Exploration of the Delivery of Oncolytic Newcastle Disease Virus by Gelatin Methacryloyl Microneedles
Abstract
1. Introduction
2. Results
2.1. NMR-H1 Spectra of GelMA and Gelatin
2.2. GelMA Swelling Rate and Degradation Rate Curve
2.3. NDV Transmission Electron Microscope
2.4. NDV Particle Size and Zeta Potential
2.5. TCID50 Immunofluorescence Assay of NDV
2.6. CCK-8 Detection of NDV Killing HepG2 and L02
2.7. SEM Images of GelMA Microneedles with Different Contents and GelMA Microneedles Encapsulating NDV
2.8. Stress–Strain Curves of GelMA Microneedles with Different Contents
2.9. Agarose and Mouse Skin Puncture Test
2.10. Immunofluorescence of NDV and NDV-Loaded GelMA Microneedles
2.11. Hemagglutination Titers of NDV and NDV-Loaded Microneedles
3. Discussion
3.1. NMR-H1 Spectra of GelMA and Gelatin
3.2. GelMA Swelling Rate and Degradation Rate Curve
3.3. NDV Transmission Electron Microscope and Particle Size and Zeta Potential
3.4. TCID50 Immunofluorescence Assay of NDV
3.5. CCK-8 Detection of NDV Killing HepG2 and L02
3.6. SEM Images of GelMA Microneedles with Different Contents and GelMA Microneedles Encapsulating NDV
3.7. Stress–Strain Curves of GelMA Microneedles with Different Contents
3.8. Agarose and Mouse Skin Puncture Test
3.9. Immunofluorescence of NDV and NDV-Loaded GelMA Microneedles
3.10. Hemagglutination Titers of NDV and NDV-Loaded Microneedles
4. Materials and Methods
4.1. Reagents, Viruses, Cell Lines, and Animals
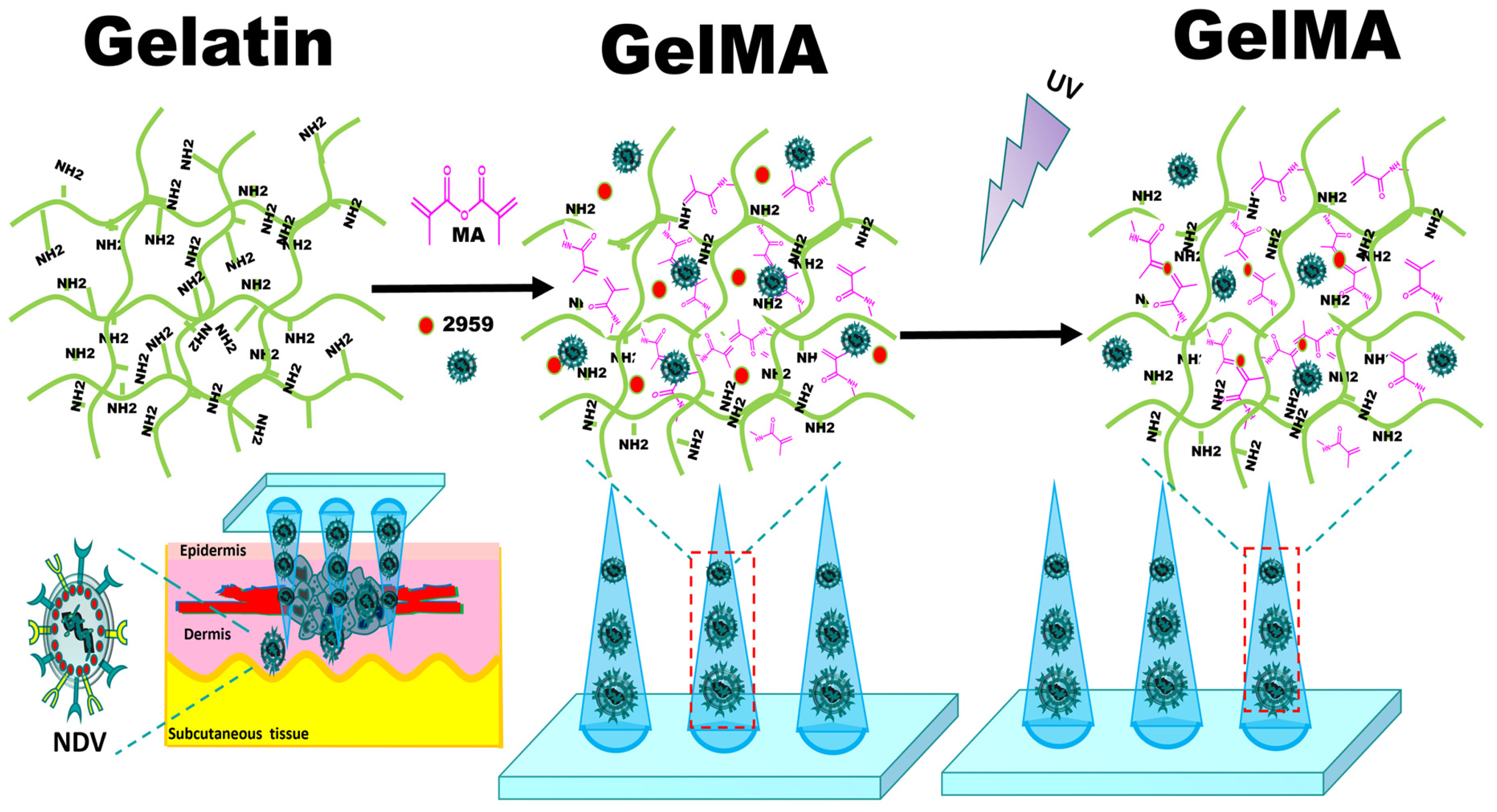
4.2. Synthesis of GelMA
4.3. NMR Detection of GelMA
4.4. Determination of the Swelling Rate and Degradation Rate of GelMA
4.5. Morphology Observation of NDV
4.6. Determination of NDV Particle Size and Zeta Potential
4.7. TCID50 Determination of NDV
4.8. Cell Viability Assay of NDV
4.9. Preparation of GelMA Microneedles with Different Contents and Preparation of GelMA Microneedles Encapsulating NDV
4.10. SEM Images of GelMA Microneedles with Different Contents and GelMA Microneedles Encapsulating NDV
4.11. Stress–Strain Curves of GelMA Microneedles with Different Contents
4.12. Agarose Gel Puncture Experiment of GelMA Microneedles
4.13. Mouse Skin Puncture Experiment of GelMA Microneedles
4.14. NDV Release was Detected by Immunofluorescence
4.15. Hemagglutination Test of Different Sample Solutions
4.16. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Kaufman, H.L.; Kohlhapp, F.J.; Zloza, A. Oncolytic viruses: A new class of immunotherapy drugs. Nat. Rev. Drug Discov. 2015, 14, 642–662. [Google Scholar] [CrossRef] [PubMed]
