Irisin Protects Musculoskeletal Homeostasis via a Mitochondrial Quality Control Mechanism
Abstract
:1. Introduction
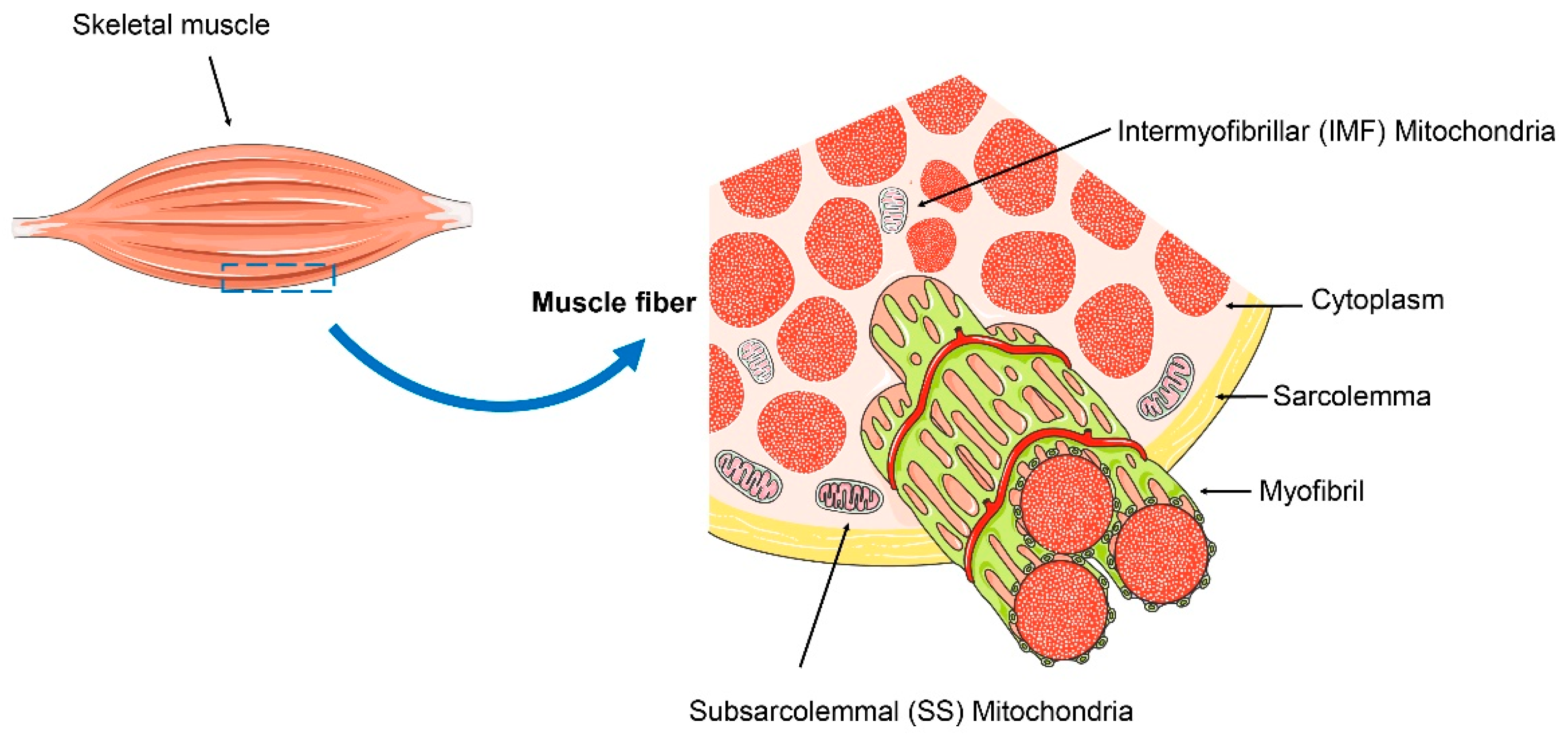
2. Mitochondrial Quality Control in Skeletal Muscle Stability
3. Myokine Irisin’s Role for Musculoskeletal Disorders
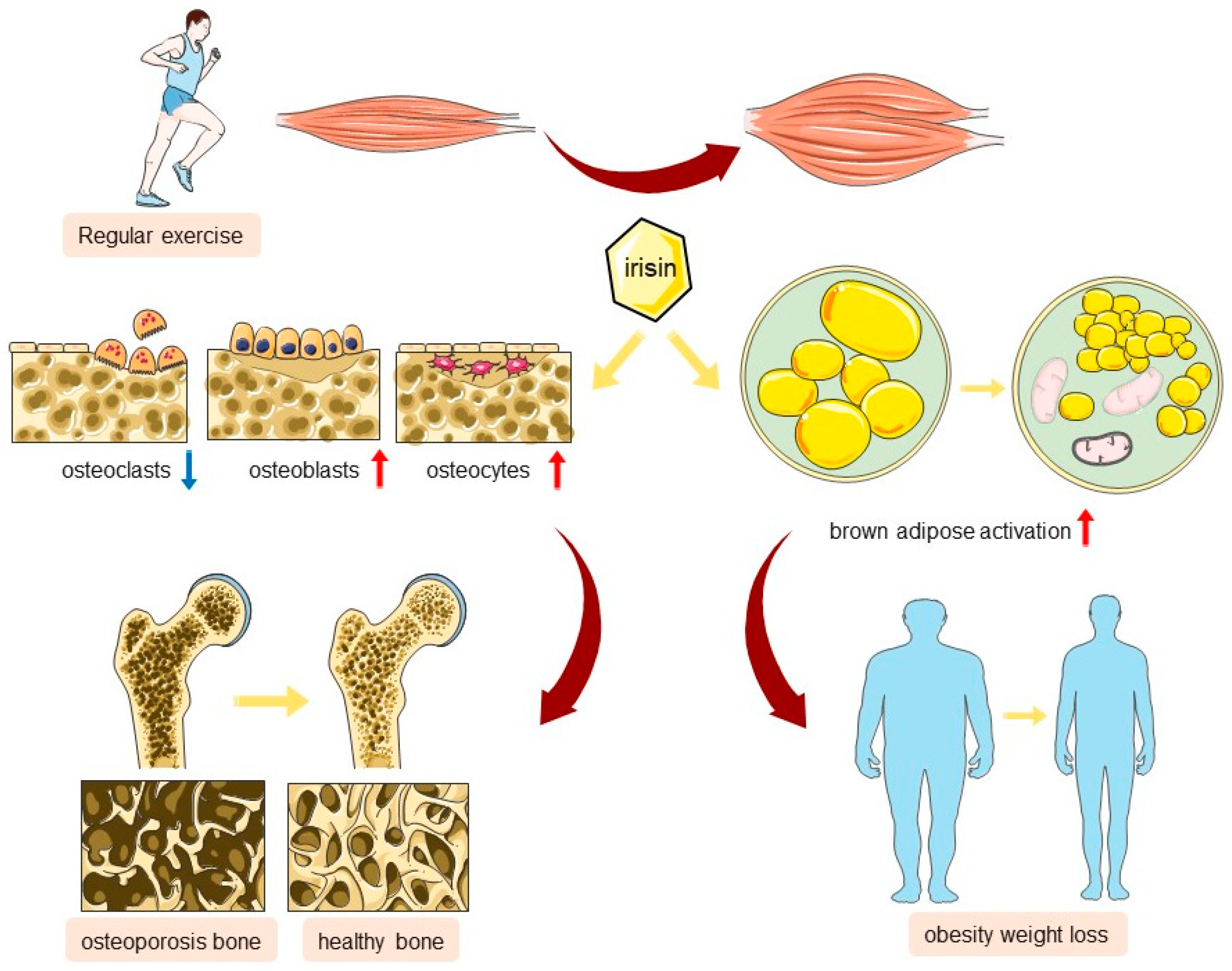
3.1. Secretion and Regulation of Irisin
3.2. Irisin: Sustaining Mitochondrial Homeostasis for Enhanced Musculoskeletal Wellness
3.2.1. The Role of Irisin in Bone/Cartilage Metabolism
3.2.2. The Role of Irisin in Brown Adipose Activation
3.2.3. The Role of Irisin in Myogenesis
3.3. Irisin Plays a Role in Maintaining Mitochondrial Homeostasis in Musculoskeletal Diseases
Mitochondrial Dysfunction in Adolescent Idiopathic Scoliosis
4. Debates on Irisin’s Role and Measurement in Humans
5. Summary and Prospects
Author Contributions
Funding
Conflicts of Interest
References
- Jiao, H.; Jiang, D.; Hu, X.; Du, W.; Ji, L.; Yang, Y.; Li, X.; Sho, T.; Wang, X.; Li, Y.; et al. Mitocytosis, a migrasome-mediated mitochondrial quality-control process. Cell 2021, 184, 2896–2910.e13. [Google Scholar] [CrossRef] [PubMed]
- Eldeeb, M.A.; Thomas, R.A.; Ragheb, M.A.; Fallahi, A.; Fon, E.A. Mitochondrial quality control in health and in Parkinson’s disease. Physiol. Rev. 2022, 102, 1721–1755. [Google Scholar] [CrossRef] [PubMed]
- An, H.; Zhou, B.; Ji, X. Mitochondrial quality control in acute ischemic stroke. J. Cereb. Blood Flow Metab. 2021, 41, 3157–3170. [Google Scholar] [CrossRef]
- Liu, D.; Gao, Y.; Liu, J.; Huang, Y.; Yin, J.; Feng, Y.; Shi, L.; Meloni, B.P.; Zhang, C.; Zheng, M.; et al. Intercellular mitochondrial transfer as a means of tissue revitalization. Signal Transduct. Target. Ther. 2021, 6, 65. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Diao, S.; Fan, Z. The role and mechanism of mitochondrial functions and energy metabolism in the function regulation of the mesenchymal stem cells. Stem Cell Res. Ther. 2021, 12, 140. [Google Scholar] [CrossRef]
- Song, Y.; Lu, S.; Geng, W.; Feng, X.; Luo, R.; Li, G.; Yang, C. Mitochondrial quality control in intervertebral disc degeneration. Exp. Mol. Med. 2021, 53, 1124–1133. [Google Scholar] [CrossRef] [PubMed]
- Yan, C.; Shi, Y.; Yuan, L.; Lv, D.; Sun, B.; Wang, J.; Liu, X.; An, F. Mitochondrial quality control and its role in osteoporosis. Front. Endocrinol. 2023, 14, 1077058. [Google Scholar] [CrossRef]
- Zhang, L.; Lv, J.; Wang, C.; Ren, Y.; Yong, M. Myokine, a key cytokine for physical exercise to alleviate sarcopenic obesity. Mol. Biol. Rep. 2023, 50, 2723–2734. [Google Scholar] [CrossRef] [PubMed]
- Ost, M.; Coleman, V.; Kasch, J.; Klaus, S. Regulation of myokine expression: Role of exercise and cellular stress. Free Radic. Biol. Med. 2016, 98, 78–89. [Google Scholar] [CrossRef]
- Kim, H.; Wrann, C.; Jedrychowski, M.P.; Vidoni, S.; Kitase, Y.; Nagano, K.; Zhou, C.; Chou, J.; Parkman, V.; Novick, S.; et al. Irisin Mediates Effects on Bone and Fat via αV Integrin Receptors. Cell 2018, 175, 1756–1768.e17. [Google Scholar] [CrossRef]
- Tao, L.; Wang, J.; Wang, K.; Liu, Q.; Li, H.; Xu, S.; Gu, C.; Zhu, Y. Exerkine FNDC5/irisin-enriched exosomes promote proliferation and inhibit ferroptosis of osteoblasts through interaction with Caveolin-1. Aging Cell 2024, 23, e14181. [Google Scholar] [CrossRef] [PubMed]
- Falsetti, I.; Palmini, G.; Donati, S.; Aurilia, C.; Iantomasi, T.; Brandi, M.L. Irisin and Its Role in Postmenopausal Osteoporosis and Sarcopenia. Biomedicines 2024, 12, 928. [Google Scholar] [CrossRef] [PubMed]
- Shimonty, A.; Pin, F.; Prideaux, M.; Peng, G.; Huot, J.; Kim, H.; Rosen, C.J.; Spiegelman, B.M.; Bonewald, L.F. Deletion of FNDC5/irisin modifies murine osteocyte function in a sex-specific manner. eLife 2024, 12, RP92263. [Google Scholar] [CrossRef] [PubMed]
- Du, Z.-Y.; Zhu, H.-L.; Chang, W.; Zhang, Y.-F.; Ling, Q.; Wang, K.-W.; Zhang, J.; Zhang, Q.-B.; Kan, X.-L.; Wang, Q.-N.; et al. Maternal prednisone exposure during pregnancy elevates susceptibility to osteoporosis in female offspring: The role of mitophagy/FNDC5 alteration in skeletal muscle. J. Hazard. Mater. 2024, 469, 133997. [Google Scholar] [CrossRef]
