Connective Tissue Growth Factor: Regulation, Diseases, and Drug Discovery
Abstract
1. Introduction
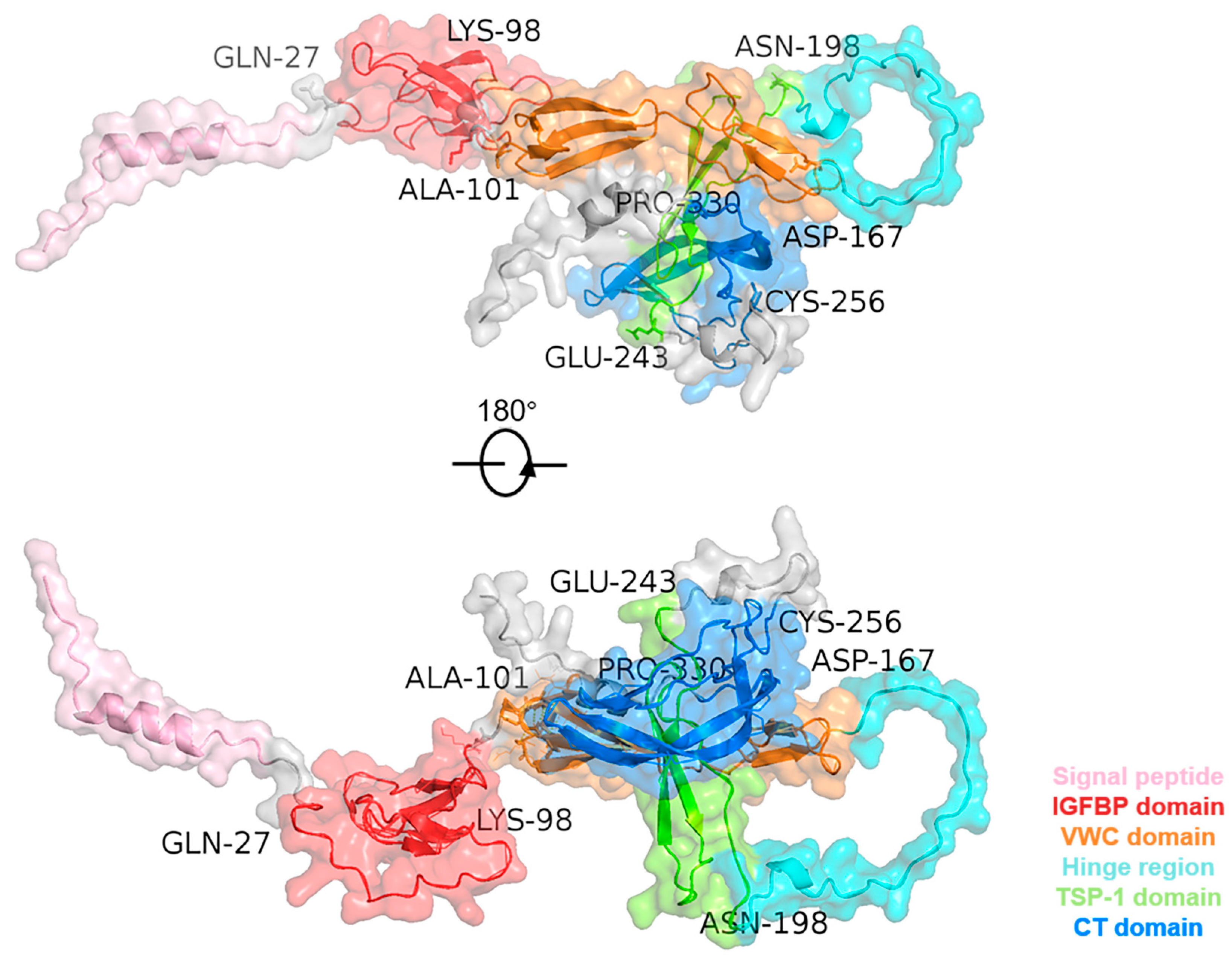
2. Interaction to Molecules and Related Signaling Pathways of CTGF Domains
2.1. IGFBP Domain
2.2. VWC Domain
2.3. TSP-1 Domain
2.4. CT Domain
3. Roles of CTGF in Different Diseases
3.1. Fibrosis-Related Diseases in the Tissues
3.2. Cancer Diseases
3.3. Neurodegenerative Diseases
3.4. Ophthalmic Diseases
3.5. Cardiovascular Diseases
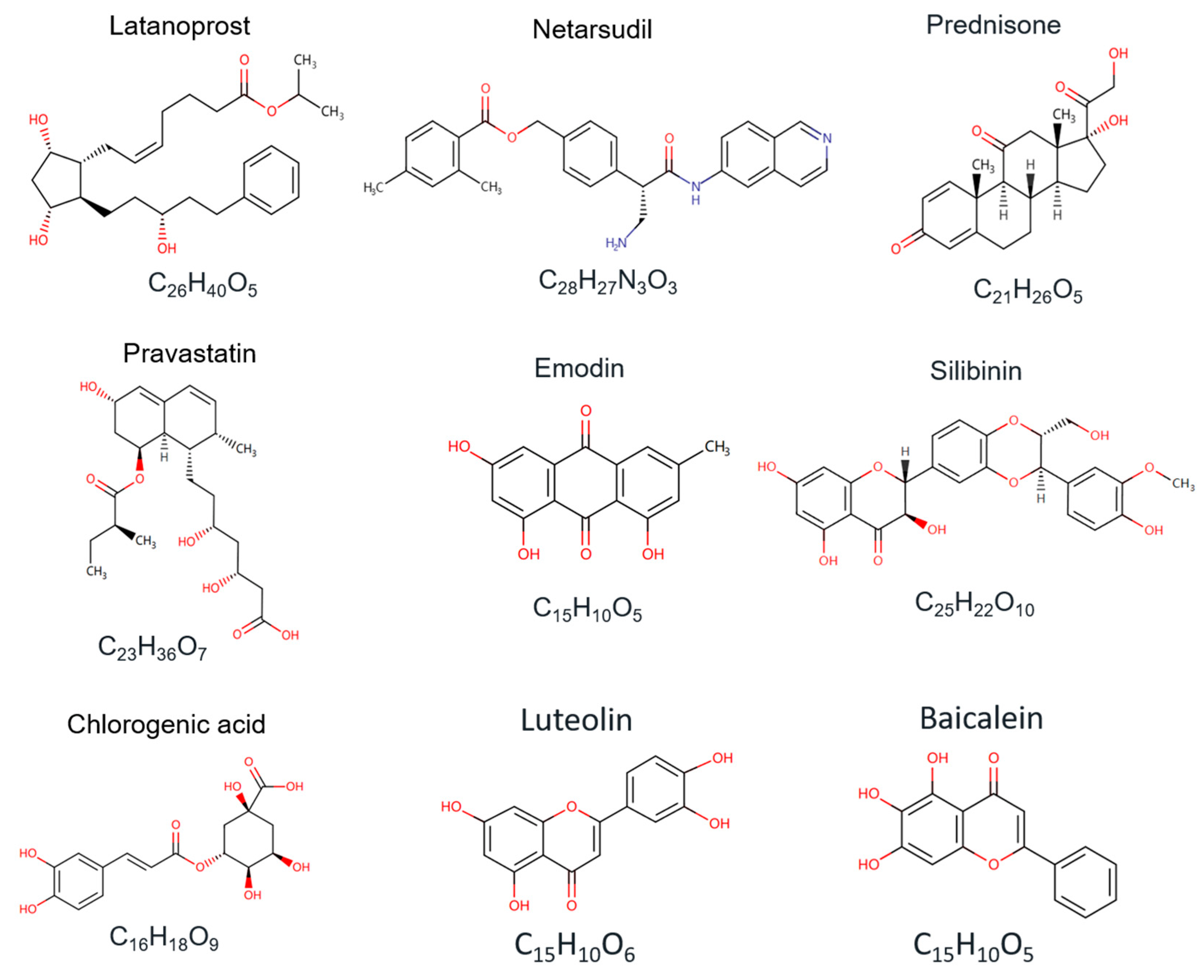
4. CTGF Targeted and Inhibitory Drug Discovery
5. Non-Clinical and Clinical Trials of CTGF-Targeted and Inhibitory Therapy
| Candidates or Trial Titles | Targets | Indications | Status | Types | Ref. | ClinicalTrials ID. |
|---|---|---|---|---|---|---|
| Latanoprost | CTGF, PTGFR | Glaucoma, Hypertensive eye disease | Marketing | Chemical compound | [137] | NCT05283395 |
| Netarsudil | CTGF, TGFBR2 | Glaucoma, Hypertensive eye disease, Corneal edema | Marketing | Chemical compound | [138] | NCT03808688 |
| Prednisone | GCR | Duchenne muscular dystrophy, Prostate cancer, Autoimmune hepatitis | Marketing | Chemical compound | [142] | NCT03439670 |
| FG-3019 | CTGF | Duchenne muscular dystrophy, Pulmonary fibrosis | Clinical Phase III | Monoclonal antibody | [58] | NCT04632940 NCT04419558 NCT04371666 |
| OLX-10010 | CTGF | Pulmonary fibrosis, Proliferative skin scarring | Clinical Phase II | siRNA | [139] | NCT04012099 NCT04877756 |
| RXI-109 | CTGF | Skin scarring, Age-related macular degeneration, Subfoveal choroidal Neovascularization, Subretinal scarring | Clinical Phase II | siRNA | [154] | NCT02079168 NCT02030275 NCT02599064 |
| Pravastatin | TGF-β1, CTGF | Delayed cutaneous, Subcutaneous Radio-induced Fibrosis | Clinical Phase II | Chemical compound | [155] | NCT01268202 |
| PRS-220 | CTGF | Pulmonary fibrosis | Clinical Phase I | Chemical compound | [156] | NCT05473533 |
6. Conclusions and Perspectives
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Fu, M.; Peng, D.; Lan, T.; Wei, Y.; Wei, X. Multifunctional regulatory protein connective tissue growth factor (CTGF): A potential therapeutic target for diverse diseases. Acta Pharm. Sin. B 2022, 12, 1740–1760. [Google Scholar] [CrossRef]
- Shen, Y.-W.; Zhou, Y.-D.; Chen, H.-Z.; Luan, X.; Zhang, W.-D. Targeting CTGF in cancer: An emerging therapeutic opportunity. Trends Cancer 2021, 7, 511–524. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Zhou, C.; Yuan, Q.; Zhang, D.; Xie, J.; Zou, S. CTGF facilitates cell-cell communication in chondrocytes via PI3K/Akt signalling pathway. Cell Prolif. 2021, 54, e13001. [Google Scholar] [CrossRef] [PubMed]
- Hendesi, H.; Barbe, M.F.; Safadi, F.F.; Monroy, M.A.; Popoff, S.N. Integrin mediated adhesion of osteoblasts to connective tissue growth factor (CTGF/CCN2) induces cytoskeleton reorganization and cell differentiation. PLOS ONE 2015, 10, e0115325. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.-C.; Wang, E.Y.; Yi, Y.; Thakur, A.; Tsai, S.-H.; Hoodless, P.A. S1P stimulates proliferation by upregulating CTGF expression through S1PR2-mediated YAP activation. Mol. Cancer Res. 2018, 16, 1543–1555. [Google Scholar] [CrossRef] [PubMed]
- Sun, C.; Zhang, H.; Liu, X. Emerging role of CCN family proteins in fibrosis. J. Cell. Physiol. 2021, 236, 4195–4206. [Google Scholar] [CrossRef] [PubMed]
- Zaykov, V.; Chaqour, B. The CCN2/CTGF interactome: An approach to understanding the versatility of CCN2/CTGF molecular activities. J. Cell Commun. Signal. 2021, 15, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhang, N.; Chu, H.Y.; Yu, Y.; Zhang, Z.-K.; Zhang, G.; Zhang, B.-T. Connective tissue growth factor: From molecular understandings to drug discovery. Front. Cell Dev. Biol. 2020, 8, 593269. [Google Scholar] [CrossRef]
- Perbal, B. CCN proteins: Multifunctional signalling regulators. Lancet 2004, 363, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.R.; Liszewska, E.; Jaworski, J. Matricellular proteins of the Cyr61/CTGF/NOV (CCN) family and the nervous system. Front. Cell. Neurosci. 2015, 9, 237. [Google Scholar] [CrossRef]
- Talia, C.; Connolly, L.; Fowler, P.A. The insulin-like growth factor system: A target for endocrine disruptors? Environ. Int. 2021, 147, 106311. [Google Scholar] [CrossRef] [PubMed]
- Yanagihara, T.; Tsubouchi, K.; Gholiof, M.; Chong, S.G.; Lipson, K.E.; Zhou, Q.; Scallan, C.; Upagupta, C.; Tikkanen, J.; Keshavjee, S.; et al. Connective-tissue growth factor contributes to TGF-β1–induced lung fibrosis. Am. J. Respir. Cell Mol. Biol. 2022, 66, 260–270. [Google Scholar] [CrossRef]
- Yang, L.; Zheng, X.; Mo, C.; Li, S.; Liu, Z.; Yang, G.; Zhao, Q.; Li, S.; Mou, C. Transcriptome analysis and identification of genes associated with chicken sperm storage duration. Poult. Sci. 2020, 99, 1199–1208. [Google Scholar] [CrossRef]
- Cheng, W.-H.; Lee, K.-Y.; Yu, M.-C.; Chen, J.-Y.; Lin, C.-H.; Chen, B.-C. Pref-1 induced lung fibroblast differentiation by hypoxia through integrin α5β1/ERK/AP-1 cascade. Eur. J. Pharmacol. 2021, 909, 174385. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-S.; Nagalla, S.R.; Oh, Y.; Wilson, E.; Roberts, C.T., Jr.; Rosenfeld, R.G. Identification of a family of low-affinity insulin-like growth factor binding proteins (IGFBPs): Characterization of connective tissue growth factor as a member of the IGFBP superfamily. Proc. Natl. Acad. Sci. USA 1997, 94, 12981–12986. [Google Scholar] [CrossRef]
