Imaging Flow Cytometry and Convolutional Neural Network-Based Classification Enable Discrimination of Hematopoietic and Leukemic Stem Cells in Acute Myeloid Leukemia
Abstract
1. Introduction
2. Results
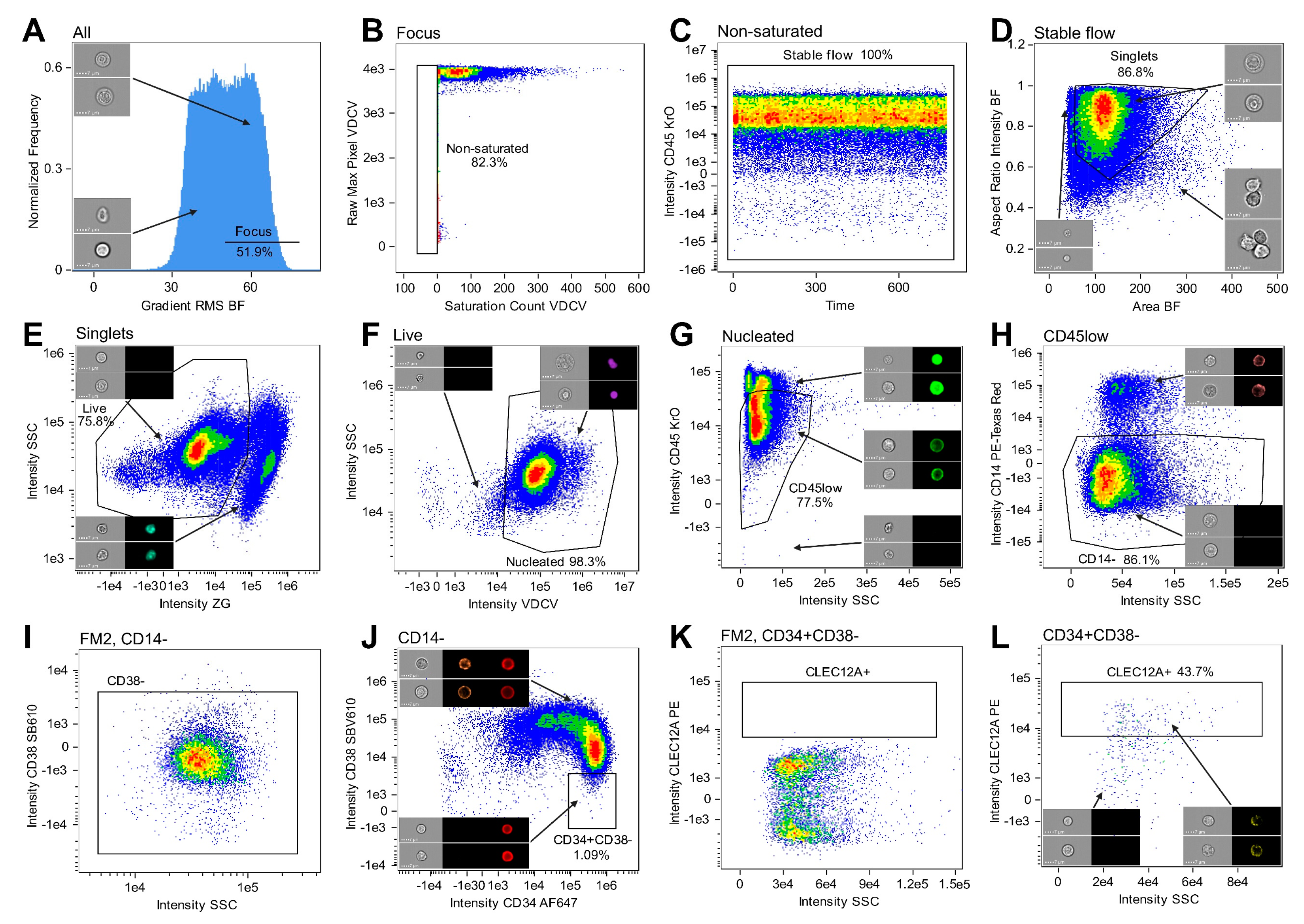
2.1. IFC Permits Immunophenotypic Identification of HSCs and LSCs
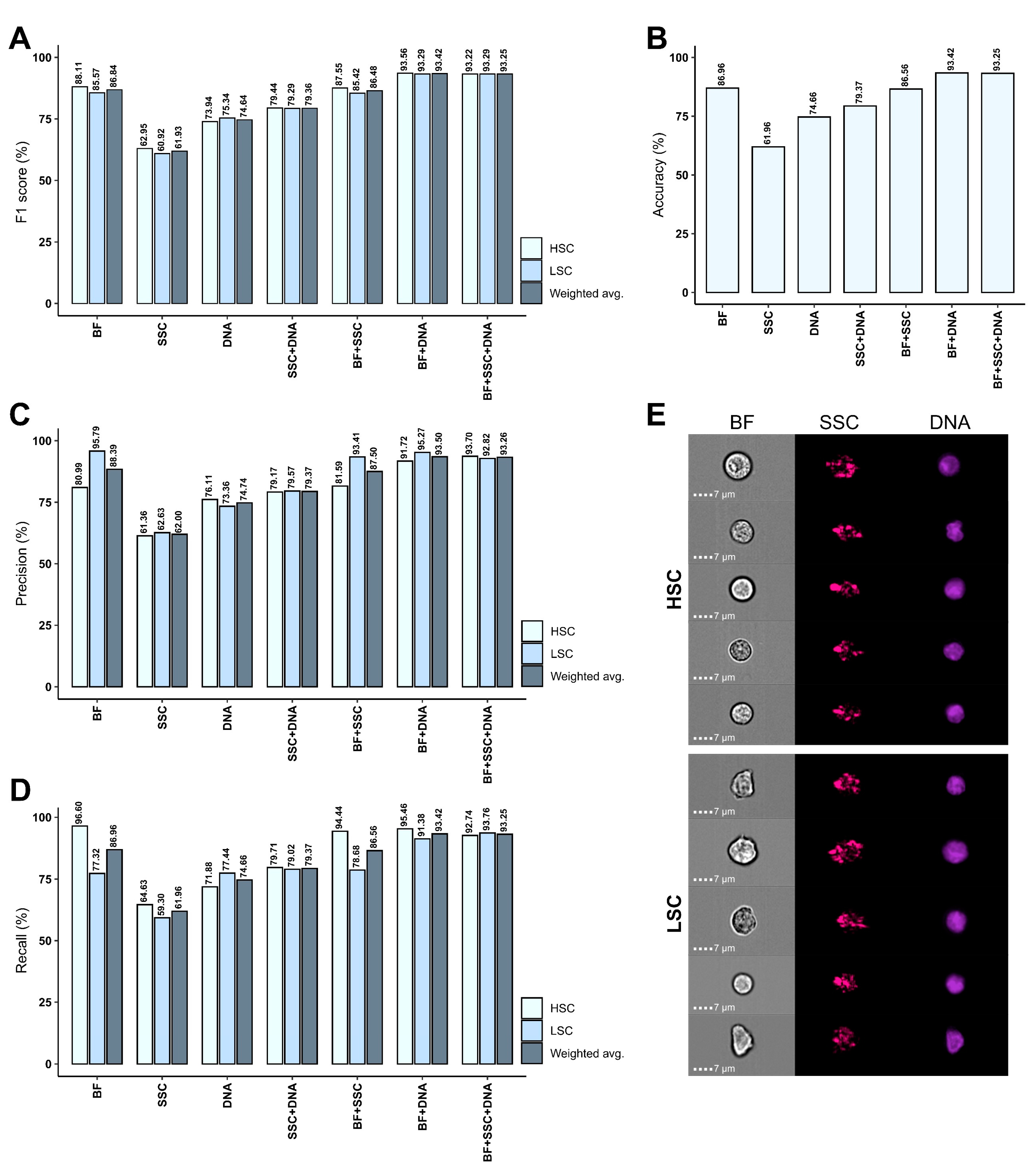
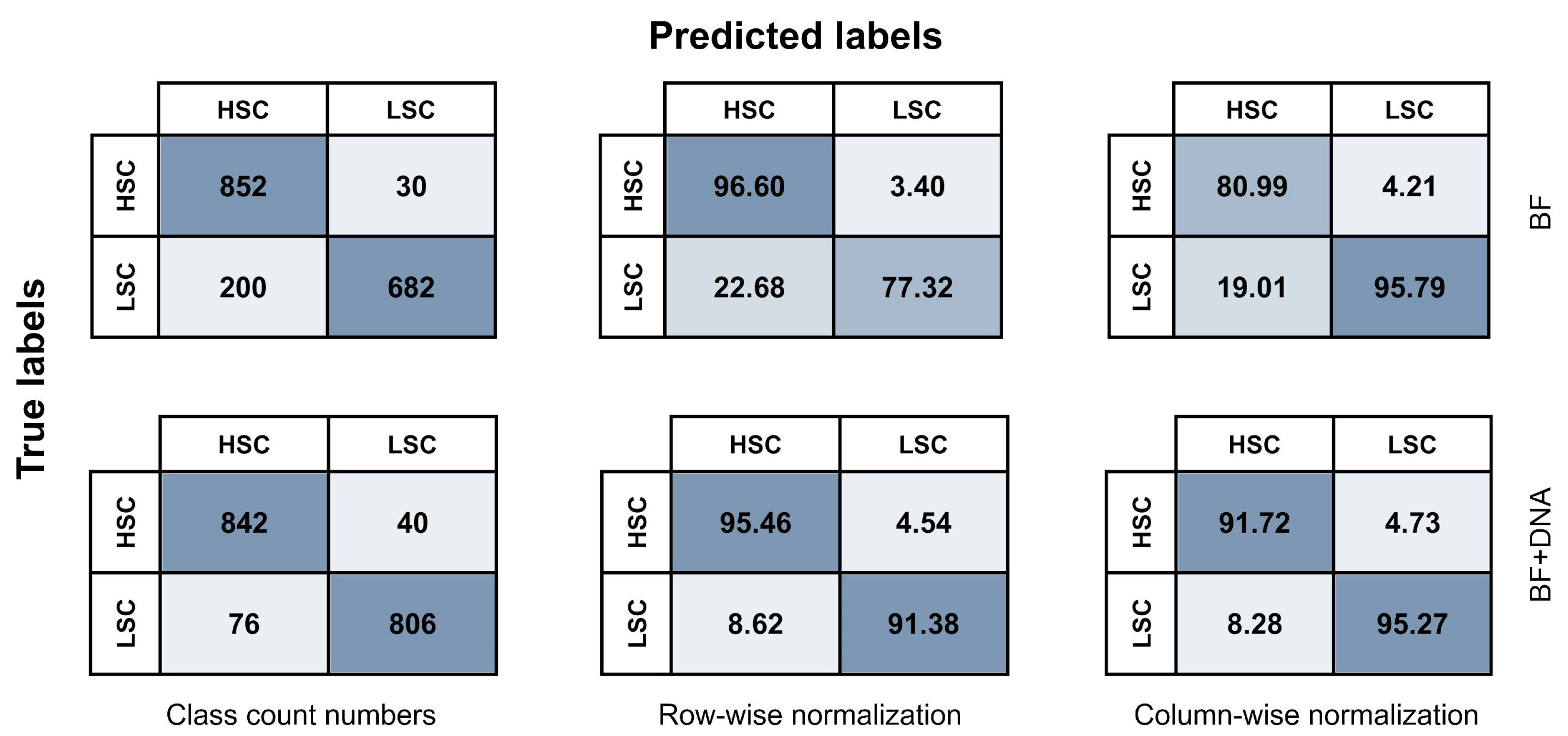
2.2. AI-Based Image Analysis Enables Accurate HSC-LSC Discrimination
2.3. Model Performance Varies Substantially between AML Patients
3. Discussion
4. Materials and Methods
4.1. Bone Marrow Samples
4.2. Sample Preparation
4.3. Staining Procedure
4.4. IFC Configuration and Acquisition
4.5. Gating of Healthy and Leukemic Stem Cell Populations
4.6. Data Partitioning and Class Balancing
4.7. CNN Model Development Using Amnis® AI
4.8. Patient-Specific LSC Classification
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jani, C.T.; Ahmed, A.; Singh, H.; Mouchati, C.; Al Omari, O.; Bhatt, P.S.; Sharma, R.; Farooq, M.; Liu, W.; Shalhoub, J.; et al. Burden of AML, 1990–2019: Estimates From the Global Burden of Disease Study. JCO Glob. Oncol. 2023, 9, e2300229. [Google Scholar] [CrossRef] [PubMed]
- van Gils, N.; Denkers, F.; Smit, L. Escape from Treatment; the Different Faces of Leukemic Stem Cells and Therapy Resistance in Acute Myeloid Leukemia. Front. Oncol. 2021, 11, 1454. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, F.; Yoshida, S.; Saito, Y.; Hijikata, A.; Kitamura, H.; Tanaka, S.; Nakamura, R.; Tanaka, T.; Tomiyama, H.; Saito, N.; et al. Chemotherapy-Resistant Human AML Stem Cells Home to and Engraft within the Bone-Marrow Endosteal Region. Nat. Biotechnol. 2007, 25, 1315–1321. [Google Scholar] [CrossRef] [PubMed]
- Terwijn, M.; Zeijlemaker, W.; Kelder, A.; Rutten, A.P.; Snel, A.N.; Scholten, W.J.; Pabst, T.; Verhoef, G.; Löwenberg, B.; Zweegman, S.; et al. Leukemic Stem Cell Frequency: A Strong Biomarker for Clinical Outcome in Acute Myeloid Leukemia. PLoS ONE 2014, 9, e107587. [Google Scholar] [CrossRef] [PubMed]
- Long, N.A.; Golla, U.; Sharma, A.; Claxton, D.F. Acute Myeloid Leukemia Stem Cells: Origin, Characteristics, and Clinical Implications. Stem Cell Rev. Rep. 2022, 18, 1211–1226. [Google Scholar] [CrossRef] [PubMed]
- De Kouchkovsky, I.; Abdul-Hay, M. Acute Myeloid Leukemia: A Comprehensive Review and 2016 Update. Blood Cancer J. 2016, 6, e441. [Google Scholar] [CrossRef] [PubMed]
- Pelcovits, A.; Niroula, R. Acute Myeloid Leukemia: A Review. R. I. Med. J. 2020, 103, 38–40. [Google Scholar]
- Newell, L.F.; Cook, R.J. Advances in Acute Myeloid Leukemia. BMJ 2021, 375, n2026. [Google Scholar] [CrossRef] [PubMed]
- Shimony, S.; Stahl, M.; Stone, R.M. Acute Myeloid Leukemia: 2023 Update on Diagnosis, Risk-Stratification, and Management. Am. J. Hematol. 2023, 98, 502–526. [Google Scholar] [CrossRef]
- Döhner, H.; Estey, E.; Grimwade, D.; Amadori, S.; Appelbaum, F.R.; Büchner, T.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Larson, R.A.; et al. Diagnosis and Management of AML in Adults: 2017 ELN Recommendations from an International Expert Panel. Blood 2017, 129, 424–447. [Google Scholar] [CrossRef]
- Döhner, H.; Estey, E.H.; Amadori, S.; Appelbaum, F.R.; Büchner, T.; Burnett, A.K.; Dombret, H.; Fenaux, P.; Grimwade, D.; Larson, R.A.; et al. Diagnosis and Management of Acute Myeloid Leukemia in Adults: Recommendations from an International Expert Panel, on Behalf of the European LeukemiaNet. Blood 2010, 115, 453–474. [Google Scholar] [CrossRef] [PubMed]
