Expressions of HuR, Methyl-HuR and Phospho-HuR in Endometrial Endometrioid Adenocarcinoma Are Associated with Clinical Features
Abstract
1. Introduction
2. Results
2.1. Population Characteristics
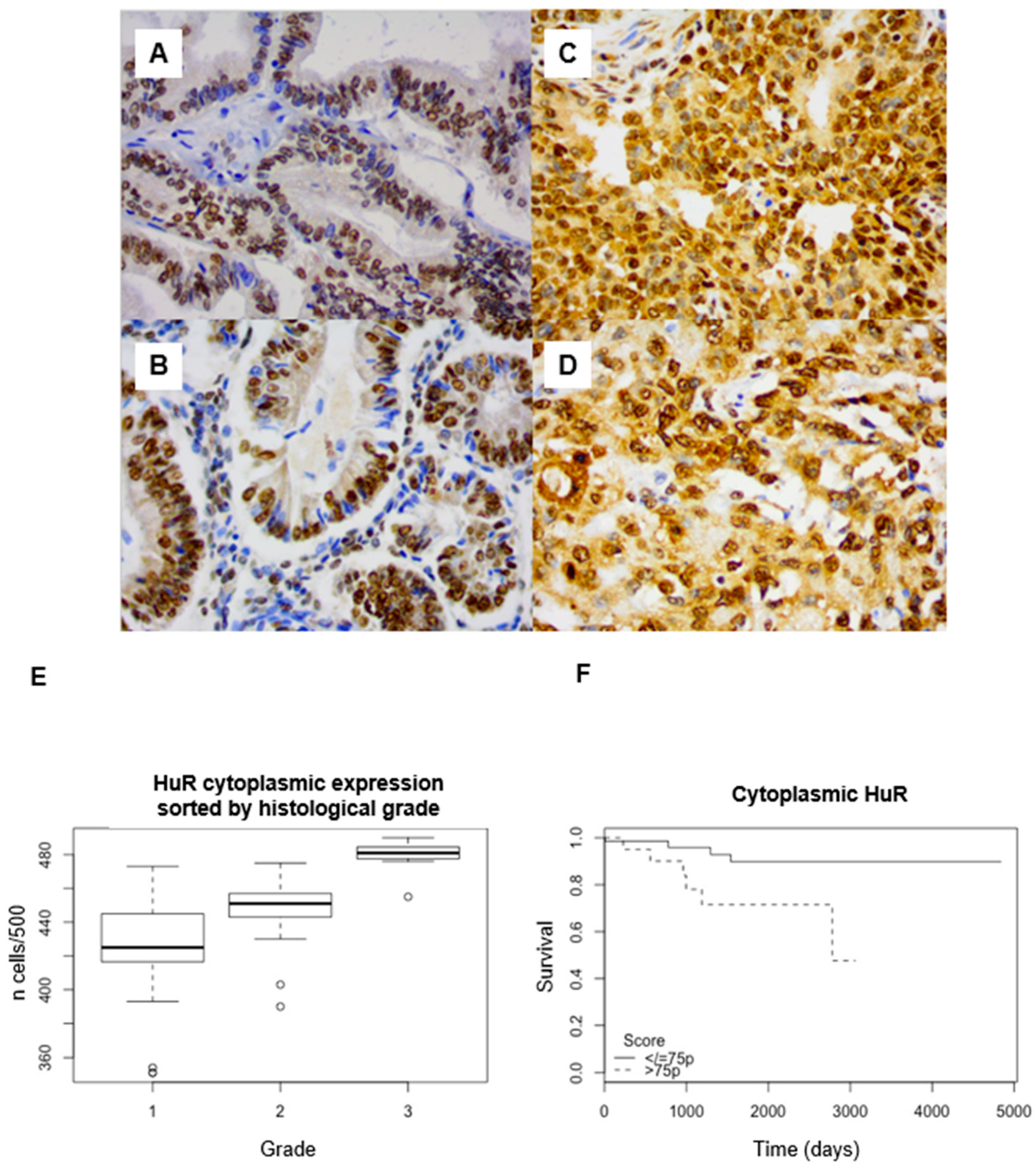
2.2. HuR Expression in Endometrioid Endometrial Cancer
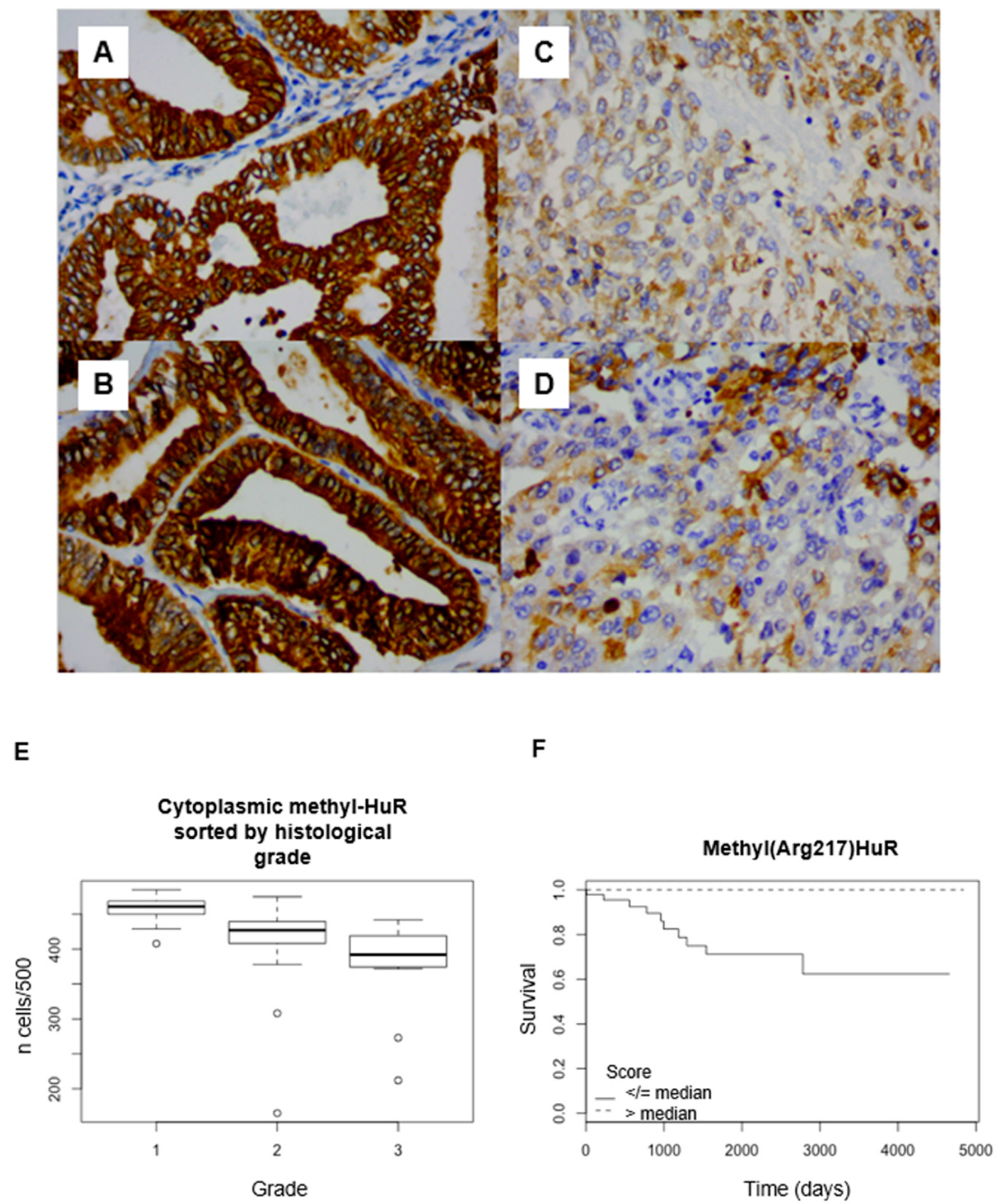
2.3. Post-Translational Modified HuR Expression
2.4. Proliferation Markers Correlation with HuR Expression
2.5. Inter-Observer Reproducibility
3. Discussion
3.1. HuR Is Overexpressed in Endometrial Adenocarcinoma
3.2. Cell Proliferation Markers Are Correlated with HuR Overexpression
3.3. Significance of mHuR Expression
3.4. Significance of pHuR Expression
3.5. Clinical Perspectives
4. Materials and Methods
4.1. Study Population
4.2. Immunohistochemistry
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Fleming, G.F.; Brunetto, V.L.; Cella, D.; Look, K.Y.; Reid, G.C.; Munkarah, A.R.; Kline, R.; Burger, R.A.; Goodman, A.; Burks, R.T. Phase III trial of doxorubicin plus cisplatin with or without paclitaxel plus filgrastim in advanced endometrial carcinoma: A gynecologic oncology group study. J. Clin. Oncol. 2004, 22, 2159–2166. [Google Scholar] [CrossRef]
- Ma, W.-J.; Furneaux, H. Localization of the human HuR gene to chromosome 19p13.2. Hum. Genet. 1997, 99, 32–33. [Google Scholar] [CrossRef]
- Mukherjee, N.; Corcoran, D.L.; Nusbaum, J.D.; Reid, D.W.; Georgiev, S.; Hafner, M.; Ascano, M.; Tuschl, T.; Ohler, U.; Keene, J.D. Integrative regulatory mapping indicates that the RNA-binding protein HuR couples Pre-mRNA processing and mRNA stability. Mol. Cell 2011, 43, 327–339. [Google Scholar] [CrossRef]
- Wang, J.; Guo, Y.; Chu, H.; Guan, Y.; Bi, J.; Wang, B. Multiple functions of the RNA-binding protein HuR in cancer progression, treatment responses and prognosis. Int. J. Mol. Sci. 2013, 14, 10015–10041. [Google Scholar] [CrossRef]
- López de Silanes, I.; Fan, J.; Yang, X.; Zonderman, A.B.; Potapova, O.; Pizer, E.S.; Gorospe, M. Role of the RNA-binding protein HuR in colon carcinogenesis. Oncogene 2003, 22, 7146–7154. [Google Scholar] [CrossRef]
- Yoo, P.S.; Sullivan, C.A.W.; Kiang, S.; Gao, W.; Uchio, E.M.; Chung, G.G.; Cha, C.H. Tissue microarray analysis of 560 patients with colorectal adenocarcinoma: High expression of HuR predicts poor survival. Ann. Surg. Oncol. 2009, 16, 200–207. [Google Scholar] [CrossRef]
