Association between Autism Spectrum Disorder, Trace Elements, and Intracranial Fluid Spaces
Abstract
:1. Introduction
2. Results
2.1. Data on the Study Groups
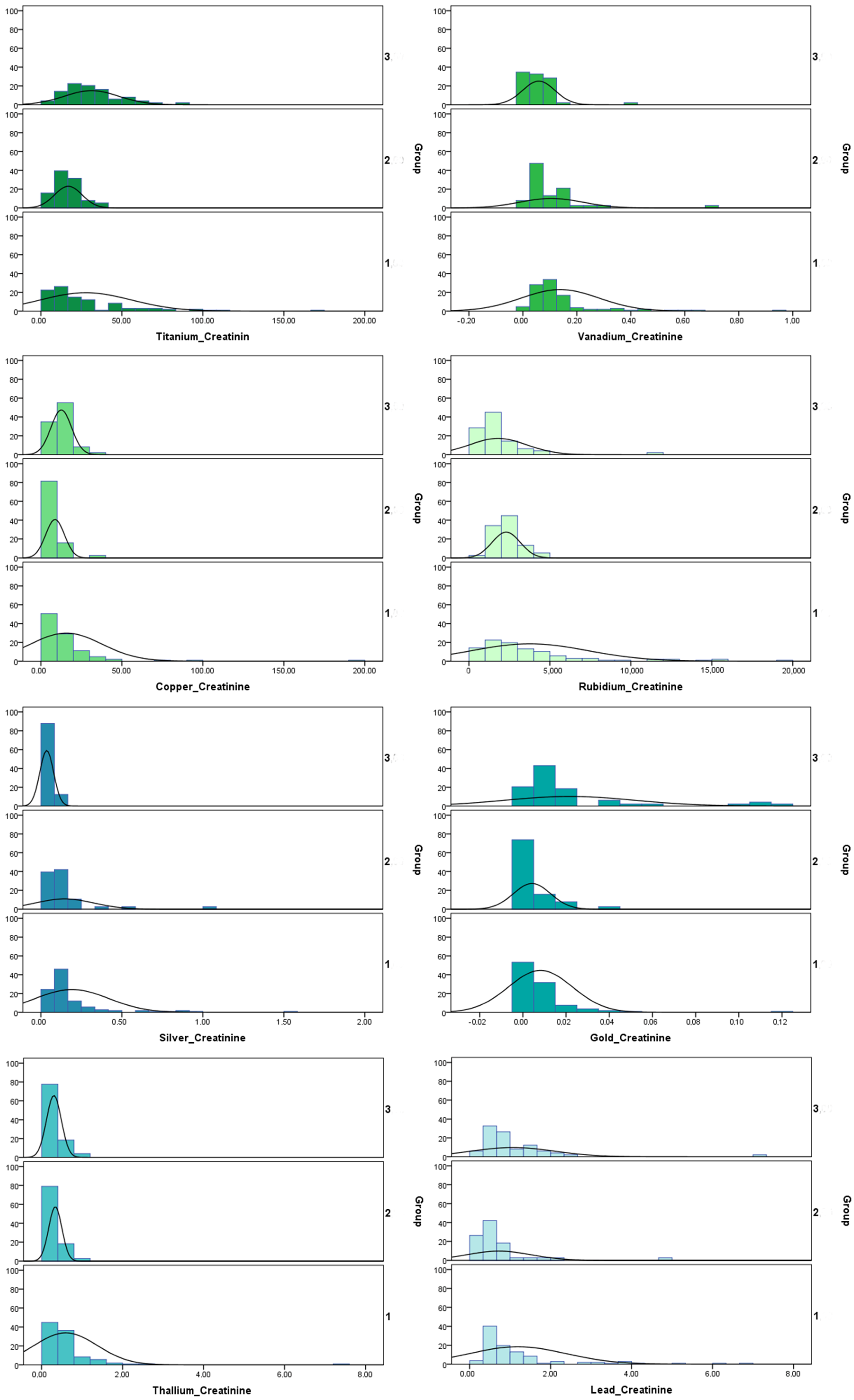
2.2. Concentration of Trace Elements in Urine Samples
2.2.1. Comparison of Metal Concentrations between Children with ASD and Healthy Controls
2.2.2. Comparison of Metal Concentrations between Children with HF-ASD and Healthy Controls
2.2.3. Comparison of Metal Concentrations between Children with ASD and Children with HF-ASD
2.2.4. Comparison of Metal Concentrations between Children with ASD or HF-ASD Grouped by Deficit (Mild, Moderate, and Severe)
2.2.5. Comparison of Metal Concentrations between Children with ASD or HF-ASD with Epilepsy and without Epilepsy
2.3. Correlations between Metal Concentrations in Urine with Brain MRI Findings
3. Discussion
3.1. Essential Metals
3.2. Specific Trace Elements
3.3. General Discussion
4. Materials and Methods
4.1. Study Cohort
4.2. Laboratory Evaluation of Urine
4.3. Calculation of Linear Indexes of the Intracranial Fluid Spaces
- -
- Evans’ Index (maximum distance between anterior horns divided by maximum internal skull diameter),
- -
- Bifrontal Index (the maximum distance between anterior horns divided by the maximum internal diameter of the frontal bone),
- -
- Bicaudate Index (Minimum bicaudate nuclei distance divided by internal skull diameter measured along the same line),
- -
- Bicaudate-Frontal Index (the minimum bicaudate nuclei distance divided by the maximum distance between anterior horns),
- -
- Bicaudate-Temporal Index (the minimum bicaudate nuclei distance divided by maximum internal skull diameter),
- -
- Schiersmann’s Index (the maximum external diameter of the skull divided by cella media distance),
- -
- Huckman Number (the sum of the maximum distance between anterior horns and minimum bicaudate nuclei distance) [39].
