The Relationship between Vascular Biomarkers (Serum Endocan and Endothelin-1), NT-proBNP, and Renal Function in Chronic Kidney Disease, IgA Nephropathy: A Cross-Sectional Study
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Biomarker Measurement
4.2. Arterial Stiffness Measurement
4.3. Echocardiographic Measurement
4.4. Statistical Analysis
5. Conclusions
6. Limitations of the Study
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z.; Naicker, S.; Plattner, B.; Saran, R.; Wang, A.Y.; Yang, C.W. Chronic kidney disease: Global dimension and perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef] [PubMed]
- Gansevoort, R.T.; Correa-Rotter, R.; Hemmelgarn, B.R.; Jafar, T.H.; Heerspink, H.J.; Mann, J.F.; Matsushita, K.; Wen, C.P. Chronic kidney disease and cardiovascular risk: Epidemiology, mechanisms, and prevention. Lancet 2013, 382, 339–352. [Google Scholar] [CrossRef] [PubMed]
- Kwon, C.S.; Daniele, P.; Forsythe, A.; Ngai, C. A Systematic Literature Review of the Epidemiology, Health-Related Quality of Life Impact, and Economic Burden of Immunoglobulin A Nephropathy. J. Health Econ. Outcomes Res. 2021, 8, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Wakai, K.; Kawamura, T.; Endoh, M.; Kojima, M.; Tomino, Y.; Tamakoshi, A.; Ohno, Y.; Inaba, Y.; Sakai, H. A scoring system to predict renal outcome in IgA nephropathy: From a nationwide prospective study. Nephrol. Dial. Transplant. 2006, 21, 2800–2808. [Google Scholar] [CrossRef]
- Berthoux, F.; Mohey, H.; Laurent, B.; Mariat, C.; Afiani, A.; Thibaudin, L. Predicting the risk for dialysis or death in IgA nephropathy. J. Am. Soc. Nephrol. 2011, 22, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Tomioka, M.; Hiromura, K.; Sakairi, T.; Takeuchi, S.; Maeshima, A.; Kaneko, Y.; Kuroiwa, T.; Takeuchi, T.; Nojima, Y. Nestin is a novel marker for renal tubulointerstitial injury in immunoglobulin A nephropathy. Nephrology 2010, 15, 568–574. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, Y.G.; Lee, S.H.; Moon, J.Y.; Jeong, K.H.; Lee, T.W.; Ihm, C.G. Clinicopathological role of kidney injury molecule-1 in immunoglobulin A nephropathy. Kidney Res. Clin. Pract. 2014, 33, 139–143. [Google Scholar] [CrossRef]
- Rhee, H.; Shin, N.; Shin, M.J.; Yang, B.Y.; Kim, I.Y.; Song, S.H.; Lee, D.W.; Lee, S.B.; Kwak, I.S.; Seong, E.Y. High serum and urine neutrophil gelatinaseassociated lipocalin levels are independent predictors of renal progression in patients with immunoglobulin A nephropathy. Korean J. Intern. Med. 2015, 30, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Sarrazin, S.; Adam, E.; Lyon, M.; Depontieu, F.; Motte, V.; Landolfi, C.; Lortat-Jacob, H.; Bechard, D.; Lassalle, P.; Delehedde, M. Endocan or endothelial cell specific molecule-1 (ESM-1): A potential novel endothelial cell marker and a new target for cancer therapy. Biochim. Biophys. Acta (BBA)-Rev. Cancer 2006, 1765, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.M.; Zuo, L.; Zhou, Q.; Gui, S.Y.; Shi, R.; Wu, Q.; Wei, W.; Wang, Y. Expression and distribution of endocan in human tissues. Biotech. Histochem. 