Hormone Regulation in Testicular Development and Function
Abstract
:1. Introduction
2. Testis Physiology
2.1. Testicular Structure
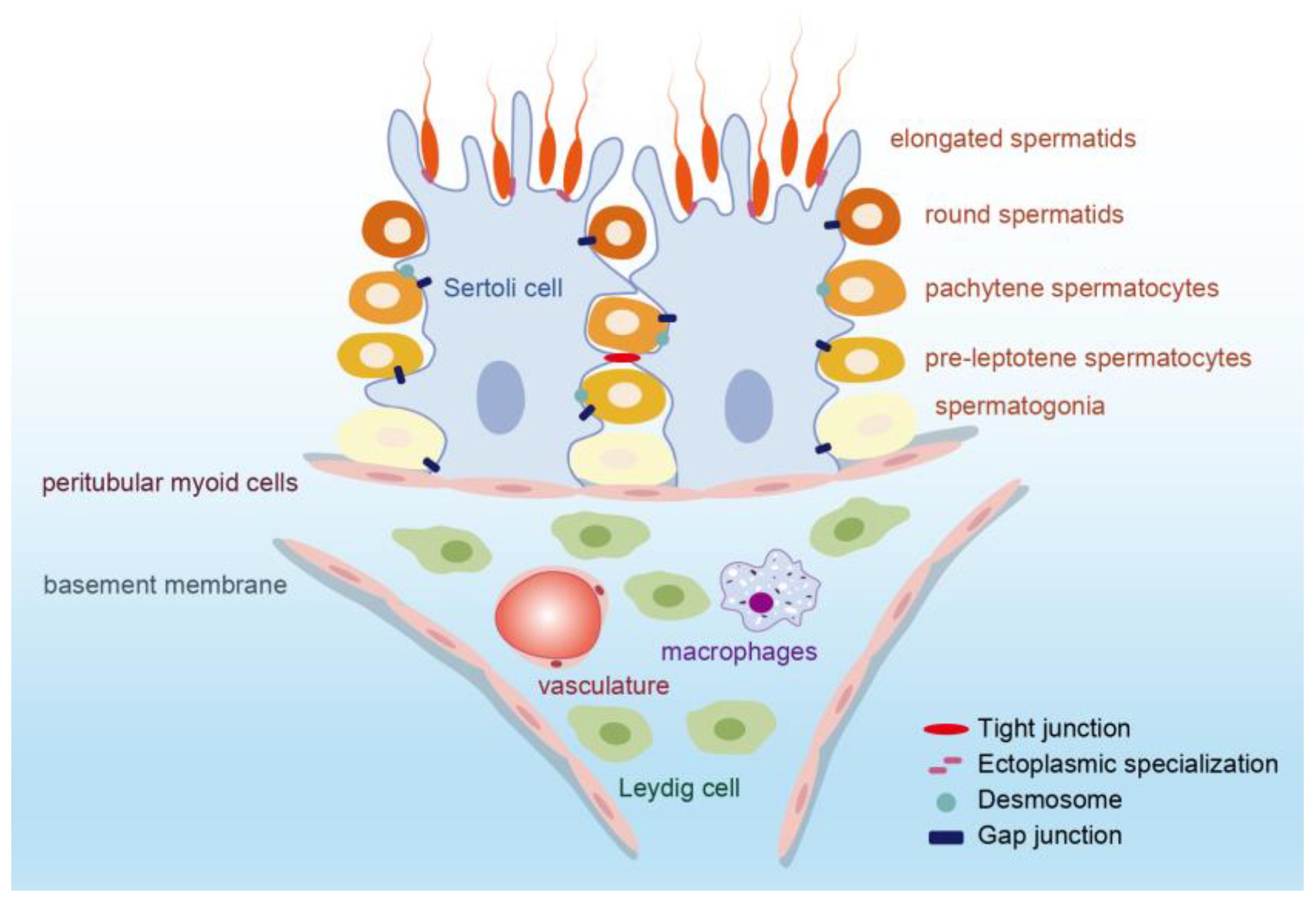
2.1.1. Seminiferous Tubule
2.1.2. Interstitial Tissue
2.1.3. Blood–Testis Barrier (BTB)
2.2. Testicular Function
2.2.1. Spermatogenesis
2.2.2. Testosterone Production
3. Hormone Regulation in Testicular Development and Function
3.1. Testosterone
3.2. FSH
3.3. Inhibin B
3.4. Activin A
3.5. Anti-Müllerian Hormone (AMH)
3.6. Insulin-like Factor 3 (INSL3)
3.7. Estrogen
3.8. Prolactin (PRL)
3.9. Oxytocin (OT)
4. The HPG Axis in Hormonal Regulation
4.1. HPG Axis in Fetal Life
4.2. HPG Axis in Minipuberty
4.3. HPG Axis in Puberty
4.4. HPG Axis in Adulthood
5. Hormone Disorders and Male Hormonal Contraceptive
5.1. Hypogonadism
5.2. Male Hormonal Contraceptive
5.3. Research and Future Perspective
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Levine, H.; Jørgensen, N.; Martino-Andrade, A.; Mendiola, J.; Weksler-Derri, D.; Jolles, M.; Pinotti, R.; Swan, S.H. Temporal trends in sperm count: A systematic review and meta-regression analysis of samples collected globally in the 20th and 21st centuries. Hum. Reprod. Update 2023, 29, 157–176. [Google Scholar] [CrossRef] [PubMed]
- Levine, H.; Jørgensen, N.; Martino-Andrade, A.; Mendiola, J.; Weksler-Derri, D.; Mindlis, I.; Pinotti, R.; Swan, S.H. Temporal trends in sperm count: A systematic review and meta-regression analysis. Hum. Reprod. Update 2017, 23, 646–659. [Google Scholar] [CrossRef] [PubMed]
- Shah, W.; Khan, R.; Shah, B.; Khan, A.; Dil, S.; Liu, W.; Wen, J.; Jiang, X. The Molecular Mechanism of Sex Hormones on Sertoli Cell Development and Proliferation. Front. Endocrinol. 2021, 12, 648141. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, M.-C.; McBeath, E. Sertoli Cell-Germ Cell Interactions Within the Niche: Paracrine and Juxtacrine Molecular Communications. Front. Endocrinol. 2022, 13, 897062. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Yan, M.; Ge, R.; Cheng, C.Y. Crosstalk between Sertoli and Germ Cells in Male Fertility. Trends Mol. Med. 2020, 26, 215–231. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-Y.; Willis, W.D.; Eddy, E.M. Targeting the Gdnf Gene in peritubular myoid cells disrupts undifferentiated spermatogonial cell development. Proc. Natl. Acad. Sci. USA 2016, 113, 1829–1834. [Google Scholar] [CrossRef]
- Wang, M.; Yang, Y.; Cansever, D.; Wang, Y.; Kantores, C.; Messiaen, S.; Moison, D.; Livera, G.; Chakarov, S.; Weinberger, T.; et al. Two populations of self-maintaining monocyte-independent macrophages exist in adult epididymis and testis. Proc. Natl. Acad. Sci. USA 2021, 118, e2013686117. [Google Scholar] [CrossRef]
- DeFalco, T.; Potter, S.J.; Williams, A.V.; Waller, B.; Kan, M.J.; Capel, B. Macrophages Contribute to the Spermatogonial Niche in the Adult Testis. Cell Rep. 2015, 12, 1107–1119. [Google Scholar] [CrossRef] [PubMed]
- Lokka, E.; Lintukorpi, L.; Cisneros-Montalvo, S.; Makela, J.A.; Tyystjarvi, S.; Ojasalo, V.; Gerke, H.; Toppari, J.; Rantakari, P.; Salmi, M. Generation, localization and functions of macrophages during the development of testis. Nat. Commun. 2020, 11, 4375. [Google Scholar] [CrossRef]
- Fijak, M.; Meinhardt, A. The testis in immune privilege. Immunol. Rev. 2006, 213, 66–81. [Google Scholar] [CrossRef]
- Mruk, D.D.; Cheng, C.Y. The Mammalian Blood-Testis Barrier: Its Biology and Regulation. Endocr. Rev. 2015, 36, 564–591. [Google Scholar] [CrossRef] [PubMed]
- Stanton, P.G. Regulation of the blood-testis barrier. Semin. Cell Dev. Biol. 2016, 59, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.; Sriram, A.; Wayne Vogl, A. Internalization of Intact Intercellular Junctions in the Testis by Clathrin/Actin-Mediated Endocytic Structures: Tubulobulbar Complexes. Anat. Rec. 2018, 301, 2080–2085. [Google Scholar] [CrossRef] [PubMed]
- Mao, B.; Bu, T.; Mruk, D.; Li, C.; Sun, F.; Cheng, C.Y. Modulating the Blood-Testis Barrier Towards Increasing Drug Delivery. Trends Pharmacol. Sci. 2020, 41, 690–700. [Google Scholar] [CrossRef] [PubMed]
- Akama, T.O.; Nakagawa, H.; Sugihara, K.; Narisawa, S.; Ohyama, C.; Nishimura, S.-I.; O‘Brien, D.A.; Moremen, K.W.; Millan, J.L.; Fukuda, M.N. Germ cell survival through carbohydrate-mediated interaction with Sertoli cells. Science 2002, 295, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Xu, J.; Zhao, Z.; Gong, L.; Su, Y.; Fang, Z.; Chen, P.; Liu, Y.; Zhang, L.; Xu, F. Triphenyl phosphate induced apoptosis of mice testicular Leydig cells and TM3 cells through ROS-mediated mitochondrial fusion inhibition. Ecotoxicol. Environ. Saf. 2023, 256, 114876. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Li, X.; Li, L.; Chen, H.; Ge, R.-S. Insights into the Development of the Adult Leydig Cell Lineage from Stem Leydig Cells. Front.. Physiol. 2017, 8, 430. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.C.; Lei, Z.; Rao, C.V.; Beck, J.; Lamb, D.J. De novo testosterone production in luteinizing hormone receptor knockout mice after transplantation of leydig stem cells. Endocrinology 2004, 145, 4011–4015. [Google Scholar] [CrossRef] [PubMed]
- Ge, R.-S.; Dong, Q.; Sottas, C.M.; Papadopoulos, V.; Zirkin, B.R.; Hardy, M.P. In search of rat stem Leydig cells: Identification, isolation, and lineage-specific development. Proc. Natl. Acad. Sci. USA 2006, 103, 2719–2724. [Google Scholar] [CrossRef]
- Young, J.; Xu, C.; Papadakis, G.E.; Acierno, J.S.; Maione, L.; Hietamäki, J.; Raivio, T.; Pitteloud, N. Clinical Management of Congenital Hypogonadotropic Hypogonadism. Endocr. Rev. 2019, 40, 669–710. [Google Scholar] [CrossRef]
- Rey, R.A. Recent advancement in the treatment of boys and adolescents with hypogonadism. Ther. Adv. Endocrinol. Metab. 2022, 13, 20420188211065660. [Google Scholar] [CrossRef] [PubMed]
- Lundgaard Riis, M.; Matilionyte, G.; Nielsen, J.E.; Melau, C.; Greenald, D.; Juul Hare, K.; Langhoff Thuesen, L.; Dreisler, E.; Aaboe, K.; Brenøe, P.T.; et al. Identification of a window of androgen sensitivity for somatic cell function in human fetal testis cultured ex vivo. BMC Med. 2022, 20, 399. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, A.B.; Aldhowayan, A.; Almuhanna, M.M.; Alghamdi, A.M. Persistent Mullerian duct syndrome, (PMDS): Case report and review of literature. Urol. Case Rep. 2022, 42, 102031. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Huang, J.; Gao, L.; Sang, Y.; Li, X.; Zhou, G.; Cao, L.; Lu, H.; Zhou, X.; Ren, L. Maternal exposure to PM2.5 disrupting offspring spermatogenesis through induced sertoli cells apoptosis via inhibin B hypermethylation in mice. Ecotoxicol. Environ. Saf. 2022, 241, 113760. [Google Scholar] [CrossRef] [PubMed]
- Bay, K.; Main, K.M.; Toppari, J.; Skakkebæk, N.E. Testicular descent: INSL3, testosterone, genes and the intrauterine milieu. Nat. Rev. Urol. 2011, 8, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Christin-Maitre, S.; Young, J. Androgens and spermatogenesis. Ann. Endocrinol. 2022, 83, 155–158. [Google Scholar] [CrossRef]