4.4. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Masi, A.; DeMayo, M.M.; Glozier, N.; Guastella, A.J. An Overview of Autism Spectrum Disorder, Heterogeneity and Treatment Options. Neurosci. Bull. 2017, 33, 183–193. [Google Scholar] [CrossRef]
- Rochat, M.J.; Distefano, G.; Maffei, M.; Toni, F.; Posar, A.; Scaduto, M.C.; Resca, F.; Cameli, C.; Bacchelli, E.; Maestrini, E.; et al. Brain Magnetic Resonance Findings in 117 Children with Autism Spectrum Disorder under 5 Years Old. Brain Sci. 2020, 10, 741. [Google Scholar] [CrossRef]
- Osredkar, J.; Gosar, D.; Maček, J.; Kumer, K.; Fabjan, T.; Finderle, P.; Šterpin, S.; Zupan, M.; Jekovec Vrhovšek, M. Urinary Markers of Oxidative Stress in Children with Autism Spectrum Disorder (ASD). Antioxidants 2019, 8, 187. [Google Scholar] [CrossRef]
- Zhang, J.; Li, X.; Shen, L.; Khan, N.U.; Zhang, X.; Chen, L.; Zhao, H.; Luo, P. Trace elements in children with autism spectrum disorder: A meta-analysis based on case-control studies. J. Trace Elem. Med. Biol. 2021, 67, 126782. [Google Scholar] [CrossRef]
- Adams, J.B.; Holloway, C.E.; George, F.; Quig, D. Analyses of toxic metals and essential minerals in the hair of Arizona children with autism and associated conditions, and their mothers. Biol. Trace Elem. Res. 2006, 110, 193–210. [Google Scholar] [CrossRef]
- Saghazadeh, A.; Rezaei, N. Systematic review and meta-analysis links autism and toxic metals and highlights the impact of country development status: Higher blood and erythrocyte levels for mercury and lead, and higher hair antimony, cadmium, lead, and mercury. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2017, 79 Pt B, 340–368. [Google Scholar] [CrossRef]
- Qureshi, F.; Adams, J.; Coleman, D.; Quig, D.; Hahn, J. Urinary Essential Elements of Young Children with Autism Spectrum Disorder and Their Mothers. Res. Autism Spectr. Disord. 2020, 72, 101518. [Google Scholar] [CrossRef]
- Fiore, M.; Barone, R.; Copat, C.; Grasso, A.; Cristaldi, A.; Rizzo, R.; Ferrante, M. Metal and essential element levels in hair and association with autism severity. J. Trace Elem. Med. Biol. 2020, 57, 126409. [Google Scholar] [CrossRef]
- Akyuzlu, D.K.; Kayaalti, Z.; Soylemez, E.; Soylemezoglu, T. Association between Autism and Arsenic, Lead, Cadmium, Manganese Levels in Hair and Urine. J. Pharm. Pharmacol. 2014, 2, 140–144. [Google Scholar]
- Mizuno, Y.; Kagitani-Shimono, K.; Jung, M.; Makita, K.; Takiguchi, S.; Fujisawa, T.X.; Tachibana, M.; Nakanishi, M.; Mohri, I.; Taniike, M.; et al. Structural brain abnormalities in children and adolescents with comorbid autism spectrum disorder and attention-deficit/hyperactivity disorder. Transl. Psychiatry 2019, 9, 332. [Google Scholar] [CrossRef]
- Jomova, K.; Makova, M.; Alomar, S.Y.; Alwasel, S.H.; Nepovimova, E.; Kuca, K.; Rhodes, C.J.; Valko, M. Essential metals in health and disease. Chem. Interact. 2022, 367, 110173. [Google Scholar] [CrossRef]