- Yan, S.; Zhang, M.; Yang, G.; Sun, Y.; Ai, D. CTGF promotes the osteoblast differentiation of human periodontal ligament stem cells by positively regulating BMP2/Smad signal transduction. BioMed. Res. Int. 2022, 2022, 2938015. [Google Scholar] [CrossRef] [PubMed]
- Lambi, A.G.; Harris, M.Y.; Amin, M.; Joiner, P.G.; A Hilliard, B.; Assari, S.; Popoff, S.N.; Barbe, M.F. Blocking CCN2 reduces established bone loss induced by prolonged intense loading by increasing osteoblast activity in rats. JBMR Plus 2023, 7, e10783. [Google Scholar] [CrossRef]
- Ohta, K.; Aoyama, E.; Ahmad, S.A.I.; Ito, N.; Anam, M.B.; Kubota, S.; Takigawa, M. CCN2/CTGF binds the small leucine rich proteoglycan protein Tsukushi. J. Cell Commun. Signal. 2019, 13, 113–118. [Google Scholar] [CrossRef]
- Hoshijima, M.; Hattori, T.; Aoyama, E.; Nishida, T.; Kubota, S.; Kamioka, H.; Takigawa, M. Roles of interaction between CCN2 and Rab14 in aggrecan production by chondrocytes. Int. J. Mol. Sci. 2020, 21, 2769. [Google Scholar] [CrossRef]
- Dillinger, A.E.; Kuespert, S.; Seleem, A.A.; Neuendorf, J.; Schneider, M.; Fuchshofer, R. CCN2/CTGF tip the balance of growth factors towards TGF-β2 in primary open-angle glaucoma. Front. Mol. Biosci. 2023, 10, 1045411. [Google Scholar] [CrossRef]
- Peng, D.; Fu, M.; Wang, M.; Wei, Y.; Wei, X. Targeting TGF-β signal transduction for fibrosis and cancer therapy. Mol. Cancer 2022, 21, 104. [Google Scholar] [CrossRef]
- Abreu, J.G.; Ketpura, N.I.; Reversade, B.; De Robertis, E.M. Connective-tissue growth factor (CTGF) modulates cell signalling by BMP and TGF-β. Nature Cell Biol. 2002, 4, 599–604. [Google Scholar] [CrossRef]
- Hu, H.-H.; Chen, D.-Q.; Wang, Y.-N.; Feng, Y.-L.; Cao, G.; Vaziri, N.D.; Zhao, Y.-Y. New insights into TGF-β/Smad signaling in tissue fibrosis. Chem. Biol. Interact. 2018, 292, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.Q.; Roestenberg, P.; van Nieuwenhoven, F.A.; Bovenschen, N.; Li, Z.; Xu, L.; Oliver, N.; Aten, J.; Joles, J.A.; Vial, C.; et al. CTGF inhibits BMP-7 signaling in diabetic nephropathy. J. Am. Soc. Nephrol. 2008, 19, 2098–2107. [Google Scholar] [CrossRef]
- Mundy, C.; Gannon, M.; Popoff, S.N. Connective tissue growth factor (CTGF/CCN2) negatively regulates BMP-2 induced osteoblast differentiation and signaling. J. Cell. Physiol. 2014, 229, 672–681. [Google Scholar] [CrossRef]
- Aoyama, E.; Hattori, T.; Hoshijima, M.; Araki, D.; Nishida, T.; Kubota, S.; Takigawa, M. N-terminal domains of CCN family 2/connective tissue growth factor bind to aggrecan. Biochem. J. 2009, 420, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Qin, Z.; Fisher, G.J.; Quan, T. Cysteine-rich Protein 61 (CCN1) Domain-specific stimulation of matrix metalloproteinase-1 expression through αVβ3 integrin in human skin fibroblasts. J. Biol. Chem. 2013, 288, 12386–12394. [Google Scholar] [CrossRef]
- Dawson, D.W.; Pearce, S.F.A.; Zhong, R.; Silverstein, R.L.; Frazier, W.A.; Bouck, N.P. CD36 mediates the in vitro inhibitory effects of thrombospondin-1 on endothelial cells. J. Cell Biol. 1997, 138, 707–717. [Google Scholar] [CrossRef]
- Bornstein, P. Thrombospondins as matricellular modulators of cell function. J. Clin. Investig. 2001, 107, 929–934. [Google Scholar] [CrossRef]
- Inoki, I.; Shiomi, T.; Hashimoto, G.; Enomoto, H.; Nakamura, H.; Makino, K.-I.; Ikeda, E.; Takata, S.; Kobayashi, K.-I.; Okada, Y. Connective tissue growth factor binds vascular endothelial growth factor (VEGF) and inhibits VEGF-induced angiogenesis. FASEB J. 2002, 16, 219–221. [Google Scholar] [CrossRef]
- Choi, W.; Nensel, A.K.; Droho, S.; Fattah, M.A.; Mokashi-Punekar, S.; Swygart, D.I.; Burton, S.T.; Schwartz, G.W.; Lavine, J.A.; Gianneschi, N.C. Thrombospondin-1 proteomimetic polymers exhibit anti-angiogenic activity in a neovascular age-related macular degeneration mouse model. Sci. Adv. 2023, 9, eadi8534. [Google Scholar] [CrossRef] [PubMed]
- Pi, L.; Sun, C.; Jn-Simon, N.; Basha, S.; Thomas, H.; Figueroa, V.; Zarrinpar, A.; Cao, Q.; Petersen, B. CCN2/CTGF promotes liver fibrosis through crosstalk with the Slit2/Robo signaling. J. Cell Commun. Signal. 2023, 17, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Yang, Z.; Wang, X.; Jiao, Y.; Xie, X.; Lin, J.; Zhang, H.; Han, J.; Jiang, K.; Ye, Q. Suppression of estrogen receptor transcriptional activity by connective tissue growth factor. PLoS ONE 2011, 6, e20028. [Google Scholar] [CrossRef] [PubMed]
- Gao, R.; Brigstock, D.R. A novel integrin 5 1 binding domain in module 4 of connective tissue growth factor (CCN2/CTGF) promotes adhesion and migration of activated pancreatic stellate cells. Gut 2006, 55, 856–862. [Google Scholar] [CrossRef]
- Yoshida, K.; Munakata, H. Connective tissue growth factor binds to fibronectin through the type I repeat modules and enhances the affinity of fibronectin to fibrin. Biochim. Biophys. Acta 2007, 1770, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Pi, L.; Ding, X.; Jorgensen, M.; Pan, J.-J.; Oh, S.-H.; Pintilie, D.; Brown, A.; Song, W.-Y.; Petersen, B.E. Connective tissue growth factor with a novel fibronectin binding site promotes cell adhesion and migration during rat oval cell activation. Hepatology 2008, 47, 996–1004. [Google Scholar] [CrossRef] [PubMed]
- Surmann-Schmitt, C.; Sasaki, T.; Hattori, T.; Eitzinger, N.; Schett, G.; von der Mark, K.; Stock, M. The Wnt antagonist Wif-1 interacts with CTGF and inhibits CTGF activity. J. Cell. Physiol. 2012, 227, 2207–2216. [Google Scholar] [CrossRef]
- Mercurio, S.; Latinkic, B.; Itasaki, N.; Krumlauf, R.; Smith, J.C. Connective-tissue growth factor modulates WNT signalling and interacts with the WNT receptor complex. Development 2004, 131, 2137–2147. [Google Scholar] [CrossRef]
