Does the Composition of Gut Microbiota Affect Chronic Kidney Disease? Molecular Mechanisms Contributed to Decreasing Glomerular Filtration Rate
Abstract
1. Introduction
2. Review Methodology
3. What Is Renal Failure?
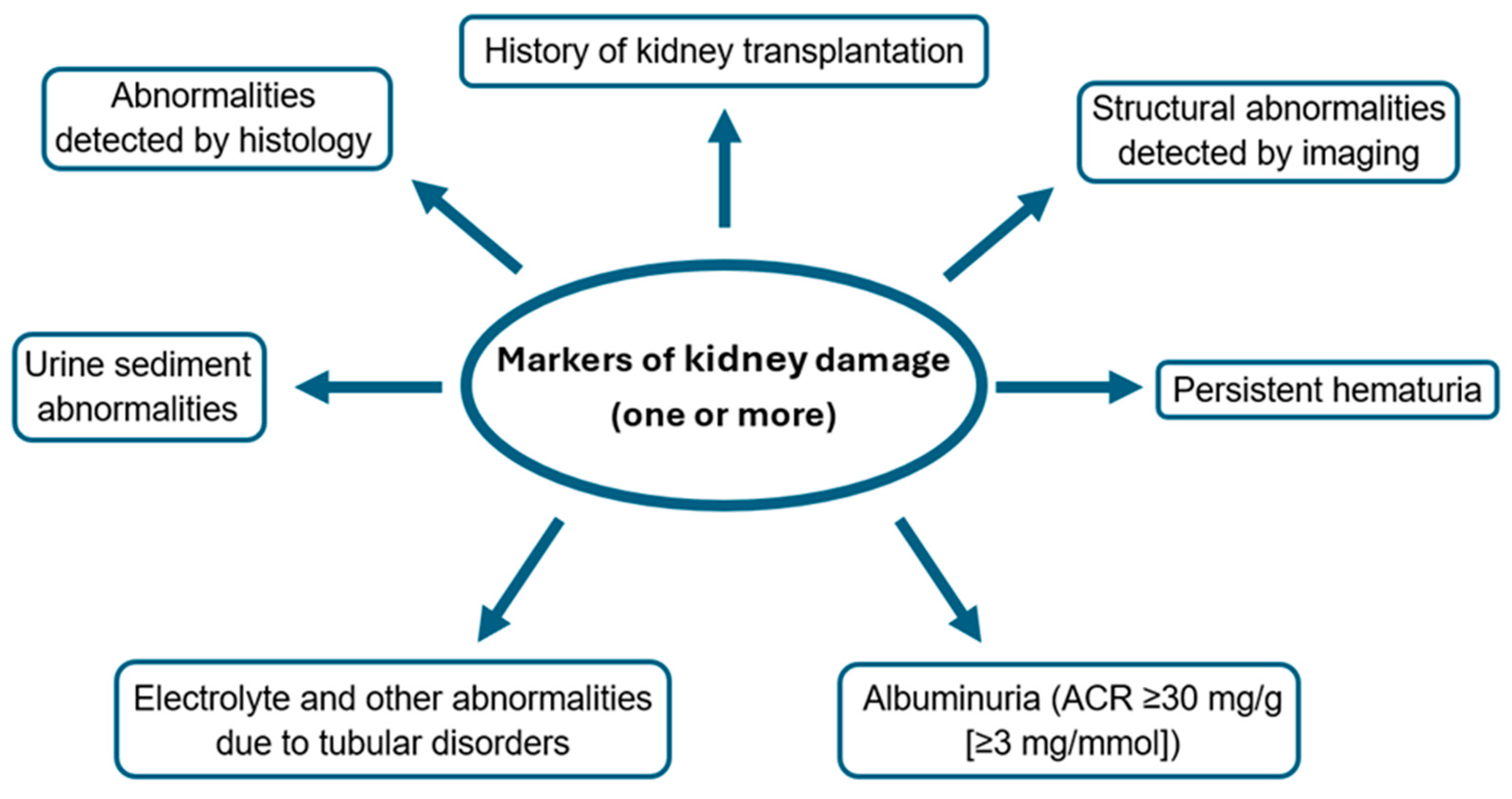
3.1. Definition, Types
3.2. Etiology and Causes
3.3. Standard Treatment
3.3.1. Treatment of Hypertension
3.3.2. Treatment of Diabetes Mellitus
3.3.3. Cardiovascular Disease Risk Reduction
3.4. Complications
4. Molecular Basis of Renal Failure
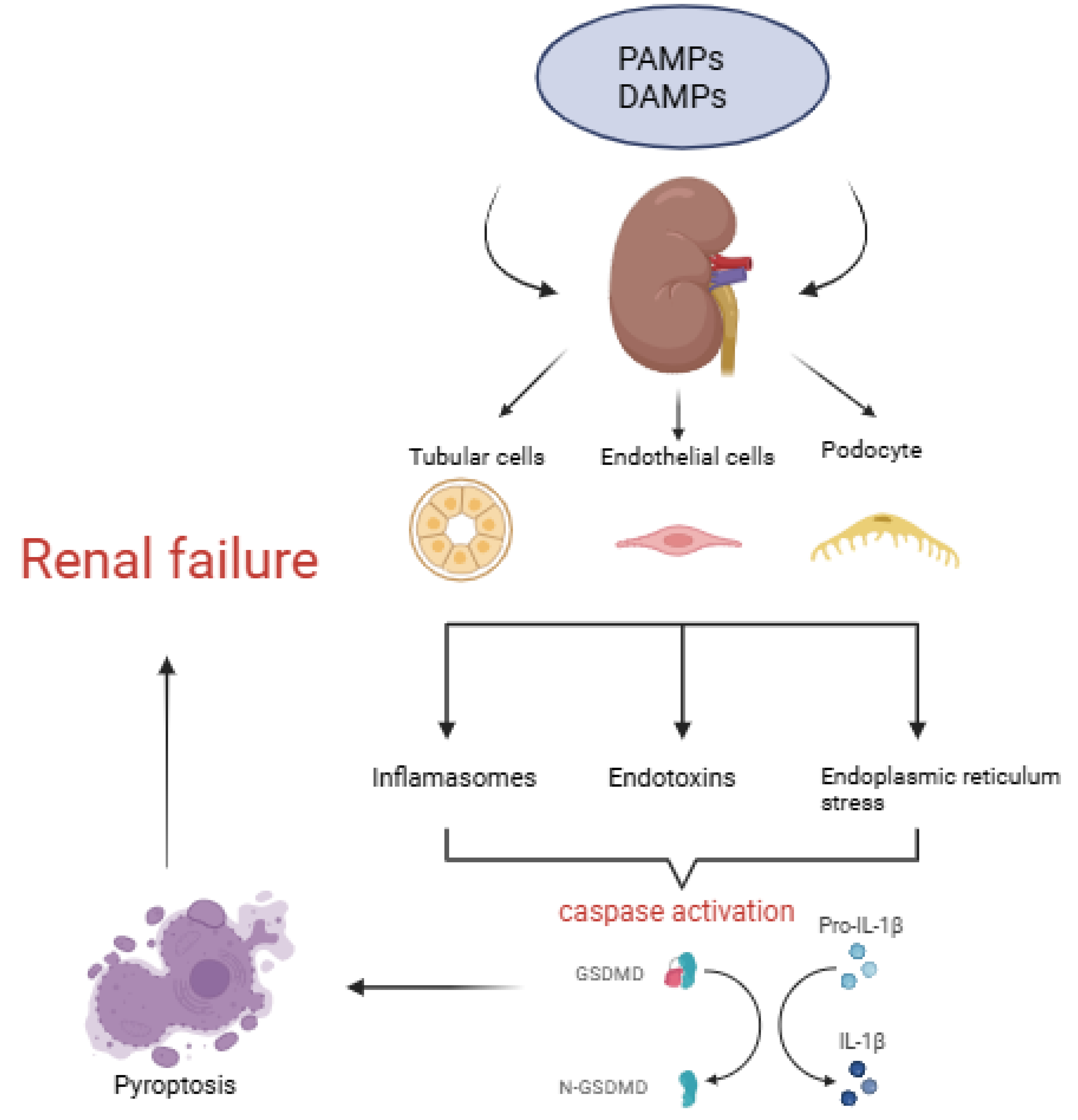
4.1. Programmed Cell Death
4.2. The Co-Occurrence of Obesity and Renal Failure
4.3. Uremic Toxins
5. Association between Chronic Kidney Disease and Gut Microbiota
5.1. Basic Microbiological Information and Molecular Aspects
5.2. Microbiological Assessment and Used Technical Methods
5.3. Quantitative and Qualitative Gut Microbiota Analysis in Patients with CKD and ESRD Compared to the Healthy Population
6. Potential Role of Probiotics in the Treatment of Chronic Kidney Disease
6.1. Gut Dysbiosis and Chronic Kidney Disease—Can We Treat Both?
6.2. What Are Probiotics?
6.3. Probiotics and Renal Failure: Mechanisms of Action
- Reduction in uremic toxins: Probiotics could support a reduction in the production and absorption of uremic toxins by modifying the gut microbiota composition. Research has shown that specific probiotic strains, including Lactobacillus and Bifidobacterium, have the potential to decrease the levels of indoxyl sulfate and p-cresyl sulfate, which may potentially slow the progression of kidney disease [92].
