Obesity-Related Ciliopathies: Focus on Advances of Biomarkers
Abstract
:1. Introduction
1.1. Primary Cilia and Obesity
1.2. Obesity-Related Ciliopathies
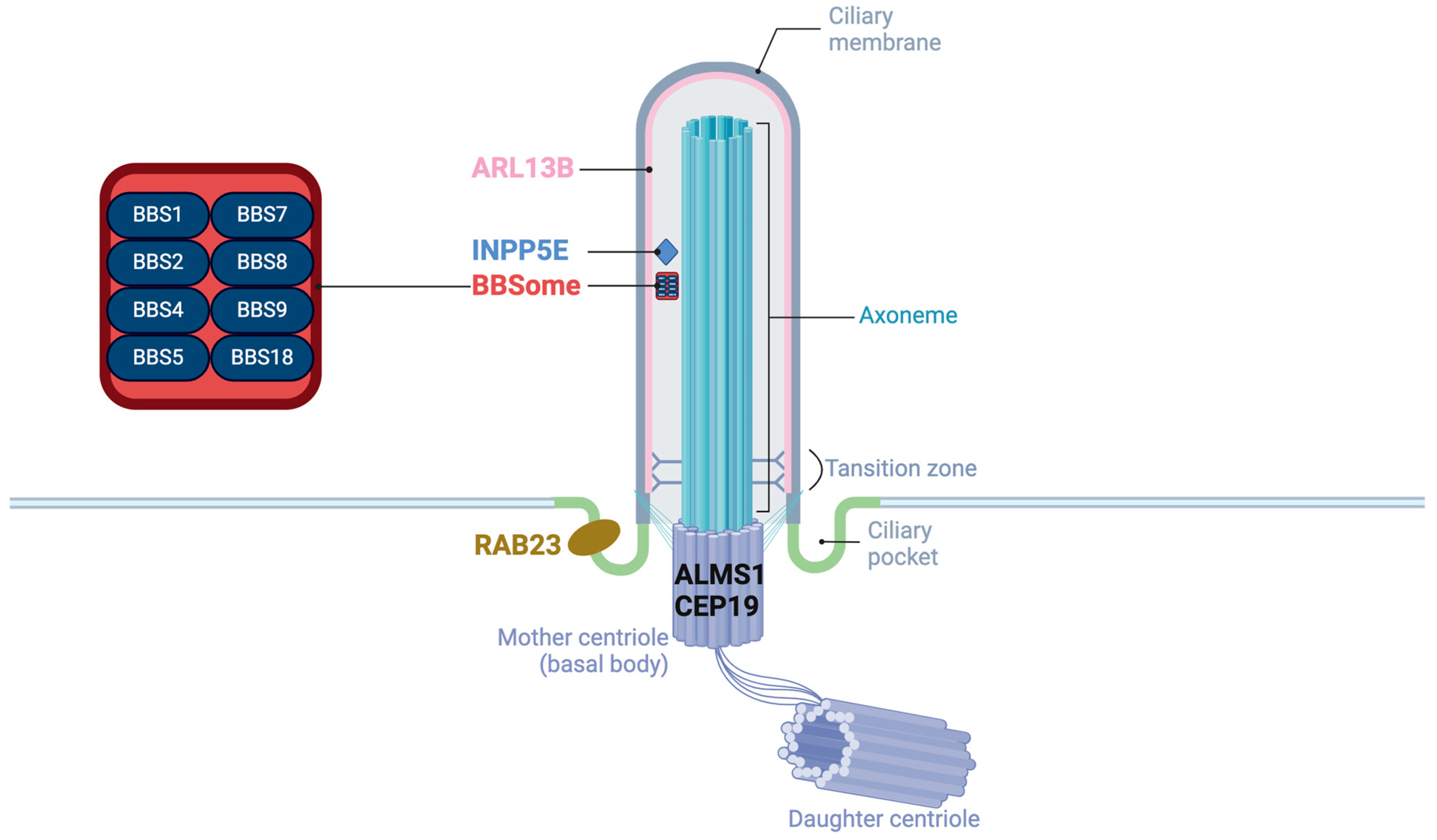
1.2.1. Localization and Functions in Cilia
1.2.2. Clinical Presentations, Diagnosis, and Treatment
1.2.3. Characteristics of Obesity
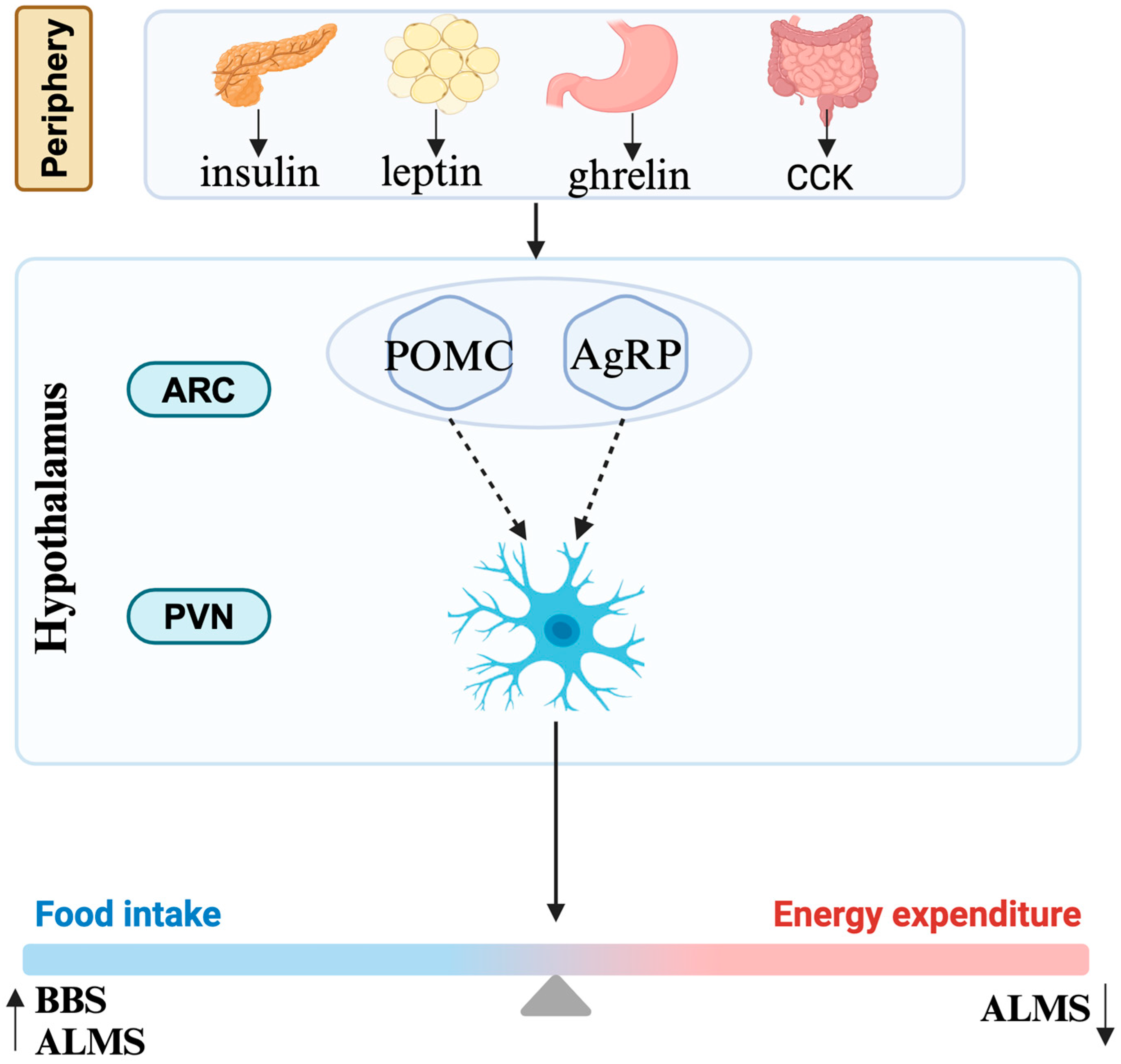
1.2.4. Mechanism of Obesity
2. Advance of Biomarkers
2.1. Diagnosis and Differential Diagnosis
2.2. Variability in Clinical Presentation, Progress, and Prognosis
2.2.1. Genotype–Phenotype Correlation
2.2.2. Other Biomarkers from Multi-Omics Data
| Clinical Features | Correlation Detection | Biomarkers/Specific Methods | Comment | References | |
|---|---|---|---|---|---|
| Fatty liver | Imaging analysis | SWE, TE | SWE plays an important predictive role in the progression of fatty liver to fibrosis in patients with ALMS | Silvia et al. [62] | |
| Metabolomics | ALT/AST ratio, APRI, FIB-4 | Predicts liver fibrosis in liver disease to some extent | Guangqin et al. [63], Erin et al. [64] | ||
| Cardiomyopathy | Imaging analysis | ECV | ECV expansion might be a more robust predictor of adverse cardiovascular outcomes | Nicola et al. [66] | |
| Metabolomics | NT-proBNP, high-sensitivity troponin, elevated triglycerides | Elevated triglycerides are proposed as a potential marker for cardiac fibrosis | Ashwin et al. [65], Nicola et al. [66] | ||
| Kidney | Proteomics | u-FN, CD44 antigen, lysosomal α-glucosidase | u-FN, CD44 antigen, and lysosomal α-glucosidase significantly correlated with glomerular filtration rate | Marianna et al. [75] | |
| Fibrosis | MiRNA sequencing | miRNAs (miR-324-5p, miR-27a, miR-27b, miR-29b, and miR-25) | MiRNAs could potentially serve as biomarkers for fibrosis in ALMS | Merlin et al. [73] | |
| Obesity and related metabolic syndromes | MiRNA sequencing | miRNAs (miR-30a-5p, miR-92b-3p, miR-99a-5p, miR-122-5p, miR-192-5p, miR-193a-5p, miR-199a-3p, and miR-205-5p) | MiR-301a-3p expression was significantly reduced in both ALMS and BBS patients; miR-92b-3p expression was decreased in ALMS but increased in BBS; miRNAs could serve as valuable biomarkers of disease progression in patients with ALMS and BBS | Agnieszka et al. [67] | |
| Metabolomics | Non-targeted metabolomics analysis | PC, LPE, long-chain fatty acid (FA 26:1; O2), acylcarnitines, tetrahydroaldosterone-3-glucuronide | LPEs are major markers of disease progression; only long-chain fatty acid (FA 26:1; O2) showed a negative correlation with age in ALMS and BBS patients | Krzysztof et al. [68] | |
| Serum bone metabolism marker testing | OC, DPD, s-RANKL | OC and DPD levels were negatively correlated with the HOMA-IR index | Krzysztof et al. [72] | ||
3. Discussion
4. Conclusions
5. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| GWAS | Genome-wide association studies |
| ADCY3 | Adenylate cyclase 3 |
| MC4R | Melanocortin 4 Receptor |
| GLP-1 | Glucagon-like Peptide-1 |
| BBS | Bardet–Biedl syndrome |
| ALMS | Alström syndrome |
| CRPT | Carpenter syndrome |
| MORMS | Mental retardation, truncal obesity, retinal dystrophy, and micropenis syndrome |
| MOSPGF | Morbid obesity and spermatogenic failure |
| JBTS | Joubert syndrome |
| HGMD | Human Gene Mutation Database |
| IFT | Intraflagellar transport |
| Shh | Sonic Hedgehog |
| Hh | Hedgehog |
| BMI | Body mass index |
| AgRP | Agouti-related protein |
| POMC | Pro-opiomelanocortin |
| NGS | Next-generation sequencing |
| ACMG | American College of Medical Genetics and Genomics |
| VUS | Variant of uncertain significance |
| DCM | Dilated cardiomyopathy |
| HCM | Hypertrophic cardiomyopathy |
| T2DM | Type 2 diabetes mellitus |
| NAFLD | Non-alcoholic fatty liver disease |
| ALT | Alanine aminotransferase |
| AST | Aspartate aminotransferase |
| APRI | AST-to-platelet ratio index |
| FIB-4 | Fibrosis-4 Index |
| TE | Transient elastography |
| SWE | Shear-wave elastography |
| NT-proBNP | N-terminal pro-brain natriuretic peptide |
| ECV | Extracellular volume |
| miRNA | MicroRNA |
| HOMA-IR | Homeostasis Model Assessment of Insulin Resistance |
| HbA1c | Glycated Hemoglobin A1c |
| PC | Phosphatidylcholine |
| LPE | Lysophosphatidylethanolamine |
| FA | Fatty acid |
| OC | Osteocalcin |
| DPD | Deoxypyridinoline |
| s-RANKL | Serum receptor activator of nuclear factor kappa-Β ligand |
| CKD | Chronic kidney disease |
| DTI | Diffusion tensor imaging |
| u-FN | Urinary fibronectin |
| GFR | Glomerular filtration rate |
| max-Uosm | Maximum urine osmolality |
| ΔeGFR | Estimated glomerular filtration rate |
| WES | Whole-exome sequencing |
| PCR | Polymerase chain reaction |
| AMI | Acute myocardial infarction |
| CCK | Cholecystokinin |
| ARC | Arcuate nucleus |
| PVN | Paraventricular nucleus |
References
- Wallmeier, J.; Nielsen, K.G.; Kuehni, C.E.; Lucas, J.S.; Leigh, M.W.; Zariwala, M.A.; Omran, H. Motile ciliopathies. Nat. Rev. Dis. Primers 2020, 6, 77. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wen, X.; Wang, Z.; Lin, Z.; Li, C.; Zhou, H.; Yu, H.; Li, Y.; Cheng, Y.; Chen, Y.; et al. Ciliary transition zone proteins coordinate ciliary protein composition and ectosome shedding. Nat. Commun. 2022, 13, 3997. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.; Ullah, R.; Wang, J.B.; Fu, J.F. Trends of obesity and overweight among children and adolescents in China. World J. Pediatr. 2023, 19, 1115–1126. [Google Scholar] [CrossRef] [PubMed]
- World Obesity Atlas 2023. Available online: https://www.worldobesityday.org/assets/downloads/ (accessed on 31 July 2024).