- Denkert, C.; Weichert, W.; Pest, S.; Koch, I.; Licht, D.; Köbel, M.; Reles, A.; Sehouli, J.; Dietel, M.; Hauptmann, S. Overexpression of the embryonic-lethal abnormal vision-like protein HuR in ovarian carcinoma is a prognostic factor and is associated with increased cyclooxygenase 2 expression. Cancer Res. 2004, 64, 189–195. [Google Scholar] [CrossRef]
- Denkert, C.; Weichert, W.; Winzer, K.-J.; Müller, B.-M.; Noske, A.; Niesporek, S.; Kristiansen, G.; Guski, H.; Dietel, M.; Hauptmann, S. Expression of the ELAV-like protein HuR is associated with higher tumor grade and increased cyclooxygenase-2 expression in human breast carcinoma. Clin. Cancer Res. 2004, 10, 5580–5586. [Google Scholar] [CrossRef]
- Gauchotte, G.; Hergalant, S.; Vigouroux, C.; Casse, J.-M.; Houlgatte, R.; Kaoma, T.; Helle, D.; Brochin, L.; Rech, F.; Peyre, M.; et al. Cytoplasmic overexpression of RNA-binding protein HuR is a marker of poor prognosis in meningioma, and HuR knockdown decreases meningioma cell growth and resistance to hypoxia. J. Pathol. 2017, 242, 421–434. [Google Scholar] [CrossRef]
- Vigouroux, C.; Casse, J.-M.; Battaglia-Hsu, S.-F.; Brochin, L.; Luc, A.; Paris, C.; Lacomme, S.; Gueant, J.-L.; Vignaud, J.-M.; Gauchotte, G. Methyl(R217)HuR and MCM6 are inversely correlated and are prognostic markers in non small cell lung carcinoma. Lung Cancer 2015, 89, 189–196. [Google Scholar] [CrossRef]
- Wang, D.; Wang, M.; Hu, C.; Shuang, T.; Zhou, Y.; Yan, X. Expression of the ELAV-like protein HuR in the cytoplasm is associated with endometrial carcinoma progression. Tumor Biol. 2014, 35, 11939–11947. [Google Scholar] [CrossRef]
- Hotton, J.; Agopiantz, M.; Leroux, A.; Charra-Brunaud, C.; Marie, B.; Busby-Venner, H.; Morel, O.; Guéant, J.-L.; Vignaud, J.-M.; Battaglia-Hsu, S.-F.; et al. Minichromosome maintenance complex component 6 (MCM6) expression correlates with histological grade and survival in endometrioid endometrial adenocarcinoma. Virchows Arch. 2018, 472, 623–633. [Google Scholar] [CrossRef]
- Kundu, P.; Fabian, M.R.; Sonenberg, N.; Bhattacharyya, S.N.; Filipowicz, W. HuR protein attenuates miRNA-mediated repression by promoting miRISC dissociation from the target RNA. Nucleic Acids Res. 2012, 40, 5088–5100. [Google Scholar] [CrossRef]
