Morassutti, D.; Roisen, F.; Nickel, D.; et al. Multipotential stem cells from the adult mouse brain proliferate and self-renew in response to basic fibroblast growth factor. J. Neurosci. 1996, 16, 1091–1100. [Google Scholar] [CrossRef]
- Gage, J.R.F.H.; Ray, J.; Fisher, L.J. Isolation, Characterization, and use of Stem Cells from the CNS. Annu. Rev. Neurosci. 1995, 18, 159–192. [Google Scholar] [CrossRef]
- Yan, H.Q.; Yu, J.; Kline, A.E.; Letart, P.; Jenkins, L.W.; Marion, D.W.; Dixon, C. Evaluation of combined fibroblast growth factor-2 and moderate hypothermia therapy in traumatically brain injured rats. Brain Res. 2000, 887, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Rabchevsky, A.G.; Fugaccia, I.; Fletcher-Turner, A.; Blades, D.A.; Mattson, M.P.; Scheff, S.W. Basic Fibroblast Growth Factor (bFGF) Enhances Tissue Sparing and Functional Recovery Following Moderate Spinal Cord Injury. J. Neurotrauma 1999, 16, 817–830. [Google Scholar] [CrossRef]
- Lee, T.T.; Green, B.A.; Dietrich, W.D.; Yezierski, R.P. Neuroprotective Effects of Basic Fibroblast Growth Factor Following Spinal Cord Contusion Injury in the Rat. J. Neurotrauma 1999, 16, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.N.; Oh, S.H.; Lee, K.H.; Yoon, D.H. Effect of human mesenchymal stem cell transplantation combined with growth factor infusion in the repair of injured spinal cord. Adv. Funct. Reparative Neurosurg. 2006, 99, 133–136. [Google Scholar] [CrossRef]
- Klimaschewski, L.; Claus, P. Fibroblast Growth Factor Signalling in the Diseased Nervous System. Mol. Neurobiol. 2021, 58, 3884–3902. [Google Scholar] [CrossRef]
- Umemori, H.; Linhoff, M.W.; Ornitz, D.M.; Sanes, J.R. FGF22 and Its Close Relatives Are Presynaptic Organizing Molecules in the Mammalian Brain. Cell 2004, 118, 257–270. [Google Scholar] [CrossRef]
- Lee, C.H.; Javed, D.; Althaus, A.L.; Parent, J.M.; Umemori, H. Neurogenesis is enhanced and mossy fiber sprouting arises in FGF7-deficient mice during development. Mol. Cell. Neurosci. 2012, 51, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Kliewer, S.A.; Mangelsdorf, D.J. Bile Acids as Hormones: The FXR-FGF15/19 Pathway. Dig. Dis. 2015, 33, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Song, K.-H.; Li, T.; Owsley, E.; Strom, S.; Chiang, J.Y.L. Bile acids activate fibroblast growth factor 19 signaling in human hepatocytes to inhibit cholesterol 7α-hydroxylase gene expression. Hepatology 2009, 49, 297–305. [Google Scholar] [CrossRef]
- Fu, L.; John, L.M.; Adams, S.H.; Yu, X.X.; Tomlinson, E.; Renz, M.; Williams, P.M.; Soriano, R.; Corpuz, R.; Moffat, B.; et al. Fibroblast Growth Factor 19 Increases Metabolic Rate and Reverses Dietary and Leptin-Deficient Diabetes. Endocrinology 2004, 145, 2594–2603. [Google Scholar] [CrossRef]
- Tomlinson, E.; Fu, L.; John, L.; Hultgren, B.; Huang, X.; Renz, M.; Stephan, J.P.; Tsai, S.P.; Powell-Braxton, L.; French, D.; et al. Transgenic mice expressing human fibroblast growth factor-19 display increased metabolic rate and decreased adiposity. Endocrinology 2002, 143, 1741–1747. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, S.; Damron, H.A.; Hillgartner, F. Fibroblast Growth Factor-19, a Novel Factor That Inhibits Hepatic Fatty Acid Synthesis. J. Biol. Chem. 2009, 284, 10023–10033. [Google Scholar] [CrossRef]
