Influence of Anticoagulants and Heparin Contaminants on the Suitability of MMP-9 as a Blood-Derived Biomarker
Abstract
1. Introduction
2. Results
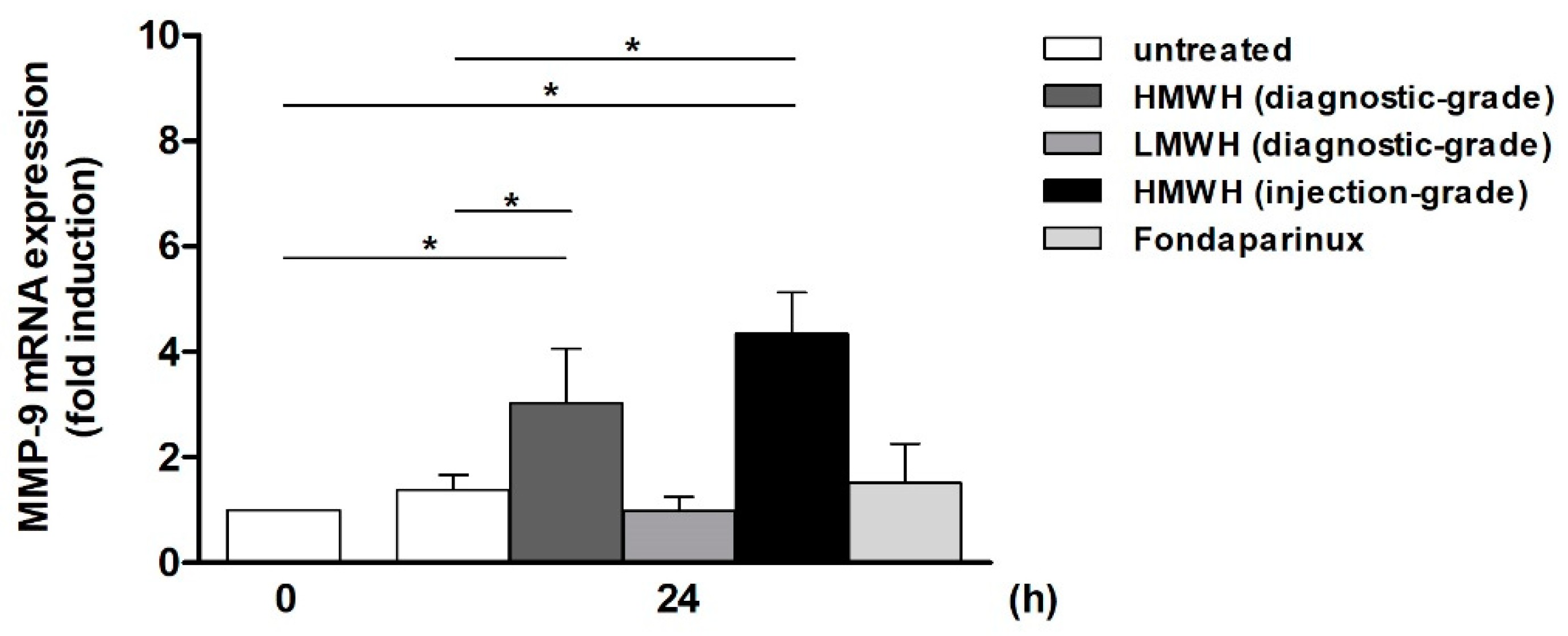
2.1. Supernatants of Anticoagulant-Treated Jurkat Cells Mediate Differential Effects on MMP-9 mRNA Expression in THP-1 Cells
2.1.1. Diagnostic-Grade High- and Low-Molecular-Weight Heparin and Fondaparinux
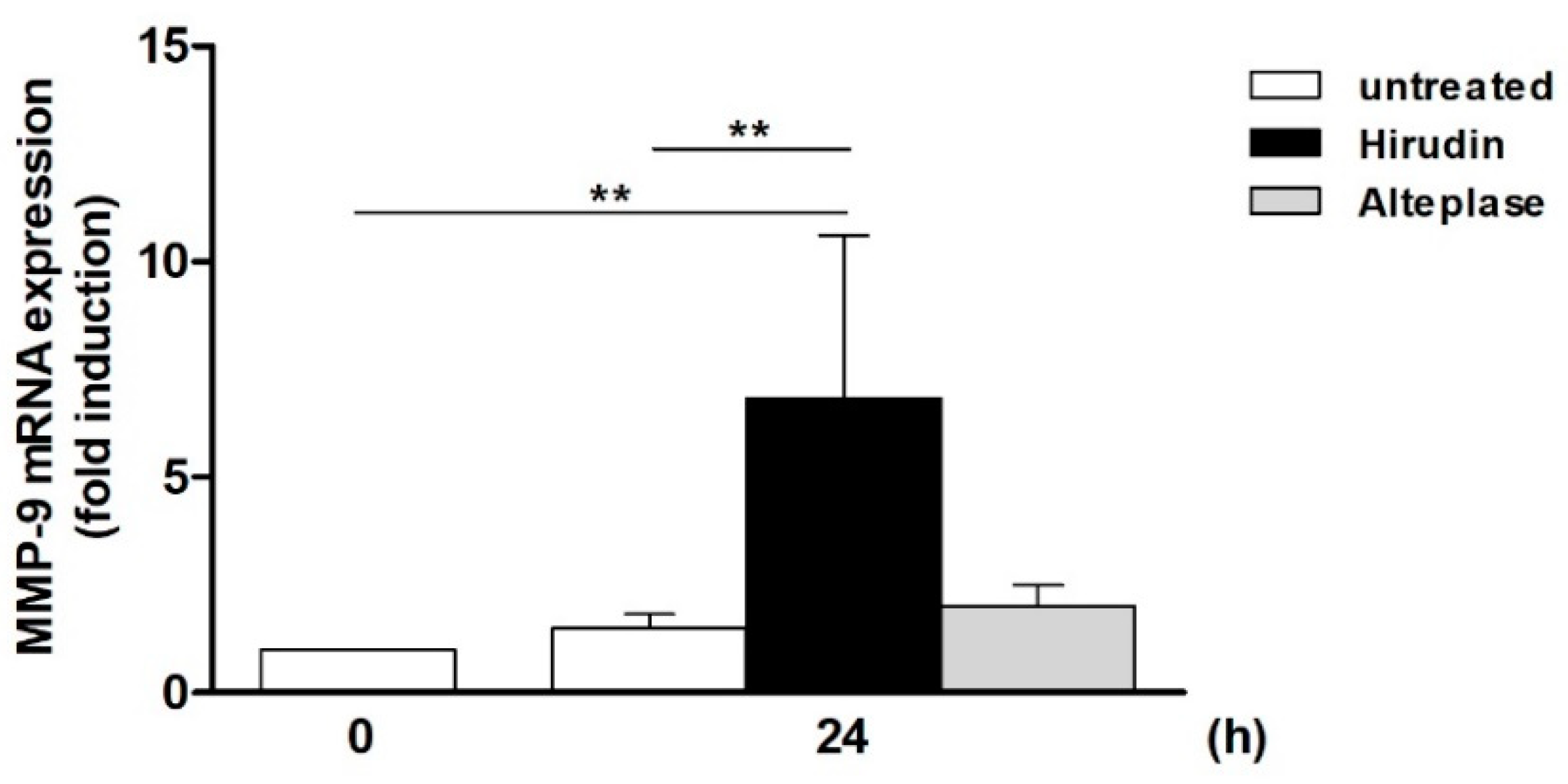
2.1.2. Hirudin and Alteplase
2.2. Supernatants of Heparin Contaminant-Treated Jurkat Cells Mediate Differential Effects on MMP-9 mRNA Expression in THP-1 Cells
2.2.1. Hyaluronic Acid, Dermatan Sulfate, and Chondroitin Sulfate
2.2.2. Over-Sulfated Chondroitin Sulfate
2.3. Characterization of Cytokine/Chemokine Patterns Expressed in Response to Anticoagulants and Contaminants
2.3.1. Anticoagulants: HMWH, LMWH, Hirudin, and Alteplase
2.3.2. Contaminants: HA, DS, CS, and OSCS
