A Comprehensive Review of Xanthan Gum-Based Oral Drug Delivery Systems
Abstract
1. Introduction
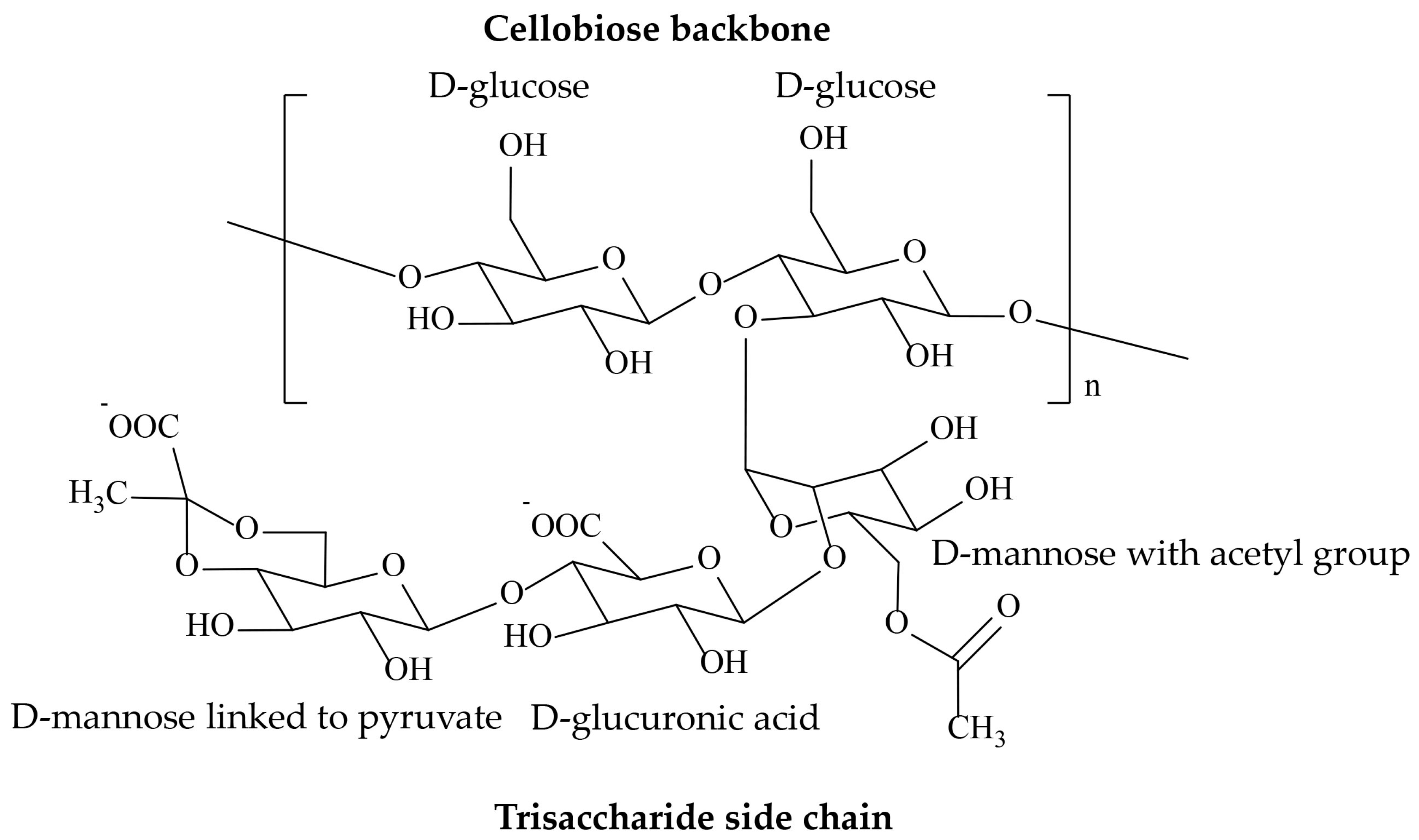
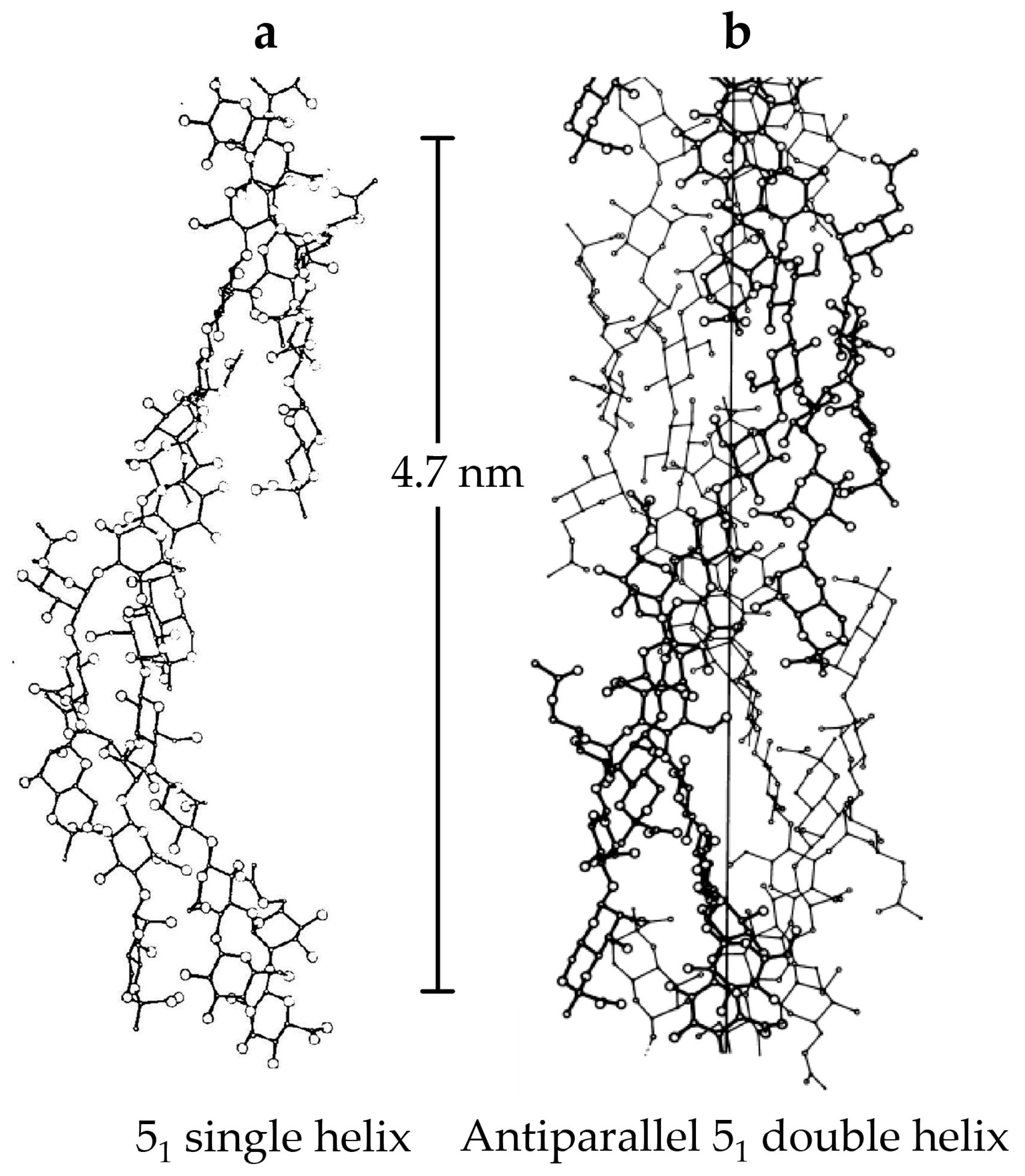
2. Source, Structure, and Properties
3. Applications
3.1. Sustained Release System
3.2. Gastroretentive Systems
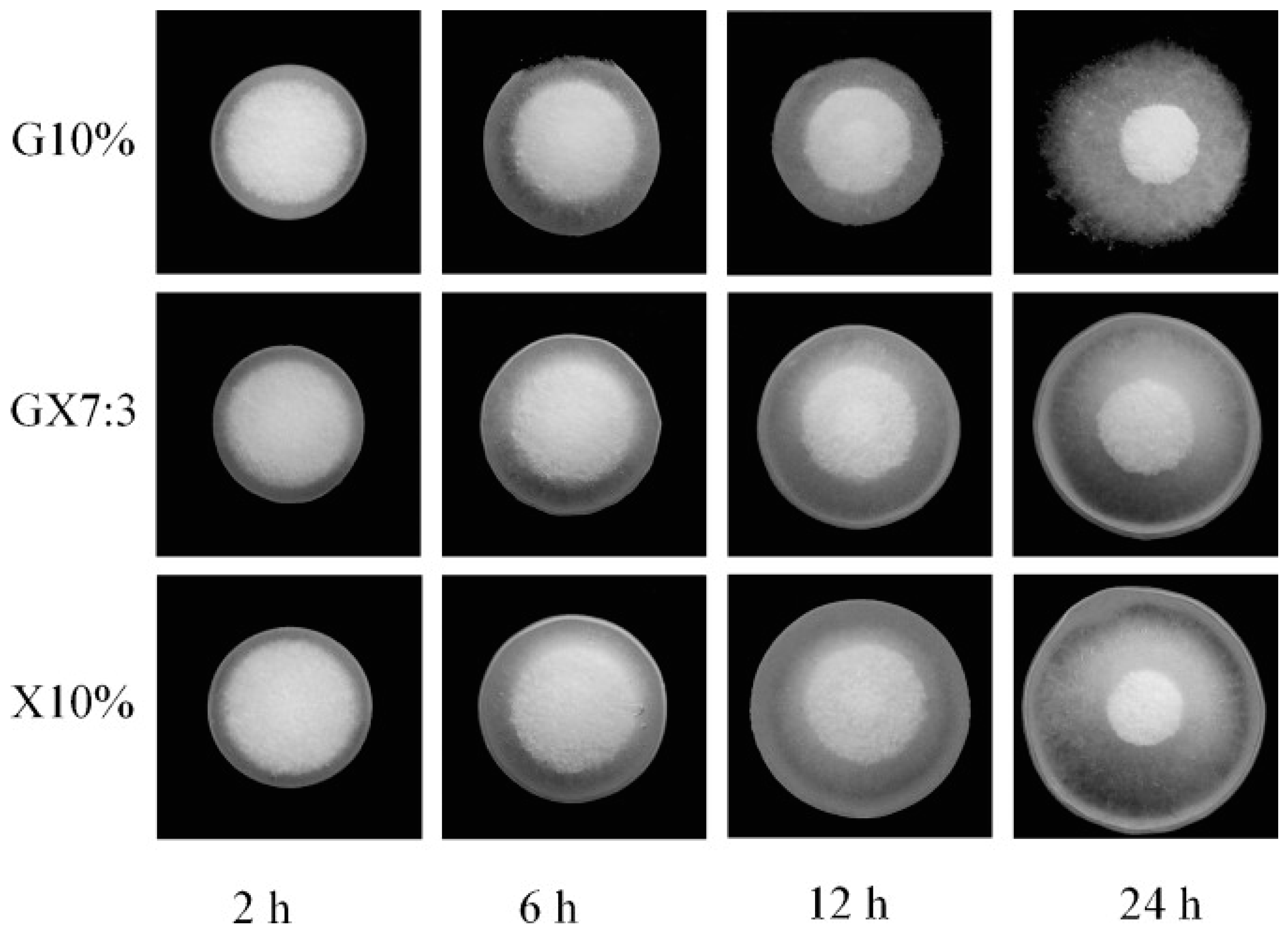
3.3. Colon-Specific Delivery Systems
3.4. Protein Delivery Systems
4. Conclusions and Future Prospects
Funding
Conflicts of Interest
References
- Ferreira, D.d.S.; de Souza Costa, L.A.; Campos, M.I.; Bispo, M.D.; Krause, L.C.; Hernández Macedo, M.L.; Lopez, J.A. Production of xanthan gum from soybean biodiesel: A preliminary study. BMC Proc. 2014, 8 (Suppl. 4), P174. [Google Scholar] [CrossRef]
- Bhat, I.M.; Wani, S.M.; Mir, S.A.; Masoodi, F.A. Advances in xanthan gum production, modifications and its applications. Biocatal. Agric. Biotechnol. 2022, 42, 102328. [Google Scholar] [CrossRef]
- Morris, E. Ordered conformation of xanthan in solutions and “weak gels”: Single helix, double helix—Or both? Food Hydrocoll. 2017, 86, 18–25. [Google Scholar] [CrossRef]
- Petri, D.F.S. Xanthan gum: A versatile biopolymer for biomedical and technological applications. J. Appl. Polym. Sci. 2015, 132, 42035. [Google Scholar] [CrossRef]
- Palaniraj, A.; Jayaraman, V. Production, recovery and applications of xanthan gum by Xanthomonas campestris. J. Food Eng. 2011, 106, 1–12. [Google Scholar] [CrossRef]
- García-Ochoa, F.; Santos, V.E.; Casas, J.A.; Gómez, E. Xanthan gum: Production, recovery, and properties. Biotechnol. Adv. 2000, 18, 549–579. [Google Scholar] [CrossRef]
- Dzionek, A.; Wojcieszyńska, D.; Guzik, U. Use of xanthan gum for whole cell immobilization and its impact in bioremediation—A review. Bioresour. Technol. 2022, 351, 126918. [Google Scholar] [CrossRef]
- Kuppuswami, G.M. FERMENTATION (INDUSTRIAL)|Production of Xanthan Gum. In Encyclopedia of Food Microbiology, 2nd ed.; Batt, C.A., Tortorello, M.L., Eds.; Academic Press: Oxford, UK, 2014; pp. 816–821. [Google Scholar]
- Lazzari, A.; Kleinebudde, P.; Knop, K. Xanthan gum as a rate-controlling polymer for the development of alcohol resistant matrix tablets and mini-tablets. Int. J. Pharm. 2018, 536, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Kar, R.; Mohapatra, S.; Bhanja, S.; Das, D.; Barik, B. Formulation and In Vitro Characterization of Xanthan Gum-Based Sustained Release Matrix Tables of Isosorbide-5-Mononitrate. Iran. J. Pharm. Res. 2010, 9, 13–19. [Google Scholar]
- Talukdar, M.M.; Van den Mooter, G.; Augustijns, P.; Tjandra-Maga, T.; Verbeke, N.; Kinget, R. In vivo evaluation of xanthan gum as a potential excipient for oral controlled-release matrix tablet formulation. Int. J. Pharm. 1998, 169, 105–113. [Google Scholar] [CrossRef]
- El-Gazayerly, O.N. Release of pentoxifylline from xanthan gum matrix tablets. Drug Dev. Ind. Pharm. 2003, 29, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Abu Fara, D.; Dadou, S.M.; Rashid, I.; Al-Obeidi, R.; Antonijevic, M.D.; Chowdhry, B.Z.; Badwan, A. A Direct Compression Matrix Made from Xanthan Gum and Low Molecular Weight Chitosan Designed to Improve Compressibility in Controlled Release Tablets. Pharmaceutics 2019, 11, 603. [Google Scholar] [CrossRef] [PubMed]
- Zeng, W.M. Oral controlled release formulation for highly water-soluble drugs: Drug--sodium alginate--xanthan gum--zinc acetate matrix. Drug Dev. Ind. Pharm. 2004, 30, 491–495. [Google Scholar] [CrossRef]
- Patel, V.F.; Patel, N.M. Statistical evaluation of influence of xanthan gum and guar gum blends on dipyridamole release from floating matrix tablets. Drug Dev. Ind. Pharm. 2007, 33, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Wang, K.; Liu, M.; He, Z. In vitro evaluations of konjac glucomannan and xanthan gum mixture as the sustained release material of matrix tablet. Carbohydr. Polym. 2008, 73, 241–247. [Google Scholar] [CrossRef]
