Serum Lipocalin-2 Levels as a Biomarker in Pre- and Post-Pubertal Klinefelter Syndrome Patients: A Pilot Study
Abstract
1. Introduction
2. Results
2.1. Lipocalin-2 Serum Levels
2.2. Metabolic Assessments
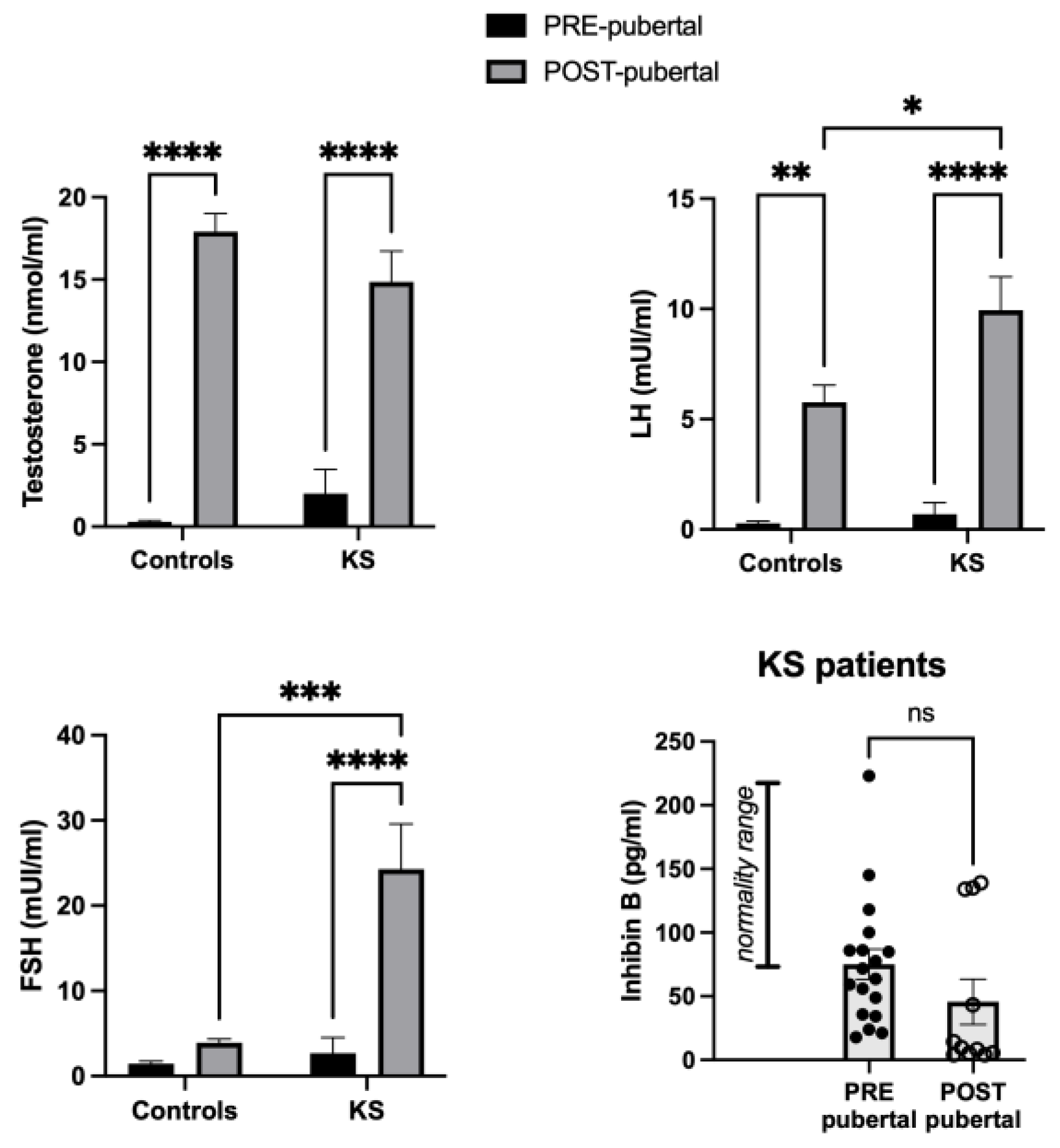
2.2.1. Sex Hormone Profile
2.2.2. Lipid Profile
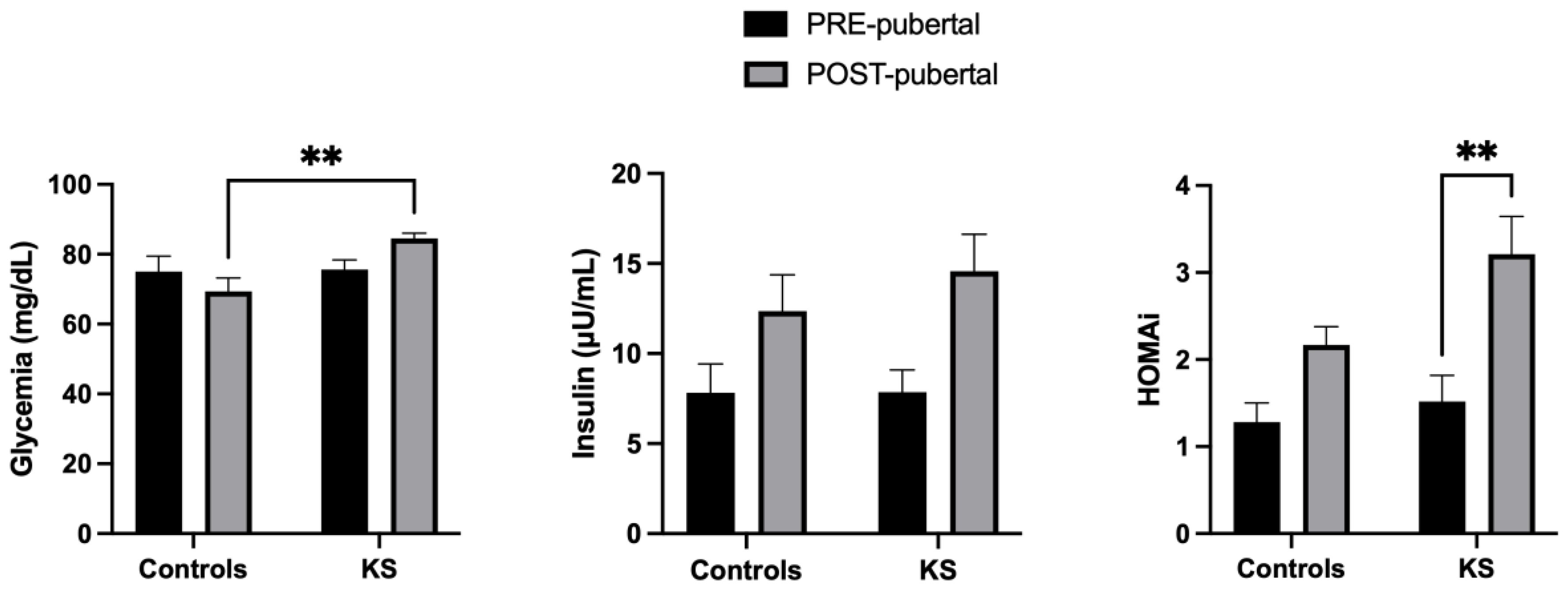
2.2.3. Glucose Profile
2.3. Spearman Correlation LCN-2 vs. Clinical/Metabolic Parameters
3. Discussion
4. Materials and Methods
4.1. Patients Enrollment
4.2. Serum Lipocalin-2 (LCN-2) Analysis
4.3. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lanfranco, F.; Kamischke, A.; Zitzmann, M.; Nieschlag, E. Klinefelter’s Syndrome. Lancet 2004, 364, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.M.; Ross, J.L. Klinefelter Syndrome. In Encyclopedia of Endocrine Diseases; Academic Press: Cambridge, MA, USA, 2018; pp. 561–567. ISBN 9780128122006. [Google Scholar]
- Spaziani, M.; Mileno, B.; Rossi, F.; Granato, S.; Tahani, N.; Anzuini, A.; Lenzi, A.; Radicioni, A.F. Endocrine and Metabolic Evaluation of Classic Klinefelter Syndrome and High-Grade Aneuploidies of Sexual Chromosomes with Male Phenotype: Are They Different Clinical Conditions? Eur. J. Endocrinol. 2018, 178, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Wikström, A.M.; Raivio, T.; Hadziselimovic, F.; Wikström, S.; Tuuri, T.; Dunkel, L. Klinefelter Syndrome in Adolescence: Onset of Puberty Is Associated with Accelerated Germ Cell Depletion. J. Clin. Endocrinol. Metab. 2004, 89, 2263–2270. [Google Scholar] [CrossRef] [PubMed]
- De Sanctis, V.; Ciccone, S. Fertility Preservation in Adolescents with Klinefelter’s Syndrome. Pediatr. Endocrinol. Rev. 2010, 8 (Suppl. 1), 178–181. [Google Scholar] [PubMed]
- Davis, S.M.; DeKlotz, S.; Nadeau, K.J.; Kelsey, M.M.; Zeitler, P.S.; Tartaglia, N.R. High Prevalence of Cardiometabolic Risk Features in Adolescents with 47,XXY/Klinefelter Syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2020, 184, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Kanakis, G.A.; Nieschlag, E. Klinefelter Syndrome: More than Hypogonadism. Metabolism 2018, 86, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Spaziani, M.; Radicioni, A.F. Metabolic and Cardiovascular Risk Factors in Klinefelter Syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2020, 184, 334–343. [Google Scholar] [CrossRef]