- Dombret, H.; Gardin, C. An Update of Current Treatments for Adult Acute Myeloid Leukemia. Blood 2016, 127, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Döhner, H.; Weisdorf, D.J.; Bloomfield, C.D. Acute Myeloid Leukemia. N. Engl. J. Med. 2015, 373, 1136–1152. [Google Scholar] [CrossRef] [PubMed]
- Bradbury, C.; Houlton, A.E.; Akiki, S.; Gregg, R.; Rindl, M.; Khan, J.; Ward, J.; Khan, N.; Griffiths, M.; Nagra, S.; et al. Prognostic Value of Monitoring a Candidate Immunophenotypic Leukaemic Stem/Progenitor Cell Population in Patients Allografted for Acute Myeloid Leukaemia. Leukemia 2015, 29, 988–991. [Google Scholar] [CrossRef] [PubMed]
- van Rhenen, A.; Moshaver, B.; Kelder, A.; Feller, N.; Nieuwint, A.W.M.; Zweegman, S.; Ossenkoppele, G.J.; Schuurhuis, G.J. Aberrant Marker Expression Patterns on the CD34+CD38- Stem Cell Compartment in Acute Myeloid Leukemia Allows to Distinguish the Malignant from the Normal Stem Cell Compartment Both at Diagnosis and in Remission. Leukemia 2007, 21, 1700–1707. [Google Scholar] [CrossRef] [PubMed]
- Döhner, H.; Wei, A.H.; Appelbaum, F.R.; Craddock, C.; DiNardo, C.D.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Godley, L.A.; Hasserjian, R.P.; et al. Diagnosis and Management of AML in Adults: 2022 Recommendations from an International Expert Panel on Behalf of the ELN. Blood 2022, 140, 1345–1377. [Google Scholar] [CrossRef] [PubMed]
- Grimwade, D.; Freeman, S.D. Defining Minimal Residual Disease in Acute Myeloid Leukemia: Which Platforms Are Ready for “Prime Time”? Blood 2014, 124, 3345–3355. [Google Scholar] [CrossRef] [PubMed]
- Schuurhuis, G.J.; Heuser, M.; Freeman, S.; Béné, M.-C.; Buccisano, F.; Cloos, J.; Grimwade, D.; Haferlach, T.; Hills, R.K.; Hourigan, C.S.; et al. Minimal/Measurable Residual Disease in AML: A Consensus Document from the European LeukemiaNet MRD Working Party. Blood 2018, 131, 1275–1291. [Google Scholar] [CrossRef] [PubMed]
- Blachly, J.S.; Walter, R.B.; Hourigan, C.S. The Present and Future of Measurable Residual Disease Testing in Acute Myeloid Leukemia. Haematologica 2022, 107, 2810–2822. [Google Scholar] [CrossRef]
- Canali, A.; Vergnolle, I.; Bertoli, S.; Largeaud, L.; Nicolau, M.-L.; Rieu, J.-B.; Tavitian, S.; Huguet, F.; Picard, M.; Bories, P.; et al. Prognostic Impact of Unsupervised Early Assessment of Bulk and Leukemic Stem Cell Measurable Residual Disease in Acute Myeloid Leukemia. Clin. Cancer Res. 2023, 29, 134–142. [Google Scholar] [CrossRef]
- Zeijlemaker, W.; Grob, T.; Meijer, R.; Hanekamp, D.; Kelder, A.; Carbaat-Ham, J.C.; Oussoren-Brockhoff, Y.J.M.; Snel, A.N.; Veldhuizen, D.; Scholten, W.J.; et al. CD34(+)CD38(−) Leukemic Stem Cell Frequency to Predict Outcome in Acute Myeloid Leukemia. Leukemia 2019, 33, 1102–1112. [Google Scholar] [CrossRef] [PubMed]
- Zeijlemaker, W.; Kelder, A.; Cloos, J.; Schuurhuis, G.J. Immunophenotypic Detection of Measurable Residual (Stem Cell) Disease Using LAIP Approach in Acute Myeloid Leukemia. Curr. Protoc. Cytom. 2019, 91, e66. [Google Scholar] [CrossRef] [PubMed]
- Jordan, C.T.; Upchurch, D.; Szilvassy, S.J.; Guzman, M.L.; Howard, D.S.; Pettigrew, A.L.; Meyerrose, T.; Rossi, R.; Grimes, B.; Rizzieri, D.A.; et al. The Interleukin-3 Receptor Alpha Chain Is a Unique Marker for Human Acute Myelogenous Leukemia Stem Cells. Leukemia 2000, 14, 1777–1784. [Google Scholar] [CrossRef] [PubMed]
