High-Risk HPV CISH Detection in Cervical Biopsies with Weak and/or Focal p16 Immunohistochemical Positivity
Abstract
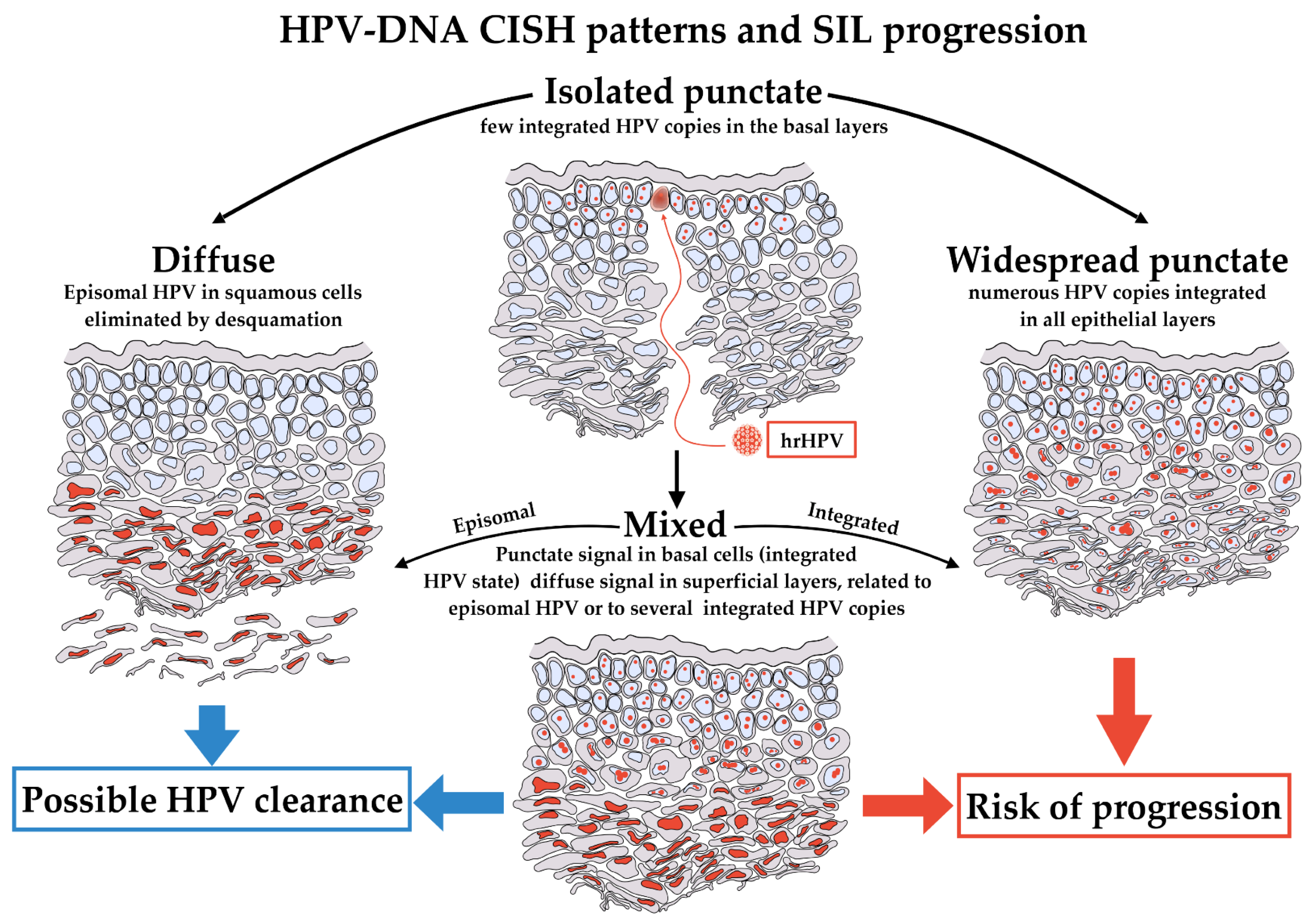
:1. Introduction
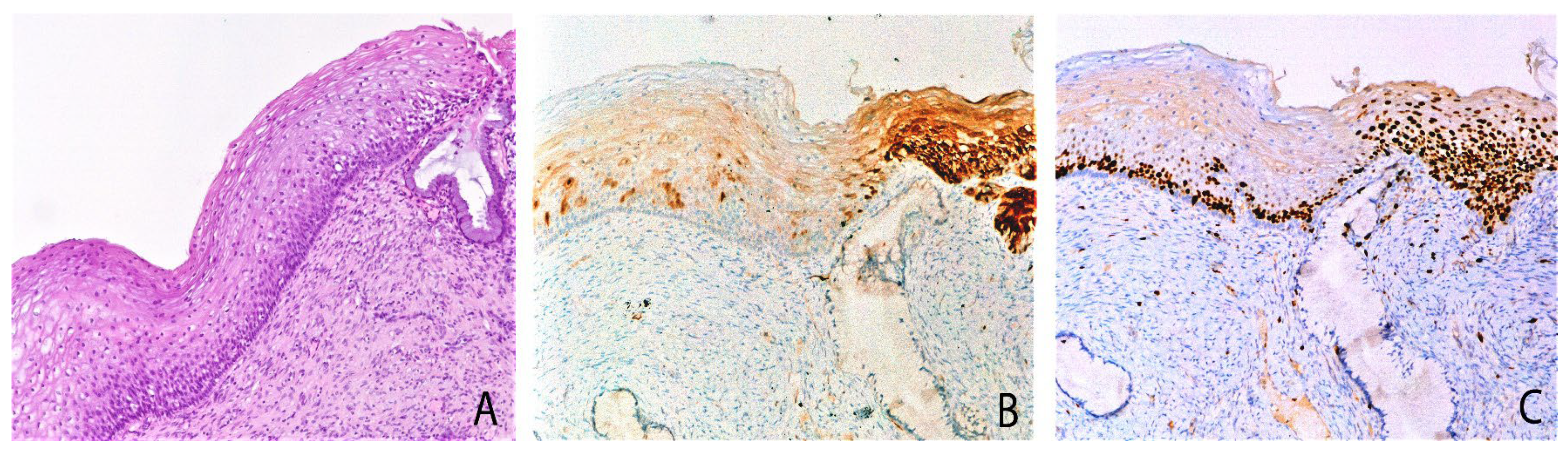
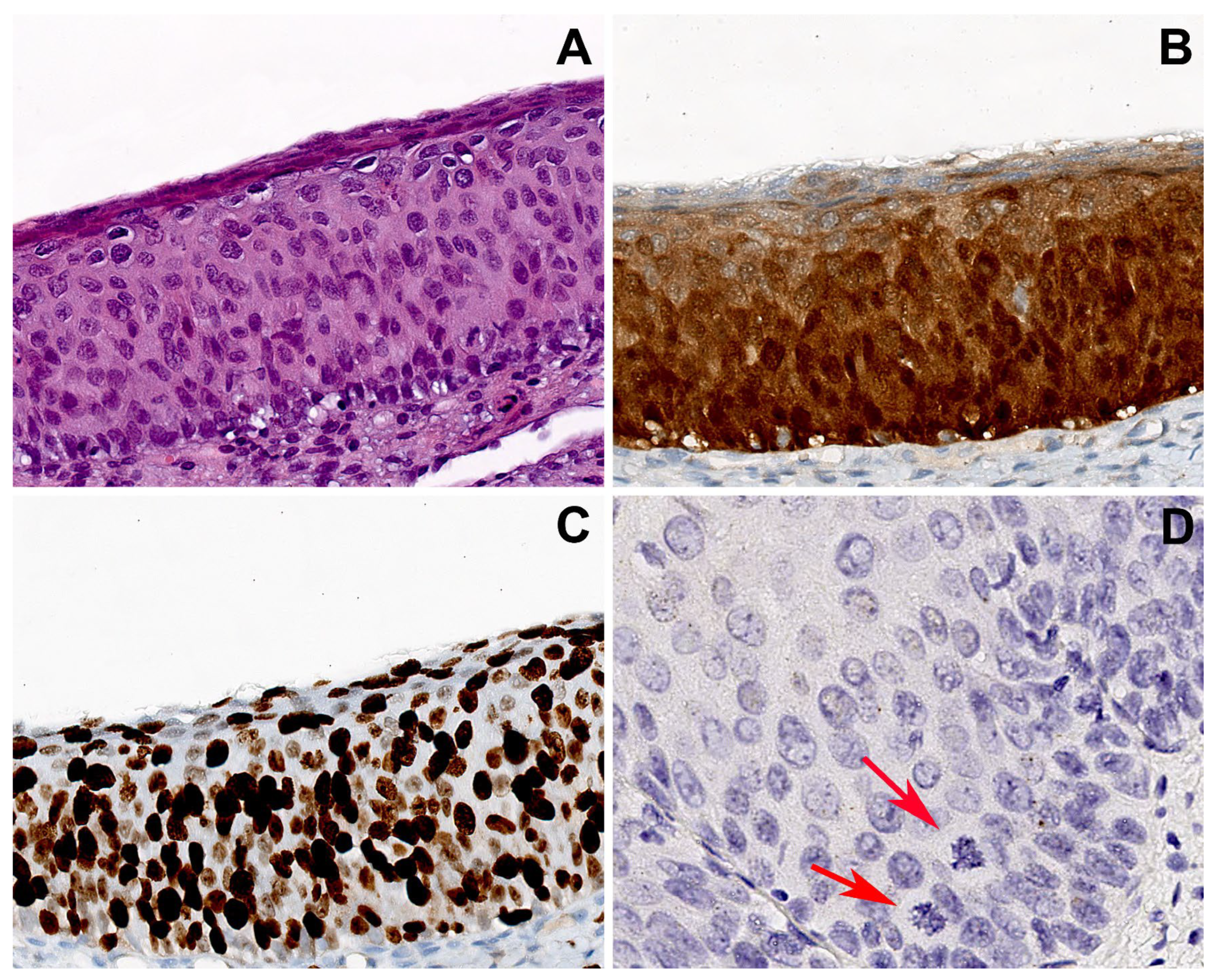
2. Results
- -
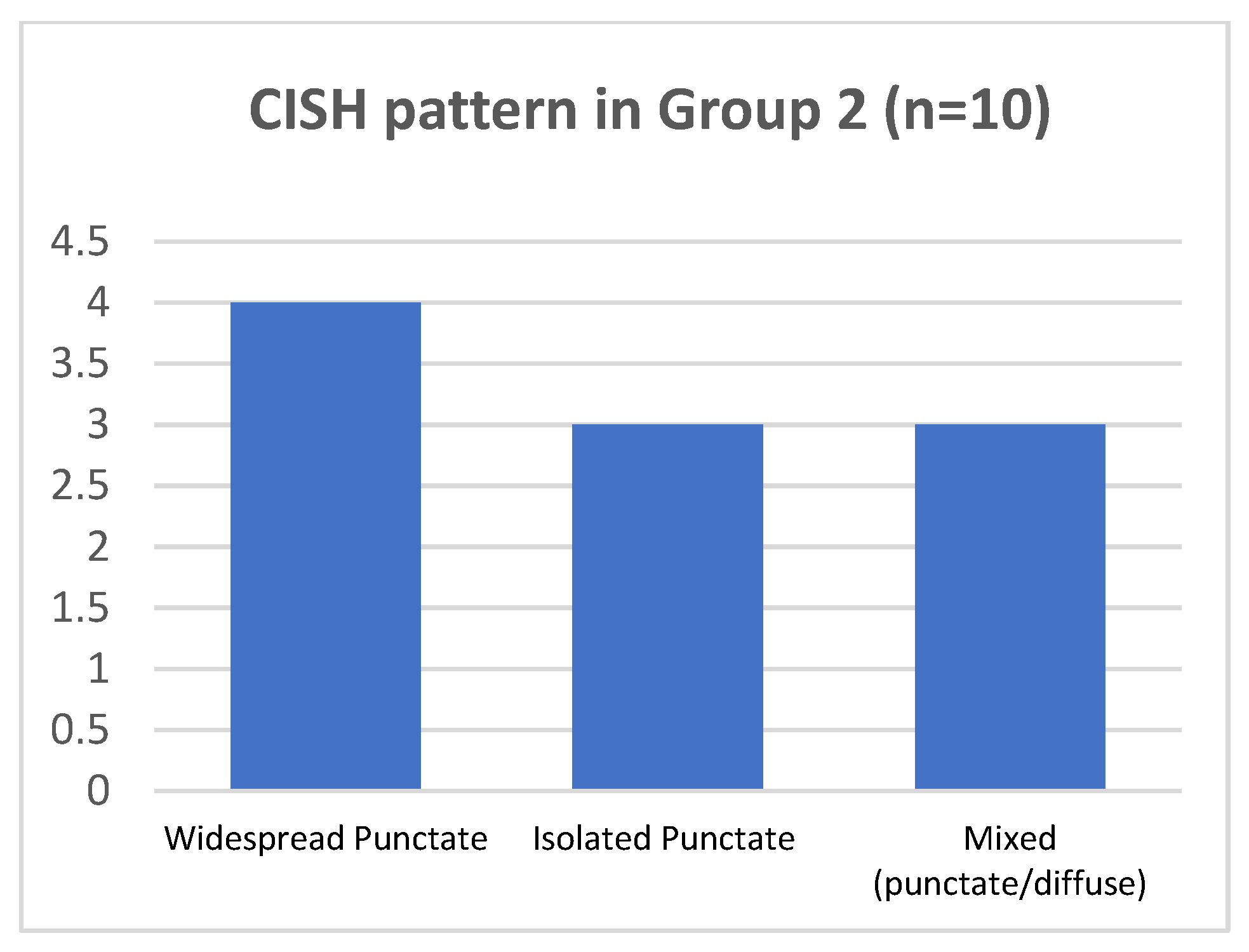
- In 4/20 cases harboring HPV 16 by DNA-test, the isolate punctate pattern was present in rare nuclei;
- -
- In 4/20 cases, harboring HPV 31, the widespread punctate CISH pattern was encountered;
- -
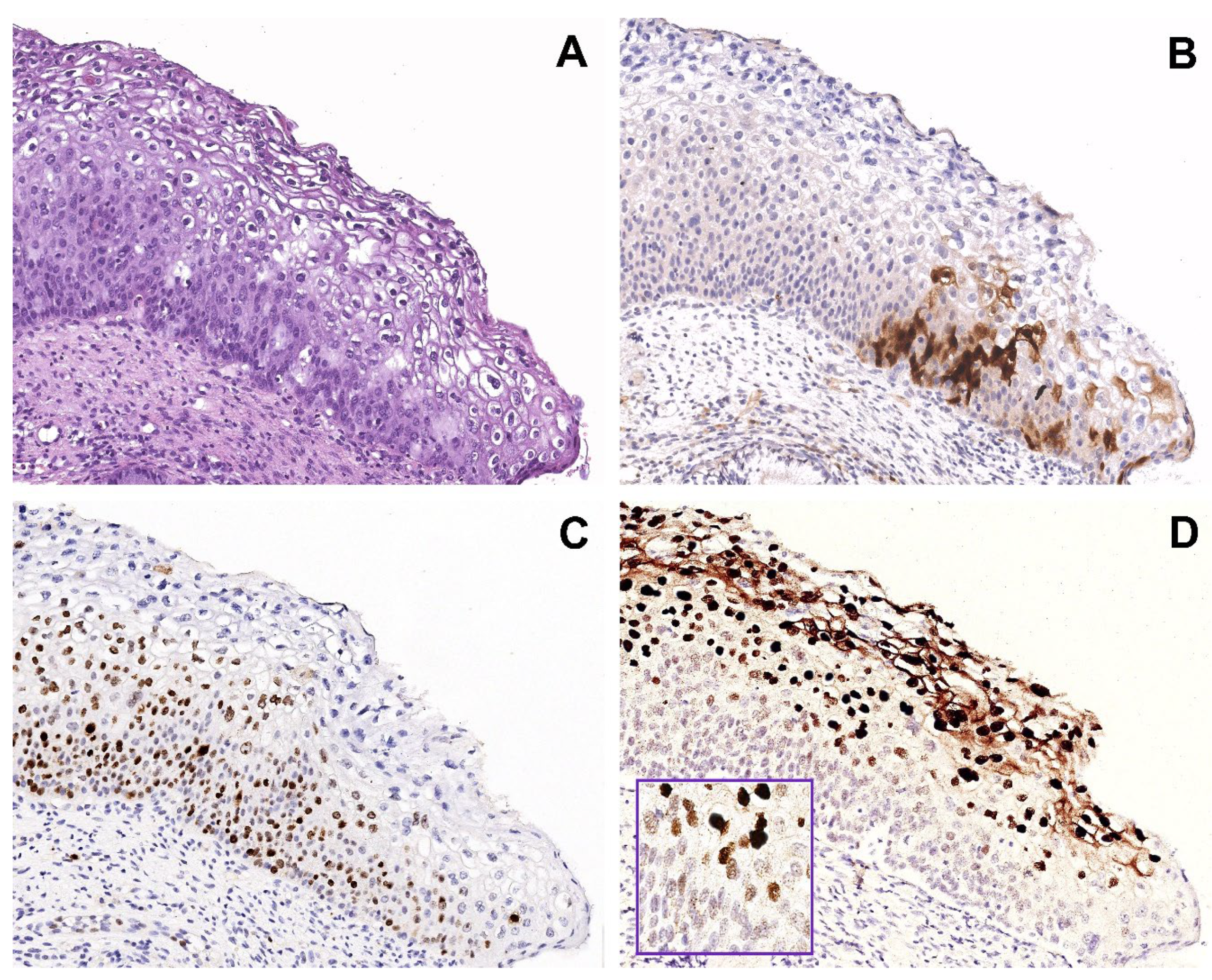
- In 4/20 cases (two with HPV31 and two with HPV51) a mixed CISH pattern was evidenced (Figure 1D).
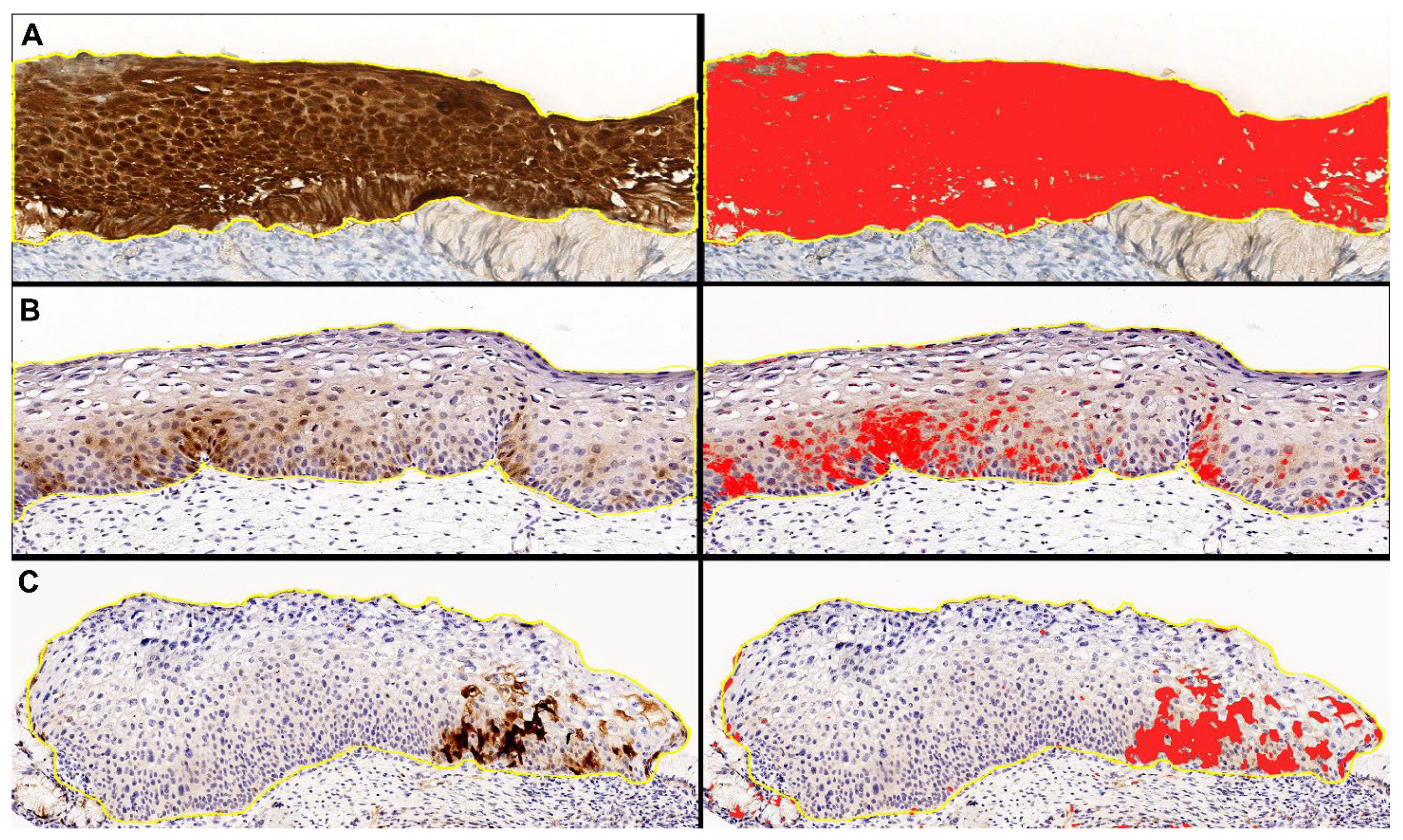
3. Discussion
4. Materials and Methods
4.1. Samples Collection
4.2. HPV Detection and Genotyping
4.3. Immunohistochemical Assay
4.4. Chromogenic DNA In Situ Hybridization (DNA-CISH) Assay
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Graham, S.V. The human papillomavirus replication cycle, and its links to cancer progression: A comprehensive review. Clin. Sci. 2017, 131, 2201–2221. [Google Scholar] [CrossRef] [PubMed]
- Scurry, J.; Wilkinson, E.J. Review of terminology of precursors of vulvar squamous cell carcinoma. J. Low. Genit. Tract Dis. 2006, 10, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Partridge, J.M.; Hughes, J.P.; Feng, Q.; Winer, R.L.; Weaver, B.A.; Xi, L.F.; Stern, M.E.; Lee, S.; O’reilly, S.F.; Hawes, S.E.; et al. Genital human papillomavirus infection in men: Incidence and risk factors in a cohort of university students. J. Infect. Dis. 2007, 196, 1128–1136. [Google Scholar] [CrossRef]
- Hartwig, S.; Syrjänen, S.; Dominiak-Felden, G.; Brotons, M.; Castellsagué, X. Estimation of the epidemiological burden of human papillomavirus-related cancers and non-malignant diseases in men in Europe: A review. BMC Cancer 2012, 12, 30. [Google Scholar] [CrossRef] [PubMed]