- Shang, X.; Hao, X.; Hou, W.; Liu, J.; Chi, R.; Deng, X.; Pan, C.; Xu, T. Exercise-induced modulation of myokine irisin on muscle-bone unit in the rat model of post-traumatic osteoarthritis. J. Orthop. Surg. Res. 2024, 19, 49. [Google Scholar] [CrossRef]
- Estell, E.; Ichikawa, T.; Giffault, P.; Bonewald, L.; Spiegelman, B.; Rosen, C. Irisin Enhances Mitochondrial Function in Osteoclast Progenitors during Differentiation. Biomedicines 2023, 11, 3311. [Google Scholar] [CrossRef]
- Hu, X.; Wang, Z.; Wang, W.; Cui, P.; Kong, C.; Chen, X.; Lu, S. Irisin as an agent for protecting against osteoporosis: A review of the current mechanisms and pathways. J. Adv. Res. 2024, 62, 175–186. [Google Scholar] [CrossRef]
- Pang, B.P.S.; Chan, W.S.; Chan, C.B. Mitochondria Homeostasis and Oxidant/Antioxidant Balance in Skeletal Muscle-Do Myokines Play a Role? Antioxidants 2021, 10, 179. [Google Scholar] [CrossRef]
- Prasad, V.; Millay, D.P. Skeletal muscle fibers count on nuclear numbers for growth. Semin. Cell Dev. Biol. 2021, 119, 3–10. [Google Scholar] [CrossRef]
- Cai, L.; Shi, L.; Peng, Z.; Sun, Y.; Chen, J. Ageing of skeletal muscle extracellular matrix and mitochondria: Finding a potential link. Ann. Med. 2023, 55, 2240707. [Google Scholar] [CrossRef]
- Taylor, D.F.; Bishop, D.J. Transcription Factor Movement and Exercise-Induced Mitochondrial Biogenesis in Human Skeletal Muscle: Current Knowledge and Future Perspectives. Int. J. Mol. Sci. 2022, 23, 1517. [Google Scholar] [CrossRef] [PubMed]
- Joaquim, M.; Escobar-Henriques, M. Role of Mitofusins and Mitophagy in Life or Death Decisions. Front. Cell Dev. Biol. 2020, 8, 572182. [Google Scholar] [CrossRef] [PubMed]
- Nakano, D.; Machida, S. Mitochondrial fusion- and fission-related protein expression in the regulation of skeletal muscle mass. Physiol. Rep. 2022, 10, e15281. [Google Scholar] [CrossRef]
- Zheng, P.; Ma, W.; Gu, Y.; Wu, H.; Bian, Z.; Liu, N.; Yang, D.; Chen, X. High-fat diet causes mitochondrial damage and downregulation of mitofusin-2 and optic atrophy-1 in multiple organs. J. Clin. Biochem. Nutr. 2023, 73, 61–76. [Google Scholar] [CrossRef]
- Martinez-Vicente, M. Neuronal Mitophagy in Neurodegenerative Diseases. Front. Mol. Neurosci. 2017, 10, 64. [Google Scholar] [CrossRef] [PubMed]
- Su, S.-H.; Wu, Y.-F.; Wang, D.-P.; Hai, J. Inhibition of excessive autophagy and mitophagy mediates neuroprotective effects of URB597 against chronic cerebral hypoperfusion. Cell Death Dis. 2018, 9, 733. [Google Scholar] [CrossRef]
- Fu, T.; Xu, Z.; Liu, L.; Guo, Q.; Wu, H.; Liang, X.; Zhou, D.; Xiao, L.; Liu, L.; Liu, Y.; et al. Mitophagy Directs Muscle-Adipose Crosstalk to Alleviate Dietary Obesity. Cell Rep. 2018, 23, 1357–1372. [Google Scholar] [CrossRef]
- Cairns, G.; Thumiah-Mootoo, M.; Abbasi, M.R.; Gourlay, M.; Racine, J.; Larionov, N.; Prola, A.; Khacho, M.; Burelle, Y. PINK1 deficiency alters muscle stem cell fate decision and muscle regenerative capacity. Stem Cell Rep. 2024, 19, 673–688. [Google Scholar] [CrossRef]
- Carnio, S.; LoVerso, F.; Baraibar, M.A.; Longa, E.; Khan, M.M.; Maffei, M.; Reischl, M.; Canepari, M.; Loefler, S.; Kern, H.; et al. Autophagy impairment in muscle induces neuromuscular junction degeneration and precocious aging. Cell Rep. 2014, 8, 1509–1521. [Google Scholar] [CrossRef]
- Collier, J.J.; Guissart, C.; Oláhová, M.; Sasorith, S.; Piron-Prunier, F.; Suomi, F.; Zhang, D.; Martinez-Lopez, N.; Leboucq, N.; Bahr, A.; et al. Developmental Consequences of Defective ATG7-Mediated Autophagy in Humans. N. Engl. J. Med. 2021, 384, 2406–2417. [Google Scholar] [CrossRef]
- Therdyothin, A.; Phiphopthatsanee, N.; Isanejad, M. The Effect of Omega-3 Fatty Acids on Sarcopenia: Mechanism of Action and Potential Efficacy. Mar. Drugs 2023, 21, 399. [Google Scholar] [CrossRef] [PubMed]
- Tincknell, J.B.; Kugler, B.A.; Spicuzza, H.; Berger, N.; Yan, H.; You, T.; Zou, K. High-intensity interval training attenuates impairment in regulatory protein machinery of mitochondrial quality control in skeletal muscle of diet-induced obese mice. Appl. Physiol. Nutr. Metab. 2024, 49, 236–249. [Google Scholar] [CrossRef] [PubMed]