- Haubner, S.; Perna, F.; Köhnke, T.; Schmidt, C.; Berman, S.; Augsberger, C.; Schnorfeil, F.M.; Krupka, C.; Lichtenegger, F.S.; Liu, X.; et al. Coexpression Profile of Leukemic Stem Cell Markers for Combinatorial Targeted Therapy in AML. Leukemia 2019, 33, 64–74. [Google Scholar] [CrossRef] [PubMed]
- van Rhenen, A.; van Dongen, G.A.M.S.; Kelder, A.; Rombouts, E.J.; Feller, N.; Moshaver, B.; Stigter-van Walsum, M.; Zweegman, S.; Ossenkoppele, G.J.; Jan Schuurhuis, G. The Novel AML Stem Cell Associated Antigen CLL-1 Aids in Discrimination between Normal and Leukemic Stem Cells. Blood 2007, 110, 2659–2666. [Google Scholar] [CrossRef] [PubMed]
- Lapidot, T.; Sirard, C.; Vormoor, J.; Murdoch, B.; Hoang, T.; Caceres-Cortes, J.; Minden, M.; Paterson, B.; Caligiuri, M.A.; Dick, J.E. A Cell Initiating Human Acute Myeloid Leukaemia after Transplantation into SCID Mice. Nature 1994, 367, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Bonnet, D.; Dick, J.E. Human Acute Myeloid Leukemia Is Organized as a Hierarchy That Originates from a Primitive Hematopoietic Cell. Nat. Med. 1997, 3, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Majeti, R. Biology and Relevance of Human Acute Myeloid Leukemia Stem Cells. Blood 2017, 129, 1577–1585. [Google Scholar] [CrossRef] [PubMed]
- Petersen, M.A.; Rosenberg, C.A.; Brøndum, R.F.; Aggerholm, A.; Kjeldsen, E.; Rahbek, O.; Ludvigsen, M.; Hasle, H.; Roug, A.S.; Bill, M. Immunophenotypically Defined Stem Cell Subsets in Paediatric AML Are Highly Heterogeneous and Demonstrate Differences in BCL-2 Expression by Cytogenetic Subgroups. Br. J. Haematol. 2022, 197, 452–466. [Google Scholar] [CrossRef] [PubMed]
- Petersen, M.A.; Bill, M.; Rosenberg, C.A. OMIP 072: A 15-Color Panel for Immunophenotypic Identification, Quantification, and Characterization of Leukemic Stem Cells in Children with Acute Myeloid Leukemia. Cytom. Part A J. Int. Soc. Anal. Cytol. 2021, 99, 382–387. [Google Scholar] [CrossRef]
- Bill, M.; Aggerholm, A.; Kjeldsen, E.; Roug, A.S.; Hokland, P.; Nederby, L. Revisiting CLEC12A as Leukaemic Stem Cell Marker in AML: Highlighting the Necessity of Precision Diagnostics in Patients Eligible for Targeted Therapy. Br. J. Haematol. 2019, 184, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Bill, M.; van Kooten Niekerk, P.B.; Woll, P.S.; Laine Herborg, L.; Stidsholt Roug, A.; Hokland, P.; Nederby, L. Mapping the CLEC12A Expression on Myeloid Progenitors in Normal Bone Marrow; Implications for Understanding CLEC12A-Related Cancer Stem Cell Biology. J. Cell. Mol. Med. 2018, 22, 2311–2318. [Google Scholar] [CrossRef] [PubMed]
- Arnone, M.; Konantz, M.; Hanns, P.; Paczulla Stanger, A.M.; Bertels, S.; Godavarthy, P.S.; Christopeit, M.; Lengerke, C. Acute Myeloid Leukemia Stem Cells: The Challenges of Phenotypic Heterogeneity. Cancers 2020, 12, 3742. [Google Scholar] [CrossRef]
- Han, Y.; Gu, Y.; Zhang, A.C.; Lo, Y.-H. Review: Imaging Technologies for Flow Cytometry. Lab Chip 2016, 16, 4639–4647. [Google Scholar] [CrossRef] [PubMed]
- Doan, M.; Vorobjev, I.; Rees, P.; Filby, A.; Wolkenhauer, O.; Goldfeld, A.E.; Lieberman, J.; Barteneva, N.; Carpenter, A.E.; Hennig, H. Diagnostic Potential of Imaging Flow Cytometry. Trends Biotechnol. 2018, 36, 649–652. [Google Scholar] [CrossRef]
