Obstructive Sleep Apnea and Parkinson’s Disease: Bidirectional Clinical and Pathophysiologic Links
Abstract
1. Introduction
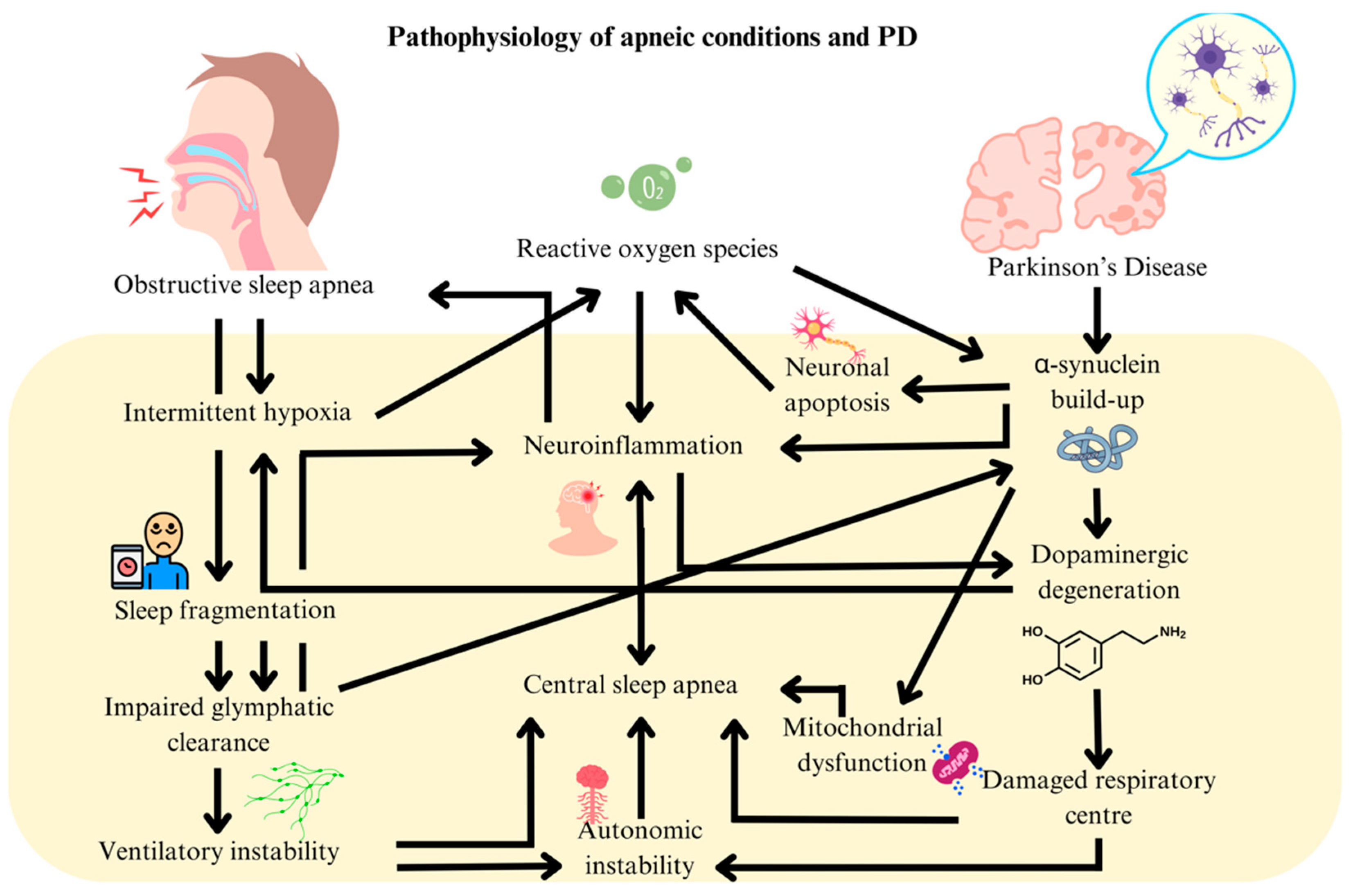
2. Pathophysiology of PD and OSA
3. Clinical Evidence Linking OSA and PD
4. Therapeutic Options for the Intersection of OSA and PD
5. Diagnostic Overlap Between Sleep Apnea and PD
6. Lack of Effective Therapy Targeting Both OSA and PD
7. Level of Evidence and Research Limitations
8. Brain Localization in OSA and PD
9. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yeghiazarians, Y.; Jneid, H.; Tietjens, J.R.; Redline, S.; Brown, D.L.; El-Sherif, N.; Mehra, R.; Bozkurt, B.; Ndumele, C.E.; Somers, V.K.; et al. Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 144, E56–E67. [Google Scholar] [CrossRef] [PubMed]
- Ben-Shlomo, Y.; Darweesh, S.; Llibre-Guerra, J.; Marras, C.; Luciano, M.S.; Tanner, C. The epidemiology of Parkinson’s disease. Lancet 2024, 403, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.D.J.; Chan, C.K.M.; Chua, W.Y.; Chao, Y.; Chan, L.L.; Tan, E.K. A Systemic Review and Meta-Analysis of the Risk of Venous Thromboembolic Events in Parkinson’s Patients. Eur. J. Neurol. 2025, 32, e70047. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.-H.; Hwang, Y.S.; Oh, S.-Y.; Shin, B.-S.; Kang, M.G.; Lee, M.G.; Yeom, S.W.; Lee, J.H.; Kang, H.G.; Kim, J.S. Bidirectional association between Parkinson’s disease and obstructive sleep apnea: A cohort study. J. Clin. Sleep Med. 2023, 19, 1615–1623. [Google Scholar] [CrossRef]
- Weihs, A.; Frenzel, S.; Grabe, H.J. The Link Between Obstructive Sleep Apnoea and Neurodegeneration and Cognition. Curr. Sleep Med. Rep. 2021, 7, 87–96. [Google Scholar] [CrossRef]
- El Amine, B.; Fournier, J.; Minoves, M.; Baillieul, S.; Roche, F.; Perek, N.; Pépin, J.-L.; Tamisier, R.; Khouri, C.; Rome, C.; et al. Cerebral oxidative stress, inflammation and apoptosis induced by intermittent hypoxia: A systematic review and meta-analysis of rodent data. Eur. Respir. Rev. 2024, 33, 240162. [Google Scholar] [CrossRef]
- Wang, Y.; Zou, W.; Jin, Z.; Yin, S.; Chi, X.; Li, J.; Sun, Y.; Wu, J.; Kou, L.; Xia, Y.; et al. Sleep, glymphatic system, and Parkinson’s disease. Ageing Neurodegener. Dis. 2024, 4. [Google Scholar] [CrossRef]
- Milagro, J.; Deviaene, M.; Gil, E.; Lázaro, J.; Buyse, B.; Testelmans, D.; Borzée, P.; Willems, R.; Van Huffel, S.; Bailón, R.; et al. Autonomic Dysfunction Increases Cardiovascular Risk in the Presence of Sleep Apnea. Front. Physiol. 2019, 10, 620. [Google Scholar] [CrossRef]
- Burtscher, J.; Duderstadt, Y.; Gatterer, H.; Burtscher, M.; Vozdek, R.; Millet, G.P.; Hicks, A.A.; Ehrenreich, H.; Kopp, M. Hypoxia Sensing and Responses in Parkinson’s Disease. Int. J. Mol. Sci. 2024, 25, 1759. [Google Scholar] [CrossRef]
