The Antidepressant Drug Amitriptyline Affects Human SH-SY5Y Neuroblastoma Cell Proliferation and Modulates Autophagy
Abstract
1. Introduction
2. Results
2.1. Amitriptyline Induced a Concentration and Time-Dependent Reduction in Cell Viability in SH-SY5Y Cultures
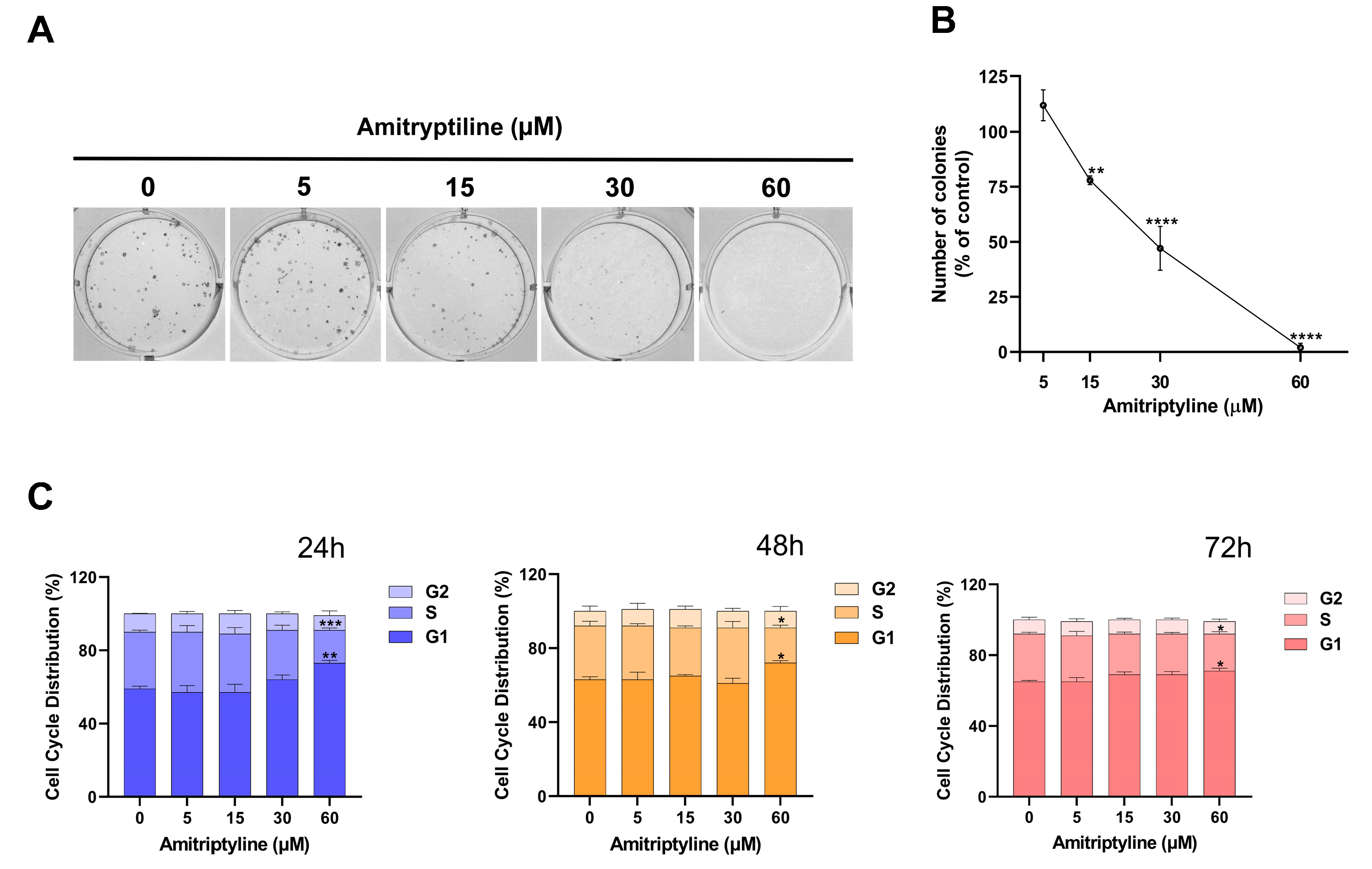
2.2. Amitriptyline Reduced SH-SY5Y Clonogenic Capacity
2.3. Autophagy Is Modulated in SH-SY5Y Cell Cultures Exposed to Amitriptyline
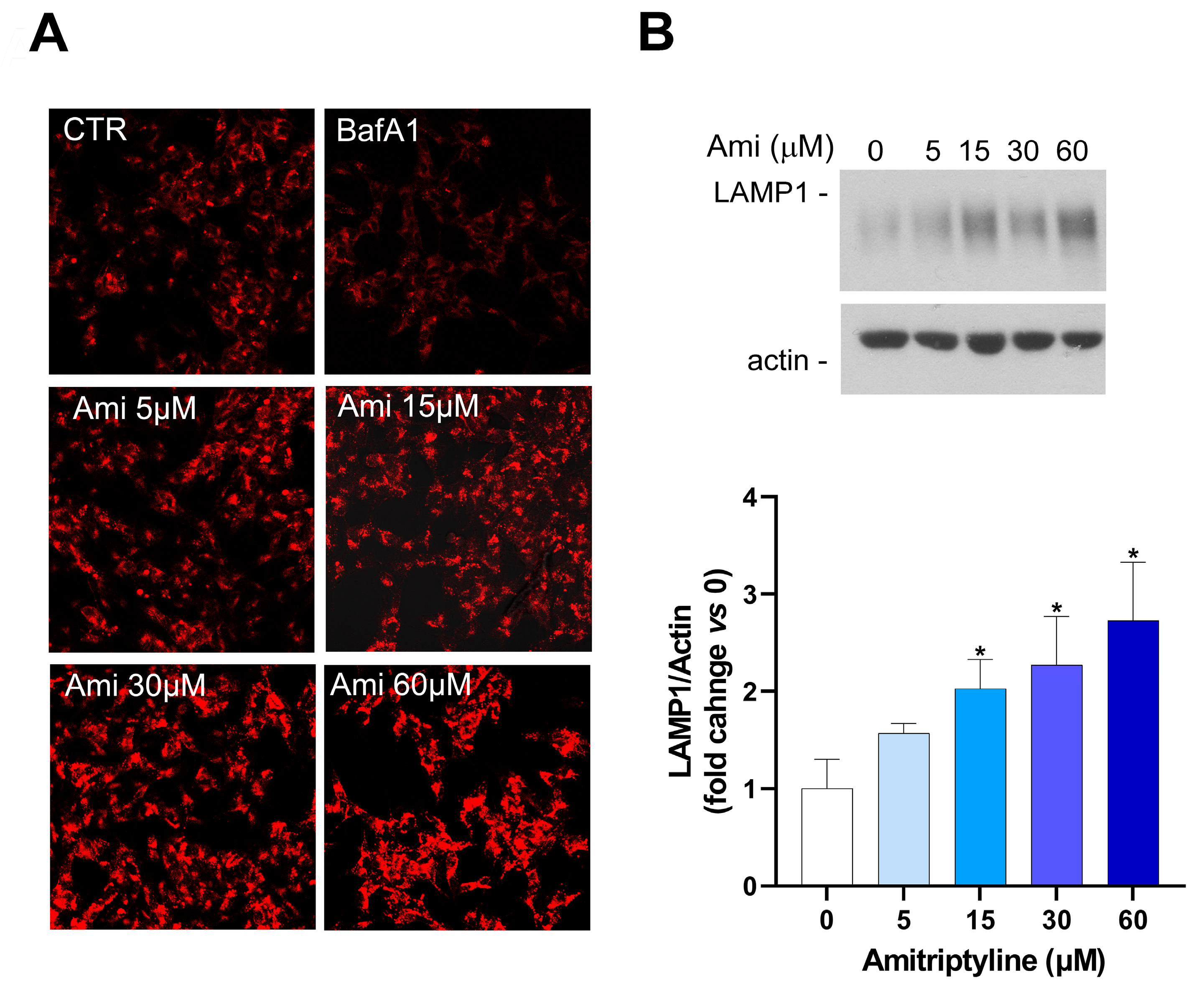
2.4. Amitriptyline Does Not Affect Lysosomal pH but Induces Lysosomes Accumulation
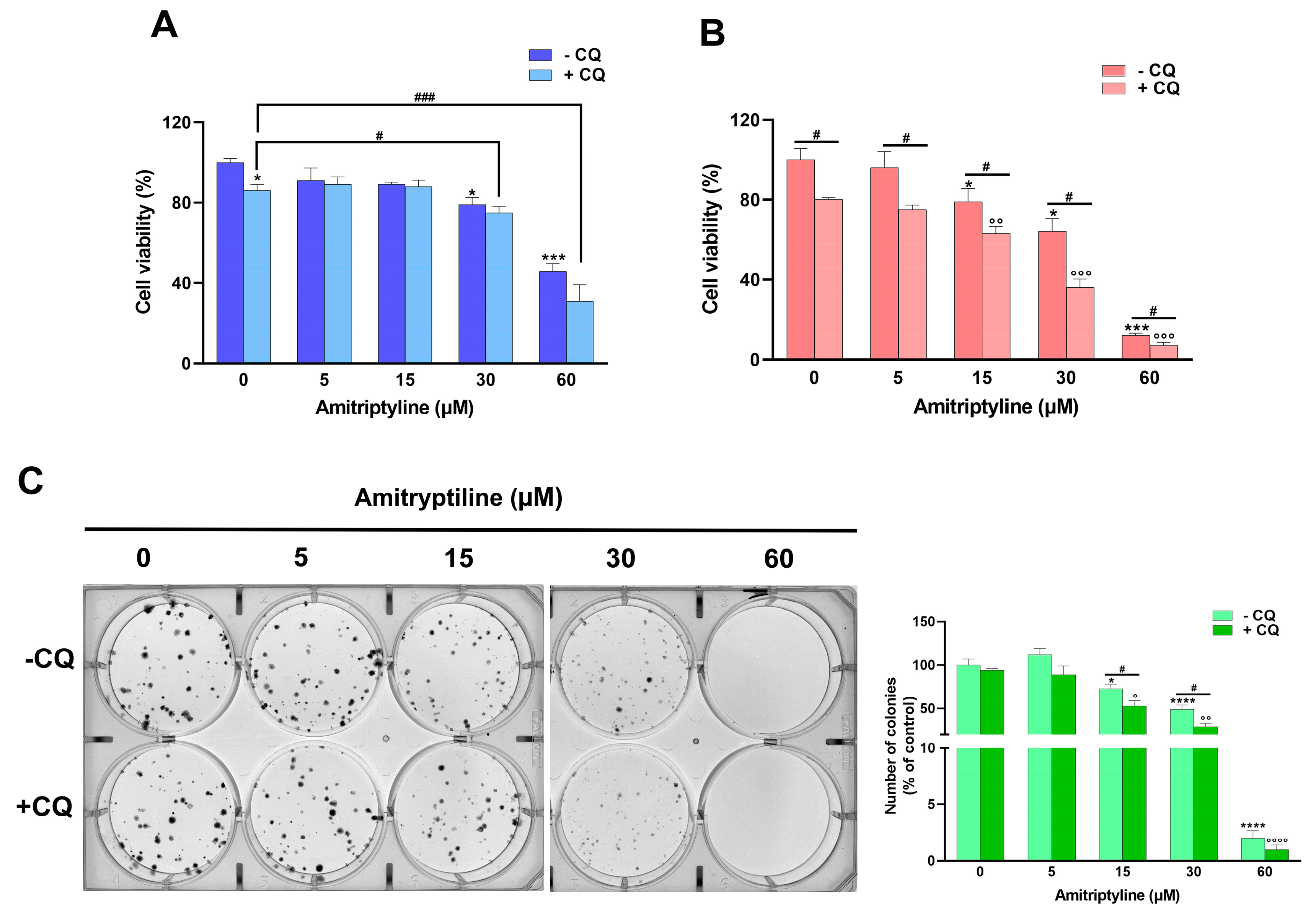
2.5. Autophagy Modulation Does Not Take Part to the Cytotoxic Effects of Amitriptyline
2.6. Reduced Clonogenic Capacity in Amitriptyline Treated Cells Does Not Depend on Autophagy Modulation
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Reagents
5.2. Cell Cultures and Treatments
5.3. Cell Viability Study
5.4. Immunocytochemistry
5.5. Phase-Contrast Microscopy, Measurement of Cells Confluence and Neurites Count
5.6. Live-Cell Labeling of Acidic Compartments
5.7. TUNEL Assay
5.8. Protein Extraction and Western Blot Analysis
5.9. Clonogenic Assay
5.10. Cell Cycle Analysis
5.11. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Friedrich, M.J. Depression Is the Leading Cause of Disability Around the World. JAMA 2017, 317, 1517. [Google Scholar] [CrossRef] [PubMed]
- Wan-Fei, K.; Hassan, S.T.S.; Sann, L.M.; Ismail, S.I.F.; Raman, R.A.; Ibrahim, F. Depression, anxiety and quality of life in stroke survivors and their family caregivers: A pilot study using an actor/partner interdependence model. Electron. Physician 2017, 9, 4924–4933. [Google Scholar] [CrossRef] [PubMed]
- Guekht, A. Epilepsy, Comorbidities and Treatments. Curr. Pharm. Des. 2017, 23, 5702–5726. [Google Scholar] [CrossRef]
- Brozek, P.; Brachmanska, M.; Rabiczko, K.; Bulska, W.; Ciulkowicz, M.; Krzystanek, E. Depression, sleep disturbances and anxiety in patients with relapsing-remitting multiple sclerosis: A longitudinal cohort observation. Psychiatr. Danub. 2017, 29, 464–468. [Google Scholar]
