Menstrual Blood Stem Cells-Derived Exosomes as Promising Therapeutic Tools in Premature Ovarian Insufficiency Induced by Gonadotoxic Systemic Anticancer Treatment
Abstract
:1. Introduction
2. Gonadotoxicity Induced by Systemic Anticancer Treatment in Women
3. Challenges in POI Induced by Systemic Anticancer Treatment
- i.
- Gonadotropin-releasing hormone agonists
- ii.
- Platelet-rich plasma therapy
- iii.
- Mesenchymal stem cell therapy
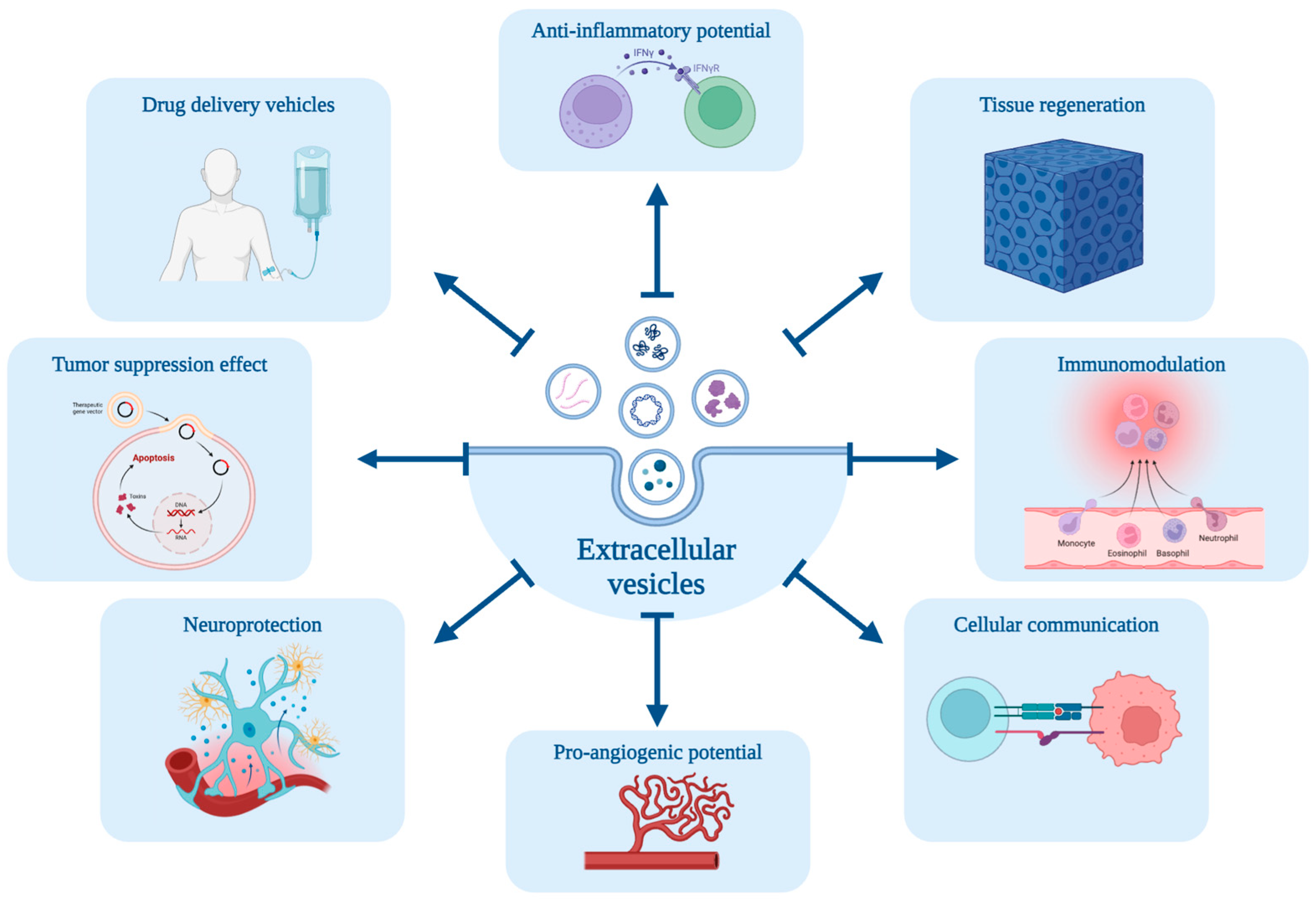
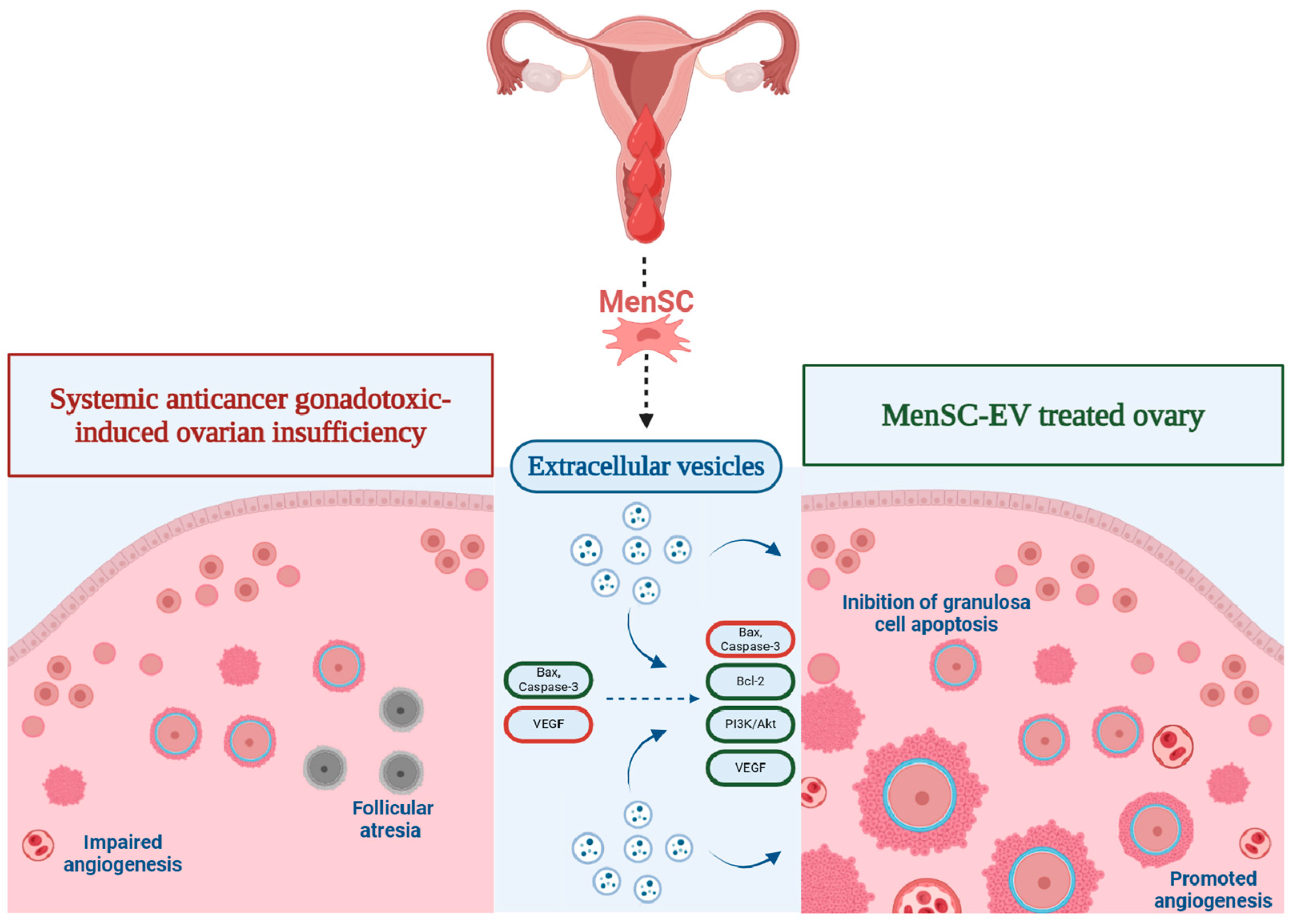
4. Clinical Potential of Extracellular Vesicles Derived from MenSC on Premature Ovarian Insufficiency
- i.
