LC/MS-Based Untargeted Lipidomics Reveals Lipid Signatures of Sarcopenia
Abstract
1. Introduction
2. Results
2.1. Characteristics of the Studied Population
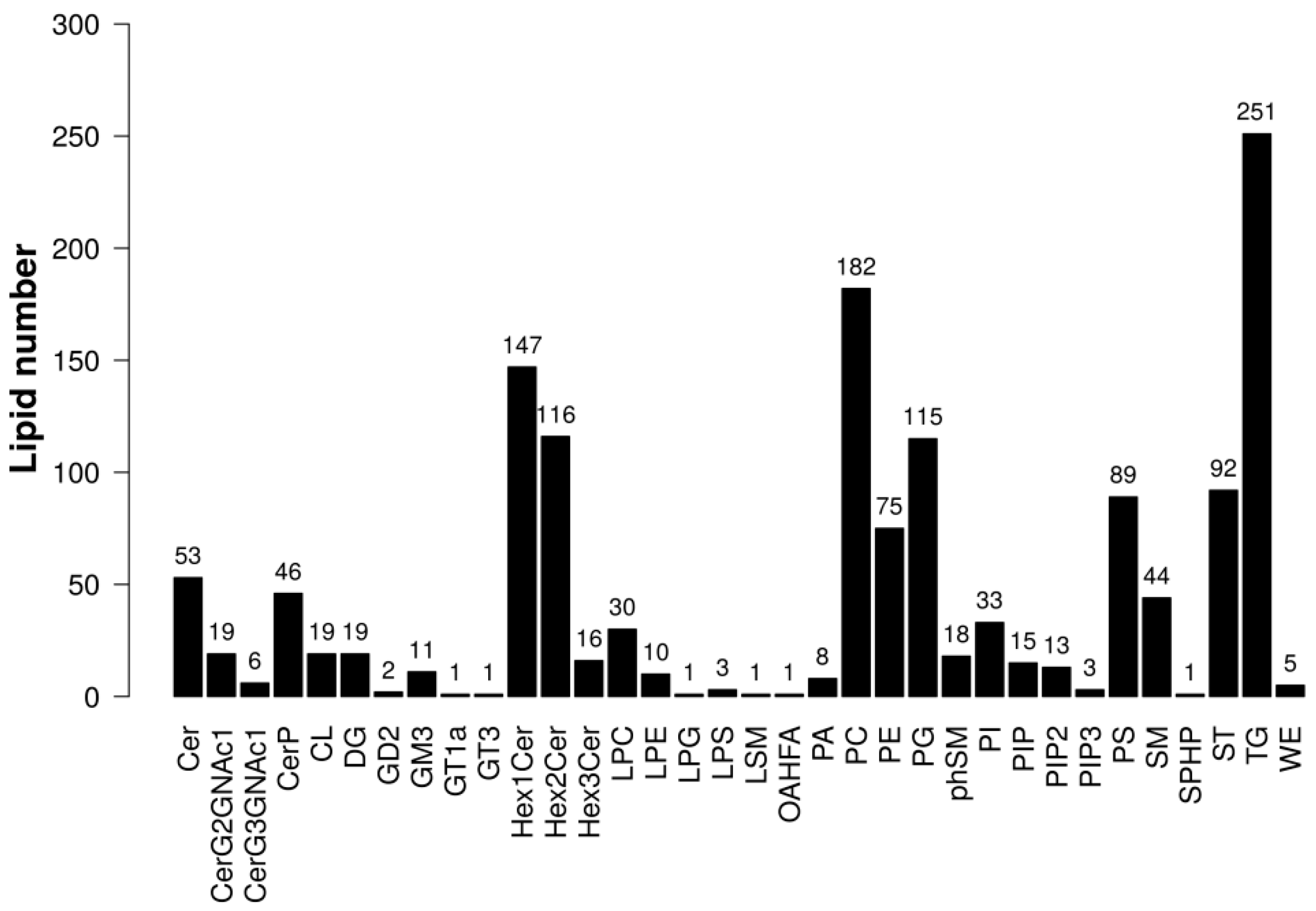
2.2. Univariate and Multivariate Statistical Analysis of Lipids
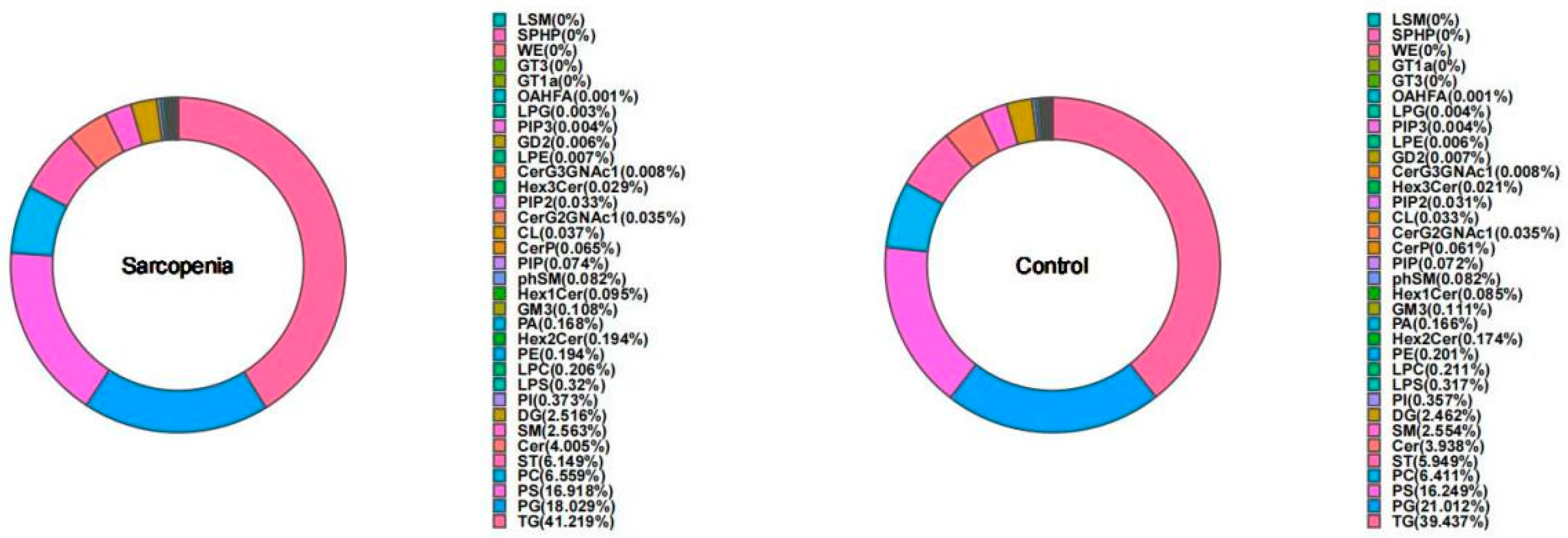
2.3. Differential Lipids between the Sarcopenia and Control Groups
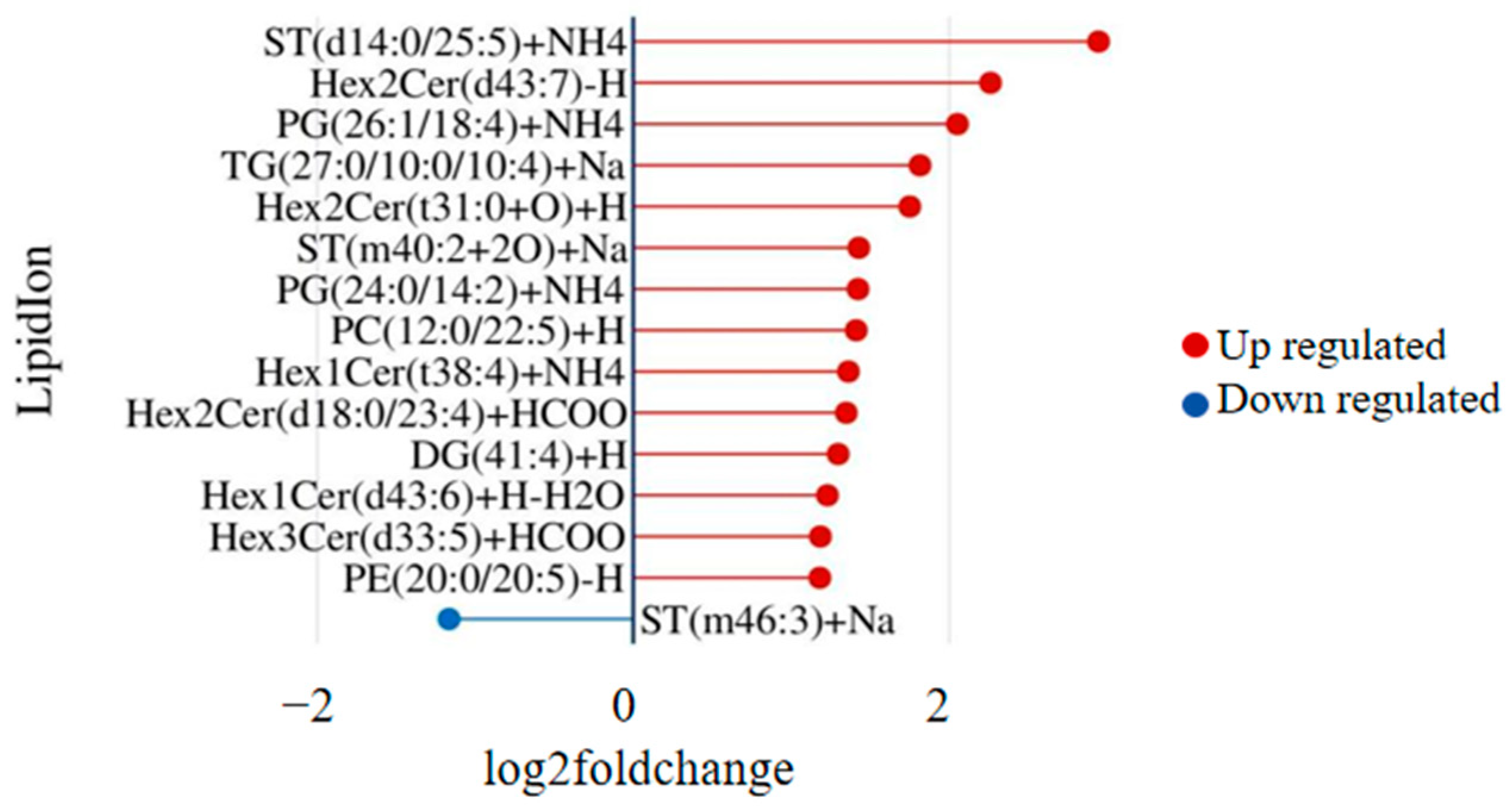
2.4. Lipid Coexpression Network Modules Linked to Sarcopenia
3. Pathway Analysis
4. Discussion
Advantages and Disadvantages
5. Materials and Methods
5.1. Study Participants
5.2. Assessment of Sarcopenia
5.3. Sample Preparation and Lipid Extraction
5.4. LC/MS Method for Lipid Analysis
5.5. Statistical Analysis
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jeejeebhoy, K.N. Malnutrition, fatigue, frailty, vulnerability, sarcopenia and cachexia: Overlap of clinical features. Curr. Opin. Clin. Nutr. Metab. Care 2012, 15, 213–219. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Sayer, A.A. Sarcopenia. Lancet 2019, 393, 2636–2646. [Google Scholar] [CrossRef]
- Hinkley, J.M.; Cornnell, H.H.; Standley, R.A.; Chen, E.Y.; Narain, N.R.; Greenwood, B.P.; Bussberg, V.; Tolstikov, V.V.; Kiebish, M.A.; Yi, F.; et al. Older adults with sarcopenia have distinct skeletal muscle phosphodiester, phosphocreatine, and phospholipid profiles. Aging Cell 2020, 19, e13135. [Google Scholar] [CrossRef]
- Al Saedi, A.; Debruin, D.A.; Hayes, A.; Hamrick, M. Lipid metabolism in sarcopenia. Bone 2022, 164, 116539. [Google Scholar] [CrossRef] [PubMed]
- Picca, A.; Calvani, R.; Bossola, M.; Allocca, E.; Menghi, A.; Pesce, V.; Lezza, A.M.S.; Bernabei, R.; Landi, F.; Marzetti, E. Update on mitochondria and muscle aging: All wrong roads lead to sarcopenia. Biol. Chem. 2018, 399, 421–436. [Google Scholar] [CrossRef] [PubMed]
