C-Phycocyanin Prevents Oxidative Stress, Inflammation, and Lung Remodeling in an Ovalbumin-Induced Rat Asthma Model
Abstract
:1. Introduction
2. Results
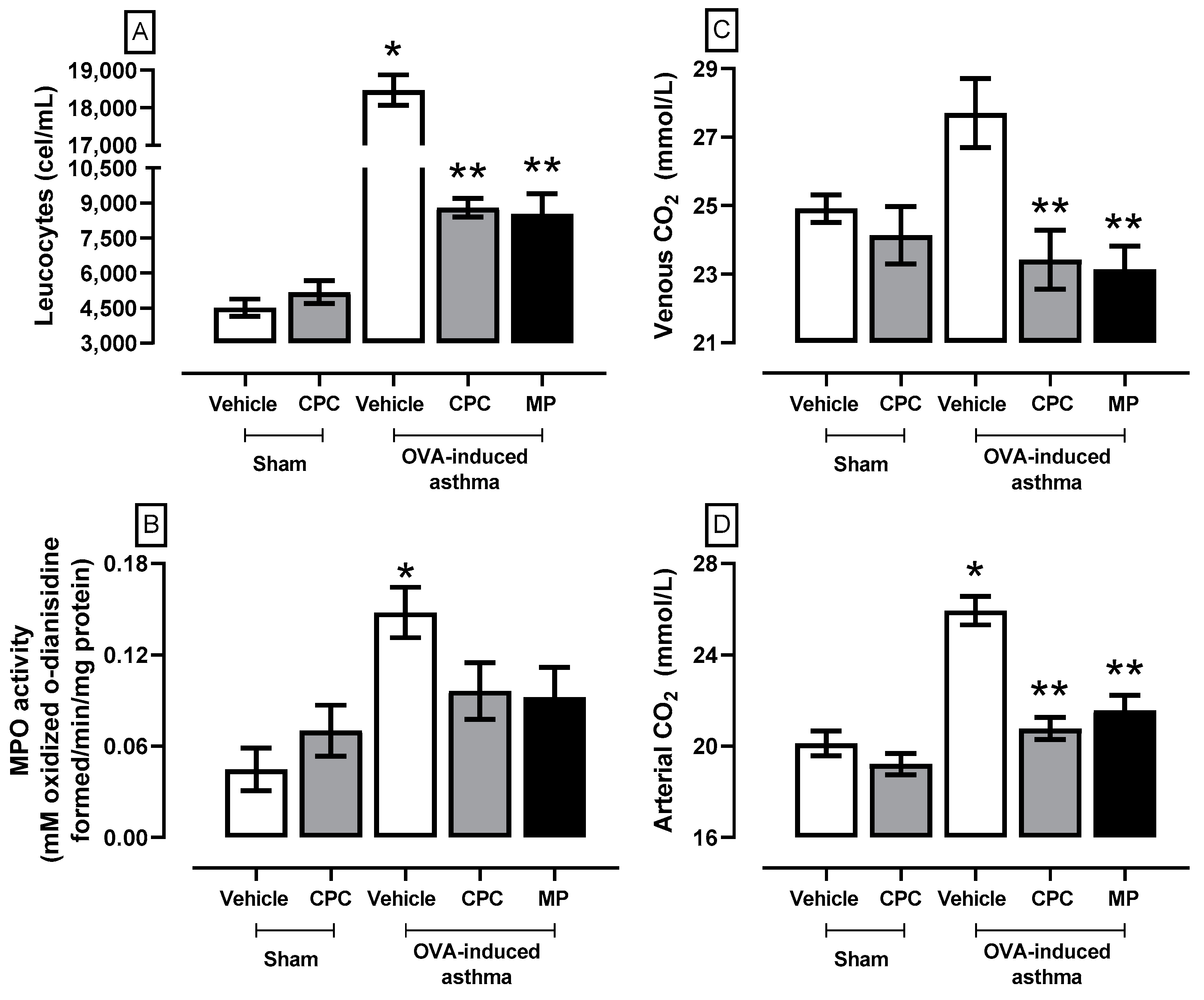
2.1. Effect of CPC on Clinical Pathology Markers Related to Asthma
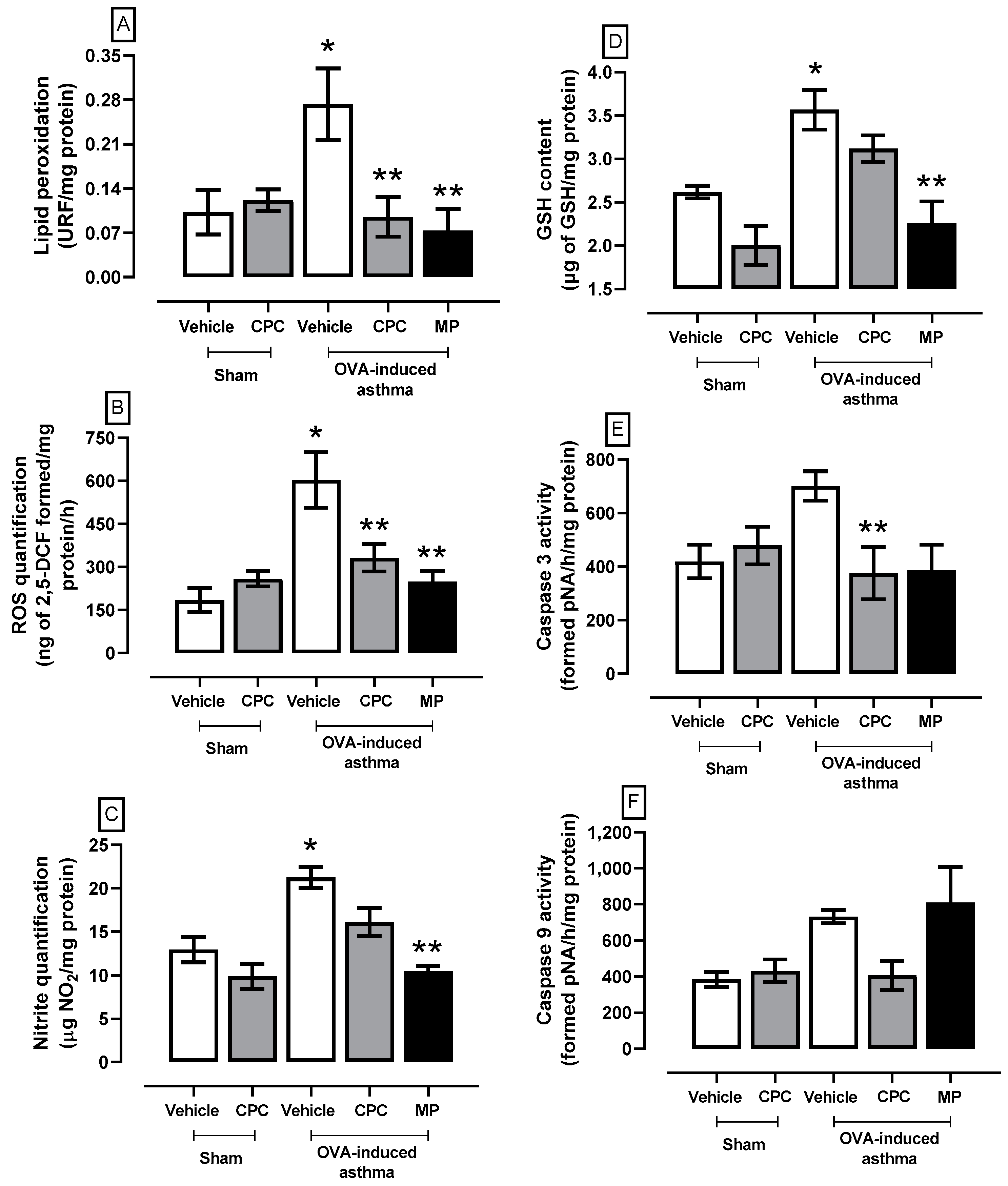
2.2. Effect of CPC on Asthma-Induced Oxidative Stress and Cellular Damage
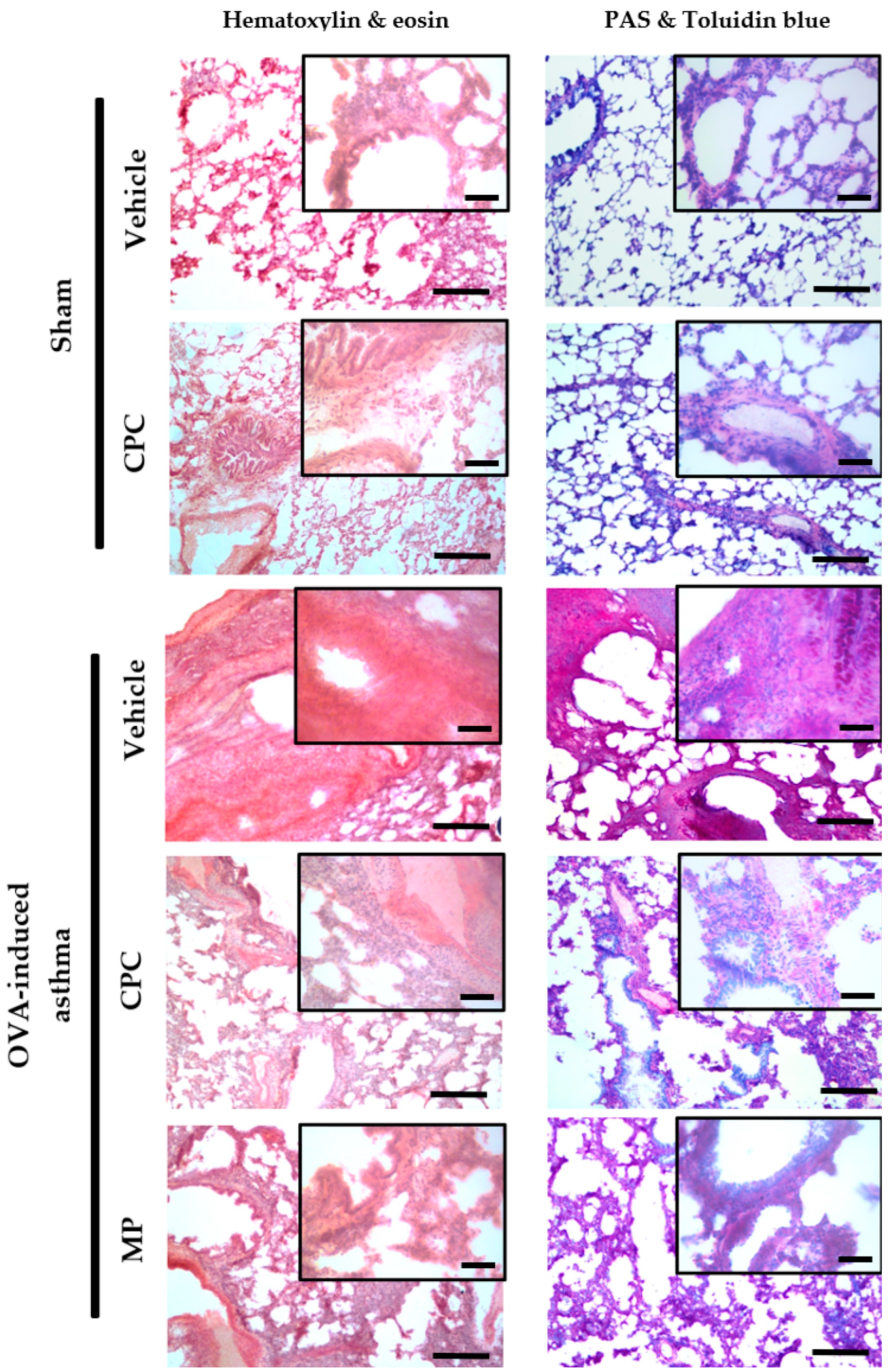
2.3. Histopathological Study of the Lung of Ovalbumin-Challenged Asthmatic Rats
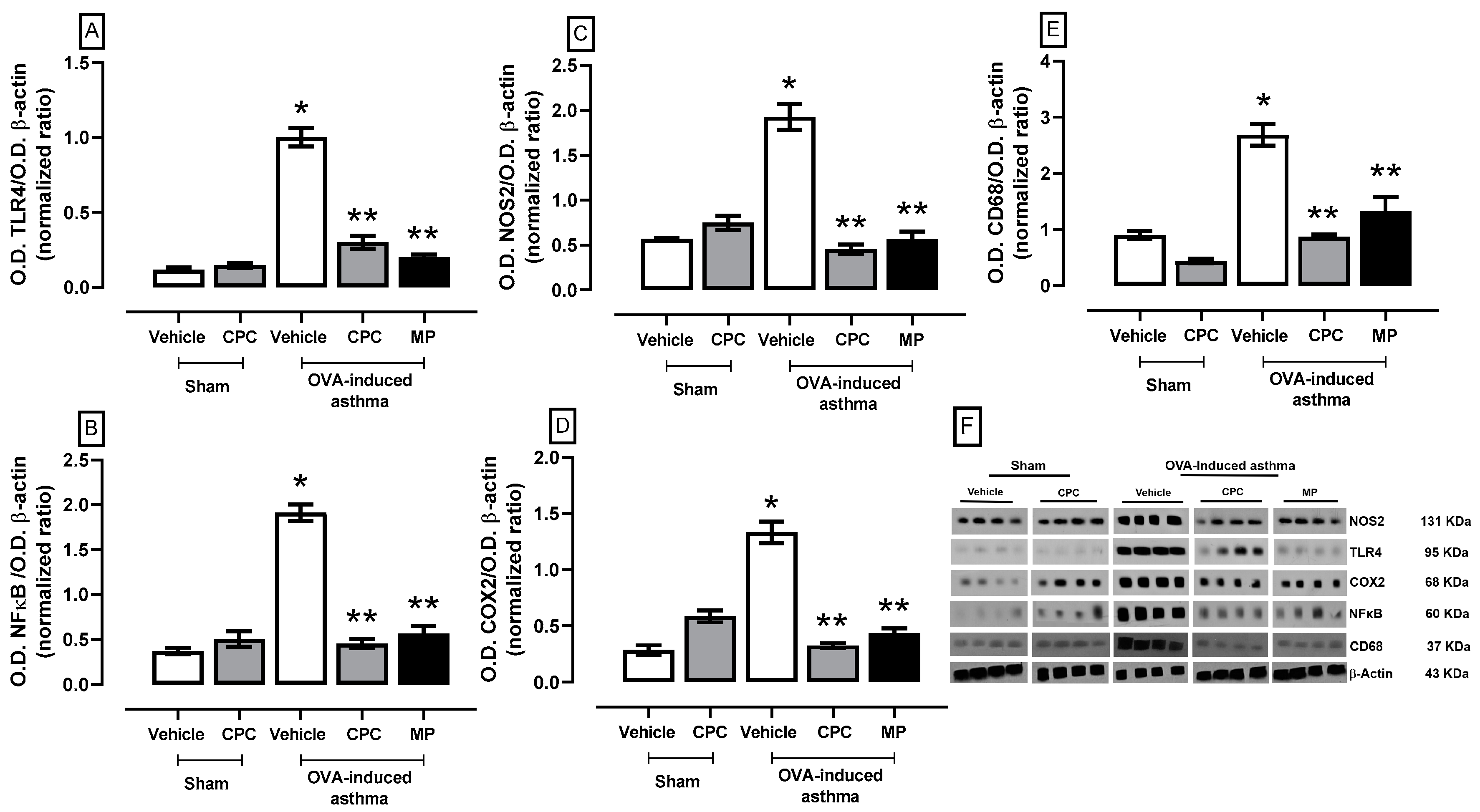
2.4. Participation of the TLR4/NFκB/COX2/NOS2 Pathway and Macrophages on OVA-Induced Asthma
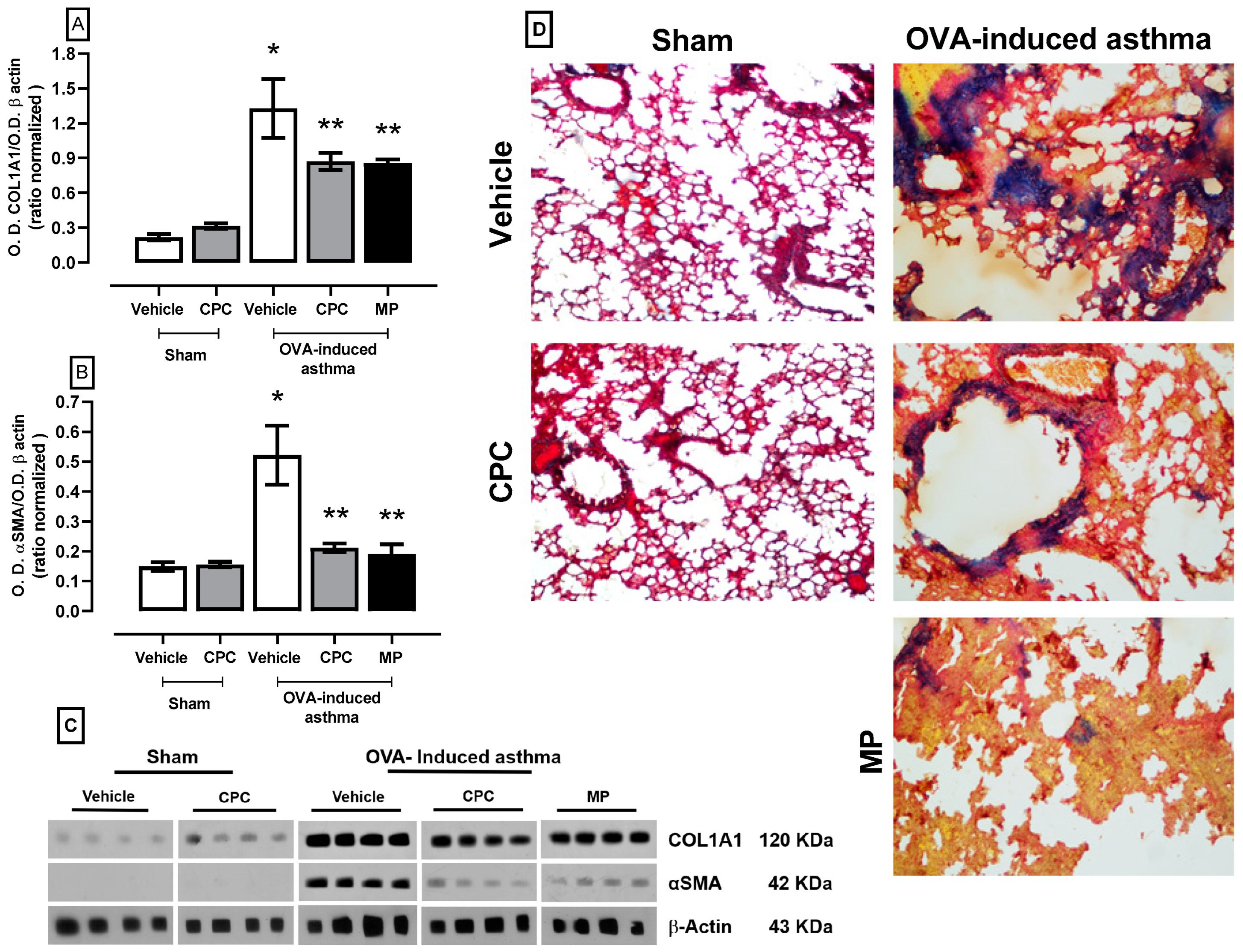
2.5. Effect of CPC on the Expression of Collagen1a1 and αSMA as Lung Remodeling Markers
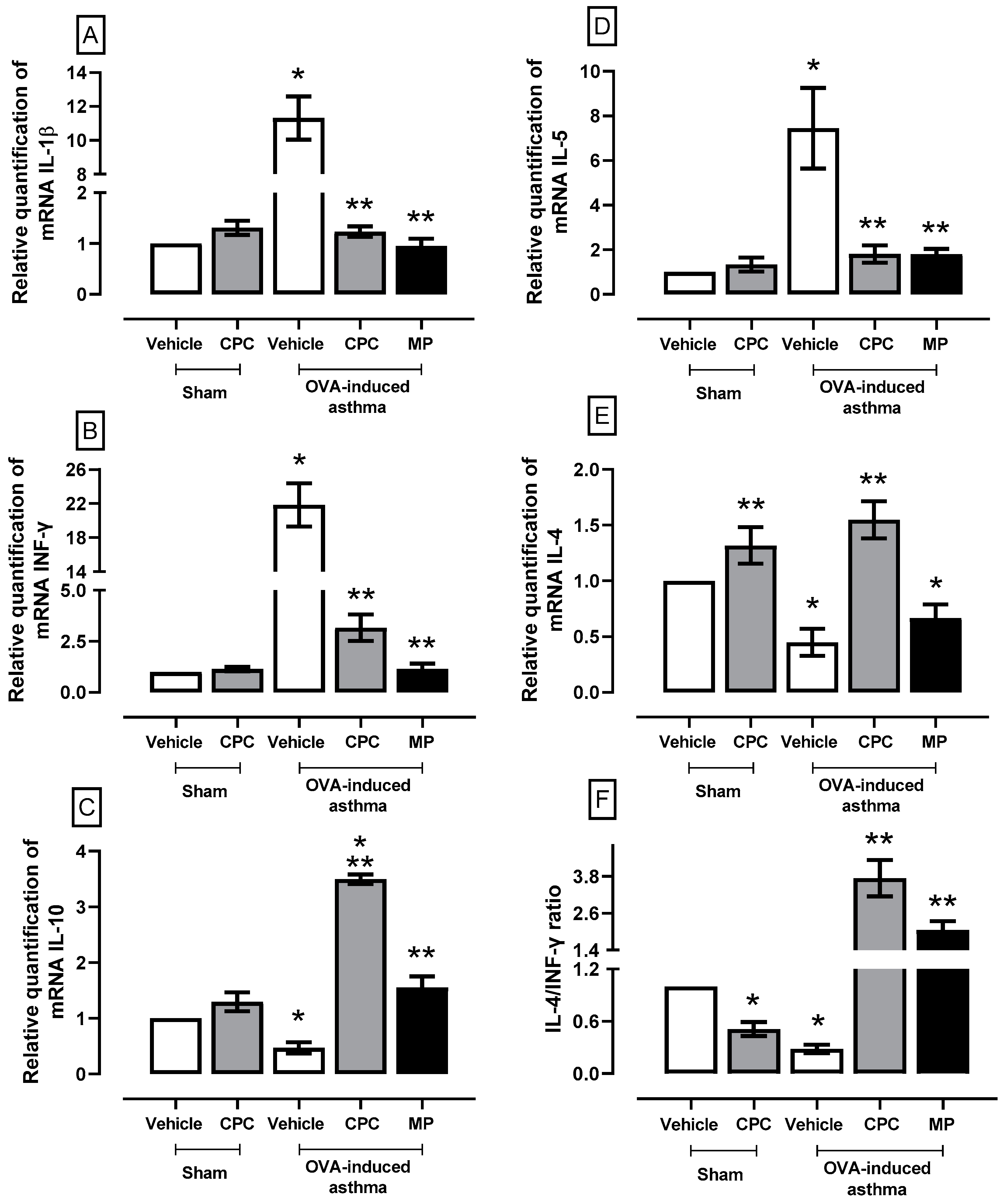
2.6. Effect of CPC on a Cytokine Expression Related to the Inflammatory Process in Asthma
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Oxidative Stress and REDOX Environment Markers
4.3. Biochemical, Histological, and Molecular Assays
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mims, J.W. Asthma: Definitions and pathophysiology. Int. Forum. Allergy Rhinol. 2015, 5 (Suppl. S1), S2–S6. [Google Scholar] [CrossRef] [PubMed]
- Sze, E.; Bhalla, A.; Nair, P. Mechanisms and therapeutic strategies for non-t2 asthma. Allergy 2020, 75, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.; Yang, F.; Bai, M.; Zong, Y.; Li, Z.; Meng, X.; Zhao, X.; Wang, J. Airway immune response in the mouse models of obesity-related asthma. Front. Physiol. 2022, 13, 909209. [Google Scholar] [CrossRef] [PubMed]
- Shangyao, M.; Hao, D.; Yong, X.; Lixia, Y.; Lili, W. Chryseriol attenuates the progression of ova-induced asthma in mice through NF-ΚκB/HIF-1αα and MAPK/STAT1 pathways. Allergol. Immunopathol. 2023, 51, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Roshan, M.H.K.; Tambo, A.; Pace, N.P. The role of TLR2, TLR4, and TLR9 in the pathogenesis of atheroscle-rosis. Int. J. Inflamm. 2016, 2016, 1532832. [Google Scholar] [CrossRef] [PubMed]