- Potes, Y.; Díaz-Luis, A.; Bermejo-Millo, J.C.; Pérez-Martínez, Z.; de Luxán-Delgado, B.; Rubio-González, A.; Menéndez-Valle, I.; Gutiérrez-Rodríguez, J.; Solano, J.J.; Caballero, B.; et al. Melatonin Alleviates the Impairment of Muscle Bioenergetics and Protein Quality Control Systems in Leptin-Deficiency-Induced Obesity. Antioxidants 2023, 12, 1962. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Zhang, Q.; Ma, W.; Hu, R.; Gu, Y.; Bian, Z.; Yang, D.; Chen, X.; Wu, H. Low-dose atorvastatin protects skeletal muscle mitochondria in high-fat diet-fed mice with mitochondrial autophagy inhibition and fusion enhancement. Eur. J. Pharmacol. 2023, 959, 176085. [Google Scholar] [CrossRef] [PubMed]
- Tung, Y.-T.; Chiang, P.-C.; Chen, Y.-L.; Chien, Y.-W. Effects of Melatonin on Lipid Metabolism and Circulating Irisin in Sprague-Dawley Rats with Diet-Induced Obesity. Molecules 2020, 25, 3329. [Google Scholar] [CrossRef]
- Sun, B.; Wu, H.; Lu, J.; Zhang, R.; Shen, X.; Gu, Y.; Shi, C.; Zhang, Y.; Yuan, W. Irisin reduces bone fracture by facilitating osteogenesis and antagonizing TGF-β/Smad signaling in a growing mouse model of osteogenesis imperfecta. J. Orthop. Transl. 2023, 38, 175–189. [Google Scholar] [CrossRef]
- Vadalà, G.; Di Giacomo, G.; Ambrosio, L.; Cicione, C.; Tilotta, V.; Russo, F.; Papalia, R.; Denaro, V. Effect of Irisin on Human Nucleus Pulposus Cells: New Insights into the Biological Cross-talk Between Muscle and Intervertebral Disk. Spine 2023, 48, 468–475. [Google Scholar] [CrossRef]
- Behera, J.; Ison, J.; Voor, M.J.; Tyagi, N. Exercise-Linked Skeletal Irisin Ameliorates Diabetes-Associated Osteoporosis by Inhibiting the Oxidative Damage-Dependent miR-150-FNDC5/Pyroptosis Axis. Diabetes 2022, 71, 2777–2792. [Google Scholar] [CrossRef]
- Colaianni, G.; Oranger, A.; Dicarlo, M.; Lovero, R.; Storlino, G.; Pignataro, P.; Fontana, A.; Di Serio, F.; Ingravallo, A.; Caputo, G.; et al. Irisin Serum Levels and Skeletal Muscle Assessment in a Cohort of Charcot-Marie-Tooth Patients. Front. Endocrinol. 2022, 13, 886243. [Google Scholar] [CrossRef]
- Bi, J.; Zhang, J.; Ren, Y.; Du, Z.; Li, Q.; Wang, Y.; Wei, S.; Yang, L.; Zhang, J.; Liu, C.; et al. Irisin alleviates liver ischemia-reperfusion injury by inhibiting excessive mitochondrial fission, promoting mitochondrial biogenesis and decreasing oxidative stress. Redox Biol. 2019, 20, 296–306. [Google Scholar] [CrossRef]
- Liu, J.-F.; Su, G.; Chen, L.-X.; Zhou, J.-P.; Gao, J.; Zhang, J.-J.; Wu, Q.-H.; Chen, W.; Chen, D.-Y.; Zhang, Z.-C. Irisin Attenuates Apoptosis Following Ischemia-Reperfusion Injury Through Improved Mitochondria Dynamics and ROS Suppression Mediated Through the PI3K/Akt/mTOR Axis. Mol. Neurobiol. 2023, 60, 4261–4272. [Google Scholar] [CrossRef]
- Li, H.; Qin, S.; Liang, Q.; Xi, Y.; Bo, W.; Cai, M.; Tian, Z. Exercise Training Enhances Myocardial Mitophagy and Improves Cardiac Function via Irisin/FNDC5-PINK1/Parkin Pathway in MI Mice. Biomedicines 2021, 9, 701. [Google Scholar] [CrossRef]
- Waseem, R.; Shamsi, A.; Mohammad, T.; Hassan, M.I.; Kazim, S.N.; Chaudhary, A.A.; Rudayni, H.A.; Al-Zharani, M.; Ahmad, F.; Islam, A. FNDC5/Irisin: Physiology and Pathophysiology. Molecules 2022, 27, 1118. [Google Scholar] [CrossRef]
- He, X.; Hua, Y.; Li, Q.; Zhu, W.; Pan, Y.; Yang, Y.; Li, X.; Wu, M.; Wang, J.; Gan, X. FNDC5/irisin facilitates muscle-adipose-bone connectivity through ubiquitination-dependent activation of runt-related transcriptional factors RUNX1/2. J. Biol. Chem. 2022, 298, 101679. [Google Scholar] [CrossRef]
- Wang, P.-W.; Pang, Q.; Zhou, T.; Song, X.-Y.; Pan, Y.-J.; Jia, L.-P.; Zhang, A.-H. Irisin alleviates vascular calcification by inhibiting VSMC osteoblastic transformation and mitochondria dysfunction via AMPK/Drp1 signaling pathway in chronic kidney disease. Atherosclerosis 2022, 346, 36–45. [Google Scholar] [CrossRef]
- Zhang, X.; Xu, S.; Hu, Y.; Liu, Q.; Liu, C.; Chai, H.; Luo, Y.; Jin, L.; Li, S. Irisin exhibits neuroprotection by preventing mitochondrial damage in Parkinson’s disease. NPJ Park. Dis. 2023, 9, 13. [Google Scholar] [CrossRef]
- Zerlotin, R.; Oranger, A.; Pignataro, P.; Dicarlo, M.; Maselli, F.; Mori, G.; Colucci, S.C.; Grano, M.; Colaianni, G. Irisin and Secondary Osteoporosis in Humans. Int. J. Mol. Sci. 2022, 23, 690. [Google Scholar] [CrossRef]
- Kawao, N.; Kawaguchi, M.; Ohira, T.; Ehara, H.; Mizukami, Y.; Takafuji, Y.; Kaji, H. Renal failure suppresses muscle irisin expression, and irisin blunts cortical bone loss in mice. J. Cachexia Sarcopenia Muscle 2022, 13, 758–771. [Google Scholar] [CrossRef]
