The Effects of Growth Hormone Treatment Beyond Growth Promotion in Patients with Genetic Syndromes: A Systematic Review of the Literature
Abstract
1. Introduction
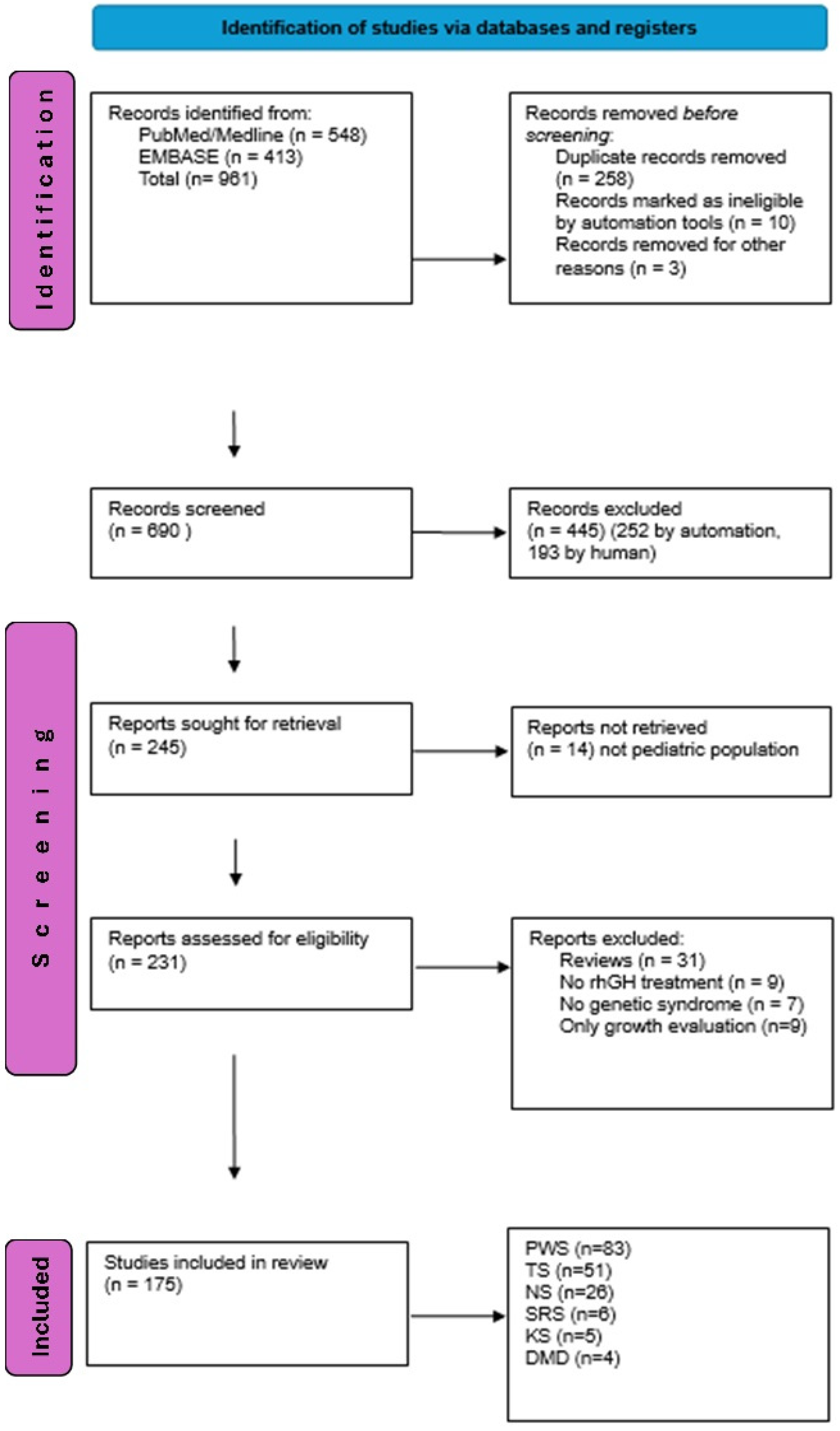
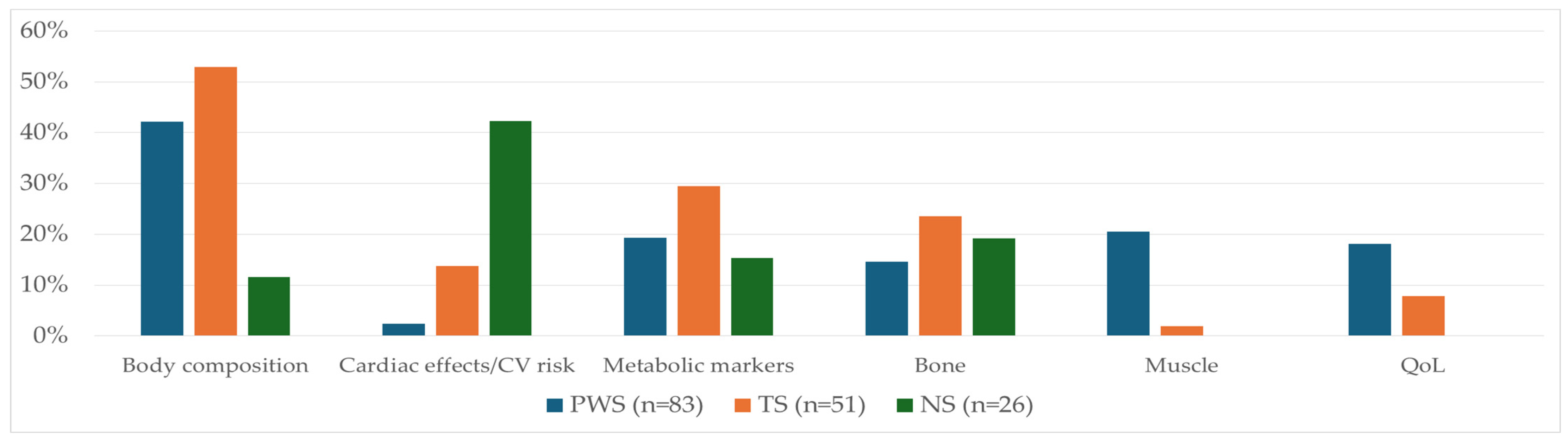
2. Material and Methods
3. The Results
4. Discussion: The Effects of rhGH Treatment beyond Growth Promotion in Genetic Syndromes
4.1. Prader–Willi Syndrome
4.2. Turner Syndrome
4.3. Noonan Syndrome
4.4. Silver–Russel Syndrome
4.5. Kabuki Syndrome
4.6. Duchenne Muscular Dystrophy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cassidy, S.B.; Schwartz, S.; Miller, J.L.; Driscoll, D.J. Prader-Willi syndrome. Genet. Med. 2012, 14, 10–26. [Google Scholar] [CrossRef] [PubMed]
- Kimonis, V.E.; Tamura, R.; Gold, J.A.; Patel, N.; Surampalli, A.; Manazir, J.; Miller, J.L.; Roof, E.; Dykens, E.; Butler, M.G.; et al. Early diagnosis in Prader-Willi syndrome reduces obesity and associated co-morbidities. Genes 2019, 10, 898. [Google Scholar] [CrossRef]
- Deal, C.L.; Tony, M.; Höybye, C.; Allen, D.B.; Tauber, M.; Christiansen, J.S.; 2011 Growth Hormone in Prader-Willi Syndrome Clinical Care Guidelines Workshop Participants. Growth Hormone Research Society workshop summary: Consensus guidelines for recombinant human growth hormone therapy in Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 2013, 98, E1072–E1087. [Google Scholar] [CrossRef] [PubMed]
- Gravholt, C.H.; Andersen, N.H.; Conway, G.S.; Dekkers, O.M.; Geffner, M.E.; Klein, K.O.; Lin, A.E.; Mauras, N.; Quigley, C.A.; Rubin, K.; et al. Clinical practice guidelines for the care of girls and women with Turner syndrome: Proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur. J. Endocrinol. 2017, 177, G1–G70. [Google Scholar] [CrossRef] [PubMed]
- Gravholt, C.H.; Viuff, M.; Just, J.; Sandahl, K.; Brun, S.; van der Velden, J.; Andersen, N.H.; Skakkebaek, A. The changing face of Turner syndrome. Endocr. Rev. 2023, 44, 33–69. [Google Scholar] [CrossRef]
- Al Shaikh, A.; Daftardar, H.; Alghamdi, A.A.; Jamjoom, M.; Awidah, S.; Ahmed, M.E.; Soliman, A.T. Effect of growth hormone treatment on children with idiopathic short stature (ISS), idiopathic growth hormone deficiency (IGHD), small for gestational age (SGA) and Turner syndrome (TS) in a tertiary care center. Acta Biomed. 2020, 91, 29–40. [Google Scholar]
- Backeljauw, P.; Kanumakala, S.; Loche, S.; Schwab, K.O.; Pfäffle, R.W.; Höybye, C.; Lundberg, E.; Battelino, T.; Kriström, B.; Giemza, T.; et al. Safety and Effectiveness of Recombinant Human Growth Hormone in Children with Turner Syndrome: Data from the PATRO Children Study. Horm. Res. Paediatr. 2021, 94, 133–143. [Google Scholar] [CrossRef]
- Wasniewska, M.; De Luca, F.; Bergamaschi, R.; Guarneri, M.P.; Mazzanti, L.; Matarazzo, P.; Petri, A.; Crisafulli, G.; Salzano, G.; Lombardo, F. Early treatment with GH alone in Turner syndrome: Prepubertal catch-up growth and waning effect. Eur. J. Endocrinol. 2004, 151, 567–572. [Google Scholar] [CrossRef]
- Baxter, L.; Bryant, J.; Cave, C.B.; Milne, R. Recombinant growth hormone for children and adolescents with Turner syndrome. Cochrane Database Syst. Rev. 2007, 1, CD003887. [Google Scholar] [CrossRef]
- Irzyniec, T.; Jeż, W.; Lepska, K.; Maciejewska-Paszek, I.; Frelich, J. Childhood growth hormone treatment in women with Turner syndrome—Benefits and adverse effects. Sci. Rep. 2019, 9, 15951. [Google Scholar] [CrossRef]
- Noonan, J.A.; Kappelgaard, A.M. The efficacy and safety of growth hormone therapy in children with noonan syndrome: A review of the evidence. Horm. Res. Paediatr. 2015, 83, 157–166. [Google Scholar] [CrossRef]
- Stagi, S.; Ferrari, V.; Ferrari, M.; Priolo, M.; Tartaglia, M. Inside the Noonan “universe”: Literature review on growth, GH/IGF axis and rhGH treatment: Facts and concerns. Front. Endocrinol. 2022, 13, 951331. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.E.; Allanson, J.E.; Tartaglia, M.; Gelb, B.D. Noonan syndrome. Lancet 2013, 381, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Sarkozy, A.; Carta, C.; Moretti, S.; Zampino, G.; Digilio, M.C.; Pantaleoni, F.; Scioletti, A.P.; Esposito, G.; Cordeddu, V.; Lepri, F.; et al. Germline BRAF mutations in Noonan, LEOPARD, and cardiofaciocutaneous syndromes: Molecular diversity and associated phenotypic spectrum. Hum. Mutat. 2009, 30, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Sodero, G.; Cipolla, C.; Pane, L.C.; Sessa, L.; Malavolta, E.; Arzilli, F.; Leoni, C.; Zampino, G.; Rigante, D. Efficacy and safety of growth hormone therapy in children with Noonan syndrome. Growth Horm. IGF Res. 2023, 69–70, 101532. [Google Scholar] [CrossRef]
- Rohrer, T.R.; Abuzzahab, J.; Backeljauw, P.; Birkegård, A.C.; Blair, J.; Dahlgren, J.; Júlíusson, P.B.; Ostrow, V.; Pietropoli, A.; Polak, M.; et al. Long-term effectiveness and safety of childhood growth hormone treatment in Noonan syndrome. Horm. Res. Paediatr. 2020, 93, 380–395. [Google Scholar] [CrossRef]
- Tamburrino, F.; Mazzanti, L.; Scarano, E.; Gibertoni, D.; Sirolli, M.; Zioutas, M.; Schiavariello, C.; Perri, A.; Mantovani, A.; Rossi, C.; et al. Lipid profile in Noonan syndrome and related disorders: Trend by age, sex and genotype. Front. Endocrinol. 2023, 14, 1209339. [Google Scholar] [CrossRef]
- Malaquias, A.C.; Brasil, A.S.; Pereira, A.C.; Arnhold, I.J.; Mendonca, B.B.; Bertola, D.R.; Jorge, A.A. Growth standards of patients with Noonan and Noonan-like syndromes with mutations in the RAS/MAPK pathway. Am. J. Med. Genet. A 2012, 158A, 2700–2706. [Google Scholar] [CrossRef]
- Jorge, A.A.L.; Edouard, T.; Maghnie, M.; Pietropoli, A.; Kelepouris, N.; Romano, A.; Zenker, M.; Horikawa, R. Outcomes in growth hormone-treated Noonan syndrome children: Impact of PTPN11 mutation status. Endocr. Connect. 2022, 11, e210615. [Google Scholar] [CrossRef]
- Chacko, E.M.; Rapaport, R. Short stature and its treatment in Turner and Noonan syndromes. Curr. Opin. Endocrinol. Diabetes Obes. 2012, 19, 40–46. [Google Scholar] [CrossRef]
- Moore, G.E.; Abu-Amero, S.; Wakeling, E.; Hitchins, M.; Monk, D.; Stanier, P.; Preece, M. The search for the gene for Silver-Russell syndrome. Acta Paediatr. 1999, 88, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Wollmann, H.A.; Kirchner, T.; Enders, H.; Preece, M.A.; Ranke, M.B. Growth and symptoms in Silver-Russell syndrome: Review on the basis of 386 patients. Eur. J. Pediatr. 1995, 154, 958–968. [Google Scholar] [CrossRef]
- Netchine, I.; Rossignol, S.; Dufourg, M.N.; Azzi, S.; Rousseau, A.; Perin, L.; Houang, M.; Steunou, V.; Esteva, B.; Thibaud, N.; et al. 11p15 imprinting center region 1 loss of methylation is a common and specific cause of typical Russell-Silver syndrome: Clinical scoring system and epigenetic-phenotypic correlations. J. Clin. Endocrinol. Metab. 2007, 92, 3148–3154. [Google Scholar] [CrossRef] [PubMed]
- Wakeling, E.L.; Brioude, F.; Lokulo-Sodipe, O.; O’Connell, S.M.; Salem, J.; Bliek, J.; Canton, A.P.; Chrzanowska, K.H.; Davies, J.H.; Dias, R.P.; et al. Diagnosis and management of Silver-Russell syndrome: First international consensus statement. Nat. Rev. Endocrinol. 2017, 13, 105–124. [Google Scholar] [CrossRef] [PubMed]
- Abraham, E.; Altiok, H.; Lubicky, J.P. Musculoskeletal manifestations of Russell-Silver syndrome. J. Pediatr. Orthop. 2004, 24, 552–564. [Google Scholar] [CrossRef]
- Bliek, J.; Terhal, P.; van den Bogaard, M.J.; Maas, S.; Hamel, B.; Salieb-Beugelaar, G.; Simon, M.; Letteboer, T.; van der Smagt, J.; Kroes, H.; et al. Hypomethylation of the H19 gene causes not only Silver-Russell syndrome (SRS) but also isolated asymmetry or an SRS-like phenotype. Am. J. Hum. Genet. 2006, 78, 604–614. [Google Scholar] [CrossRef]
- Bruce, S.; Hannula-Jouppi, K.; Peltonen, J.; Kere, J.; Lipsanen-Nyman, M. Clinically distinct epigenetic subgroups in Silver-Russell syndrome: The degree of H19 hypomethylation associates with phenotype severity and genital and skeletal anomalies. J. Clin. Endocrinol. Metab. 2009, 94, 579–587. [Google Scholar] [CrossRef]
- Wakeling, E.L.; Amero, S.A.; Alders, M.; Bliek, J.; Forsythe, E.; Kumar, S.; Lim, D.H.; MacDonald, F.; Mackay, D.J.; Maher, E.R.; et al. Epigenotype-phenotype correlations in Silver-Russell syndrome. J. Med. Genet. 2010, 47, 760–768. [Google Scholar] [CrossRef]
- Fuke, T.; Mizuno, S.; Nagai, T.; Hasegawa, T.; Horikawa, R.; Miyoshi, Y.; Muroya, K.; Kondoh, T.; Numakura, C.; Sato, S.; et al. Molecular and clinical studies in 138 Japanese patients with Silver-Russell syndrome. PLoS ONE 2013, 8, e60105. [Google Scholar] [CrossRef]
