FLT3-TKD Measurable Residual Disease Detection Using Droplet Digital PCR and Clinical Applications in Acute Myeloid Leukemia
Abstract
:1. Introduction
2. Results
2.1. Accuracy
2.2. Limit of Detection (LoD)
2.3. Limit of Blank (LoB)
2.4. Linearity
2.5. Precision
2.6. Robustness
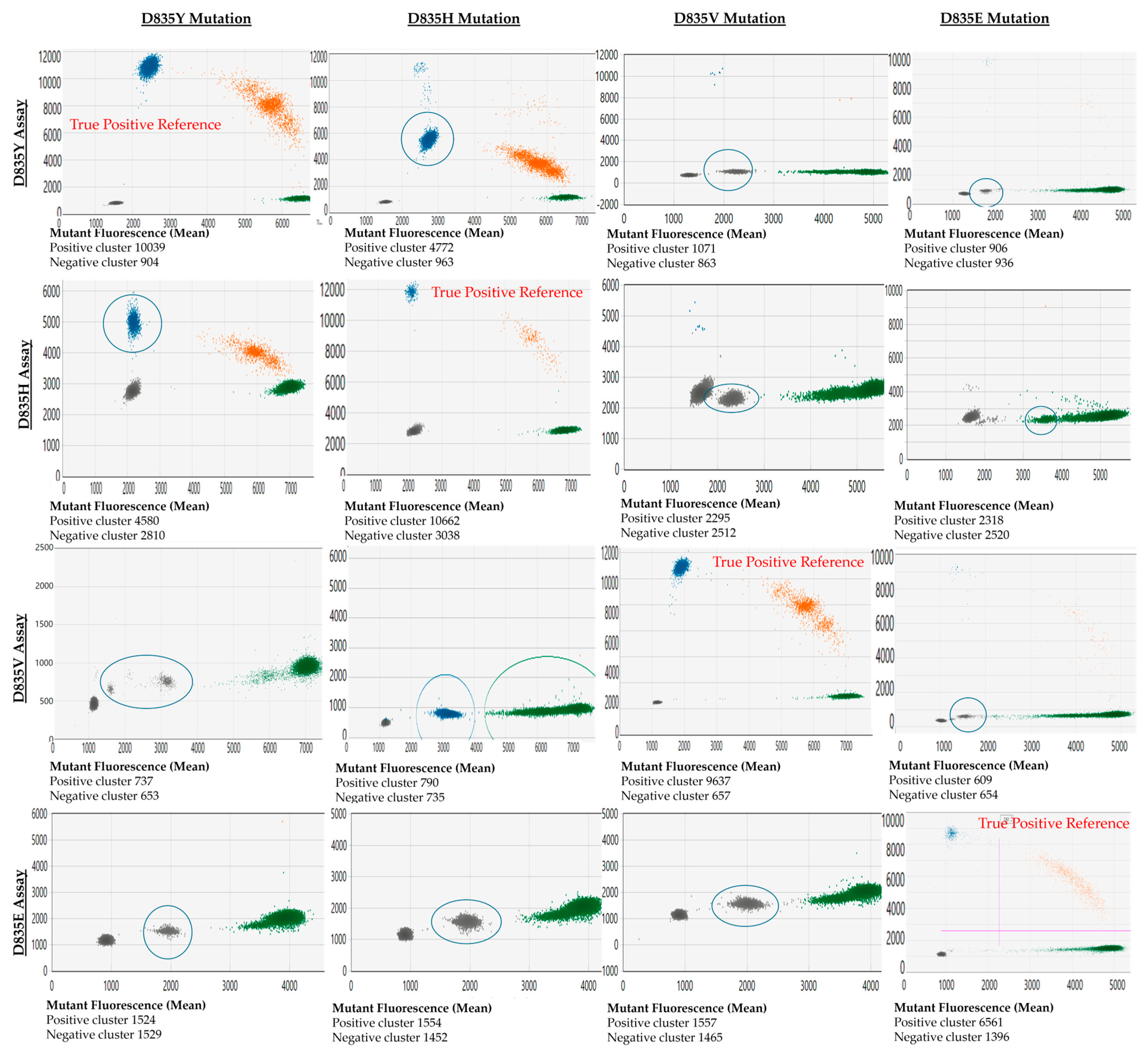
2.7. Assay Cross-Reactivity
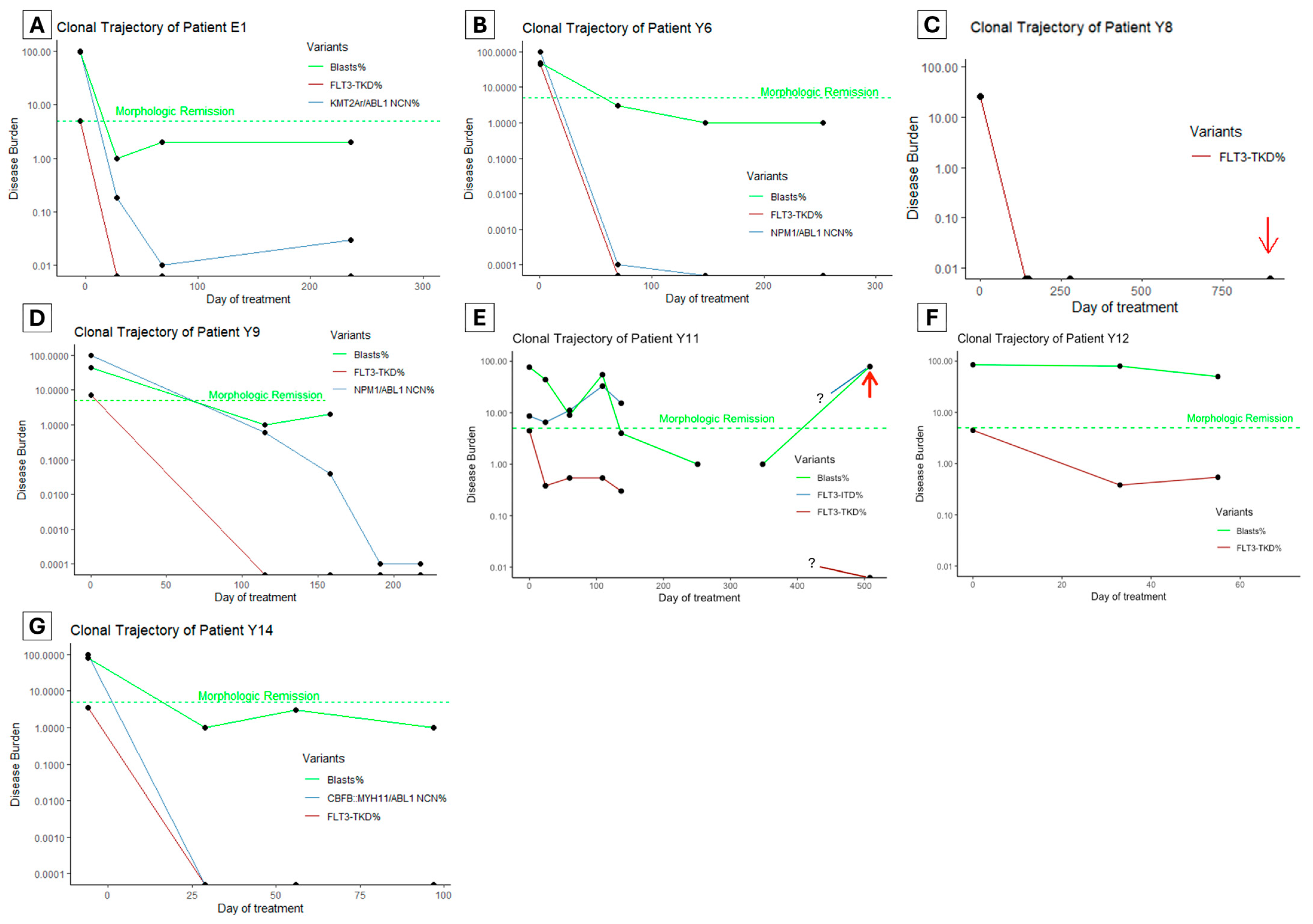
2.8. Clinical Utility
3. Discussion
4. Materials and Methods
4.1. Sample Preparation
4.2. ddPCR Method
4.3. Performance Assessment and Statistics
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- DiNardo, C.D.; Erba, H.P.; Freeman, S.D.; Wei, A.H. Acute myeloid leukaemia. Lancet 2023, 401, 2073–2086. [Google Scholar] [CrossRef]
- Döhner, H.; Wei, A.H.; Appelbaum, F.R.; Craddock, C.; DiNardo, C.D.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Godley, L.A.; Hasserjian, R.P.; et al. Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood 2022, 140, 1345–1377. [Google Scholar] [CrossRef]
- Patnaik, M.M. The importance of FLT3 mutational analysis in acute myeloid leukemia. Leuk. Lymphoma 2018, 59, 2273–2286. [Google Scholar] [CrossRef] [PubMed]
- Staudt, D.; Murray, H.C.; McLachlan, T.; Alvaro, F.; Enjeti, A.K.; Verrills, N.M.; Dun, M.D. Targeting Oncogenic Signaling in Mutant FLT3 Acute Myeloid Leukemia: The Path to Least Resistance. Int. J. Mol. Sci. 2018, 19, 3198. [Google Scholar] [CrossRef]
- Li, S.; Li, N.; Chen, Y.; Zheng, Z.; Guo, Y. FLT3-TKD in the prognosis of patients with acute myeloid leukemia: A meta-analysis. Front. Oncol. 2023, 13, 1086846. [Google Scholar] [CrossRef] [PubMed]
- Stone, R.M.; Mandrekar, S.J.; Sanford, B.L.; Laumann, K.; Geyer, S.; Bloomfield, C.D.; Thiede, C.; Prior, T.W.; Döhner, K.; Marcucci, G.; et al. Midostaurin plus Chemotherapy for Acute Myeloid Leukemia with a FLT3 Mutation. N. Engl. J. Med. 2017, 377, 454–464. [Google Scholar] [CrossRef] [PubMed]
- Perl, A.E.; Martinelli, G.; Cortes, J.E.; Neubauer, A.; Berman, E.; Paolini, S.; Montesinos, P.; Baer, M.R.; Larson, R.A.; Ustun, C.; et al. Gilteritinib or Chemotherapy for Relapsed or Refractory FLT3-Mutated AML. N. Engl. J. Med. 2019, 381, 1728–1740. [Google Scholar] [CrossRef]
