Differential Fatty Acid Response of Resident Macrophages in Human Skeletal Muscle Fiber and Intermuscular Adipose Tissue
Abstract
1. Introduction
2. Results
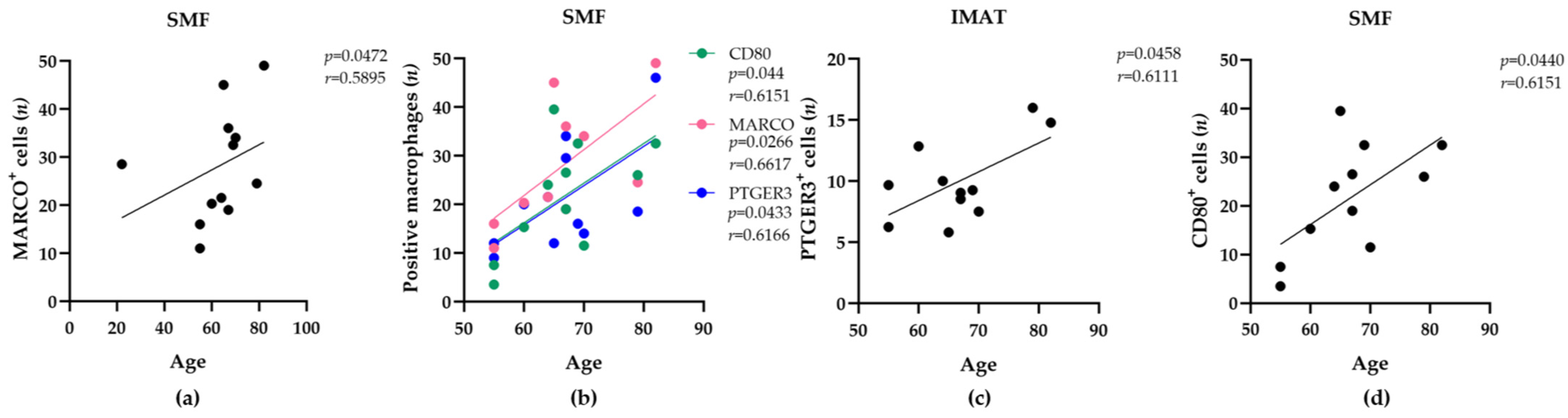
2.1. The Abundance of Resident MARCO+, CD80+, PTGER3+ Macrophages in Human Skeletal Muscle Tissue Increases with Age and BMI
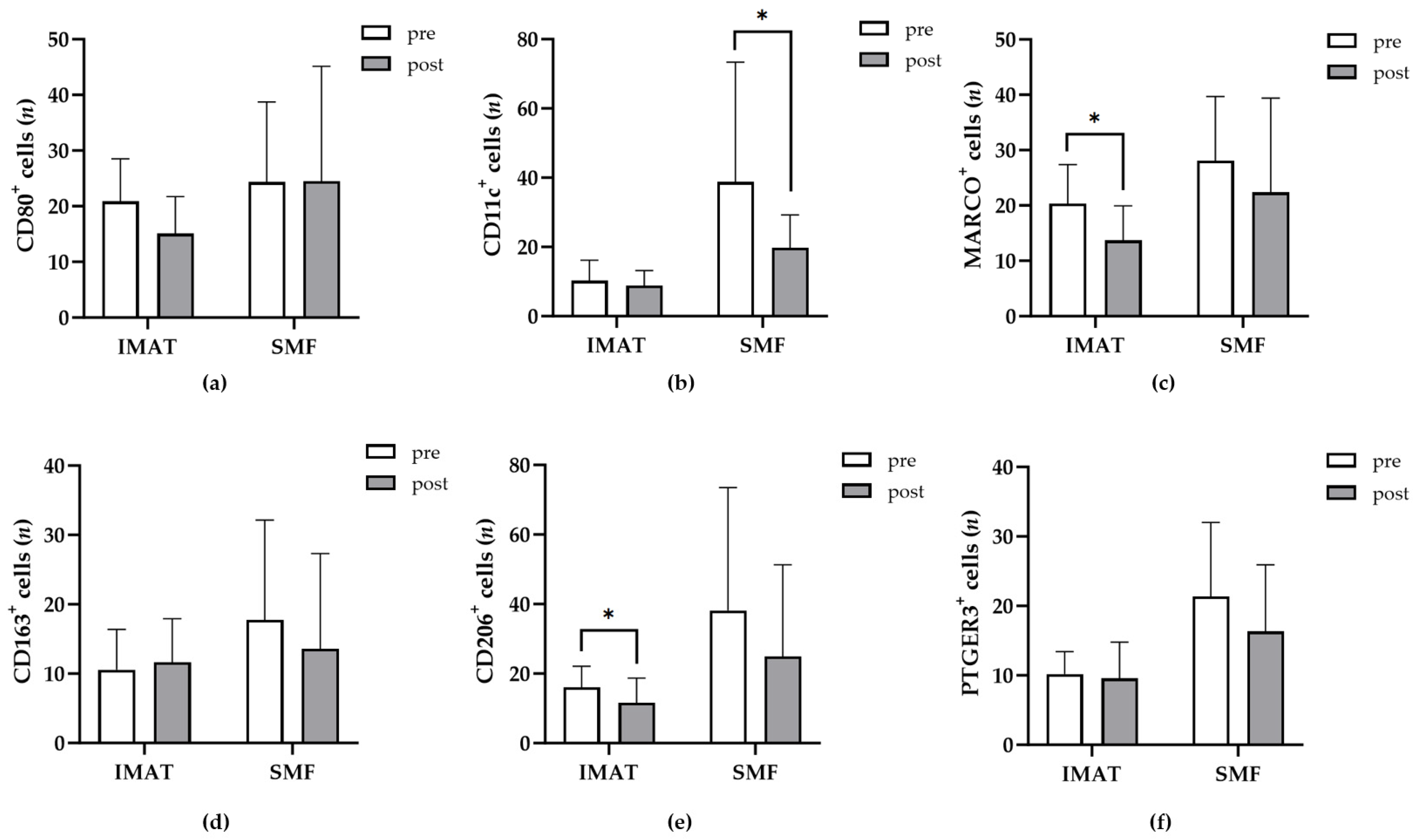
2.2. Macrophage Populations within Adjacent SMF and IMAT Differ
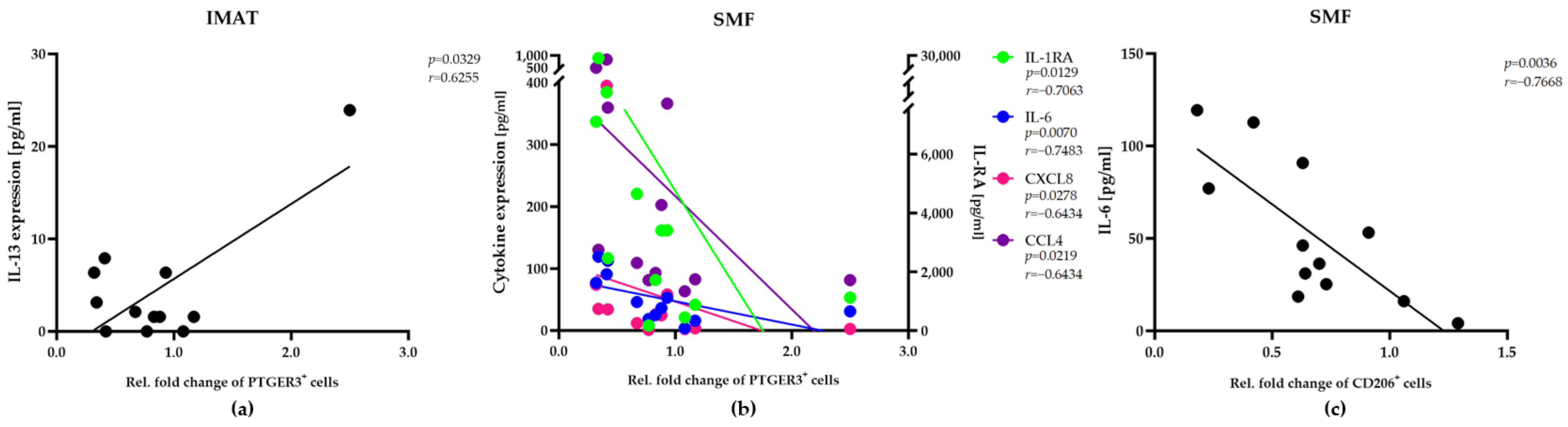
2.3. Alterations in the Abundance of the IMAT- and SMF-Resident Macrophage Populations Are Correlated with Selective Expression of Cytokines/Chemokines
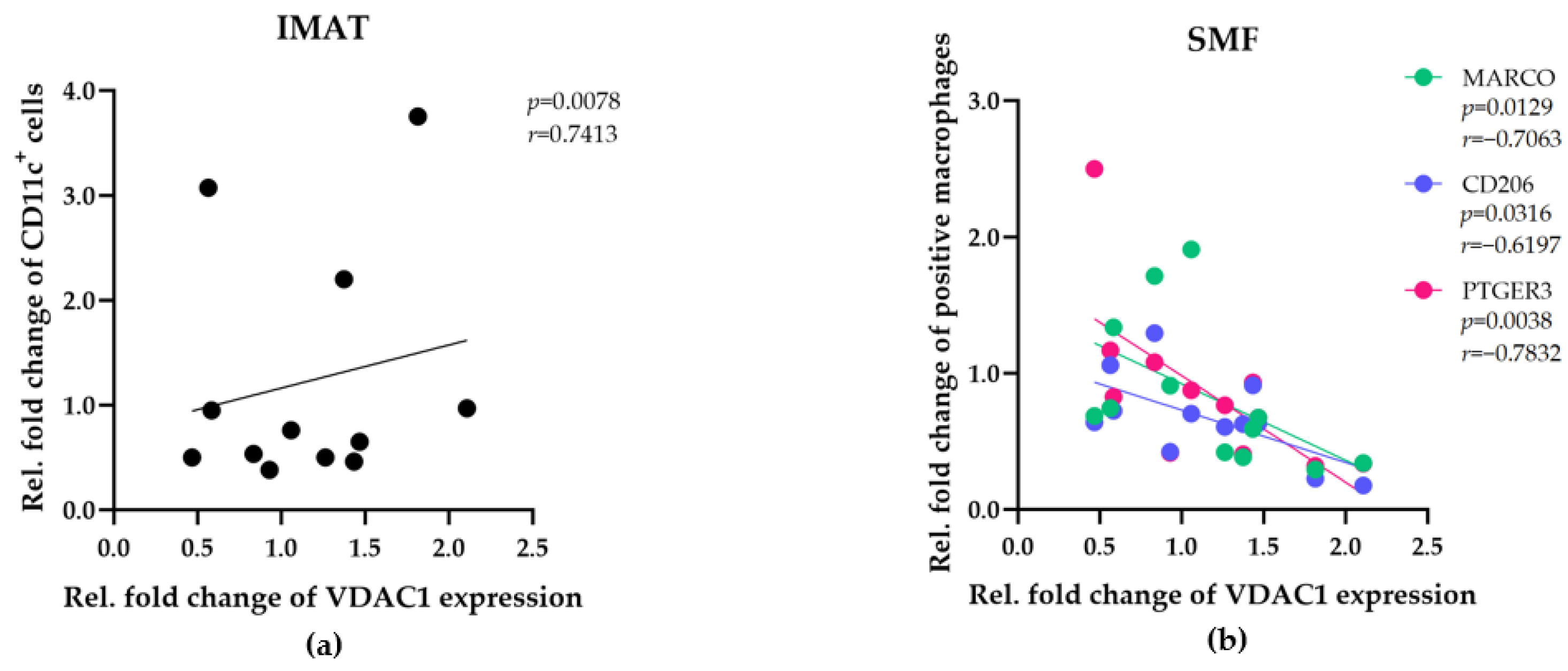
2.4. Alterations in the Abundance of IMAT- and SMF-Resident Macrophage Populations Are Correlated with Mitochondrial Activity
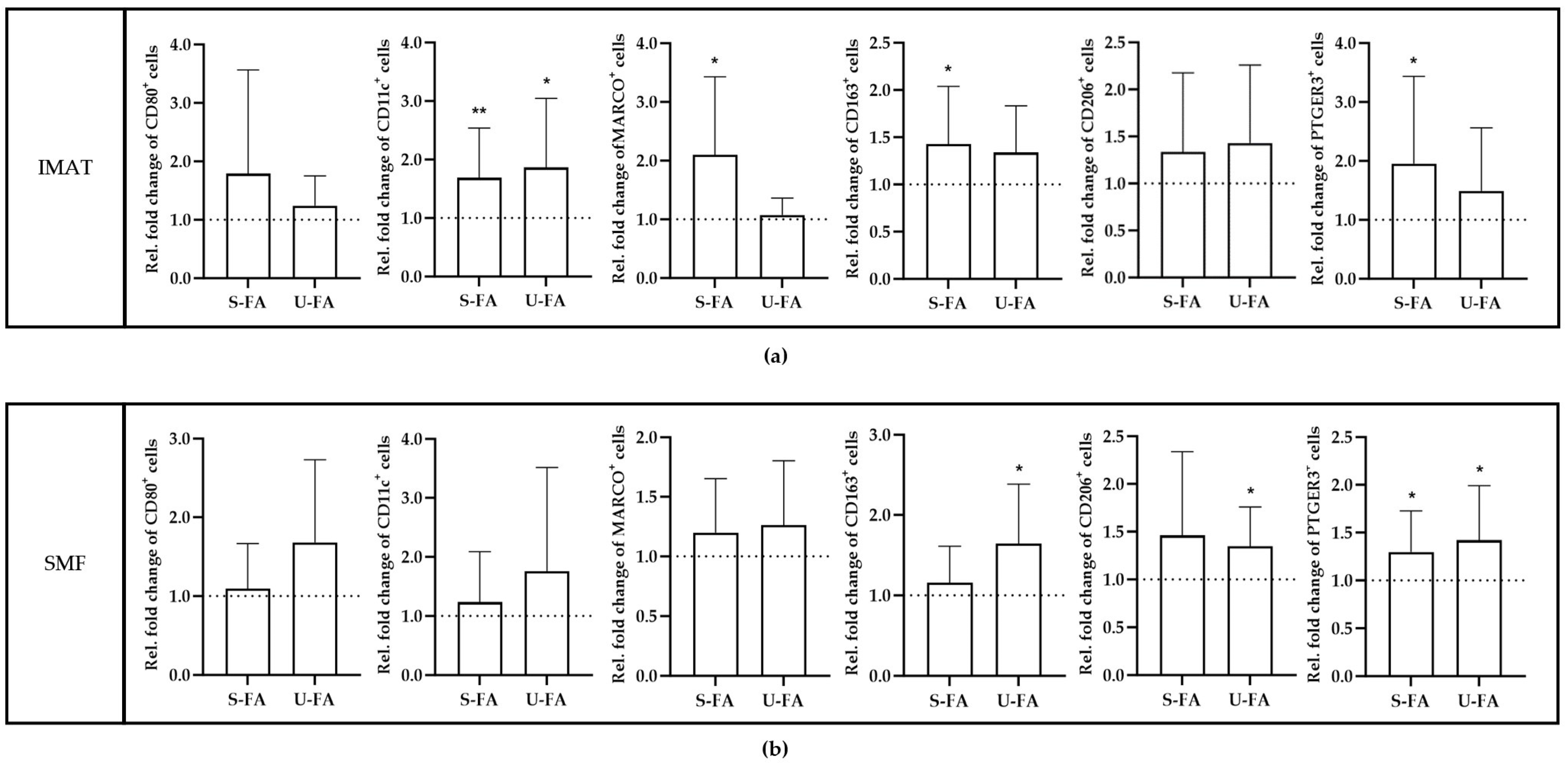
2.5. The Increase in Macrophage Populations in Response to FAs Is Significantly Different between IMATs and SMFs
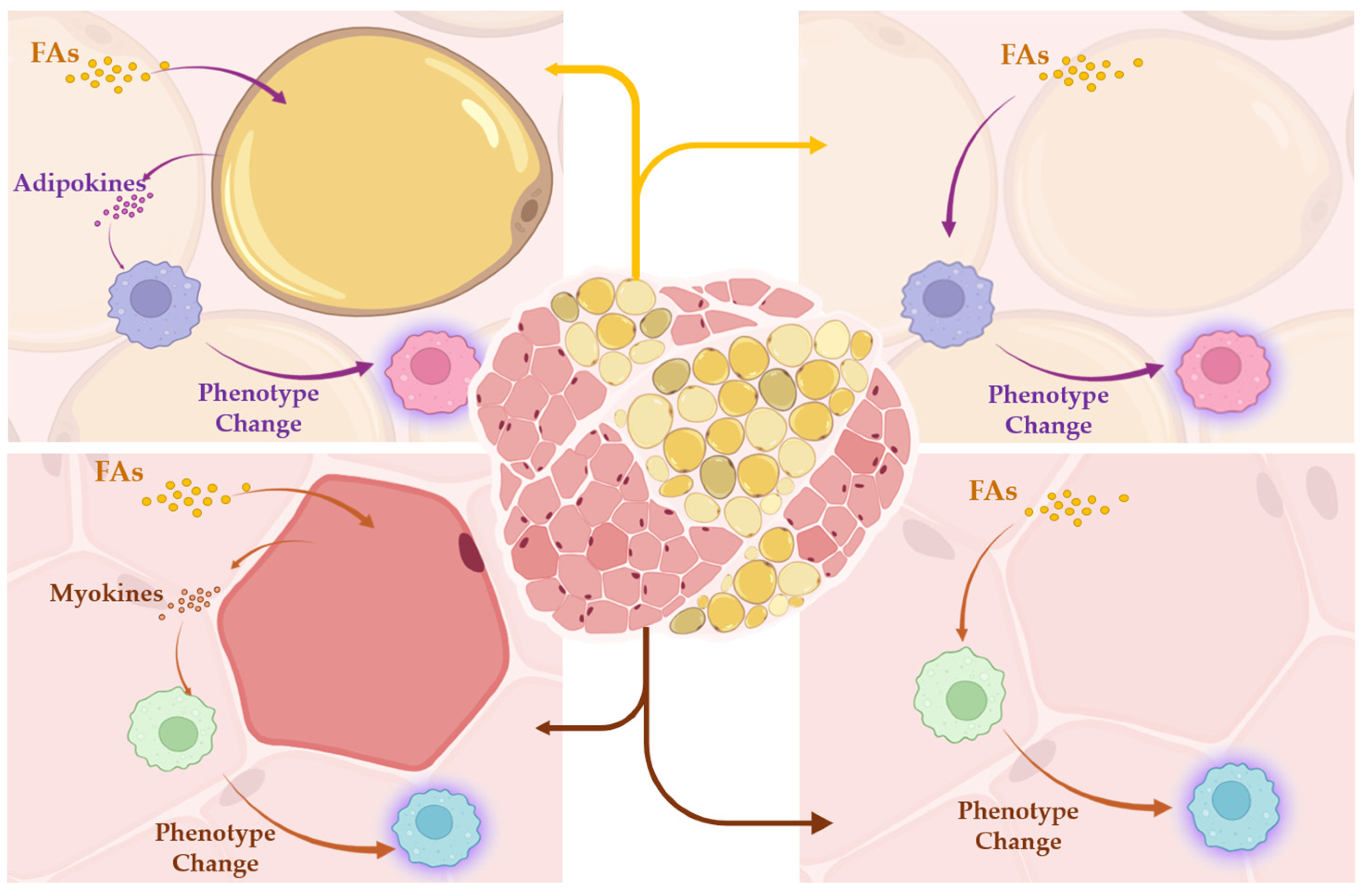
2.6. The FA-Induced Increase in Macrophage Populations Is Inversely Orchestrated between IMATs and SMFs
3. Discussion
4. Materials and Methods
4.1. Collecting of Skeletal Muscle Tissue Specimens
4.2. Quantification of Cytokines/Chemokines Expression in Tissue Samples
4.3. Handling and Maintaining of Human Tissue Samples
4.4. Hematoxylin and Eosin (HE) Staining
4.5. Immunofluorescence (IF) Detection of Human Macrophage Markers
4.6. HE and IF Imaging
4.7. Statistical Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pedersen, B.K.; Steensberg, A.; Keller, P.; Keller, C.; Fischer, C.; Hiscock, N.; van Hall, G.; Plomgaard, P.; Febbraio, M.A. Muscle-derived interleukin-6: Lipolytic, anti-inflammatory and immune regulatory effects. Pflugers Arch. 2003, 446, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Li, J.; Li, X.; Liu, Y. Intermuscular adipose tissue in obesity and related disorders: Cellular origins, biological characteristics and regulatory mechanisms. Front. Endocrinol. 2023, 14, 1280853. [Google Scholar] [CrossRef] [PubMed]