- Bardsley, M.Z.; Falkner, B.; Kowal, K.; Ross, J.L. Insulin Resistance and Metabolic Syndrome in Prepubertal Boys with Klinefelter Syndrome. Acta Paediatr. 2011, 100, 866–870. [Google Scholar] [CrossRef]
- Bao, G.; Clifton, M.; Hoette, T.M.; Mori, K.; Deng, S.-X.; Qiu, A.; Viltard, M.; Williams, D.; Paragas, N.; Leete, T.; et al. Iron Traffics in Circulation Bound to a Siderocalin (Ngal)—Catechol Complex. Nat. Chem. Biol. 2010, 6, 602–609. [Google Scholar] [CrossRef]
- Romejko, K.; Markowska, M.; Niemczyk, S. The Review of Current Knowledge on Neutrophil Gelatinase-Associated Lipocalin (NGAL). Int. J. Mol. Sci. 2023, 24, 10470. [Google Scholar] [CrossRef]
- Al Jaberi, S.; Cohen, A.; D’Souza, C.; Abdulrazzaq, Y.M.; Ojha, S.; Bastaki, S.; Adeghate, E.A. Lipocalin-2: Structure, Function, Distribution and Role in Metabolic Disorders. Biomed. Pharmacother. 2021, 142, 112002. [Google Scholar] [CrossRef]
- Jang, Y.; Lee, J.H.; Wang, Y.; Sweeney, G. Emerging Clinical and Experimental Evidence for the Role of Lipocalin-2 in Metabolic Syndrome. Clin. Exp. Pharmacol. Physiol. 2012, 39, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Lam, K.S.L.; Kraegen, E.W.; Sweeney, G.; Zhang, J.; Tso, A.W.K.; Chow, W.S.; Wat, N.M.S.; Xu, J.Y.; Hoo, R.L.C.; et al. Lipocalin-2 Is an Inflammatory Marker Closely Associated with Obesity, Insulin Resistance, and Hyperglycemia in Humans. Clin. Chem. 2007, 53, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Vijay-Kumar, M.; Gentsch, J.R.; Kaiser, W.J.; Borregaard, N.; Offermann, M.K.; Neish, A.S.; Gewirtz, A.T. Protein Kinase R Mediates Intestinal Epithelial Gene Remodeling in Response to Double-Stranded RNA and Live Rotavirus. J. Immunol. 2005, 174, 6322–6331. [Google Scholar] [CrossRef] [PubMed]
- Çelik, T.; Altekin, E.; Işgüder, R.; Kenesari, Y.; Duman, M.; Arslan, N. Evaluation of Neutrophil Gelatinase-Associated Lipocalin in Pediatric Patients with Acute Rotavirus Gastroenteritis and Dehydration. Ital. J. Pediatr. 2013, 39, 52. [Google Scholar] [CrossRef]