- Exosomes: These are small vesicles ranging from 30 to 150 nanometers in diameter. They originate from the endosomal system, specifically from the intraluminal vesicles formed within multivesicular bodies (MVB). Exosomes are released into the extracellular environment when MVB fuse with the plasma membrane [6].
- ii.
- Microvesicles: Also referred to as ectosomes, these vesicles vary from 100 to 1000 nanometers in diameter. They are generated through the outward budding and fission of the plasma membrane [6].
- iii.
- Apoptotic bodies: These are relatively larger vesicles, ranging from 500 to 2000 nanometers in diameter, formed during apoptosis. They encapsulate cellular debris and apoptotic fragments [6].
- (a)
- Isolation and characterization of EV derived from MenSC
- (b)
- Characterization of the isolated EV involves several advanced techniques.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, M.; Zhu, Q.; Huang, Y.; Tang, W.; Dai, J.; Guo, Y.; Xiong, J.; Zhang, J.; Zhou, S.; Fu, F.; et al. Ovarian reserve in reproductive-aged patients with cancer before gonadotoxic treatment: A systematic review and meta-analysis. Hum. Reprod. Open 2023, 2023, hoad024. [Google Scholar] [CrossRef] [PubMed]
- Karavani, G.; Rottenstreich, A.; Schachter-Safrai, N.; Cohen, A.; Weintraub, M.; Imbar, T.; Revel, A. Chemotherapy-based gonadotoxicity risk evaluation as a predictor of reproductive outcomes in post-pubertal patients following ovarian tissue cryopreservation. BMC Womens Health 2021, 21, 201. [Google Scholar] [CrossRef] [PubMed]
- Bedoschi, G.; Navarro, P.A.; Oktay, K. Chemotherapy-induced damage to ovary: Mechanisms and clinical impact. Future Oncol. 2016, 12, 2333–2344. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Li, X.; Zhang, Y.; Han, Y.; Chang, F.; Ding, J. Mesenchymal stem cells for regenerative medicine. Cells 2019, 8, 886. [Google Scholar] [CrossRef] [PubMed]
- Bozorgmehr, M.; Gurung, S.; Darzi, S.; Nikoo, S.; Kazemnejad, S.; Zarnani, A.H.; Gargett, C.E. Endometrial and Menstrual Blood Mesenchymal Stem/Stromal Cells: Biological Properties and Clinical Application. Front. Cell Dev. Biol. 2020, 8, 497. [Google Scholar] [CrossRef] [PubMed]
- Jeppesen, D.K.; Zhang, Q.; Franklin, J.L.; Coffey, R.J. Extracellular vesicles and nanoparticles: Emerging complexities. Trends Cell Biol. 2023, 33, 667–681. [Google Scholar] [CrossRef] [PubMed]
- de Pedro, M.Á.; López, E.; González-Nuño, F.M.; Pulido, M.; Álvarez, V.; Marchena, A.M.; Preußer, C.; Szymański, W.; Pogge von Strandmann, E.; Graumann, J.; et al. Menstrual blood-derived mesenchymal stromal cells: Impact of preconditioning on the cargo of extracellular vesicles as potential therapeutics. Stem Cell Res. Ther. 2023, 14, 187. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Yahaya, B.H.; Pan, Y.; Liu, Y.; Lin, J. Menstrual blood-derived endometrial stem cell, a unique and promising alternative in the stem cell-based therapy for chemotherapy-induced premature ovarian insufficiency. Stem Cell Res. Ther. 2023, 14, 327. [Google Scholar] [CrossRef] [PubMed]
- Lambertini, M.; Peccatori, F.A.; Demeestere, I.; Amant, F.; Wyns, C.; Stukenborg, J.B.; Paluch-Shimon, S.; Halaska, M.J.; Uzan, C.; Meissner, J.; et al. Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO Clinical Practice Guidelines. Ann. Oncol. 2020, 31, 1664–1678. [Google Scholar] [CrossRef] [PubMed]