2012, 87, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Grigoriu, B.D.; Depontieu, F.; Scherpereel, A.; Gourcerol, D.; Devos, P.; Ouatas, T.; Lafitte, J.J.; Copin, M.C.; Tonnel, A.B.; Lassalle, P. Endocan expression and relationship with survival in human non-small cell lung cancer. Clin. Cancer Res. 2006, 12, 4575–4582. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, M.I.; Siriopol, D.; Saglam, M.; Kurt, Y.G.; Unal, H.U.; Eyileten, T.; Gok, M.; Cetinkaya, H.; Oguz, Y.; Sari, S.; et al. Plasma endocan levels associate with inflammation, vascular abnormalities, cardiovascular events, and survival in chronic kidney disease. Kidney Int. 2014, 86, 1213–1220. [Google Scholar] [CrossRef] [PubMed]
- Cakmak, M.; Yilmaz, H.; Ba_glar, E.; Darcin, T.; Inan, O.; Aktas, A.; Celik, H.T.; Ozdemir, O.; Atalay, C.R.; Akcay, A. Serum levels of endocan correlate with the presence and severity of pre-eclampsia. Clin. Exp. Hypertens. 2016, 38, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Pauly, D.; Hamed, S.; Behnes, M.; Lepiorz, D.; Lang, S.; Akin, I.; Borggrefe, M.; Bertsch, T.; Hoffmann, U. Endothelial cell-specific molecule-1/endocan: Diagnostic and prognostic value in patients suffering from severe sepsis and septic shock. J. Crit. Care 2016, 31, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.S.; Yang, W.; Luo, T.; Wang, J.M.; Jing, Y.Y. Serum endocan levels are correlated with the presence and severity of coronary artery disease in patients with hypertension. Genet. Test. Mol. Biomark. 2015, 19, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Jiang, L.; Yu, X.-H.; Hu, M.; Zhang, Y.-K.; Liu, X.; He, P.; Ouyang, X. Endocan: A Key Player of Cardiovascular Disease. Front. Cardiovasc. Med. 2022, 8, 798699. [Google Scholar] [CrossRef] [PubMed]
- Bertaglia, G.; Ossi, E.; Casonato, A.; Miglietta, A.; Forino, M.; Baggio, B.; Gambaro, G. Von Willebrand factor abnormalities in IgA nephropathy. Nephrol. Dial. Transplant. 1997, 12, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Zhai, Y.L.; Zhu, L.; Shi, S.F.; Liu, L.J.; Lv, J.C.; Zhang, H. Elevated soluble VEGF receptor sFlt-1 correlates with endothelial injury in IgA nephropathy. PLoS ONE 2014, 9, e101779. [Google Scholar] [CrossRef] [PubMed]
- Oka, S.; Obata, Y.; Sato, S.; Torigoe, K.; Sawa, M.; Abe, S.; Muta, K.; Ota, Y.; Kitamura, M.; Kawasaki, S.; et al. Serum endocan as a predictive marker for decreased urine volume in peritoneal dialysis patients. Med. Sci. Monit. 2017, 23, 1464–1470. [Google Scholar] [CrossRef]
- Poon, P.Y.; Ng, J.K.; Fung, W.W.; Chow, K.M.; Kwan, B.C.; Li, P.K.; Szeto, C.C. Relationship between plasma endocan level and clinical outcome of chinese peritoneal dialysis patients. Kidney Blood Press. Res. 2019, 44, 1259–1270. [Google Scholar] [CrossRef]
