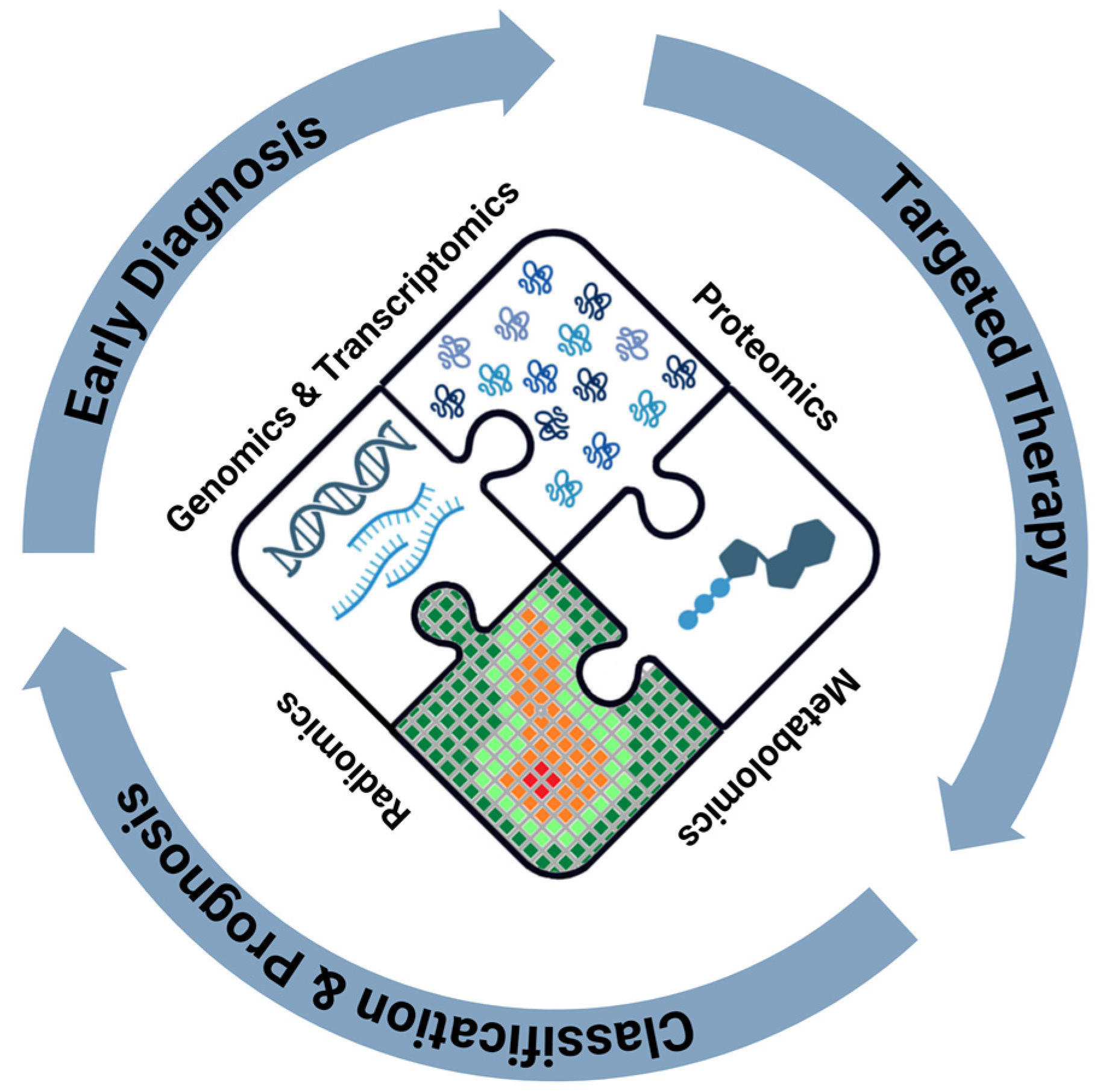
Understanding the Conundrum of Pancreatic Cancer in the Omics Sciences Era
Abstract
:1. Introduction
2. Metabolic Changes in Pancreatic Cancer Cells
3. Metabolomics
| Article | Results |
|---|---|
| Sugimoto et al. (2010) [28] | Analysis of 57 different metabolites in saliva samples using capillary electrophoresis time-of-flight mass spectrometry to discriminate PDAC patients from healthy controls with an AUC of 0.993. |
| Daemen et al. (2015) [24] | Identification of three metabolic subtypes in PDAC: low proliferating (low amino acid and carbohydrate levels), glycolytic (enrichment of glycolysis and serine pathway components, association with mesenchymal subtype), and lipogenic (abundance of different lipid metabolites, association with epithelial subtype). |
| Yu et al. (2015) [27] | Glucose-dependent metabolic (Warburg and mixed) subtypes associated with nerve infiltration (p = 0.0003), UICC stage (p = 0.0004), activated autophagic status in tumor (p = 0.0167), positive marginal status (p < 0.0001), lymphatic invasion (p < 0.0001), and activated autophagic status in stroma (p = 0.0002), respectively. Glutamine-dependent metabolic (non-canonical and mixed) subtypes associated with vascular invasion (p = 0.0073), highest percentage of activated autophagy in tumors (p = 0.0034), and shorter overall survival (p < 0.001) in PDAC. |
| Mehta et al. (2017) [29] | Identification of a panel of 10 blood metabolites using targeted mass spectrometry to discriminate PDAC from healthy control (AUC = 0.997) patients with type 2 diabetes mellitus (AUC = 0.992) and colorectal cancer patients (AUC = 0.653). |
| Mayerle et al. (2018) [31] | Identification of a composite panel of biomarkers (9 metabolites—class of lipids including sphinganine-1-phosphate, two sphingomyelins, and one ceramide) to distinguish all stages of PDAC and resectable PDAC from CP with higher accuracy (90.6% and 90.8% respectively) than CA 19-9 (AUC 0.94 vs. 0.85, p < 0.001 for all tumor stages; 0.93 vs. 0.84, p < 0.001 for resectable PDAC). |
| Luo et al. (2020) [30] | Analysis of five metabolite biomarkers in plasma (creatine, inosine, beta-sitosterol, sphinganine and glycocholic acid) with higher accuracy and specificity to diagnose PDAC than conventional biomarkers (CA 125, CA 19-9, CA 242, and CEA). Role of succinic acid and gluconic acid in monitoring progression and metastasis of PDAC at different stages. |
| Kaoutari et al. (2021) [26] | Association of a metabolic signature with PDAC molecular gradient (R = 0.44 and p < 0.001) to predict clinical outcomes (p < 0.001, HR = 2.68, 95% CI: 1.5–4.9), transcriptomic phenotypes, and drug resistance (gemcitabine, oxaliplatin, docetaxel, SN-38, and 5-Fluorouracil). |
| Mahajan et al. (2021) [33] | Identification of three metabolic PDAC subtypes associated with distinct complex lipid patterns: subtype 1 (reduced ceramide levels, strong enrichment of triacylglycerols), 2 (increased abundance of ceramides, sphingomyelin, and other complex sphingolipids), and 3 (decreased levels of sphingolipid metabolites). |
| Mahajan et al. (2022) [32] | Role of i-Metabolic Signature (12 analytes + CA 19-9) in distinguishing PDAC from CP with AUC of 97.2%, 93.5%, and 92.2% in the identification and validation of cohorts 1 and 2, respectively. Role of m-Metabolic signature (4 analytes + CA 19-9) in discriminating PDAC from CP with a sensitivity of 77.3%, a specificity of 89.6%, and an overall accuracy of 82.4%. |
4. Proteomics
| Article | Proteins | Results |
|---|---|---|
| Papapanagiotou et al. (2018) [37] | SPARC, Osteonectin | Sensitivity of 84.6% and specificity of 87.5% in detection of early-stage PDAC. |
| Jin et al. (2018) [38] | ZIP4 | Discrimination between malignant pancreatic cancer patients and benign pancreatic disease patients with an AUC of 0.89. |
| Saukkonen et al. (2016) [39] | PROX1, β-catenin | High PROX1 (48%) and β-catenin (65%) expression in PDAC associated with lower risk of death from PDAC (HR = 0.63; 95% CI, 0.42–0.95, p = 0.026; and HR = 0.54; 95% CI, 0.35–0.82, p = 0.004; respectively). Combined high expression predicting lower risk of death from PDAC (HR = 0.46; 95% CI, 0.28–0.76, p = 0.002). |
| Mohamed et al. (2016) [40] | ADH, MIC-1 | High sensitivity (90%) and specificity (83%) for ADH in detecting early PDAC. Improved efficacy when ADH and MIC-1 combined to CA 19-9 (p = 0.023, AUC 0.89). |
| Capello et al. (2017) [41] | TIPM1, LRG1, CA 19-9 | Improvement of sensitivity (0.849 vs. 0.667) at 95% specificity with an AUC of 0.949 (95% CI, 0.92–0.98) and 0.887 (95% CI, 0.82–0.96) in discriminating early-stage PDAC vs. healthy subjects in combined validation and test sets, respectively. Better performance compared to CA 19-9 alone (p < 0.001 combined validation set; p = 0.008 test set). |
| Yoneyama et al. (2016) [42] | IGFBP2, IGFBP3 | Sensitivity of 68.4% and 76.3% and specificity of 67.7% and 70.7%, respectively, for IGFBP2 and IGFBP3 in detecting early-stage PDAC. IGFBP2 associated with increased risk of diseases of pancreatic malignancy. Combination of IGFBP2 and IGFBP3 with CA 19-9 with an AUC of 0.90. |
| Chang et al. (2009) [43] | Osteopontin, Chitinase 3-like 1, CA 19-9 | Higher sensitivity for PDAC compared with CA 19-9 alone (93% vs. 80%). CEA and CA 125 with prognostic significance for survival for local advanced PDAC (p < 0.003). |
| Brand et al. (2011) [44] | CA 19-9, CEA, TIMP-1 | Higher sensitivity (respectively 76% and 71%) and specificity (respectively 90% and 89%) in discriminating PDAC from benign subjects in training tests and independent validation sets. |
| McKinney et al. (2011) [45] | BGN, PEDF, THBS-2, βIGH3 | Up-regulation in BGN, PEDF, THBS-2, and βIGH3 associated with PDAC progression, as players in tumor microenvironment, cell proliferation, or angiogenic processes. |
| Ehmann et al. (2007) [46] | Apolipoprotein A-II, transthyretin, apolipoprotein A-I | Sensitivity of 100% and specificity of 98% for training data set and sensitivity of 83% and specificity of 77% for test data in differentiation of PDAC from healthy controls. |
| Nicoletti et al. (2023) [47] | MSLN, MUC4, ANXA10, GPC-1 | Selective expression of MSLN, MUC4, ANXA10, and GPC-1 in the neoplastic tissue compared to non-tumor ductal and acinar tissues (p < 0.001). |
| Tian et al. (2019) [48] | Fibrillar collagen COL6A3, FBN-1, FN1, fibrinogens, POSTN, PRELP, FMOD, DCN, OGN, ASPN | Overexpression of COL6A3, FBN-1, FN1, fibrinogens (FGA, FGB, and FGG), and POSTN in PDAC. OGN, PRELP, FMOD, DCN, and ASPN associated with worse prognosis. |
| Zhou et al. (2019) [49] | BASP1, WT1 | BASP1 association with prolongation of survival (HR 0.468, 95% CI, 0.257–0.852, p = 0.013) and better response to adjuvant chemotherapy treatment in PDAC. WTI association with worsened survival (HR 1.636, 95% CI, 1.083–2.473, p = 0.019) and resistance to chemotherapy. |
| Fong et al. (2008) [50] | TROP2, JAM-A | TROP2 overexpression associated with decreased overall survival (p< 0.01), presence of lymph node metastasis (p = 0.04), tumor grade (p = 0.01), and poor progression-free survival after surgery (p < 0.01). |
| Zong et al. (2011) [51] | TBX4 | High expression (62.3%) in PDAC associated with longer survival (p = 0.010). |
| Schafer et al. (2012) [52] | HSP27 | High expression in PDAC correlated inversely with nuclear p53 accumulation and associated with better response to chemotherapy with Gemcitabine. |
| Marechal et al. (2010) [53] | dCK | Association with prolonged survival after adjuvant Gemcitabine for resected pancreatic adenocarcinoma as independent prognostic factor (DFS: HR, 3.48; 95% CI, 1.66–7.31; p = 0.001; OS: HR, 3.2; 95% CI, 1.44–7.13; p = 0.004). |