- Pascual, R.M.; Peters, S.P. Airway remodeling contributes to the progressive loss of lung function in asthma: An overview. J. Allergy Clin. Immunol. 2005, 116, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.L.; Grayson, M.H.; Strothman, K. Advances in asthma: New understandings of asthma’s natural history, risk factors, underlying mechanisms, and clinical management. J. Allergy Clin. Immunol. 2021, 148, 1430–1441. [Google Scholar] [CrossRef]
- Barnig, C.; Frossard, N.; Levy, B.D. Towards targeting resolution pathways of airway inflammation in asthma. Pharmacol. Ther. 2018, 186, 98–113. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Qiu, C. Research advances in airway remodeling in asthma: A narrative review. Ann. Transl. Med. 2022, 10, 1023. [Google Scholar] [CrossRef]
- Rowe, B.; Spooner, C.; Ducharme, F.; Bretzlaff, J.; Bota, G. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst. Rev. 2001, CD000195. [Google Scholar] [CrossRef]
- Alangari, A.A. Corticosteroids in the treatment of acute asthma. Ann. Thorac. Med. 2014, 9, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.B.; Mims, J.W.; Clinger, J.D. The burden of asthma and allergic rhinitis. Otolaryngol. Clin. N. Am. 2024, 57, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, B.; Jones, P.W.; Yunus, F.; Lan, L.T.T.; Boonsawat, W.; Ismaila, A.; Ascioglu, S. Direct healthcare costs associated with management of asthma: Comparison of two treatment regimens in Indonesia, Thailand and Vietnam. J. Asthma 2022, 59, 1213–1220. [Google Scholar] [CrossRef] [PubMed]
- Hardtstock, F.; Krieger, J.; Wilke, T.; Lukas, M.; Ultsch, B.; Welte, R.; Quinzler, R.; Maywald, U.; Timmermann, H. Use of biologic therapies in the treatment of asthma—A comparative real world data analysis on healthcare resource utilization and costs before and after therapy initiation. J. Asthma. Allergy 2022, 15, 407–418. [Google Scholar] [CrossRef]