- Massafra, V.; Milona, A.; Vos, H.R.; Burgering, B.M.T.; van Mil, S.W.C. Quantitative liver proteomics identifies FGF19 targets that couple metabolism and proliferation. PLoS ONE 2017, 12, e0171185. [Google Scholar] [CrossRef]
- Alvarez-Sola, G.; Uriarte, I.; Latasa, M.U.; Fernandez-Barrena, M.G.; Urtasun, R.; Elizalde, M.; Barcena-Varela, M.; Jiménez, M.; Chang, H.; Barbero, R.; et al. Fibroblast growth factor 15/19 (FGF15/19) protects from diet-induced hepatic steatosis: Development of an FGF19-based chimeric molecule to promote fatty liver regeneration. Gut 2017, 66, 1818–1828. [Google Scholar] [CrossRef]
- Ryan, K.K.; Kohli, R.; Gutierrez-Aguilar, R.; Gaitonde, S.G.; Woods, S.C.; Seeley, R.J. Fibroblast Growth Factor-19 Action in the Brain Reduces Food Intake and Body Weight and Improves Glucose Tolerance in Male Rats. Endocrinology 2013, 154, 9–15. [Google Scholar] [CrossRef]
- Bookout, A.L.; De Groot, M.H.M.; Owen, B.; Lee, S.; Gautron, L.; Lawrence, H.L.; Ding, X.; Elmquist, J.K.; Takahashi, J.; Mangelsdorf, D.; et al. FGF21 regulates metabolism and circadian behavior by acting on the nervous system. Nat. Med. 2013, 19, 1147–1152. [Google Scholar] [CrossRef] [PubMed]
- Marcelin, G.; Jo, Y.-H.; Li, X.; Schwartz, G.J.; Zhang, Y.; Dun, N.J.; Lyu, R.-M.; Blouet, C.; Chang, J.K.; Chua, S., Jr. Central action of FGF19 reduces hypothalamic AGRP/NPY neuron activity and improves glucose metabolism. Mol. Metab. 2014, 3, 19–28. [Google Scholar] [CrossRef]
- Wu, A.-L.; Coulter, S.; Liddle, C.; Wong, A.; Eastham-Anderson, J.; French, D.M.; Peterson, A.S.; Sonoda, J. FGF19 Regulates Cell Proliferation, Glucose and Bile Acid Metabolism via FGFR4-Dependent and Independent Pathways. PLoS ONE 2011, 6, e17868. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Wang, X.; Phung, V.; Lindhout, D.A.; Mondal, K.; Hsu, J.-Y.; Yang, H.; Humphrey, M.; Ding, X.; Arora, T.; et al. Separating Tumorigenicity from Bile Acid Regulatory Activity for Endocrine Hormone FGF19. Cancer Res. 2014, 74, 3306–3316. [Google Scholar] [CrossRef]
- Tacer, K.F.; Bookout, A.L.; Ding, X.; Kurosu, H.; John, G.B.; Wang, L.; Goetz, R.; Mohammadi, M.; Kuro-O, M.; Mangelsdorf, D.J.; et al. Research Resource: Comprehensive Expression Atlas of the Fibroblast Growth Factor System in Adult Mouse. Mol. Endocrinol. 2010, 24, 2050–2064. [Google Scholar] [CrossRef]
- Coskun, T.; Bina, H.A.; Schneider, M.A.; Dunbar, J.D.; Hu, C.C.; Chen, Y.; Moller, D.E.; Kharitonenkov, A. Fibroblast Growth Factor 21 Corrects Obesity in Mice. Endocrinology 2008, 149, 6018–6027. [Google Scholar] [CrossRef]
- Xu, J.; Lloyd, D.J.; Hale, C.; Stanislaus, S.; Chen, M.; Sivits, G.; Vonderfecht, S.; Hecht, R.; Li, Y.-S.; Lindberg, R.A.; et al. Fibroblast Growth Factor 21 Reverses Hepatic Steatosis, Increases Energy Expenditure, and Improves Insulin Sensitivity in Diet-Induced Obese Mice. Diabetes 2009, 58, 250–259. [Google Scholar] [CrossRef] [PubMed]
- Kharitonenkov, A.; Beals, J.M.; Micanovic, R.; Strifler, B.A.; Rathnachalam, R.; Wroblewski, V.J.; Li, S.; Koester, A.; Ford, A.M.; Coskun, T.; et al. Rational Design of a Fibroblast Growth Factor 21-Based Clinical Candidate, LY2405319. PLoS ONE 2013, 8, e58575. [Google Scholar] [CrossRef]