- Heuser, M.; Freeman, S.D.; Ossenkoppele, G.J.; Buccisano, F.; Hourigan, C.S.; Ngai, L.L.; Tettero, J.M.; Bachas, C.; Baer, C.; Béné, M.-C.; et al. 2021 Update on MRD in acute myeloid leukemia: A consensus document from the European LeukemiaNet MRD Working Party. Blood 2021, 138, 2753–2767. [Google Scholar] [CrossRef]
- Murphy, K.M.; Levis, M.; Hafez, M.J.; Geiger, T.; Cooper, L.C.; Smith, B.D.; Small, D.; Berg, K.D. Detection of FLT3 internal tandem duplication and D835 mutations by a multiplex polymerase chain reaction and capillary electrophoresis assay. J. Mol. Diagn. 2003, 5, 96–102. [Google Scholar] [CrossRef]
- Bergeron, J.; Capo-Chichi, J.M.; Tsui, H.; Mahe, E.; Berardi, P.; Minden, M.D.; Brandwein, J.M.; Schuh, A.C. The Clinical Utility of FLT3 Mutation Testing in Acute Leukemia: A Canadian Consensus. Curr. Oncol. 2023, 30, 10410–10436. [Google Scholar] [CrossRef]
- Rare Mutation Detection Best Practice Guidelines. June 2022. Available online: https://www.bio-rad.com/webroot/web/pdf/lsr/literature/Bulletin_6628.pdf (accessed on 26 March 2024).
- Tiong, I.S.; Loo, S. Targeting Measurable Residual Disease (MRD) in Acute Myeloid Leukemia (AML): Moving beyond Prognostication. Int. J. Mol. Sci. 2023, 24, 4790. [Google Scholar] [CrossRef] [PubMed]
- Kottaridis, P.D.; Gale, R.E.; Langabeer, S.E.; Frew, M.E.; Bowen, D.T.; Linch, D.C. Studies of FLT3 mutations in paired presentation and relapse samples from patients with acute myeloid leukemia: Implications for the role of FLT3 mutations in leukemogenesis, minimal residual disease detection, and possible therapy with FLT3 inhibitors. Blood 2002, 100, 2393–2398. [Google Scholar] [CrossRef] [PubMed]
- Dillon, L.W.; Gui, G.; Page, K.M.; Ravindra, N.; Wong, Z.C.; Andrew, G.; Mukherjee, D.; Zeger, S.L.; El Chaer, F.; Spellman, S.; et al. DNA Sequencing to Detect Residual Disease in Adults with Acute Myeloid Leukemia Prior to Hematopoietic Cell Transplant. JAMA 2023, 329, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Hegde, P.S.; Andrew, G.; Gui, G.; Ravindra, N.; Mukherjee, D.; Wong, Z.; Auletta, J.J.; El Chaer, F.; Corner, A.; Devine, S.M.; et al. Persistence of FLT3-TKD in Blood Prior to Allogeneic Transplant Is Associated with Increased Relapse and Death in Adults with AML in First Remission. Blood 2023, 142 (Suppl. S1), 2941. [Google Scholar] [CrossRef]