- Improvement of gut barrier function: Renal failure could compromise the integrity of the gut barrier, leading to increased intestinal permeability (leaky gut). Moreover, probiotics could strengthen the gut barrier by promoting the growth of beneficial bacteria that enhance gut integrity. These microorganisms might reduce the translocation of harmful bacteria and toxins from the gut into the bloodstream while also potentially mitigating systemic inflammation and further kidney damage [115].
- Metabolic benefits: Probiotics have the potential to enhance metabolic profiles by increasing insulin sensitivity, reducing oxidative stress, and lowering lipid levels [21].
- Anti-inflammatory effects: Chronic inflammation represents a pivotal element in the advancement of renal failure. Probiotics could exert anti-inflammatory effects by modulating the immune response and reducing the production of pro-inflammatory cytokines, thereby aiding in the protection of kidney tissues from further damage [116].
- Regulation of blood pressure: Hypertension is both a cause and a consequence of renal failure. Some probiotic strains could help regulate blood pressure by producing bioactive peptides that inhibit angiotensin-converting enzyme (ACE), a key regulator of blood pressure. Improved blood pressure control can reduce the stress on the kidneys and slow the progression of kidney disease [117].
6.4. The Use of Probiotics and Synbiotics in Kidney Diseases
6.5. The Use of Probiotics and Synbiotics in Chronic Kidney Disease
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hill, N.R.; Fatoba, S.T.; Oke, J.L.; Hirst, J.A.; O’Callaghan, C.A.; Lasserson, D.S.; Hobbs, F.D.R. Global Prevalence of Chronic Kidney Disease—A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0158765. [Google Scholar] [CrossRef]
- Evans, M.; Lewis, R.D.; Morgan, A.R.; Whyte, M.B.; Hanif, W.; Bain, S.C.; Davies, S.; Dashora, U.; Yousef, Z.; Patel, D.C.; et al. A Narrative Review of Chronic Kidney Disease in Clinical Practice: Current Challenges and Future Perspectives. Adv. Ther. 2021, 39, 33–43. [Google Scholar] [CrossRef]
- Webster, A.C.; Nagler, E.V.; Morton, R.L.; Masson, P. Chronic Kidney Disease. Lancet 2017, 389, 1238–1252. [Google Scholar] [CrossRef]
- Charles, C.; Ferris, A.H. Chronic Kidney Disease. Prim. Care Clin. Off. Pr. 2020, 47, 585–595. [Google Scholar] [CrossRef]
- Anders, H.-J.; Andersen, K.; Stecher, B. The intestinal microbiota, a leaky gut, and abnormal immunity in kidney disease. Kidney Int. 2013, 83, 1010–1016. [Google Scholar] [CrossRef]
- Vanholder, R.; Baurmeister, U.; Brunet, P.; Cohen, G.; Glorieux, G.; Jankowski, J. A Bench to Bedside View of Uremic Toxins. J. Am. Soc. Nephrol. 2008, 19, 863–870. [Google Scholar] [CrossRef]
- Zaimi, M.; Grapsa, E. Current therapeutic approach of chronic kidney disease-mineral and bone disorder. Ther. Apher. Dial. 2024, 28, 671–689. [Google Scholar] [CrossRef]
- Romagnani, P.; Remuzzi, G.; Glassock, R.; Levin, A.; Jager, K.J.; Tonelli, M.; Massy, Z.; Wanner, C.; Anders, H.-J. Chronic kidney disease. Nat. Rev. Dis. Primers. 2017, 3, 17088. [Google Scholar] [CrossRef]
- Krukowski, H.; Valkenburg, S.; Madella, A.-M.; Garssen, J.; van Bergenhenegouwen, J.; Overbeek, S.A.; Huys, G.R.B.; Raes, J.; Glorieux, G. Gut microbiome studies in CKD: Opportunities, pitfalls and therapeutic potential. Nat. Rev. Nephrol. 2022, 19, 87–101. [Google Scholar] [CrossRef]
- Zhang, P.; Wang, X.; Li, S.; Cao, X.; Zou, J.; Fang, Y.; Shi, Y.; Xiang, F.; Shen, B.; Li, Y.; et al. Metagenome-wide analysis uncovers gut microbial signatures and implicates taxon-specific functions in end-stage renal disease. Genome Biol. 2023, 24, 226. [Google Scholar] [CrossRef]
- Wang, H.; Ainiwaer, A.; Song, Y.; Qin, L.; Peng, A.; Bao, H.; Qin, H. Perturbed gut microbiome and fecal and serum metabolomes are associated with chronic kidney disease severity. Microbiome 2023, 11, 3. [Google Scholar] [CrossRef]
- Li, J.; Shen, Y.; Yan, K.; Wang, S.; Jiao, J.; Chi, H.; Zhong, J.-C.; Dong, Y.; Wang, P. The compositional and functional imbalance of the gut microbiota in CKD linked to disease patterns. J. Transl. Med. 2024, 22, 773. [Google Scholar] [CrossRef]
- Tokarek, J.; Budny, E.; Saar, M.; Kućmierz, J.; Młynarska, E.; Rysz, J.; Franczyk, B. Does the Composition of Gut Microbiota Affect Hypertension? Molecular Mechanisms Involved in Increasing Blood Pressure. Int. J. Mol. Sci. 2023, 24, 1377. [Google Scholar] [CrossRef]
- Gurung, M.; Li, Z.; You, H.; Rodrigues, R.; Jump, D.B.; Morgun, A.; Shulzhenko, N. Role of gut microbiota in type 2 diabetes pathophysiology. EBioMedicine 2020, 51, 102590. [Google Scholar] [CrossRef]
- Neuen, B.L.; Heerspink, H.J.; Vart, P.; Claggett, B.L.; Fletcher, R.A.; Arnott, C.; Costa, J.d.O.; Falster, M.O.; Pearson, S.-A.; Mahaffey, K.W.; et al. Estimated Lifetime Cardiovascular, Kidney, and Mortality Benefits of Combination Treatment With SGLT2 Inhibitors, GLP-1 Receptor Agonists, and Nonsteroidal MRA Compared With Conventional Care in Patients With Type 2 Diabetes and Albuminuria. Circulation 2024, 149, 450–462. [Google Scholar] [CrossRef]
- Liu, C.; Yang, L.; Wei, W.; Fu, P. Efficacy of probiotics/synbiotics supplementation in patients with chronic kidney disease: A systematic review and meta-analysis of randomized controlled trials. Front. Nutr. 2024, 11, 1434613. [Google Scholar] [CrossRef]
- Meijers, B.; Evenepoel, P.; Anders, H.-J. Intestinal microbiome and fitness in kidney disease. Nat. Rev. Nephrol. 2019, 15, 531–545. [Google Scholar] [CrossRef]
- Cosola, C.; Rocchetti, M.M.; di Bari, I.; Acquaviva, P.M.; Maranzano, V.; Corciulo, S.; Di Ciaula, A.; Di Palo, D.M.; La Forgia, F.M.; Fontana, S.; et al. An Innovative Synbiotic Formulation Decreases Free Serum Indoxyl Sulfate, Small Intestine Permeability and Ameliorates Gastrointestinal Symptoms in a Randomized Pilot Trial in Stage IIIb-IV CKD Patients. Toxins 2021, 13, 334. [Google Scholar] [CrossRef]
- Lim, P.S.; Wang, H.F.; Lee, M.C.; Chiu, L.-S.; Wu, M.-Y.; Chang, W.-C.; Wu, T.K. The Efficacy of Lactobacillus-Containing Probiotic Supplementation in Hemodialysis Patients: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Ren. Nutr. 2021, 31, 189–198. [Google Scholar] [CrossRef]
