Alternatives to Conventional Topical Dosage Forms for Targeted Skin Penetration of Diclofenac Sodium
Abstract
1. Introduction
2. Results
2.1. Influence of Formulation Changes on Physical Stability
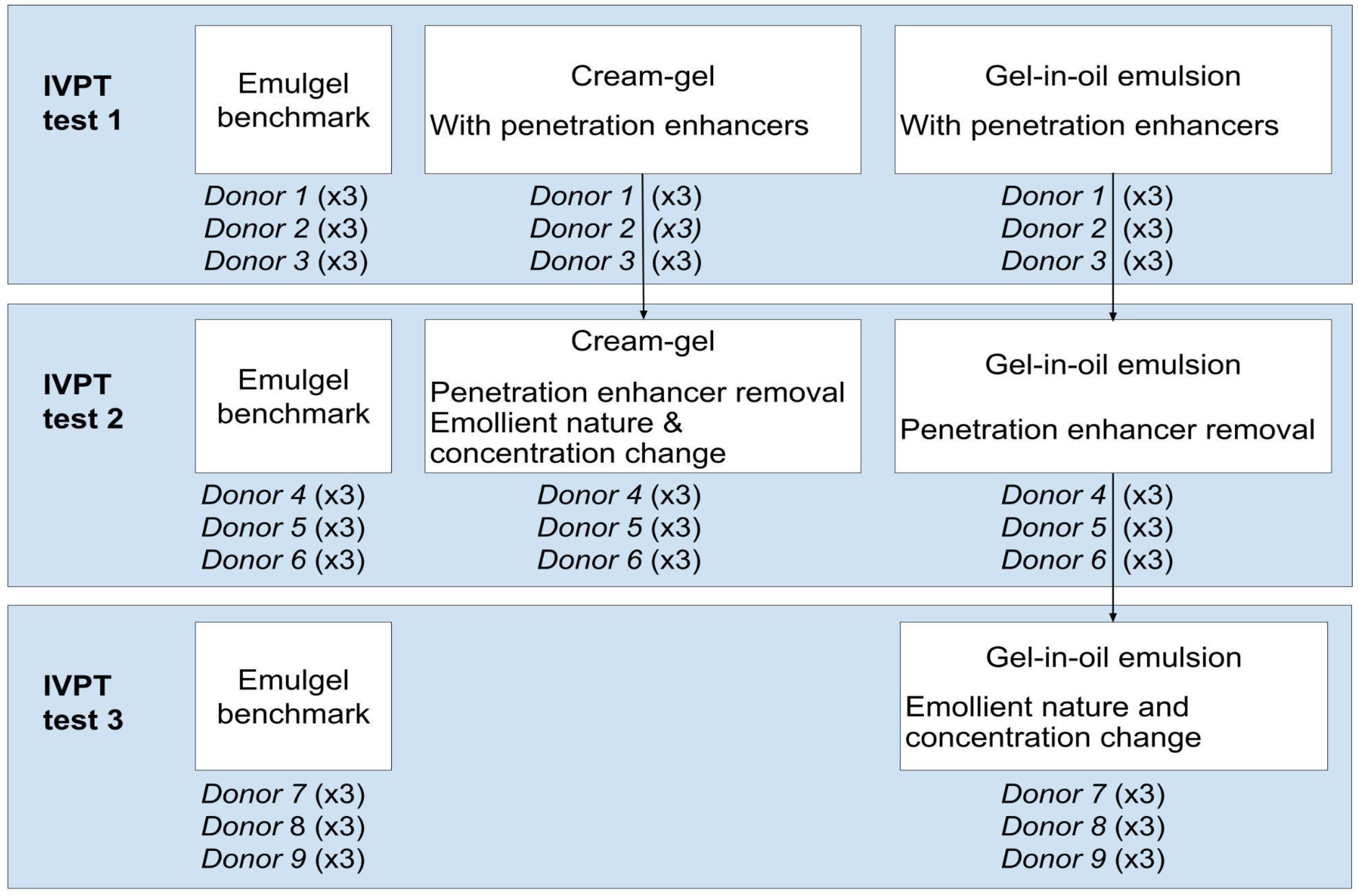
2.2. Experimental Results of IVPT
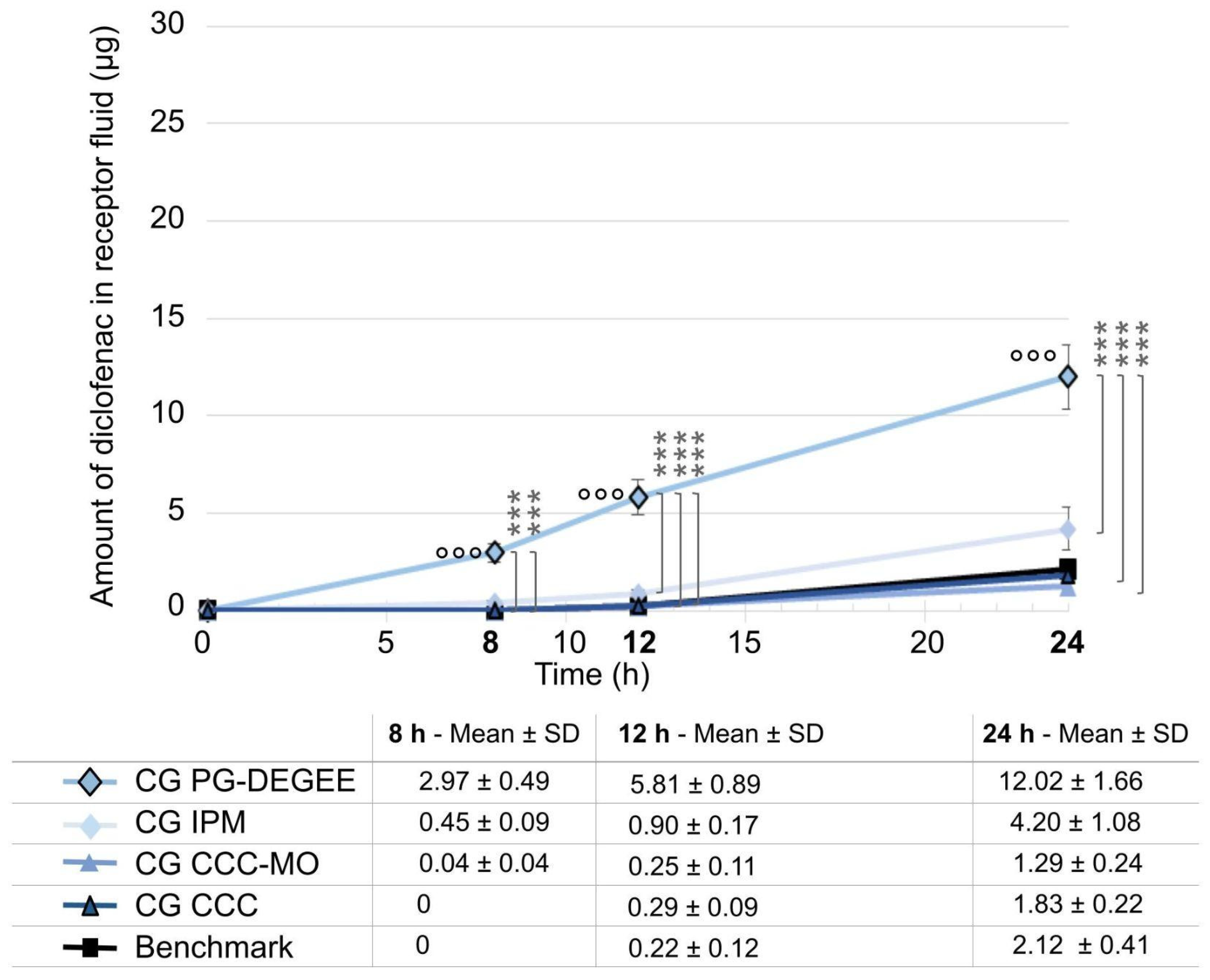
2.2.1. Test 1: Starting Compositions with Glycols as Penetration Enhancer
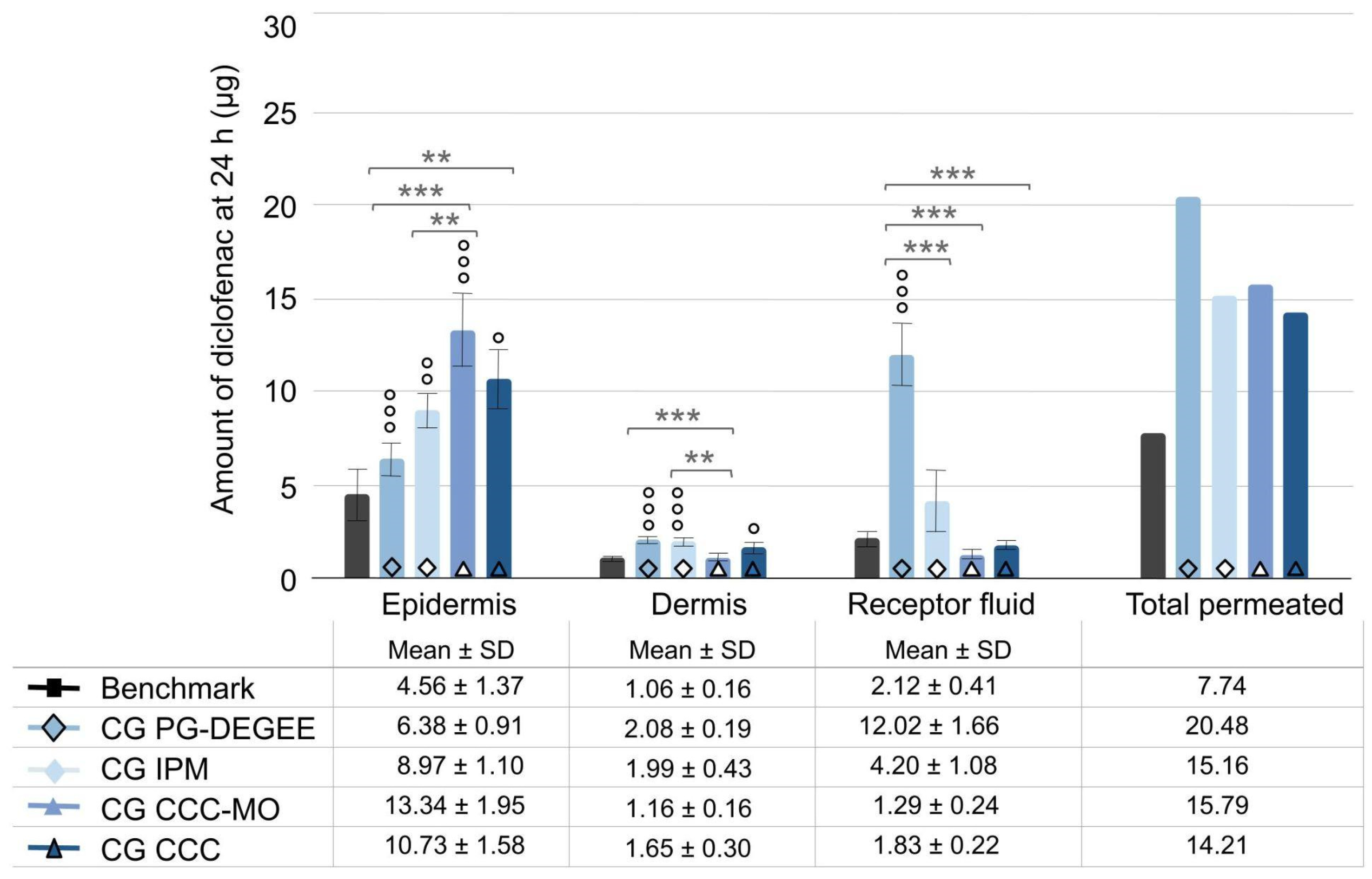
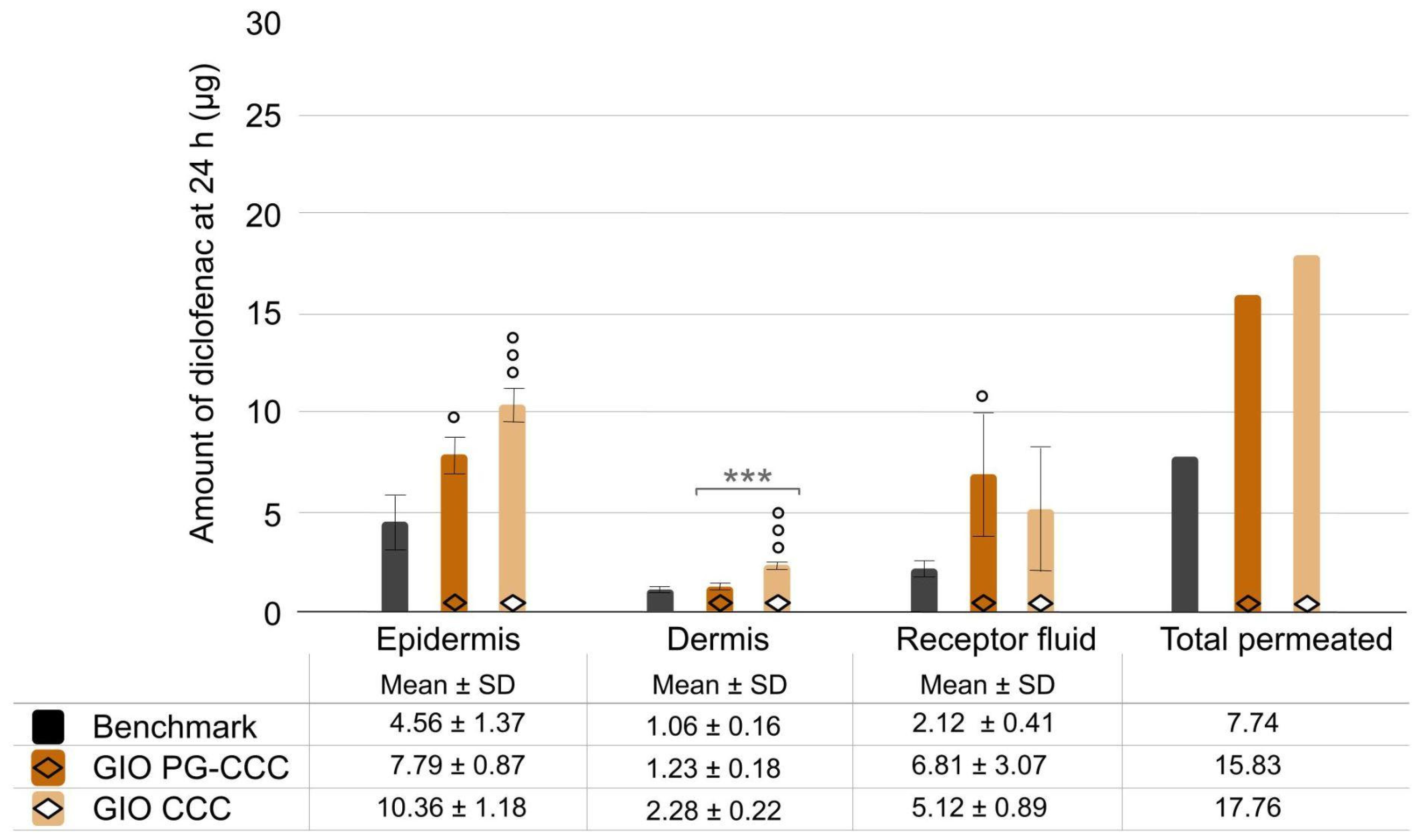
2.2.2. Test 2: Impact of Solvent Removal and Emollient Changes in Cream–Gel
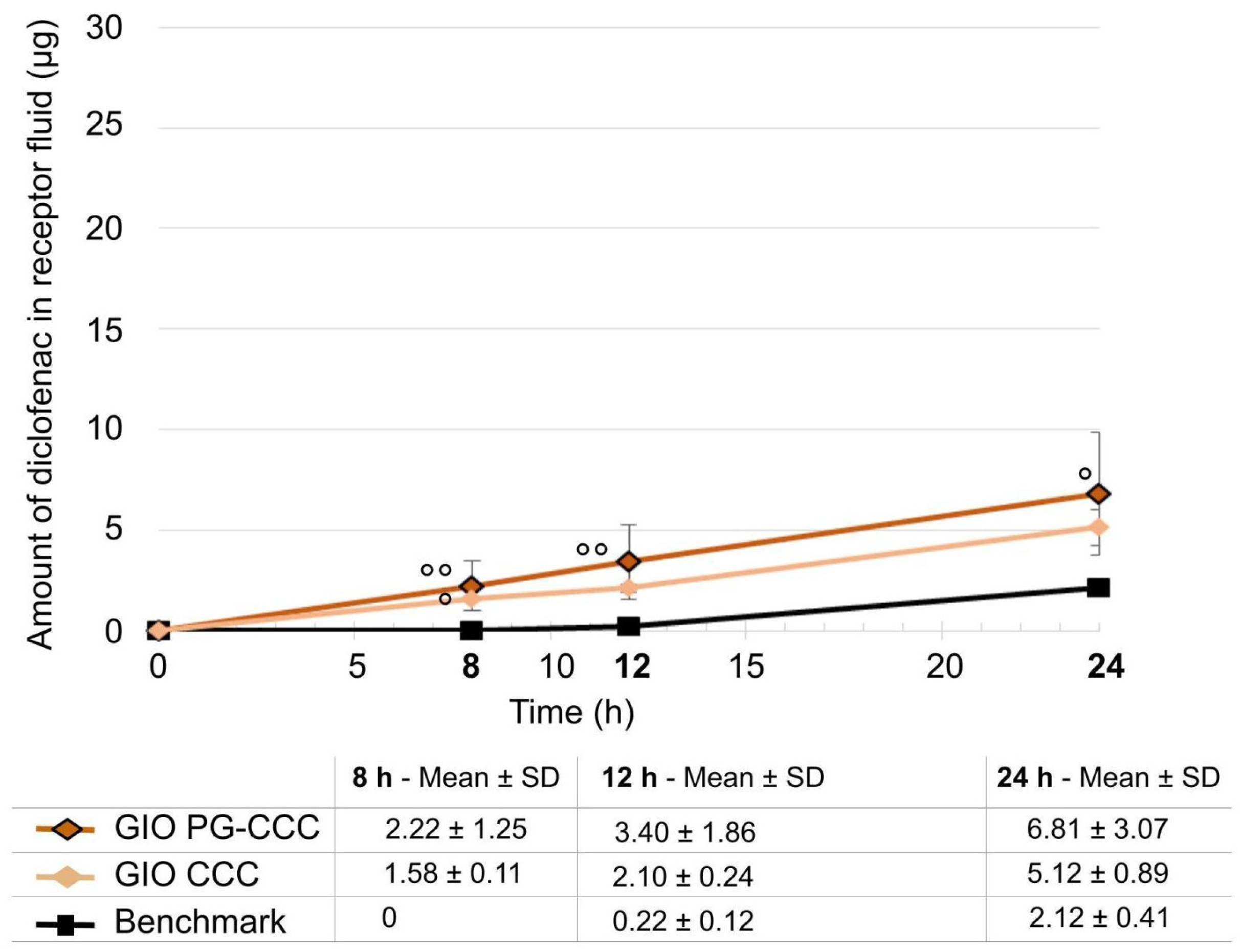
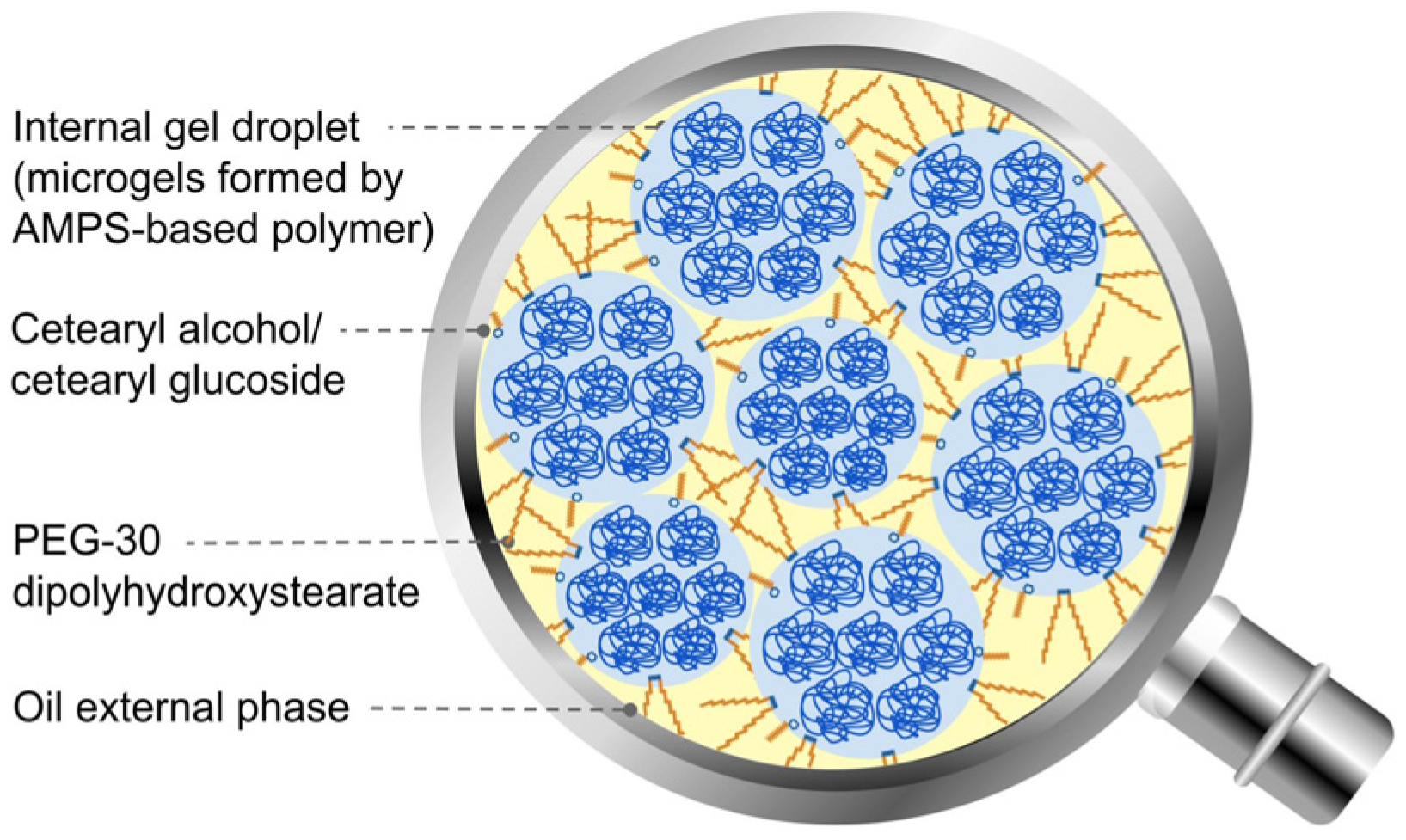
2.2.3. Test 2: Impact of Solvent Removal in Gel-in-Oil Emulsion
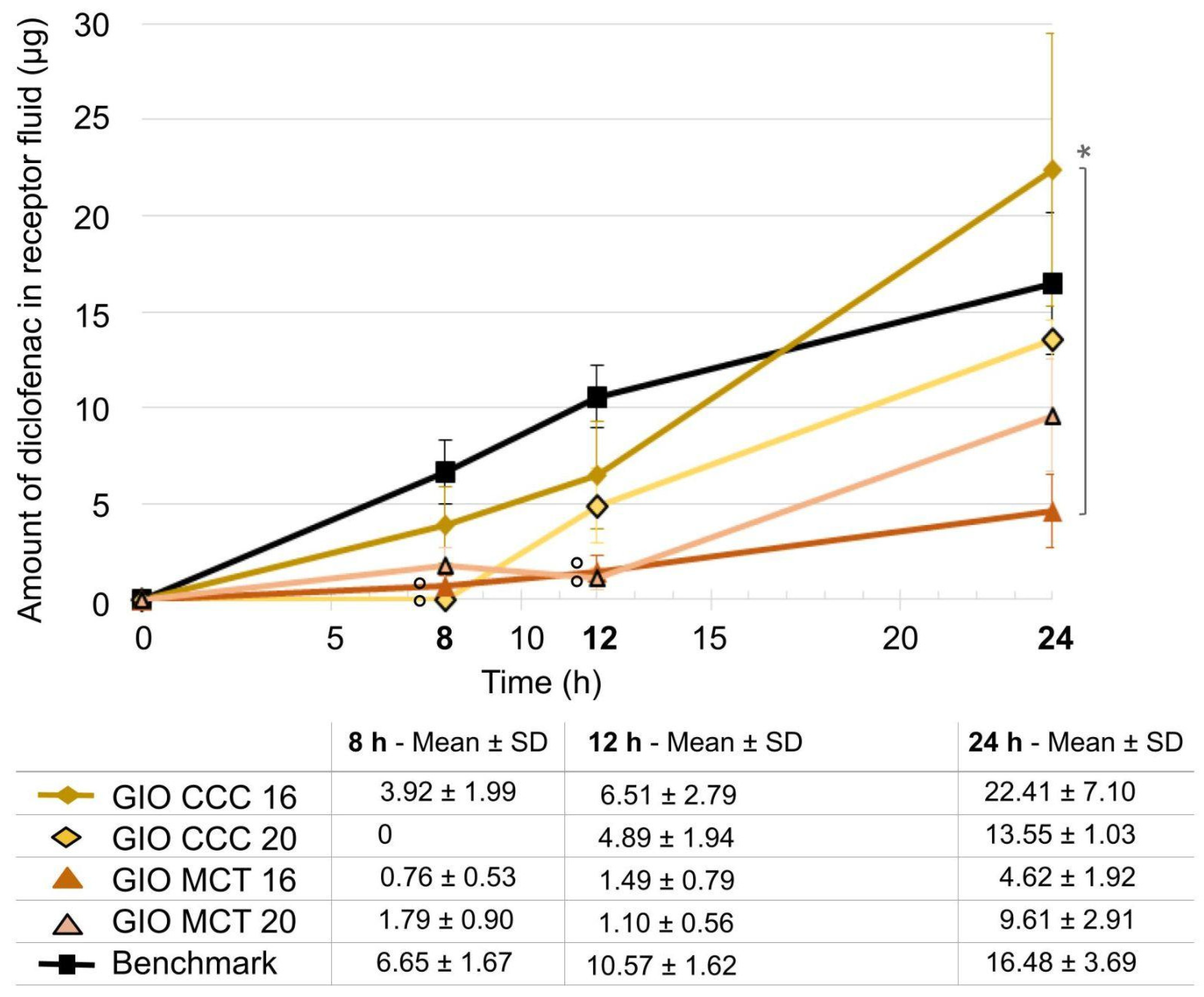
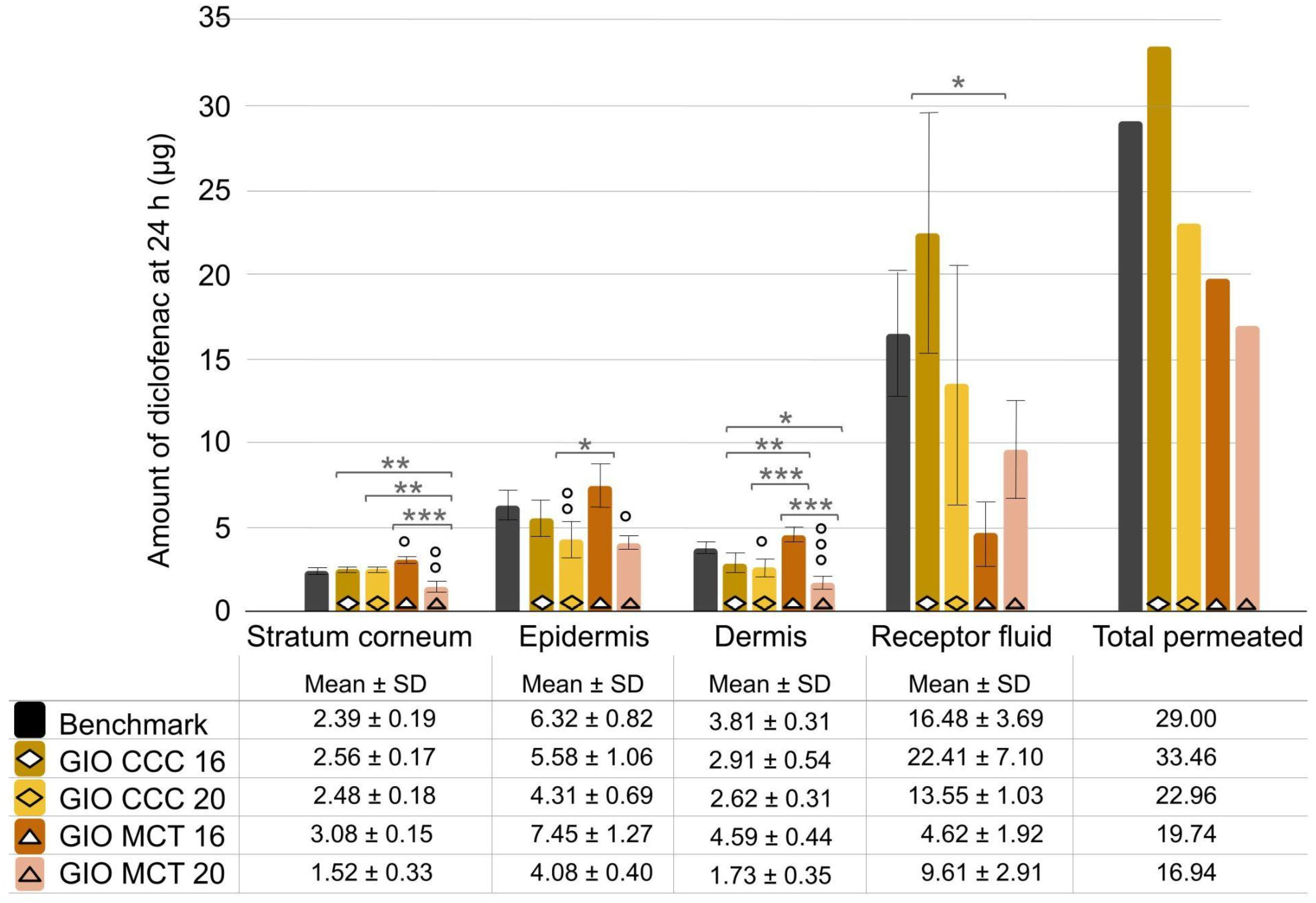
2.2.4. Test 3: Impact of Emollient Type and Concentration Changes in Gel-in-Oil Emulsion
2.3. Rheological Characterisation
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. Benchmark Composition
4.3. Preparation of Formulations
4.4. Physical Stability Assessment
4.5. IVPT Protocol
4.6. Rheological Characterisation
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APMS | 2-Acrylamido-2-Methyl-Propane-Sulfonic Acid |
| ANOVA | Analysis of Variance |
| API | Active Pharmaceutical Ingredient |
| CCC | Coco-caprylate/caprate |
| CG | Cream–gel |
| DEGEE | Diethylene glycol monoethyl ether |
| IPM | Isopropyl myristate |
| IVPT | In vitro Permeation Test |
| HPLC-UV | High-Performance Liquid Chromatography–Ultra-Violet spectroscopy |
| GIO | Gel-in-Oil |
| MCT | Medium-chain Triglyceride |
| MO | Mineral oil |
| NA | Not applicable |
| OECD | Organization for Economic Cooperation and Development |
| PBS | Phosphate buffer saline |
| PG | Propylene glycol |
| pH | Potential of Hydrogen References |
| RT | Room temperature |
| SD | Standard Deviation |
References
- Dragicevic, N.; Maibach, H.I. (Eds.) . Percutaneous Penetration Enhancers Drug Penetration into/through the Skin: Methodology and General Considerations; Springer: Berlin, Germany, 2017; pp. 3–153. [Google Scholar]
- Waghule, T.; Singhvi, G.; Dubey, S.K.; Pandey, M.M.; Gupta, G.; Singh, M.; Dua, K. Microneedles: A smart approach and increasing potential for transdermal drug delivery system. In Biomedicine & Pharmacotherapy; Townsend, D., Ed.; Elsevier: Issy-les-Moulineaux, France, 2019; Volume 109, pp. 1249–1258. [Google Scholar] [CrossRef]