- Fix, C.; Jordan, C.; Cano, P.; Walker, W.H. Testosterone activates mitogen-activated protein kinase and the cAMP response element binding protein transcription factor in Sertoli cells. Proc. Natl. Acad. Sci. USA 2004, 101, 10919–10924. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Watkins, S.C.; Walker, W.H. Testosterone activates mitogen-activated protein kinase via Src kinase and the epidermal growth factor receptor in sertoli cells. Endocrinology 2007, 148, 2066–2074. [Google Scholar] [CrossRef]
- Shupe, J.; Cheng, J.; Puri, P.; Kostereva, N.; Walker, W.H. Regulation of Sertoli-germ cell adhesion and sperm release by FSH and nonclassical testosterone signaling. Mol. Endocrinol. 2011, 25, 238–252. [Google Scholar] [CrossRef]
- Itman, C.; Wong, C.; Hunyadi, B.; Ernst, M.; Jans, D.A.; Loveland, K.L. Smad3 dosage determines androgen responsiveness and sets the pace of postnatal testis development. Endocrinology 2011, 152, 2076–2089. [Google Scholar] [CrossRef]
- Edelsztein, N.Y.; Racine, C.; di Clemente, N.; Schteingart, H.F.; Rey, R.A. Androgens downregulate anti-Müllerian hormone promoter activity in the Sertoli cell through the androgen receptor and intact steroidogenic factor 1 sites. Biol. Reprod. 2018, 99, 1303–1312. [Google Scholar] [CrossRef]
- Lan, K.-C.; Chen, Y.-T.; Chang, C.; Chang, Y.-C.; Lin, H.-J.; Huang, K.-E.; Kang, H.-Y. Up-regulation of SOX9 in sertoli cells from testiculopathic patients accounts for increasing anti-mullerian hormone expression via impaired androgen receptor signaling. PLoS ONE 2013, 8, e76303. [Google Scholar] [CrossRef]
- De Gendt, K.; Denolet, E.; Willems, A.; Daniels, V.W.; Clinckemalie, L.; Denayer, S.; Wilkinson, M.F.; Claessens, F.; Swinnen, J.V.; Verhoeven, G. Expression of Tubb3, a beta-tubulin isotype, is regulated by androgens in mouse and rat Sertoli cells. Biol. Reprod. 2011, 85, 934–945. [Google Scholar] [CrossRef]
- Willems, A.; Batlouni, S.R.; Esnal, A.; Swinnen, J.V.; Saunders, P.T.K.; Sharpe, R.M.; França, L.R.; De Gendt, K.; Verhoeven, G. Selective ablation of the androgen receptor in mouse sertoli cells affects sertoli cell maturation, barrier formation and cytoskeletal development. PLoS ONE 2010, 5, e14168. [Google Scholar] [CrossRef] [PubMed]
- Legacki, E.; Conley, A.J.; Nitta-Oda, B.J.; Berger, T. Porcine sertoli cell proliferation after androgen receptor inactivation. Biol. Reprod. 2015, 92, 93. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Liu, D.; Liu, S.; Li, C.; Guo, J. Lycium barbarum Polysaccharide Ameliorates Heat-Stress-Induced Impairment of Primary Sertoli Cells and the Blood-Testis Barrier in Rat via Androgen Receptor and Akt Phosphorylation. Evid. Based Complement. Alternat Med. 2021, 2021, 5574202. [Google Scholar] [CrossRef]
- Wang, J.-M.; Li, Z.-F.; Yang, W.-X. What Does Androgen Receptor Signaling Pathway in Sertoli Cells During Normal Spermatogenesis Tell Us? Front. Endocrinol. 2022, 13, 838858. [Google Scholar] [CrossRef] [PubMed]
- Toocheck, C.; Clister, T.; Shupe, J.; Crum, C.; Ravindranathan, P.; Lee, T.-K.; Ahn, J.-M.; Raj, G.V.; Sukhwani, M.; Orwig, K.E.; et al. Mouse Spermatogenesis Requires Classical and Nonclassical Testosterone Signaling. Biol. Reprod. 2016, 94, 11. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.H.N.; Mruk, D.D.; Lee, W.M.; Cheng, C.Y. Blood-testis barrier dynamics are regulated by testosterone and cytokines via their differential effects on the kinetics of protein endocytosis and recycling in Sertoli cells. FASEB J. 2008, 22, 1945–1959. [Google Scholar] [CrossRef]
- Meng, J.; Holdcraft, R.W.; Shima, J.E.; Griswold, M.D.; Braun, R.E. Androgens regulate the permeability of the blood-testis barrier. Proc. Natl. Acad. Sci. USA 2005, 102, 16696–16700. [Google Scholar] [CrossRef]
- Chakraborty, P.; William Buaas, F.; Sharma, M.; Smith, B.E.; Greenlee, A.R.; Eacker, S.M.; Braun, R.E. Androgen-dependent sertoli cell tight junction remodeling is mediated by multiple tight junction components. Mol. Endocrinol. 2014, 28, 1055–1072. [Google Scholar] [CrossRef] [PubMed]
- Bulldan, A.; Dietze, R.; Shihan, M.; Scheiner-Bobis, G. Non-classical testosterone signaling mediated through ZIP9 stimulates claudin expression and tight junction formation in Sertoli cells. Cell Signal 2016, 28, 1075–1085. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, D.; Dietze, R.; Shihan, M.; Kirch, U.; Scheiner-Bobis, G. Dehydroepiandrosterone Sulfate Stimulates Expression of Blood-Testis-Barrier Proteins Claudin-3 and -5 and Tight Junction Formation via a Gnα11-Coupled Receptor in Sertoli Cells. PLoS ONE 2016, 11, e0150143. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.-S.; Yeh, S.; Chen, L.-M.; Lin, H.-Y.; Zhang, C.; Ni, J.; Wu, C.-C.; di Sant’Agnese, P.A.; deMesy-Bentley, K.L.; Tzeng, C.-R.; et al. Androgen receptor in sertoli cell is essential for germ cell nursery and junctional complex formation in mouse testes. Endocrinology 2006, 147, 5624–5633. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Shi, Y.-Q.; Yang, W.; Li, Y.-C.; Hu, Z.-Y.; Liu, Y.-X. Testosterone upregulation of tissue type plasminogen activator expression in Sertoli cells: tPA expression in Sertoli cells. Endocrine 2007, 32, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Gunnarsson, M.; Lecander, I.; Abrahamsson, P.A. Factors of the plasminogen activator system in human testis, as demonstrated by in-situ hybridization and immunohistochemistry. Mol. Hum. Reprod. 1999, 5, 934–940. [Google Scholar] [CrossRef]
- Li, X.-X.; Chen, S.-R.; Shen, B.; Yang, J.-L.; Ji, S.-Y.; Wen, Q.; Zheng, Q.-S.; Li, L.; Zhang, J.; Hu, Z.-Y.; et al. The Heat-Induced Reversible Change in the Blood-Testis Barrier, (BTB) Is Regulated by the Androgen Receptor, (AR) via the Partitioning-Defective Protein, (Par) Polarity Complex in the Mouse. Biol. Reprod. 2013, 89, 12. [Google Scholar] [CrossRef]
- Xia, Q.; Zhang, D.; Wang, J.; Zhang, X.; Song, W.; Chen, R.; Li, H.; Xie, W.; Zou, K. Androgen Indirectly Regulates Gap Junction Component Connexin 43 Through Wilms Tumor-1 in Sertoli Cells. Stem Cells Dev. 2020, 29, 169–176. [Google Scholar] [CrossRef]
- Tanaka, T.; Kanatsu-Shinohara, M.; Lei, Z.; Rao, C.V.; Shinohara, T. The Luteinizing Hormone-Testosterone Pathway Regulates Mouse Spermatogonial Stem Cell Self-Renewal by Suppressing WNT5A Expression in Sertoli Cells. Stem Cell Rep. 2016, 7, 279–291. [Google Scholar] [CrossRef]
- Wang, J.; Li, J.; Xu, W.; Xia, Q.; Gu, Y.; Song, W.; Zhang, X.; Yang, Y.; Wang, W.; Li, H.; et al. Androgen promotes differentiation of PLZF+ spermatogonia pool via indirect regulatory pattern. Cell Commun. Signal 2019, 17, 57. [Google Scholar] [CrossRef]
- Nóbrega, R.H.; Morais, R.D.V.d.S.; Crespo, D.; de Waal, P.P.; de França, L.R.; Schulz, R.W.; Bogerd, J. Fsh Stimulates Spermatogonial Proliferation and Differentiation in Zebrafish via Igf3. Endocrinology 2015, 156, 3804–3817. [Google Scholar] [CrossRef] [PubMed]
- Maiti, S.; Meistrich, M.L.; Wilson, G.; Shetty, G.; Marcelli, M.; McPhaul, M.J.; Morris, P.L.; Wilkinson, M.F. Irradiation selectively inhibits expression from the androgen-dependent Pem homeobox gene promoter in sertoli cells. Endocrinology 2001, 142, 1567–1577. [Google Scholar] [CrossRef] [PubMed]