- Barrows, I.R.; Ramezani, A.; Raj, D.S. Gut Feeling in AKI. J. Am. Soc. Nephrol. 2015, 26, 1755–1757. [Google Scholar] [CrossRef][Green Version]
- de Araújo, É.M.R.; Meneses, G.C.; Carioca, A.A.F.; Martins, A.M.C.; Daher, E.D.F.; da Silva Junior, G.B. Use of probiotics in patients with chronic kidney disease on hemodialysis: A randomized clinical trial. Braz. J. Nephrol. 2023, 45, 152–161. [Google Scholar] [CrossRef]
- Stevens, P.E.; Ahmed, S.B.; Carrero, J.J.; Foster, B.; Francis, A.; Hall, R.K.; Herrington, W.G.; Hill, G.; Inker, L.A.; Kazancıoğlu, R.; et al. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024, 105, S117–S314. [Google Scholar]
- Bertram, J.F.; Douglas-Denton, R.N.; Diouf, B.; Hughson, M.D.; Hoy, W.E. Human nephron number: Implications for health and disease. Pediatr. Nephrol. 2011, 26, 1529–1533. [Google Scholar] [CrossRef]
- Ibrahim, H.N.; E Rosenberg, M.; Hostetter, T.H. Role of the renin-angiotensin-aldosterone system in the progression of renal disease: A critical review. Semin. Nephrol. 1997, 17, 431–440. [Google Scholar]
- Gagliardini, E.; Conti, S.; Benigni, A.; Remuzzi, G.; Remuzzi, A. Imaging of the Porous Ultrastructure of the Glomerular Epithelial Filtration Slit. J. Am. Soc. Nephrol. 2010, 21, 2081–2089. [Google Scholar] [CrossRef]
- Ruggenenti, P.; Cravedi, P.; Remuzzi, G. Mechanisms and Treatment of CKD. J. Am. Soc. Nephrol. 2012, 23, 1917–1928. [Google Scholar] [CrossRef]
- Durvasula, R.V.; Petermann, A.T.; Hiromura, K.; Blonski, M.; Pippin, J.; Mundel, P.; Pichler, R.; Griffin, S.; Couser, W.G.; Shankland, S.J. Activation of a local tissue angiotensin system in podocytes by mechanical strain. Kidney Int. 2004, 65, 30–39. [Google Scholar] [CrossRef][Green Version]
- Benigni, A.; Gagliardini, E.; Remuzzi, G. Changes in glomerular perm-selectivity induced by angiotensin II imply podocyte dysfunction and slit diaphragm protein rearrangement. Semin. Nephrol. 2004, 24, 131–140. [Google Scholar] [CrossRef]
- Barnes, J.L.; Gorin, Y. Myofibroblast differentiation during fibrosis: Role of NAD(P)H oxidases. Kidney Int. 2011, 79, 944–956. [Google Scholar] [CrossRef]
- Abbate, M.; Zoja, C.; Remuzzi, G. How Does Proteinuria Cause Progressive Renal Damage? J. Am. Soc. Nephrol. 2006, 17, 2974–2984. [Google Scholar] [CrossRef]
- Abbate, M.; Zoja, C.; Morigi, M.; Rottoli, D.; Angioletti, S.; Tomasoni, S.; Zanchi, C.; Longaretti, L.; Donadelli, R.; Remuzzi, G. Transforming Growth Factor-β1 Is Up-Regulated by Podocytes in Response to Excess Intraglomerular Passage of Proteins. Am. J. Pathol. 2002, 161, 2179–2193. [Google Scholar] [CrossRef]
- Johnson, D.W.; Saunders, H.J.; Baxter, R.C.; Field, M.J.; Pollock, C.A. Paracrine stimulation of human renal fibroblasts by proximal tubule cells. Kidney Int. 1998, 54, 747–757. [Google Scholar] [CrossRef]
- Zeisberg, M.; Neilson, E.G. Mechanisms of Tubulointerstitial Fibrosis. J. Am. Soc. Nephrol. 2010, 21, 1819–1834. [Google Scholar] [CrossRef]
- Schlondorff, D.O. Overview of factors contributing to the pathophysiology of progressive renal disease. Kidney Int. 2008, 74, 860–866. [Google Scholar] [CrossRef]
- Liu, Y. New Insights into Epithelial-Mesenchymal Transition in Kidney Fibrosis. J. Am. Soc. Nephrol. 2010, 21, 212–222. [Google Scholar] [CrossRef]
- Lovisa, S.; LeBleu, V.S.; Tampe, B.; Sugimoto, H.; Vadnagara, K.; Carstens, J.L.; Wu, C.-C.; Hagos, Y.; Burckhardt, B.C.; Pentcheva-Hoang, T.; et al. Epithelial-to-mesenchymal transition induces cell cycle arrest and parenchymal damage in renal fibrosis. Nat. Med. 2015, 21, 998–1009. [Google Scholar] [CrossRef]
- Grande, M.T.; Sánchez-Laorden, B.; López-Blau, C.; A De Frutos, C.; Boutet, A.; Arévalo, M.; Rowe, R.G.; Weiss, S.J.; López-Novoa, J.M.; Nieto, M.A. Snail1-induced partial epithelial-to-mesenchymal transition drives renal fibrosis in mice and can be targeted to reverse established disease. Nat. Med. 2015, 21, 989–997. [Google Scholar] [CrossRef]
- Cano, A.; Pérez-Moreno, M.A.; Rodrigo, I.; Locascio, A.; Blanco, M.J.; Del Barrio, M.G.; Portillo, F.; Nieto, M.A. The transcription factor Snail controls epithelial–mesenchymal transitions by repressing E-cadherin expression. Nat. Cell Biol. 2000, 2, 76–83. [Google Scholar] [CrossRef]
- Zhou, B.P.; Deng, J.; Xia, W.; Xu, J.; Li, Y.M.; Gunduz, M.; Hung, M.-C. Dual regulation of Snail by GSK-3β-mediated phosphorylation in control of epithelial–mesenchymal transition. Nat. Cell Biol. 2004, 6, 931–940. [Google Scholar] [CrossRef]
- Widjaja, A.A.; Viswanathan, S.; Shekeran, S.G.; Adami, E.; Lim, W.-W.; Chothani, S.; Tan, J.; Goh, J.W.T.; Chen, H.M.; Lim, S.Y.; et al. Targeting endogenous kidney regeneration using anti-IL11 therapy in acute and chronic models of kidney disease. Nat. Commun. 2022, 13, 7497. [Google Scholar] [CrossRef]
- Huang, S.; Susztak, K. Epithelial Plasticity versus EMT in Kidney Fibrosis. Trends Mol. Med. 2015, 22, 4–6. [Google Scholar] [CrossRef]
- Widjaja, A.A.; Viswanathan, S.; Ting, J.G.W.; Tan, J.; Shekeran, S.G.; Carling, D.; Lim, W.-W.; Cook, S.A. IL11 stimulates ERK/P90RSK to inhibit LKB1/AMPK and activate mTOR initiating a mesenchymal program in stromal, epithelial, and cancer cells. iScience 2022, 25, 104806. [Google Scholar] [CrossRef]
- Strikoudis, A.; Cieślak, A.; Loffredo, L.; Chen, Y.-W.; Patel, N.; Saqi, A.; Lederer, D.J.; Snoeck, H.-W. Modeling of Fibrotic Lung Disease Using 3D Organoids Derived from Human Pluripotent Stem Cells. Cell Rep. 2019, 27, 3709–3723.e5. [Google Scholar] [CrossRef]
- Chen, T.K.; Knicely, D.H.; Grams, M.E. Chronic Kidney Disease Diagnosis and Management. JAMA 2019, 322, 1294–1304. [Google Scholar] [CrossRef]
- Inker, L.A.; Astor, B.C.; Fox, C.H.; Isakova, T.; Lash, J.P.; Peralta, C.A.; Kurella Tamura, M.; Feldman, H.I. KDOQI US Commentary on the 2012 KDIGO Clinical Practice Guideline for the Evaluation and Management of CKD. Am. J. Kidney Dis. 2014, 63, 713–735. [Google Scholar] [CrossRef]
- Stevens, P.E.; Levin, A. Evaluation and Management of Chronic Kidney Disease: Synopsis of the kidney disease: Improving Global Outcomes 2012 Clinical Practice Guideline. Ann. Intern. Med. 2013, 158, 825–830. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar]
