Intestinal Epithelial Creatine Transporter SLC6A8 Dysregulation in Inflammation and in Response to Adherent Invasive E. coli Infection
Abstract
:1. Introduction
2. Results
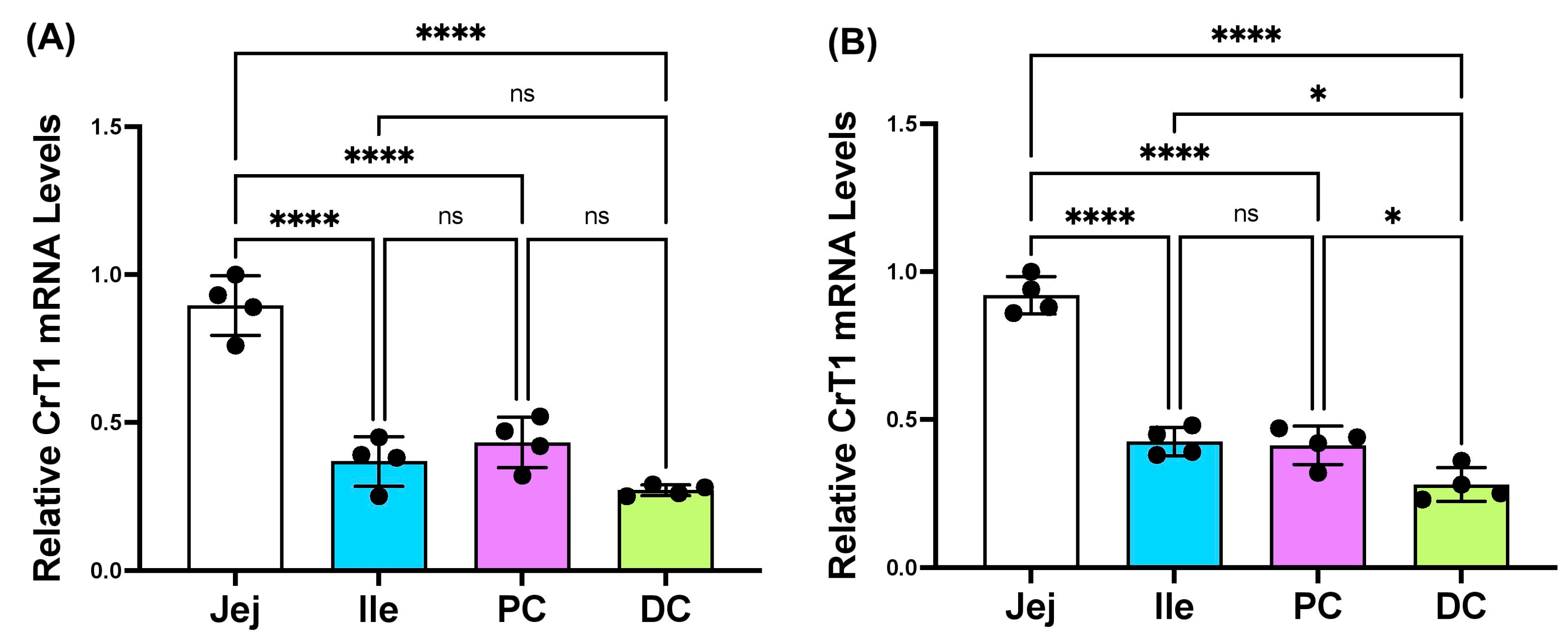
2.1. mRNA and Protein Levels of CrT1 along the Length of Rat, Mouse, and Human Intestines
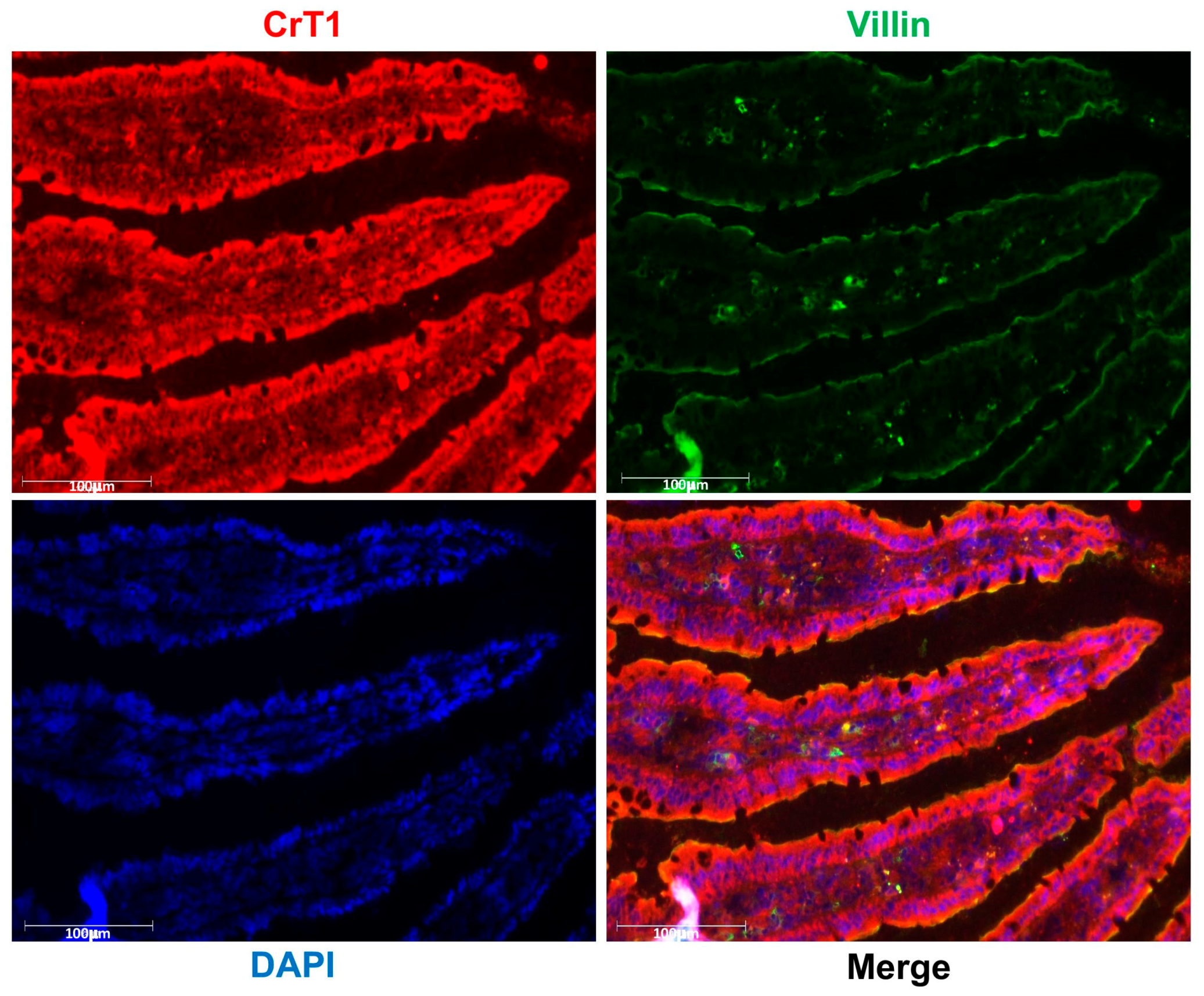
2.2. CrT1 Is Predominantly Localized on the Luminal Surface of Enterocytes
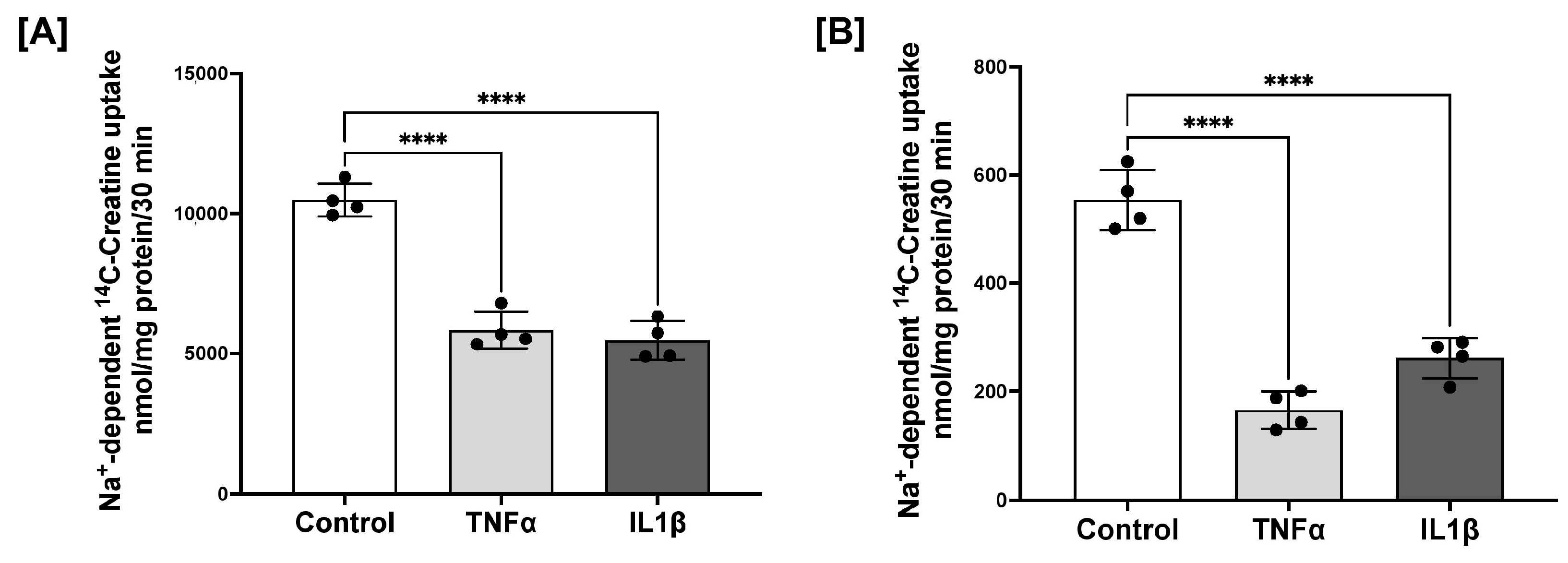
2.3. CrT1 Function and Expression Are Decreased in Inflammation
2.4. TNFα and IL1β Treatments Decrease CrT1 Promoter Activity in Caco-2 Cells
2.5. CrT1 Expression Is Decreased In Vivo in Ileitis
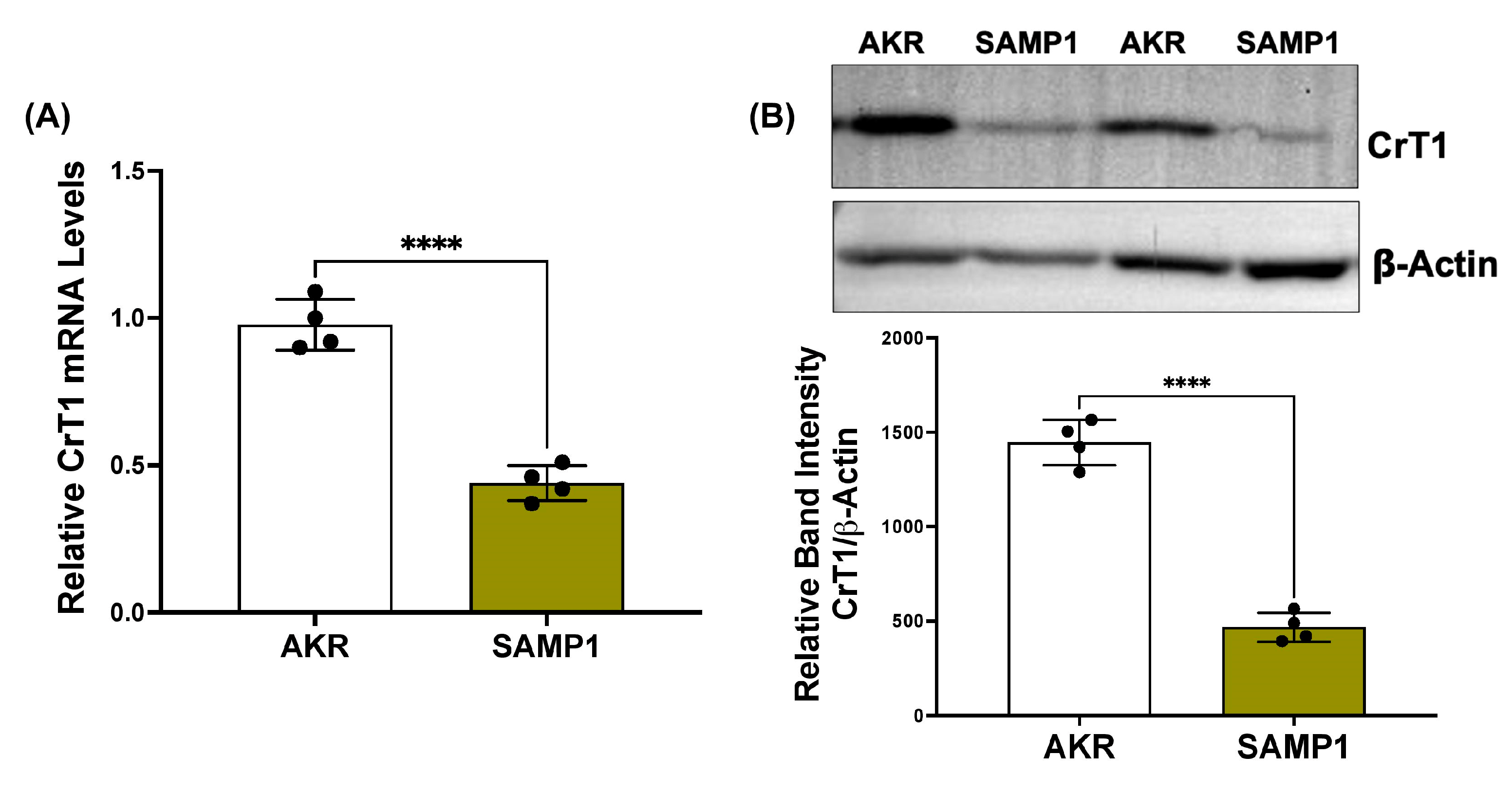
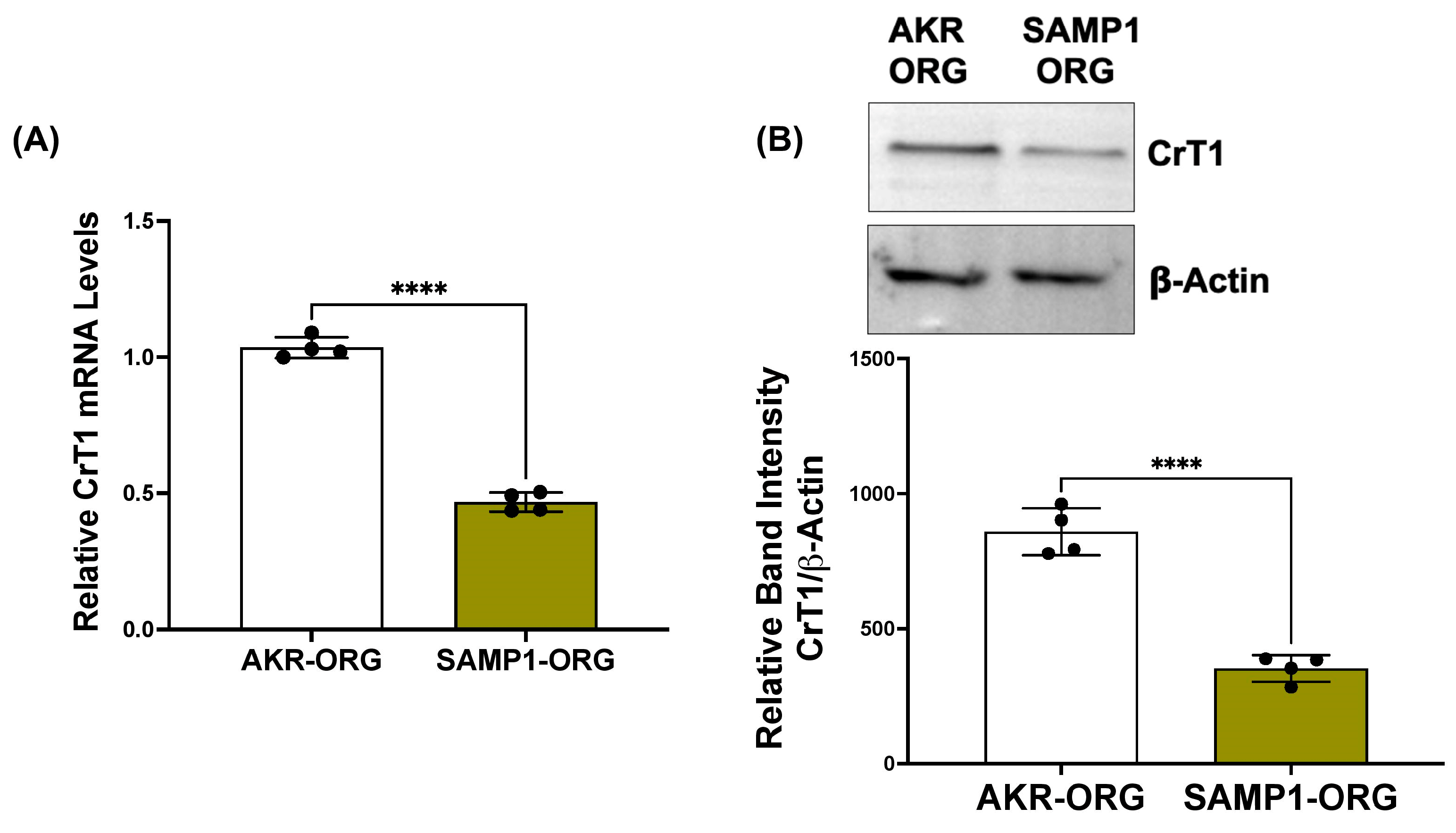
2.6. CrT1 Expression Is Decreased in SAMP1 Small Intestinal Organoids Compared to AKR Organoids
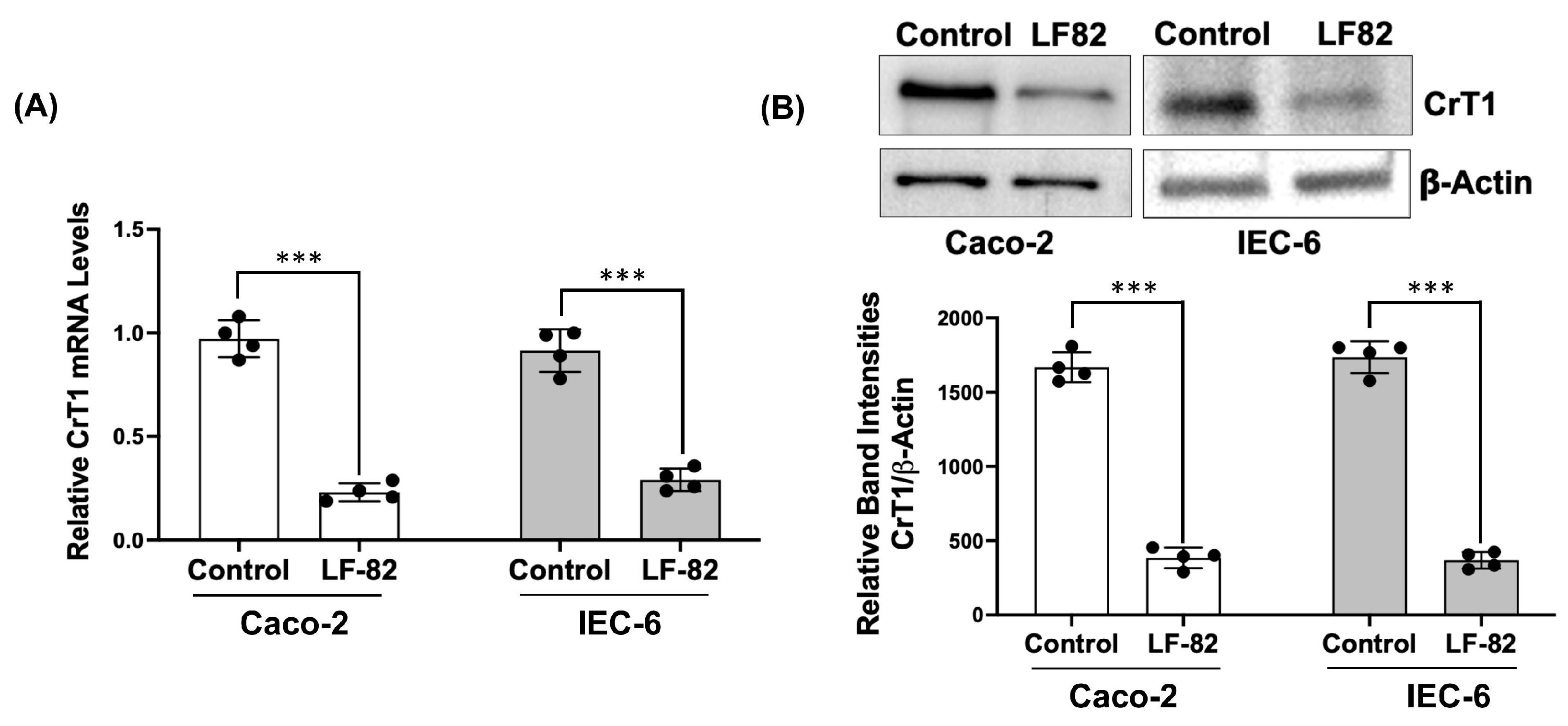
2.7. AIEC Infection Decreases CrT1 Expression In Vitro
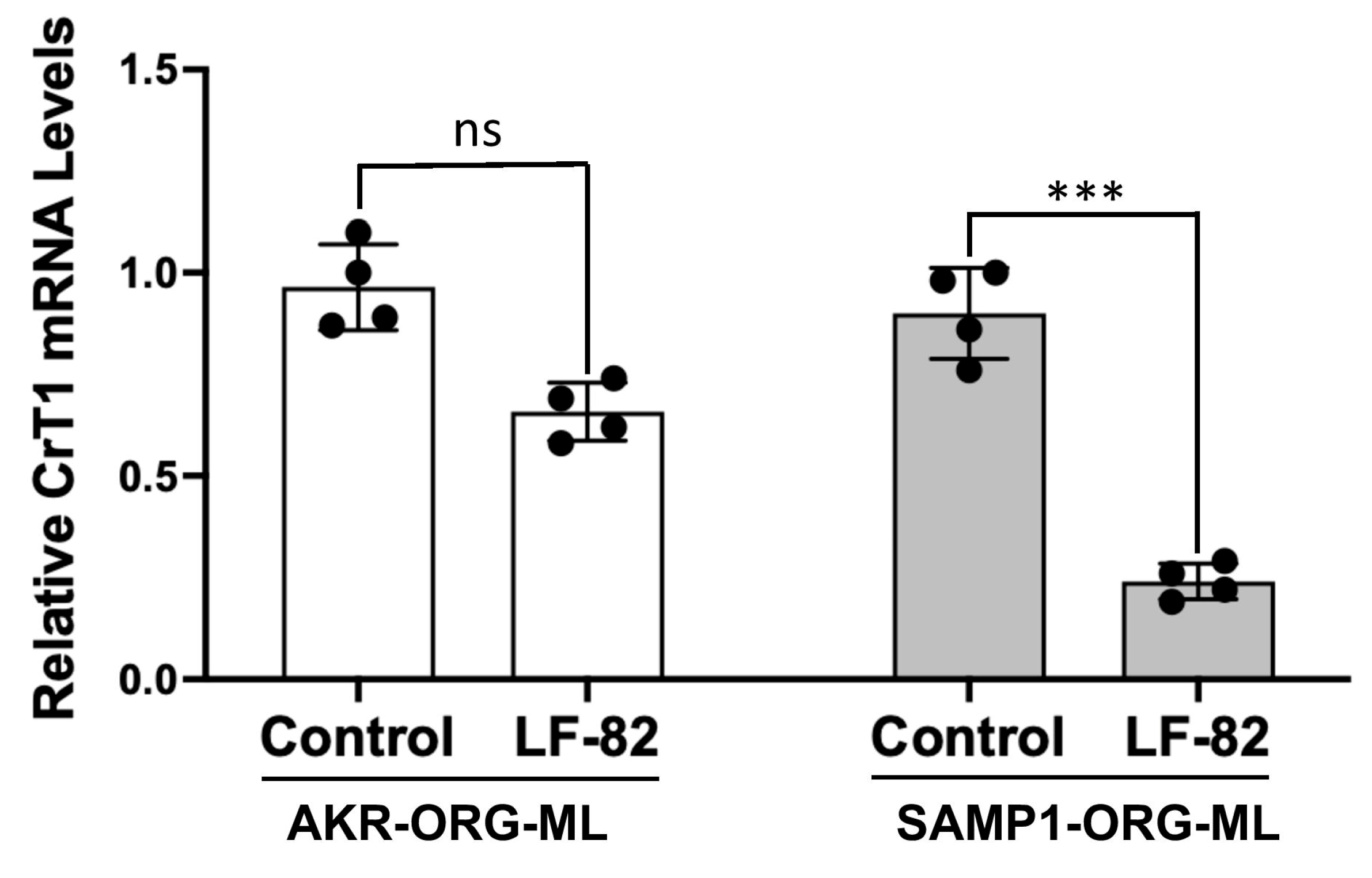
2.8. AIEC Infection Diminishes CrT1 in SAMP1 Organoid-Derived Monolayers
3. Discussion
4. Materials and Methods
4.1. Animal Studies and Human Intestinal Biopsy Samples
4.2. Generation of Crypt-Derived Organoids and Organoid-Derived Monolayers
4.3. Cell Culture and Treatment
4.4. Bacterial Cultures and Treatments of Cell Monolayers and Organoid-Derived Monolayers
4.5. Measurement of CrT1 Function
4.6. Real-Time Quantitative Polymerase Chain Reaction
4.7. Western Blotting
4.8. Promoter Activity
4.9. Immunofluorescence Studies in Mouse and Rat Mucosa
4.10. Data Analysis and Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| IECs | Intestinal epithelial cells |
| AIEC | Adherent invasive E. coli |
| IBD | Inflammatory bowel disease |
| CD | Crohn’s disease |
| UC | Ulcerative colitis |
| Cr | Creatine |
| CrT1 | Creatine transporter |
| IL1β | Interleukin β |
| TNFα | Tumor necrosis factor α |
| GAPDH | Glyceraldehyde 3 phosphate dehydrogenase |
| B2M | β2 microglobulin |
References