- O‘Donnell, L.; McLachlan, R.I.; Wreford, N.G.; Robertson, D.M. Testosterone promotes the conversion of round spermatids between stages VII and VIII of the rat spermatogenic cycle. Endocrinology 1994, 135, 2608–2614. [Google Scholar] [CrossRef] [PubMed]
- O‘Donnell, L.; McLachlan, R.I.; Wreford, N.G.; de Kretser, D.M.; Robertson, D.M. Testosterone withdrawal promotes stage-specific detachment of round spermatids from the rat seminiferous epithelium. Biol. Reprod. 1996, 55, 895–901. [Google Scholar] [CrossRef]
- Chen, S.-R.; Hao, X.-X.; Zhang, Y.; Deng, S.-L.; Wang, Z.-P.; Wang, Y.-Q.; Wang, X.-X.; Liu, Y.-X. Androgen receptor in Sertoli cells regulates DNA double-strand break repair and chromosomal synapsis of spermatocytes partially through intercellular EGF-EGFR signaling. Oncotarget 2016, 7, 18722–18735. [Google Scholar] [CrossRef] [PubMed]
- Stanton, P.G.; Sluka, P.; Foo, C.F.H.; Stephens, A.N.; Smith, A.I.; McLachlan, R.I.; O‘Donnell, L. Proteomic changes in rat spermatogenesis in response to in vivo androgen manipulation; impact on meiotic cells. PLoS ONE 2012, 7, e41718. [Google Scholar] [CrossRef] [PubMed]
- Larose, H.; Kent, T.; Ma, Q.; Shami, A.N.; Harerimana, N.; Li, J.Z.; Hammoud, S.S.; Handel, M.A. Regulation of meiotic progression by Sertoli-cell androgen signaling. Mol. Biol. Cell 2020, 31, 2841–2862. [Google Scholar] [CrossRef] [PubMed]
- Câmara, M.L.; Almeida, T.B.; de Santi, F.; Rodrigues, B.M.; Cerri, P.S.; Beltrame, F.L.; Sasso-Cerri, E. Fluoxetine-induced androgenic failure impairs the seminiferous tubules integrity and increases ubiquitin carboxyl-terminal hydrolase L1, (UCHL1): Possible androgenic control of UCHL1 in germ cell death? Biomed. Pharmacother. 2019, 109, 1126–1139. [Google Scholar] [CrossRef] [PubMed]
- Panneerdoss, S.; Viswanadhapalli, S.; Abdelfattah, N.; Onyeagucha, B.C.; Timilsina, S.; Mohammad, T.A.; Chen, Y.; Drake, M.; Vuori, K.; Kumar, T.R.; et al. Cross-talk between miR-471-5p and autophagy component proteins regulates LC3-associated phagocytosis, (LAP) of apoptotic germ cells. Nat. Commun. 2017, 8, 598. [Google Scholar] [CrossRef]
- Hazra, R.; Corcoran, L.; Robson, M.; McTavish, K.J.; Upton, D.; Handelsman, D.J.; Allan, C.M. Temporal role of Sertoli cell androgen receptor expression in spermatogenic development. Mol. Endocrinol. 2013, 27, 12–24. [Google Scholar] [CrossRef]
- Elliott, M.R.; Zheng, S.; Park, D.; Woodson, R.I.; Reardon, M.A.; Juncadella, I.J.; Kinchen, J.M.; Zhang, J.; Lysiak, J.J.; Ravichandran, K.S. Unexpected requirement for ELMO1 in clearance of apoptotic germ cells in vivo. Nature 2010, 467, 333–337. [Google Scholar] [CrossRef]
- McLachlan, R.I.; Wreford, N.G.; O‘Donnell, L.; de Kretser, D.M.; Robertson, D.M. The endocrine regulation of spermatogenesis: Independent roles for testosterone and FSH. J. Endocrinol. 1996, 148, 1–9. [Google Scholar] [CrossRef]
- Beardsley, A.; O‘Donnell, L. Characterization of normal spermiation and spermiation failure induced by hormone suppression in adult rats. Biol. Reprod. 2003, 68, 1299–1307. [Google Scholar] [CrossRef]
- Chapin, R.E.; Wine, R.N.; Harris, M.W.; Borchers, C.H.; Haseman, J.K. Structure and control of a cell-cell adhesion complex associated with spermiation in rat seminiferous epithelium. J. Androl. 2001, 22, 1030–1052. [Google Scholar] [CrossRef]
- Hughes, I.A.; Deeb, A. Androgen resistance. Best. Pract. Res. Clin. Endocrinol. Metab. 2006, 20, 577–598. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, H.E.; Cortes, D.; Rajpert-De Meyts, E.; Ritzén, E.M.; Nordenskjöld, A.; Skakkebaek, N.E.; Toppari, J. Development and descent of the testis in relation to cryptorchidism. Acta Paediatr. 2007, 96, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Baskin, L.S.; Himes, K.; Colborn, T. Hypospadias and endocrine disruption: Is there a connection? Environ. Health Perspect. 2001, 109, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Skakkebaek, N.E.; Rajpert-De Meyts, E.; Main, K.M. Testicular dysgenesis syndrome: An increasingly common developmental disorder with environmental aspects. Hum. Reprod. 2001, 16, 972–978. [Google Scholar] [CrossRef]
- Welsh, M.; Saunders, P.T.K.; Fisken, M.; Scott, H.M.; Hutchison, G.R.; Smith, L.B.; Sharpe, R.M. Identification in rats of a programming window for reproductive tract masculinization, disruption of which leads to hypospadias and cryptorchidism. J. Clin. Investig. 2008, 118, 1479–1490. [Google Scholar] [CrossRef]
- Zirkin, B.R.; Awoniyi, C.; Griswold, M.D.; Russell, L.D.; Sharpeh, R. Is FSH Required for Adult Spermatogenesis? J. Androl. 1994, 15, 273–276. [Google Scholar] [CrossRef]
- Das, N.; Kumar, T.R. Molecular regulation of follicle-stimulating hormone synthesis, secretion and action. J. Mol. Endocrinol. 2018, 60, R131–R155. [Google Scholar] [CrossRef] [PubMed]
- Gloaguen, P.; Crépieux, P.; Heitzler, D.; Poupon, A.; Reiter, E. Mapping the follicle-stimulating hormone-induced signaling networks. Front. Endocrinol. 2011, 2, 45. [Google Scholar] [CrossRef] [PubMed]
- Ulloa-Aguirre, A.; Reiter, E.; Crépieux, P. FSH Receptor Signaling: Complexity of Interactions and Signal Diversity. Endocrinology 2018, 159, 3020–3035. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.; Hwang, B.D. Follicle-stimulating hormone transiently induces expression of protooncogene c-myc in primary Sertoli cell cultures of early pubertal and prepubertal rat. Mol. Cell Endocrinol. 1995, 111, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.M.; McKinnell, C.; Kivlin, C.; Fisher, J.S. Proliferation and functional maturation of Sertoli cells, and their relevance to disorders of testis function in adulthood. Reproduction 2003, 125, 769–784. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-M.; Li, Z.-F.; Yang, W.-X.; Tan, F.-Q. Follicle-stimulating hormone signaling in Sertoli cells: A licence to the early stages of spermatogenesis. Reprod. Biol. Endocrinol. 2022, 20, 97. [Google Scholar] [CrossRef] [PubMed]
- Maccarrone, M.; Cecconi, S.; Rossi, G.; Battista, N.; Pauselli, R.; Finazzi-Agrò, A. Anandamide activity and degradation are regulated by early postnatal aging and follicle-stimulating hormone in mouse Sertoli cells. Endocrinology 2003, 144, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Godmann, M.; Kosan, C.; Behr, R. Krüppel-like factor 4 is widely expressed in the mouse male and female reproductive tract and responds as an immediate early gene to activation of the protein kinase A in TM4 Sertoli cells. Reproduction 2010, 139, 771–782. [Google Scholar] [CrossRef]
- Delfino, F.; Walker, W.H. Stage-specific nuclear expression of NF-kappaB in mammalian testis. Mol. Endocrinol. 1998, 12, 1696–1707. [Google Scholar]
- Hamil, K.G.; Conti, M.; Shimasaki, S.; Hall, S.H. Follicle-stimulating hormone regulation of AP-1: Inhibition of c-jun and stimulation of jun-B gene transcription in the rat Sertoli cell. Mol. Cell Endocrinol. 1994, 99, 269–277. [Google Scholar] [CrossRef]