- Korotkova, M.; Lundberg, I.E. The skeletal muscle arachidonic acid cascade in health and inflammatory disease. Nat. Rev. Rheumatol. 2014, 10, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Bosma, M.; Kersten, S.; Hesselink, M.K.; Schrauwen, P. Re-evaluating lipotoxic triggers in skeletal muscle: Relating intramyocellular lipid metabolism to insulin sensitivity. Prog. Lipid Res. 2012, 51, 36–49. [Google Scholar] [CrossRef]
- Batsis, J.A.; Villareal, D.T. Sarcopenic obesity in older adults: Aetiology, epidemiology and treatment strategies. Nat. Rev. Endocrinol. 2018, 14, 513–537. [Google Scholar] [CrossRef]
- Lisko, I.; Stenholm, S.; Raitanen, J.; Hurme, M.; Hervonen, A.; Jylhä, M.; Tiainen, K. Association of Body Mass Index and Waist Circumference With Physical Functioning: The Vitality 90+ Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 70, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Xu, B.; Zhang, K.; Zhu, W.; Lian, X.; Xu, Y.; Chen, Z.; Liu, L.; Guo, Z. The association of lipid metabolism and sarcopenia among older patients: A cross-sectional study. Sci. Rep. 2023, 13, 17538. [Google Scholar] [CrossRef] [PubMed]
- Han, P.; Yuan, C.; Chen, X.; Hu, Y.; Hu, X.; Xu, Z.; Guo, Q. Metabolic signatures and potential biomarkers of sarcopenia in suburb-dwelling older Chinese: Based on untargeted GC-MS and LC-MS. Skelet. Muscle 2024, 14, 4. [Google Scholar] [CrossRef] [PubMed]
- Lydic, T.A.; Goo, Y.H. Lipidomics unveils the complexity of the lipidome in metabolic diseases. Clin. Transl. Med. 2018, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Bieberich, E. It’s a lipid’s world: Bioactive lipid metabolism and signaling in neural stem cell differentiation. Neurochem. Res. 2012, 37, 1208–1229. [Google Scholar] [CrossRef] [PubMed]