- Buonafine, M.; Martinez-Martinez, E.; Jaisser, F. More than a Simple Biomarker: The Role of NGAL in Cardiovascular and Renal Diseases. Clin. Sci. 2018, 132, 909–923. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.H.; Wang, X.; Li, S.; Liu, Y.; Akbar, R.; Fan, G.C. Lipocalin Family Proteins and Their Diverse Roles in Cardiovascular Disease. Pharmacol. Ther. 2023, 244, 108385. [Google Scholar] [CrossRef]
- Finocchi, F.; Pelloni, M.; Balercia, G.; Pallotti, F.; Radicioni, A.F.; Lenzi, A.; Lombardo, F.; Paoli, D. Seminal Plasma MiRNAs in Klinefelter Syndrome and in Obstructive and Non-Obstructive Azoospermia. Mol. Biol. Rep. 2020, 47, 4373–4382. [Google Scholar] [CrossRef]
- Fiore, M.; Tarani, L.; Radicioni, A.; Spaziani, M.; Ferraguti, G.; Putotto, C.; Gabanella, F.; Maftei, D.; Lattanzi, R.; Minni, A.; et al. Serum Prokineticin-2 in Prepubertal and Adult Klinefelter Individuals. Can. J. Physiol. Pharmacol. 2022, 100, 151–157. [Google Scholar] [CrossRef]
- He, H.; Huang, T.; Yu, F.; Chen, K.; Guo, S.; Zhang, L.; Tang, X.; Yuan, X.; Liu, J.; Zhou, Y. KIF2C Affects Sperm Cell Differentiation in Patients with Klinefelter Syndrome, as Revealed by RNA-Seq and scRNA-Seq Data. FEBS Open Bio 2022, 12, 1465–1474. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, Z.; Gao, Y.; Lin, H.; Zhu, Z.; Zheng, H.; Ye, W.; Luo, Z.; Qing, Z.; Xiao, X.; et al. Leydig Cell Metabolic Disorder Act as a New Mechanism Affecting for Focal Spermatogenesis in Klinefelter Syndrome Patients: A Real World Cross-Sectional Study Base on the Age. Front. Endocrinol. 2023, 14, 1266730. [Google Scholar] [CrossRef]
- Fujino, R.S.; Tanaka, K.; Morimatsu, M.; Tamura, K.; Kogo, H.; Hara, T. Spermatogonial Cell-Mediated Activation of an IκBζ-Independent Nuclear Factor-ΚB Pathway in Sertoli Cells Induces Transcription of the Lipocalin-2 Gene. Mol. Endocrinol. 2006, 20, 904–915. [Google Scholar] [CrossRef][Green Version]
- Tanaka, K.; Tamura, H.; Tanaka, H.; Katoh, M.; Futamata, Y.; Seki, N.; Nishimune, Y.; Hara, T. Spermatogonia-Dependent Expression of Testicular Genes in Mice. Dev. Biol. 2002, 246, 466–479. [Google Scholar] [CrossRef]
