Abstract
Cancer remains a significant global health challenge, with millions of deaths attributed to it annually. Radiotherapy, a cornerstone in cancer treatment, aims to destroy cancer cells while minimizing harm to healthy tissues. However, the harmful effects of irradiation on normal cells present a formidable obstacle. To mitigate these effects, researchers have explored using radioprotectors and mitigators, including natural compounds derived from secondary plant metabolites. This review outlines the diverse classes of natural compounds, elucidating their roles as protectants of healthy cells. Furthermore, the review highlights the potential of these compounds as radioprotective agents capable of enhancing the body’s resilience to radiation therapy. By integrating natural radioprotectors into cancer treatment regimens, clinicians may improve therapeutic outcomes while minimizing the adverse effects on healthy tissues. Ongoing research in this area holds promise for developing complementary strategies to optimize radiotherapy efficacy and enhance patient quality of life.
1. Introduction
Cancer is believed to be a group of diseases that can occur anywhere in the body, and involves uncontrolled, abnormal cell growth that spreads or invades other parts of the organism. In 2022, global cancer statistics from the International Agency for Research on Cancer revealed close to 20 million new cases of cancer and 9.7 million deaths from cancer [1]. The data suggest that approximately one in five men or women will develop cancer in their lifetime, while around one in nine men and one in 12 women will die from it. According to US National Cancer Institute, it is projected that 2,001,140 new cancer cases will be identified in the United States in 2024, and 611,720 individuals will die from the disease [2]. Most types of cancer seem to evolve from one cell, which is genetically damaged and divides uncontrollably.
Irradiation might be used as a radical stand-alone cancer treatment or as a part of a combination therapy that includes surgeries, chemotherapy or/and hormonal therapy, immunotherapy, and hyperthermia [3,4,5,6]. Radiotherapy might be performed as an add-on before surgery to reduce the size of a tumor or after the procedure to radiate the surgical site to relegate the residual cancer cells. Irradiation likewise plays a role in palliative care [7]. X-rays, and alpha, beta, and gamma ionizing radiation (IR) are exploited in therapy [8]. A free radical, an atom or molecule carrying in its outer shell one or more unpaired electrons, is capable of independent existence, damages DNA, and causes the death of healthy and cancer cells [9].
According to Cox et al. [10], there are less sensitive tissues (e.g., the bile ducts, uterus, and vagina) that can tolerate an approximately 100-times higher doses than sensitive tissues (e.g., bone marrow, lens, and gonads). Post-radiation effects occur after hours or days on acutely responding tissues, like arterioles, bladder, bone marrow, capillaries, colon, esophagus, larynx, lymph node, oral mucosa, ovary, salivary gland, skin, small bowel, stomach, testis, and vagina. Tissues that reveal radiation effects in a few weeks to a few months after radiotherapy are categorized as sub-acutely responding tissues: brain, heart, kidney, liver, lung, and spinal cord. Late effects can occur after sufficient doses of radiation in all tissues. Nevertheless, several tissues manifest only late effects without previous acute effects: bile ducts, bone, breast, cartilage, lymph vessels, pancreas (endocrine), pituitary, thyroid, and uterus.
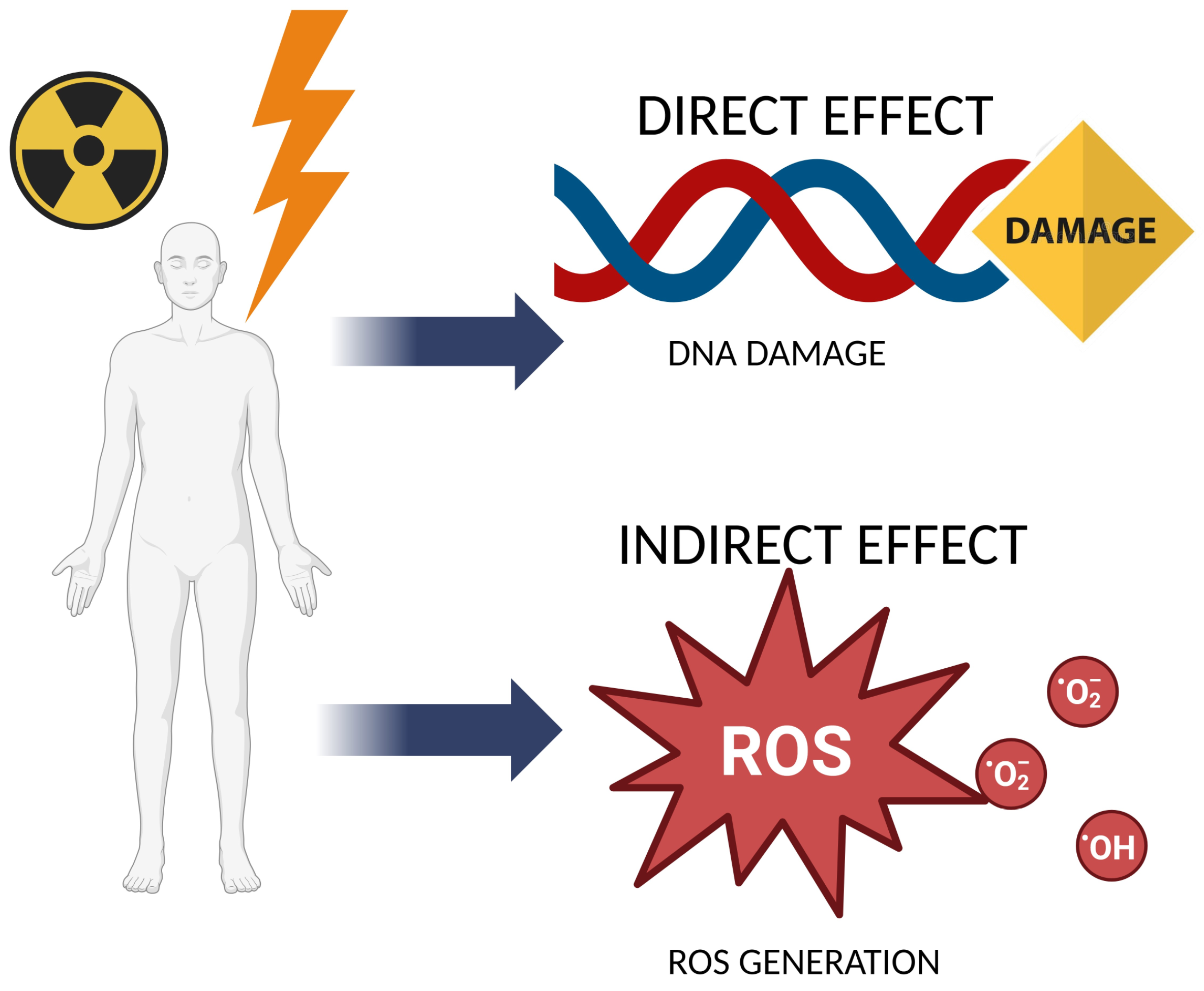
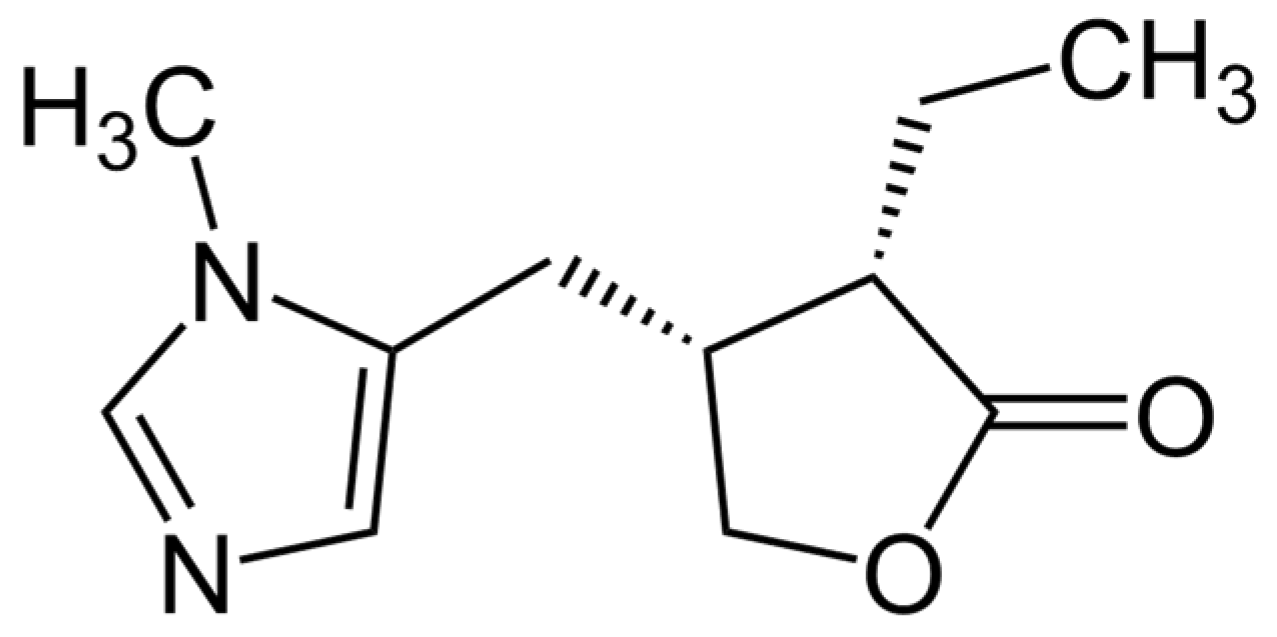
The mechanism of the harmful effects of ionizing radiation (IR) is strongly related to the increase in oxidative stress in irradiated tissues (Figure 1). It is known that IR can penetrate the cells of living organisms, causing the ionization of organic and inorganic compounds. Due to the high water content in cells, infrared radiolysis of water molecules is the primary process contributing to the increased formation of reactive oxygen species (ROS) and oxidative stress. ROS can also occur because mitochondria are IR-susceptible, and their dysfunction increases ROS generation. Next, ROS react rapidly with macromolecules, leading to cell dysfunction and apoptotic death.
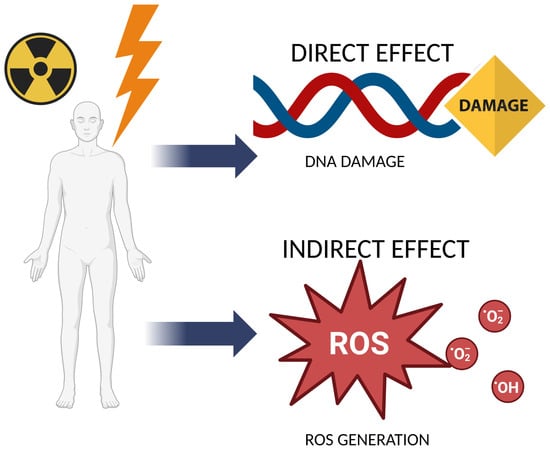
Figure 1.
The mechanisms of the harmful effects of ionizing radiation (Abbrev.—reactive oxygen species (ROS)).
Moreover, by altering DNA or proteins responsible for stabilizing the DNA structure, IR can also indirectly affect oxidative–antioxidant homeostasis in the cells, causing affected cells to become more susceptible to ROS damage (Figure 1). Besides, antioxidants or genes encoding enzymatic antioxidants may be damaged by IR, increasing oxidative stress [11]. Einor et al. [12], in a meta-analysis based on 41 studies on various biological matrices, showed that IR generates ROS even at low doses. Moreover, in studies on both in vivo and in vitro models, it was noted that irradiation increased the concentration of malondialdehyde (MDA), nitroxyl anion (NO•), and calcium ions and decreased superoxide dismutase (SOD) and catalase (CAT) activity and glutathione (GSH) concentration [11,13,14]. Szumiel [15] has proposed a relation between IR-induced oxidative stress, changes in mitochondrial DNA, and epigenetic changes in nuclear DNA, where IR-induced ROS generation causes mutations in mitochondrial DNA, which in turn contributes to ROS generation, creating a vicious circle. Mitochondrial DNA mutations affect the nuclear DNA epigenetic control mechanisms; they reduce methyltransferase activity, thus causing global DNA hypomethylation [16]. Hence, direct IR-related adverse side effects may develop as a result of increased oxidative stress, and ROS-related diseases may also develop. Therefore, it is crucial to identify effective and safe preventive compounds that protect human health tissues against IR damage [17].
On the other hand, it should be noted that ROS have a dual role in cancer development. They may lead to epigenetic alterations that promote the acceleration of tumor progression. Oxidative stress can induce nuclear DNA activation, which leads to the initiation of cancer. Moreover, ROS also inhibit T cells and natural killer (NK) cells and promote M2 macrophage recruitment and macrophage polarization; consequently, cancer cells can, in this way, escape immune surveillance and immune defenses. Moreover, ROS promote tumor invasion and metastasis by inducing epithelial–mesenchymal transition in cancer cells.
On the other hand, massive ROS accumulation can lead to tumor growth inhibition in two ways. Firstly, it blocks tumor cell proliferation by inhibiting the proliferation, cell cycle, and nucleotide and adenosine 5γ-triphosphate (ATP) biosynthesis signaling pathway. Secondly, it induces tumor cell death via activation of stress in the endoplasmic reticulum, apoptosis in mitochondrial and p53 pathways, and the ferroptosis pathway. However, cancer cells can adapt to ROS through a self-adaptation system, while healthy cells cannot. By contrast, on the other side, higher levels of ROS promote genome instability, inducing activation of cancer cell death or inhibiting resistance to anticancer treatment [18].
All this shows how complex oxidative stress is in the context of cancer and healthy cells. Radiotherapy, which impacts ROS generation, aims to destroy cancer cells and, at the same time, save as many normal cells as possible [19]. Regrettably, nowadays, there is no technique to exclude the degenerative consequences of irradiation entirely on normal cells; thus, it is crucial to come up with possibilities that can forcefully neutralize its side effects. Radiosensitizers increase the sensitivity of tumor cells to treatment; the cells become more vulnerable to the treatment after being damaged by the agent, or the damage will escalate with the irradiation [20].
Substances used to protect normal tissue cells depending on the administration time, with respect to radiation exposure time, can be divided into radioprotectors, mitigators, and treatment [21]. Radioprotectors are agents delivered before or at the time of irradiation to minimize the damage in healthy cells. Mitigators might be administered even after radiation exposure. Treatment is used after radiotherapy to expiate the normal tissue injury and improve the quality of life.
Radioprotectors and mitigators can be derived from secondary plant metabolites found in various plants. These natural compounds play a role in enhancing the body’s resilience to radiation therapy. Research in this area is ongoing, and identifying specific plant-derived compounds with radioprotective or mitigative effects holds promise for developing complementary strategies to enhance the effectiveness of radiotherapy while minimizing damage to healthy cells. Integrating these natural compounds into cancer treatment approaches could improve outcomes and reduce side effects for individuals undergoing radiation therapy.
Secondary plant metabolites are a diverse group of organic compounds produced by plants that go beyond the essential functions of growth, development, and reproduction. Unlike primary metabolites, which are critical to the basic life processes of plants, secondary metabolites serve various ecological roles, primarily in interactions with the environment, defense mechanisms, and adaptation to stressors [22].
The terpenes class encompasses monoterpenes like limonene and pinene, sesquiterpenes (caryophyllene and farnesene), diterpenes such as taxol and gibberellins, and complex polyterpenes like gutta-percha [23,24,25]. Phenolics, including coumarins (umbelliferone and aesculin), furanocoumarins (angelicin and bergapten), stilbenes (resveratrol and pterostilbene), flavonoids (kaempferol and hesperidin), and tannins (ellagic acid and catechins), play vital roles in plant defense and antioxidant activity [26,27,28]. Nitrogen-containing compounds comprise alkaloids (morphine and emetine), cyanogenic glucosides (amygdalin and prunasin), and non-protein amino acids (canavanine and mimosine) [29,30,31]. The sulfur-containing compounds class contains glucosinolates (sulforaphane), phytoalexins (camalexin), phytochelatins, and thionins (viscotoxin) [32,33,34,35]. Many isolated substances, plant extracts, and powders have been researched to be radioprotective agents.
2. Mechanisms of Radioprotective Effects
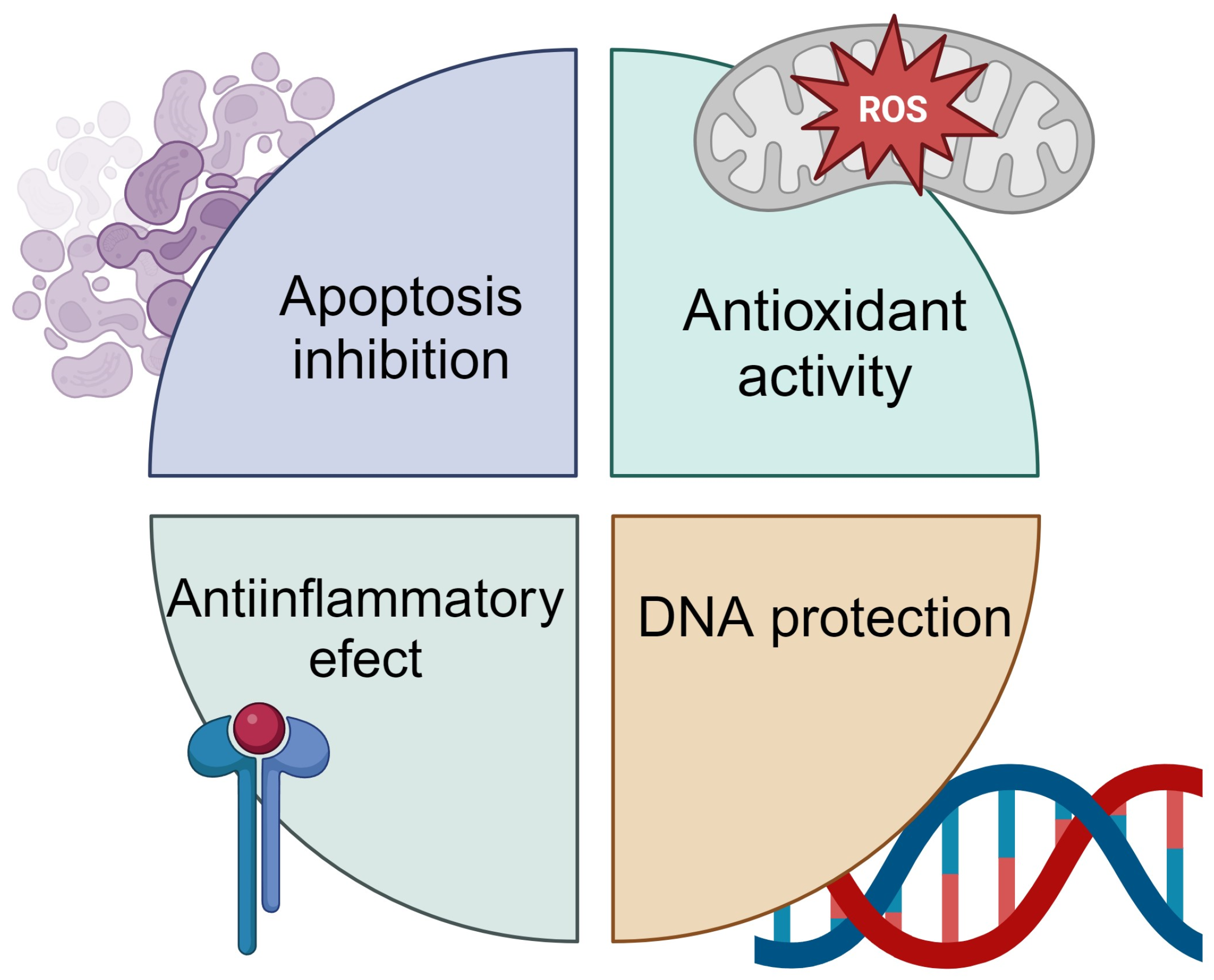
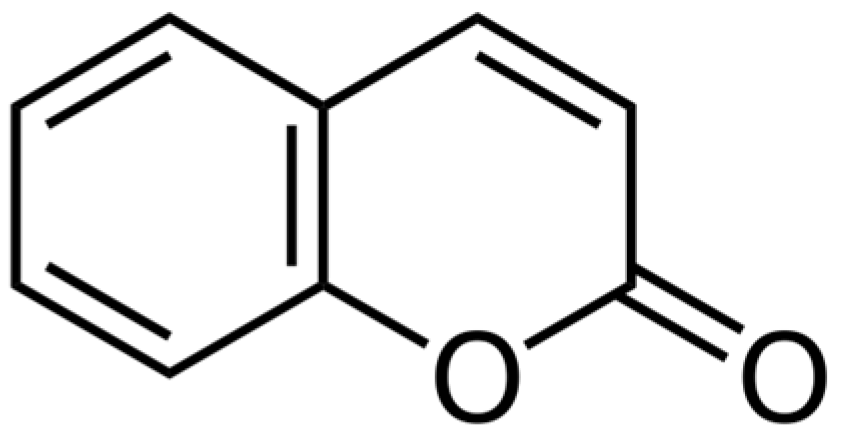
Radioprotective effects of plant substances have been attributed to various mechanisms, including immunostimulatory activity, antioxidant properties, DNA repair modulation, and an impact on apoptosis (Figure 2). In contrast to synthetic radioprotectors like thiol, plant compounds offer a safer and more economical option, being less toxic and often derived from substances commonly used in traditional medicine. As pointed out by Dowlath et al. [36], for a compound to be an ideal radioprotector, several functional properties must be present: (a) repair DNA and cell damage; (b) help rebuild damaged organs; (c) immunomodulation; (d) scavenging free radicals; and (e) oxidative stress reduction. These plant compounds meet the criteria for ideal radioprotectors due to their various mechanisms of action that effectively shield against the harmful effects of radiation [37]. Additionally, many plant-origin substances boast extended half-lives and show minimal interactions with other drugs administered during therapy. Similarly, terpenes have been implicated in radioprotective effects by upregulating nuclear factor erythroid 2-related factor 2 (Nrf2). This master transcription factor regulates antioxidant responses, thereby protecting cells from radiation-induced oxidative stress [38].
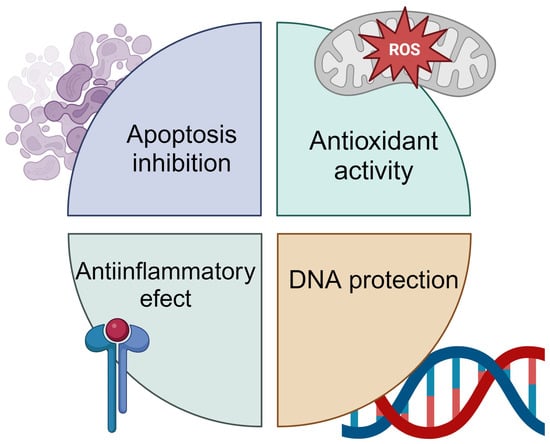
Figure 2.
Mechanisms of radioprotective effects of plant compounds. (Abbrev.—reactive oxygen species (ROS)).
2.1. Antioxidant Activity
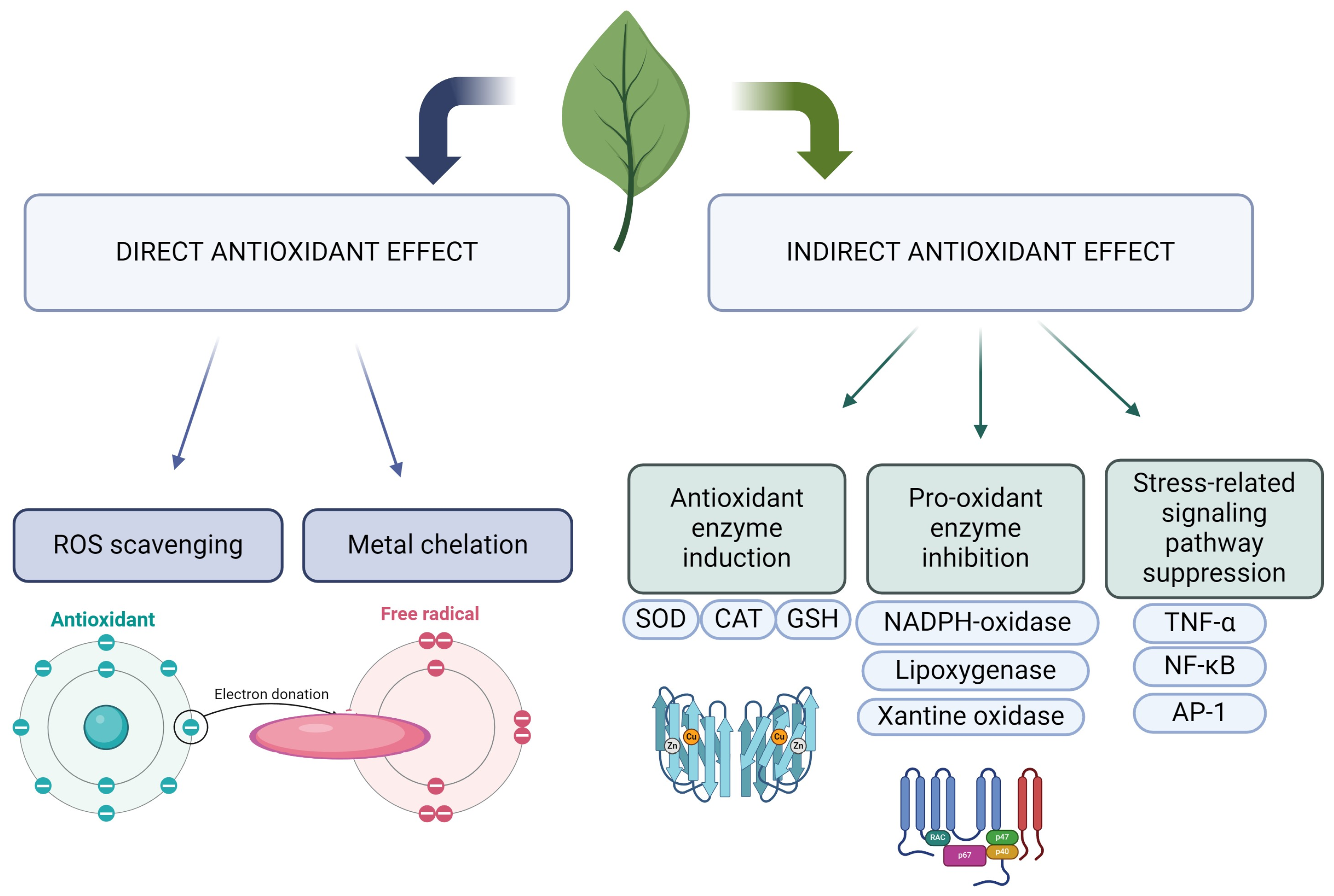
Natural substances can exhibit protective effects on cells exposed to radiation due to their potent antioxidant activity. The antioxidant mechanisms include both direct actions, such as free radical scavenging and metal chelation, and indirect mechanisms (Figure 3). Indirect mechanisms involve the induction of antioxidant enzymes such as superoxide dismutase (SOD), catalase (CAT), and glutathione (GSH), as well as the inhibition of pro-oxidant enzymes like NADPH oxidase, lipoxygenase, and xanthine oxidase [39]. These actions help to reduce oxidative stress in cells. The transfer of electrons to free radicals by phenolic compounds interrupts oxidative reactions, thereby mitigating the harmful effects of ROS generated by radiation [40]. Compounds such as polyphenols, which possess some of the strongest antioxidant properties, also affect pathways closely associated with oxidative stress, such as TNF-alpha and NF-kappa B [41]. Through these multifaceted mechanisms, natural substances can effectively mitigate the oxidative damage caused by radiation. Specifically, flavonoids have been reported to scavenge free radicals, inhibit cell apoptosis, and promote DNA repair, thereby mitigating radiation-induced damage [42,43].
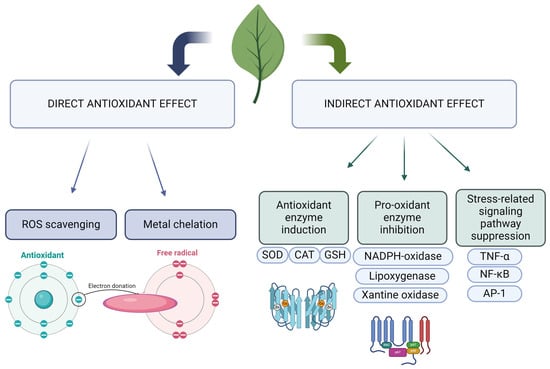
Figure 3.
Antioxidant mechanisms of natural compounds (Abbrev.—reactive oxygen species (ROS), superoxide dismutase (SOD), catalase (CAT), glutathione (GSH), nicotinamide adenine dinucleotide phosphate oxidase (NADPH-oxidase), tumor necrosis factor (TNF), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), and activator protein 1 (AP-1)).