- Yang, H.; Boonme, P.; Amnuaikit, T. Investigation of transdermal permeation behavior of diclofenac sodium microemulsion by confocal laser scanning microscopy. Acta Pol. Pharm. 2023, 80, 129–141. [Google Scholar] [CrossRef]
- Chando, A.; Monin, M.; Mural, Q.; Shaily, L. Topical nanocarriers for management of Rheumatoid Arthritis: A review. BioMed Pharmacother. 2021, 141, 111880. [Google Scholar]
- Liu, Y.; Zhao, J.; Wang, L.; Yan, B.; Gu, Y.; Chang, P.; Wang, Y. Nanocrystals technology for transdermal delivery of water-insoluble drugs. Curr. Drug Deliv. 2018, 15, 1221–1229. [Google Scholar] [CrossRef]
- Garg, N.K.; Tandel, N.; Bhadada, S.K.; Tyagi, R.K. Nanostructured lipid carrier–mediated transdermal delivery of aceclofenac hydrogel present an effective therapeutic approach for inflammatory diseases. Front. Pharmacol. 2021, 12, 713616. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Yang, R.; Yuan, S.; Ding, S.; Wu, Z.; Wu, Z.; Qi, X. Soft multiple emulsions demonstrating reversible freeze-thawing capacity and enhanced skin permeability of diclofenac sodium. Colloid Polym. Sci. 2018, 296, 471–481. [Google Scholar] [CrossRef]
- Bonacucina, G.; Cespi, M.; Palmieri, G.F. Characterization and stability of emulsion gels based on acrylamide/sodium acryloyldimethyl taurate copolymer. AAPS PharmSciTech 2009, 10, 368–375. [Google Scholar] [CrossRef]
- Tan, J.; Chavda, R.; Baldwin, H.; Dreno, B. Management of acne vulgaris with trifarotene. J. Cutan. Med. Surg. 2023, 27, 368–374. [Google Scholar] [CrossRef]
- Puget, A.; Marchand, R.; Roso, A. How to achieve different drug delivery vehicles with simple cold process. In Proceedings of the World Congress on Emulsions, Cité Centre des Congrès, Lyon, France, 12–14 October 2010. [Google Scholar]
- Puget, A.; Amalric, C.; Shen, J. How to achieve a great diversity of vehicles for drug delivery by using a minimum number of ingredients. In Proceedings of the Skin And Formulation Posters, Group 5: Physical Pharmacy, 3rd Symposium & Skin Forum, 10th Annual Meeting, Palais Des Congrès De, Versailles, Versailles, France, 9–10 March 2009. [Google Scholar]
- Bulcourt, C.; Gavinet, B. Flexible formulations to combine high amount of solvents and oils. In Proceedings of the Skin Forum, 2022 18th Annual Meeting, Malmö, Sweden, 21–22 June 2022. [Google Scholar]
