Antioxidants in Photoaging: From Molecular Insights to Clinical Applications
Abstract
:1. Introduction
2. Materials and Methods
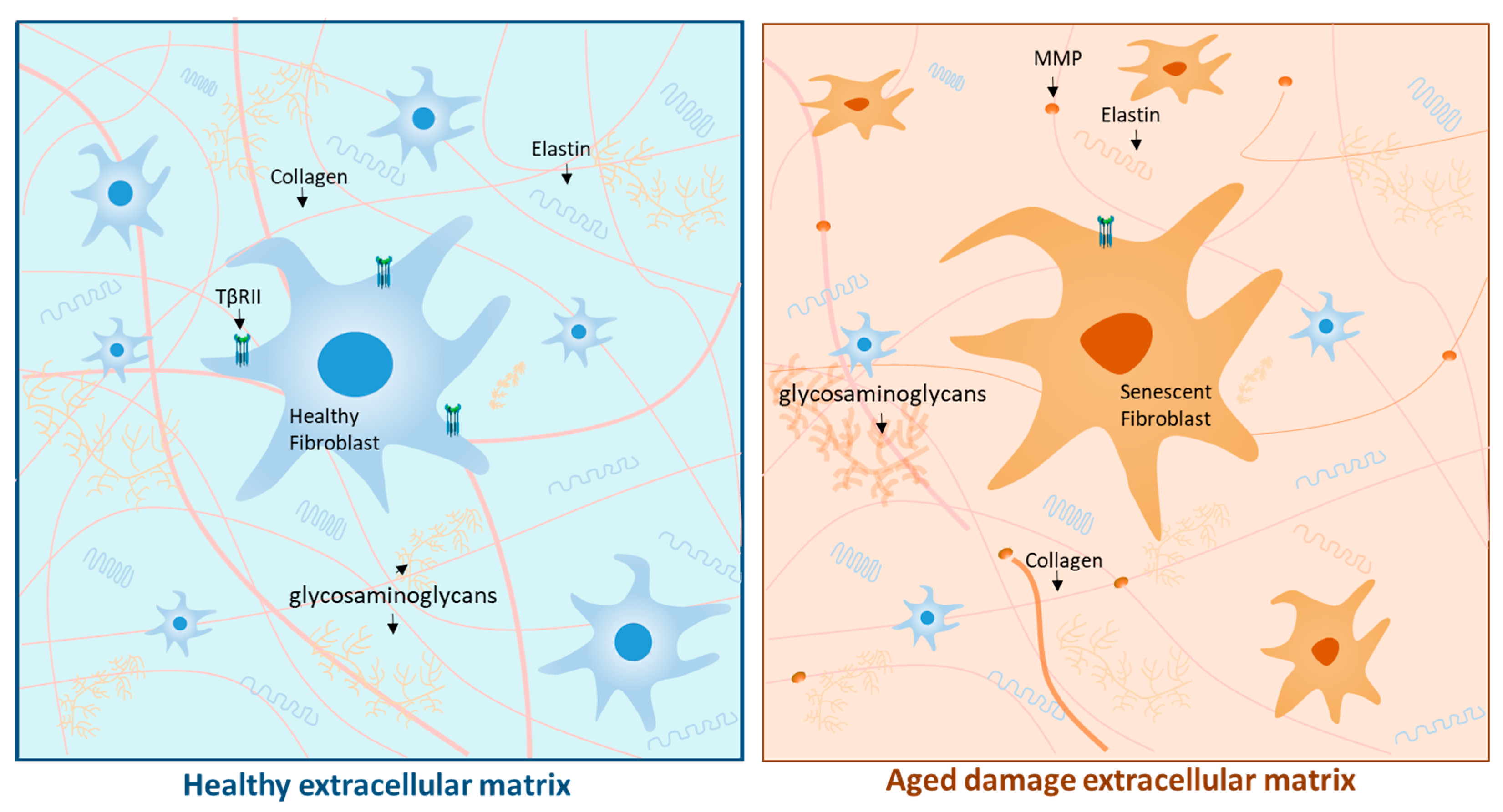
3. Physiological Aging: The Skin’s Stopwatch
4. Photoaging: Underlying Mechanisms and Implications of Oxidative Stress
4.1. Characteristics of Ultraviolet Radiation
4.2. DNA Damage due to Ultraviolet Radiation
4.3. Reactive Oxygen Species and Cellular Signaling Pathways Responsible for the Loss of Skin Integrity
4.4. Ultraviolet Radiation-Mediated Cytotoxicity
5. Antioxidant System and Skin Health
6. Antioxidants against Photoaging: Clinical Evidence
| Authors | Antioxidant | Methodology | Results |
|---|---|---|---|
| Lauer et al. [81] | Vitamin C | Clinical trial with 33 volunteers who were supplemented with vitamin C or placebo for 4 weeks, using in vivo spectroscopy and placebo control. | Oral administration of vitamin C rapidly enhances skin’s radical-scavenging activity, with higher doses providing greater benefits. |
| Chiu et al. [104] | Polyphenols | A randomized, double-blind, clinical trial pilot study was conducted to evaluate the effects of a combination regimen of topical and oral green tea supplementation on 40 women who had moderate PA. | There was a significant increase in elastic tissue content in treated specimens at the histological level. |
| Lephart et al. [100] | Polyphenols | In vitro study on human-skin-equivalent cultures with resveratrol exposure at 1.0% for 24 h. | Resveratrol improves skin aging by stimulating SIRT1, extracellular matrix proteins, and antioxidants while inhibiting biomarkers of inflammation and dermal aging. |
| Tanaka et al. [108] | Phytochemical | Preclinical study of an in vivo mouse model treated with ointments containing DMSO or CIN and irradiated multiple times with UVB for 10 weeks. | CIN reduces ROS production and repairs DNA damage in vitro. Topical application inhibits wrinkle formation, epidermal hyperplasia, and dermal inflammation. CIN promotes antioxidative processes and prevents UVB-induced collagen degradation. |
| Rizwan et al. [115] | Carotenoids | Randomized, single-blinded, controlled trial study evaluating 20 women who ingested 55 gr tomato paste (rich in lycopene) daily for 12 weeks. | After supplementing, there was a significant reduction in DNA damage and a decrease in activity of MMP1 and fibrillin-1, all mediated by UVR. |
| Ying et al. [130] | Marine-algae-derived | In vivo study of a murine model treated with MAA solutions in concentrations of 5, 10, and 20 mg/mL. | The MAA compounds regulated the NF-κB pathway, resulting in increased antioxidant enzymes and decreased proinflammatory cytokines. |
7. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rittié, L.; Fisher, G.J. Natural and Sun-Induced Aging of Human Skin. Cold Spring Harb. Perspect. Med. 2015, 5, a015370. [Google Scholar] [CrossRef] [PubMed]
- Langton, A.K.; Graham, H.K.; Griffiths, C.E.M.; Watson, R.E.B. Ageing significantly impacts the biomechanical function and structural composition of skin. Exp. Dermatol. 2019, 28, 981–984. [Google Scholar] [CrossRef] [PubMed]
- Rinnerthaler, M.; Bischof, J.; Streubel, M.K.; Trost, A.; Richter, K. Oxidative Stress in Aging Human Skin. Biomolecules 2015, 5, 545–589. [Google Scholar] [CrossRef] [PubMed]
- Pandel, R.; Poljšak, B.; Godic, A.; Dahmane, R. Skin Photoaging and the Role of Antioxidants in Its Prevention. Int. Sch. Res. Not. 2013, 2013, e930164. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, F.; Woodby, B.; Pecorelli, A.; Schiavone, M.L.; Pambianchi, E.; Messano, N.; Therrien, J.-P.; Choudhary, H.; Valacchi, G. Additive effect of combined pollutants to UV induced skin OxInflammation damage. Evaluating the protective topical application of a cosmeceutical mixture formulation. Redox Biol. 2020, 34, 101481. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Chien, A.L.; Kang, S. Photoaging. Dermatol. Clin. 2014, 32, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Green, A.C.; Hughes, M.C.B.; McBride, P.; Fourtanier, A. Factors Associated with Premature Skin Aging (Photoaging) before the Age of 55: A Population-Based Study. Dermatology 2010, 222, 74–80. [Google Scholar] [CrossRef]
- Albrecht, S.; Jung, S.; Müller, R.; Lademann, J.; Zuberbier, T.; Zastrow, L.; Reble, C.; Beckers, I.; Meinke, M.C. Skin type differences in solar-simulated radiation-induced oxidative stress. Br. J. Dermatol. 2019, 180, 597–603. [Google Scholar] [CrossRef]
- Maddin, S.; Lauharanta, J.; Agache, P.; Burrows, L.; Zultak, M.; Bulger, L. Isotretinoin improves the appearance of photodamaged skin: Results of a 36-week, multicenter, double-blind, placebo-controlled trial. J. Am. Acad. Dermatol. 2000, 42, 56–63. [Google Scholar] [CrossRef]