- Siljee, J.E.; Wang, Y.; Bernard, A.A.; Ersoy, B.A.; Zhang, S.; Marley, A.; Von Zastrow, M.; Reiter, J.F.; Vaisse, C. Subcellular localization of MC4R with ADCY3 at neuronal primary cilia underlies a common pathway for genetic predisposition to obesity. Nat. Genet. 2018, 50, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Vaisse, C.; Reiter, J.F.; Berbari, N.F. Cilia and Obesity. Cold Spring Harb. Perspect. Biol. 2017, 9, a028217. [Google Scholar] [CrossRef] [PubMed]
- Engle, S.E.; Bansal, R.; Antonellis, P.J.; Berbari, N.F. Cilia signaling and obesity. Semin. Cell Dev. Biol. 2021, 110, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Lovera, M.; Lüders, J. The ciliary impact of nonciliary gene mutations. Trends Cell Biol. 2021, 31, 876–887. [Google Scholar] [CrossRef] [PubMed]
- Reiter, J.F.; Leroux, M.R. Genes and molecular pathways underpinning ciliopathies. Nat. Rev. Mol. Cell Biol. 2017, 18, 533–547. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, F.; Benzing, T.; Katsanis, N. Ciliopathies. N. Engl. J. Med. 2011, 364, 1533–1543. [Google Scholar] [CrossRef]
- Tobin, J.L.; Beales, P.L. The nonmotile ciliopathies. Genet. Med. 2009, 11, 386–402. [Google Scholar] [CrossRef]
- Legendre, M.; Zaragosi, L.-E.; Mitchison, H.M. Motile cilia and airway disease. Semin. Cell Dev. Biol. 2021, 110, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.D.; Beck, S.; Maffei, P.; Naggert, J.K. Alström Syndrome. Eur. J. Hum. Genet. 2007, 15, 1193–1202. [Google Scholar] [CrossRef] [PubMed]
- Forsythe, E.; Beales, P.L. Bardet-Biedl syndrome. Eur. J. Hum. Genet. 2013, 21, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Twigg, S.R.F.; Lloyd, D.; Jenkins, D.; Elçioglu, N.E.; Cooper, C.D.O.; Al-Sannaa, N.; Annagür, A.; Gillessen-Kaesbach, G.; Hüning, I.; Knight, S.J.L.; et al. Mutations in multidomain protein MEGF8 identify a Carpenter syndrome subtype associated with defective lateralization. Am. J. Hum. Genet. 2012, 91, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Hampshire, D.J.; Ayub, M.; Springell, K.; Roberts, E.; Jafri, H.; Rashid, Y.; Bond, J.; Riley, J.H.; Woods, C.G. MORM syndrome (mental retardation, truncal obesity, retinal dystrophy and micropenis), a new autosomal recessive disorder, links to 9q34. Eur. J. Hum. Genet. 2006, 14, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Shalata, A.; Ramirez, M.C.; Desnick, R.J.; Priedigkeit, N.; Buettner, C.; Lindtner, C.; Mahroum, M.; Abdul-Ghani, M.; Dong, F.; Arar, N.; et al. Morbid obesity resulting from inactivation of the ciliary protein CEP19 in humans and mice. Am. J. Hum. Genet. 2013, 93, 1061–1071. [Google Scholar] [CrossRef] [PubMed]
- Katsanis, N.; Ansley, S.J.; Badano, J.L.; Eichers, E.R.; Lewis, R.A.; Hoskins, B.E.; Scambler, P.J.; Davidson, W.S.; Beales, P.L.; Lupski, J.R. Triallelic inheritance in Bardet-Biedl syndrome, a Mendelian recessive disorder. Science 2001, 293, 2256–2259. [Google Scholar] [CrossRef] [PubMed]
- Paisey, R.B.; Steeds, R.; Barrett, T.; Williams, D.; Geberhiwot, T.; Gunay-Aygun, M. Alström Syndrome. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. Available online: http://www.ncbi.nlm.nih.gov/books/NBK1267/ (accessed on 25 April 2024).
- Marshall, J.D.; Maffei, P.; Collin, G.B.; Naggert, J.K. Alström Syndrome: Genetics and Clinical Overview. Curr. Genom. 2011, 12, 225–235. [Google Scholar] [CrossRef]
- Marshall, J.D.; Bronson, R.T.; Collin, G.B.; Nordstrom, A.D.; Maffei, P.; Paisey, R.B.; Carey, C.; MacDermott, S.; Russell-Eggitt, I.; Shea, S.E.; et al. New Alström Syndrome Phenotypes Based on the Evaluation of 182 Cases. Arch. Intern. Med. 2005, 165, 675–683. [Google Scholar] [CrossRef]
- Bea-Mascato, B.; Valverde, D. Genotype–phenotype associations in Alström syndrome: A systematic review and meta-analysis. J. Med. Genet. 2024, 61, 18–26. [Google Scholar] [CrossRef]
- Melluso, A.; Secondulfo, F.; Capolongo, G.; Capasso, G.; Zacchia, M. Bardet-Biedl Syndrome: Current Perspectives and Clinical Outlook. Ther. Clin. Risk Manag. 2023, 19, 115–132. [Google Scholar] [CrossRef] [PubMed]
- Forsyth, R.; Gunay-Aygun, M. Bardet-Biedl Syndrome Overview. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. Available online: http://www.ncbi.nlm.nih.gov/books/NBK1363/ (accessed on 27 April 2024).