- Gaich, G.; Chien, J.Y.; Fu, H.; Glass, L.C.; Deeg, M.A.; Holland, W.L.; Kharitonenkov, A.; Bumol, T.; Schilske, H.K.; Moller, D.E. The Effects of LY2405319, an FGF21 Analog, in Obese Human Subjects with Type 2 Diabetes. Cell Metab. 2013, 18, 333–340. [Google Scholar] [CrossRef]
- Shapter, A.E. The overpass syndrome. Can. Med. Assoc. J. 1992, 146, 113. [Google Scholar]
- Quarles, L.D. Skeletal secretion of FGF-23 regulates phosphate and vitamin D metabolism. Nat. Rev. Endocrinol. 2012, 8, 276–286. [Google Scholar] [CrossRef]
- Consortium, A. Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat. Genet. 2000, 26, 345–348. [Google Scholar]
- Shimada, T.; Urakawa, I.; Yamazaki, Y.; Hasegawa, H.; Hino, R.; Yoneya, T.; Takeuchi, Y.; Fujita, T.; Fukumoto, S.; Yamashita, T. FGF-23 transgenic mice demonstrate hypophosphatemic rickets with reduced expression of sodium phosphate cotransporter type IIa. Biochem. Biophys. Res. Commun. 2004, 314, 409–414. [Google Scholar] [CrossRef]
- Larsson, T.; Marsell, R.; Schipani, E.; Ohlsson, C.; Ljunggren, O.; Tenenhouse, H.S.; Jppner, H.; Jonsson, K.B. Transgenic mice expressing fibroblast growth factor 23 under the control of the alpha1(I) collagen promoter exhibit growth retardation, osteomalacia, and disturbed phosphate homeostasis. Endocrinology 2004, 145, 3087–3094. [Google Scholar] [CrossRef]
- Bai, X.; Miao, D.; Li, J.; Goltzman, D.; Karaplis, A.C. Transgenic Mice Overexpressing Human Fibroblast Growth Factor 23 (R176Q) Delineate a Putative Role for Parathyroid Hormone in Renal Phosphate Wasting Disorders. Endocrinology 2004, 145, 5269–5279. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Hui, E.Y.L.; Woo, Y.C.; Yeung, C.Y.; Chow, W.S.; Yuen, M.M.A.; Fong, C.H.Y.; Xu, A.; Lam, K.S.L. Circulating Fibroblast Growth Factor 21 Levels Predict Progressive Kidney Disease in Subjects with Type 2 Diabetes and Normoalbuminuria. J. Clin. Endocrinol. Metab. 2015, 100, 1368–1375. [Google Scholar] [CrossRef]
- El-Saeed, A.M.; El-Mohasseb, G.F. Circulating Fibroblast Growth Factors 21 and 23 as Biomarkers of Progression in Diabetic Nephropathy in Type 2 Diabetes with Normoalbuminuria. Egypt. J. Immunol. 2017, 24, 93–99. [Google Scholar]
- Aono, Y.; Yamazaki, Y.; Yasutake, J.; Kawata, T.; Hasegawa, H.; Urakawa, I.; Fujita, T.; Wada, M.; Yamashita, T.; Fukumoto, S.; et al. Therapeutic Effects of Anti-FGF23 Antibodies in Hypophosphatemic Rickets/Osteomalacia. J. Bone Miner. Res. 2009, 24, 1879–1888. [Google Scholar] [CrossRef] [PubMed]
- Masuda, Y.; Ohta, H.; Morita, Y.; Nakayama, Y.; Miyake, A.; Itoh, N.; Konishi, M. Expression of Fgf23 in Activated Dendritic Cells and Macrophages in Response to Immunological Stimuli in Mice. Biol. Pharm. Bull. 2015, 38, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Jonker, J.W.; Suh, J.M.; Atkins, A.R.; Ahmadian, M.; Li, P.; Whyte, J.; He, M.; Juguilon, H.; Yin, Y.-Q.; Phillips, C.T.; et al. A PPARgamma-FGF1 axis is required for adaptive adipose remodelling and metabolic homeostasis. Nature 2012, 485, 391–394. [Google Scholar] [CrossRef]
- Byrd, V.M.; Ballard, D.W.; Miller, G.G.; Thomas, J.W. Fibroblast growth factor-1 (FGF-1) enhances IL-2 production and nuclear translocation of NF-kappaB in FGF receptor-bearing Jurkat T cells. J. Immunol. 1999, 162, 5853–5859. [Google Scholar] [CrossRef]