- Stolbrink, M.; Thomson, H.; Hadfield, R.M.; Ozoh, O.B.; Nantanda, R.; Jayasooriya, S.; Allwood, B.; Halpin, D.M.G.; Salvi, S.; de Oca, M.M.; et al. The availability, cost, and affordability of essential medicines for asthma and COPD in low-income and middle-income countries: A systematic review. Lancet Glob. Health 2022, 10, e1423–e1442. [Google Scholar] [CrossRef]
- Maurya, A.P.; Chauhan, J.; Yadav, D.K.; Gangwar, R.; Maurya, V.K. Nutraceuticals and their impact on human health. In Preparation of Phytopharmaceuticals for the Management of Disorders; Elsevier: Amsterdam, The Netherlands, 2021; pp. 229–254. [Google Scholar]
- Riaz, K.; Butt, M.S.; Sharif, M.K.; Faisal, M.N. Therapeutic efficacy of spirulina against ovalbumin and ciga-rette smoke-induced asthma-specific stress biomarkers in Sprague-Dawley rats. Food Sci. Nutr. 2023, 11, 972–982. [Google Scholar] [CrossRef] [PubMed]
- Bannu, S.M.; Lomada, D.; Gulla, S.; Chandrasekhar, T.; Reddanna, P.; Reddy, M.C. Potential therapeutic ap-plications of C-phycocyanin. Curr. Drug Metab. 2020, 20, 967–976. [Google Scholar] [CrossRef] [PubMed]
- Grover, P.; Bhatnagar, A.; Kumari, N.; Narayan Bhatt, A.; Kumar Nishad, D.; Purkayastha, J. C-phycocyanin-a novel protein from Spirulina platensis in vivo toxicity, antioxidant and immunomodulatory studies. Saudi J. Biol. Sci. 2021, 28, 1853–1859. [Google Scholar] [CrossRef] [PubMed]
- Duman, Y.; Tufan, G. Chromatographic purification of C-phycocyanin from Spirulina platensis: Assessing antioxidant activity and stability. J. Sci. Food Agric. 2024; online ahead of print. [Google Scholar] [CrossRef]
- Liu, R.; Qin, S.; Li, W. Phycocyanin: Anti-inflammatory effect and mechanism. Biomed. Pharmacother. 2022, 153, 113362. [Google Scholar] [CrossRef]
- Romay, C.; Gonzalez, R.; Ledon, N.; Remirez, D.; Rimbau, V. C-phycocyanin: A biliprotein with antioxidant, anti-inflammatory and neuroprotective effects. Curr. Protein Pept. Sci. 2003, 4, 207–216. [Google Scholar] [CrossRef]