- Lee, Y.-C.; Liao, C.-J.; Li, P.-T.; Tzeng, W.-F.; Chu, S.-T. Mouse Lipocalin as an Enhancer of Spermatozoa Motility. Mol. Biol. Rep. 2003, 30, 165–172. [Google Scholar] [CrossRef]
- Elangovan, N.; Lee, Y.-C.; Tzeng, W.-F.; Chu, S.-T. Delivery of Ferric Ion to Mouse Spermatozoa Is Mediated by Lipocalin Internalization. Biochem. Biophys. Res. Commun. 2004, 319, 1096–1104. [Google Scholar] [CrossRef] [PubMed]
- Chu, S.T.; Lee, Y.C.; Nein, K.M.; Chen, Y.H. Expression, Immunolocalization and Sperm-Association of a Protein Derived from 24p3 Gene in Mouse Epididymis. Mol. Reprod. Dev. 2000, 57, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Nenkova, G.; Petrov, L.; Alexandrova, A. Role of Trace Elements for Oxidative Status and Quality of Human Sperm. Balk. Med. J. 2017, 34, 343–348. [Google Scholar] [CrossRef]
- Kang, Z.; Qiao, N.; Tan, Z.; Tang, Z.; Li, Y. Expression Patterns and Changes of the LCN2 Gene in the Testes of Induced Cryptorchidism and Busulfan-Treated Mice. Syst. Biol. Reprod. Med. 2017, 63, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Kehrer, J.P. Lipocalin-2: Pro- or Anti-Apoptotic? Cell Biol. Toxicol. 2010, 26, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Renault, L.; Labrune, E.; d’Estaing, S.G.; Cuzin, B.; Lapoirie, M.; Benchaib, M.; Lornage, J.; Soignon, G.; de Souza, A.; Dijoud, F.; et al. Delaying Testicular Sperm Extraction in 47,XXY Klinefelter Patients Does Not Impair the Sperm Retrieval Rate, and AMH Levels Are Higher When TESE Is Positive. Hum. Reprod. 2022, 37, 2518–2531. [Google Scholar] [CrossRef] [PubMed]
- Meyers, K.; López, M.; Ho, J.; Wills, S.; Rayalam, S.; Taval, S. Lipocalin-2 Deficiency May Predispose to the Progression of Spontaneous Age-Related Adiposity in Mice. Sci. Rep. 2020, 10, 14589. [Google Scholar] [CrossRef] [PubMed]
- Bojesen, A.; Kristensen, K.; Birkebaek, N.H.; Fedder, J.; Mosekilde, L.; Bennett, P.; Laurberg, P.; Frystyk, J.; Flyvbjerg, A.; Christiansen, J.S.; et al. The metabolic syndrome is frequent in Klinefelter’s syndrome and is associated with abdominal obesity and hypogonadism. Diabetes Care 2006, 29, 1591–1598. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, T.; Yamaguchi, K.; Kondo, Y.; Takenaka, A.; Fujisawa, M. Metabolic syndrome in men with Klinefelter’s syndrome. Urology 2008, 71, 1109–1113. [Google Scholar] [CrossRef] [PubMed]