- Khalaji, A.; Behnoush, A.H.; Mohtasham Kia, Y.; Alehossein, P.; Bahiraie, P. High circulating endocan in chronic kidney disease? A systematic review and meta-analysis. PLoS ONE 2023, 18, e0289710. [Google Scholar] [CrossRef] [PubMed]
- Kohan, D.E. Endothelin, hypertension and chronic kidney disease: New insights. Curr. Opin. Nephrol. Hypertens. 2010, 19, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Schmidt, I.M.; Sabbisetti, V.; Tio, M.C.; Opotowsky, A.R.; Waikar, S.S. Plasma endothelin-1 and risk of death and hospitalization in patients undergoing maintenance hemodialysis. Clin. J. Am. Soc. Nephrol. 2020, 15, 784–793. [Google Scholar] [CrossRef] [PubMed]
- Davenport, A.P.; Hyndman, K.A.; Dhaun, N.; Southan, C.; Kohan, D.E.; Pollock, J.S.; Pollock, D.M.; Webb, D.J.; Maguire, J.J. Endothelin. Pharmacol. Rev. 2016, 68, 357–418. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, H.N.; Rivera-Gonzalez, O.; Gibert, Y.; Speed, J.S. Endothelin-1 in the pathophysiology of obesity and insulin resistance. Obes. Rev. 2020, 21, e13086. [Google Scholar] [CrossRef] [PubMed]
- Kohan, D.E.; Barton, M. Endothelin and endothelin antagonists in chronic kidney disease. Kidney Int. 2014, 86, 896–904. [Google Scholar] [CrossRef] [PubMed]
- Kohan, D.E.; Bedard, P.W.; Jenkinson, C.; Hendry, B.; Komers, R. Mechanism of protective actions of sparsentan in the kidney: Lessons from studies in models of chronic kidney disease. Clin. Sci. 2024, 138, 645–662. [Google Scholar] [CrossRef]
- Chiu, A.W.; Bredenkamp, N. Sparsentan: A First-in-Class Dual Endothelin and Angiotensin II Receptor Antagonist. Ann. Pharmacother. 2024, 58, 645–656. [Google Scholar] [CrossRef] [PubMed]
- Mishra, R.K.; Li, Y.; Ricardo, A.C.; Yang, W.; Keane, M.; Cuevas, M.; Christenson, R.; de Filippi, C.; Chen, J.; He, J.; et al. Association of N-terminal pro-B-type natriuretic peptide with left ventricular structure and function in chronic kidney disease (from the Chronic Renal Insufficiency Cohort [CRIC]). Am. J. Cardiol. 2013, 111, 432–438. [Google Scholar] [CrossRef]
- DeFilippi, C.R.; Fink, J.C.; Nass, C.M.; Chen, H.; Christenson, R. N-terminal pro-B-type natriuretic peptide for predicting coronary disease and left ventricular hypertrophy in asymptomatic CKD not requiring dialysis. Am. J. Kidney Dis. 2005, 46, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Paoletti, E.; De Nicola, L.; Gabbai, F.B.; Chiodini, P.; Ravera, M.; Pieracci, L.; Marre, S.; Cassottana, P.; Lucà, S.; Vettoretti, S.; et al. Associations of left ventricular hypertrophy and 1986 Clinical Journal of the American Society of Nephrology geometry with adverse outcomes in patients with CKD and hypertension. Clin. J. Am. Soc. Nephrol. 2016, 11, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Scheven, L.; de Jong, P.E.; Hillege, H.L.; Lambers Heerspink, H.J.; van Pelt, L.J.; Kootstra, J.E.; Bakker, S.J.; Gansevoort, R.T. High-sensitive troponin T and N-terminal pro-B type natriuretic peptide are associated with cardiovascular events despite the cross-sectional association with albuminuria and glomerular filtration rate. Eur. Heart J. 2012, 33, 2272–2281. [Google Scholar] [CrossRef]