2.2. DNA Protection
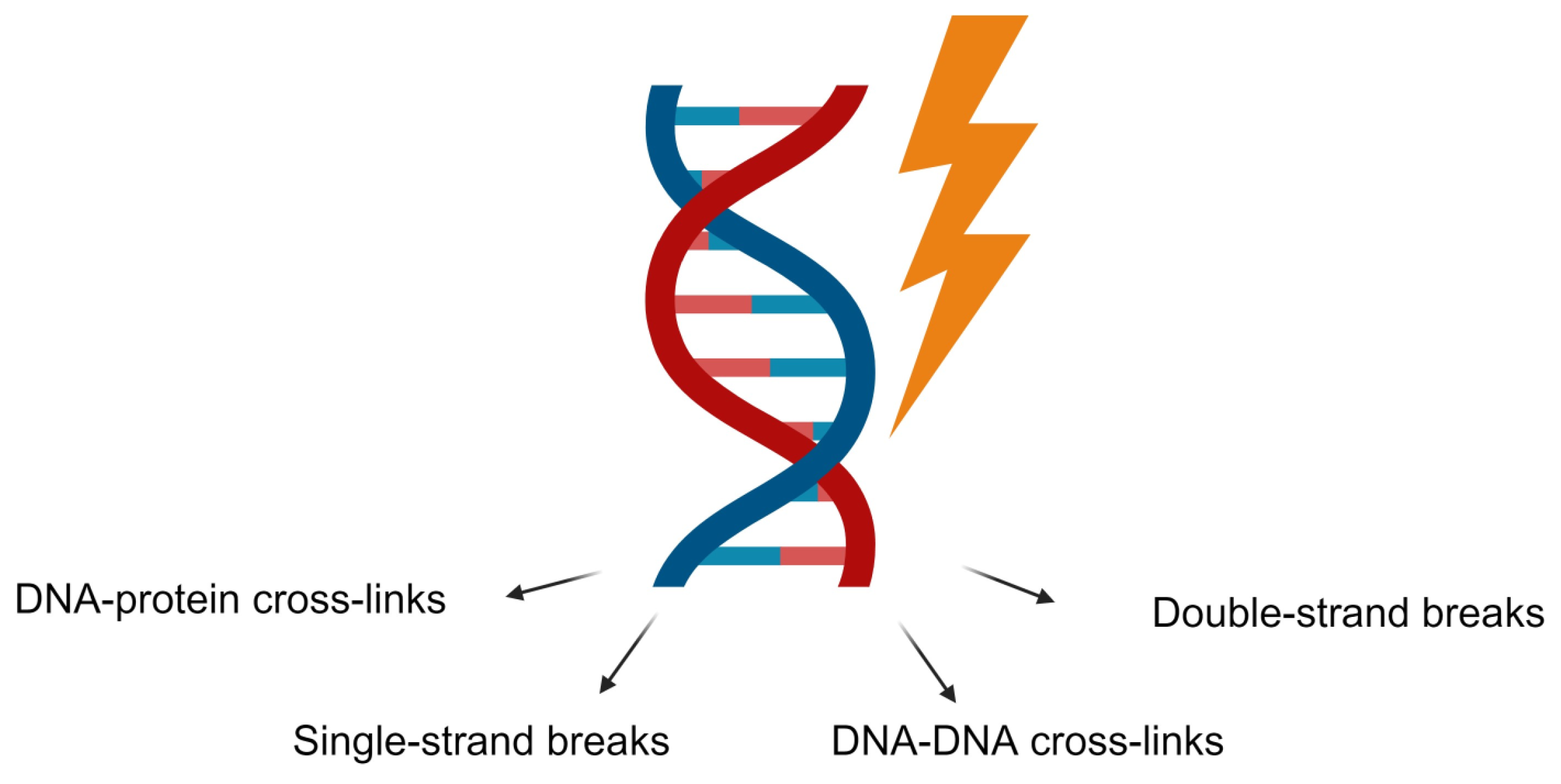
Radiation can directly lead to DNA damage, such as single- or double-strand breaks (DSBs), base damage, and DNA–DNA or DNA–protein cross-links, with these changes clustering as complex, localized, multiple damaged sites (Figure 4) [44]. DNA-DSB damage is considered the most deadly event following ionizing radiation [45]. Radioprotectants can regulate DNA repair genes and protect against radiation-induced damage by ensuring the repair of DNA lesions [46]. This regulation helps mitigate the effects of ionizing radiation and maintain genomic stability [47]. Radioprotectants help mitigate radiation-induced damage by upregulating DNA repair genes and enhancing DNA repair pathways like homologous recombination (HR) and non-homologous end joining (NHEJ). They also boost base excision repair (BER) and nucleotide excision repair (NER) mechanisms, ensuring efficient repair of oxidative lesions [41,48,49]. Additionally, radioprotectants increase the activity of antioxidant proteins, reducing oxidative damage and the burden on DNA repair systems [50].
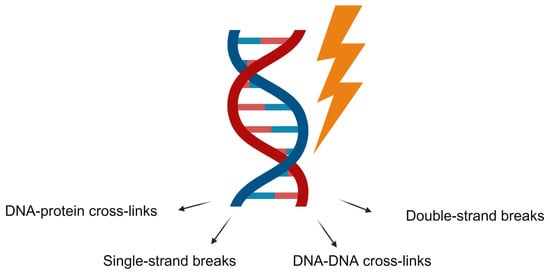
Figure 4.
DNA damage induced by radiation.
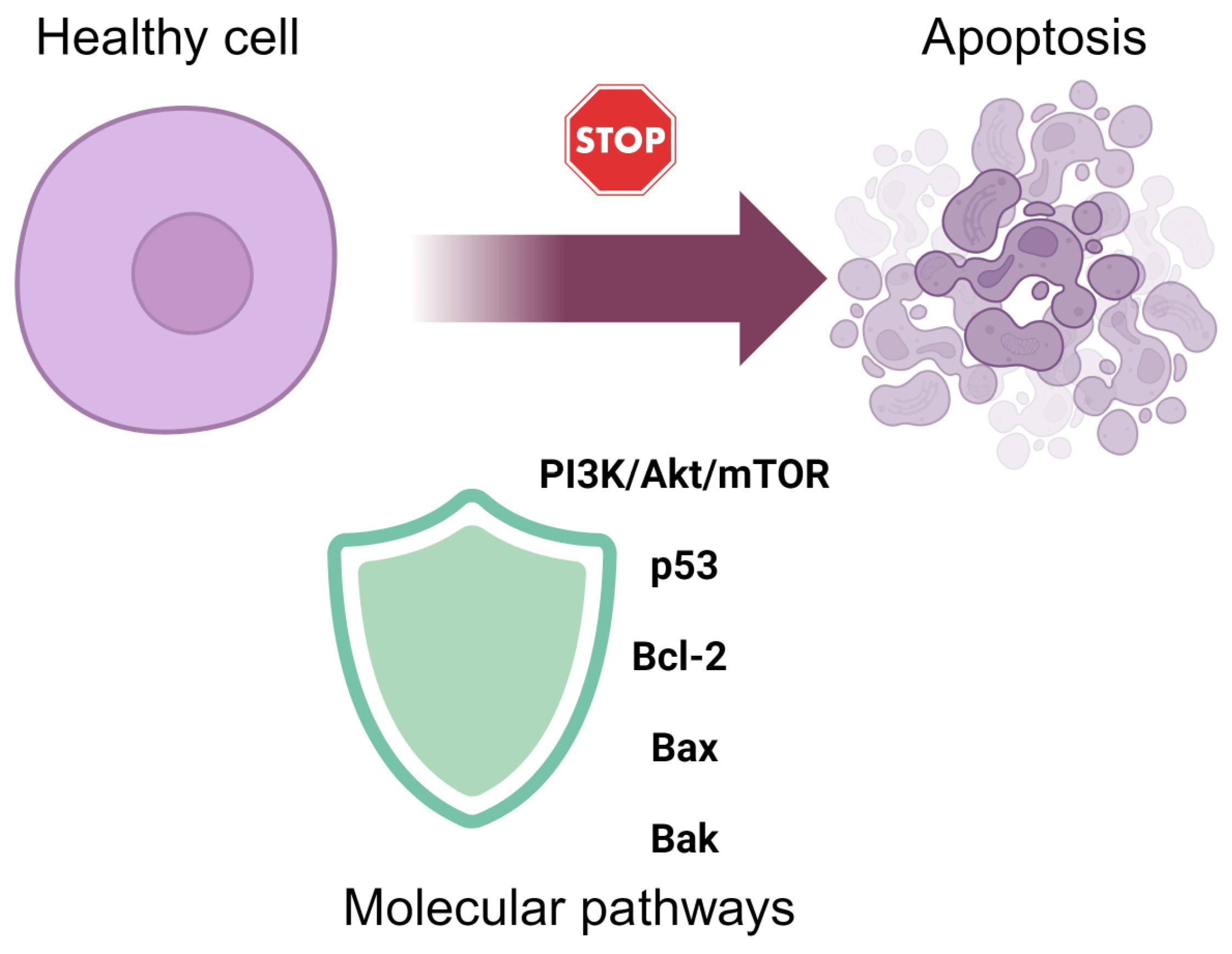
2.3. Apoptosis Inhibition
Apoptosis, or programmed cell death, is a crucial process that allows the body to remove damaged or unwanted cells [51]. In the context of radiation exposure, healthy cells can undergo apoptosis due to the oxidative stress and DNA damage induced by radiation. Natural radioprotectors can play a significant role in preventing apoptosis in these cells, thereby mitigating the harmful effects of radiation [52]. Natural radioprotectors can influence several key molecular pathways involved in apoptosis (Figure 5). One such pathway is the PI3K/Akt/mTOR pathway, which promotes cell survival and growth. Activation of this pathway by natural compounds can enhance cell survival by inhibiting pro-apoptotic signals [53]. Additionally, the p53 protein, known as the “guardian of the genome”, is a critical regulator of apoptosis in response to DNA damage [54]. Natural radioprotectors can inhibit the activity of p53, thereby reducing the initiation of the apoptotic process [55]. Such activity concerns, among others, apigenin [56]. Furthermore, the Bcl-2 family of proteins, including Bcl-2, Bax, and Bak, plays a pivotal role in the regulation of apoptosis. Bcl-2 is an antiapoptotic protein that promotes cell survival, while Bax and Bak are pro-apoptotic proteins that promote cell death [57]. Natural radioprotectors can increase the expression of Bcl-2 while decreasing the levels of Bax and Bak, thus tipping the balance towards cell survival rather than apoptosis [57]. The PI3K/AKT/mTOR signaling pathway has been implicated in the apoptotic effects of certain plant extracts on cancer cells [58].
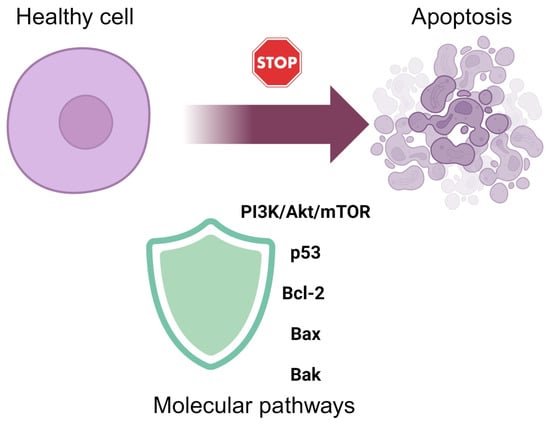
Figure 5.
Mechanisms of inhibiting apoptosis.
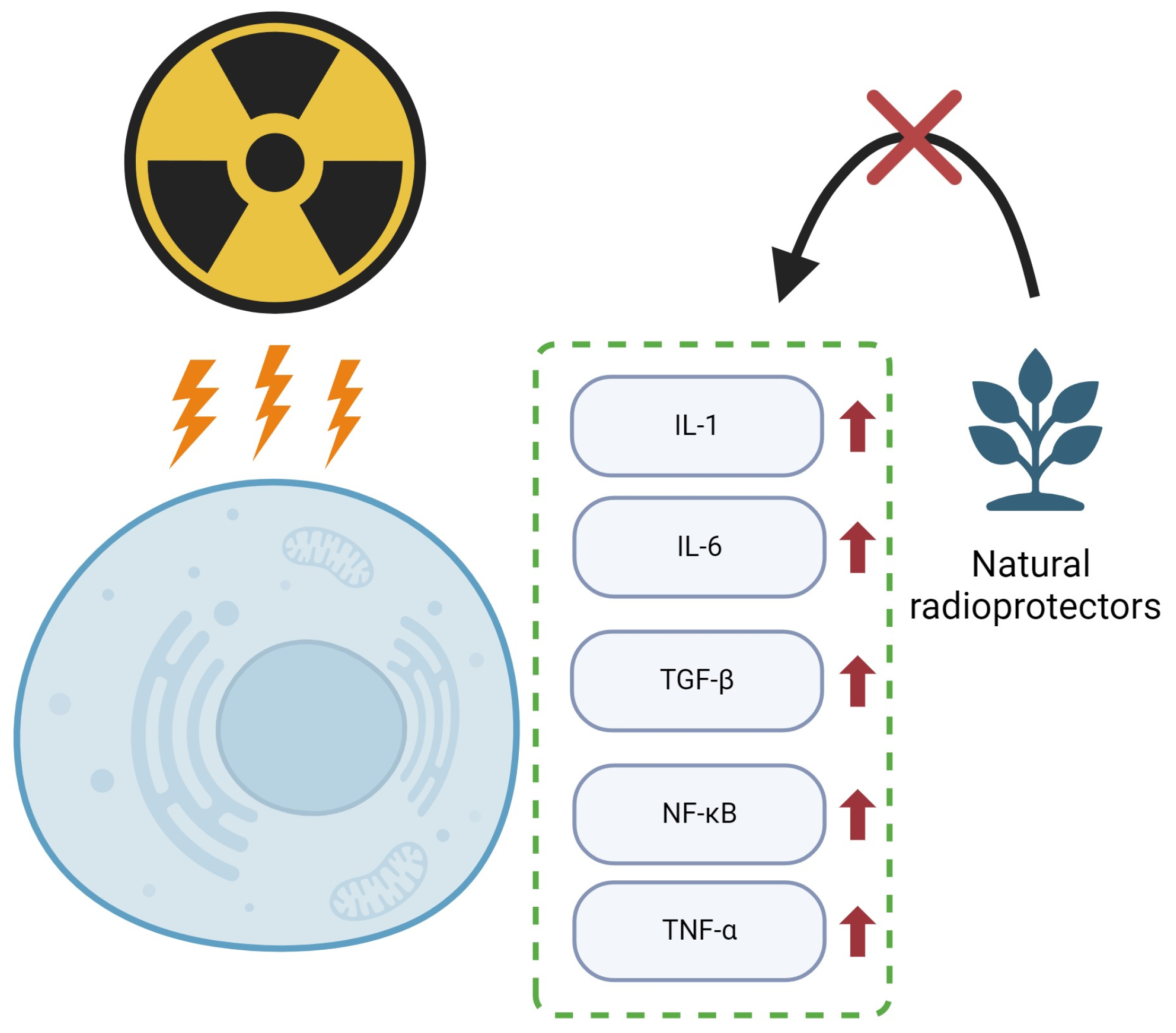
2.4. Antiinflammatory Effect
Radiation therapy can lead to extensive damage to the body, including the activation of the immune response and the occurrence of widespread inflammation [59]. Therefore, it is important to effectively mitigate the side effects associated with inflammation, and certain natural products and their active ingredients can achieve this through their anti-inflammatory effects [60]. After exposure to ionizing radiation, the body produces various pro-inflammatory cytokines and chemokines, such as interleukin-1 (IL-1), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and transforming growth factor beta (TGF-β) [61]. TGF-β is particularly important in radiation-induced damage, as it mediates tissue fibrosis, such as in the lungs and skin (Figure 6) [62]. Additionally, TGF-β1 activation is induced indirectly by ionizing radiation through the damage to endothelial cells, disrupting the balance of reactive oxygen and nitrogen species [63]. Plant compounds have been studied for their effects on different signaling pathways, such as TGF-β. Natural radioprotectors can help reduce inflammation and tissue damage through a variety of mechanisms [64]. Compounds like resveratrol and crocetin have demonstrated radioprotective effects by attenuating radiation-induced dysfunction in salivary glands and intestinal epithelial cells, respectively [65,66]
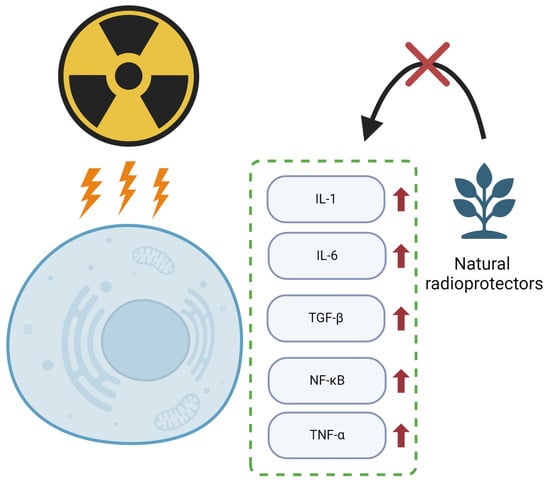
Figure 6.
Mechanisms of natural radioprotectors in reducing radiation-induced inflammation (Abbrev.—interleukin (IL), transforming growth factor β (TGF-β), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), and tumor necrosis factor α (TNF-α)).
3. Radiomodulation In Vitro Models
With respect to radioprotective potential, numerous in vitro studies have been conducted on various cell lines. These investigations aim to elucidate the efficacy and mechanisms underlying the radioprotective properties of potential agents. These studies involve exposing different cell types to IR in controlled laboratory settings to assess the ability of specific substances to mitigate the harmful effects of radiation. The outcomes of these in vitro studies contribute valuable insights to our understanding of the radioprotective potential of various compounds. In addition to studying radioprotective potential, in vitro investigations also explore the phenomenon of radiosensitization, particularly concerning its differential effects on healthy and cancerous cell lines. Radiosensitization involves enhancing the sensitivity of cells to IR and potentially increasing the efficacy of radiation therapy in cancer treatment. By observing changes in, e.g., cell survival or DNA damage, the impact of studied compounds or extracts on the radiosensitivity of the cells can be studied (Table 1).

Table 1.
In vitro studies on radiomodulating effects of natural compounds.
4. Radioprotection in Animal Models
Radioprotection studies on animals such as mice, rats, dogs, guinea pigs, minipigs, and rabbits are essential for understanding the impact of radiation on organisms and developing effective health protection strategies. These studies should adhere to the principles of the 3Rs (Replacement, Reduction, and Refinement) and comply with local regulations. To date, numerous animal studies have been conducted. The studies are summarised in Table 2.
4.1. Studies Performed on Mice and Rats
The most commonly used animal model for in vivo studies of radioprotective agents is in mice and rats. These animals are small mammals, adaptive to new surroundings, easy to breed, pleasant-natured, procreate fast, and have a short lifespan. They might be used to prove the radioprotective properties of substances, extracts, and oils. In the M.E. assayed study, rats were administered with Nigella sativa oil (1 mL/kg b.w.) orally for 5 days a week for four weeks; after the last intubation, animals were gamma irradiated (4 Gy) [82]. In the only radiation-exposed group, rats had leukopenia and exhibited a decrease in total protein concentration in plasma, an increase in malondialdehyde as a lipid peroxidation marker, and a rise in GSHpx activity. All parameters were significantly closer to a normal range in rats treated with black seed oil. P. Uma Devi studied orientin (Ot), vicenin (Vc)- flavonoids from Ocimum sanctum leaves, MPG (2-mercaptopropionyl glycine), and WR-2721 as radioprotectants [83]. The potential of the substances was evaluated based on chromosome aberration in mice’s bone marrow cells. Examined animals were divided based on the injected intraperitoneally substances: 50 µg/kg b.w. of Ot or Vc; 20 mg/kg b.w. of MPG; and 150 mg/kg b.w. of WR-2721. Then, after 30 min, mice were exposed to 2.0 Gy gamma radiation. The most effective radioprotectant was WR-2721, and the least effective was MPG. Flavonoids of Ocimum sanctum yielded comparable results. In another study, mice were used to evaluate the protective effects against radiation of T. cordifolia root alcoholic extract [84]. Increased animal survival was obtained after 90 min of preliminary irradiation with the extract intraperitoneally administrated. According to antioxidation, anti-inflammation, and metal chelation, the extract inhibits lipid peroxidation, radiation-induced micronuclei formation, genotoxicity, and hemopoietic cell injury. More instances of the use of mice and rats are contained in Table 1.
4.2. Studies Performed on Dogs
Studies are also performed on dogs. Bradley performed irradiation using neutrons and photons with a mean energy of 15 MeV on beagle dogs [85]. The irradiated fields were the spinal cord, lung, and brain. Nonirradiated and photon-irradiated dogs did not develop any neoplasms. In the group of 46 neutron beam-irradiated dogs, 7 of them developed neoplasms (15%) within the irradiated parts. Also, in 1981, Zook and Bradley partial-body irradiated 39 beagle dogs with photons and neutrons with a mean energy of 15 MeV [86]. After proper thorax irradiation, all dogs developed degenerative and occlusive changes in vessels according to atrial lesions. Beagles died of hepatic failures, neoplasms, and myocardial infarction. The pathologic score of cardiac injury was higher for neutrons than for protons. In another study, beagles were used to determine the radioprotective effects of polysaccharides extracted from Sipunculus nudus. Cui I. dogs were orally administered polysaccharides (50, 100, and 200 mg/kg body weight) for seven days and radiated with 2 Gy γ-radiation, and then, for a further 27 days, they maintained polysaccharides administration. After radiation, untreated beagle dogs developed hematopoietic bone marrow damage. In contrast, other dogs stood out with an improved blood picture, hematopoietic activity, a decrease in nitric oxide concentration, and a rise in SOD activity.
4.3. Studies Performed on the Guinea Pig Model
Patients after radiotherapy might have sensorineural hearing loss. Some studies have attempted to prevent this in a guinea pig model. The guinea pigs were treated with an intra-peritoneal or intra-tympanic dose of aminothiol PrC-210 (3-(methyl-amino)-2-((methylamino)methyl)propane-1-thiol) a week before inner ear irradiation (3000cGy) [87]. The substance was not cytotoxic and did not impact morphology or the number of cochlear hair cells. One week after irradiation, auditory brainstem response thresholds of the test guinea pig group were better than in the not-injected, irradiated group. The spiral ganglion was efficiently less degenerated in Aminothiol PrC-210-treated animals. Combined in vitro and in vivo study of the potential radioprotective properties of metformin was performed by M. A. Mujica-Mota. In an in vitro study, The House Ear Institute–Organ of Corti 1 (HEI-OC1) cells were administered with 0–5 mM metformin 24 h before 15 Gy irradiation [88]. The guinea pigs were supplemented with metformin dissolved in water to obtain the 100 mg/kg/d dose three days before irradiation and until the end of the experiment [88]. The radiation of 3.5 Gy per day (2.6 min) lasted four weeks from Monday to Friday. Metformin was neither ototoxic nor radioprotective in vitro or in vivo. Orciprenaline and carbachol are radioprotectants at the medicinal treatment dose administered before irradiation of the minipigs [89]. In the study, 36 Gy X-irradiation was administered for six days at 6 Gy for three weeks. Acinar cells were more numerous, and there were significantly fewer pathological changes in the cells.
4.4. Studies Performed on Rabbits
Single gamma radiation (4 Gy) on rabbits influences the rabbits’ life duration [90]. Interestingly, irradiated inbred rabbits live shorter lives than outbred ones. Rabbits were fed a standard diet enriched with 100 and 200 ppm of Yuca schidigera extract; four weeks later, they were injected with 0.11–0.15 GBq Technetium-99 mIt (emits a single gamma photon) in 1 ml physiological serum [91]. Blood samples were taken before and 10 and 60 min after injection. The rabbits with diet enriched with YSE presented lower malondialdehyde concentrations before and after radiation compared to control rabbits. The concentration of nitric oxide (NO) was only significantly lowered for the rabbits supplemented with a higher concentration of YSE before injection, but after the procedure, there was no significant decrease in the upraised level of plasma NO. The reduction in plasma cholesterol concentration after radiation exposure was faster and more intense in the supplemented group than in the control group of rabbits. There was no significant difference between the levels of and total antioxidant activity in treated and untreated groups. Supplementation of Yuca schidigera extract only partially presented antioxidant effects on rabbits exposed to gamma radiation. In the Georgieva et al. [92] study, rabbits were injected with intramuscular 0.24 g/kg Haberlea rhodopensis extract 2 h before or 30 min after 2.0 Gy of gamma radiation. The increase after radiation plasma concentration of malondialdehyde as a lipid peroxidation marker was reduced in groups injected with Haberlea rhodopensis extract before or after radiation. However, the alkaline comet assay results performed on peripheral lymphocytes showed that only the group previously treated with the extract lowered the irradiation-induced increase in DNA damage frequency. The studies showed that the extract of Haberlea rhodopensis, directly and indirectly, has radioprotective properties. Another study, according to Penchev et al. [93], confirms that HRE is a radioprotectant. After a preliminary injection of 0.24 g/kg b.w. of Haberlea rhodopensis extract, the tubular diameter and area of the seminiferous tubules escalated compared to only a 2 Gy gamma radiation-exposed group of rabbits. Moreover, the pathological lesions in the tubular structure were less malign in the Haberlea rhodopensis extract-treated group of rabbits.
Macaca mulatta were gamma irradiated with 60 Co at a lethal dose of 6.8 Gy for 30 min (22.8 cGy/min) [94]. Additionally, 5 min before radiation exposure, juvenile rhesus macaques were administered intramuscularly with 40–120 mg/kg of indralin. Indralin at a dose of 120 mg/kg saved five out of six monkeys from death. It reduced lesions, delayed and reduced the severity of the hemorrhagic syndrome of the disease, and lenified leukopenia and anemia. Indralin is a strong radioprotectant.

Table 2.
In vivo studies of natural compounds and plant extracts for radioprotection.
Table 2.
In vivo studies of natural compounds and plant extracts for radioprotection.
| Substance/Plant | Application | Radioprotective Dose for Mouse (M) or Rat (R) | Time of Application | Proposed Mechanism |
|---|---|---|---|---|
| Aegle marmelos | Intraperitoneal [95] | 15 mg/kg M body weight (optimum) | For 5 days before irradiation | Free-radical scavenging, inhibition of lipid peroxidation, elevation of GSH, and increased activity of antioxidative enzymes |
| Ageratum conyzoides | Intraperitoneal [96] | 75 mg/kg M body weight (optimum) | Before irradiation | Scavenging of ROS, increased antioxidant status, and stimulation of the immune system |
| Borago officinalis | Oral [97] | 50 mg/kg R body weight | For one week before irradiation and 2 weeks after irradiation | Antioxidant activity, inhibition of MDA, and prevention against GSH depletion |
| 3 h after irradiation and daily for 2 weeks after irradiation | ||||
| Eugenol | Oral [98] | 150 mg/kg body weight (optimal) | 3 h after irradiation and daily for 2 weeks | Protection against oxidative stress, induction of detoxifying enzymes, scavenging of free radicals, inhibition of lipid peroxidation |
| Genistein | Subcutaneous [99] | 200 mg/kg body weight (optimal) | 24 h before irradiation | Estrogenic activity, antioxidant properties, immunostimulatory activity and its role in signal transduction pathways where it is an inhibitor of topoisomerase, protein kinase and caspases involved in apoptotic pathways, cytokine release |
| Oral [100] | 160 mg/kg M body weight | For seven consecutive days before irradiation | ||
| Glycyrrhiza glabra | Intraperitoneal [101] | 4 mg/kg M body weight | Before irradiation | Scavenging of free radicals |
| Hippophae rhamnoides | Intraperitoneal [102] | 30 mg/kg M body weight | 30 min before irradiation | Free-radical scavenging, acceleration of stem cell proliferation, and immunostimulation |
| Curcumin | Oral [103] | 20 mg/kg M body weight (optimal) | 2 h before irradiation and 24/30/48 h after irradiation | Scavenging of free radicals and the elevation of cellular antioxidants, upregulation of CAT, glutathione transferase (GST), GSHpx, SOD, and their mRNAs, reduction in lipid peroxidation, elevation in GSH and increase in sulphydryl groups, inhibition of activation of Protein Kinase C (PKC), Mitogen-Activated Protein Kinase (MAPK), and NO [k’] |
| Folic acid | Intraperitoneal [104] | 1.6 mg/kg M body weight | For 10 days after irradiation | Scavenging of free radicals, mainly by peroxynitrite scavenging and lipid peroxidation inhibition |
| luteolin | Oral [105] | 10 µmol/kg M body weight | 2 h before irradiation | Scavenging potency towards free radicals |
| Orgotein | Subcutaneous [106] | 400 mg/kg M body weight (optimal) | 1 to 2 h before irradiation | Anti-inflammatory action of the drug |
| Panax ginseng | Intraperitoneal [107] | 50 mg/kg M body weight | 36 and 12 h before irradiation | Antioxidant and free-radical-scavenging activities of the ginsenosides |
| Intraperitoneal [108] | 10 mg/kg M body weight | For 4 days before irradiation | Inhibition of initiation of free-radical processes by antiradical actions, e.g., inhibition of lipid peroxidation | |
| Resveratrol | Intraperitoneal [109] | 50 and 100 mg/kg M body weight | 2 h before irradiation | Antioxidant mechanisms |
| Oral [110] | 20 mg/kg M body weight (optimal) | For 7 days before irradiation and 30 days after irradiation | Antioxidant properties: scavenging free radicals, regulation of the redox of a cell by differentially affecting the expression of various oxidases and antioxidant enzymes | |
| Rutin | Oral [111] | 10 mg/kg M body weight (optimal) | For 5 days before irradiation | Scavenging of free radicals resulting in decreased oxidative stress in animals, normalization of intracellular antioxidant levels, anti-lipid peroxidative effect |
| Quercetin | Oral [111] | 20 mg/kg M body weight (optimal) | For 5 days before irradiation | Scavenging of free radicals resulting in decreased oxidative stress in animals, normalization of intracellular antioxidant levels, anti-lipid peroxidative effect |
5. Forms of Administration of Radioprotectants
Substances of radioprotective importance can be applied both topically and orally. Each method has advantages and disadvantages, and scientific studies have considered both.
Several factors must be considered when developing a topical preparation with radioprotective effects. The advantages of such a formulation include targeted delivery to the affected area, potentially reducing systemic side effects, and providing a more localized protective effect against radiation-induced damage [112,113]. Additionally, the use of topical formulations can offer better patient compliance and ease of application, particularly in scenarios where oral administration may be challenging, such as in cases of oral mucositis resulting from radiation therapy [114,115]. Furthermore, the potential for controlled drug delivery and the ability to maintain stable drug formulations in the solid state can be advantageous for topical oral preparations, especially in scenarios where storage at ambient temperature and longer shelf-life are crucial [116,117].