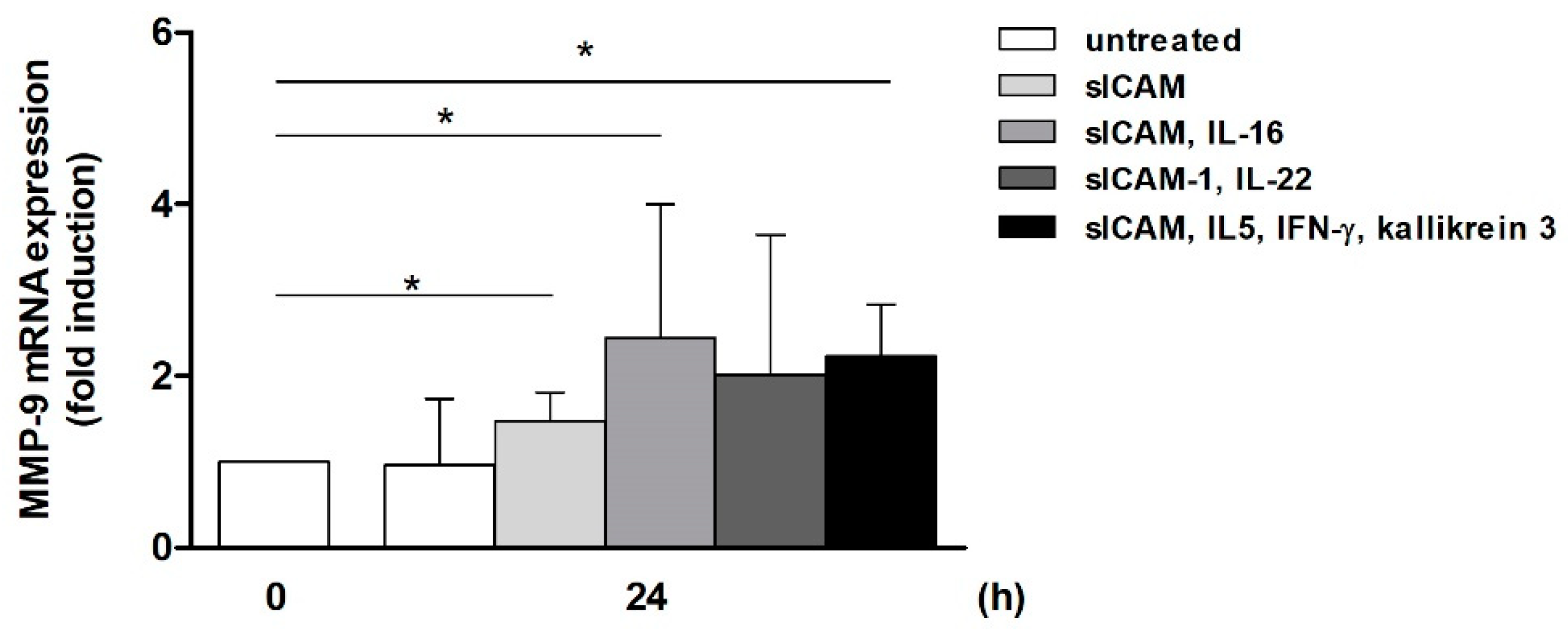
2.4. Induction of MMP-9 mRNA Expression in Monocytic THP-1 Cells by T-Cell-Derived Mediators
3. Discussion
3.1. Specific Anticoagulants Can Act as Inducers of MMP-9 mRNA Expression
3.2. Heparin Contaminants Can Intensify Anticoagulant-Induced MMP-9 Expression
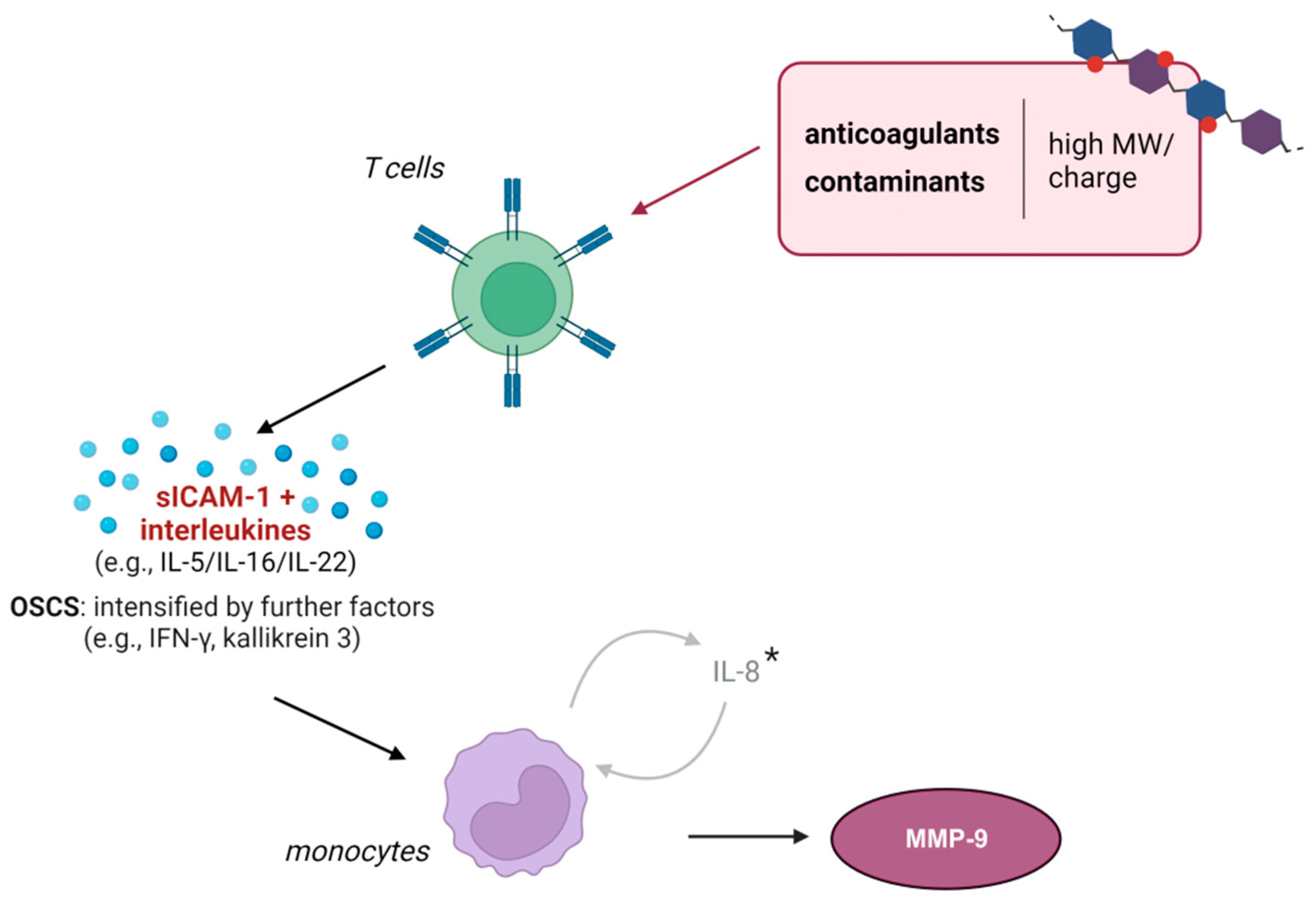
3.3. Soluble Mediators Link T Cell Activation with Monocytic MMP-9 Expression
3.4. Summary
4. Materials and Methods
4.1. Cell Lines and Cell Culture Conditions
4.2. Reagents
4.3. Cell Culture Experiments
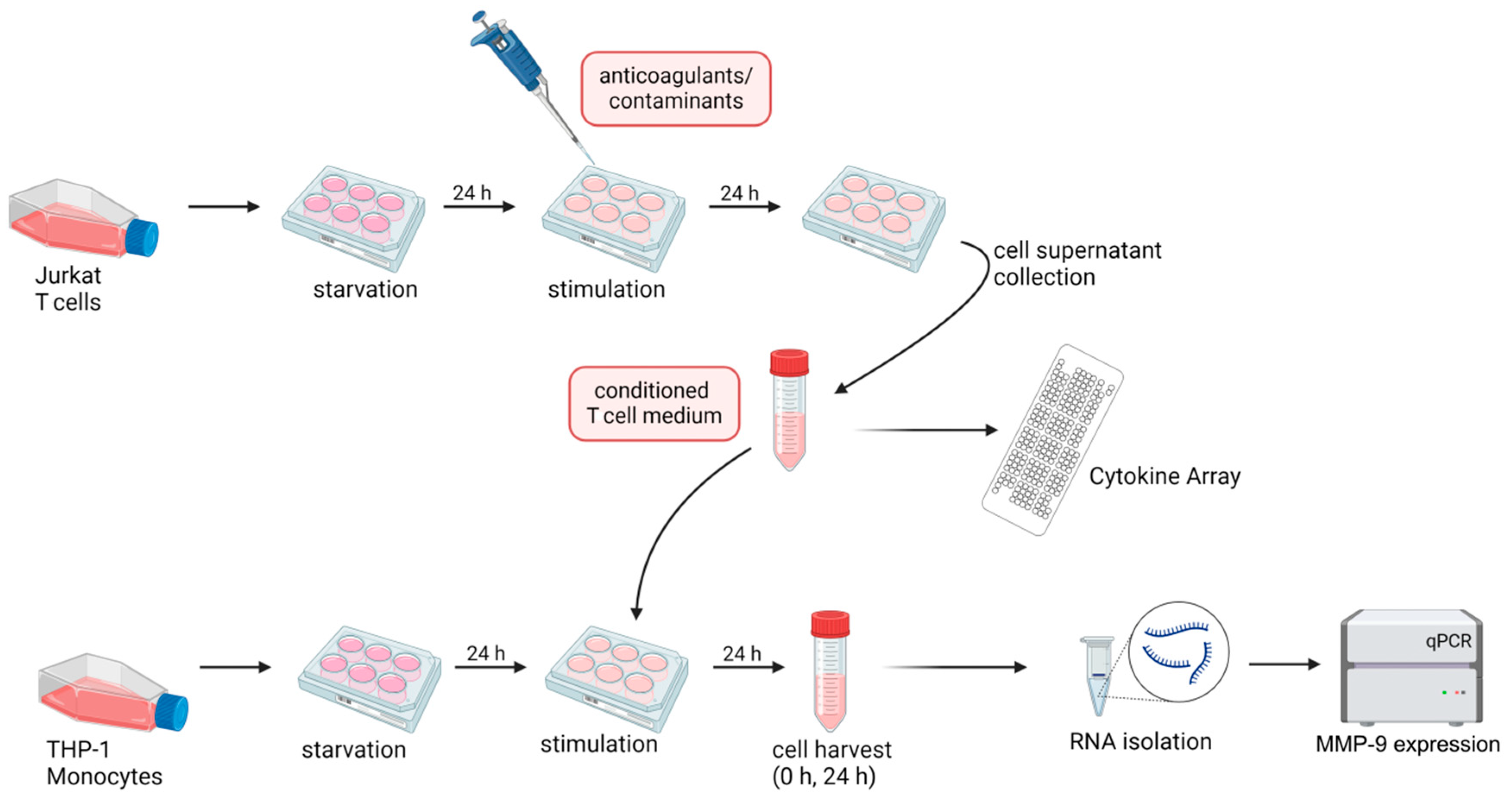
4.3.1. Supernatant Transfer Experiments
4.3.2. Cytokine Stimulation Experiments
4.4. RNA Extraction, cDNA Synthesis, and Quantitative (q)PCR
4.5. Proteome Profiler Array
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Onishi, A.; St Ange, K.; Dordick, J.S.; Linhardt, R.J. Heparin and anticoagulation. Front. Biosci. 2016, 21, 1372–1392. [Google Scholar]