- Imbert, R.; Moffa, F.; Tsepelidis, S.; Simon, P.; Delbaere, A.; Devreker, F.; Dechene, J.; Ferster, A.; Veys, I.; Fastrez, M.; et al. Safety and usefulness of cryopreservation of ovarian tissue to preserve fertility: A 12-year retrospective analysis. Hum. Reprod. 2014, 29, 1931–1940. [Google Scholar] [CrossRef] [PubMed]
- Meirow, D. Reproduction post-chemotherapy in young cancer patients. Mol. Cell. Endocrinol. 2000, 169, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Friedler, S.; Koc, O.; Gidoni, Y.; Raziel, A.; Ron-El, R. Ovarian response to stimulation for fertility preservation in women with malignant disease: A systematic review and meta-analysis. Fertil. Steril. 2012, 97, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Oktay, K.; Harvey, B.E.; Partridge, A.H.; Quinn, G.P.; Reinecke, J.; Taylor, H.S.; Wallace, W.H.; Wang, E.T.; Loren, A.W. Fertility Preservation in Patients with Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2018, 36, 1994–2001. [Google Scholar] [CrossRef] [PubMed]
- Shai, D.; Aviel-Ronen, S.; Spector, I.; Raanani, H.; Shapira, M.; Gat, I.; Roness, H.; Meirow, D. Ovaries of patients recently treated with alkylating agent chemotherapy indicate the presence of acute follicle activation, elucidating its role among other proposed mechanisms of follicle loss. Fertil. Steril. 2021, 115, 1239–1249. [Google Scholar] [CrossRef] [PubMed]
- Spears, N.; Lopes, F.; Stefansdottir, A.; Rossi, V.; De Felici, M.; Anderson, R.A.; Klinger, F.G. Ovarian damage from chemotherapy and current approaches to its protection. Hum. Reprod. Update 2019, 25, 673–693. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Qi, H.; Li, Z.; Bao, Y.; Yang, K.; Min, Q. Research progress on the premature ovarian failure caused by cisplatin therapy. Front. Oncol. 2023, 13, 1276310. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Wu, T.; Chen, D.; Wei, S.; Tang, W.; Xue, L.; Xiong, J.; Huang, Y.; Guo, Y.; Chen, Y.; et al. The effects and mechanism of taxanes on chemotherapy-associated ovarian damage: A review of current evidence. Front. Endocrinol. 2022, 13, 1025018. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Liu, J.; Chen, K.; Li, S.; Wang, Y.; Yang, Y.; Deng, H.; Jia, W.; Rao, N.; Liu, Q.; et al. What lies behind chemotherapy-induced amenorrhea for breast cancer patients: A meta-analysis. Breast Cancer Res. Treat. 2014, 145, 113–128. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.J.; Choi, Y.M.; Jun, J.K.; Lee, K.-H.; Kim, T.-Y.; Han, W.; Im, S.-A. Amenorrhea and menopause in patients with breast cancer after chemotherapy. J. Breast Cancer 2019, 22, 624–634. [Google Scholar] [CrossRef] [PubMed]
- Shandley, L.M.; Spencer, J.B.; Fothergill, A.; Mertens, A.C.; Manatunga, A.; Paplomata, E.; Howards, P.P. Impact of tamoxifen therapy on fertility in breast cancer survivors. Fertil. Steril. 2017, 107, 243–252.e5. [Google Scholar] [CrossRef] [PubMed]
- Himpe, J.; Lammerant, S.; Van den Bergh, L.; Lapeire, L.; De Roo, C. The Impact of Systemic Oncological Treatments on the Fertility of Adolescents and Young Adults—A Systematic Review. Life 2023, 13, 1209. [Google Scholar] [CrossRef] [PubMed]