- Denis, A.; Bulcourt, C.; Ben Arous, J.; Roso, A. The influence of innovative versatile polymers in skin delivery: Formulation of diclofenac sodium and permeation study. In Proceedings of the 12th World Meeting on Pharmaceutics, Biopharmaceutics & Pharmaceutical Technology, Vienna, Austria, 8–11 February 2021. [Google Scholar]
- Higaki, K.; Asai, M.; Suyama, T.; Nakayama, K.; Ogawara, K.I.; Kimura, T. Estimation of intradermal disposition kinetics of drugs: II. Factors determining penetration of drugs from viable skin to muscular layer. Int. J. Pharm. 2002, 239, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Brunner, M.; Davies, D.; Martin, W.; Leuratti, C.; Lackner, E.; Müller, M. A new topical formulation enhances relative diclofenac bioavailability in healthy male subjects. Br. J. Clin. Pharmacol. 2011, 71, 852–859. [Google Scholar] [CrossRef]
- Base de Données Publique des Médicaments—French Public Medicines Database. Available online: https://base-donnees-publique.medicaments.gouv.fr/affichageDoc.php?specid=60851678&typedoc=R (accessed on 22 May 2023).
- Osborne, D.W. Diethylene glycol monoethyl ether: An emerging solvent in topical dermatology products. J. Cosmet. Dermatol. 2011, 10, 324–329. [Google Scholar] [CrossRef]
- Arellano, A.; Santoyo, S.; Martın, C.; Ygartua, P. Influence of propylene glycol and isopropyl myristate on the in vitro percutaneous penetration of diclofenac sodium from carbopol gels. Eur. J. Pharm. Sci. 1999, 7, 129–135. [Google Scholar] [CrossRef] [PubMed]
- OECD. Test No. 428: Skin Absorption: In Vitro Method, OECD Guidelines for the Testing of Chemicals, Section 4; OECD Publishing: Paris, France, 2004. [Google Scholar] [CrossRef]
- Akomeah, F.K.; Martin, G.P.; Brown, M.B. Variability in human skin permeability in vitro: Comparing penetrants with different physicochemical properties. J. Pharm. Sci. 2007, 96, 824–834. [Google Scholar] [CrossRef] [PubMed]
- Franken, A.; Eloff, F.C.; Du Plessis, J.; Badenhorst, C.J.; Du Plessis, J.L. In vitro permeation of platinum through African and Caucasian skin. Toxicol. Lett. 2015, 232, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Chilcott, R.; Barai, N.; Beezer, A.; Brain, S.; Brown, M.; Bunge, A.; Burgess, S.; Cross, S.; Dalton, C.; Dias, M.; et al. Inter- and intralaboratory variation of in vitro diffusion cell measurements: An international multicenter study using quasi-standardized methods and materials. J. Pharm. Sci. 2005, 94, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Thanushree, H.R.; Kiran Kumar, G.B.; Acharya, A. Formulation development of diclofenac sodium emulgel using aloe vera gel for transdermal drug delivery system. Int. J. Pharm. Sci. Nanotechnol. 2017, 10, 3858–3865. [Google Scholar]