- Blas-Valdivia, V.; Moran-Dorantes, D.N.; Rojas-Franco, P.; Franco-Colin, M.; Mirhosseini, N.; Davarnejad, R.; Halajisani, A.; Tavakoli, O.; Cano-Europa, E. C-phycocyanin prevents acute myocardial infarction-induced oxidative stress, inflammation and cardiac damage. Pharm. Biol. 2022, 60, 755–763. [Google Scholar] [CrossRef]
- Fernandes e Silva, E.; Figueira, F.D.S.; Lettnin, A.P.; Carrett-Dias, M.; Filgueira, D.D.M.V.B.; Kalil, S.; Trin-dade, G.S.; Votto, A.P.D.S. C-phycocyanin: Cellular targets, mechanisms of action and multi drug resistance in cancer. Pharmacol. Rep. 2018, 70, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Franco, P.; Garcia-Pliego, E.; Vite-Aquino, A.G.; Franco-Colin, M.; Serrano-Contreras, J.I.; Paniagua-Castro, N.; Gallardo-Casas, C.A.; Blas-Valdivia, V.; Cano-Europa, E. The nutraceutical antihyper-tensive action of c-phycocyanin in chronic kidney disease is related to the prevention of endothelial dysfunction. Nutrients 2022, 14, 1464. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Bago, A.; Lascurain, R.; Hernandez-Carreño, P.E.; Gallardo-Vera, F.; Argueta-Donohue, J.; Jime-nez-Trejo, F.; Fuentes-Zavaleta, D.A.; Beltran-Ontiveros, S.A.; Becerril-Camacho, D.M.; Contreras-Rodriguez, V.A.; et al. Sex, age, and regional disparities in the burden of asthma in Mexico from 1990 to 2019: A Secondary Analysis of the Global Burden of Disease Study. Sustainability 2023, 15, 12599. [Google Scholar] [CrossRef]
- Cano Salas, M.D.C.; Miguel Reyes, J.L.; Sánchez Trejo, K.; López Estrada, E.D.C.; Salas Hernández, J.; Arroyo Rojas, M.E.; Castañeda Valdivia, M.; Escobar Preciado, M.; Guzmán Vázquez, S.; García-García, S.R.; et al. Economic burden assessment for the management of asthma patients at Mexico’s National Institute for Respiratory Diseases. Rev. Alerg. Mex. 2024, 71, 12–22. [Google Scholar] [CrossRef]
- Cellat, M.; Kuzu, M.; İşler, C.T.; Etyemez, M.; Dikmen, N.; Uyar, A.; Gökçek, İ.; Türk, E.; Güvenç, M. Tyrosol Improves Ovalbumin (OVA)-induced asthma in rat model through prevention of airway inflammation. Naunyn. Schmiedebergs Arch. Pharmacol. 2021, 394, 2061–2075. [Google Scholar] [CrossRef]
