Emerging Roles of Bile Acids and TGR5 in the Central Nervous System: Molecular Functions and Therapeutic Implications
Abstract
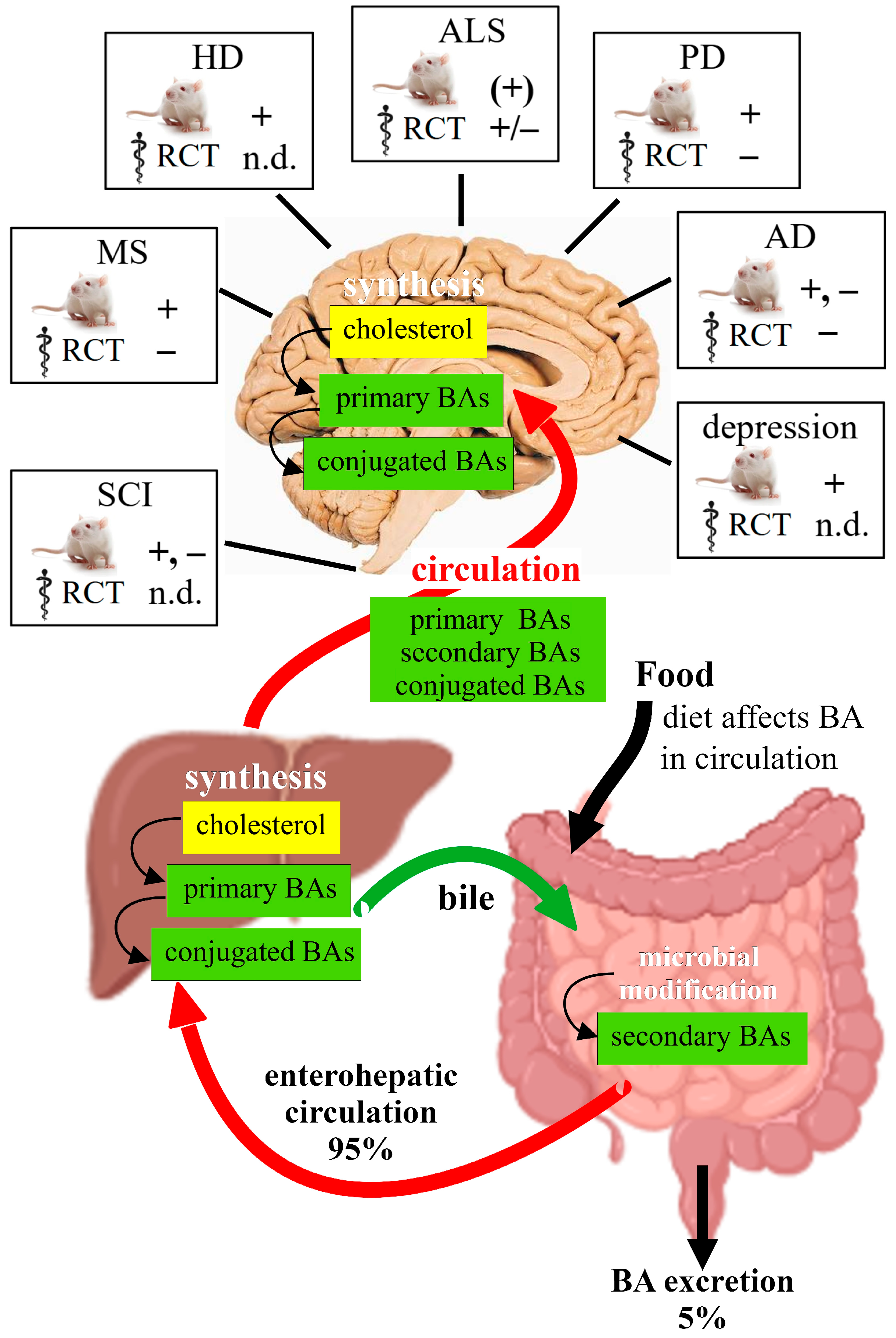
1. Is the Central Nervous System (CNS) a Source of BAs?
2. Bile Acid Signaling in the Nervous System
2.1. Molecular Signaling of TGR5
2.1.1. TGR5 Expression in the CNS
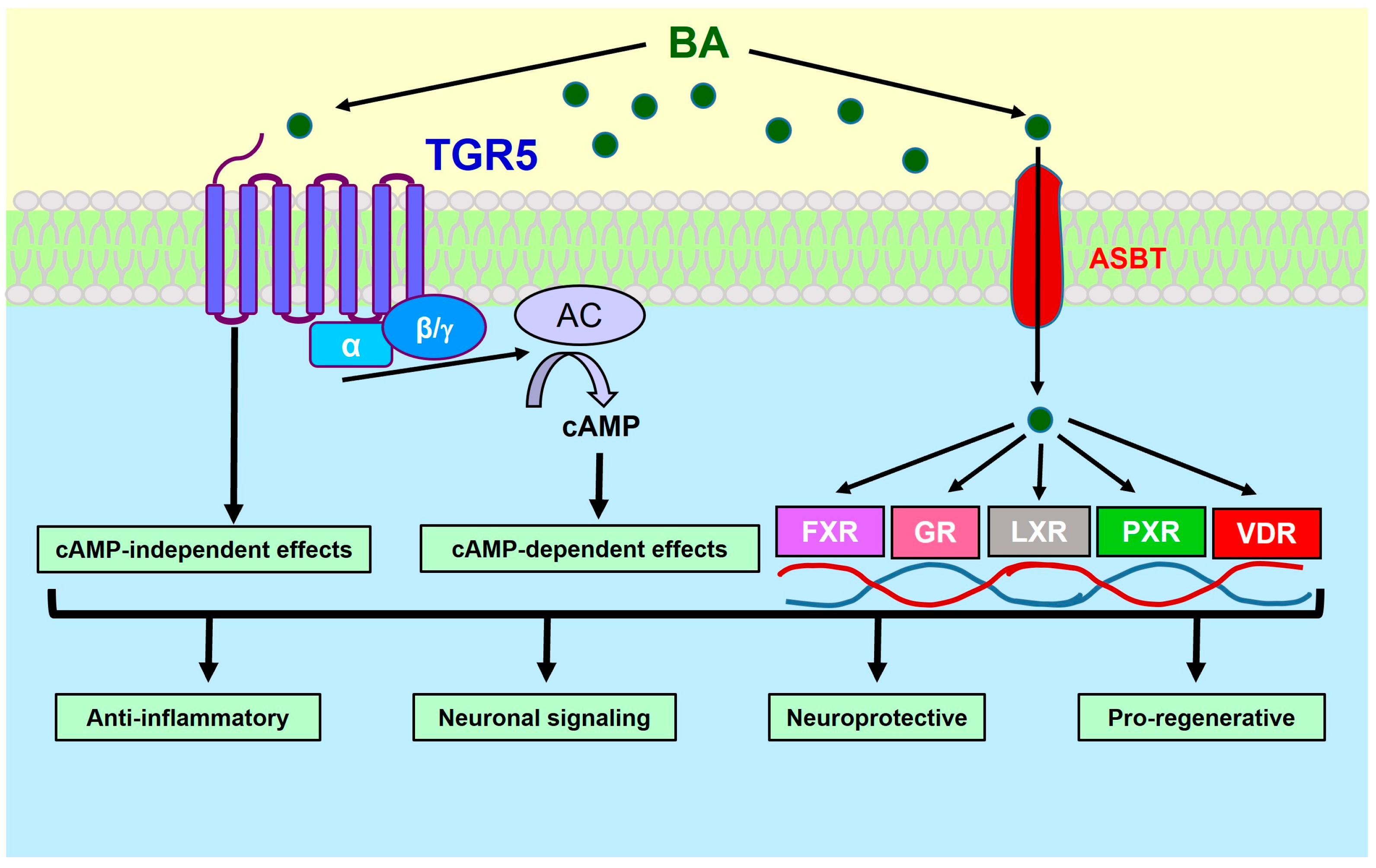
2.1.2. The cAMP Pathway
2.1.3. Neuronal Excitability
2.2. Putative Physiological Functions of TGR5 in the Brain
2.2.1. Sensory Signaling
2.2.2. Mood and Memory
2.2.3. Apoptosis and Microglia Activity
3. Bile Acids in Neuropathologies
3.1. Alterations of BA Metabolism in Neurodegenerative Diseases
3.1.1. Amyotrophic Lateral Sclerosis
3.1.2. Parkinson’s Disease
3.1.3. Huntington’s Disease
3.1.4. Alzheimer’s Disease
3.1.5. Depression and Psychiatric Disorders
3.1.6. Multiple Sclerosis
3.2. Therapeutic Efficacy of BA Treatment in Neuropathology
3.2.1. Spinal Cord Injury
3.2.2. Amyotrophic Lateral Sclerosis
3.2.3. Parkinson’s Disease
3.2.4. Huntington’s Disease
3.2.5. Alzheimer’s Disease and Dementia
3.2.6. Clinical Depression
3.2.7. Multiple Sclerosis
3.2.8. Stroke and Cerebral Ischemia
3.3. Molecular Mechanisms Associated with BA Effects in Disease Models
3.3.1. Anti-Inflammatory Effect via Production of cAMP
3.3.2. Endoplasmic Reticulum Stress
3.3.3. Reduction in Apoptosis and Mitochondrial Dysfunction
3.3.4. Bile Acids as Chaperones
3.3.5. Physiology of Nerve Cells
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chiang, J.Y.L.; Ferrell, J.M. Bile Acid Metabolism in Liver Pathobiology. Gene Expr. 2018, 18, 71–87. [Google Scholar] [CrossRef] [PubMed]
- Pandak, W.M.; Kakiyama, G. The Acidic Pathway of Bile Acid Synthesis: Not Just an Alternative Pathway. Liver Res. 2019, 3, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Kevresan, S.; Kuhajda, K.; Kandrac, J.; Fawcett, J.P.; Mikov, M. Biosynthesis of Bile Acids in Mammalian Liver. Eur. J. Drug Metab. Pharmacokinet. 2006, 31, 145–156. [Google Scholar] [CrossRef]
- Bruusgaard, A.; Thaysen, E.H. Increased Ratio of Glycine/Taurine Conjugated Bile Acids in the Early Diagnosis of Terminal Ileopathy. Acta Med. Scand. 1970, 188, 547–548. [Google Scholar] [CrossRef] [PubMed]
- Bremer, J. Species Differences in the Conjugation of Free Bile Acids with Taurine and Glycine. Biochem. J. 1956, 63, 507–513. [Google Scholar] [CrossRef]
- Ridlon, J.M.; Kang, D.J.; Hylemon, P.B. Bile Salt Biotransformations by Human Intestinal Bacteria. J. Lipid Res. 2006, 47, 241–259. [Google Scholar] [CrossRef]
- Ridlon, J.M.; Harris, S.C.; Bhowmik, S.; Kang, D.J.; Hylemon, P.B. Consequences of Bile Salt Biotransformations by Intestinal Bacteria. Gut Microbes 2016, 7, 22–39. [Google Scholar] [CrossRef]
- Engelking, L.R.; Dasher, C.A.; Hirschowitz, B.I. Within-Day Fluctuations in Serum Bile-Acid Concentrations among Normal Control Subjects and Patients with Hepatic Disease. Am. J. Clin. Pathol. 1980, 73, 196–201. [Google Scholar] [CrossRef]
- Greenwood, J.; Adu, J.; Davey, A.J.; Abbott, N.J.; Bradbury, M.W.B. The Effect of Bile Salts on the Permeability and Ultrastructure of the Perfused, Energy-Depleted, Rat Blood-Brain Barrier. J. Cereb. Blood Flow Metab. 1991, 11, 644–654. [Google Scholar] [CrossRef]
- Bron, B.; Waldram, R.; Silk, D.B.A.; Williams, R. Serum, Cerebrospinal Fluid, and Brain Levels of Bile Acids in Patients with Fulminant Hepatic Failure. Gut 1977, 18, 692–696. [Google Scholar] [CrossRef]
- Tripodi, V.; Contin, M.; Fernández, M.A.; Lemberg, A. Bile Acids Content in Brain of Common Duct Ligated Rats. Ann. Hepatol. 2012, 11, 930–934. [Google Scholar] [CrossRef]
- Baloni, P.; Funk, C.C.; Yan, J.; Yurkovich, J.T.; Kueider-Paisley, A.; Nho, K.; Heinken, A.; Jia, W.; Mahmoudiandehkordi, S.; Louie, G.; et al. Metabolic Network Analysis Reveals Altered Bile Acid Synthesis and Metabolism in Alzheimer’s Disease. Cell Rep. Med. 2020, 1, 100138. [Google Scholar] [CrossRef] [PubMed]
- Higashi, T.; Watanabe, S.; Tomaru, K.; Yamazaki, W.; Yoshizawa, K.; Ogawa, S.; Nagao, H.; Minato, K.; Maekawa, M.; Mano, N. Unconjugated Bile Acids in Rat Brain: Analytical Method Based on LC/ESI-MS/MS with Chemical Derivatization and Estimation of Their Origin by Comparison to Serum Levels. Steroids 2017, 125, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, T.; Sato, A.; Nishimoto-Kusunose, S.; Yoshizawa, K.; Higashi, T. Further Evidence for Blood-to-Brain Influx of Unconjugated Bile Acids by Passive Diffusion: Determination of Their Brain-to-Serum Concentration Ratios in Rats by LC/MS/MS. Steroids 2024, 204, 109397. [Google Scholar] [CrossRef]
- St-Pierre, M.V.; Kullak-Ublick, G.A.; Hagenbuch, B.; Meier, P.J. Transport of Bile Acids in Hepatic and Non-Hepatic Tissues. J. Exp. Biol. 2001, 204, 1673–1686. [Google Scholar] [CrossRef] [PubMed]
- Choudhuri, S.; Cherrington, N.J.; Li, N.; Klaassen, C.D. Constitutive Expression of Various Xenobiotic and Endobiotic Transporter MRNAs in the Choroid Plexus of Rats. Drug Metab. Dispos. 2003, 31, 1337–1345. [Google Scholar] [CrossRef]
- Ose, A.; Kusuhara, H.; Endo, C.; Tohyama, K.; Miyajima, M.; Kitamura, S.; Sugiyama, Y. Functional Characterization of Mouse Organic Anion Transporting Peptide 1a4 in the Uptake and Efflux of Drugs across the Blood-Brain Barrier. Drug Metab. Dispos. 2010, 38, 168–176. [Google Scholar] [CrossRef]
- Nizamutdinov, D.; Demorrow, S.; McMillin, M.; Kain, J.; Mukherjee, S.; Zeitouni, S.; Frampton, G.; Bricker, P.C.S.; Hurst, J.; Shapiro, L.A. Hepatic Alterations Are Accompanied by Changes to Bile Acid Transporter-Expressing Neurons in the Hypothalamus after Traumatic Brain Injury. Sci. Rep. 2017, 7, 40112. [Google Scholar] [CrossRef]
- Dietschy, J.M. Central Nervous System: Cholesterol Turnover, Brain Development and Neurodegeneration. Biol. Chem. 2009, 390, 287–293. [Google Scholar] [CrossRef]
- Björkhem, I.; Meaney, S.; Fogelman, A.M. Brain Cholesterol: Long Secret Life behind a Barrier. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 806–815. [Google Scholar] [CrossRef]
- Heverin, M.; Bogdanovic, N.; Lütjohann, D.; Bayer, T.; Pikuleva, I.; Bretillon, L.; Diczfalusy, U.; Winblad, B.; Björkhem, I. Changes in the Levels of Cerebral and Extracerebral Sterols in the Brain of Patients with Alzheimer’s Disease. J. Lipid Res. 2004, 45, 186–193. [Google Scholar] [CrossRef]
- Bogdanovic, N.; Bretillon, L.; Lund, E.G.; Diczfalusy, U.; Lannfelt, L.; Winblad, B.; Russell, D.W.; Björkhem, I. On the Turnover of Brain Cholesterol in Patients with Alzheimer’s Disease. Abnormal Induction of the Cholesterol-Catabolic Enzyme CYP46 in Glial Cells. Neurosci. Lett. 2001, 314, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Lund, E.G.; Guileyardo, J.M.; Russell, D.W. CDNA Cloning of Cholesterol 24-Hydroxylase, a Mediator of Cholesterol Homeostasis in the Brain. Proc. Natl. Acad. Sci. USA 1999, 96, 7238–7243. [Google Scholar] [CrossRef]
- Brown, J.; Theisler, C.; Silberman, S.; Magnuson, D.; Gottardi-Littell, N.; Lee, J.M.; Yager, D.; Crowley, J.; Sambamurti, K.; Rahman, M.M.; et al. Differential Expression of Cholesterol Hydroxylases in Alzheimer’s Disease. J. Biol. Chem. 2004, 279, 34674–34681. [Google Scholar] [CrossRef]