- Bzhalava, D.; Eklund, C.; Dillner, J. International standardization and classification of human papillomavirus types. Virology 2015, 476, 341–344. [Google Scholar] [CrossRef]
- Pyeon, D.; Pearce, S.M.; Lank, S.M.; Ahlquist, P.; Lambert, P.F. Establishment of human papillomavirus infection requires cell cycle progression. PLoS Pathog. 2009, 5, e1000318. [Google Scholar] [CrossRef]
- Kadaja, M.; Silla, T.; Ustav, E.; Ustav, M. Papillomavirus DNA replication—From initiation to genomic instability. Virology 2009, 384, 360–368. [Google Scholar] [CrossRef]
- Mpunga, T.; Chantal Umulisa, M.; Tenet, V.; Rugwizangoga, B.; Milner, D.A., Jr.; Munyanshongore, C.; Heideman, D.A.; Bleeker, M.C.; Tommasino, M.; Franceschi, S.; et al. Human papillomavirus genotypes in cervical and other HPV-related anogenital cancer in Rwanda, according to HIV status. Int. J. Cancer 2020, 146, 1514–1522. [Google Scholar] [CrossRef]
- Hebner, C.M.; Laimins, L.A. Human papillomaviruses: Basic mechanisms of pathogenesis and oncogenicity. Rev. Med. Virol. 2006, 16, 83–97. [Google Scholar] [CrossRef]
- Mantovani, F.; Banks, L. The human papillomavirus E6 protein and its contribution to malignant progression. Oncogene 2001, 20, 7874–7887. [Google Scholar] [CrossRef]
- Mabruk, M. The mystery of human papillomaviruses in carcinogenesis. Expert Rev. Mol. Diagn. 2008, 8, 1–4. [Google Scholar] [CrossRef] [PubMed]
- da Mata, S.; Ferreira, J.; Nicolás, I.; Esteves, S.; Esteves, G.; Lérias, S.; Silva, F.; Saco, A.; Cochicho, D.; Cunha, M.; et al. P16 and HPV Genotype Significance in HPV-Associated Cervical Cancer-A Large Cohort of Two Tertiary Referral Centers. Int. J. Mol. Sci. 2021, 22, 2294. [Google Scholar] [CrossRef] [PubMed]
- Darragh, T.M.; Colgan, T.J.; Thomas Cox, J.; Heller, D.S.; Henry, M.R.; Luff, R.D.; McCalmont, T.; Nayar, R.; Palefsky, J.M.; Stoler, M.H.; et al. The Lower Anogenital Squamous Terminology Standardization project for HPV-associated lesions: Background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Int. J. Gynecol. Pathol. 2013, 32, 76–115. [Google Scholar] [CrossRef] [PubMed]