- Li, C.W.; Yu, K.; Shyh-Chang, N.; Jiang, Z.; Liu, T.; Ma, S.; Luo, L.; Guang, L.; Liang, K.; Ma, W.; et al. Pathogenesis of sarcopenia and the relationship with fat mass: Descriptive review. J. Cachexia Sarcopenia Muscle 2022, 13, 781–794. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Barnes, G.T.; Yang, Q.; Tan, G.; Yang, D.; Chou, C.J.; Sole, J.; Nichols, A.; Ross, J.S.; Tartaglia, L.A.; et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J. Clin. Investig. 2003, 112, 1821–1830. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.M.; Perrard, X.Y.; Brunner, G.; Lui, H.; Sparks, L.M.; Smith, S.R.; Wang, X.; Shi, Z.Z.; Lewis, D.E.; Wu, H.; et al. Intermuscular and perimuscular fat expansion in obesity correlates with skeletal muscle T cell and macrophage infiltration and insulin resistance. Int. J. Obes. 2015, 39, 1607–1618. [Google Scholar] [CrossRef]
- Kovalik, J.P.; Slentz, D.; Stevens, R.D.; Kraus, W.E.; Houmard, J.A.; Nicoll, J.B.; Lea-Currie, Y.R.; Everingham, K.; Kien, C.L.; Buehrer, B.M.; et al. Metabolic remodeling of human skeletal myocytes by cocultured adipocytes depends on the lipolytic state of the system. Diabetes 2011, 60, 1882–1893. [Google Scholar] [CrossRef]
- Irrcher, I.; Adhihetty, P.J.; Joseph, A.M.; Ljubicic, V.; Hood, D.A. Regulation of mitochondrial biogenesis in muscle by endurance exercise. Sports Med. 2003, 33, 783–793. [Google Scholar] [CrossRef]
- Serbulea, V.; Upchurch, C.M.; Schappe, M.S.; Voigt, P.; DeWeese, D.E.; Desai, B.N.; Meher, A.K.; Leitinger, N. Macrophage phenotype and bioenergetics are controlled by oxidized phospholipids identified in lean and obese adipose tissue. Proc. Natl. Acad. Sci. USA 2018, 115, E6254–E6263. [Google Scholar] [CrossRef]
