Time-Restricted Feeding Protects against Renal Ischemia-Reperfusion Injury in Mice
Abstract
:1. Introduction
2. Results
2.1. TRF Mitigates Pathological Damage in IRI-Induced AKI
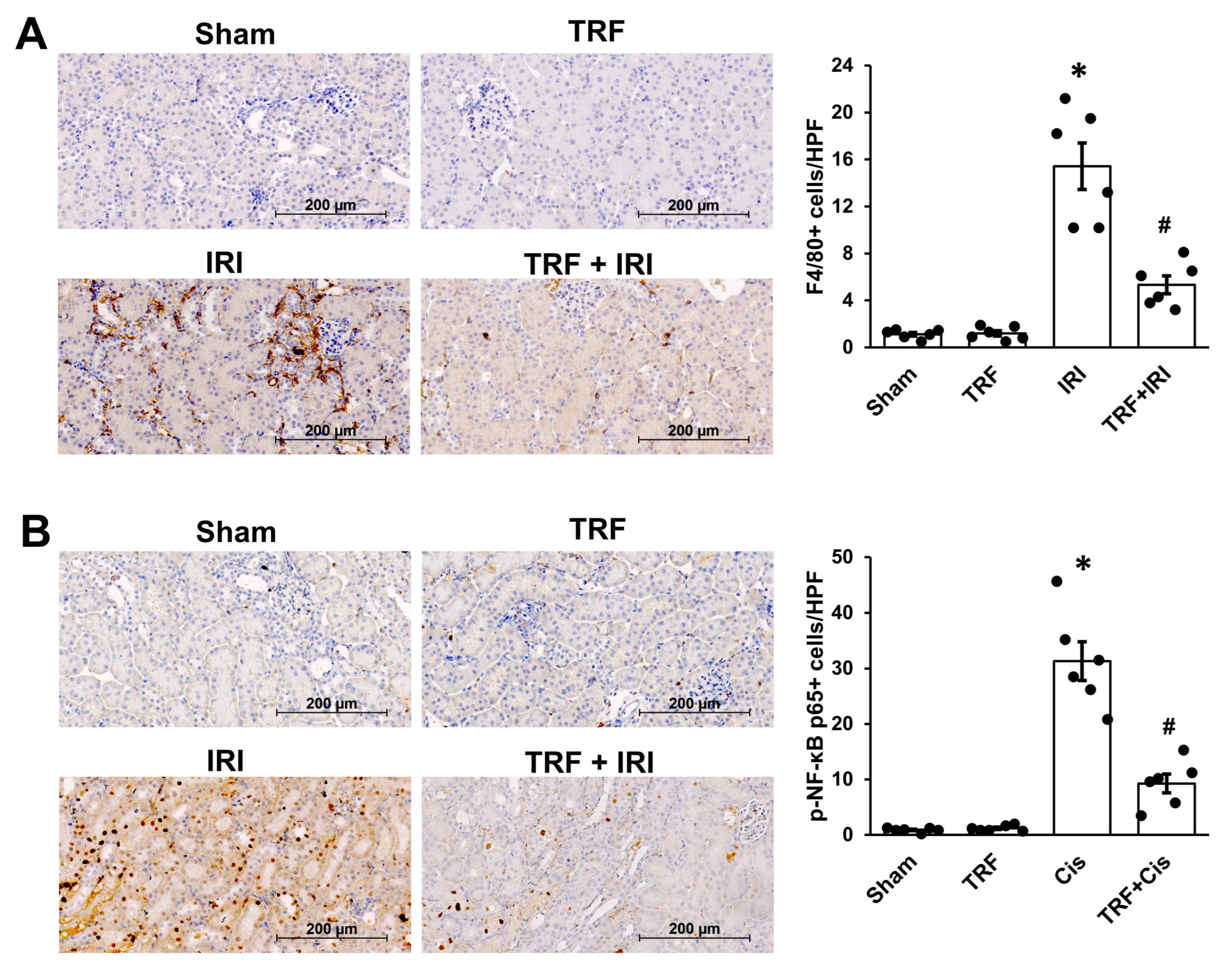
2.2. TRF Mitigates Inflammation in IRI-Induced AKI
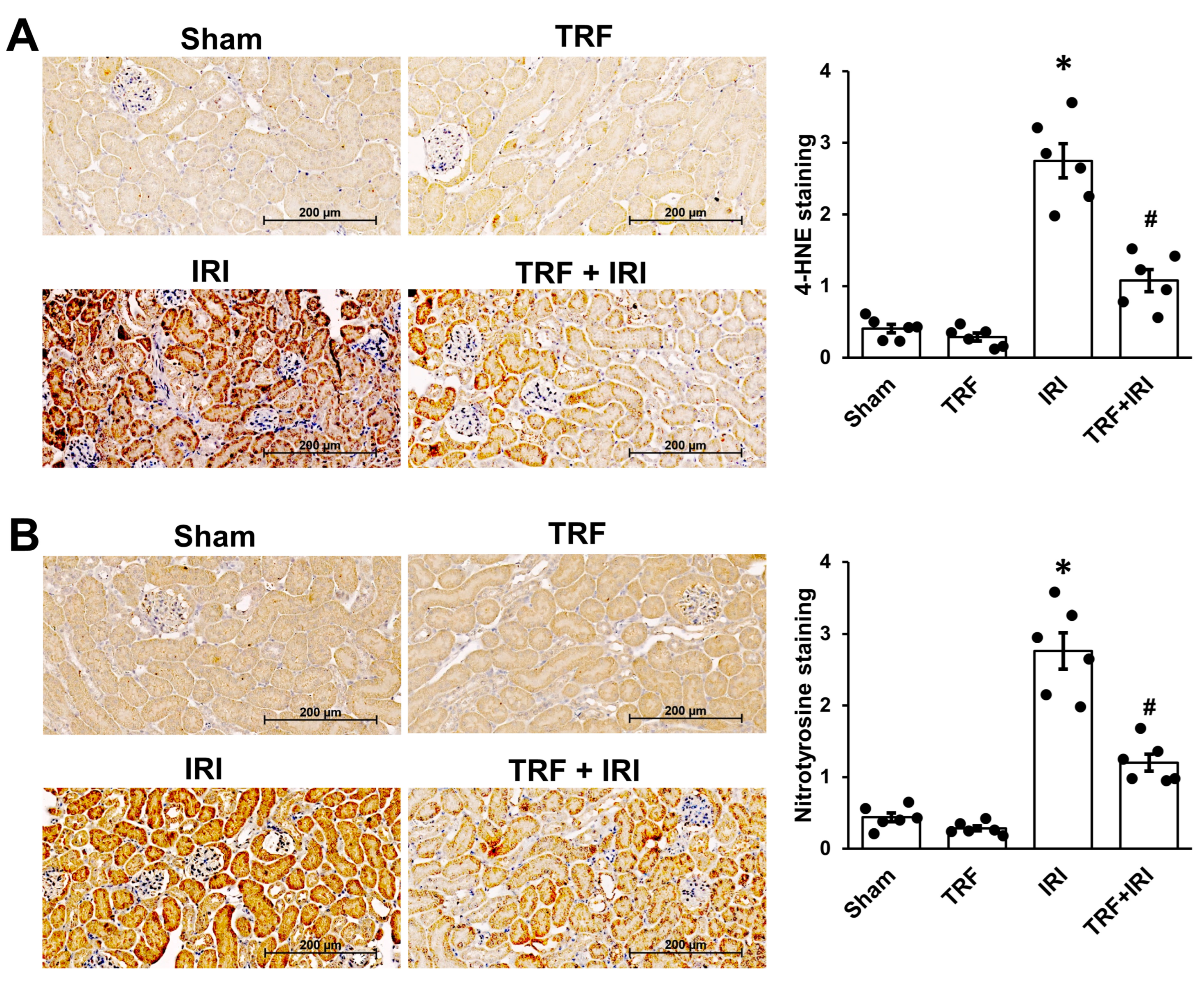
2.3. TRF Mitigates Oxidative Stress in IRI-Induced AKI
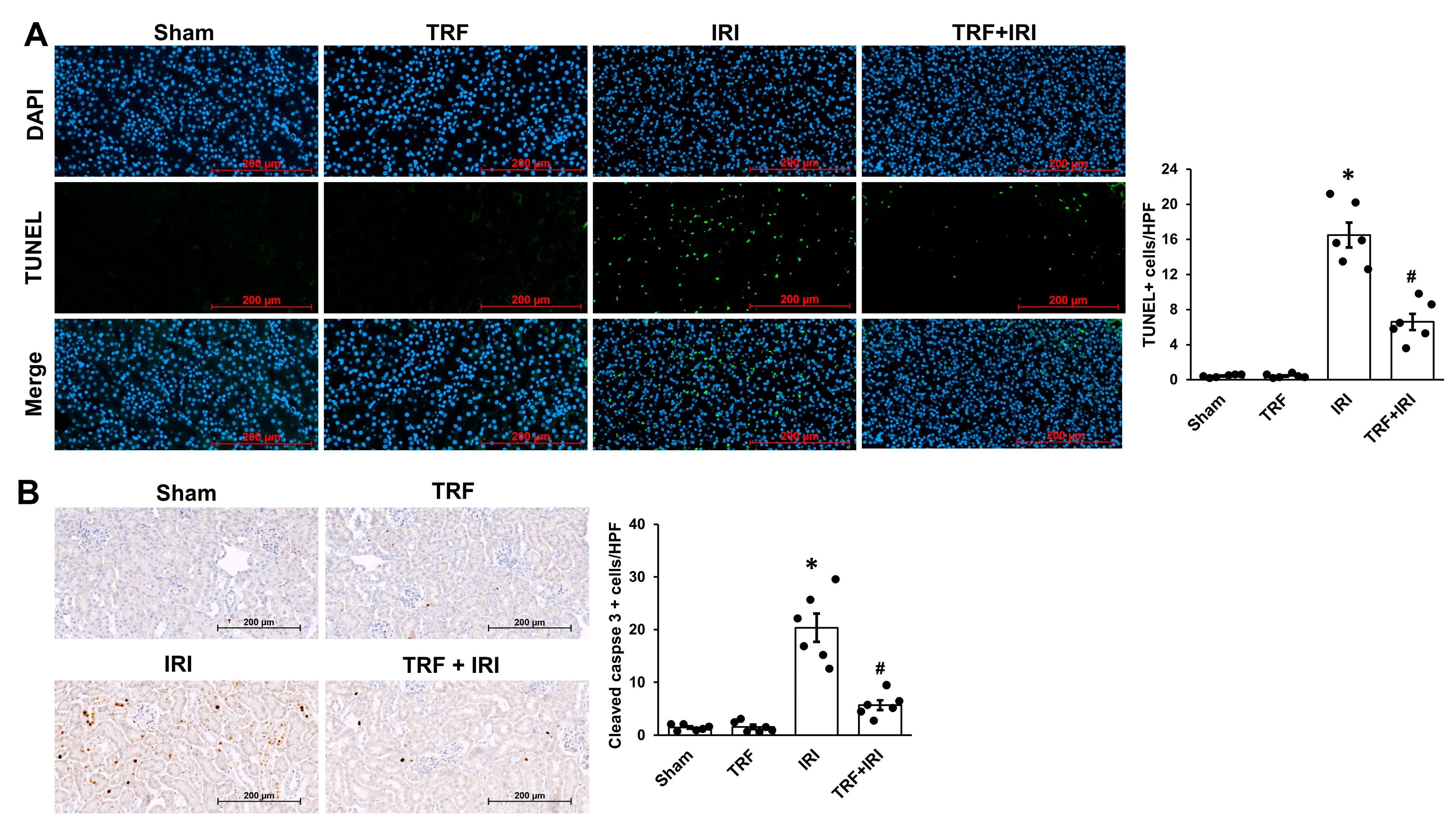
2.4. TRF Mitigates Tubular Apoptosis in IRI-Induced AKI
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Body Weight, food Intake, and Blood Measurements
4.3. Histology
4.4. Immunohistochemistry
4.5. Terminal Deoxynucleotidyl Transferase (TdT)-Mediated Deoxyuridine Triphosphate Nick End Labeling (TUNEL) Staining
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Susantitaphong, P.; Cruz, D.N.; Cerda, J.; Abulfaraj, M.; Alqahtani, F.; Koulouridis, I.; Jaber, B.L. Acute Kidney Injury Advisory Group of the American Society of, Nephrology World Incidence of Aki: A Meta-Analysis. Clin. J. Am. Soc. Nephrol. 2013, 8, 1482–1493. [Google Scholar] [CrossRef]
- Sun, L.; Hua, R.X.; Wu, Y.; Zou, L.X. Acute Kidney Injury in Hospitalized Adults with Chronic Kidney Disease: Comparing Crock, Kdigo, and Combined Criteria. Kidney Res. Clin. Pract. 2023, 42, 639–648. [Google Scholar] [CrossRef]