- Zamarin, D.; Holmgaard, R.B.; Ricca, J.; Plitt, T.; Palese, P.; Sharma, P.; Merghoub, T.; Wolchok, J.D.; Allison, J.P. Intratumoral modulation of the inducible co-stimulator icos by recombinant oncolytic virus promotes systemic anti-tumour immunity. Nat. Commun. 2017, 8, 14340. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.M.; McFadden, G. Oncolytic viruses: Newest frontier for cancer immunotherapy. Cancers 2021, 13, 5452. [Google Scholar] [CrossRef]
- Burman, B.; Pesci, G.; Zamarin, D. Newcastle disease virus at the forefront of cancer immunotherapy. Cancers 2020, 12, 3552. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.; Huang, Y.; Huang, Y.; Yang, Y.; Zhao, Y.; Martyniuk, C.J. Toxicity assessment of the herbicide acetochlor in the human liver carcinoma (hepg2) cell line. Chemosphere 2020, 243, 125345. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Huang, L.; Zhao, Y.; Hu, T. Musk xylene induces malignant transformation of human liver cell line l02 via repressing the tgf-beta signaling pathway. Chemosphere 2017, 168, 1506–1514. [Google Scholar] [CrossRef] [PubMed]
- Kwong, S.P.; Huang, Z.; Ji, L.; Wang, C. Porimin: The key to (+)-usnic acid-induced liver toxicity and oncotic cell death in normal human l02 liver cells. J. Ethnopharmacol. 2021, 270, 113873. [Google Scholar] [CrossRef] [PubMed]
- Ren, G.; Tian, G.; Liu, Y.; He, J.; Gao, X.; Yu, Y.; Liu, X.; Zhang, X.; Sun, T.; Liu, S.; et al. Recombinant Newcastle disease virus encoding il-12 and/or il-2 as potential candidate for hepatoma carcinoma therapy. Technol. Cancer Res. Treat. 2016, 15, NP83–NP94. [Google Scholar] [CrossRef] [PubMed]
- Chu, Z.; Yang, S.; Li, Q.; Shang, J.; Ren, Z.; Ren, F. The v protein in oncolytic Newcastle disease virus promotes hepg2 hepatoma cell proliferation at the single-cell level. BMC Cancer 2023, 23, 346. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Zhang, Q.; Xu, D.; Li, Y.; Fan, Y.; Li, W.; Yin, X.; Zhang, Y.; Liu, J.; Li, X.; et al. Antitumor effect of the Newcastle disease viral hemagglutinin-neuraminidase gene is expressed through an oncolytic adenovirus effect in osteosarcoma cells. Anticancer. Drugs 2018, 29, 197–207. [Google Scholar] [CrossRef] [PubMed]
- He, D.; Sun, L.; Li, C.; Hu, N.; Sheng, Y.; Chen, Z.; Li, X.; Chi, B.; Jin, N. Anti-tumor effects of an oncolytic adenovirus expressing hemagglutinin-neuraminidase of Newcastle disease virus in vitro and in vivo. Viruses 2014, 6, 856–874. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Lin, Y.; Li, K.; Liang, J.; Xiao, X.; Cai, J.; Tan, Y.; Xing, F.; Mai, J.; Li, Y.; et al. Naturally existing oncolytic virus m1 is nonpathogenic for the nonhuman primates after multiple rounds of repeated intravenous injections. Hum. Gene Ther. 2016, 27, 700–711. [Google Scholar] [CrossRef] [PubMed]