- Clemente-Suarez, V.J.; Redondo-Florez, L.; Beltran-Velasco, A.I.; Martin-Rodriguez, A.; Martinez-Guardado, I.; Navarro-Jimenez, E.; Laborde-Cardenas, C.C.; Tornero-Aguilera, J.F. The Role of Adipokines in Health and Disease. Biomedicines 2023, 11, 1290. [Google Scholar] [CrossRef]
- Zunner, B.E.M.; Wachsmuth, N.B.; Eckstein, M.L.; Scherl, L.; Schierbauer, J.R.; Haupt, S.; Stumpf, C.; Reusch, L.; Moser, O. Myokines and Resistance Training: A Narrative Review. Int. J. Mol. Sci. 2022, 23, 3501. [Google Scholar] [CrossRef]
- Gautier, E.L.; Shay, T.; Miller, J.; Greter, M.; Jakubzick, C.; Ivanov, S.; Helft, J.; Chow, A.; Elpek, K.G.; Gordonov, S.; et al. Gene-expression profiles and transcriptional regulatory pathways that underlie the identity and diversity of mouse tissue macrophages. Nat. Immunol. 2012, 13, 1118–1128. [Google Scholar] [CrossRef] [PubMed]
- Wynn, T.A.; Chawla, A.; Pollard, J.W. Macrophage biology in development, homeostasis and disease. Nature 2013, 496, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Dick, S.A.; Wong, A.; Hamidzada, H.; Nejat, S.; Nechanitzky, R.; Vohra, S.; Mueller, B.; Zaman, R.; Kantores, C.; Aronoff, L.; et al. Three tissue resident macrophage subsets coexist across organs with conserved origins and life cycles. Sci. Immunol. 2022, 7, eabf7777. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Mara, A.B.; Musial, S.C.; Kolling, F.W.; Gibbings, S.L.; Gerebtsov, N.; Jakubzick, C.V. Coordinated chemokine expression defines macrophage subsets across tissues. Nat. Immunol. 2024, 25, 1110–1122. [Google Scholar] [CrossRef]
- Murray, P.J.; Allen, J.E.; Biswas, S.K.; Fisher, E.A.; Gilroy, D.W.; Goerdt, S.; Gordon, S.; Hamilton, J.A.; Ivashkiv, L.B.; Lawrence, T.; et al. Macrophage activation and polarization: Nomenclature and experimental guidelines. Immunity 2014, 41, 14–20. [Google Scholar] [CrossRef]
- Bao, Y.; Wang, G.; Li, H. Approaches for studying human macrophages. Trends Immunol. 2024, 45, 237–247. [Google Scholar] [CrossRef]