- Skapa, P.; Robova, H.; Rob, L.; Zamecnik, J. p16(INK4a) immunoprofiles of squamous lesions of the uterine cervix-implications for the reclassification of atypical immature squamous metaplasia. Pathol. Oncol. Res. 2013, 19, 707–714. [Google Scholar] [CrossRef]
- Yu, L.; Fei, L.; Liu, X.; Pi, X.; Wang, L.; Chen, S. Application of p16/Ki-67 dual-staining cytology in cervical cancers. J. Cancer 2019, 10, 2654–2660. [Google Scholar] [CrossRef]
- Cabibi, D.; Napolitano, C.; Giannone, A.G.; Micciulla, M.C.; Porcasi, R.; Lo Coco, R.; Bosco, L.; Vinciguerra, M.; Capra, G. Predictive Role of the p16 Immunostaining Pattern in Atypical Cervical Biopsies with Less Common High Risk HPV Genotypes. Diagnostics 2021, 11, 1947. [Google Scholar] [CrossRef]
- Kelesidis, T.; Aish, L.; Steller, M.A.; Aish, I.S.; Shen, J.; Foukas, P.; Panayiotides, J.; Petrikkos, G.; Karakitsos, P.; Tsiodras, S. Human papillomavirus (HPV) detection using in situ hybridization in histologic samples: Correlations with cytologic changes and polymerase chain reaction HPV detection. Am. J. Clin. Pathol. 2011, 136, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.F.; Matthews, A.; Kandil, D.; Adamson, C.S.; Trotman, W.E.; Cooper, K. Discrimination of ‘driver’ and ‘passenger’ HPV in tonsillar carcinomas by the polymerase chain reaction, chromogenic in situ hybridization, and p16(INK4a) immunohistochemistry. Head Neck Pathol. 2011, 5, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Kalof, A.N.; Evans, M.F.; Simmons-Arnold, L.; Beatty, B.G.; Cooper, K. p16INK4A immunoexpression and HPV in situ hybridization signal patterns: Potential markers of high-grade cervical intraepithelial neoplasia. Am. J. Surg. Pathol. 2005, 29, 674–679. [Google Scholar] [CrossRef]
- Klaes, R.; Friedrich, T.; Spitkovsky, D.; Ridder, R.; Rudy, W.; Petry, U.; Dallenbach-Hellweg, G.; Schmidt, D.; von Knebel Doeberitz, M. Overexpression of p16(INK4A) as a specific marker for dysplastic and neoplastic epithelial cells of the cervix uteri. Int. J. Cancer 2001, 92, 276–284. [Google Scholar] [CrossRef]