However, developing a topical preparation with radioprotective effects also presents challenges. Ensuring the sterility of the formulation is critical, particularly for burn wounds, to prevent infections and promote effective wound healing [118,119]. Additionally, the formulation must be designed to penetrate the skin barrier effectively to reach the target tissues and provide the desired radioprotective effects. Furthermore, the potential for microbial contamination in burn wounds necessitates using antimicrobial agents in the formulation to prevent infections and promote healing. Moreover, the formulation should be designed to minimize disruption of the body’s natural healing mechanisms and maintain a moist, aseptic environment to support optimal wound healing. The use of topical preparations containing colored plant compounds can also disrupt the image of the wound.
Also, oral delivery of radioprotective agents presents advantages and disadvantages in protecting against radiation-induced damage. One significant advantage is the potential for systemic protection. Oral administration of radioprotective agents allows for the distribution of protection throughout the entire body, safeguarding multiple organs and tissues simultaneously [120,121]. This systemic approach is crucial in mitigating the broad impact of radiation exposure. Another notable benefit is enhanced patient compliance. Oral administration offers a familiar and convenient drug delivery route, potentially improving patient adherence to radioprotective treatment regimens [121]. The accessibility of oral delivery may contribute to better patient cooperation, a crucial factor in the success of radiation protection strategies.
Moreover, the versatility of oral formulations allows for targeted delivery to specific tissues or organs. This targeted approach enables localized protection against radiation-induced injury, offering a more tailored and efficient protective mechanism [120,122]. Eliminating procedures, such as using ointments and gels, is another advantage. Additionally, oral formulations can be designed for controlled release, providing sustained and prolonged radioprotective effects. This controlled-release feature adds to the efficacy of oral delivery, ensuring a more consistent and prolonged protection against radiation exposure.
However, the oral delivery of radioprotective agents has its challenges. One notable drawback is the variability in drug absorption, leading to inconsistent bioavailability and potentially affecting the overall efficacy of radioprotective agents [120]. Gastrointestinal side effects, such as nausea, vomiting, and diarrhea, are associated with oral administration and can impact patient tolerance and compliance. First-pass metabolism in the liver poses another challenge. Orally administered drugs undergo this metabolic process, which can result in reduced bioavailability and efficacy of radioprotective agents [123]. Overcoming the hurdles of first-pass metabolism is essential for optimizing the protective effects of orally delivered radioprotective agents. Furthermore, oral formulations may exhibit a delayed onset of action compared to parenteral routes, potentially limiting their effectiveness in acute radiation exposure scenarios. In situations requiring immediate response, this delay could be a critical factor to consider.
In summary, while oral delivery of radioprotective agents offers systemic protection, patient compliance, and potential for targeted delivery, it is not without challenges. The variability in absorption, gastrointestinal side effects, first-pass metabolism, delayed onset of action, and sterility requirements may impact the overall efficacy of this delivery method. Careful consideration of these factors is essential in determining the suitability of oral administration for radioprotective strategies.
6. Compounds of Natural Origin Showing Radioprotective Activity
6.1. Terpenes
A large group of hydrocarbons is terpenes. These substances are built up from isoprene units. According to the number of units, we can differentiate monoterpenes (C10H16), sesquiterpenes (C15H24), diterpenes (C20H32), and so on. Similarly named, terpenoids stand for substances that have been terpenes derivates, such as naturally oxidated or chemically modified terpenes.
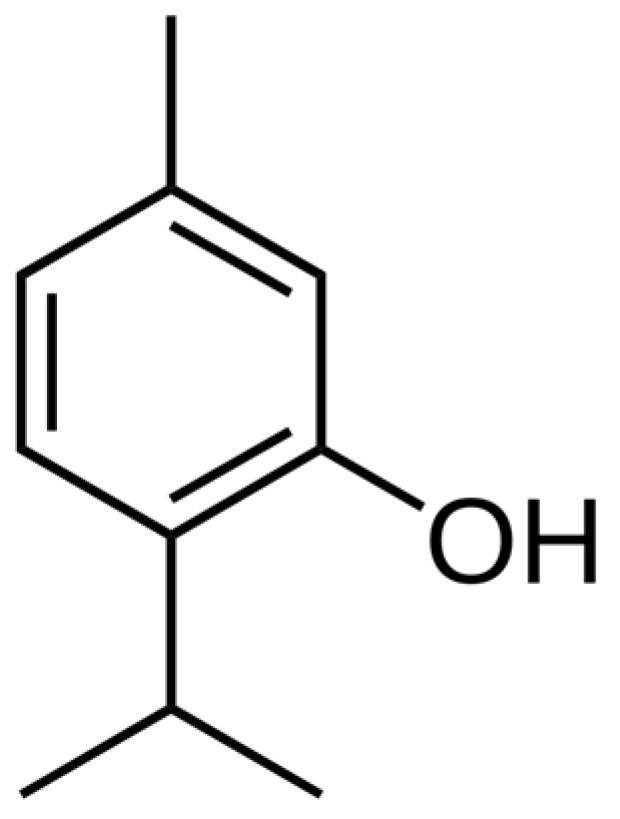
Carvacrol and thymol (Figure 7), known for their antioxidative, anti-inflammatory, and radioprotective properties, demonstrated nephroprotective potential in rats subjected to gamma irradiation. The findings suggest these compounds may alleviate acute RN by mitigating oxidative stress, inflammation, and apoptosis. Additionally, the preservation of the Calcitonin Gene-Related Peptide-Tumor Necrosis Factor Alpha (CGRP-TNF-α) loop and the in silico molecular docking simulations support the notion that carvacrol and thymol could enhance the therapeutic benefits of gamma irradiation [124]. In rats, thymol (present, e.g., in Thymus sp.) showed significant protection in acute and chronic post-radiation damage in salivary glands [125]. According to Sueishi et al. [126], menthol (Mentha piperita) is the strongest radioprotector of the three monoterpenes linalol, thymol, and menthol. A study conducted by Mahran et al. [127] demonstrates the radioprotective effects of carvacrol and thymol, particularly in rescuing ovarian reserve through counteracting oxidative stress and dysregulated cross-talk between (Insulin-like Growth Factor 1) IGF-1 and TNF-α.
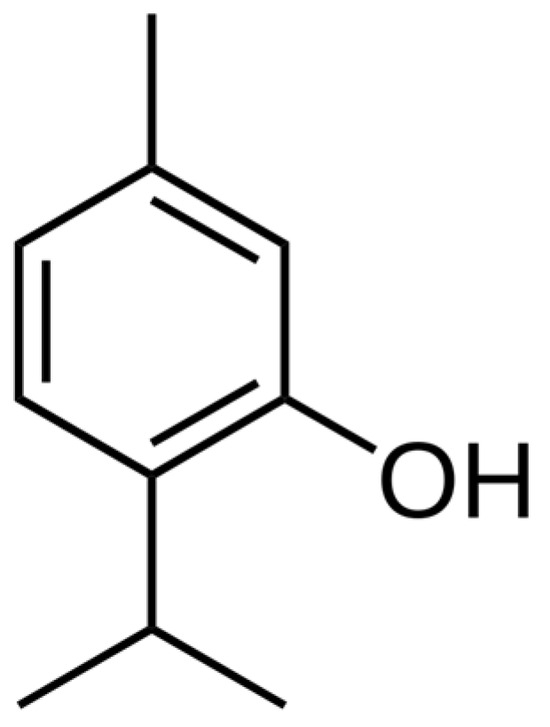
Figure 7.
The structure of thymol.
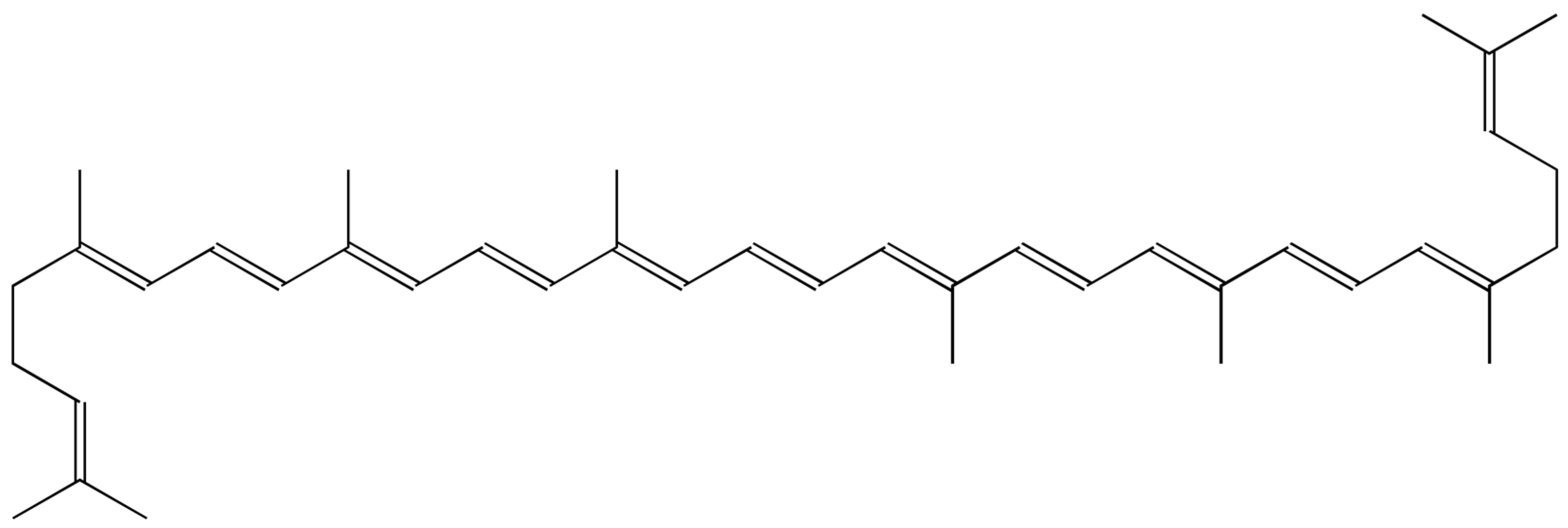
6.2. Carotenoids
Carotenoids are pigments produced by plants. They are the most commonly known to be responsible for the color of tomatoes, carrots, pumpkins, corn, and bananas. We differentiate two classes: oxygen-containing xanthophylls and carotenes. In the first group, we can include lutein and zeaxanthin. We can assign α-carotene, β-carotene, and lycopene to the no-oxygen class. According to Vasudeva et al. [128], lutein showed protection over cytogenetic damages induced by radiation in Swiss albino mice; it also has antioxidant and anti-inflammatory properties. Lycopene (Figure 8) is another carotenoid that manifests radioprotective properties. Pretreatment of mice with lycopene before irradiation reduced radiation sickness and prolonged the lifespan of the animals. Lycopene increased the level of hepatic GSH, GSHpx, and SOD in irradiated rats and also played a protective role for cultured human lymphocytes [129,130]. In the group of carotenoids, there is also a radiosensitizer, crocin, which is a compound of saffron. In the study on head and neck cancer cell line (HN-5), the cells were administered crocin in different concentrations (12.5–1000 µg/mL) and were then irradiated. The substance reduced cell viability, induced apoptosis, and sharpened radiation’s effect [131]. The survival rate of cells treated with crocin is comparable to that of cells treated with amifostine—the only radioprotector clinically approved by the US Food and Drug Administration (FDA) after irradiation with a dose of 6 Gy. Crocin resulted in significant prevention of radiation-induced damage in peripheral blood cells.
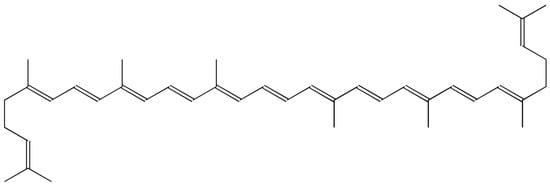
Figure 8.
The structure of lycopene.
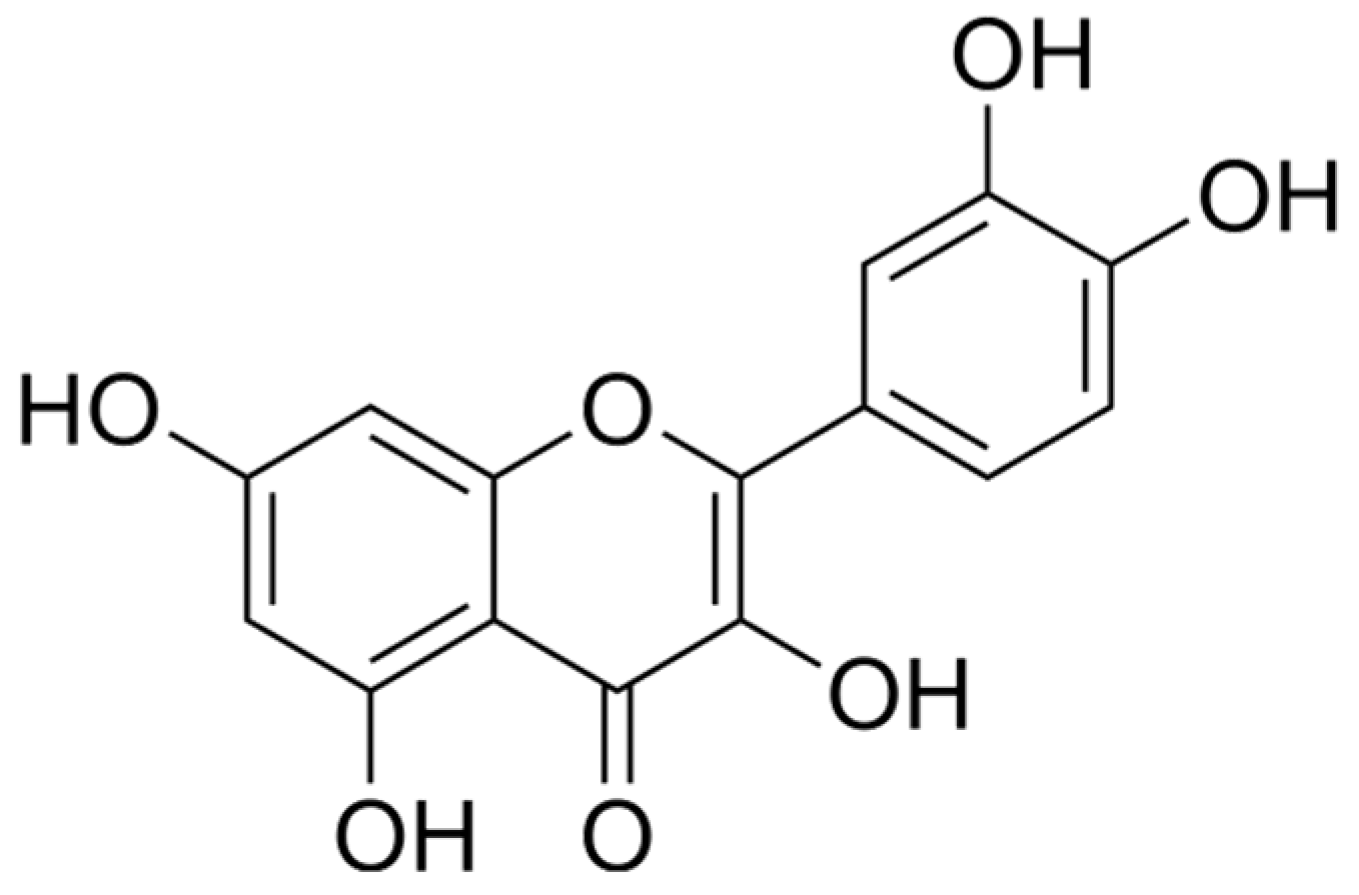
6.3. Flavonoids
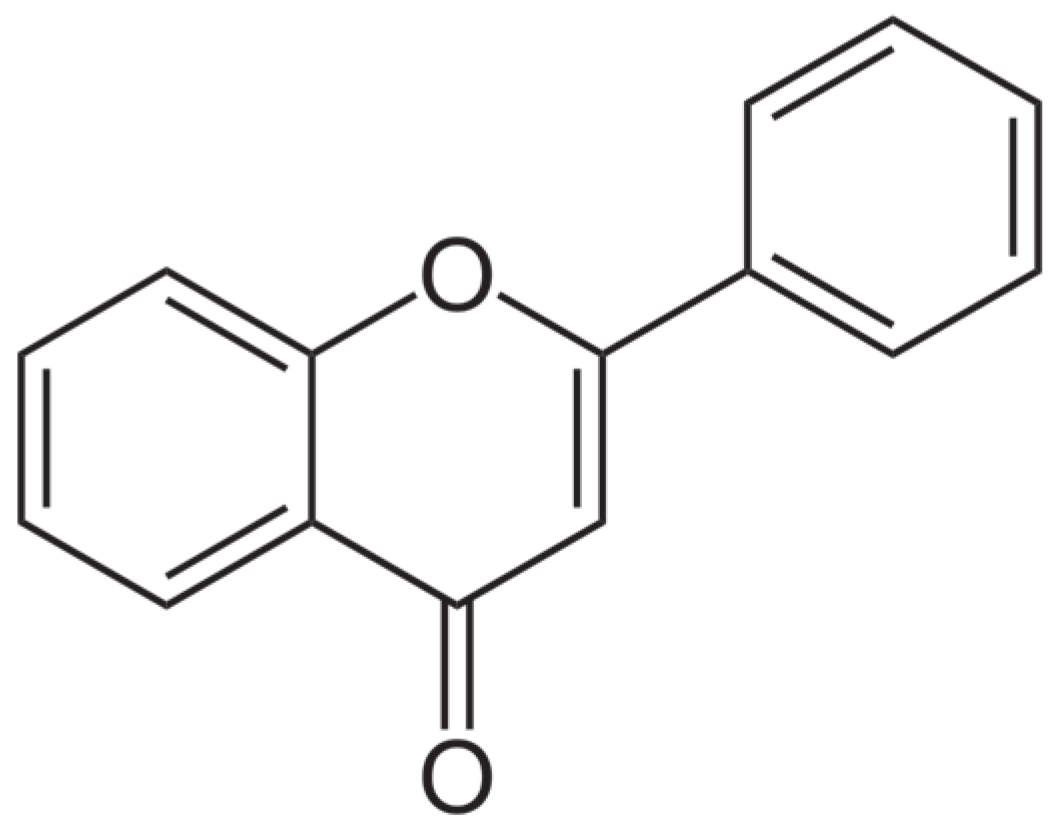
Flavonoids have a structure of a 15-carbon skeleton that consists of two benzene rings (Figure 9). They might occur in a free form as hydrophobic aglycone or as a combination of aglycone with a sugar–glycoside (C-glycoside or O-glycoside), which is soluble in water. They are present in many fruits and vegetables, green and black teas, red wine, beans, and grains. They have an influence on the human body in various directions. Flavonoids are anti-inflammatory, antibacterial, antimutagenic, antioxidant, and helpful in treating cardiovascular diseases [26,132]. They inhibit cyclo-oxygenase, lipoxygenase, acetylcholinesterase, and butyrylcholinesterase [133,134,135]. Depending on the structure, flavonoids consist of flavanones, flavones, flavonols, isoflavonoids, and chalcone.
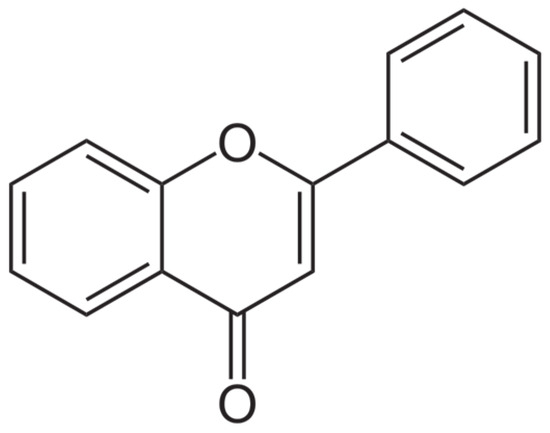
Figure 9.
The general structure of the 15-carbon skeleton of flavonoids.
6.3.1. Hesperidin
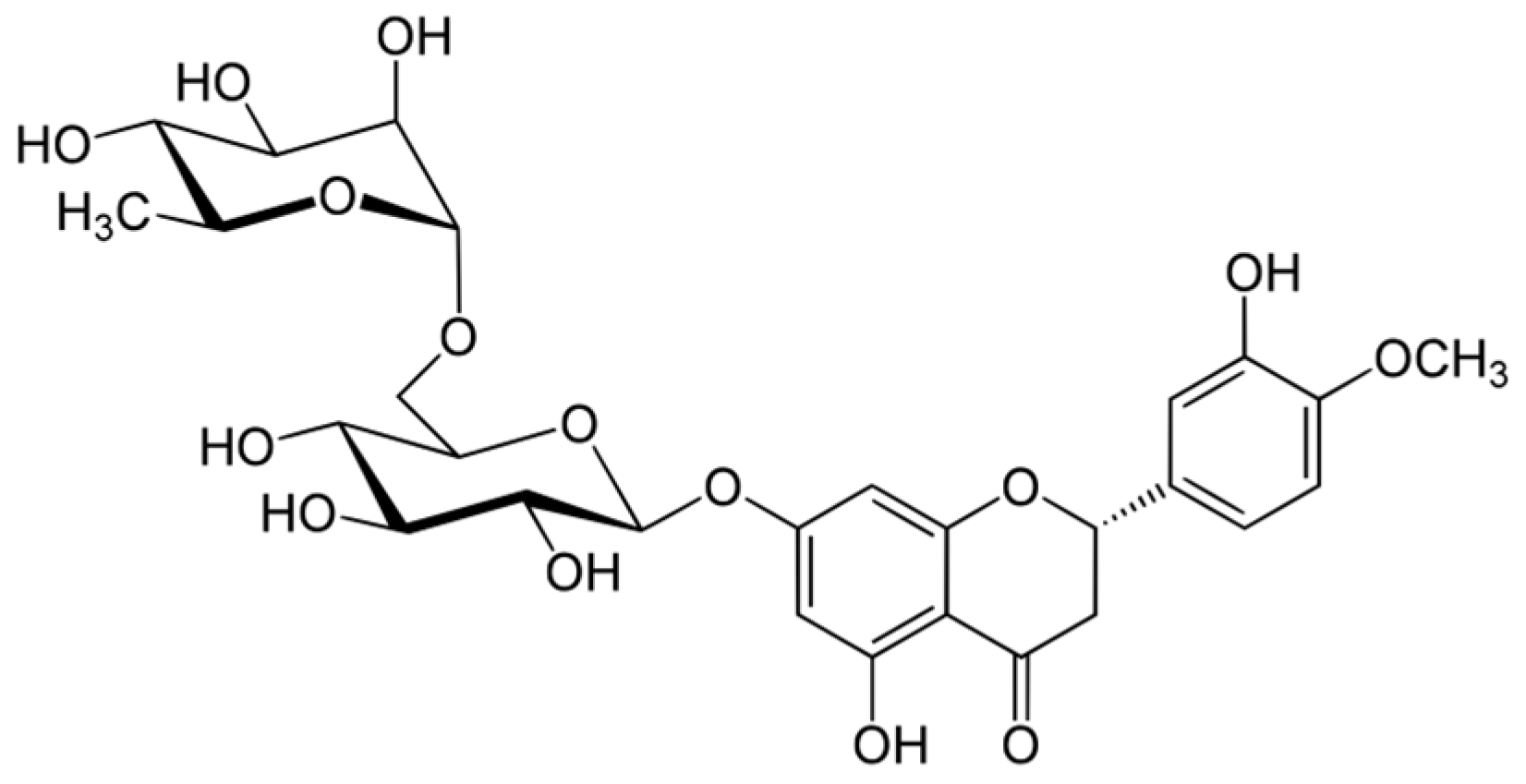
A flavanone, hesperidin (Figure 10), is found in citrus fruits. The administration of hesperidin decreased inflammation, fibrosis, and myocyte necrosis in rats [13,136]. Unfortunately, it did not reduce myocardial degeneration or vascular leakage [13].
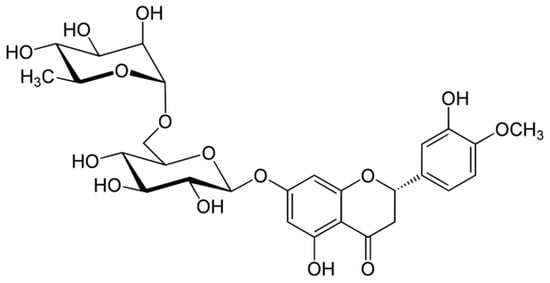
Figure 10.
The structure of hesperidin.
The article by Musa et al. [137] provides a comprehensive review of the potential radioprotective effects of hesperidin. The systematic review explores hesperidin’s antioxidant, anti-inflammatory, and antiapoptotic abilities as a potential radioprotective agent against IR-induced damage. In one of the studies on mice, liver hesperidin was administered intragastrically before irradiation, which increased the level of antioxidant enzymes and reduced DNA damage [138]. The wounds on irradiated mice contract later, slower, and healing takes longer. The synthesis of fundamental wound healing components, DNA, collagen, hexosamine, and NO were declined. Pretreatment of mice with (100 mg/kg body mass) hesperidin before γ-radiation resulted in faster recovery of mice wounds; it contracted more, and it shortened the time of the process. The synthesis of essential wound healing factors determined in the study was increased in these mice. Moreover, the density of blood vessels and fibroblasts in the wounds was greater in hesperidin-treated mice [139]. The volunteers took 250 mg of hesperidin once; then, the blood was withdrawn at different time points and irradiated. Every blood sample had an increased level of micronuclei; however, hesperidin intake before irradiation reduced it. The most efficient change was reported for the blood sample withdrawn one hour after hesperidin consumption. The results underline the possibility of lymphocyte protection against genotoxicity with hesperidin [140]. In the study conducted by Haddadi et al. [136], the initiation of angiogenesis was observed through the induction of the VEGF gene. This process stimulated epithelialization, promoted collagen deposition, and enhanced cellular proliferation. These effects collectively contributed to the facilitation of wound healing and provided protective mechanisms against radiation-induced damage to the skin.
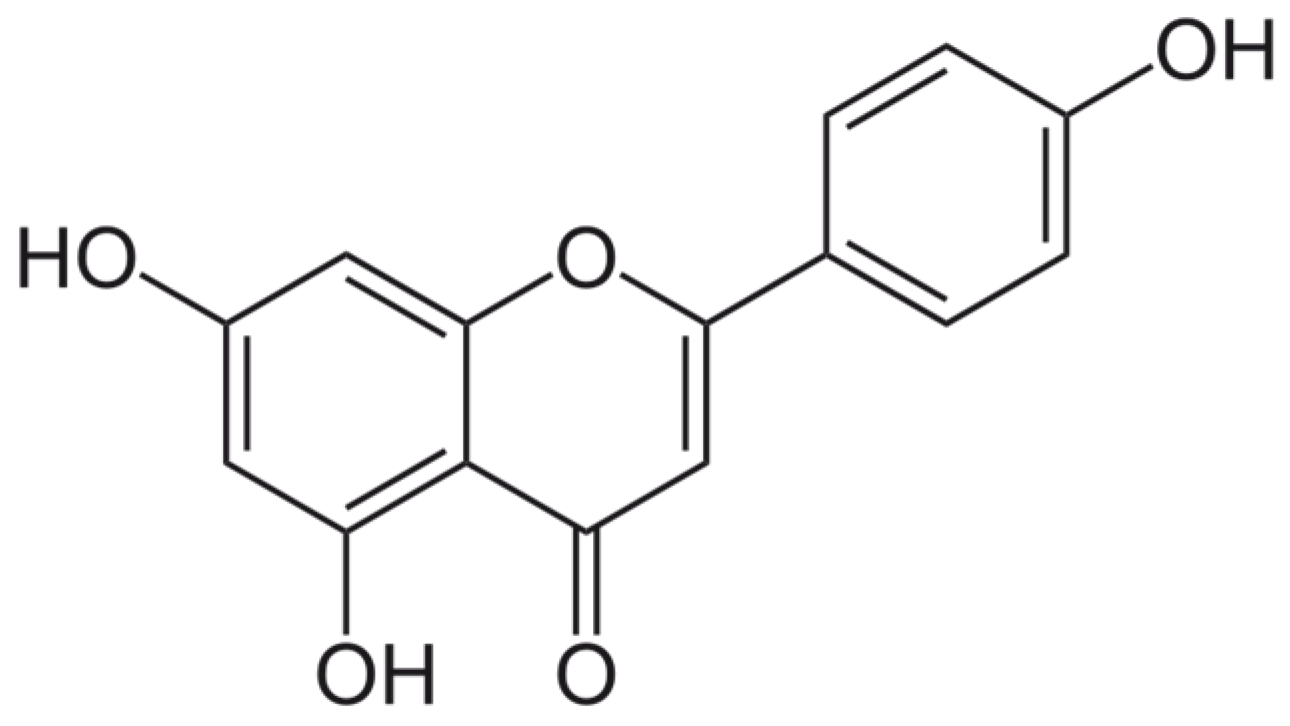
6.3.2. Apigenin
In the subgroup of flavones, apigenin (Figure 11) is a ROS scavenger; it reduces clastogenic post-radiation effects and decreases hematological damage [44,45]. The human peripheral blood lymphocytes were treated with apigenin an hour before irradiation. It reduced the ROS level and decreased the apoptosis frequency in cells. Moreover, it is opposed to decreased mitochondrial membrane potential in human peripheral blood lymphocytes. It influences antioxidative enzymes—apigenin increases the level of GSH, CAT, and SOD. It protects from lipid peroxidation and micronuclei formation in irradiated lymphocytes.
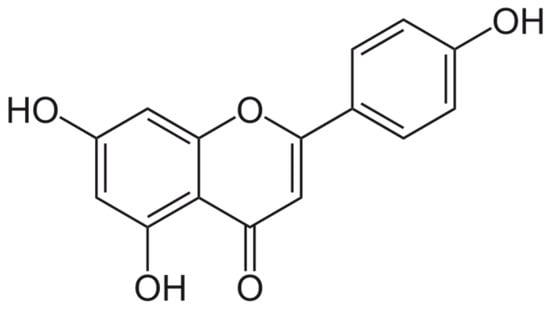
Figure 11.