- Trim, W.V.; Walhin, J.P.; Koumanov, F.; Bouloumie, A.; Lindsay, M.A.; Chen, Y.C.; Travers, R.L.; Turner, J.E.; Thompson, D. Divergent immunometabolic changes in adipose tissue and skeletal muscle with ageing in healthy humans. J. Physiol. 2022, 600, 921–947. [Google Scholar] [CrossRef]
- Tomiyama, K.I.; Funada, M. Synthetic cannabinoid CP-55,940 induces apoptosis in a human skeletal muscle model via regulation of CB1 receptors and L-type Ca2+ channels. Arch. Toxicol. 2021, 95, 617–630. [Google Scholar] [CrossRef]
- Relaix, F.; Zammit, P.S. Satellite cells are essential for skeletal muscle regeneration: The cell on the edge returns centre stage. Development 2012, 139, 2845–2856. [Google Scholar] [CrossRef]
- Wibberley, A.; Staunton, C.A.; Feetham, C.H.; Vereninov, A.A.; Barrett-Jolley, R. An in vitro model of skeletal muscle volume regulation. PLoS ONE 2015, 10, e0127889. [Google Scholar] [CrossRef]
- Urciuolo, A.; Serena, E.; Ghua, R.; Zatti, S.; Giomo, M.; Mattei, N.; Vetralla, M.; Selmin, G.; Luni, C.; Vitulo, N.; et al. Engineering a 3D in vitro model of human skeletal muscle at the single fiber scale. PLoS ONE 2020, 15, e0232081. [Google Scholar] [CrossRef] [PubMed]
- Covert, L.T.; Patel, H.; Osman, A.; Duncan, L.; Dvergsten, J.; Truskey, G.A. Effect of type I interferon on engineered pediatric skeletal muscle: A promising model for juvenile dermatomyositis. Rheumatology 2024, 63, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Hao, D.; Becker, N.; Muckter, E.; Muller, A.; Pishnamaz, M.; Bollheimer, L.C.; Hildebrand, F.; Nourbakhsh, M. In Vitro Model of Human Skeletal Muscle Tissue for the Study of Resident Macrophages and Stem Cells. Biology 2022, 11, 936. [Google Scholar] [CrossRef] [PubMed]
- Krasniewski, L.K.; Chakraborty, P.; Cui, C.Y.; Mazan-Mamczarz, K.; Dunn, C.; Piao, Y.; Fan, J.; Shi, C.; Wallace, T.; Nguyen, C.; et al. Single-cell analysis of skeletal muscle macrophages reveals age-associated functional subpopulations. eLife 2022, 11, e77974. [Google Scholar] [CrossRef]