| Mann et al. (2012) [54] | Notch1, Notch3, Notch4, HES-1, HEY-1 | Increased expression in tumor tissue and locally advanced and metastatic PDAC compared to resectable PDAC (p ≤ 0.001). Notch3 and HEY-1 expression associated with reduced OS and DFS following tumor resection. |
| Khushman et al. (2017) [55] | CD63, CD9 | Higher expression in pathologic tissues compared with adjacent normal tissues (mean multiplicative Q score with p = 0.0041 and p = 0.0018; mean Q score with p < 0.0001 and p < 0.0124). |
| Schultz et al. (2015) [56] | YKL-40, IL-6, CA 19-9 | Significant OR for prediction of PDAC:
|
| McCaffery et al. (2013) [58] | IGF-1, IGFBP2-3 | Improved OS association in treatment with Ganitumab with higher levels of IGF-1 (16 vs. 6.8 months-HR, 0.25; 95% CI: 0.09–0.67), IGF-2 (16 vs. 5.9 months-HR, 0.24; 95% CI: 0.09–0.68), and IGFBP-3 (16 vs. 6.8 months-HR, 0.28; 95% CI: 0.11–0.73), or lower levels of IGFBP-2 (12.7 vs. 6.6 months-HR, 0.19; 95% CI: 0.07–0.55) in PDAC. |
5. Genomics
| Article | Imaging | Results |
|---|---|---|
| Hosein et al. (2022) [59] | KRAS, P53, CDKN2A, SMAD4, BRCA1/2, PALB2, dMMR, BRAF, NRG1, NTRK | KRAS, TP53, CDKN2A, and SMAD4 mutations present in >90% of patients with PDAC. Association of chromatin modification genes (ARID1A, KMT2D, and KMT2C), DNA repair genes (BRCA1, BRCA2, and PALB2), and additional oncogenes (BRAF, MYC, FGFR1) in about 10% of patients with PDAC. |
| Varghese et al. (2021) [63] | ETV6-NTRK3, TPR-NTRK1, SCLA5-NRG1, ATP1B1-NRG1 fusions, IDH1 R132C mutation, mismatch repair deficiency | Association of KRAS wild-type cancers (ETV6-NTRK3, TPR-NTRK1, SCLA5-NRG1, and ATP1B1-NRG1 fusions, IDH1 R132C mutation, and mismatch repair deficiency) with early-onset of disease. |
| Ben Aharon et al. (2019) [64] | SMAD4 | Association of SMAD4 higher mutation rates, higher expression levels of phospo-GSK3 and increased activation of TGFb pathway with early-onset PDAC. |
| Ala et al. (2021) [65] | C-Myc | Association of C-Myc overexpression with chemoresistance, intra-tumor angiogenesis, epithelial–mesenchymal transition, metastasis, and aggressive behavior of PDAC. |
| Wang et al. (2023) [66] | NCAPG2 | Association of NCAPG2 overexpression with immune cell infiltration, immune checkpoint genes, tumor mutational burden, and microsatellite instability. Association of NCAPG2 down-regulation with reduced proliferation, invasion, and metastasis in PDAC. |
| Golan et al. (2019) [67] | BRCA1, BRCA2 | Association of Olaparib (PARP inhibitor) treatment with longer median progression-free survival than in the placebo group (7.4 months vs. 3.8 months; HR for disease progression or death, 0.53; 95% confidence interval, 0.35 to 0.82; p = 0.004). |
| Hallin et al. (2022) [69] | KRAS | Association of KRAS mutant inhibitors (MRTX1133) with marked tumor regression (≥30%) in PDAC. |
| Strickler et al. (2023) [70] | KRAS | Association of KRAS G12C inhibitor (Sotorasib) with anticancer activity and acceptable safety profile in advanced PDAC that had received previous treatment. |
| Bekaii-Saab et al. (2023) [71] | KRAS | Association of KRAS G12C inhibitor (Adagrasib) with encouraging response (median progression-free survival of 7.4 months—95% CI, 5.3 to 8.6) and good tolerance in pretreated PDAC patients. |
| Garcia et al. (2017) [72] | BRAF, RTK, MAPK | Association of BRAF alterations (p.N486_P490del in-frame deletion, BRAFV600E mutation, BRAF fusion), receptor tyrosine kinase (RTK) fusions (ROS1, NRG1, NTRKQ, NTRK3, and FGFR2), and MAPK pathway alterations (amplifications in EGFR, ERBB2, and MET) with PDAC. |
| Reese et al. (2020) [75] | miR-200b, miR-200c | Association of overexpression of miR-200b and miR-200c with PDAC as compared to healthy controls (p < 0.001; p = 0.024) and CP (p = 0.005; p = 0.19). Correlation of high expression of miR-200c and miR-200b with shorter overall survival (p = 0.038 and p = 0.013 respectively). |
| Li et al. (2010) [76] | miR-200a, miR-200b | Association of miR-200a and miR-200b hypomethylation and overexpression with PDAC. Association of elevated levels of miR-200a and miR-200b with PDAC and CP compared with healthy controls (p < 0.00019). |
| Pu et al. (2020) [77] | miR-21, miR-212-3p, miR-10b | Association of higher levels of miR-21 and miR-10b with PDAC. miR-21 with better diagnostic performance (p = 0.0003, AUC 0.72). Better diagnostic value with combination of miR-21 and miR-10b (p < 0.0001, AUC 0.79). Role of miR-21 in distinguishing early-stage PDAC from control and advanced-stage PDAC (p < 0.05, early-stage vs. healthy; p < 0.001, early-stage vs. advanced stage). |
| Que et al. (2013) [78] | miR-17-5p, miR-21, miR-155 and miR-196a | Association of low expression of miR-155 and miR-196a and high expression of miR-17-5P with PDAC. Correlation of high levels of miR-17-5p with metastasis and advanced PDAC. |
6. Transcriptomics
| Article | Technique | Results |
|---|---|---|
| Moncada et al. (2020) [80] | Single-cell RNA seq | Defined subpopulations and spatial organization of cells composing PC tissues and reveal their complex interactions. |
| Raghavan et al. (2021) [81] | Single-cell RNA seq | Systematic profiling of metastatic PC biopsies and matched organoid models provided a view of cellular states, their regulation by tumor microenvironment, and the ability to modulate these states to impact drug responses. Cancer subtype influenced tumor microenvironment in terms of immunosuppressive macrophages and T-cell infiltration. |
| Hwang et al. (2022) [82] | Single-cell RNA seq + spatial transcriptomics | Identified multicellular dynamics and further evolution in PC cell biology associated with neoadjuvant treatment. |
| Cui Zhou et al. (2022) [83] | Single-cell RNA seq + spatial transcriptomics | Identified tumor and transitional subpopulations of cells with distinct histological features. Chemoresistance was determined by an increase in inflammatory cytokines in the tumor microenvironment as an adaptive response to stress in cancer cells. |
| Falcomatà et al. (2022) [84] | Single-cell RNA seq + CRISPR screen + immunophenotyping | Study of intratumor infiltration of cytotoxic and effector T-cells and sensitization of mesenchymal PC to PD-L1 immune checkpoint inhibition. |
| Barthel et al. (2023) [79] | Single-cell RNA seq + spatial transcriptomics | Multimodal approaches to elucidate PC biology and response to therapy. |
7. Radiomics
| Article | Imaging | Results |
|---|---|---|
| Săftoiu et al. (2008) [97] | EUS | Sensitivity of 91.4%, specificity of 87.9%, and accuracy of 89.7% in differentiating benign (normal pancreas, CP) and malignant masses (PDAC, NET), respectively. Positive predictive value of 88.9% and negative predictive value of 90.6%. |
| Chakraborty et al. (2017) [113] | CT | Texture analysis to quantify heterogeneity in CT images to accurately predict 2-year survival in patients with PDAC (AUC of 0.90 and accuracy of 82.86% with the leave-one-image-out technique and an AUC of 0.80 and accuracy of 75.0% with three-fold cross-validation). |
| Cassinotto et al. (2017) [114] | CT | Lymph node ratio (R2 = 0.15), kurtosis (R2 = 0.08), and CENTRAL-AV (R2 = 0.04) associated with early-recurrence in resectable PDAC. CENTRAL-AV < 62 Hounsfield units associated with a shorter 1-year DFS (35% versus 68%, p = 0.004). |
| Zhang et al. (2018) [100] | CT | Rad score could predict postoperative pancreatic fistula in patients undergoing pancreaticoduodenectomy with an AUC of 0.82 in the training cohort and of 0.76 in the validation cohort. |
| Attiyeh et al. (2018) [106] | CT | Quantitative image features combined with CA 19-9 achieved a c-index of 0.69 [integrated Brier score (IBS) 0.224] on the test data, while combining CA 19-9, imaging, and the Brennan score achieved a c-index of 0.74 (IBS 0.200) on the test data in resected PDAC. |