- Bao, J.-F.; She, Q.-Y.; Hu, P.-P.; Jia, N.; Li, A. Irisin, a fascinating field in our times. Trends Endocrinol. Metab. 2022, 33, 601–613. [Google Scholar] [CrossRef]
- Nie, Y.; Dai, B.; Guo, X.; Liu, D. Cleavage of FNDC5 and insights into its maturation process. Mol. Cell. Endocrinol. 2020, 510, 110840. [Google Scholar] [CrossRef]
- Liu, S.; Cui, F.; Ning, K.; Wang, Z.; Fu, P.; Wang, D.; Xu, H. Role of irisin in physiology and pathology. Front. Endocrinol. 2022, 13, 962968. [Google Scholar] [CrossRef]
- Sundarrajan, L.; Yeung, C.; Hahn, L.; Weber, L.P.; Unniappan, S. Irisin regulates cardiac physiology in zebrafish. PLoS ONE 2017, 12, e0181461. [Google Scholar] [CrossRef]
- Huh, J.Y.; Dincer, F.; Mesfum, E.; Mantzoros, C.S. Irisin stimulates muscle growth-related genes and regulates adipocyte differentiation and metabolism in humans. Int. J. Obes. 2014, 38, 1538–1544. [Google Scholar] [CrossRef]
- Nie, Y.; Liu, D. N-Glycosylation is required for FDNC5 stabilization and irisin secretion. Biochem. J. 2017, 474, 3167–3177. [Google Scholar] [CrossRef]
- Boström, P.; Wu, J.; Jedrychowski, M.P.; Korde, A.; Ye, L.; Lo, J.C.; Rasbach, K.A.; Boström, E.A.; Choi, J.H.; Long, J.Z.; et al. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 2012, 481, 463–468. [Google Scholar] [CrossRef]
- Pang, M.; Yang, J.; Rao, J.; Wang, H.; Zhang, J.; Wang, S.; Chen, X.; Dong, X. Time-Dependent Changes in Increased Levels of Plasma Irisin and Muscle PGC-1α and FNDC5 after Exercise in Mice. Tohoku J. Exp. Med. 2018, 244, 93–103. [Google Scholar] [CrossRef]
- Pekkala, S.; Wiklund, P.K.; Hulmi, J.J.; Ahtiainen, J.P.; Horttanainen, M.; Pöllänen, E.; Mäkelä, K.A.; Kainulainen, H.; Häkkinen, K.; Nyman, K.; et al. Are skeletal muscle FNDC5 gene expression and irisin release regulated by exercise and related to health? J. Physiol. 2013, 591, 5393–5400. [Google Scholar] [CrossRef]
- Panati, K.; Suneetha, Y.; Narala, V.R. Irisin/FNDC5--An updated review. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 689–697. [Google Scholar]
- Maak, S.; Norheim, F.; Drevon, C.A.; Erickson, H.P. Progress and Challenges in the Biology of FNDC5 and Irisin. Endocr. Rev. 2021, 42, 436–456. [Google Scholar] [CrossRef]
- Erickson, H.P. Irisin and FNDC5 in retrospect: An exercise hormone or a transmembrane receptor? Adipocyte 2013, 2, 289–293. [Google Scholar] [CrossRef]
- Zhao, Y.; Li, H.; Donelan, W.; Li, S.; Tang, D. Expression of Recombinant Rat Secretable FNDC5 in Pichia Pastoris and Detection of Its Biological Activity. Front. Endocrinol. 2022, 13, 852015. [Google Scholar] [CrossRef]
- Fu, J.; Li, F.; Tang, Y.; Cai, L.; Zeng, C.; Yang, Y.; Yang, J. The Emerging Role of Irisin in Cardiovascular Diseases. J. Am. Heart Assoc. 2021, 10, e022453. [Google Scholar] [CrossRef]
- Kazeminasab, F.; Sadeghi, E.; Afshari-Safavi, A. Comparative Impact of Various Exercises on Circulating Irisin in Healthy Subjects: A Systematic Review and Network Meta-Analysis. Oxid. Med. Cell. Longev. 2022, 2022, 8235809. [Google Scholar] [CrossRef]
- Nygaard, H.; Slettaløkken, G.; Vegge, G.; Hollan, I.; Whist, J.E.; Strand, T.; Rønnestad, B.R.; Ellefsen, S. Irisin in blood increases transiently after single sessions of intense endurance exercise and heavy strength training. PLoS ONE 2015, 10, e0121367. [Google Scholar] [CrossRef]
- Roca-Rivada, A.; Castelao, C.; Senin, L.L.; Landrove, M.O.; Baltar, J.; Belén Crujeiras, A.; Seoane, L.M.; Casanueva, F.F.; Pardo, M. FNDC5/irisin is not only a myokine but also an adipokine. PLoS ONE 2013, 8, e60563. [Google Scholar] [CrossRef]
- Rodríguez, A.; Becerril, S.; Ezquerro, S.; Méndez-Giménez, L.; Frühbeck, G. Crosstalk between adipokines and myokines in fat browning. Acta Physiol. 2017, 219, 362–381. [Google Scholar] [CrossRef]
- Dai, D.; Xu, F.; Sun, R.; Yuan, L.; Sheng, Z.; Xie, Z. Decreased lower-extremity muscle performance is associated with decreased hip bone mineral density and increased estimated fracture risk in community-dwelling postmenopausal women. Arch. Osteoporos. 2020, 15, 173. [Google Scholar] [CrossRef]