- Massa, R.; Marliera, L.N.; Martorana, A.; Cicconi, S.; Pierucci, D.; Giacomini, P.; De Pinto, V.; Castellani, L. Intracellular localization and isoform expression of the voltage-dependent anion channel (VDAC) in normal and dystrophic skeletal muscle. J. Muscle Res. Cell Motil. 2000, 21, 433–442. [Google Scholar] [CrossRef]
- Liu, G.; Wang, Y.; Pan, Y.; Tian, L.; Choi, M.H.; Wang, L.; Kim, J.Y.; Zhang, J.; Cheng, S.H.; Zhang, L. Hypertonicity induces mitochondrial extracellular vesicles (MEVs) that activate TNF-alpha and beta-catenin signaling to promote adipocyte dedifferentiation. Stem Cell Res. Ther. 2023, 14, 333. [Google Scholar] [CrossRef]
- Wueest, S.; Rapold, R.A.; Rytka, J.M.; Schoenle, E.J.; Konrad, D. Basal lipolysis, not the degree of insulin resistance, differentiates large from small isolated adipocytes in high-fat fed mice. Diabetologia 2009, 52, 541–546. [Google Scholar] [CrossRef]
- Chen, X.; Hao, D.; Becker, N.; Muller, A.; Pishnamaz, M.; Bollheimer, L.C.; Hildebrand, F.; Nourbakhsh, M. Unsaturated Long-Chain Fatty Acids Activate Resident Macrophages and Stem Cells in a Human Skeletal Muscle Tissue Model. Biology 2023, 12, 1111. [Google Scholar] [CrossRef]
- Szczesny, S.E. Ex vivo models of musculoskeletal tissues. Connect. Tissue Res. 2020, 61, 245–247. [Google Scholar] [CrossRef]
- Suka Aryana, I.G.P.; Paulus, I.B.; Kalra, S.; Daniella, D.; Kuswardhani, R.A.T.; Suastika, K.; Wibisono, S. The Important Role of Intermuscular Adipose Tissue on Metabolic Changes Interconnecting Obesity, Ageing and Exercise: A Systematic Review. touchRev. Endocrinol. 2023, 19, 54–59. [Google Scholar] [CrossRef]