- Azzi, S.; Salem, J.; Thibaud, N.; Chantot-Bastaraud, S.; Lieber, E.; Netchine, I.; Harbison, M.D. A prospective study validating a clinical scoring system and demonstrating phenotypical-genotypical correlations in Silver-Russell syndrome. J. Med. Genet. 2015, 52, 446–453. [Google Scholar] [CrossRef]
- Yamaguchi, K.T., Jr.; Salem, J.B.; Myung, K.S.; Romero, A.N., Jr.; Skaggs, D.L. Spinal deformity in Russell-Silver syndrome. Spine Deform. 2015, 3, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.B.; Bigham, A.W.; Buckingham, K.J.; Hannibal, M.C.; McMillin, M.J.; Gildersleeve, H.I.; Beck, A.E.; Tabor, H.K.; Cooper, G.M.; Mefford, H.C.; et al. Exome sequencing identifies MLL2 mutations as a cause of Kabuki syndrome. Nat. Genet. 2010, 42, 790–793. [Google Scholar] [CrossRef]
- Paulussen, A.D.; Stegmann, A.P.; Blok, M.J.; Tserpelis, D.; Posma-Velter, C.; Detisch, Y.; Smeets, E.E.; Wagemans, A.; Schrander, J.J.; van den Boogaard, M.J.; et al. MLL2 mutation spectrum in 45 patients with Kabuki syndrome. Hum. Mutat. 2011, 32, E2018–E2025. [Google Scholar] [CrossRef]
- Miyake, N.; Mizuno, S.; Okamoto, N.; Ohashi, H.; Shiina, M.; Ogata, K.; Tsurusaki, Y.; Nakashima, M.; Saitsu, H.; Niikawa, N.; et al. KDM6A point mutations cause Kabuki syndrome. Hum. Mutat. 2013, 34, 108–110. [Google Scholar] [CrossRef]
- Adam, M.P.; Hudgins, L.; Hannibal, M. Kabuki Syndrome. In GeneReviews®; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993–2024. Updated 2022. Available online: https://www.ncbi.nlm.nih.gov/sites/books/NBK62111/ (accessed on 17 September 2024).
- Venugopal, V.; Pavlakis, S. Duchenne Muscular Dystrophy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Updated 10 July 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482346/ (accessed on 17 September 2024).
- Heydemann, A.; Siemionow, M. A brief review of Duchenne muscular dystrophy treatment options, with an emphasis on two novel strategies. Biomedicines 2023, 11, 830. [Google Scholar] [CrossRef]
- Zhang, T.; Kong, X. Recent advances of glucocorticoids in the treatment of Duchenne muscular dystrophy (Review). Exp. Ther. Med. 2021, 21, 447. [Google Scholar] [CrossRef]
- Møller, N.; Lunde Jørgensen, J.O. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocr. Rev. 2009, 30, 152–177. [Google Scholar] [CrossRef]
- Improda, N.; Capalbo, D.; Esposito, A.; Salerno, M. Muscle and skeletal health in children and adolescents with GH deficiency. Best. Pract. Res. Clin. Endocrinol. Metab. 2016, 30, 771–783. [Google Scholar] [CrossRef]
- Nishad, R.; Mukhi, D.; Menon, R.K.; Pasupulati, A.K. Growth hormone and metabolic homeostasis. EMJ Diabetes 2018, 6, 78–87. [Google Scholar] [CrossRef]
- Sas, T.; Mulder, P.; Hokken-Koelega, A. Body composition, blood pressure, and lipid metabolism before and during long-term growth hormone (GH) treatment in children with short stature born small for gestational age either with or without GH deficiency. J. Clin. Endocrinol. Metab. 2000, 85, 3786–3792. [Google Scholar]
- Gleeson, H.; Barreto, E.S.; Salvatori, R.; Costa, L.; Oliveira, C.R.; Pereira, R.M.; Clayton, P.; Aguiar-Oliveira, M.H. Metabolic effects of growth hormone (GH) replacement in children and adolescents with severe isolated GH deficiency due to a GHRH receptor mutation. Clin. Endocrinol. 2007, 66, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Meazza, C.; Elsedfy, H.H.; Pagani, S.; Bozzola, E.; El Kholy, M.; Bozzola, M. Metabolic parameters and adipokine profile in growth hormone deficient (GHD) children before and after 12-month GH treatment. Horm. Metab. Res. 2014, 46, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Ciresi, A.; Amato, M.C.; Giordano, C. Reduction in insulin sensitivity and inadequate β-cell capacity to counteract the increase in insulin resistance in children with idiopathic growth hormone deficiency during 12 months of growth hormone treatment. J. Endocrinol. Investig. 2015, 38, 351–359. [Google Scholar] [CrossRef]
- Chen, M.; Gan, D.; Luo, Y.; Rampersad, S.; Xu, L.; Yang, S.; Li, N.; Li, H. Effect of recombinant human growth hormone therapy on blood lipid and carotid intima-media thickness in children with growth hormone deficiency. Pediatr. Res. 2018, 83, 954–960. [Google Scholar] [CrossRef]
- Ferruzzi, A.; Vrech, M.; Pietrobelli, A.; Cavarzere, P.; Zerman, N.; Guzzo, A.; Flodmark, C.E.; Piacentini, G.; Antoniazzi, F. The influence of growth hormone on pediatric body composition: A systematic review. Front. Endocrinol. 2023, 14, 1093691. [Google Scholar] [CrossRef]
- Ciresi, A.; Guarnotta, V.; Pizzolanti, G.; Giordano, C. Comparison between euglycemic hyperinsulinemic clamp and surrogate indices of insulin sensitivity in children with growth hormone deficiency. Growth Horm. IGF Res. 2018, 39, 40–44. [Google Scholar] [CrossRef]
- Witkowska-Sedek, E.; Labochka, D.; Stelmaszczyk-Emmel, A.; Majcher, A.; Kucharska, A.; Sobol, M.; Kadziela, K.; Pyrzak, B. Evaluation of glucose metabolism in children with growth hormone deficiency during long-term growth hormone treatment. J. Physiol. Pharmacol. 2018, 69, 219–230. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Myers, S.E.; Carrel, A.L.; Whitman, B.Y.; Allen, D.B. Sustained benefit after 2 years of growth hormone on body composition, fat utilization, physical strength and agility, and growth in Prader-Willi syndrome. J. Pediatr. 2000, 137, 42–49. [Google Scholar] [CrossRef]
- Lin, H.Y.; Lin, S.P.; Tsai, L.P.; Chao, M.C.; Chen, M.R.; Chuang, C.K.; Huang, C.Y.; Tsai, F.J.; Chou, I.C.; Chiu, P.C.; et al. Effects of growth hormone treatment on height, weight, and obesity in Taiwanese patients with Prader-Willi syndrome. J. Chin. Med. Assoc. 2008, 71, 305–309. [Google Scholar] [CrossRef][Green Version]
- Festen, D.A.; de Lind van Wijngaarden, R.; van Eekelen, M.; Otten, B.J.; Wit, J.M.; Duivenvoorden, H.J.; Hokken-Koelega, A.C. Randomized controlled GH trial: Effects on anthropometry, body composition and body proportions in a large group of children with Prader-Willi syndrome. Clin. Endocrinol. 2008, 69, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Abe, Y.; Oto, Y.; Itabashi, H.; Shiraishi, M.; Yoshino, A.; Obata, K.; Murakami, N.; Nagai, T. Characterization of fat distribution in Prader-Willi syndrome: Relationships with adipocytokines and influence of growth hormone treatment. Am. J. Med. Genet. A 2013, 161A, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Höybye, C. Growth hormone treatment of Prader-Willi syndrome has long-term, positive effects on body composition. Acta Paediatr. 2015, 104, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Festen, D.A.; van Toorenenbergen, A.; Duivenvoorden, H.J.; Hokken-Koelega, A.C. Adiponectin levels in prepubertal children with Prader-Willi syndrome before and during growth hormone therapy. J. Clin. Endocrinol. Metab. 2007, 92, 1549–1554. [Google Scholar] [CrossRef][Green Version]
- Sohn, Y.B.; Kwak, M.J.; Kim, S.J.; Park, S.W.; Kim, C.H.; Kim, M.Y.; Kwon, E.K.; Paik, K.H.; Jin, D.K. Correlation of adiponectin receptor expression with cytokines and insulin sensitivity in growth hormone (GH)-treated children with Prader-Willi syndrome and in non-GH-treated obese children. J. Clin. Endocrinol. Metab. 2010, 95, 1371–1377. [Google Scholar] [CrossRef]
- Myers, S.E.; Davis, A.; Whitman, B.Y.; Santiago, J.V.; Landt, M. Leptin concentrations in Prader-Willi syndrome before and after growth hormone replacement. Clin. Endocrinol. 2000, 52, 101–105. [Google Scholar] [CrossRef]
- Crinò, A.; Di Giorgio, G.; Manco, M.; Grugni, G.; Maggioni, A. Effects of growth hormone therapy on glucose metabolism and insulin sensitivity indices in prepubertal children with Prader-Willi syndrome. Horm. Res. 2007, 68, 83–90. [Google Scholar] [CrossRef]
- Fintini, D.; Grugni, G.; Bocchini, S.; Brufani, C.; Di Candia, S.; Corrias, A.; Delvecchio, M.; Salvatoni, A.; Ragusa, L.; Greggio, N.; et al. Disorders of glucose metabolism in Prader-Willi syndrome: Results of a multicenter Italian cohort study. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 842–847. [Google Scholar] [CrossRef]
- Alsaif, M.; Field, C.J.; Colin-Ramirez, E.; Prado, C.M.; Haqq, A.M. Serum asprosin concentrations in children with Prader-Willi syndrome: Correlations with metabolic parameters. J. Clin. Med. 2022, 11, 2268. [Google Scholar] [CrossRef]
- Hauffa, B.P.; Haase, K.; Range, I.M.; Unger, N.; Mann, K.; Petersenn, S. The effect of growth hormone on the response of total and acylated ghrelin to a standardized oral glucose load and insulin resistance in children with Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 2007, 92, 834–840. [Google Scholar] [CrossRef][Green Version]