- EFSA Panel on Food Additives and Nutrient Sources added to Food (ANS); Mortensen, A.; Aguilar, F.; Crebelli, R.; Di Domenico, A.; Frutos, M.J.; Galtier, P.; Gott, D.; Gundert-Remy, U.; Lambré, C.; et al. Re-evaluation of xanthan gum (E 415) as a food additive. EFSA J. 2017, 15, e04909. [Google Scholar] [PubMed]
- Abu Elella, M.H.; Sabaa, M.; Hanna, D.H.; Abdel-Aziz, M.M.; Mohamed, R.R. Antimicrobial pH-sensitive protein carrier based on modified xanthan gum. J. Drug Deliv. Sci. Technol. 2020, 57, 101673. [Google Scholar] [CrossRef]
- Ng, J.Y.; Obuobi, S.; Chua, M.L.; Zhang, C.; Hong, S.; Kumar, Y.; Gokhale, R.; Ee, P.L.R. Biomimicry of microbial polysaccharide hydrogels for tissue engineering and regenerative medicine—A review. Carbohydr. Polym. 2020, 241, 116345. [Google Scholar] [CrossRef]
- Li, R.; Feke, D.L. Rheological and kinetic study of the ultrasonic degradation of locust bean gum in aqueous saline and salt-free solutions. Ultrason. Sonochem. 2015, 27, 334–338. [Google Scholar] [CrossRef]
- Casas, J.A.; Santos, V.E.; García-Ochoa, F. Xanthan gum production under several operational conditions: Molecular structure and rheological properties☆. Enzym. Microb. Technol. 2000, 26, 282–291. [Google Scholar] [CrossRef]
- Carvalho, L.T.; Vieira, T.A.; Zhao, Y.; Celli, A.; Medeiros, S.F.; Lacerda, T.M. Recent advances in the production of biomedical systems based on polyhydroxyalkanoates and exopolysaccharides. Int. J. Biol. Macromol. 2021, 183, 1514–1539. [Google Scholar] [CrossRef] [PubMed]
- Maji, B.; Maiti, S. Chemical modification of xanthan gum through graft copolymerization: Tailored properties and potential applications in drug delivery and wastewater treatment. Carbohydr. Polym. 2021, 251, 117095. [Google Scholar] [CrossRef] [PubMed]
- Abu Elella, M. Synthesis and Potential Applications of Modified Xanthan Gum. J. Chem. Eng. Res. Updates 2021, 8, 73–97. [Google Scholar] [CrossRef]
- Moorhouse, R.; Walkinshaw, M.D.; Arnott, S. Xanthan Gum—Molecular Conformation and Interactions. In Extracellular Microbial Polysaccharides; American Chemical Society: Washington, DC, USA, 1977; Volume 45, pp. 90–102. [Google Scholar]
- Brunchi, C.-E.; Bercea, M.; Morariu, S.; Dascalu, M. Some properties of xanthan gum in aqueous solutions: Effect of temperature and pH. J. Polym. Res. 2016, 23, 123. [Google Scholar] [CrossRef]
- Martins, D.; Dourado, F.; Gama, M. Effect of ionic strength, pH and temperature on the behaviour of re-dispersed BC:CMC—A comparative study with xanthan gum. Food Hydrocoll. 2023, 135, 108163. [Google Scholar] [CrossRef]
- Valente, É.C.; Polêto, M.D.; de Oliveira, T.V.; Soares, L.d.S.; dos Reis Coimbra, J.S.; Guimarães, A.P.; de Oliveira, E.B. Effects of the Cations Li+, Na+, K+, Mg2+, or Ca2+ on Physicochemical Properties of Xanthan Gum in Aqueous Medium—A view from Computational Molecular Dynamics Calculations. Food Biophys. 2023, 18, 32–47. [Google Scholar] [CrossRef]
- Nsengiyumva, E.M.; Heitz, M.P.; Alexandridis, P. Thermal hysteresis phenomena in aqueous xanthan gum solutions. Food Hydrocoll. 2023, 144, 108973. [Google Scholar] [CrossRef]
- Nishinari, K.; Doi, E. Food Hydrocolloids: Structures, Properties, and Functions; Springer Science & Business Media: New York, NY, USA, 2012. [Google Scholar]
- Nsengiyumva, E.M.; Heitz, M.P.; Alexandridis, P. Salt and Temperature Effects on Xanthan Gum Polysaccharide in Aqueous Solutions. Int. J. Mol. Sci. 2024, 25, 490. [Google Scholar] [CrossRef] [PubMed]
- Bejenariu, A.; Popa, M.; Picton, L.; Le Cerf, D. Effect of concentration, pH and temperature on xanthan conformation: A preliminary study before cross-linking. Rev. Roum. Chim. 2010, 55, 147–152. [Google Scholar]
- Bueno, V.B.; Petri, D.F.S. Xanthan hydrogel films: Molecular conformation, charge density and protein carriers. Carbohydr. Polym. 2014, 101, 897–904. [Google Scholar] [CrossRef]