- Fan, X.C.; Steitz, J.A. HNS, a nuclear-cytoplasmic shuttling sequence in HuR. Proc. Natl. Acad. Sci. USA 1998, 95, 15293–15298. [Google Scholar] [CrossRef]
- López de Silanes, I.; Lal, A.; Gorospe, M. HuR: Post-transcriptional paths to malignancy. RNA Biol. 2005, 2, 11–13. [Google Scholar] [CrossRef]
- Nabors, L.B.; Gillespie, G.Y.; Harkins, L.; King, P.H. HuR, a RNA stability factor, is expressed in malignant brain tumors and binds to adenine- and uridine-rich elements within the 3′ untranslated regions of cytokine and angiogenic factor mRNAs. Cancer Res. 2001, 61, 2154–2161. [Google Scholar]
- Heinonen, M.; Bono, P.; Narko, K.; Chang, S.-H.; Lundin, J.; Joensuu, H.; Furneaux, H.; Hla, T.; Haglund, C.; Ristimäki, A. Cytoplasmic HuR expression is a prognostic factor in invasive ductal breast carcinoma. Cancer Res. 2005, 65, 2157–2161. [Google Scholar] [CrossRef]
- Erkinheimo, T.-L.; Sivula, A.; Lassus, H.; Heinonen, M.; Furneaux, H.; Haglund, C.; Butzow, R.; Ristimäki, A. Cytoplasmic HuR expression correlates with epithelial cancer cell but not with stromal cell cyclooxygenase-2 expression in mucinous ovarian carcinoma. Gynecol. Oncol. 2005, 99, 14–19. [Google Scholar] [CrossRef]
- A Milne, A.N.; Carvalho, R.; Morsink, F.M.; Musler, A.R.; de Leng, W.W.J.; Ristimäki, A.; A Offerhaus, G.J. Early-onset gastric cancers have a different molecular expression profile than conventional gastric cancers. Mod. Pathol. 2006, 19, 564–572. [Google Scholar] [CrossRef]
- Denkert, C.; Koch, I.; von Keyserlingk, N.; Noske, A.; Niesporek, S.; Dietel, M.; Weichert, W. Expression of the ELAV-like protein HuR in human colon cancer: Association with tumor stage and cyclooxygenase-2. Mod. Pathol. 2006, 19, 1261–1269. [Google Scholar] [CrossRef]
- Karipcin, F.S.; Ensari, T.A.; Kayisli, U.A.; Guzel, E.; Kallen, C.B.; Seli, E. The mRNA-binding protein HuR is regulated in the menstrual cycle and repressed in ectopic endometrium. Reprod. Sci. Thousand Oaks Calif. 2011, 18, 145–155. [Google Scholar] [CrossRef]
- Gauchotte, G.; Bédel, C.; Lardenois, E.; Hergalant, S.; Cuglietta, L.; Pflaum, R.; Lacomme, S.; Pina, H.; Treffel, M.; Rech, F.; et al. A High MCM6 Proliferative Index in Atypical Meningioma Is Associated with Shorter Progression Free and Overall Survivals. Cancers 2023, 15, 535. [Google Scholar] [CrossRef]