- Tsoumpou, I.; Arbyn, M.; Kyrgiou, M.; Wentzensen, N.; Koliopoulos, G.; Martin-Hirsch, P.; Malamou-Mitsi, V.; Paraskevaidis, E. p16(INK4a) immunostaining in cytological and histological specimens from the uterine cervix: A systematic review and meta-analysis. Cancer Treat. Rev. 2009, 35, 210–220. [Google Scholar] [CrossRef]
- Liu, Y.; Alqatari, M.; Sultan, K.; Ye, F.; Gao, D.; Sigel, K.; Zhang, D.; Kalir, T. Using p16 immunohistochemistry to classify morphologic cervical intraepithelial neoplasia 2: Correlation of ambiguous staining patterns with HPV subtypes and clinical outcome. Hum. Pathol. 2017, 66, 144–151. [Google Scholar] [CrossRef]
- Cabibi, D.; Giovannelli, L.; Martorana, A.; Migliore, M.C.; Tripodo, C.; Campione, M.; Ammatuna, P.; Aragona, F. Predictive role of histological features and Ki67 pattern on high-risk HPV presence in atypical cervical lesions. Histopathology 2007, 51, 713–716. [Google Scholar] [CrossRef]
- Boyer, S.N.; Wazer, D.E.; Band, V. E7 protein of human papilloma virus-16 induces degradation of retinoblastoma protein through the ubiquitin-proteasome pathway. Cancer Res. 1996, 56, 4620–4624. [Google Scholar]
- Giarrè, M.; Caldeira, S.; Malanchi, I.; Ciccolini, F.; Leão, M.J.; Tommasino, M. Induction of pRb degradation by the human papillomavirus type 16 E7 protein is essential to efficiently overcome p16INK4a-imposed G1 cell cycle Arrest. J. Virol. 2001, 75, 4705–4712. [Google Scholar] [CrossRef]
- Fatima, N.; Cohen, C.; Lawson, D.; Siddiqui, M.T. Automated and manual human papilloma virus in situ hybridization and p16 immunohistochemistry: Comparison in metastatic oropharyngeal carcinoma. Acta Cytol. 2013, 57, 633–640. [Google Scholar] [CrossRef]