- Lavrnja, I.; Smiljanic, K.; Savic, D.; Mladenovic-Djordjevic, A.; Tesovic, K.; Kanazir, S.; Pekovic, S. Expression Profiles of Cholesterol Metabolism-Related Genes Are Altered during Development of Experimental Autoimmune Encephalomyelitis in the Rat Spinal Cord. Sci. Rep. 2017, 7, 2702. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Zhu, J.; Guo, S.; Wong, B.J.; Chehab, F.F.; Ferriero, D.M.; Jiang, X. Upregulation of Cholesterol 24-Hydroxylase Following Hypoxia-Ischemia in Neonatal Mouse Brain. Pediatr. Res. 2018, 83, 1218–1227. [Google Scholar] [CrossRef]
- Nishimura, M.; Yaguti, H.; Yoshitsugu, H.; Naito, S.; Satoh, T. Tissue Distribution of MRNA Expression of Human Cytochrome P450 Isoforms Assessed by High-Sensitivity Real-Time Reverse Transcription PCR. Yakugaku Zasshi 2003, 123, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Mano, N.; Sato, Y.; Nagata, M.; Goto, T.; Goto, J. Bioconversion of 3β-Hydroxy-5-Cholenoic Acid into Chenodeoxycholic Acid by Rat Brain Enzyme Systems. J. Lipid Res. 2004, 45, 1741–1748. [Google Scholar] [CrossRef]
- Sjöstedt, E.; Zhong, W.; Fagerberg, L.; Karlsson, M.; Mitsios, N.; Adori, C.; Oksvold, P.; Edfors, F.; Limiszewska, A.; Hikmet, F.; et al. An Atlas of the Protein-Coding Genes in the Human, Pig, and Mouse Brain. Science 2020, 367, eaay5947. [Google Scholar] [CrossRef]
- Björkhem, I.; Lütjohann, D.; Diczfalusy, U.; Ståhle, L.; Ahlborg, G.; Wahren, J. Cholesterol Homeostasis in Human Brain: Turnover of 24S- Hydroxycholesterol and Evidence for a Cerebral Origin of Most of This Oxysterol in the Circulation. J. Lipid Res. 1998, 39, 1594–1600. [Google Scholar] [CrossRef]
- Gilardi, F.; Viviani, B.; Galmozzi, A.; Boraso, M.; Bartesaghi, S.; Torri, A.; Caruso, D.; Crestani, M.; Marinovich, M.; de Fabiani, E. Expression of Sterol 27-Hydroxylase in Glial Cells and Its Regulation by Liver X Receptor Signaling. Neuroscience 2009, 164, 530–540. [Google Scholar] [CrossRef]
- Tsaousidou, M.K.; Ouahchi, K.; Warner, T.T.; Yang, Y.; Simpson, M.A.; Laing, N.G.G.; Wilkinson, P.A.; Madrid, R.E.; Patel, H.; Hentati, F.; et al. Sequence Alterations within CYP7B1 Implicate Defective Cholesterol Homeostasis in Motor-Neuron Degeneration. Am. J. Hum. Genet. 2008, 82, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Trap, C.; Nato, F.; Chalbot, S.; Kim, S.B.; Lafaye, P.; Morfin, R. Immunohistochemical Detection of the Human Cytochrome P4507B1: Production of a Monoclonal Antibody after CDNA Immunization. J. Neuroimmunol. 2005, 159, 41–47. [Google Scholar] [CrossRef]
- Wicher, G.; Norlin, M. Estrogen-Mediated Regulation of Steroid Metabolism in Rat Glial Cells; Effects on Neurosteroid Levels via Regulation of CYP7B1-Mediated Catalysis. J. Steroid Biochem. Mol. Biol. 2015, 145, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Ogundare, M.; Theofilopoulos, S.; Lockhart, A.; Hall, L.J.; Arenas, E.; Sjövall, J.; Brenton, A.G.; Wang, Y.; Griffiths, W.J. Cerebrospinal Fluid Steroidomics: Are Bioactive Bile Acids Present in Brain? J. Biol. Chem. 2010, 285, 4666–4679. [Google Scholar] [CrossRef]
- Wanke, F.; Moos, S.; Croxford, A.L.; Heinen, A.P.; Gräf, S.; Kalt, B.; Tischner, D.; Zhang, J.; Christen, I.; Bruttger, J.; et al. EBI2 Is Highly Expressed in Multiple Sclerosis Lesions and Promotes Early CNS Migration of Encephalitogenic CD4 T Cells. Cell Rep. 2017, 18, 1270–1284. [Google Scholar] [CrossRef] [PubMed]
- Rutkowska, A.; Preuss, I.; Gessier, F.; Sailer, A.W.; Dev, K.K. EBI2 Regulates Intracellular Signaling and Migration in Human Astrocyte. Glia 2015, 63, 341–351. [Google Scholar] [CrossRef]
- Khanna, M.; Qin, K.N.; Cheng, K.C. Distribution of 3α-Hydroxysteroid Dehydrogenase in Rat Brain and Molecular Cloning of Multiple CDNAs Encoding Structurally Related Proteins in Humans. J. Steroid Biochem. Mol. Biol. 1995, 53, 41–46. [Google Scholar] [CrossRef]
- Dufort, I.; Labrie, F. Human Types 1 and 3 3a-Hydroxysteroid Dehydrogenases: Differential Lability and Tissue Distribution. J. Clin. Endocrinol. Metab. 2001, 86, 841–846. [Google Scholar] [CrossRef][Green Version]
- Penning, T.M.; Burczynski, M.E.; Jez, J.M.; Hung, C.F.; Lin, H.K.; Ma, H.; Moore, M.; Palackal, N.; Ratnam, K. Human 3α-Hydroxysteroid Dehydrogenase Isoforms (AKR1C1-AKR1C4) of the Aldo-Keto Reductase Superfamily: Functional Plasticity and Tissue Distribution Reveals Roles in the Inactivation and Formation of Male and Female Sex Hormones. Biochem. J. 2000, 351, 67–77. [Google Scholar] [CrossRef]
- Appanna, N.; Gibson, H.; Gangitano, E.; Dempster, N.J.; Morris, K.; George, S.; Arvaniti, A.; Gathercole, L.L.; Keevil, B.; Penning, T.M.; et al. Differential Activity and Expression of Human 5β-Reductase (Akr1d1) Splice Variants. J. Mol. Endocrinol. 2021, 66, 181–194. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Qiu, Y.; Su, M.; Wang, L.; Gong, Q.; Wei, X. Activation of the Bile Acid Receptors TGR5 and FXR in the Spinal Dorsal Horn Alleviates Neuropathic Pain. CNS Neurosci. Ther. 2023, 29, 1981–1998. [Google Scholar] [CrossRef]
- Lloyd-Evans, E.; Waller-Evans, H. Biosynthesis and Signalling Functions of Central and Peripheral Nervous System Neurosteroids in Health and Disease. Essays Biochem. 2020, 64, 591–606. [Google Scholar] [CrossRef] [PubMed]
- Lund, E.G.; Xie, C.; Kotti, T.; Turley, S.D.; Dietschy, J.M.; Russell, D.W. Knockout of the Cholesterol 24-Hydroxylase Gene in Mice Reveals a Brain-Specific Mechanism of Cholesterol Turnover. J. Biol. Chem. 2003, 278, 22980–22988. [Google Scholar] [CrossRef] [PubMed]
- Kakiyama, G.; Marques, D.; Takei, H.; Nittono, H.; Erickson, S.; Fuchs, M.; Rodriguez-Agudo, D.; Gil, G.; Hylemon, P.B.; Zhou, H.; et al. Mitochondrial Oxysterol Biosynthetic Pathway Gives Evidence for CYP7B1 as Controller of Regulatory Oxysterols. J. Steroid Biochem. Mol. Biol. 2019, 189, 36–47. [Google Scholar] [CrossRef]
- Li, X.; Pandak, W.M.; Erickson, S.K.; Ma, Y.; Yin, L.; Hylemon, P.; Ren, S. Biosynthesis of the Regulatory Oxysterol, 5-Cholesten-3β,25-Diol 3-Sulfate, in Hepatocytes. J. Lipid Res. 2007, 48, 2587–2596. [Google Scholar] [CrossRef]
- Cali, J.J.; Russell, D.W. Characterization of Human Sterol 27-Hydroxylase: A Mitochondrial Cytochrome P-450 That Catalyzes Multiple Oxidation Reactions in Bile Acid Biosynthesis. J. Biol. Chem. 1991, 266, 7774–7778. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.Y.; Lewis, M.; Doherty, J.J.; Shi, Y.; Cashikar, A.G.; Amelianchik, A.; Tymchuk, S.; Sullivan, P.M.; Qian, M.; Covey, D.F.; et al. 25-Hydroxycholesterol Amplifies Microglial IL-1β Production in an ApoE Isoform-Dependent Manner. J. Neuroinflammation 2020, 17, 192. [Google Scholar] [CrossRef]
- Cyster, J.G.; Dang, E.V.; Reboldi, A.; Yi, T. 25-Hydroxycholesterols in Innate and Adaptive Immunity. Nat. Rev. Immunol. 2014, 14, 731–743. [Google Scholar] [CrossRef]
- Diczfalusy, U.; Olofsson, K.E.; Carlsson, A.M.; Gong, M.; Golenbock, D.T.; Rooyackers, O.; Fläring, U.; Björkbacka, H. Marked Upregulation of Cholesterol 25-Hydroxylase Expression by Lipopolysaccharide. J. Lipid Res. 2009, 50, 2258–2264. [Google Scholar] [CrossRef]
- Stiles, A.R.; McDonald, J.G.; Bauman, D.R.; Russell, D.W. CYP7B1: One Cytochrome P450, Two Human Genetic Diseases, and Multiple Physiological Functions. J. Biol. Chem. 2009, 284, 28485–28489. [Google Scholar] [CrossRef]
- Hurley, M.J.; Bates, R.; Macnaughtan, J.; Schapira, A.H.V. Bile Acids and Neurological Disease. Pharmacol. Ther. 2022, 240, 108311. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, K.; Tornese, P.; Cocco, A.; Albanese, A. Tauroursodeoxycholic Acid: A Potential Therapeutic Tool in Neurodegenerative Diseases. Transl. Neurodegener. 2022, 11, 33. [Google Scholar] [CrossRef]