| Chu et al. (2019) [95] | CT | Overall accuracy of 99.2% and AUC 99.9% for random forest binary classification (PDAC and normal pancreas). 100% of PDAC correctly classified with 100% sensitivity and 98.5% specificity. |
| Bian et al. (2019) [98] | CT | Significant association between the arterial rad-score and the lymph node metastasis (p < 0.0001) in PDAC. |
| Cozzi et al. (2019) [105] | CT | Significant association of clinical-radiomic signature with overall survival in training and validation sets (p = 0.01 and 0.05; concordance index 0.73 and 0.75 respectively) after stereotactic body radiotherapy for PDAC. |
| Wei et al. (2019) [107] | CT | Radiomics-based computer-aided diagnosis scheme could increase preoperative diagnostic accuracy (AUC = 0.767, sensitivity = 0.686, specificity = 0.709) in differentiating pancreatic serous cystic neoplasms from other pancreatic cystic neoplasms. |
| Corral et al. (2019) [110] | MRI | Deep learning protocol with high sensitivity and specificity to detect dysplasia (92% and 52%, respectively), high-grade dysplasia or cancer (75% and 78%, respectively), and an accuracy comparable to radiologic criteria (AUC 0.76 for American Gastroenterology Association, 0.77 for Fukuoka and 0.78 for the deep learning protocol, p = 0.90). |
| Kuwahara et al. (2019) [111] | EUS | Artificial intelligence deep learning algorithm with a significantly greater score for malignant IPMNs than benign IPMNs (0.808 vs. 0.104, p < 0.001). High sensitivity, specificity and accuracy of AI malignant probability (95.7%, 92.6% and 94.0%, respectively) in detecting malignant IPMNs. |
| Liu et al. (2020) [99] | CT | Radiomics LOG model with higher predictive efficiency compared to the conventional preoperative evaluation method of lymph node status (AUC = 0.84; 95% CI, 0.758~0.925 vs. AUC = 0.68; 95% CI, 0.566~0.798) in the resectable PDAC. |
| Park et al. (2020) [94] | CT | Differentiation of AIP from PDAC with 95.2% accuracy (59/62; 95% CI, 89.8–100%) and AUC of 0.975 (95% CI, 0.936–1.0). 100% of PDAC correctly classified with thin-slice venous phase with 89.7% sensitivity (26/29; 95% CI, 78.6–100%) and 100% specificity (33/33; 95% CI, 93–100%). |
| Parr et al. (2020) [104] | CT | Role of a 6-feature radiomic signature in achieving better overall survival prediction performance (mean concordance index 0.66 vs. 0.54) and of a 7-feature radiomic signature in predicting recurrence (mean concordance index 0.78 vs. 0.66 on resampled cross-validation test sets) in PDAC. |
| Li et al. (2021) [101] | CT | Extreme gradient boosting classifier (XGBoost) showed sensitivity, specificity, accuracy, positive and negative predictive values of 0.81, 0.60, 0.69, 0.63, and 0.79, respectively, for the training set, and 0.81, 0.58, 0.68, 0.61, and 0.79, respectively, for the validation set in predicting CD8+ tumor-infiltrating lymphocyte expression levels in PDAC. |
| Huang et al. (2021) [108] | CT | Arterial radiomics model constructed by the 3D-ROI feature performed better (AUC: 0.914) than venous (AUC: 0.815) in predicting the invasiveness of pancreatic solid pseudopapillary neoplasms. |
| Watson et al. (2021) [102] | Deep learning models predicted pathologic tumor response to neoadjuvant therapy in PC (AUC for the response to chemotherapy and resectability were 0.738 and 0.783, respectively). | |
| Watson et al. (2021) [109] | CT | Deep learning model correctly predicted malignancy of pancreatic cystic neoplasms (3 of 3 malignant lesions and 5 of 6 benign lesions), performing better than consensus guidelines (2 of 3 malignant lesions as high risk and 4 of 6 benign lesions as worrisome). |
| Mukherjee et al. (2022) [96] | CT | Support random machine with the highest sensitivity (95.5%; 95% CI, 85.5–100.0), specificity (90.3; 95% CI, 84.3–91.5), F1-score (89.5; 95% CI, 82.3–91.7), AUC (0.98; 95% CI, 0.94–0.98) and accuracy (92.2%; 95% CI, 86.7–93.7) for differentiation of PDAC at the prediagnostic stage from normal pancreas. |
8. Single-Cell Profiling, Multi-Omics, Future Applications and Perspectives of Omics Sciences
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AUC | area under the curve |
| ADH | alcohol dehydrogenase |
| AIP | autoimmune pancreatitis |
| ANXA10 | annexin A10 |
| ASPN | asporin |
| BASP1 | brain acid soluble protein 1 |
| BGN | biglycan |
| CI | confidence interval |
| CP | chronic pancreatitis |
| CRISPR | clustered regularly interspaced short palindromic repeats |
| CT | computed tomography |
| dCK | deoxycytidine kinase |
| DCN | decorin |
| DFS | disease-free survival |
| EUS | endoscopic ultrasound |
| FBN-1 | fibrillin-1 |
| FMOD | fibromodulin |
| FN1 | fibronectin |
| GPC-1 | glypican 1 |
| HR | hazard ratio |
| HSP27 | heat shock protein 27 |
| IGF | insulin-like growth factor |
| IGFBP | insulin-like growth factor-binding protein |
| IPMN | intraductal papillary mucinous neoplasia |
| JAM-A | junctional adhesion molecule A |
| LRG1 | leucine-rich alpha-2 glycoprotein 1 |
| MIC-1 | circulating macrophage inhibitory cytokine |
| MRI | magnetic resonance imaging |
| MSLN | mesothelin |
| MUC4 | mucin 4 |
| NET | neuroendocrine tumor |
| OGN | osteoglycin |
| OR | odds ratio |
| PC | pancreatic cancer |
| PDAC | pancreatic ductal adenocarcinoma |
| PEDF | pigment epithelium factor |
| POSTN | periostin |
| SPARC | secreted protein acidic and rich in cystein |
| TBX4 | T-box transcription factor 4 |
| THBS2 | thrombospondin-2 |
| TIMP1 | tissue inhibitor of metalloproteinase-1 |
| UICC | union for international cancer control |
| WT1 | Wilms tumor protein |
| βIGH3 | TGF-β induced protein ig-h3 precursor |
References
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- Kleeff, J.; Korc, M.; Apte, M.; La Vecchia, C.; Johnson, C.D.; Biankin, A.V.; Neale, R.E.; Tempero, M.; Tuveson, D.A.; Hruban, R.H.; et al. Pancreatic cancer. Nat. Rev. Dis. Primers 2016, 2, 16022. [Google Scholar] [CrossRef] [PubMed]
- Strobel, O.; Neoptolemos, J.; Jäger, D.; Büchler, M.W. Optimizing the outcomes of pancreatic cancer surgery. Nat. Rev. Clin. Oncol. 2019, 16, 11–26. [Google Scholar] [CrossRef] [PubMed]
- GBD2017 Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2019, 4, 934–947. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Lok, V.; Ngai, C.H.; Zhang, L.; Yuan, J.; Lao, X.Q.; Ng, K.; Chong, C.; Zheng, Z.-J.; Wong, M.C. Worldwide Burden of, Risk Factors for, and Trends in Pancreatic Cancer. Gastroenterology 2021, 160, 744–754. [Google Scholar] [CrossRef] [PubMed]
- Ho, W.J.; Jaffee, E.M.; Zheng, L. The tumour microenvironment in pancreatic cancer—Clinical challenges and opportunities. Nat. Rev. Clin. Oncol. 2020, 17, 527–540. [Google Scholar] [CrossRef] [PubMed]
- Collisson, E.A.; Sadanandam, A.; Olson, P.; Gibb, W.J.; Truitt, M.; Gu, S.; Cooc, J.; Weinkle, J.; Kim, G.E.; Jakkula, L.; et al. Subtypes of pancreatic ductal adenocarcinoma and their differing responses to therapy. Nat. Med. 2011, 17, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Moffitt, R.A.; Marayati, R.; Flate, E.L.; Volmar, K.E.; Loeza, S.G.H.; Hoadley, K.A.; Rashid, N.U.; Williams, L.A.; Eaton, S.C.; Chung, A.H.; et al. Virtual microdissection identifies distinct tumor- and stroma-specific subtypes of pancreatic ductal adenocarcinoma. Nat. Genet. 2015, 47, 1168–1178. [Google Scholar] [CrossRef] [PubMed]
- Puleo, F.; Nicolle, R.; Blum, Y.; Cros, J.; Marisa, L.; Demetter, P.; Quertinmont, E.; Svrcek, M.; Elarouci, N.; Iovanna, J.L.; et al. Stratification of Pancreatic Ductal Adenocarcinomas Based on Tumor and Microenvironment Features. Gastroenterology 2018, 155, 1999–2013.e3. [Google Scholar] [CrossRef]