- Guan, Q. A Comprehensive Review and Update on the Pathogenesis of Inflammatory Bowel Disease. J. Immunol. Res. 2019, 2019, 7247238. [Google Scholar] [CrossRef] [PubMed]
- de Souza, H.S.; Fiocchi, C. Immunopathogenesis of IBD: Current state of the art. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 13–27. [Google Scholar] [CrossRef]
- M’Koma, A.E. The Multifactorial Etiopathogeneses Interplay of Inflammatory Bowel Disease: An Overview. Gastrointest. Disord. 2019, 1, 75–105. [Google Scholar] [CrossRef] [PubMed]
- McDowell, C.; Farooq, U.; Haseeb, M. Inflammatory Bowel Disease; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Christensen, C.; Knudsen, A.; Arnesen, E.K.; Hatlebakk, J.G.; Sletten, I.S.; Fadnes, L.T. Diet, Food, and Nutritional Exposures and Inflammatory Bowel Disease or Progression of Disease: An Umbrella Review. Adv. Nutr. 2024, 15, 100219. [Google Scholar] [CrossRef] [PubMed]
- Manski, S.; Noverati, N.; Policarpo, T.; Rubin, E.; Shivashankar, R. Diet and Nutrition in Inflammatory Bowel Disease: A Review of the Literature. Crohns Colitis 360 2024, 6, otad077. [Google Scholar] [CrossRef] [PubMed]
- Hashash, J.G.; Elkins, J.; Lewis, J.D.; Binion, D.G. AGA Clinical Practice Update on Diet and Nutritional Therapies in Patients With Inflammatory Bowel Disease: Expert Review. Gastroenterology 2024, 166, 521–532. [Google Scholar] [CrossRef] [PubMed]
- Santana, P.T.; Rosas, S.L.B.; Ribeiro, B.E.; Marinho, Y.; de Souza, H.S.P. Dysbiosis in Inflammatory Bowel Disease: Pathogenic Role and Potential Therapeutic Targets. Int. J. Mol. Sci. 2022, 23, 3464. [Google Scholar] [CrossRef]
- Roediger, W.E. The colonic epithelium in ulcerative colitis: An energy-deficiency disease? Lancet 1980, 2, 712–715. [Google Scholar] [CrossRef]
- Roediger, W.E. The starved colon—Diminished mucosal nutrition, diminished absorption, and colitis. Dis. Colon. Rectum 1990, 33, 858–862. [Google Scholar] [CrossRef]