- Hsu, H.-H.; Chiu, C.-Y.; Chen, W.-C.; Yang, Y.-R.; Wang, R.-Y. Effects of exercise on bone density and physical performance in postmenopausal women: A systematic review and meta-analysis. PM R 2024. ahead of print. [Google Scholar] [CrossRef]
- Gibbs, J.C.; Craven, B.C.; Moore, C.; Thabane, L.; Adachi, J.D.; Giangregorio, L.M. Muscle Density and Bone Quality of the Distal Lower Extremity Among Individuals with Chronic Spinal Cord Injury. Top. Spinal Cord Inj. Rehabil. 2015, 21, 282–293. [Google Scholar] [CrossRef]
- Alazzam, A.M.; Goldsmith, J.A.; Khalil, R.E.; Khan, M.R.; Gorgey, A.S. Denervation impacts muscle quality and knee bone mineral density after spinal cord injury. Spinal Cord 2023, 61, 276–284. [Google Scholar] [CrossRef]
- Ceroni, D.; Martin, X.; Delhumeau, C.; Rizzoli, R.; Kaelin, A.; Farpour-Lambert, N. Effects of cast-mediated immobilization on bone mineral mass at various sites in adolescents with lower-extremity fracture. J. Bone Jt. Surg. Am. 2012, 94, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Jing, P.; Liu, Z.; Wang, Y.; Han, Z.; Wang, Y.; Zheng, Z.; Wu, Y.; Wang, T.; Li, Y.; et al. Serum levels of irisin in postmenopausal women with osteoporotic hip fractures. Cytokine 2021, 148, 155708. [Google Scholar] [CrossRef]
- Yan, J.; Liu, H.; Guo, W.; Yang, J. Low serum concentrations of Irisin are associated with increased risk of hip fracture in Chinese older women. Jt. Bone Spine Rev. Rhum. 2017, 85, 353–358. [Google Scholar] [CrossRef]
- Anastasilakis, A.; Polyzos, S.; Makras, P.; Gkiomisi, A.; Bisbinas, I.; Katsarou, A.; Filippaios, A.; Mantzoros, C. Circulating irisin is associated with osteoporotic fractures in postmenopausal women with low bone mass but is not affected by either teriparatide or denosumab treatment for 3 months. Osteoporos. Int. 2014, 25, 1633–1642. [Google Scholar] [CrossRef]
- Colaianni, G.; Cuscito, C.; Mongelli, T.; Pignataro, P.; Buccoliero, C.; Liu, P.; Lu, P.; Sartini, L.; Comite, M.D.; Mori, G.; et al. The myokine irisin increases cortical bone mass. Proc. Natl. Acad. Sci. USA 2015, 112, 12157–12162. [Google Scholar] [CrossRef] [PubMed]
- Colaianni, G.; Cuscito, C.; Mongelli, T.; Oranger, A.; Mori, G.; Brunetti, G.; Colucci, S.; Cinti, S.; Grano, M. Irisin Enhances Osteoblast Differentiation In Vitro. Int. J. Endocrinol. 2014, 2014, 902186. [Google Scholar] [CrossRef]
- Kan, T.; He, Z.; Du, J.; Xu, M.; Cui, J.; Han, X.; Tong, D.; Li, H.; Yan, M.; Yu, Z. Irisin promotes fracture healing by improving osteogenesis and angiogenesis. J. Orthop. Transl. 2022, 37, 37–45. [Google Scholar] [CrossRef]
- Qiao, X.Y.; Nie, Y.; Ma, Y.X.; Chen, Y.; Cheng, R.; Yinrg, W.Y.; Hu, Y.; Xu, W.M.; Xu, L.Z. Irisin promotes osteoblast proliferation and differentiation via activating the MAP kinase signaling pathways. Sci. Rep. 2016, 6, 18732. [Google Scholar] [CrossRef]
- Wang, F.-S.; Kuo, C.-W.; Ko, J.-Y.; Chen, Y.-S.; Wang, S.-Y.; Ke, H.-J.; Kuo, P.-C.; Lee, C.-H.; Wu, J.-C.; Lu, W.-B.; et al. Irisin Mitigates Oxidative Stress, Chondrocyte Dysfunction and Osteoarthritis Development through Regulating Mitochondrial Integrity and Autophagy. Antioxidants 2020, 9, 810. [Google Scholar] [CrossRef]
- Ma, Y.; Qiao, X.; Zeng, R.; Cheng, R.; Zhang, J.; Luo, Y.; Nie, Y.; Hu, Y.; Yang, Z.; Zhang, J.; et al. Irisin promotes proliferation but inhibits differentiation in osteoclast precursor cells. FASEB J. 2018, 32, 5813–5823. [Google Scholar] [CrossRef]
- Zhu, X.; Li, X.; Wang, X.; Chen, T.; Tao, F.; Liu, C.; Tu, Q.; Shen, G.; Chen, J.J. Irisin deficiency disturbs bone metabolism. J. Cell. Physiol. 2021, 236, 664–676. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Jian, Z.; Wang, H.; Xu, L.; Zhang, T.; Song, J. Irisin Promotes Osteogenesis by Modulating Oxidative Stress and Mitophagy through SIRT3 Signaling under Diabetic Conditions. Oxid. Med. Cell. Longev. 2022, 2022, 3319056. [Google Scholar] [CrossRef] [PubMed]
- Xin, C.; Zhang, Z.; Gao, G.; Ding, L.; Yang, C.; Wang, C.; Liu, Y.; Guo, Y.; Yang, X.; Zhang, L.; et al. Irisin Attenuates Myocardial Ischemia/Reperfusion Injury and Improves Mitochondrial Function through AMPK Pathway in Diabetic Mice. Front. Pharmacol. 2020, 11, 565160. [Google Scholar] [CrossRef]