- Chan-Seng-Yue, M.; Kim, J.C.; Wilson, G.W.; Ng, K.; Flores-Figueroa, E.; O’Kane, G.M.; Connor, A.A.; Denroche, R.E.; Grant, R.C.; McLeod, J.; et al. Transcription phenotypes of pancreatic cancer are driven by genomic events during tumor evolution. Nat. Genet. 2020, 52, 231–240. [Google Scholar] [CrossRef]
- Zhou, X.; Hu, K.; Bailey, P.; Springfeld, C.; Roth, S.; Kurilov, R.; Brors, B.; Gress, T.; Buchholz, M.; An, J.; et al. Clinical Impact of Molecular Subtyping of Pancreatic Cancer. Front. Cell Dev. Biol. 2021, 9, 743908. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Otsuka, M.; Seimiya, T.; Iwata, T.; Kishikawa, T.; Koike, K. The biological role of metabolic reprogramming in pancreatic cancer. Medcomm 2020, 1, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Hayashi, H.; Matsumura, K.; Uemura, N.; Shiraishi, Y.; Sato, H.; Baba, H. Biological and Clinical Impacts of Glucose Metabolism in Pancreatic Ductal Adenocarcinoma. Cancers 2023, 15, 498. [Google Scholar] [CrossRef] [PubMed]
- Son, J.; Lyssiotis, C.A.; Ying, H.; Wang, X.; Hua, S.; Ligorio, M.; Perera, R.M.; Ferrone, C.R.; Mullarky, E.; Shyh-Chang, N.; et al. Glutamine supports pancreatic cancer growth through a KRAS-regulated metabolic pathway. Nature 2013, 496, 101–105, Erratum in Nature 2013, 499, 504. [Google Scholar] [CrossRef] [PubMed]
- Efeyan, A.; Comb, W.C.; Sabatini, D.M. Nutrient-sensing mechanisms and pathways. Nature 2015, 517, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Xu, R.; Song, J.; Ruze, R.; Chen, Y.; Wang, C.; Xu, Q. Lipid metabolism in pancreatic cancer: Emerging roles and potential targets. Cancer Commun. 2022, 42, 1234–1256. [Google Scholar] [CrossRef] [PubMed]
- Patra, K.C.; Kato, Y.; Mizukami, Y.; Widholz, S.; Boukhali, M.; Revenco, I.; Grossman, E.A.; Ji, F.; Sadreyev, R.I.; Liss, A.S.; et al. Mutant GNAS drives pancreatic tumourigenesis by inducing PKA-mediated SIK suppression and reprogramming lipid metabolism. Nature 2018, 20, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Dai, E.; Han, L.; Liu, J.; Xie, Y.; Zeh, H.J.; Kang, R.; Bai, L.; Tang, D. Ferroptotic damage promotes pancreatic tumorigenesis through a TMEM173/STING-dependent DNA sensor pathway. Nat. Commun. 2020, 11, 6339. [Google Scholar] [CrossRef]
- Carrer, A.; Trefely, S.; Zhao, S.; Campbell, S.L.; Norgard, R.J.; Schultz, K.C.; Sidoli, S.; Parris, J.L.D.; Affronti, H.C.; Sivanand, S.; et al. Acetyl-CoA Metabolism Supports Multistep Pancreatic Tumorigenesis. Cancer Discov. 2019, 9, 416–435. [Google Scholar] [CrossRef]
- Bian, Y.; Yu, Y.; Wang, S.; Li, L. Up-regulation of fatty acid synthase induced by EGFR/ERK activation promotes tumor growth in pancreatic cancer. Biochem. Biophys. Res. Commun. 2015, 463, 612–617. [Google Scholar] [CrossRef]
- Nishi, K.; Suzuki, M.; Yamamoto, N.; Matsumoto, A.; Iwase, Y.; Yamasaki, K.; Otagiri, M.; Yumita, N. Glutamine Deprivation Enhances Acetyl-CoA Carboxylase Inhibitor-induced Death of Human Pancreatic Cancer Cells. Anticancer. Res. 2018, 38, 6683–6689. [Google Scholar] [CrossRef]
- Halbrook, C.J.; Lyssiotis, C.A.; di Magliano, M.P.; Maitra, A. Pancreatic cancer: Advances and challenges. Cell 2023, 186, 1729–1754. [Google Scholar] [CrossRef] [PubMed]
- Daemen, A.; Peterson, D.; Sahu, N.; McCord, R.; Du, X.; Liu, B.; Kowanetz, K.; Hong, R.; Moffat, J.; Gao, M.; et al. Metabolite profiling stratifies pancreatic ductal adenocarcinomas into subtypes with distinct sensitivities to metabolic inhibitors. Proc. Natl. Acad. Sci. USA 2015, 112, E4410–E4417. [Google Scholar] [CrossRef] [PubMed]
- Daemen, A.; Liu, B.; Song, K.; Kwong, M.; Gao, M.; Hong, R.; Nannini, M.; Peterson, D.; Liederer, B.M.; de la Cruz, C.; et al. Pan-Cancer Metabolic Signature Predicts Co-Dependency on Glutaminase and De Novo Glutathione Synthesis Linked to a High-Mesenchymal Cell State. Cell Metab. 2018, 28, 383–399.e9. [Google Scholar] [CrossRef]
- El Kaoutari, A.; Fraunhoffer, N.A.; Hoare, O.; Teyssedou, C.; Soubeyran, P.; Gayet, O.; Roques, J.; Lomberk, G.; Urrutia, R.; Dusetti, N.; et al. Metabolomic profiling of pancreatic adenocarcinoma reveals key features driving clinical outcome and drug resistance. EBioMedicine 2021, 66, 103332. [Google Scholar] [CrossRef]
- Yu, M.; Zhou, Q.; Zhou, Y.; Fu, Z.; Tan, L.; Ye, X.; Zeng, B.; Gao, W.; Zhou, J.; Liu, Y.; et al. Metabolic Phenotypes in Pancreatic Cancer. PLoS ONE 2015, 10, e0115153. [Google Scholar] [CrossRef]
- Sugimoto, M.; Wong, D.T.; Hirayama, A.; Soga, T.; Tomita, M. Capillary electrophoresis mass spectrometry-based saliva metabolomics identified oral, breast and pancreatic cancer-specific profiles. Metabolomics 2009, 6, 78–95. [Google Scholar] [CrossRef] [PubMed]
- Mehta, K.Y.; Wu, H.-J.; Menon, S.S.; Fallah, Y.; Zhong, X.; Rizk, N.; Unger, K.; Mapstone, M.; Fiandaca, M.S.; Federoff, H.J.; et al. Metabolomic biomarkers of pancreatic cancer: A meta-analysis study. Oncotarget 2017, 8, 68899–68915. [Google Scholar] [CrossRef]
- Luo, X.; Liu, J.; Wang, H.; Lu, H. Metabolomics identified new biomarkers for the precise diagnosis of pancreatic cancer and associated tissue metastasis. Pharmacol. Res. 2020, 156, 104805. [Google Scholar] [CrossRef]
- Mayerle, J.; Kalthoff, H.; Reszka, R.; Kamlage, B.; Peter, E.; Schniewind, B.; Maldonado, S.G.; Pilarsky, C.; Heidecke, C.-D.; Schatz, P.; et al. Metabolic biomarker signature to differentiate pancreatic ductal adenocarcinoma from chronic pancreatitis. Gut 2017, 67, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, U.M.; Oehrle, B.; Sirtl, S.; Alnatsha, A.; Goni, E.; Regel, I.; Beyer, G.; Vornhülz, M.; Vielhauer, J.; Chromik, A.; et al. Independent Validation and Assay Standardization of Improved Metabolic Biomarker Signature to Differentiate Pancreatic Ductal Adenocarcinoma from Chronic Pancreatitis. Gastroenterology 2022, 163, 1407–1422. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, U.M.; Alnatsha, A.; Li, Q.; Oehrle, B.; Weiss, F.-U.; Sendler, M.; Distler, M.; Uhl, W.; Fahlbusch, T.; Goni, E.; et al. Plasma Metabolome Profiling Identifies Metabolic Subtypes of Pancreatic Ductal Adenocarcinoma. Cells 2021, 10, 1821. [Google Scholar] [CrossRef] [PubMed]
- Goossens, N.; Nakagawa, S.; Sun, X.; Hoshida, Y. Cancer biomarker discovery and validation. Transl. Cancer Res. 2015, 4, 256–269. [Google Scholar] [CrossRef] [PubMed]
- Hanash, S. Disease proteomics. Nature 2003, 422, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Aslam, B.; Basit, M.; Nisar, M.A.; Khurshid, M.; Rasool, M.H. Proteomics: Technologies and Their Applications. J. Chromatogr. Sci. 2017, 55, 182–196. [Google Scholar] [CrossRef] [PubMed]
- Papapanagiotou, A.; Sgourakis, G.; Karkoulias, K.; Raptis, D.; Parkin, E.; Brotzakis, P.; Panchal, S.; Papavassiliou, A.G. Osteonectin as a screening marker for pancreatic cancer: A prospective study. J. Int. Med. Res. 2018, 46, 2769–2779. [Google Scholar] [CrossRef]
- Jin, H.; Liu, P.; Wu, Y.; Meng, X.; Wu, M.; Han, J.; Tan, X. Exosomal zinc transporter ZIP4 promotes cancer growth and is a novel diagnostic biomarker for pancreatic cancer. Cancer Sci. 2018, 109, 2946–2956. [Google Scholar] [CrossRef]
- Saukkonen, K.; Hagström, J.; Mustonen, H.; Juuti, A.; Nordling, S.; Kallio, P.; Alitalo, K.; Seppänen, H.; Haglund, C. PROX1 and β-catenin are prognostic markers in pancreatic ductal adenocarcinoma. BMC Cancer 2016, 16, 472. [Google Scholar] [CrossRef]
- Mohamed, A.A.; Soliman, H.; Ismail, M.; Ziada, D.; Farid, T.M.; Aref, A.M.; Al Daly, M.E.; Elmageed, Z.Y.A. Evaluation of circulating ADH and MIC-1 as diagnostic markers in Egyptian patients with pancreatic cancer. Pancreatology 2015, 15, 34–39. [Google Scholar] [CrossRef]
- Capello, M.; Bantis, L.E.; Scelo, G.; Zhao, Y.; Li, P.; Dhillon, D.S.; Patel, N.J.; Kundnani, D.L.; Wang, H.; Abbruzzese, J.L.; et al. Sequential Validation of Blood-Based Protein Biomarker Candidates for Early-Stage Pancreatic Cancer. JNCI J. Natl. Cancer Inst. 2016, 109, djw266. [Google Scholar] [CrossRef] [PubMed]