- Merino Salvador, M.; Gómez de Cedrón, M.; Moreno Rubio, J.; Falagán Martínez, S.; Sánchez Martínez, R.; Casado, E.; Ramírez de Molina, A.; Sereno, M. Lipid metabolism and lung cancer. Crit. Rev. Oncol./Hematol. 2017, 112, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Kane, J.P.; Pullinger, C.R.; Goldfine, I.D.; Malloy, M.J. Dyslipidemia and diabetes mellitus: Role of lipoprotein species and interrelated pathways of lipid metabolism in diabetes mellitus. Curr. Opin. Pharmacol. 2021, 61, 21–27. [Google Scholar] [CrossRef] [PubMed]
- van Meer, G. Cellular lipidomics. EMBO J. 2005, 24, 3159–3165. [Google Scholar] [CrossRef] [PubMed]
- Eid, S.; Sas, K.M.; Abcouwer, S.F.; Feldman, E.L.; Gardner, T.W.; Pennathur, S.; Fort, P.E. New insights into the mechanisms of diabetic complications: Role of lipids and lipid metabolism. Diabetologia 2019, 62, 1539–1549. [Google Scholar] [CrossRef]
- Kohno, S.; Keenan, A.L.; Ntambi, J.M.; Miyazaki, M. Lipidomic insight into cardiovascular diseases. Biochem. Biophys. Res. Commun. 2018, 504, 590–595. [Google Scholar] [CrossRef]
- Guijas, C.; Montenegro-Burke, J.R.; Warth, B.; Spilker, M.E.; Siuzdak, G. Metabolomics activity screening for identifying metabolites that modulate phenotype. Nat. Biotechnol. 2018, 36, 316–320. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Hu, C.; Xuan, Q.; Xu, G. Recent advances in analytical strategies for mass spectrometry-based lipidomics. Anal. Chim. Acta 2020, 1137, 156–169. [Google Scholar] [CrossRef] [PubMed]
- Bi, B.; Dong, X.; Yan, M.; Zhao, Z.; Liu, R.; Li, S.; Wu, H. Dyslipidemia is associated with sarcopenia of the elderly: A meta-analysis. BMC Geriatr. 2024, 24, 181. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.I.; Julliand, S.; Reeds, D.N.; Sinacore, D.R.; Klein, S.; Mittendorfer, B. Fish oil-derived n-3 PUFA therapy increases muscle mass and function in healthy older adults. Am. J. Clin. Nutr. 2015, 102, 115–122. [Google Scholar] [CrossRef] [PubMed]
- De Spiegeleer, A.; Beckwée, D.; Bautmans, I.; Petrovic, M. Pharmacological Interventions to Improve Muscle Mass, Muscle Strength and Physical Performance in Older People: An Umbrella Review of Systematic Reviews and Meta-analyses. Drugs Aging 2018, 35, 719–734. [Google Scholar] [CrossRef] [PubMed]