- Ruddy, K.J.; Zheng, Y.; Tayob, N.; Hu, J.; Dang, C.T.; Yardley, D.A.; Isakoff, S.J.; Valero, V.V.; Faggen, M.G.; Mulvey, T.M.; et al. Chemotherapy-related amenorrhea (CRA) after adjuvant ado-trastuzumab emtansine (T-DM1) compared to paclitaxel in combination with trastuzumab (TH) (TBCRC033: ATEMPT Trial). Breast Cancer Res. Treat. 2021, 189, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Lambertini, M.; Ceppi, M.; Anderson, R.A.; Cameron, D.A.; Bruzzone, M.; Franzoi, M.A.; Massarotti, C.; El-Abed, S.; Wang, Y.; Lecocq, C.; et al. Impact of Anti-HER2 Therapy Alone and with Weekly Paclitaxel on the Ovarian Reserve of Young Women with HER2-Positive Breast Cancer. JNCCN J. Natl. Compr. Cancer Netw. 2023, 21, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Lambertini, M.; Campbell, C.; Bines, J.; Korde, L.A.; Izquierdo, M.; Fumagalli, D.; Del Mastro, L.; Ignatiadis, M.; Pritchard, K.; Wolff, A.C.; et al. Adjuvant Anti-HER2 Therapy, treatment-related amenorrhea, and survival in premenopausal HER2-positive early breast cancer patients. J. Natl. Cancer Inst. 2019, 111, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Imai, A.; Ichigo, S.; Matsunami, K.; Takagi, H.; Kawabata, I. Ovarian function following targeted anti-angiogenic therapy with bevacizumab. Mol. Clin. Oncol. 2017, 6, 807–810. [Google Scholar] [CrossRef] [PubMed]
- Ishizuka, B. Current Understanding of the Etiology, Symptomatology, and Treatment Options in Premature Ovarian Insufficiency (POI). Front. Endocrinol. 2021, 12, 626924. [Google Scholar] [CrossRef] [PubMed]
- Chon, S.J.; Umair, Z.; Yoon, M.S. Premature Ovarian Insufficiency: Past, Present, and Future. Front. Cell Dev. Biol. 2021, 9, 672890. [Google Scholar] [CrossRef] [PubMed]
- Hickey, M.; Szabo, R.A.; Hunter, M.S. Non-hormonal treatments for menopausal symptoms. BMJ (Clin. Res. Ed.) 2017, 359, j5101. [Google Scholar] [CrossRef]
- Piasecka-Srader, J.; Blanco, F.F.; Delman, D.H.; Dixon, D.A.; Geiser, J.L.; Ciereszko, R.E.; Petroff, B.K. Tamoxifen prevents apoptosis and follicle loss from cyclophosphamide in cultured rat ovaries. Biol. Reprod. 2015, 92, 132. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Turan, V.; Lierman, S.; Cuvelier, C.; De Sutter, P.; Oktay, K. Sphingosine-1-phosphate prevents chemotherapy-induced human primordial follicle death. Hum. Reprod. 2014, 29, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Moore, H.C.; Unger, J.M.; Phillips, K.A.; Boyle, F.; Hitre, E.; Porter, D.; Francis, P.A.; Goldstein, L.J.; Gomez, H.L.; Vallejos, C.S.; et al. Goserelin for Ovarian Protection during Breast-Cancer Adjuvant Chemotherapy. N. Engl. J. Med. 2015, 372, 923–932. [Google Scholar] [CrossRef] [PubMed]
- Duittoz, A.H.; Forni, P.E.; Giacobini, P.; Golan, M.; Mollard, P.; Negrón, A.L.; Radovick, S.; Wray, S. Development of the gonadotropin-releasing hormone system. J. Neuroendocrinol. 2022, 34, e13087. [Google Scholar] [CrossRef] [PubMed]