- Yoneyama, T.; Ohtsuki, S.; Honda, K.; Kobayashi, M.; Iwasaki, M.; Uchida, Y.; Okusaka, T.; Nakamori, S.; Shimahara, M.; Ueno, T.; et al. Identification of IGFBP2 and IGFBP3 As Compensatory Biomarkers for CA19-9 in Early-Stage Pancreatic Cancer Using a Combination of Antibody-Based and LC-MS/MS-Based Proteomics. PLoS ONE 2016, 11, e0161009. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.T.; Zahn, J.M.; Horecka, J.; Kunz, P.L.; Ford, J.M.; Fisher, G.A.; Le, Q.T.; Chang, D.T.; Ji, H.; Koong, A.C. Identification of a biomarker panel using a multiplex proximity ligation assay improves accuracy of pancreatic cancer diagnosis. J. Transl. Med. 2009, 7, 105. [Google Scholar] [CrossRef] [PubMed]
- Brand, R.E.; Nolen, B.M.; Zeh, H.J.; Allen, P.J.; Eloubeidi, M.A.; Goldberg, M.; Elton, E.; Arnoletti, J.P.; Christein, J.D.; Vickers, S.M.; et al. Serum Biomarker Panels for the Detection of Pancreatic Cancer. Clin. Cancer Res. 2011, 17, 805–816. [Google Scholar] [CrossRef] [PubMed]
- McKinney, K.Q.; Lee, Y.-Y.; Choi, H.-S.; Groseclose, G.; Iannitti, D.A.; Martinie, J.B.; Russo, M.W.; Lundgren, D.H.; Han, D.K.; Bonkovsky, H.L.; et al. Discovery of putative pancreatic cancer biomarkers using subcellular proteomics. J. Proteom. 2010, 74, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Ehmann, M.; Felix, K.; Hartmann, D.; Schnölzer, M.; Nees, M.; Vorderwülbecke, S.; Bogumil, R.; Büchler, M.W.; Friess, H. Identification of Potential Markers for the Detection of Pancreatic Cancer Through Comparative Serum Protein Expression Profiling. Pancreas 2007, 34, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, A.; Vitale, F.; Quero, G.; Paratore, M.; Fiorillo, C.; Negri, M.; Carlino, A.; Inzani, F.; Gasbarrini, A.; Alfieri, S.; et al. Immunohistochemical Evaluation of the Expression of Specific Membrane Antigens in Patients with Pancreatic Ductal Adenocarcinoma. Cancers 2023, 15, 4586. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.; Clauser, K.R.; Öhlund, D.; Rickelt, S.; Huang, Y.; Gupta, M.; Mani, D.R.; Carr, S.A.; Tuveson, D.A.; Hynes, R.O. Proteomic analyses of ECM during pancreatic ductal adenocarcinoma progression reveal different contributions by tumor and stromal cells. Proc. Natl. Acad. Sci. USA 2019, 116, 19609–19618. [Google Scholar] [CrossRef]
- Zhou, Q.; Andersson, R.; Hu, D.; Bauden, M.; Kristl, T.; Sasor, A.; Pawłowski, K.; Pla, I.; Hilmersson, K.S.; Zhou, M.; et al. Quantitative proteomics identifies brain acid soluble protein 1 (BASP1) as a prognostic biomarker candidate in pancreatic cancer tissue. EBioMedicine 2019, 43, 282–294. [Google Scholar] [CrossRef]
- Fong, D.; Moser, P.; Krammel, C.; Gostner, J.M.; Margreiter, R.; Mitterer, M.; Gastl, G.; Spizzo, G. High expression of TROP2 correlates with poor prognosis in pancreatic cancer. Br. J. Cancer 2008, 99, 1290–1295. [Google Scholar] [CrossRef]
- Zong, M.; Meng, M.; Li, L. Low Expression of TBX4 Predicts Poor Prognosis in Patients with Stage II Pancreatic Ductal Adenocarcinoma. Int. J. Mol. Sci. 2011, 12, 4953–4963. [Google Scholar] [CrossRef]
- Schäfer, C.; Seeliger, H.; Bader, D.C.; Assmann, G.; Buchner, D.; Guo, Y.; Ziesch, A.; Palagyi, A.; Ochs, S.; Laubender, R.P.; et al. Heat shock protein 27 as a prognostic and predictive biomarker in pancreatic ductal adenocarcinoma. J. Cell. Mol. Med. 2011, 16, 1776–1791. [Google Scholar] [CrossRef] [PubMed]
- Maréchal, R.; Mackey, J.R.; Lai, R.; Demetter, P.; Peeters, M.; Polus, M.; Cass, C.E.; Salmon, I.; Devière, J.; Van Laethem, J. Deoxycitidine kinase is associated with prolonged survival after adjuvant gemcitabine for resected pancreatic adenocarcinoma. Cancer 2010, 116, 5200–5206. [Google Scholar] [CrossRef] [PubMed]
- Mann, C.D.; Bastianpillai, C.; Neal, C.P.; Masood, M.M.; Jones, D.J.L.; Teichert, F.; Singh, R.; Karpova, E.; Berry, D.P.; Manson, M.M. Notch3 and Hey-1 as Prognostic Biomarkers in Pancreatic Adenocarcinoma. PLoS ONE 2012, 7, e51119. [Google Scholar] [CrossRef]
- Khushman, M.; Bhardwaj, A.; Patel, G.K.; Laurini, J.A.; Roveda, K.; Tan, M.C.; Patton, M.C.B.; Singh, S.; Taylor, W.; Singh, A.P. Exosomal Markers (CD63 and CD9) Expression Pattern Using Immunohistochemistry in Resected Malignant and Nonmalignant Pancreatic Specimens. Pancreas 2017, 46, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Schultz, N.A.; Christensen, I.J.; Werner, J.; Giese, N.; Jensen, B.V.; Larsen, O.; Bjerregaard, J.K.; Pfeiffer, P.; Calatayud, D.; Nielsen, S.E.; et al. Diagnostic and Prognostic Impact of Circulating YKL-40, IL-6, and CA 19.9 in Patients with Pancreatic Cancer. PLoS ONE 2013, 8, e67059. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Kong, L.; Jin, H.; Wu, Y.; Tan, X.; Song, B. Differential secretome of pancreatic cancer cells in serum-containing conditioned medium reveals CCT8 as a new biomarker of pancreatic cancer invasion and metastasis. Cancer Cell Int. 2019, 19, 262. [Google Scholar] [CrossRef] [PubMed]
- McCaffery, I.; Tudor, Y.; Deng, H.; Tang, R.; Suzuki, S.; Badola, S.; Kindler, H.L.; Fuchs, C.S.; Loh, E.; Patterson, S.D.; et al. Putative Predictive Biomarkers of Survival in Patients with Metastatic Pancreatic Adenocarcinoma Treated with Gemcitabine and Ganitumab, an IGF1R Inhibitor. Clin. Cancer Res. 2013, 19, 4282–4289. [Google Scholar] [CrossRef] [PubMed]
- Hosein, A.N.; Dougan, S.K.; Aguirre, A.J.; Maitra, A. Translational advances in pancreatic ductal adenocarcinoma therapy. Nat. Cancer 2022, 3, 272–286. [Google Scholar] [CrossRef]
- O’Kane, G.M.; Lowery, M.A. Moving the Needle on Precision Medicine in Pancreatic Cancer. J. Clin. Oncol. 2022, 40, 2693–2705. [Google Scholar] [CrossRef]
- Waddell, N.; Pajic, M.; Patch, A.-M.; Chang, D.K.; Kassahn, K.S.; Bailey, P.; Johns, A.L.; Miller, D.; Nones, K.; Quek, K.; et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature 2015, 518, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Philip, P.A.; Azar, I.; Xiu, J.; Hall, M.J.; Hendifar, A.E.; Lou, E.; Hwang, J.J.; Gong, J.; Feldman, R.; Ellis, M.; et al. Molecular Characterization of KRAS Wild-type Tumors in Patients with Pancreatic Adenocarcinoma. Clin. Cancer Res. 2022, 28, 2704–2714. [Google Scholar] [CrossRef] [PubMed]
- Varghese, A.M.; Singh, I.; Singh, R.; Kunte, S.; Chou, J.F.; Capanu, M.; Wong, W.; Lowery, M.A.; Stadler, Z.K.; Salo-Mullen, E.; et al. Early-Onset Pancreas Cancer: Clinical Descriptors, Genomics, and Outcomes. JNCI J. Natl. Cancer Inst. 2021, 113, 1194–1202. [Google Scholar] [CrossRef]
- Ben-Aharon, I.; Elkabets, M.; Pelossof, R.; Yu, K.H.; Iacubuzio-Donahue, C.A.; Leach, S.D.; Lowery, M.A.; Goodman, K.A.; O’Reilly, E.M. Genomic Landscape of Pancreatic Adenocarcinoma in Younger versus Older Patients: Does Age Matter? Clin. Cancer Res. 2019, 25, 2185–2193. [Google Scholar] [CrossRef]
- Ala, M. Target c-Myc to treat pancreatic cancer. Cancer Biol. Ther. 2022, 23, 34–50. [Google Scholar] [CrossRef]
- Wang, Q.; Li, Z.; Zhou, S.; Li, Z.; Huang, X.; He, Y.; Zhang, Y.; Zhao, X.; Tang, Y.; Xu, M. NCAPG2 could be an immunological and prognostic biomarker: From pan-cancer analysis to pancreatic cancer validation. Front. Immunol. 2023, 14, 1097403. [Google Scholar] [CrossRef]
- Golan, T.; Hammel, P.; Reni, M.; Van Cutsem, E.; Macarulla, T.; Hall, M.J.; Park, J.-O.; Hochhauser, D.; Arnold, D.; Oh, D.-Y.; et al. Maintenance Olaparib for Germline BRCA-Mutated Metastatic Pancreatic Cancer. N. Engl. J. Med. 2019, 381, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Pishvaian, M.J.; Blais, E.M.; Brody, J.R.; Lyons, E.; DeArbeloa, P.; Hendifar, A.; Mikhail, S.; Chung, V.; Sahai, V.; Sohal, D.P.S.; et al. Overall survival in patients with pancreatic cancer receiving matched therapies following molecular profiling: A retrospective analysis of the Know Your Tumor registry trial. Lancet Oncol. 2020, 21, 508–518. [Google Scholar] [CrossRef]