- Matsushita, K.; Sang, Y.; Ballew, S.H.; Astor, B.C.; Hoogeveen, R.C.; Solomon, S.D.; Ballantyne, C.M.; Woodward, M.; Coresh, J. Cardiac and kidney markers for cardiovascular prediction in individuals with chronic kidney disease: The Atherosclerosis Risk in Communities study. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1770–1777. [Google Scholar] [CrossRef] [PubMed]
- Bansal, N.; Hyre Anderson, A.; Yang, W.; Christenson, R.H.; de Filippi, C.R.; Deo, R.; Dries, D.L.; Go, A.S.; He, J.; Kusek, J.W.; et al. High-sensitivity troponin T and N-terminal pro-B-type natriuretic peptide (NTproBNP) and risk of incident heart failure in patients with CKD: The Chronic Renal Insufficiency Cohort (CRIC) Study. J. Am. Soc. Nephrol. 2015, 26, 946–956. [Google Scholar] [CrossRef] [PubMed]
- Sági, B.; Vas, T.; Jakabfi-Csepregi, R.; Horváth-Szalai, Z.; Kőszegi, T.; Csiky, B.; Nagy, J.; Kovács, T.J. The Role of Two Heart Biomarkers in IgA Nephropathy. Int. J. Mol. Sci. 2023, 24, 10336. [Google Scholar] [CrossRef]
- Yoon, S.Y.; Kim, J.S.; Jung, S.W.; Kim, Y.G.; Moon, J.Y.; Lee, S.H.; Yim, S.V.; Hwang, H.S.; Jeong, K. Clinical significance of urinary inflammatory biomarkers in patients with IgA nephropathy. BMC Nephrol. 2024, 25, 142. [Google Scholar] [CrossRef] [PubMed]
- Jankowski, J.; Floege, J.; Fliser, D.; Böhm, M.; Marx, N. Cardiovascular Disease in Chronic Kidney Disease. Circulation 2021, 143, 1157–1172. [Google Scholar] [CrossRef]
- Nalewajska, M.; Gurazda, K.; Marchelek-Myśliwiec, M.; Pawlik, A.; Dziedziejko, V. The Role of Endocan in Selected Kidney Diseases. Int. J. Mol. Sci. 2020, 21, 6119. [Google Scholar] [CrossRef] [PubMed]
- Samouilidou, E.; Athanasiadou, V.; Grapsa, E. Prognostic and Diagnostic Value of Endocan in Kidney Diseases. Int. J. Nephrol. 2022, 2022, 3861092. [Google Scholar] [CrossRef] [PubMed]
- Fliser, D.; Wiecek, A.; Suleymanlar, G.; Ortiz, A.; Massy, Z.; Lindholm, B.; Martinez-Castelao, A.; Agarwal, R.; Jager, K.J.; Dekker, F.W.; et al. The dysfunctional endothelium in CKD and in cardiovascular disease: Mapping the origin(s) of cardiovascular problems in CKD and of kidney disease in cardiovascular conditions for a research agenda. Kidney Int. Suppl. 2011, 1, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Lu, L.L.; Wang, Y.T.; Zhou, J.B.; Wang, C.X.; Xin, J.D.; Gao, J.D. Endothelial injury and inflammation in patients with hyperuricemic nephropathy at chronic kidney disease stages 1–2 and 3–4. World J. Clin. Cases 2022, 10, 11766–11774. [Google Scholar] [CrossRef] [PubMed]