- Malvy, J.-M.D.; Guinot, C.; Preziosi, P.; Vaillant, L.; Tenenhaus, M.; Galan, P.; Hercberg, S.; Tschachler, E. Epidemiologic determinants of skin photoaging: Baseline data of the SU.VI.MAX. cohort. J. Am. Acad. Dermatol. 2000, 42, 47–55. [Google Scholar] [CrossRef]
- Czajka, A.; Kania, E.M.; Genovese, L.; Corbo, A.; Merone, G.; Luci, C.; Sibilla, S. Daily oral supplementation with collagen peptides combined with vitamins and other bioactive compounds improves skin elasticity and has a beneficial effect on joint and general wellbeing. Nutr. Res. 2018, 57, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, Y.; Takahashi, Y.; Kishimoto, Y.; Taguchi, C.; Suzuki, N.; Yokoyama, M.; Kondo, K. Consumption of Polyphenols in Coffee and Green Tea Alleviates Skin Photoaging in Healthy Japanese Women. Clin. Cosmet. Investig. Dermatol. 2020, 13, 165–172. [Google Scholar] [CrossRef]
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. The Hallmarks of Aging. Cell 2013, 153, 1194–1217. [Google Scholar] [CrossRef] [PubMed]
- da Costa, J.P.; Vitorino, R.; Silva, G.M.; Vogel, C.; Duarte, A.C.; Rocha-Santos, T. A synopsis on aging—Theories, mechanisms and future prospects. Ageing Res. Rev. 2016, 29, 90–112. [Google Scholar] [CrossRef] [PubMed]
- Soares, J.P.; Cortinhas, A.; Bento, T.; Leitão, J.C.; Collins, A.R.; Gaivã, I.; Mota, M.P. Aging and DNA damage in humans: A meta-analysis study. Aging 2014, 6, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.-W.; Kwon, S.-H.; Choi, J.-Y.; Na, J.-I.; Huh, C.-H.; Choi, H.-R.; Park, K.-C. Molecular Mechanisms of Dermal Aging and Antiaging Approaches. Int. J. Mol. Sci. 2019, 20, 2126. [Google Scholar] [CrossRef] [PubMed]
- Tominaga, K.; Suzuki, H.I. TGF-β Signaling in Cellular Senescence and Aging-Related Pathology. Int. J. Mol. Sci. 2019, 20, 5002. [Google Scholar] [CrossRef]
- Fisher, G.J.; Shao, Y.; He, T.; Qin, Z.; Perry, D.; Voorhees, J.J.; Quan, T. Reduction of fibroblast size/mechanical force down-regulates TGF-β type II receptor: Implications for human skin aging. Aging Cell 2016, 15, 67–76. [Google Scholar] [CrossRef]
- Russell-Goldman, E.; Murphy, G.F. The Pathobiology of Skin Aging: New Insights into an Old Dilemma. Am. J. Pathol. 2020, 190, 1356–1369. [Google Scholar] [CrossRef]
- Lee, Y.I.; Choi, S.; Roh, W.S.; Lee, J.H.; Kim, T.-G. Cellular Senescence and Inflammaging in the Skin Microenvironment. Int. J. Mol. Sci. 2021, 22, 3849. [Google Scholar] [CrossRef]
- Gruber, F.; Kremslehner, C.; Eckhart, L.; Tschachler, E. Cell aging and cellular senescence in skin aging—Recent advances in fibroblast and keratinocyte biology. Exp. Gerontol. 2020, 130, 110780. [Google Scholar] [CrossRef] [PubMed]
- Wlaschek, M.; Maity, P.; Makrantonaki, E.; Scharffetter-Kochanek, K. Connective Tissue and Fibroblast Senescence in Skin Aging. J. Investig. Dermatol. 2021, 141, 985–992. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Campisi, J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2014, 69 (Suppl. S1), S4–S9. [Google Scholar] [CrossRef]
- Doles, J.; Storer, M.; Cozzuto, L.; Roma, G.; Keyes, W.M. Age-associated inflammation inhibits epidermal stem cell function. Genes Dev. 2012, 26, 2144–2153. [Google Scholar] [CrossRef] [PubMed]
- Lynch, B.; Bonod-Bidaud, C.; Ducourthial, G.; Affagard, J.-S.; Bancelin, S.; Psilodimitrakopoulos, S.; Ruggiero, F.; Allain, J.-M.; Schanne-Klein, M.-C. How aging impacts skin biomechanics: A multiscale study in mice. Sci. Rep. 2017, 7, 13750. [Google Scholar] [CrossRef]
- Harn, H.I.-C.; Chen, C.-C.; Wang, S.-P.; Lei, M.; Chuong, C.-M. Tissue Mechanics in Haired Murine Skin: Potential Implications for Skin Aging. Front. Cell Dev. Biol. 2021, 9, 635340. Available online: https://www.frontiersin.org/articles/10.3389/fcell.2021.635340 (accessed on 25 November 2023). [CrossRef]
- Zhang, S.; Duan, E. Fighting against Skin Aging: The Way from Bench to Bedside. Cell Transpl. 2018, 27, 729–738. [Google Scholar] [CrossRef]
- Liochev, S.I. Reactive oxygen species and the free radical theory of aging. Free. Radic. Biol. Med. 2013, 60, 1–4. [Google Scholar] [CrossRef]
- Fan, Q.; Chen, L.; Cheng, S.; Li, F.; Lau, W.B.; Wang, L.F.; Liu, J.H. Aging Aggravates Nitrate-Mediated ROS/RNS Changes. Oxid. Med. Cell. Longev. 2014, 2014, e376515. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, X.; Vikash, V.; Ye, Q.; Wu, D.; Liu, Y.; Dong, W. ROS and ROS-Mediated Cellular Signaling. Oxid. Med. Cell. Longev. 2016, 2016, e4350965. [Google Scholar] [CrossRef]
- Zhang, M.; Liu, N.; Liu, H. Determination of the Total Mass of Antioxidant Substances and Antioxidant Capacity per Unit Mass in Serum Using Redox Titration. Bioinorg. Chem. Appl. 2014, 2014, 928595. [Google Scholar] [CrossRef]