- Bouaré, F.; Noureldine, M.H.A.; Hajhouji, F.; Ghannane, H.; Jallo, G.I.; Benali, S.A. Complex craniosynostosis in the context of Carpenter’s syndrome. Childs Nerv. Syst. ChNS Off. J. Int. Soc. Pediatr. Neurosurg. 2022, 38, 831–835. [Google Scholar] [CrossRef] [PubMed]
- Hidestrand, P.; Vasconez, H.; Cottrill, C. Carpenter syndrome. J. Craniofac. Surg. 2009, 20, 254–256. [Google Scholar] [CrossRef] [PubMed]
- Temtamy, S.A. Carpenter’s syndrome: Acrocephalopolysyndactyly. An autosomal recessive syndrome. J. Pediatr. 1966, 69, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.; Seelow, D.; Jehee, F.S.; Perlyn, C.A.; Alonso, L.G.; Bueno, D.F.; Donnai, D.; Josifova, D.; Mathijssen, I.M.J.; Morton, J.E.V.; et al. RAB23 Mutations in Carpenter Syndrome Imply an Unexpected Role for Hedgehog Signaling in Cranial-Suture Development and Obesity. Am. J. Hum. Genet. 2007, 80, 1162–1170. [Google Scholar] [CrossRef] [PubMed]
- Khairat, R.; Elhossini, R.; Sobreira, N.; Wohler, E.; Otaify, G.; Mohamed, A.M.; Raouf, E.R.A.; Sayed, I.; Aglan, M.; Ismail, S.; et al. Expansion of the phenotypic and mutational spectrum of Carpenter syndrome. Eur. J. Med. Genet. 2022, 65, 104377. [Google Scholar] [CrossRef]
- Jacoby, M.; Cox, J.J.; Gayral, S.; Hampshire, D.J.; Ayub, M.; Blockmans, M.; Pernot, E.; Kisseleva, M.V.; Compère, P.; Schiffmann, S.N.; et al. INPP5E mutations cause primary cilium signaling defects, ciliary instability and ciliopathies in human and mouse. Nat. Genet. 2009, 41, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Drole Torkar, A.; Avbelj Stefanija, M.; Bertok, S.; Podkrajšek, K.T.; Debeljak, M.; Kranjc, B.S.; Battelino, T.; Kotnik, P. Novel Insights Into Monogenic Obesity Syndrome Due to INPP5E Gene Variant: A Case Report of a Female Patient. Front. Endocrinol. 2021, 12, 581134. [Google Scholar] [CrossRef]
- Thomas, S.; Cantagrel, V.; Mariani, L.; Serre, V.; Lee, J.-E.; Elkhartoufi, N.; de Lonlay, P.; Desguerre, I.; Munnich, A.; Boddaert, N.; et al. Identification of a novel ARL13B variant in a Joubert syndrome-affected patient with retinal impairment and obesity. Eur. J. Hum. Genet. 2015, 23, 621–627. [Google Scholar] [CrossRef]
- Hearn, T.; Spalluto, C.; Phillips, V.J.; Renforth, G.L.; Copin, N.; Hanley, N.A.; Wilson, D.I. Subcellular localization of ALMS1 supports involvement of centrosome and basal body dysfunction in the pathogenesis of obesity, insulin resistance, and type 2 diabetes. Diabetes 2005, 54, 1581–1587. [Google Scholar] [CrossRef]
- The CEP19-RABL2 GTPase Complex Binds IFT-B to Initiate Intraflagellar Transport at the Ciliary Base—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/28625565/ (accessed on 29 June 2024).
- Gerondopoulos, A.; Strutt, H.; Stevenson, N.L.; Sobajima, T.; Levine, T.P.; Stephens, D.J.; Strutt, D.; Barr, F.A. Planar Cell Polarity Effector Proteins Inturned and Fuzzy Form a Rab23 GEF Complex. Curr. Biol. 2019, 29, 3323–3330.e8. [Google Scholar] [CrossRef] [PubMed]
- Bardet-Biedl Syndrome: Genetics, Molecular Pathophysiology, and Disease Management—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/27853007/ (accessed on 21 July 2024).