- Ohkawara, B.; Kobayakawa, A.; Kanbara, S.; Hattori, T.; Kubota, S.; Ito, M.; Masuda, A.; Takigawa, M.; Lyons, K.M.; Ishiguro, N.; et al. CTGF/CCN2 facilitates LRP4-mediated formation of the embryonic neuromuscular junction. Embo Rep. 2020, 21, e48462. [Google Scholar] [CrossRef]
- Ohkawara, B.; Ito, M.; Ohno, K. Secreted signaling molecules at the neuromuscular junction in physiology and pathology. Int. J. Mol. Sci. 2021, 22, 2455. [Google Scholar] [CrossRef]
- Xu, J.; Xu, X.; Jiang, L.; Dua, K.; Hansbro, P.M.; Liu, G. SARS-CoV-2 induces transcriptional signatures in human lung epithelial cells that promote lung fibrosis. Respir. Res. 2020, 21, 182. [Google Scholar] [CrossRef] [PubMed]
- Dolivo, D.; Weathers, P.; Dominko, T. Artemisinin and artemisinin derivatives as anti-fibrotic therapeutics. Acta Pharm. Sin. B 2021, 11, 322–339. [Google Scholar] [CrossRef] [PubMed]
- Richeldi, L.; Pérez, E.R.F.; Costabel, U.; Albera, C.; Lederer, D.J.; Flaherty, K.R.; Ettinger, N.; Perez, R.; Scholand, M.B.; Goldin, J.; et al. Pamrevlumab, an anti-connective tissue growth factor therapy, for idiopathic pulmonary fibrosis (praise): A phase 2, randomised, double-blind, placebo-controlled trial. Lancet Respir. Med. 2020, 8, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Kok, H.M.; Falke, L.L.; Goldschmeding, R.; Nguyen, T.Q. Targeting CTGF, EGF and PDGF pathways to prevent progression of kidney disease. Nat. Rev. Nephrol. 2014, 10, 700–711. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.-M.; Kim, B.; Lee, S.-M.; Han, J.; Bae, H.-S.; Han, S.-B.; Lee, D.; Ham, I.-H.; Hur, H.; Kim, E.; et al. Characterization of gastric cancer-stimulated signaling pathways and function of CTGF in cancer-associated fibroblasts. Cell Commun. Signal. 2024, 22, 8. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.S.; Madala, S.K.; Ramalingam, T.R.; Gochuico, B.R.; Rosas, I.O.; Cheever, A.W.; Wynn, T.A. Bleomycin and IL-1β–mediated pulmonary fibrosis is IL-17A dependent. J. Exp. Med. 2010, 207, 535–552. [Google Scholar] [CrossRef] [PubMed]
- Wree, A.; McGeough, M.D.; Inzaugarat, M.E.; Eguchi, A.; Schuster, S.; Johnson, C.D.; Peña, C.A.; Geisler, L.J.; Papouchado, B.G.; Hoffman, H.M.; et al. NLRP3 inflammasome driven liver injury and fibrosis: Roles of IL-17 and TNF in mice. Hepatology 2018, 67, 736–749. [Google Scholar] [CrossRef] [PubMed]
- Henderson, N.C.; Rieder, F.; Wynn, T.A. Fibrosis: From mechanisms to medicines. Nature 2020, 587, 555–566. [Google Scholar] [CrossRef]
- Mahdy, M.A.A. Skeletal muscle fibrosis: An overview. Cell Tissue Res. 2019, 375, 575–588. [Google Scholar] [CrossRef]
- Wynn, T.A.; Ramalingam, T.R. Mechanisms of fibrosis: Therapeutic translation for fibrotic disease. Nat. Med. 2012, 18, 1028–1040. [Google Scholar] [CrossRef]
- Toda, N.; Mukoyama, M.; Yanagita, M.; Yokoi, H. CTGF in kidney fibrosis and glomerulonephritis. Inflamm. Regen. 2018, 38, 14. [Google Scholar] [CrossRef] [PubMed]
- Bickelhaupt, S.; Erbel, C.; Timke, C.; Wirkner, U.; Dadrich, M.; Flechsig, P.; Tietz, A.; Pföhler, J.; Gross, W.; Peschke, P.; et al. Effects of CTGF blockade on attenuation and reversal of radiation-induced pulmonary fibrosis. J. Natl. Cancer Inst. 2017, 109. [Google Scholar] [CrossRef] [PubMed]
- Yin, Q.; Liu, H. Connective tissue growth factor and renal fibrosis. Adv. Exp. Med. Biol. 2019, 1165, 365–380. [Google Scholar] [CrossRef] [PubMed]
- Kodama, T.; Takehara, T.; Hikita, H.; Shimizu, S.; Shigekawa, M.; Tsunematsu, H.; Li, W.; Miyagi, T.; Hosui, A.; Tatsumi, T.; et al. Increases in p53 expression induce CTGF synthesis by mouse and human hepatocytes and result in liver fibrosis in mice. J. Clin. Investig. 2011, 121, 3343–3356. [Google Scholar] [CrossRef] [PubMed]
- Davidson, E.N.B.; Vitters, E.L.; Mooren, F.M.; Oliver, N.; Berg, W.B.V.D.; van der Kraan, P.M. Connective tissue growth factor/CCN2 overexpression in mouse synovial lining results in transient fibrosis and cartilage damage. Arthritis Rheum. 2006, 54, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Li, W.; Song, C.; Leng, H. CTGF as a multifunctional molecule for cartilage and a potential drug for osteoarthritis. Front. Endocrinol. 2022, 13, 1040526. [Google Scholar] [CrossRef] [PubMed]
- Duan, D.; Goemans, N.; Takeda, S.; Mercuri, E.; Aartsma-Rus, A. Duchenne muscular dystrophy. Nat. Rev. Dis. Primers 2021, 7, 13. [Google Scholar] [CrossRef] [PubMed]
- Raghu, G.; Scholand, M.B.; de Andrade, J.; Lancaster, L.; Mageto, Y.; Goldin, J.; Brown, K.K.; Flaherty, K.R.; Wencel, M.; Wanger, J.; et al. FG-3019 anti-connective tissue growth factor monoclonal antibody: Results of an open-label clinical trial in idiopathic pulmonary fibrosis. Eur. Respir. J. 2016, 47, 1481–1491. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Ni, J.; Beretov, J.; Graham, P.; Li, Y. Triple-negative breast cancer therapeutic resistance: Where is the Achilles’ heel? Cancer Lett. 2021, 497, 100–111. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, J.; Kim, H.S.; Kang, Y.J. Unraveling connective tissue growth factor as a therapeutic target and assessing kahweol as a potential drug candidate in triple-negative breast cancer treatment. Int. J. Mol. Sci. 2023, 24, 16307. [Google Scholar] [CrossRef]
- Kim, H.; Son, S.; Ko, Y.; Shin, I. CTGF regulates cell proliferation, migration, and glucose metabolism through activation of FAK signaling in triple-negative breast cancer. Oncogene 2021, 40, 2667–2681. [Google Scholar] [CrossRef]