- Hallin, J.; Bowcut, V.; Calinisan, A.; Briere, D.M.; Hargis, L.; Engstrom, L.D.; Laguer, J.; Medwid, J.; Vanderpool, D.; Lifset, E.; et al. Anti-tumor efficacy of a potent and selective non-covalent KRASG12D inhibitor. Nat. Med. 2022, 28, 2171–2182. [Google Scholar] [CrossRef]
- Strickler, J.H.; Satake, H.; George, T.J.; Yaeger, R.; Hollebecque, A.; Garrido-Laguna, I.; Schuler, M.; Burns, T.F.; Coveler, A.L.; Falchook, G.S.; et al. Sotorasib in KRAS p.G12C–Mutated Advanced Pancreatic Cancer. New Engl. J. Med. 2023, 388, 33–43. [Google Scholar] [CrossRef]
- Bekaii-Saab, T.S.; Yaeger, R.; Spira, A.I.; Pelster, M.S.; Sabari, J.K.; Hafez, N.; Barve, M.; Velastegui, K.; Yan, X.; Shetty, A.; et al. Adagrasib in Advanced Solid Tumors Harboring a KRASG12C Mutation. J. Clin. Oncol. 2023, 41, 4097–4106. [Google Scholar] [CrossRef] [PubMed]
- Garcia, E.P.; Minkovsky, A.; Jia, Y.; Ducar, M.D.; Shivdasani, P.; Gong, X.; Ligon, A.H.; Sholl, L.M.; Kuo, F.C.; MacConaill, L.E.; et al. Validation of OncoPanel: A Targeted Next-Generation Sequencing Assay for the Detection of Somatic Variants in Cancer. Arch. Pathol. Lab. Med. 2017, 141, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Anastasiadou, E.; Jacob, L.S.; Slack, F.J. Non-coding RNA networks in cancer. Nat. Rev. Cancer 2018, 18, 5–18. [Google Scholar] [CrossRef]
- Cheng, L.; Sharples, R.A.; Scicluna, B.J.; Hill, A.F. Exosomes provide a protective and enriched source of miRNA for biomarker profiling compared to intracellular and cell-free blood. J. Extracell. Vesicles 2014, 3, 23743. [Google Scholar] [CrossRef]
- Reese, M.; Flammang, I.; Yang, Z.; Dhayat, S.A. Potential of Exosomal microRNA-200b as Liquid Biopsy Marker in Pancreatic Ductal Adenocarcinoma. Cancers 2020, 12, 197. [Google Scholar] [CrossRef]
- Li, A.; Omura, N.; Hong, S.-M.; Vincent, A.; Walter, K.; Griffith, M.; Borges, M.; Goggins, M. Pancreatic Cancers Epigenetically Silence SIP1 and Hypomethylate and Overexpress miR-200a/200b in Association with Elevated Circulating miR-200a and miR-200b Levels. Cancer Res. 2010, 70, 5226–5237. [Google Scholar] [CrossRef]
- Pu, X.; Ding, G.; Wu, M.; Zhou, S.; Jia, S.; Cao, L. Elevated expression of exosomal microRNA-21 as a potential biomarker for the early diagnosis of pancreatic cancer using a tethered cationic lipoplex nanoparticle biochip. Oncol. Lett. 2020, 19, 2062–2070. [Google Scholar] [CrossRef] [PubMed]
- Que, R.; Ding, G.; Chen, J.; Cao, L. Analysis of serum exosomal microRNAs and clinicopathologic features of patients with pancreatic adenocarcinoma. World J. Surg. Oncol. 2013, 11, 219. [Google Scholar] [CrossRef]
- Bärthel, S.; Falcomatà, C.; Rad, R.; Theis, F.J.; Saur, D. Single-cell profiling to explore pancreatic cancer heterogeneity, plasticity and response to therapy. Nat. Cancer 2023, 4, 454–467. [Google Scholar] [CrossRef]
- Moncada, R.; Barkley, D.; Wagner, F.; Chiodin, M.; Devlin, J.C.; Baron, M.; Hajdu, C.H.; Simeone, D.M.; Yanai, I. Integrating microarray-based spatial transcriptomics and single-cell RNA-seq reveals tissue architecture in pancreatic ductal adenocarcinomas. Nat. Biotechnol. 2020, 38, 333–342. [Google Scholar] [CrossRef]
- Raghavan, S.; Winter, P.S.; Navia, A.W.; Williams, H.L.; DenAdel, A.; Lowder, K.E.; Galvez-Reyes, J.; Kalekar, R.L.; Mulugeta, N.; Kapner, K.S.; et al. Microenvironment drives cell state, plasticity, and drug response in pancreatic cancer. Cell 2021, 184, 6119–6137.e26. [Google Scholar] [CrossRef]
- Hwang, W.L.; Jagadeesh, K.A.; Guo, J.A.; Hoffman, H.I.; Yadollahpour, P.; Reeves, J.W.; Mohan, R.; Drokhlyansky, E.; Van Wittenberghe, N.; Ashenberg, O.; et al. Single-nucleus and spatial transcriptome profiling of pancreatic cancer identifies multicellular dynamics associated with neoadjuvant treatment. Nat. Genet. 2022, 54, 1178–1191. [Google Scholar] [CrossRef]
- Zhou, D.C.; Jayasinghe, R.G.; Chen, S.; Herndon, J.M.; Iglesia, M.D.; Navale, P.; Wendl, M.C.; Caravan, W.; Sato, K.; Storrs, E.; et al. Spatially restricted drivers and transitional cell populations cooperate with the microenvironment in untreated and chemo-resistant pancreatic cancer. Nat. Genet. 2022, 54, 1390–1405. [Google Scholar] [CrossRef] [PubMed]
- Falcomatà, C.; Bärthel, S.; Widholz, S.A.; Schneeweis, C.; Montero, J.J.; Toska, A.; Mir, J.; Kaltenbacher, T.; Heetmeyer, J.; Swietlik, J.J.; et al. Selective multi-kinase inhibition sensitizes mesenchymal pancreatic cancer to immune checkpoint blockade by remodeling the tumor microenvironment. Nat. Cancer 2022, 3, 318–336. [Google Scholar] [CrossRef] [PubMed]
- Limkin, E.J.; Sun, R.; Dercle, L.; Zacharaki, E.I.; Robert, C.; Reuzé, S.; Schernberg, A.; Paragios, N.; Deutsch, E.; Ferté, C. Promises and challenges for the implementation of computational medical imaging (radiomics) in oncology. Ann. Oncol. 2017, 28, 1191–1206. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewski, M.R.; Gillies, R.J. The Biological Meaning of Radiomic Features. Radiology 2021, 299, E256. [Google Scholar] [CrossRef] [PubMed]
- Marti-Bonmati, L.; Cerdá-Alberich, L.; Pérez-Girbés, A.; Beveridge, R.D.; Orón, E.M.; Rojas, J.P.; Alberich-Bayarri, A. Pancreatic cancer, radiomics and artificial intelligence. Br. J. Radiol. 2022, 95, 20220072. [Google Scholar] [CrossRef] [PubMed]
- Fusco, R.; Granata, V.; Petrillo, A. Introduction to Special Issue of Radiology and Imaging of Cancer. Cancers 2020, 12, 2665. [Google Scholar] [CrossRef] [PubMed]
- Alberich-Bayarri, Á.; Hernández-Navarro, R.; Ruiz-Martínez, E.; García-Castro, F.; García-Juan, D.; Martí-Bonmatí, L. Development of imaging biomarkers and generation of big data. La Radiol. medica 2017, 122, 444–448. [Google Scholar] [CrossRef] [PubMed]
- E, L.; Xu, Y.; Wu, Z.; Li, L.; Zhang, N.; Yang, H.; Schwartz, L.H.; Lu, L.; Zhao, B.D. Differentiation of Focal-Type Autoimmune Pancreatitis From Pancreatic Ductal Adenocarcinoma Using Radiomics Based on Multiphasic Computed Tomography. J. Comput. Assist. Tomogr. 2020, 44, 511–518. [Google Scholar] [CrossRef]
- Kaissis, G.; Ziegelmayer, S.; Lohöfer, F.; Steiger, K.; Algül, H.; Muckenhuber, A.; Yen, H.-Y.; Rummeny, E.; Friess, H.; Schmid, R.; et al. A machine learning algorithm predicts molecular subtypes in pancreatic ductal adenocarcinoma with differential response to gemcitabine-based versus FOLFIRINOX chemotherapy. PLoS ONE 2019, 14, e0218642. [Google Scholar] [CrossRef] [PubMed]
- Kaissis, G.A.; Ziegelmayer, S.; Lohöfer, F.K.; Harder, F.N.; Jungmann, F.; Sasse, D.; Muckenhuber, A.; Yen, H.-Y.; Steiger, K.; Siveke, J.; et al. Image-Based Molecular Phenotyping of Pancreatic Ductal Adenocarcinoma. J. Clin. Med. 2020, 9, 724. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Grassi, R.; Fusco, R.; Galdiero, R.; Setola, S.; Palaia, R.; Belli, A.; Silvestro, L.; Cozzi, D.; Brunese, L.; et al. Pancreatic cancer detection and characterization: State of the art and radiomics. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 3684–3699. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Chu, L.; Hruban, R.; Vogelstein, B.; Kinzler, K.; Yuille, A.; Fouladi, D.; Shayesteh, S.; Ghandili, S.; Wolfgang, C.; et al. Differentiating autoimmune pancreatitis from pancreatic ductal adenocarcinoma with CT radiomics features. Diagn. Interv. Imaging 2020, 101, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.C.; Park, S.; Kawamoto, S.; Fouladi, D.F.; Shayesteh, S.; Zinreich, E.S.; Graves, J.S.; Horton, K.M.; Hruban, R.H.; Yuille, A.L.; et al. Utility of CT Radiomics Features in Differentiation of Pancreatic Ductal Adenocarcinoma From Normal Pancreatic Tissue. Am. J. Roentgenol. 2019, 213, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Patra, A.; Khasawneh, H.; Korfiatis, P.; Rajamohan, N.; Suman, G.; Majumder, S.; Panda, A.; Johnson, M.P.; Larson, N.B.; et al. Radiomics-based Machine-learning Models Can Detect Pancreatic Cancer on Prediagnostic Computed Tomography Scans at a Substantial Lead Time Before Clinical Diagnosis. Gastroenterology 2022, 163, 1435–1446.e3. [Google Scholar] [CrossRef] [PubMed]