- Baquero, M.; Martín, N. Depressive symptoms in neurodegenerative diseases. World J. Clin. Cases 2015, 3, 682–693. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Chan, M.; Bhatti, H.; Halton, M.; Grassi, L.; Johansen, C.; Meader, N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011, 12, 160–174. [Google Scholar] [CrossRef]
- Bortolato, B.; Hyphantis, T.N.; Valpione, S.; Perini, G.; Maes, M.; Morris, G.; Kubera, M.; Köhler, C.A.; Fernandes, B.S.; Stubbs, B.; et al. Depression in cancer: The many biobehavioral pathways driving tumor progression. Cancer Treat. Rev. 2017, 52, 58–70. [Google Scholar] [CrossRef] [PubMed]
- Becker, M.; Weinberger, T.; Chandy, A.; Schmukler, S. Depression during Pregnancy and Postpartum. Curr. Psychiatry Rep. 2016, 18, 32. [Google Scholar] [CrossRef]
- Martínez-Paredes, J.F.; Jácome-Pérez, N. Depression in Pregnancy. Rev. Colomb. Psiquiatr. 2019, 48, 58–65. [Google Scholar] [CrossRef]
- Szpunar, M.J.; Malaktaris, A.; Baca, S.A.; Hauger, R.L.; Lang, A.J. Are alterations in estradiol, cortisol, and inflammatory cytokines associated with depression during pregnancy and postpartum? An exploratory study. Brain Behav. Immun.-Health 2021, 16, 100309. [Google Scholar] [CrossRef]
- Comorbid depression in medical diseases. Nat. Rev. Dis. Primers 2020, 6, 70. [CrossRef] [PubMed]
- Karrouri, R.; Hammani, Z.; Benjelloun, R.; Otheman, Y. Major depressive disorder: Validated treatments and future challenges. World J. Clin. Cases 2021, 9, 9350–9367. [Google Scholar] [CrossRef] [PubMed]
- Cherrie, M.; Curtis, S.; Baranyi, G.; McTaggart, S.; Cunningham, N.; Licence, K.; Dibben, C.; Bambra, C.; Pearce, J. Use of sequence analysis for classifying individual antidepressant trajectories to monitor population mental health. BMC Psychiatry 2020, 20, 551. [Google Scholar] [CrossRef] [PubMed]
- Kleine, R.; Galimov, A.; Hanewinkel, R.; Unger, J.; Sussman, S.; Hansen, J. Impact of the COVID-19 pandemic on young people with and without pre-existing mental health problems. Sci. Rep. 2023, 13, 6111. [Google Scholar] [CrossRef] [PubMed]