- Colgan, S.P.; Wang, R.X.; Hall, C.H.T.; Bhagavatula, G.; Lee, J.S. Revisiting the “starved gut” hypothesis in inflammatory bowel disease. Immunometabolism 2023, 5, e0016. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Wang, R.X.; Alexeev, E.E.; Colgan, S.P. Intestinal Inflammation as a Dysbiosis of Energy Procurement: New Insights into an Old Topic. Gut Microbes 2021, 13, 1–20. [Google Scholar] [CrossRef]
- Singh, V.; Kumar, A.; Raheja, G.; Priyamvada, S.; Saksena, S.; Jhandier, M.N.; Gill, R.K.; Alrefai, W.A.; Borthakur, A.; Dudeja, P.K.; et al. Lactobacillus acidophilus attenuates downregulation of DRA function and expression in inflammatory models. Am. J. Physiol. Gastrointest. Liver Physiol. 2014, 307, G623–G631. [Google Scholar] [CrossRef] [PubMed]
- Prasad, H.; Visweswariah, S.S. Impaired Intestinal Sodium Transport in Inflammatory Bowel Disease: From the Passenger to the Driver’s Seat. Cell Mol. Gastroenterol. Hepatol. 2021, 12, 277–292. [Google Scholar] [CrossRef] [PubMed]
- Anbazhagan, A.N.; Priyamvada, S.; Alrefai, W.A.; Dudeja, P.K. Pathophysiology of IBD associated diarrhea. Tissue Barriers 2018, 6, e1463897. [Google Scholar] [CrossRef]
- Rahman, M.M.; Borthakur, A.; Afroz, S.; Arthur, S.; Sundaram, U. Unique Regulation of Intestinal Villus Epithelial Cl−/HCO3− Exchange by Cyclooxygenase Pathway Metabolites of Arachidonic Acid in a Mouse Model of Spontaneous Ileitis. Int. J. Mol. Sci. 2021, 22, 4171. [Google Scholar] [CrossRef] [PubMed]
- Borthakur, A.; Anbazhagan, A.N.; Kumar, A.; Raheja, G.; Singh, V.; Ramaswamy, K.; Dudeja, P.K.; Anandam, K.Y.; Alwan, O.A.; Subramanian, V.S.; et al. The probiotic Lactobacillus plantarum counteracts TNF-alpha-induced downregulation of SMCT1 expression and function. Am. J. Physiol. Gastrointest. Liver Physiol. 2010, 299, G928–G934. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Chatterjee, I.; Gujral, T.; Alakkam, A.; Coffing, H.; Anbazhagan, A.N.; Borthakur, A.; Saksena, S.; Gill, R.K.; Alrefai, W.A.; et al. Activation of Nuclear Factor-kappaB by Tumor Necrosis Factor in Intestinal Epithelial Cells and Mouse Intestinal Epithelia Reduces Expression of the Chloride Transporter SLC26A3. Gastroenterology 2017, 153, 1338–1350.e3. [Google Scholar] [CrossRef] [PubMed]