- Fried, L.F.; Emanuele, N.; Zhang, J.H.; Brophy, M.; Conner, T.A.; Duckworth, W.; Leehey, D.J.; McCullough, P.A.; O’COnnor, T.; Palevsky, P.M.; et al. Combined Angiotensin Inhibition for the Treatment of Diabetic Nephropathy. N. Engl. J. Med. 2013, 369, 1892–1903. [Google Scholar] [CrossRef]
- Guideline Development Group; Bilo, H.; Coentrão, L.; Couchoud, C.; Covic, A.; De Sutter, J.; Drechsler, C.; Gnudi, L.; Goldsmith, D.; Heaf, J.; et al. Clinical Practice Guideline on management of patients with diabetes and chronic kidney disease stage 3b or higher (eGFR < 45 mL/min). Nephrol. Dial. Transplant. 2015, 30, ii1–ii142. [Google Scholar]
- Shurraw, S.; Hemmelgarn, B.; Lin, M.; Majumdar, S.R.; Klarenbach, S.; Manns, B.; Bello, A.; James, M.; Turin, T.C.; Tonelli, M.; et al. Association Between Glycemic Control and Adverse Outcomes in People with Diabetes Mellitus and Chronic Kidney Disease. Arch. Intern. Med. 2011, 171, 1920–1927. [Google Scholar] [CrossRef]
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998, 352, 837–853. [Google Scholar] [CrossRef]
- Anderson, T.J.; Grégoire, J.; Pearson, G.J.; Barry, A.R.; Couture, P.; Dawes, M.; Francis, G.A.; Genest, J., Jr.; Grover, S.; Gupta, M.; et al. 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. Can. J. Cardiol. 2016, 32, 1263–1282. [Google Scholar] [CrossRef]
- Tonelli, M.; Wanner, C. Lipid Management in Chronic Kidney Disease: Synopsis of the kidney disease: Improving Global Outcomes 2013 Clinical Practice Guideline. Ann. Intern. Med. 2014, 160, 182–189. [Google Scholar] [CrossRef]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; Lefevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef]
- Thomas, B.; Matsushita, K.; Abate, K.H.; Al-Aly, Z.; Ärnlöv, J.; Asayama, K.; Atkins, R.; Badawi, A.; Ballew, S.H.; Banerjee, A.; et al. Global Cardiovascular and Renal Outcomes of Reduced GFR. J. Am. Soc. Nephrol. 2017, 28, 2167–2179. [Google Scholar] [CrossRef]
- Agapova, O.A.; Fang, Y.; Sugatani, T.; Seifert, M.E.; Hruska, K.A. Ligand trap for the activin type IIA receptor protects against vascular disease and renal fibrosis in mice with chronic kidney disease. Kidney Int. 2016, 89, 1231–1243. [Google Scholar] [CrossRef]
- Lau, A.; Rahn, J.J.; Chappellaz, M.; Chung, H.; Benediktsson, H.; Bihan, D.; von Mässenhausen, A.; Linkermann, A.; Jenne, C.N.; Robbins, S.M.; et al. Dipeptidase-1 governs renal inflammation during ischemia reperfusion injury. Sci. Adv. 2022, 8, eabm0142. [Google Scholar] [CrossRef]
- Linkermann, A. Nonapoptotic cell death in acute kidney injury and transplantation. Kidney Int. 2016, 89, 46–57. [Google Scholar] [CrossRef]
- Belavgeni, A.; Meyer, C.; Stumpf, J.; Hugo, C.; Linkermann, A. Ferroptosis and Necroptosis in the Kidney. Cell Chem. Biol. 2020, 27, 448–462. [Google Scholar] [CrossRef]
- Lamade, A.M.; Wu, L.; Dar, H.H.; Mentrup, H.L.; Shrivastava, I.H.; Epperly, M.W.; Croix, C.M.S.; Tyurina, Y.Y.; Anthonymuthu, T.S.; Yang, Q.; et al. Inactivation of RIP3 kinase sensitizes to 15LOX/PEBP1-mediated ferroptotic death. Redox Biol. 2022, 50, 102232. [Google Scholar] [CrossRef]
- Tonnus, W.; Meyer, C.; Steinebach, C.; Belavgeni, A.; von Mässenhausen, A.; Gonzalez, N.Z.; Maremonti, F.; Gembardt, F.; Himmerkus, N.; Latk, M.; et al. Dysfunction of the key ferroptosis-surveilling systems hypersensitizes mice to tubular necrosis during acute kidney injury. Nat. Commun. 2021, 12, 4402. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, Y.; Xu, Y. Pyroptosis in Kidney Disease. J. Mol. Biol. 2021, 434, 167290. [Google Scholar] [CrossRef] [PubMed]
- Elias, E.E.; Lyons, B.; Muruve, D.A. Gasdermins and pyroptosis in the kidney. Nat. Rev. Nephrol. 2023, 19, 337–350. [Google Scholar] [CrossRef] [PubMed]
- Tong, X.; Tang, R.; Xiao, M.; Xu, J.; Wang, W.; Zhang, B.; Liu, J.; Yu, X.; Shi, S. Targeting cell death pathways for cancer therapy: Recent developments in necroptosis, pyroptosis, ferroptosis, and cuproptosis research. J. Hematol. Oncol. 2022, 15, 174. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Zhang, J.-Y.; Liu, X.-S.; Chen, H.-Z.; Ai, Y.-L.; Cheng, K.; Sun, R.-Y.; Zhou, D.; Han, J.; Wu, Q. Tom20 senses iron-activated ROS signaling to promote melanoma cell pyroptosis. Cell Res. 2018, 28, 1171–1185. [Google Scholar] [CrossRef]
- Zhang, K.-J.; Wu, Q.; Jiang, S.-M.; Ding, L.; Liu, C.-X.; Xu, M.; Wang, Y.; Zhou, Y.; Li, L. Pyroptosis: A New Frontier in Kidney Diseases. Oxidative Med. Cell. Longev. 2021, 2021, 6686617. [Google Scholar] [CrossRef]
- Świerczyński, M.; Fichna, J. Inflamasom jako czynnik sprawczy i ochronny w patogenezie nieswoistych chorób zapalnych jelit. Postępy Biochem. 2021, 67, 44–53. [Google Scholar] [CrossRef]
- Shahzad, K.; Fatima, S.; Khawaja, H.; Elwakiel, A.; Gadi, I.; Ambreen, S.; Zimmermann, S.; Mertens, P.R.; Biemann, R.; Isermann, B. Podocyte-specific Nlrp3 inflammasome activation promotes diabetic kidney disease. Kidney Int. 2022, 102, 766–779. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, Z.; Ruan, J.; Pan, Y.; Magupalli, V.G.; Wu, H.; Lieberman, J. Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature 2016, 535, 153–158. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, X.; Song, Y.; Caballero, B.; Cheskin, L. Association between obesity and kidney disease: A systematic review and meta-analysis. Kidney Int. 2008, 73, 19–33. [Google Scholar] [CrossRef]
- Sharma, I.; Liao, Y.; Zheng, X.; Kanwar, Y.S. New Pandemic: Obesity and Associated Nephropathy. Front. Med. 2021, 8, 673556. [Google Scholar] [CrossRef] [PubMed]
- Câmara, N.O.S.; Iseki, K.; Kramer, H.; Liu, Z.-H.; Sharma, K. Kidney disease and obesity: Epidemiology, mechanisms and treatment. Nat. Rev. Nephrol. 2017, 13, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Ge, X.; Li, X.; He, J.; Wei, X.; Du, J.; Sun, J.; Li, X.; Xun, Z.; Liu, W.; et al. High-fat diet promotes renal injury by inducing oxidative stress and mitochondrial dysfunction. Cell Death Dis. 2020, 11, 914. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.; Cui, H.; Wang, Y.; Ju, F.; Cai, Y.; Gang, X.; Wang, G. The role of lipotoxicity in kidney disease: From molecular mechanisms to therapeutic prospects. Biomed. Pharmacother. 2023, 161, 114465. [Google Scholar] [CrossRef] [PubMed]