The structure of apigenin.
Furthermore, it enhanced the expression of Bcl-2 and lessened the expression of p53, p21, Bax, and NF-kB. As a potent antioxidant, apigenin protects human peripheral blood lymphocytes from radiation-induced injuries [56]. In a study on radiation-induced intestinal injury (RIII), apigenin, a natural flavone, has significantly improved survival in C57 mice after lethal irradiation [141]. Apigenin pretreatment expedited the restoration of the crypt–villus structure, enhancing crypt regeneration, epithelial cell differentiation, and increased villus length. Mechanistically, apigenin demonstrated neuroprotective potential by upregulating Nrf2 and HO-1, reducing oxidative stress, and promoting intestinal crypt cell proliferation while inhibiting apoptosis.
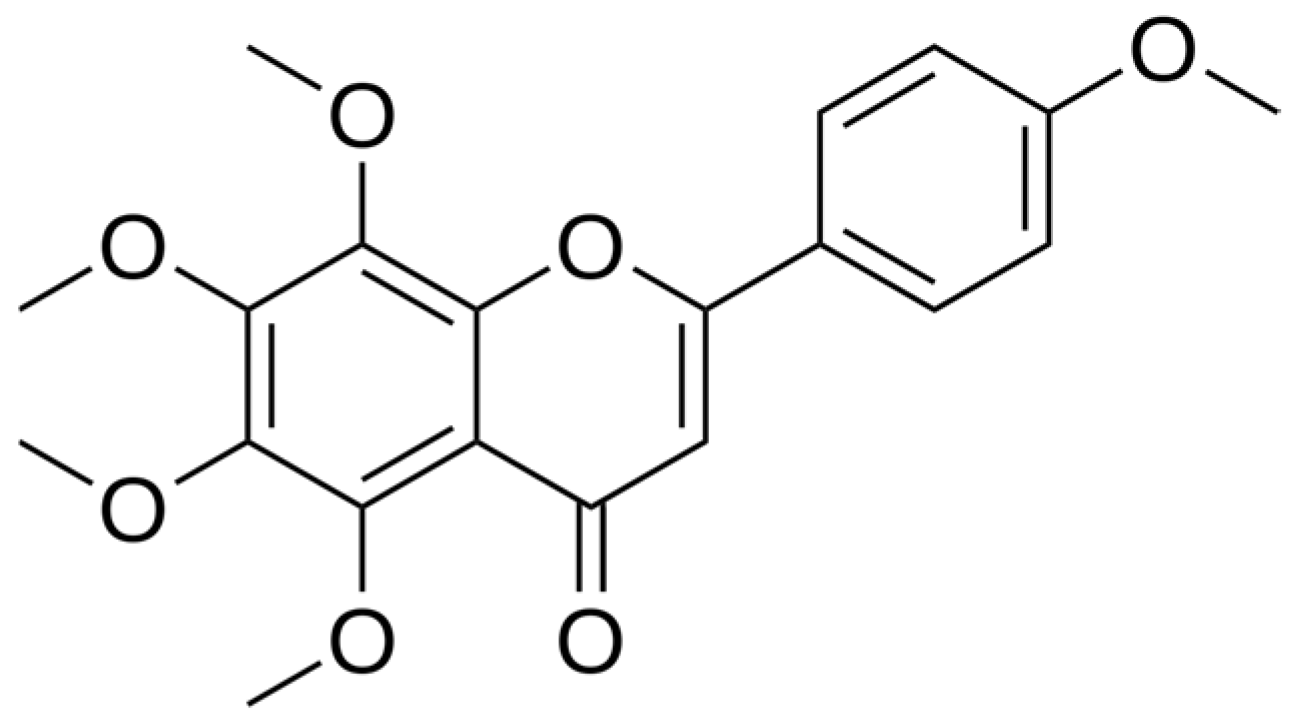
6.3.3. Tangeretin
Tangeretin (Figure 12) is an antioxidant that induces apoptosis in human leukemia cells. It upregulates a suppressor of tumor microRNA—miR-410. Moreover, repeated expression of miR-410 results in counteraction of radiation-induced epithelial–mesenchymal transition. Tangeretin is a radiosensitizer of gastric cancer cells and an antimetastasis agent [142]. Luteolin is a potent antioxidant; it upregulates Bax and decreases the expression of Bcl-2. It induces apoptosis in HT-29 colon cancer cells by promoting antioxidant properties and activating MAPK signaling. It increases the level of GSH and antioxidative enzymes like synthetase GSH and CAT [143]. In the study, the mice were intragastrically administered luteolin (5 mmol/kg) 6 h before γ-radiation [144]. Next, the micronucleated reticulocytes in peripheral blood were measured. Luteolin turned out to be an antioxidative and anticlastogenic agent. Surprisingly, luteolin generates ROS after exposure to X-ray and UV radiation like O2 [145].
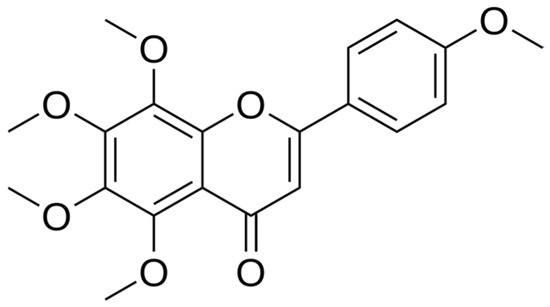
Figure 12.
The structure of tangeretin.
6.3.4. Quercetin
Flavonols like quercetin (Figure 13) and glucosides, such as rutin, are radioprotective factors. Pretreatment of mice with these substances before gamma radiation resulted in the elevation of the level of antioxidative enzymes like GSH, CAT, and SOD, and lipid peroxidation was reduced [146]. Moreover, quercetin protects white blood cells and DNA from post-radiation damage [147]. In the in vitro study, pretreatment of lymphocytes with rutin before gamma radiation reduced the number of micronuclei protecting white blood cells. There was also a decline in DNA damage according to the determination of percent tail DNA and olive tail moment [146]. Rutin’s derivate, troxerutin, administered prior to gamma irradiation increased the activity of antioxidative enzymes of the liver and reduced the damage that radiation caused to the organ [148]. Troxerutin reduces radiation-induced lipid peroxidation in the liver and spleen in normal cells; it also protects from DNA damage according to the determination of the percentage of DNA in white blood cells and bone marrow [149]. The 30-day survival after gamma irradiation was determined in the study conducted in mice. Troxerutin turned out to be a radioprotector depending on the dose; it significantly elevated the survival of the animals [150].
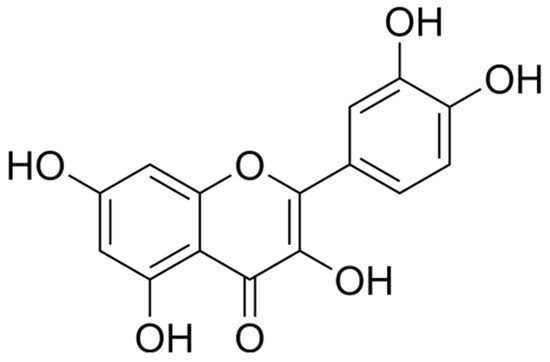
Figure 13.
The structure of quercetin.
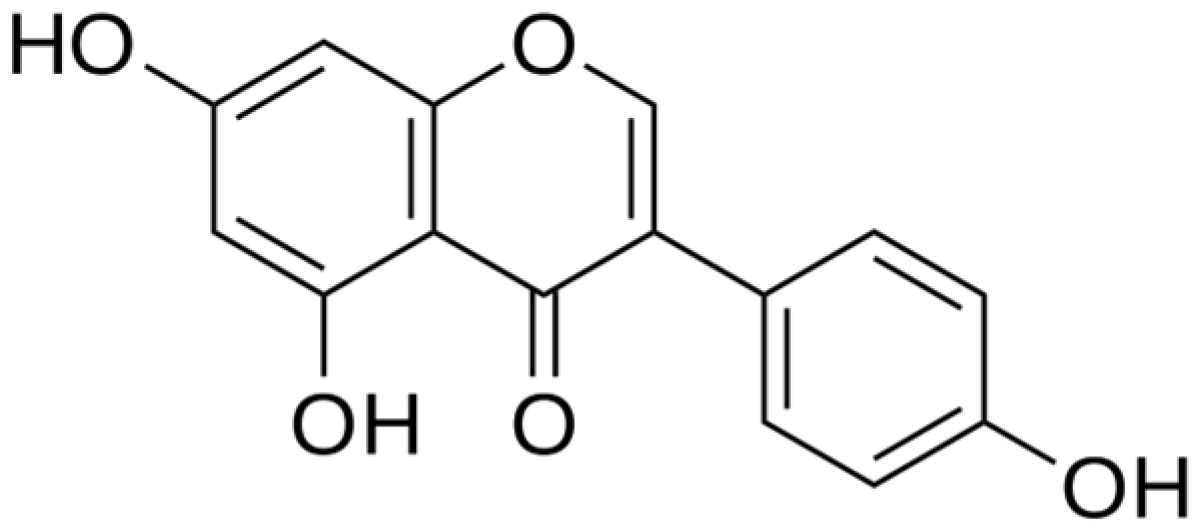
6.4. Isoflavonoids
Genistein, an isoflavonoid (Figure 14), shows dose-dependent effects on the human liver cell line. In concentrations of 1.5 µM, as a radioprotectant, it inhibited apoptosis and reduced DNA damage, and in concentrations of 20 µM and 40 μM, it played the role of radiosensitizer [151]. Moreover, genistein administered 24 h before gamma irradiation in mice elevated the survival of the animals [99]. The isoflavonoid reduced the increase in breathing rate in rats post radiation during early pneumonitis. Moreover, the animals survived longer than just the irradiated group. It also declined TNF-α, IL-1β, and TGF-β levels and protected rats’ DNA. However, treatment with genistein did not prevent animals’ death; it only delayed it. Genistein at 200 mg/kg administered to mice one day prior to irradiation resulted in a reduction in tubular atrophy compared to the only radiated group. Moreover, the post-radiation elevated malondialdehyde level was lowered due to genistein [152].
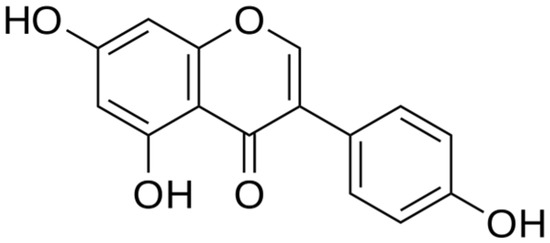
Figure 14.
The structure of genistein.
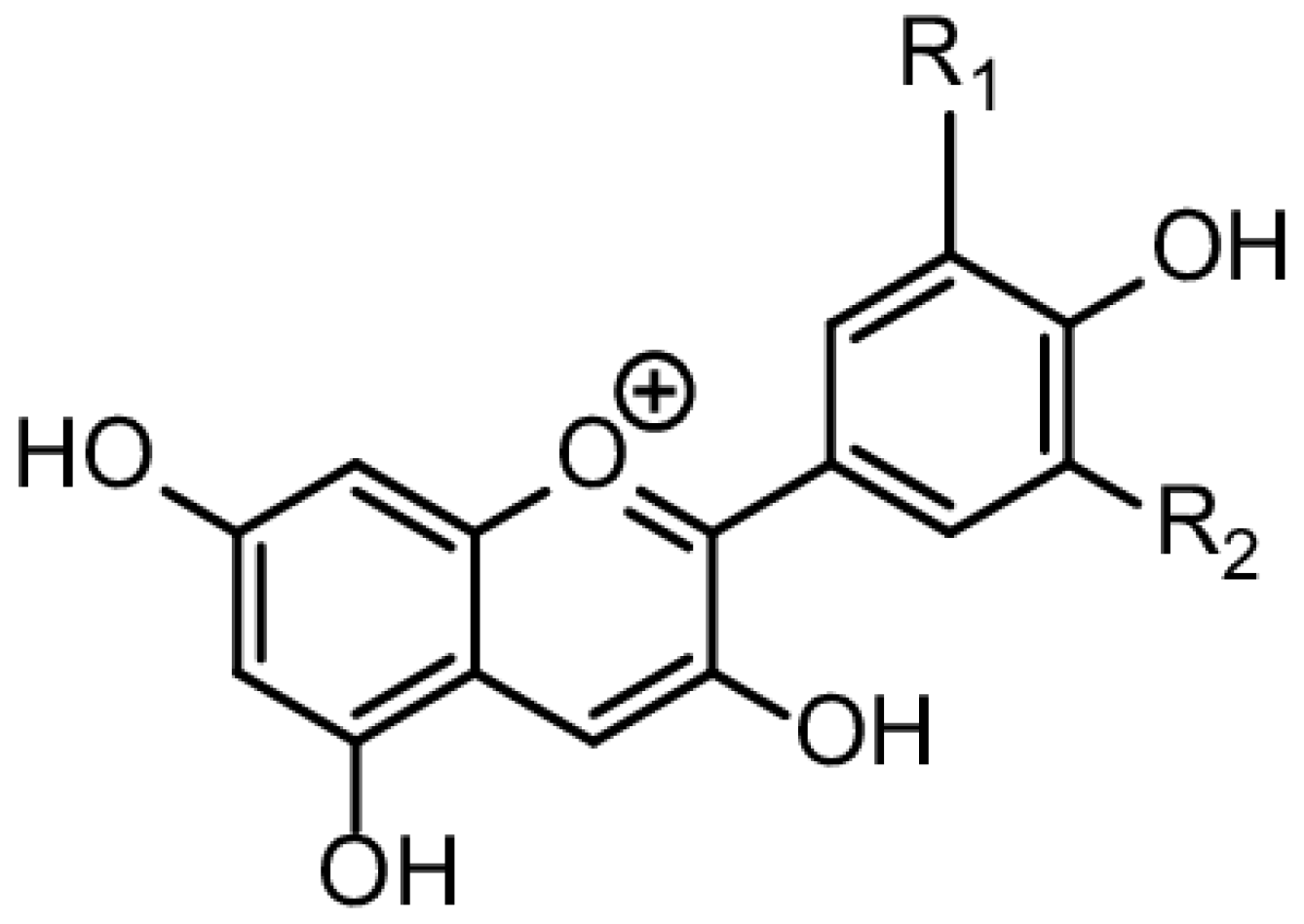
6.5. Anthocyanins
Anthocyanins, a type of phytochemical found in various fruits (Figure 15), have been studied for their potential radioprotective effects. Fan et al. [153] demonstrated that anthocyanin-rich extracts from lingonberries effectively mitigated radiation-induced damage in mice without causing acute toxicity. Similarly, anthocyanins extracted from Vaccinium Vitis-idea L fruits showed radioprotective properties in a preclinical in vivo study [154]. Moreover, the anthocyanins present in date syrup were attributed to its radioprotective effect on DNA, along with other constituents like proanthocyanidins, β-carotene, and selenium [155].
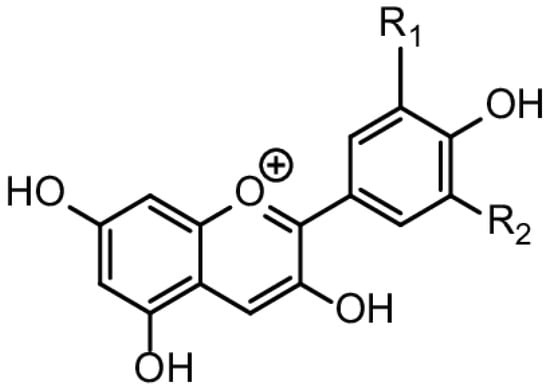
Figure 15.
The structure of anthocyanins.
Studies have also explored the radioprotective effects of anthocyanins against different types of radiation. While Fan et al. [153] focused on IR, Kim et al. [69] mentioned the radioprotective effects of delphinidin, a type of anthocyanin, against proton beam exposure.
Overall, anthocyanins have shown promise in providing radioprotective benefits, potentially due to their antioxidant properties. These compounds have been associated with mitigating radiation-induced damage, protecting against DNA double-strand breaks, and enhancing cell survival post radiation exposure. The diverse sources of anthocyanins, ranging from lingonberries to Vaccinium Vitis-idaea L fruits, highlight the potential of these phytochemicals in offering radioprotective effects. The antioxidant activity of anthocyanins involves processes such as hydrogen atom transfer (HAT) or single-electron transfer (SET), enabling them to scavenge radiation-induced ROS [69]. These mechanisms help mitigate oxidative stress and DNA damage caused by radiation exposure, contributing to the radioprotective characteristics of anthocyanins.
Moreover, the radioprotective effects of anthocyanins may involve modulating inflammatory responses and cellular toxicity induced by radiation. Anthocyanins act as radioprotective agents by targeting the oxidative stress response and inflammation pathways, enhancing cellular resilience against radiation-induced damage [156,157]. Encapsulating anthocyanins in nanocarriers enhances their radioprotective capabilities by prolonging their retention time and ensuring sustained protection against radiation-induced oxidative stress [158].
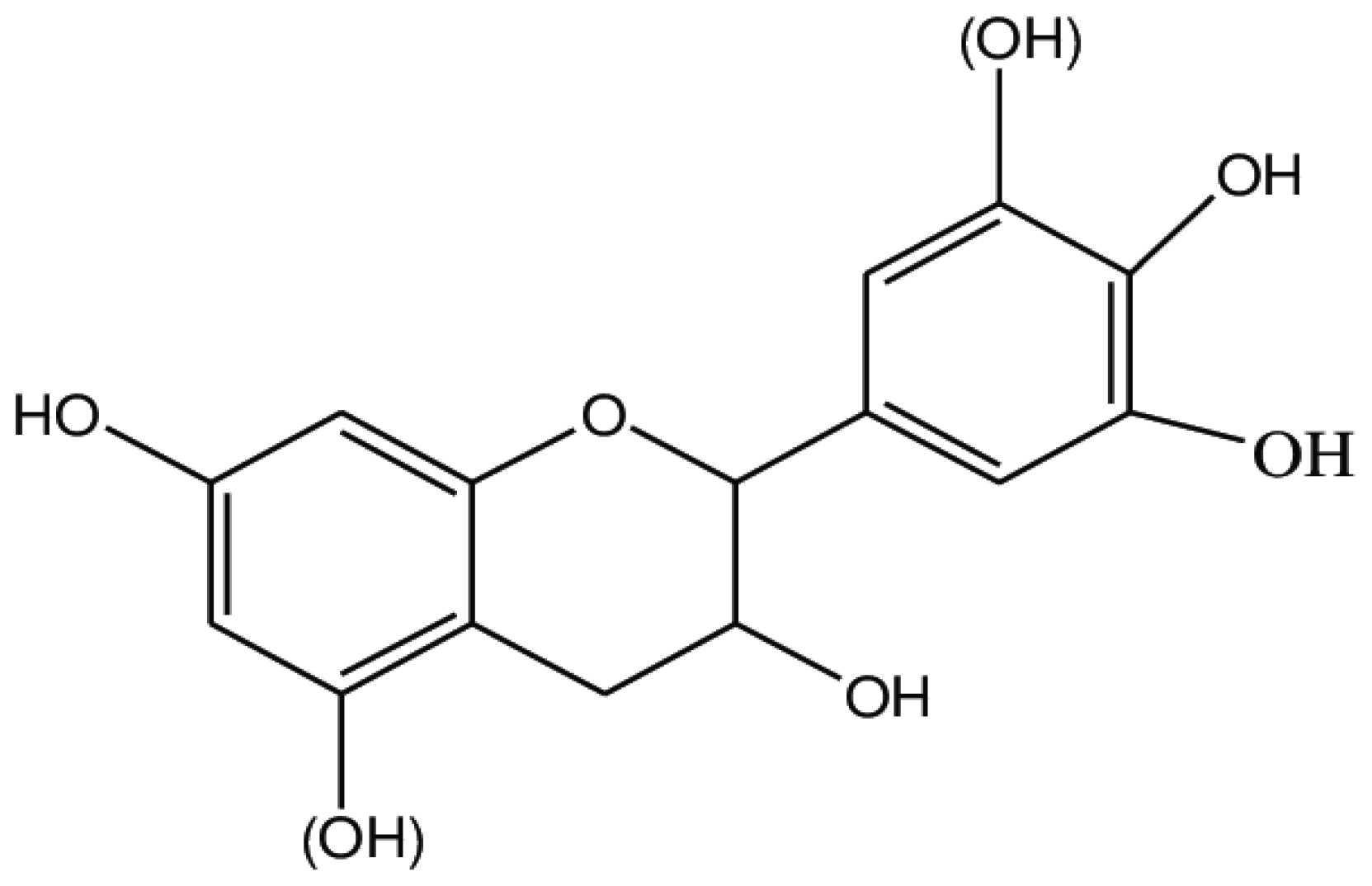
6.6. Tannins
Tannins are polyphenolic (Figure 16), water-soluble compounds that precipitate proteins and amino acids. They have antimicrobial, anti-inflammatory, and antimutagenic properties and they might be helpful in a topical application on the skin according to their astringency [159,160]. Oral administration of 100 mg/kg body weight of gallic acid to mice before gamma irradiation increased the level of GSH, decreased DNA damage, and inhibited lipid peroxidation [161]. Persimmon tannin from Diospyros kaki L.f. was studied in the radioprotective direction. Pretreatment of human embryonic kidney 293T cells with persimmon tannin before gamma-radiation increased cell viability, reduced apoptosis, and reduced ROS levels [162]. Chinese hamster lung fibroblasts were gamma radiated, but before that, they were pretreated with geraniin, another tannin, isolated from Nymphaea tetragona [163]. The tannin reduced the level of ROS, increased the activity of antioxidative enzymes such as SOD and CAT, and reduced cell apoptosis. Substances from this group may be radioprotectants and radiosensitizers like ellagic acid. Ellagic acid increases oxidative stress in cancer cells. After administration of 10 µM of the substance 12 h before the radiation of the human hepatocellular carcinoma cell line—HepG2, the generation of ROS was increased, it upregulated p53, apoptosis of the cells was increased, and the survival markers were worse, like phosphorylated Akt, phosphorylated NF-kB, and phosphorylated STAT3, compared to only radiated cells. Combining radiotherapy with ellagic acid administration might result in using lower doses of radiation [164].
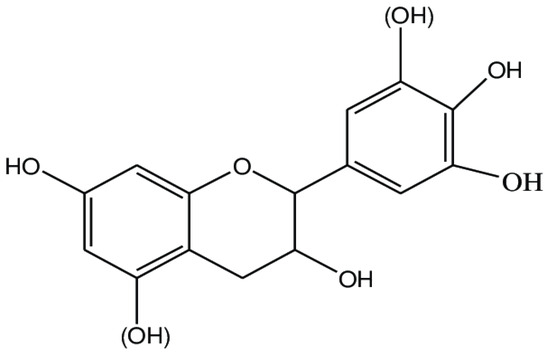
Figure 16.
Structure of flavonoid unit of condensed tannins.
The quinones are cyclic, unsaturated organic compounds that are known for aperient, antimicrobial, and antiparasitic properties; they also have antioxidant and antitumor activity, and they might prevent cardiovascular diseases and osteoporosis [165,166,167]. Pyrroloquinoline quinone, which presents naturally in soil and kiwifruit, takes part in a variety of physiological processes such as cellular energy metabolism, antioxidation, redox reactions, and mitochondrial biogenesis in muscles [168]. Pyrroloquinoline quinone showed radioprotective activity on X-ray irradiated mice on their parotid glands due to reduction in DNA damage and ROS scavenging and inhibition of apoptosis [169]. In another study, administering pyrroloquinoline quinone to mice accelerated the recuperation of leukocytes, reticulocytes, and bone marrow cells after radiation [170]. The quinone increased the survival of gamma-radiated mice and expedited hematopoietic recovery. In vitro gamma radiation enhanced lipid peroxidation and increased nitric oxide and hydroxyl radicals. However, hydroquinone inhibited the process and scavenged the harmful radicals [171].
6.7. Alcaloids
Plant alkaloids, a diverse group of natural compounds, can be classified into various classes based on their chemical structures (Figure 17). These include indole alkaloids, isoquinoline alkaloids, tropane alkaloids, quinoline alkaloids, pyrrolidine alkaloids, piperidine alkaloids, and purine alkaloids. Each class exhibits unique properties, contributing to the pharmacological diversity of these plant-derived compounds [172]. Pretreatment of mice with sanguinarine (present, e.g., in Sanguinaria sp., Argemone sp., and Chelidonium majus) prolonged the survival of animals after radiation. Moreover, it decreased intestinal and lung damage [173]. Intake of the imidazole derivate pilocarpine (Piolocarpus sp.) helped patients to increase salivary flow and decrease xerostomia [174]. The most commonly known alkaloid, caffeine, is present in coffee, tea, and cacao.
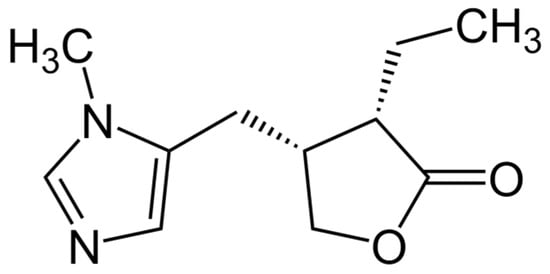
Figure 17.
The structure of pilocarpine.
6.8. Coumarins
Coumarins classified as benzopyrone derivates (Figure 18) are poorly soluble in water but soluble in alcohol and lipids. In vitro, pretreatment with umbelliferone in isolated human blood lymphocytes inhibited ROS, increased the activity of antioxidant enzymes, and reduced lipid peroxidation apoptosis [175]. The coumarin isofraxidin shows radioprotective properties in human leukemia cell lines by decreasing ROS generation; it is opposed to the decrease in mitochondrial membrane potential; and it reduces the expression of Bax in mitochondria [176]. The antiangiogenic synthetic isocoumarin, NM-3, combined with radiotherapy in mice with Lewis lung carcinoma, reduces the tumor volume compared to radiation alone [177].
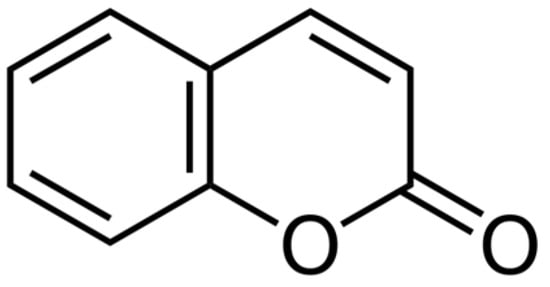
Figure 18.
The basic structure of coumarins.
The radiochemical study of the antioxidant activity of biologically essential compounds from plant materials revealed that unsubstituted coumarin exhibited more significant radioprotective activity [178]. It additionally demonstrated the radioprotective potential of interruptin C, a coumarin-derived compound, in protecting normal breast MCF-10A and HaCaT cells against radiation-induced damage [70]. Furthermore, researchers investigated the inhibitory effect of coumarin on the germination of ryegrass and its potential application as coumarin–carbon dots nanocomposites, suggesting its potential as an herbicidal agent [179].
Moreover, it highlighted the antioxidant activity of coumarin, emphasizing its potential role in combating radiation-induced inflammation [180]. It additionally explored the radioprotective effect of whey hydrolysate peptides against γ-radiation-induced oxidative stress in BALB/c mice, providing insights into the potential radioprotective properties of coumarins [181]. Furthermore, Sharapov et al. [182] investigated the radioprotective role of peroxiredoxin 6, shedding light on its potential mechanisms of action.
7. Plant Materials
7.1. Glycyrrhiza glabra
Glycyrrhiza glabra, family Fabaceae, comes from South Europe and Asia. It is an expectorant, antiulcer, slightly laxative, antioxidant plant [183]. The plant might be used to prevent and treat oral mucositis connected with radiation cancer treatment [184]. The study by Mamgain et al. [185] investigates the efficacy of Glycyrrhiza glabra on radiation-induced mucositis in head-and-neck cancer patients. Glycyrrhiza glabra was observed to be effective and delayed the development of a severe form of mucositis. Glycyrrhizin, derived from licorice root, demonstrates significant protective effects against radiation-induced damage in submandibular glands (SMGs). It reduces oxidative stress, downregulates high mobility group box-1/ toll-like receptor 5 (HMGB1/TLR5) signaling, and preserves mitochondrial integrity, ultimately inhibiting apoptosis. Glycyrrhizin could serve as a promising mitochondria-targeted antioxidant to prevent radiation sialadenitis in head-and-neck cancer patients undergoing radiotherapy [186]. The root extract decreased lipid peroxidation in microsomal membranes of rat liver induced by gamma radiation [187]. Albino rats treated with licorice and then irradiated presented counteraction to radiation-induced decrease in GSH, SOD, and CAT; it also decreased the level of triglyceride and total cholesterol [188]. Glycyrrhizic acid protects human leukocytes from gamma radiation-induced DNA damage, depending on the concentration of the substance. Moreover, in the study on mice administered intraperitoneally with glycyrrhizic acid, the compound counteracted the strand break in the DNA of white blood cells and bone marrow cells [189]. Silver nanoparticles, in conjunction with glycyrrhizic acid, exhibit enhanced capability in safeguarding cellular DNA from harm caused by IR. The heightened protective efficacy of this compound, in contrast to individual silver nanoparticles or glycyrrhizic acid, may be attributed to the combined free-radical scavenging properties inherent in both glycyrrhizic acid and silver nanoparticles within the complex [190].