- Palaniappan, B.; Sundaram, S.; Arthur, S.; Afroz, S.; Sundaram, U. Inducible Nitric Oxide Regulates Na-Glucose Co-transport in a Spontaneous SAMP1/YitFc Mouse Model of Chronic Ileitis. Nutrients 2020, 12, 3116. [Google Scholar] [CrossRef]
- van de Kamp, J.M.; Mancini, G.M.; Salomons, G.S. X-linked creatine transporter deficiency: Clinical aspects and pathophysiology. J. Inherit. Metab. Dis. 2014, 37, 715–733. [Google Scholar] [CrossRef]
- Wallimann, T.; Hall, C.H.T.; Colgan, S.P.; Glover, L.E. Creatine Supplementation for Patients with Inflammatory Bowel Diseases: A Scientific Rationale for a Clinical Trial. Nutrients 2021, 13, 1429. [Google Scholar] [CrossRef]
- Turer, E.; McAlpine, W.; Wang, K.-W.; Lu, T.; Li, X.; Tang, M.; Zhan, X.; Wang, T.; Zhan, X.; Bu, C.-H.; et al. Creatine maintains intestinal homeostasis and protects against colitis. Proc. Natl. Acad. Sci. USA 2017, 114, E1273–E1281. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.H.; Lee, J.S.; Murphy, E.M.; Gerich, M.E.; Dran, R.; Glover, L.E.; Abdulla, Z.I.; Skelton, M.R.; Colgan, S.P. Creatine Transporter, Reduced in Colon Tissues From Patients With Inflammatory Bowel Diseases, Regulates Energy Balance in Intestinal Epithelial Cells, Epithelial Integrity, and Barrier Function. Gastroenterology 2020, 159, 984–998.e1. [Google Scholar] [CrossRef]
- Peral, M.J.; García-Delgado, M.; Calonge, M.L.; Durán, J.M.; De La Horra, M.C.; Wallimann, T.; Speer, O.; Ilundáin, A. Human, rat and chicken small intestinal Na+ − Cl− -creatine transporter: Functional, molecular characterization and localization. J. Physiol. 2002, 545, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Dolatabadi, R.K.; Feizi, A.; Halaji, M.; Fazeli, H.; Adibi, P. The Prevalence of Adherent-Invasive Escherichia coli and Its Association With Inflammatory Bowel Diseases: A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 730243. [Google Scholar] [CrossRef] [PubMed]