- Balata, G.F.; Shamardl, H.E.; Abd Elmoneim, H.M.; Hakami, A.A.; Almodhwahi, M.A. Propolis emulgel: A natural remedy for burn and wound. Drug Dev. Ind. Pharm. 2018, 44, 1797–1808. [Google Scholar] [CrossRef] [PubMed]
- Daood, N.M.; Jassim, E.Z.; Ghareeb, M.M.; Zeki, H. Studying the effect of different gelling agent on the preparation and characterization of metronidazole as topical emulgel. Asian J. Pharm. Clin. Res. 2019, 12, 571–577. [Google Scholar] [CrossRef]
- Khan, B.A.; Ullah, S.; Khan, M.K.; Alshahrani, S.M.; Braga, V.A. Formulation and evaluation of Ocimum basilicum-based emulgel for wound healing using animal model. Saudi Pharm. J. 2020, 28, 1842–1850. [Google Scholar] [CrossRef]
- Khan, B.A.; Ahmad, S.; Khan, M.K.; Hosny, K.M.; Bukhary, D.M.; Iqbal, H.; Murshid, S.S.; Halwani, A.A.; Alissa, M.; Menaa, F. Fabrication and characterizations of pharmaceutical emulgel co-loaded with naproxen-eugenol for improved analgesic and anti-inflammatory effects. Gels 2022, 8, 608. [Google Scholar] [CrossRef]
- Kalayi, M.; Yeğen, G.; Okur, N.; Aksu, B. Evaluation of emulgel formulations contain diclofenac sodium via quality by design approach. J. Res. Pharm. 2022, 26, 460–468. [Google Scholar] [CrossRef]
- Manian, M.; Jain, P.; Vora, D.; Banga, A.K. Formulation and Evaluation of the In Vitro Performance of Topical Dermatological Products Containing Diclofenac Sodium. Pharmaceutics 2022, 14, 1892. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Imran, M.; Mohammed, Y. Topical Semisolid Products—Understanding the Impact of Metamorphosis on Skin Penetration and Physicochemical Properties. Pharmaceutics 2022, 14, 2487. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, I. Rheology Control Agents for Cosmetics. In Rheology of Biological Soft Matter; Fundamentals and Applications; Kaneda, I., Ed.; Springer: Tokyo, Japan, 2017; pp. 295–321. [Google Scholar] [CrossRef]
- Lessmann, H.; Schnuch, A.; Geier, J.; Uter, W. Skin-sensitizing and irritant properties of propylene glycol: Data analysis of a multicentre surveillance network (IVDK*) and review of the literature. Contact Dermat. 2005, 53, 247–259. [Google Scholar] [CrossRef] [PubMed]