- Heden, T.D.; Neufer, P.D.; Funai, K. Looking Beyond Structure: Membrane Phospholipids of Skeletal Muscle Mitochondria. Trends Endocrinol. Metab. TEM 2016, 27, 553–562. [Google Scholar] [CrossRef]
- Wang, X.; Xiao, R.; Li, H.; Li, T.; Guan, L.; Ding, H.; Li, X.; Zheng, H.; Yu, K.; Zhao, A.; et al. Correlation between Mild Cognitive Impairment and Sarcopenia: The Prospective Role of Lipids and Basal Metabolic Rate in the Link. Nutrients 2022, 14, 5321. [Google Scholar] [CrossRef] [PubMed]
- Uchitomi, R.; Hatazawa, Y.; Senoo, N.; Yoshioka, K.; Fujita, M.; Shimizu, T.; Miura, S.; Ono, Y.; Kamei, Y. Metabolomic Analysis of Skeletal Muscle in Aged Mice. Sci. Rep. 2019, 9, 10425. [Google Scholar] [CrossRef]
- Klein, M.E.; Mauch, S.; Rieckmann, M.; Martínez, D.G.; Hause, G.; Noutsias, M.; Hofmann, U.; Lucas, H.; Meister, A.; Ramos, G.; et al. Phosphatidylserine (PS) and phosphatidylglycerol (PG) nanodispersions as potential anti-inflammatory therapeutics: Comparison of in vitro activity and impact of pegylation. Nanomed. Nanotechnol. Biol. Med. 2020, 23, 102096. [Google Scholar] [CrossRef]
- Kuronuma, K.; Mitsuzawa, H.; Takeda, K.; Nishitani, C.; Chan, E.D.; Kuroki, Y.; Nakamura, M.; Voelker, D.R. Anionic pulmonary surfactant phospholipids inhibit inflammatory responses from alveolar macrophages and U937 cells by binding the lipopolysaccharide-interacting proteins CD14 and MD-2. J. Biol. Chem. 2009, 284, 25488–25500. [Google Scholar] [CrossRef]
- Senoo, N.; Miyoshi, N.; Kobayashi, E.; Morita, A.; Tanihata, J.; Takeda, S.; Miura, S. Glycerophospholipid profile alterations are associated with murine muscle-wasting phenotype. Muscle Nerve 2020, 62, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Wolfgang, M.J. Remodeling glycerophospholipids affects obesity-related insulin signaling in skeletal muscle. J. Clin. Investig. 