- Krutmann, J.; Schikowski, T.; Morita, A.; Berneburg, M. Environmentally-Induced (Extrinsic) Skin Aging: Exposomal Factors and Underlying Mechanisms. J. Investig. Dermatol. 2021, 141, 1096–1103. [Google Scholar] [CrossRef]
- Wolf, A.M.; Nishimaki, K.; Kamimura, N.; Ohta, S. Real-Time Monitoring of Oxidative Stress in Live Mouse Skin. J. Investig. Dermatol. 2014, 134, 1701–1709. [Google Scholar] [CrossRef] [PubMed]
- Liebel, F.; Kaur, S.; Ruvolo, E.; Kollias, N.; Southall, M.D. Irradiation of Skin with Visible Light Induces Reactive Oxygen Species and Matrix-Degrading Enzymes. J. Investig. Dermatol. 2012, 132, 1901–1907. [Google Scholar] [CrossRef] [PubMed]
- D’Orazio, J.; Jarrett, S.; Amaro-Ortiz, A.; Scott, T. UV Radiation and the Skin. Int. J. Mol. Sci. 2013, 14, 12222–12248. [Google Scholar] [CrossRef]
- Modenese, A.; Korpinen, L.; Gobba, F. Solar Radiation Exposure and Outdoor Work: An Underestimated Occupational Risk. Int. J. Environ. Res. Public Health 2018, 15, 2063. [Google Scholar] [CrossRef] [PubMed]
- Ibuki, Y.; Allanson, M.; Dixon, K.M.; Reeve, V.E. Radiation Sources Providing Increased UVA/UVB Ratios Attenuate the Apoptotic Effects of the UVB Waveband UVA-Dose-Dependently in Hairless Mouse Skin. J. Investig. Dermatol. 2007, 127, 2236–2244. [Google Scholar] [CrossRef]
- Langton, A.K.; Alessi, S.; Hann, M.; Chien, A.L.-L.; Kang, S.; Griffiths, C.E.M.; Watson, R.E.B. Aging in Skin of Color: Disruption to Elastic Fiber Organization Is Detrimental to Skin’s Biomechanical Function. J. Investig. Dermatol. 2019, 139, 779–788. [Google Scholar] [CrossRef] [PubMed]
- Schuch, A.P.; Moreno, N.C.; Schuch, N.J.; Menck, C.F.M.; Garcia, C.C.M. Sunlight damage to cellular DNA: Focus on oxidatively generated lesions. Free. Radic. Biol. Med. 2017, 107, 110–124. [Google Scholar] [CrossRef]
- Roy, S. Impact of UV Radiation on Genome Stability and Human Health. Adv. Exp. Med. Biol. 2017, 996, 207–219. [Google Scholar]
- Mullenders, L.H.F. Solar UV damage to cellular DNA: From mechanisms to biological effects. Photochem. Photobiol. Sci. 2018, 17, 1842–1852. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.P.; Häder, D.-P. UV-induced DNA damage and repair: A review. Photochem. Photobiol. Sci. 2002, 1, 225–236. [Google Scholar] [CrossRef] [PubMed]
- Kciuk, M.; Marciniak, B.; Mojzych, M.; Kontek, R. Focus on UV-Induced DNA Damage and Repair—Disease Relevance and Protective Strategies. Int. J. Mol. Sci. 2020, 21, 7264. [Google Scholar] [CrossRef] [PubMed]
- Bataille, V.; Bykov, V.J.; Sasieni, P.; Harulow, S.; Cuzick, J.; Hemminki, K. Photoadaptation to ultraviolet (UV) radiation in vivo: Photoproducts in epidermal cells following UVB therapy for psoriasis. Br. J. Dermatol. 2000, 143, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Yoshimoto, S.; Kohara, N.; Sato, N.; Ando, H.; Ichihashi, M. Riboflavin Plays a Pivotal Role in the UVA-Induced Cytotoxicity of Fibroblasts as a Key Molecule in the Production of H2O2 by UVA Radiation in Collaboration with Amino Acids and Vitamins. Int. J. Mol. Sci. 2020, 21, 554. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, D.R.; Libardi, S.H.; Skibsted, L.H. Riboflavin as a photosensitizer. Effects on human health and food quality. Food Funct. 2012, 3, 487–502. [Google Scholar] [CrossRef] [PubMed]
- Dizdaroglu, M.; Jaruga, P. Mechanisms of Free Radical-Induced Damage to DNA. Free. Radic. Res. 2012, 46, 382–419. Available online: https://pubmed.ncbi.nlm.nih.gov/22276778/ (accessed on 24 December 2023). [CrossRef] [PubMed]
- Mouret, S.; Forestier, A.; Douki, T. The specificity of UVA-induced DNA damage in human melanocytes. Photochem. Photobiol. Sci. 2012, 11, 155–162. [Google Scholar] [CrossRef]
- Ikehata, H.; Kawai, K.; Komura, J.; Sakatsume, K.; Wang, L.; Imai, M.; Higashi, S.; Nikaido, O.; Yamamoto, K.; Hieda, K.; et al. UVA1 Genotoxicity Is Mediated Not by Oxidative Damage but by Cyclobutane Pyrimidine Dimers in Normal Mouse Skin. J. Investig. Dermatol. 2008, 128, 2289–2296. [Google Scholar] [CrossRef]
- Genovese, L.; Corbo, A.; Sibilla, S. An Insight into the Changes in Skin Texture and Properties following Dietary Intervention with a Nutricosmeceutical Containing a Blend of Collagen Bioactive Peptides and Antioxidants. Ski. Pharmacol. Physiol. 2017, 30, 146–158. [Google Scholar] [CrossRef]
- Yamaba, H.; Haba, M.; Kunita, M.; Sakaida, T.; Tanaka, H.; Yashiro, Y.; Nakata, S. Morphological change of skin fibroblasts induced by UV Irradiation is involved in photoaging. Exp. Dermatol. 2016, 25, 45–51. [Google Scholar] [CrossRef]