- Bhattacharya, I.; Pradhan, B.S.; Sarda, K.; Gautam, M.; Basu, S.; Majumdar, S.S. A switch in Sertoli cell responsiveness to FSH may be responsible for robust onset of germ cell differentiation during prepubartal testicular maturation in rats. Am. J. Physiol. Endocrinol. Metab. 2012, 303, E886–E898. [Google Scholar] [CrossRef] [PubMed]
- Rossi, P.; Dolci, S. Paracrine mechanisms involved in the control of early stages of Mammalian spermatogenesis. Front. Endocrinol 2013, 4, 181. [Google Scholar] [CrossRef] [PubMed]
- Jabarpour, M.; Tajik, P. Evaluation of the effect of follicular stimulating hormone on the in vitro bovine spermatogonial stem cells self-renewal: An experimental study. Int. J. Reprod. Biomed. 2017, 15, 795–802. [Google Scholar] [CrossRef]
- Simon, L.; Ekman, G.C.; Tyagi, G.; Hess, R.A.; Murphy, K.M.; Cooke, P.S. Common and distinct factors regulate expression of mRNA for ETV5 and GDNF, Sertoli cell proteins essential for spermatogonial stem cell maintenance. Exp. Cell Res. 2007, 313, 3090–3099. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, H.; Kanastu-Shinohara, M.; Ogonuki, N.; Kamimura, S.; Ogura, A.; Yabe-Nishimura, C.; Mori, Y.; Morimoto, T.; Watanabe, S.; Otsu, K.; et al. ROS amplification drives mouse spermatogonial stem cell self-renewal. Life Sci. Alliance 2019, 2, e201900374. [Google Scholar] [CrossRef] [PubMed]
- Rossi, P.; Dolci, S.; Albanesi, C.; Grimaldi, P.; Ricca, R.; Geremia, R. Follicle-stimulating hormone induction of steel factor, (SLF) mRNA in mouse Sertoli cells and stimulation of DNA synthesis in spermatogonia by soluble SLF. Dev. Biol. 1993, 155, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhang, Y.; Zhang, X.; Sun, J.; Hao, J. BMP4/Smad signaling pathway induces the differentiation of mouse spermatogonial stem cells via upregulation of Sohlh2. Anat. Rec. 2014, 297, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Hedger, M.P.; Winnall, W.R. Regulation of activin and inhibin in the adult testis and the evidence for functional roles in spermatogenesis and immunoregulation. Mol. Cell Endocrinol. 2012, 359, 30–42. [Google Scholar] [CrossRef]
- Hakovirta, H.; Syed, V.; Jégou, B.; Parvinen, M. Function of interleukin-6 as an inhibitor of meiotic DNA synthesis in the rat seminiferous epithelium. Mol. Cell Endocrinol. 1995, 108, 193–198. [Google Scholar] [CrossRef]
- Eto, K. Nociceptin and meiosis during spermatogenesis in postnatal testes. Vitam. Horm. 2015, 97, 167–186. [Google Scholar]
- Deschildre, C.; Ji, J.W.; Chater, S.; Dacheux, F.; Selva, J.; Albert, M.; Bailly, M.; Hatey, F.; Benahmed, M. Expression of galectin-3 and its regulation in the testes. Int. J. Androl. 2007, 30, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Suomalainen, L.; Dunkel, L.; Ketola, I.; Eriksson, M.; Erkkilä, K.; Oksjoki, R.; Taari, K.; Heikinheimo, M.; Pentikäinen, V. Activator protein-1 in human male germ cell apoptosis. Mol. Hum. Reprod. 2004, 10, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Abel, M.H.; Baker, P.J.; Charlton, H.M.; Monteiro, A.; Verhoeven, G.; De Gendt, K.; Guillou, F.; O‘Shaughnessy, P.J. Spermatogenesis and sertoli cell activity in mice lacking sertoli cell receptors for follicle-stimulating hormone and androgen. Endocrinology 2008, 149, 3279–3285. [Google Scholar] [CrossRef] [PubMed]
- Wreford, N.G.; Rajendra Kumar, T.; Matzuk, M.M.; de Kretser, D.M. Analysis of the testicular phenotype of the follicle-stimulating hormone beta-subunit knockout and the activin type II receptor knockout mice by stereological analysis. Endocrinology 2001, 142, 2916–2920. [Google Scholar] [CrossRef] [PubMed]
- Casarini, L.; Crépieux, P. Molecular Mechanisms of Action of FSH. Front. Endocrinol. 2019, 10, 305. [Google Scholar] [CrossRef] [PubMed]
- Dierich, A.; Sairam, M.R.; Monaco, L.; Fimia, G.M.; Gansmuller, A.; LeMeur, M.; Sassone-Corsi, P. Impairing follicle-stimulating hormone, (FSH) signaling in vivo: Targeted disruption of the FSH receptor leads to aberrant gametogenesis and hormonal imbalance. Proc. Natl. Acad. Sci. USA 1998, 95, 13612–13617. [Google Scholar] [CrossRef] [PubMed]
- Abel, M.H.; Wootton, A.N.; Wilkins, V.; Huhtaniemi, I.; Knight, P.G.; Charlton, H.M. The effect of a null mutation in the follicle-stimulating hormone receptor gene on mouse reproduction. Endocrinology 2000, 141, 1795–1803. [Google Scholar] [CrossRef]
- O‘Shaughnessy, P.J.; Monteiro, A.; Abel, M. Testicular development in mice lacking receptors for follicle stimulating hormone and androgen. PLoS ONE 2012, 7, e35136. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Mao, J.; Cui, M.; Liu, Z.; Wang, X.; Xiong, S.; Nie, M.; Wu, X. Novel FSHβ mutation in a male patient with isolated FSH deficiency and infertility. Eur. J. Med. Genet. 2017, 60, 335–339. [Google Scholar] [CrossRef]
- Rougier, C.; Hieronimus, S.; Panaïa-Ferrari, P.; Lahlou, N.; Paris, F.; Fenichel, P. Isolated follicle-stimulating hormone, (FSH) deficiency in two infertile men without FSH β gene mutation: Case report and literature review. Ann. Endocrinol. 2019, 80, 234–239. [Google Scholar] [CrossRef]
- Gromoll, J.; Simoni, M.; Nieschlag, E. An activating mutation of the follicle-stimulating hormone receptor autonomously sustains spermatogenesis in a hypophysectomized man. J. Clin. Endocrinol. Metab. 1996, 81, 1367–1370. [Google Scholar] [PubMed]
- Oduwole, O.O.; Peltoketo, H.; Huhtaniemi, I.T. Role of Follicle-Stimulating Hormone in Spermatogenesis. Front. Endocrinol. 2018, 9, 763. [Google Scholar] [CrossRef] [PubMed]
- Oduwole, O.O.; Peltoketo, H.; Poliandri, A.; Vengadabady, L.; Chrusciel, M.; Doroszko, M.; Samanta, L.; Owen, L.; Keevil, B.; Rahman, N.A.; et al. Constitutively active follicle-stimulating hormone receptor enables androgen-independent spermatogenesis. J. Clin. Investig. 2018, 128, 1787–1792. [Google Scholar] [CrossRef] [PubMed]
- Meachem, S.J.; Nieschlag, E.; Simoni, M. Inhibin B in male reproduction: Pathophysiology and clinical relevance. Eur. J. Endocrinol. 2001, 145, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Mizuno, K.; Matsumoto, D.; Nishio, H.; Nakane, A.; Kurokawa, S.; Kamisawa, H.; Maruyama, T.; Iwatsuki, S.; Umemoto, Y.; et al. Low Serum Inhibin B/Follicle-Stimulating Hormones and Anti-Müllerian Hormone/Follicle-Stimulating Hormones Ratios as Markers of Decreased Germ Cells in Infants with Bilateral Cryptorchidism. J. Urol. 2022, 207, 701–709. [Google Scholar] [CrossRef] [PubMed]
- Iliadou, P.K.; Tsametis, C.; Kaprara, A.; Papadimas, I.; Goulis, D.G. The Sertoli cell: Novel clinical potentiality. Hormones 2015, 14, 504–514. [Google Scholar] [CrossRef] [PubMed]
- Main, K.M.; Toppari, J.; Suomi, A.-M.; Kaleva, M.; Chellakooty, M.; Schmidt, I.M.; Virtanen, H.E.; Boisen, K.A.; Kai, C.M.; Damgaard, I.N.; et al. Larger testes and higher inhibin B levels in Finnish than in Danish newborn boys. J. Clin. Endocrinol. Metab. 2006, 91, 2732–2737. [Google Scholar] [CrossRef] [PubMed]
- Grinspon, R.P.; Andreone, L.; Bedecarrás, P.; Ropelato, M.G.; Rey, R.A.; Campo, S.M.; Bergadá, I. Male Central Precocious Puberty: Serum Profile of Anti-Müllerian Hormone and Inhibin B before, during, and after Treatment with GnRH Analogue. Int. J. Endocrinol. 2013, 2013, 823064. [Google Scholar] [CrossRef] [PubMed]