- Lo Giudice, M.; Cocco, A.; Reggiardo, G.; Lalli, S.; Albanese, A. Tauro-Urso-Deoxycholic Acid Trials in Amyotrophic Lateral Sclerosis: What Is Achieved and What to Expect. Clin. Drug Investig. 2023, 43, 893–903. [Google Scholar] [CrossRef]
- DeMorrow, S. Bile Acids in Hepatic Encephalopathy. J. Clin. Exp. Hepatol. 2019, 9, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Yanguas-Casás, N.; Barreda-Manso, M.A.; Nieto-Sampedro, M.; Romero-Ramírez, L. TUDCA: An Agonist of the Bile Acid Receptor GPBAR1/TGR5 With Anti-Inflammatory Effects in Microglial Cells. J. Cell. Physiol. 2017, 232, 2231–2245. [Google Scholar] [CrossRef]
- McMillin, M.; Frampton, G.; Grant, S.; Khan, S.; Diocares, J.; Petrescu, A.; Wyatt, A.; Kain, J.; Jefferson, B.; DeMorrow, S. Bile Acid-Mediated Sphingosine-1-Phosphate Receptor 2 Signaling Promotes Neuroinflammation during Hepatic Encephalopathy in Mice. Front. Cell. Neurosci. 2017, 11, 191. [Google Scholar] [CrossRef]
- McMillin, M.; Frampton, G.; Quinn, M.; Ashfaq, S.; De Los Santos, M.; Grant, S.; DeMorrow, S. Bile Acid Signaling Is Involved in the Neurological Decline in a Murine Model of Acute Liver Failure. Am. J. Pathol. 2016, 186, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Staudinger, J.L.; Goodwin, B.; Jones, S.A.; Hawkins-Brown, D.; MacKenzie, K.I.; LaTour, A.; Liu, Y.; Klaassen, C.D.; Brown, K.K.; Reinhard, J.; et al. The Nuclear Receptor PXR Is a Lithocholic Acid Sensor That Protects against Liver Toxicity. Proc. Natl. Acad. Sci. USA 2001, 98, 3369–3374. [Google Scholar] [CrossRef]
- Lamba, V.; Yasuda, K.; Lamba, J.K.; Assem, M.; Davila, J.; Strom, S.; Schuetz, E.G. PXR (NR1I2): Splice Variants in Human Tissues, Including Brain, and Identification of Neurosteroids and Nicotine as PXR Activators. Toxicol. Appl. Pharmacol. 2004, 199, 251–265. [Google Scholar] [CrossRef]
- Ishizawa, M.; Matsunawa, M.; Adachi, R.; Uno, S.; Ikeda, K.; Masuno, H.; Shimizu, M.; Iwasaki, K.I.; Yamada, S.; Makishima, M. Lithocholic Acid Derivatives Act as Selective Vitamin D Receptor Modulators without Inducing Hypercalcemia. J. Lipid Res. 2008, 49, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Prüfer, K.; Veenstra, T.D.; Jirikowski, G.F.; Kumar, R. Distribution of 1,25-Dihydroxyvitamin D3 Receptor Immunoreactivity in the Rat Brain and Spinal Cord. J. Chem. Neuroanat. 1999, 16, 135–145. [Google Scholar] [CrossRef] [PubMed]
- McMillin, M.; Frampton, G.; Quinn, M.; Divan, A.; Grant, S.; Patel, N.; Newell-Rogers, K.; DeMorrow, S. Suppression of the HPA Axis during Cholestasis Can Be Attributed to Hypothalamic Bile Acid Signaling. Mol. Endocrinol. 2015, 29, 1720–1730. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Hiipakka, R.A.; Liao, S. Selective Activation of Liver X Receptor Alpha by 6α-Hydroxy Bile Acids and Analogs. Steroids 2000, 65, 423–427. [Google Scholar] [CrossRef]
- Kainu, T.; Kononen, J.; Enmark, E.; Gustafsson, J.A.; Pelto-Huikko, M. Localization and Ontogeny of the Orphan Receptor OR-1 in the Rat Brain. J. Mol. Neurosci. 1996, 7, 29–39. [Google Scholar] [CrossRef]
- Cao, C.; Dai, L.; Mu, J.; Wang, X.; Hong, Y.; Zhu, C.; Jin, L.; Li, S. S1PR2 Antagonist Alleviates Oxidative Stress-Enhanced Brain Endothelial Permeability by Attenuating P38 and Erk1/2-Dependent CPLA2 Phosphorylation. Cell. Signal. 2019, 53, 151–161. [Google Scholar] [CrossRef]
- Liu, R.; Li, X.; Qiang, X.; Luo, L.; Hylemon, P.B.; Jiang, Z.; Zhang, L.; Zhou, H. Taurocholate Induces Cyclooxygenase-2 Expression via the Sphingosine 1-Phosphate Receptor 2 in a Human Cholangiocarcinoma Cell Line. J. Biol. Chem. 2015, 290, 30988–31002. [Google Scholar] [CrossRef]
- Studer, E.; Zhou, X.; Zhao, R.; Wang, Y.; Takabe, K.; Nagahashi, M.; Pandak, W.M.; Dent, P.; Spiegel, S.; Shi, R.; et al. Conjugated Bile Acids Activate the Sphingosine-1-Phosphate Receptor 2 in Primary Rodent Hepatocytes. Hepatology 2012, 55, 267–276. [Google Scholar] [CrossRef]
- Fleishman, J.S.; Kumar, S. Bile Acid Metabolism and Signaling in Health and Disease: Molecular Mechanisms and Therapeutic Targets. Signal Transduct. Target. Ther. 2024, 9, 97. [Google Scholar] [CrossRef]
- Pircher, P.C.; Kitto, J.L.; Petrowski, M.L.; Tangirala, R.K.; Bischoff, E.D.; Schulman, I.G.; Westin, S.K. Farnesoid X Receptor Regulates Bile Acid-Amino Acid Conjugation. J. Biol. Chem. 2003, 278, 27703–27711. [Google Scholar] [CrossRef]
- Huang, F.; Wang, T.; Lan, Y.; Yang, L.; Pan, W.; Zhu, Y.; Lv, B.; Wei, Y.; Shi, H.; Wu, H.; et al. Deletion of Mouse FXR Gene Disturbs Multiple Neurotransmitter Systems and Alters Neurobehavior. Front. Behav. Neurosci. 2015, 9, 70. [Google Scholar] [CrossRef] [PubMed]
- Lew, J.L.; Zhao, A.; Yu, J.; Huang, L.; De Pedro, N.; Peláez, F.; Wright, S.D.; Cui, J. The Farnesoid X Receptor Controls Gene Expression in a Ligand- and Promoter-Selective Fashion. J. Biol. Chem. 2004, 279, 8856–8861. [Google Scholar] [CrossRef] [PubMed]
- Xie, W.; Radominska-Pandya, A.; Shi, Y.; Simon, C.M.; Nelson, M.C.; Ong, E.S.; Waxman, D.J.; Evans, R.M. An Essential Role for Nuclear Receptors SXR/PXR in Detoxification of Cholestatic Bile Acids. Proc. Natl. Acad. Sci. USA 2001, 98, 3375–3380. [Google Scholar] [CrossRef] [PubMed]
- Boussadia, B.; Lakhal, L.; Payrastre, L.; Ghosh, C.; Pascussi, J.M.; Gangarossa, G.; Marchi, N. Pregnane X Receptor Deletion Modifies Recognition Memory and Electroencephalographic Activity. Neuroscience 2018, 370, 130–138. [Google Scholar] [CrossRef]
- Chen, X.; Chen, F.; Liu, S.; Glaeser, H.; Dawson, P.A.; Hofmann, A.F.; Kim, R.B.; Shneider, B.L.; Pang, K.S. Transactivation of Rat Apical Sodium-Dependent Bile Acid Transporter and Increased Bile Acid Transport by 1α,25-Dihydroxyvitamin D3 via the Vitamin D Receptor. Mol. Pharmacol. 2006, 69, 1913–1923. [Google Scholar] [CrossRef]
- Jurutka, P.W.; Thompson, P.D.; Whitfield, G.K.; Eichhorst, K.R.; Hall, N.; Dominguez, C.E.; Hsieh, J.C.; Haussler, C.A.; Haussler, M.R. Molecular and Functional Comparison of 1,25-Dihydroxyvitamin D3 and the Novel Vitamin D Receptor Ligand, Lithocholic Acid, in Activating Transcription of Cytochrome P450 3A4. J. Cell. Biochem. 2005, 94, 917–943. [Google Scholar] [CrossRef]
- McCarthy, T.C.; Li, X.; Sinal, C.J. Vitamin D Receptor-Dependent Regulation of Colon Multidrug Resistance-Associated Protein 3 Gene Expression by Bile Acids. J. Biol. Chem. 2005, 280, 23232–23242. [Google Scholar] [CrossRef]
- Nehring, J.A.; Zierold, C.; DeLuca, H.F. Lithocholic Acid Can Carry out in Vivo Functions of Vitamin D. Proc. Natl. Acad. Sci. USA 2007, 104, 10006–10009. [Google Scholar] [CrossRef]
- Viho, E.M.G.; Buurstede, J.C.; Mahfouz, A.; Koorneef, L.L.; Van Weert, L.T.C.M.; Houtman, R.; Hunt, H.J.; Kroon, J.; Meijer, O.C. Corticosteroid Action in the Brain: The Potential of Selective Receptor Modulation. Neuroendocrinology 2019, 109, 266–276. [Google Scholar] [CrossRef]
- Solá, S.; Amaral, J.D.; Borralho, P.M.; Ramalho, R.M.; Castro, R.E.; Aranha, M.M.; Steer, C.J.; Rodrigues, C.M.P. Functional Modulation of Nuclear Steroid Receptors by Tauroursodeoxycholic Acid Reduces Amyloid β-Peptide-Induced Apoptosis. Mol. Endocrinol. 2006, 20, 2292–2303. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Silva, S.; Da Silva, J.D.; Monteiro-Fernandes, D.; Costa, M.D.; Neves-Carvalho, A.; Raposo, M.; Soares-Cunha, C.; Correia, J.S.; Nogueira-Goncalves, G.; Fernandes, H.S.; et al. Glucocorticoid Receptor-Dependent Therapeutic Efficacy of Tauroursodeoxycholic Acid in Preclinical Models of Spinocerebellar Ataxia Type 3. J. Clin. Investig. 2024, 134, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Vaya, J.; Schipper, H.M. Oxysterols, Cholesterol Homeostasis, and Alzheimer Disease. J. Neurochem. 2007, 102, 1727–1737. [Google Scholar] [CrossRef]