- Chi, J.; Preeshagul, I.R.; Sheikh-Fayyaz, S.; Teckie, S.; Kohn, N.; Ziemba, Y.; Laser, A.; Frank, D.; Ghaly, M.; Kamdar, D.; et al. Evaluating of HPV-DNA ISH as an adjunct to p16 testing in oropharyngeal cancer. Future Sci. OA 2020, 6, Fso606. [Google Scholar] [CrossRef]
- Zito Marino, F.; Ronchi, A.; Stilo, M.; Cozzolino, I.; La Mantia, E.; Colacurci, N.; Colella, G.; Franco, R. Multiplex HPV RNA in situ hybridization/p16 immunohistochemistry: A novel approach to detect papillomavirus in HPV-related cancers. A novel multiplex ISH/IHC assay to detect HPV. Infect. Agent. Cancer 2020, 15, 46. [Google Scholar] [CrossRef]
- Mango, L.J. Computer-assisted cervical cancer screening using neural networks. Cancer Lett. 1994, 77, 155–162. [Google Scholar] [CrossRef]
- Tan, S.L.; Selvachandran, G.; Ding, W.; Paramesran, R.; Kotecha, K. Cervical Cancer Classification From Pap Smear Images Using Deep Convolutional Neural Network Models. Interdiscip Sci 2024, 16, 16–38. [Google Scholar] [CrossRef]
- Sompawong, N.; Mopan, J.; Pooprasert, P.; Himakhun, W.; Suwannarurk, K.; Ngamvirojcharoen, J.; Vachiramon, T.; Tantibundhit, C. Automated Pap Smear Cervical Cancer Screening Using Deep Learning. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; Volume 2019, pp. 7044–7048. [Google Scholar] [CrossRef]
- Ferreira, D.A.; Idris, A.; McMillan, N.A.J. Analysis of a hit-and-run tumor model by HPV in oropharyngeal cancers. J. Med. Virol. 2023, 95, e28260. [Google Scholar] [CrossRef]
- Cooper, K.; Evans, M.; Mount, S. Biology and evolution of cervical squamous intraepithelial lesions: A hypothesis with diagnostic prognostic implications. Adv. Anat. Pathol. 2003, 10, 200–203. [Google Scholar] [CrossRef]
- Zappacosta, R.; Colasante, A.; Viola, P.; D’Antuono, T.; Lattanzio, G.; Capanna, S.; Gatta, D.M.P.; Rosini, S. Chromogenic in situ hybridization and p16/Ki67 dual staining on formalin-fixed paraffin-embedded cervical specimens: Correlation with HPV-DNA test, E6/E7 mRNA test, and potential clinical applications. Biomed. Res. Int. 2013, 2013, 453606. [Google Scholar] [CrossRef]