- Gupta, N.; D’Acierno, M.; Zona, E.; Capasso, G.; Zacchia, M. Bardet–Biedl syndrome: The pleiotropic role of the chaperonin-like BBS6, 10, and 12. Proteins 2022, 190, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Niederlova, V.; Modrak, M.; Tsyklauri, O.; Huranova, M.; Stepanek, O. Meta-analysis of genotype-phenotype associations in Bardet-Biedl syndrome uncovers differences among causative genes. Hum. Mutat. 2019, 40, 2068–2087. [Google Scholar] [CrossRef] [PubMed]
- Ferent, J.; Constable, S.; Gigante, E.D.; Yam, P.T.; Mariani, L.E.; Legué, E.; Liem, K.F., Jr.; Caspary, T.; Charron, F. The Ciliary Protein Arl13b Functions Outside of the Primary Cilium in Shh-Mediated Axon Guidance. Cell Rep. 2019, 29, 3356–3366.e3. [Google Scholar] [CrossRef] [PubMed]
- Whiting, K.R.; Haer-Wigman, L.; Florijn, R.J.; van Beek, R.; Oud, M.M.; Plomp, A.S.; Boon, C.J.F.; Kroes, H.Y.; Roepman, R. Utilization of automated cilia analysis to characterize novel INPP5E variants in patients with non-syndromic retinitis pigmentosa. Eur. J. Hum. Genet. 2024. [Google Scholar] [CrossRef] [PubMed]
- Kopinke, D.; Norris, A.M.; Mukhopadhyay, S. Developmental and regenerative paradigms of cilia regulated hedgehog signaling. Semin. Cell Dev. Biol. 2021, 110, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Ding, Y.; Feng, B.; Tang, Y.; Chen, Y.; Wang, Y.; Chang, G.; Liu, S.; Wang, J.; Li, Q.; et al. Molecular and Phenotypic Expansion of Alström Syndrome in Chinese Patients. Front. Genet. 2022, 13, 808919. [Google Scholar] [CrossRef]
- Mujahid, S.; Hunt, K.F.; Cheah, Y.S.; Forsythe, E.; Hazlehurst, J.M.; Sparks, K.; Mohammed, S.; Tomlinson, J.W.; Amiel, S.A.; Carroll, P.V.; et al. The Endocrine and Metabolic Characteristics of a Large Bardet-Biedl Syndrome Clinic Population. J. Clin. Endocrinol. Metab. 2018, 103, 1834–1841. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.W. The characterization and comorbidities of heterozygous Bardet-Biedl syndrome carriers. Int. J. Med. Sci. 2024, 21, 784–794. [Google Scholar] [CrossRef]
- Meyer, J.R.; Krentz, A.D.; Berg, R.L.; Richardson, J.G.; Pomeroy, J.; Hebbring, S.J.; Haws, R.M. Kidney failure in Bardet–Biedl syndrome. Clin. Genet. 2022, 101, 429–441. [Google Scholar] [CrossRef]
- Forsythe, E.; Kenny, J.; Bacchelli, C.; Beales, P.L. Managing Bardet-Biedl Syndrome-Now and in the Future. Front. Pediatr. 2018, 6, 23. [Google Scholar] [CrossRef] [PubMed]
- Faccioli, N.; Poitou, C.; Clément, K.; Dubern, B. Current Treatments for Patients with Genetic Obesity. J. Clin. Res. Pediatr. Endocrinol. 2023, 15, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Haws, R.M.; Gordon, G.; Han, J.C.; Yanovski, J.A.; Yuan, G.; Stewart, M.W. The efficacy and safety of setmelanotide in individuals with Bardet-Biedl syndrome or Alström syndrome: Phase 3 trial design. Contemp. Clin. Trials Commun. 2021, 22, 100780. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Baig, S.; Wanninayake, S.; da Silva Xavier, G.; Dawson, C.; Paisey, R.; Geberhiwot, T. Glucagon-like peptide-1 analogues in monogenic syndromic obesity: Real-world data from a large cohort of Alström syndrome patients. Diabetes Obes. Metab. 2024, 26, 989–996. [Google Scholar] [CrossRef] [PubMed]
- Markham, A. Setmelanotide: First Approval. Drugs 2021, 81, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Trapp, C.M.; Censani, M. Setmelanotide: A promising advancement for pediatric patients with rare forms of genetic obesity. Curr. Opin. Endocrinol. Diabetes Obes. 2023, 30, 136–140. [Google Scholar] [CrossRef]
- Brüning, J.C.; Fenselau, H. Integrative neurocircuits that control metabolism and food intake. Science 2023, 381, eabl7398. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Lechtreck, K.F. The Bardet-Biedl syndrome protein complex is an adapter expanding the cargo range of intraflagellar transport trains for ciliary export. Proc. Natl. Acad. Sci. USA 2018, 115, E934–E943. [Google Scholar] [CrossRef] [PubMed]
- Loktev, A.V.; Jackson, P.K. Neuropeptide Y family receptors traffic via the Bardet-Biedl syndrome pathway to signal in neuronal primary cilia. Cell Rep. 2013, 5, 1316–1329. [Google Scholar] [CrossRef]
- Stephenson, E.J.; Kinney, C.E.; Stayton, A.S.; Han, J.C. Energy expenditure deficits drive obesity in a mouse model of Alström syndrome. Obesity 2023, 31, 2786–2798. [Google Scholar] [CrossRef]
- Hearn, T. ALMS1 and Alström syndrome: A recessive form of metabolic, neurosensory and cardiac deficits. J. Mol. Med. 2019, 97, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Xuan, J.; Yu, Y.; Qing, T.; Guo, L.; Shi, L. Next-generation sequencing in the clinic: Promises and challenges. Cancer Lett. 2013, 340, 284–295. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.D.; Muller, J.; Collin, G.B.; Milan, G.; Kingsmore, S.F.; Dinwiddie, D.; Farrow, E.G.; Miller, N.A.; Favaretto, F.; Maffei, P.; et al. Alström Syndrome: Mutation spectrum of ALMS1. Hum. Mutat. 2015, 36, 660–668. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.H.; Geberhiwot, T.; Barrett, T.G.; Paisey, R.; Semple, R.K. Refining genotype-phenotype correlation in Alström syndrome through study of primary human fibroblasts. Mol. Genet. Genomic. Med. 2017, 5, 390–404. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.D.; Hinman, E.G.; Collin, G.B.; Beck, S.; Cerqueira, R.; Maffei, P.; Milan, G.; Zhang, W.; Wilson, D.I.; Hearn, T.; et al. Spectrum of ALMS1 variants and evaluation of genotype-phenotype correlations in Alström syndrome. Hum. Mutat. 2007, 28, 1114–1123. [Google Scholar] [CrossRef] [PubMed]
- Dedeoglu, S.; Dede, E.; Oztunc, F.; Gedikbasi, A.; Yesil, G.; Dedeoglu, R. Mutation identification and prediction for severe cardiomyopathy in Alström syndrome, and review of the literature for cardiomyopathy. Orphanet. J. Rare Dis. 2022, 17, 359. [Google Scholar] [CrossRef] [PubMed]