- Kusch, A.; Hoff, U.; Bubalo, G.; Zhu, Y.; Fechner, M.; Schmidt-Ullrich, R.; Marko, L.; Muller, D.N.; Schmidt-Ott, K.M.; Gurgen, D.; et al. Novel Signalling Mechanisms and Targets in Renal Ischaemia and Reperfusion Injury. Acta Physiol. 2013, 208, 25–40. [Google Scholar] [CrossRef]
- Anton, S.D.; Moehl, K.; Donahoo, W.T.; Marosi, K.; Lee, S.A.; Mainous, A.G., 3rd; Leeuwenburgh, C.; Mattson, M.P. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity 2018, 26, 254–268. [Google Scholar] [CrossRef]
- Rojas-Morales, P.; Leon-Contreras, J.C.; Granados-Pineda, J.; Hernandez-Pando, R.; Gonzaga, G.; Sanchez-Lozada, L.G.; Osorio-Alonso, H.; Pedraza-Chaverri, J.; Tapia, E. Protection against Renal Ischemia and Reperfusion Injury by Short-Term Time-Restricted Feeding Involves the Mitochondrial Unfolded Protein Response. Free Radic. Biol. Med. 2020, 154, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Morales, P.; Leon-Contreras, J.C.; Aparicio-Trejo, O.E.; Reyes-Ocampo, J.G.; Medina-Campos, O.N.; Jimenez-Osorio, A.S.; Gonzalez-Reyes, S.; Marquina-Castillo, B.; Hernandez-Pando, R.; Barrera-Oviedo, D.; et al. Fasting Reduces Oxidative Stress, Mitochondrial Dysfunction and Fibrosis Induced by Renal Ischemia-Reperfusion Injury. Free Radic. Biol. Med. 2019, 135, 60–67. [Google Scholar] [CrossRef] [PubMed]