- Ogawa, Y.; Duru, E.A.; Ameredes, B.T. Role of IL-10 in the resolution of airway inflammation. Curr. Mol. Med. 2008, 8, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Castro-Gerónimo, V.D.; García-Rodríguez, R.V.; Sánchez-Medina, A.; Chamorro-Cevallos, G.A.; Sánchez-González, D.J.; Méndez-Bolaina, E. C-Phycocyanin: A phycobiliprotein from spirulina with metabolic syndrome and oxidative stress effects. J. Med. Food, 2023; online ahead of print. [Google Scholar] [CrossRef]
- Garcia-Pliego, E.; Franco-Colin, M.; Rojas-Franco, P.; Blas-Valdivia, V.; Serrano-Contreras, J.I.; Pentón-Rol, G.; Cano-Europa, E. Phycocyanobilin is the molecule responsible for the nephroprotective action of phycocya-nin in acute kidney injury caused by mercury. Food Funct. 2021, 12, 2985–2994. [Google Scholar] [CrossRef]
- Alzokaky, A.A.; Abdelkader, E.M.; El-Dessouki, A.M.; Khaleel, S.A.; Raslan, N.A. C-phycocyanin protects against ethanol-induced gastric ulcers in rats: Role of HMGB1/NLRP3/NF-κB pathway. Basic Clin. Pharmacol. Toxicol. 2020, 127, 265–277. [Google Scholar] [CrossRef]
- Shih, C.-M.; Cheng, S.-N.; Wong, C.-S.; Kuo, Y.-L.; Chou, T.-C. Antiinflammatory and antihyperalgesic ac-tivity of C-phycocyanin. Anesth. Analg. 2009, 108, 1303–1310. [Google Scholar] [CrossRef]
- Jiang, L.; Wang, Y.; Liu, G.; Liu, H.; Zhu, F.; Ji, H.; Li, B. C-phycocyanin exerts anti-cancer effects via the MAPK signaling pathway in MDA-MB-231 cells. Cancer Cell Int. 2018, 18, 12. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Mehrabi Nasab, E.; Arora, P.; Athari, S.S. Study effect of probiotics and prebiotics on treatment of OVA-LPS-induced of allergic asthma inflammation and pneumonia by regulating the TLR4/NF-KB signaling pathway. J. Transl. Med. 2022, 20, 130. [Google Scholar] [CrossRef]