- El-Senosy, F.M.; Abd El Aziz, R.E.M.; Kasim, S.A.; Gad, L.A.; Hassan, D.A.; Sabry, S.; El Mancy, I.M.; Shawky, T.A.; Mohamed, I.G.R.; Elmonier, R.; et al. Serum Endocan Levels and Subclinical Atherosclerosis in Patients with Chronic Kidney and End-Stage Renal Diseases. Int. J. Clin. Pract. 2022, 2022, 4524637. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, J.S.; Kim, S.Y.; Kim, Y.G.; Moon, J.Y.; Jeong, K.H.; Lee, T.W.; Ihm, C.G.; Lee, S.H. Plasma endocan level and prognosis of immunoglobulin A nephropathy. Kidney Res. Clin. Pract. 2016, 35, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Bechard, D.; Scherpereel, A.; Hammad, H.; Gentina, T.; Tsicopoulos, A.; Aumercier, M.; Pestel, J.; Dessaint, J.P.; Tonnel, A.B.; Lassalle, P. Human endothelial-cell specific molecule-1 binds directly to the integrin CD11a/CD18 (LFA-1) and blocks binding to intercellular adhesion molecule-1. J. Immunol. 2001, 167, 3099–3106. [Google Scholar] [CrossRef] [PubMed]
- Arman, Y.; Akpinar, T.S.; Kose, M.; Emet, S.; Yuruyen, G.; Akarsu, M.; Ozcan, M.; Yegit, O.; Cakmak, R.; Altun, O.; et al. Effect of glycemic regulation on endocan levels in patients with diabetes: A preliminary study. Angiology 2016, 67, 239–244. [Google Scholar] [CrossRef]
- Townsend, R.R. Arterial Stiffness in CKD: A Review. Am. J. Kidney Dis. 2019, 73, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Késői, I.; Sági, B.; Tóth, O.I.; Vas, T.; Fazekas, A.; Kovács, T.; Pintér, T.; Wittmann, I.; Nagy, J. Different effect of IgA nephropathy and polycystic kidney disease on arterial stiffness. Kidney Blood Press. Res. 2011, 34, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Sági, B.; Késői, I.; Késői, B.; Vas, T.; Csiky, B.; Kovács, T.; Nagy, J. Arterial stiffness may predict renal and cardiovascular prognosis in autosomal-dominant polycystic kidney disease. Physiol. Int. 2018, 105, 145–156. [Google Scholar] [CrossRef]
- Ohno, Y.; Kanno, Y.; Takenaka, T. Central blood pressure and chronic kidney disease. World J. Nephrol. 2016, 5, 90. [Google Scholar] [CrossRef]
- Vickery, S.; Price, C.P.; John, R.I.; Abbas, N.A.; Webb, M.C.; Kempson, M.E.; Lamb, E.J. B-type natriuretic peptide (BNP) and amino terminal proBNP in patients with CKD: Relationship to renal function and left ventricular hypertrophy. Am. J. Kidney Dis. 2005, 46, 610–620. [Google Scholar] [CrossRef]
- Barton, M. Aging and endothelin: Determinants of disease. Life Sci. 2014, 118, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Hogg, R. An evaluation of the roles of hematuria and uric acid in defining the prognosis of patients with IgA nephropathy. Pediatr. Nephrol. 2022, 37, 947–958. [Google Scholar] [CrossRef] [PubMed]