7.2. Aloe barbadensis
Aloe barbadensis, family Asphodelaceae, can be found in dry regions of various continents: Africa, America, Asia, and Europe. The plant is commonly used in cosmetics. It has healing, moisturizing, and anti-inflammatory properties according to the polysaccharide, auxin, and gibberellin content, and is a laxative due to antra-compounds, and has antiseptic properties due to saponins, salicylic acid, and lupeol [191]. Aloe vera leaf ethanolic extract administered in mice decreased lipid peroxidation and increased the concentration of reduced GSH after gamma radiation due to antioxidant and radical-scavenging properties [192]. In patients, a lotion containing Aloe vera decreases post-radiation inflammation of the skin [193]. To investigate the potential radioprotective effects of Aloe vera, Dadupanthi et al. [194] focused on the hepatosomatic index of Swiss albino mice. The research concluded that Aloe vera extract could indeed offer protection against radiation-induced oxidative stress, suggesting its ability to mitigate the harmful effects of radiation therapy.
Similarly, Nejaim et al. [195] examined the radioprotective properties of Aloe vera and zinc/copper compounds on salivary dysfunction in irradiated rats. Their findings supported the effectiveness of Aloe vera extract in treating radiation-induced burns, indicating its potential as a radioprotective agent. Furthermore, Liu et al. [196] explored the impact of a persimmon tannin–Aloe vera composite on cytotoxic activities and radioprotection against X-ray irradiation in specific cells. The tested composite shows promising radioprotective properties, protecting liver cells (L02 and HepG2) from the harmful effects of IR. PT-A effectively reduces apoptosis and produces ROS, showing better efficacy than the single components, persimmon tannin and Aloe vera.
7.3. Mentha piperita
Mentha piperita, family Lamiaceae, is a cross between Mentha aquatica and Mentha spicata, which nowadays is familiar and widespread. The most frequent use of the leaves is for gastrointestinal tract problems; they have anti-inflammatory, antioxidant, and antimicrobial properties [197,198]. Research by Jagetia and Baliga et al. [199] investigated the impact of Mentha arvensis leaf extract on the survival of mice exposed to varying doses of gamma radiation. The study demonstrated a positive effect on the survival rate of mice, suggesting that mint extract could protect against the harmful effects of radiation exposure. In another study, post-radiation damages were alleviated by M. piperita extract. The number of red and white blood cells was elevated, the level of GSH was raised, lipid peroxidation was reduced, and the weight of animals was increased compared to only radiated animals [200]. The radioprotective properties of Mentha piperita leaf extract were studied in mice testis, and its weight was raised in the group of animals not only radiated but also pretreated with extract; there was a normalization of the level of alkaline phosphatase in tests, the damage in the seminiferous epithelium was smaller in this group [201]. Mentha piperita administered before radiation in mice also decreased chromosomal damage in the bone marrow and increased the activity of antioxidant enzymes [202]. Not only is Mentha piperita a radioprotector, but Mentha arvensis also plays this role. The administration of 10 mg/kg of mint chloroform extract to mice exposed to gamma radiation prolonged the life of the animals. It protected mice from gastrointestinal and bone marrow deaths. The substance is not toxic up to the concentration of 100 mg/kg body mass [199].
The radioprotective mechanism of mint, particularly Mentha arvensis, has been explored in a study by Baliga and Rao [203]. The research suggests that the radioprotective effects of mint may be attributed to various factors, including free radical scavenging, antioxidant properties, metal chelation, anti-inflammatory effects, antimutagenic activity, and enhancement of DNA repair processes. These mechanisms collectively contribute to the ability of mint to protect against radiation-induced damage and mitigate the complications associated with radiation therapy. By scavenging free radicals, mint may help reduce oxidative stress and cellular damage caused by radiation exposure, offering a natural and effective approach to enhancing the safety and efficacy of radiation therapy.
7.4. Rosemarinus officinalis
Rosemarinus officinalis extract administered to mice for five days before gamma irradiation prolonged the lifespan of the animals. The most efficient dose was 1000 mg/kg body weight. The extract reduced lipid peroxidation and increased the level of GSH in the blood and liver after 8 Gy gamma radiation [204]. Rosemary leaf extract was dispensed in the concentration of 1000 mg/kg to Swiss albino mice, which were later exposed to 3 Gy gamma radiation. The extract-treated animals’ number of erythrocytes, white blood cells, hematocrit percentage, and hemoglobin content were elevated compared to the only radiated group. Furthermore, the GSH level was increased, and lipid peroxidation was decreased in the experimental group [204].
7.5. Ficus racemosa
The next plant, Ficus racemosa, family Moraceae, is used in Ayurveda. There were reported anti-inflammatory, antioxidant, hepatoprotective, and cardioprotective properties [205]. In vitro and in vivo extracts of F. racemosa decreased radiation-induced DNA damage. This extract inhibited activated post-radiation protein p53, which induces apoptosis [206]. Ethanol extract of Ficus racemosa shows antioxidative properties by scavenging superoxide and hydroxyl, 2,2′-Azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS•−), 2,2-Diphenyl-1-picrylhydrazyl (DPPH) radicals and inhibiting lipid peroxidation. Moreover, in the study on Chinese hamster lung fibroblast cells (V79), administration of an extract of Ficus racemose 1 h before γ-radiation decreased the number of micronucleated binuclear cells [207].
7.6. Ginkgo biloba
Ginkgo biloba leaf extract was administered to rats at 40 mg/kg for three days prior to 5 Gy gamma radiation and seven days after. The activity of antioxidant enzymes glutathione reductase and GST was raised, and the scavenging of radicals was noticed compared to the only radiated group of animals [208]. Ginkgo biloba extract (50 mg/kg daily) dispensed to rats for 15 days prior to irradiation prevented the lungs, liver, and kidneys from radiation-induced damage. It reduced malondialdehyde and myeloperoxidase activity and increased the GSH level [209]. Another study studied the radioprotective effect of fermented and not-fermented Ginkgo biloba leaf extract. Both extracts administered for 15 days to rats before gamma irradiation counteracted the decrease in SOD, GSHpx activity, the enlargement of calcium levels in the brain cytosolic fraction, malondialdehyde concentration, and stress hormones levels like epinephrine, norepinephrine, and dopamine. However, fermented Ginkgo biloba leaf extract was more efficient in preventing radiation-induced damage [210].
7.7. Hippophae rhamnoides
Hippophae rhamnoides, family Elaeagnaceae, occurs in Europe and Asia. In traditional medicine, the juice is used to heal wounds and treat ulcers, whereas oil extracts are used in skin disorders [211,212]. In gamma-irradiated rats, leaf extract decreased the level of corticosterone in plasma and the level of serotonin in both jejunum and plasma [213]. Pretreatment of mice with Hippophae rhamnoides berry extract increased the weight of the testis and the sperm count after gamma radiation. The extract might also prevent post-radiation DNA damage [214]. A fraction of Hippophae rhamnoides, rich in flavonoids, has antioxidative properties, scavenges free radicals, and has a significant potential to protect membranes. These properties were ascribed to quercetin, kaempferol, and isorhamnetin. The fraction was not toxic up to 200 mg/kg [215].
7.8. Ocimum sanctum
Ocimum sanctum, family Lamiaceae, is used in Ayurvedic medicine. It shows antioxidant, antidiabetic, antiulcer, and antifungal properties [216,217]. Holy basil decreased mortality in mice after gamma radiation and increased bone marrow stem cell survival [218,219]. Two flavonoids, Ot and Vc, extracted from Ocimum sanctum were injected intraperitoneally (50 mg/kg) into mice and irradiated, reducing the number of chromosomal aberrations in bone marrow cells. Neither Ot nor Vc showed toxicity up to the concentration of 200 mg/kg [83]. Polysaccharides of Ocimum sanctum have antioxidant properties; they decrease lipid peroxidation and protect plasmid DNA. Moreover, they safeguard mouse splenocytes from death [220].
7.9. Emblica officinalis
Emblica officinalis, a plant in the family Euphorbiaceae, is also known as Amla. The plant is used in Ayurveda; there have been reported antioxidative, anti-inflammatory, antimicrobial, antimutagenic, radiomodulatory, and chemomodulatory properties [221,222]. The plant extract or fruit extract administered in mice prior to gamma radiation resulted in an increase in the survival of animals, a decrease in lipid peroxidation, and a rise in GSH levels in the liver, blood, and brain [223,224]. Moreover, the plant extract normalized the activity of serum alkaline phosphatase. The fruit pulp of Amla also increased the survival of mice after gamma irradiation and countered the body weight loss of the animals [225].
7.10. Spinacia oleracea
Spinacia oleracea, family Chenopodiaceae, a plant growing native in south-west Asia, is used in Indian Ayurveda as a laxative, carminative, in asthma, and in leprosy [226,227]. S. oleracea extract protected the mice’s liver against gamma radiation by decreasing lipid peroxidation and increasing the GSH concentration [228]. In another study, the radioprotective potential of Spinacia oleracea was tested. The administration of 1100 mg/kg spinach extract to mice 15 days before gamma irradiation decreased lipid peroxidation in the testis, according to its antioxidant activity. Moreover, it also modulates protein, cholesterol, and glycogen values [229].
7.11. Panax ginseng
Panax ginseng, belonging to the Araliaceae family, shows various properties like reducing blood glucose, reducing inflammation, and enhancing vitality [230,231]. The root extract of P. ginseng prolonged the lifespan of irradiated mice and countered body weight loss of the animals and damage to the germ cells [232]. Administration prior to irradiation caused a decline in acid phosphatase and lipid peroxidation in mice testes [108]. In another study, the plant showed radioprotective properties to jejunal crypts of mice and inhibited apoptosis [233]. The intake of hydro-alcoholic extract of Panax ginseng by Swiss albino mice five days before gamma radiation resulted in increased survival of the animals, and it counteracted weight loss.
Furthermore, it influenced oxidative stress markers like SOD, CAT, and GST; it also reduced lipid peroxidation in the blood and liver [234]. Panax ginseng root extract was dispensed to mice prior to 6 Gy gamma irradiation. After only radiation, parameters like erythrocyte, haematocrit values, and haemoglobin concentration were decreased, and there was also an increase in lipid peroxidation in the blood and liver. Pretreatment with the extract alleviated all these parameters; moreover, the GSH level in serum and in the liver was increased [235].
7.12. Moringa oleifera
Moringa oleifera, family Moringaceae, originally comes from India. The plant exhibits antioxidant, antidiabetic, anticancer, antiulcer, and neuroprotective properties [236,237]. M. oleifera leaf methanolic extract injections protected mice bone marrow against post-radiative damage. Due to the administration of the extract, after gamma beams, there was a decrease in chromosomal aberrations in the bone marrow cells of mice. M. oleifera leaf extract protected mice liver cells against radiation-induced lipid peroxidation and increased the concentration of reduced GSH [238]. According to the Sinha et al. [239] study, pretreatment of mice with M. oleifera leaf extract before irradiation resulted in increases in the activity of antioxidant enzymes like SOD, CAT, and GSH, and in the decline in lipid peroxidation and displacement of NF-κB from cytoplasm in the mice’s liver.
Pradana et al. [240] demonstrated that Moringa oleifera extract induced the generation of ROS in epidermoid carcinoma KB cells, suggesting its potential as a radioprotective agent. Additionally, Wang et al. [241] highlighted the antimicrobial activity of Moringa oleifera, which could contribute to its radioprotective effects by preventing secondary infections post radiation exposure.
7.13. Mesua ferrera
Mesua ferrera, family Clusiaceae, also named Nagakesara, is used in Ayurveda, Unani and Siddha. The plant has hepatoprotective, antispasmodic, analgesic, antimicrobial, and antiulcer properties [242]. Studies have shown that extracts of Mesua ferrea exhibit antioxidant activity through various assays like DPPH radical-scavenging and ferric reducing power assays, along with anti-inflammatory effects demonstrated by proteinase inhibitor and albumin denaturation assays [243]. Furthermore, Mesua ferrea has been found to enhance the activity of antioxidant enzymes, reduce MDA levels, and protect organs such as the liver, kidney, and spleen from gamma radiation-induced damage [244].
7.14. Spatholobus suberectus
Spatholobus suberectus, family Fabaceae, presents wound healing, antioxidative, antiplatelet, antiapoptotic, and anti-inflammatory properties [245,246]. The post-radiation intake of ethanol extract from the plant ameliorated the number of red blood cells, white blood cells, platelets, hemoglobin, and bone marrow cells. The expression of protein Bcl-2 in bone marrow was increased; therefore, apoptosis was inhibited. The levels of antioxidative enzymes were augmented, and the increase in malondialdehyde concentration was countered [247].
7.15. Camelia sinensis
Camelia sinensis extract is rich in polyphenols, has antioxidative properties, scavenges free radicals, and inhibits lipid peroxidation. The water extract counteracted 100% of radiation-induced strand breaks in pBR322 plasmid DNA at an 80 μg/mL concentration. Moreover, in the study on the V79 cell line, it reduced the number of micronucleated cells and the amount of ROS; it also returned the integrity to the potential of the mitochondrial membrane [248]. Another study showed the influence of the pretreatment of white blood cells and erythroleukemic cells with black tea extract on radiation-induced damage. The extract increased cell viability, reduced the level of ROS and apoptosis in normal cells compared to erythroleukemic cells, and downregulated caspase-3 [249].
Furthermore, fermented black tea shows antioxidant activity according to DPPH radical scavenging. It protects DNA from radiation damage [250]. In another study, tea extract protected radiated skin; the extract inhibited proteasome function modulated NF-κB activity [251].
7.16. Nigella sativa
Macerated extract of Nigella sativa seeds was administered to mice before whole-body irradiation. The extract showed radioprotection to the liver, brain, spleen, and intestines in normal and tumor-bearing mice according to oxidative stress reduction [252]. Water-based Nigella sativa seeds extract reduced malondialdehyde amounts and elevated the activity of antioxidative enzymes like GSHpx and SOD in intestine samples of gamma-irradiated mice. Moreover, it counteracted the radiation-induced damage of jejunal mucosa, for instance, denuded villi and Lieberkühn crypts, ulceration, and congestion in atrophic mucosa [253]. In another study, DPPH free radicals were scavenged by ethanolic extract of Nigella sativa. Oral administration of the extract to Swiss albino mice prior to 2 Gy whole-body radiation reduced lipid peroxidation and increased activity of antioxidant enzymes in the spleen and liver.
Furthermore, it prolonged the lifespan of the animals. Extract of Nigella sativa also prevented DNA from radiation-induced DNA damage [252]. The study by Çanakci et al. [254] investigates the radioprotective effects of Nigella sativa on acute radiation-induced nasal mucositis in rats. The research involved the topical application of black seed oil from Nigella sativa to assess its impact on nasal mucosa following radiotherapy. The findings of the study suggest that the topical application of black seed oil demonstrates potential radioprotective effects, as evidenced by the reduction in “superficial erosion” compared to the group treated with saline after irradiation. A recent placebo-controlled study indicates that thymoquinone, the main active ingredient of Nigella sativa, demonstrates a radioprotective effect on the lung tissue of rats exposed to IR [255].
8. Clinical Studies
There is a limited amount of clinical research examining the effectiveness of natural radioprotectors. There is a need for these to be thoroughly investigated. Clinical studies on vitexin and curcumin have confirmed their effectiveness in a randomized, placebo-controlled comparative clinical trial [256,257]. The efficacy of these substances has also been confirmed in preclinical studies conducted on lymphocytes and blood samples. However, more clinical trials are needed to further confirm their effectiveness. The details of the studies are shown in Table 3.

Table 3.
Clinical and preclinical studies on the radioprotective efficacy of substances of natural origin.
9. Methods of Extraction
Extraction methods are important in the efficiency of obtaining plant extracts rich in bioactive compounds. The type of solvent used significantly influences the extraction efficiency and selectivity of bioactive compounds. Research has shown that the choice of solvent can impact the polarity of the extracted compounds, thereby affecting the overall effectiveness of the extraction process [260]. Various techniques such as ultrasound-assisted extraction (UAE), microwave-assisted extraction (MAE), and supercritical fluid extraction have been extensively researched for their effectiveness in extracting compounds like polyphenols, flavonoids, and essential oils from plant materials [261,262]. These modern extraction methods offer advantages such as higher extraction efficiency, reduced extraction times, and lower energy consumption compared to conventional methods [72]. For example, UAE has been demonstrated to enhance extraction efficiency by inducing acoustic cavitation and facilitating solvent flow into plant cells [263].
The selection of the extraction method can significantly influence the quality and quantity of the extracted compounds. Studies have emphasized the importance of factors such as plant material preparation, solvent selection, extraction technique, and process conditions in determining the extract’s composition and bioactivity [264]. Optimization of extraction conditions, often conducted using response surface methodology (RSM), enables the identification of the most efficient parameters for extracting specific compounds from plants [265,266].
However, it should be noted that the selection of a method should also consider the safety of the solvent used. Some solvents, such as carbon dioxide, are non-toxic, whereas residues of organic solvents must be strictly controlled [267,268].
10. Toxicity, Efficacy, and Cost-Effectiveness of Radioprotectors
While natural radioprotectors are generally considered to have lower toxicity profiles compared to synthetic compounds, some challenges remain. Synthetic thiol-containing compounds, although effective as radioprotectors, are limited by their toxicity, including side effects such as hypotension, nausea, and vomiting [269]. Similarly, chemical radioprotectors like AET, WR 2721, and WR 1065 have shown toxic side effects that restrict their clinical utility [161]. The toxicity of these compounds at protective doses hinders their widespread use in medical practice.
However, when using raw plant materials, one should keep in mind their toxicity. A study by Paik et al. [270] showed in a review of cases that high doses or prolonged use of ginseng (Panax ginseng) can lead to adverse effects such as insomnia, headaches, digestive issues, and more severe effects like changes in blood pressure and heart rate. Doubts may be raised about genotoxic ginseng. The Kim et al. [271] study evaluated the effect of red ginseng on toxicity, health-related quality of life, and survival after complementary chemotherapy in patients with epithelial ovarian cancer. Red ginseng significantly increased serum alanine aminotransferase and aspartate aminotransferase levels, but they were within normal limits. Moreover, there were no differences in adverse events between the placebo and red ginseng groups. In terms of quality of life, red ginseng was associated with improved emotional functioning and reduced symptoms of fatigue, nausea and vomiting, and shortness of breath, as well as reduced anxiety and disruptions affecting life and improved daytime sleepiness.
Aloe vera may have radioprotective benefits but high concentrations or extended use can lead to genotoxic effects, suggesting the need for careful consideration of dosage and duration. Aloe vera is generally considered safe when used as a food flavoring, and the polysaccharide material from the inner gel has been found to be noncytotoxic by the Cosmetic Ingredient Review Expert Panel. However, due to the cytotoxic, mutagenic, and carcinogenic properties of anthraquinones, it is important to monitor the levels of these phenolic compounds in Aloe vera whole leaf extract and latex [272,273]. There are recommendations that the maximum allowable aloin content in Aloe-derived materials for oral consumption should be less than 10 parts per million, while for nonmedical use, the recommended limit is 50 ppm or lower [272].
Curcumin, the active component of turmeric, is celebrated for its antioxidant and anti-inflammatory properties and shows potential as a radioprotector. However, excessive consumption or long-term use of curcumin supplements has been linked to liver toxicity. Reports have highlighted cases where high doses of curcumin led to liver function abnormalities and, in some instances, liver damage [274,275].
Coumarin is used as a radioprotector, but its hepatotoxicity necessitates caution. Most patients tolerate coumarin well, though a small group experiences mild to moderate liver toxicity. Instances of hepatotoxicity have led to restrictions or bans on coumarin use in several countries. Further research is needed on gene polymorphisms and environmental factors affecting coumarin metabolism [276].
The toxicity of plant raw materials should be considered individually for each resource. Ensuring the source of raw materials is crucial to avoid contaminants that can affect their safety. Contaminants can come from soil, water, or chemicals used in cultivation. Therefore, it is important to check the origin and quality of plant raw materials before use. Using raw materials from certified organic farms minimizes the risk of exposure to harmful substances.
The efficacy of natural radioprotectors is attributed to their various beneficial activities, which were exhaustively described in this review. Synthetic radioprotectors have also proven effective in safeguarding healthy tissues from radiation damage [42]. Initially, radioprotective compounds were primarily thiol-based synthetics. Amifostine (WR-2721) underwent clinical trials as a viable radioprotector. Amifostine has been FDA-approved for dryness in the mouth caused by radiation therapy [277,278].
The effectiveness of natural and synthetic radioprotectors might vary. The survival rate of cells after 6 Gy radiation treated with crocin is comparable to that of cells treated with amifostine [279]. In another study, amifostine was compared with natural agents like red ginseng, evaluating their efficacy in mitigating the adverse effects of ionizing radiation on various biological parameters, including oxidative stress markers, tissue damage, and cellular apoptosis [280]. The results indicated that both amifostine and red ginseng showed significant reductions in markers of oxidative stress and apoptosis, as well as GSH levels, compared to the control group exposed to radiation alone, suggesting that natural agents like red ginseng may offer comparable protective effects to amifostine against radiation-induced damage, potentially offering a safer and more accessible alternative in clinical settings.
Clinical trials were also conducted to explore the efficacy of both synthetic and natural radioprotectors in combating the side effects of radiotherapy, such as xerostomia. Lee et al. investigated amifostine’s effectiveness in reducing severe xerostomia during and after radiotherapy for head-and-neck squamous-cell carcinoma. However, it failed to significantly decrease grade ≥2 acute or late xerostomia compared to placebo, and it also showed increased adverse effects [281]. In contrast, Ameri et al. investigated the efficacy of an herbal compound containing Malva sylvestris and Alcea digitata vs. artificial saliva for alleviating symptoms of at least grade 1 radiation-induced xerostomia post radiotherapy [282]. Both interventions improved symptoms, but the herbal compound demonstrated additional benefits in improving the severity of dry mouth. The third study evaluated the use of 1% pilocarpine mouthwash versus placebo in patients with radiation-induced xerostomia [283]. It was found that pilocarpine mouthwash effectively maintained saliva production after radiotherapy compared to placebo. While amifostine exhibited limited efficacy and more side effects, both the herbal compound and pilocarpine mouthwash emerged as promising treatments for managing radiation-induced xerostomia in head-and-neck cancer patients.
The efficacy of herbal extracts hinges significantly on their active constituents, whose concentration can vary due to factors such as the method of extraction, climatic conditions, geographic origin, and the timing of sample collection [284,285,286]. These variables contribute to inconsistencies in the overall effectiveness of herbal preparations. However, ensuring proper characterization and rigorous scientific evaluation of herbal products can lead to the development of an ideal radioprotector with minimal toxicity and maximal efficacy. Standardization becomes crucial in this context, as it allows for consistency in the composition and potency of herbal extracts across different batches [287,288]. This ensures repeatability in outcomes and guarantees safety and efficacy in clinical applications. By establishing standardized protocols for the preparation, quality control, and assessment of herbal extracts, researchers can enhance reliability in their therapeutic effects and pave the way for safer and more effective treatments in radioprotection and beyond [289].
When considering radioprotectors for cancer patients, it is crucial to factor in both the costs of natural and synthetic options, as affordability plays a significant role in treatment decisions. Natural radioprotectors, sourced from botanicals and plant extracts, are often perceived as cost-effective due to their potentially lower production costs and easy availability. In contrast, synthetic radioprotectors like amifostine may involve higher production expenses for patients. The economic evaluation of synthetic radioprotectors should consider manufacturing costs and administration expenses. In a 2006 study on non-small-cell lung cancer patients, using amifostine incurred an average cost of USD 4421 per patient compared to USD 2709 for those not receiving it, reflecting an incremental cost of USD 1711 [290]. Currently, based on data from the drugs.com website, the cost of Ethyol® (amifostine intravenous powder for injection 500 mg) is around USD 481 for a supply of 1 g powder for injection [291].
11. Natural Radioprotectants Patents
Natural radioprotectants show significant potential due to their ability to mitigate the harmful effects of radiation exposure. Table 4 displays patented solutions involving various natural radioprotectants, solutions containing natural compounds or plant materials, or their preparations.

Table 4.
Patented solutions of natural radioprotectants.
12. Conclusions
The studies presented suggest that plant-derived substances and extracts show promise in therapy. They have various beneficial effects that could help reduce the adverse effects of radiation therapy through different mechanisms.
The intricate interactions and biological effects exerted by these natural compounds require a thorough understanding. Future research should concentrate on comprehensively grasping the mechanisms through which these substances can protect healthy cells and support anticancer therapy. This approach will enable us to optimize therapeutic strategies and customize treatment for individual patients. The diversity of natural compounds poses challenges in understanding, yet it also presents an opportunity to discover effective therapies with potential benefits for anticancer treatment and radioprotective effect. However, there are challenges in analyzing these extracts, ensuring their origin and quality, and reproducing them consistently across different varieties. It is challenging to analyze extracts and guarantee their origin and quality accurately. Without proper controls and standardized methods, it is hard to use these substances in a controlled way. To address these challenges, we need better strategies for analyzing these extracts, ensuring quality, and ensuring they are consistent across different types of plants. Collaboration between researchers, doctors, and regulators could help establish guidelines for using these plant-derived compounds in therapy. By overcoming these challenges, we can fully utilize the potential of plant-derived substances to improve existing cancer treatments. It would provide patients with more effective and safer options for managing their condition.
Author Contributions
Conceptualization, A.S.-K. and J.C.-P.; methodology, A.S.-K. and A.G.; investigation, A.S.-K. and A.G.; resources, J.C.-P.; writing—original draft preparation, A.S.-K., A.G., D.F. and J.C.-P.; writing—review and editing, A.S.-K., A.G., D.F. and J.C.-P.; visualization, A.S.-K. and A.G.; supervision, J.C.-P.; project administration, J.C.-P.; funding acquisition, J.C.-P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
Graphics are created with BioRender.com.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| Abbreviation | Component |
| ABTS | 2,2′-Azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) radical |
| A549 | Adenocarcinomic Human Alveolar Basal Epithelial Cells |
| ATP | Adenosine 5γ-Triphosphate |
| CAT | Catalase |
| CGRP-TNF-α | Calcitonin Gene-Related Peptide-Tumor Necrosis Factor Alpha |
| CHO | Chinese Hamster Ovary Cell Line |
| CPK | Creatine Phosphokinase |
| DPPH | 2,2-Diphenyl-1-picrylhydrazyl |
| FDA | US Food and Drug Administration |
| GSH | Glutathione |
| GSHpx | Glutathione Peroxidase |
| GST | Glutathione S-Transferase |
| HaCaT | Human Keratinocyte |
| HEI-OC1 | House Ear Institute–Organ of Corti 1 |
| HEL 299 | Normal Human Lung Cells |
| HepG2 | Hepatocellular Carcinoma Cell Line |
| HMGB1 | High Mobility Group Box 1 |
| HO-1 | Heme Oxygenase-1 |
| HRE | Haberlea rhodopensis Extract |
| HT-29 | Human Colorectal Adenocarcinoma Cell Line |
| IGF-1 | Insulin-like Growth Factor 1 |
| IL-1β | Interleukin-1 Beta |
| IR | Ionizing Radiation |
| MAPK | Mitogen-Activated Protein Kinase |
| MCF-10A | Non-transformed Human Mammary Epithelial Cell Line |
| MCF-7 | Human Breast Cancer Cells |
| MDA | Malondialdehyde |
| MDA-MB-231 | Breast Cancer Cell Line |
| MPG | 2-Mercaptopropionyl Glycine |
| Nrf2 | Nuclear Factor Erythroid 2-Related Factor 2 |
| NK | Natural Killer |
| NO• | Nitroxyl Anion |
| Ot | Orientin |
| PANC-1 | Human Pancreatic Epithelioid Carcinoma Cell Line |
| PC-3 | Human Prostate Cancer Cell Line |
| PPAR-γ | Peroxisome Proliferator-Activated Receptor Gamma |
| PKB | Protein Kinase B |
| PKC | Protein Kinase C |
| RIII | Radiation-Induced Intestinal Injury |
| RN | Radiation Nephropathy |
| ROS | Reactive Oxygen Species |
| SMGs | Submandibular Glands |
| SOD | Superoxide Dismutase |
| STAT | Signal Transducer and Activator of Transcription |
| T47D | Human Breast Cancer Cell Line |
| TGF-β | Transforming Growth Factor Beta |
| TNF-α | Tumor Necrosis Factor Alpha |
| VEGF | Vascular Endothelial Growth Factor |
| Vc | Vicenin |
| WHO | World Health Organization |
| YSE | Yuca schidigera Extract |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global Cancer Statistics 2022: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Cancer Statistics—NCI. Available online: https://www.cancer.gov/about-cancer/understanding/statistics (accessed on 14 June 2024).