- Zuzuárregui, J.R.P.; During, E.H. Sleep Issues in Parkinson’s Disease and Their Management. Neurother. J. Am. Soc. Exp. Neurother. 2020, 17, 1480–1494. [Google Scholar] [CrossRef]
- Chua, W.Y.; Wang, J.D.J.; Chan, C.K.M.; Chan, L.L.; Tan, E.K. Risk of aspiration pneumonia and hospital mortality in Parkinson disease: A systematic review and meta-analysis. Eur. J. Neurol. 2024, 31, e16449. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.R.; Zhang, L.; Ni Lin, Y.; Sun, X.W.; Ding, Y.J.; Li, N.; Li, H.P.; Li, S.Q.; Zhou, J.P.; Li, Q.Y. Chronic intermittent hypoxia-induced mitochondrial dysfunction mediates endothelial injury via the TXNIP/NLRP3/IL-1β signaling pathway. Free. Radic. Biol. Med. 2021, 165, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, J.L.; Martins, F.O.; Olea, E.; Prieto-Lloret, J.; Braga, P.C.; Sacramento, J.F.; Sequeira, C.O.; Negrinho, A.P.; Pereira, S.A.; Alves, M.G.; et al. Chronic Intermittent Hypoxia-Induced Dysmetabolism Is Associated with Hepatic Oxidative Stress, Mitochondrial Dysfunction and Inflammation. Antioxidants 2023, 12, 1910. [Google Scholar] [CrossRef]
- Guhathakurta, S.; Erdogdu, N.U.; Hoffmann, J.J.; Grzadzielewska, I.; Schendzielorz, A.; Seyfferth, J.; Mårtensson, C.U.; Corrado, M.; Karoutas, A.; Warscheid, B.; et al. COX17 acetylation via MOF–KANSL complex promotes mitochondrial integrity and function. Nat. Metab. 2023, 5, 1931–1952. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wen, P.; Luo, J.; Ding, H.; Cao, H.; He, W.; Zen, K.; Zhou, Y.; Yang, J.; Jiang, L. Sirtuin 3 regulates mitochondrial protein acetylation and metabolism in tubular epithelial cells during renal fibrosis. Cell Death Dis. 2021, 12, 847. [Google Scholar] [CrossRef]
- Han, J.; Kaufman, R.J. The role of ER stress in lipid metabolism and lipotoxicity. J. Lipid Res. 2016, 57, 1329–1338. [Google Scholar] [CrossRef]
- Rideout, H.J.; Chartier-Harlin, M.-C.; Fell, M.J.; Hirst, W.D.; Huntwork-Rodriguez, S.; Leyns, C.E.G.; Mabrouk, O.S.; Taymans, J.-M. The Current State-of-the Art of LRRK2-Based Biomarker Assay Development in Parkinson’s Disease. Front. Neurosci. 2020, 14, 865. [Google Scholar] [CrossRef]
- Sun, A.-P.; Liu, N.; Zhang, Y.-S.; Zhao, H.-Y.; Liu, X.-L. The relationship between obstructive sleep apnea and Parkinson’s disease: A systematic review and meta-analysis. Neurol. Sci. 2020, 41, 1153–1162. [Google Scholar] [CrossRef]
- Elfil, M.; Bahbah, E.I.; Attia, M.M.; Eldokmak, M.; Koo, B.B. Impact of Obstructive Sleep Apnea on Cognitive and Motor Functions in Parkinson’s Disease. Mov. Disord. 2021, 36, 570–580. [Google Scholar] [CrossRef]
- Aarsland, D.; Batzu, L.; Halliday, G.M.; Geurtsen, G.J.; Ballard, C.; Chaudhuri, K.R.; Weintraub, D. Parkinson disease-associated cognitive impairment. Nat. Rev. Dis. Prim. 2021, 7, 47. [Google Scholar] [CrossRef]