- Han, G.Y.; Ling, P.X.; Wang, F.; Wang, G.L.; Shao, H.R. Safety of intra-articular injection of xanthan gum into knee joint of rabbit. Chin. J. Biochem. Pharm. 2012, 33, 109–112. [Google Scholar]
- Le, X.T.; Turgeon, S.L. Rheological and structural study of electrostatic cross-linked xanthan gum hydrogels induced by [small beta]-lactoglobulin. Soft Matter 2013, 9, 3063–3073. [Google Scholar] [CrossRef]
- Roy, A.; Comesse, S.; Grisel, M.; Hucher, N.; Souguir, Z.; Renou, F. Hydrophobically modified xanthan: An amphiphilic but not associative polymer. Biomacromolecules 2014, 15, 1160–1170. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, D.N.; Meyyanathan, S.N.; Shanmugam, R.; Zielinska, A.; Campos, J.R.; Ferreira, J.D.; Souto, E.B. Development, in vitro release and in vivo bioavailability of sustained release nateglinide tablets. J. Drug Deliv. Sci. Technol. 2020, 55, 101355. [Google Scholar] [CrossRef]
- Lu, M.F.; Woodward, L.; Borodkin, S. Xanthan Gum and Alginate Based Controlled Release Theophylline Formulations. Drug Dev. Ind. Pharm. 1991, 17, 1987–2004. [Google Scholar] [CrossRef]
- Billa, N.; Yuen, K.H.; Khader, M.A.; Omar, A. Gamma-scintigraphic study of the gastrointestinal transit and in vivo dissolution of a controlled release diclofenac sodium formulation in xanthan gum matrices. Int. J. Pharm. 2000, 201, 109–120. [Google Scholar] [CrossRef]
- Gohel, M.C.; Bariya, S.H. Fabrication of triple-layer matrix tablets of venlafaxine hydrochloride using xanthan gum. AAPS PharmSciTech 2009, 10, 624–630. [Google Scholar] [CrossRef][Green Version]
- Mughal, M.A.; Iqbal, Z.; Neau, S.H. Guar gum, xanthan gum, and HPMC can define release mechanisms and sustain release of propranolol hydrochloride. AAPS PharmSciTech 2011, 12, 77–87. [Google Scholar] [CrossRef]
- Salamanca, C.H.; Yarce, C.J.; Moreno, R.A.; Prieto, V.; Recalde, J. Natural gum-type biopolymers as potential modified nonpolar drug release systems. Carbohydr. Polym. 2018, 189, 31–38. [Google Scholar] [CrossRef]
- Kumar, A.; Singh, K.; Ahuja, M. Xanthan-g-poly(acrylamide): Microwave-assisted synthesis, characterization and in vitro release behavior. Carbohydr. Polym. 2009, 76, 261–267. [Google Scholar] [CrossRef]
- Patel, J.; Maiti, S.; Moorthy, N.S.H.N. Repaglinide-laden hydrogel particles of xanthan gum derivatives for the management of diabetes. Carbohydr. Polym. 2022, 287, 119354. [Google Scholar] [CrossRef] [PubMed]
- Gohel, M.C.; Parikh, R.K.; Nagori, S.A.; Jena, D.G. Fabrication of Modified Release Tablet Formulation of Metoprolol Succinate using Hydroxypropyl Methylcellulose and Xanthan Gum. AAPS PharmSciTech 2009, 10, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Merlusca, I.P.; Plamadeala, P.; Girbea, C.; Popa, I.M. Xanthan-chitosan complex as a potential protector against injurious effects of neomycin. Cellul. Chem. Technol. 2016, 50, 577–583. [Google Scholar]
- Dumitriu, S.; Aelenei, N.; Popa, I.M.; Dumitriu, M.; Dumitriu, D. Bioactive polymers. 70. The kinetics of controlled release of neomycin in an alkaline medium. Farmaco 1992, 47, 509–518. [Google Scholar] [PubMed]
- Ćirić, A.; Medarević, Đ.; Čalija, B.; Dobričić, V.; Mitrić, M.; Djekic, L. Study of chitosan/xanthan gum polyelectrolyte complexes formation, solid state and influence on ibuprofen release kinetics. Int. J. Biol. Macromol. 2020, 148, 942–955. [Google Scholar] [CrossRef] [PubMed]
- Ćirić, A.; Medarević, Đ.; Čalija, B.; Dobričić, V.; Rmandić, M.; Barudžija, T.; Malenović, A.; Djekic, L. Effect of ibuprofen entrapment procedure on physicochemical and controlled drug release performances of chitosan/xanthan gum polyelectrolyte complexes. Int. J. Biol. Macromol. 2021, 167, 547–558. [Google Scholar] [CrossRef]
- Jian, H.; Zhu, L.; Zhang, W.; Sun, D.; Jiang, J. Galactomannan (from Gleditsia sinensis Lam.) and xanthan gum matrix tablets for controlled delivery of theophylline: In vitro drug release and swelling behavior. Carbohydr. Polym. 2012, 87, 2176–2182. [Google Scholar] [CrossRef]