- Weng, M.; Fu, B.; Zhuo, Y.; Lin, J.; Zou, Z.; Chen, Y.; Cui, J.; Li, G.; Chen, C.; Xu, Y.; et al. Association of time-averaged serum uric acid level with clinicopathological information and long-term outcomes in patients with IgA nephropathy. PeerJ 2024, 12, e17266. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.J.; Wang, C.H.; Lai, Y.H.; Kuo, C.H.; Lin, Y.L.; Hsu, B.G. Serum endocan is a risk factor for aortic stiffness in patients undergoing maintenance hemodialysis. Medicina 2024, 60, 984. [Google Scholar] [CrossRef] [PubMed]
- Peng, T.; Li, X.; Hu, Z.; Yang, X.; Ma, C. Predictive role of endothelin in left ventricular remodeling of chronic kidney disease. Ren. Fail. 2018, 40, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Diez, J.; Laviades, C. Hypertensive heart disease in the patient with chronic kidney disease. Nefrologia 2008, 28, 135–142. [Google Scholar] [PubMed]
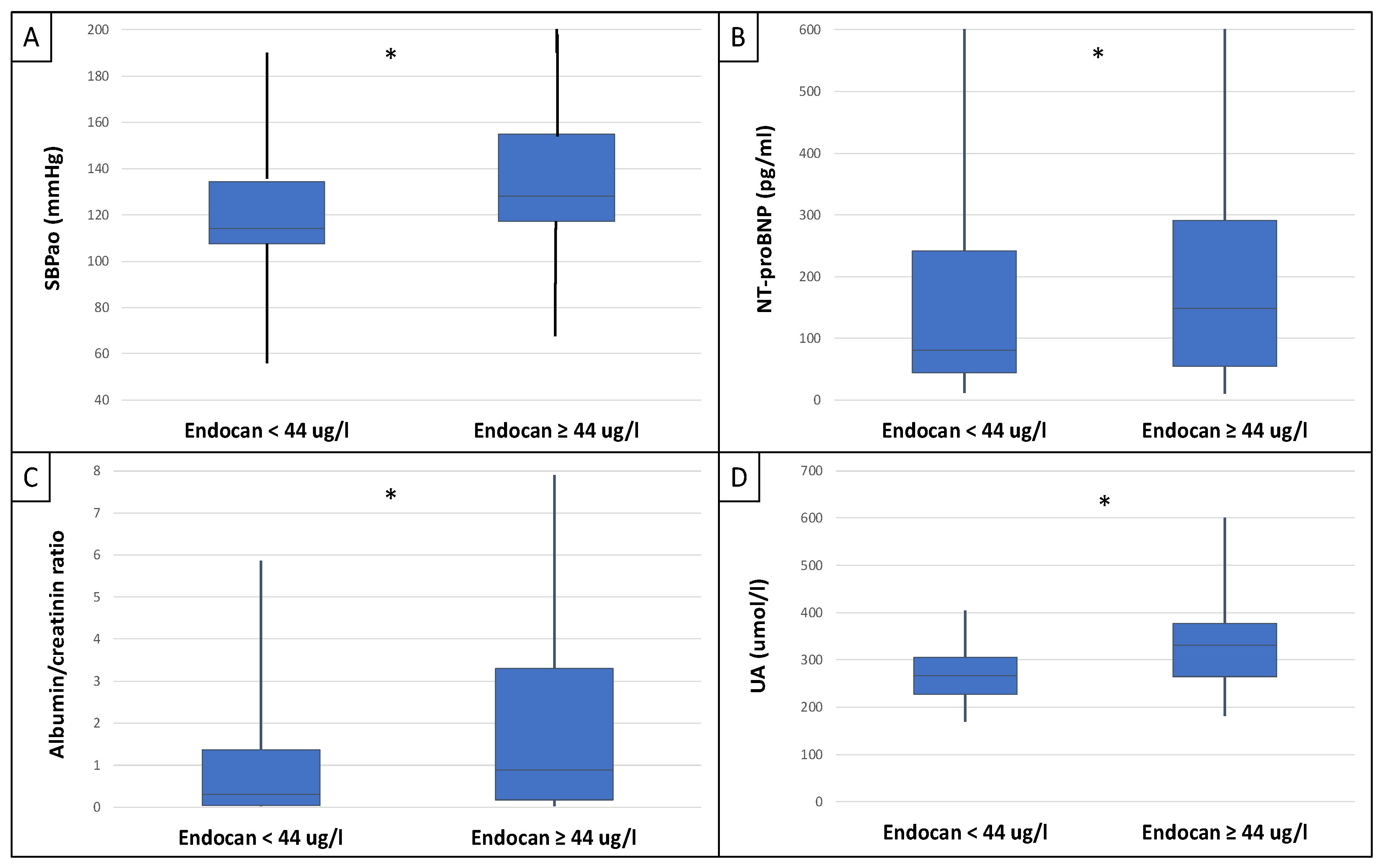
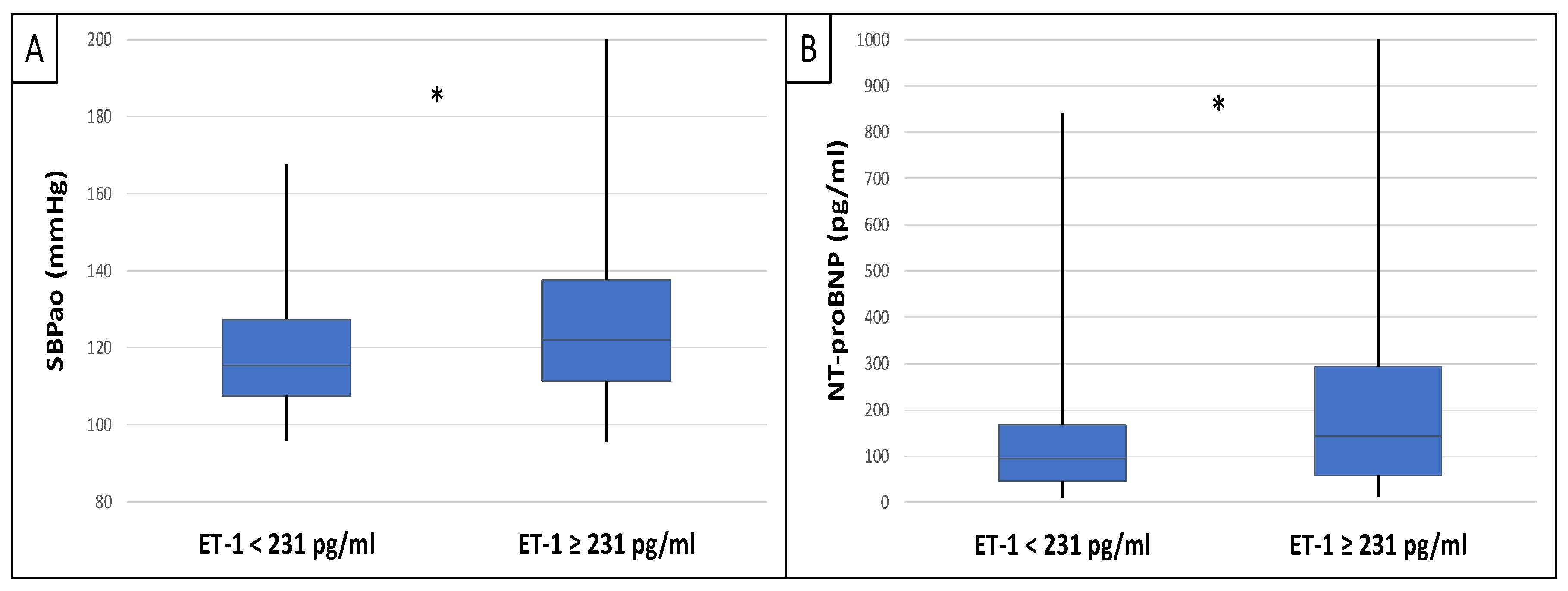
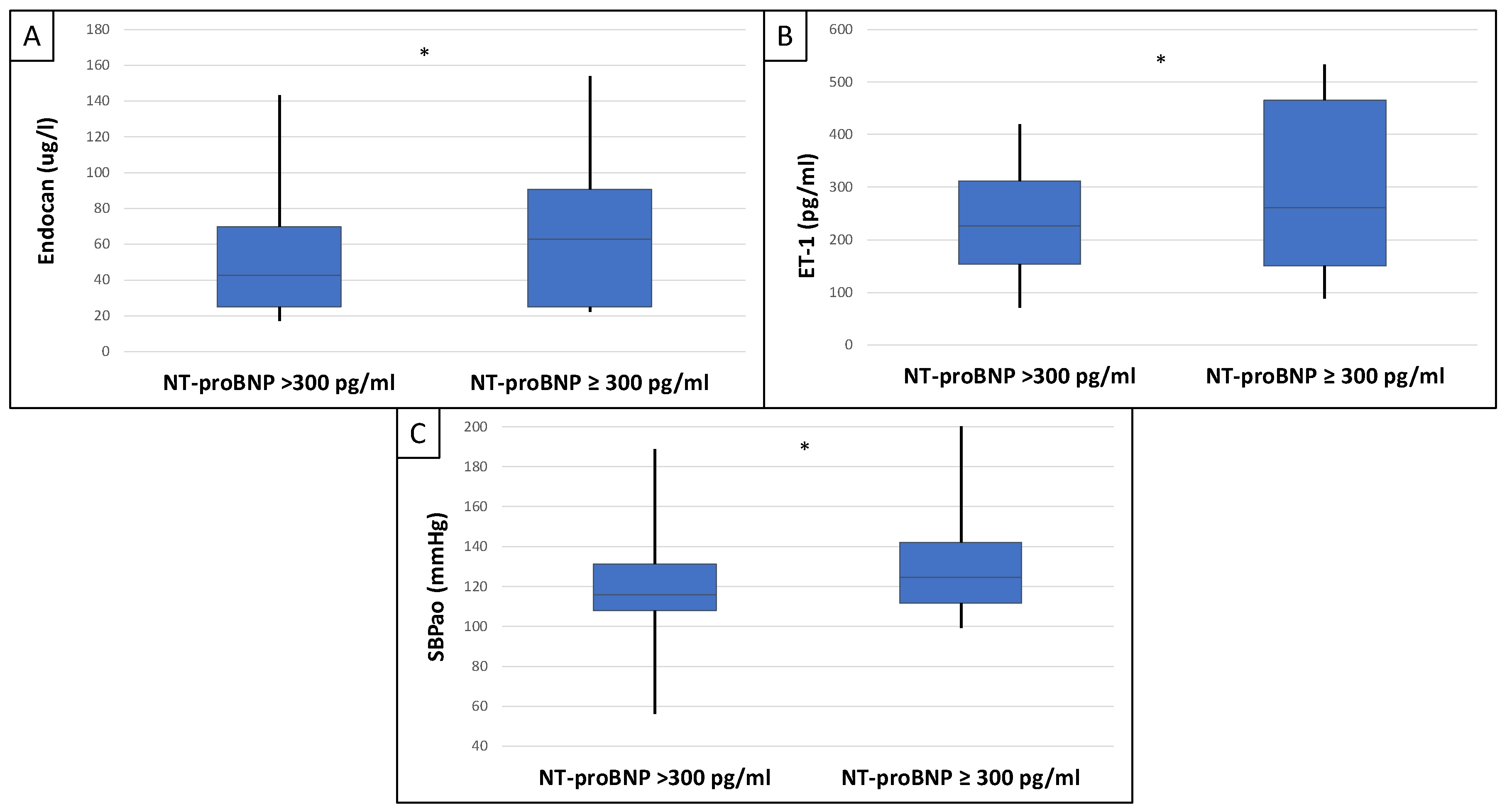
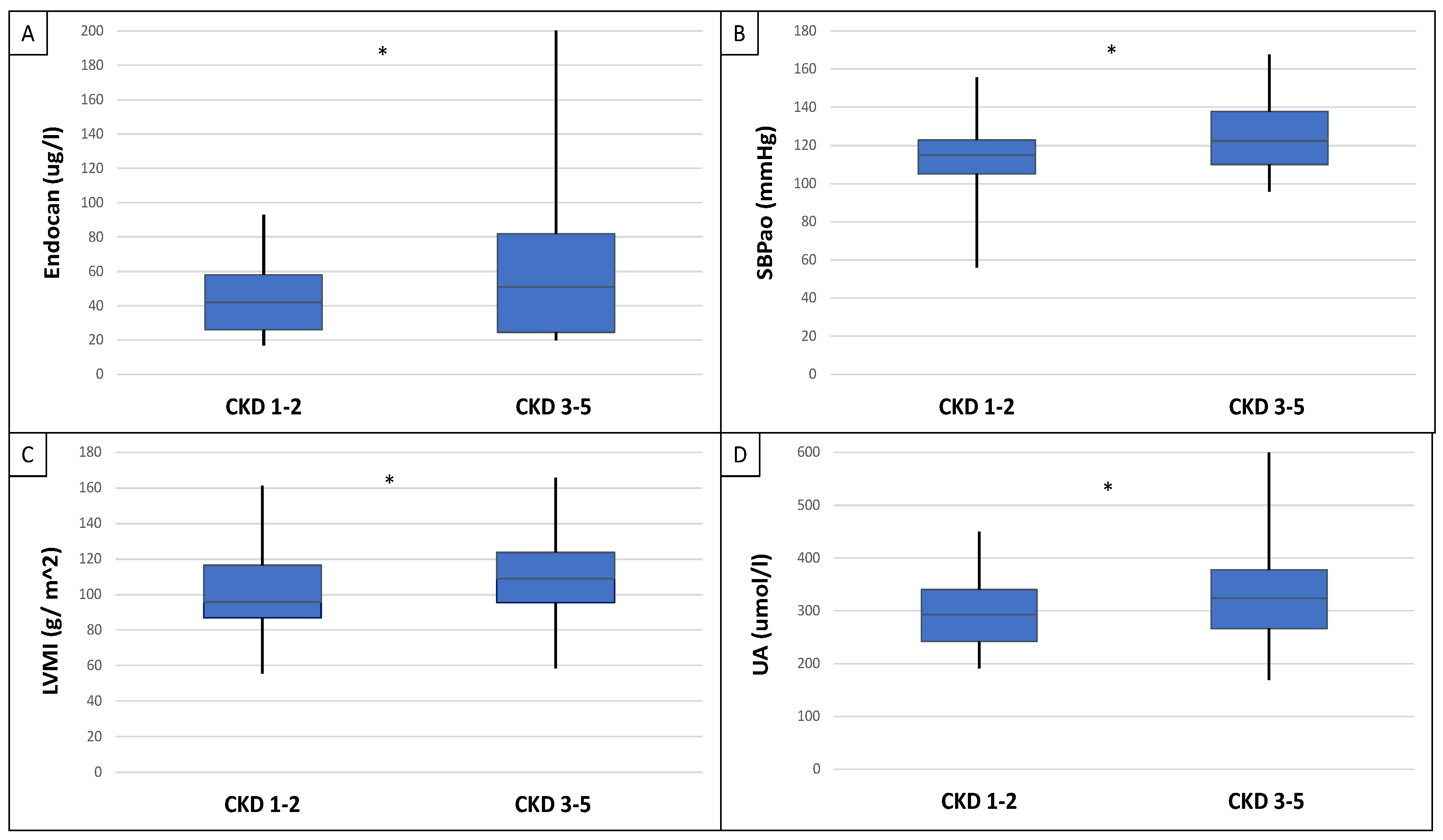
| Clinical Data | All Patients (n = 90) | Endocan < 44 ug/L (n = 44) | Endocan ≥ 44 ug/L (n = 45) | p | Endothelin-1 < 231 pg/mL (n = 46) | Endothelin-1 ≥ 231 pg/mL (n = 44) | p | CKD 1–2 (n = 42) | CKD 3–5 (n = 48) | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Male/female (n, %) | 50/40 (56/44) | 23/21 (52/48) | 26/19 (58/42) | NS | 28/18 (61/39) | 22/22 (50/50) | NS | 25/17 (60/40) | 25/23 (52/48) | NS |
| Age (year) | 54.92 ± 14.47 | 55.9 ± 14.99 | 53.9 ± 13.85 | NS | 58.2 ± 12.85 | 51.4 ± 15.5 | 0.012 * | 49.69 ± 14.80 | 59.68 ± 12.69 | <0.001 * |
| SBP/DBP (mmHg) | 124/78 ± 13/8 | 122/75 ± 13/10 | 125/80 ± 13/10 | NS | 122/76 ± 12/10 | 125/79 ± 14/10 | NS | 122/77 ± 14/8 | 125/78 ± 13/7 | NS |
| MAP (mmHg) | 88.91 ± 20.81 | 86.83 ± 22.49 | 90.83 ± 22.81 | NS | 85.41 ± 24.53 | 94.57 ± 14.3 | 0.018 * | 87.70 ± 23.15 | 91.91 ± 17.94 | NS |
| HR (beat/min) | 65.3 ± 9.49 | 64.6 ± 9.53 | 66.2 ± 12.46 | NS | 67.9 ± 9.86 | 63.1 ± 9.58 | NS | 63.8 ± 8.8 | 66.6 ± 9.87 | NS |
| cfPWV (m/s) | 9.9 ± 2.33 | 11.18 ± 5.72 | 11.99 ± 7.32 | NS | 10.7 ± 1.59 | 10.8 ± 2.77 | NS | 9.2 ± 2.18 | 10.6 ± 2.29 | 0.004 * |
| Aix (%) | 26.5 ± 13.68 | 38.95 ± 4.87 | 43.6 ± 3.73 | NS | 47.33 ± 6.91 | 39.18 ± 16.21 | NS | 25.7 ± 15.74 | 27.9 ± 11.63 | NS |
| Aorta PP (mmHg) | 38.4 ± 6.99 | 36.23 ± 7.35 | 35.97 ± 9.9 | NS | 34.5 ± 8.56 | 36.62 ± 8.77 | NS | 35.0 ± 3.46 | 43.5 ± 7.94 | NS |
| SBPao (mmHg) | 113.88 ± 12.8 | 114.55 ± 10.64 | 121.1 ± 14.03 | 0.013 * | 115.4 ± 15.57 | 122.1 ± 20.49 | 0.037 * | 115.33 ± 13.01 | 122.02 ± 12.72 | 0.044 * |
| Biomarkers | ||||||||||
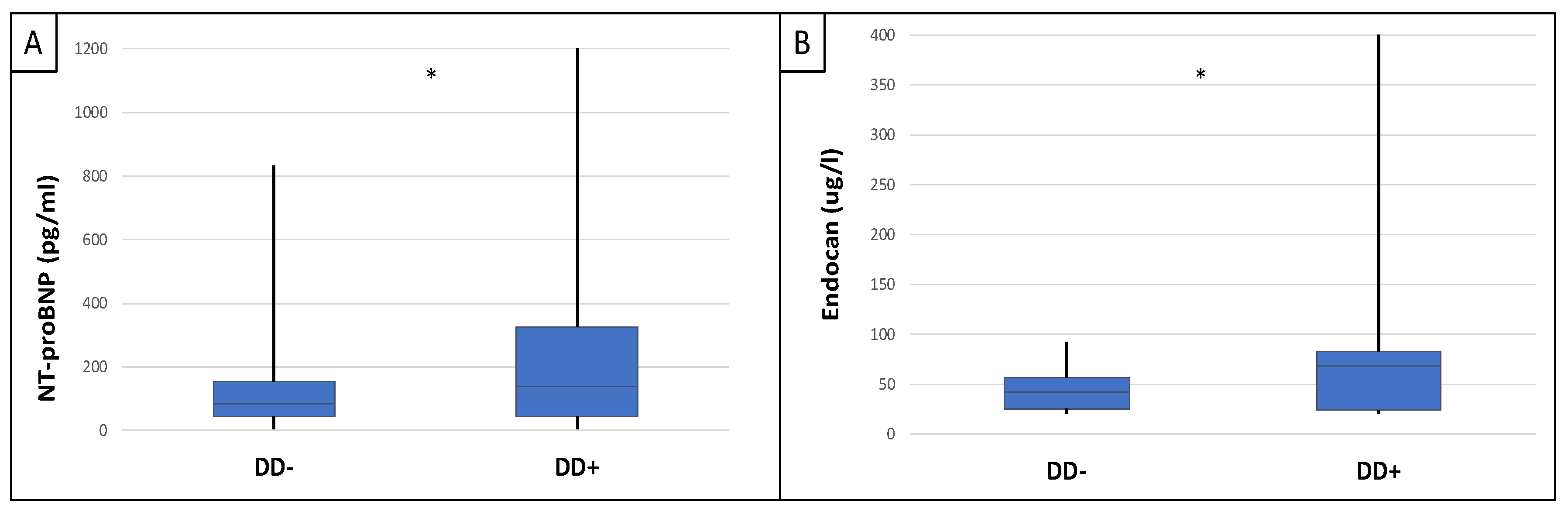
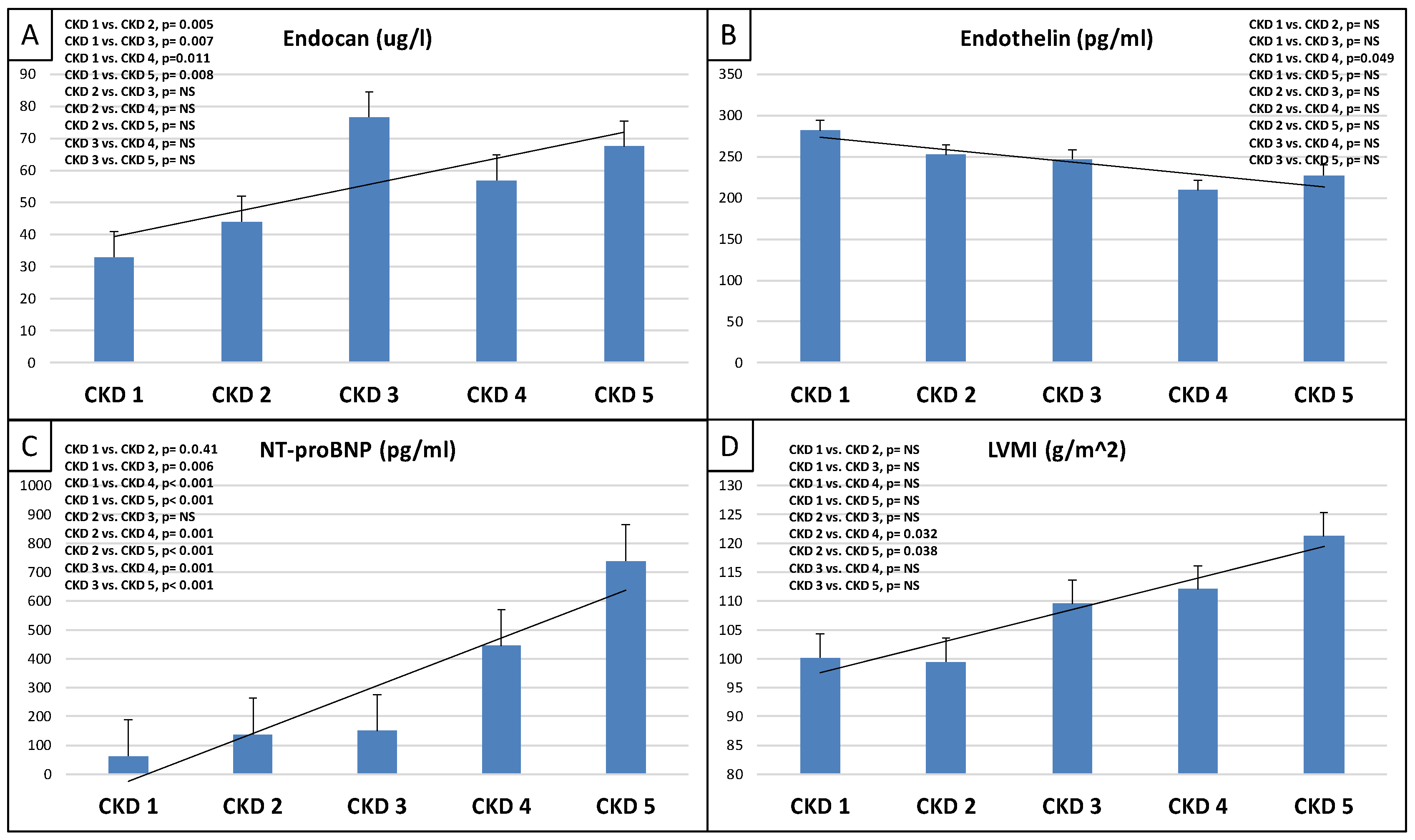
| NT-proBNP (pg/mL) | 256.22 ± 404.72 | 80.5 ± 155.57 | 148.5 ± 458.54 | 0.028 * | 94.88 ± 167.86 | 144.85 ± 418.59 | 0.038 * | 173.22 ± 382.22 | 419.03 ± 775.07 | 0.035 * |
| Endocan (ug/L) | 59.26 ± 65.75 | 27.34 ± 7.58 | 91.18 ± 80.94 | n.a. | 67.06 ± 84.72 | 51.45 ± 36.7 | NS | 42.0 ± 33.5 | 51.0 ± 37.25 | 0.047 * |