- Mendes, A.; Meneghetti, M.C.Z.; Palladino, M.V.; Justo, G.Z.; Sassaki, G.L.; Fareed, J.; Lima, M.A.; Nader, H.B. Crude Heparin Preparations Unveil the Presence of Structurally Diverse Oversulfated Contaminants. Molecules 2019, 24, 2988. [Google Scholar] [CrossRef]
- Oduah, E.I.; Linhardt, R.J.; Sharfstein, S.T. Heparin: Past, Present, and Future. Pharmaceuticals 2016, 9, 38. [Google Scholar] [CrossRef]
- McKee, J.; Bairstow, S.; Szabo, C.; Ray, J.; Wielgos, T.; Hu, P.; Chess, E.; Nordhaus, M.; Hai, T.; Campbell, J.; et al. Structure elucidation and biological activity of the oversulfated chondroitin sulfate contaminant in Baxter heparin. J. Clin. Pharmacol. 2010, 50, 1159–1170. [Google Scholar] [CrossRef]
- Arepally, G.M. Heparin-induced thrombocytopenia. Blood 2017, 129, 2864–2872. [Google Scholar] [CrossRef]
- Radziwon-Balicka, A.; Wiwe, E.F.; Jensen, T.O.; Nielsen, S.G.; Copois, M.; Sunde, N.; Peytz, N.C.; Al-Mousawi, D.A.A.; Hansen, M.C.; Petersen, J.F.; et al. Evaluation of a novel heparin-iloprost-based antithrombotic formulation blood collection tube for clinical usage. Clin. Chim. Acta 2022, 537, 87–95. [Google Scholar] [CrossRef]
- Gray, E.; Mulloy, B.; Barrowcliffe, T.W. Heparin and low-molecular-weight heparin. Thromb. Haemost. 2008, 99, 807–818. [Google Scholar]
- Hogwood, J.; Gray, E.; Mulloy, B. Heparin, Heparan Sulphate and Sepsis: Potential New Options for Treatment. Pharmaceuticals 2023, 16, 271. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, Z.; Linhardt, R.J. Lessons learned from the contamination of heparin. Nat. Prod. Rep. 2009, 26, 313–321. [Google Scholar] [CrossRef]
- European Pharmacopoeia, 10th ed.; Deutscher Apotheker Verlag: Stuttgart, Germany, 2020.
- United States Pharmacopeia, USP 44—NF 39; United States Pharmacopeia: North Bethesda, MD, USA, 2021.