- Bettini, S.; Bombonato, G.; Dassie, F.; Favaretto, F.; Piffer, L.; Bizzotto, P.; Busetto, L.; Chemello, L.; Senzolo, M.; Merkel, C.; et al. Liver Fibrosis and Steatosis in Alström Syndrome: A Genetic Model for Metabolic Syndrome. Diagnostics 2021, 11, 797. [Google Scholar] [CrossRef] [PubMed]
- Xiao, G.; Zhu, S.; Xiao, X.; Yan, L.; Yang, J.; Wu, G. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: A meta-analysis. Hepatology 2017, 66, 1486–1501. [Google Scholar] [CrossRef]
- Cleveland, E.; Bandy, A.; VanWagner, L.B. Diagnostic challenges of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Clin. Liver. Dis. 2018, 11, 98–104. [Google Scholar] [CrossRef]
- Roy, A.; Patel, L.; Yuan, M.; O'Shea, C.; Alvior, A.M.B.; Charalambides, M.; Moxon, D.; Baig, S.; Bunting, K.V.; Gehmlich, K.; et al. Defining the cardiovascular phenotype of adults with Alström syndrome. Int. J. Cardiol. 2024, 409, 132212. [Google Scholar] [CrossRef]
- Edwards, N.C.; Moody, W.E.; Yuan, M.; Warfield, A.T.; Cramb, R.; Paisey, R.B.; Geberhiwot, T.; Steeds, R.P. Diffuse Left Ventricular Interstitial Fibrosis Is Associated With Sub-Clinical Myocardial Dysfunction in Alström Syndrome: An Observational Study. Orphanet J. Rare Dis. 2015, 10, 83. [Google Scholar] [CrossRef] [PubMed]
- Zmyslowska, A.; Smyczynska, U.; Stanczak, M.; Jeziorny, K.; Szadkowska, A.; Fendler, W.; Borowiec, M. Association of circulating miRNAS in patients with Alstrőm and Bardet-Biedl syndromes with clinical course parameters. Front. Endocrinol. 2022, 13, 1057056. [Google Scholar] [CrossRef] [PubMed]
- Jeziorny, K.; Pietrowska, K.; Sieminska, J.; Zmysłowska-Polakowska, E.; Kretowski, A.; Ciborowski, M.; Zmyslowska, A. Serum metabolomics identified specific lipid compounds which may serve as markers of disease progression in patients with Alström and Bardet-Biedl syndromes. Front. Mol. Biosci. 2023, 10, 1251905. [Google Scholar] [CrossRef] [PubMed]
- Shi, M.; Han, S.; Klier, K.; Fobo, G.; Montrone, C.; Yu, S.; Harada, M.; Henning, A.-K.; Friedrich, N.; Bahls, M.; et al. Identification of candidate metabolite biomarkers for metabolic syndrome and its five components in population-based human cohorts. Cardiovasc. Diabetol. 2023, 22, 141. [Google Scholar] [CrossRef] [PubMed]
- Mihalik, S.J.; Goodpaster, B.H.; Kelley, D.E.; Chace, D.H.; Vockley, J.; Toledo, F.G.S.; DeLany, J.P. Increased levels of plasma acylcarnitines in obesity and type 2 diabetes and identification of a marker of glucolipotoxicity. Obesity 2010, 18, 1695–1700. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.R.; Ning, Y.; Yu, H.; Tang, N.J. A HPLC-Q-TOF-MS-based urinary metabolomic approach to identification of potential biomarkers of metabolic syndrome. J. Huazhong Univ. Sci Technolog. Med. Sci. 2014, 34, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Jeziorny, K.; Zmyslowska-Polakowska, E.; Wyka, K.; Pyziak-Skupień, A.; Borowiec, M.; Szadkowska, A.; Zmysłowska, A. Identification of bone metabolism disorders in patients with Alström and Bardet-Biedl syndromes based on markers of bone turnover and mandibular atrophy. Bone Rep. 2022, 17, 101600. [Google Scholar] [CrossRef] [PubMed]
- Butler, M.G.; Wang, K.; Marshall, J.D.; Rethmeyer, J.; Gunewardena, S.; Manzardo, A. Coding and noncoding expression patterns associated with rare obesity-related disorders: Prader—Willi and Alström syndromes. AGG 2015, 5, 53–75. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, P.; Zacchia, M.; Cavaliere, C.; Basso, L.; Salvatore, M.; Capasso, G.; Aiello, M. Diffusion tensor imaging for the study of early renal dysfunction in patients affected by bardet-biedl syndrome. Sci. Rep. 2021, 11, 20855. [Google Scholar] [CrossRef]
- Caterino, M.; Zacchia, M.; Costanzo, M.; Bruno, G.; Arcaniolo, D.; Trepiccione, F.; Siciliano, R.A.; Mazzeo, M.F.; Ruoppolo, M.; Capasso, G. Urine Proteomics Revealed a Significant Correlation Between Urine-Fibronectin Abundance and Estimated-GFR Decline in Patients with Bardet-Biedl Syndrome. Kidney Blood Press Res. 2018, 43, 389–405. [Google Scholar] [CrossRef]
- Marchese, E.; Caterino, M.; Fedele, R.; Pirozzi, F.; Cevenini, A.; Gupta, N.; Ingrosso, D.; Perna, A.; Capasso, G.; Ruoppolo, M.; et al. Multi-Omics Studies Unveil Extraciliary Functions of BBS10 and Show Metabolic Aberrations Underlying Renal Disease in Bardet-Biedl Syndrome. Int. J. Mol. Sci. 2022, 23, 9420. [Google Scholar] [CrossRef] [PubMed]
- Zacchia, M.; Blanco, F.D.V.; Torella, A.; Raucci, R.; Blasio, G.; Onore, M.E.; Marchese, E.; Trepiccione, F.; Vitagliano, C.; Di Iorio, V.; et al. Urine concentrating defect as presenting sign of progressive renal failure in Bardet-Biedl syndrome patients. Clin. Kidney J. 2021, 14, 1545–1551. [Google Scholar] [CrossRef]
- Fernandez-Marmiesse, A.; Gouveia, S.; Couce, M.L. NGS Technologies as a Turning Point in Rare Disease Research, Diagnosis and Treatment. Curr. Med. Chem. 2018, 25, 404–432. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Li, N.; Xu, Y.; Li, G.; Yu, T.; Yao, R.-E.; Fu, L.; Wang, J.; Yin, L.; Yin, Y.; et al. Proband-only medical exome sequencing as a cost-effective first-tier genetic diagnostic test for patients without prior molecular tests and clinical diagnosis in a developing country: The China experience. Genet. Med. 2018, 20, 1045–1053. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sánchez, S.; Álvarez-Satta, M.; Tohamy, M.A.; Beltran, S.; Derdak, S.; Valverde, D. Whole exome sequencing as a diagnostic tool for patients with ciliopathy-like phenotypes. PLoS ONE 2017, 12, e0183081. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, R.; Szymanska, K.; Basu, B.; Patel, N.; Ewida, N.; Faqeih, E.; Al Hashem, A.; Derar, N.; Alsharif, H.; Aldahmesh, M.A. Characterizing the morbid genome of ciliopathies. Genome. Biol. 2016, 17, 242. [Google Scholar] [CrossRef] [PubMed]