- Suh, J.M.; Jonker, J.W.; Ahmadian, M.; Goetz, R.; Lackey, D.; Osborn, O.; Huang, Z.; Liu, W.; Yoshihara, E.; Van Dijk, T.H.; et al. Endocrinization of FGF1 produces a neomorphic and potent insulin sensitizer. Nature 2014, 513, 436–439. [Google Scholar] [CrossRef] [PubMed]
- Harada, M.; Kamimura, D.; Arima, Y.; Kohsaka, H.; Nakatsuji, Y.; Nishida, M.; Atsumi, T.; Meng, J.; Bando, H.; Singh, R.; et al. Temporal Expression of Growth Factors Triggered by Epiregulin Regulates Inflammation Development. J. Immunol. 2015, 194, 1039–1046. [Google Scholar] [CrossRef]
- Keating, S.; Golub, E.T.; Nowicki, M.; Young, M.; Anastos, K.; Crystal, H.; Cohen, M.H.; Zhang, J.; Greenblatt, R.M.; Desai, S.; et al. The effect of HIV infection and HAART on inflammatory biomarkers in a population-based cohort of women. Aids 2011, 25, 1823–1832. [Google Scholar] [CrossRef]
- Presta, M.; Andres, G.; Leali, D.; Dell’Era, P.; Ronca, R. Inflammatory cells and chemokines sustain FGF2-induced angiogenesis. Eur. Cytokine Netw. 2009, 20, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Sautter, N.B.; Delaney, K.L.; Trune, D.R. Altered expression of tissue remodeling genes in a mouse model of acute allergic rhinitis. Int. Forum Allergy Rhinol. 2011, 1, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Sautter, N.B.; Bs, K.L.D.; Ba, F.A.H.; Trune, D.R. Tissue remodeling gene expression in a murine model of chronic rhinosinusitis. Laryngoscope 2012, 122, 711–717. [Google Scholar] [CrossRef]
- Szlachcic, A.; Sochacka, M.; Czyrek, A.; Opalinski, L.; Krowarsch, D.; Otlewski, J.; Zakrzewska, M. Low Stability of Integrin-Binding Deficient Mutant of FGF1 Restricts Its Biological Activity. Cells 2019, 8, 899. [Google Scholar] [CrossRef] [PubMed]
- Slattery, M.L.; John, E.M.; Stern, M.C.; Herrick, J.; Lundgreen, A.; Giuliano, A.R.; Hines, L.; Baumgartner, K.B.; Torres-Mejia, G.; Wolff, R.K.; et al. Associations with growth factor genes (FGF1, FGF2, PDGFB, FGFR2, NRG2, EGF, ERBB2) with breast cancer risk and survival: The Breast Cancer Health Disparities Study. Breast Cancer Res. Treat. 2013, 140, 587–601. [Google Scholar] [CrossRef]
- Ribatti, D.; Vacca, A.; Rusnati, M.; Presta, M. The discovery of basic fibroblast growth factor/fibroblast growth factor-2 and its role in haematological malignancies. Cytokine Growth Factor Rev. 2007, 18, 327–334. [Google Scholar] [CrossRef]
- Duan, T.; Zhou, D.; Yao, Y.; Shao, X. The Association of Aberrant Expression of FGF1 and mTOR-S6K1 in Colorectal Cancer. Front. Oncol. 2021, 11, 706838. [Google Scholar] [CrossRef] [PubMed]
- Giulianelli, S.; Riggio, M.; Guillardoy, T.; Pérez Piñero, C.; Gorostiaga, M.A.; Sequeira, G.; Pataccini, G.; Abascal, M.F.; Toledo, M.F.; Jacobsen, B.M.; et al. FGF2 induces breast cancer growth through ligand-independent activation and recruitment of ERalpha and PRBDelta4 isoform to MYC regulatory sequences. Int. J. Cancer 2019, 145, 1874–1888. [Google Scholar] [PubMed]
- Hamamoto, J.; Yasuda, H.; Nonaka, Y.; Fujiwara, M.; Nakamura, Y.; Soejima, K.; Betsuyaku, T. The FGF2 aptamer inhibits the growth of FGF2-FGFR pathway driven lung cancer cells. Biochem. Biophys. Res. Commun. 2018, 503, 1330–1334. [Google Scholar] [CrossRef]