- Rumpold, H.; Niedersüß-Beke, D.; Heiler, C.; Falch, D.; Wundsam, H.V.; Metz-Gercek, S.; Piringer, G.; Thaler, J. Prediction of mortality in metastatic colorectal cancer in a real-life population: A multicenter explorative analysis. BMC Cancer 2020, 20, 1149. [Google Scholar] [CrossRef] [PubMed]
- Pastushenko, I.; Brisebarre, A.; Sifrim, A.; Fioramonti, M.; Revenco, T.; Boumahdi, S.; Van Keymeulen, A.; Brown, D.; Moers, V.; Lemaire, S.; et al. Identification of the tumour transition states occurring during EMT. Nature 2018, 556, 463–468. [Google Scholar] [CrossRef]
- Shin, A.E.; Giancotti, F.G.; Rustgi, A.K. Metastatic colorectal cancer: Mechanisms and emerging therapeutics. Trends Pharmacol. Sci. 2023, 44, 222–236. [Google Scholar] [CrossRef]
- Zhu, X.; Zhong, J.; Zhao, Z.; Sheng, J.; Wang, J.; Liu, J.; Cui, K.; Chang, J.; Zhao, H.; Wong, S. Epithelial derived CTGF promotes breast tumor progression via inducing EMT and collagen I fibers deposition. Oncotarget 2015, 6, 25320–25338. [Google Scholar] [CrossRef]
- Lun, W.; Wu, X.; Deng, Q.; Zhi, F. MiR-218 regulates epithelial–mesenchymal transition and angiogenesis in colorectal cancer via targeting CTGF. Cancer Cell Int. 2018, 18, 83. [Google Scholar] [CrossRef]
- Li, J.; Gao, X.; Ji, K.; Sanders, A.J.; Zhang, Z.; Jiang, W.G.; Ji, J.; Ye, L. Differential expression of CCN family members CYR611, CTGF and NOV in gastric cancer and their association with disease progression. Oncol. Rep. 2016, 36, 2517–2525. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.Y.; Wu, M.S.; Hua, K.T.; Kuo, M.L.; Lin, M.T. Cyr61/CTGF/Nov family proteins in gastric carcinogenesis. World J. Gastroenterol. 2014, 20, 1694–1700. [Google Scholar] [CrossRef]
- Jiang, C.-G.; Lv, L.; Liu, F.-R.; Wang, Z.-N.; Li, Y.-S.; Wang, C.-Y.; Zhang, H.-Y.; Sun, Z.; Xu, H.-M. Downregulation of connective tissue growth factor inhibits the growth and invasion of gastric cancer cells and attenuates peritoneal dissemination. Mol. Cancer 2011, 10, 122. [Google Scholar] [CrossRef]
- Yang, K.; Gao, K.; Hu, G.; Wen, Y.; Lin, C.; Li, X. CTGF enhances resistance to 5-FU-mediating cell apoptosis through FAK/MEK/ERK signal pathway in colorectal cancer. OncoTargets Ther. 2016, 9, 7285–7295. [Google Scholar] [CrossRef]
- Teoh, J.Y.-C.; Huang, J.; Ko, W.Y.-K.; Lok, V.; Choi, P.; Ng, C.-F.; Sengupta, S.; Mostafid, H.; Kamat, A.M.; Black, P.C.; et al. Global trends of bladder cancer incidence and mortality, and their associations with tobacco use and gross domestic product per capita. Eur. Urol. 2020, 78, 893–906. [Google Scholar] [CrossRef]
- Yang, Y.; Yang, Y.; Yang, J.; Zhao, X.; Wei, X. Tumor microenvironment in ovarian cancer: Function and therapeutic strategy. Front. Cell Dev. Biol. 2020, 8, 758. [Google Scholar] [CrossRef]
- Liang, T.; Tao, T.; Wu, K.; Liu, L.; Xu, W.; Zhou, D.; Fang, H.; Ding, Q.; Huang, G.; Wu, S. Cancer-associated fibroblast-induced remodeling of tumor microenvironment in recurrent bladder cancer. Adv. Sci. 2023, 10, e2303230. [Google Scholar] [CrossRef]
- Gonzalez, D.; Brandan, E. CTGF/CCN2 from skeletal muscle to nervous system: Impact on neurodegenerative diseases. Mol. Neurobiol. 2019, 56, 5911–5916. [Google Scholar] [CrossRef]
- Dugger, B.N.; Dickson, D.W. Pathology of neurodegenerative diseases. Cold Spring Harb. Perspect. Biol. 2017, 9, a028035. [Google Scholar] [CrossRef] [PubMed]
- Vaquer-Alicea, J.; Diamond, M.I. Propagation of protein aggregation in neurodegenerative diseases. Annu. Rev. Biochem. 2019, 88, 785–810. [Google Scholar] [CrossRef]
- Mann, A.P.; Scodeller, P.; Hussain, S.; Braun, G.B.; Mölder, T.; Toome, K.; Ambasudhan, R.; Teesalu, T.; Lipton, S.A.; Ruoslahti, E. Identification of a peptide recognizing cerebrovascular changes in mouse models of Alzheimer’s disease. Nat. Commun. 2017, 8, 1403. [Google Scholar] [CrossRef] [PubMed]
- Lo, A.C.; Callaerts-Vegh, Z.; Nunes, A.F.; Rodrigues, C.M.; D’Hooge, R. Tauroursodeoxycholic acid (TUDCA) supplementation prevents cognitive impairment and amyloid deposition in APP/PS1 mice. Neurobiol. Dis. 2013, 50, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Chen, S.; He, Y.; Zhang, D.; Zou, S.; Xie, J.; Zhou, C. Connective tissue growth factor promotes cell-to-cell communication in human periodontal ligament stem cells via MAPK and PI3K pathway. J. Periodontol. 2022, 93, E60–E72. [Google Scholar] [CrossRef]
- Temple, S. Advancing cell therapy for neurodegenerative diseases. Cell Stem Cell 2023, 30, 512–529. [Google Scholar] [CrossRef]
- McClain, J.A.; Phillips, L.L.; Fillmore, H.L. Increased MMP-3 and CTGF expression during lipopolysaccharide-induced dopaminergic neurodegeneration. Neurosci. Lett. 2009, 460, 27–31. [Google Scholar] [CrossRef]
- Feldman, E.L.; A Goutman, S.; Petri, S.; Mazzini, L.; Savelieff, M.G.; Shaw, P.J.; Sobue, G. Amyotrophic lateral sclerosis. Lancet 2022, 400, 1363–1380. [Google Scholar] [CrossRef] [PubMed]
- Hardiman, O.; Al-Chalabi, A.; Chio, A.; Corr, E.M.; Logroscino, G.; Robberecht, W.; Shaw, P.J.; Simmons, Z.; van den Berg, L.H. Amyotrophic lateral sclerosis. Nat. Rev. Dis. Primers 2017, 3, 17071. [Google Scholar] [CrossRef]
- Gonzalez, D.; Rebolledo, D.L.; Correa, L.M.; A Court, F.; Cerpa, W.; E Lipson, K.; van Zundert, B.; Brandan, E. The inhibition of CTGF/CCN2 activity improves muscle and locomotor function in a murine ALS model. Hum. Mol. Genet. 2018, 27, 2913–2926. [Google Scholar] [CrossRef]
- Jadhav, V.; Luo, Q.; Dominguez, J.M.; Al-Sabah, J.; Chaqour, B.; Grant, M.B.; Bhatwadekar, A.D. Per2-mediated vascular dysfunction is caused by the upregulation of the connective tissue growth factor (CTGF). PLoS ONE 2016, 11, e0163367. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, A.; Che, R.C.; Zhang, A.H. Role of aldosterone in renal fibrosis. Adv. Exp. Med. Biol. 2019, 1165, 325–346. [Google Scholar] [CrossRef]