- Guerrini, M.; Beccati, D.; Shriver, Z.; Naggi, A.; Viswanathan, K.; Bisio, A.; Capila, I.; Lansing, J.C.; Guglieri, S.; Fraser, B.; et al. Oversulfated chondroitin sulfate is a contaminant in heparin associated with adverse clinical events. Nat. Biotechnol. 2008, 26, 669–675. [Google Scholar] [CrossRef]
- Hermann, K.; Frank, G.; Ring, J. Contamination of heparin by histamine: Measurement and characterization by high-performance liquid chromatography and radioimmunoassay. Allergy 1994, 49, 569–572. [Google Scholar] [CrossRef]
- Casu, B.; Naggi, A.; Oreste, P.; Torri, G.; Pangrazzj, J.; Maggi, A.; Abbadini, M.; Donati, M.B. Bleeding associated with heparin contaminants. Lancet 1987, 1, 1088. [Google Scholar] [CrossRef]
- Pan, J.; Qian, Y.; Zhou, X.; Pazandak, A.; Frazier, S.B.; Weiser, P.; Lu, H.; Zhang, L. Oversulfated chondroitin sulfate is not the sole contaminant in heparin. Nat. Biotechnol. 2010, 28, 203–207, author reply 207–211. [Google Scholar] [CrossRef]
- Beyer, T.; Matz, M.; Brinz, D.; Radler, O.; Wolf, B.; Norwig, J.; Baumann, K.; Alban, S.; Holzgrabe, U. Composition of OSCS-contaminated heparin occurring in 2008 in batches on the German market. Eur. J. Pharm. Sci. 2010, 40, 297–304. [Google Scholar] [CrossRef]
- Sapojnikova, N.; Kartvelishvili, T.; Asatiani, N.; Zinkevich, V.; Kalandadze, I.; Gugutsidze, D.; Shakarishvili, R.; Tsiskaridze, A. Correlation between MMP-9 and extracellular cytokine HMGB1 in prediction of human ischemic stroke outcome. Biochim. Biophys. Acta 2014, 1842, 1379–1384. [Google Scholar] [CrossRef]
- Huang, H. Matrix Metalloproteinase-9 (MMP-9) as a Cancer Biomarker and MMP-9 Biosensors: Recent Advances. Sensors 2018, 18, 3249. [Google Scholar] [CrossRef]
- Rababah, M.; Worthmann, H.; Deb, M.; Tryc, A.B.; Ma, Y.T.; El Bendary, O.M.; Hecker, H.; Goldbecker, A.; Heeren, M.; Brand, K.; et al. Anticoagulants affect matrix metalloproteinase 9 levels in blood samples of stroke patients and healthy controls. Clin. Biochem. 2012, 45, 483–489. [Google Scholar] [CrossRef]
- Huber, R.; Attili/Abedalkhader, R.; Kuper, D.; Hauke, L.; Luns, B.; Brand, K.; Weissenborn, K.; Lichtinghagen, R. Cellular and Molecular Effects of High-Molecular-Weight Heparin on Matrix Metalloproteinase 9 Expression. Int. J. Mol. Sci. 2019, 20, 1595. [Google Scholar] [CrossRef]
- Gerlach, R.F.; Demacq, C.; Jung, K.; Tanus-Santos, J.E. Rapid separation of serum does not avoid artificially higher matrix metalloproteinase (MMP)-9 levels in serum versus plasma. Clin. Biochem. 2007, 40, 119–123. [Google Scholar] [CrossRef]
- Mannello, F.; Jung, K.; Tonti, G.A.; Canestrari, F. Heparin affects matrix metalloproteinases and tissue inhibitors of metalloproteinases circulating in peripheral blood. Clin. Biochem. 2008, 41, 1466–1473. [Google Scholar] [CrossRef]
- White, R.H.; Daschbach, M.M.; McGahan, J.P.; Keck, K.; Parsons, G.H.; Hartling, R.P.; Mungall, D. Treatment of proximal deep-vein thrombosis using subcutaneously administered calcium heparin: Comparison with intravenous sodium heparin. Haemostasis 1992, 22, 129–137. [Google Scholar] [CrossRef]
- Walenga, J.M.; Jeske, W.P.; Samama, M.M.; Frapaise, F.X.; Bick, R.L.; Fareed, J. Fondaparinux: A synthetic heparin pentasaccharide as a new antithrombotic agent. Expert Opin. Investig. Drugs 2002, 11, 397–407. [Google Scholar] [CrossRef]
- Hu, J.; Van den Steen, P.E.; Sang, Q.X.; Opdenakker, G. Matrix metalloproteinase inhibitors as therapy for inflammatory and vascular diseases. Nat. Rev. Drug Discov. 2007, 6, 480–498. [Google Scholar] [CrossRef]
- Wollbold, J.; Huber, R.; Pohlers, D.; Koczan, D.; Guthke, R.; Kinne, R.W.; Gausmann, U. Adapted Boolean network models for extracellular matrix formation. BMC Syst. Biol. 2009, 3, 77. [Google Scholar] [CrossRef]
- Wang, X.; Khalil, R.A. Matrix Metalloproteinases, Vascular Remodeling, and Vascular Disease. Adv. Pharmacol. 2018, 81, 241–330. [Google Scholar]
- Lindsey, M.L. Assigning matrix metalloproteinase roles in ischaemic cardiac remodelling. Nat. Rev. Cardiol. 2018, 15, 471–479. [Google Scholar] [CrossRef]
- Bar-Or, A.; Nuttall, R.K.; Duddy, M.; Alter, A.; Kim, H.J.; Ifergan, I.; Pennington, C.J.; Bourgoin, P.; Edwards, D.R.; Yong, V.W. Analyses of all matrix metalloproteinase members in leukocytes emphasize monocytes as major inflammatory mediators in multiple sclerosis. Brain 2003, 126, 2738–2749. [Google Scholar] [CrossRef]
- Olejarz, W.; Lacheta, D.; Kubiak-Tomaszewska, G. Matrix Metalloproteinases as Biomarkers of Atherosclerotic Plaque Instability. Int. J. Mol. Sci. 2020, 21, 3946. [Google Scholar] [CrossRef]