- Zheng, L.; Duan, S.-L.; Dai, Y.-C.; Wu, S.-C. Role of adherent invasive Escherichia coli in pathogenesis of inflammatory bowel disease. World J. Clin. Cases 2022, 10, 11671–11689. [Google Scholar] [CrossRef] [PubMed]
- Buisson, A.; Sokol, H.; Hammoudi, N.; Nancey, S.; Treton, X.; Nachury, M.; Fumery, M.; Hébuterne, X.; Rodrigues, M.; Hugot, J.P.; et al. Role of adherent and invasive Escherichia coli in Crohn’s disease: Lessons from the postoperative recurrence model. Gut 2023, 72, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Sivignon, A.; Chervy, M.; Chevarin, C.; Ragot, E.; Billard, E.; Denizot, J.; Barnich, N. An adherent-invasive Escherichia coli-colonized mouse model to evaluate microbiota-targeting strategies in Crohn’s disease. Dis. Model. Mech. 2022, 15, dmm049707. [Google Scholar] [CrossRef] [PubMed]
- Shawki, A.; Ramirez, R.; Spalinger, M.R.; Ruegger, P.M.; Sayoc-Becerra, A.; Santos, A.N.; Chatterjee, P.; Canale, V.; Mitchell, J.D.; Macbeth, J.C.; et al. The autoimmune susceptibility gene, PTPN2, restricts expansion of a novel mouse adherent-invasive E. coli. Gut Microbes 2020, 11, 1547–1566. [Google Scholar] [CrossRef] [PubMed]
- Shawki, A.; McCole, D.F. Mechanisms of Intestinal Epithelial Barrier Dysfunction by Adherent-Invasive Escherichia coli. Cell Mol. Gastroenterol. Hepatol. 2017, 3, 41–50. [Google Scholar] [CrossRef]
- Hidalgo, I.J.; Raub, T.J.; Borchardt, R.T. Characterization of the human colon carcinoma cell line (Caco-2) as a model system for intestinal epithelial permeability. Gastroenterology 1989, 96, 736–749. [Google Scholar] [CrossRef]
- Chervy, M.; Barnich, N.; Denizot, J. Adherent-Invasive, E. coli: Update on the Lifestyle of a Troublemaker in Crohn’s Disease. Int. J. Mol. Sci. 2020, 21, 3734. [Google Scholar] [CrossRef] [PubMed]