- Tewari, A.; Grys, K.; Kollet, J.; Sarkany, R.; Young, A.R. Upregulation of MMP12 and Its Activity by UVA1 in Human Skin: Potential Implications for Photoaging. J. Investig. Dermatol. 2014, 134, 2598–2609. [Google Scholar] [CrossRef]
- He, T.; Quan, T.; Shao, Y.; Voorhees, J.J.; Fisher, G.J. Oxidative exposure impairs TGF-β pathway via reduction of type II receptor and SMAD3 in human skin fibroblasts. Age 2014, 36, 9623. [Google Scholar] [CrossRef] [PubMed]
- Indo, H.P.; Yen, H.-C.; Nakanishi, I.; Matsumoto, K.-I.; Tamura, M.; Nagano, Y.; Matsui, H.; Gusev, O.; Cornette, R.; Okuda, T.; et al. A mitochondrial superoxide theory for oxidative stress diseases and aging. J. Clin. Biochem. Nutr. 2015, 56, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pinto, M.; Moraes, C.T. Mechanisms linking mtDNA damage and aging. Free Radic. Biol. Med. 2015, 85, 250–258. [Google Scholar] [CrossRef]
- Fleury, C.; Mignotte, B.; Vayssière, J.-L. Mitochondrial Reactive Oxygen Species in Cell Death Signaling. Biochimie 2002, 84, 131–141. Available online: https://pubmed.ncbi.nlm.nih.gov/12022944/ (accessed on 24 December 2023). [CrossRef] [PubMed]
- Willems, P.H.G.M.; Rossignol, R.; Dieteren, C.E.J.; Murphy, M.P.; Koopman, W.J.H. Redox Homeostasis and Mitochondrial Dynamics. Cell Metab. 2015, 22, 207–218. [Google Scholar] [CrossRef]
- Cao, C.; Xiao, Z.; Wu, Y.; Ge, C. Diet and Skin Aging—From the Perspective of Food Nutrition. Nutrients 2020, 12, 870. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, N.K.; Norval, M. Photoimmunosuppression: A brief overview. Photodermatol. Photoimmunol. Photomed. 2013, 29, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Weiland, D.; Brachvogel, B.; Hornig-Do, H.T.; Neuhaus, J.F.; Holzer, T.; Tobin, D.J.; Niessen, C.M.; Wiesner, J.R.; Baris, O.R. Imbalance of Mitochondrial Respiratory Chain Complexes in the Epidermis Induces Severe Skin Inflammation. J. Investig. Dermatol. 2018, 138, 132–140. Available online: https://www.jidonline.org/article/S0022-202X(17)32834-8/fulltext (accessed on 24 December 2023). [CrossRef]
- Ansary, T.M.; Hossain, M.R.; Kamiya, K.; Komine, M.; Ohtsuki, M. Inflammatory Molecules Associated with Ultraviolet Radiation-Mediated Skin Aging. Int. J. Mol. Sci. 2021, 22, 3974. [Google Scholar] [CrossRef]
- Bratic, A.; Larsson, N.G. The Role of Mitochondria in Aging. J. Clin. Investig. 2013, 123, 951–957. Available online: https://www.jci.org/articles/view/64125 (accessed on 24 December 2023). [CrossRef]
- Pilkington, S.M.; Bulfone-Paus, S.; Griffiths, C.E.M.; Watson, R.E.B. Inflammaging and the Skin. J. Investig. Dermatol. 2021, 141, 1087–1095. [Google Scholar] [CrossRef]
- Ma, J.; Teng, Y.; Huang, Y.; Tao, X.; Fan, Y. Autophagy plays an essential role in ultraviolet radiation-driven skin photoaging. Front. Pharmacol. 2022, 13, 864331. [Google Scholar] [CrossRef]
- Wang, M.; Charareh, P.; Lei, X.; Zhong, J.L. Autophagy: Multiple Mechanisms to Protect Skin from Ultraviolet Radiation-Driven Photoaging. Oxid. Med. Cell. Longev. 2019, 2019, e8135985. [Google Scholar] [CrossRef]
- Sample, A.; He, Y.Y. Autophagy in UV Damage Response. Photochem. Photobiol. 2016, 93, 943–955. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/php.12691 (accessed on 24 December 2023). [CrossRef]
- Rhie, G.; Shin, M.H.; Seo, J.Y.; Choi, W.W.; Cho, K.H.; Kim, K.H.; Park, K.C.; Eun, H.C.; Chung, J.H. Aging- and Photoaging-Dependent Changes of Enzymic and Nonenzymic Antioxidants in the Epidermis and Dermis of Human Skin In Vivo. J. Investig. Dermatol. 2001, 117, 1212–1217. [Google Scholar] [CrossRef] [PubMed]
- Poljsak, B.; Šuput, D.; Milisav, I. Achieving the Balance between ROS and Antioxidants: When to Use the Synthetic Antioxidants. Oxid. Med. Cell. Longev. 2013, 2013, e956792. [Google Scholar] [CrossRef] [PubMed]
- Dhalaria, R.; Verma, R.; Kumar, D.; Puri, S.; Tapwal, A.; Kumar, V.; Nepovimova, E.; Kuca, K. Bioactive Compounds of Edible Fruits with Their Anti-Aging Properties: A Comprehensive Review to Prolong Human Life. Antioxidants 2020, 9, 1123. [Google Scholar] [CrossRef] [PubMed]
- Gulcin, İ. Antioxidants and antioxidant methods: An updated overview. Arch. Toxicol. 2020, 94, 651–715. [Google Scholar] [CrossRef]
- Gruber, J.V.; Holtz, R. Examining the Genomic Influence of Skin Antioxidants In Vitro. Mediat. Inflamm. 2010, 2010, e230450. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.C.B.; Williams, G.M.; Pageon, H.; Fourtanier, A.; Green, A.C. Dietary Antioxidant Capacity and Skin Photoaging: A 15-Year Longitudinal Study. J. Investig. Dermatol. 2021, 141, 1111–1118.e2. [Google Scholar] [CrossRef] [PubMed]