- Wang, Q.; Kong, Y.; Wu, D.-Y.; Liu, J.-H.; Jie, W.; You, Q.-L.; Huang, L.; Hu, J.; Chu, H.-D.; Gao, F.; et al. Impaired calcium signaling in astrocytes modulates autism spectrum disorder-like behaviors in mice. Nat. Commun. 2021, 12, 3321. [Google Scholar] [CrossRef]
- Skogheim, T.S.; Weyde, K.V.F.; Engel, S.M.; Aase, H.; Surén, P.; Øie, M.G.; Biele, G.; Reichborn-Kjennerud, T.; Caspersen, I.H.; Hornig, M.; et al. Metal and essential element concentrations during pregnancy and associations with autism spectrum disorder and attention-deficit/hyperactivity disorder in children. Environ. Int. 2021, 152, 106468. [Google Scholar] [CrossRef]
- Yasuda, H.; Tsutsui, T. Assessment of infantile mineral imbalances in autism spectrum disorders (ASDs). Int. J. Environ. Res. Public Health 2013, 10, 6027–6043. [Google Scholar] [CrossRef]
- Baj, J.; Flieger, W.; Flieger, M.; Forma, A.; Sitarz, E.; Skórzyńska-Dziduszko, K.; Grochowski, C.; Maciejewski, R.; Karakuła-Juchnowicz, H. Autism spectrum disorder: Trace elements imbalances and the pathogenesis and severity of autistic symptoms. Neurosci. Biobehav. Rev. 2021, 129, 117–132. [Google Scholar] [CrossRef]
- Tabatadze, T.; Zhorzholiani, L.; Kherkheulidze, M.; Kandelaki, E.; Ivanashvili, T. Hair Heavy Metal and Essential Trace Element Concentration in Children with Autism Spectrum Disorder. Georgian Med. News 2015, 77–82. [Google Scholar]
- Rahbar, M.H.; Samms-Vaughan, M.; Dickerson, A.S.; Loveland, K.A.; Ardjomand-Hessabi, M.; Bressler, J.; Shakespeare-Pellington, S.; Grove, M.L.; Pearson, D.A.; Boerwinkle, E. Blood lead concentrations in Jamaican children with and without autism spectrum disorder. Int. J. Environ. Res. Public Health 2014, 12, 83–105. [Google Scholar] [CrossRef]
- Schmidt, R.J.; Tancredi, D.J.; Krakowiak, P.; Hansen, R.L.; Ozonoff, S. Maternal intake of supplemental iron and risk of autism spectrum disorder. Am. J. Epidemiol. 2014, 180, 890–900. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fang, X.; Qu, J.; Huan, S.; Sun, X.; Li, J.; Liu, Q.; Jin, S.; Xia, W.; Xu, S.; Wu, Y.; et al. Associations of urine metals and metal mixtures during pregnancy with cord serum vitamin D Levels: A prospective cohort study with repeated measurements of maternal urinary metal concentrations. Environ. Int. 2021, 155, 106660. [Google Scholar] [CrossRef]
- Macedoni-Lukšič, M.; Gosar, D.; Bjørklund, G.; Oražem, J.; Kodrič, J.; Lešnik-Musek, P.; Zupančič, M.; France-Štiglic, A.; Sešek-Briški, A.; Neubauer, D.; et al. Levels of metals in the blood and specific porphyrins in the urine in children with autism spectrum disorders. Biol. Trace Elem. Res. 2015, 163, 2–10. [Google Scholar] [CrossRef]
- Chehbani, F.; Gallello, G.; Brahim, T.; Ouanes, S.; Douki, W.; Gaddour, N.; Sanz, M.L.C. The status of chemical elements in the blood plasma of children with autism spectrum disorder in Tunisia: A case-control study. Environ. Sci. Pollut. Res. 2020, 27, 35738–35749. [Google Scholar] [CrossRef]