- Chhabra, R.P.; Richardson, J.F. (Eds.) . Non-Newtonian Flow and Applied Rheology: Engineering Applications, 2nd ed.; Butterworth-Heinemann: Oxford, UK, 2011; 52p. [Google Scholar]
- Brummer, R.; Godersky, S. Rheological studies to objectify sensations occurring when cosmetic emulsions are applied to the skin. Colloids Surf. A Physicochem. Eng. Asp. 1999, 152, 89–94. [Google Scholar] [CrossRef]
- Kwak, M.S.; Ahn, H.J.; Song, K.W. Rheological investigation of body cream and body lotion in actual application conditions. Korea-Aust. Rheol. J. 2015, 27, 241–251. [Google Scholar] [CrossRef]
- Huynh, A.; Garcia, A.G.; Young, L.K.; Szoboszlai, M.; Liberatore, M.W.; Baki, G. Measurements meet perceptions: Rheology–texture–sensory relations when using green, bio-derived emollients in cosmetic emulsions. Int. J. Cosmet. Sci. 2021, 43, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Hasler-Nguyen, N.; Fotopoulos, G. Effect of rubbing on the in vitro skin permeation of diclofenac-diethylamine 1.16% gel. BMC Res. Notes 2012, 5, 321. [Google Scholar] [CrossRef]
- Field, T. Massage therapy research review. Complement. Ther. Clin. Pract. 2014, 24, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Paixão, V.L.B.; de Carvalho, J.F. Essential oil therapy in rheumatic diseases: A systematic review. Complement. Ther. Clin. Pract. 2021, 43, 101391. [Google Scholar] [CrossRef]
- Mahdi, M.H.; Conway, B.R.; Mills, T.; Smith, A.M. Gellan gum fluid gels for topical administration of diclofenac. Int. J. Pharm. 2016, 515, 535–542. [Google Scholar] [CrossRef]
- Thomas, S.; Shin, S.H.; Hammell, D.C.; Hassan, H.E.; Stinchcomb, A.L. Effect of controlled heat application on topical diclofenac formulations evaluated by in vitro permeation tests (IVPT) using porcine and human skin. Pharm. Res. 2020, 37, 49. [Google Scholar] [CrossRef] [PubMed]
- Elksnat, A.L.; Zscherpe, P.; Klein, K.; Cavalleri, J.M.; Meißner, J. Effect of an Oxygen-Based Mechanical Drug Delivery System on Percutaneous Permeation of Various Substances In Vitro. Pharmaceutics 2022, 14, 2722. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, K.A.; Khan, I.A.; Ishaq, S.; Iqbal, M.O.; Alqahtani, A.M.; Alqahtani, T.; Menaa, F. Formulation and evaluation of diclofenac potassium gel in sports injuries with and without phonophoresis. Gels 2022, 8, 612. [Google Scholar] [CrossRef] [PubMed]