- Ferwana, I.; Varshney, L.R. The impact of COVID-19 lockdowns on mental health patient populations in the United States. Sci. Rep. 2024, 14, 5689. [Google Scholar] [CrossRef] [PubMed]
- Bonilla-Jaime, H.; Sánchez-Salcedo, J.A.; Estevez-Cabrera, M.M.; Molina-Jiménez, T.; Cortes-Altamirano, J.L.; Alfaro-Rodríguez, A. Depression and Pain: Use of Antidepressants. Curr. Neuropharmacol. 2022, 20, 384–402. [Google Scholar] [CrossRef]
- Feighner, J.P. Overview of antidepressants currently used to treat anxiety disorders. J. Clin. Psychiatry 1999, 60, 18–22. [Google Scholar]
- Liu, Y.; Xu, X.; Dong, M.; Jia, S.; Wei, Y. Treatment of insomnia with tricyclic antidepressants: A meta-analysis of polysomnographic randomized controlled trials. Sleep Med. 2017, 34, 126–133. [Google Scholar] [CrossRef]
- Burch, R. Antidepressants for Preventive Treatment of Migraine. Curr. Treat. Options Neurol. 2019, 21, 18. [Google Scholar] [CrossRef]
- Scuteri, D.; Vulnera, M.; Piro, B.; Bossio, R.B.; Morrone, L.A.; Sandrini, G.; Tamburin, S.; Tonin, P.; Bagetta, G.; Corasaniti, M.T. Pattern of treatment of behavioural and psychological symptoms of dementia and pain: Evidence on pharmacoutilization from a large real-world sample and from a centre for cognitive disturbances and dementia. Eur. J. Clin. Pharmacol. 2021, 77, 241–249. [Google Scholar] [CrossRef]
- Pearlstein, T. Selective serotonin reuptake inhibitors for premenstrual dysphoric disorder: The emerging gold standard? Drugs 2002, 62, 1869–1885. [Google Scholar] [CrossRef] [PubMed]
- Maidment, I.D. The use of antidepressants to treat attention deficit hyperactivity disorder in adults. J. Psychopharmacol. 2003, 17, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Janssen, P.; Vos, R.; Tack, J. The influence of citalopram on interdigestive gastrointestinal motility in man. Aliment. Pharmacol. Ther. 2010, 32, 289–295. [Google Scholar] [CrossRef]
- van Kerrebroeck, P.; Abrams, P.; Lange, R.; Slack, M.; Wyndaele, J.J.; Yalcin, I.; Bump, R.C. Duloxetine versus placebo in the treatment of European and Canadian women with stress urinary incontinence. BJOG Int. J. Obstet. Gynaecol. 2004, 111, 249–257. [Google Scholar] [CrossRef]