- Feigerlová, E.; Diene, G.; Conte-Auriol, F.; Molinas, C.; Gennero, I.; Salles, J.P.; Arnaud, C.; Tauber, M. Hyperghrelinemia precedes obesity in Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 2008, 93, 2800–2805. [Google Scholar] [CrossRef] [PubMed]
- Bizzarri, C.; Rigamonti, A.E.; Luce, A.; Cappa, M.; Cella, S.G.; Berini, J.; Sartorio, A.; Müller, E.E.; Salvatoni, A. Children with Prader-Willi syndrome exhibit more evident meal-induced responses in plasma ghrelin and peptide YY levels than obese and lean children. Eur. J. Endocrinol. 2010, 162, 499–505. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kuppens, R.J.; Delhanty, P.J.; Huisman, T.M.; van der Lely, A.J.; Hokken-Koelega, A.C. Acylated and unacylated ghrelin during OGTT in Prader-Willi syndrome: Support for normal response to food intake. Clin. Endocrinol. 2016, 85, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Bakker, N.E.; Kuppens, R.J.; Siemensma, E.P.; Tummers-de Lind van Wijngaarden, R.F.; Festen, D.A.; Bindels-de Heus, G.C.; Bocca, G.; Haring, D.A.; Hoorweg-Nijman, J.J.; Houdijk, E.C.; et al. Eight years of growth hormone treatment in children with Prader-Willi syndrome: Maintaining the positive effects. J. Clin. Endocrinol. Metab. 2013, 98, 4013–4022. [Google Scholar] [CrossRef] [PubMed]
- Bakker, N.E.; Siemensma, E.P.; Koopman, C.; Hokken-Koelega, A.C. Dietary Energy Intake, Body Composition and Resting Energy Expenditure in Prepubertal Children with Prader-Willi Syndrome before and during Growth Hormone Treatment: A Randomized Controlled Trial. Horm. Res. Paediatr. 2015, 83, 321–331. [Google Scholar] [CrossRef]
- Cadoudal, T.; Buléon, M.; Sengenès, C.; Diene, G.; Desneulin, F.; Molinas, C.; Eddiry, S.; Conte-Auriol, F.; Daviaud, D.; Martin, P.G.; et al. Impairment of adipose tissue in Prader-Willi syndrome rescued by growth hormone treatment. Int. J. Obes. 2014, 38, 1234–1240. [Google Scholar] [CrossRef]
- Eiholzer, U.; l’Allemand, D.; van der Sluis, I.; Steinert, H.; Gasser, T.; Ellis, K. Body composition abnormalities in children with Prader-Willi syndrome and long-term effects of growth hormone therapy. Horm. Res. 2000, 53, 200–206. [Google Scholar] [CrossRef]
- Carrel, A.L.; Myers, S.E.; Whitman, B.Y.; Allen, D.B. Sustained benefits of growth hormone on body composition, fat utilization, physical strength and agility, and growth in Prader-Willi syndrome are dose-dependent. J. Pediatr. Endocrinol. Metab. 2001, 14, 1097–1105. [Google Scholar] [CrossRef]
- Haqq, A.M.; Stadler, D.D.; Jackson, R.H.; Rosenfeld, R.G.; Purnell, J.Q.; LaFranchi, S.H. Effects of growth hormone on pulmonary function, sleep quality, behavior, cognition, growth velocity, body composition, and resting energy expenditure in Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 2003, 88, 2206–2212. [Google Scholar] [CrossRef]
- Whitman, B.; Carrel, A.; Bekx, T.; Weber, C.; Allen, D.; Myers, S. Growth hormone improves body composition and motor development in infants with Prader-Willi syndrome after six months. J. Pediatr. Endocrinol. Metab. 2004, 17, 591–600. [Google Scholar] [CrossRef]
- Carrel, A.L.; Moerchen, V.; Myers, S.E.; Bekx, M.T.; Whitman, B.Y.; Allen, D.B. Growth hormone improves mobility and body composition in infants and toddlers with Prader-Willi syndrome. J. Pediatr. 2004, 145, 744–749. [Google Scholar] [CrossRef] [PubMed]
- Eiholzer, U.; L’allemand, D.; Schlumpf, M.; Rousson, V.; Gasser, T.; Fusch, C. Growth hormone and body composition in children younger than 2 years with Prader-Willi syndrome. J. Pediatr. 2004, 144, 753–758. [Google Scholar] [PubMed]
- Galassetti, P.; Saetrum Opgaard, O.; Cassidy, S.B.; Pontello, A. Nutrient intake and body composition variables in Prader-Willi syndrome--effect of growth hormone supplementation and genetic subtype. J. Pediatr. Endocrinol. Metab. 2007, 20, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, A.C.; Lindberg, A. Growth hormone treatment completely normalizes adult height and improves body composition in Prader-Willi syndrome: Experience from KIGS (Pfizer international growth database). Horm. Res. 2008, 70, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Eiholzer, U.; Meinhardt, U.; Gallo, C.; Schlumpf, M.; Rousson, V.; l’Allemand, D. Association between foot growth and musculoskeletal loading in children with Prader-Willi syndrome before and during growth hormone treatment. J. Pediatr. 2009, 154, 225–229. [Google Scholar] [CrossRef]
- Carrel, A.L.; Myers, S.E.; Whitman, B.Y.; Eickhoff, J.; Allen, D.B. Long-term growth hormone therapy changes the natural history of body composition and motor function in children with prader-willi syndrome. J. Clin. Endocrinol. Metab. 2010, 95, 1131–1136. [Google Scholar] [CrossRef]
- Colmenares, A.; Pinto, G.; Taupin, P.; Giuseppe, A.; Odent, T.; Trivin, C.; Laborde, K.; Souberbielle, J.C.; Polak, M. Effects on growth and metabolism of growth hormone treatment for 3 years in 36 children with Prader-Willi syndrome. Horm. Res. Paediatr. 2011, 75, 123–130. [Google Scholar] [CrossRef]
- Coupaye, M.; Lorenzini, F.; Lloret-Linares, C.; Molinas, C.; Pinto, G.; Diene, G.; Mimoun, E.; Demeer, G.; Labrousse, F.; Jauregi, J.; et al. Growth hormone therapy for children and adolescents with Prader-Willi syndrome is associated with improved body composition and metabolic status in adulthood. J. Clin. Endocrinol. Metab. 2013, 98, E328–E335. [Google Scholar] [CrossRef]
- Yang, A.; Choi, J.H.; Sohn, Y.B.; Eom, Y.; Lee, J.; Yoo, H.W.; Jin, D.K. Effects of recombinant human growth hormone treatment on growth, body composition, and safety in infants or toddlers with Prader-Willi syndrome: A randomized, active-controlled trial. Orphanet J. Rare Dis. 2019, 14, 216. [Google Scholar] [CrossRef]
- Gao, Y.; Yang, L.L.; Dai, Y.L.; Shen, Z.; Zhou, Q.; Zou, C.C. Effects of early recombinant human growth hormone treatment in young Chinese children with Prader-Willi syndrome. Orphanet J. Rare Dis. 2023, 18, 25. [Google Scholar] [CrossRef]
- Lecka-Ambroziak, A.; Wysocka-Mincewicz, M.; Doleżal-Ołtarzewska, K.; Zygmunt-Górska, A.; Wędrychowicz, A.; Żak, T.; Noczyńska, A.; Birkholz-Walerzak, D.; Stawerska, R.; Hilczer, M.; et al. Effects of Recombinant Human Growth Hormone Treatment, Depending on the Therapy Start in Different Nutritional Phases in Paediatric Patients with Prader-Willi Syndrome: A Polish Multicentre Study. J. Clin. Med. 2021, 10, 3176. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.Y.; Luo, F.H. Early psychomotor development and growth hormone therapy in children with Prader-Willi syndrome: A review. Eur. J. Pediatr. 2023. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Lecka-Ambroziak, A.; Wysocka-Mincewicz, M.; Doleżal-Ołtarzewska, K.; Zygmunt-Górska, A.; Żak, T.; Noczyńska, A.; Birkholz-Walerzak, D.; Stawerska, R.; Hilczer, M.; Obara-Moszyńska, M.; et al. Correlation of Genotype and Perinatal Period, Time of Diagnosis and Anthropometric Data before Commencement of Recombinant Human Growth Hormone Treatment in Polish Patients with Prader-Willi Syndrome. Diagnostics 2021, 11, 798. [Google Scholar] [CrossRef] [PubMed]
- Allas, S.; Caixàs, A.; Poitou, C.; Coupaye, M.; Thuilleaux, D.; Lorenzini, F.; Diene, G.; Crinò, A.; Illouz, F.; Grugni, G.; et al. AZP-531, an unacylated ghrelin analog, improves food-related behavior in patients with Prader-Willi syndrome: A randomized placebo-controlled trial. PLoS ONE 2018, 13, e0190849. [Google Scholar] [CrossRef]
- Myers, S.E.; Whitman, B.Y.; Carrel, A.L.; Moerchen, V.; Bekx, M.T.; Allen, D.B. Two years of growth hormone therapy in young children with Prader-Willi syndrome: Physical and neurodevelopmental benefits. Am. J. Med. Genet. A 2007, 143A, 443–448. [Google Scholar] [CrossRef]
- Festen, D.A.; Wevers, M.; Lindgren, A.C.; Böhm, B.; Otten, B.J.; Wit, J.M.; Duivenvoorden, H.J.; Hokken-Koelega, A.C. Mental and motor development before and during growth hormone treatment in infants and toddlers with Prader-Willi syndrome. Clin. Endocrinol. 2008, 68, 919–925. [Google Scholar] [CrossRef]
- Sode-Carlsen, R.; Farholt, S.; Rabben, K.F.; Bollerslev, J.; Schreiner, T.; Jurik, A.G.; Christiansen, J.S.; Höybye, C. Body composition, endocrine and metabolic profiles in adults with Prader-Willi syndrome. Growth Horm. IGF Res. 2010, 20, 179–184. [Google Scholar] [CrossRef]