- Andón, F.T.; Leon, S.; Ummarino, A.; Redin, E.; Allavena, P.; Serrano, D.; Anfray, C.; Calvo, A. Innate and adaptive responses of intratumoral immunotherapy with endosomal toll-like receptor agonists. Biomedicines 2022, 10, 1590. [Google Scholar] [CrossRef] [PubMed]
- Nakao, S.; Arai, Y.; Tasaki, M.; Yamashita, M.; Murakami, R.; Kawase, T.; Amino, N.; Nakatake, M.; Kurosaki, H.; Mori, M.; et al. Intratumoral expression of il-7 and il-12 using an oncolytic virus increases systemic sensitivity to immune checkpoint blockade. Sci. Transl. Med. 2020, 12, eaax7992. [Google Scholar] [CrossRef] [PubMed]
- Mozaffari Nejad, A.S.; Fotouhi, F.; Mehrbod, P.; Alikhani, M.Y. Antitumor immunity enhancement through ewcastle viral oncolysate in mice model: A promising method to treat tumors. Saudi J. Biol. Sci. 2021, 28, 5833–5840. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.; Carlisle, R. Achieving systemic delivery of oncolytic viruses. Expert. Opin. Drug Deliv. 2019, 16, 607–620. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, A.B.; Carpenter, A.M.; Aiken, R.; Hanft, S. Oncolytic virus in gliomas: A review of human clinical investigations. Ann. Oncol. 2021, 32, 968–982. [Google Scholar] [CrossRef]
- Lv, P.; Chen, H.; Cheng, H.; Liu, X.; Liu, C.; Zeng, Y.; Jiang, L.; Wang, X.; Mao, J.; Liu, G. A calcium alginate hydrogel microsphere-based transcatheter arterial viroembolization strategy for hepatocellular carcinoma. Adv. Ther. 2023, 6, 2200174. [Google Scholar] [CrossRef]
- Erfani, A.; Diaz, A.E.; Doyle, P.S. Hydrogel-enabled, local administration and combinatorial delivery of immunotherapies for cancer treatment. Mater. Today 2023, 65, 227–243. [Google Scholar] [CrossRef]
- Hao, H.; Wu, S.; Lin, J.; Zheng, Z.; Zhou, Y.; Zhang, Y.; Guo, Q.; Tian, F.; Zhao, M.; Chen, Y.; et al. Immunization against zika by entrapping live virus in a subcutaneous self-adjuvanting hydrogel. Nat. Biomed. Eng. 2023, 7, 928–942. [Google Scholar] [CrossRef]
- Li, J.; Mooney, D.J. Designing hydrogels for controlled drug delivery. Nat. Rev. Mater. 2016, 1, 16071. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, Y.; Chi, J.; Zhao, Y. Smart microneedles for therapy and diagnosis. Research 2020, 2020, 7462915. [Google Scholar] [CrossRef] [PubMed]
- Vrdoljak, A.; McGrath, M.G.; Carey, J.B.; Draper, S.J.; Hill, A.V.; O’Mahony, C.; Crean, A.M.; Moore, A.C. Coated microneedle arrays for transcutaneous delivery of live virus vaccines. J. Control Release 2012, 159, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Li, H.; Bian, Y.; Wang, Z.; Chen, G.; Zhang, X.; Miao, Y.; Wen, D.; Wang, J.; Wan, G.; et al. Bioorthogonal catalytic patch. Nat. Nanotechnol. 2021, 16, 933–941. [Google Scholar] [CrossRef]
- Li, H.; Wang, Z.; Ogunnaike, E.A.; Wu, Q.; Chen, G.; Hu, Q.; Ci, T.; Chen, Z.; Wang, J.; Wen, D.; et al. Scattered seeding of car t cells in solid tumors augments anticancer efficacy. Natl. Sci. Rev. 2022, 9, nwab172. [Google Scholar] [CrossRef] [PubMed]