- Nikolov, A.; Popovski, N. Role of Gelatinases MMP-2 and MMP-9 in Healthy and Complicated Pregnancy and Their Future Potential as Preeclampsia Biomarkers. Diagnostics 2021, 11, 480. [Google Scholar] [CrossRef]
- Liu, J.; Linhardt, R.J. Chemoenzymatic synthesis of heparan sulfate and heparin. Nat. Prod. Rep. 2014, 31, 1676–1685. [Google Scholar] [CrossRef]
- Crowther, M.; Lim, W. Low molecular weight heparin and bleeding in patients with chronic renal failure. Curr. Opin. Pulm. Med. 2007, 13, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Haverstick, D.M.; Brill, L.B., II; Scott, M.G.; Bruns, D.E. Preanalytical variables in measurement of free (ionized) calcium in lithium heparin-containing blood collection tubes. Clin. Chim. Acta 2009, 403, 102–104. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.; Cho, H.W.; Rim, J.H.; Hahn, S.M.; Han, J.W.; Lee, S.G.; Lyu, C.J.; Lim, J.B. Comparison of blood collection tubes for 29 biochemical analytes in pediatric patients with central venous catheters. Clin. Biochem. 2022, 107, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Lan, H.; Du, W.; Mo, Z.; Huang, H. The Influence of Blood Collection Tubes on Measurement of Cardiac Biomarkers. Clin. Lab. 2016, 62, 705–709. [Google Scholar] [CrossRef]
- Turpie, A.G.; Eriksson, B.I.; Bauer, K.A.; Lassen, M.R. Fondaparinux. J. Am. Acad. Orthop. Surg. 2004, 12, 371–375. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, M.; Tan, L.; Pan, N.; Zhang, L. The clinical use of Fondaparinux: A synthetic heparin pentasaccharide. Prog. Mol. Biol. Transl. Sci. 2019, 163, 41–53. [Google Scholar]
- Tan, E.; Thompson, G.; Ekstrom, C.; Lucas, M. Non-immediate heparin and heparinoid cutaneous allergic reactions: A role for fondaparinux. Intern. Med. J. 2018, 48, 73–77. [Google Scholar] [CrossRef]
- Bundhun, P.K.; Shaik, M.; Yuan, J. Choosing between Enoxaparin and Fondaparinux for the management of patients with acute coronary syndrome: A systematic review and meta-analysis. BMC Cardiovasc. Disord. 2017, 17, 116. [Google Scholar] [CrossRef]
- Nowak, G. Pharmacology of recombinant hirudin. Semin. Thromb. Hemost. 2002, 28, 415–424. [Google Scholar] [CrossRef]
- Junren, C.; Xiaofang, X.; Huiqiong, Z.; Gangmin, L.; Yanpeng, Y.; Xiaoyu, C.; Yuqing, G.; Yanan, L.; Yue, Z.; Fu, P.; et al. Pharmacological Activities and Mechanisms of Hirudin and Its Derivatives—A Review. Front. Pharmacol. 2021, 12, 660757. [Google Scholar] [CrossRef]
- Menssen, H.D.; Melber, K.; Brandt, N.; Thiel, E. The use of hirudin as universal anticoagulant in haematology, clinical chemistry and blood grouping. Clin. Chem. Lab. Med. 2001, 39, 1267–1277. [Google Scholar] [CrossRef] [PubMed]
- Lima-Oliveira, G.; Brennan-Bourdon, L.M.; Varela, B.; Arredondo, M.E.; Aranda, E.; Flores, S.; Ochoa, P. Clot activators and anticoagulant additives for blood collection. A critical review on behalf of COLABIOCLI WG-PRE-LATAM. Crit. Rev. Clin. Lab. Sci. 2021, 58, 207–224. [Google Scholar] [CrossRef] [PubMed]
- Collen, D.; Lijnen, H.R. The tissue-type plasminogen activator story. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 1151–1155. [Google Scholar] [CrossRef]
- Demaerschalk, B.M.; Kleindorfer, D.O.; Adeoye, O.M.; Demchuk, A.M.; Fugate, J.E.; Grotta, J.C.; Khalessi, A.A.; Levy, E.I.; Palesch, Y.Y.; Prabhakaran, S.; et al. Scientific Rationale for the Inclusion and Exclusion Criteria for Intravenous Alteplase in Acute Ischemic Stroke: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2016, 47, 581–641. [Google Scholar] [CrossRef]
- Brandt, K.; McGinn, K.; Quedado, J. Low-Dose Systemic Alteplase (tPA) for the Treatment of Pulmonary Embolism. Ann. Pharmacother. 2015, 49, 818–824. [Google Scholar] [CrossRef]
- Dhillon, S. Alteplase: A review of its use in the management of acute ischaemic stroke. CNS Drugs 2012, 26, 899–926. [Google Scholar] [CrossRef]
- Szajek, A.Y.; Chess, E.; Johansen, K.; Gratzl, G.; Gray, E.; Keire, D.; Linhardt, R.J.; Liu, J.; Morris, T.; Mulloy, B.; et al. The US regulatory and pharmacopeia response to the global heparin contamination crisis. Nat. Biotechnol. 2016, 34, 625–630. [Google Scholar] [CrossRef]
- Marinho, A.; Nunes, C.; Reis, S. Hyaluronic Acid: A Key Ingredient in the Therapy of Inflammation. Biomolecules 2021, 11, 1518. [Google Scholar] [CrossRef] [PubMed]
- Fallacara, A.; Baldini, E.; Manfredini, S.; Vertuani, S. Hyaluronic Acid in the Third Millennium. Polymers 2018, 10, 701. [Google Scholar] [CrossRef]
- Martel-Pelletier, J.; Farran, A.; Montell, E.; Verges, J.; Pelletier, J.P. Discrepancies in composition and biological effects of different formulations of chondroitin sulfate. Molecules 2015, 20, 4277–4289. [Google Scholar] [CrossRef]