- de Cabo, R.; Mattson, M.P. Effects of Intermittent Fasting on Health, Aging, and Disease. N. Engl. J. Med. 2019, 381, 2541–2551. [Google Scholar] [CrossRef] [PubMed]
- Bjerre, N.; Holm, L.; Quist, J.S.; Faerch, K.; Hempler, N.F. Watching, Keeping and Squeezing Time to Lose Weight: Implications of Time-Restricted Eating in Daily Life. Appetite 2021, 161, 105138. [Google Scholar] [CrossRef] [PubMed]
- Han, S.J.; Lee, H.T. Mechanisms and Therapeutic Targets of Ischemic Acute Kidney Injury. Kidney Res. Clin. Pract. 2019, 38, 427–440. [Google Scholar] [CrossRef] [PubMed]
- Sims, B.M.; Goodlett, B.L.; Allbee, M.L.; Pickup, E.J.; Chiasson, V.L.; Arenaz, C.M.; Henley, M.R.; Navaneethabalakrishnan, S.; Mitchell, B.M. Time Restricted Feeding Decreases Renal Innate Immune Cells and Blood Pressure in Hypertensive Mice. J. Hypertens. 2022, 40, 1960–1968. [Google Scholar] [CrossRef] [PubMed]
- Mattson, M.P.; Allison, D.B.; Fontana, L.; Harvie, M.; Longo, V.D.; Malaisse, W.J.; Mosley, M.; Notterpek, L.; Ravussin, E.; Scheer, F.A.; et al. Meal Frequency and Timing in Health and Disease. Proc. Natl. Acad. Sci. USA 2014, 111, 16647–16653. [Google Scholar] [CrossRef] [PubMed]
- Puchalska, P.; Crawford, P.A. Metabolic and Signaling Roles of Ketone Bodies in Health and Disease. Annu. Rev. Nutr. 2021, 41, 49–77. [Google Scholar] [CrossRef] [PubMed]