- Kumar, A.; Deepak; Sharma, S.; Srivastava, A.; Kumar, R. Synthesis of xanthan gum graft copolymer and its application for controlled release of highly water soluble Levofloxacin drug in aqueous medium. Carbohydr. Polym. 2017, 171, 211–219. [Google Scholar] [CrossRef]
- Laffleur, F.; Michalek, M. Modified xanthan gum for buccal delivery—A promising approach in treating sialorrhea. Int. J. Biol. Macromol. 2017, 102, 1250–1256. [Google Scholar] [CrossRef]
- Murtale, S.A.; Goudanavar, P.; Acharya, A.; Lokapur, J. Formulation Development of Sustain Release Tablets of Lornoxicam using Chemically Modified Xanthan Gum. Int. J. Pharm. Investig. 2022, 12, 191–198. [Google Scholar] [CrossRef]
- Hanna, D.H.; Saad, G.R. Encapsulation of ciprofloxacin within modified xanthan gum- chitosan based hydrogel for drug delivery. Bioorg. Chem. 2019, 84, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Sowmya, C.; Kumar, V.L.; Adhikari, B. Optimization and Analysis of Xanthan Gum and Hypromellose Combined Matrices for Extended Release of Ranolazine Using Quality by Design. Int. J. Pharm. Investig. 2022, 12, 87–89. [Google Scholar] [CrossRef]
- Shekarforoush, E.; Ajalloueian, F.; Zeng, G.; Mendes, A.C.; Chronakis, I.S. Electrospun xanthan gum-chitosan nanofibers as delivery carrier of hydrophobic bioactives. Mater. Lett. 2018, 228, 322–326. [Google Scholar] [CrossRef]
- Subhash Chandra Bose, P.; Srikanth Reddy, P.; Ravi, V.; Sarita, D.; Kumar, P. Formulation and evaluation of sustained release floating tablets of diltiazem HCl using xanthan gum. Int. J. Pharma Sci. 2011, 2, 319–328. [Google Scholar]
- Jagdale, S.C.; Pawar, C.R. Application of Design of Experiment for Polyox and Xanthan Gum Coated Floating Pulsatile Delivery of Sumatriptan Succinate in Migraine Treatment. BioMed Res. Int. 2014, 2014, 547212. [Google Scholar] [CrossRef]
- Shiledar, R.R.; Tagalpallewar, A.A.; Kokare, C.R. Formulation and in vitro evaluation of xanthan gum-based bilayered mucoadhesive buccal patches of zolmitriptan. Carbohydr. Polym. 2014, 101, 1234–1242. [Google Scholar] [CrossRef] [PubMed]
- Jadav, M.; Pooja, D.; Adams, D.J.; Kulhari, H. Advances in Xanthan Gum-Based Systems for the Delivery of Therapeutic Agents. Pharmaceutics 2023, 15, 402. [Google Scholar] [CrossRef]
- El-Zahaby, S.A.; Kassem, A.A.; El-Kamel, A.H. Formulation and in vitro evaluation of size expanding gastro-retentive systems of levofloxacin hemihydrate. Int. J. Pharm. 2014, 464, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, M.M.; Sharaf, R.R.; Aziz, R.K. Helicobacter pylori: A poor man’s gut pathogen? Gut Pathog. 2010, 2, 2. [Google Scholar] [CrossRef]
- Gisbert, J.P.; Pajares, J.M. Treatment of Helicobacter pylori infection: The past and the future. Eur. J. Intern. Med. 2010, 21, 357–359. [Google Scholar] [CrossRef]
- Bronner, F.; Pansu, D.; Stein, W.D. An analysis of intestinal calcium transport across the rat intestine. Am. J. Physiol. Liver Physiol. 1986, 250, G561–G569. [Google Scholar] [CrossRef] [PubMed]
- Moganti, M.; Shivakumar, H.N. Oral raft forming in situ gelling system for site specific delivery of calcium. J. Drug Deliv. Sci. Technol. 2021, 61, 102113. [Google Scholar] [CrossRef]
- Cho, J.; Na, J.; Bae, E.; Lee, T.W.; Jang, H.N.; Cho, H.S.; Chang, S.-H.; Park, D.J. The incidence, risk factors, and clinical outcomes of rhabdomyolysis associated with fenoverine prescription: A retrospective study in South Korea (1999–2014). BMC Pharmacol. Toxicol. 2020, 21, 30. [Google Scholar] [CrossRef] [PubMed]
- Rashmitha, V.; Madhusudan, R.; Pavani, S.J. Formulation and evaluation of fenoverine floating tablets. Asian J. Pharm. Clin. Res. 2021, 14, 175–180. [Google Scholar]
- Srinivasan, A.V. Propranolol: A 50-Year Historical Perspective. Ann. Indian Acad. Neurol. 2019, 22, 21–26. [Google Scholar] [CrossRef]