- Gai, Z.; Wang, T.; Visentin, M.; Kullak-Ublick, G.A.; Fu, X.; Wang, Z. Lipid Accumulation and Chronic Kidney Disease. Nutrients 2019, 11, 722. [Google Scholar] [CrossRef]
- Kennedy, D.J.; Chen, Y.; Huang, W.; Viterna, J.; Liu, J.; Westfall, K.; Tian, J.; Bartlett, D.J.; Tang, W.W.; Xie, Z.; et al. CD36 and Na/K-ATPase-α1 Form a Proinflammatory Signaling Loop in Kidney. Hypertension 2013, 61, 216–224. [Google Scholar] [CrossRef]
- Hua, W.; Huang, H.-Z.; Tan, L.-T.; Wan, J.-M.; Gui, H.-B.; Zhao, L.; Ruan, X.-Z.; Chen, X.-M.; Du, X.-G. CD36 Mediated Fatty Acid-Induced Podocyte Apoptosis via Oxidative Stress. PLoS ONE 2015, 10, e0127507. [Google Scholar] [CrossRef]
- Jung, J.H.; Choi, J.E.; Song, J.H.; Ahn, S.-H. Human CD36 overexpression in renal tubules accelerates the progression of renal diseases in a mouse model of folic acid-induced acute kidney injury. Kidney Res. Clin. Pract. 2018, 37, 30–40. [Google Scholar] [CrossRef]
- Kim, J.-J.; David, J.M.; Wilbon, S.S.; Santos, J.V.; Patel, D.M.; Ahmad, A.; Mitrofanova, A.; Liu, X.; Mallela, S.K.; Ducasa, G.M.; et al. Discoidin domain receptor 1 activation links extracellular matrix to podocyte lipotoxicity in Alport syndrome. EBioMedicine 2020, 63, 103162. [Google Scholar] [CrossRef]
- Rysz, J.; Franczyk, B.; Ławiński, J.; Olszewski, R.; Ciałkowska-Rysz, A.; Gluba-Brzózka, A. The Impact of CKD on Uremic Toxins and Gut Microbiota. Toxins 2021, 13, 252. [Google Scholar] [CrossRef]
- Ramezani, A.; Raj, D.S. The Gut Microbiome, Kidney Disease, and Targeted Interventions. J. Am. Soc. Nephrol. 2014, 25, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Rapa, S.F.; Prisco, F.; Popolo, A.; Iovane, V.; Autore, G.; Di Iorio, B.R.; Dal Piaz, F.; Paciello, O.; Nishijima, F.; Marzocco, S. Pro-Inflammatory Effects of Indoxyl Sulfate in Mice: Impairment of Intestinal Homeostasis and Immune Response. Int. J. Mol. Sci. 2021, 22, 1135. [Google Scholar] [CrossRef] [PubMed]
- Di Paola, R.; De, A.; Izhar, R.; Abate, M.; Zappavigna, S.; Capasso, A.; Perna, A.F.; La Russa, A.; Capasso, G.; Caraglia, M.; et al. Possible Effects of Uremic Toxins p-Cresol, Indoxyl Sulfate, p-Cresyl Sulfate on the Development and Progression of Colon Cancer in Patients with Chronic Renal Failure. Genes 2023, 14, 1257. [Google Scholar] [CrossRef] [PubMed]
- Vanholder, R.; Schepers, E.; Pletinck, A.; Nagler, E.V.; Glorieux, G. The Uremic Toxicity of Indoxyl Sulfate and p-Cresyl Sulfate: A Systematic Review. J. Am. Soc. Nephrol. 2014, 25, 1897–1907. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.-C.; Tomino, Y.; Lu, K.-C. Impacts of Indoxyl Sulfate and p-Cresol Sulfate on Chronic Kidney Disease and Mitigating Effects of AST-120. Toxins 2018, 10, 367. [Google Scholar] [CrossRef] [PubMed]
- Ito, S.; Osaka, M.; Higuchi, Y.; Nishijima, F.; Ishii, H.; Yoshida, M. Indoxyl Sulfate Induces Leukocyte-Endothelial Interactions through Up-regulation of E-selectin. J. Biol. Chem. 2010, 285, 38869–38875. [Google Scholar] [CrossRef]
- Nakano, T.; Katsuki, S.; Chen, M.; Decano, J.L.; Halu, A.; Lee, L.H.; Pestana, D.V.S.; Kum, A.S.T.; Kuromoto, R.K.; Golden, W.S.; et al. Uremic Toxin Indoxyl Sulfate Promotes Proinflammatory Macrophage Activation Via the Interplay of OATP2B1 and Dll4-Notch Signaling. Circulation 2019, 139, 78–96. [Google Scholar] [CrossRef]
- Watanabe, H.; Miyamoto, Y.; Otagiri, M.; Maruyama, T. Update on the Pharmacokinetics and Redox Properties of Protein-Bound Uremic Toxins. J. Pharm. Sci. 2011, 100, 3682–3695. [Google Scholar] [CrossRef]
- Shimizu, H.; Bolati, D.; Higashiyama, Y.; Nishijima, F.; Shimizu, K.; Niwa, T. Indoxyl sulfate upregulates renal expression of MCP-1 via production of ROS and activation of NF-κB, p53, ERK, and JNK in proximal tubular cells. Life Sci. 2012, 90, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, K.; Yamamoto, S.; Wakamatsu, T.; Takahashi, Y.; Kawamura, K.; Kaneko, Y.; Goto, S.; Kazama, J.J.; Narita, I. Increased Proinflammatory Cytokine Production and Decreased Cholesterol Efflux Due to Downregulation of ABCG1 in Macrophages Exposed to Indoxyl Sulfate. Toxins 2015, 7, 3155–3166. [Google Scholar] [CrossRef]
- Chang, J.-F.; Hsieh, C.-Y.; Liou, J.-C.; Liu, S.-H.; Hung, C.-F.; Lu, K.-C.; Lin, C.-C.; Wu, C.-C.; Ka, S.-M.; Wen, L.-L.; et al. Scavenging Intracellular ROS Attenuates p-Cresyl Sulfate-Triggered Osteogenesis through MAPK Signaling Pathway and NF-κB Activation in Human Arterial Smooth Muscle Cells. Toxins 2020, 12, 472. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.J.; Sidor, N.A.; Tonial, N.C.; Che, A.; Urquhart, B.L. Uremic Toxins in the Progression of Chronic Kidney Disease and Cardiovascular Disease: Mechanisms and Therapeutic Targets. Toxins 2021, 13, 142. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, H.; Yisireyili, M.; Nishijima, F.; Niwa, T. Indoxyl Sulfate Enhances p53-TGF-β1-Smad3 Pathway in Proximal Tubular Cells. Am. J. Nephrol. 2013, 37, 97–103. [Google Scholar] [CrossRef]
- Shafi, T.; Meyer, T.W.; Hostetter, T.H.; Melamed, M.L.; Parekh, R.S.; Hwang, S.; Banerjee, T.; Coresh, J.; Powe, N.R. Free Levels of Selected Organic Solutes and Cardiovascular Morbidity and Mortality in Hemodialysis Patients: Results from the Retained Organic Solutes and Clinical Outcomes (ROSCO) Investigators. PLoS ONE 2015, 10, e0126048. [Google Scholar] [CrossRef]
- Al Hinai, E.A.; Kullamethee, P.; Rowland, I.R.; Swann, J.; Walton, G.E.; Commane, D.M. Modelling the role of microbial p-cresol in colorectal genotoxicity. Gut Microbes 2018, 10, 398–411. [Google Scholar] [CrossRef]
- Li, J.; Zhao, F.; Wang, Y.; Chen, J.; Tao, J.; Tian, G.; Wu, S.; Liu, W.; Cui, Q.; Geng, B.; et al. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome 2017, 5, 14. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Xie, S.; Lv, D.; Wang, P.; He, H.; Zhang, T.; Zhou, Y.; Lin, Q.; Zhou, H.; Jiang, J.; et al. Alteration of the gut microbiota in Chinese population with chronic kidney disease. Sci. Rep. 2017, 7, 2870. [Google Scholar] [CrossRef] [PubMed]
- Aronov, P.A.; Luo, F.J.-G.; Plummer, N.S.; Quan, Z.; Holmes, S.; Hostetter, T.H.; Meyer, T.W. Colonic Contribution to Uremic Solutes. J. Am. Soc. Nephrol. 2011, 22, 1769–1776. [Google Scholar] [CrossRef]