- Venkateswaran, A.; Repa, J.J.; Lobaccaro, J.M.A.; Bronson, A.; Mangelsdorf, D.J.; Edwards, P.A. Human White/Murine ABC8 MRNA Levels Are Highly Induced in Lipid-Loaded Macrophages. A Transcriptional Role for Specific Oxysterols. J. Biol. Chem. 2000, 275, 14700–14707. [Google Scholar] [CrossRef] [PubMed]
- Terwel, D.; Steffensen, K.R.; Verghese, P.B.; Kummer, M.P.; Gustafsson, J.Å.; Holtzman, D.M.; Heneka, M.T. Critical Role of Astroglial Apolipoprotein E and Liver X Receptor-α Expression for Microglial Aβ Phagocytosis. J. Neurosci. 2011, 31, 7049–7059. [Google Scholar] [CrossRef] [PubMed]
- Schulman, I.G. Liver X Receptors Link Lipid Metabolism and Inflammation. FEBS Lett. 2017, 591, 2978–2991. [Google Scholar] [CrossRef]
- De Marino, S.; Carino, A.; Masullo, D.; Finamore, C.; Marchianò, S.; Cipriani, S.; Di Leva, F.S.; Catalanotti, B.; Novellino, E.; Limongelli, V.; et al. Hyodeoxycholic Acid Derivatives as Liver X Receptor α and G-Protein-Coupled Bile Acid Receptor Agonists. Sci. Rep. 2017, 7, 43290. [Google Scholar] [CrossRef] [PubMed]
- Kawamata, Y.; Fujii, R.; Hosoya, M.; Harada, M.; Yoshida, H.; Miwa, M.; Fukusumi, S.; Habata, Y.; Itoh, T.; Shintani, Y.; et al. A G Protein-Coupled Receptor Responsive to Bile Acids. J. Biol. Chem. 2003, 278, 9435–9440. [Google Scholar] [CrossRef]
- Keitel, V.; Görg, B.; Bidmon, H.J.; Zemtsova, I.; Spomer, L.; Zilles, K.; Häussinger, D. The Bile Acid Receptor TGR5 (Gpbar-1) Acts as a Neurosteroid Receptor in Brain. Glia 2010, 58, 1794–1805. [Google Scholar] [CrossRef]
- Pellicciari, R.; Gioiello, A.; Macchiarulo, A.; Thomas, C.; Rosatelli, E.; Natalini, B.; Sardella, R.; Pruzanski, M.; Roda, A.; Pastorini, E.; et al. Discovery of 6α-Ethyl-23(S)-Methylcholic Acid (S-EMCA, INT-777) as a Potent and Selective Agonist for the TGR5 Receptor, a Novel Target for Diabesity. J. Med. Chem. 2009, 52, 7958–7961. [Google Scholar] [CrossRef]
- Kimoto, T.; Tsurugizawa, T.; Ohta, Y.; Makino, J.; Tamura, H.O.; Hojo, Y.; Takata, N.; Kawato, S. Neurosteroid Synthesis by Cytochrome P450-Containing Systems Localized in the Rat Brain Hippocampal Neurons: N-Methyl-D-Aspartate and Calcium-Dependent Synthesis. Endocrinology 2001, 142, 3578–3589. [Google Scholar] [CrossRef]
- Yilmaz, C.; Karali, K.; Fodelianaki, G.; Gravanis, A.; Chavakis, T.; Charalampopoulos, I.; Alexaki, V.I. Neurosteroids as Regulators of Neuroinflammation. Front. Neuroendocrinol. 2019, 55, 100788. [Google Scholar] [CrossRef] [PubMed]
- McMillin, M.; Frampton, G.; Tobin, R.; Dusio, G.; Smith, J.; Shin, H.; Newell-Rogers, K.; Grant, S.; DeMorrow, S. TGR5 Signaling Reduces Neuroinflammation during Hepatic Encephalopathy. J. Neurochem. 2015, 135, 565–576. [Google Scholar] [CrossRef]
- Sato, H.; Macchiarulo, A.; Thomas, C.; Gioiello, A.; Une, M.; Hofmann, A.F.; Saladin, R.; Schoonjans, K.; Pellicciari, R.; Auwerx, J. Novel Potent and Selective Bile Acid Derivatives as TGR5 Agonists: Biological Screening, Structure-Activity Relationships, and Molecular Modeling Studies. J. Med. Chem. 2008, 51, 1831–1841. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Guan, J.; Wu, Z.; Xu, L.; Sun, C. The TGR5 Agonist INT-777 Promotes Peripheral Nerve Regeneration by Activating CAMP-Dependent Protein Kinase A in Schwann Cells. Mol. Neurobiol. 2023, 60, 1901–1913. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.; Matei, N.; McBride, D.W.; Xu, Y.; Tang, J.; Luo, B.; Zhang, J.H. Activation of TGR5 Protects Blood Brain Barrier via the BRCA1/Sirt1 Pathway after Middle Cerebral Artery Occlusion in Rats. J. Biomed. Sci. 2020, 27, 61. [Google Scholar] [CrossRef]
- Poole, D.P.; Godfrey, C.; Cattaruzza, F.; Cottrell, G.S.; Kirkland, J.G.; Pelayo, J.C.; Bunnett, N.W.; Corvera, C.U. Expression and Function of the Bile Acid Receptor GpBAR1 (TGR5) in the Murine Enteric Nervous System. Neurogastroenterol. Motil. 2010, 22, 814-e228. [Google Scholar] [CrossRef]
- Alemi, F.; Kwon, E.; Poole, D.P.; Lieu, T.M.; Lyo, V.; Cattaruzza, F.; Cevikbas, F.; Steinhoff, M.; Nassini, R.; Materazzi, S.; et al. The TGR5 Receptor Mediates Bile Acid-Induced Itch and Analgesia. J. Clin. Investig. 2013, 123, 1513–1530. [Google Scholar] [CrossRef]
- Wang, H.; Tan, Y.Z.; Mu, R.H.; Tang, S.S.; Liu, X.; Xing, S.Y.; Long, Y.; Yuan, D.H.; Hong, H. Takeda G Protein–Coupled Receptor 5 Modulates Depression-like Behaviors via Hippocampal CA3 Pyramidal Neurons Afferent to Dorsolateral Septum. Biol. Psychiatry 2021, 89, 1084–1095. [Google Scholar] [CrossRef] [PubMed]
- Perino, A.; Velázquez-Villegas, L.A.; Bresciani, N.; Sun, Y.; Huang, Q.; Fénelon, V.S.; Castellanos-Jankiewicz, A.; Zizzari, P.; Bruschetta, G.; Jin, S.; et al. Central Anorexigenic Actions of Bile Acids Are Mediated by TGR5. Nat. Metab. 2021, 3, 595–603. [Google Scholar] [CrossRef]
- Genet, C.; Strehle, A.; Schmidt, C.; Boudjelal, G.; Lobstein, A.; Schoonjans, K.; Souchet, M.; Auwerx, J.; Saladin, R.; Wagner, A. Structure—Activity Relationship Study of Betulinic Acid, a Novel and Selective TGR5 Agonist, and Its Synthetic Derivatives: Potential Impact in Diabetes. J. Med. Chem. 2010, 53, 178–190. [Google Scholar] [CrossRef]
- Cipriani, S.; Mencarelli, A.; Chini, M.G.; Distrutti, E.; Renga, B.; Bifulco, G.; Baldelli, F.; Donini, A.; Fiorucci, S. The Bile Acid Receptor GPBAR-1 (TGR5) Modulates Integrity of Intestinal Barrier and Immune Response to Experimental Colitis. PLoS ONE 2011, 6, e25637. [Google Scholar] [CrossRef] [PubMed]
- Smaling, A.; Romero-Ramírez, L.; Mey, J. Is TGR5 a Therapeutic Target for the Treatment of Spinal Cord Injury? J. Neurochem. 2023, 164, 454–467. [Google Scholar] [CrossRef]
- Guo, C.; Xie, S.; Chi, Z.; Zhang, J.; Liu, Y.; Zhang, L.; Zheng, M.; Zhang, X.; Xia, D.; Ke, Y.; et al. Bile Acids Control Inflammation and Metabolic Disorder through Inhibition of NLRP3 Inflammasome. Immunity 2016, 45, 802–816. [Google Scholar] [CrossRef]
- Pols, T.W.H.; Nomura, M.; Harach, T.; Lo Sasso, G.; Oosterveer, M.H.; Thomas, C.; Rizzo, G.; Gioiello, A.; Adorini, L.; Pellicciari, R.; et al. TGR5 Activation Inhibits Atherosclerosis by Reducing Macrophage Inflammation and Lipid Loading. Cell Metab. 2011, 14, 747–757. [Google Scholar] [CrossRef]
- Wang, Y.D.; Chen, W.D.; Yu, D.; Forman, B.M.; Huang, W. The G-Protein-Coupled Bile Acid Receptor, Gpbar1 (TGR5), Negatively Regulates Hepatic Inflammatory Response through Antagonizing Nuclear Factor Kappa Light-Chain Enhancer of Activated B Cells (NF-ΚB) in Mice. Hepatology 2011, 54, 1421–1432. [Google Scholar] [CrossRef]
- Metzger, Z.; Hoffeld, J.T.; Oppenheim, J.J. Regulation by PGE2 of the Production of Oxygen Intermediates by LPS-Activated Macrophages. J. Immunol. 1981, 127, 1109–1113. [Google Scholar] [CrossRef]
- Ollivier, V.; Parry, G.C.N.; Cobb, R.R.; De Prost, D.; Mackman, N. Elevated Cyclic AMP Inhibits NF-ΚB-Mediated Transcription in Human Monocytic Cells and Endothelial Cells. J. Biol. Chem. 1996, 271, 20828–20835. [Google Scholar] [CrossRef] [PubMed]