- Basiji, D.A. Principles of Amnis Imaging Flow Cytometry. Methods Mol. Biol. 2016, 1389, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Nassar, M.; Doan, M.; Filby, A.; Wolkenhauer, O.; Fogg, D.K.; Piasecka, J.; Thornton, C.A.; Carpenter, A.E.; Summers, H.D.; Rees, P.; et al. Label-Free Identification of White Blood Cells Using Machine Learning. Cytom. Part A 2019, 95, 836–842. [Google Scholar] [CrossRef] [PubMed]
- Doan, M.; Carpenter, A.E. Leveraging Machine Vision in Cell-Based Diagnostics to Do More with Less. Nat. Mater. 2019, 18, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Doan, M.; Case, M.; Masic, D.; Hennig, H.; McQuin, C.; Caicedo, J.; Singh, S.; Goodman, A.; Wolkenhauer, O.; Summers, H.D.; et al. Label-Free Leukemia Monitoring by Computer Vision. Cytom. Part A 2020, 97, 407–414. [Google Scholar] [CrossRef]
- Shapiro, H.M. Practical Flow Cytometry; John Wiley & Sons: Hoboken, NJ, USA, 2003; ISBN 0471434035. [Google Scholar]
- Kumar, C.C. Genetic Abnormalities and Challenges in the Treatment of Acute Myeloid Leukemia. Genes Cancer 2011, 2, 95–107. [Google Scholar] [CrossRef]
- Telford, W.G.; Bradford, J.; Godfrey, W.; Robey, R.W.; Bates, S.E. Side Population Analysis Using a Violet-Excited Cell-Permeable DNA Binding Dye. Stem Cells 2007, 25, 1029–1036. [Google Scholar] [CrossRef]
- Moshaver, B.; Wouters, R.F.; Kelder, A.; Ossenkoppele, G.J.; Westra, G.A.H.; Kwidama, Z.; Rutten, A.R.; Kaspers, G.J.L.; Zweegman, S.; Cloos, J.; et al. Relationship between CD34/CD38 and Side Population (SP) Defined Leukemia Stem Cell Compartments in Acute Myeloid Leukemia. Leuk. Res. 2019, 81, 27–34. [Google Scholar] [CrossRef]
- Bakker, A.B.H.; van den Oudenrijn, S.; Bakker, A.Q.; Feller, N.; van Meijer, M.; Bia, J.A.; Jongeneelen, M.A.C.; Visser, T.J.; Bijl, N.; Geuijen, C.A.W.; et al. C-Type Lectin-like Molecule-1: A Novel Myeloid Cell Surface Marker Associated with Acute Myeloid Leukemia. Cancer Res. 2004, 64, 8443–8450. [Google Scholar] [CrossRef]
- Galera, P.K.; Jiang, C.; Braylan, R. Immunophenotyping of Acute Myeloid Leukemia. Methods Mol. Biol. 2019, 2032, 281–296. [Google Scholar] [CrossRef] [PubMed]
- Matek, C.; Schwarz, S.; Spiekermann, K.; Marr, C. Human-Level Recognition of Blast Cells in Acute Myeloid Leukaemia with Convolutional Neural Networks. Nat. Mach. Intell. 2019, 1, 538–544. [Google Scholar] [CrossRef]
- Berenson, R.J.; Andrews, R.G.; Bensinger, W.I.; Kalamasz, D.; Knitter, G.; Buckner, C.D.; Bernstein, I.D. Antigen CD34+ Marrow Cells Engraft Lethally Irradiated Baboons. J. Clin. Investig. 1988, 81, 951–955. [Google Scholar] [CrossRef] [PubMed]
- Engelhardt, M.; Lübbert, M.; Guo, Y. CD34+ or CD34−: Which Is the More Primitive? Leukemia 2002, 16, 1603–1608. [Google Scholar] [CrossRef]
- Hao, Q.L.; Thiemann, F.T.; Petersen, D.; Smogorzewska, E.M.; Crooks, G.M. Extended Long-Term Culture Reveals a Highly Quiescent and Primitive Human Hematopoietic Progenitor Population. Blood 1996, 88, 3306–3313. [Google Scholar] [CrossRef]
- Huang, S.; Terstappen, L.W. Lymphoid and Myeloid Differentiation of Single Human CD34+, HLA-DR+, CD38- Hematopoietic Stem Cells. Blood 1994, 83, 1515–1526. [Google Scholar] [CrossRef]
- Miller, J.S.; McCullar, V.; Punzel, M.; Lemischka, I.R.; Moore, K.A. Single Adult Human CD34(+)/Lin-/CD38(-) Progenitors Give Rise to Natural Killer Cells, B-Lineage Cells, Dendritic Cells, and Myeloid Cells. Blood 1999, 93, 96–106. [Google Scholar] [CrossRef]