- Frésard, L.; Smail, C.; Ferraro, N.M.; Teran, N.A.; Li, X.; Smith, K.S.; Bonner, D.; Kernohan, K.D.; Marwaha, S.; Zappala, Z.; et al. Identification of rare-disease genes using blood transcriptome sequencing and large control cohorts. Nat. Med. 2019, 25, 911–919. [Google Scholar] [CrossRef] [PubMed]
- Modarage, K.; Malik, S.A.; Goggolidou, P. Molecular Diagnostics of Ciliopathies and Insights Into Novel Developments in Diagnosing Rare Diseases. Br. J. Biomed. Sci. 2022, 79, 10221. [Google Scholar] [CrossRef] [PubMed]
- Su, J.; Gao, C.; Wang, R.; Xiao, C.; Yang, M. Genes associated with inflammation and the cell cycle may serve as biomarkers for the diagnosis and prognosis of acute myocardial infarction in a Chinese population. Mol. Med. Rep. 2018, 18, 1311–1322. [Google Scholar] [CrossRef]
- Zhang, S.Y.; Xuan, C.; Wang, Y.; Zhang, S.-Q.; Li, H.; He, G.-W.; Tian, Q.-W. Association between ALMS 1 variants and early-onset coronary artery disease: A case-control study in Chinese population. Biosci. Rep. 2020, 40, BSR20193637. [Google Scholar] [CrossRef]
- Xuan, C.; Li, H.; Tian, Q.W.; Guo, J.J.; He, G.W.; Lun, L.M.; Wang, Q. Quantitative Assessment of Serum Amino Acids and Association with Early-Onset Coronary Artery Disease. Clin. Interv. Aging 2021, 16, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Schreyer, E.; Obringer, C.; Messaddeq, N.; Kieffer, B.; Zimmet, P.; Fleming, A.; Geberhiwot, T.; Marion, V. PATAS, a First-in-Class Therapeutic Peptide Biologic, Improves Whole-Body Insulin Resistance and Associated Comorbidities In Vivo. Diabetes 2022, 71, 2034–2047. [Google Scholar] [CrossRef] [PubMed]
| System or Organ | BBS [8,14,23,24,38,43] | ALMS [8,13,19,20,21,22,42] | CRPT [8,15,25,26,27,28,29] | MORMS [8,16,30] | MOSPGF [8,17] |
|---|---|---|---|---|---|
| Nervous system | Macrocephaly, intellectual disability, global developmental delay, cognitive impairment, poor coordination, hydrocephalus, brachycephaly, specific learning disability, neurological speech impairment, gait imbalance, delayed speech and language development, ataxia | Seizures, obsessive-compulsive behaviour, autism, aplasia/hypoplasia of the cerebellum | Trigonocephaly, sagittal craniosynostosis, oxycephaly, large foramen magnum, lambdoidal craniosynostosis, frontal bossing, brachycephaly, intellectual disability, cerebral atrophy, aplasia/hypoplasia of the corpus callosum, coronal craniosynostosis | Delayed speech and language development, intellectual disability, moderate | Intellectual disability |
| Endocrine system | Obesity, diabetes mellitus, nephrogenic diabetes insipidus, polycystic ovaries, hypertrichosis | Type II diabetes mellitus, insulin-resistant diabetes mellitus, hyperuricemia, hypertriglyceridemia, hyperinsulinemia, gynecomastia, precocious puberty, multinodular goiter, menstrual irregularities, hypothyroidism, hypergonadotropic hypogonadism, growth hormone deficiency, diabetes insipidus, polycystic ovaries, hypertrichosis, alopecia, acanthosis nigricans, global developmental delay, accelerated skeletal maturation, truncal obesity, short stature | Precocious puberty, short stature, obesity | Childhood-onset truncal obesity | Hyperbetalipoproteinemia, hypercholesterolemia, hypertriglyceridemia, insulin resistance, type II diabetes mellitus, obesity |
| Motion system | Syndactyly, postaxial hand polydactyly, foot polydactyly, mesoaxial polydactyly, finger syndactyly, radial deviation of finger, polydactyly, short foot, broad foot, brachydactyly syndrome | Scoliosis, kyphosis | Joint contracture of the hand, camptodactyly, webbed neck, short neck, toe syndactyly, talipes equinovarus, shallow acetabular fossae, pseudoepiphyses of the proximal phalanges of the hand, preaxial polydactyly, preaxial foot polydactyly, postaxial polydactyly, postaxial hand polydactyly, metatarsus adductus, lateral displacement of patellae, genu varum, genu valgum, duplication of the proximal phalanx of the hallux, cutaneous finger syndactyly, coxa vara, coxa valga, complete duplication of proximal phalanx of the thumb, clinodactyly of the 5th finger, broad thumb, brachydactyly syndrome, aplasia/hypoplasia of the middle phalanges of the toes, aplasia/hypoplasia of the middle phalanges of the hand, aplasia of the middle phalanx of the hand, scoliosis, pectus excavatum, pectus carinatum, flared iliac wings, sacral dimple, spina bifida occulta | NM | NM |
| Urinary system | Multicystic kidney dysplasia, renal insufficiency, renal hypoplasia, renal cyst, Stage 5 chronic kidney disease, renal agenesis, nephrotic syndrome, abnormality of the kidney, recurrent respiratory infections | Vesicoureteral reflux, tubulointerstitial nephritis, renal insufficiency, abnormality of the urethra, nephrocalcinosis, nephritis, glomerulopathy | Hydroureter, hydronephrosis | ||
| Reproductive system | Cryptorchidism, hypospadias, micropenis, hypoplasia of penis, hypogonadism, vaginal atresia, external genital hypoplasia, decreased testicular size, abnormality of the ovary | Decreased fertility, abnormality of the testis, abnormality of female external genitalia | Shawl scrotum, micropenis, external genital hypoplasia, cryptorchidism | Micropenis | Azoospermia, infertility, oligospermia |
| Cardiovascular system | Hypertension, left ventricular hypertrophy, bicuspid aortic valve, atria septal defect | Renovascular hypertension, pulmonary hypertension, hypertrophic cardiomyopathy, dilated cardiomyopathy, congestive heart failure, atherosclerosis | Ventricular septal defect, transposition of the great arteries, tetralogy of fallot, patent ductus arteriosus, atria septal defect, pulmonic stenosis | NM | Congestive heart failure, hypertension, myocardial infarction, premature coronary artery disease |