- Lavanya, M.; Chinna Eswaraiah, M.; Jaya, S. Design, Development and in-Vitro Characterization of Floating Tablets of Pro-pranolol Hydrochloride. Res. J. Pharm. Technol. 2020, 13, 5088–5094. [Google Scholar]
- Goh, K.L.; Choi, M.G.; Hsu, P.I.; Chun, H.J.; Mahachai, V.; Kachintorn, U.; Leelakusolvong, S.; Kim, N.; Rani, A.A.; Wong, B.C.Y.; et al. Pharmacological and Safety Profile of Dexlansoprazole: A New Proton Pump Inhibitor—Implications for Treatment of Gastroesophageal Reflux Disease in the Asia Pacific Region. J. Neurogastroenterol. Motil. 2016, 22, 355–366. [Google Scholar] [CrossRef]
- Wittbrodt, E.T.; Baum, C.; Peura, D.A. Delayed release dexlansoprazole in the treatment of GERD and erosive esophagitis. Clin. Exp. Gastroenterol. 2009, 2, 117–128. [Google Scholar]
- Sontale, R.; Koshta, A.; Muley, P.; Malviya, S.; Kharia, A. Formulation and Evaluation of Dexlansoprazole Floating Tablets. Int. J. Pharm. Life Sci. 2020, 11, 6467. [Google Scholar]
- Gangane, P.S.; Pachpute, T.; Mahapatra, D.K.; Mahajan, N.M. HPMC Polymers and Xanthan Gum Assisted Development and Characterization of Stavudine Extended Release Floating Tablets. Indian J. Pharm. Educ. Res. 2021, 55, S681–S692. [Google Scholar] [CrossRef]
- Shailaja, T.; Ramachandra, S.; Kishore, C.; Bhushan, Y.S.; Lakshmi, P. Formulation and In Vitro Evaluation of Gastro Retentive Delivery of Diltiazem Hydrochloride Using Natural Polymers. Int. J. Pharma Sci. 2013, 3, 129–135. [Google Scholar]
- Sivaneswari, S.; Karthikeyan, E.; Chandana, P.J. Novel expandable gastro retentive system by unfolding mechanism of levetiracetam using simple lattice design—Formulation optimization and in vitro evaluation. Bull. Fac. Pharm. Cairo Univ. 2017, 55, 63–72. [Google Scholar] [CrossRef]
- Jafar, M.; Mohsin, A.A.; Khalid, M.S.; Alshahrani, A.M.; Alkhateeb, F.S.; Alqarni, A.S. Ranitidine hydrochloride stomach specific bouyant microsponge: Preparation, in-vitro characterization, and in-vivo anti-ulcer activity. J. Drug Deliv. Sci. Technol. 2020, 55, 101453. [Google Scholar] [CrossRef]
- Yilma, Z.; Belete, A.; Gebre-Mariam, T. Research, Formulation and optimization of sustained release floating matrix tablets of salbutamol sulphate using xanthan gum and hydroxypropyl methylcellulose polymer blend. Int. J. Pharm. Sci. Res. 2015, 6, 1877. [Google Scholar]
- Dey, S.; Mazumder, B.; Chattopadhyay, S.; Das, M.K.; Sinha, S.; Ganguly, S.; De, K.; Mishra, M. Polymers derived from Xanthomonas campesteris and Cyamopsis tetragonolobus used as retardant materials for the formulation of sustained release floating matrix tablet of atenolol. Int. J. Biol. Macromol. 2014, 65, 346–356. [Google Scholar] [CrossRef]
- Kulkarni, N.; Wakte, P.; Naik, J. Development of floating chitosan-xanthan beads for oral controlled release of glipizide. Int. J. Pharm. Investig. 2015, 5, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Wadher, K.J.; Bute, S.W.; Milind, J.U. Formulation and Evaluation of Gastroretantive Floating Tablet using Carbopol with Xanthan Gum and Guar Gum. Int. J. ChemTech Res. 2017, 10, 300–308. [Google Scholar]
- Badhan, A.C.; Mashru, R.C.; Shah, P.P.; Thakkar, A.R.; Dobaria, N.B. Development and Evaluation of Sustained Release Gastroretentive Minimatrices for Effective Treatment of H. pylori Infection. AAPS PharmSciTech 2009, 10, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Bajracharya, R.; Min, J.Y.; Han, J.-W.; Park, B.J.; Han, H.-K. Strategic Approaches for Colon Targeted Drug Delivery: An Overview of Recent Advancements. Pharmaceutics 2020, 12, 68. [Google Scholar] [CrossRef]
- Sinha, V.R.; Kumria, R. Microbially triggered drug delivery to the colon. Eur. J. Pharm. Sci. 2003, 18, 3–18. [Google Scholar] [CrossRef]
- McClements, D.J. Food hydrocolloids: Application as functional ingredients to control lipid digestion and bioavailability. Food Hydrocoll. 2021, 111, 106404. [Google Scholar] [CrossRef]