- Guimaraes-Ferreira, L. Role of the phosphocreatine system on energetic homeostasis in skeletal and cardiac muscles. Einstein 2014, 12, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Butts, J.; Jacobs, B.; Silvis, M. Creatine Use in Sports. Sports Health 2018, 10, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Kreider, R.B.; Kalman, D.S.; Antonio, J.; Ziegenfuss, T.N.; Wildman, R.; Collins, R.; Candow, D.G.; Kleiner, S.M.; Almada, A.L.; Lopez, H.L. International Society of Sports Nutrition position stand: Safety and efficacy of creatine supplementation in exercise, sport, and medicine. J. Int. Soc. Sports Nutr. 2017, 14, 18. [Google Scholar] [CrossRef]
- Forbes, S.C.; Cordingley, D.M.; Cornish, S.M.; Gualano, B.; Roschel, H.; Ostojic, S.M.; Rawson, E.S.; Roy, B.D.; Prokopidis, K.; Giannos, P.; et al. Effects of Creatine Supplementation on Brain Function and Health. Nutrients 2022, 14, 921. [Google Scholar] [CrossRef]
- Candow, D.G.; Forbes, S.C.; Ostojic, S.M.; Prokopidis, K.; Stock, M.S.; Harmon, K.K.; Faulkner, P. “Heads Up” for Creatine Supplementation and its Potential Applications for Brain Health and Function. Sports Med. 2023, 53 (Suppl. S1), 49–65. [Google Scholar] [CrossRef]
- Li, H.; Thali, R.F.; Smolak, C.; Gong, F.; Alzamora, R.; Wallimann, T.; Scholz, R.; Pastor-Soler, N.M.; Neumann, D.; Hallows, K.R.; et al. Regulation of the creatine transporter by AMP-activated protein kinase in kidney epithelial cells. Am. J. Physiol. Renal Physiol. 2010, 299, F167–F177. [Google Scholar] [CrossRef]
- Ji, L.; Zhao, X.; Zhang, B.; Kang, L.; Song, W.; Zhao, B.; Xie, W.; Chen, L.; Hu, X. Slc6a8-Mediated Creatine Uptake and Accumulation Reprogram Macrophage Polarization via Regulating Cytokine Responses. Immunity 2019, 51, 272–284.e7. [Google Scholar] [CrossRef]