- Petzer, A.L.; Hogge, D.E.; Landsdorp, P.M.; Reid, D.S.; Eaves, C.J. Self-Renewal of Primitive Human Hematopoietic Cells (Long-Term-Culture-Initiating Cells) in Vitro and Their Expansion in Defined Medium. Proc. Natl. Acad. Sci. USA 1996, 93, 1470–1474. [Google Scholar] [CrossRef] [PubMed]
- Terstappen, L.W.; Huang, S.; Safford, M.; Lansdorp, P.M.; Loken, M.R. Sequential Generations of Hematopoietic Colonies Derived from Single Nonlineage-Committed CD34+CD38- Progenitor Cells. Blood 1991, 77, 1218–1227. [Google Scholar] [CrossRef] [PubMed]
- Seita, J.; Weissman, I.L. Hematopoietic Stem Cell: Self-Renewal versus Differentiation. Wiley Interdiscip. Rev. Syst. Biol. Med. 2010, 2, 640–653. [Google Scholar] [CrossRef] [PubMed]
- Hanekamp, D.; Snel, A.N.; Kelder, A.; Scholten, W.J.; Khan, N.; Metzner, M.; Irno-Consalvo, M.; Sugita, M.; de Jong, A.; Oude Alink, S.; et al. Applicability and Reproducibility of Acute Myeloid Leukaemia Stem Cell Assessment in a Multi-Centre Setting. Br. J. Haematol. 2020, 190, 891–900. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.W.K.; Mitchell, A.; Kennedy, J.A.; Chen, W.C.; McLeod, J.; Ibrahimova, N.; Arruda, A.; Popescu, A.; Gupta, V.; Schimmer, A.D.; et al. A 17-Gene Stemness Score for Rapid Determination of Risk in Acute Leukaemia. Nature 2016, 540, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Eppert, K.; Takenaka, K.; Lechman, E.R.; Waldron, L.; Nilsson, B.; van Galen, P.; Metzeler, K.H.; Poeppl, A.; Ling, V.; Beyene, J.; et al. Stem Cell Gene Expression Programs Influence Clinical Outcome in Human Leukemia. Nat. Med. 2011, 17, 1086–1093. [Google Scholar] [CrossRef] [PubMed]
- Taussig, D.C.; Vargaftig, J.; Miraki-Moud, F.; Griessinger, E.; Sharrock, K.; Luke, T.; Lillington, D.; Oakervee, H.; Cavenagh, J.; Agrawal, S.G.; et al. Leukemia-Initiating Cells from Some Acute Myeloid Leukemia Patients with Mutated Nucleophosmin Reside in the CD34(-) Fraction. Blood 2010, 115, 1976–1984. [Google Scholar] [CrossRef] [PubMed]
- Sarry, J.-E.; Murphy, K.; Perry, R.; Sanchez, P.V.; Secreto, A.; Keefer, C.; Swider, C.R.; Strzelecki, A.-C.; Cavelier, C.; Récher, C.; et al. Human Acute Myelogenous Leukemia Stem Cells Are Rare and Heterogeneous When Assayed in NOD/SCID/IL2Rγc-Deficient Mice. J. Clin. Investig. 2011, 121, 384–395. [Google Scholar] [CrossRef] [PubMed]
- Goardon, N.; Marchi, E.; Atzberger, A.; Quek, L.; Schuh, A.; Soneji, S.; Woll, P.; Mead, A.; Alford, K.A.; Rout, R.; et al. Coexistence of LMPP-like and GMP-like Leukemia Stem Cells in Acute Myeloid Leukemia. Cancer Cell 2011, 19, 138–152. [Google Scholar] [CrossRef] [PubMed]
- Quek, L.; Otto, G.W.; Garnett, C.; Lhermitte, L.; Karamitros, D.; Stoilova, B.; Lau, I.-J.; Doondeea, J.; Usukhbayar, B.; Kennedy, A.; et al. Genetically Distinct Leukemic Stem Cells in Human CD34- Acute Myeloid Leukemia Are Arrested at a Hemopoietic Precursor-like Stage. J. Exp. Med. 2016, 213, 1513–1535. [Google Scholar] [CrossRef]
- Ho, T.-C.; LaMere, M.; Stevens, B.M.; Ashton, J.M.; Myers, J.R.; O’Dwyer, K.M.; Liesveld, J.L.; Mendler, J.H.; Guzman, M.; Morrissette, J.D.; et al. Evolution of Acute Myelogenous Leukemia Stem Cell Properties after Treatment and Progression. Blood 2016, 128, 1671–1678. [Google Scholar] [CrossRef] [PubMed]