- Choi, Y.; Sim, S.; Park, H.-S. Is TLR4 critical for neutrophil apoptosis in occupational asthma? Allergy Asthma. Immunol. Res. 2020, 12, 560. [Google Scholar] [CrossRef]
- Yarmohammadi, F.; Hayes, A.W.; Karimi, G. Possible protective effect of resolvin D1 on inflammation in atrial fibrillation: Involvement of ER stress mediated the NLRP3 inflammasome pathway. Naunyn. Schmiedebergs Arch. Pharmacol. 2021, 394, 1613–1619. [Google Scholar] [CrossRef]
- Rojas-Franco, P.; Franco-Colín, M.; Blas-Valdivia, V.; Melendez-Camargo, M.E.; Cano-Europa, E. Arthrospira maxima (Spirulina) prevents endoplasmic reticulum stress in the kidney through its C-phycocyanin. J. Zhejiang Univ.-Sci. B 2021, 22, 603–608. [Google Scholar] [CrossRef]
- Pentón-Rol, G.; Marín-Prida, J.; McCarty, M.F. C-phycocyanin-derived phycocyanobilin as a potential nutraceutical approach for major neurodegenerative disorders and COVID-19- induced damage to the nervous system. Curr. Neuropharmacol. 2021, 19, 2250–2275. [Google Scholar] [CrossRef] [PubMed]
- Naito, Y.; Takagi, T.; Higashimura, Y. Heme oxygenase-1 and anti-inflammatory M2 macrophages. Arch. Biochem. Biophys. 2014, 564, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Prasanth, S.; Kumar Arun, G.; Haridas, M.; Sabu, A. Phycocyanin of arimne Oscillatoria sp. inhibits lipoxy-genase by protein-protein interaction-induced change of active site entry apace: A model for non-specific biofunctions of phycocyanins. Int. J. Biol. Macromol. 2020, 165, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Pyung, Y.J.; Park, D.-J.; Kim, C.G.; Yun, C.-H. Remodeling and restraining lung tissue damage through the regulation of respiratory immune responses. Tissue Eng. Regen. Med. 2023, 20, 329–339. [Google Scholar] [CrossRef]
- Gong, Z.; Li, Q.; Shi, J.; Wei, J.; Li, P.; Chang, C.-H.; Shultz, L.D.; Ren, G. Lung fibroblasts facilitate pre-metastatic niche formation by remodeling the local immune microenvironment. Immunity 2022, 55, 1483–1500.e9. [Google Scholar] [CrossRef]