- Hobby, G.P.; Karaduta, O.; Dusio, G.F.; Singh, M.; Zybailov, B.L.; Arthur, J.M. Chronic kidney disease and the gut microbiome. Am. J. Physiol. Physiol. 2019, 316, F1211–F1217. [Google Scholar] [CrossRef]
- Dou, L.; Bertrand, E.; Cerini, C.; Faure, V.; Sampol, J.; Vanholder, R.; Berland, Y.; Brunet, P. The uremic solutes p-cresol and indoxyl sulfate inhibit endothelial proliferation and wound repair. Kidney Int. 2004, 65, 442–451. [Google Scholar] [CrossRef]
- Guldris, S.C.; Parra, E.G.; Amenós, A.C. Gut microbiota in chronic kidney disease. Nefrología 2017, 37, 9–19. [Google Scholar] [CrossRef]
- Vaziri, N.D.; Wong, J.; Pahl, M.; Piceno, Y.M.; Yuan, J.; DeSantis, T.Z.; Ni, Z.; Nguyen, T.-H.; Andersen, G.L. Chronic kidney disease alters intestinal microbial flora. Kidney Int. 2013, 83, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Ning, X.; Liu, B.; Dong, R.; Bai, M.; Sun, S. Specific alterations in gut microbiota in patients with chronic kidney disease: An updated systematic review. Ren. Fail. 2021, 43, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Ouyang, S.; Xie, Y.; Gong, Z.; Du, J. Characterizing the gut microbiota in patients with chronic kidney disease. Postgrad. Med. 2020, 132, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Wu, I.-W.; Lin, C.-Y.; Chang, L.-C.; Lee, C.-C.; Chiu, C.-Y.; Hsu, H.-J.; Sun, C.-Y.; Chen, Y.-C.; Kuo, Y.-L.; Yang, C.-W.; et al. Gut Microbiota as Diagnostic Tools for Mirroring Disease Progression and Circulating Nephrotoxin Levels in Chronic Kidney Disease: Discovery and Validation Study. Int. J. Biol. Sci. 2020, 16, 420–434. [Google Scholar] [CrossRef]
- Ren, Z.; Fan, Y.; Li, A.; Shen, Q.; Wu, J.; Ren, L.; Lu, H.; Ding, S.; Ren, H.; Liu, C.; et al. Alterations of the Human Gut Microbiome in Chronic Kidney Disease. Adv. Sci. 2020, 7, 2001936. [Google Scholar] [CrossRef]
- Kim, J.E.; Kim, H.-E.; Park, J.I.; Cho, H.; Kwak, M.-J.; Kim, B.-Y.; Yang, S.H.; Lee, J.P.; Kim, D.K.; Joo, K.W.; et al. The Association between Gut Microbiota and Uremia of Chronic Kidney Disease. Microorganisms 2020, 8, 907. [Google Scholar] [CrossRef]
- Gryp, T.; Huys, G.R.; Joossens, M.; Van Biesen, W.; Glorieux, G.; Vaneechoutte, M. Isolation and Quantification of Uremic Toxin Precursor-Generating Gut Bacteria in Chronic Kidney Disease Patients. Int. J. Mol. Sci. 2020, 21, 1986. [Google Scholar] [CrossRef]
- Zhao, Z.; Zhang, W.; Guo, R.; Cui, W.; Zhang, F.; Geng, Y.; Liu, C.; Shang, J.; Xiao, J.; Wen, X. Gut Microbiome Alterations Predict Diabetic Kidney Disease in General Population. Res. Sq. 2020, 10. [Google Scholar] [CrossRef]
- Alatriste, P.V.M.; Arronte, R.U.; Espinosa, C.O.G.; Espinosa Cuevas, M.D.L.A. Efecto de lactobacillus casei shirota sobre concentraciones de urea en la enfermedad renal crónica. Nutr. Hosp. 2014, 29, 582–590. [Google Scholar]
- Neto, M.P.C.; Aquino, J.d.S.; Silva, L.d.F.R.d.; Silva, R.d.O.; Guimarães, K.S.d.L.; de Oliveira, Y.; de Souza, E.L.; Magnani, M.; Vidal, H.; Alves, J.L.d.B. Gut microbiota and probiotics intervention: A potential therapeutic target for management of cardiometabolic disorders and chronic kidney disease? Pharmacol. Res. 2018, 130, 152–163. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.d.C.S.O. Modulation of Intestinal Microbiota, Control of Nitrogen Products and Inflammation by Pre/Probiotics in Chronic Kidney Disease: A Systematic Review. Nutr. Hosp. 2018, 35, 722–730. [Google Scholar] [CrossRef] [PubMed]
- Chudzik, A.; Orzyłowska, A.; Rola, R.; Stanisz, G.J. Probiotics, Prebiotics and Postbiotics on Mitigation of Depression Symptoms: Modulation of the Brain–Gut–Microbiome Axis. Biomolecules 2021, 11, 1000. [Google Scholar] [CrossRef] [PubMed]
- Kolida, S.; Gibson, G.R. Synbiotics in Health and Disease. Annu. Rev. Food Sci. Technol. 2011, 2, 373–393. [Google Scholar] [CrossRef]
- Gou, H.-Z.; Zhang, Y.-L.; Ren, L.-F.; Li, Z.-J.; Zhang, L. How do intestinal probiotics restore the intestinal barrier? Front. Microbiol. 2022, 13, 929346. [Google Scholar] [CrossRef]
- Virk, M.S.; Virk, M.A.; He, Y.; Tufail, T.; Gul, M.; Qayum, A.; Rehman, A.; Rashid, A.; Ekumah, J.-N.; Han, X.; et al. The Anti-Inflammatory and Curative Exponent of Probiotics: A Comprehensive and Authentic Ingredient for the Sustained Functioning of Major Human Organs. Nutrients 2024, 16, 546. [Google Scholar] [CrossRef]
- Tokarek, J.; Budny, E.; Saar, M.; Stańczak, K.; Wojtanowska, E.; Młynarska, E.; Rysz, J.; Franczyk, B. Molecular Processes Involved in the Shared Pathways between Cardiovascular Diseases and Diabetes. Biomedicines 2023, 11, 2611. [Google Scholar] [CrossRef] [PubMed]
- E Cooper, T.; Khalid, R.; Chan, S.; Craig, J.C.; Hawley, C.M.; Howell, M.; Johnson, D.W.; Jaure, A.; Teixeira-Pinto, A.; Wong, G. Synbiotics, prebiotics and probiotics for people with chronic kidney disease. Cochrane Database Syst. Rev. 2023, 2023, CD013631. [Google Scholar]
- Kuo, Y.-W.; Huang, Y.-Y.; Tsai, S.-Y.; Wang, J.-Y.; Lin, J.-H.; Syu, Z.-J.; Wang, H.-S.; Hsu, Y.-C.; Chen, J.-F.; Hsia, K.-C.; et al. Probiotic Formula Ameliorates Renal Dysfunction Indicators, Glycemic Levels, and Blood Pressure in a Diabetic Nephropathy Mouse Model. Nutrients 2023, 15, 2803. [Google Scholar] [CrossRef]
- Chávez-Íñiguez, J.S.; Ibarra-Estrada, M.; Gallardo-González, A.M.; Cisneros-Hernández, A.; Granado, R.C.-D.; Chávez-Alonso, G.; Hernández-Barajas, E.M.; Romero-Muñoz, A.C.; Ramos-Avellaneda, F.; Prieto-Magallanes, M.L.; et al. Probiotics in septic acute kidney injury, a double blind, randomized control trial. Ren. Fail. 2023, 45, 2260003. [Google Scholar] [CrossRef]
- Ogawa, T.; Shimada, M.; Nagano, N.; Ito, K.; Ando, T.; Shimomura, Y.; Ando, Y.; Otsuka, K. Oral administration of Bifidobacterium longum in a gastro-resistant seamless capsule decreases serum phosphate levels in patients receiving haemodialysis. Clin. Kidney J. 2012, 5, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Nakabayashi, I.; Nakamura, M.; Kawakami, K.; Ohta, T.; Kato, I.; Uchida, K.; Yoshida, M. Effects of synbiotic treatment on serum level of p-cresol in haemodialysis patients: A preliminary study. Nephrol. Dial. Transplant. 2010, 26, 1094–1098. [Google Scholar] [CrossRef]