- Zeijlemaker, W.; Kelder, A.; Oussoren-Brockhoff, Y.J.M.; Scholten, W.J.; Snel, A.N.; Veldhuizen, D.; Cloos, J.; Ossenkoppele, G.J.; Schuurhuis, G.J. A Simple One-Tube Assay for Immunophenotypical Quantification of Leukemic Stem Cells in Acute Myeloid Leukemia. Leukemia 2016, 30, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Salek, M.; Li, N.; Chou, H.-P.; Saini, K.; Jovic, A.; Jacobs, K.B.; Johnson, C.; Lu, V.; Lee, E.J.; Chang, C.; et al. COSMOS: A Platform for Real-Time Morphology-Based, Label-Free Cell Sorting Using Deep Learning. Commun. Biol. 2023, 6, 971. [Google Scholar] [CrossRef]
- Ota, S.; Horisaki, R.; Kawamura, Y.; Ugawa, M.; Sato, I.; Hashimoto, K.; Kamesawa, R.; Setoyama, K.; Yamaguchi, S.; Fujiu, K.; et al. Ghost Cytometry. Science 2018, 360, 1246–1251. [Google Scholar] [CrossRef]
- Ng, D.P.; Simonson, P.D.; Tarnok, A.; Lucas, F.; Kern, W.; Rolf, N.; Bogdanoski, G.; Green, C.; Brinkman, R.R.; Czechowska, K. Recommendations for Using Artificial Intelligence in Clinical Flow Cytometry. Cytom. Part B Clin. Cytom. 2024, in press. [Google Scholar] [CrossRef]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R. An Introduction to Statistical Learning; Springer: New York, NY, USA, 2021. [Google Scholar]
- Rodrigues, M.A.; Probst, C.E.; Zayats, A.; Davidson, B.; Riedel, M.; Li, Y.; Venkatachalam, V. The in Vitro Micronucleus Assay Using Imaging Flow Cytometry and Deep Learning. NPJ Syst. Biol. Appl. 2021, 7, 20. [Google Scholar] [CrossRef]
- Stirling, D.R.; Swain-Bowden, M.J.; Lucas, A.M.; Carpenter, A.E.; Cimini, B.A.; Goodman, A. CellProfiler 4: Improvements in Speed, Utility and Usability. BMC Bioinform. 2021, 22, 433. [Google Scholar] [CrossRef] [PubMed]
- Hennig, H.; Rees, P.; Blasi, T.; Kamentsky, L.; Hung, J.; Dao, D.; Carpenter, A.E.; Filby, A. An Open-Source Solution for Advanced Imaging Flow Cytometry Data Analysis Using Machine Learning. Methods 2017, 112, 201–210. [Google Scholar] [CrossRef]
- Eulenberg, P.; Köhler, N.; Blasi, T.; Filby, A.; Carpenter, A.E.; Rees, P.; Theis, F.J.; Wolf, F.A. Reconstructing Cell Cycle and Disease Progression Using Deep Learning. Nat. Commun. 2017, 8, 463. [Google Scholar] [CrossRef] [PubMed]
- Doan, M.; Barnes, C.; McQuin, C.; Caicedo, J.C.; Goodman, A.; Carpenter, A.E.; Rees, P. Deepometry, a Framework for Applying Supervised and Weakly Supervised Deep Learning to Imaging Cytometry. Nat. Protoc. 2021, 16, 3572–3595. [Google Scholar] [CrossRef]
- Hui, H.; Fuller, K.A.; Erber, W.N.; Linden, M.D. Imaging Flow Cytometry in the Assessment of Leukocyte-Platelet Aggregates. Methods 2017, 112, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Doan, M.; Sebastian, J.A.; Caicedo, J.C.; Siegert, S.; Roch, A.; Turner, T.R.; Mykhailova, O.; Pinto, R.N.; McQuin, C.; Goodman, A.; et al. Objective Assessment of Stored Blood Quality by Deep Learning. Proc. Natl. Acad. Sci. USA 2020, 117, 21381–21390. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, C.A.; Bill, M.; Rodrigues, M.A.; Hauerslev, M.; Kerndrup, G.B.; Hokland, P.; Ludvigsen, M. Exploring Dyserythropoiesis in Patients with Myelodyspla Stic Syndrome by Imaging Flow Cytometry and Machine-Learning Assisted Morphometrics. Clin. Cytom. Part B 2020, 100, 554–567. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, C.A.; Rodrigues, M.A.; Bill, M.; Ludvigsen, M. Comparative Analysis of Feature-Based ML and CNN for Binucleated Erythroblast Quantification in Myelodysplastic Syndrome Patients Using Imaging Flow Cytometry Data. Sci. Rep. 2024, 14, 9349. [Google Scholar] [CrossRef] [PubMed]