- Jankowska, K.; Suszczewicz, N.; Rabijewski, M.; Dudek, P.; Zgliczyński, W.; Maksym, R.B. Inhibin-B and FSH Are Good Indicators of Spermatogenesis but Not the Best Indicators of Fertility. Life 2022, 12, 511. [Google Scholar] [CrossRef]
- Kong, X.; Ye, Z.; Chen, Y.; Zhao, H.; Tu, J.; Meng, T.; Xiong, C.; Li, H.; Gong, Y.; Zheng, L.; et al. Clinical application value of Inhibin B alone or in combination with other hormone indicators in subfertile men with different spermatogenesis status: A study of 324 Chinese men. J. Clin. Lab. Anal. 2021, 35, e23882. [Google Scholar] [CrossRef]
- Barbotin, A.-L.; Ballot, C.; Sigala, J.; Ramdane, N.; Duhamel, A.; Marcelli, F.; Rigot, J.-M.; Dewailly, D.; Pigny, P.; Mitchell, V. The serum inhibin B concentration and reference ranges in normozoospermia. Eur. J. Endocrinol. 2015, 172, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Bloise, E.; Ciarmela, P.; Dela Cruz, C.; Luisi, S.; Petraglia, F.; Reis, F.M. Activin A in Mammalian Physiology. Physiol. Rev. 2019, 99, 739–780. [Google Scholar] [CrossRef] [PubMed]
- Massagué, J. How cells read TGF-beta signals. Nat. Rev. Mol. Cell Biol. 2000, 1, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Mendis, S.H.S.; Meachem, S.J.; Sarraj, M.A.; Loveland, K.L. Activin A balances Sertoli and germ cell proliferation in the fetal mouse testis. Biol. Reprod. 2011, 84, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Archambeault, D.R.; Yao, H.H.-C. Activin A, a product of fetal Leydig cells, is a unique paracrine regulator of Sertoli cell proliferation and fetal testis cord expansion. Proc. Natl. Acad. Sci. USA 2010, 107, 10526–10531. [Google Scholar] [CrossRef] [PubMed]
- Seachrist, D.D.; Johnson, E.; Magee, C.; Clay, C.M.; Graham, J.K.; Veeramachaneni, D.N.R.; Keri, R.A. Overexpression of follistatin in the mouse epididymis disrupts fluid resorption and sperm transit in testicular excurrent ducts. Biol. Reprod. 2012, 87, 41. [Google Scholar] [CrossRef]
- Tomaszewski, J.; Joseph, A.; Archambeault, D.; Yao, H.H.-C. Essential roles of inhibin beta A in mouse epididymal coiling. Proc. Natl. Acad. Sci. USA 2007, 104, 11322–11327. [Google Scholar] [CrossRef] [PubMed]
- Whiley, P.A.F.; O‘Donnell, L.; Moody, S.C.; Handelsman, D.J.; Young, J.C.; Richards, E.A.; Almstrup, K.; Western, P.S.; Loveland, K.L. Activin A Determines Steroid Levels and Composition in the Fetal Testis. Endocrinology 2020, 161, bqaa058. [Google Scholar] [CrossRef]
- Josso, N.; Rey, R.A.; Picard, J.-Y. Anti-müllerian hormone: A valuable addition to the toolbox of the pediatric endocrinologist. Int. J. Endocrinol. 2013, 2013, 674105. [Google Scholar] [CrossRef]
- Edelsztein, N.Y.; Valeri, C.; Lovaisa, M.M.; Schteingart, H.F.; Rey, R.A. AMH Regulation by Steroids in the Mammalian Testis: Underlying Mechanisms and Clinical Implications. Front. Endocrinol. 2022, 13, 906381. [Google Scholar] [CrossRef]
- Aksglaede, L.; Sørensen, K.; Boas, M.; Mouritsen, A.; Hagen, C.P.; Jensen, R.B.; Petersen, J.H.; Linneberg, A.; Andersson, A.M.; Main, K.M.; et al. Changes in anti-Müllerian hormone, (AMH) throughout the life span: A population-based study of 1027 healthy males from birth, (cord blood) to the age of 69 years. J. Clin. Endocrinol. Metab. 2010, 95, 5357–5364. [Google Scholar] [CrossRef] [PubMed]
- Jeffery, A.; Streeter, A.J.; Hosking, J.; Wilkin, T.J.; Nelson, S.M. Anti-Müllerian hormone in children: A ten-year prospective longitudinal study, (EarlyBird 39). J. Pediatr. Endocrinol. Metab. 2015, 28, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Edelsztein, N.Y.; Grinspon, R.P.; Schteingart, H.F.; Rey, R.A. Anti-Müllerian hormone as a marker of steroid and gonadotropin action in the testis of children and adolescents with disorders of the gonadal axis. Int. J. Pediatr. Endocrinol. 2016, 2016, 20. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.M.; Donahoe, P.K.; Silverman, B.L.; Hasegawa, T.; Hasegawa, Y.; Gustafson, M.L.; Chang, Y.C.; MacLaughlin, D.T. Measurements of serum müllerian inhibiting substance in the evaluation of children with nonpalpable gonads. N. Engl. J. Med. 1997, 336, 1480–1486. [Google Scholar] [CrossRef] [PubMed]
- Ivell, R.; Mamsen, L.S.; Andersen, C.Y.; Anand-Ivell, R. Expression and Role of INSL3 in the Fetal Testis. Front. Endocrinol. 2022, 13, 868313. [Google Scholar] [CrossRef] [PubMed]
- Facondo, P.; Delbarba, A.; Maffezzoni, F.; Cappelli, C.; Ferlin, A. INSL3: A Marker of Leydig Cell Function and Testis-Bone-Skeletal Muscle Network. Protein Pept. Lett. 2020, 27, 1246–1252. [Google Scholar] [CrossRef]
- Hutson, J.M.; Southwell, B.R.; Li, R.; Lie, G.; Ismail, K.; Harisis, G.; Chen, N. The regulation of testicular descent and the effects of cryptorchidism. Endocr. Rev. 2013, 34, 725–752. [Google Scholar] [CrossRef] [PubMed]
- Kaleva, M.; Toppari, J. Genetics and hormones in testicular descent. Hormones 2003, 2, 211–216. [Google Scholar] [CrossRef]
- Nef, S.; Parada, L.F. Cryptorchidism in mice mutant for Insl3. Nat. Genet. 1999, 22, 295–299. [Google Scholar] [CrossRef]
- Kawamura, K.; Kumagai, J.; Sudo, S.; Chun, S.-Y.; Pisarska, M.; Morita, H.; Toppari, J.; Fu, P.; Wade, J.D.; Bathgate, R.A.D.; et al. Paracrine regulation of mammalian oocyte maturation and male germ cell survival. Proc. Natl. Acad. Sci. USA 2004, 101, 7323–7328. [Google Scholar] [CrossRef]
- Amory, J.K.; Page, S.T.; Anawalt, B.D.; Coviello, A.D.; Matsumoto, A.M.; Bremner, W.J. Elevated end-of-treatment serum INSL3 is associated with failure to completely suppress spermatogenesis in men receiving male hormonal contraception. J. Androl. 2007, 28, 548–554. [Google Scholar] [CrossRef]
- Anand-Ivell, R.J.K.; Relan, V.; Balvers, M.; Coiffec-Dorval, I.; Fritsch, M.; Bathgate, R.A.D.; Ivell, R. Expression of the insulin-like peptide 3, (INSL3) hormone-receptor, (LGR8) system in the testis. Biol. Reprod. 2006, 74, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Hess, R.A.; Cooke, P.S. Estrogen in the male: A historical perspective. Biol. Reprod. 2018, 99, 27–44. [Google Scholar] [CrossRef] [PubMed]
- Cooke, P.S.; Nanjappa, M.K.; Ko, C.; Prins, G.S.; Hess, R.A. Estrogens in Male Physiology. Physiol. Rev. 2017, 97, 72. [Google Scholar] [CrossRef] [PubMed]
- Nanjappa, M.K.; Hess, R.A.; Medrano, T.I.; Locker, S.H.; Levin, E.R.; Cooke, P.S. Membrane-Localized Estrogen Receptor 1 Is Required for Normal Male Reproductive Development and Function in Mice. Endocrinology 2016, 157, 2909–2919. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.W.; Nie, R.; Carnes, K.; Zhou, Q.; Sharief, N.A.Q.; Hess, R.A. The antiestrogen ICI 182,780 induces early effects on the adult male mouse reproductive tract and long-term decreased fertility without testicular atrophy. Reprod. Biol. Endocrinol. 2003, 1, 57. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.A.; Carnes, K.; França, L.R.; Hess, R.A. Infertility and testicular atrophy in the antiestrogen-treated adult male rat. Biol. Reprod. 2001, 65, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Robertson, K.M.; O‘Donnell, L.; Simpson, E.R.; Jones, M.E.E. The phenotype of the aromatase knockout mouse reveals dietary phytoestrogens impact significantly on testis function. Endocrinology 2002, 143, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- Robertson, K.M.; O‘Donnell, L.; Jones, M.E.; Meachem, S.J.; Boon, W.C.; Fisher, C.R.; Graves, K.H.; McLachlan, R.I.; Simpson, E.R. Impairment of spermatogenesis in mice lacking a functional aromatase, (cyp 19) gene. Proc. Natl. Acad. Sci. USA 1999, 96, 7986–7991. [Google Scholar] [CrossRef]