- Saito, M.; Okamatsu-Ogura, Y.; Matsushita, M.; Watanabe, K.; Yoneshiro, T.; Nio-Kobayashi, J.; Iwanaga, T.; Miyagawa, M.; Kameya, T.; Nakada, K.; et al. High incidence of metabolically active brown adipose tissue in healthy adult humans: Effects of cold exposure and adiposity. Diabetes 2009, 58, 1526–1531. [Google Scholar] [CrossRef]
- Aquilano, K.; Zhou, B.; Brestoff, J.R.; Lettieri-Barbato, D. Multifaceted mitochondrial quality control in brown adipose tissue. Trends Cell Biol. 2023, 33, 517–529. [Google Scholar] [CrossRef]
- Reza, M.M.; Subramaniyam, N.; Sim, C.M.; Ge, X.; Sathiakumar, D.; McFarlane, C.; Sharma, M.; Kambadur, R. Irisin is a pro-myogenic factor that induces skeletal muscle hypertrophy and rescues denervation-induced atrophy. Nat. Commun. 2017, 8, 1104. [Google Scholar] [CrossRef]
- Guo, M.; Yao, J.; Li, J.; Zhang, J.; Wang, D.; Zuo, H.; Zhang, Y.; Xu, B.; Zhong, Y.; Shen, F.; et al. Irisin ameliorates age-associated sarcopenia and metabolic dysfunction. J. Cachexia Sarcopenia Muscle 2023, 14, 391–405. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, R.A.; Gannon, N.P.; Mermier, C.M.; Conn, C.A. Irisin, a unique non-inflammatory myokine in stimulating skeletal muscle metabolism. J. Physiol. Biochem. 2015, 71, 679–689. [Google Scholar] [CrossRef]
- Vaughan, R.A.; Gannon, N.P.; Barberena, M.A.; Garcia-Smith, R.; Bisoffi, M.; Mermier, C.M.; Conn, C.A.; Trujillo, K.A. Characterization of the metabolic effects of irisin on skeletal muscle in vitro. Diabetes Obes. Metab. 2014, 16, 711–718. [Google Scholar] [CrossRef]
- Huh, J.Y.; Mougios, V.; Kabasakalis, A.; Fatouros, I.; Siopi, A.; Douroudos, I.I.; Filippaios, A.; Panagiotou, G.; Park, K.H.; Mantzoros, C.S. Exercise-induced irisin secretion is independent of age or fitness level and increased irisin may directly modulate muscle metabolism through AMPK activation. J. Clin. Endocrinol. Metab. 2014, 99, E2154–E2161. [Google Scholar] [CrossRef]
- Aydin, S.; Kuloglu, T.; Aydin, S.; Kalayci, M.; Yilmaz, M.; Cakmak, T.; Albayrak, S.; Gungor, S.; Colakoglu, N.; Ozercan, I.H. A comprehensive immunohistochemical examination of the distribution of the fat-burning protein irisin in biological tissues. Peptides 2014, 61, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Tang, M.; Yang, G.; Wang, L.; Gao, Q.; Zhang, H. Muscle Injury Associated Elevated Oxidative Stress and Abnormal Myogenesis in Patients with Idiopathic Scoliosis. Int. J. Biol. Sci. 2019, 15, 2584–2595. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Wu, Z.; Wang, Y.; Dai, Z.; Feng, Z.; Sun, X.; Liu, Z.; Cheng, J.; Qiu, Y.; Zhu, Z. LONP1 is associated with the incidence of idiopathic scoliosis possibly via defective mitochondrial function. Stud. Health Technol. Inform. 2021, 280, 253. [Google Scholar] [CrossRef]
- Matsushima, Y.; Takahashi, K.; Yue, S.; Fujiyoshi, Y.; Yoshioka, H.; Aihara, M.; Setoyama, D.; Uchiumi, T.; Fukuchi, S.; Kang, D. Mitochondrial Lon protease is a gatekeeper for proteins newly imported into the matrix. Commun. Biol. 2021, 4, 974. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Fu, T.; Guo, Q.; Zhou, D.; Sun, W.; Zhou, Z.; Chen, X.; Zhang, J.; Liu, L.; Xiao, L.; et al. Disuse-associated loss of the protease LONP1 in muscle impairs mitochondrial function and causes reduced skeletal muscle mass and strength. Nat. Commun. 2022, 13, 894. [Google Scholar] [CrossRef]
- Yang, G.; Tang, M.; Zhang, H.; Li, J.; Xiao, L.; Guo, C. Altered Circulating Cell-free Mitochondrial DNA of Patients with Congenital Scoliosis. Spine 2021, 46, 499–506. [Google Scholar] [CrossRef]
- Li, J.; Wang, L.; Yang, G.; Wang, Y.; Guo, C.; Liu, S.; Gao, Q.; Zhang, H. Changes in circulating cell-free nuclear DNA and mitochondrial DNA of patients with adolescent idiopathic scoliosis. BMC Musculoskelet. Disord. 2019, 20, 479. [Google Scholar] [CrossRef]
- Tan, D.-X.; Manchester, L.C.; Qin, L.; Reiter, R.J. Melatonin: A Mitochondrial Targeting Molecule Involving Mitochondrial Protection and Dynamics. Int. J. Mol. Sci. 2016, 17, 2124. [Google Scholar] [CrossRef]
- Chen, C.; Xu, C.; Zhou, T.; Gao, B.; Zhou, H.; Chen, C.; Zhang, C.; Huang, D.; Su, P. Abnormal osteogenic and chondrogenic differentiation of human mesenchymal stem cells from patients with adolescent idiopathic scoliosis in response to melatonin. Mol. Med. Rep. 2016, 14, 1201–1209. [Google Scholar] [CrossRef]