- Roso, A.; Basset, S.; Braun, O.; Mallo, P. Influence of the process of polymerization on the final properties of thickeners for cosmetics. In Proceedings of the 24th IFSCC Congress, Integration of Cosmetic Sciences, Osaka International Convention Center, Osaka, Japan, 16–19 October 2006. [Google Scholar]
- Amalric, C.; Roso, A.; Tabacchi, G. Providing stable oil continuous emulsion with a sustainable process thus increasing productivity. In Proceedings of the CESIO 7th World Surfactants Congress, Paris, France, 23–25 June 2008. [Google Scholar]
- Sun, L.; Roso, A.; Perez, C. Critical Factors to Obtain Stable High Internal Phase (HIP) Gel-in-Oil Emulsions. J. Cosmet. Sci. 2023, 74, 255–274. [Google Scholar]



| Dosage Form | Emulgel | Cream–Gel | Cream–Gel | Gel-in-Oil | Gel-in-Oil | |
|---|---|---|---|---|---|---|
| Chemical | Trial code | Benchmark [16] | CG PG | CG PG-DEGEE | GIO PG | GIO PG-DEGEE |
| Diclofenac sodium | 1% | 1% | 1% | 1% | 1% | |
| Propylene glycol | Unknown * | 10% | 10% | 10% | 10% | |
| Diethylene glycol monoethyl ether | / | / | 20% | / | 20% | |
| Isopropyl myristate | / | 16% | 16% | 16% | 16% | |
| Coco-caprylate/caprate | Unknown * | / | / | / | / | |
| Liquid paraffin | Unknown * | / | / | / | / | |
| AMPS-based polymer | / | 4% | 4% | 4% | 4% | |
| Cetearyl alcohol/cetearyl glucoside | / | / | / | 1% | 1% | |
| PEG-30 dipolyhydroxystearate | / | / | / | 3% | 3% | |
| Preservatives | / | 1% | 1% | 1% | 1% | |
| Purified water | Up to 100% | Up to 100% | Up to 100% | Up to 100% | Up to 100% | |
| Control at day 7 at RT (Room Temperature) | Visual inspection | Pourable, white ** | Compact, white, shiny, smooth | Pourable, white, shiny, smooth | Pourable, white, shiny, smooth | Liquid, white, shiny, smooth |
| Viscosity *** (mPa·s) | NA **** | 60,000 | 55,000 | 64,000 | 5000 | |
| pH | 7.2 ** | 8.2 | 7.4 | NA **** | NA**** | |
| Conductivity (µS/cm) | NA **** | NA **** | NA **** | ≤0.2 | ≤0.2 | |
| API crystallisation | None ** | None | None | None | None | |
| Stability at 3 months at RT and 45 °C | NA **** | Stable | Stable | Viscosity loss at 1 month/No visual instability | Viscosity loss at 1 month at 45 °C/1% phase separation at 3 months at 45 °C | |