- Zhong, H.; Voll, R.E.; Ghosh, S. Phosphorylation of NF-ΚB P65 by PKA Stimulates Transcriptional Activity by Promoting a Novel Bivalent Interaction with the Coactivator CBP/P300. Mol. Cell 1998, 1, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Yanguas-Casás, N.; Barreda-Manso, M.A.; Pérez-Rial, S.; Nieto–Sampedro, M.; Romero-Ramírez, L. TGFβ Contributes to the Anti-Inflammatory Effects of Tauroursodeoxycholic Acid on an Animal Model of Acute Neuroinflammation. Mol. Neurobiol. 2017, 54, 6737–6749. [Google Scholar] [CrossRef]
- Li, X.Y.; Zhang, S.Y.; Hong, Y.Z.; Chen, Z.G.; Long, Y.; Yuan, D.H.; Zhao, J.J.; Tang, S.S.; Wang, H.; Hong, H. TGR5-Mediated Lateral Hypothalamus-DCA3-Dorsolateral Septum Circuit Regulates Depressive-like Behavior in Male Mice. Neuron 2024, 112, 1795–1814. [Google Scholar] [CrossRef]
- Yasuda, H.; Hirata, S.; Inoue, K.; Mashima, H.; Ohnishi, H.; Yoshiba, M. Involvement of Membrane-Type Bile Acid Receptor M-BAR/TGR5 in Bile Acid-Induced Activation of Epidermal Growth Factor Receptor and Mitogen-Activated Protein Kinases in Gastric Carcinoma Cells. Biochem. Biophys. Res. Commun. 2007, 354, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Vassileva, G.; Golovko, A.; Markowitz, L.; Abbondanzo, S.J.; Zeng, M.; Yang, S.; Hoos, L.; Tetzloff, G.; Levitan, D.; Murgolo, N.J.; et al. Targeted Deletion of Gpbar1 Protects Mice from Cholesterol Gallstone Formation. Biochem. J. 2006, 398, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, T.; Tanaka, K.; Suzuki, J.; Miyoshi, H.; Harada, N.; Nakamura, T.; Miyamoto, Y.; Kanatani, A.; Tamai, Y. Targeted Disruption of G Protein-Coupled Bile Acid Receptor 1 (Gpbar1/M-Bar) in Mice. J. Endocrinol. 2006, 191, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Vassileva, G.; Hu, W.; Hoos, L.; Tetzloff, G.; Yang, S.; Liu, L.; Kang, L.; Davis, H.R.; Hedrick, J.A.; Lan, H.; et al. Gender-Dependent Effect of Gpbar1 Genetic Deletion on the Metabolic Profiles of Diet-Induced Obese Mice. J. Endocrinol. 2010, 205, 225–232. [Google Scholar] [CrossRef]
- Patte-Mensah, C.; Kappes, V.; Freund-Mercier, M.J.; Tsutsui, K.; Mensah-Nyagan, A.G. Cellular Distribution and Bioactivity of the Key Steroidogenic Enzyme, Cytochrome P450side Chain Cleavage, in Sensory Neural Pathways. J. Neurochem. 2003, 86, 1233–1246. [Google Scholar] [CrossRef] [PubMed]
- Legesse, D.H.; Fan, C.; Teng, J.; Zhuang, Y.; Howard, R.J.; Noviello, C.M.; Lindahl, E.; Hibbs, R.E. Structural Insights into Opposing Actions of Neurosteroids on GABAA Receptors. Nat. Commun. 2023, 14, 5091. [Google Scholar] [CrossRef]
- Song, H.; Liu, J.; Wang, L.; Hu, X.; Li, J.; Zhu, L.; Pang, R.; Zhang, A. Tauroursodeoxycholic Acid: A Bile Acid That May Be Used for the Prevention and Treatment of Alzheimer’s Disease. Front. Neurosci. 2024, 18, 1348844. [Google Scholar] [CrossRef]
- Li, C.; Wang, L.; Xie, W.; Chen, E.; Chen, Y.; Li, H.; Can, D.; Lei, A.; Wang, Y.; Zhang, J. TGR5 Deficiency in Excitatory Neurons Ameliorates Alzheimer’s Pathology by Regulating APP Processing. Sci. Adv. 2024, 10, eado1855. [Google Scholar] [CrossRef]
- Rodrigues, C.M.P.; Spellman, S.R.; Solá, S.; Grande, A.W.; Linehan-Stieers, C.; Low, W.C.; Steer, C.J. Neuroprotection by a Bile Acid in an Acute Stroke Model in the Rat. J. Cereb. Blood Flow Metab. 2002, 22, 463–471. [Google Scholar] [CrossRef]
- Castro, R.E.; Solá, S.; Ramalho, R.M.; Steer, C.J.; Rodrigues, C.M.P. The Bile Acid Tauroursodeoxycholic Acid Modulates Phosphorylation and Translocation of Bad via Phosphatidylinositol 3-Kinase in Glutamate-Induced Apoptosis of Rat Cortical Neurons. J. Pharmacol. Exp. Ther. 2004, 311, 845–852. [Google Scholar] [CrossRef]
- Wu, H.; Yu, N.; Wang, X.; Yang, Y.; Liang, H. Tauroursodeoxycholic Acid Attenuates Neuronal Apoptosis via the TGR5/ SIRT3 Pathway after Subarachnoid Hemorrhage in Rats. Biol. Res. 2020, 53, 56. [Google Scholar] [CrossRef] [PubMed]
- Zuo, G.; Zhang, T.; Huang, L.; Araujo, C.; Peng, J.; Travis, Z.; Okada, T.; Ocak, U.; Zhang, G.; Tang, J.; et al. Activation of TGR5 with INT-777 Attenuates Oxidative Stress and Neuronal Apoptosis via CAMP/PKCε/ALDH2 Pathway after Subarachnoid Hemorrhage in Rats. Free Radic. Biol. Med. 2019, 143, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Yanguas-Casás, N.; Barreda-Manso, M.A.; Nieto-Sampedro, M.; Romero-Ramírez, L. Tauroursodeoxycholic Acid Reduces Glial Cell Activation in an Animal Model of Acute Neuroinflammation. J. Neuroinflamm. 2014, 11, 50. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Deng, T.; Zhang, Y.; Su, S.; Wei, C.; Han, D. Lipopolysaccharide Inhibits Macrophage Phagocytosis of Apoptotic Neutrophils by Regulating the Production of Tumour Necrosis Factor α and Growth Arrest-Specific Gene 6. Immunology 2011, 132, 287–295. [Google Scholar] [CrossRef]
- McPhillips, K.; Janssen, W.J.; Ghosh, M.; Byrne, A.; Gardai, S.; Remigio, L.; Bratton, D.L.; Kang, J.L.; Henson, P. TNF-α Inhibits Macrophage Clearance of Apoptotic Cells via Cytosolic Phospholipase A2 and Oxidant-Dependent Mechanisms. J. Immunol. 2007, 178, 8117–8126. [Google Scholar] [CrossRef]
- Wu, S.; Romero-Ramírez, L.; Mey, J. Taurolithocholic Acid but Not Tauroursodeoxycholic Acid Rescues Phagocytosis Activity of Bone Marrow-Derived Macrophages under Inflammatory Stress. J. Cell. Physiol. 2022, 237, 1455–1470. [Google Scholar] [CrossRef]
- Romero-Ramírez, L.; Nieto-Sampedro, M.; Yanguas-Casás, N. Tauroursodeoxycholic Acid: More than Just a Neuroprotective Bile Conjugate. Neural Regen. Res. 2017, 12, 62. [Google Scholar] [CrossRef]
- Keene, C.D.; Rodrigues, C.M.P.; Eich, T.; Linehan-Stieers, C.; Abt, A.; Kren, B.T.; Steer, C.J.; Low, W.C. A Bile Acid Protects against Motor and Cognitive Deficits and Reduces Striatal Degeneration in the 3-Nitropropionic Acid Model of Huntington’s Disease. Exp. Neurol. 2001, 171, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Keene, C.D.; Rodrigues, C.M.P.; Eich, T.; Chhabra, M.S.; Steer, C.J.; Low, W.C. Tauroursodeoxycholic Acid, a Bile Acid, Is Neuroprotective in a Transgenic Animal Model of Huntington’s Disease. Proc. Natl. Acad. Sci. USA 2002, 99, 10671–10676. [Google Scholar] [CrossRef]
- Wang, S.; Xu, C.; Liu, H.; Wei, W.; Zhou, X.; Qian, H.; Zhou, L.; Zhang, H.; Wu, L.; Zhu, C.; et al. Connecting the Gut Microbiota and Neurodegenerative Diseases: The Role of Bile Acids. Mol. Neurobiol. 2023, 60, 4618–4640. [Google Scholar] [CrossRef]
- Trefflich, I.; Marschall, H.U.; Di Giuseppe, R.; Ståhlman, M.; Michalsen, A.; Lampen, A.; Abraham, K.; Weikert, C. Associations between Dietary Patterns and Bile Acids—Results from a Cross-Sectional Study in Vegans and Omnivores. Nutrients 2020, 12, 47. [Google Scholar] [CrossRef] [PubMed]
- Van Den Brink, A.C.; Brouwer-Brolsma, E.M.; Berendsen, A.A.M.; Van De Rest, O. The Mediterranean, Dietary Approaches to Stop Hypertension (DASH), and Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) Diets Are Associated with Less Cognitive Decline and a Lower Risk of Alzheimer’s Disease—A Review. Adv. Nutr. 2019, 10, 1040–1065. [Google Scholar] [CrossRef]
- Yoshioka, H.; Watanabe, M.; Nanba, F.; Suzuki, T.; Fukiya, S.; Yokota, A.; Toda, T. Administration of Cholic Acid Inhibits Equol Production from Daidzein in Mice. J. Nutr. Sci. Vitaminol. 2020, 66, 571–576. [Google Scholar] [CrossRef]
- Dodge, J.C.; Yu, J.; Sardi, S.P.; Shihabuddin, L.S. Sterol Auto-Oxidation Adversely Affects Human Motor Neuron Viability and Is a Neuropathological Feature of Amyotrophic Lateral Sclerosis. Sci. Rep. 2021, 11, 803. [Google Scholar] [CrossRef]