- De Luca, C.; Mikhal’chik, E.V.; Suprun, M.V.; Papacharalambous, M.; Truhanov, A.I.; Korkina, L.G. Skin Antiageing and Systemic Redox Effects of Supplementation with Marine Collagen Peptides and Plant-Derived Antioxidants: A Single-Blind Case-Control Clinical Study. Oxid. Med. Cell. Longev. 2016, 2016, e4389410. [Google Scholar] [CrossRef] [PubMed]
- Ribet, V.; Nobile, V.; Rossi, A.B. In situ antioxidant activity of a dermo-cosmetic product: A randomized controlled clinical study. Exp. Dermatol. 2019, 28, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, C.E.M. Drug Treatment of Photoaged Skin. Drugs Aging 1999, 14, 289–301. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, C.; Kosmadaki, M.G.; Stratigos, A.J.; Katsambas, A.D. Photoaging. Am. J. Clin. Dermatol. 2010, 11, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Poon, F.; Kang, S.; Chien, A.L. Mechanisms and treatments of photoaging. Photodermatol. Photoimmunol. Photomed. 2015, 31, 65–74. [Google Scholar] [CrossRef]
- Traber, M.G.; Stevens, J.F. Vitamins C and E: Beneficial effects from a mechanistic perspective. Free. Radic. Biol. Med. 2011, 51, 1000–1013. [Google Scholar] [CrossRef]
- Pullar, J.M.; Carr, A.C.; Vissers, M.C.M. The Roles of Vitamin C in Skin Health. Nutrients 2017, 9, 866. [Google Scholar] [CrossRef]
- Farris, P.K. Topical Vitamin C: A Useful Agent for Treating Photoaging and Other Dermatologic Conditions. Dermatol. Surg. 2005, 31, 814. [Google Scholar] [CrossRef]
- Lauer, A.-C.; Groth, N.; Haag, S.F.; Darvin, M.E.; Lademann, J.; Meinke, M.C. Dose-Dependent Vitamin C Uptake and Radical Scavenging Activity in Human Skin Measured with in vivo Electron Paramagnetic Resonance Spectroscopy. Ski. Pharmacol. Physiol. 2013, 26, 147–154. [Google Scholar] [CrossRef]
- McArdle, F.; Rhodes, L.E.; Parslew, R.A.; Close, G.L.; Jack, C.I.; Friedmann, P.S.; Jackson, M.J. Effects of oral vitamin E and β-carotene supplementation on ultraviolet radiation–induced oxidative stress in human skin2. Am. J. Clin. Nutr. 2004, 80, 1270–1275. [Google Scholar] [CrossRef]
- McArdle, F.; Rhodes, L.E.; Parslew, R.; Jack, C.I.A.; Friedmann, P.S.; Jackson, M.J. UVR-induced oxidative stress in human skin in vivo: Effects of oral vitamin C supplementation. Free. Radic. Biol. Med. 2002, 33, 1355–1362. [Google Scholar] [CrossRef]
- Nusgens, B.V.; Colige, A.C.; Lambert, C.A.; Lapière, C.M.; Humbert, P.; Rougier, A.; Haftek, M.; Richard, A.; Creidi, P. Topically Applied Vitamin C Enhances the mRNA Level of Collagens I and III, Their Processing Enzymes and Tissue Inhibitor of Matrix Metalloproteinase 1 in the Human Dermis1. J. Investig. Dermatol. 2001, 116, 853–859. [Google Scholar] [CrossRef]
- Fitzpatrick, R.E.; Rostan, E.F. Double-Blind, Half-Face Study Comparing Topical Vitamin C and Vehicle for Rejuvenation of Photodamage. Dermatol. Surg. 2002, 28, 231. [Google Scholar] [PubMed]
- Humbert, P.G.; Haftek, M.; Creidi, P.; Lapière, C.; Nusgens, B.; Richard, A.; Schmitt, D.; Rougier, A.; Zahouani, H. Topical ascorbic acid on photoaged skin. Clinical, topographical and ultrastructural evaluation: Double-blind study vs. placebo. Exp. Dermatol. 2003, 12, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Murray, J.C.; Burch, J.A.; Streilein, R.D.; Iannacchione, M.A.; Hall, R.P.; Pinnell, S.R. A topical antioxidant solution containing vitamins C and E stabilized by ferulic acid provides protection for human skin against damage caused by ultraviolet irradiation. J. Am. Acad. Dermatol. 2008, 59, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-Y.; Selim, M.A.; Shea, C.R.; Grichnik, J.M.; Omar, M.M.; Monteiro-Riviere, N.A.; Pinnell, S.R. UV photoprotection by combination topical antioxidants vitamin C and vitamin E. J. Am. Acad. Dermatol. 2003, 48, 866–874. [Google Scholar] [CrossRef] [PubMed]
- De Dormael, R.; Bastien, P.; Sextius, P.; Gueniche, A.; Ye, D.; Tran, C.; Chevalier, V.; Gomes, C.; Souverain, L.; Tricaud, C. Vitamin C Prevents Ultraviolet-induced Pigmentation in Healthy Volunteers: Bayesian Meta-analysis Results from 31 Randomized Controlled versus Vehicle Clinical Studies. J. Clin. Aesthet. Dermatol. 2019, 12, E53–E59. [Google Scholar] [PubMed]
- Placzek, M.; Gaube, S.; Kerkmann, U.; Gilbertz, K.-P.; Herzinger, T.; Haen, E.; Przybilla, B. Ultraviolet B-Induced DNA Damage in Human Epidermis Is Modified by the Antioxidants Ascorbic Acid and D-α-Tocopherol. J. Investig. Dermatol. 2005, 124, 304–307. [Google Scholar] [CrossRef] [PubMed]