- Poggiogalle, E.; Lubrano, C.; Gnessi, L.; Mariani, S.; Di Martino, M.; Catalano, C.; Lenzi, A.; Donini, L.M. The decline in muscle strength and muscle quality in relation to metabolic derangements in adult women with obesity. Clin. Nutr. 2019, 38, 2430–2435. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.P.; Chong, M.S.; Tay, L.; Yang, Y.X.; Leung, B.P.; Yeo, A.; Yew, S.; Tan, C.H.; Lim, W.S. Inter-muscular adipose tissue is associated with adipose tissue inflammation and poorer functional performance in central adiposity. Arch. Gerontol. Geriatr. 2019, 81, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, M.; Karlsen, A.; Mehling, J.; Soendenbroe, C.; Mackey, A.L.; Hyldahl, R.D. Aging is associated with an altered macrophage response during human skeletal muscle regeneration. Exp. Gerontol. 2022, 169, 111974. [Google Scholar] [CrossRef] [PubMed]
- Przybyla, B.; Gurley, C.; Harvey, J.F.; Bearden, E.; Kortebein, P.; Evans, W.J.; Sullivan, D.H.; Peterson, C.A.; Dennis, R.A. Aging alters macrophage properties in human skeletal muscle both at rest and in response to acute resistance exercise. Exp. Gerontol. 2006, 41, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Olefsky, J.M.; Glass, C.K. Macrophages, inflammation, and insulin resistance. Annu. Rev. Physiol. 2010, 72, 219–246. [Google Scholar] [CrossRef]
- Rasouli, N.; Molavi, B.; Elbein, S.C.; Kern, P.A. Ectopic fat accumulation and metabolic syndrome. Diabetes Obes. Metab. 2007, 9, 1–10. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Bergman, B.C.; Brennan, A.M.; Sparks, L.M. Intermuscular adipose tissue in metabolic disease. Nat. Rev. Endocrinol. 2023, 19, 285–298. [Google Scholar] [CrossRef]
- Ilich, J.Z.; Kelly, O.J.; Inglis, J.E.; Panton, L.B.; Duque, G.; Ormsbee, M.J. Interrelationship among muscle, fat, and bone: Connecting the dots on cellular, hormonal, and whole body levels. Ageing Res. Rev. 2014, 15, 51–60. [Google Scholar] [CrossRef]
- Virtue, S.; Masoodi, M.; de Weijer, B.A.; van Eijk, M.; Mok, C.Y.; Eiden, M.; Dale, M.; Pirraco, A.; Serlie, M.J.; Griffin, J.L.; et al. Prostaglandin profiling reveals a role for haematopoietic prostaglandin D synthase in adipose tissue macrophage polarisation in mice and humans. Int. J. Obes. 2015, 39, 1151–1160. [Google Scholar] [CrossRef][Green Version]