- Lee, I.; Nandakumar, R.; Haeusler, R.A. Alteration of Serum Bile Acids in Amyotrophic Lateral Sclerosis. Lipids 2024, 59, 85–91. [Google Scholar] [CrossRef]
- Di Gioia, D.; Bozzi Cionci, N.; Baffoni, L.; Amoruso, A.; Pane, M.; Mogna, L.; Gaggìa, F.; Lucenti, M.A.; Bersano, E.; Cantello, R.; et al. A Prospective Longitudinal Study on the Microbiota Composition in Amyotrophic Lateral Sclerosis. BMC Med. 2020, 18, 153. [Google Scholar] [CrossRef]
- Graham, S.F.; Rey, N.L.; Yilmaz, A.; Kumar, P.; Madaj, Z.; Maddens, M.; Bahado-singh, R.O.; Becker, K.; Schulz, E.; Lindsay, K.; et al. Biochemical Profiling of the Brain and Blood Metabolome in a Mouse Model of Prodromal Parkinson’s Disease Reveal Distinct Metabolic Profiles. J. Proteome Res. 2019, 17, 2460–2469. [Google Scholar] [CrossRef] [PubMed]
- Kiriyama, Y.; Nochi, H. Role of Microbiota-Modified Bile Acids in the Regulation of Intracellular Organelles and Neurodegenerative Diseases. Genes 2023, 14, 825. [Google Scholar] [CrossRef]
- Grant, S.M.; Demorrow, S. Bile Acid Signaling in Neurodegenerative and Neurological Disorders. Int. J. Mol. Sci. 2020, 21, 5982. [Google Scholar] [CrossRef] [PubMed]
- Leoni, V.; Mariotti, C.; Nanetti, L.; Salvatore, E.; Squitieri, F.; Bentivoglio, A.R.; Bandettini del Poggio, M.; Piacentini, S.; Monza, D.; Valenza, M.; et al. Whole Body Cholesterol Metabolism Is Impaired in Huntington’s Disease. Neurosci. Lett. 2011, 494, 245–249. [Google Scholar] [CrossRef]
- Chen, T.; Wang, L.; Xie, G.; Kristal, B.S.; Zheng, X.; Sun, T.; Arnold, M.; Louie, G.; Li, M.; Wu, L.; et al. Serum Bile Acids Improve Prediction of Alzheimer’s Progression in a Sex-Dependent Manner. Adv. Sci. 2024, 11, e2306576. [Google Scholar] [CrossRef]
- Marksteiner, J.; Blasko, I.; Kemmler, G.; Koal, T.; Humpel, C. Bile Acid Quantification of 20 Plasma Metabolites Identifies Lithocholic Acid as a Putative Biomarker in Alzheimer’s Disease. Metabolomics 2018, 14, 1. [Google Scholar] [CrossRef]
- Varma, V.R.; Wang, Y.; An, Y.; Varma, S.; Bilgel, M.; Doshi, J.; Legido-Quigley, C.; Delgado, J.C.; Oommen, A.M.; Roberts, J.A.; et al. Bile Acid Synthesis, Modulation, and Dementia: A Metabolomic, Transcriptomic, and Pharmacoepidemiologic Study. PLoS Med. 2021, 18, e1003615. [Google Scholar] [CrossRef]
- MahmoudianDehkordi, S.; Arnold, M.; Nho, K.; Ahmad, S.; Jia, W.; Xie, G.; Louie, G.; Kueider-Paisley, A.; Moseley, M.A.; Thompson, J.W.; et al. Altered Bile Acid Profile Associates with Cognitive Impairment in Alzheimer’s Disease—An Emerging Role for Gut Microbiome. Alzheimer’s Dement. 2019, 15, 76–92. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Zhao, M.; Li, M.; Guo, Q.; Ren, Z.; Zheng, X.; Chen, T. The Clinical and Mechanistic Roles of Bile Acids in Depression, Alzheimer’s Disease, and Stroke. Proteomics 2022, 22, e2100324. [Google Scholar] [CrossRef]
- Feng, L.; Zhou, N.; Li, Z.; Fu, D.; Guo, Y.; Gao, X.; Liu, X. Co-Occurrence of Gut Microbiota Dysbiosis and Bile Acid Metabolism Alteration Is Associated with Psychological Disorders in Crohn’s Disease. FASEB J. 2022, 36, e22100. [Google Scholar] [CrossRef] [PubMed]
- MahmoudianDehkordi, S.; Bhattacharyya, S.; Brydges, C.R.; Jia, W.; Fiehn, O.; Rush, A.J.; Dunlop, B.W.; Kaddurah-Daouk, R. Gut Microbiome-Linked Metabolites in the Pathobiology of Major Depression With or Without Anxiety—A Role for Bile Acids. Front. Neurosci. 2022, 16, 937906. [Google Scholar] [CrossRef] [PubMed]
- Freedman, S.N.; Shahi, S.K.; Mangalam, A.K. The “Gut Feeling”: Breaking Down the Role of Gut Microbiome in Multiple Sclerosis. Neurotherapeutics 2018, 15, 109–125. [Google Scholar] [CrossRef]
- Bhargava, P.; Smith, M.D.; Mische, L.; Harrington, E.; Fitzgerald, K.C.; Martin, K.; Kim, S.; Reyes, A.A.; Gonzalez-Cardona, J.; Volsko, C.; et al. Bile Acid Metabolism Is Altered in Multiple Sclerosis and Supplementation Ameliorates Neuroinflammation. J. Clin. Investig. 2020, 130, 3467–3482. [Google Scholar] [CrossRef]
- Ladakis, A.D.C.; Harrison, K.L.; Smith, M.D.; Solem, K.; Gadani, S.; Jank, L.; Hwang, S.; Farhadi, F.; Dewey, B.E.; Fitzgerald, K.C.; et al. Bile Acid Metabolites Predict Multiple Sclerosis Progression and Supplementation Is Safe in Progressive Disease. medRxiv 2024. [Google Scholar] [CrossRef]
- Weng, J.; Wang, L.; Wang, K.; Su, H.; Luo, D.; Yang, H.; Wen, Y.; Wu, Q.; Li, X. Tauroursodeoxycholic Acid Inhibited Apoptosis and Oxidative Stress in H2O2-Induced BMSC Death via Modulating the Nrf-2 Signaling Pathway: The Therapeutic Implications in a Rat Model of Spinal Cord Injury. Mol. Neurobiol. 2023, 61, 3753–3768. [Google Scholar] [CrossRef]
- Wu, S.; García-Rama, C.; Romero-Ramírez, L.; de Munter, J.P.J.M.; Wolters, E.C.; Kramer, B.W.; Mey, J. Tauroursodeoxycholic Acid Reduces Neuroinflammation but Does Not Support Long Term Functional Recovery of Rats with Spinal Cord Injury. Biomedicines 2022, 10, 1501. [Google Scholar] [CrossRef]
- Han, G.H.; Kim, S.J.; Ko, W.K.; Lee, D.; Han, I.B.; Sheen, S.H.; Hong, J.B.; Sohn, S. Transplantation of Tauroursodeoxycholic Acid–Inducing M2-Phenotype Macrophages Promotes an Anti-Neuroinflammatory Effect and Functional Recovery after Spinal Cord Injury in Rats. Cell Prolif. 2021, 54, e13050. [Google Scholar] [CrossRef] [PubMed]
- Sahu, S.; Li, R.; Kadeyala, P.K.; Liu, S.; Schachner, M. The Human Natural Killer-1 (HNK-1) Glycan Mimetic Ursolic Acid Promotes Functional Recovery after Spinal Cord Injury in Mouse. J. Nutr. Biochem. 2018, 55, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.L.; Ren, C.H.; Feng, J.; Ou, C.H.; Liu, L. Oleanolic Acid Inhibits Mouse Spinal Cord Injury through Suppressing Inflammation and Apoptosis via the Blockage of P38 and JNK MAPKs. Biomed. Pharmacother. 2020, 123, 109752. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Luan, J.; Huang, T.; Deng, T.; Li, X.; Xiao, Z.; Zhan, J.; Luo, D.; Hou, Y.; Xu, L.; et al. Tauroursodeoxycholic Acid Alleviates Secondary Injury in Spinal Cord Injury Mice by Reducing Oxidative Stress, Apoptosis, and Inflammatory Response. J. Neuroinflamm. 2021, 18, 216. [Google Scholar] [CrossRef]
- Thams, S.; Lowry, E.R.; Larraufie, M.H.; Spiller, K.J.; Li, H.; Williams, D.J.; Hoang, P.; Jiang, E.; Williams, L.A.; Sandoe, J.; et al. A Stem Cell-Based Screening Platform Identifies Compounds That Desensitize Motor Neurons to Endoplasmic Reticulum Stress. Mol. Ther. 2019, 27, 87–101. [Google Scholar] [CrossRef]
- Parry, G.J.; Rodrigues, C.M.P.; Aranha, M.M.; Hilbert, S.J.; Davey, C.; Kelkar, P.; Low, W.C.; Steer, C.J. Safety, Tolerability, and Cerebrospinal Fluid Penetration of Ursodeoxycholic Acid in Patients With Amyotrophic Lateral Sclerosis. Clin. Neuropharmacol. 2010, 33, 17–21. [Google Scholar] [CrossRef]
- Min, J.H.; Hong, Y.H.; Sung, J.J.; Kim, S.M.; Lee, J.B.; Lee, K.W. Oral Solubilized Ursodeoxycholic Acid Therapy in Amyotrophic Lateral Sclerosis: A Randomized Cross-over Trial. J. Korean Med. Sci. 2012, 27, 200–206. [Google Scholar] [CrossRef]
- Paganoni, S.; Hendrix, S.; Dickson, S.P.; Knowlton, N.; Macklin, E.A.; Berry, J.D.; Elliott, M.A.; Maiser, S.; Karam, C.; Caress, J.B.; et al. Long-Term Survival of Participants in the CENTAUR Trial of Sodium Phenylbutyrate-Taurursodiol in Amyotrophic Lateral Sclerosis. Muscle Nerve 2021, 63, 31–39. [Google Scholar] [CrossRef]