2021, 131, e148176. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Liang, X.; Wu, T.; Jiang, J.; Jiang, Y.; Zhang, S.; Ruan, Y.; Zhang, H.; Zhang, C.; Chen, P.; et al. Integrative analysis of metabolomics and proteomics reveals amino acid metabolism disorder in sepsis. J. Transl. Med. 2022, 20, 123. [Google Scholar] [CrossRef]
- Yang, Y.; Wu, L.; Lv, Y.; Miao, Z.; Wang, Y.; Yan, J.; Li, J.; Li, C.; Ding, H. LC-MS/MS based untargeted lipidomics uncovers lipid signatures of late-onset preeclampsia. Biochimie 2023, 208, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Zhang, L.; Su, G.; Kijlstra, A.; Yang, P. Specific sweat metabolite profile in ocular Behcet’s disease. Int. Immunopharmacol. 2021, 97, 107812. [Google Scholar] [CrossRef]
- Langfelder, P.; Horvath, S. WGCNA: An R package for weighted correlation network analysis. BMC Bioinform. 2008, 9, 559. [Google Scholar] [CrossRef]
- Chen, X.; Shao, S.; Wu, X.; Feng, J.; Qu, W.; Gao, Q.; Sun, J.; Wan, H. LC/MS-based untargeted lipidomics reveals lipid signatures of nonpuerperal mastitis. Lipids Health Dis. 2023, 22, 122. [Google Scholar] [CrossRef]



| Sarcopenia (n = 40) | Control (n = 40) | p | |
|---|---|---|---|
| Age (years) | 73.33 ± 3.30 | 72.88 ± 3.31 | 0.545 |
| BMI (kg/m2) | 23.70 ± 2.88 | 26.23 ± 2.98 | <0.001 |
| Sex | -- | ||
| Male | 18 (45.0) | 18 (45.0) | |
| Female | 22 (55.0) | 22 (55.0) | |
| Marital status | 0.999 | ||
| Married | 29 (72.5) | 30 (75.0) | |
| Widowed, divorced, or separated | 11 (27.5) | 10 (25.0) | |
| Family economic levels | 0.638 | ||
| Poor | 2 (5.0) | 3 (7.5) | |
| Relatively poor | 8 (20.0) | 11 (27.5) | |
| Relatively good | 24 (60.0) | 23 (57.5) | |
| Good | 6 (15.0) | 3 (7.5) | |
| Smoking | 0.754 | ||
| Never | 30 (75.0) | 32 (80.0) | |
| Active smoker | 5 (12.5) | 3 (7.5) | |
| Former smoker | 5 (12.5) | 5 (12.5) | |
| Alcohol consumption | 0.797 | ||
| less than once a month | 33 (82.5) | 33 (82.5) | |