- Zhao, G.; Gan, X.-Y.; Li, J.-R.; Wu, X.-X.; Liu, S.-Y.; Jin, Y.-S.; Zhang, K.-R.; Wu, H.-M. Analysis of Whole Blood and Urine Trace Elements in Children with Autism Spectrum Disorders and Autistic Behaviors. Biol. Trace Elem. Res. 2023, 201, 627–635. [Google Scholar] [CrossRef]
- Abd Wahil, M.S.; Ja’afar, M.H.; Md Isa, Z. Assessment of Urinary Lead (Pb) and Essential Trace Elements in Autism Spectrum Disorder: A Case-Control Study Among Preschool Children in Malaysia. Biol. Trace Elem. Res. 2022, 200, 97–121. [Google Scholar] [CrossRef]
- Smith, D.R.; Strupp, B.J. Animal Models of Childhood Exposure to Lead or Manganese: Evidence for Impaired Attention, Impulse Control, and Affect Regulation and Assessment of Potential Therapies. Neurotherapeutics 2023, 20, 3–21. [Google Scholar] [CrossRef]
- Hessabi, M.; Rahbar, M.H.; Dobrescu, I.; Bach, M.A.; Kobylinska, L.; Bressler, J.; Grove, M.L.; Loveland, K.A.; Mihailescu, I.; Nedelcu, M.C.; et al. Concentrations of Lead, Mercury, Arsenic, Cadmium, Manganese, and Aluminum in Blood of Romanian Children Suspected of Having Autism Spectrum Disorder. Int. J. Environ. Res. Public Health 2019, 16, 2303. [Google Scholar] [CrossRef]
- Ding, M.; Shi, S.; Qie, S.; Li, J.; Xi, X. Association between heavy metals exposure (cadmium, lead, arsenic, mercury) and child autistic disorder: A systematic review and meta-analysis. Front. Pediatr. 2023, 11, 1169733. [Google Scholar] [CrossRef]
- Błażewicz, A.; Grabrucker, A.M. Metal Profiles in Autism Spectrum Disorders: A Crosstalk between Toxic and Essential Metals. Int. J. Mol. Sci. 2022, 24, 308. [Google Scholar] [CrossRef]
- García-Fernández, L.; Hernández, A.V.; Suárez Moreno, V.; Fiestas, F. La evidencia acerca de la controversia de las vacunas que contienen timerosal y su asociación con el autismo [Addressing the controversy regarding the association between thimero-sal-containing vaccines and autism]. Rev. Peru. Med. Exp. Salud Publica 2013, 30, 268–274. [Google Scholar]
- Dickerson, A.S.; Rotem, R.S.; Christian, M.A.; Nguyen, V.T.; Specht, A.J. Potential Sex Differences Relative to Autism Spectrum Disorder and Metals. Curr. Environ. Health Rep. 2017, 4, 405–414. [Google Scholar] [CrossRef]
- Ecker, C.; Pretzsch, C.M.; Bletsch, A.; Mann, C.; Schaefer, T.; Ambrosino, S.; Tillmann, J.; Yousaf, A.; Chiocchetti, A.; Lombardo, M.V.; et al. Interindividual Differences in Cortical Thickness and Their Genomic Underpinnings in Autism Spectrum Disorder. Am. J. Psychiatry 2022, 179, 242–254. [Google Scholar] [CrossRef]
- Dekhil, O.; Hajjdiab, H.; Shalaby, A.; Ali, M.T.; Ayinde, B.; Switala, A.; Elshamekh, A.; Ghazal, M.; Keynton, R.; Barnes, G.; et al. Using resting state functional MRI to build a personalized autism diagnosis system. PLoS ONE 2018, 13, e0206351. [Google Scholar] [CrossRef]
- Munch, T.N.; Hedley, P.L.; Hagen, C.M.; Bækvad-Hansen, M.; Bybjerg-Grauholm, J.; Grove, J.; Nordentoft, M.; Børglum, A.D.; Mortensen, P.B.; Werge, T.M.; et al. Co-occurring hydrocephalus in autism spectrum disorder: A Danish population-based cohort study. J. Neurodev. Disord. 2021, 13, 19. [Google Scholar] [CrossRef]