- Kuiper, E.J.; van Zijderveld, R.; Roestenberg, P.; Lyons, K.M.; Goldschmeding, R.; Klaassen, I.; Van Noorden, C.J.F.; Schlingemann, R.O. Connective tissue growth factor is necessary for retinal capillary basal lamina thickening in diabetic mice. J. Histochem. Cytochem. 2008, 56, 785–792. [Google Scholar] [CrossRef]
- Van Geest, R.J.; Leeuwis, J.W.; Dendooven, A.; Pfister, F.; Bosch, K.; Hoeben, K.A.; Vogels, I.M.; Van der Giezen, D.M.; Dietrich, N.; Hammes, H.-P.; et al. Connective tissue growth factor is involved in structural retinal vascular changes in long-term experimental diabetes. J. Histochem. Cytochem. 2014, 62, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Nasser, S.; Yee, M.; Graves, D.T.; Roy, S. A long-term sirna strategy regulates fibronectin overexpression and improves vascular lesions in retinas of diabetic rats. Mol. Vis. 2011, 17, 3166–3174. [Google Scholar]
- Daniel, E.; Toth, C.A.; Grunwald, J.E.; Jaffe, G.J.; Martin, D.F.; Fine, S.L.; Huang, J.; Ying, G.-S.; Hagstrom, S.A.; Winter, K.; et al. Risk of scar in the comparison of age-related macular degeneration treatments trials. Ophthalmology 2014, 121, 656–666. [Google Scholar] [CrossRef]
- Van Geest, R.J.; Klaassen, I.; Lesnik-Oberstein, S.Y.; Tan, H.S.; Mura, M.; Goldschmeding, R.; Van Noorden, C.J.F.; Schlingemann, R.O. Vitreous TIMP-1 levels associate with neovascularization and TGF-β2 levels but not with fibrosis in the clinical course of proliferative diabetic retinopathy. J. Cell Commun. Signal. 2013, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Dong, L.-J.; Du, X.-L.; Niu, R.; Hu, B.-J. Research progress on the role of connective tissue growth factor in fibrosis of diabetic retinopathy. Int. J. Ophthalmol. 2018, 11, 1550–1554. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.S.; Mander, S.; Hussein, K.A.; Elsherbiny, N.M.; Smith, S.B.; Al-Shabrawey, M.; Tawfik, A. Hyperhomocysteinemia disrupts retinal pigment epithelial structure and function with features of age-related macular degeneration. Oncotarget 2016, 7, 8532–8545. [Google Scholar] [CrossRef] [PubMed]
- Radeke, M.J.; Radeke, C.M.; Shih, Y.-H.; Hu, J.; Bok, D.; Johnson, L.V.; Coffey, P.J. Restoration of mesenchymal retinal pigmented epithelial cells by TGFβ pathway inhibitors: Implications for age-related macular degeneration. Genome Med. 2015, 7, 58. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Jiang, N.; Zhang, Y.; Ye, S.; Liang, X.; Wang, X.; Lin, X.; Zong, R.; Chen, H.; Liu, Z. Fenofibrate inhibits subretinal fibrosis through suppressing TGF-β—Smad2/3 signaling and Wnt signaling in neovascular age-related macular degeneration. Front. Pharmacol. 2020, 11, 580884. [Google Scholar] [CrossRef] [PubMed]
- Yeung, V.; Boychev, N.; Farhat, W.; Ntentakis, D.P.; Hutcheon, A.E.K.; Ross, A.E.; Ciolino, J.B. Extracellular vesicles in corneal fibrosis/scarring. Int. J. Mol. Sci. 2022, 23, 5921. [Google Scholar] [CrossRef] [PubMed]
- Klaassen, I.; van Geest, R.J.; Kuiper, E.J.; van Noorden, C.J.; Schlingemann, R.O. The role of CTGF in diabetic retinopathy. Exp. Eye Res. 2015, 133, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Jayaram, H.; Kolko, M.; Friedman, D.S.; Gazzard, G. Glaucoma: Now and beyond. Lancet 2023, 402, 1788–1801. [Google Scholar] [CrossRef] [PubMed]
- Browne, J.G.; Ho, S.L.; Kane, R.; Oliver, N.; Clark, A.F.; O’Brien, C.J.; Crean, J.K. Connective tissue growth factor is increased in pseudoexfoliation glaucoma. Investig. Opthalmology Vis. Sci. 2011, 52, 3660–3666. [Google Scholar] [CrossRef]
- Weinreb, R.N.; Aung, T.; Medeiros, F.A. The Pathophysiology and treatment of glaucoma: A review. JAMA 2014, 311, 1901–1911. [Google Scholar] [CrossRef]
- Mallone, F.; Costi, R.; Marenco, M.; Plateroti, R.; Minni, A.; Attanasio, G.; Artico, M.; Lambiase, A. Understanding drivers of ocular fibrosis: Current and future therapeutic perspectives. Int. J. Mol. Sci. 2021, 22, 11748. [Google Scholar] [CrossRef]
- Wang, Y.; Chang, T.; Wu, T.; Ye, W.; Wang, Y.; Dou, G.; Du, H.; Hui, Y.; Guo, C. Connective tissue growth factor promotes retinal pigment epithelium mesenchymal transition via the PI3K/AKT signaling pathway. Mol. Med. Rep. 2021, 23, 389. [Google Scholar] [CrossRef]
- Dobaczewski, M.; Bujak, M.; Li, N.; Gonzalez-Quesada, C.; Mendoza, L.H.; Wang, X.-F.; Frangogiannis, N.G. Smad3 signaling critically regulates fibroblast phenotype and function in healing myocardial infarction. Circ. Res. 2010, 107, 418–428. [Google Scholar] [CrossRef]
- Ungvari, Z.; Valcarcel-Ares, M.N.; Tarantini, S.; Yabluchanskiy, A.; Fülöp, G.A.; Kiss, T.; Csiszar, A. Connective tissue growth factor (CTGF) in age-related vascular pathologies. GeroScience 2017, 39, 491–498. [Google Scholar] [CrossRef]
- Wang, W.-B.; Li, H.-P.; Yan, J.; Zhuang, F.; Bao, M.; Liu, J.-T.; Qi, Y.-X.; Han, Y. CTGF regulates cyclic stretch-induced vascular smooth muscle cell proliferation via microrna-19b-3p. Exp. Cell Res. 2019, 376, 77–85. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Chen, Z.; Martin, M.; Zhang, J.; Sangwung, P.; Woo, B.; Tremoulet, A.H.; Shimizu, C.; Jain, M.K.; Burns, J.C.; et al. miR-483 Targeting of CTGF suppresses endothelial-to-mesenchymal transition: Therapeutic implications in Kawasaki disease. Circ. Res. 2017, 120, 354–365. [Google Scholar] [CrossRef]