- Werninghaus, K.; Meydani, M.; Bhawan, J.; Margolis, R.; Blumberg, J.B.; Gilchrest, B.A. Evaluation of the Photoprotective Effect of Oral Vitamin E Supplementation. Arch. Dermatol. 1994, 130, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Petruk, G.; Del Giudice, R.; Rigano, M.M.; Monti, D.M. Antioxidants from Plants Protect against Skin Photoaging. Oxid. Med. Cell. Longev. 2018, 2018, e1454936. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Lee, J.-H. Protective effects of resveratrol on UVB-irradiated HaCaT cells through attenuation of the caspase pathway. Oncol. Rep. 2008, 19, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Perde-Schrepler, M.; Chereches, G.; Brie, I.; Tatomir, C.; Postescu, I.D.; Soran, L.; Filip, A. Grape seed extract as photochemopreventive agent against UVB-induced skin cancer. J. Photochem. Photobiol. B Biol. 2013, 118, 16–21. [Google Scholar] [CrossRef]
- Auh, J.-H.; Madhavan, J. Protective effect of a mixture of marigold and rosemary extracts on UV-induced photoaging in mice. Biomed. Pharmacother. 2021, 135, 111178. [Google Scholar] [CrossRef]
- Orqueda, M.E.; Moreno, M.A.; Zampini, I.C.; Bravo, K.; Osorio, E.; Isla, M.I. Potential use of medicinal plants from Argentinean highland as agent anti-photoaging. J. Cosmet. Dermatol. 2021, 20, 1188–1196. [Google Scholar] [CrossRef]
- Mnich, C.D.; Hoek, K.S.; Virkki, L.V.; Farkas, A.; Dudli, C.; Laine, E.; Urosevic, M.; Dummer, R. Green tea extract reduces induction of p53 and apoptosis in UVB-irradiated human skin independent of transcriptional controls. Exp. Dermatol. 2009, 18, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Constantinescu, T.; Mihis, A.G. Resveratrol as a privileged molecule with antioxidant activity. Food Chem. Adv. 2023, 3, 100539. [Google Scholar] [CrossRef]
- Davies, S.; Contri, R.V.; Guterres, S.S.; Pohlmann, A.R.; Guerreiro, I.C.K. Simultaneous nanoencapsulation of lipoic acid and resveratrol with improved antioxidant properties for the skin. Colloids Surf. B Biointerfaces 2020, 192, 111023. [Google Scholar] [CrossRef]
- Lephart, E.D.; Sommerfeldt, J.M.; Andrus, M.B. Resveratrol: Influences on gene expression in human skin. J. Funct. Foods 2014, 10, 377–384. [Google Scholar] [CrossRef]
- Alonso, C.; Martí, M.; Barba, C.; Carrer, V.; Rubio, L.; Coderch, L. Skin permeation and antioxidant efficacy of topically applied resveratrol. Arch. Dermatol. Res. 2017, 309, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Biswas, P.; Dellanoce, C.; Vezzoli, A.; Mrakic-Sposta, S.; Malnati, M.; Beretta, A.; Accinni, R. Antioxidant Activity with Increased Endogenous Levels of Vitamin C, E and A Following Dietary Supplementation with a Combination of Glutathione and Resveratrol Precursors. Nutrients 2020, 12, 3224. [Google Scholar] [CrossRef]
- Maruki-Uchida, H.; Morita, M.; Yonei, Y.; Sai, M. Effect of Passion Fruit Seed Extract Rich in Piceatannol on the Skin of Women: A Randomized, Placebo-Controlled, Double-Blind Trial. J. Nutr. Sci. Vitaminol. 2018, 64, 75–80. [Google Scholar] [CrossRef]
- Chiu, A.E.; Chan, J.L.; Kern, D.G.; Kohler, S.; Rehmus, W.E.; Kimball, A.B. Double-Blinded, Placebo-Controlled Trial of Green Tea Extracts in the Clinical and Histologic Appearance of Photoaging Skin. Dermatol. Surg. 2005, 31, 855. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Sánchez, A.; Barrajón-Catalán, E.; Caturla, N.; Castillo, J.; Benavente-García, O.; Alcaraz, M.; Micol, V. Protective effects of citrus and rosemary extracts on UV-induced damage in skin cell model and human volunteers. J. Photochem. Photobiol. B Biol. 2014, 136, 12–18. [Google Scholar] [CrossRef]
- Heinrich, U.; Neukam, K.; Tronnier, H.; Sies, H.; Stahl, W. Long-Term Ingestion of High Flavanol Cocoa Provides Photoprotection against UV-Induced Erythema and Improves Skin Condition in Women1. J. Nutr. 2006, 136, 1565–1569. [Google Scholar] [CrossRef]
- Zhang, C.; Fan, L.; Fan, S.; Wang, J.; Luo, T.; Tang, Y.; Chen, Z.; Yu, L. Cinnamomum cassia Presl: A Review of Its Traditional Uses, Phytochemistry, Pharmacology and Toxicology. Molecules 2019, 24, 3473. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y.; Uchi, H.; Furue, M. Antioxidant cinnamaldehyde attenuates UVB-induced photoaging. J. Dermatol. Sci. 2019, 96, 151–158. [Google Scholar] [CrossRef]
- Cho, H.-S.; Lee, M.-H.; Lee, J.W.; No, K.-O.; Park, S.-K.; Lee, H.-S.; Kang, S.; Cho, W.-G.; Park, H.J.; Oh, K.W.; et al. Anti-wrinkling effects of the mixture of vitamin C, vitamin E, pycnogenol and evening primrose oil, and molecular mechanisms on hairless mouse skin caused by chronic ultraviolet B irradiation. Photodermatol. Photoimmunol. Photomed. 2007, 23, 155–162. [Google Scholar] [CrossRef]
- Stahl, W.; Sies, H. Carotenoids and Protection against Solar UV Radiation. Ski. Pharmacol. Appl. Ski. Physiol. 2002, 15, 291–296. [Google Scholar] [CrossRef]