- Fonseca, R.J.; Oliveira, S.N.; Pomin, V.H.; Mecawi, A.S.; Araujo, I.G.; Mourao, P.A. Effects of oversulfated and fucosylated chondroitin sulfates on coagulation. Challenges for the study of anticoagulant polysaccharides. Thromb. Haemost. 2010, 103, 994–1004. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Shi, L.; Qin, Y.; Li, F. Research and Application of Chondroitin Sulfate/Dermatan Sulfate-Degrading Enzymes. Front. Cell Dev. Biol. 2020, 8, 560442. [Google Scholar] [CrossRef] [PubMed]
- Liaw, P.C.; Austin, R.C.; Fredenburgh, J.C.; Stafford, A.R.; Weitz, J.I. Comparison of heparin- and dermatan sulfate-mediated catalysis of thrombin inactivation by heparin cofactor II. J. Biol. Chem. 1999, 274, 27597–27604. [Google Scholar] [CrossRef] [PubMed]
- Volpi, N. Chondroitin Sulfate Safety and Quality. Molecules 2019, 24, 1447. [Google Scholar] [CrossRef] [PubMed]
- Malmstrom, A.; Bartolini, B.; Thelin, M.A.; Pacheco, B.; Maccarana, M. Iduronic acid in chondroitin/dermatan sulfate: Biosynthesis and biological function. J. Histochem. Cytochem. 2012, 60, 916–925. [Google Scholar] [CrossRef]
- Liverani, L.; Mascellani, G.; Spelta, F. Heparins: Process-related physico-chemical and compositional characteristics, fingerprints and impurities. Thromb. Haemost. 2009, 102, 846–853. [Google Scholar]
- Gray, A.; Litinas, E.; Jeske, W.; Fareed, J.; Hoppensteadt, D. Interactions of oversulfated chondroitin sulfate (OSCS) from different sources with unfractionated heparin. Clin. Appl. Thromb. Hemost. 2012, 18, 166–173. [Google Scholar] [CrossRef]
- Pan, J.; Qian, Y.; Zhou, X.; Lu, H.; Ramacciotti, E.; Zhang, L. Chemically oversulfated glycosaminoglycans are potent modulators of contact system activation and different cell signaling pathways. J. Biol. Chem. 2010, 285, 22966–22975. [Google Scholar] [CrossRef]
- Li, B.; Suwan, J.; Martin, J.G.; Zhang, F.; Zhang, Z.; Hoppensteadt, D.; Clark, M.; Fareed, J.; Linhardt, R.J. Oversulfated chondroitin sulfate interaction with heparin-binding proteins: New insights into adverse reactions from contaminated heparins. Biochem. Pharmacol. 2009, 78, 292–300. [Google Scholar] [CrossRef]
- Hogwood, J.; Naggi, A.; Torri, G.; Page, C.; Rigsby, P.; Mulloy, B.; Gray, E. The effect of increasing the sulfation level of chondroitin sulfate on anticoagulant specific activity and activation of the kinin system. PLoS ONE 2018, 13, e0193482. [Google Scholar] [CrossRef]
- Carranza, Y.E.; Durand-Rougley, C.; Doctor, V. Effect of oversulfation on the chemical and biological properties of chondroitin-4-sulfate. Blood Coagul. Fibrinolysis. 2008, 19, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Fareed, J.; Walenga, J.M.; Jeske, W.P.; Hoppensteadt, D.; Prechel, M.; Iqbal, O.; Adiguzel, C.; Clark, M.; Litinas, E.; Cunanan, J.; et al. Biological Profile of the Hyper/Oversulfated Chondroitin Sulfate Contaminant Isolated from Recalled Heparin. Semin. Thromb. Hemost. 2008, 34, 119–127. [Google Scholar] [CrossRef][Green Version]
- Wang, S.; Sugahara, K.; Li, F. Chondroitin sulfate/dermatan sulfate sulfatases from mammals and bacteria. Glycoconj. J. 2016, 33, 841–851. [Google Scholar] [CrossRef] [PubMed]
- Greinacher, A.; Michels, I.; Schafer, M.; Kiefel, V.; Mueller-Eckhardt, C. Heparin-associated thrombocytopenia in a patient treated with polysulphated chondroitin sulphate: Evidence for immunological crossreactivity between heparin and polysulphated glycosaminoglycan. Br. J. Haematol. 1992, 81, 252–254. [Google Scholar] [CrossRef]
- Warkentin, T.E.; Greinacher, A. Heparin-induced anaphylactic and anaphylactoid reactions: Two distinct but overlapping syndromes. Expert Opin. Drug Saf. 2009, 8, 129–144. [Google Scholar] [CrossRef] [PubMed]
- Trojano, M.; Avolio, C.; Liuzzi, G.M.; Ruggieri, M.; Defazio, G.; Liguori, M.; Santacroce, M.P.; Paolicelli, D.; Giuliani, F.; Riccio, P.; et al. Changes of serum sICAM-1 and MMP-9 induced by rIFNbeta-1b treatment in relapsing-remitting MS. Neurology 1999, 53, 1402–1408. [Google Scholar] [CrossRef]
- Ji, Y.; Yang, X.; Li, J.; Lu, Z.; Li, X.; Yu, J.; Li, N. IL-22 promotes the migration and invasion of gastric cancer cells via IL-22R1/AKT/MMP-9 signaling. Int. J. Clin. Exp. Pathol. 2014, 7, 3694–3703. [Google Scholar]
- Kim, E.Y.; Choi, B.; Kim, J.E.; Park, S.O.; Kim, S.M.; Chang, E.J. Interleukin-22 Mediates the Chemotactic Migration of Breast Cancer Cells and Macrophage Infiltration of the Bone Microenvironment by Potentiating S1P/SIPR Signaling. Cells 2020, 9, 131. [Google Scholar] [CrossRef]