- Zheng, Y.; Chang, X.; Huang, Y.; He, D. The application of antidepressant drugs in cancer treatment. Biomed. Pharmacother. Biomed. Pharmacother. 2023, 157, 113985. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Yang, X.; Yu, B. Repurposing antidepressants for anticancer drug discovery. Drug Discov. Today 2022, 27, 1924–1935. [Google Scholar] [CrossRef]
- Bielecka, A.M.; Obuchowicz, E. Antidepressant drugs as a complementary therapeutic strategy in cancer. Exp. Biol. Med. 2013, 238, 849–858. [Google Scholar] [CrossRef]
- Lv, G.B.; Wang, T.T.; Zhu, H.L.; Wang, H.K.; Sun, W.; Zhao, L.F. Vortioxetine induces apoptosis and autophagy of gastric cancer AGS cells via the PI3K/AKT pathway. FEBS Open Bio 2020, 10, 2157–2165. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Qiu, Y.; Yang, L.; Peng, L.; Xia, Z.; Hou, L.N.; Fang, C.; Qi, H.; Chen, H.Z. Desipramine induces apoptosis in rat glioma cells via endoplasmic reticulum stress-dependent CHOP pathway. J. Neuro-Oncol. 2011, 101, 41–48. [Google Scholar] [CrossRef]
- Zafir, A.; Ara, A.; Banu, N. Invivo antioxidant status: A putative target of antidepressant action. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2009, 33, 220–228. [Google Scholar] [CrossRef]
- Kannen, V.; Hintzsche, H.; Zanette, D.L.; Silva, W.A., Jr.; Garcia, S.B.; Waaga-Gasser, A.M.; Stopper, H. Antiproliferative effects of fluoxetine on colon cancer cells and in a colonic carcinogen mouse model. PLoS ONE 2012, 7, e50043. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.K.; Chen, H.W.; Chiang, I.T.; Chen, C.C.; Liao, J.F.; Su, T.P.; Tung, C.Y.; Uchitomi, Y.; Hwang, J.J. Mirtazapine inhibits tumor growth via immune response and serotonergic system. PLoS ONE 2012, 7, e38886. [Google Scholar] [CrossRef] [PubMed]
- Hamon, M.; Blier, P. Monoamine neurocircuitry in depression and strategies for new treatments. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2013, 45, 54–63. [Google Scholar] [CrossRef]
- Thour, A.; Marwaha, R. Amitriptyline. In StatPearls; StatPearls Publishing Copyright: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK537225/ (accessed on 22 September 2024).