- Munhoz, R.R.; Pereira, A.A.; Sasse, A.D.; Hoff, P.M.; Traina, T.A.; Hudis, C.A.; Marques, R.J. Gonadotropin-releasing hormone agonists for ovarian function preservation in premenopausal women undergoing chemotherapy for early-stage breast cancer: A systematic review and meta-analysis. JAMA Oncol. 2016, 2, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Collins, T.; Alexander, D.; Barkatali, B. Platelet-rich plasma: A narrative review. EFORT Open Rev. 2021, 64, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Dehghani, F.; Aboutalebi, H.; Esmaeilpour, T.; Panjehshahin, M.R.; Bordbar, H. Effect of platelet-rich plasma (PRP) on ovarian structures in cyclophosphamide-induced ovarian failure in female rats: A stereological study. Toxicol. Mech. Methods 2018, 28, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Lv, S.; Guo, Z.; Gong, X.; Wang, C.; Zhang, X.; Meng, K. Potential Therapeutic Options for Premature Ovarian Insufficiency: Experimental and Clinical Evidence. Reprod. Sci. 2023, 30, 3428–3442. [Google Scholar] [CrossRef] [PubMed]
- Budak, Ö.; Bostancl, M.S.; Toprak, V.; Doǧanay, S.; Köse, O. Protective Effects of Platelet-rich plasma for in vitro Fertilization of Rats with Ovarian Failure Induced by Cyclophosphamide. Rev. Bras. Ginecol. Obstet. 2022, 44, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Liu, B.; Jiang, R.; Liao, S.; Wei, Z.; Bi, Y.; Liu, X.; Deng, R.; Jin, Y.; Tan, Y.; et al. G-CSF-mobilized peripheral blood mononuclear cells combined with platelet-rich plasma accelerate restoration of ovarian function in cyclophosphamide-induced POI rats. Biol. Reprod. 2019, 101, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Kolios, G.; Moodley, Y. Introduction to stem cells and regenerative medicine. Respiration 2012, 85, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Zhang, X.; Fan, Z.; Wang, Y.; Yao, G.; Wan, X.; Liu, Z.; Yang, B.; Yu, L. Human amniotic mesenchymal stem cells improve the follicular microenvironment to recover ovarian function in premature ovarian failure mice. Stem Cell Res. Ther. 2019, 10, 299. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, S.A.; Shalaby, S.; Brakta, S.; Elam, L.; Elsharoud, A.; Al-Hendy, A. Umbilical cord blood mesenchymal stem cells as an infertility treatment for chemotherapy induced premature ovarian insufficiency. Biomedicines 2019, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Su, J.; Ding, L.; Cheng, J.; Yang, J.; Li, X.; Yan, G.; Sun, H.; Dai, J.; Hu, Y. Transplantation of adipose-derived stem cells combined with collagen scaffolds restores ovarian function in a rat model of premature ovarian insufficiency. Hum. Reprod. 2016, 31, 1075–1086. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Lin, L.; Sha, C.; Li, T.; Zhao, D.; Wei, H.; Chen, Q.; Liu, Y.; Chen, X.; Xu, W.; et al. Bone marrow mesenchymal stem cell-derived exosomal miR-144-5p improves rat ovarian function after chemotherapy-induced ovarian failure by targeting PTEN. Lab. Investig. 2020, 100, 342–352. [Google Scholar] [CrossRef] [PubMed]
- Dalirfardouei, R.; Jamialahmadi, K.; Mahdipour, E. A feasible method for the isolation of mesenchymal stem cells from menstrual blood and their exosomes. Tissue Cell. 2018, 55, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Matsuzaka, Y.; Yashiro, R. Therapeutic Strategy of Mesenchymal-Stem-Cell-Derived Extracellular Vesicles as Regenerative Medicine. Int. J. Mol. Sci. 2022, 23, 6480. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Qu, J.; Mei, Q.; Chen, X.; Fang, Y.; Chen, L.; Li, Y.; Xiang, C. Small extracellular vesicles from menstrual blood-derived mesenchymal stem cells (MenSCs) as a novel therapeutic impetus in regenerative medicine. Stem Cell Res. Ther. 2021, 12, 433. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Xiang, B.; Wang, X.; Xiang, C. Exosomes derived from human menstrual blood-derived stem cells alleviate fulminant hepatic failure. Stem Cell Res. Ther. 2017, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Dai, J.; Su, Y.; Zhong, S.; Cong, L.; Liu, B.; Yang, J.; Tao, Y.; He, Z.; Chen, C.; Jiang, Y. Exosomes: Key players in cancer and potential therapeutic strategy. Signal Transduct. Target. Ther. 2020, 5, 145. [Google Scholar] [CrossRef]