| Dosage Form | Emulgel | Cream–Gel | Cream–Gel | Cream–Gel | Cream–Gel | Gel-in-Oil | Gel-in-Oil | |
|---|---|---|---|---|---|---|---|---|
| Chemical | Trial code | Benchmark | CG PG-DEGEE | CG IPM | CG CCC-MO | CG CCC | GIO PG-CCC | GIO CCC |
| Diclofenac sodium | 1% | 1% | 1% | 1% | 1% | 1% | 1% | |
| Propylene glycol | Unknown * | 10% | / | / | / | 10% | / | |
| Diethylene glycol monoethyl ether | / | 20% | / | / | / | / | / | |
| Isopropyl myristate | / | 16% | 16% | / | / | / | / | |
| Coco-caprylate/caprate | Unknown * | / | / | 8% | 8% | 16% | 16% | |
| Liquid paraffin | Unknown * | / | / | 8% | / | / | / | |
| AMPS-based polymer | / | 4% | 4% | 4% | 4% | 4% | 4% | |
| Cetearyl alcohol/cetearyl glucoside | / | / | / | / | / | 1% | 1% | |
| PEG-30 dipolyhydroxystearate | / | / | / | / | / | 3% | 3% | |
| Preservatives | / | 1% | 1% | 1% | 1% | 1% | 1% | |
| Purified water | Up to 100% | Up to 100% | Up to 100% | Up to 100% | Up to 100% | Up to 100% | Up to 100% | |
| Control at day 7 at RT | Visual inspection | Pourable, white ** | Pourable, white, shiny, smooth | Pourable, white, smooth | Pourable, white, smooth | Compact, white, smooth | Liquid, white | Pourable, white |
| Viscosity *** (mPa·s) | NA **** | 55,000 | 65,000 | 64,000 | 57,000 | 14,490 | 56,300 | |
| pH | 7.2 ** | 7.4 | 8.8 | 8.3 | 8.2 | NA **** | NA **** | |
| Conductivity (µS/cm) | NA **** | NA **** | NA **** | NA **** | NA **** | ≤0.2 | ≤0.2 | |
| API crystallisation | None ** | None | None | None | None | None | None | |
| Stability at 3 months at RT and 45 °C | NA **** | Stable | Stable | Stable | Stable | Viscosity loss at 1 month at 45 °C/1% phase separation at 3 months at 45 °C | Viscosity loss at 1 month at 45 °C/Beginning of phase separation at 3 months at 45 °C | |
| Dosage Form | Emulgel | Gel-in-Oil | Gel-in-Oil | Gel-in-Oil | Gel-in-Oil | |
|---|---|---|---|---|---|---|
| Chemical | Trial code | Benchmark | GIO CCC 16 | GIO CCC 20 | GIO MCT 16 | GIO MCT 20 |
| Diclofenac sodium | 1% | 1% | 1% | 1% | 1% | |
| Coco-caprylate/caprate | Unknown * | 16% | 20% | / | / | |
| Medium-chain triglyceride | / | / | / | 16% | 20% | |
| Coco-caprylate/caprate | Unknown * | / | / | / | / | |
| Liquid paraffin | Unknown * | / | / | / | / | |
| AMPS-based polymer | / | 4% | 4% | 4% | 4% | |
| Cetearyl alcohol/cetearyl glucoside | / | 1% | 1% | 1% | 1% | |
| PEG-30 dipolyhydroxystearate | / | 3% | 3% | 3% | 3% | |