- Reggiardo, G.; Lo Giudice, M.; Lalli, S.; Rinaldi, G.; Albanese, A. Cox Regression and Survival Analysis from the Tauro-Urso-Deoxycholic Trial in Amyotrophic Lateral Sclerosis. Front. Neurol. 2023, 14, 1163855. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.B.; Flynn, J.F.; Palacios, A.M. Capitalizing on Hope: Questionable Marketing Approval and Pricing of a New ALS Drug. Int. J. Soc. Determ. Health Health Serv. 2024. [Google Scholar] [CrossRef] [PubMed]
- Duan, W.M.; Rodrigues, C.M.P.; Zhao, L.R.; Steer, C.J.; Low, W.C. Tauroursodeoxycholic Acid Improves the Survival and Function of Nigral Transplants in a Rat Model of Parkinson’s Disease (Cell Transplantation 11:3 (195-205)). Cell Transplant. 2002, 11, 195, Erratum in Cell Transplant. 2002, 11, 619. [Google Scholar] [CrossRef]
- Castro-Caldas, M.; Carvalho, A.N.; Rodrigues, E.; Henderson, C.J.; Wolf, C.R.; Rodrigues, C.M.P.; Gama, M.J. Tauroursodeoxycholic Acid Prevents MPTP-Induced Dopaminergic Cell Death in a Mouse Model of Parkinson’s Disease. Mol. Neurobiol. 2012, 46, 475–486. [Google Scholar] [CrossRef]
- Moreira, S.; Fonseca, I.; Nunes, M.J.; Rosa, A.; Lemos, L.; Rodrigues, E.; Carvalho, A.N.; Outeiro, T.F.; Rodrigues, C.M.P.; Gama, M.J.; et al. Nrf2 Activation by Tauroursodeoxycholic Acid in Experimental Models of Parkinson’s Disease. Exp. Neurol. 2017, 295, 77–87. [Google Scholar] [CrossRef]
- Rosa, A.I.; Duarte-Silva, S.; Silva-Fernandes, A.; Nunes, M.J.; Carvalho, A.N.; Rodrigues, E.; Gama, M.J.; Rodrigues, C.M.P.; Maciel, P.; Castro-Caldas, M. Tauroursodeoxycholic Acid Improves Motor Symptoms in a Mouse Model of Parkinson’s Disease. Mol. Neurobiol. 2018, 55, 9139–9155. [Google Scholar] [CrossRef] [PubMed]
- Mendes, M.O.; Rosa, A.I.; Carvalho, A.N.; Nunes, M.J.; Dionísio, P.; Rodrigues, E.; Costa, D.; Duarte-Silva, S.; Maciel, P.; Rodrigues, C.M.P.; et al. Neurotoxic Effects of MPTP on Mouse Cerebral Cortex: Modulation of Neuroinflammation as a Neuroprotective Strategy. Mol. Cell. Neurosci. 2019, 96, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Qi, H.; Shen, D.; Jiang, C.; Wang, H.; Chang, M. Ursodeoxycholic Acid Protects Dopaminergic Neurons from Oxidative Stress via Regulating Mitochondrial Function, Autophagy, and Apoptosis in MPTP/MPP+-Induced Parkinson’s Disease. Neurosci. Lett. 2021, 741, 135493. [Google Scholar] [CrossRef] [PubMed]
- Payne, T.; Appleby, M.; Buckley, E.; van Gelder, L.M.A.; Mullish, B.H.; Sassani, M.; Dunning, M.J.; Hernandez, D.; Scholz, S.W.; McNeill, A.; et al. A Double-Blind, Randomized, Placebo-Controlled Trial of Ursodeoxycholic Acid (UDCA) in Parkinson’s Disease. Mov. Disord. 2023, 38, 1493–1502. [Google Scholar] [CrossRef]
- Dionísio, P.A.; Amaral, J.D.; Ribeiro, M.F.; Lo, A.C.; D’Hooge, R.; Rodrigues, C.M.P. Amyloid-β Pathology Is Attenuated by Tauroursodeoxycholic Acid Treatment in APP/PS1 Mice after Disease Onset. Neurobiol. Aging 2015, 36, 228–240. [Google Scholar] [CrossRef]
- Lo, A.C.; Callaerts-Vegh, Z.; Nunes, A.F.; Rodrigues, C.M.P.; D’Hooge, R. Tauroursodeoxycholic Acid (TUDCA) Supplementation Prevents Cognitive Impairment and Amyloid Deposition in APP/PS1 Mice. Neurobiol. Dis. 2013, 50, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Nunes, A.F.; Amaral, J.D.; Lo, A.C.; Fonseca, M.B.; Viana, R.J.S.; Callaerts-Vegh, Z.; D’Hooge, R.; Rodrigues, C.M.P. TUDCA, a Bile Acid, Attenuates Amyloid Precursor Protein Processing and Amyloid-β Deposition in APP/PS1 Mice. Mol. Neurobiol. 2012, 45, 440–454. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.; Zhao, L.; Zhao, M.; Bao, T.; Chen, T.; Zhao, A.; Zheng, X.; Gu, X.; Sun, T.; Guo, Y.; et al. Increased Intestinal Bile Acid Absorption Contributes to Age-Related Cognitive Impairment. Cell Rep. Med. 2024, 5, 101543. [Google Scholar] [CrossRef]
- Neuroscientists at Alzheimer’s Drug Discovery Foundation AMX0035. Cognitive Vitality Reports 2021. Available online: https://www.alzdiscovery.org/uploads/cognitive_vitality_media/AMX0035_UPDATE3_%28drug%29.pdf (accessed on 10 August 2024).
- Lu, X.; Yang, R.R.; Zhang, J.L.; Wang, P.; Gong, Y.; Hu, W.F.; Wu, Y.; Gao, M.H.; Huang, C. Tauroursodeoxycholic Acid Produces Antidepressant-like Effects in a Chronic Unpredictable Stress Model of Depression via Attenuation of Neuroinflammation, Oxido-Nitrosative Stress, and Endoplasmic Reticulum Stress. Fundam. Clin. Pharmacol. 2018, 32, 363–377. [Google Scholar] [CrossRef]
- Cheng, L.; Huang, C.; Chen, Z. Tauroursodeoxycholic Acid Ameliorates Lipopolysaccharide-Induced Depression Like Behavior in Mice via the Inhibition of Neuroinflammation and Oxido-Nitrosative Stress. Pharmacology 2019, 103, 93–100. [Google Scholar] [CrossRef]
- Kim, Y.K.; Na, K.S.; Myint, A.M.; Leonard, B.E. The Role of Pro-Inflammatory Cytokines in Neuroinflammation, Neurogenesis and the Neuroendocrine System in Major Depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2016, 64, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Bao, H.; Li, H.; Jia, Y.; Xiao, Y.; Luo, S.; Zhang, D.; Han, L.; Dai, L.; Xiao, C.; Feng, L.; et al. Ganoderic Acid A Exerted Antidepressant-like Action through FXR Modulated NLRP3 Inflammasome and Synaptic Activity. Biochem. Pharmacol. 2021, 188, 114561. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Bai, Y.; Han, X.; Yuan, J.; Wang, L.; He, Y.; Yang, L.; Wu, H.; Shi, H.; Wu, X. Taurochenodeoxycholic Acid Reduces Astrocytic Neuroinflammation and Alleviates Experimental Autoimmune Encephalomyelitis in Mice. Immunobiology 2023, 228, 152388. [Google Scholar] [CrossRef]
- Wang, Z.; Li, J.; Xu, Y.; Liu, Y.; Zhang, Z.; Xu, Q.; Lin, J.; Jiang, Y.; Wang, Y.; Jing, J.; et al. Elevated Gut Microbiota Metabolite Bile Acids Confer Protective Effects on Clinical Prognosis in Ischemic Stroke Patients. Front. Neurosci. 2024, 18, 1388748. [Google Scholar] [CrossRef]
- Liang, H.; Matei, N.; McBride, D.W.; Xu, Y.; Zhou, Z.; Tang, J.; Luo, B.; Zhang, J.H. TGR5 Activation Attenuates Neuroinflammation via Pellino3 Inhibition of Caspase-8/NLRP3 after Middle Cerebral Artery Occlusion in Rats. J. Neuroinflamm. 2021, 18, 40. [Google Scholar] [CrossRef]
- Kaur, N.; Singh, R.; Das, A.P.; Agarwal, S.M.; Dhingra, N.; Kaur, T. Identification of Bile Acid-Derived Chemical Chaperone(s) Targeting E46K-Mutated Alpha-Synuclein Protein to Treat Parkinson’s Disease: Molecular Modelling, Docking, ADME, and Simulation Studies. Appl. Biochem. Biotechnol. 2024, 196, 2086–2109. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Yan, J.; Huang, L.; Araujo, C.; Peng, J.; Gao, L.; Liu, S.; Tang, J.; Zuo, G.; Zhang, J.H. INT-777 Attenuates NLRP3-ASC Inflammasome-Mediated Neuroinflammation via TGR5/CAMP/PKA Signaling Pathway after Subarachnoid Hemorrhage in Rats. Brain. Behav. Immun. 2021, 91, 587–600. [Google Scholar] [CrossRef] [PubMed]
- Romero-Ramírez, L.; García-Rama, C.; Wu, S.; Mey, J. Bile Acids Attenuate PKM2 Pathway Activation in Proinflammatory Microglia. Sci. Rep. 2022, 12, 1459. [Google Scholar] [CrossRef] [PubMed]
- Palsson-Mcdermott, E.M.; Curtis, A.M.; Goel, G.; Lauterbach, M.A.R.; Sheedy, F.J.; Gleeson, L.E.; Van Den Bosch, M.W.M.; Quinn, S.R.; Domingo-Fernandez, R.; Johnson, D.G.W.; et al. Pyruvate Kinase M2 Regulates Hif-1α Activity and Il-1β Induction and Is a Critical Determinant of the Warburg Effect in LPS-Activated Macrophages. Cell Metab. 2015, 21, 65–80. [Google Scholar] [CrossRef]