- Kinget, R.; Kalala, W.; Vervoort, L.; Van den Mooter, G. Colonic drug targeting. J. Drug Target. 1998, 6, 129–149. [Google Scholar] [CrossRef] [PubMed]
- Scheline, R.R. Metabolism of foreign compounds by gastrointestinal microorganisms. Pharmacol. Rev. 1973, 25, 451–523. [Google Scholar]
- Sinha, V.R.; Mittal, B.R.; Bhutani, K.K.; Kumria, R. Colonic drug delivery of 5-fluorouracil: An in vitro evaluation. Int. J. Pharm. 2004, 269, 101–108. [Google Scholar] [CrossRef]
- Sinha, V.R.; Singh, A.; Singh, S.; Bhinge, J.R. Compression coated systems for colonic delivery of 5-fluorouracil. J. Pharm. Pharmacol. 2007, 59, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Chu, J.S.; Fix, J.A. Colon-specific drug delivery: New approaches and in vitro/in vivo evaluation. Int. J. Pharm. 2002, 235, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ibekwe, V.; Khela, M.; Evans, D.; Basit, A. A new concept in colonic drug targeting: A combined pH-responsive and bacterially-triggered drug delivery technology. Aliment. Pharmacol. Ther. 2008, 28, 911–916. [Google Scholar] [CrossRef]
- Mutalik, S.; Suthar, N.A.; Managuli, R.S.; Shetty, P.K.; Avadhani, K.; Kalthur, G.; Kulkarni, R.V.; Thomas, R. Development and performance evaluation of novel nanoparticles of a grafted copolymer loaded with curcumin. Int. J. Biol. Macromol. 2016, 86, 709–720. [Google Scholar] [CrossRef] [PubMed]
- Ham, M.; Moss, A.C. Mesalamine in the treatment and maintenance of remission of ulcerative colitis. Expert Rev. Clin. Pharmacol. 2012, 5, 113–123. [Google Scholar] [CrossRef]
- Deltenre, P.; Berson, A.; Marcellin, P.; Degott, C.; Biour, M.; Pessayre, D.J. Mesalazine (5-aminosalicylic acid) induced chronic hepatitis. Gut 1999, 44, 886–888. [Google Scholar] [CrossRef]
- Ransford, R.; Langman, M.J. Sulphasalazine and mesalazine: Serious adverse reactions re-evaluated on the basis of suspected adverse reaction reports to the Committee on Safety of Medicines. Gut 2002, 51, 536–539. [Google Scholar] [CrossRef] [PubMed]
- Perez-Colon, E.; Dadlani, G.H.; Wilmot, I.; Miller, M. Mesalamine-induced myocarditis and coronary vasculitis in a pediatric ulcerative colitis patient: A case report. Case Rep. Pediatr. 2011, 2011, 524364. [Google Scholar] [CrossRef] [PubMed]
- Kaur, R.; Gulati, M.; Singh, S.K. Role of synbiotics in polysaccharide assisted colon targeted microspheres of mesalamine for the treatment of ulcerative colitis. Int. J. Biol. Macromol. 2017, 95, 438–450. [Google Scholar] [CrossRef] [PubMed]
- Asghar, L.F.A.; Chure, C.B.; Chandran, S. Colon Specific Delivery of Indomethacin: Effect of Incorporating pH Sensitive Polymers in Xanthan Gum Matrix Bases. AAPS PharmSciTech 2009, 10, 418–429. [Google Scholar] [CrossRef] [PubMed]
- Trombino, S.; Serini, S.; Cassano, R.; Calviello, G. Xanthan gum-based materials for omega-3 PUFA delivery: Preparation, characterization and antineoplastic activity evaluation. Carbohydr. Polym. 2019, 208, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S.; Saruchi; Kaith, B.S.; Kaur, M.; Sharma, N.; Kumar, V. Cross-linked xanthan gum–starch hydrogels as promising materials for controlled drug delivery. Cellulose 2020, 27, 4565–4589. [Google Scholar] [CrossRef]
- Niranjan, K.; Shivapooja, A.; Muthyala, J.; Pinakin, P.J.A. Effect of guar gum and xanthan gum compression coating on release studies of metronidazole in human fecal media for colon targeted drug delivery systems. Asian J. Pharm. Clin. Res. 2013, 6, 315–318. [Google Scholar]
- Caddeo, C.; Nácher, A.; Díez-Sales, O.; Merino-Sanjuán, M.; Fadda, A.M.; Manconi, M. Chitosan-xanthan gum microparticle-based oral tablet for colon-targeted and sustained delivery of quercetin. J. Microencapsul. 2014, 31, 694–699. [Google Scholar] [CrossRef]
- Alvarez-Manceñido, F.; Landin, M.; Martínez-Pacheco, R. Konjac glucomannan/xanthan gum enzyme sensitive binary mixtures for colonic drug delivery. Eur. J. Pharm. Biopharm. 2008, 69, 573–581. [Google Scholar] [CrossRef]