| Preservatives | / | 1% | 1% | 1% | 1% | |
| Purified water | Up to 100% | Up to 100% | Up to 100% | Up to 100% | Up to 100% | |
| Control at day 7 at RT | Visual inspection | Pourable, white ** | Liquid, white, smooth | Liquid, white, smooth | Compact, white, smooth | Liquid, white, smooth |
| Viscosity *** (mPa·s) | NA **** | 14,300 | 7320 | 103,000 | 26,000 | |
| pH | 7.2 ** | NA **** | NA **** | NA **** | NA **** | |
| Conductivity (µS/cm) | NA **** | ≤0.2 | ≤0.2 | ≤0.2 | ≤0.2 | |
| API crystallisation | None ** | None | None | None | None | |
| Stability at 3 months at RT and 45 °C | NA **** | Beginning of phase separation at 45 °C | 1% phase separation at 7 days at 45 °C and 1 month at RT | Stable | Beginning of phase separation at 7 days at 45 °C | |
| Trial Code | Benchmark | CG CCC | GIO MCT 16 | ||
|---|---|---|---|---|---|
| Dosage form | Emulgel | Cream–gel | Gel-in-oil emulsion | ||
| Flow | Rate index n | 0.449 | 0.402 | 0.708 | |
| Yield stress (Pa) | 30.8 | 19.4 | 11.3 | ||
| Thixotropy | Recovery time (s) | 11 | 7 | 28 | |
| Structural recovery (%) | 84 | 105 | 140 | ||
| Oscillation Amplitude | Linear domain | Complex modulus G* (Pa) | 368 | 388 | 184 |
| tan δ | 0.11 | 0.13 | 0.38 | ||
| Plastic domain | σL (Pa) | 5.64 | 10.79 | 2.24 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gavinet, B.; Sigurani, S.; Garcia, C.; Roso, A. Alternatives to Conventional Topical Dosage Forms for Targeted Skin Penetration of Diclofenac Sodium. Int. J. Mol. Sci. 2024, 25, 7432. https://doi.org/10.3390/ijms25137432
Gavinet B, Sigurani S, Garcia C, Roso A. Alternatives to Conventional Topical Dosage Forms for Targeted Skin Penetration of Diclofenac Sodium. International Journal of Molecular Sciences. 2024; 25(13):7432. https://doi.org/10.3390/ijms25137432
Chicago/Turabian StyleGavinet, Benjamin, Séverine Sigurani, Christine Garcia, and Alicia Roso. 2024. "Alternatives to Conventional Topical Dosage Forms for Targeted Skin Penetration of Diclofenac Sodium" International Journal of Molecular Sciences 25, no. 13: 7432. https://doi.org/10.3390/ijms25137432
APA StyleGavinet, B., Sigurani, S., Garcia, C., & Roso, A. (2024). Alternatives to Conventional Topical Dosage Forms for Targeted Skin Penetration of Diclofenac Sodium. International Journal of Molecular Sciences, 25(13), 7432. https://doi.org/10.3390/ijms25137432