- Duong, H.T.T.; Yin, Y.; Le, T.M.D.; Jeong, J.H.; Lee, D.S. Highly prolonged release of the cancer vaccine and immunomodulator via a two-layer biodegradable microneedle for prophylactic treatment of metastatic cancer. Biomacromolecules 2023, 24, 1209–1219. [Google Scholar] [CrossRef]
- Song, G.; Sun, Y.; Liu, T.; Zhang, X.; Zeng, Z.; Wang, R.; Li, P.; Li, C.; Jiang, G. Transdermal delivery of cu-doped polydopamine using microneedles for photothermal and chemodynamic synergistic therapy against skin melanoma. Chem. Eng. J. 2021, 426, 130790. [Google Scholar] [CrossRef]
- Luo, Z.; Sun, W.; Fang, J.; Lee, K.; Li, S.; Gu, Z.; Dokmeci, M.R.; Khademhosseini, A. Biodegradable gelatin methacryloyl microneedles for transdermal drug delivery. Adv. Healthc. Mater. 2019, 8, e1801054. [Google Scholar] [CrossRef]
- Zhou, X.; Luo, Z.; Baidya, A.; Kim, H.J.; Wang, C.; Jiang, X.; Qu, M.; Zhu, J.; Ren, L.; Vajhadin, F.; et al. Biodegradable beta-cyclodextrin conjugated gelatin methacryloyl microneedle for delivery of water-insoluble drug. Adv. Healthc. Mater. 2020, 9, e2000527. [Google Scholar] [CrossRef]
- Gan, S.; Zheng, Z.; Zhang, M.; Long, L.; Zhang, X.; Tan, B.; Zhu, Z.; Liao, J.; Chen, W. Lyophilized platelet-rich fibrin exudate-loaded carboxymethyl chitosan/gelma hydrogel for efficient bone defect repair. ACS Appl. Mater. Interfaces 2023, 15, 26349–26362. [Google Scholar] [CrossRef] [PubMed]
- Chi, J.; Zhang, X.; Chen, C.; Shao, C.; Zhao, Y.; Wang, Y. Antibacterial and angiogenic chitosan microneedle array patch for promoting wound healing. Bioact. Mater. 2020, 5, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Stinson, J.A.; Raja, W.K.; Lee, S.; Kim, H.B.; Diwan, I.; Tutunjian, S.; Panilaitis, B.; Omenetto, F.G.; Tzipori, S.; Kaplan, D.L. Silk fibroin microneedles for transdermal vaccine delivery. ACS Biomater. Sci. Eng. 2017, 3, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Bejleri, D.; Streeter, B.W.; Nachlas, A.L.Y.; Brown, M.E.; Gaetani, R.; Christman, K.L.; Davis, M.E. A bioprinted cardiac patch composed of cardiac-specific extracellular matrix and progenitor cells for heart repair. Adv. Healthc. Mater. 2018, 7, e1800672. [Google Scholar] [CrossRef] [PubMed]
- Ella, E.; Harel, Y.; Abraham, M.; Wald, H.; Benny, O.; Karsch-Bluman, A.; Vincent, D.; Laurent, D.; Amir, G.; Izhar, U.; et al. Matrix metalloproteinase 12 promotes tumor propagation in the lung. J. Thorac. Cardiovasc. Surg. 2018, 155, 2164–2175.e1. [Google Scholar] [CrossRef] [PubMed]