- Robertson, K.M.; Simpson, E.R.; Lacham-Kaplan, O.; Jones, M.E. Characterization of the fertility of male aromatase knockout mice. J. Androl. 2001, 22, 825–830. [Google Scholar] [CrossRef]
- Assinder, S.; Davis, R.; Fenwick, M.; Glover, A. Adult-only exposure of male rats to a diet of high phytoestrogen content increases apoptosis of meiotic and post-meiotic germ cells. Reproduction 2007, 133, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Wynder, J.L.; Nicholson, T.M.; DeFranco, D.B.; Ricke, W.A. Estrogens and Male Lower Urinary Tract Dysfunction. Curr. Urol. Rep. 2015, 16, 61. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Hu, W.; Majumdar, S.; Gauntner, T.; Li, Y.; Shi, G.; Kasper, S.; Prins, G.S. Distinct actions of ERα and ERβ in human prostate stem and progenitor cell self-renewal and differentiation. Endocrinology 2016, 64, 928. [Google Scholar] [CrossRef]
- Raut, S.; Deshpande, S.; Balasinor, N.H. Unveiling the Role of Prolactin and its Receptor in Male Reproduction. Horm. Metab. Res. 2019, 51, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Nag, S.; Sanyal, S.; Ghosh, K.K.; Biswas, N.M. Prolactin suppression and spermatogenic developments in maturing rats. A quantitative study. Horm. Res. 1981, 15, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Steger, R.W.; Chandrashekar, V.; Zhao, W.; Bartke, A.; Horseman, N.D. Neuroendocrine and reproductive functions in male mice with targeted disruption of the prolactin gene. Endocrinology 1998, 139, 3691–3695. [Google Scholar] [CrossRef] [PubMed]
- Buvat, J. Hyperprolactinemia and sexual function in men: A short review. Int. J. Impot. Res. 2003, 15, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Buvat, J.; Lemaire, A.; Buvat-Herbaut, M.; Fourlinnie, J.C.; Racadot, A.; Fossati, P. Hyperprolactinemia and sexual function in men. Horm. Res. 1985, 22, 196–203. [Google Scholar] [CrossRef]
- Spaggiari, G.; Costantino, F.; Granata, A.R.M.; Tagliavini, S.; Canu, G.; Varani, M.; De Santis, M.C.; Roli, L.; Trenti, T.; Simoni, M.; et al. Prolactin and spermatogenesis: New lights on the interplay between prolactin and sperm parameters. Endocrine 2023, 81, 330–339. [Google Scholar] [CrossRef]
- Thackare, H.; Nicholson, H.D.; Whittington, K. Oxytocin--its role in male reproduction and new potential therapeutic uses. Hum. Reprod. Update 2006, 12, 437–448. [Google Scholar] [CrossRef]
- Assinder, S.J.; Rezvani, A.; Nicholson, H.D. Oxytocin promotes spermiation and sperm transfer in the mouse. Int. J. Androl. 2002, 25, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Anjum, S.; Anuradha, A.; Krishna, A. A possible direct action of oxytocin on spermatogenesis and steroidogenesis in pre-pubertal mouse. Andrologia 2018. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Caligioni, C.S.; Oliver, C.; Jamur, M.C.; Franci, C.R. Presence of oxytocin receptors in the gonadotrophin-releasing hormone, (GnRH) neurones in female rats: A possible direct action of oxytocin on GnRH neurones. J. Neuroendocrinol. 2007, 19, 439–448. [Google Scholar] [CrossRef] [PubMed]
- Navarro, V.M. Metabolic regulation of kisspeptin—The link between energy balance and reproduction. Nat. Rev. Endocrinol. 2020, 16, 407–420. [Google Scholar] [CrossRef] [PubMed]
- Guimiot, F.; Chevrier, L.; Dreux, S.; Chevenne, D.; Caraty, A.; Delezoide, A.L.; de Roux, N. Negative fetal FSH/LH regulation in late pregnancy is associated with declined kisspeptin/KISS1R expression in the tuberal hypothalamus. J. Clin. Endocrinol. Metab. 2012, 97, E2221–E2229. [Google Scholar] [CrossRef] [PubMed]
- Salonia, A.; Rastrelli, G.; Hackett, G.; Seminara, S.B.; Huhtaniemi, I.T.; Rey, R.A.; Hellstrom, W.J.G.; Palmert, M.R.; Corona, G.; Dohle, G.R.; et al. Paediatric and adult-onset male hypogonadism. Nat. Rev. Dis. Primers 2019, 5, 38. [Google Scholar] [CrossRef]
- Cate, R.L. Anti-Müllerian Hormone Signal Transduction involved in Müllerian Duct Regression. Front.. Endocrinol. 2022, 13, 905324. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.-Y.; Zhang, H.-X.; Xiao, Z.; Qiao, J.; Li, R. Regulation of anti-Müllerian hormone, (AMH) in males and the associations of serum AMH with the disorders of male fertility. Asian J. Androl. 2019, 21, 109–114. [Google Scholar]
- Schwanzel-Fukuda, M.; Crossin, K.L.; Pfaff, D.W.; Bouloux, P.M.; Hardelin, J.P.; Petit, C. Migration of luteinizing hormone-releasing hormone, (LHRH) neurons in early human embryos. J. Comp. Neurol. 1996, 366, 547–557. [Google Scholar] [CrossRef]
- Debieve, F.; Beerlandt, S.; Hubinont, C.; Thomas, K. Gonadotropins, prolactin, inhibin A, inhibin B, and activin A in human fetal serum from midpregnancy and term pregnancy. J. Clin. Endocrinol. Metab. 2000, 85, 270–274. [Google Scholar] [CrossRef]
- Troisi, R.; Potischman, N.; Roberts, J.M.; Harger, G.; Markovic, N.; Cole, B.; Lykins, D.; Siiteri, P.; Hoover, R.N. Correlation of serum hormone concentrations in maternal and umbilical cord samples. Cancer Epidemiol. Biomark. Prev. 2003, 12, 452–456. [Google Scholar]
- Walker, W.H. Androgen Actions in the Testis and the Regulation of Spermatogenesis. Adv. Exp. Med. Biol. 2021, 1288, 175–203. [Google Scholar] [PubMed]
- Mullen, R.D.; Behringer, R.R. Molecular genetics of Müllerian duct formation, regression and differentiation. Sex. Dev. 2014, 8, 281–296. [Google Scholar] [CrossRef] [PubMed]
- Skakkebaek, N.E.; Rajpert-De Meyts, E.; Buck Louis, G.M.; Toppari, J.; Andersson, A.-M.; Eisenberg, M.L.; Jensen, T.K.; Jørgensen, N.; Swan, S.H.; Sapra, K.J.; et al. Male Reproductive Disorders and Fertility Trends: Influences of Environment and Genetic Susceptibility. Physiol. Rev. 2016, 96, 55–97. [Google Scholar] [CrossRef] [PubMed]
- Lucaccioni, L.; Trevisani, V.; Boncompagni, A.; Marrozzini, L.; Berardi, A.; Iughetti, L. Minipuberty: Looking Back to Understand Moving Forward. Front.. Pediatr. 2020, 8, 612235. [Google Scholar] [CrossRef] [PubMed]
- Becker, M.; Hesse, V. Minipuberty: Why Does it Happen? Horm. Res. Paediatr. 2020, 93, 76–84. [Google Scholar] [CrossRef]
- Kuiri-Hänninen, T.; Sankilampi, U.; Dunkel, L. Activation of the hypothalamic-pituitary-gonadal axis in infancy: Minipuberty. Horm. Res. Paediatr. 2014, 82, 73–80. [Google Scholar] [CrossRef]
- Cortes, D.; Müller, J.; Skakkebaek, N.E. Proliferation of Sertoli cells during development of the human testis assessed by stereological methods. Int. J. Androl. 1987, 10, 589–596. [Google Scholar] [CrossRef]
- Hadziselimovic, F.; Herzog, B. The importance of both an early orchidopexy and germ cell maturation for fertility. Lancet 2001, 358, 1156–1157. [Google Scholar] [CrossRef]