- Dopheide, J.A. Recognizing and treating depression in children and adolescents. Am. J. Health-Syst. Pharm. 2006, 63, 233–243. [Google Scholar] [CrossRef]
- Radley, D.C.; Finkelstein, S.N.; Stafford, R.S. Off-label prescribing among office-based physicians. Arch. Intern. Med. 2006, 166, 1021–1026. [Google Scholar] [CrossRef]
- Tesfaye, S.; Sloan, G.; Petrie, J.; White, D.; Bradburn, M.; Julious, S.; Rajbhandari, S.; Sharma, S.; Rayman, G.; Gouni, R.; et al. Comparison of amitriptyline supplemented with pregabalin, pregabalin supplemented with amitriptyline, and duloxetine supplemented with pregabalin for the treatment of diabetic peripheral neuropathic pain (OPTION-DM): A multicentre, double-blind, randomised crossover trial. Lancet 2022, 400, 680–690. [Google Scholar] [CrossRef] [PubMed]
- Farag, H.M.; Yunusa, I.; Goswami, H.; Sultan, I.; Doucette, J.A.; Eguale, T. Comparison of Amitriptyline and US Food and Drug Administration-Approved Treatments for Fibromyalgia: A Systematic Review and Network Meta-analysis. JAMA Netw. Open 2022, 5, e2212939. [Google Scholar] [CrossRef]
- Gonzalez-Martinez, A.; Guerrero-Peral, Á.L.; Arias-Rivas, S.; Silva, L.; Sierra, Á.; Gago-Veiga, A.B.; García-Azorín, D. Amitriptyline for post-COVID headache: Effectiveness, tolerability, and response predictors. J. Neurol. 2022, 269, 5702–5709. [Google Scholar] [CrossRef]
- Mizushima, N. Autophagy: Process and function. Genes Dev. 2007, 21, 2861–2873. [Google Scholar] [CrossRef]
- Rein, T. Is Autophagy Involved in the Diverse Effects of Antidepressants? Cells 2019, 8, 44. [Google Scholar] [CrossRef]
- Shao, S.; Zhuang, X.; Zhang, L.; Qiao, T. Antidepressants Fluoxetine Mediates Endoplasmic Reticulum Stress and Autophagy of Non-Small Cell Lung Cancer Cells Through the ATF4-AKT-mTOR Signaling Pathway. Front. Pharmacol. 2022, 13, 904701. [Google Scholar] [CrossRef] [PubMed]
- Chinnapaka, S.; Bakthavachalam, V.; Munirathinam, G. Repurposing antidepressant sertraline as a pharmacological drug to target prostate cancer stem cells: Dual activation of apoptosis and autophagy signaling by deregulating redox balance. Am. J. Cancer Res. 2020, 10, 2043–2065. [Google Scholar] [PubMed]
- Hwang, H.Y.; Shim, J.S.; Kim, D.; Kwon, H.J. Antidepressant drug sertraline modulates AMPK-MTOR signaling-mediated autophagy via targeting mitochondrial VDAC1 protein. Autophagy 2021, 17, 2783–2799. [Google Scholar] [CrossRef] [PubMed]
- Cavaliere, F.; Fornarelli, A.; Bertan, F.; Russo, R.; Marsal-Cots, A.; Morrone, L.A.; Adornetto, A.; Corasaniti, M.T.; Bano, D.; Bagetta, G.; et al. The tricyclic antidepressant clomipramine inhibits neuronal autophagic flux. Sci. Rep. 2019, 9, 4881. [Google Scholar] [CrossRef]
- Su, J.M.; Wang, L.Y.; Liang, Y.L.; Zha, X.L. Role of cell adhesion signal molecules in hepatocellular carcinoma cell apoptosis. World J. Gastroenterol. 2005, 11, 4667–4673. [Google Scholar] [CrossRef]
- Suzanne, M.; Steller, H. Letting go: Modification of cell adhesion during apoptosis. J. Biol. 2009, 8, 49. [Google Scholar] [CrossRef]
- He, L.; Fu, Y.; Tian, Y.; Wang, X.; Zhou, X.; Ding, R.B.; Qi, X.; Bao, J. Antidepressants as Autophagy Modulators for Cancer Therapy. Molecules 2023, 28, 7594. [Google Scholar] [CrossRef]
- Kwon, Y.; Bang, Y.; Moon, S.H.; Kim, A.; Choi, H.J. Amitriptyline interferes with autophagy-mediated clearance of protein aggregates via inhibiting autophagosome maturation in neuronal cells. Cell Death Dis. 2020, 11, 874. [Google Scholar] [CrossRef]
- Rossi, M.; Munarriz, E.R.; Bartesaghi, S.; Milanese, M.; Dinsdale, D.; Guerra-Martin, M.A.; Bampton, E.T.; Glynn, P.; Bonanno, G.; Knight, R.A.; et al. Desmethylclomipramine induces the accumulation of autophagy markers by blocking autophagic flux. J. Cell Sci. 2009, 122, 3330–3339. [Google Scholar] [CrossRef]
- Gassen, N.C.; Hartmann, J.; Schmidt, M.V.; Rein, T. FKBP5/FKBP51 enhances autophagy to synergize with antidepressant action. Autophagy 2015, 11, 578–580. [Google Scholar] [CrossRef]