- Reus, L.; Pelzer, B.J.; Otten, B.J.; Siemensma, E.P.; van Alfen-van der Velden, J.A.; Festen, D.A.; Hokken-Koelega, A.C.; Nijhuis-van der Sanden, M.W. Growth hormone combined with child-specific motor training improves motor development in infants with Prader-Willi syndrome: A randomized controlled trial. Res. Dev. Disabil. 2013, 34, 3092–3103. [Google Scholar] [CrossRef]
- Reus, L.; Pillen, S.; Pelzer, B.J.; van Alfen-van der Velden, J.A.; Hokken-Koelega, A.C.; Zwarts, M.; Otten, B.J.; Nijhuis-van der Sanden, M.W. Growth hormone therapy, muscle thickness, and motor development in Prader-Willi syndrome: An RCT. Pediatrics 2014, 134, e1619–e1627. [Google Scholar] [CrossRef]
- Lafortuna, C.L.; Minocci, A.; Capodaglio, P.; Gondoni, L.A.; Sartorio, A.; Vismara, L.; Rizzo, G.; Grugni, G. Skeletal muscle characteristics and motor performance after 2-year growth hormone treatment in adults with prader-willi syndrome. J. Clin. Endocrinol. Metab. 2014, 99, 1816–1824. [Google Scholar] [CrossRef]
- Hyde, A.M.; Chavoya, F.A.; Silveira, F.V.; Beam, W.C.; Rubin, D.A. Metabolic responses to walking in children with Prader-Willi syndrome on growth hormone replacement therapy. Am. J. Med. Genet. A 2018, 176, 2513–2516. [Google Scholar] [CrossRef] [PubMed]
- Corripio, R.; Tubau, C.; Calvo, L.; Brun, C.; Capdevila, N.; Larramona, H.; Gabau, E. Safety and effectiveness of growth hormone therapy in infants with Prader-Willi syndrome younger than 2 years: A prospective study. J. Pediatr. Endocrinol. Metab. 2019, 32, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Cheng, R.Q.; Ying, Y.Q.; Qiu, Z.Q.; Fu, J.F.; Gong, C.X.; Yang, Y.L.; Shi, W.; Li, H.; Ma, M.S.; Wang, C.Y.; et al. Early recombinant human growth hormone treatment improves mental development and alleviates deterioration of motor function in infants and young children with Prader-Willi syndrome. World J. Pediatr. 2023, 19, 438–449. [Google Scholar] [CrossRef]
- Gondoni, L.A.; Vismara, L.; Marzullo, P.; Vettor, R.; Liuzzi, A.; Grugni, G. Growth hormone therapy improves exercise capacity in adult patients with Prader-Willi syndrome. J. Endocrinol. Investig. 2008, 31, 765–772. [Google Scholar] [CrossRef]
- Marzullo, P.; Marcassa, C.; Minocci, A.; Campini, R.; Eleuteri, E.; Gondoni, L.A.; Aimaretti, G.; Sartorio, A.; Scacchi, M.; Grugni, G. Long-term echocardiographic and cardioscintigraphic effects of growth hormone treatment in adults with Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 2015, 100, 2106–2114. [Google Scholar] [CrossRef]
- Hauffa, B.P.; Knaup, K.; Lehmann, N.; Neudorf, U.; Nagel, B. Effects of growth hormone therapy on cardiac dimensions in children and adolescents with Prader-Willi syndrome. Horm. Res. Paediatr. 2011, 75, 56–62. [Google Scholar] [CrossRef]
- Manzardo, A.M.; Heinemann, J.; McManus, B.; Loker, C.; Loker, J.; Butler, M.G. Venous thromboembolism in Prader-Willi syndrome: A questionnaire survey. Genes 2019, 10, 550. [Google Scholar] [CrossRef]
- l’Allemand, D.; Eiholzer, U.; Schlumpf, M.; Steinert, H.; Riesen, W. Cardiovascular risk factors improve during 3 years of growth hormone therapy in Prader-Willi syndrome. Eur. J. Pediatr. 2000, 159, 835–842. [Google Scholar] [CrossRef]
- de Lind van Wijngaarden, R.F.; Cianflone, K.; Gao, Y.; Leunissen, R.W.; Hokken-Koelega, A.C. Cardiovascular and metabolic risk profile and acylation-stimulating protein levels in children with Prader-Willi syndrome and effects of growth hormone treatment. J. Clin. Endocrinol. Metab. 2010, 95, 1758–1766. [Google Scholar] [CrossRef]
- de Lind van Wijngaarden, R.F.; Festen, D.A.; Otten, B.J.; van Mil, E.G.; Rotteveel, J.; Odink, R.J.; van Leeuwen, M.; Haring, D.A.; Bocca, G.; Mieke Houdijk, E.C.; et al. Bone mineral density and effects of growth hormone treatment in prepubertal children with Prader-Willi syndrome: A randomized controlled trial. J. Clin. Endocrinol. Metab. 2009, 94, 3763–3771. [Google Scholar] [CrossRef][Green Version]
- Khare, M.; Gold, J.A.; Wencel, M.; Billimek, J.; Surampalli, A.; Duarte, B.; Pontello, A.; Galassetti, P.; Cassidy, S.; Kimonis, V.E. Effect of genetic subtypes and growth hormone treatment on bone mineral density in Prader-Willi syndrome. J. Pediatr. Endocrinol. Metab. 2014, 27, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Bakker, N.E.; Kuppens, R.J.; Siemensma, E.P.; Tummers-de Lind van Wijngaarden, R.F.; Festen, D.A.; Bindels-de Heus, G.C.; Bocca, G.; Haring, D.A.; Hoorweg-Nijman, J.J.; Houdijk, E.C.; et al. Bone mineral density in children and adolescents with Prader-Willi syndrome: A longitudinal study during puberty and 9 years of growth hormone treatment. J. Clin. Endocrinol. Metab. 2015, 100, 1609–1618. [Google Scholar] [CrossRef]
- Oto, Y.; Murakami, N.; Inoue, T.; Matsubara, K.; Saima, S.; Ogata, H.; Ihara, H.; Nagai, T.; Matsubara, T. Growth hormone treatment and bone mineral density in pediatric patients with Prader-Willi syndrome. J. Pediatr. Endocrinol. Metab. 2021, 34, 1181–1184. [Google Scholar] [CrossRef]
- Drabik, M.; Lewiński, A.; Stawerska, R. Management of Prader-Labhart-Willi syndrome in children and in adults, with particular emphasis on the treatment with recombinant human growth hormone. Pediatr. Endocrinol. Diabetes Metab. 2022, 28, 64–74. [Google Scholar] [CrossRef]
- Jørgensen, A.P.; Ueland, T.; Sode-Carlsen, R.; Schreiner, T.; Rabben, K.F.; Farholt, S.; Høybye, C.; Christiansen, J.S.; Bollerslev, J. Glucose homeostasis in adults with Prader-Willi syndrome during treatment with growth hormone: Results from a 12-month prospective study. Growth Horm. IGF Res. 2014, 24, 16–21. [Google Scholar] [CrossRef]
- Brunetti, G.; Grugni, G.; Piacente, L.; Delvecchio, M.; Ventura, A.; Giordano, P.; Grano, M.; D’Amato, G.; Laforgia, D.; Crinò, A.; et al. Analysis of circulating mediators of bone remodeling in Prader-Willi syndrome. Calcif. Tissue Int. 2018, 102, 635–643. [Google Scholar] [CrossRef]
- Donze, S.H.; Kuppens, R.J.; Bakker, N.E.; van Alfen-van der Velden, J.A.E.M.; Hokken-Koelega, A.C.S. Bone mineral density in young adults with Prader-Willi syndrome: A randomized, placebo-controlled, crossover GH trial. Clin. Endocrinol. 2018, 88, 806–812. [Google Scholar] [CrossRef]
- Craig, M.E.; Cowell, C.T.; Larsson, P.; Zipf, W.B.; Reiter, E.O.; Albertsson Wikland, K.; Ranke, M.B.; Price, D.A.; KIGS International Board. Growth hormone treatment and adverse events in Prader-Willi syndrome: Data from KIGS (the Pfizer International Growth Database). Clin. Endocrinol. 2006, 65, 178–185. [Google Scholar] [CrossRef]
- de Lind van Wijngaarden, R.F.; de Klerk, L.W.; Festen, D.A.; Hokken-Koelega, A.C. Scoliosis in Prader-Willi syndrome: Prevalence, effects of age, gender, body mass index, lean body mass and genotype. Arch. Dis. Child. 2008, 93, 1012–1016. [Google Scholar] [CrossRef]
- de Lind van Wijngaarden, R.F.; de Klerk, L.W.; Festen, D.A.; Duivenvoorden, H.J.; Otten, B.J.; Hokken-Koelega, A.C. Randomized controlled trial to investigate the effects of growth hormone treatment on scoliosis in children with Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 2009, 94, 1274–1280. [Google Scholar] [CrossRef]
- Grootjen, L.N.; Rutges, J.P.H.J.; Damen, L.; Donze, S.H.; Juriaans, A.F.; Kerkhof, G.F.; Hokken-Koelega, A.C.S. Effects of 8 years of growth hormone treatment on scoliosis in children with Prader-Willi syndrome. Eur. J. Endocrinol. 2021, 185, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Roof, E.; Stone, W.; MacLean, W.; Feurer, I.D.; Thompson, T.; Butler, M.G. Intellectual characteristics of Prader-Willi syndrome: Comparison of genetic subtypes. J. Intellect. Disabil. Res. 2000, 44, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Butler, M.G.; Bittel, D.C.; Kibiryeva, N.; Talebizadeh, Z.; Thompson, T. Behavioral differences among subjects with Prader-Willi syndrome and type I or type II deletion and maternal disomy. Pediatrics 2004, 113, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Bakker, N.E.; Siemensma, E.P.; van Rijn, M.; Festen, D.A.; Hokken-Koelega, A.C. Beneficial effect of growth hormone treatment on health-related quality of life in children with Prader-Willi syndrome: A randomized controlled trial and longitudinal study. Horm. Res. Paediatr. 2015, 84, 231–239. [Google Scholar] [CrossRef]
- Rosenberg, A.G.W.; Passone, C.G.B.; Pellikaan, K.; Damiani, D.; van der Lely, A.J.; Polak, M.; Bernardo, W.M.; de Graaff, L.C.G. Growth hormone treatment for adults with Prader-Willi syndrome: A meta-analysis. J. Clin. Endocrinol. Metab. 2021, 106, 3068–3091. [Google Scholar] [CrossRef]
- Whitman, B.Y.; Myers, S.; Carrel, A.; Allen, D. The behavioral impact of growth hormone treatment for children and adolescents with Prader-Willi syndrome: A 2-year, controlled study. Pediatrics 2002, 109, e35. [Google Scholar] [CrossRef]