| Endothelin-1 (pg/mL) | 230.95 ± 101.95 | 260.96 ± 96.86 | 221.13 ± 103.03 | 0.034 * | 154.15 ± 47.49 | 327.94 ± 58.59 | n.a. | 251.89 ± 108.19 | 231.58 ± 95.17 | NS |
| Metabolic Parameters | ||||||||||
| BMI (kg/m2) | 28.51 ± 5.75 | 27.93 ± 5.45 | 29.57 ± 5.95 | NS | 29.79 ± 5.37 | 27.25 ± 5.81 | 0.019 * | 27.57 ± 5.21 | 29.34 ± 6.17 | NS |
| Obesity (n, %) | 60 (67) | 30 (68) | 30 (67) | NS | 33 (72) | 27 (61) | NS | 25 (60) | 35 (73) | NS |
| Hypertension (n, %) | 78 (87) | 38 (86) | 40 (89) | NS | 42 (91) | 36 (82) | 0.040 * | 28 (67) | 43 (90) | 0.005 * |
| Diabetes mellitus (n, %) | 16 (18) | 8 (18) | 8 (18) | NS | 12 (26) | 4 (9) | 0.013 * | 3 (7) | 12 (25) | 0.013 * |
| Dyslipidemia (n, %) | 32 (36) | 14 (32) | 17 (38) | NS | 17 (37) | 14 (32) | NS | 16 (38) | 16 (33) | NS |
| Metabolic syndrome (n, %) | 39 (43) | 17 (39) | 22 (49) | NS | 21 (46) | 18 (41) | NS | 16 (38) | 23 (48) | NS |
| Echocardiographic Parameters | ||||||||||
| LVEF(%) | 63.42 ± 5.86 | 63.96 ± 5.44 | 62.8 ± 6.18 | NS | 62.16 ± 5.59 | 64.7 ± 5.78 | 0.022 * | 65.25 ± 5.39 | 63.18 ± 6.02 | NS |
| LVMI (g/m2) | 102.76 ± 27.8 | 108.05 ± 25.18 | 105.89 ± 22.14 | NS | 105.89 ± 23.53 | 108.05 ± 23.92 | NS | 95.74.63 ± 22.37 | 108.94 ± 23.21 | 0.022 * |
| LVM (g) | 214.68 ± 62.2 | 222.55 ± 76.42 | 209.43 ± 47.66 | NS | 216.87 ± 61.91 | 211.8 ± 60.03 | NS | 234.4 ± 75.6 | 238.0 ± 51.26 | NS |
| RWT | 0.43 ± 0.07 | 0.37 ± 0.04 | 0.45 ± 0.07 | 0.026 * | 0.43 ± 0.07 | 0.44 ± 0.08 | NS | 0.468 ± 0.08 | 0.472 ± 0.07 | NS |
| LAD (mm) | 45.67 ± 6.05 | 45.56 ± 4.68 | 45.75 ± 7.13 | NS | 45.86 ± 6.75 | 45.17 ± 5.66 | NS | 44.81 ± 6.25 | 47.12 ± 5.52 | 0.014 * |
| LVEDd (mm) | 48.91 ± 4.39 | 48.71 ± 5.17 | 49.12 ± 3.4 | NS | 49.34 ± 4.33 | 48.5 ± 4.41 | NS | 48.1 ± 4.37 | 49.6 ± 4.29 | NS |
| LVESd (mm) | 30.17 ± 6.85 | 30.59 ± 8.74 | 29.75 ± 4.05 | NS | 29.86 ± 3.98 | 30.51 ± 8.98 | NS | 29.48 ± 8.69 | 30.81 ± 4.47 | NS |
| IVSd (mm) | 11.24 ± 1.44 | 11.26 ± 1.29 | 11.25 ± 1.58 | NS | 11.27 ± 1.41 | 11.20 ± 1.47 | NS | 11.04 ± 1.49 | 11.42 ± 1.37 | NS |
| LVPWd (mm) | 11.48 ± 1.57 | 11.47 ± 1.46 | 11.51 ± 1.68 | NS | 11.41 ± 1.46 | 11.55 ± 1.67 | NS | 11.29 ± 1.58 | 11.66 ± 1.54 | NS |
| RVIDd (mm) | 25.44 ± 7.56 | 24.81 ± 5.45 | 25.2 ± 5.78 | NS | 24.61 ± 5.67 | 25.48 ± 5.89 | NS | 23.52 ± 3.43 | 27.49 ± 6.23 | 0.044 * |
| LVH (n, %) | 41 (45) | 22 (50) | 19 (42) | NS | 17 (37) | 24 (54) | NS | 16 (38) | 25 (52) | NS |
| DD (n/%) | 44 (49) | 22 (50) | 22 (49) | NS | 21 (45) | 23 (52) | NS | 18 (43) | 26 (54) | NS |
| E/A | 1.03 ± 0.38 | 1.01 ± 0.36 | 1.05 ± 0.39 | NS | 1.03 ± 0.39 | 1.0 ± 0.36 | NS | 1.11 ± 0.39 | 0.98 ± 0.37 | NS |
| Laboratory Results | ||||||||||
| Creatinin (umol/L) | 155.41 ± 120.24 | 140.73 ± 102.21 | 170.09 ± 134.31 | NS | 164 ± 133.14 | 147.62 ± 106.64 | NS | 85.64 ± 15.29 | 212.77 ± 137.34 | n.a. |