- Bartis, D.; Mise, N.; Mahida, R.Y.; Eickelberg, O.; Thickett, D.R. Epithelial–mesenchymal transition in lung development and disease: Does it exist and is it important? Thorax 2014, 69, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Shinde, A.V.; Humeres, C.; Frangogiannis, N.G. The role of α-smooth muscle actin in fibroblast-mediated matrix contraction and remodeling. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2017, 1863, 298–309. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Liu, G.; Han, J.; Zhu, F.; Dong, X.; Li, B. C-phycocyanin inhibits epithelial-to-mesenchymal transition in Caski cells. Cancer Cell Int. 2020, 20, 292. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Chiang, Y.F.; Huang, C.Y.; Shieh, T.M.; Kao, C.; Chang, F.K.; Huang, T.C.; Ali, M.; Chang, H.Y.; Hong, Y.H.; et al. Spirulina phycocyanin extract and its active components suppress epitheli-al-mesenchymal transition process in endometrial cancer via targeting TGF-Beta1/SMAD4 signaling pathway. Biomed. Pharmacother. 2022, 152, 113219. [Google Scholar] [CrossRef] [PubMed]
- Lewis, B.W.; Ford, M.L.; Khan, A.Q.; Walum, J.; Britt, R.D. Chronic allergen challenge induces corticosteroid insensitivity with persistent airway remodeling and type 2 inflammation. Front. Pharmacol. 2022, 13, 855247. [Google Scholar] [CrossRef] [PubMed]
- Akkuş, Y.; Baş, V.N.; Yılmaz, Z. Cushing syndrome induced by long term use of corticosteroids in the management of atopic dermatitis. Pediatr. Endocrinol. Diabetes Metab. 2020, 26, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Milara, J.; Morell, A.; Roger, I.; Montero, P.; Cortijo, J. Mechanisms underlying corticosteroid resistance in patients with asthma: A review of current knowledge. Expert. Rev. Respir. Med. 2023, 17, 701–715. [Google Scholar] [CrossRef]
- GOB NOM-062-ZOO-1999; Especificaciones Técnicas para la Producción, Cuidado y uso de los Animales de Laboratorio. CDMX: Mexico City, Mexico, 2001.