- Wang, Y.; Becker, D. Antisense targeting of basic fibroblast growth factor and dibroblast growth factor receptor-1 in human melanomas blocks intratumoral angiogenesis and tumor growth. Nat. Med. 1997, 3, 887–893. [Google Scholar] [CrossRef] [PubMed]
- Maerz, W.J.; Baselga, J.; Reuter, V.E.; Mellado, B.; Myers, M.L.; Bosl, G.J.; Spinella, M.J.; Dmitrovsky, E. FGF4 dissociates anti-tumorigenic from differentiation signals of retinoic acid in human embryonal carcinomas. Oncogene 1998, 17, 761–767. [Google Scholar] [CrossRef]
- Yasuda, K.; Torigoe, T.; Mariya, T.; Asano, T.; Kuroda, T.; Matsuzaki, J.; Ikeda, K.; Yamauchi, M.; Emori, M.; Asanuma, H.; et al. Fibroblasts induce expression of FGF4 in ovarian cancer stem-like cells/cancer-initiating cells and upregulate their tumor initiation capacity. Lab. Investig. 2014, 94, 1355–1369. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, H.; Yang, Y. Expression of Fibroblast Growth Factor 5 (FGF5) and Its Influence on Survival of Breast Cancer Patients. Experiment 2018, 24, 3524–3530. [Google Scholar] [CrossRef]
- Guo, S.; Jiang, S.; Epperla, N.; Ma, Y.; Maadooliat, M.; Ye, Z.; Olson, B.; Wang, M.; Kitchner, T.; Joyce, J.; et al. A gene-based recessive diplotype exome scan discovers FGF6, a novel hepcidin-regulating iron-metabolism gene. Blood 2019, 133, 1888–1898. [Google Scholar] [CrossRef]
- Shaoul, R.; Eliahu, L.; Sher, I.; Hamlet, Y.; Miselevich, I.; Goldshmidt, O.; Ron, D. Elevated expression of FGF7 protein is common in human gastric diseases. Biochem. Biophys. Res. Commun. 2006, 350, 825–833. [Google Scholar] [CrossRef]
- Dorkin, T.J.; Robinson, M.C.; Marsh, C.; Bjartell, A.; Neal, D.E.; Leung, H.Y. FGF8 over-expression in prostate cancer is associated with decreased patient survival and persists in androgen independent disease. Oncogene 1999, 18, 2755–2761. [Google Scholar] [CrossRef] [PubMed]
- Bera, A.; Leighton, X.-M.; Pollard, H.; Srivastava, M. Cyclin E and FGF8 are downstream cell growth regulators in distinct tumor suppressor effects of ANXA7 in hormone-resistant cancer cells of breast versus prostate origin. Trends Cancer Res. 2018, 13, 55–62. [Google Scholar] [PubMed]
- Hegab, A.E.; Ozaki, M.; Kagawa, S.; Hamamoto, J.; Yasuda, H.; Naoki, K.; Soejima, K.; Yin, Y.; Kinoshita, T.; Yaguchi, T.; et al. Tumor associated macrophages support the growth of FGF9-induced lung adenocarcinoma by multiple mechanisms. Lung Cancer 2018, 119, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Clayton, N.S.; Grose, R.P. Emerging Roles of Fibroblast Growth Factor 10 in Cancer. Front. Genet. 2018, 9, 499. [Google Scholar] [CrossRef]
- Li, J.; Cao, J.; Li, P.; Yao, Z.; Deng, R.; Ying, L.; Tian, J. Construction of a novel mRNA-signature prediction model for prognosis of bladder cancer based on a statistical analysis. BMC Cancer 2021, 21, 858. [Google Scholar] [CrossRef]
- Li, S.; Zhou, B.; Xue, M.; Zhu, J.; Tong, G.; Fan, J.; Zhu, K.; Hu, Z.; Chen, R.; Dong, Y.; et al. Macrophage-specific FGF12 promotes liver fibrosis progression in mice. Hepatology 2023, 77, 816–833. [Google Scholar] [CrossRef]
- Bublik, D.R.; Bursac, S.; Sheffer, M.; Oršolić, I.; Shalit, T.; Tarcic, O.; Kotler, E.; Mouhadeb, O.; Hoffman, Y.; Fuchs, G.; et al. Regulatory module involving FGF13, miR-504, and p53 regulates ribosomal biogenesis and supports cancer cell survival. Proc. Natl. Acad. Sci. USA 2017, 114, E496–E505. [Google Scholar] [CrossRef]