| 1–3 times per month | 2 (5.0) | 1 (2.5) | |
| 1–3 times per week | 2 (5.0) | 2 (5.0) | |
| More than 3 times per week | 1 (2.5) | 3 (7.5) | |
| Stopped drinking | 2 (5.0) | 1 (2.5) | |
| TC (mmol/L) | 6.70 ± 4.67 | 5.49 ± 1.41 | 0.119 |
| TG (mmol/L) | 1.54 ± 0.63 | 1.44 ± 0.90 | 0.575 |
| HDL-C (mmol/L) | 1.62 ± 0.42 | 1.44 ± 0.30 | 0.029 |
| LDL-C (mmol/L) | 3.38 ± 1.05 | 3.07 ± 0.78 | 0.135 |
| SMI (kg/m2) | 5.78 ± 0.71 | 6.79 ± 0.86 | <0.001 |
| Thigh circumference (cm) | 47.35 ± 8.22 | 47.95 ± 5.07 | 0.696 |
| Calf circumference (cm) | 31.92 ± 3.41 | 34.38 ± 3.23 | 0.001 |
| Maximum grip strength (kg) | 18.58 ± 5.84 | 27.30 ± 6.91 | <0.001 |
| Daily walking steps (steps) | 0.246 | ||
| ≤2000 | 16 (40.0) | 8 (20.0) | |
| 2001–4000 | 6 (15.0) | 9 (22.5) | |
| 4001–7000 | 12 (30.0) | 11 (27.5) | |
| 7001–10,000 | 4 (10.0) | 9 (22.5) | |
| ≥10,000 | 2 (5.0) | 3 (7.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Q.; Zhang, Z.; He, P.; Mao, X.; Jing, X.; Hu, Y.; Jing, L. LC/MS-Based Untargeted Lipidomics Reveals Lipid Signatures of Sarcopenia. Int. J. Mol. Sci. 2024, 25, 8793. https://doi.org/10.3390/ijms25168793
Yang Q, Zhang Z, He P, Mao X, Jing X, Hu Y, Jing L. LC/MS-Based Untargeted Lipidomics Reveals Lipid Signatures of Sarcopenia. International Journal of Molecular Sciences. 2024; 25(16):8793. https://doi.org/10.3390/ijms25168793
Chicago/Turabian StyleYang, Qianwen, Zhiwei Zhang, Panpan He, Xueqian Mao, Xueyi Jing, Ying Hu, and Lipeng Jing. 2024. "LC/MS-Based Untargeted Lipidomics Reveals Lipid Signatures of Sarcopenia" International Journal of Molecular Sciences 25, no. 16: 8793. https://doi.org/10.3390/ijms25168793
APA StyleYang, Q., Zhang, Z., He, P., Mao, X., Jing, X., Hu, Y., & Jing, L. (2024). LC/MS-Based Untargeted Lipidomics Reveals Lipid Signatures of Sarcopenia. International Journal of Molecular Sciences, 25(16), 8793. https://doi.org/10.3390/ijms25168793