- Qu, M.; Kim, H.J.; Zhou, X.; Wang, C.; Jiang, X.; Zhu, J.; Xue, Y.; Tebon, P.; Sarabi, S.A.; Ahadian, S.; et al. Biodegradable microneedle patch for transdermal gene delivery. Nanoscale 2020, 12, 16724–16729. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Wang, X.; Wu, D.; Yi, K.; Zhao, Y. Yunnan baiyao-loaded multifunctional microneedle patches for rapid hemostasis and cutaneous wound healing. J. Nanobiotechnol. 2023, 21, 178. [Google Scholar] [CrossRef]
- Sun, Y.; Yang, L.; Du, L.; Zhou, Y.; Xu, K.; Chen, J.; He, Y.; Qu, Q.; Miao, Y.; Xing, M.; et al. Duo-role platelet-rich plasma: Temperature-induced fibrin gel and growth factors’ reservoir for microneedles to promote hair regrowth. J. Adv. Res. 2024, 55, 89–102. [Google Scholar] [CrossRef]
- Zhang, X.; Fu, X.; Chen, G.; Wang, Y.; Zhao, Y. Versatile ice microneedles for transdermal delivery of diverse actives. Adv. Sci. 2021, 8, e2101210. [Google Scholar] [CrossRef]
- Liu, Y.; Long, L.; Zhang, F.; Hu, X.; Zhang, J.; Hu, C.; Wang, Y.; Xu, J. Microneedle-mediated vascular endothelial growth factor delivery promotes angiogenesis and functional recovery after stroke. J. Control Release 2021, 338, 610–622. [Google Scholar] [CrossRef] [PubMed]
- Turvey, M.E.; Uppu, D.; Mohamed Sharif, A.R.; Bidet, K.; Alonso, S.; Ooi, E.E.; Hammond, P.T. Microneedle-based intradermal delivery of stabilized dengue virus. Bioeng. Transl. Med. 2019, 4, e10127. [Google Scholar] [CrossRef] [PubMed]
- Choi, I.J.; Cha, H.R.; Hwang, S.J.; Baek, S.K.; Lee, J.M.; Choi, S.O. Live vaccinia virus-coated microneedle array patches for smallpox vaccination and stockpiling. Pharmaceutics 2021, 13, 209. [Google Scholar] [CrossRef]
- Boone, C.E.; Wang, C.; Lopez-Ramirez, M.A.; Beiss, V.; Shukla, S.; Chariou, P.L.; Kupor, D.; Rueda, R.; Wang, J.; Steinmetz, N.F. Active microneedle administration of plant virus nanoparticles for cancer in situ vaccination improves immunotherapeutic efficacy. ACS Appl. Nano Mater. 2020, 3, 8037–8051. [Google Scholar] [CrossRef] [PubMed]
- Shirahama, H.; Lee, B.H.; Tan, L.P.; Cho, N.J. Precise tuning of facile one-pot gelatin methacryloyl (gelma) synthesis. Sci. Rep. 2016, 6, 31036. [Google Scholar] [CrossRef] [PubMed]
- Nichol, J.W.; Koshy, S.T.; Bae, H.; Hwang, C.M.; Yamanlar, S.; Khademhosseini, A. Cell-laden microengineered gelatin methacrylate hydrogels. Biomaterials 2010, 31, 5536–5544. [Google Scholar] [CrossRef] [PubMed]
- Yue, K.; Trujillo-de Santiago, G.; Alvarez, M.M.; Tamayol, A.; Annabi, N.; Khademhosseini, A. Synthesis, properties, and biomedical applications of gelatin methacryloyl (gelma) hydrogels. Biomaterials 2015, 73, 254–271. [Google Scholar] [CrossRef]
- Bher, A.; Cho, Y.; Auras, R. Boosting degradation of biodegradable polymers. Macromol. Rapid Commun. 2023, 44, e2200769. [Google Scholar] [CrossRef]