- Zhang, Z.; Liu, X.; Chen, D.; Yu, J. Radiotherapy Combined with Immunotherapy: The Dawn of Cancer Treatment. Signal Transduct. Target. Ther. 2022, 7, 258. [Google Scholar] [CrossRef] [PubMed]
- Böhmer, D.; Wirth, M.; Miller, K.; Budach, V.; Heidenreich, A.; Wiegel, T. Radiotherapy and Hormone Treatment in Prostate Cancer. Dtsch. Arztebl. Int. 2016, 113, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.; Jung, S.; Baek, S.H. Combination Therapy of Radiation and Hyperthermia, Focusing on the Synergistic Anti-Cancer Effects and Research Trends. Antioxidants 2023, 12, 924. [Google Scholar] [CrossRef]
- Jagsi, R.; Griffith, K.A.; Harris, E.E.; Wright, J.L.; Recht, A.; Taghian, A.G.; Lee, L.; Moran, M.S.; Small, W.; Johnstone, C.; et al. Omission of Radiotherapy After Breast-Conserving Surgery for Women With Breast Cancer with Low Clinical and Genomic Risk: 5-Year Outcomes of IDEA. J. Clin. Oncol. 2023, JCO2302270. [Google Scholar] [CrossRef]
- Simone, C.B., II. Focus on Oncology: The Role of Palliative Radiation Therapy in Patients with Pancreatic Cancer. Ann. Palliat. Med. 2023, 12, 1122124. [Google Scholar] [CrossRef] [PubMed]
- Jaksic, A.; Nikolov, J.; Palma, A. Special Issue: Applications of Radiation in Science and Technology. Eur. Phys. J. Spec. Top. 2023, 232, 1459–1463. [Google Scholar] [CrossRef]
- Chaudhary, P.; Janmeda, P.; Docea, A.O.; Yeskaliyeva, B.; Abdull Razis, A.F.; Modu, B.; Calina, D.; Sharifi-Rad, J. Oxidative Stress, Free Radicals and Antioxidants: Potential Crosstalk in the Pathophysiology of Human Diseases. Front. Chem. 2023, 11, 1158198. [Google Scholar] [CrossRef]
- Cox, J.D.; Ang, K.K. Radiation Oncology E-Book: Rationale, Technique, Results; Elsevier Health Sciences: Amsterdam, The Netherlands, 2009; ISBN 978-0-323-07660-9. [Google Scholar]
- Sage, E.; Shikazono, N. Radiation-Induced Clustered DNA Lesions: Repair and Mutagenesis. Free Radic. Biol. Med. 2017, 107, 125–135. [Google Scholar] [CrossRef]
- Einor, D.; Bonisoli-Alquati, A.; Costantini, D.; Mousseau, T.A.; Møller, A.P. Ionizing Radiation, Antioxidant Response and Oxidative Damage: A Meta-Analysis. Sci. Total Environ. 2016, 548–549, 463–471. [Google Scholar] [CrossRef]
- Rezaeyan, A.; Haddadi, G.H.; Hosseinzadeh, M.; Moradi, M.; Najafi, M. Radioprotective Effects of Hesperidin on Oxidative Damages and Histopathological Changes Induced by X-Irradiation in Rats Heart Tissue. J. Med. Phys. 2016, 41, 182–191. [Google Scholar] [CrossRef]
- Shaban, N.Z.; Ahmed Zahran, A.M.; El-Rashidy, F.H.; Abdo Kodous, A.S. Protective Role of Hesperidin against γ-Radiation-Induced Oxidative Stress and Apoptosis in Rat Testis. J. Biol. Res. (Thessal.) 2017, 24, 5. [Google Scholar] [CrossRef]
- Szumiel, I. Ionizing Radiation-Induced Oxidative Stress, Epigenetic Changes and Genomic Instability: The Pivotal Role of Mitochondria. Int. J. Radiat. Biol. 2015, 91, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Aranda-Rivera, A.K.; Cruz-Gregorio, A.; Arancibia-Hernández, Y.L.; Hernández-Cruz, E.Y.; Pedraza-Chaverri, J. RONS and Oxidative Stress: An Overview of Basic Concepts. Oxygen 2022, 2, 437–478. [Google Scholar] [CrossRef]
- Nuszkiewicz, J.; Woźniak, A.; Szewczyk-Golec, K. Ionizing Radiation as a Source of Oxidative Stress-The Protective Role of Melatonin and Vitamin D. Int. J. Mol. Sci. 2020, 21, 5804. [Google Scholar] [CrossRef]
- Huang, R.; Chen, H.; Liang, J.; Li, Y.; Yang, J.; Luo, C.; Tang, Y.; Ding, Y.; Liu, X.; Yuan, Q.; et al. Dual Role of Reactive Oxygen Species and Their Application in Cancer Therapy. J. Cancer 2021, 12, 5543–5561. [Google Scholar] [CrossRef]
- Zarepisheh, M.; Hong, L.; Zhou, Y.; Huang, Q.; Yang, J.; Jhanwar, G.; Pham, H.D.; Dursun, P.; Zhang, P.; Hunt, M.A.; et al. Automated and Clinically Optimal Treatment Planning for Cancer Radiotherapy. INFORMS J. Appl. Anal. 2022, 52, 69–89. [Google Scholar] [CrossRef] [PubMed]
- Komorowska, D.; Radzik, T.; Kalenik, S.; Rodacka, A. Natural Radiosensitizers in Radiotherapy: Cancer Treatment by Combining Ionizing Radiation with Resveratrol. Int. J. Mol. Sci. 2022, 23, 10627. [Google Scholar] [CrossRef]
- Singh, V.K.; Seed, T.M. Pharmacological Management of Ionizing Radiation Injuries: Current and Prospective Agents and Targeted Organ Systems. Expert. Opin. Pharmacother. 2020, 21, 317–337. [Google Scholar] [CrossRef]
- Reshi, Z.A.; Ahmad, W.; Lukatkin, A.S.; Javed, S.B. From Nature to Lab: A Review of Secondary Metabolite Biosynthetic Pathways, Environmental Influences, and In Vitro Approaches. Metabolites 2023, 13, 895. [Google Scholar] [CrossRef]
- Hosseini, M.; Pereira, D.M. The Chemical Space of Terpenes: Insights from Data Science and AI. Pharmaceuticals 2023, 16, 202. [Google Scholar] [CrossRef] [PubMed]
- Masyita, A.; Mustika Sari, R.; Dwi Astuti, A.; Yasir, B.; Rahma Rumata, N.; Emran, T.B.; Nainu, F.; Simal-Gandara, J. Terpenes and Terpenoids as Main Bioactive Compounds of Essential Oils, Their Roles in Human Health and Potential Application as Natural Food Preservatives. Food Chem. X 2022, 13, 100217. [Google Scholar] [CrossRef] [PubMed]
- Proshkina, E.; Plyusnin, S.; Babak, T.; Lashmanova, E.; Maganova, F.; Koval, L.; Platonova, E.; Shaposhnikov, M.; Moskalev, A. Terpenoids as Potential Geroprotectors. Antioxidants 2020, 9, 529. [Google Scholar] [CrossRef]
- Liga, S.; Paul, C.; Péter, F. Flavonoids: Overview of Biosynthesis, Biological Activity, and Current Extraction Techniques. Plants 2023, 12, 2732. [Google Scholar] [CrossRef] [PubMed]
- Duta-Bratu, C.-G.; Nitulescu, G.M.; Mihai, D.P.; Olaru, O.T. Resveratrol and Other Natural Oligomeric Stilbenoid Compounds and Their Therapeutic Applications. Plants 2023, 12, 2935. [Google Scholar] [CrossRef] [PubMed]
- Heghes, S.C.; Vostinaru, O.; Mogosan, C.; Miere, D.; Iuga, C.A.; Filip, L. Safety Profile of Nutraceuticals Rich in Coumarins: An Update. Front. Pharmacol. 2022, 13, 803338. [Google Scholar] [CrossRef] [PubMed]
- Deng, P.; Cui, B.; Zhu, H.; Phommakoun, B.; Zhang, D.; Li, Y.; Zhao, F.; Zhao, Z. Accumulation Pattern of Amygdalin and Prunasin and Its Correlation with Fruit and Kernel Agronomic Characteristics during Apricot (Prunus armeniaca L.) Kernel Development. Foods 2021, 10, 397. [Google Scholar] [CrossRef] [PubMed]
- Urriolabeitia, A.; De Sancho, D.; López, X. Influence of the Nonprotein Amino Acid Mimosine in Peptide Conformational Propensities from Novel Amber Force Field Parameters. J. Phys. Chem. B 2022, 126, 2959–2967. [Google Scholar] [CrossRef]
- Faisal, S.; Badshah, S.L.; Kubra, B.; Emwas, A.-H.; Jaremko, M. Alkaloids as Potential Antivirals. A Comprehensive Review. Nat. Prod. Bioprospect. 2023, 13, 4. [Google Scholar] [CrossRef] [PubMed]
- Mahn, A.; Castillo, A. Potential of Sulforaphane as a Natural Immune System Enhancer: A Review. Molecules 2021, 26, 752. [Google Scholar] [CrossRef]
- Liao, A.; Li, L.; Wang, T.; Lu, A.; Wang, Z.; Wang, Q. Discovery of Phytoalexin Camalexin and Its Derivatives as Novel Antiviral and Antiphytopathogenic-Fungus Agents. J. Agric. Food Chem. 2022, 70, 2554–2563. [Google Scholar] [CrossRef] [PubMed]
- Seregin, I.V.; Kozhevnikova, A.D. Phytochelatins: Sulfur-Containing Metal(Loid)-Chelating Ligands in Plants. Int. J. Mol. Sci. 2023, 24, 2430. [Google Scholar] [CrossRef] [PubMed]
- Yousefvand, S.; Fattahi, F.; Hosseini, S.M.; Urech, K.; Schaller, G. Viscotoxin and Lectin Content in Foliage and Fruit of Viscum album L. on the Main Host Trees of Hyrcanian Forests. Sci. Rep. 2022, 12, 10383. [Google Scholar] [CrossRef] [PubMed]
- Dowlath, M.J.H.; Karuppannan, S.K.; Sinha, P.; Dowlath, N.S.; Arunachalam, K.D.; Ravindran, B.; Chang, S.W.; Nguyen-Tri, P.; Nguyen, D.D. Effects of Radiation and Role of Plants in Radioprotection: A Critical Review. Sci. Total Environ. 2021, 779, 146431. [Google Scholar] [CrossRef] [PubMed]
- Arora, R.; Gupta, D.; Chawla, R.; Sagar, R.K.; Sharma, A.; Kumar, R.; Prasad, J.; Singh, S.; Samanta, N.; Sharma, R. Radioprotection by Plant Products: Present Status and Future Prospects. Phytother. Res. 2005, 19, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Tavakkoli, A.; Iranshahi, M.; Hasheminezhad, S.H.; Hayes, A.W.; Karimi, G. The Neuroprotective Activities of Natural Products Through the Nrf2 Upregulation. Phytother. Res. 2019, 33, 2256–2273. [Google Scholar] [CrossRef]
- Jomova, K.; Raptova, R.; Alomar, S.Y.; Alwasel, S.H.; Nepovimova, E.; Kuca, K.; Valko, M. Reactive Oxygen Species, Toxicity, Oxidative Stress, and Antioxidants: Chronic Diseases and Aging. Arch. Toxicol. 2023, 97, 2499–2574. [Google Scholar] [CrossRef] [PubMed]
- de Amorim, E.L.C.; Cruz, P.; Filho, J.V.; Silva, I.C.; Costa, U.; Oliveira, J.; Medeiros, M.S.; Diniz, M.; Machado, K.; Xavier, A.C.; et al. Brazilian Caatinga: Phenolic Contents, Industrial and Therapeutic Applications. In Phenolic Compounds—Chemistry, Synthesis, Diversity, Non-Conventional Industrial, Pharmaceutical and Therapeutic Applications; IntechOpen: London, UK, 2021; ISBN 978-1-83969-347-2. [Google Scholar]
- Mamun, A.A.; Shao, C.; Geng, P.; Wang, S.; Xiao, J. Polyphenols Targeting NF-κB Pathway in Neurological Disorders: What We Know So Far? Int. J. Biol. Sci. 2024, 20, 1332–1355. [Google Scholar] [CrossRef]
- Wang, L.; Wang, Z.; Cao, Y.; Lu, W.; Kuang, L.; Hua, D. Strategy for Highly Efficient Radioprotection by a Selenium-Containing Polymeric Drug with Low Toxicity and Long Circulation. Acs Appl. Mater. Interfaces 2020, 12, 44534–44540. [Google Scholar] [CrossRef]
- Saralamma, V.V.G.; Kim, E.H.; Lee, H.J.; Raha, S.; Lee, W.S.; Heo, J.D.; Lee, S.J.; Won, C.-K.; Kim, G.-S. Flavonoids: A New Generation Molecule to Stimulate Programmed Cell Deaths in Cancer Cells. J. Biomed. Transl. Res. 2017, 18, 30–37. [Google Scholar] [CrossRef]
- Cannan, W.J.; Pederson, D.S. Mechanisms and Consequences of Double-Strand DNA Break Formation in Chromatin. J. Cell Physiol. 2016, 231, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Toulany, M. Targeting DNA Double-Strand Break Repair Pathways to Improve Radiotherapy Response. Genes 2019, 10, 25. [Google Scholar] [CrossRef] [PubMed]
- Koukourakis, M.I. Radiation Damage and Radioprotectants: New Concepts in the Era of Molecular Medicine. Br. J. Radiol. 2012, 85, 313–330. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Collins, L.B.; Chen, T.; Herr, N.; Takeda, S.; Sun, W.; Swenberg, J.A.; Nakamura, J. Oxidative Stress at Low Levels Can Induce Clustered DNA Lesions Leading to NHEJ Mediated Mutations. Oncotarget 2016, 7, 25377–25390. [Google Scholar] [CrossRef] [PubMed]
- Lagunas-Rangel, F.A.; Bermúdez-Cruz, R.M. Natural Compounds That Target DNA Repair Pathways and Their Therapeutic Potential to Counteract Cancer Cells. Front. Oncol. 2020, 10, 598174. [Google Scholar] [CrossRef] [PubMed]
- Biau, J.; Chautard, E.; Verrelle, P.; Dutreix, M. Altering DNA Repair to Improve Radiation Therapy: Specific and Multiple Pathway Targeting. Front. Oncol. 2019, 9, 1009. [Google Scholar] [CrossRef] [PubMed]
- Merlin, J.P.J.; Mathavarajah, S.; Dellaire, G.; Murphy, K.P.J.; Rupasinghe, H.P.V. A Dietary Antioxidant Formulation Ameliorates DNA Damage Caused by γ-Irradiation in Normal Human Bronchial Epithelial Cells In Vitro. Antioxidants 2022, 11, 1407. [Google Scholar] [CrossRef] [PubMed]
- Elmore, S. Apoptosis: A Review of Programmed Cell Death. Toxicol. Pathol. 2007, 35, 495–516. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Huang, Y.; Zheng, L.; Wu, H.; Zou, B.; Xu, Y. Exploring Natural Products as Radioprotective Agents for Cancer Therapy: Mechanisms, Challenges, and Opportunities. Cancers 2023, 15, 3585. [Google Scholar] [CrossRef]
- Peng, Y.; Wang, Y.; Zhou, C.; Mei, W.; Zeng, C. PI3K/Akt/mTOR Pathway and Its Role in Cancer Therapeutics: Are We Making Headway? Front. Oncol. 2022, 12, 819128. [Google Scholar] [CrossRef]
- Williams, A.B.; Schumacher, B. P53 in the DNA-Damage-Repair Process. Cold Spring Harb. Perspect. Med. 2016, 6, a026070. [Google Scholar] [CrossRef]
- Morita, A.; Takahashi, I.; Sasatani, M.; Aoki, S.; Wang, B.; Ariyasu, S.; Tanaka, K.; Yamaguchi, T.; Sawa, A.; Nishi, Y.; et al. A Chemical Modulator of P53 Transactivation That Acts as a Radioprotective Agonist. Mol. Cancer Ther. 2017, 17, 432–442. [Google Scholar] [CrossRef]
- Begum, N.; Prasad, N.R. Apigenin, a Dietary Antioxidant, Modulates Gamma Radiation-Induced Oxidative Damages in Human Peripheral Blood Lymphocytes. Biomed. Prev. Nutr. 2012, 2, 16–24. [Google Scholar] [CrossRef]
- Qian, S.; Wei, Z.; Yang, W.; Huang, J.; Yang, Y.; Wang, J. The Role of BCL-2 Family Proteins in Regulating Apoptosis and Cancer Therapy. Front. Oncol. 2022, 12, 985363. [Google Scholar] [CrossRef]
- Tlili, H.; Macovei, A.; Buonocore, D.; Lanzafame, M.; Najjaa, H.; Lombardi, A.; Pagano, A.; Dossena, M.; Verri, M.; Arfa, A.B.; et al. The Polyphenol/Saponin-Rich Rhus Tripartita Extract Has an Apoptotic Effect on THP-1 Cells through the PI3K/AKT/mTOR Signaling Pathway. BMC Complement. Med. Ther. 2021, 21, 153. [Google Scholar] [CrossRef]
- Barker, H.E.; Paget, J.T.E.; Khan, A.A.; Harrington, K.J. The Tumour Microenvironment after Radiotherapy: Mechanisms of Resistance and Recurrence. Nat. Rev. Cancer 2015, 15, 409–425. [Google Scholar] [CrossRef]
- Arulselvan, P.; Fard, M.T.; Tan, W.S.; Gothai, S.; Fakurazi, S.; Norhaizan, M.E.; Kumar, S.S. Role of Antioxidants and Natural Products in Inflammation. Oxid. Med. Cell Longev. 2016, 2016, 5276130. [Google Scholar] [CrossRef]
- Jeong, H.; Bok, S.; Hong, B.-J.; Choi, H.-S.; Ahn, G.-O. Radiation-Induced Immune Responses: Mechanisms and Therapeutic Perspectives. Blood Res. 2016, 51, 157–163. [Google Scholar] [CrossRef]
- Gans, I.; El Abiad, J.M.; James, A.W.; Levin, A.S.; Morris, C.D. Administration of TGF-ß Inhibitor Mitigates Radiation-Induced Fibrosis in a Mouse Model. Clin. Orthop. Relat. Res. 2021, 479, 468–474. [Google Scholar] [CrossRef]
- Baselet, B.; Sonveaux, P.; Baatout, S.; Aerts, A. Pathological Effects of Ionizing Radiation: Endothelial Activation and Dysfunction. Cell Mol. Life Sci. 2018, 76, 699–728. [Google Scholar] [CrossRef]
- Jit, B.P.; Pradhan, B.; Dash, R.; Bhuyan, P.P.; Behera, C.; Behera, R.K.; Sharma, A.; Alcaraz, M.; Jena, M. Phytochemicals: Potential Therapeutic Modulators of Radiation Induced Signaling Pathways. Antioxidants 2021, 11, 49. [Google Scholar] [CrossRef]
- Zhang, C.; Chen, K.; Wang, J.; Zheng, Z.; Luo, Y.; Zhou, W.; Zhuo, Z.; Liang, J.; Sha, W.; Chen, H. Protective Effects of Crocetin against Radiation-Induced Injury in Intestinal Epithelial Cells. Biomed. Res. Int. 2020, 2020, 2906053. [Google Scholar] [CrossRef]
- Gramatyka, M. The Radioprotective Activity of Resveratrol—Metabolomic Point of View. Metabolites 2022, 12, 478. [Google Scholar] [CrossRef]
- Hasanzadeh, M.; Bahreyni Toossi, M.T.; Vaziri-Nezamdoost, F.; Khademi, S.; Darroudi, M.; Azimian, H. Comparison of Radioprotective Effects of Colloidal Synthesis of Selenium Nanoparticles in Aqueous Rosemary Extract and Rosemary in Chinese Hamster Ovary (CHO) Cells. J. Nanostructures 2022, 12, 711–717. [Google Scholar] [CrossRef]
- Al Fares, E.; Sanikidze, T.; Kalmakhelidze, S.; Topuria, D.; Mansi, L.; Kitson, S.; Molazadeh, M. The Alleviating Effect of Herniarin Against Ionizing Radiation-Induced Genotoxicity and Cytotoxicity in Human Peripheral Blood Lymphocytes. Curr. Radiopharm. 2022, 15, 141–147. [Google Scholar] [CrossRef]
- Kim, H.M.; Kim, S.H.; Kang, B.S. Radioprotective Effects of Delphinidin on Normal Human Lung Cells against Proton Beam Exposure. Nutr. Res. Pr. 2018, 12, 41–46. [Google Scholar] [CrossRef]
- Chumsuwan, N.; Khongkow, P.; Kaewsuwan, S.; Kanokwiroon, K. Interruptin C, a Radioprotective Agent, Derived from Cyclosorus terminans Protect Normal Breast MCF-10A and Human Keratinocyte HaCaT Cells against Radiation-Induced Damage. Molecules 2022, 27, 3298. [Google Scholar] [CrossRef]
- Staneva, D.; Dimitrova, N.; Popov, B.; Alexandrova, A.; Georgieva, M.; Miloshev, G. Haberlea rhodopensis Extract Tunes the Cellular Response to Stress by Modulating DNA Damage, Redox Components, and Gene Expression. Int. J. Mol. Sci. 2023, 24, 15964. [Google Scholar] [CrossRef]
- Zhang, Q.-W.; Lin, L.-G.; Ye, W.-C. Techniques for Extraction and Isolation of Natural Products: A Comprehensive Review. Chin. Med. 2018, 13, 20. [Google Scholar] [CrossRef]
- Du, Y.; Jia, C.; Liu, Y.; Li, Y.; Wang, J.; Sun, K. Isorhamnetin Enhances the Radiosensitivity of A549 Cells Through Interleukin-13 and the NF-κB Signaling Pathway. Front. Pharmacol. 2021, 11, 610772. [Google Scholar] [CrossRef]
- Abolhassani, Y.; Mirzaei, S.; Nejabat, M.; Talebian, S.; Gholamhosseinian, H.; Iranshahi, M.; Rassouli, F.B.; Jamialahmadi, K. 7-Geranyloxcycoumarin Enhances Radio Sensitivity in Human Prostate Cancer Cells. Mol. Biol. Rep. 2023, 50, 5709–5717. [Google Scholar] [CrossRef]
- Al Bitar, S.; Ballout, F.; Monzer, A.; Kanso, M.; Saheb, N.; Mukherji, D.; Faraj, W.; Tawil, A.; Doughan, S.; Hussein, M.; et al. Thymoquinone Radiosensitizes Human Colorectal Cancer Cells in 2D and 3D Culture Models. Cancers 2022, 14, 1363. [Google Scholar] [CrossRef]
- Mahdizade Valojerdi, F.; Goliaei, B.; Rezakhani, N.; Nikoofar, A.; Keshmiri Neghab, H.; Soheilifar, M.H.; Bigdeli, B. In vitro radiosensitization of T47D and MDA-MB-231 breast cancer cells with the neoflavonoid dalbergin. Middle East J. Cancer 2023, 14, 205–218. [Google Scholar]
- Hassan, A.A.; Abdel-Rafei, M.K.; Sherif, N.H.; Askar, M.A.; Thabet, N.M. Antitumor and Radiosensitizing Effects of Anagallis Arvensis Hydromethanolic Extract on Breast Cancer Cells through Upregulating FOXO3, Let-7, and Mir-421 Expression. Pharmacol. Res.-Mod. Chin. Med. 2022, 5, 100179. [Google Scholar] [CrossRef]
- Elbakry, M.M.M.; ElBakary, N.M.; Hagag, S.A.; Hemida, E.H.A. Pomegranate Peel Extract Sensitizes Hepatocellular Carcinoma Cells to Ionizing Radiation, Induces Apoptosis and Inhibits MAPK, JAK/STAT3, β-Catenin/NOTCH, and SOCS3 Signaling. Integr. Cancer Ther. 2023, 22, 15347354221151021. [Google Scholar] [CrossRef]
- Jing, Z.; Li, M.; Wang, H.; Yang, Z.; Zhou, S.; Ma, J.; Meng, E.; Zhang, H.; Liang, W.; Hu, W.; et al. Gallic Acid-Gold Nanoparticles Enhance Radiation-Induced Cell Death of Human Glioma U251 Cells. IUBMB Life 2021, 73, 398–407. [Google Scholar] [CrossRef]
- Pacifico, S.; Bláha, P.; Faramarzi, S.; Fede, F.; Michaličková, K.; Piccolella, S.; Ricciardi, V.; Manti, L. Differential Radiomodulating Action of Olea europaea L. Cv. Caiazzana Leaf Extract on Human Normal and Cancer Cells: A Joint Chemical and Radiobiological Approach. Antioxidants 2022, 11, 1603. [Google Scholar] [CrossRef]
- Yang, E.S.; Choi, M.J.; Kim, J.H.; Choi, K.S.; Kwon, T.K. Combination of Withaferin A and X-Ray Irradiation Enhances Apoptosis in U937 Cells. Toxicol. In Vitro 2011, 25, 1803–1810. [Google Scholar] [CrossRef]
- Assayed, M.E. Radioprotective Effects of Black Seed (Nigella Sativa) Oil against Hemopoietic Damage and Immunosuppression in Gamma-Irradiated Rats. Immunopharmacol. Immunotoxicol. 2010, 32, 284–296. [Google Scholar] [CrossRef]
- Devi, P.U.; Bisht, K.S.; Vinitha, M. A Comparative Study of Radioprotection by Ocimum Flavonoids and Synthetic Aminothiol Protectors in the Mouse. Br. J. Radiol. 1998, 71, 782–784. [Google Scholar] [CrossRef]
- Tripathi, Y.B.; Singh, A.V. Role of Rubia cordifolia Linn. in Radiation Protection. Indian. J. Exp. Biol. 2007, 45, 620–625. [Google Scholar] [PubMed]
- Bradley, E.W.; Zook, B.C.; Casarett, G.W.; Deye, J.A.; Adoff, L.M.; Rogers, C.C. Neoplasia in Fast Neutron-Irradiated Beagles. J. Natl. Cancer Inst. 1981, 67, 729–738. [Google Scholar] [PubMed]
- Zook, B.C.; Bradley, E.W.; Casarett, G.W.; Rogers, C.C. Pathologic Changes in the Hearts of Beagles Irradiated with Fractionated Fast Neutrons or Photons. Radiat. Res. 1981, 88, 607–618. [Google Scholar] [CrossRef] [PubMed]
- Giese, A.P.J.; Guarnaschelli, J.G.; Ward, J.A.; Choo, D.I.; Riazuddin, S.; Ahmed, Z.M. Radioprotective Effect of Aminothiol PrC-210 on Irradiated Inner Ear of Guinea Pig. PLoS ONE 2015, 10, e0143606. [Google Scholar] [CrossRef] [PubMed]
- Mujica-Mota, M.A.; Salehi, P.; Devic, S.; Daniel, S.J. Safety and Otoprotection of Metformin in Radiation-Induced Sensorineural Hearing Loss in the Guinea Pig. Otolaryngol. Head. Neck Surg. 2014, 150, 859–865. [Google Scholar] [CrossRef] [PubMed]
- Lotz, S.; Caselitz, J.; Tschakert, H.; Rehpenning, W.; Seifert, G. Radioprotection of Minipig Salivary Glands by Orciprenaline-Carbachol. An Ultrastructural and Semiquantitative Light Microscopic Study. Virchows Arch. A Pathol. Anat. Histopathol. 1990, 417, 119–128. [Google Scholar] [CrossRef]
- Tanchev, S.; Georgieva, S.; Gencheva, D.; Sotirov, L.; Koynarski, T.; Petrov, V. Life Duration of Inbred and Outbreed Rabbits, Irradiated with Gamma Rays. Bulg. J. Agric. Sci. 2015, 21, 404–408. [Google Scholar]
- Enginar, H.; Avcı, G.; Eryavuz, A.; Kaya, E.; Kucukkurt, I.; Fidan, A.F. Effect of Yucca Schidigera Extract on Lipid Pe Roxidation and Antioxidant Activity in Rabbits Ex Posed to γ-Radiation. Rev. De. Med. Vet. 2006, 157, 415. [Google Scholar]
- Georgieva, S.; Popov, B.; Bonev, G. Radioprotective Effect of Haberlea rhodopensis (Friv.) Leaf Extract on Gamma-Radiation-Induced DNA Damage, Lipid Peroxidation and Antioxidant Levels in Rabbit Blood. Indian. J. Exp. Biol. 2013, 51, 29–36. [Google Scholar]
- Penchev, G.; Georgieva, S.; Popov, B. Protection against Radiation-Induced Testicular Injury in Rabbits by Haberlea rhodopensis (a Balkan Ressurection Plant) Extract. Bulg. J. Vet. Med. 2018, 21, 313–321. [Google Scholar] [CrossRef]
- Vasin, M.V.; Semenov, L.F.; Suvorov, N.N.; Antipov, V.V.; Ushakov, I.B.; Ilyin, L.A.; Lapin, B.A. Protective Effect and the Therapeutic Index of Indralin in Juvenile Rhesus Monkeys. J. Radiat. Res. 2014, 55, 1048–1055. [Google Scholar] [CrossRef]
- Jagetia, G.C.; Venkatesh, P.; Baliga, M.S. Evaluation of the Radioprotective Effect of Bael Leaf (Aegle marmelos) Extract in Mice. Int. J. Radiat. Biol. 2004, 80, 281–290. [Google Scholar] [CrossRef]
- Jagetia, G.C.; Shirwaikar, A.; Rao, S.K.; Bhilegaonkar, P.M. Evaluation of the Radioprotective Effect of Ageratum conyzoides Linn. Extract in Mice Exposed to Different Doses of Gamma Radiation. J. Pharm. Pharmacol. 2003, 55, 1151–1158. [Google Scholar] [CrossRef]
- Khattab, H.A.H.; Abdallah, I.Z.A.; Yousef, F.M.; Huwait, E.A. Efficiency of borage seeds oil against gamma irradiation-induced hepatotoxicity in male rats: Possible antioxidant activity. Afr. J. Tradit. Complement. Altern. Med. 2017, 14, 169–179. [Google Scholar] [CrossRef]
- Tiku, A.B.; Abraham, S.K.; Kale, R.K. Eugenol as an in Vivo Radioprotective Agent. J. Radiat. Res. 2004, 45, 435–440. [Google Scholar] [CrossRef]
- Landauer, M.R.; Srinivasan, V.; Seed, T.M. Genistein Treatment Protects Mice from Ionizing Radiation Injury. J. Appl. Toxicol. 2003, 23, 379–385. [Google Scholar] [CrossRef]
- Zhou, Y.; Mi, M.-T. Genistein Stimulates Hematopoiesis and Increases Survival in Irradiated Mice. J. Radiat. Res. 2005, 46, 425–433. [Google Scholar] [CrossRef]