- Grammatikakis, I.; Abdelmohsen, K.; Gorospe, M. Posttranslational control of HuR function. Wiley Interdiscip. Rev. RNA 2017, 8, e1372. [Google Scholar] [CrossRef]
- Li, H.; Park, S.; Kilburn, B.; Jelinek, M.A.; Henschen-Edman, A.; Aswad, D.W.; Stallcup, M.R.; Laird-Offringa, I.A. Lipopolysaccharide-induced methylation of HuR, an mRNA-stabilizing protein, by CARM1. Coactivator-associated arginine methyltransferase. J. Biol. Chem. 2002, 277, 44623–44630. [Google Scholar] [CrossRef]
- Vázquez-Chantada, M.; Fernández-Ramos, D.; Embade, N.; Martínez-Lopez, N.; Varela-Rey, M.; Woodhoo, A.; Luka, Z.; Wagner, C.; Anglim, P.P.; Finnell, R.H.; et al. HuR/methyl-HuR and AUF1 regulate the MAT expressed during liver proliferation, differentiation, and carcinogenesis. Gastroenterology 2010, 138, 1943–1953. [Google Scholar] [CrossRef]
- Kim, H.H.; Abdelmohsen, K.; Lal, A.; Pullmann, R.; Yang, X.; Galban, S.; Srikantan, S.; Martindale, J.L.; Blethrow, J.; Shokat, K.M.; et al. Nuclear HuR accumulation through phosphorylation by Cdk1. Minerva Anestesiol. 2008, 22, 1804–1815. [Google Scholar] [CrossRef]
- Doller, A.; Schlepckow, K.; Schwalbe, H.; Pfeilschifter, J.; Eberhardt, W. Tandem phosphorylation of serines 221 and 318 by protein kinase Cdelta coordinates mRNA binding and nucleocytoplasmic shuttling of HuR. Mol. Cell. Biol. 2010, 30, 1397–1410. [Google Scholar] [CrossRef]
- Latorre, E.; Castiglioni, I.; Gatto, P.; Carelli, S.; Quattrone, A.; Provenzani, A. Loss of Protein Kinase Cδ/HuR Interaction Is Necessary to Doxorubicin Resistance in Breast Cancer Cell Lines. Experiment 2014, 349, 99–106. [Google Scholar] [CrossRef]
- Sorosky, J.I. Endometrial cancer. Obstet. Gynecol. 2008, 111 Pt 1, 436–447. [Google Scholar] [CrossRef] [PubMed]
- Heinonen, M.; Fagerholm, R.; Aaltonen, K.; Kilpivaara, O.; Aittomäki, K.; Blomqvist, C.; Heikkilä, P.; Haglund, C.; Nevanlinna, H.; Ristimäki, A. Prognostic Role of HuR in Hereditary Breast Cancer. Clin. Cancer Res. 2007, 13, 6959–6963. [Google Scholar] [CrossRef]