- Whittington, H.A.; Armstrong, L.; Uppington, K.M.; Millar, A.B. Interleukin-22: A potential immunomodulatory molecule in the lung. Am. J. Respir. Cell Mol. Biol. 2004, 31, 220–226. [Google Scholar] [CrossRef]
- Van den Steen, P.E.; Dubois, B.; Nelissen, I.; Rudd, P.M.; Dwek, R.A.; Opdenakker, G. Biochemistry and molecular biology of gelatinase B or matrix metalloproteinase-9 (MMP-9). Crit. Rev. Biochem. Mol. Biol. 2002, 37, 375–536. [Google Scholar] [CrossRef]
- Prassas, I.; Eissa, A.; Poda, G.; Diamandis, E.P. Unleashing the therapeutic potential of human kallikrein-related serine proteases. Nat. Rev. Drug. Discov. 2015, 14, 183–202. [Google Scholar] [CrossRef] [PubMed]
- de Souza, L.R.; Melo, P.M.; Paschoalin, T.; Carmona, A.K.; Kondo, M.; Hirata, I.Y.; Blaber, M.; Tersariol, I.; Takatsuka, J.; Juliano, M.A.; et al. Human tissue kallikreins 3 and 5 can act as plasminogen activator releasing active plasmin. Biochem. Biophys. Res. Commun. 2013, 433, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Sartorius, H.; Moench, A.; Fellmer, K.E. Effect of heparin on the course of experimental nephritis-nephrosis. Z. Gesamte Exp. Med. 1955, 125, 572–586. [Google Scholar] [CrossRef] [PubMed]
- Frömke, J. Einsatz und Wirkung von Medikamenten. In Standardoperationen in der Gefäßchirurgie; Steinkopff Verlag: Darmstadt, Germany, 2006; pp. 47–61. [Google Scholar]
- Huber, R.; Kunisch, E.; Gluck, B.; Egerer, R.; Sickinger, S.; Kinne, R.W. Comparison of conventional and real-time RT-PCR for the quantitation of jun protooncogene mRNA and analysis of junB mRNA expression in synovial membranes and isolated synovial fibroblasts from rheumatoid arthritis patients. Z. Rheumatol. 2003, 62, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Gunther, J.; Vogt, N.; Hampel, K.; Bikker, R.; Page, S.; Muller, B.; Kandemir, J.; Kracht, M.; Dittrich-Breiholz, O.; Huber, R.; et al. Identification of two forms of TNF tolerance in human monocytes: Differential inhibition of NF-kappaB/AP-1- and PP1-associated signaling. J. Immunol. 2014, 192, 3143–3155. [Google Scholar] [CrossRef] [PubMed]
- Schwettmann, L.; Wehmeier, M.; Jokovic, D.; Aleksandrova, K.; Brand, K.; Manns, M.P.; Lichtinghagen, R.; Bahr, M.J. Hepatic expression of A disintegrin and metalloproteinase (ADAM) and ADAMs with thrombospondin motives (ADAM-TS) enzymes in patients with chronic liver diseases. J. Hepatol. 2008, 49, 243–250. [Google Scholar] [CrossRef]
- Gutsch, R.; Kandemir, J.D.; Pietsch, D.; Cappello, C.; Meyer, J.; Simanowski, K.; Huber, R.; Brand, K. CCAAT/enhancer-binding protein beta inhibits proliferation in monocytic cells by affecting the retinoblastoma protein/E2F/cyclin E pathway but is not directly required for macrophage morphology. J. Biol. Chem. 2011, 286, 22716–22729. [Google Scholar] [CrossRef]

| Anticoagulant | Secreted Mediators |
|---|---|
| HMWH (injection-grade) | sICAM-1, IL-16 |
| LMWH (injection-grade) | - |
| HMWH (diagnostic-grade) | sICAM-1, IL-22 |
| LMWH (diagnostic-grade) | - |
| Fondaparinux | - |
| Hirudin | diverse factors 1 |
| Alteplase | - |
| Contaminant | Secreted Mediators |
|---|---|
| HA (100 µg) | - |
| HA (200 µg) | - |
| DS | sICAM-1 |
| CS | sICAM-1 |
| OSCS | sICAM-1, IL-5, IFN-γ, kallikrein 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Küper, D.; Klos, J.; Kühl, F.; Attili, R.; Brand, K.; Weissenborn, K.; Lichtinghagen, R.; Huber, R. Influence of Anticoagulants and Heparin Contaminants on the Suitability of MMP-9 as a Blood-Derived Biomarker. Int. J. Mol. Sci. 2024, 25, 10106. https://doi.org/10.3390/ijms251810106
Küper D, Klos J, Kühl F, Attili R, Brand K, Weissenborn K, Lichtinghagen R, Huber R. Influence of Anticoagulants and Heparin Contaminants on the Suitability of MMP-9 as a Blood-Derived Biomarker. International Journal of Molecular Sciences. 2024; 25(18):10106. https://doi.org/10.3390/ijms251810106
Chicago/Turabian StyleKüper, Daniela, Josefin Klos, Friederike Kühl, Rozan Attili, Korbinian Brand, Karin Weissenborn, Ralf Lichtinghagen, and René Huber. 2024. "Influence of Anticoagulants and Heparin Contaminants on the Suitability of MMP-9 as a Blood-Derived Biomarker" International Journal of Molecular Sciences 25, no. 18: 10106. https://doi.org/10.3390/ijms251810106
APA StyleKüper, D., Klos, J., Kühl, F., Attili, R., Brand, K., Weissenborn, K., Lichtinghagen, R., & Huber, R. (2024). Influence of Anticoagulants and Heparin Contaminants on the Suitability of MMP-9 as a Blood-Derived Biomarker. International Journal of Molecular Sciences, 25(18), 10106. https://doi.org/10.3390/ijms251810106