- Lee, M.K.; Ryu, H.; Van, J.Y.; Kim, M.J.; Jeong, H.H.; Jung, W.K.; Jun, J.Y.; Lee, B. The Role of Macrophage Populations in Skeletal Muscle Insulin Sensitivity: Current Understanding and Implications. Int. J. Mol. Sci. 2023, 24, 11467. [Google Scholar] [CrossRef]
- Jiang, L.Q.; Franck, N.; Egan, B.; Sjogren, R.J.; Katayama, M.; Duque-Guimaraes, D.; Arner, P.; Zierath, J.R.; Krook, A. Autocrine role of interleukin-13 on skeletal muscle glucose metabolism in type 2 diabetic patients involves microRNA let-7. Am. J. Physiol. Endocrinol. Metab. 2013, 305, E1359–E1366. [Google Scholar] [CrossRef] [PubMed]
- Poledne, R.; Malinska, H.; Kubatova, H.; Fronek, J.; Thieme, F.; Kauerova, S.; Lesna, I.K. Polarization of Macrophages in Human Adipose Tissue is Related to the Fatty Acid Spectrum in Membrane Phospholipids. Nutrients 2019, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Morales, F.E.; IglayReger, H.B.; Treutelaar, M.K.; Rothberg, A.E.; Hubal, M.J.; Nadler, E.P.; Robidoux, J.; Barakat, H.; Horowitz, J.F.; et al. Expression of macrophage genes within skeletal muscle correlates inversely with adiposity and insulin resistance in humans. Appl. Physiol. Nutr. Metab. 2018, 43, 187–193. [Google Scholar] [CrossRef]
- Amouzou, C.; Breuker, C.; Fabre, O.; Bourret, A.; Lambert, K.; Birot, O.; Fedou, C.; Dupuy, A.M.; Cristol, J.P.; Sutra, T.; et al. Skeletal Muscle Insulin Resistance and Absence of Inflammation Characterize Insulin-Resistant Grade I Obese Women. PLoS ONE 2016, 11, e0154119. [Google Scholar] [CrossRef] [PubMed]


| Participants | Sex | Age (Years) | BMI (kg/m2) | Type 2 Diabetes (T2D) |
|---|---|---|---|---|
| P1 | Female | 79 | 22.8 | No |
| P2 | Female | 67 | 46.9 | Yes |
| P3 | Female | 55 | 16.7 | No |
| P4 | Female | 64 | 33.8 | No |