- Sacks, D.; Baxter, B.; Campbell, B.C.V.; Carpenter, J.S.; Cognard, C.; Dippel, D.; Eesa, M.; Fischer, U.; Hausegger, K.; Hirsch, J.A.; et al. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int. J. Stroke 2018, 13, 612–632. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.; Lahlou, N.; Bardsley, M.; Temple, M.C.; Kowal, K.; Pyle, L.; Zeitler, P.; Ross, J. Gonadal function is associated with cardiometabolic health in pre-pubertal boys with Klinefelter syndrome. Andrology 2016, 4, 1169–1177. [Google Scholar] [CrossRef]
- Davis, S.M.; Cox-Martin, M.G.; Bardsley, M.Z.; Kowal, K.; Zeitler, P.S.; Ross, J.L. Effects of Oxandrolone on Cardiometabolic Health in Boys with Klinefelter Syndrome: A Randomized Controlled Trial. J. Clin. Endocrinol. Metab. 2017, 102, 176–184. [Google Scholar] [CrossRef]
- Sesti, F.; Pofi, R.; Pozza, C.; Minnetti, M.; Gianfrilli, D.; Kanakis, G.A. Cardiovascular Complications in Patients with Klinefelter’s Syndrome. Curr. Pharm. Des. 2020, 26, 5556–5563. [Google Scholar] [CrossRef]
- Shields-Cutler, R.R.; Crowley, J.R.; Miller, C.D.; Stapleton, A.E.; Cui, W.; Henderson, J.P. Human Metabolome-derived Cofactors Are Required for the Antibacterial Activity of Siderocalin in Urine. J. Biol. Chem. 2016, 291, 25901–25910. [Google Scholar] [CrossRef]
- Markle, J.G.; Fish, E.N. SeXX matters in immunity. Trends Immunol. 2014, 35, 97–104. [Google Scholar] [CrossRef]
- Panimolle, F.; Tiberti, C.; Spaziani, M.; Riitano, G.; Lucania, G.; Anzuini, A.; Lenzi, A.; Gianfrilli, D.; Sorice, M.; Radicioni, A.F. Non-organ-specific autoimmunity in adult 47,XXY Klinefelter patients and higher-grade X-chromosome aneuploidies. Clin. Exp. Immunol. 2021, 205, 316–325. [Google Scholar] [CrossRef]
- Sarrate, Z.; Vidal, F.; Blanco, J. Role of Sperm Fluorescent in situ Hybridization Studies in Infertile Patients: Indications, Study Approach, and Clinical Relevance. Fertil. Steril. 2010, 93, 1892–1902. [Google Scholar] [CrossRef] [PubMed]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Ostrowski, S.; Dobrowolski, J.C. What Does the HOMA Index Really Measure? RSC Adv. 2014, 4, 44158–44161. [Google Scholar] [CrossRef]