- Sridhar, B.K.; Srinatha, A.; Zaman, B.B.; Ragunandan, H. Development and evaluation of microbial degradation dependent compression coated secnidazole tablets for colonic delivery. Indian J. Pharm. Sci. 2011, 73, 641–648. [Google Scholar]
- You, Y.C.; Dong, L.Y.; Dong, K.; Xu, W.; Yan, Y.; Zhang, L.; Wang, K.; Xing, F.J. In vitro and in vivo application of pH-sensitive colon-targeting polysaccharide hydrogel used for ulcerative colitis therapy. Carbohydr. Polym. 2015, 130, 243–253. [Google Scholar] [CrossRef] [PubMed]
- Suhail, M.; Chiu, I.H.; Lai, Y.R.; Khan, A.; Al-Sowayan, N.S.; Ullah, H.; Wu, P.C. Xanthan-Gum/Pluronic-F-127-Based-Drug-Loaded Polymeric Hydrogels Synthesized by Free Radical Polymerization Technique for Management of Attention-Deficit/Hyperactivity Disorder. Gels 2023, 9, 640. [Google Scholar] [CrossRef] [PubMed]
- Mushtaq, R.Y.; Naveen, N.R.; Tiyyagura, P.; Hosny, K.M.; Alahmadi, A.A.; Majrashi, M.A.; Mamidipalli, N.R.; Safhi, A.Y.; Alissa, M.; Sabei, F.Y.; et al. Development, optimization and in-vivo pharmacokinetic evaluation of flubiprofen nanocrystal tablets for efficient chronotherapy against rheumatoid arthritis. J. Drug Deliv. Sci. Technol. 2024, 91, 105240. [Google Scholar] [CrossRef]
- Araújo, F.; Fonte, P.; Santos, H.A.; Sarmento, B.J. Oral delivery of glucagon-like peptide-1 and analogs: Alternatives for diabetes control? J. Diabetes Sci. Technol. 2012, 6, 1486–1497. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Gong, L.; Zhang, R.; Li, S.; Yu, H.; Liu, Y.; Xue, Y.; Huang, D.; Xu, N.; Wang, Y.; et al. Fibroblast growth factor 21 inhibited inflammation and fibrosis after myocardial infarction via EGR1. Eur. J. Pharmacol. 2021, 910, 174470. [Google Scholar] [CrossRef]
- Verma, S.; Goand, U.K.; Husain, A.; Katekar, R.A.; Garg, R.; Gayen, J.R. Challenges of peptide and protein drug delivery by oral route: Current strategies to improve the bioavailability. Drug Dev. Res. 2021, 82, 927–944. [Google Scholar] [CrossRef]
- Zhu, Q.; Chen, Z.; Paul, P.K.; Lu, Y.; Wu, W.; Qi, J. Oral delivery of proteins and peptides: Challenges, status quo and future perspectives. Acta Pharm. Sin. B 2021, 11, 2416–2448. [Google Scholar] [CrossRef]
- Maiti, S.; Ray, S.; Mandal, B.; Sarkar, S.; Sa, B. Carboxymethyl xanthan microparticles as a carrier for protein delivery. J. Microencapsul. 2007, 24, 743–756. [Google Scholar] [CrossRef]
- Sabaa, M.W.; Hanna, D.H.; Abu Elella, M.H.; Mohamed, R.R. Encapsulation of bovine serum albumin within novel xanthan gum based hydrogel for protein delivery. Mater. Sci. Eng. C 2019, 94, 1044–1055. [Google Scholar] [CrossRef]
- Song, X.; Chen, Y.; Sun, H.; Liu, X.; Leng, X. Physicochemical and functional properties of chitosan-stabilized selenium nanoparticles under different processing treatments. Food Chem. 2020, 331, 127378. [Google Scholar] [CrossRef]
- Zhu, Y.; Sun, X.; Luo, X.; Ding, J.; Fan, F.; Li, P.; Shen, X.; Fang, Y. Encapsulation of selenium-containing peptides in xanthan gum-lysozyme nanoparticles as a powerful gastrointestinal delivery system. Food Res. Int. 2022, 156, 111351. [Google Scholar] [CrossRef] [PubMed]
- Casadidio, C.; Mayol, L.; Biondi, M.; Scuri, S.; Cortese, M.; Hennink, W.E.; Vermonden, T.; De Rosa, G.; Di Martino, P.; Censi, R. Anionic polysaccharides for stabilization and sustained release of antimicrobial peptides. Int. J. Pharm. 2023, 636, 122798. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Piñeiro, I.; Alvarez-Trabado, J.; Márquez, J.; Badiola, I.; Sanchez, A. Xanthan gum-functionalised span nanoparticles for gene targeting to endothelial cells. Colloids Surf. B Biointerfaces 2018, 170, 411–420. [Google Scholar] [CrossRef] [PubMed]



| Appearance | Off-white to pale yellow, free-flowing powder |
| Melting point | 64.43 °C |
| Moisture content | 8–15% |
| Ash | 7–12% |
| Solubility | Highly soluble in both cold and hot water, practically insoluble in organic solvents |