- Xiong, J.; Cheng, J.; Shen, H.; Ren, C.; Wang, L.; Gao, C.; Zhu, T.; Li, X.; Ding, W.; Zhu, D.; et al. Detection of HPV and Human Chromosome Sites by Dual-Color Fluorescence In Situ Hybridization Reveals Recurrent HPV Integration Sites and Heterogeneity in Cervical Cancer. Front. Oncol. 2021, 11, 734758. [Google Scholar] [CrossRef]
- Pett, M.; Coleman, N. Integration of high-risk human papillomavirus: A key event in cervical carcinogenesis? J. Pathol. 2007, 212, 356–367. [Google Scholar] [CrossRef]
- Omori, M.; Hashi, A.; Nakazawa, K.; Yuminamochi, T.; Yamane, T.; Hirata, S.; Katoh, R.; Hoshi, K. Estimation of prognoses for cervical intraepithelial neoplasia 2 by p16INK4a immunoexpression and high-risk HPV in situ hybridization signal types. Am. J. Clin. Pathol. 2007, 128, 208–217. [Google Scholar] [CrossRef]
- Nuño, T.; García, F. The Lower Anogenital Squamous Terminology Project and its implications for clinical care. Obstet. Gynecol. Clin. N. Am. 2013, 40, 225–233. [Google Scholar] [CrossRef]
- Giovannelli, L.; Lama, A.; Capra, G.; Giordano, V.; Aricò, P.; Ammatuna, P. Detection of human papillomavirus DNA in cervical samples: Analysis of the new PGMY-PCR compared to the hybrid capture II and MY-PCR assays and a two-step nested PCR assay. J. Clin. Microbiol. 2004, 42, 3861–3864. [Google Scholar] [CrossRef]
- Safaeian, M.; Herrero, R.; Hildesheim, A.; Quint, W.; Freer, E.; Van Doorn, L.J.; Porras, C.; Silva, S.; González, P.; Bratti, M.C.; et al. Comparison of the SPF10-LiPA system to the Hybrid Capture 2 Assay for detection of carcinogenic human papillomavirus genotypes among 5,683 young women in Guanacaste, Costa Rica. J. Clin. Microbiol. 2007, 45, 1447–1454. [Google Scholar] [CrossRef]
- Bankhead, P.; Loughrey, M.B.; Fernández, J.A.; Dombrowski, Y.; McArt, D.G.; Dunne, P.D.; McQuaid, S.; Gray, R.T.; Murray, L.J.; Coleman, H.G.; et al. QuPath: Open source software for digital pathology image analysis. Sci. Rep. 2017, 7, 16878. [Google Scholar] [CrossRef]