- Săftoiu, A.; Vilmann, P.; Gorunescu, F.; Gheonea, D.I.; Gorunescu, M.; Ciurea, T.; Popescu, G.L.; Iordache, A.; Hassan, H.; Iordache, S. Neural network analysis of dynamic sequences of EUS elastography used for the differential diagnosis of chronic pancreatitis and pancreatic cancer. Gastrointest. Endosc. 2008, 68, 1086–1094. [Google Scholar] [CrossRef] [PubMed]
- Bian, Y.; Guo, S.; Jiang, H.; Gao, S.; Shao, C.; Cao, K.; Fang, X.; Li, J.; Wang, L.; Hua, W.; et al. Relationship Between Radiomics and Risk of Lymph Node Metastasis in Pancreatic Ductal Adenocarcinoma. Pancreas 2019, 48, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Gu, Q.; Hu, X.; Tan, X.; Liu, J.; Xie, A.; Huang, F. Applying a radiomics-based strategy to preoperatively predict lymph node metastasis in the resectable pancreatic ductal adenocarcinoma. J. X-Ray Sci. Technol. 2020, 28, 1113–1121. [Google Scholar] [CrossRef]
- Zhang, W.; Cai, W.; He, B.; Xiang, N.; Fang, C.; Jia, F. A radiomics-based formula for the preoperative prediction of postoperative pancreatic fistula in patients with pancreaticoduodenectomy. Cancer Manag. Res. 2018, 10, 6469–6478. [Google Scholar] [CrossRef]
- Li, J.; Shi, Z.; Liu, F.; Fang, X.; Cao, K.; Meng, Y.; Zhang, H.; Yu, J.; Feng, X.; Li, Q.; et al. XGBoost Classifier Based on Computed Tomography Radiomics for Prediction of Tumor-Infiltrating CD8+ T-Cells in Patients With Pancreatic Ductal Adenocarcinoma. Front. Oncol. 2021, 11, 671333. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.D.; Baimas-George, M.R.; Murphy, K.J.; Pickens, R.C.; Iannitti, D.A.; Martinie, J.B.; Baker, E.H.; Vrochides, D.; Ocuin, L.M. Pure and Hybrid Deep Learning Models can Predict Pathologic Tumor Response to Neoadjuvant Therapy in Pancreatic Adenocarcinoma: A Pilot Study. Am. Surg. 2020, 87, 1901–1909. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.-H.; Cheng, Y.-J.; Jin, Z.-Y.; Xue, H.-D. Unresectable pancreatic ductal adenocarcinoma: Role of CT quantitative imaging biomarkers for predicting outcomes of patients treated with chemotherapy. Eur. J. Radiol. 2019, 113, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Parr, E.; Du, Q.; Zhang, C.; Lin, C.; Kamal, A.; McAlister, J.; Liang, X.; Bavitz, K.; Rux, G.; Hollingsworth, M.; et al. Radiomics-Based Outcome Prediction for Pancreatic Cancer Following Stereotactic Body Radiotherapy. Cancers 2020, 12, 1051. [Google Scholar] [CrossRef] [PubMed]
- Cozzi, L.; Comito, T.; Fogliata, A.; Franzese, C.; Franceschini, D.; Bonifacio, C.; Tozzi, A.; Di Brina, L.; Clerici, E.; Tomatis, S.; et al. Computed tomography based radiomic signature as predictive of survival and local control after stereotactic body radiation therapy in pancreatic carcinoma. PLoS ONE 2019, 14, e0210758. [Google Scholar] [CrossRef] [PubMed]
- Attiyeh, M.A.; Chakraborty, J.; Doussot, A.; Langdon-Embry, L.; Mainarich, S.; Gönen, M.; Balachandran, V.P.; D’angelica, M.I.; DeMatteo, R.P.; Jarnagin, W.R.; et al. Survival Prediction in Pancreatic Ductal Adenocarcinoma by Quantitative Computed Tomography Image Analysis. Ann. Surg. Oncol. 2018, 25, 1034–1042. [Google Scholar] [CrossRef] [PubMed]
- Wei, R.; Lin, K.; Yan, W.; Guo, Y.; Wang, Y.; Li, J.; Zhu, J. Computer-Aided Diagnosis of Pancreas Serous Cystic Neoplasms: A Radiomics Method on Preoperative MDCT Images. Technol. Cancer Res. Treat. 2019, 18. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.-P.; Liu, S.-Y.; Han, Y.-J.; Li, L.-M.; Liang, P.; Gao, J.-B. Development of CT-Based Imaging Signature for Preoperative Prediction of Invasive Behavior in Pancreatic Solid Pseudopapillary Neoplasm. Front. Oncol. 2021, 11, 677814. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.D.; Lyman, W.B.; Passeri, M.J.; Murphy, K.J.; Sarantou, J.P.; Iannitti, D.A.; Martinie, J.B.; Vrochides, D.; Baker, E.H. Use of Artificial Intelligence Deep Learning to Determine the Malignant Potential of Pancreatic Cystic Neoplasms With Preoperative Computed Tomography Imaging. Am. Surg. 2021, 87, 602–607. [Google Scholar] [CrossRef]
- Corral, J.E.; Hussein, S.; Kandel, P.; Bolan, C.W.; Bagci, U.; Wallace, M.B. Deep Learning to Classify Intraductal Papillary Mucinous Neoplasms Using Magnetic Resonance Imaging. Pancreas 2019, 48, 805–810. [Google Scholar] [CrossRef]
- Kuwahara, T.; Hara, K.; Mizuno, N.; Okuno, N.; Matsumoto, S.; Obata, M.; Kurita, Y.; Koda, H.; Toriyama, K.; Onishi, S.; et al. Usefulness of Deep Learning Analysis for the Diagnosis of Malignancy in Intraductal Papillary Mucinous Neoplasms of the Pancreas. Clin. Transl. Gastroenterol. 2019, 10, e00045-8. [Google Scholar] [CrossRef]
- Koay, E.J.; Lee, Y.; Cristini, V.; Lowengrub, J.S.; Kang, Y.; Lucas, F.A.S.; Hobbs, B.P.; Ye, R.; Elganainy, D.; Almahariq, M.; et al. A Visually Apparent and Quantifiable CT Imaging Feature Identifies Biophysical Subtypes of Pancreatic Ductal Adenocarcinoma. Clin. Cancer Res. 2018, 24, 5883–5894. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, J.; Langdon-Embry, L.; Cunanan, K.M.; Escalon, J.G.; Allen, P.J.; Lowery, M.A.; O’reilly, E.M.; Gönen, M.; Do, R.G.; Simpson, A.L. Preliminary study of tumor heterogeneity in imaging predicts two year survival in pancreatic cancer patients. PLoS ONE 2017, 12, e0188022. [Google Scholar] [CrossRef] [PubMed]
- Cassinotto, C.; Chong, J.; Zogopoulos, G.; Reinhold, C.; Chiche, L.; Lafourcade, J.-P.; Cuggia, A.; Terrebonne, E.; Dohan, A.; Gallix, B. Resectable pancreatic adenocarcinoma: Role of CT quantitative imaging biomarkers for predicting pathology and patient outcomes. Eur. J. Radiol. 2017, 90, 152–158. [Google Scholar] [CrossRef]
- Iwatate, Y.; Hoshino, I.; Yokota, H.; Ishige, F.; Itami, M.; Mori, Y.; Chiba, S.; Arimitsu, H.; Yanagibashi, H.; Nagase, H.; et al. Radiogenomics for predicting p53 status, PD-L1 expression, and prognosis with machine learning in pancreatic cancer. Br. J. Cancer 2020, 123, 1253–1261. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.; Wang, F.; Lei, Z.; Li, J.; Ma, M.; Yan, Y.; Zhang, W.; Chen, X.; Xu, B.; Hu, T. An Integrated Multi-Omics Analysis Identifying Immune Subtypes of Pancreatic Cancer. Int. J. Mol. Sci. 2023, 25, 142. [Google Scholar] [CrossRef]
- Yousuf, S.; Qiu, M.; von Voithenberg, L.V.; Hulkkonen, J.; Macinkovic, I.; Schulz, A.R.; Hartmann, D.; Mueller, F.; Mijatovic, M.; Ibberson, D.; et al. Spatially Resolved Multi-Omics Single-Cell Analyses Inform Mechanisms of Immune Dysfunction in Pancreatic Cancer. Gastroenterology 2023, 165, 891–908.e14. [Google Scholar] [CrossRef]
- Zhang, J.; Song, J.; Tang, S.; Zhao, Y.; Wang, L.; Luo, Y.; Tang, J.; Ji, Y.; Wang, X.; Li, T.; et al. Multi-omics analysis reveals the chemoresistance mechanism of proliferating tissue-resident macrophages in PDAC via metabolic adaptation. Cell Rep. 2023, 42, 112620. [Google Scholar] [CrossRef]
- Li, X.; Du, Y.; Jiang, W.; Dong, S.; Li, W.; Tang, H.; Yi, J.; Zhou, W.; Zhang, H. Integrated transcriptomics, proteomics and metabolomics-based analysis uncover TAM2-associated glycolysis and pyruvate metabolic remodeling in pancreatic cancer. Front. Immunol. 2023, 14, 1170223. [Google Scholar] [CrossRef]
- Zhao, Y.; Tang, J.; Jiang, K.; Liu, S.-Y.; Aicher, A.; Heeschen, C. Liquid biopsy in pancreatic cancer—Current perspective and future outlook. Biochim. Biophys. Acta (BBA) Rev. Cancer 2023, 1878, 188868. [Google Scholar] [CrossRef]