- Brieber, S.; Neufang, S.; Bruning, N.; Kamp-Becker, I.; Remschmidt, H.; Herpertz-Dahlmann, B.; Fink, G.R.; Konrad, K. Structural brain abnormalities in adolescents with autism spectrum disorder and patients with attention deficit/hyperactivity disorder. J. Child Psychol. Psychiatry 2007, 48, 1251–1258. [Google Scholar] [CrossRef]
- Postema, M.C.; van Rooij, D.; Anagnostou, E.; Arango, C.; Auzias, G.; Behrmann, M.; Filho, G.B.; Calderoni, S.; Calvo, R.; Daly, E.; et al. Altered structural brain asymmetry in autism spectrum disorder in a study of 54 datasets. Nat. Commun. 2019, 10, 4598, Erratum in Nat. Commun. 2021, 12, 7260. [Google Scholar] [CrossRef]
- Lord, C.; Risi, S.; Lambrecht, L.; Cook, J.E.H.; Leventhal, B.L.; DiLavore, P.C.; Pickles, A.; Rutter, M. The autism diagnostic observation schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. J. Autism Dev. Disord. 2000, 30, 205–223. [Google Scholar] [CrossRef]
- Vovk Ornik, N. Kriteriji za Opredelitev Vrste in Stopnje Primanjkljajev, ovir oz. Motenj Otrok s Posebnimi Potrebami; Zavod RS za šolstvo: Ljubljana, Slovenia, 2014. [Google Scholar]
- CLSI. Evaluation of Detection Capability for Clinical Laboratory Measurement Procedures; Approved Guideline—Second Edition; CLSI document EP17-A2; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012. [Google Scholar]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.-C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef]
- Wilk, R.; Kluczewska, E.; Syc, B.; Bajor, G. Normative values for selected linear indices of the intracranial fluid spaces based on CT images of the head in children. Pol. J. Radiol. 2011, 76, 16–25. [Google Scholar]
- Strunecka, A.; Strunecky, O. Chronic Fluoride Exposure and the Risk of Autism Spectrum Disorder. Int. J. Environ. Res. Public Health 2019, 16, 3431. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Esteban-Figuerola, P.; Canals, J.; Fernández-Cao, J.C.; Arija Val, V. Differences in food consumption and nutritional intake between children with autism spectrum disorders and typically developing children: A meta-analysis. Autism 2018, 23, 1079–1095, Erratum in Autism 2020, 24, 531–536. [Google Scholar] [CrossRef]

| Element | Group A1 (n = 107) | Group B1 (n = 38) | Group C1 (n = 49) |
|---|---|---|---|
| Li | 23.3 (14.4–50.8) | 23.6 (13.9–30.7) | 24.5 (17.4–30.9) |
| Be | 0.02 (0.02–0.05) | 0.02 (0.01–0.03) | 0.03 (0.01–0.07) |
| Mg | 86,531.7 (51,554.7–149,422.6) | 81,625.5 (56,748.3–121,036.7) | 136,982.1 (61,908.1–195,288.7) |
| Al | 3.40 (1.57–8.61) | 2.00 (1.05–5.31) | 4.78 (1.82–9.29) |
| Ca | 4860.7 (2130.3–10147.1) | 5417.9 (2803.7–9516.8) | 6616.5 (3585.8–10672.0) |
| Ti | 17.65 (10.19–33.29) | 15.52 (9.09–22.25) | 28.09 (18.83–39.00) |
| V | 0.09 (0.06–0.15) | 0.06 (0.04–0.14) | 0.05 (0.02–0.08) |
| Cr | 0.25 (0.18–0.49) | 0.18 (0.12–0.32) | 0.33 (0.21–0.48) |
| Mn | 0.43 (0.33–0.73) | 0.29 (0.23–0.53) | 0.44 (0.30–0.62) |