- Zhou, S.; Sun, L.; Cao, C.; Wu, P.; Li, M.; Sun, G.; Fei, G.; Ding, X.; Wang, R. Hypoxia-induced microRNA-26b inhibition contributes to hypoxic pulmonary hypertension via CTGF. J. Cell. Biochem. 2018, 119, 1942–1952. [Google Scholar] [CrossRef] [PubMed]
- Ha, Y.M.; Lee, D.H.; Kim, M.; Kang, Y.J. High glucose induces connective tissue growth factor expression and extracellular matrix accumulation in rat aorta vascular smooth muscle cells via extracellular signal-regulated kinase 1/2. Korean J. Physiol. Pharmacol. 2013, 17, 307–314. [Google Scholar] [CrossRef]
- Hwang, A.-R.; Nam, J.-O.; Kang, Y.J. Fluvastatin inhibits advanced glycation end products-induced proliferation, migration, and extracellular matrix accumulation in vascular smooth muscle cells by targeting connective tissue growth factor. Korean J. Physiol. Pharmacol. 2018, 22, 193–201. [Google Scholar] [CrossRef]
- Libby, P. The changing landscape of atherosclerosis. Nature 2021, 592, 524–533. [Google Scholar] [CrossRef]
- Paredes, F.; Williams, H.C.; Suster, I.; Tejos, M.; Fuentealba, R.; Bogan, B.; Holden, C.M.; Martin, A.S. Metabolic regulation of the proteasome under hypoxia by Poldip2 controls fibrotic signaling in vascular smooth muscle cells. Free Radic. Biol. Med. 2023, 195, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Liu, C.; Cao, B.; Cao, Z.; Zhai, H.; Liu, B.; Jin, S.; Yang, X.; Lv, C.; Wang, J. Connective tissue growth factor-targeting DNA aptamer suppresses pannus formation as diagnostics and therapeutics for rheumatoid arthritis. Front. Immunol. 2022, 13, 934061. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.J.; Han, J.C.; Park, D.Y.; Cho, J.; Kee, C. Effect of connective tissue growth factor gene editing using adeno-associated virus–mediated CRISPR–Cas9 on rabbit glaucoma filtering surgery outcomes. Gene Ther. 2021, 28, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Song, R.; Li, G.; Li, S. Aspidin PB, a novel natural anti-fibrotic compound, inhibited fibrogenesis in TGF-β1-stimulated keloid fibroblasts via PI-3K/Akt and Smad signaling pathways. Chem. Biol. Interact. 2015, 238, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Shao, S.; Duan, W.; Xu, Q.; Li, X.; Han, L.; Li, W.; Zhang, D.; Wang, Z.; Lei, J. Curcumin suppresses hepatic stellate cell-induced hepatocarcinoma angiogenesis and invasion through downregulating CTGF. Oxidative Med. Cell. Longev. 2019, 2019, 8148510. [Google Scholar] [CrossRef] [PubMed]
- Sakai, N.; Kamimura, K.; Miyamoto, H.; Ko, M.; Nagoya, T.; Setsu, T.; Sakamaki, A.; Yokoo, T.; Kamimura, H.; Soki, H.; et al. Letrozole ameliorates liver fibrosis through the inhibition of the CTGF pathway and 17β-hydroxysteroid dehydrogenase 13 expression. J. Gastroenterol. 2023, 58, 53–68. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, A.G.; Wanjari, U.R.; Nagarajan, D.; Vibhaa, K.K.; Anagha, V.; Chakraborty, R.; Renu, K.; Dey, A.; Vellingiri, B.; Gopalakrishnan, A.V. Letrozole: Pharmacology, toxicity and potential therapeutic effects. Life Sci. 2022, 310, 121074. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Jin, Y.; Gao, Z.; Zeng, Y.; Du, J.; Yan, H.; Chen, X.; Ping, L.; Lin, N.; Yang, B.; et al. Autophagic degradation of CCN2 (cellular communication network factor 2) causes cardiotoxicity of sunitinib. Autophagy 2022, 18, 1152–1173. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Usinger, W.; Nichols, B.; Gray, J.; Xu, L.; Seeley, T.W.; Brenner, M.; Guo, G.; Zhang, W.; Oliver, N.; et al. Cooperative interaction of CTGF and TGF-β in animal models of fibrotic disease. Fibrogenesis Tissue Repair 2011, 4, 4. [Google Scholar] [CrossRef]
- Ramazani, Y.; Knops, N.; Elmonem, M.A.; Nguyen, T.Q.; Arcolino, F.O.; Heuvel, L.v.D.; Levtchenko, E.; Kuypers, D.; Goldschmeding, R. Connective tissue growth factor (CTGF) from basics to clinics. Matrix Biol. 2018, 68-69, 44–66. [Google Scholar] [CrossRef]
- Leask, A. A centralized communication network: Recent insights into the role of the cancer associated fibroblast in the development of drug resistance in tumors. Semin. Cell Dev. Biol. 2020, 101, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Picozzi, V.; Alseidi, A.; Winter, J.; Pishvaian, M.; Mody, K.; Glaspy, J.; Larson, T.; Matrana, M.; Carney, M.; Porter, S.; et al. Gemcitabine/nab-paclitaxel with pamrevlumab: A novel drug combination and trial design for the treatment of locally advanced pancreatic cancer. ESMO Open 2020, 5, e000668. [Google Scholar] [CrossRef] [PubMed]
- Kaplon, H.; Muralidharan, M.; Schneider, Z.; Reichert, J.M. Antibodies to watch in 2020. mAbs 2020, 12, 1703531. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Wu, G.; Jin, J.; Wang, H.; Zhang, J.; Liu, L.; Zhao, H.; Wang, J.; Yang, X. A fully human connective tissue growth factor blocking monoclonal antibody ameliorates experimental rheumatoid arthritis through inhibiting angiogenesis. BMC Biotechnol. 2023, 23, 6. [Google Scholar] [CrossRef] [PubMed]