- Cruz-Mora, J.; Martínez-Hernández, N.E.; Martindel Campo-Lopez, F.; Viramontes-Hörner, D.; Vizmanos-Lamotte, B.; Muñoz-Valle, J.F.; García-García, G.; Parra-Rojas, I.; Castro-Alarcón, N. Effects of a Symbiotic on Gut Microbiota in Mexican Patients with End-Stage Renal Disease. J. Ren. Nutr. 2014, 24, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Viramontes-Hörner, D.; Márquez-Sandoval, F.; Martín-Del-Campo, F.; Vizmanos-Lamotte, B.; Sandoval-Rodríguez, A.; Armendáriz-Borunda, J.; García-Bejarano, H.; Renoirte-López, K.; García-García, G. Effect of a Symbiotic Gel (Lactobacillus acidophilus + Bifidobacterium lactis + Inulin) on Presence and Severity of Gastrointestinal Symptoms in Hemodialysis Patients. J. Ren. Nutr. 2015, 25, 284–291. [Google Scholar] [CrossRef]
- Guida, B.; Germanò, R.; Trio, R.; Russo, D.; Memoli, B.; Grumetto, L.; Barbato, F.; Cataldi, M. Effect of short-term synbiotic treatment on plasma p-cresol levels in patients with chronic renal failure: A randomized clinical trial. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 1043–1049. [Google Scholar] [CrossRef]
- Rossi, M.; Johnson, D.W.; Morrison, M.; Pascoe, E.M.; Coombes, J.S.; Forbes, J.M.; Szeto, C.-C.; McWhinney, B.C.; Ungerer, J.P.; Campbell, K.L. Synbiotics Easing Renal Failure by Improving Gut Microbiology (SYNERGY): A Randomized Trial. Clin. J. Am. Soc. Nephrol. 2016, 11, 223–231. [Google Scholar] [CrossRef]
- Simenhoff, M.L.; Dunn, S.R.; Zollner, G.P.; Fitzpatrick, M.E.; Emery, S.M.; Sandine, W.E.; Ayres, J.W. Biomodulation of the Toxic and Nutritional Effects of Small Bowel Bacterial Overgrowth in End-Stage Kidney Disease Using Freeze-Dried Lacto-bacillus Acidophilus. Miner. Electrolyte Metab. 1996, 22, 92–96. [Google Scholar] [PubMed]
- Takayama, F.; Taki, K.; Niwa, T. Bifidobacterium in gastro-resistant seamless capsule reduces serum levels of indoxyl sulfate in patients on hemodialysis. Am. J. Kidney Dis. 2003, 41, S142–S145. [Google Scholar] [CrossRef] [PubMed]
- Taki, K.; Takayama, F.; Niwa, T. Beneficial effects of Bifidobacteria in a gastroresistant seamless capsule on hyperhomocysteinemia in hemodialysis patients. J. Ren. Nutr. 2005, 15, 77–80. [Google Scholar] [CrossRef]
- Ando, Y.; Miyata, Y.; Tanba, K.; Saito, O.; Muto, S.; Kurosu, M.; Homma, S.; Kusano, E.; Asano, Y. Effect of oral intake of an enteric capsule preparation containing Bifidobacterium longum on the progression of chronic renal failure. Nihon Jinzo Gakkai Shi 2003, 45, 759–764. [Google Scholar]
- Hida, M.; Aiba, Y.; Sawamura, S.; Suzuki, N.; Satoh, T.; Koga, Y. Inhibition of the Accumulation of Uremic Toxins in the Blood and Their Precursors in the Feces after Oral Administration of Lebenin®, a Lactic Acid Bacteria Preparation, to Uremic Patients Undergoing Hemodialysis. Nephron 1996, 74, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, R.; Pechenyak, B.; Vyas, U.; Ranganathan, P.; Weinberg, A.; Liang, P.; Mallappallil, M.C.; Norin, A.J.; Friedman, E.A.; Saggi, S.J. Randomized Controlled Trial of Strain-Specific Probiotic Formulation (Renadyl) in Dialysis Patients. BioMed Res. Int. 2014, 2014, 568571. [Google Scholar] [CrossRef] [PubMed]
- Wang, I.-K.; Wu, Y.-Y.; Yang, Y.-F.; Ting, I.-W.; Lin, C.-C.; Yen, T.-H.; Chen, J.-H.; Wang, C.-H.; Huang, C.-C.; Lin, H.-C. The effect of probiotics on serum levels of cytokine and endotoxin in peritoneal dialysis patients: A randomised, double-blind, placebo-controlled trial. Benef. Microbes 2015, 6, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Ranganathan, N.; Friedman, E.A.; Tam, P.; Rao, V.; Ranganathan, P.; Dheer, R. Probiotic dietary supplementation in patients with stage 3 and 4 chronic kidney disease: A 6-month pilot scale trial in Canada. Curr. Med. Res. Opin. 2009, 25, 1919–1930. [Google Scholar] [CrossRef]
- Ranganathan, N.; Ranganathan, P.; Friedman, E.A.; Joseph, A.; Delano, B.; Goldfarb, D.S.; Tam, P.; Rao, A.V.; Anteyi, E.; Musso, C.G. Pilot study of probiotic dietary supplementation for promoting healthy kidney function in patients with chronic kidney disease. Adv. Ther. 2010, 27, 634–647. [Google Scholar] [CrossRef]
| Stages | GFR (mL/min/1.73 m2) | Classification |
|---|---|---|
| G1 | >90 | Normal or high |
| G2 | 60–89 | Mildly decreased |
| G3a | 45–59 | Mildly to moderately decreased |
| G3b | 30–44 | Moderately to severely decreased |
| G4 | 15–29 | Severely decreased |
| G5 | <15 | Kidney failure |
| Category | AER (mg/24 h) | ACR (mg/mmol) | Classification |
|---|---|---|---|
| A1 | <30 | <3 | Normal to mildly increased |
| A2 | 30–300 | 3–30 | Moderately increased |
| A3 | >300 | >30 | Severely increased |
| Phylum | Class | Order | Family | Genus | Species | Gram Classification | Presence in CKD |
|---|---|---|---|---|---|---|---|
| Bacteroidota | Bacteroidia | Bacteroidales | Bacteroidaceae | Bacteroides | Fragilis | Negative | Lower |
| Bacteroidetes | Bacteroidia | Bacteroidales | Prevotellaceae * | Prevotella | - | Negative | Lower |
| Bacillota | Bacilli | Lactobacillales | Lactobacillaceae * | Lactobacillus | - | Positive | Lower |
| Bacillota | Clostridia | Eubacteriales | Lachnospiraceae | Roseburia | Hominis | Positive | Lower |
| Bacillota | Clostridia | Eubacteriales | Oscillospiraceae | Faecalibacterium | Prausnitzii | Positive | Lower |
| Bacillota | Negativicutes | Vellionellales | Veillonellaceae * | Veillonella | Parvula | Negative | Lower |
| Bacillota | Clostridia | Eubacteriales | Lachnospiraceae | Lachnospira | - | Positive | Lower |
| Bacillota | Negativicutes | Veillonellales | Veillonellaceae * | Dialister | Succinatiphilus | Negative | Lower |
| Firmicutes | Clostridia | Clostridiales | Clostridiaceae | - | - | Positive | Lower |
| Bacillota | Clostridia | Clostridiales | Eubacteriaceae * | Eubacterium | Rectale | Positive | Lower |
| Firmicutes | Clostridia | Clostridiales | Ruminococcaceae | Ruminococcus | Bromii, Callidus | Positive | Lower |
| Bacillota | Clostridia | Eubacteriales | Lachnospiraceae | Blautia | - | Positive | Lower |
| Phylum | Class | Order | Family | Genus | Species | Gram Classification | Presence in CKD |
|---|---|---|---|---|---|---|---|
| Firmicutes | Bacilli | Lactobacillales | Enterococcaceae * | Enterococcus | - | Positive | Higher |
| Pseudomonadota | Gammaproteobacteria | Enterobacteriales | Enterobacteriaceae * | Klebsiella | - | Negative | Higher |