- Gomora-Garcia, J.C.; Montiel, T.; Huttenrauch, M.; Salcido-Gomez, A.; Garcia-Velazquez, L.; Ramiro-Cortes, Y.; Gomora, J.C.; Castro-Obregon, S.; Massieu, L. Effect of the Ketone Body, D-Beta-Hydroxybutyrate, on Sirtuin2-Mediated Regulation of Mitochondrial Quality Control and the Autophagy-Lysosomal Pathway. Cells 2023, 12, 486. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Hu, D.; Mao, Y.; Yang, H.; Liao, W.; Xu, W.; Ge, P.; Zhang, H.; Sang, X.; Lu, X.; et al. Alteration in Gut Microbiota Caused by Time-Restricted Feeding Alleviate Hepatic Ischaemia Reperfusion Injury in Mice. J. Cell. Mol. Med. 2019, 23, 1714–1722. [Google Scholar] [CrossRef] [PubMed]
- Abas, E.; Sabry, M.M. Intermittent Fasting Attenuates Apoptosis, Modulates Autophagy and Preserves Telocytes in Doxorubicin Induced Cardiotoxicity in Albino Rats: A Histological Study. Egypt. J. Histol. 2020, 43, 663–683. [Google Scholar] [CrossRef]
- Saat, T.C.; van der Pluijm, I.; Ridwan, Y.; van Damme-van den Engel, S.; van Heijningen, P.M.; Clahsen-van Groningen, M.C.; Verhagen, H.J.M.; IJzermans, J.N.M.; Essers, J.; de Bruin, R.W.F. Pre-Operative Fasting Provides Long Term Protection against Chronic Renal Damage Induced by Ischaemia Reperfusion Injury in Wild Type and Aneurysm Prone Fibulin-4 Mice. Eur. J. Vasc. Endovasc. Surg. 2020, 60, 905–915. [Google Scholar] [CrossRef]