| Subjects | Variable | Correlation Coefficient (rho) | p Value | |
|---|---|---|---|---|
| Healthy Controls | Pre-pubertal | HDL (mg/dL) | −0.854 | 0.003 * |
| KS individuals | 0.223 | 0.423 | ||
| Healthy Controls | LH (mUI/mL) | −0.73 | 0.025 * | |
| KS individuals | 0.014 | 0.959 | ||
| KS individuals | All individuals | Inhibin B (pg/mL) | 0.405 | 0.045 * |
| Pre-pubertal | 0.521 | 0.059 | ||
| Post-pubertal | 0.26 | 0.441 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paparella, R.; Ferraguti, G.; Fiore, M.; Menghi, M.; Micangeli, G.; Tarani, F.; Ligotino, A.; Messina, M.P.; Ceccanti, M.; Minni, A.; et al. Serum Lipocalin-2 Levels as a Biomarker in Pre- and Post-Pubertal Klinefelter Syndrome Patients: A Pilot Study. Int. J. Mol. Sci. 2024, 25, 2214. https://doi.org/10.3390/ijms25042214
Paparella R, Ferraguti G, Fiore M, Menghi M, Micangeli G, Tarani F, Ligotino A, Messina MP, Ceccanti M, Minni A, et al. Serum Lipocalin-2 Levels as a Biomarker in Pre- and Post-Pubertal Klinefelter Syndrome Patients: A Pilot Study. International Journal of Molecular Sciences. 2024; 25(4):2214. https://doi.org/10.3390/ijms25042214
Chicago/Turabian StylePaparella, Roberto, Giampiero Ferraguti, Marco Fiore, Michela Menghi, Ginevra Micangeli, Francesca Tarani, Aurora Ligotino, Marisa Patrizia Messina, Mauro Ceccanti, Antonio Minni, and et al. 2024. "Serum Lipocalin-2 Levels as a Biomarker in Pre- and Post-Pubertal Klinefelter Syndrome Patients: A Pilot Study" International Journal of Molecular Sciences 25, no. 4: 2214. https://doi.org/10.3390/ijms25042214
APA StylePaparella, R., Ferraguti, G., Fiore, M., Menghi, M., Micangeli, G., Tarani, F., Ligotino, A., Messina, M. P., Ceccanti, M., Minni, A., Barbato, C., Lucarelli, M., Tarani, L., & Petrella, C. (2024). Serum Lipocalin-2 Levels as a Biomarker in Pre- and Post-Pubertal Klinefelter Syndrome Patients: A Pilot Study. International Journal of Molecular Sciences, 25(4), 2214. https://doi.org/10.3390/ijms25042214