- Gandhi, N.M.; Maurya, D.K.; Salvi, V.; Kapoor, S.; Mukherjee, T.; Nair, C.K.K. Radioprotection of DNA by Glycyrrhizic Acid through Scavenging Free Radicals. J. Radiat. Res. 2004, 45, 461–468. [Google Scholar] [CrossRef]
- Goel, H.C.; Prasad, J.; Singh, S.; Sagar, R.K.; Kumar, I.P.; Sinha, A.K. Radioprotection by a Herbal Preparation of Hippophae rhamnoides, RH-3, against Whole Body Lethal Irradiation in Mice. Phytomedicine 2002, 9, 15–25. [Google Scholar] [CrossRef]
- Abraham, S.K.; Sarma, L.; Kesavan, P.C. Protective Effects of Chlorogenic Acid, Curcumin and Beta-Carotene against Gamma-Radiation-Induced in Vivo Chromosomal Damage. Mutat. Res. 1993, 303, 109–112. [Google Scholar] [CrossRef]
- Pote, M.S.; Gandhi, N.M.; Mishra, K.P. Antiatherogenic and Radioprotective Role of Folic Acid in Whole Body Gamma-Irradiated Mice. Mol. Cell Biochem. 2006, 292, 19–25. [Google Scholar] [CrossRef]
- Shimoi, K.; Masuda, S.; Shen, B.; Furugori, M.; Kinae, N. Radioprotective Effects of Antioxidative Plant Flavonoids in Mice. Mutat. Res. 1996, 350, 153–161. [Google Scholar] [CrossRef]
- Cividalli, A.; Adami, M.; De Tomasi, F.; Palmisano, L.; Pardini, M.C.; Spanò, M.; Mauro, F. Orgotein as a Radioprotector in Normal Tissues. Experiments on Mouse Skin and a Murine Adenocarcinoma. Acta Radiol. Oncol. 1985, 24, 273–277. [Google Scholar] [CrossRef]
- Lee, H.J.; Kim, S.R.; Kim, J.C.; Kang, C.M.; Lee, Y.S.; Jo, S.K.; Kim, T.H.; Jang, J.S.; Nah, S.Y.; Kim, S.H. In Vivo Radioprotective Effect of Panax Ginseng C.A. Meyer and Identification of Active Ginsenosides. Phytother. Res. 2006, 20, 392–395. [Google Scholar] [CrossRef]
- Kumar, M.; Sharma, M.K.; Saxena, P.S.; Kumar, A. Radioprotective Effect of Panax Ginseng on the Phosphatases and Lipid Peroxidation Level in Testes of Swiss Albino Mice. Biol. Pharm. Bull. 2003, 26, 308–312. [Google Scholar] [CrossRef]
- Koohian, F.; Shanei, A.; Shahbazi-Gahrouei, D.; Hejazi, S.H.; Moradi, M.-T. The Radioprotective Effect of Resveratrol Against Genotoxicity Induced by γ-Irradiation in Mice Blood Lymphocytes. Dose Response 2017, 15, 1559325817705699. [Google Scholar] [CrossRef]
- Zhang, H.; Zhai, Z.; Wang, Y.; Zhang, J.; Wu, H.; Wang, Y.; Li, C.; Li, D.; Lu, L.; Wang, X.; et al. Resveratrol Ameliorates Ionizing Irradiation-Induced Long-Term Hematopoietic Stem Cell Injury in Mice. Free Radic. Biol. Med. 2013, 54, 40–50. [Google Scholar] [CrossRef]
- Patil, S.L.; Somashekarappa, H.; Rajashekhar, K. Radiomodulatory Role of Rutin and Quercetin in Swiss Albino Mice Exposed to the Whole Body Gamma Radiation. Indian. J. Nucl. Med. 2012, 27, 237–242. [Google Scholar] [CrossRef]
- Hirsch, E.; Vass, P.; Démuth, B.; Petho, Z.; Bitay, E.; Andersen, S.K.; Vigh, T.; Verreck, G.; Molnar, K.; Nagy, Z.; et al. Electrospinning Scale-Up and Formulation Development of PVA Nanofibers Aiming Oral Delivery of Biopharmaceuticals. Express Polym. Lett. 2019, 13, 590–603. [Google Scholar] [CrossRef]
- Leite, C.B.S.; Coelho, J.M.; Muehlmann, L.A.; Azevedo, R.B. Skin Delivery of Glucosamine and Chondroitin Sulphates—A Perspective on the Conservative Treatment for Osteoarthritis of the Knee. J. Biosci. Med. 2017, 5, 11–20. [Google Scholar] [CrossRef]
- Moghaddam, S.S.; Momeni, M.; Atabaki, S.M.; Shabestari, T.M.; Boustanshenas, M.; Afshar, M.; Roham, M. Topical Treatment of Second-Degree Burn Wounds With Lactobacillus Plantarum Supernatant: Phase I Trial. Iran. J. Pathol. 2022, 17, 460. [Google Scholar] [CrossRef]
- Moroz, E.; Matoori, S.; Leroux, J. Oral Delivery of Macromolecular Drugs: Where We Are After Almost 100 Years of Attempts. Adv. Drug Deliv. Rev. 2016, 101, 108–121. [Google Scholar] [CrossRef]
- Mayandi, V.; Chua, A.W.C.; Dhand, C.; Lim, F.P.; Aung, T.T.; Harini, S.; Dwivedi, N.; Periayah, M.H.; Sridhar, S.; Fazil, M.H.; et al. Multifunctional Antimicrobial Nanofiber Dressings Containing Ε-Polylysine for the Eradication of Bacterial Bioburden and Promotion of Wound Healing in Critically Colonized Wounds. Acs Appl. Mater. Interfaces 2020, 12, 15989–16005. [Google Scholar] [CrossRef]
- Yildiz, S.C.; Demir, C.; Cengiz, M.; Ayhanci, A. Protective Properties of Kefir on Burn Wounds of Mice That Were Infected with S. aureus, P. auroginasa and E. coli. Cell. Mol. Biol. 2019, 65, 60–65. [Google Scholar] [CrossRef]
- Chalwade, C.; Sawant, A.; Katyal, I. Study to Determine the Effect of Diaper-Based Wound Care Method in Reducing Wound Contamination Period in Patients Suffering From Perianal Burn Wound. Indian. J. Plast. Surg. 2023, 56, 378–381. [Google Scholar] [CrossRef]
- Sahu, R.K.; Midya, M. “Hand Inside Glove”: Useful Method of Burn Dressing in Children. J. Fam. Med. Prim. Care 2019, 8, 1483–1485. [Google Scholar] [CrossRef]
- Molkentine, J.M.; Fujimoto, T.N.; Horvath, T.D.; Grossberg, A.J.; Garcia, C.J.G.; Deorukhkar, A.; de la Cruz Bonilla, M.; Lin, D.; Samuel, E.L.G.; Chan, W.K.; et al. Enteral Activation of WR-2721 Mediates Radioprotection and Improved Survival From Lethal Fractionated Radiation. Sci. Rep. 2019, 9, 1949. [Google Scholar] [CrossRef]
- Rathbone, M.J.; Pather, I.; Şenel, S. Overview of Oral Mucosal Delivery. In Oral Mucosal Drug Delivery and Therapy. Advances in Delivery Science and Technology; Springer: Boston, MA, USA, 2015. [Google Scholar] [CrossRef]
- Ledet, G.; Biswas, S.K.; Kumar, V.P.; Graves, R.A.; Mitchner, D.M.; Parker, T.M.; Bostanian, L.A.; Ghosh, S.; Mandal, T.K. Development of Orally Administered Γ-Tocotrienol (GT3) Nanoemulsion for Radioprotection. Int. J. Mol. Sci. 2016, 18, 28. [Google Scholar] [CrossRef]
- Zgair, A.; Dawood, Y.; Ibrahem, S.M.; Back, H.; Kagan, L.; Gershkovich, P.; Lee, J.B. Predicting Intestinal and Hepatic First-Pass Metabolism of Orally Administered Testosterone Undecanoate. Appl. Sci. 2020, 10, 7283. [Google Scholar] [CrossRef]
- Mahran, Y.F.; Al-Kharashi, L.A.; Atawia, R.T.; Alanazi, R.T.; Dhahi, A.M.B.; Alsubaie, R.; Badr, A.M. Radioprotective Effects of Carvacrol and/or Thymol against Gamma Irradiation-Induced Acute Nephropathy: In Silico and In Vivo Evidence of the Involvement of Insulin-like Growth Factor-1 (IGF-1) and Calcitonin Gene-Related Peptide. Biomedicines 2023, 11, 2521. [Google Scholar] [CrossRef]
- Abedi, S.M.; Yarmand, F.; Motallebnejad, M.; Seyedmajidi, M.; Moslemi, D.; Bijani, A.; Hosseinimehr, S.J. Radioprotective Effect of Thymol Against Salivary Glands Dysfunction Induced by Ionizing Radiation in Rats. Iran. J. Pharm. Res. 2016, 15, 861–866. [Google Scholar]
- Sueishi, Y.; Nii, R. Monoterpene’s Multiple Free Radical Scavenging Capacity as Compared with the Radioprotective Agent Cysteamine and Amifostine. Bioorganic Med. Chem. Lett. 2018, 28, 3031–3033. [Google Scholar] [CrossRef]
- Mahran, Y.F.; Badr, A.M.; Aldosari, A.; Bin-Zaid, R.; Alotaibi, H.N. Carvacrol and Thymol Modulate the Cross-Talk between TNF-α and IGF-1 Signaling in Radiotherapy-Induced Ovarian Failure. Oxidative Med. Cell. Longev. 2019, 2019, e3173745. [Google Scholar] [CrossRef]
- Vasudeva, V.; Tenkanidiyoor, Y.S.; Peter, A.J.; Shetty, J.; Lakshman, S.P.; Fernandes, R.; Patali, K.A. Radioprotective Efficacy of Lutein in Ameliorating Electron Beam Radiation-Induced Oxidative Injury in Swiss Albino Mice. Iran. J. Med. Sci. 2018, 43, 41–51. [Google Scholar]
- Meydan, D.; Gursel, B.; Bilgici, B.; Can, B.; Ozbek, N. Protective Effect of Lycopene against Radiation-Induced Hepatic Toxicity in Rats. J. Int. Med. Res. 2011, 39, 1239–1252. [Google Scholar] [CrossRef]
- Srinivasan, M.; Devipriya, N.; Kalpana, K.B.; Menon, V.P. Lycopene: An Antioxidant and Radioprotector against Gamma-Radiation-Induced Cellular Damages in Cultured Human Lymphocytes. Toxicology 2009, 262, 43–49. [Google Scholar] [CrossRef]
- Vazifedan, V.; Mousavi, S.H.; Sargolzaei, J.; Soleymanifard, S.; Fani Pakdel, A. Study of Crocin & Radiotherapy-Induced Cytotoxicity and Apoptosis in the Head and Neck Cancer (HN-5) Cell Line. Iran. J. Pharm. Res. 2017, 16, 230–237. [Google Scholar]
- Kumar, S.; Pandey, A.K. Chemistry and Biological Activities of Flavonoids: An Overview. Sci. World J. 2013, 2013, 162750. [Google Scholar] [CrossRef]
- Rybak, M.; Wojdyło, A. Inhibition of α-Amylase, α-Glucosidase, Pancreatic Lipase, 15-Lipooxygenase and Acetylcholinesterase Modulated by Polyphenolic Compounds, Organic Acids, and Carbohydrates of Prunus Domestica Fruit. Antioxidants 2023, 12, 1380. [Google Scholar] [CrossRef]
- Li, M.; Qian, M.; Jiang, Q.; Tan, B.; Yin, Y.; Han, X. Evidence of Flavonoids on Disease Prevention. Antioxidants 2023, 12, 527. [Google Scholar] [CrossRef]
- Ysrafil, Y.; Sapiun, Z.; Slamet, N.S.; Mohamad, F.; Hartati, H.; Damiti, S.A.; Alexandra, F.D.; Rahman, S.; Masyeni, S.; Harapan, H.; et al. Anti-Inflammatory Activities of Flavonoid Derivates. ADMET DMPK 2023, 11, 331–359. [Google Scholar] [CrossRef]
- Haddadi, G.H.; Rezaeyan, A.; Mosleh-Shirazi, M.A.; Hosseinzadeh, M.; Fardid, R.; Najafi, M.; Salajegheh, A. Hesperidin as Radioprotector against Radiation-Induced Lung Damage in Rat: A Histopathological Study. J. Med. Phys. 2017, 42, 25–32. [Google Scholar] [CrossRef]
- Musa, A.E.; Omyan, G.; Esmaely, F.; Shabeeb, D. Radioprotective effect of hesperidin: A systematic review. Medicina 2019, 55, 370. [Google Scholar] [CrossRef]
- Kalpana, K.B.; Devipriya, N.; Srinivasan, M.; Vishwanathan, P.; Thayalan, K.; Menon, V.P. Evaluating the Radioprotective Effect of Hesperidin in the Liver of Swiss Albino Mice. Eur. J. Pharmacol. 2011, 658, 206–212. [Google Scholar] [CrossRef]
- Jagetia, G.; Rao, K. Hesperidin Treatment Abates Radiation-Induced Delay In Healing of Deep Cutaneous Excision Wound of Mice Hemi-Body Exposed to Different Doses of γ-Radiation. Clin. Dermatol. Dermatitis 2018, 1, 104. [Google Scholar]
- Hosseinimehr, S.J.; Mahmoudzadeh, A.; Ahmadi, A.; Mohamadifar, S.; Akhlaghpoor, S. Radioprotective Effects of Hesperidin against Genotoxicity Induced by Gamma-Irradiation in Human Lymphocytes. Mutagenesis 2009, 24, 233–235. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Peng, R.; Chen, Z.; Yu, H.; Wang, S.; Dong, S.; Li, W.; Shao, W.; Dai, J.; Li, F.; et al. The Protective Effects of Apigenin Against Radiation-Induced Intestinal Injury. Dose Response 2022, 20, 15593258221113791. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zheng, L.; Sun, Y.; Wang, T.; Wang, B. Tangeretin Enhances Radiosensitivity and Inhibits the Radiation-Induced Epithelial-Mesenchymal Transition of Gastric Cancer Cells. Oncol. Rep. 2015, 34, 302–310. [Google Scholar] [CrossRef]
- Kang, K.A.; Piao, M.J.; Ryu, Y.S.; Hyun, Y.J.; Park, J.E.; Shilnikova, K.; Zhen, A.X.; Kang, H.K.; Koh, Y.S.; Jeong, Y.J.; et al. Luteolin Induces Apoptotic Cell Death via Antioxidant Activity in Human Colon Cancer Cells. Int. J. Oncol. 2017, 51, 1169–1178. [Google Scholar] [CrossRef]
- Shimoi, K.; Masuda, S.; Furugori, M.; Esaki, S.; Kinae, N. Radioprotective Effect of Antioxidative Flavonoids in Gamma-Ray Irradiated Mice. Carcinogenesis 1994, 15, 2669–2672. [Google Scholar] [CrossRef]
- Toyama, M.; Mori, T.; Takahashi, J.; Iwahashi, H. Luteolin as Reactive Oxygen Generator by X-Ray and UV Irradiation. Radiat. Phys. Chem. 2018, 146, 11–18. [Google Scholar] [CrossRef]
- Patil, S.L.; Mallaiah, S.H.; Patil, R.K. Antioxidative and Radioprotective Potential of Rutin and Quercetin in Swiss Albino Mice Exposed to Gamma Radiation. J. Med. Phys. 2013, 38, 87–92. [Google Scholar] [CrossRef]
- Benkovic, V.; Knezevic, A.H.; Dikic, D.; Lisicic, D.; Orsolic, N.; Basic, I.; Kosalec, I.; Kopjar, N. Radioprotective Effects of Propolis and Quercetin in Gamma-Irradiated Mice Evaluated by the Alkaline Comet Assay. Phytomedicine 2008, 15, 851–858. [Google Scholar] [CrossRef]
- Ping, X.; Junqing, J.; Junfeng, J.; Enjin, J. Radioprotective Effects of Troxerutin against Gamma Irradiation in Mice Liver. Int. J. Radiat. Biol. 2012, 88, 607–612. [Google Scholar] [CrossRef]
- Maurya, D.K.; Salvi, V.P.; Krishnan Nair, C.K. Radioprotection of Normal Tissues in Tumor-Bearing Mice by Troxerutin. J. Radiat. Res. 2004, 45, 221–228. [Google Scholar] [CrossRef]
- Ping, X.; Junqing, J.; Junfeng, J.; Enjin, J. Radioprotective Effects of Troxerutin against Gamma Irradiation in V79 Cells and Mice. Asian Pac. J. Cancer Prev. 2011, 12, 2593–2596. [Google Scholar] [PubMed]
- Song, L.; Ma, L.; Cong, F.; Shen, X.; Jing, P.; Ying, X.; Zhou, H.; Jiang, J.; Fu, Y.; Yan, H. Radioprotective Effects of Genistein on HL-7702 Cells via the Inhibition of Apoptosis and DNA Damage. Cancer Lett. 2015, 366, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Canyilmaz, E.; Uslu, G.H.; Bahat, Z.; Kandaz, M.; Mungan, S.; Haciislamoglu, E.; Mentese, A.; Yoney, A. Comparison of the Effects of Melatonin and Genistein on Radiation-Induced Nephrotoxicity: Results of an Experimental Study. Biomed. Rep. 2016, 4, 45–50. [Google Scholar] [CrossRef]
- Fan, Z.-L.; Wang, Z.-Y.; Zuo, L.-L.; Tian, S.-Q. Protective Effect of Anthocyanins from Lingonberry on Radiation-Induced Damages. Int. J. Environ. Res. Public Health 2012, 9, 4732–4743. [Google Scholar] [CrossRef]
- Shamilov, A.A.; Bubenchikova, V.N.; Chernikov, M.V.; Pozdnyakov, D.I.; Garsiya, E.R. Vaccinium vitis-Idaea L.: Chemical Contents, Pharmacological Activities. Pharm. Sci. 2020, 26, 344–362. [Google Scholar] [CrossRef]
- Abou-Zeid, S.M.; EL-bialy, B.E.; EL-borai, N.B.; AbuBakr, H.O.; Elhadary, A.M.A. Radioprotective Effect of Date Syrup on Radiation-Induced Damage in Rats. Sci. Rep. 2018, 8, 7423. [Google Scholar] [CrossRef] [PubMed]
- Batanony, M.E.; El-Feky, A.M. Manipulation of Different Phytochemical Classes Against Inflammation Induced by Radiations. Egypt. J. Chem. 2021, 65, 81–96. [Google Scholar] [CrossRef]
- Gheleshli, N.; Ghasemi, A.; Hosseinimehr, S.J. The Influence of Piperine on Radioprotective Effect of Curcumin in Irradiated Human Lymphocytes. Turk. J. Pharm. Sci. 2018, 16, 366. [Google Scholar] [CrossRef] [PubMed]
- Amin, F.; Shah, S.A.; Badshah, H.; Khan, M.; Kim, M.O. Anthocyanins Encapsulated by PLGA@PEG Nanoparticles Potentially Improved Its Free Radical Scavenging Capabilities via P38/JNK Pathway against Aβ1–42-Induced Oxidative Stress. J. Nanobiotechnol. 2017, 15. [Google Scholar] [CrossRef] [PubMed]
- de Melo, L.F.M.; Aquino-Martins, V.G. de Q.; Silva, A.P. da; Oliveira Rocha, H.A.; Scortecci, K.C. Biological and Pharmacological Aspects of Tannins and Potential Biotechnological Applications. Food Chem. 2023, 414, 135645. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarek, B. Tannic Acid with Antiviral and Antibacterial Activity as A Promising Component of Biomaterials—A Minireview. Materials 2020, 13, 3224. [Google Scholar] [CrossRef] [PubMed]
- Nair, G.G.; Nair, C.K.K. Radioprotective Effects of Gallic Acid in Mice. Biomed. Res. Int. 2013, 2013, 953079. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Huang, Y.; Liang, J.; Ou, M.; Chen, J.; Li, G. Extraction, Purification and Anti-Radiation Activity of Persimmon Tannin from Diospyros Kaki L.f. J. Env. Radioact. 2016, 162–163, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.A.; Lee, I.K.; Zhang, R.; Piao, M.J.; Kim, K.C.; Kim, S.Y.; Shin, T.; Kim, B.J.; Lee, N.H.; Hyun, J.W. Radioprotective Effect of Geraniin via the Inhibition of Apoptosis Triggered by γ-Radiation-Induced Oxidative Stress. Cell Biol. Toxicol. 2011, 27, 83–94. [Google Scholar] [CrossRef]
- Ahire, V.; Kumar, A.; Mishra, K.P.; Kulkarni, G. Ellagic Acid Enhances Apoptotic Sensitivity of Breast Cancer Cells to γ-Radiation. Nutr. Cancer 2017, 69, 904–910. [Google Scholar] [CrossRef]
- Dongmo Zeukang, R.; Kalinski, J.-C.; Tembeni, B.; Goosen, E.D.; Tembu, J.; Tabopda Kuiate, T.; Ngono Bikobo, D.S.; Tagatsing Fotsing, M.; Atchadé, A.D.T.; Siwe-Noundou, X. Quinones from Cordia Species from 1972 to 2023: Isolation, Structural Diversity and Pharmacological Activities. Nat. Prod. Bioprospect. 2023, 13, 52. [Google Scholar] [CrossRef]
- Chan-Zapata, I.; Borges-Argáez, R.; Ayora-Talavera, G. Quinones as Promising Compounds against Respiratory Viruses: A Review. Molecules 2023, 28, 1981. [Google Scholar] [CrossRef] [PubMed]
- Cores, Á.; Carmona-Zafra, N.; Clerigué, J.; Villacampa, M.; Menéndez, J.C. Quinones as Neuroprotective Agents. Antioxidants 2023, 12, 1464. [Google Scholar] [CrossRef]
- Saihara, K.; Kamikubo, R.; Ikemoto, K.; Uchida, K.; Akagawa, M. Pyrroloquinoline Quinone, a Redox-Active o-Quinone, Stimulates Mitochondrial Biogenesis by Activating the SIRT1/PGC-1α Signaling Pathway. Biochemistry 2017, 56, 6615–6625. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Chen, N.; Miao, D. Radioprotective Effects of Pyrroloquinoline Quinone on Parotid Glands in C57BL/6J Mice. Exp. Ther. Med. 2016, 12, 3685–3693. [Google Scholar] [CrossRef]
- Xiong, X.-H.; Zhao, Y.; Ge, X.; Yuan, S.-J.; Wang, J.-H.; Zhi, J.-J.; Yang, Y.-X.; Du, B.-H.; Guo, W.-J.; Wang, S.-S.; et al. Production and Radioprotective Effects of Pyrroloquinoline Quinone. Int. J. Mol. Sci. 2011, 12, 8913–8923. [Google Scholar] [CrossRef]
- Jamwal, V.; Mishra, S.; Singh, A.; Kumar, R. Free Radical Scavenging and Radioprotective Activities of Hydroquinone in Vitro. J. Radioprot. Res. 2014, 2, 37–45. [Google Scholar] [CrossRef]
- Dey, P.; Kundu, A.; Kumar, A.; Gupta, M.; Lee, B.M.; Bhakta, T.; Dash, S.; Kim, H.S. Analysis of Alkaloids (Indole Alkaloids, Isoquinoline Alkaloids, Tropane Alkaloids). Recent. Adv. Nat. Prod. Anal. 2020, 505–567. [Google Scholar] [CrossRef]
- Xu, J.-Y.; Zhao, L.; Chong, Y.; Jiao, Y.; Qin, L.-Q.; Fan, S.-J. Protection Effect of Sanguinarine on Whole-Body Exposure of X Radiation in BALB/c Mice. Braz. J. Pharm. Sci. 2014, 50, 101–106. [Google Scholar] [CrossRef]
- Pimentel, M.J.; Filho, M.M.V.B.; Araújo, M.; Gomes, D.Q.; DA Costa, L.J. Evaluation of Radioprotective Effect of Pilocarpine Ingestion on Salivary Glands. Anticancer. Res. 2014, 34, 1993–1999. [Google Scholar] [PubMed]
- Kanimozhi, G.; Prasad, N.R.; Ramachandran, S.; Pugalendi, K.V. Umbelliferone Modulates Gamma-Radiation Induced Reactive Oxygen Species Generation and Subsequent Oxidative Damage in Human Blood Lymphocytes. Eur. J. Pharmacol. 2011, 672, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Zhao, Q.-L.; ur Rehman, M.; Jawaid, P.; Cui, Z.-G.; Ahmed, K.; Kondo, T.; Saitoh, J.-I.; Noguchi, K. Isofraxidin Enhances Hyperthermia-induced Apoptosis via Redox Modification in Acute Monocytic Leukemia U937 Cells. Mol. Med. Rep. 2023, 27, 41. [Google Scholar] [CrossRef] [PubMed]
- Salloum, R.M.; Jaskowiak, N.T.; Mauceri, H.J.; Seetharam, S.; Beckett, M.A.; Koons, A.M.; Hari, D.M.; Gupta, V.K.; Reimer, C.; Kalluri, R.; et al. NM-3, an Isocoumarin, Increases the Antitumor Effects of Radiotherapy without Toxicity. Cancer Res. 2000, 60, 6958–6963. [Google Scholar] [PubMed]
- Antropova, I.G.; Revina, A.A.; Kurakina, E.; Magomedbekov, E.P. Radiation Chemical Investigation of Antioxidant Activity of Biologically Important Compounds From Plant Materials. Acs Omega 2020, 5, 5976–5983. [Google Scholar] [CrossRef] [PubMed]
- Yang, N.; He, X.; Ran, L.; Yang, F.; Ma, C.; Chen, H.; Xiang, D.; Shen, G.; Zhang, P.; He, L.; et al. The Mechanism of Coumarin Inhibits Germination of Ryegrass (Lolium perenne) and Its Application as Coumarin-Carbon Dots Nanocomposites. Pest. Manag. Sci. 2023, 79, 2182–2190. [Google Scholar] [CrossRef] [PubMed]
- Citarella, A.; Vittorio, S.; Dank, C.; Ielo, L. Syntheses, Reactivity, and Biological Applications of Coumarins. Front. Chem. 2024, 12, 1362992. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.-R.; Zhu, N.; Hao, Y.-T.; Yu, X.-C.; Li, Z.; Mao, R.-X.; Liu, R.; Kang, J.-W.; Hu, J.-N.; Li, Y. Radioprotective Effect of Whey Hydrolysate Peptides against γ-Radiation-Induced Oxidative Stress in BALB/c Mice. Nutrients 2021, 13, 816. [Google Scholar] [CrossRef] [PubMed]
- Sharapov, M.G.; Novoselov, V.I.; Gudkov, S.V. Radioprotective Role of Peroxiredoxin 6. Antioxidants 2019, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- Wahab, S.; Annadurai, S.; Abullais, S.S.; Das, G.; Ahmad, W.; Ahmad, M.F.; Kandasamy, G.; Vasudevan, R.; Ali, M.S.; Amir, M. Glycyrrhiza glabra (Licorice): A Comprehensive Review on Its Phytochemistry, Biological Activities, Clinical Evidence and Toxicology. Plants 2021, 10, 2751. [Google Scholar] [CrossRef]
- Das, D.; Agarwal, S.K.; Chandola, H.M. Protective Effect of Yashtimadhu (Glycyrrhiza glabra) against Side Effects of Radiation/Chemotherapy in Head and Neck Malignancies. Ayu 2011, 32, 196–199. [Google Scholar] [CrossRef]
- Mamgain, R.K.; Gupta, M.; Mamgain, P.; Verma, S.K.; Pruthi, D.S.; Kandwal, A.; Saini, S. The Efficacy of an Ayurvedic Preparation of Yashtimadhu (Glycyrrhiza glabra) on Radiation-Induced Mucositis in Head-and-Neck Cancer Patients: A Pilot Study. J. Cancer Res. Ther. 2020, 16, 458. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.-R.; Wang, X.-Y.; Sun, Y.-M.; Zhang, C.; Liu, K.J.; Zhang, F.-Y.; Xiang, B. Glycyrrhizin Protects Submandibular Gland Against Radiation Damage by Enhancing Antioxidant Defense and Preserving Mitochondrial Homeostasis. Antioxid. Redox Signal. 2023. [Google Scholar] [CrossRef] [PubMed]
- Shetty, T.K.; Satav, J.G.; Nair, C.K.K. Protection of DNA and Microsomal Membranes in Vitro by Glycyrrhiza glabra L. against Gamma Irradiation. Phytother. Res. 2002, 16, 576–578. [Google Scholar] [CrossRef]
- Darwish, M.M.; Hussien, E.M.; Haggag, A.M. Possible Role of Licorice Roots (Glycyrrhiza glabra) as a Natural Radioprotector against Oxidative Damage in Rats. Egypt. J. Radiat. Sci. Appl. 2007, 20, 95–108. [Google Scholar]
- Tan, Q.-Y.; Hu, Q.; Zhu, S.; Jia, L.; Xiao, J.; Su, H.; Huang, S.; Zhang, J.; Jin, J. Licorice Root Extract and Magnesium Isoglycyrrhizinate Protect against Triptolide-Induced Hepatotoxicity via up-Regulation of the Nrf2 Pathway. Drug Deliv. 2018, 25, 1213–1223. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekharan, D.K.; Khanna, P.K.; Nair, C.K.K. Cellular Radioprotecting Potential of Glyzyrrhizic Acid, Silver Nanoparticle and Their Complex. Mutat. Res. /Genet. Toxicol. Environ. Mutagen. 2011, 723, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.; González-Burgos, E.; Iglesias, I.; Gómez-Serranillos, M.P. Pharmacological Update Properties of Aloe Vera and Its Major Active Constituents. Molecules 2020, 25, 1324. [Google Scholar] [CrossRef] [PubMed]
- Dadupanthi, P. Radioprotection of aloe vera against biochemical alterations in swiss albino mice. Int. J. Curr. Pharm. Res. 2018, 10, 55–59. [Google Scholar] [CrossRef]
- Haddad, P.; Amouzgar–Hashemi, F.; Samsami, S.; Chinichian, S.; Oghabian, M.A. Aloe Vera for Prevention of Radiation-Induced Dermatitis: A Self-Controlled Clinical Trial. Curr. Oncol. 2013, 20, e345. [Google Scholar] [CrossRef]
- Dadupanthi, P. Radioprotective effects of aloe vera on hepatosomatic index of swiss albino mice. Int. J. Curr. Pharm. Res. 2019, 97–99. [Google Scholar] [CrossRef]
- Nejaim, Y.; Silva, A.I.; Vasconcelos, T.V.; Silva, E.J.; de Almeida, S.M. Evaluation of Radioprotective Effect of Aloe Vera and Zinc/Copper Compounds against Salivary Dysfunction in Irradiated Rats. J. Oral. Sci. 2014, 56, 191–194. [Google Scholar] [CrossRef][Green Version]