- Agopiantz, M.; Forgez, P.; Casse, J.-M.; Lacomme, S.; Charra-Brunaud, C.; Clerc-Urmès, I.; Morel, O.; Bonnet, C.; Guéant, J.-L.; Vignaud, J.-M.; et al. Expression of neurotensin receptor 1 in endometrial adenocarcinoma is correlated with histological grade and clinical outcome. Virchows Arch. 2017, 471, 521–530. [Google Scholar] [CrossRef]
- Ozalp, S.; Yalcin, O.T.; Tanir, H.M.; Kabukcuoglu, S.; Erol, G. p53 overexpression as a prognostic indicator in endometrial carcinoma. Eur. J. Gynaecol. Oncol. 2003, 24, 275–278. [Google Scholar]
- Nelson, G.S.; Pink, A.; Lee, S.; Han, G.; Morris, D.; Ogilvie, T.; Duggan, M.A.; Köbel, M. MMR deficiency is common in high-grade endometrioid carcinomas and is associated with an unfavorable outcome. Gynecol. Oncol. 2013, 131, 309–314. [Google Scholar] [CrossRef]
- Majumder, M.; Chakraborty, P.; Mohan, S.; Mehrotra, S.; Palanisamy, V. HuR as a molecular target for cancer therapeutics and immune-related disorders. Adv. Drug Deliv. Rev. 2022, 188, 114442. [Google Scholar] [CrossRef]
- D’agostino, V.G.; Adami, V.; Provenzani, A. A novel high throughput biochemical assay to evaluate the HuR protein-RNA complex formation. PLoS ONE 2013, 8, e72426. [Google Scholar] [CrossRef]
- Pryzbylkowski, P.; Obajimi, O.; Keen, J.C. Trichostatin A and 5 Aza-2′ deoxycytidine decrease estrogen receptor mRNA stability in ER positive MCF7 cells through modulation of HuR. Breast Cancer Res. Treat. 2008, 111, 15–25. [Google Scholar] [CrossRef]
- Doller, A.; Badawi, A.; Schmid, T.; Brauß, T.; Pleli, T.; zu Heringdorf, D.M.; Piiper, A.; Pfeilschifter, J.; Eberhardt, W. The cytoskeletal inhibitors latrunculin A and blebbistatin exert antitumorigenic properties in human hepatocellular carcinoma cells by interfering with intracellular HuR trafficking. Exp. Cell Res. 2015, 330, 66–80. [Google Scholar] [CrossRef]
- Fialcowitz-White, E.J.; Brewer, B.Y.; Ballin, J.D.; Willis, C.D.; Toth, E.A.; Wilson, G.M. Specific protein domains mediate cooperative assembly of HuR oligomers on AU-rich mRNA-destabilizing sequences. J. Biol. Chem. 2007, 282, 20948–20959. [Google Scholar] [CrossRef]
- Höhn, A.K.; Brambs, C.E.; Hiller, G.G.R.; May, D.; Schmoeckel, E.; Horn, L.-C. 2020 WHO Classification of Female Genital Tumors. Obstet. Gynecol. 2021, 81, 1145–1153. [Google Scholar] [CrossRef]