| Viscosity | 13–35 cP (1 g/L solution at 25 °C) |
| pH | 6.0 to 8.0 for a 10 g/L solution |
| LogP | 3.926 (estimated) |
| Polymer Matrix | Formulation Type | Formulation Composition | Drug | Key Features | Reference |
|---|---|---|---|---|---|
| XG | Matrix tablet | 20, 40, and 60% w/w | Propranolol hydrochloride |
| [41] |
| XG (Mn of 2000 KDa–16,000 KDa) | Tablet | 0, 25 and 40% w/w | Quetiapine fumarate |
| [42] |
| XG (1% aqueous solution viscosity of 1350 cps at 25 °C) | Matrix tablet | 14.2%, 19%, 23.8%, 28.57%, 33.3%, and 38% w/w | Isosorbide-5-mononitrate |
| [10] |
| XG | Matrix tablet | 3.4, 6, 12.1, 17.2, and 29.3% w/w | Pentoxifylline |
| [12] |
| XG-graft-poly (N-vinyl-2-pyrrolidone) (XG-g-PNVP) | Microbead | Polymer to drug ratio 10:1 | Levofloxacin |
| [51] |
| Thiolated XG | Disc | Polymer to drug ratio 2:1 | Tannic acid |
| [52] |
| Thiolated XG | Matrix tablet | 14.1, 17.5, and 20.8% w/w | Lornoxicam |
| [53] |
| N-trimethyl chitosan/CMXG (1:1 weight ratio) | Hydrogel | Drug to hydrogel ratio ranging from 0.44:99.56 to 3.52:96.48 | Ciprofloxacin |
| [54] |
| Galactomannan/XG (0:10, 3:7, 5:5, 7:3, and 10:0 weight ratios) | Matrix tablet | 10% w/w | Theophylline |
| [50] |
| XG/HPMC | Matrix tablet | Combination of XG (10–20% w/w) and HPMC (2.75–4.25% w/w) | Ranolazine |
| [55] |
| XG (Mw about 2000 kDa)/chitosan (Mw 28 kD, degree of deacetylation of 89%) | Nanofiber | Electrospun solution consists of XG (0.75% w/v), chitosan (3% w/v), and curcumin (2% w/v) | Curcumin |
| [56] |
| Polymer Matrix | Formulation Type | Drug | Key Features | Reference |
|---|---|---|---|---|
| XG, HPMC K15, and HPMC K100M | Floating matrix tablet | Stavudine |
| [73] |
| XG | Floating tablets | Diltiazem hydrochloride |
| [74] |
| Carbopol 934P/XG | Mucoadhesive patch | Levetiracetam |
| [75] |
| Eudragit/XG | Buoyant microsponge | Ranitidine hydrochloride |
| [76] |
| XG/HPMC | Floating matrix tablet | Salbutamol sulphate |
| [77] |
| XG/guar gum | Floating matrix tablet | Atenolol |
| [78] |
| Chitosan/XG | Floating beads | Glipizide |
| [79] |
| Carbopol 934/XG | Floating matrix tablet | Domperidone |
| [80] |
| XG/HPMC K100M CR/polyethylene oxide coagulant/carbopol 974P | Floating and gastric bioadhesive minimatrices | Amoxicillin |
| [81] |
| Polymer Matrix | Formulation Type | Drug | Key Features | Reference |
|---|---|---|---|---|
| XG | Microspheres | α-linolenic acid (ALA) |
| [98] |
| Cross-linked XG–starch | Hydrogel | Aspirin, paracetamol |
| [99] |
| XG/guar gum | Compression-coated tablets | Metronidazole |
| [100] |
| Chitosan/XG | Microparticle-based tablets | Quercetin |
| [101] |
| Konjac glucomannan/XG | Tablets | Diltiazem |
| [102] |
| Konjac glucomannan/XG | Matrix tablets | Cimetidine |
| [16] |
| XG/guar gum and XG/guar gum/chitosan | Compression-coated tablets | Secnidazole |
| [103] |
| Konjac gum, XG, and sodium alginate | Hydrogel | Hydrocortisone sodium succinate |
| [104] |
| XG/pluronic F-127 | Hydrogel | Atomoxetine HCl |
| [105] |
| CMXG/sodium alginate | Compression-coated tablets | Flurbiprofen |
| [106] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Layek, B. A Comprehensive Review of Xanthan Gum-Based Oral Drug Delivery Systems. Int. J. Mol. Sci. 2024, 25, 10143. https://doi.org/10.3390/ijms251810143
Layek B. A Comprehensive Review of Xanthan Gum-Based Oral Drug Delivery Systems. International Journal of Molecular Sciences. 2024; 25(18):10143. https://doi.org/10.3390/ijms251810143
Chicago/Turabian StyleLayek, Buddhadev. 2024. "A Comprehensive Review of Xanthan Gum-Based Oral Drug Delivery Systems" International Journal of Molecular Sciences 25, no. 18: 10143. https://doi.org/10.3390/ijms251810143
APA StyleLayek, B. (2024). A Comprehensive Review of Xanthan Gum-Based Oral Drug Delivery Systems. International Journal of Molecular Sciences, 25(18), 10143. https://doi.org/10.3390/ijms251810143