- Liu, Z.-G.; Qian, X.; Wang, Z.-M.; Ning, J.-L.; Qin, C.-K.; Huang, Z.-M.; Li, Y.-M.; He, N.; Lin, D.-H.; Zhou, Z.-D.; et al. Effects of Persimmon Tannin-Aloe Vera Composite on Cytotoxic Activities, and Radioprotection Against X-Rays Irradiated in Human Hepatoma and Hepatic Cells. J. Biomed. Nanotechnol. 2021, 17, 2043–2052. [Google Scholar] [CrossRef]
- Hudz, N.; Kobylinska, L.; Pokajewicz, K.; Horčinová Sedláčková, V.; Fedin, R.; Voloshyn, M.; Myskiv, I.; Brindza, J.; Wieczorek, P.P.; Lipok, J. Mentha piperita: Essential Oil and Extracts, Their Biological Activities, and Perspectives on the Development of New Medicinal and Cosmetic Products. Molecules 2023, 28, 7444. [Google Scholar] [CrossRef]
- Hemeg, H.A.; Moussa, I.M.; Ibrahim, S.; Dawoud, T.M.; Alhaji, J.H.; Mubarak, A.S.; Kabli, S.A.; Alsubki, R.A.; Tawfik, A.M.; Marouf, S.A. Antimicrobial Effect of Different Herbal Plant Extracts against Different Microbial Population. Saudi J. Biol. Sci. 2020, 27, 3221–3227. [Google Scholar] [CrossRef]
- Jagetia, G.C.; Baliga, M.S. Influence of the Leaf Extract of Mentha arvensis Linn. (Mint) on the Survival of Mice Exposed to Different Doses of Gamma Radiation. Strahlenther. Onkol. 2002, 178, 91–98. [Google Scholar] [CrossRef]
- Samarth, R.M.; Kumar, A. Radioprotection of Swiss Albino Mice by Plant Extract Mentha piperita (Linn.). J. Radiat. Res. 2003, 44, 101–109. [Google Scholar] [CrossRef]
- Samarth, R.M.; Samarth, M. Protection against Radiation-Induced Testicular Damage in Swiss Albino Mice by Mentha piperita (Linn.). Basic. Clin. Pharmacol. Toxicol. 2009, 104, 329–334. [Google Scholar] [CrossRef]
- Samarth, R.M.; Kumar, A. Mentha piperita (Linn.) Leaf Extract Provides Protection against Radiation Induced Chromosomal Damage in Bone Marrow of Mice. Indian. J. Exp. Biol. 2003, 41, 229–237. [Google Scholar]
- Baliga, M.S.; Rao, S. Radioprotective Potential of Mint: A Brief Review. J. Cancer Res. Ther. 2010, 6, 255–262. [Google Scholar] [CrossRef]
- Sancheti, G.; Goyal, P.K. Prevention of Radiation Induced Hematological Alterations by Medicinal Plant Rosmarinus Officinalis, in Mice. Afr. J. Tradit. Complement. Altern. Med. 2006, 4, 165–172. [Google Scholar] [CrossRef]
- Singh, B.; Sharma, R.A. Updated Review on Indian Ficus Species. Arab. J. Chem. 2023, 16, 104976. [Google Scholar] [CrossRef]
- Vinutha, K.; Vidya, S.M.; Suchetha, N.K.; Sanjeev, G.; Nagendra, H.G.; Pradeepa, V.C. Radioprotective Activity of Ficus Racemosa Ethanol Extract against Electron Beam Induced DNA Damage in Vitro, in VIVO and in Silico. Int. J. Pharm. Pharm. Sci. 2015, 7, 110–119. [Google Scholar]
- Veerapur, V.; Prabhakar, K.; Parihar, V.; Kandadi, M.; SB, R.; Mishra, B.; Rao, S.; Srinivasan, K.K.; Priyadarsini, I.; Unnikrishnan, M.K. Ficus racemosa Stem Bark Extract: A Potent Antioxidant and a Probable Natural Radioprotector. Evid. Based Complement. Altern. Med. 2007, 6, 317–324. [Google Scholar] [CrossRef]
- Okumus, S.; Taysi, S.; Orkmez, M.; Saricicek, E.; Demir, E.; Adli, M.; Al, B. The Effects of Oral Ginkgo Biloba Supplementation on Radiation-Induced Oxidative Injury in the Lens of Rat. Pharmacogn. Mag. 2011, 7, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Sener, G.; Kabasakal, L.; Atasoy, B.M.; Erzik, C.; Velioğlu-Oğünç, A.; Cetinel, S.; Gedik, N.; Yeğen, B.C. Ginkgo Biloba Extract Protects against Ionizing Radiation-Induced Oxidative Organ Damage in Rats. Pharmacol. Res. 2006, 53, 241–252. [Google Scholar] [CrossRef]
- Ismail, A.F.M.; El-Sonbaty, S.M. Fermentation Enhances Ginkgo Biloba Protective Role on Gamma-Irradiation Induced Neuroinflammatory Gene Expression and Stress Hormones in Rat Brain. J. Photochem. Photobiol. B Biol. 2016, 158, 154–163. [Google Scholar] [CrossRef]
- He, N.; Wang, Q.; Huang, H.; Chen, J.; Wu, G.; Zhu, M.; Shao, F.; Yan, Z.; Sang, Z.; Cao, L.; et al. A Comprehensive Review on Extraction, Structure, Detection, Bioactivity, and Metabolism of Flavonoids from Sea Buckthorn (Hippophae rhamnoides L.). J. Food Biochem. 2023, 2023, e4839124. [Google Scholar] [CrossRef]
- Dubey, R.K.; Shukla, S.; Shukla, V.; Singh, S. Sea Buckthorn: A Potential Dietary Supplement with Multifaceted Therapeutic Activities. Intell. Pharm. 2023. [Google Scholar] [CrossRef]
- Gupta, V.; Bala, M.; Prasad, J.; Singh, S.; Gupta, M. Leaves of Hippophae rhamnoides Prevent Taste Aversion in Gamma-Irradiated Rats. J. Diet. Suppl. 2011, 8, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Sureshbabu, A.V.S.; Barik, T.K.; Namita, I.; Prem Kumar, I. Radioprotective Properties of Hippophae rhamnoides (Sea Buckthorn) Extract in Vitro. Int. J. Health Sci. (Qassim) 2008, 2, 45–62. [Google Scholar]
- Chawla, R.; Arora, R.; Singh, S.; Sagar, R.K.; Sharma, R.K.; Kumar, R.; Sharma, A.; Gupta, M.L.; Singh, S.; Prasad, J.; et al. Radioprotective and Antioxidant Activity of Fractionated Extracts of Berries of Hippophae rhamnoides. J. Med. Food 2007, 10, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Pooja; Kumar, A. A Systemic Review of Tulsi (Ocimum tenuiflorum or Ocimum sanctum): Phytoconstituents, Ethnobotanical and Pharmacological Profile. Res. J. Pharmacogn. Phytochem. 2023, 15, 179–188. [Google Scholar] [CrossRef]
- Hasan, M.R.; Alotaibi, B.S.; Althafar, Z.M.; Mujamammi, A.H.; Jameela, J. An Update on the Therapeutic Anticancer Potential of Ocimum sanctum L.: “Elixir of Life”. Molecules 2023, 28, 1193. [Google Scholar] [CrossRef]
- Devi, P.U.; Ganasoundari, A. Radioprotective Effect of Leaf Extract of Indian Medicinal Plant Ocimum sanctum. Indian J. Exp. Biol. 1995, 33, 205–208. [Google Scholar] [PubMed]
- Ganasoundari, A.; Zare, S.M.; Devi, P.U. Modification of Bone Marrow Radiosensensitivity by Medicinal Plant Extracts. Br. J. Radiol. 1997, 70, 599–602. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, M.; Chintalwar, G.J.; Chattopadhyay, S. Antioxidant and Radioprotective Properties of an Ocimum sanctum Polysaccharide. Redox Rep. 2005, 10, 257–264. [Google Scholar] [CrossRef]
- Bhat, S.; Farooq, A.; Iqbal, A. A Comprehensive Review of Emblica Officinalis (Āmla): Its Medicinal Properties and Therapeutic Uses. Int. J. Unani Integr. Med. 2023, 7, 01–03. [Google Scholar] [CrossRef]
- Gandhi, Y.; Grewal, J.; Jain, V.; Rawat, H.; Mishra, S.K.; Kumar, V.; Kumar, R.; Shakya, S.K.; Sharma, P.; Dhanjal, D.S.; et al. Emblica Officinalis: A Promising Herb Confining Versatile Applications. S. Afr. J. Bot. 2023, 159, 519–531. [Google Scholar] [CrossRef]
- Singh, I.; Sharma, A.; Jindal, A.; Soyal, D.; Goyal, P.K. Protective effect of emblica officinalis fruit extract against gamma irradiation in mice. Pharmacologyonline 2006, 2, 128–150. [Google Scholar]
- Singh, I.; Sharma, A.; Jindal, A.; Soyal, D.; Goyal, P. Fruit Extract of Emblica Officinalis (Amla) Protects Radiation Induced Biochemical Lesions In The Brain of Swiss Albino Mice. Ann. Neurosci. 2006, 13, 65–71. [Google Scholar] [CrossRef]
- Singh, I.; Sharma, A.; Nunia, V.; Goyal, P.K. Radioprotection of Swiss Albino Mice by Emblica Officinalis. Phytother. Res. 2005, 19, 444–446. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Liang, W.; Wan, J.; Wang, M. Spinach (Spinacia oleracea) Microgreen Prevents the Formation of Advanced Glycation End Products in Model Systems and Breads. Curr. Res. Food Sci. 2023, 6, 100490. [Google Scholar] [CrossRef] [PubMed]
- Naseem, A.; Akhtar, S.; Ismail, T.; Qamar, M.; Sattar, D.; Saeed, W.; Esatbeyoglu, T.; Bartkiene, E.; Rocha, J.M. Effect of Growth Stages and Lactic Acid Fermentation on Anti-Nutrients and Nutritional Attributes of Spinach (Spinacia oleracea). Microorganisms 2023, 11, 2343. [Google Scholar] [CrossRef]
- Bhatia, A.L.; Jain, M. Spinacia oleracea L. Protects against Gamma Radiations: A Study on Glutathione and Lipid Peroxidation in Mouse Liver. Phytomedicine 2004, 11, 607–615. [Google Scholar] [CrossRef] [PubMed]
- Sisodia, R.; Yadav, R.K.; Sharma, K.V.; Bhatia, A.L. Spinacia oleracea Modulates Radiation-Induced Biochemical Changes in Mice Testis. Indian. J. Pharm. Sci. 2008, 70, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Niu, H.; Li, Q.; Jiao, L.; Li, H.; Wu, W. Active Compounds of Panax Ginseng in the Improvement of Alzheimer’s Disease and Application of Spatial Metabolomics. Pharmaceuticals 2023, 17, 38. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Wang, Y.; Xu, Q.; Ma, J.; Li, X.; Tian, Y.; Wen, Y.; Chen, T. Ginseng and Health Outcomes: An Umbrella Review. Front. Pharmacol. 2023, 14, 1069268. [Google Scholar] [CrossRef] [PubMed]
- Pande, S.; Kumar, M.; Kumar, A. Evaluation of Radiomodifying Effects of Root Extract of Panax Ginseng. Phytother. Res. 1998, 12, 13–17. [Google Scholar] [CrossRef]
- Kim, S.H.; Son, C.H.; Nah, S.Y.; Jo, S.K.; Jang, J.S.; Shin, D.H. Modification of Radiation Response in Mice by Panax Ginseng and Diethyldithiocarbamate. In Vivo 2001, 15, 407–411. [Google Scholar]
- Verma, P.; Jahan, S.; Kim, T.H.; Goyal, P.K. Management of Radiation Injuries by Panax Ginseng Extract. J. Ginseng Res. 2011, 35, 261–271. [Google Scholar] [CrossRef]
- Verma, P.; Sharma, P.; Parmar, J.; Sharma, P.; Agrawal, A.; Goyal, P.K. Amelioration of Radiation-Induced Hematological and Biochemical Alterations in Swiss Albino Mice by Panax Ginseng Extract. Integr. Cancer Ther. 2011, 10, 77–84. [Google Scholar] [CrossRef]
- Su, X.; Lu, G.; Ye, L.; Shi, R.; Zhu, M.; Yu, X.; Li, Z.; Jia, X.; Feng, L. Moringa Oleifera Lam.: A Comprehensive Review on Active Components, Health Benefits and Application. RSC Adv. 2023, 13, 24353–24384. [Google Scholar] [CrossRef] [PubMed]
- Jikah, A.N.; Edo, G.I. Moringa Oleifera: A Valuable Insight into Recent Advances in Medicinal Uses and Pharmacological Activities. J. Sci. Food Agric. 2023, 103, 7343–7361. [Google Scholar] [CrossRef]
- Sinha, M.; Das, D.K.; Datta, S.; Ghosh, S.; Dey, S. Amelioration of Ionizing Radiation Induced Lipid Peroxidation in Mouse Liver by Moringa Oleifera Lam. Leaf Extract. Indian J. Exp. Biol. 2012, 50, 209–215. [Google Scholar] [PubMed]
- Sinha, M.; Das, D.K.; Bhattacharjee, S.; Majumdar, S.; Dey, S. Leaf Extract of Moringa Oleifera Prevents Ionizing Radiation-Induced Oxidative Stress in Mice. J. Med. Food 2011, 14, 1167–1172. [Google Scholar] [CrossRef]
- Pradana, D.L.C.; Rahmi, E.P.; Muti, A.F. The Lethality Dose and Antioxidant Activity of Moringa Oleifera Leaves Extract. IOP Conf. Ser. Earth Environ. Sci. 2022, 1104, 012017. [Google Scholar] [CrossRef]
- Wang, L.; Chen, X.; Wu, A.-M. Mini Review on Antimicrobial Activity and Bioactive Compounds of Moringa Oleifera. Med. Chem. 2016, 6. [Google Scholar] [CrossRef]
- Pahurkar, S.V.; Surana, A.R.; Pawar, P.R. A Review of Ethnopharmacological Uses, Phytochemistry and Pharmacological Attributes of Mesua ferrea Linn. Curr. Tradit. Med. 2023, 10, 1–13. [Google Scholar] [CrossRef]
- Krishnaswamy, M.; Murthuza, S.; Ramachandrappa, D. Antioxidant and Anti-Inflammatory Potency of Mesua ferrea Linn. Indian J. Appl. Res. 2013, 3, 55–59. [Google Scholar]
- Murthuza, S.; Manjunatha, B.K. Radioprotective and Immunomodulatory Effects of Mesua ferrea (Linn.) from Western Ghats of India., in Irradiated Swiss Albino Mice and Splenic Lymphocytes. J. Radiat. Res. Appl. Sci. 2018, 11, 66–74. [Google Scholar] [CrossRef]
- Huang, X.; Fei, Q.; Yu, S.; Liu, S.; Zhang, L.; Chen, X.; Cao, L.; Wang, Z.; Shan, M. A Comprehensive Review: Botany, Phytochemistry, Traditional Uses, Pharmacology, and Toxicology of Spatholobus suberectus Vine Stems. J. Ethnopharmacol. 2023, 312, 116500. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Ganesan, K.; Liu, Q.; Chen, J. A Review of the Pharmacological Potential of Spatholobus Suberectus Dunn on Cancer. Cells 2022, 11, 2885. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.-Z.; Wang, Y.-N.; Tan, X.; Liu, P.; Guo, D.-H.; Yan, C. Protective Effect of JXT Ethanol Extract on Radiation-Induced Hematopoietic Alteration and Oxidative Stress in the Liver. Oxid. Med. Cell Longev. 2018, 2018, 9017835. [Google Scholar] [CrossRef] [PubMed]
- Pal, S.; Saha, C.; Dey, S.K. Studies on Black Tea (Camellia sinensis) Extract as a Potential Antioxidant and a Probable Radioprotector. Radiat. Environ. Biophys. 2013, 52, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, D.; Dey, S.K.; Saha, C. Antagonistic Effects of Black Tea against Gamma Radiation-Induced Oxidative Damage to Normal Lymphocytes in Comparison with Cancerous K562 Cells. Radiat. Environ. Biophys. 2014, 53, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Mondal, T.; Pal, S.; Dey, S.K. Fermented Black Tea Ameliorates Gamma Radiationinducedcellular and DNA Damage in Human Blood Lymphocytes. Int. J. Biotechnol. Res. 2015, 3, 55–64. [Google Scholar]
- Pajonk, F.; Riedisser, A.; Henke, M.; McBride, W.H.; Fiebich, B. The Effects of Tea Extracts on Proinflammatory Signaling. BMC Med. 2006, 4, 28. [Google Scholar] [CrossRef] [PubMed]
- Velho-Pereira, R.; Kumar, A.; Pandey, B.N.; Mishra, K.P.; Jagtap, A.G. Radioprotection by Macerated Extract of Nigella Sativa in Normal Tissues of Fibrosarcoma Bearing Mice. Indian J. Pharm. Sci. 2012, 74, 403–414. [Google Scholar] [CrossRef] [PubMed]
- Kanter, M.; Uzal, C.; Erboga, M.; Takir, M.; Kostek, O. Protective Effects of Nigella Sativa on Gamma Radiation-Induced Jejunal Mucosal Damage in Rats. Pathol.-Res. Pract. 2016, 212, 437–443. [Google Scholar] [CrossRef]
- Çanakci, H.; Yılmaz, A.A.Ş.; Canpolat, M.S.; Şeneldir, H.; Kır, G.; Eris, A.H.; Mayadağlı, A.; Oysu, Ç. Evaluation of the Effect of Topical Application of Nigella Sativa on Acute Radiation-Induced Nasal Mucositis. J. Craniofacial Surg. 2018, 29, e279–e282. [Google Scholar] [CrossRef]
- Doğru, S.; Taysi, S.; Yücel, A. Effects of Thymoquinone in the Lungs of Rats against Radiation-Induced Oxidative Stress. Eur. Rev. Med. Pharmacol. Sci. 2024, 28, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Hejazi, J.; Rastmanesh, R.; Taleban, F.-A.; Molana, S.-H.; Hejazi, E.; Ehtejab, G.; Hara, N. Effect of Curcumin Supplementation During Radiotherapy on Oxidative Status of Patients with Prostate Cancer: A Double Blinded, Randomized, Placebo-Controlled Study. Nutr. Cancer 2016, 68, 77–85. [Google Scholar] [CrossRef]
- Van Hien, T.; Huong, N.B.; Hung, P.M.; Duc, N.B. Radioprotective effect of vitexin in breast cancer patients undergoing cobalt-60 radiotherapy. Integr. Cancer Ther. 2002, 1, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.-K.; O’Brien, K.F.; Wang, W.; Johnke, R.M.; Sheng, C.; Benhabib, S.M.; Wang, T.; Allison, R.R. Radioprotective Effect of American Ginseng on Human Lymphocytes at 90 Minutes Postirradiation: A Study of 40 Cases. J. Altern. Complement. Med. 2010, 16, 561–567. [Google Scholar] [CrossRef]
- Hosseinimehr, S.J.; Mahmoudzadeh, A.; Azadbakht, M.; Akhlaghpoor, S. Radioprotective Effects of Hawthorn against Genotoxicity Induced by Gamma Irradiation in Human Blood Lymphocytes. Radiat. Environ. Biophys. 2009, 48, 95–98. [Google Scholar] [CrossRef]
- Kaczorová, D.; Karalija, E.; Dahija, S.; Bešta-Gajević, R.; Parić, A.; Ćavar Zeljković, S. Influence of Extraction Solvent on the Phenolic Profile and Bioactivity of Two Achillea Species. Molecules 2021, 26, 1601. [Google Scholar] [CrossRef]
- Kumar, K.; Srivastav, S.; Sharanagat, V.S. Ultrasound Assisted Extraction (UAE) of Bioactive Compounds from Fruit and Vegetable Processing by-Products: A Review. Ultrason. Sonochem 2020, 70, 105325. [Google Scholar] [CrossRef]
- Kaufmann, B.; Christen, P. Recent Extraction Techniques for Natural Products: Microwave-Assisted Extraction and Pressurised Solvent Extraction. Phytochem. Anal. 2002, 13, 105–113. [Google Scholar] [CrossRef]
- Shen, L.; Pang, S.; Zhong, M.; Sun, Y.; Qayum, A.; Liu, Y.; Rashid, A.; Xu, B.; Liang, Q.; Ma, H.; et al. A Comprehensive Review of Ultrasonic Assisted Extraction (UAE) for Bioactive Components: Principles, Advantages, Equipment, and Combined Technologies. Ultrason. Sonochemistry 2023, 101, 106646. [Google Scholar] [CrossRef]
- Jibhkate, Y.; Awachat, A.; Lohiya, R.; Umekar, M.; Hemke, A.; Gupta, K. Extraction: An Important Tool in the Pharmaceutical Field. Int. J. Sci. Res. Arch. 2023, 10, 555–568. [Google Scholar] [CrossRef]
- Gościniak, A.; Bazan-Woźniak, A.; Pietrzak, R.; Cielecka-Piontek, J. Pomegranate Flower Extract—The Health-Promoting Properties Optimized by Application of the Box–Behnken Design. Molecules 2022, 27, 6616. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, J.; Yu, X.; Shu, Y.; Zhang, S.; Zhang, Y. Extraction Optimization by Using Response Surface Methodology and Purification of Yellow Pigment from Gardenia jasminoides Var. radicans Makikno. Food Sci. Nutr. 2021, 9, 822–832. [Google Scholar] [CrossRef]
- Beckman, E.J. Supercritical and Near-Critical CO2 in Green Chemical Synthesis and Processing. J. Supercrit. Fluids 2004, 28, 121–191. [Google Scholar] [CrossRef]
- Tankiewicz, M.; Namieśnik, J.; Sawicki, W. Analytical Procedures for Quality Control of Pharmaceuticals in Terms of Residual Solvents Content: Challenges and Recent Developments. TrAC Trends Anal. Chem. 2016, 80, 328–344. [Google Scholar] [CrossRef]
- Hosseinimehr, S.J. Trends in the Development of Radioprotective Agents. Drug Discov. Today 2007, 12, 794–805. [Google Scholar] [CrossRef]
- Paik, D.J.; Lee, C.H. Review of Cases of Patient Risk Associated with Ginseng Abuse and Misuse. J. Ginseng Res. 2015, 39, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Kim, M.-K.; Lee, M.; Kwon, B.-S.; Suh, D.H.; Song, Y.S. Effect of Red Ginseng on Genotoxicity and Health-Related Quality of Life after Adjuvant Chemotherapy in Patients with Epithelial Ovarian Cancer: A Randomized, Double Blind, Placebo-Controlled Trial. Nutrients 2017, 9, 772. [Google Scholar] [CrossRef]
- Elmore, A.R. Cosmetic Ingredient Review Expert Panel Final Report on the Safety Assessment of AloeAndongensis Extract, Aloe Andongensis Leaf Juice, Aloe Arborescens Leaf Extract, Aloe Arborescens Leaf Juice, Aloe Arborescens Leaf Protoplasts, Aloe Barbadensis Flower Extract, Aloe Barbadensis Leaf, Aloe Barbadensis Leaf Extract, Aloe Barbadensis Leaf Juice, Aloe Barbadensis Leaf Polysaccharides, Aloe Barbadensis Leaf Water, Aloe Ferox Leaf Extract, Aloe Ferox Leaf Juice, and Aloe Ferox Leaf Juice Extract. Int. J. Toxicol. 2007, 26 (Suppl 2), 1–50. [Google Scholar] [CrossRef]
- Boudreau, M.D.; Beland, F.A. An Evaluation of the Biological and Toxicological Properties of Aloe Barbadensis (Miller), Aloe Vera. J. Environ. Sci. Health C Environ. Carcinog. Ecotoxicol. Rev. 2006, 24, 103–154. [Google Scholar] [CrossRef]
- Sohal, A.; Alhankawi, D.; Sandhu, S.; Chintanaboina, J. Turmeric-Induced Hepatotoxicity: Report of 2 Cases. Int. Med. Case Rep. J. 2021, 14, 849–852. [Google Scholar] [CrossRef] [PubMed]
- Luber, R.P.; Rentsch, C.; Lontos, S.; Pope, J.D.; Aung, A.K.; Schneider, H.G.; Kemp, W.; Roberts, S.K.; Majeed, A. Turmeric Induced Liver Injury: A Report of Two Cases. Case Rep. Hepatol. 2019, 2019, 6741213. [Google Scholar] [CrossRef] [PubMed]
- Pitaro, M.; Croce, N.; Gallo, V.; Arienzo, A.; Salvatore, G.; Antonini, G. Coumarin-Induced Hepatotoxicity: A Narrative Review. Molecules 2022, 27, 9063. [Google Scholar] [CrossRef] [PubMed]
- Crook, A.; De Lima Leite, A.; Payne, T.; Bhinderwala, F.; Woods, J.; Singh, V.K.; Powers, R. Radiation Exposure Induces Cross-Species Temporal Metabolic Changes That Are Mitigated in Mice by Amifostine. Sci. Rep. 2021, 11, 14004. [Google Scholar] [CrossRef] [PubMed]
- Amifostine—NCI. Available online: https://www.cancer.gov/about-cancer/treatment/drugs/amifostine (accessed on 15 June 2024).
- Wang, L.; Cao, Y.; Zhang, X.; Liu, C.; Yin, J.; Kuang, L.; He, W.; Hua, D. Reactive Oxygen Species-Responsive Nanodrug of Natural Crocin-i with Prolonged Circulation for Effective Radioprotection. Colloids Surf. B Biointerfaces 2022, 213, 112441. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, H.; Karakoc, Y.; Tumkaya, L.; Mercantepe, T.; Sevinc, H.; Yilmaz, A.; Yılmaz Rakıcı, S. The Protective Effects of Red Ginseng and Amifostine against Renal Damage Caused by Ionizing Radiation. Hum. Exp. Toxicol. 2022, 41, 9603271221143029. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.G.; Freeman, A.R.; Roos, D.E.; Milner, A.D.; Borg, M.F. Randomized Double-Blind Trial of Amifostine versus Placebo for Radiation-Induced Xerostomia in Patients with Head and Neck Cancer. J. Med. Imaging Radiat. Oncol. 2019, 63, 142–150. [Google Scholar] [CrossRef]
- Ameri, A.; Heydarirad, G.; Rezaeizadeh, H.; Choopani, R.; Ghobadi, A.; Gachkar, L. Evaluation of Efficacy of an Herbal Compound on Dry Mouth in Patients With Head and Neck Cancers: A Randomized Clinical Trial. J. Evid. Based Complement. Altern. Med. 2016, 21, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Motahari, P.; Pakdel, F.; Hashemzadeh, N.; Heydari, F.; Eghdam Zamiri, R.; Katebi, K. The Effect of 1% Pilocarpine Mouthwash on Salivary Flow Rate in Patients with Radiation-Induced Xerostomia: A Double-Blind Randomized Clinical Trial. Middle East. J. Cancer 2024, 15, 108–116. [Google Scholar] [CrossRef]
- Tourabi, M.; Metouekel, A.; Ghouizi, A.E.; Jeddi, M.; Nouioura, G.; Laaroussi, H.; Hosen, M.E.; Benbrahim, K.F.; Bourhia, M.; Salamatullah, A.M.; et al. Efficacy of Various Extracting Solvents on Phytochemical Composition, and Biological Properties of Mentha longifolia L. Leaf Extracts. Sci. Rep. 2023, 13, 18028. [Google Scholar] [CrossRef]
- Vanhaelen, M.; Lejoly, J.; Hanocq, M.; Molle, L. Climatic and Geographical Aspects of Medicinal Plant Constituents. In The Medicinal Plant Industry; Routledge: New York, NY, USA, 2017; pp. 59–76. ISBN 978-0-203-73639-5. [Google Scholar]
- Heinrich, M.; Jalil, B.; Abdel-Tawab, M.; Echeverria, J.; Kulić, Ž.; McGaw, L.J.; Pezzuto, J.M.; Potterat, O.; Wang, J.-B. Best Practice in the Chemical Characterisation of Extracts Used in Pharmacological and Toxicological Research—The ConPhyMP—Guidelines 1 2. Front. Pharmacol. 2022, 13, 953205. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.A.L.S.; Ferreira, M.R.A. Standardization and quality control of herbal medicines. In Recent Developments in Phytomedicine Technology; New Developments in Medical Research; de Freitas, L.A.P., Teixeira, C.C.C., Zamarioli, C.M., Eds.; Nova Science Publisher: Hauppauge, NY, USA, 2017. [Google Scholar]
- Wang, H.; Chen, Y.; Wang, L.; Liu, Q.; Yang, S.; Wang, C. Advancing Herbal Medicine: Enhancing Product Quality and Safety through Robust Quality Control Practices. Front. Pharmacol. 2023, 14, 1265178. [Google Scholar] [CrossRef] [PubMed]
- Garg, V.; Dhar, V.; Sharma, A.; Dutt, R. Facts about Standardization of Herbal Medicine: A Review. Zhong Xi Yi Jie He Xue Bao = J. Chin. Integr. Med. 2012, 10, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Touchette, D.R.; Stevenson, J.G.; Jensen, G. Cost-Effectiveness Analysis of Amifostine (Ethyol©) in Patients with Non-Small Cell Lung Cancer. J. Aging Pharmacother. 2006, 13, 109–126. [Google Scholar] [CrossRef]
- Amifostine Prices, Coupons, Copay & Patient Assistance. Available online: https://www.drugs.com/price-guide/amifostine (accessed on 15 June 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).