- Li, J.; Li, N.; Chen, Y.; Hui, S.; Fan, J.; Ye, B.; Fan, Z.; Zhang, J.; Zhao, R.C.; Zhuang, Q. SPRY4 is responsible for pathogenesis of adolescent idiopathic scoliosis by contributing to osteogenic differentiation and melatonin response of bone marrow-derived mesenchymal stem cells. Cell Death Dis. 2019, 10, 805. [Google Scholar] [CrossRef]
- Feng, Z.; Wu, Z.; Ma, Y.; Chen, Q.; Liu, Z.; Qiu, Y.; Zhu, Z. Higher Baseline Serum Myokine of FSTL1 May Serve as a Potential Predictive Biomarker for Successful Brace Treatment in Girls With Adolescent Idiopathic Scoliosis. Spine 2023, 48, 1756–1762. [Google Scholar] [CrossRef]
- Chen, W.; Wang, D.; Ma, L.; Wu, F.; Ren, Q.; Tao, J.; Chen, X.; Zhang, A. Chronic arsenite exposure induced skeletal muscle atrophy by disrupting angiotensin II-melatonin axis in rats. Environ. Toxicol. 2024, 39, 1350–1359. [Google Scholar] [CrossRef] [PubMed]
- Qi, J.-L.; Zhang, Z.-D.; Dong, Z.; Shan, T.; Yin, Z.-S. mir-150-5p inhibits the osteogenic differentiation of bone marrow-derived mesenchymal stem cells by targeting irisin to regulate the p38/MAPK signaling pathway. J. Orthop. Surg. 2024, 19, 190. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Kim, S.E.; Kim, S.; Ahn, M.B.; Cho, W.K.; Cho, K.S.; Jung, M.H. The association of serum irisin with anthropometric, metabolic, and bone parameters in obese children and adolescents. Front. Endocrinol. 2023, 14, 1326851. [Google Scholar] [CrossRef]
- Liang, H.; Qi, W.; Jiajue, R.; Chi, Y.; Liu, W.; Wang, O.; Li, M.; Xing, X.; Yu, W.; Jiang, Y.; et al. Serum Irisin level is associated with fall risk, muscle strength, and cortical porosity in postmenopausal women. Front. Endocrinol. 2023, 14, 1096950. [Google Scholar] [CrossRef] [PubMed]
- Demir, C.; Dursun, A.D.; Sarıyıldız, G.T.; Arslan, A.İ. Serum irisin levels and osteoporosis in patients with advanced chronic kidney disease and renal transplant recipients. Int. Urol. Nephrol. 2023, 55, 1821–1828. [Google Scholar] [CrossRef]
- Colaianni, G.; Errede, M.; Sanesi, L.; Notarnicola, A.; Celi, M.; Zerlotin, R.; Storlino, G.; Pignataro, P.; Oranger, A.; Pesce, V.; et al. Irisin Correlates Positively With BMD in a Cohort of Older Adult Patients and Downregulates the Senescent Marker p21 in Osteoblasts. J. Bone Miner. Res. 2021, 36, 305–314. [Google Scholar] [CrossRef]
- Palermo, A.; Strollo, R.; Maddaloni, E.; Tuccinardi, D.; D’Onofrio, L.; Briganti, S.; Defeudis, G.; Pascalis, M.D.; Lazzaro, M.; Colleluori, G.; et al. Irisin is associated with osteoporotic fractures independently of bone mineral density, body composition or daily physical activity. Clin. Endocrinol. 2015, 82, 615–619. [Google Scholar] [CrossRef]
- Kim, J.-H.; Lee, D.-C. Mitochondrial DNA copy number in peripheral blood is associated with femoral neck bone mineral density in postmenopausal women. J. Rheumatol. 2012, 39, 1465–1472. [Google Scholar] [CrossRef]
- Sun, K.; Jing, X.; Guo, J.; Yao, X.; Guo, F. Mitophagy in degenerative joint diseases. Autophagy 2021, 17, 2082–2092. [Google Scholar] [CrossRef]
- Li, M.; Yu, Y.; Xue, K.; Li, J.; Son, G.; Wang, J.; Qian, W.; Wang, S.; Zheng, J.; Yang, C.; et al. Genistein mitigates senescence of bone marrow mesenchymal stem cells via ERRα-mediated mitochondrial biogenesis and mitophagy in ovariectomized rats. Redox Biol. 2023, 61, 102649. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, D.; Zhang, Y.; Ge, J.; Yang, C. Mitochondria-specific antioxidant MitoTEMPO alleviates senescence of bone marrow mesenchymal stem cells in ovariectomized rats. J. Cell. Physiol. 2024, 239, e31323. [Google Scholar] [CrossRef] [PubMed]
- Marques-Carvalho, A.; Silva, B.; Pereira, F.B.; Kim, H.-N.; Almeida, M.; Sardão, V.A. Oestradiol and osteoclast differentiation: Effects on p53 and mitochondrial metabolism. Eur. J. Clin. Investig. 2024, 54, e14195. [Google Scholar] [CrossRef]
- Marques-Carvalho, A.; Sardão, V.A.; Kim, H.-N.; Almeida, M. ECSIT is essential for RANKL-induced stimulation of mitochondria in osteoclasts and a target for the anti-osteoclastogenic effects of estrogens. Front. Endocrinol. 2023, 14, 1110369. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Wang, A.; Shen, G.; Wang, X.; Liu, G.; Yang, F.; Chen, B.; Wang, M.; Xu, Y. Hepcidin-induced reduction in iron content and PGC-1β expression negatively regulates osteoclast differentiation to play a protective role in postmenopausal osteoporosis. Aging 2021, 13, 11296–11314. [Google Scholar] [CrossRef]