- Xin, T.; Mao, J.; Liu, L.; Tang, J.; Wu, L.; Yu, X.; Gu, Y.; Cui, W.; Chen, L. Programmed sustained release of recombinant human bone morphogenetic protein-2 and inorganic ion composite hydrogel as artificial periosteum. ACS Appl. Mater. Interfaces 2020, 12, 6840–6851. [Google Scholar] [CrossRef]
- Song, L.; Chi, J.; Li, Z.; Tao, Y.; Sun, Y.; Zhou, Q.; Lu, S.; Huang, Q.; Huang, S.; Lu, X.; et al. An inflammation-responsive double-layer microneedle patch for recurrent atopic dermatitis therapy. Int. J. Pharm. 2023, 643, 123215. [Google Scholar] [CrossRef]
- Mlynarczyk, G.; Gudowska-Sawczuk, M.; Mroczko, B.; Bruczko-Goralewska, M.; Romanowicz, L.; Tokarzewicz, A. Higher content but no specific activity in gelatinase b (mmp-9) compared with gelatinase a (mmp-2) in human renal carcinoma. Cancers 2023, 15, 5475. [Google Scholar] [CrossRef] [PubMed]
- Haghniaz, R.; Kim, H.J.; Montazerian, H.; Baidya, A.; Tavafoghi, M.; Chen, Y.; Zhu, Y.; Karamikamkar, S.; Sheikhi, A.; Khademhosseini, A. Tissue adhesive hemostatic microneedle arrays for rapid hemorrhage treatment. Bioact. Mater. 2023, 23, 314–327. [Google Scholar] [CrossRef]
- Zhao, Z.Q.; Liang, L.; Hu, L.F.; He, Y.T.; Jing, L.Y.; Liu, Y.; Chen, B.Z.; Guo, X.D. Subcutaneous implantable microneedle system for the treatment of alzheimer’s disease by delivering donepezil. Biomacromolecules 2022, 23, 5330–5339. [Google Scholar] [CrossRef] [PubMed]
- Smither, S.J.; Lear-Rooney, C.; Biggins, J.; Pettitt, J.; Lever, M.S.; Olinger, G.G., Jr. Comparison of the plaque assay and 50% tissue culture infectious dose assay as methods for measuring filovirus infectivity. J. Virol. Methods 2013, 193, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Wulff, N.H.; Tzatzaris, M.; Young, P.J. Monte Carlo simulation of the Spearman-Kaerber TCID50. J. Clin. Bioinf. 2012, 2, 5. [Google Scholar] [CrossRef] [PubMed]
- Malenovska, H. Virus quantitation by transmission electron microscopy, tcid(5)(0), and the role of timing virus harvesting: A case study of three animal viruses. J. Virol. Methods 2013, 191, 136–140. [Google Scholar] [CrossRef]
- Altomonte, J.; Marozin, S.; Schmid, R.M.; Ebert, O. Engineered Newcastle disease virus as an improved oncolytic agent against hepatocellular carcinoma. Mol. Ther. 2010, 18, 275–284. [Google Scholar] [CrossRef]
- He, J.; Pan, Z.; Tian, G.; Liu, X.; Liu, Y.; Guo, X.; An, Y.; Song, L.; Wu, H.; Cao, H.; et al. Newcastle disease virus chimeras expressing the hemagglutinin- neuraminidase protein of mesogenic strain exhibits an enhanced anti-hepatoma efficacy. Virus Res. 2016, 221, 23–29. [Google Scholar] [CrossRef]