- Resovi, A.; Borsotti, P.; Ceruti, T.; Passoni, A.; Zucchetti, M.; Berndt, A.; Riser, B.L.; Taraboletti, G.; Belotti, D. CCN-based therapeutic peptides modify pancreatic ductal adenocarcinoma microenvironment and decrease tumor growth in combination with chemotherapy. Cells 2020, 9, 952. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Xiao, J.; Li, J.; Yu, H.; Zhao, Q.; Tang, Q.; Chen, H.; Liu, H.; Wu, K.; Lei, J.; et al. Discovery and design of novel cyclic peptides as specific inhibitors targeting CCN2 and disrupting CCN2/EGFR interaction for kidney fibrosis treatment. J. Med. Chem. 2023, 66, 8251–8266. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Huo, Y.; Tian, H.; Zhang, Q.; Lv, Y.; Hao, Z. In vitro selection and characterization of deoxyribonucleic acid aptamers against connective tissue growth factor. Biochem. Biophys. Res. Commun. 2015, 457, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.; Gentzkow, G.; Berman, G.; Senne, L.; Jewell, M.; Connall, T.P.; Miller, S.R.; Galiano, R.D.; Young, L. Anti-CTGF oligonucleotide reduces severity of postsurgical hypertrophic scars in a randomized, double-blind, within-subject, placebo-controlled study. Plast. Reconstr. Surg. 2018, 142, 192e–201e. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Qu, M.; Li, L.; Liu, T.; Lin, M.; Yu, X. SiRNA in MSC-derived exosomes silences CTGF gene for locomotor recovery in spinal cord injury rats. Stem Cell Res. Ther. 2021, 12, 334. [Google Scholar] [CrossRef]
- Castleberry, S.A.; Golberg, A.; Abu Sharkh, M.; Khan, S.; Almquist, B.D.; Austen, W.G.; Yarmush, M.L.; Hammond, P.T. Nanolayered siRNA delivery platforms for local silencing of CTGF reduce cutaneous scar contraction in third-degree burns. Biomaterials 2016, 95, 22–34. [Google Scholar] [CrossRef]
- Nikam, R.R.; Gore, K.R. Journey of siRNA: Clinical developments and targeted delivery. Nucleic Acid Ther. 2018, 28, 209–224. [Google Scholar] [CrossRef]
- Rinaldi, C.; Wood, M.J.A. Antisense oligonucleotides: The next frontier for treatment of neurological disorders. Nat. Rev. Neurol. 2018, 14, 9–21. [Google Scholar] [CrossRef]
- Ren, M.; Zhou, J.; Song, Z.; Mei, H.; Zhou, M.; Fu, Z.F.; Han, H.; Zhao, L. Aptamer and RVG functionalized gold nanorods for targeted photothermal therapy of neurotropic virus infection in the mouse brain. Chem. Eng. J. 2021, 411, 128557. [Google Scholar] [CrossRef]
- Wang, Y.; Kong, Q.-J.; Sun, J.-C.; Yang, Y.; Wang, H.-B.; Zhang, Q.; Shi, J.-G. Lentivirus-mediated silencing of the CTGF gene suppresses the formation of glial scar tissue in a rat model of spinal cord injury. Spine J. Off. J. N. Am. Spine Soc. 2018, 18, 164–172. [Google Scholar] [CrossRef]
- Bao, H.; Jiang, K.; Meng, K.; Liu, W.; Liu, P.; Du, Y.; Wang, D. TGF-β2 induces proliferation and inhibits apoptosis of human tenon capsule fibroblast by miR-26 and its targeting of CTGF. Biomed. Pharmacother. 2018, 104, 558–565. [Google Scholar] [CrossRef] [PubMed]
- Wei, P.; Xie, Y.; Abel, P.W.; Huang, Y.; Ma, Q.; Li, L.; Hao, J.; Wolff, D.W.; Wei, T.; Tu, Y. Transforming growth factor (TGF)-β1-induced miR-133a inhibits myofibroblast differentiation and pulmonary fibrosis. Cell Death Dis. 2019, 10, 670. [Google Scholar] [CrossRef] [PubMed]
- A Lewis, R.; Levy, B.; Ramirez, N.; Kopczynski, C.C.; Usner, D.W.; Novack, G.D.; PG324-CS201 Study Group. Fixed-dose combination of AR-13324 and latanoprost: A double-masked, 28-day, randomised, controlled study in patients with open-angle glaucoma or ocular hypertension. Br. J. Ophthalmol. 2016, 100, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Kahook, M.Y.; Serle, J.B.; Mah, F.S.; Kim, T.; Raizman, M.B.; Heah, T.; Ramirez-Davis, N.; Kopczynski, C.C.; Usner, D.W.; Novack, G.D. Long-term safety and ocular hypotensive efficacy evaluation of Netarsudil ophthalmic solution: Rho kinase elevated IOP treatment trial (ROCKET-2). Am. J. Ophthalmol. 2019, 200, 130–137. [Google Scholar] [CrossRef]
- Hwang, J.; Chang, C.; Kim, J.H.; Oh, C.T.; Lee, H.N.; Lee, C.; Oh, D.; Lee, C.; Kim, B.; Hong, S.W.; et al. Development of cell-penetrating asymmetric interfering RNA targeting connective tissue growth factor. J. Investig. Dermatol. 2016, 136, 2305–2313. [Google Scholar] [CrossRef]
- Morales, M.G.; Gutierrez, J.; Cabello-Verrugio, C.; Cabrera, D.; Lipson, K.E.; Goldschmeding, R.; Brandan, E. Reducing CTGF/CCN2 slows down mdx muscle dystrophy and improves cell therapy. Hum. Mol. Genet. 2013, 22, 4938–4951. [Google Scholar] [CrossRef]
- Wang, T.; Zhang, Y.; Chi, M.; Zhao, C.; Cao, L.; Tian, C.; Kamei, K.; Zheng, Y.; Jiang, Q. A novel fixed-combination timolol-netarsudil-latanoprost ophthalmic solution for the treatment of glaucoma and ocular hypertension. Asian J. Pharm. Sci. 2022, 17, 938–948. [Google Scholar] [CrossRef] [PubMed]
- Guglieri, M.; Clemens, P.R.; Perlman, S.J.; Smith, E.C.; Horrocks, I.; Finkel, R.S.; Mah, J.K.; Deconinck, N.; Goemans, N.; Haberlova, J.; et al. Efficacy and safety of vamorolone vs. placebo and prednisone among boys with duchenne muscular dystrophy: A randomized clinical trial. JAMA Neurol. 2022, 79, 1005–1014. [Google Scholar] [CrossRef] [PubMed]
- Li, D.-Y.; Li, R.-F.; Sun, D.-X.; Pu, D.-D.; Zhang, Y.-H. Mesenchymal stem cell therapy in pulmonary fibrosis: A meta-analysis of preclinical studies. Stem Cell Res. Ther. 2021, 12, 461. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Zeng, Y.; Wang, D. Stem cell-based therapy for pulmonary fibrosis. Stem Cell Res. Ther. 2022, 13, 492. [Google Scholar] [CrossRef] [PubMed]
- Eom, Y.W.; Shim, K.Y.; Baik, S.K. Mesenchymal stem cell therapy for liver fibrosis. Korean J. Intern. Med. 2015, 30, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Huang, B.; Jin, T.; Ocansey, D.K.W.; Jiang, J.; Mao, F. Intestinal fibrosis in inflammatory bowel disease and the prospects of mesenchymal stem cell therapy. Front. Immunol. 2022, 13, 835005. [Google Scholar] [CrossRef] [PubMed]
- Cushnie, T.P.T.; Cushnie, B.; Echeverría, J.; Fowsantear, W.; Thammawat, S.; Dodgson, J.L.; Law, S.; Clow, S.M. Bioprospecting for antibacterial drugs: A multidisciplinary perspective on natural product source material, bioassay selection and avoidable pitfalls. Pharm. Res. 2020, 37, 125. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Song, J.; Kong, L.; Yuan, T.; Li, W.; Zhang, W.; Hou, B.; Lu, Y.; Du, G. The strategies and techniques of drug discovery from natural products. Pharmacol. Ther. 2020, 216, 107686. [Google Scholar] [CrossRef]