- Su, T.; Huang, L.; Zhang, N.; Peng, S.; Li, X.; Wei, G.; Zhai, E.; Zeng, Z.; Xu, L. FGF14 Functions as a Tumor Suppressor through Inhibiting PI3K/AKT/mTOR Pathway in Colorectal Cancer. J. Cancer 2020, 11, 819–825. [Google Scholar] [CrossRef]
- He, W.; Liu, X.; Luo, Z.; Li, L.; Fang, X. FGF16 regulated by miR-520b enhances the cell proliferation of lung cancer. Open Med. 2021, 16, 419–427. [Google Scholar] [CrossRef]
- Koneczny, I.; Schulenburg, A.; Hudec, X.; Knöfler, M.; Holzmann, K.; Piazza, G.; Reynolds, R.; Valent, P.; Marian, B. Autocrine fibroblast growth factor 18 signaling mediates Wnt-dependent stimulation of CD44-positive human colorectal adenoma cells. Mol. Carcinog. 2015, 54, 789–799. [Google Scholar] [CrossRef]
- Zhang, J.; Zhou, Y.; Huang, T.; Wu, F.; Pan, Y.; Dong, Y.; Wang, Y.; Chan, A.K.Y.; Liu, L.; Kwan, J.S.H.; et al. FGF18, a prominent player in FGF signaling, promotes gastric tumorigenesis through autocrine manner and is negatively regulated by miR-590-5p. Oncogene 2019, 38, 33–46. [Google Scholar] [CrossRef]
- Ling, Y.; Du, Q. FGF10/FGF17 as prognostic and drug response markers in acute myeloid leukemia. Curr. Res. Transl. Med. 2022, 70, 103316. [Google Scholar] [CrossRef] [PubMed]
- Sawey, E.T.; Chanrion, M.; Cai, C.; Wu, G.; Zhang, J.; Zender, L.; Zhao, A.; Busuttil, R.W.; Yee, H.; Stein, L.; et al. Identification of a Therapeutic Strategy Targeting Amplified FGF19 in Liver Cancer by Oncogenomic Screening. Cancer Cell 2011, 19, 347–358. [Google Scholar] [CrossRef]
- Wang, H.; Venkatesh, M.; Li, H.; Goetz, R.; Mukherjee, S.; Biswas, A.; Zhu, L.; Kaubisch, A.; Wang, L.; Pullman, J.; et al. Pregnane X receptor activation induces FGF19-dependent tumor aggressiveness in humans and mice. J. Clin. Investig. 2011, 121, 3220–3232. [Google Scholar] [CrossRef]
- Desnoyers, L.R.; Pai, R.; E Ferrando, R.; Hötzel, K.; Le, T.; Ross, J.; Carano, R.; D’Souza, A.; Qing, J.; Mohtashemi, I.; et al. Targeting FGF19 inhibits tumor growth in colon cancer xenograft and FGF19 transgenic hepatocellular carcinoma models. Oncogene 2008, 27, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Tao, W.; Li, L. Glioma cell-derived FGF20 suppresses macrophage function by activating beta-catenin. Cell Signal. 2022, 89, 110181. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Li, X.; Luo, Y. FGF21 in obesity and cancer: New insights. Cancer Lett. 2021, 499, 5–13. [Google Scholar] [CrossRef]
- Zhang, Z.; Qin, Y.; Ji, S.; Xu, W.; Liu, M.; Hu, Q.; Ye, Z.; Fan, G.; Yu, X.; Liu, W.; et al. FGFBP1-mediated crosstalk between fibroblasts and pancreatic cancer cells via FGF22/FGFR2 promotes invasion and metastasis of pancreatic cancer. Acta Biochim. Biophys. Sin. 2021, 53, 997–1008. [Google Scholar] [CrossRef]
- Feng, S.; Wang, J.; Zhang, Y.; Creighton, C.J.; Ittmann, M. FGF23 promotes prostate cancer progression. Oncotarget 2015, 6, 17291–17301. [Google Scholar] [CrossRef]
- Alvarez-Sola, G.; Uriarte, I.; Latasa, M.U.; Urtasun, R.; Bárcena-Varela, M.; Elizalde, M.; Jiménez, M.; Rodriguez-Ortigosa, C.M.; Corrales, F.J.; Fernández-Barrena, M.G.; et al. Fibroblast Growth Factor 15/19 in Hepatocarcinogenesis. Dig Dis. 2017, 35, 158–165. [Google Scholar] [CrossRef]