| P5 | Female | 60 | 22.1 | No |
| P6 | Female | 55 | 22.6 | No |
| P7 | Female | 69 | 22.3 | No |
| P8 | Female | 70 | 20.0 | No |
| P9 | Female | 82 | 30.5 | No |
| P10 | Male | 67 | 28.6 | No |
| P11 | Female | 22 | 20.3 | No |
| P12 | Male | 65 | 24.2 | No |
| IMAT | SMF | |||
|---|---|---|---|---|
| S-FA | U-FA | S-FA | U-FA | |
| CD80 | 0.1406 | 0.1684 | 0.1406 | 0.0710 |
| CD11c | 0.0098 | 0.0273 | 0.0098 | 0.1602 |
| MARCO | 0.0210 | 0.4209 | 0.0210 | 0.1598 |
| CD163 | 0.0427 | 0.0592 | 0.0427 | 0.0224 |
| CD206 | 0.4648 | 0.3613 | 0.4648 | 0.0261 |
| PTGER3 | 0.0244 | 0.1934 | 0.0244 | 0.0195 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, X.; Müller, A.; Pishnamaz, M.; Hildebrand, F.; Bollheimer, L.C.; Nourbakhsh, M. Differential Fatty Acid Response of Resident Macrophages in Human Skeletal Muscle Fiber and Intermuscular Adipose Tissue. Int. J. Mol. Sci. 2024, 25, 10722. https://doi.org/10.3390/ijms251910722
Chen X, Müller A, Pishnamaz M, Hildebrand F, Bollheimer LC, Nourbakhsh M. Differential Fatty Acid Response of Resident Macrophages in Human Skeletal Muscle Fiber and Intermuscular Adipose Tissue. International Journal of Molecular Sciences. 2024; 25(19):10722. https://doi.org/10.3390/ijms251910722
Chicago/Turabian StyleChen, Xiaoying, Aline Müller, Miguel Pishnamaz, Frank Hildebrand, Leo Cornelius Bollheimer, and Mahtab Nourbakhsh. 2024. "Differential Fatty Acid Response of Resident Macrophages in Human Skeletal Muscle Fiber and Intermuscular Adipose Tissue" International Journal of Molecular Sciences 25, no. 19: 10722. https://doi.org/10.3390/ijms251910722
APA StyleChen, X., Müller, A., Pishnamaz, M., Hildebrand, F., Bollheimer, L. C., & Nourbakhsh, M. (2024). Differential Fatty Acid Response of Resident Macrophages in Human Skeletal Muscle Fiber and Intermuscular Adipose Tissue. International Journal of Molecular Sciences, 25(19), 10722. https://doi.org/10.3390/ijms251910722