| Urea nitrogen (mmol/L) | 14.85 ± 13.56 | 14.62 ± 11.56 | 15.01 ± 14.01 | NS | 14.92 ± 13.76 | 14.71 ± 12.04 | NS | 8.1 ± 2.9 | 17.87 ± 15.41 | n.a. |
| eGFR (mL/min) | 47.57 ± 23.24 | 58.6 ± 26.35 | 52.79 ± 26.26 | NS | 53.92 ± 26.24 | 57.38 ± 26.57 | NS | 72.61 ± 7.11 | 34.5 ± 16.32 | n.a. |
| AU (mg/L) | 247.62 ± 312.78 | 218.2 ± 334.19 | 276.3 ± 287.5 | NS | 201.36 ± 243.43 | 292.73 ± 362.37 | NS | 111.32 ± 204.06 | 323.63 ± 345.01 | <0.001 * |
| Uric acid (umol/L) | 314.23 ± 83.72 | 302.72 ± 61.55 | 332.0 ± 92.18 | 0.045 * | 330.92 ± 86.08 | 298.34 ± 77.05 | 0.040 * | 293.79 ± 61.4 | 326.38 ± 98.92 | NS |
| Total cholesterol (mmol/L) | 4.93 ± 1.31 | 4.95 ± 1.13 | 4.92 ± 1.44 | NS | 4.9 ± 1.48 | 4.95 ± 1.1 | NS | 4.98 ± 1.36 | 4.89 ± 1.3 | NS |
| HDL-C (mmol/L) | 1.34 ± 0.42 | 1.36 ± 0.46 | 1.32 ± 0.45 | NS | 1.29 ± 0.4 | 1.39 ± 0.42 | NS | 1.42 ± 0.43 | 1.28 ± 0.41 | NS |
| LDL-C (mmol) | 2.90 ± 1.14 | 2.91 ± 0.98 | 2.89 ± 1.25 | NS | 2.93 ± 1.27 | 2.87 ± 0.97 | NS | 2.94 ± 1.21 | 2.85 ± 1.09 | NS |
| TG (mmol) | 1.85 ± 1.36 | 1.63 ± 0.94 | 2.56 ± 1.62 | NS | 2.01 ± 1.58 | 1.69 ± 1.04 | NS | 1.73 ± 1.47 | 1.97 ± 1.27 | NS |
| Hb (g/dL) | 133.71 ± 28.68 | 137.52 ± 16.99 | 138.3 ± 16.1 | NS | 137.05 ± 17.4 | 138.8 ± 1566 | NS | 144.16 ± 14.47 | 124.88 ± 34.65 | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sági, B.; Vas, T.; Gál, C.; Horváth-Szalai, Z.; Kőszegi, T.; Nagy, J.; Csiky, B.; Kovács, T.J. The Relationship between Vascular Biomarkers (Serum Endocan and Endothelin-1), NT-proBNP, and Renal Function in Chronic Kidney Disease, IgA Nephropathy: A Cross-Sectional Study. Int. J. Mol. Sci. 2024, 25, 10552. https://doi.org/10.3390/ijms251910552
Sági B, Vas T, Gál C, Horváth-Szalai Z, Kőszegi T, Nagy J, Csiky B, Kovács TJ. The Relationship between Vascular Biomarkers (Serum Endocan and Endothelin-1), NT-proBNP, and Renal Function in Chronic Kidney Disease, IgA Nephropathy: A Cross-Sectional Study. International Journal of Molecular Sciences. 2024; 25(19):10552. https://doi.org/10.3390/ijms251910552
Chicago/Turabian StyleSági, Balázs, Tibor Vas, Csenge Gál, Zoltán Horváth-Szalai, Tamás Kőszegi, Judit Nagy, Botond Csiky, and Tibor József Kovács. 2024. "The Relationship between Vascular Biomarkers (Serum Endocan and Endothelin-1), NT-proBNP, and Renal Function in Chronic Kidney Disease, IgA Nephropathy: A Cross-Sectional Study" International Journal of Molecular Sciences 25, no. 19: 10552. https://doi.org/10.3390/ijms251910552
APA StyleSági, B., Vas, T., Gál, C., Horváth-Szalai, Z., Kőszegi, T., Nagy, J., Csiky, B., & Kovács, T. J. (2024). The Relationship between Vascular Biomarkers (Serum Endocan and Endothelin-1), NT-proBNP, and Renal Function in Chronic Kidney Disease, IgA Nephropathy: A Cross-Sectional Study. International Journal of Molecular Sciences, 25(19), 10552. https://doi.org/10.3390/ijms251910552