| # | Age | Pap Test Result | Colposcopy | HISTOLOGY | Ki67 | p16 | HPV-DNA LiPa Test | hrHPV CISH Pattern |
|---|---|---|---|---|---|---|---|---|
| 1 | 26 | ASCUS | ANTZ1 | Metaplasia and Koilocytosis | 1+ | 1+ | 31 | Widespread Punctate |
| 2 | 53 | ASCUS | ANTZ1 | Metaplasia and Koilocytosis | 1+ | 1+ | 16 | Negative |
| 3 | 37 | LSIL | ANTZ1 | H-SIL | 3+ | 1+ | 51 | Negative |
| 4 | 44 | ASCUS | ANTZ1 | H-SIL | 3+ | 1+/3+ | 31 | Mixed (punctate/diffuse) |
| 5 | 31 | ASCUS | ANTZ2 | Metaplasia and Koilocytosis | 1+ | 1+ | 31 | Widespread Punctate |
| 6 | 44 | ASCUS | ANTZ1 | L-SIL | 1+ | 1+ | 16 | Negative |
| 7 | 64 | NILM | ANTZ1 | L-SIL | 2+ | 1+ | 16 | Isolated Punctate |
| 8 | 34 | NILM | ANTZ1 | L-SIL | 1+ | 1+/3+ | 31 | Widespread Punctate |
| 9 | 74 | ASCUS | ANTZ1 | L-SIL | 1+ | 1+ | 16 | Negative |
| 10 | 33 | ASCUS | ANTZ1 | L-SIL | 1+ | 1+ | 16 | Isolated Punctate |
| 11 | 42 | ASCUS | ANTZ1 | H-SIL | 3+ | 1+ | 51 | Mixed (punctate/diffuse) |
| 12 | 58 | ASCUS | ANTZ2 | Metaplasia and Koilocytosis | 1+ | 1+ | 16 | Negative |
| 13 | 61 | ASCH | ANTZ1 | H-SIL | 3+ | 1+ | 51 | Negative |
| 14 | 38 | ASCUS | ANTZ1 | H-SIL | 3+ | 1+/3+ | 31 | Mixed (punctate/diffuse) |
| 15 | 37 | LSIL | ANTZ1 | H-SIL | 3+ | 1+ | 51 | Mixed (punctate/diffuse) |
| 16 | 33 | NILM | ANTZ1 | L-SIL | 1+ | 1+/3+ | 31 | Widespread Punctate |
| 17 | 50 | LSIL | ANTZ1 | L-SIL | 1+ | 1+ | 16 | Negative |
| 18 | 36 | ASCUS | ANTZ1 | L-SIL | 1+ | 1+ | 16 | Negative |
| 19 | 65 | ASCUS | ANTZ1 | L-SIL | 2+ | 1+ | 16 | Isolated Punctate |
| 20 | 45 | ASCUS | ANTZ2 | L-SIL | 1+ | 1+ | 16 | Isolated Punctate |
| # | Age | Pap Test | Colposcopy | HISTOLOGY | Ki67 | p16 | HPV-DNA LiPa Test | hrHPV CISH Pattern |
|---|---|---|---|---|---|---|---|---|
| 1 | 55 | ASCUS | ANTZ1 | H-SIL | 3+ | 3+ | 31–33–51 | Widespread Punctate |
| 2 | 63 | ASCUS | ANTZ1 | H-SIL/SCC | 3+ | 3+ | 16 | Widespread Punctate |
| 3 | 40 | ASCUS | ANTZ2 | H-SIL | 3+ | 3+ | 16 | Mixed (punctate/diffuse) |