| Bacillota | Bacilli | Lactobacillales | Streptococcaceae | Streptococcus | - | Positive | Higher |
| Pseudomonadota | Gammaproteobacteria | Enterobacterales | Enterobacteriaceae * | Escherichia | - | Negative | Higher |
| Proteobacteria * | Deltaproteobacteria | Desulfovibrionales | Desulfovibrionaceae | Desulfovibrio | - | Negative | Higher |
| Firmicutes | Clostridia | Clostridiales | Ruminococcaceae | Oscillibacter | - | Positive | Higher |
| Bacillota | Negativicutes | Selenomonadales | Selenomonadaceae | - | - | Negative | Higher |
| Bacillota | Clostridia | Eubacteriales | Oscillospiraceae | Flavonifractor | Plautii | Positive | Higher |
| Pseudomonadota | Gammaproteobacteria | Enterobacterales | Enterobacteriaceae * | Citrobacter | Freundii | Negative | Higher |
| Bacteroidota | Bacteroidia | Bacteroidales | Rikenellaceae | Alistipes | Werkmanii | Negative | Higher |
| Verrucomicrobiota | Verrucomicrobiae | Verrucomicrobiales | Akkermansiaceae | Akkermansia | - | Negative | Higher |
| Intestinal Tract | Normal | ACKD/CKD |
|---|---|---|
| Stomach | Helicobacter, Lactobacillus | No change observed |
| Duodenum | Lactococcus, Streptococcus, Staphylococcus | Increased |
| Jejunum | Streptococcus, Lactobacillus, Enterococcus | Increased |
| Ileum | Clostridium, Enterobacteriaceae, Bacteroides | Increased |
| Colon | Fusobacterium | Aerobic overgrowth c.a. 100 times |
| Prevotellaceae | Bifidobacterium spp., Lactobacillus | |
| Proteus | Acinetobcter, Proteus spp. | |
| Actinobacteria | Enterobacteria, E. coli | |
| Bacteroides | Proteobacteria | |
| Firmicutes | Increased |
| Name of a Challenge | Importance |
|---|---|
| Strain-specific effects | Identifying a highly specific strain that could be useful and excluding those that are ineffective |
| Long-term safety and efficacy | Long-term studies are necessary to provide definitive evidence regarding the efficacy of the proposed treatment |
| Individual variability | The organism’s response to the probiotic is variable |
| Regulatory and quality issues | Ensuring the optimal quality and quantity of the product |
| Authors | Synbiotic | Results |
|---|---|---|
| T. Ogawa et al. [121] | Bifidobacterium longum JBL01 oligosaccharides | Decrease phosphorous levels that returned to baseline 2 weeks later |
| I. Nakabayashi et al. [122] | Bifidobacterium breve Yakult Lactobacillus casei Shirota galactooligosaccharides | Decrease in p-cresol in plasma Returning to correct bowel movement Connection of p-cresol level and constipation |
| J. Cruz-Mora et al. [123] | Bifidobacterium lactis Lactobacillus acidophilus inulin | Increase in Bifidobacteria in feces Decrease of Lactobacilli in feces Alleviation of gastrointestinal symptoms |
| D. Viramontes-Hörner et al. [124] | Bifidobacterium lactis Lactobacillus acidophilus Inulin | Diminishing of CRP and TNF-alpha levels. Alleviation of gastrointestinal symptoms |
| B. Guida et al. [125] | Lactobacillus casei subsp. Rhamnosus, Lactobacillus plantarum, Bifidobacterium infantis, Lactobacillus gasseri, Lactobacillus salivarius, Streptococcus thermophilus, Lactobacillus sporogenes, resistant tapioca starch and inulin | Decrease in p-cresol in plasma |
| M. Rossi et al. [126] | Bifidobacteria Lactobacillus Streptococcus Inulin Galactooligosaccharides Fructooligosaccharides | Increased Bifidobacteria Decreased Ruminococcaceae Slight increase in albuminuria No alteration in inflammation markers and oxidative stress Decrease PCS |
| Authors | Probiotic | Results |
|---|---|---|
| M. L. Simenhoff et al. [127] | Lactobacillus acidophilus | ↓ Dimethylamine, ↓Nitrosodimethylamine |
| F. Takayama et al. [128] | Bifidobacterium longum JCM008 | ↓ Indoxyl sulfate |
| K. Taki et al. [129] | Bifidobacterium longum | ↓ Homocysteine, indoxyl sulfate, and triglycerides |
| Y. Ando et al. [130] | Bifidobacterium longum | Lowering of CKD’s progression in patients with con Cr ≥4 mg/dl or P ≥ 4 mg/dl |
| M. Hida et al. [131] | Lebenin | ↓ p-cresol in feces and in serum |
| R. Natarajan et al. [132] | Renadyl | Reduction in CRP, leucocyte count, and indoxyl glucuronide |
| I.-K. Wang et al. [133] | Bifidobacterium catenulatum A302, Lactobacillus plantarum A87, Bifidobacterium longum A101, Bifidobacterium bifidum A218, | ↑ IL-10 Slight preservation of kidney function ↓ TNF-α, IL-5, IL-6, and endotoxin |
| P. V. M. Alatriste et al. [110] | Lactobacillus casei shirota | ↓ Urea |
| N. Ranganathan et al. [134] | Streptococcus thermophilus KB27, Bifidobacterium longum KB35, Lactobacillus acidophilus KB31 | ↑ Quality of life |
| N. Ranganathan et al. [135] | Bifidobacterium longum KB35, Lactobacillus acidophilus KB31, Streptococcus thermophilus KB27, | ↑ Quality of life |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Młynarska, E.; Budny, E.; Saar, M.; Wojtanowska, E.; Jankowska, J.; Marciszuk, S.; Mazur, M.; Rysz, J.; Franczyk, B. Does the Composition of Gut Microbiota Affect Chronic Kidney Disease? Molecular Mechanisms Contributed to Decreasing Glomerular Filtration Rate. Int. J. Mol. Sci. 2024, 25, 10429. https://doi.org/10.3390/ijms251910429
Młynarska E, Budny E, Saar M, Wojtanowska E, Jankowska J, Marciszuk S, Mazur M, Rysz J, Franczyk B. Does the Composition of Gut Microbiota Affect Chronic Kidney Disease? Molecular Mechanisms Contributed to Decreasing Glomerular Filtration Rate. International Journal of Molecular Sciences. 2024; 25(19):10429. https://doi.org/10.3390/ijms251910429
Chicago/Turabian StyleMłynarska, Ewelina, Emilian Budny, Maciej Saar, Ewa Wojtanowska, Justyna Jankowska, Szymon Marciszuk, Marcin Mazur, Jacek Rysz, and Beata Franczyk. 2024. "Does the Composition of Gut Microbiota Affect Chronic Kidney Disease? Molecular Mechanisms Contributed to Decreasing Glomerular Filtration Rate" International Journal of Molecular Sciences 25, no. 19: 10429. https://doi.org/10.3390/ijms251910429
APA StyleMłynarska, E., Budny, E., Saar, M., Wojtanowska, E., Jankowska, J., Marciszuk, S., Mazur, M., Rysz, J., & Franczyk, B. (2024). Does the Composition of Gut Microbiota Affect Chronic Kidney Disease? Molecular Mechanisms Contributed to Decreasing Glomerular Filtration Rate. International Journal of Molecular Sciences, 25(19), 10429. https://doi.org/10.3390/ijms251910429