- Xiao, S.; Du, J.; Yuan, G.; Luo, X.; Song, L. Granulosa Cells-Related MicroRNAs in Ovarian Diseases: Mechanism, Facts and Perspectives. Reprod. Sci. 2024. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Dong, Z.; Cao, Y.; Wang, H.; Liu, S.; Liao, L.; Jin, Y.; Yuan, L.; Li, B. MSC-Derived Exosome Promotes M2 Polarization and Enhances Cutaneous Wound Healing. Stem Cells Int. 2019, 2019, 7132708. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, R.; Asef-Kabiri, L.; Yousefi, H.; Sarvnaz, H.; Salehi, M.; Akbari, M.E.; Eskandari, N. The roles of tumor-derived exosomes in altered differentiation, maturation and function of dendritic cells. Mol. Cancer 2021, 20, 83. [Google Scholar] [CrossRef] [PubMed]
- Sohrabi, B.; Dayeri, B.; Zahedi, E.; Khoshbakht, S.; Pour, N.N.; Ranjbar, H.; Nejad, A.D.; Noureddini, M.; Alani, B. Mesenchymal stem cell (MSC)-derived exosomes as novel vehicles for delivery of miRNAs in cancer therapy. Cancer Gene Ther. 2022, 29, 1105–1116. [Google Scholar] [CrossRef] [PubMed]
- Song, A.; Zhang, S.; Zhao, X.; Wu, S.; Qi, X.; Gao, S.; Qi, J.; Li, P.; Tan, J. Exosomes derived from menstrual blood stromal cells ameliorated premature ovarian insufficiency and granulosa cell apoptosis by regulating SMAD3/AKT/MDM2/P53 pathway via delivery of thrombospondin-1. Biomed. Pharmacother. 2023, 166, 115319. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Huang, B.; Su, P.; Chang, Q.; Li, P.; Song, A.; Zhao, X.; Yuan, Z.; Tan, J. Concentrated exosomes from menstrual blood-derived stromal cells improves ovarian activity in a rat model of premature ovarian insufficiency. Stem Cell Res. Ther. 2021, 12, 178. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, S.; Qi, J.; Zhao, F.; Lu, Y.; Li, S.; Wu, S.; Li, P.; Tan, J. PDGFBB improved the biological function of menstrual blood-derived stromal cells and the anti-fibrotic properties of exosomes. Stem Cell Res. Ther. 2023, 14, 113. [Google Scholar] [CrossRef] [PubMed]
- Qi, J.; Zhang, X.; Zhang, S.; Wu, S.; Lu, Y.; Li, S.; Li, P.; Tan, J. P65 mediated UBR4 in exosomes derived from menstrual blood stromal cells to reduce endometrial fibrosis by regulating YAP Ubiquitination. J. Nanobiotechnol. 2023, 21, 305. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Liu, D. The function of exosomes in ovarian granulosa cells. Cell Tissue Res. 2023, 394, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Shi, B.; Deng, W.; Long, X.; Zhao, R.; Wang, Y.; Chen, W.; Xu, G.; Sheng, J.; Wang, D.; Cao, S. miR-21 increases c-kit++ cardiac stem cell proliferation in vitro through PTEN/PI3K/Akt signaling. PeerJ 2017, 5, e2859. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Zhou, Y.; Li, H.J. Advances in mesenchymal stem cell exosomes: A review. Stem Cell Res. Ther. 2021, 12, 71. [Google Scholar] [CrossRef]