- Pang, T.C.; Po, J.W.; Becker, T.M.; Goldstein, D.; Pirola, R.C.; Wilson, J.S.; Apte, M.V. Circulating tumour cells in pancreatic cancer: A systematic review and meta-analysis of clinicopathological implications. Pancreatology 2020, 21, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, A.; Negri, M.; Paratore, M.; Vitale, F.; Ainora, M.E.; Nista, E.C.; Gasbarrini, A.; Zocco, M.A.; Verme, L.Z.D. Diagnostic and Prognostic Role of Extracellular Vesicles in Pancreatic Cancer: Current Evidence and Future Perspectives. Int. J. Mol. Sci. 2023, 24, 885. [Google Scholar] [CrossRef] [PubMed]
- Melo, S.A.; Luecke, L.B.; Kahlert, C.; Fernandez, A.F.; Gammon, S.T.; Kaye, J.; LeBleu, V.S.; Mittendorf, E.A.; Weitz, J.; Rahbari, N.; et al. Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature 2015, 523, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Frampton, A.E.; Prado, M.M.; López-Jiménez, E.; Fajardo-Puerta, A.B.; Jawad, Z.A.; Lawton, P.; Giovannetti, E.; Habib, N.A.; Castellano, L.; Stebbing, J.; et al. Glypican-1 is enriched in circulating-exosomes in pancreatic cancer and correlates with tumor burden. Oncotarget 2018, 9, 19006–19013. [Google Scholar] [CrossRef] [PubMed]
- Lucien, F.; Lac, V.; Billadeau, D.D.; Borgida, A.; Gallinger, S.; Leong, H.S. Glypican-1 and glycoprotein 2 bearing extracellular vesicles do not discern pancreatic cancer from benign pancreatic diseases. Oncotarget 2019, 10, 1045–1055. [Google Scholar] [CrossRef] [PubMed]
- Konoshenko, M.Y.; Lekchnov, E.A.; Vlassov, A.V.; Laktionov, P.P. Isolation of Extracellular Vesicles: General Methodologies and Latest Trends. BioMed Res. Int. 2018, 2018, 8545347. [Google Scholar] [CrossRef] [PubMed]
- Welsh, J.A.; Goberdhan, D.C.I.; O’Driscoll, L.; Buzas, E.I.; Blenkiron, C.; Bussolati, B.; Cai, H.; Di Vizio, D.; Driedonks, T.A.P.; Erdbrügger, U.; et al. Minimal information for studies of extracellular vesicles (MISEV2023): From basic to advanced approaches. J. Extracell. Vesicles 2024, 13, e12404. [Google Scholar] [CrossRef] [PubMed]
- Yeon, S.-E.; No, D.Y.; Lee, S.-H.; Nam, S.W.; Oh, I.-H.; Lee, J.; Kuh, H.-J. Application of Concave Microwells to Pancreatic Tumor Spheroids Enabling Anticancer Drug Evaluation in a Clinically Relevant Drug Resistance Model. PLoS ONE 2013, 8, e73345. [Google Scholar] [CrossRef] [PubMed]
- Ootani, A.; Li, X.; Sangiorgi, E.; Ho, Q.T.; Ueno, H.; Toda, S.; Sugihara, H.; Fujimoto, K.; Weissman, I.L.; Capecchi, M.R.; et al. Sustained in vitro intestinal epithelial culture within a Wnt-dependent stem cell niche. Nat. Med. 2009, 15, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Sereti, E.; Papapostolou, I.; Dimas, K. Pancreatic Cancer Organoids: An Emerging Platform for Precision Medicine? Biomedicines 2023, 11, 890. [Google Scholar] [CrossRef]
- Boj, S.F.; Hwang, C.-I.; Baker, L.A.; Chio, I.I.C.; Engle, D.D.; Corbo, V.; Jager, M.; Ponz-Sarvise, M.; Tiriac, H.; Spector, M.S.; et al. Organoid Models of Human and Mouse Ductal Pancreatic Cancer. Cell 2015, 160, 324–338. [Google Scholar] [CrossRef] [PubMed]
- Neal, J.T.; Li, X.; Zhu, J.; Giangarra, V.; Grzeskowiak, C.L.; Ju, J.; Liu, I.H.; Chiou, S.-H.; Salahudeen, A.A.; Smith, A.R.; et al. Organoid Modeling of the Tumor Immune Microenvironment. Cell 2018, 175, 1972–1988.e16. [Google Scholar] [CrossRef] [PubMed]
- Walsh, A.J.; Castellanos, J.A.; Nagathihalli, N.S.; Merchant, N.B.; Skala, M.C. Optical Imaging of Drug-Induced Metabolism Changes in Murine and Human Pancreatic Cancer Organoids Reveals Heterogeneous Drug Response. Pancreas 2016, 45, 863–869. [Google Scholar] [CrossRef] [PubMed]
- Tiriac, H.; Belleau, P.; Engle, D.D.; Plenker, D.; Deschenes, A.; Somerville, T.D.D.; Froeling, F.E.M.; Burkhart, R.A.; Denroche, R.E.; Jang, G.H.; et al. Organoid Profiling Identifies Common Responders to Chemotherapy in Pancreatic Cancer. Cancer Discov. 2018, 8, 1112–1129. [Google Scholar] [CrossRef]
- Driehuis, E.; van Hoeck, A.; Moore, K.; Kolders, S.; Francies, H.E.; Gulersonmez, M.C.; Stigter, E.C.A.; Burgering, B.; Geurts, V.; Gracanin, A.; et al. Pancreatic cancer organoids recapitulate disease and allow personalized drug screening. Proc. Natl. Acad. Sci. USA 2019, 116, 26580–26590. [Google Scholar] [CrossRef]
- Sepich-Poore, G.D.; Zitvogel, L.; Straussman, R.; Hasty, J.; Wargo, J.A.; Knight, R. The microbiome and human cancer. Science 2021, 371, eabc4552. [Google Scholar] [CrossRef] [PubMed]
- Papa, V.; Schepis, T.; Coppola, G.; Chiappetta, M.F.; Del Vecchio, L.E.; Rozera, T.; Quero, G.; Gasbarrini, A.; Alfieri, S.; Papa, A. The Role of Microbiota in Pancreatic Cancer. Cancers 2023, 15, 3143. [Google Scholar] [CrossRef] [PubMed]
- Kartal, E.; Schmidt, T.S.B.; Molina-Montes, E.; Rodríguez-Perales, S.; Wirbel, J.; Maistrenko, O.M.; Akanni, W.; Alhamwe, B.A.; Alves, R.J.; Carrato, A.; et al. A faecal microbiota signature with high specificity for pancreatic cancer. Gut 2022, 71, 1359–1372. [Google Scholar] [CrossRef]
- Tintelnot, J.; Xu, Y.; Lesker, T.R.; Schönlein, M.; Konczalla, L.; Giannou, A.D.; Pelczar, P.; Kylies, D.; Puelles, V.G.; Bielecka, A.A.; et al. Microbiota-derived 3-IAA influences chemotherapy efficacy in pancreatic cancer. Nature 2023, 615, 168–174. [Google Scholar] [CrossRef]
- de Melo, M.; Curi, T.; Miyasaka, C.; Palanch, A.; Curi, R. Effect of Indole Acetic Acid on Oxygen Metabolism in Cultured Rat Neutrophil. Gen. Pharmacol. Vasc. Syst. 1998, 31, 573–578. [Google Scholar] [CrossRef]
- Roviello, G.; Ramello, M.; Catalano, M.; D’angelo, A.; Conca, R.; Gasperoni, S.; Dreoni, L.; Petrioli, R.; Ianza, A.; Nobili, S.; et al. Association between neutropenia and survival to nab-paclitaxel and gemcitabine in patients with metastatic pancreatic cancer. Sci. Rep. 2020, 10, 19281. [Google Scholar] [CrossRef]
- Boicean, A.; Ichim, C.; Todor, S.B.; Anderco, P.; Popa, M.L. The Importance of Microbiota and Fecal Microbiota Transplantation in Pancreatic Disorders. Diagnostics 2024, 14, 861. [Google Scholar] [CrossRef]
- Park, E.M.; Chelvanambi, M.; Bhutiani, N.; Kroemer, G.; Zitvogel, L.; Wargo, J.A. Targeting the gut and tumor microbiota in cancer. Nat. Med. 2022, 28, 690–703. [Google Scholar] [CrossRef] [PubMed]
- Osipov, A.; Theodorescu, D. Artificial intelligence uses multi-omic data to predict pancreatic cancer outcomes. Nat. Cancer 2024, 5, 226–227. [Google Scholar] [CrossRef]
- Tovar, D.R.; Rosenthal, M.H.; Maitra, A.; Koay, E.J. Potential of artificial intelligence in the risk stratification for and early detection of pancreatic cancer. Artif. Intell. Surg. 2023, 3, 14–26. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicoletti, A.; Paratore, M.; Vitale, F.; Negri, M.; Quero, G.; Esposto, G.; Mignini, I.; Alfieri, S.; Gasbarrini, A.; Zocco, M.A.; et al. Understanding the Conundrum of Pancreatic Cancer in the Omics Sciences Era. Int. J. Mol. Sci. 2024, 25, 7623. https://doi.org/10.3390/ijms25147623
Nicoletti A, Paratore M, Vitale F, Negri M, Quero G, Esposto G, Mignini I, Alfieri S, Gasbarrini A, Zocco MA, et al. Understanding the Conundrum of Pancreatic Cancer in the Omics Sciences Era. International Journal of Molecular Sciences. 2024; 25(14):7623. https://doi.org/10.3390/ijms25147623
Chicago/Turabian StyleNicoletti, Alberto, Mattia Paratore, Federica Vitale, Marcantonio Negri, Giuseppe Quero, Giorgio Esposto, Irene Mignini, Sergio Alfieri, Antonio Gasbarrini, Maria Assunta Zocco, and et al. 2024. "Understanding the Conundrum of Pancreatic Cancer in the Omics Sciences Era" International Journal of Molecular Sciences 25, no. 14: 7623. https://doi.org/10.3390/ijms25147623
APA StyleNicoletti, A., Paratore, M., Vitale, F., Negri, M., Quero, G., Esposto, G., Mignini, I., Alfieri, S., Gasbarrini, A., Zocco, M. A., & Zileri Dal Verme, L. (2024). Understanding the Conundrum of Pancreatic Cancer in the Omics Sciences Era. International Journal of Molecular Sciences, 25(14), 7623. https://doi.org/10.3390/ijms25147623