| Fe | 2.77 (0.06–6.62) | 2.34 (0.83–4.44) | 3.80 (1.93–5.69) |
| Co | 0.4 (0.2–1.0) | 0.5 (0.3–0.7) | 0.6 (0.3–1.0) |
| Ni | 0.56 (0.29–1.60) | 0.38 (0.28–0.96) | 0.83 (0.36–1.51) |
| Cu | 9.69 (6.49–18.25) | 7.54 (5.66–9.22) | 11.59 (8.65–15.59) |
| Zn | 385.88 (249.26–639.53) | 462.83 (289.25–629.64) | 487.26 (292.32–699.29) |
| Ga | 0.03 (0.02–0.06) | 0.02 (0.02–0.04) | 0.03 (0.02–0.06) |
| As | 6.74 (3.43–15.60) | 4.93 (2.46–15.95) | 4.35 (2.64–9.10) |
| Se | 23.91 (15.25–32.38) | 20.09 (16.98–25.07) | 23.2 (16.87–27.45) |
| Rb | 2682.9 (1581.3–4750.4) | 2265.4 (1655.7–2685.6) | 1395.1 (752.9–2113.2) |
| Sr | 103.72 (57.69–207.41) | 103.71 (70.59–169.62) | 130.66 (77.67–173.92) |
| Mo | 71.88 (41.44–111.45) | 60.12 (42.02–84.22) | 65.68 (44.76–92.33) |
| Ag | 0.12 (0.09–0.19) | 0.09 (0.06–0.13) | 0.02 (0.01–0.06) |
| Cd | 0.09 (0.06–0.15) | 0.07 (0.05–0.11) | 0.11 (0.08–0.16) |
| Sn | 0.38 (0.16–1.04) | 0.27 (0.12–0.69) | 0.34 (0.21–0.61) |
| Sb | 0.06 (0.04–0.13) | 0.05 (0.03–0.07) | 0.05 (0.02–0.07) |
| Cs | 8.39 (5.55–13.64) | 7.54 (5.32–9.01) | 7.09 (4.64–9.05) |
| Ba | 2.07 (0.99–4.79) | 2.82 (1.35–5.07) | 2.75 (1.7–5.29) |
| Au | 0 (0.00–0.01) | 0 (0.00–0.01) | 0.01 (0.01–0.02) |
| Hg | 0.13 (0.05–0.28) | 0.165 (0.08–0.38) | 0.15 (0.07–0.28) |
| Tl | 0.42 (0.25–0.64) | 0.32 (0.23–0.38) | 0.27 (0.18–0.39) |
| Pb | 0.73 (0.52–1.31) | 0.52 (0.32–0.74) | 0.83 (0.54–1.42) |
| U | 0.01 (0.00–0.01) | 0.01 (0.00–0.01) | 0.01 (0.00–0.01) |
| Group A1 vs. Group C1 | Group A1 vs. Group B1 | Group B1 vs. Group C1 | |
|---|---|---|---|
| Li | 0.750 (1.000) | 0.400 (1.000) | 0.584 (1.000) |
| Be | 0.664 (1.000) | 0.011 (0.33) * | 0.020 (0.600) * |
| Mg | 0.096 (1.000) | 0.500 (1.000) | 0.020 (0.600) * |
| Al | 0.325 (1.000) | 0.033 (0.99) * | 0.011 (0.330) * |
| Ca | 0.144 (1.000) | 0.472 (1.000) | 0.436 (1.000) |
| Ti | 0.006 (0.180) * | 0.244 (1.000) | <0.001 (<0.001) ** |
| V | <0.001 (<0.001) ** | 0.037 (1.000) * | 0.011 (0.330) * |
| Cr | 0.357 (1.000) | 0.003 (0.090) * | 0.002 (0.060) * |
| Mn | 0.387 (1.000) | 0.002 (0.060) * | 0.045 (1.000) * |
| Fe | 0.194 (1.000) | 0.927 (1.000) | 0.094 (1.000) |
| Co | 0.166 (1.000) | 0.618 (1.000) | 0.279 (1.000) |
| Ni | 0.505 (1.000) | 0.085 (1.000) | 0.019 (0.570) * |
| Cu | 0.397 (1.000) | 0.006 (0.180) * | <0.001 (0.005) ** |
| Zn | 0.228 (1.000) | 0.607 (1.000) | 0.555 (1.000) |
| Ga | 0.705 (1.000) | 0.004 (0.120) * | 0.023 (0.690) * |
| As | 0.038 (1.000) * | 0.551 (1.000) | 0.360 (1.000) |
| Se | 0.425 (1.000) | 0.106 (1.000) | 0.342 (1.000) |
| Rb | <0.001 (<0.001) ** | 0.069 (1.000) | <0.001 (0.010) ** |
| Sr | 0.805 (1.000) | 0.679 (1.000) | 0.426 (1.000) |
| Mo | 0.713 (1.000) | 0.251 (1.000) | 0.342 (1.000) |
| Ag | <0.001 (<0.001) ** | 0.055 (1.000) | <0.001 (<0.001) ** |
| Cd | 0.156 (1.000) | 0.098 (1.000) | 0.010 (0.300) * |
| Sn | 0.96 (1.000) | 0.228 (1.000) | 0.241 (1.000) |
| Sb | 0.011 (0.330) * | 0.112 (1.000) | 0.561 (1.000) |
| Cs | 0.010 (0.300) * | 0.083 (1.000) | 0.419 (1.000) |