- Siemensma, E.P.; Tummers-de Lind van Wijngaarden, R.F.; Festen, D.A.; Troeman, Z.C.; van Alfen-van der Velden, A.A.; Otten, B.J.; Rotteveel, J.; Odink, R.J.; Bindels-de Heus, G.C.; van Leeuwen, M.; et al. Beneficial effects of growth hormone treatment on cognition in children with Prader-Willi syndrome: A randomized controlled trial and longitudinal study. J. Clin. Endocrinol. Metab. 2012, 97, 2307–2314. [Google Scholar] [CrossRef]
- Böhm, B.; Ritzén, E.M.; Lindgren, A.C. Growth hormone treatment improves vitality and behavioural issues in children with Prader-Willi syndrome. Acta Paediatr. 2015, 104, 59–67. [Google Scholar] [CrossRef]
- Lo, S.T.; Festen, D.A.; Tummers-de Lind van Wijngaarden, R.F.; Collin, P.J.; Hokken-Koelega, A.C. Beneficial effects of long-term growth hormone treatment on adaptive functioning in infants with Prader-Willi syndrome. Am. J. Intellect. Dev. Disabil. 2015, 120, 315–327. [Google Scholar] [CrossRef]
- Lo, S.T.; Siemensma, E.P.; Festen, D.A.; Collin, P.J.; Hokken-Koelega, A.C. Behavior in children with Prader-Willi syndrome before and during growth hormone treatment: A randomized controlled trial and 8-year longitudinal study. Eur. Child Adolesc. Psychiatry 2015, 24, 1091–1101. [Google Scholar] [CrossRef]
- Kuppens, R.J.; Mahabier, E.F.; Bakker, N.E.; Siemensma, E.P.; Donze, S.H.; Hokken-Koelega, A.C. Effect of cessation of GH treatment on cognition during transition phase in Prader-Willi syndrome: Results of a 2-year crossover GH trial. Orphanet J. Rare Dis. 2016, 11, 153. [Google Scholar] [CrossRef] [PubMed]
- Grootjen, L.N.; Trueba-Timmermans, D.J.; Damen, L.; Mahabier, E.F.; Kerkhof, G.F.; Hokken-Koelega, A.C.S. Long-term growth hormone treatment of children with PWS: The earlier the start, the better the outcomes? J. Clin. Med. 2022, 11, 2496. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, R.; Swanson, H.D.; Butler, M.G.; Flodman, P.; Gold, J.A.; Miller, J.L.; Roof, E.; Osann, K.; Dykens, E.; Driscoll, D.J.; et al. Molecular classes and growth hormone treatment effects on behavior and emotion in patients with Prader-Willi syndrome. J. Clin. Med. 2022, 11, 2572. [Google Scholar] [CrossRef] [PubMed]
- Dykens, E.M.; Roof, E.; Hunt-Hawkins, H. Cognitive and adaptive advantages of growth hormone treatment in children with Prader-Willi syndrome. J. Child Psychol. Psychiatry 2017, 58, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Festen, D.A.; de Weerd, A.W.; van den Bossche, R.A.; Joosten, K.; Hoeve, H.; Hokken-Koelega, A.C. Sleep-related breathing disorders in prepubertal children with Prader-Willi syndrome and effects of growth hormone treatment. J. Clin. Endocrinol. Metab. 2006, 91, 4911–4915. [Google Scholar] [CrossRef][Green Version]
- Miller, J.; Silverstein, J.; Shuster, J.; Driscoll, D.J.; Wagner, M. Short-term effects of growth hormone on sleep abnormalities in Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 413–417. [Google Scholar] [CrossRef]
- Wilson, S.S.; Cotterill, A.M.; Harris, M.A. Growth hormone and respiratory compromise in Prader-Willi Syndrome. Arch. Dis. Child. 2006, 91, 349–350. [Google Scholar] [CrossRef]
- Salvatoni, A.; Veronelli, E.; Nosetti, L.; Berini, J.; de Simone, S.; Iughetti, L.; Bosio, L.; Chiumello, G.; Grugni, G.; Delù, G.; et al. Short-term effects of growth hormone treatment on the upper airways of non severely obese children with Prader-Willi syndrome. J. Endocrinol. Investig. 2009, 32, 601–605. [Google Scholar] [CrossRef]
- Miller, J.L.; Shuster, J.; Theriaque, D.; Driscoll, D.J.; Wagner, M. Sleep disordered breathing in infants with Prader-Willi syndrome during the first 6 weeks of growth hormone therapy: A pilot study. J. Clin. Sleep Med. 2009, 5, 448–453. [Google Scholar] [CrossRef]
- Nixon, G.M.; Rodda, C.P.; Davey, M.J. Longitudinal association between growth hormone therapy and obstructive sleep apnea in a child with Prader-Willi syndrome. J. Clin. Endocrinol. Metab. 2011, 96, 29–33. [Google Scholar] [CrossRef]
- Katz-Salamon, M.; Lindgren, A.C.; Cohen, G. The effect of growth hormone on sleep-related cardio-respiratory control in Prader-Willi syndrome. Acta Paediatr. 2012, 101, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Al-Saleh, S.; Al-Naimi, A.; Hamilton, J.; Zweerink, A.; Iaboni, A.; Narang, I. Longitudinal evaluation of sleep-disordered breathing in children with Prader-Willi Syndrome during 2 years of growth hormone therapy. J. Pediatr. 2013, 162, 263–268.e1. [Google Scholar] [CrossRef] [PubMed]
- Berini, J.; Spica Russotto, V.; Castelnuovo, P.; Di Candia, S.; Gargantini, L.; Grugni, G.; Iughetti, L.; Nespoli, L.; Nosetti, L.; Padoan, G.; et al. Growth hormone therapy and respiratory disorders: Long-term follow-up in PWS children. J. Clin. Endocrinol. Metab. 2013, 98, E1516–E1523. [Google Scholar] [CrossRef] [PubMed]
- Lecka-Ambroziak, A.; Jȩdrzejczak, M.; Wysocka-Mincewicz, M.; Szalecki, M. Sleep-related breathing disorders in patients with Prader-Willi syndrome depending on the period of growth hormone treatment. Endokrynol. Pol. 2017, 68, 676–681. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zimmermann, M.; Laemmer, C.; Woelfle, J.; Fimmers, R.; Gohlke, B. Sleep-disordered breathing in children with Prader-Willi syndrome in relation to growth hormone therapy onset. Horm. Res. Paediatr. 2020, 93, 85–93. [Google Scholar] [CrossRef]
- Guo, H.; Fu, J.; Zhou, Y.; Luo, F.; Cheng, R. Evaluating the effect of recombinant human growth hormone treatment on sleep-related breathing disorders in toddlers with Prader-Willi syndrome: A one-year retrospective cohort study. BMC Pediatr. 2024, 24, 32. [Google Scholar] [CrossRef]
- Krantz, E.; Landin-Wilhelmsen, K.; Trimpou, P.; Bryman, I.; Wide, U. Health-related quality of life in Turner syndrome and the influence of growth hormone therapy: A 20-year follow-up. J. Clin. Endocrinol. Metab. 2019, 104, 5073–5083. [Google Scholar] [CrossRef]
- Blackett, P.R.; Rundle, A.C.; Frane, J.; Blethen, S.L. Body mass index (BMI) in Turner Syndrome before and during growth hormone (GH) therapy. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 232–235. [Google Scholar] [CrossRef]
- Ari, M.; Bakalov, V.K.; Hill, S.; Bondy, C.A. The effects of growth hormone treatment on bone mineral density and body composition in girls with turner syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 4302–4305. [Google Scholar] [CrossRef]
- Wooten, N.; Bakalov, V.K.; Hill, S.; Bondy, C.A. Reduced abdominal adiposity and improved glucose tolerance in growth hormone-treated girls with Turner syndrome. J. Clin. Endocrinol. Metab. 2008, 93, 2109–2114. [Google Scholar] [CrossRef]
- Baldin, A.D.; Fabbri, T.; Siviero-Miachon, A.A.; Spinola-Castro, A.M.; Lemos-Marini, S.H.; Baptista, M.T.; D’Souza-Li, L.F.; Maciel-Guerra, A.T.; Guerra, G., Jr. Effects of growth hormone on body proportions in Turner syndrome compared with non-treated patients and normal women. J. Endocrinol. Investig. 2010, 33, 691–695. [Google Scholar] [CrossRef] [PubMed]
- Baldin, A.D.; Fabbri, T.; Siviero-Miachon, A.A.; Spinola-Castro, A.M.; de Lemos-Marini, S.H.; Baptista, M.T.; D’Souza-Li, L.F.; Maciel-Guerra, A.T.; Guerra-Junior, G. Growth hormone effect on body composition in Turner syndrome. Endocrine 2011, 40, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Schrier, L.; de Kam, M.L.; McKinnon, R.; Che Bakri, A.; Oostdijk, W.; Sas, T.C.; Menke, L.A.; Otten, B.J.; de Muinck Keizer-Schrama, S.M.; Kristrom, B.; et al. Comparison of body surface area versus weight-based growth hormone dosing for girls with Turner syndrome. Horm. Res. Paediatr. 2014, 81, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Al, A.D.K.; Şükür, N.M.; Özturan, E.K.; Öztürk, A.P.; Poyrazoğlu, Ş.; Baş, F.; Darendeliler, F.F. Body proportions in patients with Turner syndrome on growth hormone treatment. Turk. J. Med. Sci. 2023, 53, 518–525. [Google Scholar] [CrossRef]
- Irzyniec, T.J.; Jeż, W. The influence of hormonal replacement and growth hormone treatment on the lipids in Turner syndrome. Gynecol. Endocrinol. 2014, 30, 250–253. [Google Scholar] [CrossRef]
- Sas, T.C.; de Muinck Keizer-Schrama, S.M.; Stijnen, T.; Aanstoot, H.J.; Drop, S.L. Carbohydrate metabolism during long-term growth hormone (GH) treatment and after discontinuation of GH treatment in girls with Turner syndrome participating in a randomized dose-response study. Dutch Advisory Group on Growth Hormone. J. Clin. Endocrinol. Metab. 2000, 85, 769–775. [Google Scholar]