| 4 | 38 | HSIL | ANTZ2 | H-SIL | 3+ | 3+ | 16 | Isolated Punctate |
| 5 | 33 | HSIL | NVTZ | H-SIL | 3+ | 3+ | 16 | Isolated Punctate |
| 6 | 42 | ASCUS | ANTZ1 | H-SIL | 2+ | 3+ | 16–18–31–51 | Mixed (punctate/diffuse) |
| 7 | 48 | LSIL | ANTZ2 | H-SIL | 3+ | 3+ | 31–33 | Widespread Punctate |
| 8 | 76 | ASCH | ANTZ2 | H-SIL | 3+ | 3+ | 16 | Widespread Punctate |
| 9 | 32 | HSIL | ANTZ2 | H-SIL | 3+ | 3+ | 16 | Mixed (punctate/diffuse) |
| 10 | 30 | ASCUS | ANTZ1 | H-SIL | 3+ | 3+ | 16 | Isolated Punctate |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabibi, D.; Giannone, A.G.; Quattrocchi, A.; Lo Coco, R.; Formisano, E.; Porcasi, R.; Benfante, V.; Comelli, A.; Capra, G. High-Risk HPV CISH Detection in Cervical Biopsies with Weak and/or Focal p16 Immunohistochemical Positivity. Int. J. Mol. Sci. 2024, 25, 5354. https://doi.org/10.3390/ijms25105354
Cabibi D, Giannone AG, Quattrocchi A, Lo Coco R, Formisano E, Porcasi R, Benfante V, Comelli A, Capra G. High-Risk HPV CISH Detection in Cervical Biopsies with Weak and/or Focal p16 Immunohistochemical Positivity. International Journal of Molecular Sciences. 2024; 25(10):5354. https://doi.org/10.3390/ijms25105354
Chicago/Turabian StyleCabibi, Daniela, Antonino Giulio Giannone, Alberto Quattrocchi, Roberta Lo Coco, Eleonora Formisano, Rossana Porcasi, Viviana Benfante, Albert Comelli, and Giuseppina Capra. 2024. "High-Risk HPV CISH Detection in Cervical Biopsies with Weak and/or Focal p16 Immunohistochemical Positivity" International Journal of Molecular Sciences 25, no. 10: 5354. https://doi.org/10.3390/ijms25105354
APA StyleCabibi, D., Giannone, A. G., Quattrocchi, A., Lo Coco, R., Formisano, E., Porcasi, R., Benfante, V., Comelli, A., & Capra, G. (2024). High-Risk HPV CISH Detection in Cervical Biopsies with Weak and/or Focal p16 Immunohistochemical Positivity. International Journal of Molecular Sciences, 25(10), 5354. https://doi.org/10.3390/ijms25105354