| Ba | 0.064 (1.000) | 0.454 (1.000) | 0.411 (1.000) |
| Au | <0.001 (0.001) ** | 0.040 (1.000) * | <0.001 (<0.001) ** |
| Hg | 0.267 (1.000) | 0.230 (1.000) | 0.821 (1.000) |
| Tl | <0.001 (0.007) ** | 0.010 (0.300) * | 0.249 (1.000) |
| Pb | 0.826 (1.000) | <0.001 (0.010) ** | 0.001 (0.03) ** |
| U | 0.648 (1.000) | 0.672 (1.000) | 0.623 (1.000) |
| (A) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Huckman Index | Evans Index | Bifrontal Index | Bicaudate Frontal Index | Bicaudate Index | Bicaudate Temporal Index | Schiersmann Index | Number of Statistically Significant Correlations | Autism Deficit Score | Epilepsy Present | |
| Li | 0.294 | 0.324 | 0.343 | 0.250 | 0.309 | 0.340 | −0.087 | 0 | 0.228 | 0.094 |
| Be | 0.410 * | 0.488 ** | 0.572 ** | 0.523 ** | 0.606 ** | 0.615 ** | −0.395 * | 7 | 0.114 | 0.210 |
| Mg | 0.216 | 0.209 | 0.369 | 0.078 | 0.120 | 0.158 | −0.194 | 0 | −0.425 * | −0.009 |
| Al | 0.060 | 0.288 | 0.307 | 0.200 | 0.217 | 0.268 | 0.114 | 0 | 0.218 | −0.059 |
| Ca | 0.308 | 0.148 | 0.207 | 0.411 * | 0.371 | 0.383 * | −0.180 | 2 | −0.177 | −0.023 |
| Ti | 0.194 | 0.382 * | 0.494 ** | 0.198 | 0.263 | 0.302 | −0.326 | 2 | −0.189 | −0.114 |
| V | 0.529 ** | 0.511 ** | 0.556 ** | 0.266 | 0.407 * | 0.453 * | −0.311 | 5 | −0.189 | 0.314 |
| Cr | 0.644 ** | 0.610 ** | 0.517 ** | 0.511 ** | 0.674 ** | 0.704 ** | −0.251 | 6 | 0.000 | 0.515 * |
| Mn | 0.238 | 0.287 | 0.455 * | 0.160 | 0.228 | 0.259 | −0.132 | 1 | −0.169 | 0.154 |
| Fe | 0.022 | 0.049 | 0.284 | 0.001 | −0.026 | 0.020 | −0.053 | 0 | −0.222 | −0.045 |
| Co | 0.428 * | 0.459 * | 0.416 * | 0.431 * | 0.486 ** | 0.555 ** | −0.347 | 6 | −0.280 | 0.233 |
| Ni | 0.061 | 0.249 | 0.093 | 0.139 | 0.099 | 0.218 | −0.034 | 0 | −0.061 | −0.105 |
| Cu | 0.374 | 0.488 ** | 0.482 ** | 0.408 * | 0.503 ** | 0.530 ** | −0.419 * | 6 | −0.168 | 0.110 |
| Zn | 0.246 | 0.149 | 0.063 | 0.269 | 0.225 | 0.265 | −0.314 | 0 | −0.206 | −0.018 |
| Ga | 0.059 | 0.141 | 0.369 | 0.053 | 0.062 | 0.101 | −0.063 | 0 | −0.153 | −0.009 |
| As | −0.065 | −0.210 | −0.056 | −0.129 | −0.127 | −0.175 | 0.252 | 0 | −0.281 | −0.128 |
| Se | 0.386 * | 0.432 * | 0.376 * | 0.257 | 0.345 | 0.390 * | −0.325 | 4 | −0.195 | 0.143 |
| Rb | 0.464 * | 0.471 * | 0.468 * | 0.458 * | 0.549 ** | 0.581 ** | −0.355 | 6 | −0.223 | 0.301 |
| Sr | 0.300 | 0.338 | 0.368 | 0.290 | 0.310 | 0.369 | −0.313 | 0 | −0.255 | −0.082 |
| Mo | 0.189 | 0.269 | 0.242 | 0.111 | 0.164 | 0.218 | −0.035 | 0 | −0.136 | 0.237 |
| Ag | 0.530 ** | 0.471 * | 0.526 ** | 0.303 | 0.422 * | 0.466 * | −0.340 | 5 | −0.178 | 0.336 |
| Cd | 0.159 | 0.285 | 0.311 | 0.429 * | 0.436 * | 0.467 * | −0.187 | 3 | −0.006 | 0.137 |
| Sn | 0.090 | 0.030 | −0.148 | 0.244 | 0.196 | 0.216 | −0.201 | 0 | −0.118 | 0.216 |
| Sb | 0.171 | 0.218 | 0.090 | 0.070 | 0.057 | 0.136 | −0.271 | 0 | 0.037 | −0.070 |
| Cs | 0.576 ** | 0.597 ** | 0.526 ** | 0.495 ** | 0.618 ** | 0.664 ** | −0.403 * | 7 | −0.164 | 0.350 |
| Ba | 0.308 | 0.186 | 0.223 | 0.351 | 0.308 | 0.346 | −0.229 | 0 | −0.184 | −0.135 |