- Andersen, M.N.; Al-Karradi, S.N.H.; Kragstrup, T.W.; Hokland, M. Elimination of Erroneous Results in Flow Cytometry Caused by Antibody Binding to Fc Receptors on Human Monocytes and Macrophages. Cytom. Part A J. Int. Soc. Anal. Cytol. 2016, 89, 1001–1009. [Google Scholar] [CrossRef] [PubMed]
- Probst, C.; Zayats, A.; Venkatachalam, V.; Davidson, B. Advanced Characterization of Silicone Oil Droplets in Protein Therapeutics Using Artificial Intelligence Analysis of Imaging Flow Cytometry Data. J. Pharm. Sci. 2020, 109, 2996–3005. [Google Scholar] [CrossRef] [PubMed]
- Abadi, M.; Agarwal, A.; Barham, P.; Brevdo, E.; Chen, Z.; Citro, C.; Corrado, G.S.; Davis, A.; Dean, J.; Devin, M. Tensorflow: Large-Scale Machine Learning on Heterogeneous Distributed Systems. arXiv 2016, arXiv:1603.04467. [Google Scholar]
- Simonyan, K.; Zisserman, A. Very Deep Convolutional Networks for Large-Scale Image Recognition. arXiv 2014, arXiv:1409.1556. [Google Scholar]


| Model Class | Training Data | Validation Data | Testing Data | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Objects (n) | Precision (%) | Recall (%) | F1 (%) | Objects (n) | Precision (%) | Recall (%) | F1 (%) | Objects (n) | Precision (%) | Recall (%) | F1 (%) | |
| BF | ||||||||||||
| HSC | 7054 | 80.84 | 97.33 | 88.33 | 882 | 81.11 | 97.85 | 88.69 | 882 | 80.99 | 96.60 | 88.11 |
| LSC | 7054 | 96.65 | 76.94 | 85.67 | 882 | 97.29 | 77.21 | 86.09 | 882 | 95.79 | 77.32 | 85.57 |
| Weighted avg. | 14,108 | 88.75 | 87.13 | 87.00 | 1764 | 89.20 | 87.53 | 87.39 | 1764 | 88.39 | 86.96 | 86.84 |
| SSC | ||||||||||||
| HSC | 7054 | 61.58 | 64.66 | 63.08 | 882 | 61.42 | 65.87 | 63.57 | 882 | 61.36 | 64.63 | 62.95 |
| LSC | 7054 | 62.80 | 59.65 | 61.19 | 882 | 63.20 | 58.62 | 60.82 | 882 | 62.63 | 59.30 | 60.92 |
| Weighted avg. | 14,108 | 62.19 | 62.16 | 62.13 | 1764 | 62.31 | 62.24 | 62.20 | 1764 | 62.00 | 61.96 | 61.93 |
| DNA | ||||||||||||
| HSC | 7054 | 78.77 | 75.28 | 76.98 | 882 | 76.04 | 74.83 | 75.43 | 882 | 76.11 | 71.88 | 73.94 |
| LSC | 7054 | 76.33 | 79.71 | 77.98 | 882 | 75.22 | 76.42 | 75.82 | 882 | 73.36 | 77.44 | 75.34 |
| Weighted avg. | 14,108 | 77.55 | 77.50 | 77.48 | 1764 | 75.63 | 75.62 | 75.62 | 1764 | 74.74 | 74.66 | 74.64 |
| SSC + DNA | ||||||||||||
| HSC | 7054 | 80.84 | 82.04 | 81.43 | 882 | 78.42 | 81.97 | 80.16 | 882 | 79.17 | 79.71 | 79.44 |
| LSC | 7054 | 81.77 | 80.55 | 81.15 | 882 | 81.12 | 77.44 | 79.23 | 882 | 79.57 | 79.02 | 79.29 |
| Weighted avg. | 14,108 | 81.30 | 81.29 | 81.29 | 1764 | 79.77 | 79.71 | 79.69 | 1764 | 79.37 | 79.37 | 79.36 |
| BF + SSC | ||||||||||||
| HSC | 7054 | 81.87 | 95.11 | 87.99 | 882 | 82.43 | 95.24 | 88.37 | 882 | 81.59 | 94.44 | 87.55 |
| LSC | 7054 | 94.17 | 78.93 | 85.88 | 882 | 94.36 | 79.71 | 86.42 | 882 | 93.41 | 78.68 | 85.42 |
| Weighted avg. | 14,108 | 88.02 | 87.02 | 86.94 | 1764 | 88.40 | 87.47 | 87.40 | 1764 | 87.50 | 86.56 | 86.48 |
| BF + DNA | ||||||||||||
| HSC | 7054 | 93.41 | 96.31 | 94.84 | 882 | 94.14 | 96.49 | 95.30 | 882 | 91.72 | 95.46 | 93.56 |
| LSC | 7054 | 96.20 | 93.21 | 94.68 | 882 | 96.40 | 93.99 | 95.18 | 882 | 95.27 | 91.38 | 93.29 |
| Weighted avg. | 14,108 | 94.81 | 94.76 | 94.76 | 1764 | 95.27 | 95.24 | 95.24 | 1764 | 93.50 | 93.42 | 93.42 |
| BF + SSC + DNA | ||||||||||||
| HSC | 7054 | 94.88 | 94.78 | 94.83 | 882 | 95.24 | 95.24 | 95.24 | 882 | 93.70 | 92.74 | 93.22 |