| Digestive system | Hepatic fibrosis, hepatic failure, biliary tract abnormality, aganglionic megacolon | Splenomegaly, portal hypertension, hepatomegaly, hepatic steatosis, elevated hepatic transaminases, cirrhosis, chronic hepatic failure, chronic active hepatitis | NM | NM | Hepatic steatosis |
| Respiratory system | Respiratory distress, bronchiolitis, recurrent respiratory infections, asthma | Recurrent pneumonia, asthma, respiratory insufficiency, pulmonary fibrosis | NM | NM | NM |
| Face | High palate, low-set, posteriorly rotated ears, prominent nasal bridge, short neck, downslanted palpebral fissures, medial flaring of the eyebrow, hypodontia, dental crowding, abnormalities of the teeth | Round face, hyperostosis frontalis interna, gingivitis, abnormalities of the teeth | Wide nasal bridge, upslanted palpebral fissure, underdeveloped supraorbital ridges, sparse eyebrow, retrognathia, preauricular pit, persistence of primary teeth, narrow palate, micrognathia, malar flattening, hypoplasia of the maxilla, hypoplasia of midface, highly arched eyebrow, high palate, depressed nasal bridge, anteverted nares, agenesis of permanent teeth | NM | NM |
| Eyes | Strabismus, retinopathy, rod-cone dystrophy, abnormal electroretinogram, cataract, myopia, retinal degeneration, cone/cone–rod dystrophy, abnormality of retinal pigmentation, nyctalopia, macular dystrophy, glaucoma, congenital primary aphakia, astigmatism, nystagmus | Deeply set eye, subcapsular cataract, pigmentary retinopathy, photophobia, nystagmus, cone/cone–rod dystrophy, chorioretinal abnormality, blindness | Hypertelorism, epicanthus, telecanthus, optic atrophy, opacification of the corneal stroma, microcornea | Cataract, retinal dystrophy, visual impairment | NM |
| Ear | Hearing impairment, recurrent otitis media | Progressive sensorineural hearing impairment, otitis media | Sensorineural hearing impairment, protruding ear, low-set ears, conductive hearing impairment, abnormality of the pinna | NM | NM |
| Other | Hyposmia, situs inversus totalis | Pes planus, hypoalphalipoproteinemia | Umbilical hernia, omphalocele, polysplenia, wide intermamillary distance, supernumerary nipple, hypoplastic nipples, situs inversus totalis, cutis laxa | NM | Hypoalphalipoproteinemia |
| Diseases | Gene | Age of Onset Range | Incidence | BMI | Common Co-Morbidities | Comment |
|---|---|---|---|---|---|---|
| BBS [14,24] | BBS1-22, IFT74, SCLT1, SCAPER, NPHP | Birth—3 years | 89% | 35.7 ± 8.0 kg/m2 | Retinal cone–rod dystrophy, postaxial polydactyly, cognitive impairment, hypogonadism and genitourinary abnormalities, kidney disease | Central obesity; birth weight typically normal. |
| ALMS [19] | ALMS1 | Birth—5 years | 70–98% | NM | Cone–rod dystrophy, progressive sensorineural hearing loss, short stature, hypogonadism (central or primary), progressive renal disease, insulin resistance/type 2 diabetes mellitus | Birth weight typically normal; hyperphagia and excessive weight gain begin during the first years, resulting in childhood obesity. |
| CRPT [26,28] | MEGF8, RAB23 | NM | 90% | NM | Craniosynostosis, polydactyly, cardiac defects | High birth weight and obesity were prevalent. |
| MORMS [16,30] | INPP5E | 5–15 years | NM | NM | Impaired intellectual development, retinal dystrophy, micropenis | Truncal obesity |
| MOSPGF [17] | CEP19 | Birth—3 years | 91% | >40.0 kg/m2 | Spermatogenic failure, hypertension, type 2 diabetes mellitus | Morbid obesity |
| Genotype | Distinguishing Clinical Features/Comments |
|---|---|
| ALMS1 variants in exon 16 [60] | Early onset (before one year old) of retinal degeneration, urinary system dysfunction, dilated cardiomyopathy, and diabetes |
| ALMS1 variants in exon 8 [60] | Milder symptoms or later onset of kidney disease |
| ALMS1 truncated around exon 10 [22] | A higher prevalence of liver dysfunction and experience worse disease progression |
| ALMS1 c.7911dupC [61] | Severe cardiomyopathy |
| BBS1 [38] | Relatively less “syndromic” penetrance of renal anomalies |
| BBS2 [38] | Relatively more “syndromic” penetrance of renal anomalies “Leanest” of obesity phenotype |
| BBS3 [38] (ARL6) | Lowest “syndromic” penetrance of cognitive impairment and renal anomalies |
| BBS4 [38] | Low penetrance of renal anomalies Early-onset morbid obesity |
| BBS5 [38] | Relatively more “syndromic” |
| BBS6 [38] (MKKS) | More likely to have CHD and genitourinary malformations |
| BBS7 [38] | Relatively more “syndromic” penetrance of renal anomalies |
| BBS8 [38] (TTC8) | Relatively less “syndromic” penetrance of renal anomalies |
| BBS9 [38] | High penetrance of renal anomalies |
| BBS10 [38] | Most severe renal impairment Significant adiposity |
| BBS12 [38] | Significant adiposity |
| BBS21 [38] (C8rorf37) | High penetrance of polydactyly |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Q.; Huang, Y.; Gao, S.; Ding, Y.; Zhang, H.; Chang, G.; Wang, X. Obesity-Related Ciliopathies: Focus on Advances of Biomarkers. Int. J. Mol. Sci. 2024, 25, 8484. https://doi.org/10.3390/ijms25158484
Zhang Q, Huang Y, Gao S, Ding Y, Zhang H, Chang G, Wang X. Obesity-Related Ciliopathies: Focus on Advances of Biomarkers. International Journal of Molecular Sciences. 2024; 25(15):8484. https://doi.org/10.3390/ijms25158484
Chicago/Turabian StyleZhang, Qianwen, Yiguo Huang, Shiyang Gao, Yu Ding, Hao Zhang, Guoying Chang, and Xiumin Wang. 2024. "Obesity-Related Ciliopathies: Focus on Advances of Biomarkers" International Journal of Molecular Sciences 25, no. 15: 8484. https://doi.org/10.3390/ijms25158484