- Zschocke, J.; Zimmermann, N.; Berning, B.; Ganal, V.; Holsboer, F.; Rein, T. Antidepressant drugs diversely affect autophagy pathways in astrocytes and neurons--dissociation from cholesterol homeostasis. Neuropsychopharmacology 2011, 36, 1754–1768. [Google Scholar] [CrossRef] [PubMed]
- Zschocke, J.; Rein, T. Antidepressants encounter autophagy in neural cells. Autophagy 2011, 7, 1247–1248. [Google Scholar] [CrossRef] [PubMed]
- Tanida, I.; Ueno, T.; Kominami, E. LC3 conjugation system in mammalian autophagy. Int. J. Biochem. Cell Biol. 2004, 36, 2503–2518. [Google Scholar] [CrossRef]
- Klionsky, D.J.; Elazar, Z.; Seglen, P.O.; Rubinsztein, D.C. Does bafilomycin A1 block the fusion of autophagosomes with lysosomes? Autophagy 2008, 4, 849–850. [Google Scholar] [CrossRef] [PubMed]
- Funk, R.S.; Krise, J.P. Cationic amphiphilic drugs cause a marked expansion of apparent lysosomal volume: Implications for an intracellular distribution-based drug interaction. Mol. Pharm. 2012, 9, 1384–1395. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, I.; Clemmensen, K.K.B.; Fogde, D.L.; Dietrich, T.N.; Giacobini, J.D.; Bilgin, M.; Jäättelä, M.; Maeda, K. Cationic amphiphilic drugs induce accumulation of cytolytic lysoglycerophospholipids in the lysosomes of cancer cells and block their recycling into common membrane glycerophospholipids. Mol. Biol. Cell 2024, 35, ar25. [Google Scholar] [CrossRef]
- Vater, M.; Möckl, L.; Gormanns, V.; Schultz Fademrecht, C.; Mallmann, A.M.; Ziegart-Sadowska, K.; Zaba, M.; Frevert, M.L.; Bräuchle, C.; Holsboer, F.; et al. New insights into the intracellular distribution pattern of cationic amphiphilic drugs. Sci. Rep. 2017, 7, 44277. [Google Scholar] [CrossRef]
- Chazotte, B. Labeling lysosomes in live cells with LysoTracker. Cold Spring Harb. Protoc. 2011, 2011, pdb.prot5571. [Google Scholar] [CrossRef]
- Yoshimori, T.; Yamamoto, A.; Moriyama, Y.; Futai, M.; Tashiro, Y. Bafilomycin A1, a specific inhibitor of vacuolar-type H(+)-ATPase, inhibits acidification and protein degradation in lysosomes of cultured cells. J. Biol. Chem. 1991, 266, 17707–17712. [Google Scholar] [CrossRef]
- Frake, R.A.; Ricketts, T.; Menzies, F.M.; Rubinsztein, D.C. Autophagy and neurodegeneration. J. Clin. Investig. 2015, 125, 65–74. [Google Scholar] [CrossRef]
- Yun, C.W.; Lee, S.H. The Roles of Autophagy in Cancer. Int. J. Mol. Sci. 2018, 19, 3466. [Google Scholar] [CrossRef] [PubMed]
- Adornetto, A.; Parisi, V.; Morrone, L.A.; Corasaniti, M.T.; Bagetta, G.; Tonin, P.; Russo, R. The Role of Autophagy in Glaucomatous Optic Neuropathy. Front. Cell Dev. Biol. 2020, 8, 121. [Google Scholar] [CrossRef] [PubMed]
- Berliocchi, L.; Maiarù, M.; Varano, G.P.; Russo, R.; Corasaniti, M.T.; Bagetta, G.; Tassorelli, C. Spinal autophagy is differently modulated in distinct mouse models of neuropathic pain. Mol. Pain 2015, 11, 3. [Google Scholar] [CrossRef]
- Shi, Q.; Pei, F.; Silverman, G.A.; Pak, S.C.; Perlmutter, D.H.; Liu, B.; Bahar, I. Mechanisms of Action of Autophagy Modulators Dissected by Quantitative Systems Pharmacology Analysis. Int. J. Mol. Sci. 2020, 21, 2855. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xu, H.L.; Liu, Y.X.; An, N.; Zhao, S.; Bao, J.K. Autophagy modulation as a target for anticancer drug discovery. Acta Pharmacol. Sin. 2013, 34, 612–624. [Google Scholar] [CrossRef]
- Gao, L.; Jauregui, C.E.; Teng, Y. Targeting autophagy as a strategy for drug discovery and therapeutic modulation. Future Med. Chem. 2017, 9, 335–345. [Google Scholar] [CrossRef]
- Arimochi, H.; Morita, K. Characterization of cytotoxic actions of tricyclic antidepressants on human HT29 colon carcinoma cells. Eur. J. Pharmacol. 2006, 541, 17–23. [Google Scholar] [CrossRef]
- Xia, Z.; Bergstrand, A.; DePierre, J.W.; Nässberger, L. The antidepressants imipramine, clomipramine, and citalopram induce apoptosis in human acute myeloid leukemia HL-60 cells via caspase-3 activation. J. Biochem. Mol. Toxicol. 1999, 13, 338–347. [Google Scholar] [CrossRef]
- Levkovitz, Y.; Gil-Ad, I.; Zeldich, E.; Dayag, M.; Weizman, A. Differential induction of apoptosis by antidepressants in glioma and neuroblastoma cell lines: Evidence for p-c-Jun, cytochrome c, and caspase-3 involvement. J. Mol. Neurosci. 2005, 27, 29–42. [Google Scholar] [CrossRef]