| LSC | 7054 | 94.79 | 94.88 | 94.84 | 882 | 95.24 | 95.24 | 95.24 | 882 | 92.82 | 93.76 | 93.29 |
| Weighted avg. | 14,108 | 94.83 | 94.83 | 94.83 | 1764 | 95.24 | 95.24 | 95.24 | 1764 | 93.26 | 93.25 | 93.25 |
| Patient No. | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Age at diagnosis | 67 | 71 | 69 | 63 | 56 |
| Gender | M | M | M | F | F |
| Blast percentage * | 68% | 20% | 62% | 94% | 49% |
| Percentage of CLEC12A+ LSCs † | 30.42% | 1.73% | 0.09% | 4.17% | 0.09% |
| Karyotype ‡ | 46,XY [25] | Complex karyotype | 46,XY,add(1)(q31) [4]/46,XY [21] | 46,XX [25] | 46,XX,inv(16)(p13q22) [23]/46,XX [2] |
| iFISH § | No clonal aberrations | del(5q)(80%), del(7q)(72%), monosomi16 (78%) | ND | inv(16)(76%) | inv(16)(68%) |
| Immunophenotype | CD45lowCD34+ CD117+CD13+ CD33−HLA-DR+ CD14−CD64− CD38−/(+)CLEC12A+CD123+CD7− CD19−CD10− | CD45lowCD34+ CD117+CD38+/−CD13+HLA-DR+ CD33+CLEC12A+/− CD123(+)CD38+/− | CD45lowCD117+/−CD13+HLA-DR+ CD33(+)CD56+ CD38+CD7−CD19−CLEC12A+CD123+/− | CD45lowCD34+ CD117+HLA-DR+ CD13+CD33+ CD123+CLEC12A+ CD64−CD38+/− | CD34+CD117+ CD13+CD33+ HLA-DR+CD38+ CD64+CLEC12A+ CD123+CD14−CD4−CD56− CD2+/− |
| FLT3-ITD | No mutation | No mutation | Mutation | No mutation | No mutation |
| Targeted panel sequencing | ASXL1, CEBPA(x3), NRAS(x2), SRSF2, TET2(x2) | TP53 | ASXL1, EZH2(x2), FLT3(ITDx2, TKDx1), RUNX1, SETBP1 | ASXL1, FLT3 (TKDx2) | No mutations |
| NBM | No. HSCs | AML | No. LSCs |
|---|---|---|---|
| NBM1 | 1543 | AML1 | 1840 |
| NBM2 | 547 | ||
| NBM3 | 299 | AML2 | 1840 |
| NBM4 | 1393 | ||
| NBM5 | 522 | AML3 | 1839 |
| NBM6 | 1285 | ||
| NBM7 | 96 | AML4 | 1840 |
| NBM8 | 584 | ||
| NBM9 | 861 | AML5 | 1459 |
| NBM10 | 1688 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hybel, T.E.; Jensen, S.H.; Rodrigues, M.A.; Hybel, T.E.; Pedersen, M.N.; Qvick, S.H.; Enemark, M.H.; Bill, M.; Rosenberg, C.A.; Ludvigsen, M. Imaging Flow Cytometry and Convolutional Neural Network-Based Classification Enable Discrimination of Hematopoietic and Leukemic Stem Cells in Acute Myeloid Leukemia. Int. J. Mol. Sci. 2024, 25, 6465. https://doi.org/10.3390/ijms25126465
Hybel TE, Jensen SH, Rodrigues MA, Hybel TE, Pedersen MN, Qvick SH, Enemark MH, Bill M, Rosenberg CA, Ludvigsen M. Imaging Flow Cytometry and Convolutional Neural Network-Based Classification Enable Discrimination of Hematopoietic and Leukemic Stem Cells in Acute Myeloid Leukemia. International Journal of Molecular Sciences. 2024; 25(12):6465. https://doi.org/10.3390/ijms25126465
Chicago/Turabian StyleHybel, Trine Engelbrecht, Sofie Hesselberg Jensen, Matthew A. Rodrigues, Thomas Engelbrecht Hybel, Maya Nautrup Pedersen, Signe Håkansson Qvick, Marie Hairing Enemark, Marie Bill, Carina Agerbo Rosenberg, and Maja Ludvigsen. 2024. "Imaging Flow Cytometry and Convolutional Neural Network-Based Classification Enable Discrimination of Hematopoietic and Leukemic Stem Cells in Acute Myeloid Leukemia" International Journal of Molecular Sciences 25, no. 12: 6465. https://doi.org/10.3390/ijms25126465
APA StyleHybel, T. E., Jensen, S. H., Rodrigues, M. A., Hybel, T. E., Pedersen, M. N., Qvick, S. H., Enemark, M. H., Bill, M., Rosenberg, C. A., & Ludvigsen, M. (2024). Imaging Flow Cytometry and Convolutional Neural Network-Based Classification Enable Discrimination of Hematopoietic and Leukemic Stem Cells in Acute Myeloid Leukemia. International Journal of Molecular Sciences, 25(12), 6465. https://doi.org/10.3390/ijms25126465