- Kumar, A.; Jaitak, V. Natural products as multidrug resistance modulators in cancer. Eur. J. Med. Chem. 2019, 176, 268–291. [Google Scholar] [CrossRef]
- Shanmuganathan, S.; Angayarkanni, N. Chebulagic acid and Chebulinic acid inhibit TGF-β1 induced fibrotic changes in the chorio-retinal endothelial cells by inhibiting ERK phosphorylation. Microvasc. Res. 2019, 121, 14–23. [Google Scholar] [CrossRef]
- Xu, L.; Gao, J.; Huang, D.; Lin, P.; Yao, D.; Yang, F.; Zhang, Y.; Yang, X.; Wu, M.; Ye, C. Emodin ameliorates tubulointerstitial fibrosis in obstructed kidneys by inhibiting EZH2. Biochem. Biophys. Res. Commun. 2021, 534, 279–285. [Google Scholar] [CrossRef]
- Eraky, S.M.; El-Mesery, M.; El-Karef, A.; Eissa, L.A.; El-Gayar, A.M. Silymarin and caffeine combination ameliorates experimentally-induced hepatic fibrosis through down-regulation of LPAR1 expression. Biomed. Pharmacother. 2018, 101, 49–57. [Google Scholar] [CrossRef]
- Yang, F.; Luo, L.; Zhu, Z.-D.; Zhou, X.; Wang, Y.; Xue, J.; Zhang, J.; Cai, X.; Chen, Z.-L.; Ma, Q.; et al. Chlorogenic acid inhibits liver fibrosis by blocking the miR-21-regulated TGF-β1/Smad7 signaling pathway in vitro and in vivo. Front. Pharmacol. 2017, 8, 929. [Google Scholar] [CrossRef]
- Libertine, L.; Pavco, P.; Young, V.L.; Paz, N.G.; Hunstad, J.; Cauwenbergh, G. Update on phase 2 clinical trial results of RXI-109 treatment to reduce the formation of hypertrophic dermal scars. J. Am. Acad. Dermatol. 2015, 72, AB273. [Google Scholar]
- Rana, A.; Singh, T.U.; Sharma, M.; Gari, M.; Kumar, T.; Parida, S.; Lingaraju, M.C.; Mariappan, A.K.; Kumar, A.; Kumar, D. Pravastatin attenuates isoprenaline induced cardiac fibrosis in a mouse model. Biotech. Histochem. 2023, 98, 567–577. [Google Scholar] [CrossRef]
- Neiens, V.; Pavlidou, M.; Wurzenberger, C.; Hansbauer, E.-M.; Gruener, S.; Peper-Gabriel, J.; Heinig, K.; Jaquin, T.; Konitsiotis, A.; Morgenstern, J.; et al. PRS-220, a novel inhalable therapeutic intervention for IPF, targeting CTGF directly in the lung. Am. J. Respir. Crit. Care Med. 2002, 1, 205. [Google Scholar]
- Stolz, J.; Alm, A. Latanoprost in the treatment of glaucoma. Clin. Ophthalmol. 2014, 8, 1967–1985. [Google Scholar] [CrossRef]
- Rebolledo, D.L.; González, D.; Faundez-Contreras, J.; Contreras, O.; Vio, C.P.; Murphy-Ullrich, J.E.; Lipson, K.E.; Brandan, E. Denervation-induced skeletal muscle fibrosis is mediated by CTGF/CCN2 independently of TGF-β. Matrix Biol. 2019, 82, 20–37. [Google Scholar] [CrossRef]
- Wan, L.-Y.; Yuan, W.-F.; Ai, W.-B.; Ai, Y.-W.; Wang, J.-J.; Chu, L.-Y.; Zhang, Y.-Q.; Wu, J.-F. An exploration of aptamer internalization mechanisms and their applications in drug delivery. Expert Opin. Drug Deliv. 2019, 16, 207–218. [Google Scholar] [CrossRef]
- Liu, Y.; Qian, X.; Ran, C.; Li, L.; Fu, T.; Su, D.; Xie, S.; Tan, W. Aptamer-based targeted protein degradation. ACS Nano 2023, 17, 6150–6164. [Google Scholar] [CrossRef]
- Leask, A. Potential Therapeutic Targets for Cardiac Fibrosis: TGFbeta, angiotensin, endothelin, CCN2, and PDGF, partners in fibroblast activation. Circ. Res. 2010, 106, 1675–1680. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, A.; Cunningham, J.L. Connective tissue growth factor in tumor pathogenesis. Fibrogenesis Tissue Repair 2012, 5, S8. [Google Scholar] [CrossRef] [PubMed]
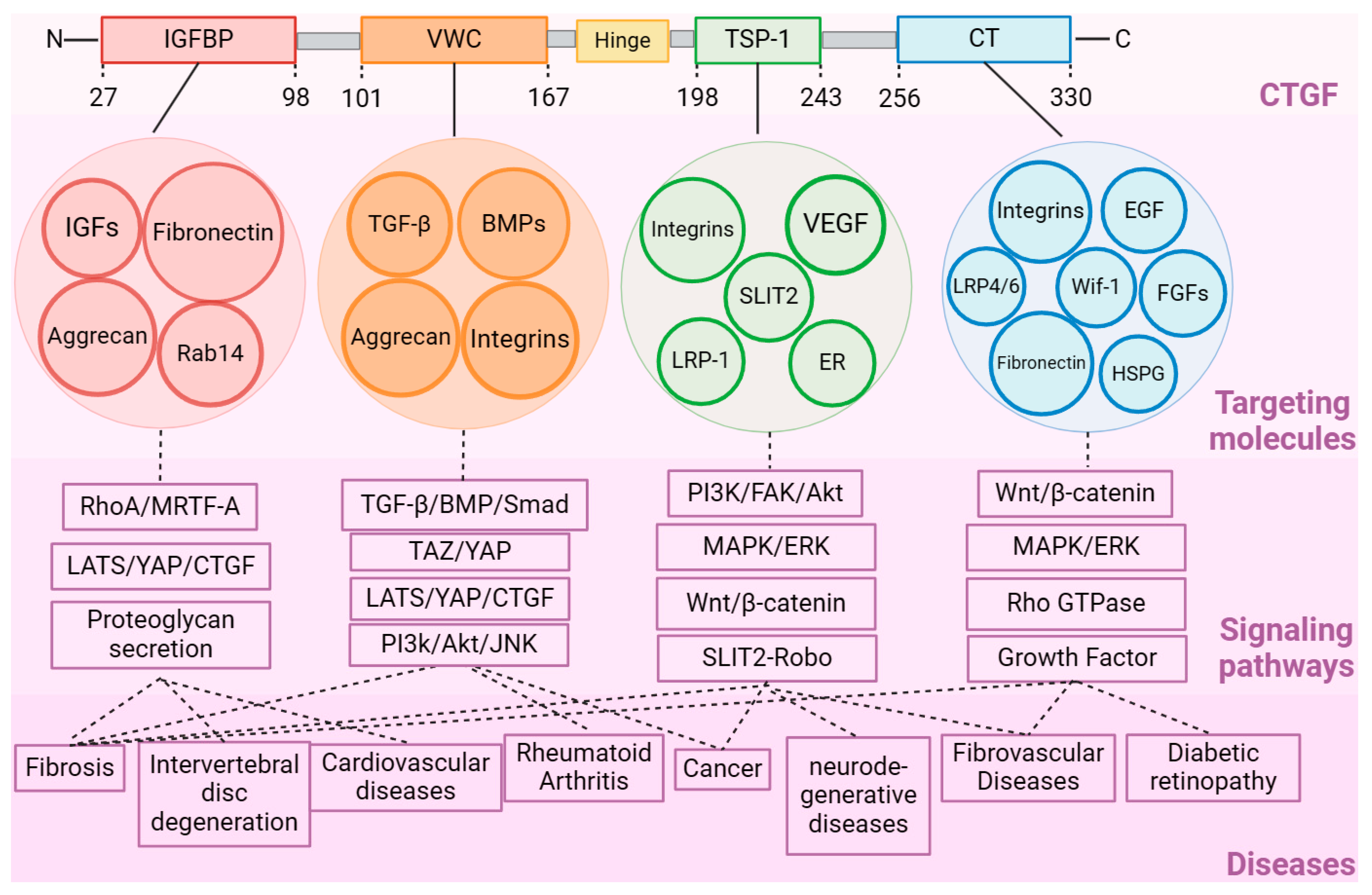
| Domains of CTGF | Targeting Molecules | Related Downstream Pathways of Targeted Molecules | Related Diseases Regulated by the Signaling Pathways |
|---|---|---|---|
| IGFBP | IGFs Fibronectin Aggrecan Rab14 | RhoA/MRTF-A LATS/YAP/CTGF Proteoglycan secretion | Tissue fibrosis Intervertebral disc degeneration |
| VWC | TGF-β BMPs Integrins Aggrecan | TGF-β/BMP/Smad TAZ/YAP LATS/YAP/CTGF PI3k/Akt/JNK | Tissue fibrosis Rheumatoid Arthritis Cancer |
| TSP-1 | Integrin α3β1 Integrin α3β3 VEGF LRP-1 SLIT2 ER | PI3K/FAK/Akt MAPK/ERK Wnt/β-catenin SLIT2-Robo | Fibrosis Breast Cancer Alzheimer’s Disease Fibrovascular Diseases |
| CT | Wif-1 EGF FGFs Integrin α5β1 Integrin α5β3 LRP-4/6 Fibronectin HSPG | Wnt/β-catenin MAPK/ERK Rho GTPase Signaling Growth Factor Signaling | Fibrosis Abnormal blood vessel growth Diabetic retinopathy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ren, M.; Yao, S.; Chen, T.; Luo, H.; Tao, X.; Jiang, H.; Yang, X.; Zhang, H.; Yu, S.; Wang, Y.; et al. Connective Tissue Growth Factor: Regulation, Diseases, and Drug Discovery. Int. J. Mol. Sci. 2024, 25, 4692. https://doi.org/10.3390/ijms25094692
Ren M, Yao S, Chen T, Luo H, Tao X, Jiang H, Yang X, Zhang H, Yu S, Wang Y, et al. Connective Tissue Growth Factor: Regulation, Diseases, and Drug Discovery. International Journal of Molecular Sciences. 2024; 25(9):4692. https://doi.org/10.3390/ijms25094692
Chicago/Turabian StyleRen, Meishen, Shanshan Yao, Tienan Chen, Hang Luo, Xiaohui Tao, Hewen Jiang, Xin Yang, Huarui Zhang, Sifan Yu, Yin Wang, and et al. 2024. "Connective Tissue Growth Factor: Regulation, Diseases, and Drug Discovery" International Journal of Molecular Sciences 25, no. 9: 4692. https://doi.org/10.3390/ijms25094692
APA StyleRen, M., Yao, S., Chen, T., Luo, H., Tao, X., Jiang, H., Yang, X., Zhang, H., Yu, S., Wang, Y., Lu, A., & Zhang, G. (2024). Connective Tissue Growth Factor: Regulation, Diseases, and Drug Discovery. International Journal of Molecular Sciences, 25(9), 4692. https://doi.org/10.3390/ijms25094692