- Kim, I.Y.; Park, Y.K.; Song, S.H.; Seong, E.Y.; Lee, D.W.; Bae, S.S.; Lee, S.B. Role of Akt1 in Renal Fibrosis and Tubular Dedifferentiation During the Progression of Acute Kidney Injury to Chronic Kidney Disease. Korean J. Intern. Med. 2021, 36, 962–974. [Google Scholar] [CrossRef]
- Kim, M.J.; Kim, Y.S.; Kim, S.R.; Lee, D.W.; Lee, S.B.; Kim, I.Y. Pre-Treatment with Beta-Hydroxybutyrate Mitigates Cisplatin-Induced Acute Kidney Injury. Biochem. Biophys. Res. Commun. 2024, 695, 149482. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.K.; Kim, Y.S.; Kim, M.J.; Kim, S.R.; Lee, D.W.; Lee, S.B.; Kim, I.Y. Time-Restricted Feeding Protects against Renal Ischemia-Reperfusion Injury in Mice. Int. J. Mol. Sci. 2024, 25, 7652. https://doi.org/10.3390/ijms25147652
Kim DK, Kim YS, Kim MJ, Kim SR, Lee DW, Lee SB, Kim IY. Time-Restricted Feeding Protects against Renal Ischemia-Reperfusion Injury in Mice. International Journal of Molecular Sciences. 2024; 25(14):7652. https://doi.org/10.3390/ijms25147652
Chicago/Turabian StyleKim, Do Kyun, Young Suk Kim, Min Jeong Kim, Seo Rin Kim, Dong Won Lee, Soo Bong Lee, and Il Young Kim. 2024. "Time-Restricted Feeding Protects against Renal Ischemia-Reperfusion Injury in Mice" International Journal of Molecular Sciences 25, no. 14: 7652. https://doi.org/10.3390/ijms25147652