- Xie, M.; Yu, Y.; Kang, R.; Zhu, S.; Yang, L.; Zeng, L.; Sun, X.; Yang, M.; Billiar, T.R.; Wang, H.; et al. PKM2-dependent glycolysis promotes NLRP3 and AIM2 inflammasome activation. Nat. Commun. 2016, 7, 13280. [Google Scholar] [CrossRef]
- Tsunawaki, S.; Spornt, M.; Ding, A.; Nathan, C. Deactivation of Macrophages by Transforming Growth Factor-β. Nature 1988, 334, 260–262. [Google Scholar] [CrossRef] [PubMed]
- Imai, K.; Takeshita, A.; Hanazawa, S. Transforming Growth Factor-β Inhibits Lipopolysaccharide-Stimulated Expression of Inflammatory Cytokines in Mouse Macrophages through Downregulation of Activation Protein 1 and CD14 Receptor Expression. Infect. Immun. 2000, 68, 2418–2423. [Google Scholar] [CrossRef]
- Launay, N.; Ruiz, M.; Grau, L.; Ortega, F.J.; Ilieva, E.V.; Martínez, J.J.; Galea, E.; Ferrer, I.; Knecht, E.; Pujol, A.; et al. Tauroursodeoxycholic Bile Acid Arrests Axonal Degeneration by Inhibiting the Unfolded Protein Response in X-Linked Adrenoleukodystrophy. Acta Neuropathol. 2017, 133, 283–301. [Google Scholar] [CrossRef]
- Uppala, J.K.; Gani, A.R.; Ramaiah, K.V.A. Chemical Chaperone, TUDCA Unlike PBA, Mitigates Protein Aggregation Efficiently and Resists ER and Non-ER Stress Induced HepG2 Cell Death. Sci. Rep. 2017, 7, 3831. [Google Scholar] [CrossRef]
- Ochiai, T.; Nagayama, T.; Matsui, K.; Amano, K.; Sano, T.; Wakabayashi, T.; Iwatsubo, T. Tauroursodeoxycholic Acid Attenuates Diet-Induced and Age-Related Peripheral Endoplasmic Reticulum Stress and Cerebral Amyloid Pathology in a Mouse Model of Alzheimer’s Disease. J. Prev. Alzheimers Dis. 2021, 8, 483–494. [Google Scholar] [CrossRef]
- Zhang, Z.; Chen, J.; Chen, F.; Yu, D.; Li, R.; Lv, C.; Wang, H.; Li, H.; Li, J.; Cai, Y. Tauroursodeoxycholic Acid Alleviates Secondary Injury in the Spinal Cord via Up-Regulation of CIBZ Gene. Cell Stress Chaperones 2018, 23, 551–560. [Google Scholar] [CrossRef]
- Van Der Harg, J.M.; Nölle, A.; Zwart, R.; Boerema, A.S.; Van Haastert, E.S.; Strijkstra, A.M.; Hoozemans, J.J.M.; Scheper, W. The Unfolded Protein Response Mediates Reversible Tau Phosphorylation Induced by Metabolic Stress. Cell Death Dis. 2014, 5, e1393. [Google Scholar] [CrossRef] [PubMed]
- Ramalho, R.M.; Borralho, P.M.; Castro, R.E.; Solá, S.; Steer, C.J.; Rodrigues, C.M.P. Tauroursodeoxycholic Acid Modulates P53-Mediated Apoptosis in Alzheimer’s Disease Mutant Neuroblastoma Cells. J. Neurochem. 2006, 98, 1610–1618. [Google Scholar] [CrossRef] [PubMed]
- Miao, L.; Dong, Y.; Zhou, F.-B.; Chang, Y.-L.; Suo, Z.-G.; Ding, H.-Q. Protective Effect of TUDCA after Spinal Cord Injury. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 1133–1141. [Google Scholar]
- Kusaczuk, M. Tauroursodeoxycholate—Bile Acid with Chaperoning Activity: Molecular and Cellular Effects and Therapeutic Perspectives. Cells 2019, 8, 1471. [Google Scholar] [CrossRef] [PubMed]
- Cortez, L.; Sim, V. The Therapeutic Potential of Chemical Chaperones in Protein Folding Diseases. Prion 2014, 8, 197–202. [Google Scholar] [CrossRef]
- Cortez, L.M.; Campeau, J.; Norman, G.; Kalayil, M.; Van der Merwe, J.; McKenzie, D.; Sim, V.L. Bile Acids Reduce Prion Conversion, Reduce Neuronal Loss, and Prolong Male Survival in Models of Prion Disease. J. Virol. 2015, 89, 7660–7672. [Google Scholar] [CrossRef]
- Norman, G.; Campeau, J.; Sima, V.L. High Dose and Delayed Treatment with Bile Acids Ineffective in RML Prion-Infected Mice. Antimicrob. Agents Chemother. 2018, 62, 1128. [Google Scholar] [CrossRef]
- Viana, R.J.S.; Nunes, A.F.; Castro, R.E.; Ramalho, R.M.; Meyerson, J.; Fossati, S.; Ghiso, J.; Rostagno, A.; Rodrigues, C.M.P. Tauroursodeoxycholic Acid Prevents E22Q Alzheimer’s Aβ Toxicity in Human Cerebral Endothelial Cells. Cell. Mol. Life Sci. 2009, 66, 1094–1104. [Google Scholar] [CrossRef]
- Zangerolamo, L.; Vettorazzi, J.F.; Rosa, L.R.O.; Carneiro, E.M.; Barbosa, H.C.L. The Bile Acid TUDCA and Neurodegenerative Disorders: An Overview. Life Sci. 2021, 272, 119252. [Google Scholar] [CrossRef]
- Ramalho, R.M.; Nunes, A.F.; Dias, R.B.; Amaral, J.D.; Lo, A.C.; D’Hooge, R.; Sebastião, A.M.; Rodrigues, C.M.P. Tauroursodeoxycholic Acid Suppresses Amyloid β-Induced Synaptic Toxicity in Vitro and in APP/PS1 Mice. Neurobiol. Aging 2013, 34, 551–561. [Google Scholar] [CrossRef] [PubMed]


| Enzyme | CNS | Neuron | Astroc. | Microg. | Oligod. | SC |
|---|---|---|---|---|---|---|
| CYP7A1 | low | –(42) | +(42) | +(42) | – | – |
| CYP7B1 | +(31–34) | +(31, 33) | +(31) | +(31) | +(29) | +(34) |
| CYP8B1 | – | – | – | – | – | – |
| CH25H | low | +(29) | – | +(36, 49) | – | +(29) |
| CYP271 | +(24, 31) | +(24, 31) | +(24, 31) | +(31) | +(24, 31) | +(29) |
| CYP391 | low | +(27, 29) | +(27, 29) | +(27, 29) | +(27, 29) | +(29) |
| CYP461 | +(22, 23) | +(22, 23) | +(24, 31) | +(25) | +(26) | +(29) |
| AKR1D1 | Low (41) | – | – | – | – | – |
| 3αHSD | +(38–40) | – | – | – | – | – |
| HSD3B7 | +(35–37) | +(29) | +(37) | +(36) | +(29) | +(29) |
| Condition | Bile Acid | Trial Number | St | Title | Ph |
|---|---|---|---|---|---|
| ALS | TUDCA | NCT00877604 | C | Efficacy and tolerability of TUDCA in ALS | 2 |
| “ | “ | NCT05753852 | R | BA supplementation in patients | 3 |
| “ | “ | NCT03800524 | A | Safety and efficacy of TUDCA as add-on treatment in patients affected by ALS | 3 |
| “ | TUDCA/phenyl butyrate | NCT04987671 | A | Pharmacokinetics and pharmacodynamics study of AMX0035 in patients with ALS | 1 + 2 |
| “ | “ | NCT03127514 | C | AMX0035 in patients with ALS | 2 |
| “ | “ | NCT03488524 | C | Open label extension of AMX0035 in ALS | 2 |
| “ | “ | NCT05286372 | M | An intermediate size expanded-access protocol of AMX0035 for ALS | M |
| “ | “ | NCT04516096 | C | A compassionate use protocol of AMX0035 for treatment of patients with ALS | 2 + 3 |
| “ | “ | NCT05021536 | A | Phase III trial of AMX0035 for ALS treatment | 3 |
| “ | “ | NCT05619783 | R | Extension study evaluating the safety and tolerability of AMX0035 | 3 |
| PD | UDCA | NCT02967250 | C | Brain bioenergetics in PD and response to repeated oral UDCA treatment | 1 |
| “ | “ | NCT03840005 | C | Trial of UDCA for PD: the “UP” study | 2 |
| HD | Ursodiol | NCT00514774 | U | Ursodiol in HD | 1 |
| AD | TUDCA/phenyl butyrate | NCT03533257 | C | Safety and biological activity of AMX0035 for the treatment of AD | 2 |
| MS | TUDCA | NCT03423121 | C | BA supplementation in patients with MS | 1 + 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero-Ramírez, L.; Mey, J. Emerging Roles of Bile Acids and TGR5 in the Central Nervous System: Molecular Functions and Therapeutic Implications. Int. J. Mol. Sci. 2024, 25, 9279. https://doi.org/10.3390/ijms25179279
Romero-Ramírez L, Mey J. Emerging Roles of Bile Acids and TGR5 in the Central Nervous System: Molecular Functions and Therapeutic Implications. International Journal of Molecular Sciences. 2024; 25(17):9279. https://doi.org/10.3390/ijms25179279
Chicago/Turabian StyleRomero-Ramírez, Lorenzo, and Jörg Mey. 2024. "Emerging Roles of Bile Acids and TGR5 in the Central Nervous System: Molecular Functions and Therapeutic Implications" International Journal of Molecular Sciences 25, no. 17: 9279. https://doi.org/10.3390/ijms25179279
APA StyleRomero-Ramírez, L., & Mey, J. (2024). Emerging Roles of Bile Acids and TGR5 in the Central Nervous System: Molecular Functions and Therapeutic Implications. International Journal of Molecular Sciences, 25(17), 9279. https://doi.org/10.3390/ijms25179279