- Jing, X.; Du, T.; Chen, K.; Guo, J.; Xiang, W.; Yao, X.; Sun, K.; Ye, Y.; Guo, F. Icariin protects against iron overload-induced bone loss via suppressing oxidative stress. J. Cell. Physiol. 2019, 234, 10123–10137. [Google Scholar] [CrossRef]
- Ho, M.-Y.; Wang, C.-Y. Role of Irisin in Myocardial Infarction, Heart Failure, and Cardiac Hypertrophy. Cells 2021, 10, 2103. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Xu, Z.; Liu, Y.; Wang, Z.; Li, Y.; Xu, X.; Chen, C.; Xia, T.; Liao, Q.; Yao, Y.; et al. Irisin protects mitochondria function during pulmonary ischemia/reperfusion injury. Sci. Transl. Med. 2017, 9, eaao6298. [Google Scholar] [CrossRef]
- Ivanov, I.P.; Firth, A.E.; Michel, A.M.; Atkins, J.F.; Baranov, P.V. Identification of evolutionarily conserved non-AUG-initiated N-terminal extensions in human coding sequences. Nucleic Acids Res. 2011, 39, 4220–4234. [Google Scholar] [CrossRef]
- Raschke, S.; Elsen, M.; Gassenhuber, H.; Sommerfeld, M.; Schwahn, U.; Brockmann, B.; Jung, R.; Wisløff, U.; Tjønna, A.E.; Raastad, T.; et al. Evidence against a beneficial effect of irisin in humans. PLoS ONE 2013, 8, e73680. [Google Scholar] [CrossRef]
- Timmons, J.A.; Baar, K.; Davidsen, P.K.; Atherton, P.J. Is irisin a human exercise gene? Nature 2012, 488, E9–E10, discussion E10–E11. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, E.; Norheim, F.; Thiede, B.; Holen, T.; Ohashi, T.; Schering, L.; Lee, S.; Brenmoehl, J.; Thomas, S.; Drevon, C.; et al. Irisin—A myth rather than an exercise-inducible myokine. Sci. Rep. 2015, 5, 8889. [Google Scholar] [CrossRef] [PubMed]

| Date of Publish | Research Type | Sample Size | Subjects | Conclusion | Reference |
|---|---|---|---|---|---|
| 24 January | cross-section study | 103 | Children and adolescents | Serum irisin levels are associated with bone quality in children and adolescents. | [104] |
| 23 February | cross-section study | 138 | Postmenopausal women | Serum irisin levels are positively correlated with BMD. Low serum irisin levels are associated with a high risk of falls and low muscle strength. | [105] |
| 23 July | cross-section study | 74 | Patients with chronic kidney disease | Serum irisin levels are positively correlated with femoral BMD. | [106] |
| 21 December | cross-section and case–control study | 430 (215:215) | Postmenopausal women with/without hip fractures | Decreased circulating irisin serum levels are associated with an increased risk of hip fractures related to osteoporosis. | [72] |
| 21 February | cross-section study | 62 | Elderly patients with arthroplasty surgery | Circulating irisin levels are negatively correlated with the incidence of age-related osteoporosis. | [107] |
| 15 April | cross-section study | 72 (36:36) | Overweight patients with/without osteoporosis | Circulating irisin levels are negatively correlated with vertebral fragility fractures. | [108] |
| 14 May | matched case–control study | 125 (50:25; 25:25) | Postmenopausal women with low bone mass and osteoporosis | Circulating irisin levels are negatively correlated with osteoporotic fractures. | [74] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, C.; Wu, Y.; Zhu, S.; Liu, H.; Xu, S. Irisin Protects Musculoskeletal Homeostasis via a Mitochondrial Quality Control Mechanism. Int. J. Mol. Sci. 2024, 25, 10116. https://doi.org/10.3390/ijms251810116
Zhao C, Wu Y, Zhu S, Liu H, Xu S. Irisin Protects Musculoskeletal Homeostasis via a Mitochondrial Quality Control Mechanism. International Journal of Molecular Sciences. 2024; 25(18):10116. https://doi.org/10.3390/ijms251810116
Chicago/Turabian StyleZhao, Chong, Yonghao Wu, Shuaiqi Zhu, Haiying Liu, and Shuai Xu. 2024. "Irisin Protects Musculoskeletal Homeostasis via a Mitochondrial Quality Control Mechanism" International Journal of Molecular Sciences 25, no. 18: 10116. https://doi.org/10.3390/ijms251810116
APA StyleZhao, C., Wu, Y., Zhu, S., Liu, H., & Xu, S. (2024). Irisin Protects Musculoskeletal Homeostasis via a Mitochondrial Quality Control Mechanism. International Journal of Molecular Sciences, 25(18), 10116. https://doi.org/10.3390/ijms251810116