- Calniquer, G.; Khanin, M.; Ovadia, H.; Linnewiel-Hermoni, K.; Stepensky, D.; Trachtenberg, A.; Sedlov, T.; Braverman, O.; Levy, J.; Sharoni, Y. Combined Effects of Carotenoids and Polyphenols in Balancing the Response of Skin Cells to UV Irradiation. Molecules 2021, 26, 1931. [Google Scholar] [CrossRef]
- Zerres, S.; Stahl, W. Carotenoids in human skin. Biochim. Biophys. Acta BBA Mol. Cell Biol. Lipids 2020, 1865, 158588. [Google Scholar] [CrossRef] [PubMed]
- Köpcke, W.; Krutmann, J. Protection from Sunburn with β-Carotene—A Meta-analysis†. Photochem. Photobiol. 2008, 84, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Lopes, L.B.; VanDeWall, H.; Li, H.T.; Venugopal, V.; Li, H.K.; Naydin, S.; Hosmer, J.; Levendusky, M.; Zheng, H.; Bentley, M.V.L.B.; et al. Topical Delivery of Lycopene using Microemulsions: Enhanced Skin Penetration and Tissue Antioxidant Activity. J. Pharm. Sci. 2010, 99, 1346–1357. [Google Scholar] [CrossRef]
- Rizwan, M.; Rodriguez-Blanco, I.; Harbottle, A.; Birch-Machin, M.A.; Watson, R.E.B.; Rhodes, L.E. Tomato paste rich in lycopene protects against cutaneous photodamage in humans in vivo: A randomized controlled trial: Photoprotection by lycopene. Br. J. Dermatol. 2011, 164, 154–162. [Google Scholar] [CrossRef]
- Grether-Beck, S.; Marini, A.; Jaenicke, T.; Stahl, W.; Krutmann, J. Molecular evidence that oral supplementation with lycopene or lutein protects human skin against ultraviolet radiation: Results from a double-blinded, placebo-controlled, crossover study. Br. J. Dermatol. 2017, 176, 1231–1240. [Google Scholar] [CrossRef] [PubMed]
- Ito, N.; Seki, S.; Ueda, F. The Protective Role of Astaxanthin for UV-Induced Skin Deterioration in Healthy People—A Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients 2018, 10, 817. [Google Scholar] [CrossRef]
- Baswan, S.M.; Marini, A.; Klosner, A.E.; Jaenicke, T.; Leverett, J.; Murray, M.; Gellenbeck, K.W.; Krutmann, J. Orally administered mixed carotenoids protect human skin against ultraviolet A-induced skin pigmentation: A double-blind, placebo-controlled, randomized clinical trial. Photodermatol. Photoimmunol. Photomed. 2020, 36, 219–225. [Google Scholar] [CrossRef]
- Stahl, W.; Heinrich, U.; Aust, O.; Tronnier, H.; Sies, H. Lycopene-rich products and dietary photoprotection. Photochem. Photobiol. Sci. 2006, 5, 238–242. [Google Scholar] [CrossRef]
- Costa, A.; Lindmark, L.; Arruda, L.H.F.; Assumpção, E.C.; Ota, F.S.; Pereira, M. de O.; Langen, S.S.B. Clinical, biometric and ultrasound assessment of the effects of daily use of a nutraceutical composed of lycopene, acerola extract, grape seed extract and Biomarine Complex in photoaged human skin. An. Bras. Dermatol. 2012, 87, 52–61. [Google Scholar] [CrossRef]
- Costa, A.; Pereira, E.S.P.; Assumpção, E.C.; dos Santos, F.B.C.; Ota, F.S.; Pereira, M.d.O.; Fidelis, M.C.; Fávaro, R.; Langen, S.S.B.; de Arruda, L.H.F.; et al. Assessment of clinical effects and safety of an oral supplement based on marine protein, vitamin C, grape seed extract, zinc, and tomato extract in the improvement of visible signs of skin aging in men. Clin. Cosmet. Investig. Dermatol. 2015, 8, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Granger, C.; Aladren, S.; Delgado, J.; Garre, A.; Trullas, C.; Gilaberte, Y. Prospective Evaluation of the Efficacy of a Food Supplement in Increasing Photoprotection and Improving Selective Markers Related to Skin Photo-Ageing. Dermatol. Ther. 2020, 10, 163–178. [Google Scholar] [CrossRef] [PubMed]
- Stephens, T.J.; Sigler, M.L.; Herndon, J.H., Jr.; Dispensa, L.; Moigne, A.L. A placebo-controlled, double-blind clinical trial to evaluate the efficacy of Imedeen® Time Perfection® for improving the appearance of photodamaged skin. Clin. Cosmet. Investig. Dermatol. 2016, 9, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Stephens, T.J.; Sigler, M.L.; Hino, P.D.; Moigne, A.L.; Dispensa, L. A Randomized, Double-blind, Placebo-controlled Clinical Trial Evaluating an Oral Anti-aging Skin Care Supplement for Treating Photodamaged Skin. J. Clin. Aesthet. Dermatol. 2016, 9, 25–32. [Google Scholar] [PubMed]
- Dumoulin, M.; Gaudout, D.; Lemaire, B. Clinical effects of an oral supplement rich in antioxidants on skin radiance in women. Clin. Cosmet. Investig. Dermatol. 2016, 9, 315–324. [Google Scholar] [CrossRef]
- Motwani, M.S.; Khan, K.; Pai, A.; Joshi, R. Efficacy of a collagen hydrolysate and antioxidants-containing nutraceutical on metrics of skin health in Indian women. J. Cosmet. Dermatol. 2020, 19, 3371–3382. [Google Scholar] [CrossRef]
- Xie, Y.; Zhu, G.; Yi, J.; Ji, Y.; Xia, Y.; Zheng, Y.; Ye, C. A new product of multi-plant extracts improved skin photoaging: An oral intake in vivo study. J. Cosmet. Dermatol. 2022, 21, 3406–3415. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, J.-E.; Kim, K.H.; Kang, N.J. Beneficial Effects of Marine Algae-Derived Carbohydrates for Skin Health. Mar. Drugs 2018, 16, 459. [Google Scholar] [CrossRef]