- Rácz, B.; Spengler, G. Repurposing Antidepressants and Phenothiazine Antipsychotics as Efflux Pump Inhibitors in Cancer and Infectious Diseases. Antibiotics 2023, 12, 137. [Google Scholar] [CrossRef]
- Varga, A.; Nugel, H.; Baehr, R.; Marx, U.; Hevér, A.; Nacsa, J.; Ocsovszky, I.; Molnar, J. Reversal of multidrug resistance by amitriptyline in vitro. Anticancer Res. 1996, 16, 209–211. [Google Scholar] [PubMed]
- O’Brien, F.E.; Dinan, T.G.; Griffin, B.T.; Cryan, J.F. Interactions between antidepressants and P-glycoprotein at the blood-brain barrier: Clinical significance of in vitro and in vivo findings. Br. J. Pharmacol. 2012, 165, 289–312. [Google Scholar] [CrossRef] [PubMed]
- Asensi-Cantó, A.; Rodríguez-Braun, E.; Beltrán-Videla, A.; Hurtado, A.M.; Conesa-Zamora, P. Effects of imipramine on cancer patients over-expressing Fascin1; description of the HITCLIF clinical trial. Front. Oncol. 2023, 13, 1238464. [Google Scholar] [CrossRef] [PubMed]
- Cordero, M.D.; Sánchez-Alcázar, J.A.; Bautista-Ferrufino, M.R.; Carmona-López, M.I.; Illanes, M.; Ríos, M.J.; Garrido-Maraver, J.; Alcudia, A.; Navas, P.; de Miguel, M. Acute oxidant damage promoted on cancer cells by amitriptyline in comparison with some common chemotherapeutic drugs. Anti-Cancer Drugs 2010, 21, 932–944. [Google Scholar] [CrossRef]
- Motafeghi, F.; Shahsavari, R.; Mortazavi, P.; Shokrzadeh, M. Anticancer effect of paroxetine and amitriptyline on HT29 and A549 cell lines. Toxicol. In Vitro 2023, 87, 105532. [Google Scholar] [CrossRef]
- Huang, Y.H.; Yeh, C.T. Anticancer Effects of Antidepressants in Hepatocellular Carcinoma Cells. Anticancer Res. 2023, 43, 1201–1206. [Google Scholar] [CrossRef]
- Mao, X.; Hou, T.; Cao, B.; Wang, W.; Li, Z.; Chen, S.; Fei, M.; Hurren, R.; Gronda, M.; Wu, D.; et al. The tricyclic antidepressant amitriptyline inhibits D-cyclin transactivation and induces myeloma cell apoptosis by inhibiting histone deacetylases: In vitro and in silico evidence. Mol. Pharmacol. 2011, 79, 672–680. [Google Scholar] [CrossRef]
- Pula, G.; Pistilli, A.; Montagnoli, C.; Stabile, A.M.; Rambotti, M.G.; Rende, M. The tricyclic antidepressant amitriptyline is cytotoxic to HTB114 human leiomyosarcoma and induces p75NTR-dependent apoptosis. Anti-Cancer Drugs 2013, 24, 899–910. [Google Scholar] [CrossRef]
- Zinnah, K.M.A.; Park, S.Y. Sensitizing TRAIL-resistant A549 lung cancer cells and enhancing TRAIL-induced apoptosis with the antidepressant amitriptyline. Oncol. Rep. 2021, 46, 144. [Google Scholar] [CrossRef]
- Evason, K.J.; Francisco, M.T.; Juric, V.; Balakrishnan, S.; Lopez Pazmino, M.D.P.; Gordan, J.D.; Kakar, S.; Spitsbergen, J.; Goga, A.; Stainier, D.Y. Identification of Chemical Inhibitors of β-Catenin-Driven Liver Tumorigenesis in Zebrafish. PLoS Genet. 2015, 11, e1005305. [Google Scholar] [CrossRef]
- Higgins, S.C.; Pilkington, G.J. The in vitro effects of tricyclic drugs and dexamethasone on cellular respiration of malignant glioma. Anticancer Res. 2010, 30, 391–397. [Google Scholar] [PubMed]
- Lee, M.Y.; Hong, S.; Kim, N.; Shin, K.S.; Kang, S.J. Tricyclic Antidepressants Amitriptyline and Desipramine Induced Neurotoxicity Associated with Parkinson’s Disease. Mol. Cells 2015, 38, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Villanueva-Paz, M.; Cordero, M.D.; Pavón, A.D.; Vega, B.C.; Cotán, D.; De la Mata, M.; Oropesa-Ávila, M.; Alcocer-Gomez, E.; de Lavera, I.; Garrido-Maraver, J.; et al. Amitriptyline induces mitophagy that precedes apoptosis in human HepG2 cells. Genes Cancer 2016, 7, 260–277. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Che, X.; Zheng, Q.; Wu, A.; Pan, K.; Shao, A.; Wu, Q.; Zhang, J.; Hong, Y. Caspases: A molecular switch node in the crosstalk between autophagy and apoptosis. Int. J. Biol. Sci. 2014, 10, 1072–1083. [Google Scholar] [CrossRef] [PubMed]
- Ashoor, R.; Yafawi, R.; Jessen, B.; Lu, S. The contribution of lysosomotropism to autophagy perturbation. PLoS ONE 2013, 8, e82481. [Google Scholar] [CrossRef]