- Blätte, T.J.; Schmalbrock, L.K.; Skambraks, S.; Lux, S.; Cocciardi, S.; Dolnik, A.; Döhner, H.; Döhner, K.; Bullinger, L. getITD for FLT3-ITD-based MRD monitoring in AML. Leukemia 2019, 33, 2535–2539. [Google Scholar] [CrossRef] [PubMed]
- Loo, S.; Dillon, R.; Ivey, A.; Anstee, N.S.; Othman, J.; Tiong, I.S.; Potter, N.; Jovanovic, J.; Runglall, M.; Chong, C.C.; et al. Pretransplant FLT3-ITD MRD assessed by high-sensitivity PCR-NGS determines posttransplant clinical outcome. Blood 2022, 140, 2407–2411. [Google Scholar] [CrossRef] [PubMed]
- Sirajuddin, P.; Gregory, A.; Kushal, S.; Day, G.-J. Streamlining the Detection of FLT3 Internal Tandem Duplication (FLT3-ITD) Using the Cepheid Genexpert® Automated System. Blood 2023, 142 (Suppl. S1), 6036. [Google Scholar] [CrossRef]
- Kushal, S.; Calayag, K.; Das, S.; Saatian, B.; Xie, G.; Bates, M.; Day, G.-J. Development of a Fast and Quantitative FLT3-TKD Mutation Prototype Using Lab in a Cartridge™ Technology. Blood 2023, 142, 2290. [Google Scholar] [CrossRef]
- Ge, S.S.; Qiu, Q.C.; Dai, H.P.; Shen, X.D.; Wu, T.M.; Du, J.H.; Wan, C.L.; Shen, H.J.; Wu, D.P.; Xue, S.L.; et al. Mutation spectrum of FLT3 and significance of non-canonical FLT3 mutations in haematological malignancy. Br. J. Haematol. 2023, 202, 539–549. [Google Scholar] [CrossRef]
- Othman, J.; Potter, N.; Mokretar, K.; Taussig, D.; Khan, A.; Krishnamurthy, P.; Latif, A.L.; Cahalin, P.; Aries, J.; Amer, M.; et al. FLT3 inhibitors as MRD-guided salvage treatment for molecular failure in FLT3 mutated AML. Leukemia 2023, 37, 2066–2072. [Google Scholar] [CrossRef]
- Wei, A.H.; Iland, H.J.; Reynolds, J.; Loo, S.; Chua, C.C.; Westerman, D.; Tiong, I.S.; Ivey, A.; Blombery, P.; Anstee, N.S.; et al. ALLG AMLM26 Phase 1B/2 Study Investigating Novel Therapies to Target Early Relapse and Clonal Evolution As Pre-Emptive Therapy in AML (INTERCEPT): A Multi-Arm, Precision-Based, Recursive, Platform Trial. Blood 2022, 140 (Suppl. S1), 3341–3343. [Google Scholar] [CrossRef]