- Li, Q.; Liu, M.; Sun, Y.; Jin, T.; Zhu, P.; Wan, X.; Hou, Y.; Tu, G. SLC6A8-mediated intracellular creatine accumulation enhances hypoxic breast cancer cell survival via ameliorating oxidative stress. J. Exp. Clin. Cancer Res. 2021, 40, 168. [Google Scholar] [CrossRef]
- Li, J.; Xu, S. Diagnosis and Treatment of X-Linked Creatine Transporter Deficiency: Case Report and Literature Review. Brain Sci. 2023, 13, 1382. [Google Scholar] [CrossRef]
- Duran-Trio, L.; Fernandes-Pires, G.; Grosse, J.; Soro-Arnaiz, I.; Roux-Petronelli, C.; Binz, P.A.; De Bock, K.; Cudalbu, C.; Sandi, C.; Braissant, O. Creatine transporter-deficient rat model shows motor dysfunction, cerebellar alterations, and muscle creatine deficiency without muscle atrophy. J. Inherit. Metab. Dis. 2022, 45, 278–291. [Google Scholar] [CrossRef] [PubMed]
- Pizarro, T.T.; Pastorelli, L.; Bamias, G.; Garg, R.R.; Reuter, B.K.; Mercado, J.R.; Chieppa, M.; Arseneau, K.O.; Ley, K.; Cominelli, F. SAMP1/YitFc mouse strain: A spontaneous model of Crohn’s disease-like ileitis. Inflamm. Bowel Dis. 2011, 17, 2566–2584. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Lee, D. Dietary Creatine as a Possible Novel Treatment for Crohn’s Ileitis. ACG Case Rep. J. 2016, 3, e173. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Stange, D.E.; Ferrante, M.; Vries, R.G.J.; Van Es, J.H.; Van Den Brink, S.; Van Houdt, W.J.; Pronk, A.; Van Gorp, J.; Siersema, P.D.; et al. Long-term expansion of epithelial organoids from human colon, adenoma, adenocarcinoma, and Barrett’s epithelium. Gastroenterology 2011, 141, 1762–1772. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Chatterjee, I.; Anbazhagan, A.N.; Jayawardena, D.; Priyamvada, S.; Alrefai, W.A.; Sun, J.; Borthakur, A.; Dudeja, P.K. Cryptosporidium parvum disrupts intestinal epithelial barrier function via altering expression of key tight junction and adherens junction proteins. Cell Microbiol. 2018, 20, e12830. [Google Scholar] [CrossRef]