- Song, N.; Zhong, J.; Hu, Q.; Gu, T.; Yang, B.; Zhang, J.; Yu, J.; Ma, X.; Chen, Q.; Qi, J.; et al. FGF18 Enhances Migration and the Epithelial-Mesenchymal Transition in Breast Cancer by Regulating Akt/GSK3beta/Beta-Catenin Signaling. Cell Physiol. Biochem. 2018, 49, 1019–1032. [Google Scholar] [CrossRef] [PubMed]
- Florenzano, P.; Hartley, I.R.; Jimenez, M.; Roszko, K.; Gafni, R.I.; Collins, M.T. Tumor-Induced Osteomalacia. Calcif. Tissue Int. 2021, 108, 128–142. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Su, N.; Jin, M.; Qi, H.; Yang, J.; Li, C.; Du, X.; Luo, F.; Chen, B.; Shen, Y.; et al. Intermittent PTH (1-34) injection rescues the retarded skeletal development and postnatal lethality of mice mimicking human achondroplasia and thanatophoric dysplasia. Hum. Mol. Genet. 2012, 21, 3941–3955. [Google Scholar] [CrossRef] [PubMed]
- Anreddy, N.; Patel, A.; Sodani, K.; Kathawala, R.J.; Chen, E.P.; Wurpel, J.N.; Chen, Z.-S. PD173074, a selective FGFR inhibitor, reverses MRP7 (ABCC10)-mediated MDR. Acta Pharm. Sin. B 2014, 4, 202–207. [Google Scholar] [CrossRef] [PubMed]
- A Wainberg, Z.; Enzinger, P.C.; Kang, Y.-K.; Qin, S.; Yamaguchi, K.; Kim, I.-H.; Saeed, A.; Oh, S.C.; Li, J.; Turk, H.M.; et al. Bemarituzumab in patients with FGFR2b-selected gastric or gastro-oesophageal junction adenocarcinoma (FIGHT): A randomised, double-blind, placebo-controlled, phase 2 study. Lancet Oncol. 2022, 23, 1430–1440. [Google Scholar] [CrossRef] [PubMed]

| Fgfs | Human | Mus musculus | Xenopus tropicalis |
|---|---|---|---|
| Fgf1 | Chr5: 142,001,623–142,022,227 (20,605 bp) | Chr18: 38,971,725–39,062,532 (90,807 bp) | Chr3: 37,101,483–37,152,750 (51.27 kb) |
| Fgf2 | Chr4: 124,206,684–124,278,197 (71,514 bp) | Chr3: 37,402,616–37,464,255 (61,639 bp) | Chr1: 65,933,388–65,960,806 (27.42 kb) |
| Fgf3 | Chr11: 69,397,666–69,406,878 (9213 bp) | Chr7: 144,392,349–144,397,085 (4736 bp) | Chr4: 12,654,687–12,775,488 (120.8 kb) |
| Fgf4 | Chr11: 69,360,727–69,363,101 (2375 bp) | Chr7: 144,415,123–144,418,982 (3859 bp) | Chr4: 12,805,564–12,818,136 (12.57 kb) |
| Fgf5 | Chr4: 81,646,219–81,666,886 (20,668 bp) | Chr5: 98,402,043–98,424,892 (22,849 bp) | Chr1: 95,522,903–95,569,520 (46.62 kb) |
| Fgf6 | Chr12: 4,413,569–4,425,041 (11,473 bp) | Chr6: 126,992,505–127,001,681 (9176 bp) | Chr3: 11,179,405–11,197,664 (18.26 kb) |
| Fgf7 | Chr15: 47,431,515–47,495,579 (64,065 bp) | Chr2: 125,876,578–125,933,105 (56,527 bp) | Chr3: 104,281,252–104,316,082 (34.83 kb) |
| Fgf8 | Chr10: 103,194,668–103,200,244 (5577 bp) | Chr19: 45,724,930–45,742,941 (18,011 bp) | Chr7: 31,012,191–31,022,187 (10 kb) |
| Fgf9 | Chr13: 20,043,875–20,074,184 (30,310 bp) | Chr14: 58,308,131–58,350,311 (42,180 bp) | Chr2: 157,463,721–157,503,485 (39.77 kb) |
| Fgf10 | Chr5: 44,350,598–44,434,285 (83,688 bp) | Chr13: 118,851,235–118,929,109 (77,874 bp) | Chr1: 194,526,912–194,599,107 (72.2 kb) |
| Fgf11 | Chr17: 7,543,254–7,548,814 (5561 bp) | Chr11: 69,686,894–69,693,775 (6881 bp) | Scaffold_2560: 505–2966 |
| Fgf12 | Chr3: 193,182,711–193,446,925 (264,215 bp) | Chr16: 27,976,535–28,571,995 (595,460 bp) | Chr5: 105,036,268–105,258,133 (221.87 kb) |
| Fgf13 | ChrX: 136,419,343–136,499,434 (80,092 bp) | ChrX: 58,107,499–58,630,932 (523,433 bp) | Chr8: 69,689,404–69,876,346 (186.94 kb) |