- Mukherjee, A.A.; Kandhare, A.D.; Rojatkar, S.R.; Bodhankar, S.L. Ameliorative effects of Artemisia pallens in a murine model of ovalbumin-induced allergic asthma via modulation of biochemical perturbations. Biomed. Pharmacother. 2017, 94, 880–889. [Google Scholar] [CrossRef]

| Gene | Primers | Product Length (BP) | Annealing Temperature |
|---|---|---|---|
| IL-1β | 5′-agcccatcctctgtgactcatg-3′ 5′-gctgatgtaccagttggggaac-3′ | 104 | 60.5 °C |
| INF-γ | 5′-ttttgcagctctgcctcat-3′ 5′-agcatccatgctacttgagttaaa-3′ | 106 | 63 °C |
| IL-10 | 5′-tgccaagccttgtcagaaathg3′ 5′-tgagtgtcacgtaggcttcta-3′ | 386 | 58 °C |
| IL-5 | 5′-aactctcagctgtgtctgggc-3′ 5′-gacttccattgcccactctgta-3′ | 367 | 59 °C |
| IL-4 | 5′-accttgctgtcaccctgttc-3′ 5′-gttgtgagcgtggactcattc-3′ | 352 | 60.5 °C |
| β-Actin | 5′-agcccatcctctgtgactcatg-3′ 5′-gctgatgtaccagttggggaac-3′ | 422 | 63 °C |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mundo-Franco, Z.; Luna-Herrera, J.; Castañeda-Sánchez, J.I.; Serrano-Contreras, J.I.; Rojas-Franco, P.; Blas-Valdivia, V.; Franco-Colín, M.; Cano-Europa, E. C-Phycocyanin Prevents Oxidative Stress, Inflammation, and Lung Remodeling in an Ovalbumin-Induced Rat Asthma Model. Int. J. Mol. Sci. 2024, 25, 7031. https://doi.org/10.3390/ijms25137031
Mundo-Franco Z, Luna-Herrera J, Castañeda-Sánchez JI, Serrano-Contreras JI, Rojas-Franco P, Blas-Valdivia V, Franco-Colín M, Cano-Europa E. C-Phycocyanin Prevents Oxidative Stress, Inflammation, and Lung Remodeling in an Ovalbumin-Induced Rat Asthma Model. International Journal of Molecular Sciences. 2024; 25(13):7031. https://doi.org/10.3390/ijms25137031
Chicago/Turabian StyleMundo-Franco, Zayra, Julieta Luna-Herrera, Jorge Ismael Castañeda-Sánchez, José Iván Serrano-Contreras, Plácido Rojas-Franco, Vanessa Blas-Valdivia, Margarita Franco-Colín, and Edgar Cano-Europa. 2024. "C-Phycocyanin Prevents Oxidative Stress, Inflammation, and Lung Remodeling in an Ovalbumin-Induced Rat Asthma Model" International Journal of Molecular Sciences 25, no. 13: 7031. https://doi.org/10.3390/ijms25137031