- Ettayebi, K.; Crawford, S.E.; Murakami, K.; Broughman, J.R.; Karandikar, U.; Tenge, V.R.; Neill, F.H.; Blutt, S.E.; Zeng, X.-L.; Qu, L.; et al. Replication of human noroviruses in stem cell-derived human enteroids. Science 2016, 353, 1387–1393. [Google Scholar] [CrossRef]
- Borthakur, A.; Priyamvada, S.; Kumar, A.; Natarajan, A.A.; Gill, R.K.; Alrefai, W.A.; Dudeja, P.K. A novel nutrient sensing mechanism underlies substrate-induced regulation of monocarboxylate transporter-1. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 303, G1126–G1133. [Google Scholar] [CrossRef]




| Gene | Primer Sequence (5′-3′) |
|---|---|
| Human slc6a8 | F: CTTCATCATGTCGTGCGTGG R: GCGATCAGGACGTAGGGAAT |
| Mouse slc6a8 | F: TGGGGGTAAGGGTGGAATGTA R: TGTCATCCATGAAGCGGTCA |
| Rat slc6a8 | F: CCTCAACTGGGAAGTGACCC R: AGGACCACGTAGGGGAATGT |
| Human GAPDH | F: TGCACCACCAACTGCTTAGC R: GGCATGGACTGTGGTCATGAG |
| Mouse GAPDH | F: TGTGTCCGTCGTGGATCTGA R: CCTGCTTCACCACCTCTTGAT |
| RAT GAPDH | F: GGCAAGTTCAACGGCACAG R: CGCCAGTAGACTCCAC GAC |
| Mouse β2-Microglobulin | F: CTGGTGCTTGTCTCACTGAC R: GTTCAGTATGTTCGGCTTCC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sawant, H.; Selvaraj, R.; Manogaran, P.; Borthakur, A. Intestinal Epithelial Creatine Transporter SLC6A8 Dysregulation in Inflammation and in Response to Adherent Invasive E. coli Infection. Int. J. Mol. Sci. 2024, 25, 6537. https://doi.org/10.3390/ijms25126537
Sawant H, Selvaraj R, Manogaran P, Borthakur A. Intestinal Epithelial Creatine Transporter SLC6A8 Dysregulation in Inflammation and in Response to Adherent Invasive E. coli Infection. International Journal of Molecular Sciences. 2024; 25(12):6537. https://doi.org/10.3390/ijms25126537
Chicago/Turabian StyleSawant, Harshal, Rajesh Selvaraj, Prasath Manogaran, and Alip Borthakur. 2024. "Intestinal Epithelial Creatine Transporter SLC6A8 Dysregulation in Inflammation and in Response to Adherent Invasive E. coli Infection" International Journal of Molecular Sciences 25, no. 12: 6537. https://doi.org/10.3390/ijms25126537