- Yao, S.; Wang, Y.; Chi, J.; Yu, Y.; Zhao, Y.; Luo, Y.; Wang, Y. Porous mof microneedle array patch with photothermal responsive nitric oxide delivery for wound healing. Adv. Sci. 2022, 9, e2103449. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ye, Y.; Hochu, G.M.; Sadeghifar, H.; Gu, Z. Enhanced cancer immunotherapy by microneedle patch-assisted delivery of anti-pd1 antibody. Nano Lett. 2016, 16, 2334–2340. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Chen, G.; Liu, Y.; Sun, L.; Sun, L.; Zhao, Y. Black phosphorus-loaded separable microneedles as responsive oxygen delivery carriers for wound healing. ACS Nano 2020, 14, 5901–5908. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Kang, E.; Kwon, O.J.; Yun, T.J.; Park, H.K.; Kim, P.H.; Kim, S.W.; Kim, J.H.; Yun, C.O. Local sustained delivery of oncolytic adenovirus with injectable alginate gel for cancer virotherapy. Gene Ther. 2013, 20, 880–892. [Google Scholar] [CrossRef]
- Le, T.M.D.; Jung, B.K.; Li, Y.; Duong, H.T.T.; Nguyen, T.L.; Hong, J.W.; Yun, C.O.; Lee, D.S. Physically crosslinked injectable hydrogels for long-term delivery of oncolytic adenoviruses for cancer treatment. Biomater. Sci. 2019, 7, 4195–4207. [Google Scholar] [CrossRef] [PubMed]
- Oh, E.; Oh, J.E.; Hong, J.; Chung, Y.; Lee, Y.; Park, K.D.; Kim, S.; Yun, C.O. Optimized biodegradable polymeric reservoir-mediated local and sustained co-delivery of dendritic cells and oncolytic adenovirus co-expressing il-12 and gm-csf for cancer immunotherapy. J. Control Release 2017, 259, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Kousar, K.; Naseer, F.; Abduh, M.S.; Anjum, S.; Ahmad, T. Cd44 targeted delivery of oncolytic Newcastle disease virus encapsulated in thiolated chitosan for sustained release in cervical cancer: A targeted immunotherapy approach. Front. Immunol. 2023, 14, 1175535. [Google Scholar] [CrossRef] [PubMed]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Q.; Na, J.; Liu, X.; He, J. Exploration of the Delivery of Oncolytic Newcastle Disease Virus by Gelatin Methacryloyl Microneedles. Int. J. Mol. Sci. 2024, 25, 2353. https://doi.org/10.3390/ijms25042353
Zhang Q, Na J, Liu X, He J. Exploration of the Delivery of Oncolytic Newcastle Disease Virus by Gelatin Methacryloyl Microneedles. International Journal of Molecular Sciences. 2024; 25(4):2353. https://doi.org/10.3390/ijms25042353
Chicago/Turabian StyleZhang, Qiang, Jintong Na, Xiyu Liu, and Jian He. 2024. "Exploration of the Delivery of Oncolytic Newcastle Disease Virus by Gelatin Methacryloyl Microneedles" International Journal of Molecular Sciences 25, no. 4: 2353. https://doi.org/10.3390/ijms25042353
APA StyleZhang, Q., Na, J., Liu, X., & He, J. (2024). Exploration of the Delivery of Oncolytic Newcastle Disease Virus by Gelatin Methacryloyl Microneedles. International Journal of Molecular Sciences, 25(4), 2353. https://doi.org/10.3390/ijms25042353