- Schlatt, S.; Zhengwei, Y.; Meehan, T.; de Kretser, D.M.; Loveland, K.L. Application of morphometric techniques to postnatal rat testes in organ culture: Insights into testis growth. Cell Tissue Res. 1999, 298, 335–343. [Google Scholar] [CrossRef]
- Terasawa, E. The mechanism underlying the pubertal increase in pulsatile GnRH release in primates. J. Neuroendocrinol. 2022, 34, e13119. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.C.; Butler, G.E.; Kelnar, C.J.; Stirling, H.F.; Huhtaniemi, I. Patterns of pulsatile luteinizing hormone and follicle-stimulating hormone secretion in prepubertal, (midchildhood) boys and girls and patients with idiopathic hypogonadotropic hypogonadism, (Kallmann’s syndrome): A study using an ultrasensitive time-resolved immunofluorometric assay. J. Clin. Endocrinol. Metab. 1991, 72, 1229–1237. [Google Scholar] [PubMed]
- Garcia, J.P.; Keen, K.L.; Seminara, S.B.; Terasawa, E. Role of Kisspeptin and NKB in Puberty in Nonhuman Primates: Sex Differences. Semin. Reprod. Med. 2019, 37, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Koskenniemi, J.J.; Virtanen, H.E.; Toppari, J. Testicular growth and development in puberty. Curr. Opin. Endocrinol. Diabetes Obes. 2017, 24, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Hero, M.; Tommiska, J.; Vaaralahti, K.; Laitinen, E.-M.; Sipilä, I.; Puhakka, L.; Dunkel, L.; Raivio, T. Circulating antimüllerian hormone levels in boys decline during early puberty and correlate with inhibin B. Fertil. Steril. 2012, 97, 1242–1247. [Google Scholar] [CrossRef] [PubMed]
- Radicioni, A.F.; Anzuini, A.; De Marco, E.; Nofroni, I.; Castracane, V.D.; Lenzi, A. Changes in serum inhibin B during normal male puberty. Eur. J. Endocrinol. 2005, 152, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Spaziani, M.; Tarantino, C.; Tahani, N.; Gianfrilli, D.; Sbardella, E.; Lenzi, A.; Radicioni, A.F. Hypothalamo-Pituitary axis and puberty. Mol. Cell Endocrinol. 2021, 520, 111094. [Google Scholar] [CrossRef]
- Ferlin, A.; Garolla, A.; Rigon, F.; Rasi Caldogno, L.; Lenzi, A.; Foresta, C. Changes in serum insulin-like factor 3 during normal male puberty. J. Clin. Endocrinol. Metab. 2006, 91, 3426–3431. [Google Scholar] [CrossRef]
- Zhang, Z.; Kang, D.; Li, H. The effects of testosterone on bone health in males with testosterone deficiency: A systematic review and meta-analysis. BMC Endocr. Disord. 2020, 20, 33. [Google Scholar] [CrossRef]
- Mohamad, N.-V.; Soelaiman, I.-N.; Chin, K.-Y. A concise review of testosterone and bone health. Clin. Interv. Aging 2016, 11, 1317–1324. [Google Scholar] [CrossRef]
- Warren, A.M.; Grossmann, M. Haematological actions of androgens. Best Pract. Res. Clin. Endocrinol. Metab. 2022, 36, 101653. [Google Scholar] [CrossRef] [PubMed]
- Krausz, C. Male infertility: Pathogenesis and clinical diagnosis. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 271–285. [Google Scholar] [CrossRef] [PubMed]
- Papanikolaou, N.; Luo, R.; Jayasena, C.N. Fertility Considerations in Hypogonadal Men. Endocrinol. Metab. Clin. North Am. 2022, 51, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Bhasin, S.; Brito, J.P.; Cunningham, G.R.; Hayes, F.J.; Hodis, H.N.; Matsumoto, A.M.; Snyder, P.J.; Swerdloff, R.S.; Wu, F.C.; Yialamas, M.A. Testosterone Therapy in Men with Hypogonadism: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2018, 103, 1715–1744. [Google Scholar] [CrossRef] [PubMed]
- Basaria, S. Male hypogonadism. Lancet 2014, 383, 1250–1263. [Google Scholar] [CrossRef] [PubMed]
- Richard-Eaglin, A. Male and Female Hypogonadism. Nurs. Clin. North Am. 2018, 53, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Sigalos, J.T.; Pastuszak, A.W.; Khera, M. Hypogonadism: Therapeutic Risks, Benefits, and Outcomes. Med. Clin. North Am. 2018, 102, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Khalafalla, K.; Pagani, R.L.; Ohlander, S.J.; Niederberger, C.S. Male Hypogonadism and Fertility. In Testosterone: From Basic to Clinical Aspects; Hohl, A., Ed.; Springer International Publishing: Cham, Switzerland, 2023; pp. 245–265. [Google Scholar]
- Silveira, L.F.G.; Latronico, A.C. Approach to the patient with hypogonadotropic hypogonadism. J. Clin. Endocrinol. Metab. 2013, 98, 1781–1788. [Google Scholar] [CrossRef]
- Finer, L.B.; Zolna, M.R. Declines in Unintended Pregnancy in the United States, 2008–2011. N. Engl. J. Med. 2016, 374, 843–852. [Google Scholar] [CrossRef]
- Sundaram, A.; Vaughan, B.; Kost, K.; Bankole, A.; Finer, L.; Singh, S.; Trussell, J. Contraceptive Failure in the United States: Estimates from the 2006–2010 National Survey of Family Growth. Perspect. Sex Reprod. Health 2017, 49, 7–16. [Google Scholar] [CrossRef]
- Turner, T.T.; Jones, C.E.; Howards, S.S.; Ewing, L.L.; Zegeye, B.; Gunsalus, G.L. On the androgen microenvironment of maturing spermatozoa. Endocrinology 1984, 115, 1925–1932. [Google Scholar] [CrossRef]
- McLachlan, R.I.; O‘Donnell, L.; Meachem, S.J.; Stanton, P.G.; de Kretser, D.M.; Pratis, K.; Robertson, D.M. Identification of specific sites of hormonal regulation in spermatogenesis in rats, monkeys, and man. Recent. Prog. Horm. Res. 2002, 57, 149–179. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.A.; Baird, D.T. Male contraception. Endocr. Rev. 2002, 23, 735–762. [Google Scholar] [CrossRef]
- Long, J.E.; Lee, M.S.; Blithe, D.L. Update on Novel Hormonal and Nonhormonal Male Contraceptive Development. J. Clin. Endocrinol. Metab. 2021, 106, e2381–e2392. [Google Scholar] [CrossRef] [PubMed]
- Abbe, C.R.; Page, S.T.; Thirumalai, A. Male Contraception. Yale J. Biol. Med. 2020, 93, 603–613. [Google Scholar] [PubMed]
- Swerdloff, R.S.; Wang, C.; White, W.B.; Kaminetsky, J.; Gittelman, M.C.; Longstreth, J.A.; Dudley, R.E.; Danoff, T.M. A New Oral Testosterone Undecanoate Formulation Restores Testosterone to Normal Concentrations in Hypogonadal Men. J. Clin. Endocrinol. Metab. 2020, 105, 2515–2531. [Google Scholar] [CrossRef] [PubMed]
- Nieschlag, E.; Kumar, N.; Sitruk-Ware, R. 7α-methyl-19-nortestosterone, (MENTR): The population council’s contribution to research on male contraception and treatment of hypogonadism. Contraception 2013, 87, 288–295. [Google Scholar] [CrossRef] [PubMed]
- von Eckardstein, S.; Noe, G.; Brache, V.; Nieschlag, E.; Croxatto, H.; Alvarez, F.; Moo-Young, A.; Sivin, I.; Kumar, N.; Small, M.; et al. A clinical trial of 7 alpha-methyl-19-nortestosterone implants for possible use as a long-acting contraceptive for men. J. Clin. Endocrinol. Metab. 2003, 88, 5232–5239. [Google Scholar] [CrossRef] [PubMed]
- Attardi, B.J.; Engbring, J.A.; Gropp, D.; Hild, S.A. Development of dimethandrolone 17beta-undecanoate, (DMAU) as an oral male hormonal contraceptive: Induction of infertility and recovery of fertility in adult male rabbits. J. Androl. 2011, 32, 530–540. [Google Scholar] [CrossRef]
- Wu, S.; Yuen, F.; Swerdloff, R.S.; Pak, Y.; Thirumalai, A.; Liu, P.Y.; Amory, J.K.; Bai, F.; Hull, L.; Blithe, D.L.; et al. Safety and Pharmacokinetics of Single-Dose Novel Oral Androgen 11β-Methyl-19-Nortestosterone-17β-Dodecylcarbonate in Men. J. Clin. Endocrinol. Metab. 2019, 104, 629–638. [Google Scholar] [CrossRef]