- Pangestuti, R.; Siahaan, E.A.; Kim, S.-K. Photoprotective Substances Derived from Marine Algae. Mar. Drugs 2018, 16, 399. [Google Scholar] [CrossRef]
- Ying, R.; Zhang, Z.; Zhu, H.; Li, B.; Hou, H. The Protective Effect of Mycosporine-Like Amino Acids (MAAs) from Porphyra yezoensis in a Mouse Model of UV Irradiation-Induced Photoaging. Mar. Drugs 2019, 17, 470. [Google Scholar] [CrossRef]
- Wang, K.; Deng, Y.; He, Y.; Cao, J.; Zhang, L.; Qin, L.; Qu, C.; Li, H.; Miao, J. Protective Effect of Mycosporine-like Amino Acids Isolated from an Antarctic Diatom on UVB-Induced Skin Damage. Int. J. Mol. Sci. 2023, 24, 15055. [Google Scholar] [CrossRef]
- Lalegerie, F.; Lajili, S.; Bedoux, G.; Taupin, L.; Stiger-Pouvreau, V.; Connan, S. Photo-protective compounds in red macroalgae from Brittany: Considerable diversity in mycosporine-like amino acids (MAAs). Mar. Environ. Res. 2019, 147, 37–48. [Google Scholar] [CrossRef]
- Zeng, J.; Lu, J. Mechanisms of action involved in ozone-therapy in skin diseases. Int. Immunopharmacol. 2018, 56, 235–241. [Google Scholar] [CrossRef]
- Lacerda, A.C.; Grillo, R.; De Barros, T.E.P.; Martins, C.B.; De Carvalho Luposeli, F. Efficacy of biostimulatory ozone therapy: Case report and literature review. J. Cosmet. Dermatol. 2022, 21, 130–133. [Google Scholar] [CrossRef]
- Makarov, I.V.; Shchukin, Y.V.; Lukashova, A.V. Effect of combined application of ozone therapy and gravitational therapy on the remote results of complex treatment of geriatric patients. Adv. Gerontol. 2017, 30, 558–562. [Google Scholar]
- Crane, J.D.; MacNeil, L.G.; Lally, J.S.; Ford, R.J.; Bujak, A.L.; Brar, I.K.; Kemp, B.E.; Raha, S.; Steinberg, G.R.; Tarnopolsky, M.A. Exercise-stimulated interleukin-15 is controlled by AMPK and regulates skin metabolism and aging. Aging Cell 2015, 14, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.; Chung, E.; Diffee, G.; Ji, L.L. Exercise training attenuates aging-associated mitochondrial dysfunction in rat skeletal muscle: Role of PGC-1α. Exp. Gerontol. 2013, 48, 1343–1350. [Google Scholar] [CrossRef]
- clinicaltrials.gov. Integrative Skin Science and Research. Effects of Mango Intake on Skin Health and Gut Microbiome Changes in Postmenopausal Women; Report No.: NCT04869852. May 2021. Available online: https://clinicaltrials.gov/study/NCT04869852 (accessed on 31 December 2022).
- clinicaltrials.gov. Integrative Skin Science and Research. Prospective, Randomized Controlled Study on the Effects of Dietary Soy Protein on Facial; Report No.: NCT04871750. May 2021. Available online: https://clinicaltrials.gov/study/NCT04871750 (accessed on 31 December 2022).
- clinicaltrials.gov. Integrative Skin Science and Research. Prospective, Double-Blinded, Randomized Placebo Controlled Study of an Oral Herbal Supplement on Photoaged Skin and Elasticity; Report No.: NCT06146140. November 2023. Available online: https://clinicaltrials.gov/study/NCT06146140 (accessed on 31 December 2022).
- Sivamani, R.; clinicaltrials.gov. Double Blind Placebo Controlled Oral Supplementation of Astaxanthin on Skin Photoaging, Hydration and Elasticity; Report No.: NCT05882084. July 2023. Available online: https://clinicaltrials.gov/study/NCT05882084 (accessed on 31 December 2022).
- Sivamani, R.; clinicaltrials.gov. The Effects of a Longevity Supplement on Skin Health, Blood Biomarkers and Mental Health; Report No.: NCT05262036. October 2023. Available online: https://clinicaltrials.gov/study/NCT05262036 (accessed on 31 December 2022).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calvo, M.J.; Navarro, C.; Durán, P.; Galan-Freyle, N.J.; Parra Hernández, L.A.; Pacheco-Londoño, L.C.; Castelanich, D.; Bermúdez, V.; Chacin, M. Antioxidants in Photoaging: From Molecular Insights to Clinical Applications. Int. J. Mol. Sci. 2024, 25, 2403. https://doi.org/10.3390/ijms25042403
Calvo MJ, Navarro C, Durán P, Galan-Freyle NJ, Parra Hernández LA, Pacheco-Londoño LC, Castelanich D, Bermúdez V, Chacin M. Antioxidants in Photoaging: From Molecular Insights to Clinical Applications. International Journal of Molecular Sciences. 2024; 25(4):2403. https://doi.org/10.3390/ijms25042403
Chicago/Turabian StyleCalvo, María José, Carolina Navarro, Pablo Durán, Nataly J. Galan-Freyle, Luis Alberto Parra Hernández, Leonardo C Pacheco-Londoño, Desiree Castelanich, Valmore Bermúdez, and Maricarmen Chacin. 2024. "Antioxidants in Photoaging: From Molecular Insights to Clinical Applications" International Journal of Molecular Sciences 25, no. 4: 2403. https://doi.org/10.3390/ijms25042403