- Chen, Z.; Li, Y.; Yu, H.; Shen, Y.; Ju, C.; Ma, G.; Liu, Y.; Kim, I.M.; Weintraub, N.L.; Tang, Y. Isolation of Extracellular Vesicles from Stem Cells. Methods Mol. Biol. 2017, 1660, 389–394. [Google Scholar] [PubMed]
- Chen, Y.; Qian, H.; Mak, M.; Tao, Z. Protocol for isolating and identifying small extracellular vesicles derived from human umbilical cord mesenchymal stem cells. STAR Protoc. 2024, 5, 103197. [Google Scholar] [CrossRef]
| Damaging Effects of Chemotherapy | Potential Protectants |
|---|---|
| Accelerated PMF activation | AMH Crocetin Immunomodulator AS101 Melatonin, Ghrelin mTOR inhibitors |
| Follicular atresia | Antioxidants Bortezomib Dexrazoxane G-CSF LH Imatinib Melatonin, Ghrelin Sphingolipids |
| Damage to ovarian vasculature | G-CSF Sphingolipids |
| Direct loss of PMF | ATM, ATR inhibitors CK1, CHK2 inhibitors LH Sphingolipids Tamoxifen Tyrosine kinase inhibitors |
| Ovarian inflammation | Tamoxifen |
| Aspect | Platelet-Rich Plasma | Mesenchymal Stem Cells | MSC-Derived Exosomes |
|---|---|---|---|
| Source | Autologous (patient’s own blood) | Bone marrow Adipose tissue Umbilical cord blood | Harvested from culture medium of MSC |
| Tumorigenic Potential | Low risk of tumor recurrence | Potential to influence tumor growth; can promote or inhibit cancer depending on the microenvironment and source | Lower risk of tumorigenesis compared to whole MSC; potential to influence tumor biology |
| Immunogenicity | Minimal risk of immunogenic reactions or disease transmission | Risk of immune rejection or graft-versus-host disease, particularly with allogeneic MSC | Reduced risk of immune rejection or adverse immune responses compared to whole MSC |
| Common Side Effects | Pain at injection site Infection Local inflammation | Infection Thrombosis Ectopic tissue formation | Inflammatory responses (less severe than those associated with cellular therapies) |
| Safety Summary | Considered safe with minimal immunogenic risks; favorable for cancer survivors | Higher risk due to potential tumorigenicity and immunomodulatory effects | Safer than whole MSC with lower immunogenic and tumorigenic risks; long-term effects and optimal dosing require further study |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robalo Cordeiro, M.; Roque, R.; Laranjeiro, B.; Carvalhos, C.; Figueiredo-Dias, M. Menstrual Blood Stem Cells-Derived Exosomes as Promising Therapeutic Tools in Premature Ovarian Insufficiency Induced by Gonadotoxic Systemic Anticancer Treatment. Int. J. Mol. Sci. 2024, 25, 8468. https://doi.org/10.3390/ijms25158468
Robalo Cordeiro M, Roque R, Laranjeiro B, Carvalhos C, Figueiredo-Dias M. Menstrual Blood Stem Cells-Derived Exosomes as Promising Therapeutic Tools in Premature Ovarian Insufficiency Induced by Gonadotoxic Systemic Anticancer Treatment. International Journal of Molecular Sciences. 2024; 25(15):8468. https://doi.org/10.3390/ijms25158468
Chicago/Turabian StyleRobalo Cordeiro, Mariana, Ricardo Roque, Bárbara Laranjeiro, Carlota Carvalhos, and Margarida Figueiredo-Dias. 2024. "Menstrual Blood Stem Cells-Derived Exosomes as Promising Therapeutic Tools in Premature Ovarian Insufficiency Induced by Gonadotoxic Systemic Anticancer Treatment" International Journal of Molecular Sciences 25, no. 15: 8468. https://doi.org/10.3390/ijms25158468