- Yuen, F.; Thirumalai, A.; Pham, C.; Swerdloff, R.S.; Anawalt, B.D.; Liu, P.Y.; Amory, J.K.; Bremner, W.J.; Dart, C.; Wu, H.; et al. Daily Oral Administration of the Novel Androgen 11β-MNTDC Markedly Suppresses Serum Gonadotropins in Healthy Men. J. Clin. Endocrinol. Metab. 2020, 105, e835–e847. [Google Scholar] [CrossRef] [PubMed]
- Ilani, N.; Roth, M.Y.; Amory, J.K.; Swerdloff, R.S.; Dart, C.; Page, S.T.; Bremner, W.J.; Sitruk-Ware, R.; Kumar, N.; Blithe, D.L.; et al. A new combination of testosterone and nestorone transdermal gels for male hormonal contraception. J. Clin. Endocrinol. Metab. 2012, 97, 3476–3486. [Google Scholar] [CrossRef] [PubMed]
- Campelia, G.D.; Abbe, C.; Nickels, L.M.; McElmeel, E.; Amory, J.K. “Shared risk”: Reframing risk analysis in the ethics of novel male contraceptives. Contraception 2020, 102, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Oduwole, O.O.; Vydra, N.; Wood, N.E.M.; Samanta, L.; Owen, L.; Keevil, B.; Donaldson, M.; Naresh, K.; Huhtaniemi, I.T. Overlapping dose responses of spermatogenic and extragonadal testosterone actions jeopardize the principle of hormonal male contraception. FASEB J. 2014, 28, 2566–2576. [Google Scholar] [CrossRef] [PubMed]
- Ibtisham, F.; Honaramooz, A. Spermatogonial Stem Cells for In Vitro Spermatogenesis and In Vivo Restoration of Fertility. Cells 2020, 9, 745. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Huang, X.; Dou, L.; Yan, M.; Shen, T.; Tang, W.; Li, J. Aging and aging-related diseases: From molecular mechanisms to interventions and treatments. Signal Transduct. Target. Ther. 2022, 7, 391. [Google Scholar] [CrossRef] [PubMed]
- Diamanti-Kandarakis, E.; Bourguignon, J.-P.; Giudice, L.C.; Hauser, R.; Prins, G.S.; Soto, A.M.; Zoeller, R.T.; Gore, A.C. Endocrine-disrupting chemicals: An Endocrine Society scientific statement. Endocr. Rev. 2009, 30, 293–342. [Google Scholar] [CrossRef]
- Gargus, E.S.; Rogers, H.B.; McKinnon, K.E.; Edmonds, M.E.; Woodruff, T.K. Engineered reproductive tissues. Nat. Biomed. Eng. 2020, 4, 381–393. [Google Scholar] [CrossRef]
- Malijauskaite, S.; Connolly, S.; Newport, D.; McGourty, K. Gradients in the in vivo intestinal stem cell compartment and their in vitro recapitulation in mimetic platforms. Cytokine Growth Factor. Rev. 2021, 60, 76–88. [Google Scholar] [CrossRef]
- O‘Donnell, L.; Stanton, P.; de Kretser, D.M. Endocrinology of the Male Reproductive System and Spermatogenesis. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatanya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Bashiri, Z.; Gholipourmalekabadi, M.; Khadivi, F.; Salem, M.; Afzali, A.; Cham, T.-C.; Koruji, M. In vitro spermatogenesis in artificial testis: Current knowledge and clinical implications for male infertility. Cell Tissue Res. 2023, 394, 393–421. [Google Scholar] [CrossRef]
- Sato, T.; Katagiri, K.; Gohbara, A.; Inoue, K.; Ogonuki, N.; Ogura, A.; Kubota, Y.; Ogawa, T. In vitro production of functional sperm in cultured neonatal mouse testes. Nature 2011, 471, 504–507. [Google Scholar] [CrossRef] [PubMed]
- Yokonishi, T.; Sato, T.; Komeya, M.; Katagiri, K.; Kubota, Y.; Nakabayashi, K.; Hata, K.; Inoue, K.; Ogonuki, N.; Ogura, A.; et al. Offspring production with sperm grown in vitro from cryopreserved testis tissues. Nat. Commun. 2014, 5, 4320. [Google Scholar] [CrossRef] [PubMed]



| Hormones | Secretory Regions | Target Cells | Disordered Diseases |
|---|---|---|---|
| GnRH | hypothalamic neurosecretory cells | pituitary gonadotrophs | precocious puberty, hypergonadism, Kallmann syndrome, oligospermia [20] |
| LH | pituitary gonadotrophs | Leydig cells | hypogonadism [21] |
| FSH | pituitary gonadotrophs | Sertoli cells, peritubular myoid cells, Spermatogoniums | hypogonadism [21] |
| T | Leydig cells, Sertoli cells | germ cells, Sertoli cells, PMCs | TDS, micropenis [21,22] |
| AMH | Sertoli cells | Müllerian ducts mesenchymal cells | persistent Müllerian duct syndrome (PMDS) [23] |
| Inhibin B | Sertoli cells | pituitary gonadotrophs | spermatogenesis disorder [24] |
| INSL3 | Leydig cells | Leydig cells | cryptorchidism [25] |
| Hormones | Fetal Life | Minipuberty | Puberty |
|---|---|---|---|
| GnRH | serum LH and FSH levels in the second trimester are independent of GnRH, and then GnRH gradually controls the release of LH and FSH [155] | stimulates Sertoli cells to secrete inhibin B and AMH, and Leydig cells to produce INSL3 | increases gradually, triggering the secretion of LH and FSH |
| LH | replaces HCG to promote the secretion of testosterone by Leydig cells [21] | stimulates Leydig cells to release testosterone | stimulated the differentiation of Leydig cells and their ability to produce testosterone |
| FSH | stimulates Sertoli cell proliferation and increases AMH and inhibin B | stimulates Sertoli cell proliferation and increases AMH and inhibin B | stimulates the proliferation of immature Sertoli cells and spermatogonia |
| T | induces the differentiation and development of the mesonephric duct into seminal vesicles, epididymis, and spermaduct [156] | promotes the conversion of germ cells into spermatogonia | initiation of spermatogenesis |
| AMH | causes fallopian tube regression in men, preventing the formation of the uterus and fallopian tubes [157] | as a diagnostic indicator of male fertility-related disorders [158] | as a diagnostic indicator of male fertility-related disorders [158] |
| Inhibin B | regulates FSH secretion and acts as a marker for Sertoli cell function | regulates FSH secretion and acts as a marker for Sertoli cell function | inhibit FSH secretion and markers of sperm production in men |
| INSL3 | the regulation of intra-abdominal testicular descent by regulating the growth and differentiation of the gubernaculum [129] | as an accurate measure of Leydig cell functional capacity [125] | as an accurate measure of Leydig cell functional capacity [125] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, L.; Lin, W.; Wang, Z.; Huang, R.; Xia, H.; Li, Z.; Deng, J.; Ye, T.; Huang, Y.; Yang, Y. Hormone Regulation in Testicular Development and Function. Int. J. Mol. Sci. 2024, 25, 5805. https://doi.org/10.3390/ijms25115805
Li L, Lin W, Wang Z, Huang R, Xia H, Li Z, Deng J, Ye T, Huang Y, Yang Y. Hormone Regulation in Testicular Development and Function. International Journal of Molecular Sciences. 2024; 25(11):5805. https://doi.org/10.3390/ijms25115805
Chicago/Turabian StyleLi, Lu, Wanqing Lin, Zhaoyang Wang, Rufei Huang, Huan Xia, Ziyi Li, Jingxian Deng, Tao Ye, Yadong Huang, and Yan Yang. 2024. "Hormone Regulation in Testicular Development and Function" International Journal of Molecular Sciences 25, no. 11: 5805. https://doi.org/10.3390/ijms25115805
APA StyleLi, L., Lin, W., Wang, Z., Huang, R., Xia, H., Li, Z., Deng, J., Ye, T., Huang, Y., & Yang, Y. (2024). Hormone Regulation in Testicular Development and Function. International Journal of Molecular Sciences, 25(11), 5805. https://doi.org/10.3390/ijms25115805