| Sample Code | HRM | Sanger Sequencing | ddPCR Allelic Frequency | NGS VAF or AR by CE | Concordance |
|---|---|---|---|---|---|
| E1 | Detected | Not detected | 4.97% | 4.8% | Yes |
| H1 | Detected | Not detected | 3.77% | 5.7% * | Yes |
| H2 | Detected | D835H | 41.70% | n/p | Yes |
| H3 | Detected | D835H | 24.75% | 25.4% * | Yes |
| H4 | Detected | D835H | 6.77% | 6% | Yes |
| H5 | Detected | D835H | 25.30% | n/p | Yes |
| V1 | Detected | D835V | 20.10% | n/p | Yes |
| V2 | Detected | D835V | 26.90% | n/p | Yes |
| V3 | Detected | D835V | 42.30% | n/p | Yes |
| V4 | Detected | Not detected | 6.29% | n/p | Yes |
| Y1 | Detected | Not detected | 5.96% | 5% | Yes |
| Y2 | Detected | D835Y | 10% | 10% | Yes |
| Y3 | Detected | D835Y | 21.30% | n/p | Yes |
| Y4 | Detected | D835Y | 45.60% | 42% | Yes |
| Y5 | Detected | D835Y | 18.20% | 13% | Yes |
| Y6 | Detected | D835Y | 25.54% | 42% | Yes |
| Y7 | Detected | D835Y | 6.98% | 7% | Yes |
| Y8 | Detected | D835Y | 38.30% | n/a | Yes |
| Y9 | Not detected | Not detected | 1% | 1% | Yes |
| Y10 | Detected | D835Y | 4.42% | 4% | Yes |
| Y11 | Detected | D835Y | 26.58% | 25.20% | Yes |
| Y12 | Detected | D835Y | 3.59% | n/p | Yes |
| WT1 | Not detected | n/p | 0.00% | n/p | Yes |
| WT2 | Not detected | n/p | 0.00% | n/p | Yes |
| WT3 | Not detected | n/p | 0.00% | n/p | Yes |
| WT4 | Not detected | n/p | 0.00% | n/p | Yes |
| WT5 | Not detected | n/p | 0.00% | n/p | Yes |
| WT6 | Not detected | n/p | 0.00% | n/p | Yes |
| Allelic Frequency | D835Y | D835V | D835H | D835E | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Replicates | Triplicate Combinations * | Positive Combinations (%) | Replicates | Triplicate Combinations * | Positive Combinations (%) | Replicates | Triplicate Combinations * | Positive Combinations (%) | Replicates | Triplicate Combinations * | Positive Combinations (%) | |
| 1% | 2 | NA | NA | 2 | NA | NA | 4 | 4 | 4 (100%) | 4 | 4 | 4 (100%) |
| 0.1% | 7 | 35 | 35 (100%) | 4 | 4 | 4 (100%) | 4 | 4 | 4 (100%) | 4 | 4 | 4 (100%) |
| 0.01% | 16 | 560 | 560 (100%) | 12 | 220 | 215 (97.5%) | 10 | 120 | 120 (100%) | 12 | 220 | 220 (100%) |
| 0.005% | 4 | 4 | 4 (100%) | NA | NA | NA | 4 | 4 | 2 (50%) | 4 | 4 | 4 (100%) |