- Theo, S.; De Keizer-Schrama, S.M.; Aanstoot, H.J.; Stijnen, T.; Drop, S. Carbohydrate metabolism during growth hormone treatment and after discontinuation of growth hormone treatment in girls with Turner syndrome treated with once or twice daily growth hormone injections. Clin. Endocrinol. 2000, 52, 741–747. [Google Scholar]
- Van Pareren, Y.K.; De Muinck Keizer-Schrama, S.M.; Stijnen, T.; Sas, T.C.; Drop, S.L. Effect of discontinuation of long-term growth hormone treatment on carbohydrate metabolism and risk factors for cardiovascular disease in girls with Turner syndrome. J. Clin. Endocrinol. Metab. 2002, 87, 5442–5448. [Google Scholar] [CrossRef]
- Bannink, E.M.; van der Palen, R.L.; Mulder, P.G.; de Muinck Keizer-Schrama, S.M. Long-term follow-up of GH-treated girls with Turner syndrome: Metabolic consequences. Horm. Res. 2009, 71, 343–349. [Google Scholar] [CrossRef]
- Qi, W.; Li, S.; Shen, Q.; Guo, X.; Rong, H. Effects of recombinant human growth hormone therapy on carbohydrate, lipid and protein metabolisms of children with Turner syndrome. Pak. J. Med. Sci. 2014, 30, 731–734. [Google Scholar] [CrossRef]
- Gnacińska, M.; Magnuszewska, H.; Sworczak, K. Metabolic consequences of recombinant human growth hormone therapy in patients with Turner syndrome. Pediatr. Endocrinol. Diabetes Metab. 2023, 29, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Gravholt, C.H.; Naeraa, R.W.; Brixen, K.; Kastrup, K.W.; Mosekilde, L.; Jørgensen, J.O.; Christiansen, J.S. Short-term growth hormone treatment in girls with Turner syndrome decreases fat mass and insulin sensitivity: A randomized, double-blind, placebo-controlled, crossover study. Pediatrics 2002, 110, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Radetti, G.; Pasquino, B.; Gottardi, E.; Boscolo Contadin, I.; Aimaretti, G.; Rigon, F. Insulin sensitivity in Turner’s syndrome: Influence of GH treatment. Eur. J. Endocrinol. 2004, 151, 351–354. [Google Scholar] [CrossRef]
- Mazzanti, L.; Bergamaschi, R.; Castiglioni, L.; Zappulla, F.; Pirazzoli, P.; Cicognani, A. Turner syndrome, insulin sensitivity and growth hormone treatment. Horm. Res. 2005, 64 (Suppl. S3), 51–57. [Google Scholar] [CrossRef]
- Darendeliler, F.; Aycan, Z.; Cetinkaya, E.; Vidilisan, S.; Bas, F.; Bideci, A.; Demirel, F.; Darcan, S.; Buyukgebiz, A.; Yildiz, M.; et al. Effects of growth hormone on growth, insulin resistance and related hormones (ghrelin, leptin and adiponectin) in Turner syndrome. Horm. Res. 2007, 68, 1–7. [Google Scholar] [CrossRef]
- Dyrka, K.; Rozkiewicz, N.; Obara-Moszynska, M.; Niedziela, M. The influence of growth hormone therapy on the cardiovascular system in Turner syndrome. J. Pediatr. Endocrinol. Metab. 2020, 33, 1363–1372. [Google Scholar] [CrossRef]
- van den Berg, J.; Bannink, E.M.; Wielopolski, P.A.; Pattynama, P.M.; de Muinck Keizer-Schrama, S.M.; Helbing, W.A. Aortic distensibility and dimensions and the effects of growth hormone treatment in the turner syndrome. Am. J. Cardiol. 2006, 97, 1644–1649. [Google Scholar] [CrossRef]
- Matura, L.A.; Sachdev, V.; Bakalov, V.K.; Rosing, D.R.; Bondy, C.A. Growth hormone treatment and left ventricular dimensions in Turner syndrome. J. Pediatr. 2007, 150, 587–591. [Google Scholar] [CrossRef]
- Radetti, G.; Crepaz, R.; Milanesi, O.; Paganini, C.; Cesaro, A.; Rigon, F.; Pitscheider, W. Cardiac performance in Turner’s syndrome patients on growth hormone therapy. Horm. Res. 2001, 55, 240–244. [Google Scholar] [CrossRef]
- Sas, T.C.; De Muinck Keizer-Schrama, S.M.; Stijnen, T.; Asarfi, A.; Van Leeuwen, W.J.; Van Teunenbroek, A.; Van Rijn, R.R.; Drop, S.L. A longitudinal study on bone mineral density until adulthood in girls with Turner’s syndrome participating in a growth hormone injection frequency-response trial. Clin. Endocrinol. 2000, 52, 531–536. [Google Scholar] [CrossRef]
- Sas, T.C.; de Muinck Keizer-Schrama, S.M.; Stijnen, T.; van Teunenbroek, A.; van Leeuwen, W.J.; Asarfi, A.; van Rijn, R.R.; Drop, S.L.; Dutch Advisory Group on Growth Hormone. Bone mineral density assessed by phalangeal radiographic absorptiometry before and during long-term growth hormone treatment in girls with Turner’s syndrome participating in a randomized dose-response study. Pediatr. Res. 2001, 50, 417–422. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wikiera, B.; Iwanicka, Z.; Barg, E.; Serafinowicz, E. Urinary deoxypyridinoline, serum osteocalcin and bone mineral density in girls with Turner’s syndrome. J. Pediatr. Endocrinol. Metab. 2003, 16, 1175–1177. [Google Scholar] [CrossRef] [PubMed]
- Bakalov, V.K.; Van, P.L.; Baron, J.; Reynolds, J.C.; Bondy, C.A. Growth hormone therapy and bone mineral density in Turner syndrome. J. Clin. Endocrinol. Metab. 2004, 89, 4886–4889. [Google Scholar] [CrossRef][Green Version]
- Aycan, Z.; Cetinkaya, E.; Darendeliler, F.; Vidinlisan, S.; Bas, F.; Bideci, A.; Demirel, F.; Darcan, S.; Buyukgebiz, A.; Yildiz, M.; et al. The effect of growth hormone treatment on bone mineral density in prepubertal girls with Turner syndrome: A multicentre prospective clinical trial. Clin. Endocrinol. 2008, 68, 769–772. [Google Scholar] [CrossRef]
- Augoulea, A.; Zachou, G.; Lambrinoudaki, I. Turner syndrome and osteoporosis. Maturitas 2019, 130, 41–49. [Google Scholar] [CrossRef]
- Schweizer, R.; Mayer, J.; Binder, G. Normal bone density but altered geometry in girls with Turner syndrome. J. Pediatr. Endocrinol. Metab. 2023, 36, 270–277. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Hjerrild, B.E.; Naeraa, R.W.; Engbaek, F.; Mosekilde, L.; Christiansen, J.S. Effect of growth hormone and 17beta-oestradiol treatment on metabolism and body composition in girls with Turner syndrome. Clin. Endocrinol. 2005, 62, 616–622. [Google Scholar] [CrossRef]
- McVey, L.C.; Fletcher, A.; Murtaza, M.; Donaldson, M.; Wong, S.C.; Mason, A. Skeletal disproportion in girls with Turner syndrome and longitudinal change with growth-promoting therapy. Clin. Endocrinol. 2021, 94, 797–803. [Google Scholar] [CrossRef]
- Juloski, J.; Glisic, B.; Scepan, I.; Milasin, J.; Mitrovic, K.; Babic, M. Ontogenetic changes of craniofacial complex in Turner syndrome patients treated with growth hormone. Clin. Oral. Investig. 2013, 17, 1563–1571. [Google Scholar] [CrossRef]
- Juloski, J.; Dumančić, J.; Šćepan, I.; Lauc, T.; Milašin, J.; Kaić, Z.; Dumić, M.; Babić, M. Growth hormone positive effects on craniofacial complex in Turner syndrome. Arch. Oral. Biol. 2016, 71, 10–15. [Google Scholar] [CrossRef]
- Sampaolo, P.; Calcaterra, V.; Klersy, C.; Alfei, A.; De Leonardis, C.; Maino, M.; Larizza, D. Pelvic ultrasound evaluation in patients with Turner syndrome during treatment with growth hormone. Ultrasound Obstet. Gynecol. 2003, 22, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Mondal, S.; Gargari, P.; Nagendra, L.; Mandal, S.; Kumar, R.C.; Shah, P.; Haldar, M.; Chowdhury, S.; Mukhopadhyay, S. Growth hormone therapy is associated with improved uterine dimensions in girls with Turner syndrome prior to oestrogen replacement. Clin. Endocrinol. 2024, 100, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Bannink, E.M.; Raat, H.; Mulder, P.G.; de Muinck Keizer-Schrama, S.M. Quality of life after growth hormone therapy and induced puberty in women with Turner syndrome. J. Pediatr. 2006, 148, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Amundson, E.; Boman, U.W.; Barrenäs, M.L.; Bryman, I.; Landin-Wilhelmsen, K. Impact of growth hormone therapy on quality of life in adults with turner syndrome. J. Clin. Endocrinol. Metab. 2010, 95, 1355–1359. [Google Scholar] [CrossRef]
- Taback, S.P.; Van Vliet, G. Health-related quality of life of young adults with Turner syndrome following a long-term randomized controlled trial of recombinant human growth hormone. BMC Pediatr. 2011, 11, 49. [Google Scholar] [CrossRef]
- van Pareren, Y.K.; Duivenvoorden, H.J.; Slijper, F.M.; Koot, H.M.; Drop, S.L.; de Muinck Keizer-Schrama, S.M. Psychosocial functioning after discontinuation of long-term growth hormone treatment in girls with Turner syndrome. Horm. Res. 2005, 63, 238–244. [Google Scholar] [CrossRef]
- Davenport, M.L.; Roush, J.; Liu, C.; Zagar, A.J.; Eugster, E.; Travers, S.; Fechner, P.Y.; Quigley, C.A. Growth hormone treatment does not affect incidences of middle ear disease or hearing loss in infants and toddlers with Turner syndrome. Horm. Res. Paediatr. 2010, 74, 23–32. [Google Scholar] [CrossRef]
- Espat, J.; Chamberlain, R.S.; Sklar, C.; Blumgart, L.H. Hepatic adenoma associated with recombinant human growth hormone therapy in a patient with Turner’s syndrome. Dig. Surg. 2000, 17, 640–643. [Google Scholar] [CrossRef]