| Fgf14 | Chr13: 100,073,036–100,752,125 (679,090 bp) | Chr14: 124,211,853–124,915,098 (703,245 bp) | Chr2: 119,766,570–120,110,357 (343.79 kb) |
| Fgf15 | Missing | Chr7: 1,444,502,269–1,444,454,690 (47,579 bp) | Missing |
| Fgf16 | ChrX: 77,447,389–77,457,278 (9889 bp) | ChrX: 104,808,083–104,820,138 (12,055 bp) | Chr8: 45,583,466–45,609,547 (26.08 kb) |
| Fgf17 | Chr8: 21,922,365–21,928,256 (5892 bp) | Chr 17: 70,873,643–70,880,064 (6421 bp) | Missing |
| Fgf18 | Chr5: 170,827,589–170,865,098 (37,510 bp) | Chr 11: 33,066,970–33,097,400 (30,430 bp) | Missing |
| Fgf19 | Chr11: 69,285,937–69,292,036 (6100 bp) | Missing | Chr4: 12,861,360–12,867,681 (6.32 kb) |
| Fgf20 | Chr8: 16,860,698–16,870,038 (9341 bp) | Chr 8: 40,732,207–40,739,994 (7787 bp) | Chr1: 42,116,142–42,120,691 (4.55 kb) |
| Fgf21 | Chr19: 53,951,306–53,953,289 (1984 bp) | Chr 7: 45,263,314–45,264,914 (1600 bp) | Missing |
| Fgf22 | Chr19: 590,926–594,604 (3679 bp) | Chr 10: 79,590,887–79,593,629 (2742 bp) | Chr1: 105,764,076–105,794,176 (30.1 kb) |
| Fgf23 | Chr12: 4,347,654–4,359,141 (11,488 bp) | Chr6: 127,049,865–127,059,259 (9394 bp) | Chr3: 11,271,103–11,276,872 (5.77 kb) |
| FGFs | Human (aa) | Mus musculus (aa) | Xenopus tropicalis (aa) |
|---|---|---|---|
| FGF1 | 155 | 155 | 155 |
| FGF2 | 155 | 154 | 154 |
| FGF3 | 239 | 245 | 236 |
| FGF4 | 206 | 202 | 192 |
| FGF5 | 268 | 264 | 251 |
| FGF6 | 208 | 208 | 195 |
| FGF7 | 194 | 194 | 194 |
| FGF8 | 233 | 244 | 211 |
| FGF9 | 208 | 208 | 208 |
| FGF10 | 208 | 209 | 196 |
| FGF11 | 225 | 225 | 133 |
| FGF12 | 243 | 243 | 243 |
| FGF13 | 245 | 245 | 255 |
| FGF14 | 247 | 247 | 252 |
| FGF15 | NA | 218 | NA |
| FGF16 | 207 | 207 | 202 |
| FGF17 | 216 | 216 | NA |
| FGF18 | 207 | 207 | NA |
| FGF19 | 216 | NA | 215 |
| FGF20 | 211 | 211 | 208 |
| FGF21 | 209 | 210 | NA |
| FGF22 | 170 | 162 | 175 |
| FGF23 | 251 | 251 | 254 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goutam, R.S.; Kumar, V.; Lee, U.; Kim, J. Exploring the Structural and Functional Diversity among FGF Signals: A Comparative Study of Human, Mouse, and Xenopus FGF Ligands in Embryonic Development and Cancer Pathogenesis. Int. J. Mol. Sci. 2023, 24, 7556. https://doi.org/10.3390/ijms24087556
Goutam RS, Kumar V, Lee U, Kim J. Exploring the Structural and Functional Diversity among FGF Signals: A Comparative Study of Human, Mouse, and Xenopus FGF Ligands in Embryonic Development and Cancer Pathogenesis. International Journal of Molecular Sciences. 2023; 24(8):7556. https://doi.org/10.3390/ijms24087556
Chicago/Turabian StyleGoutam, Ravi Shankar, Vijay Kumar, Unjoo Lee, and Jaebong Kim. 2023. "Exploring the Structural and Functional Diversity among FGF Signals: A Comparative Study of Human, Mouse, and Xenopus FGF Ligands in Embryonic Development and Cancer Pathogenesis" International Journal of Molecular Sciences 24, no. 8: 7556. https://doi.org/10.3390/ijms24087556
APA StyleGoutam, R. S., Kumar, V., Lee, U., & Kim, J. (2023). Exploring the Structural and Functional Diversity among FGF Signals: A Comparative Study of Human, Mouse, and Xenopus FGF Ligands in Embryonic Development and Cancer Pathogenesis. International Journal of Molecular Sciences, 24(8), 7556. https://doi.org/10.3390/ijms24087556