| PFS | OS | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | LOG RANK | Cox Univariate Analyses | Log Rank | Cox Univariate Analyses | ||||
| p-Value | HR | 95% CI | p-Value | p-Value | HR | 95% CI | p-Value | |
| WHO grade | 0.5 | 1.767 | 0.658–4.742 | 0.26 | 0.1 | 2.548 | 1.047–6.204 | 0.039 * |
| HuR expression | ||||||||
| Nuclear | 0.187 | 0.356 | 0.072–1.168 | 0.207 | 0.763 | 1.21 | 0.35–4.187 | 0.763 |
| Cytoplasmic | 0.7 | 0.775 | 0193–3.109 | 0.72 | 0.021 * | 4 | 1.1–14.2 | 0.033 * |
| m-HuR expression | ||||||||
| Nuclear | 0.8 | 1.147 | 0.287–4.589 | 0.846 | 0.9 | 1.095 | 0.317-3.783 | 0.886 |
| Cytoplasmic | 0.03 * | 0.991 | 0.984–0.998 | 0.007 * | 0.003 * | 0.989 | 0.983–0.996 | 0.001 * |
| p-HuR expression | ||||||||
| Nuclear | 0.208 | 0.372 | 0.075–1.845 | 0.226 | 0.06 | 0.257 | 0.054–1.219 | 0.087 |
| Cytoplasmic | 0.741 | 1.269 | 0.317–5.082 | 0.736 | 0.7 | 1.232 | 0.356–4.265 | 0.742 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hotton, J.; Gauchotte, G.; Mougel, R.; Migliorini, M.; Lacomme, S.; Battaglia-Hsu, S.-F.; Agopiantz, M. Expressions of HuR, Methyl-HuR and Phospho-HuR in Endometrial Endometrioid Adenocarcinoma Are Associated with Clinical Features. Int. J. Mol. Sci. 2024, 25, 954. https://doi.org/10.3390/ijms25020954
Hotton J, Gauchotte G, Mougel R, Migliorini M, Lacomme S, Battaglia-Hsu S-F, Agopiantz M. Expressions of HuR, Methyl-HuR and Phospho-HuR in Endometrial Endometrioid Adenocarcinoma Are Associated with Clinical Features. International Journal of Molecular Sciences. 2024; 25(2):954. https://doi.org/10.3390/ijms25020954
Chicago/Turabian StyleHotton, Judicaël, Guillaume Gauchotte, Romane Mougel, Mégane Migliorini, Stéphanie Lacomme, Shyue-Fang Battaglia-Hsu, and Mikaël Agopiantz. 2024. "Expressions of HuR, Methyl-HuR and Phospho-HuR in Endometrial Endometrioid Adenocarcinoma Are Associated with Clinical Features" International Journal of Molecular Sciences 25, no. 2: 954. https://doi.org/10.3390/ijms25020954
APA StyleHotton, J., Gauchotte, G., Mougel, R., Migliorini, M., Lacomme, S., Battaglia-Hsu, S.-F., & Agopiantz, M. (2024). Expressions of HuR, Methyl-HuR and Phospho-HuR in Endometrial Endometrioid Adenocarcinoma Are Associated with Clinical Features. International Journal of Molecular Sciences, 25(2), 954. https://doi.org/10.3390/ijms25020954