- Chen, S.H.; Hung, C.S.; Lo, F.S.; Wang, H.S.; Jung, S.M.; Lui, T.N. Primitive neuroectodermal tumor of the brain in a girl with Turner syndrome diagnosed after 4 years of growth hormone therapy. Eur. J. Pediatr. 2006, 165, 344–345. [Google Scholar] [CrossRef]
- Pinsker, J.E.; Crudo, D.F. Ganglioneuroblastoma in a young child with Turner syndrome. J. Pediatr. Endocrinol. Metab. 2012, 25, 799–800. [Google Scholar] [CrossRef]
- Tang, W.J.; Huang, Y.; Chen, L.; Zheng, S.; Dong, K.R. Small intestinal tubular adenoma in a pediatric patient with Turner syndrome. World J. Gastroenterol. 2013, 19, 2122–2125. [Google Scholar] [CrossRef] [PubMed]
- Wasniewska, M.; Bergamaschi, R.; Matarazzo, P.; Predieri, B.; Bertelloni, S.; Petri, A.; Sposito, M.; Messina, M.F.; De Luca, F. Italian Study Group for Turner Syndrome. Increased liver enzymes and hormonal therapies in girls and adolescents with Turner syndrome. J. Endocrinol. Investig. 2005, 28, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Noordam, C.; Peer, P.G.; Francois, I.; De Schepper, J.; van den Burgt, I.; Otten, B.J. Long-term GH treatment improves adult height in children with Noonan syndrome with and without mutations in protein tyrosine phosphatase, non-receptor-type 11. Eur. J. Endocrinol. 2008, 159, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Raaijmakers, R.; Noordam, C.; Karagiannis, G.; Gregory, J.W.; Hertel, N.T.; Sipilä, I.; Otten, B.J. Response to growth hormone treatment and final height in Noonan syndrome in a large cohort of patients in the KIGS database. J. Pediatr. Endocrinol. Metab. 2008, 21, 267–273. [Google Scholar] [CrossRef]
- Ranke, M.B.; Lindberg, A.; Carlsson, M.; Camacho-Hübner, C.; Rooman, R. Treatment with Growth Hormone in Noonan Syndrome Observed during 25 Years of KIGS: Near Adult Height and Outcome Prediction. Horm. Res. Paediatr. 2019, 91, 46–55. [Google Scholar] [CrossRef]
- Noordam, C.; Span, J.; van Rijn, R.R.; Gomes-Jardin, E.; van Kuijk, C.; Otten, B.J. Bone mineral density and body composition in Noonan’s syndrome: Effects of growth hormone treatment. J. Pediatr. Endocrinol. Metab. 2002, 15, 81–87. [Google Scholar] [CrossRef]
- Lee, P.A.; Ross, J.; Germak, J.A.; Gut, R. Effect of 4 years of growth hormone therapy in children with Noonan syndrome in the American Norditropin Studies: Web-Enabled Research (ANSWER) Program® registry. Int. J. Pediatr. Endocrinol. 2012, 2012, 15. [Google Scholar] [CrossRef]
- Zavras, N.; Meazza, C.; Pilotta, A.; Gertosio, C.; Pagani, S.; Tinelli, C.; Bozzola, M. Five-year response to growth hormone in children with Noonan syndrome and growth hormone deficiency. Ital. J. Pediatr. 2015, 41, 71. [Google Scholar] [CrossRef]
- Delagrange, M.; Rousseau, V.; Cessans, C.; Pienkowski, C.; Oliver, I.; Jouret, B.; Cartault, A.; Diene, G.; Tauber, M.; Salles, J.P.; et al. Low bone mass in Noonan syndrome children correlates with decreased muscle mass and low IGF-1 levels. Bone 2021, 153, 116170. [Google Scholar] [CrossRef]
- Stevenson, D.A.; Allen, S.; Tidyman, W.E.; Carey, J.C.; Viskochil, D.H.; Stevens, A.; Hanson, H.; Sheng, X.; Thompson, B.A.; Okumura, M.J.; et al. Peripheral muscle weakness in RASopathies. Muscle Nerve 2012, 46, 394–399. [Google Scholar] [CrossRef]
- Croonen, E.A.; Essink, M.; van der Burgt, I.; Draaisma, J.M.; Noordam, C.; Nijhuis-van der Sanden, M.W.G. Motor performance in children with Noonan syndrome. Am. J. Med. Genet. A 2017, 173, 2335–2345. [Google Scholar] [CrossRef] [PubMed]
- Gelb, B.D.; Roberts, A.E.; Tartaglia, M. Cardiomyopathies in Noonan syndrome and the other RASopathies. Prog. Pediatr. Cardiol. 2015, 39, 13–19. [Google Scholar] [CrossRef] [PubMed]
- MacFarlane, C.E.; Brown, D.C.; Johnston, L.B.; Patton, M.A.; Dunger, D.B.; Savage, M.O.; McKenna, W.J.; Kelnar, C.J. Growth hormone therapy and growth in children with Noonan’s syndrome: Results of 3 years’ follow-up. J. Clin. Endocrinol. Metab. 2001, 86, 1953–1956. [Google Scholar]
- Noordam, C.; Draaisma, J.M.; van den Nieuwenhof, J.; van der Burgt, I.; Otten, B.J.; Daniels, O. Effects of growth hormone treatment on left ventricular dimensions in children with Noonan’s syndrome. Horm. Res. 2001, 56, 110–113. [Google Scholar] [CrossRef]
- Romano, A.; Kaski, J.P.; Dahlgren, J.; Kelepouris, N.; Pietropoli, A.; Rohrer, T.R.; Polak, M. Cardiovascular safety of growth hormone treatment in Noonan syndrome: Real-world evidence. Endocr. Connect. 2022, 11, e210549. [Google Scholar] [CrossRef]
- Kızılcan Çetin, S.; Ramoğlu, M.G.; Şıklar, Z.; Özsu, E.; Aycan, Z.; Tutar, H.E.; Berberoğlu, M. The effect of growth hormone therapy on cardiac outcomes in Noonan syndrome: Long term follow-up results. J. Clin. Res. Pediatr. Endocrinol. 2022, 14, 422–432. [Google Scholar] [CrossRef]
- Romano, A.A.; Dana, K.; Bakker, B.; Davis, D.A.; Hunold, J.J.; Jacobs, J.; Lippe, B. Growth response, near-adult height, and patterns of growth and puberty in patients with noonan syndrome treated with growth hormone. J. Clin. Endocrinol. Metab. 2009, 94, 2338–2344. [Google Scholar] [CrossRef]
- Malaquias, A.C.; Noronha, R.M.; Souza, T.T.O.; Homma, T.K.; Funari, M.F.A.; Yamamoto, G.L.; Silva, F.V.; Moraes, M.B.; Honjo, R.S.; Kim, C.A.; et al. Impact of growth hormone therapy on adult height in patients with PTPN11 mutations related to Noonan syndrome. Horm. Res. Paediatr. 2019, 91, 252–261. [Google Scholar] [CrossRef]
- Seo, G.H.; Yoo, H.W. Growth hormone therapy in patients with Noonan syndrome. Ann. Pediatr. Endocrinol. Metab. 2018, 23, 176–181. [Google Scholar] [CrossRef]
- Ogawa, M.; Moriya, N.; Ikeda, H.; Tanae, A.; Tanaka, T.; Ohyama, K.; Mori, O.; Yazawa, T.; Fujita, K.; Seino, Y.; et al. Clinical evaluation of recombinant human growth hormone in Noonan syndrome. Endocr. J. 2004, 51, 61–68. [Google Scholar] [CrossRef][Green Version]
- Osio, D.; Dahlgren, J.; Wikland, K.A.; Westphal, O. Improved final height with long-term growth hormone treatment in Noonan syndrome. Acta Paediatr. 2005, 94, 1232–1237. [Google Scholar] [CrossRef] [PubMed]
- Noronha, R.M.; Villares, S.M.F.; Torres, N.; Quedas, E.P.S.; Homma, T.K.; Albuquerque, E.V.A.; Moraes, M.B.; Funari, M.F.A.; Bertola, D.R.; Jorge, A.A.L.; et al. Noonan syndrome patients beyond the obvious phenotype: A potential unfavorable metabolic profile. Am. J. Med. Genet. A 2021, 185, 774–780. [Google Scholar] [CrossRef]
- Papadopoulou, A.; Bountouvi, E. Skeletal defects and bone metabolism in Noonan, Costello and cardio-facio-cutaneous syndromes. Front. Endocrinol. 2023, 14, 1231828. [Google Scholar] [CrossRef]
- Şıklar, Z.; Genens, M.; Poyrazoğlu, Ş.; Baş, F.; Darendeliler, F.; Bundak, R.; Aycan, Z.; Savaş Erdeve, Ş.; Çetinkaya, S.; Güven, A.; et al. The growth characteristics of patients with Noonan syndrome: Results of three years of growth hormone treatment: A Nationwide Multicenter Study. J. Clin. Res. Pediatr. Endocrinol. 2016, 8, 305–312. [Google Scholar] [CrossRef]
- Romano, A.A.; Allanson, J.E.; Dahlgren, J.; Gelb, B.D.; Hall, B.; Pierpont, M.E.; Roberts, A.E.; Robinson, W.; Takemoto, C.M.; Noonan, J.A. Noonan syndrome: Clinical features, diagnosis, and management guidelines. Pediatrics 2010, 126, 746–759. [Google Scholar] [CrossRef]
- Jongmans, M.C.; van der Burgt, I.; Hoogerbrugge, P.M.; Noordam, K.; Yntema, H.G.; Nillesen, W.M.; Kuiper, R.P.; Ligtenberg, M.J.; van Kessel, A.G.; van Krieken, J.H.; et al. Cancer risk in patients with Noonan syndrome carrying a PTPN11 mutation. Eur. J. Hum. Genet. 2011, 19, 870–874. [Google Scholar] [CrossRef]
- Wu, X.; Wu, J.; Yuan, Y.; Yang, L.; Yu, L. Noonan syndrome: rhGH treatment and PTPN11 mutation. Mol. Genet. Genom. Med. 2023, 11, e2266. [Google Scholar] [CrossRef]
- Moos, D.; Droitcourt, C.; Rancherevince, D.; Marec Berard, P.; Skowron, F. Atypical granular cell tumor occurring in an individual with Noonan syndrome treated with growth hormone. Pediatr. Dermatol. 2012, 29, 665–666. [Google Scholar] [CrossRef]
- Rakover, Y.; Dietsch, S.; Ambler, G.R.; Chock, C.; Thomsett, M.; Cowell, C.T. Growth hormone therapy in Silver Russell syndrome: 5 years experience of the Australian and New Zealand Growth database (OZGROW). Eur. J. Pediatr. 1996, 155, 851–857. [Google Scholar] [CrossRef]
- Christofordis, A.; Maniadaki, I.; Stanhope, R. Managing children with Russell-Silver syndrome: More than just growth hormone treatment? J. Pediatr. Endocrinol. Metab. 2005, 18, 651–652. [Google Scholar] [CrossRef]