| Au | 0.526 ** | 0.622 ** | 0.578 ** | 0.292 | 0.424 * | 0.510 ** | −0.318 | 5 | −0.077 | 0.261 |
| Hg | 0.374 * | 0.346 | 0.206 | 0.338 | 0.393 * | 0.428 * | −0.359 | 3 | 0.161 | 0.209 |
| Tl | 0.374 * | 0.390 * | 0.402 * | 0.380 * | 0.427 * | 0.478 * | −0.240 | 6 | −0.309 | 0.167 |
| Pb | 0.402 * | 0.406 * | 0.548 ** | 0.393 * | 0.476 * | 0.499 ** | −0.151 | 6 | −0.041 | 0.260 |
| U | 0.121 | 0.190 | 0.339 | 0.045 | 0.032 | 0.111 | −0.104 | 0 | −0.126 | −0.044 |
| Starost_MR | 0.123 | 0.013 | −0.209 | 0.197 | 0.135 | 0.174 | 0.137 | 0 | −0.196 | 0.104 |
| Starost | 0.019 | −0.058 | −0.320 | 0.143 | 0.081 | 0.110 | 0.197 | 0 | −0.272 | 0.264 |
| Huckman index | 1 | 0.785 ** | 0.710 ** | 0.624 ** | 0.790 ** | 0.826 ** | −0.597 ** | 7 | −0.153 | 0.410 * |
| Evans index | 0.785 ** | 1 | 0.803 ** | 0.327 | 0.600 ** | 0.683 ** | −0.536 ** | 6 | −0.052 | 0.397 * |
| Bifrontal index | 0.710 ** | 0.803 ** | 1 | 0.408 * | 0.650 ** | 0.649 ** | −0.448 * | 7 | 0.053 | 0.281 |
| Bicaudate frontal indec | 0.624 ** | 0.327 | 0.408 * | 1 | 0.928 ** | 0.909 ** | −0.422 * | 6 | 0.059 | 0.188 |
| Bicaudate index | 0.790 ** | 0.600 ** | 0.650 ** | 0.928 ** | 1 | 0.979 ** | −0.517 ** | 7 | 0.065 | 0.364 |
| Bicaudate temporal index | 0.826 ** | 0.683 ** | 0.649 ** | 0.909 ** | 0.979 ** | 1 | −0.537 ** | 7 | 0.017 | 0.357 |
| Schiersmann index | −0.597 ** | −0.536 ** | −0.448 * | −0.422 * | −0.517 ** | −0.537 ** | 1 | 7 | 0.150 | −0.107 |
| (B) | ||||||||||
| Huckman Index | Evans Index | Bifrontal Index | Bicaudate Frontal Indec | Bicaudate Index | Bicaudate Temporal Index | Schiersmann Index | Number of Statistically Significant Correlations | Autism Deficit Score | Epilepsy Present | |
| Number of elevated metal concentrations | 0.515 ** | 0.535 ** | 0.574 ** | 0.389 * | 0.498 ** | 0.544 ** | −0.429 * | 7 (5 of them strong (p < 0.01, two-tailed) | −0.222 | 0.200 |
| Number of elevated metals, excluding essential | 0.532 ** | 0.549 ** | 0.587 ** | 0.370 * | 0.488 ** | 0.534 ** | −0.412 * | 6 (5 of them strong (p < 0.01, two-tailed) | −0.202 | 0.200 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mlinarič, M.; Jekovec Vrhovšek, M.; Neubauer, D.; France Štiglic, A.; Osredkar, J. Association between Autism Spectrum Disorder, Trace Elements, and Intracranial Fluid Spaces. Int. J. Mol. Sci. 2024, 25, 8050. https://doi.org/10.3390/ijms25158050
Mlinarič M, Jekovec Vrhovšek M, Neubauer D, France Štiglic A, Osredkar J. Association between Autism Spectrum Disorder, Trace Elements, and Intracranial Fluid Spaces. International Journal of Molecular Sciences. 2024; 25(15):8050. https://doi.org/10.3390/ijms25158050
Chicago/Turabian StyleMlinarič, Matej, Maja Jekovec Vrhovšek, David Neubauer, Alenka France Štiglic, and Joško Osredkar. 2024. "Association between Autism Spectrum Disorder, Trace Elements, and Intracranial Fluid Spaces" International Journal of Molecular Sciences 25, no. 15: 8050. https://doi.org/10.3390/ijms25158050