- Guan, Y.; Li, X.; Umetani, M.; Boini, K.M.; Li, P.L.; Zhang, Y. Tricyclic antidepressant amitriptyline inhibits autophagic flux and prevents tube formation in vascular endothelial cells. Basic Clin. Pharmacol. Toxicol. 2019, 124, 370–384. [Google Scholar] [CrossRef]
- Kazmi, F.; Hensley, T.; Pope, C.; Funk, R.S.; Loewen, G.J.; Buckley, D.B.; Parkinson, A. Lysosomal sequestration (trapping) of lipophilic amine (cationic amphiphilic) drugs in immortalized human hepatocytes (Fa2N-4 cells). Drug Metab. Dispos. 2013, 41, 897–905. [Google Scholar] [CrossRef]
- Nadanaciva, S.; Lu, S.; Gebhard, D.F.; Jessen, B.A.; Pennie, W.D.; Will, Y. A high content screening assay for identifying lysosomotropic compounds. Toxicol. In Vitro 2011, 25, 715–723. [Google Scholar] [CrossRef]
- Kornhuber, J.; Henkel, A.W.; Groemer, T.W.; Städtler, S.; Welzel, O.; Tripal, P.; Rotter, A.; Bleich, S.; Trapp, S. Lipophilic cationic drugs increase the permeability of lysosomal membranes in a cell culture system. J. Cell. Physiol. 2010, 224, 152–164. [Google Scholar] [CrossRef]
- Yim, W.W.; Mizushima, N. Lysosome biology in autophagy. Cell Discov. 2020, 6, 6. [Google Scholar] [CrossRef]
- Xu, J.; Gu, J.; Pei, W.; Zhang, Y.; Wang, L.; Gao, J. The role of lysosomal membrane proteins in autophagy and related diseases. FEBS J. 2023, 291, 3762–3785. [Google Scholar] [CrossRef] [PubMed]
- Gentile, D.; Berliocchi, L.; Russo, R.; Bagetta, G.; Corasaniti, M.T. Effects of the autophagy modulators d-limonene and chloroquine on vimentin levels in SH-SY5Y cells. Biochem. Biophys. Res. Commun. 2020, 533, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Russo, R.; Cassiano, M.G.V.; Ciociaro, A.; Adornetto, A.; Varano, G.P.; Chiappini, C.; Berliocchi, L.; Tassorelli, C.; Bagetta, G.; Corasaniti, M.T. Role of D-Limonene in autophagy induced by bergamot essential oil in SH-SY5Y neuroblastoma cells. PLoS ONE 2014, 9, e113682. [Google Scholar] [CrossRef] [PubMed]
- Corasaniti, M.T.; Bilotta, A.; Strongoli, M.C.; Navarra, M.; Bagetta, G.; Di Renzo, G. HIV-1 coat protein gp120 stimulates interleukin-1beta secretion from human neuroblastoma cells: Evidence for a role in the mechanism of cell death. Br. J. Pharmacol. 2001, 134, 1344–1350. [Google Scholar] [CrossRef] [PubMed]
- Yordanov, Y.I. Hep G2 cell culture confluence measurement in phase-contrast micrographs–a user-friendly, open-source software-based approach. Toxicol. Mech. Methods 2020, 30, 146–152. [Google Scholar] [CrossRef]
- Pemberton, K.; Mersman, B.; Xu, F. Using ImageJ to Assess Neurite Outgrowth in Mammalian Cell Cultures: Research Data Quantification Exercises in Undergraduate Neuroscience Lab. J. Undergrad. Neurosci. Educ. 2018, 16, A186–A194. [Google Scholar]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adornetto, A.; Laganà, M.L.; Satriano, A.; Licastro, E.; Corasaniti, M.T.; Bagetta, G.; Russo, R. The Antidepressant Drug Amitriptyline Affects Human SH-SY5Y Neuroblastoma Cell Proliferation and Modulates Autophagy. Int. J. Mol. Sci. 2024, 25, 10415. https://doi.org/10.3390/ijms251910415
Adornetto A, Laganà ML, Satriano A, Licastro E, Corasaniti MT, Bagetta G, Russo R. The Antidepressant Drug Amitriptyline Affects Human SH-SY5Y Neuroblastoma Cell Proliferation and Modulates Autophagy. International Journal of Molecular Sciences. 2024; 25(19):10415. https://doi.org/10.3390/ijms251910415
Chicago/Turabian StyleAdornetto, Annagrazia, Maria Luisa Laganà, Andrea Satriano, Ester Licastro, Maria Tiziana Corasaniti, Giacinto Bagetta, and Rossella Russo. 2024. "The Antidepressant Drug Amitriptyline Affects Human SH-SY5Y Neuroblastoma Cell Proliferation and Modulates Autophagy" International Journal of Molecular Sciences 25, no. 19: 10415. https://doi.org/10.3390/ijms251910415
APA StyleAdornetto, A., Laganà, M. L., Satriano, A., Licastro, E., Corasaniti, M. T., Bagetta, G., & Russo, R. (2024). The Antidepressant Drug Amitriptyline Affects Human SH-SY5Y Neuroblastoma Cell Proliferation and Modulates Autophagy. International Journal of Molecular Sciences, 25(19), 10415. https://doi.org/10.3390/ijms251910415