- Toumba, M.; Albanese, A.; Azcona, C.; Stanhope, R. Effect of long-term growth hormone treatment on final height of children with Russell-Silver syndrome. Horm. Res. Paediatr. 2010, 74, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Smeets, C.C.; Zandwijken, G.R.; Renes, J.S.; Hokken-Koelega, A.C. Long-term results of GH treatment in Silver-Russell syndrome (SRS): Do they benefit the same as non-SRS short-SGA? J. Clin. Endocrinol. Metab. 2016, 101, 2105–2112. [Google Scholar] [CrossRef] [PubMed]
- Sienko, M.; Petriczko, E.; Zajaczek, S.; Zygmunt-Gorska, A.; Starzyk, J.; Korpysz, A.; Petriczko, J.; Walczak, A.; Walczak, M. The effects of growth hormone therapy on the somatic development of a group of Polish children with Silver-Russell syndrome. Neuro Endocrinol. Lett. 2017, 38, 415–421. [Google Scholar] [PubMed]
- Lokulo-Sodipe, O.; Giabicani, E.; Canton, A.P.M.; Ferrand, N.; Child, J.; Wakeling, E.L.; Binder, G.; Netchine, I.; Mackay, D.J.G.; Inskip, H.M.; et al. Height and body mass index in molecularly confirmed Silver-Russell syndrome and the long-term effects of growth hormone treatment. Clin. Endocrinol. 2022, 97, 284–292. [Google Scholar] [CrossRef]
- Lee, P.A.; Chernausek, S.D.; Hokken-Koelega, A.C.S.; Czernichow, P. International small for gestational age advisory board consensus development conference statement: Management of short children born small for gestational age. Pediatrics 2003, 111, 1253–1261. [Google Scholar] [CrossRef]
- Świąder-Leśniak, A.; Jurkiewicz, D.; Kołodziejczyk, H.; Kozłowska, A.; Korpysz, A.; Szalecki, M.; Chrzanowska, K. The effects of 3-year growth hormone treatment and body composition in Polish patients with Silver-Russell syndrome. Endokrynol. Pol. 2023, 74, 285–293. [Google Scholar] [CrossRef]
- Willemsen, R.H.; Arends, N.J.; Bakker-van Waarde, W.M.; Jansen, M.; van Mil, E.G.; Mulder, J.; Odink, R.J.; Reeser, M.; Rongen-Westerlaken, C.; Stokvis-Brantsma, W.H.; et al. Long-term effects of growth hormone (GH) treatment on body composition and bone mineral density in short children born small-for-gestational-age: Six-year follow-up of a randomized controlled GH trial. Clin. Endocrinol. 2007, 67, 485–492. [Google Scholar] [CrossRef]
- Smeets, C.C.; Renes, J.S.; van der Steen, M.; Hokken-Koelega, A.C. Metabolic health and long-term safety of growth hormone treatment in Silver-Russell syndrome. J. Clin. Endocrinol. Metab. 2017, 102, 983–991. [Google Scholar] [CrossRef]
- Chrzanowska, J.A.; Bubula, L.; Noczyńska, A.; Zubkiewicz-Kucharska, A. To increase body height and muscle strength—One medicine for two diseases? Case report of a boy with Silver-Russell syndrome and Duchenne muscular dystrophy. Pediatr. Endocrinol. Diabetes Metab. 2021, 27, 298–304. [Google Scholar] [CrossRef]
- Shott, D.A.; Remmel, R.; Plasqui, G.; Stumpel, C.T.R.M.; Gerver, W.J.M. Metabolic effects of growth hormone treatment on body composition, energy expenditure and physical activity in Kabuki Syndrome. In Growth Hormone therapy in Kabuki Syndrome; Maastricht University: Maastricht, The Netherlands, 2018; Chapter 6. [Google Scholar] [CrossRef]
- van Montfort, L.; Gerver, W.J.M.; Kooger, B.L.S.; Plat, J.; Bierau, J.; Stumpel, C.T.R.M.; Schott, D.A. Follow-up study of growth hormone therapy in children with Kabuki syndrome: Two-year treatment results. Horm. Res. Paediatr. 2021, 94, 285–296. [Google Scholar] [CrossRef]
- Schott, D.A.; Kooger, B.L.S.; Plat, J.; Bierau, J.; Stumpel, C.T.R.M.; Gerver, W.J.M. Cardiovascular markers in Kabuki Syndrome children before and after 12-month growth hormone treatment. In Growth Hormone in Kabuki Syndrome; Maastricht University: Maastricht, The Netherlands, 2018; Chapter 7; ISBN 978-94-6323-434-4. [Google Scholar]
- McQueen, M.J.; Hawken, S.; Wang, X.; Ounpuu, S.; Sniderman, A.; Probstfield, J.; Steyn, K.; Sanderson, J.E.; Hasani, M.; Volkova, E.; et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): A case-control study. Lancet 2008, 372, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Wasan, K.M.; Brocks, D.R.; Lee, S.D.; Sachs-Barrable, K.; Thornton, S.J. Impact of lipoproteins on the biological activity and disposition of hydrophobic drugs: Implications for drug discovery. Nat. Rev. Drug Discov. 2008, 7, 84–99. [Google Scholar] [CrossRef] [PubMed]
- Schott, D.A.; Stumpel, C.T.R.M.; Klaassens, M. Hypermobility in individuals with Kabuki syndrome: The effect of growth hormone treatment. Am. J. Med. Genet. A 2019, 179, 219–223. [Google Scholar] [CrossRef]
- Bahl, N.; Stone, G.; McLean, M.; Ho, K.K.Y.; Birzniece, V. Decorin, a growth hormone-regulated protein in humans. Eur. J. Endocrinol. 2018, 178, 145–152. [Google Scholar] [CrossRef]
- Cittadini, A.; Ines Comi, L.; Longobardi, S.; Rocco Petretta, V.; Casaburi, C.; Passamano, L.; Merola, B.; Durante-Mangoni, E.; Saccà, L.; Politano, L. A preliminary randomized study of growth hormone administration in Becker and Duchenne muscular dystrophies. Eur. Heart J. 2003, 24, 664–672. [Google Scholar] [CrossRef]
- Rutter, M.M.; Collins, J.; Rose, S.R.; Woo, J.G.; Sucharew, H.; Sawnani, H.; Hor, K.N.; Cripe, L.H.; Wong, B.L. Growth hormone treatment in boys with Duchenne muscular dystrophy and glucocorticoid-induced growth failure. Neuromuscul. Disord. 2012, 22, 1046–1056. [Google Scholar] [CrossRef]
- Lavi, E.; Cohen, A.; Libdeh, A.A.; Tsabari, R.; Zangen, D.; Dor, T. Growth hormone therapy for children with Duchenne muscular dystrophy and glucocorticoid induced short stature. Growth Horm. IGF Res. 2023, 72–73, 101558. [Google Scholar] [CrossRef]
- Mazziotti, G.; Giustina, A. Glucocorticoids and the regulation of growth hormone secretion. Nat. Rev. Endocrinol. 2013, 9, 265–276. [Google Scholar] [CrossRef]
- Fang, X.B.; Song, Z.B.; Xie, M.S.; Liu, Y.M.; Zhang, W.X. Synergistic effect of glucocorticoids and IGF-1 on myogenic differentiation through the Akt/GSK-3β pathway in C2C12 myoblasts. Int. J. Neurosci. 2020, 130, 1125–1135. [Google Scholar] [CrossRef]
| Name of Syndrome | Body Composition | Cardiac Effects/ CV Risk | Metabolic Markers | Bone Structure | Muscle/ Motor Function | QoL |
|---|---|---|---|---|---|---|
| PWS | ↓ FM ↑ LBM no effect on BMI | ↑ LV mass preservation of systolic/diastolic function ↓ CV risk ↓thromboembolism risk | ↓ LDL ↑ HDL/LDL ↓ HOMA-IR | ↑ bone geometry, strength, and mass ↑ BMD ↓ scoliosis risk | ↑ motor function | ↑ QoL ↑ cognition ↑ motor development ↑ nonverbal and total IQ |
| TS | ↓ FM ↑ LBM | aorta widening or increase of the aorta growth rate * | improvement in lipid profile | ↑ BMD | ↑ muscle mass ↑ muscle volume | ↑ QoL |
| NS | ↓ FM no effect on BMI | no significant adverse effect on LV dimensions and cardiac function ** | no effects or ↑ glucose/insulin no effect on lipid profile * | ↑ BMD no effect on scoliosis risk | no data | no data |
| SRS | ↓ or ↑ %FM ↑LBM | no data | ↑ fasting glucose | no data | ↑ muscle mass ↑ BMD | ↑ QoL ↑ perception skills |
| KS | ↑ LBM no effect or ↓ BMI | no data | ↓ LDL ↓ IL-8 no effect on glucose/insulin | no data | ↓ hypermobility of joints ↑ motor skills | no data |
| DMD | ↑ LBM ↓ BMI | ↑ LV mass ↓ systolic stress * | ↑ fasting insulin no effect on glucose | no data | no effect on skeletal muscle function | no data |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kucharska, A.; Witkowska-Sędek, E.; Erazmus, M.; Artemniak-Wojtowicz, D.; Krajewska, M.; Pyrżak, B. The Effects of Growth Hormone Treatment Beyond Growth Promotion in Patients with Genetic Syndromes: A Systematic Review of the Literature. Int. J. Mol. Sci. 2024, 25, 10169. https://doi.org/10.3390/ijms251810169
Kucharska A, Witkowska-Sędek E, Erazmus M, Artemniak-Wojtowicz D, Krajewska M, Pyrżak B. The Effects of Growth Hormone Treatment Beyond Growth Promotion in Patients with Genetic Syndromes: A Systematic Review of the Literature. International Journal of Molecular Sciences. 2024; 25(18):10169. https://doi.org/10.3390/ijms251810169
Chicago/Turabian StyleKucharska, Anna, Ewelina Witkowska-Sędek, Michał Erazmus, Dorota Artemniak-Wojtowicz, Maria Krajewska, and Beata Pyrżak. 2024. "The Effects of Growth Hormone Treatment Beyond Growth Promotion in Patients with Genetic Syndromes: A Systematic Review of the Literature" International Journal of Molecular Sciences 25, no. 18: 10169. https://doi.org/10.3390/ijms251810169
APA StyleKucharska, A., Witkowska-Sędek, E., Erazmus, M., Artemniak-Wojtowicz, D., Krajewska, M., & Pyrżak, B. (2024). The Effects of Growth Hormone Treatment Beyond Growth Promotion in Patients with Genetic Syndromes: A Systematic Review of the Literature. International Journal of Molecular Sciences, 25(18), 10169. https://doi.org/10.3390/ijms251810169