| Allelic Frequency | D835Y | D835V | D835H | D835E | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD (n) | CV% | Mean ± SD (n) | CV% | Mean ± SD (n) | CV% | Mean ± SD (n) | CV% | |
| 1% | 0.99 ± 0.65 (7) | 6.6 | 0.82 ± 0.009 (2) | 1.1 | 1.46 ± 0.063 (4) | 4.3 | 2.23 ± 0.142 (4) | 6.4 |
| 0.1% | 0.13 ± 0.029 (7) | 21.6 | 0.09 ± 0.026 (4) | 27.7 | 0.14 ± 0.013 (4) | 9.4 | 0.29 ± 0.041 (4) | 13.9 |
| 0.01% | 0.02 ± 0.008 (16) | 41.1 | 0.02 ± 0.008 (12) | 54.2 | 0.018 ± 0.002 (10) | 12.6 | 0.029 ± 0.011 (16) | 38.9 |
| D835 Variant | Replicates | Mean Allelic Frequency | SD | CV% |
|---|---|---|---|---|
| D835Y | 4 | 25.53 | 0.26 | 1% |
| D835V | 3 | 42.43 | 0.26 | 0.6% |
| D835H | 2 | 25.16 | 0.14 | 0.6% |
| D835E | 2 | 4.93 | 0.03 | 0.7% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, E.W.; Tran, N.Y.K.; McCulloch, D.; Krigstein, M.; Catalano, A.; Othman, J.; Abadir, E.; Smith, C.; Iland, H. FLT3-TKD Measurable Residual Disease Detection Using Droplet Digital PCR and Clinical Applications in Acute Myeloid Leukemia. Int. J. Mol. Sci. 2024, 25, 5771. https://doi.org/10.3390/ijms25115771
Li EW, Tran NYK, McCulloch D, Krigstein M, Catalano A, Othman J, Abadir E, Smith C, Iland H. FLT3-TKD Measurable Residual Disease Detection Using Droplet Digital PCR and Clinical Applications in Acute Myeloid Leukemia. International Journal of Molecular Sciences. 2024; 25(11):5771. https://doi.org/10.3390/ijms25115771
Chicago/Turabian StyleLi, Eric Wenlong, Ngoc Yen Kim Tran, Derek McCulloch, Michael Krigstein, Alberto Catalano, Jad Othman, Edward Abadir, Cheryl Smith, and Harry Iland. 2024. "FLT3-TKD Measurable Residual Disease Detection Using Droplet Digital PCR and Clinical Applications in Acute Myeloid Leukemia" International Journal of Molecular Sciences 25, no. 11: 5771. https://doi.org/10.3390/ijms25115771
APA StyleLi, E. W., Tran, N. Y. K., McCulloch, D., Krigstein, M., Catalano, A., Othman, J., Abadir, E., Smith, C., & Iland, H. (2024). FLT3-TKD Measurable Residual Disease Detection Using Droplet Digital PCR and Clinical Applications in Acute Myeloid Leukemia. International Journal of Molecular Sciences, 25(11), 5771. https://doi.org/10.3390/ijms25115771