- Zhu, J.; Zhao, Y.; Jiang, Y.; Pan, Y.; Jiang, X.; Wang, Y.; Li, D.; Zhang, L. The relationship between obstructive sleep apnea and visual hallucinations in PD patients: A polysomnography study. Front. Neurol. 2024, 14, 1275660. [Google Scholar] [CrossRef] [PubMed]
- Mullins, A.E.; Parekh, A.; Kam, K.; Castillo, B.; Roberts, Z.J.; Fakhoury, A.; Valencia, D.I.; Schoenholz, R.; Tolbert, T.M.; Bronstein, J.Z.; et al. Selective Continuous Positive Airway Pressure Withdrawal With Supplemental Oxygen During Slow-Wave Sleep as a Method of Dissociating Sleep Fragmentation and Intermittent Hypoxemia-Related Sleep Disruption in Obstructive Sleep Apnea. Front. Physiol. 2021, 12, 750516. [Google Scholar] [CrossRef] [PubMed]
- Gros, P.; Mery, V.P.; Lafontaine, A.-L.; Robinson, A.; Benedetti, A.; Kimoff, R.J.; Kaminska, M. Obstructive sleep apnea in Parkinson’s disease patients: Effect of Sinemet CR taken at bedtime. Sleep Breath. 2016, 20, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Dong, Z.-F.; Pan, P.-L.; Shi, H.-C.; Liu, C.-F. Obstructive sleep apnea in Parkinson’s disease: A study in 239 Chinese patients. Sleep Med. 2020, 67, 237–243. [Google Scholar] [CrossRef]
- Anjum, M.F.; Smyth, C.; Dijk, D.J.; Starr, P.; Denison, T.; Little, S. Multi-night cortico-basal recordings reveal mechanisms of NREM slow wave suppression and spontaneous awakenings at high-temporal resolution in Parkinson’s disease. Res. Sq. 2023, rs. 3, rs-3484527. [Google Scholar] [CrossRef]
- Tolleson, C.M.; Bagai, K.; Walters, A.S.; Davis, T.L. A Pilot Study Assessing the Effects of Pallidal Deep Brain Stimulation on Sleep Quality and Polysomnography in Parkinson’s Patients. Neuromodulation Technol. Neural Interface 2016, 19, 724–730. [Google Scholar] [CrossRef]
- Nuber, S.; Zhang, X.; McCaffery, T.D.; Moors, T.E.; Adom, M.-A.; Hahn, W.N.; Martin, D.; Ericsson, M.; Tripathi, A.; Dettmer, U.; et al. Generation of G51D and 3D mice reveals decreased α-synuclein tetramer-monomer ratios promote Parkinson’s disease phenotypes. NPJ Park. Dis. 2024, 10, 47. [Google Scholar] [CrossRef]
- Fei, W.; Jiao, W.; Feng, X.; Chen, X.; Wang, Y. Intermittent hypoxia mimicking obstructive sleep apnea aggravates early brain injury following ICH via neuroinflammation and apoptosis. Mol. Med. Rep. 2021, 24, 824. [Google Scholar] [CrossRef]
- Qian, L.; Rawashdeh, O.; Kasas, L.; Milne, M.R.; Garner, N.; Sankorrakul, K.; Marks, N.; Dean, M.W.; Kim, P.R.; Sharma, A.; et al. Cholinergic basal forebrain degeneration due to sleep-disordered breathing exacerbates pathology in a mouse model of Alzheimer’s disease. Nat. Commun. 2022, 13, 6543. [Google Scholar] [CrossRef]
- Zhu, B.; Park, J.-M.; Coffey, S.R.; Russo, A.; Hsu, I.-U.; Wang, J.; Su, C.; Chang, R.; Lam, T.T.; Gopal, P.P.; et al. Single-cell transcriptomic and proteomic analysis of Parkinson’s disease brains. Sci. Transl. Med. 2024, 16, eabo1997. [Google Scholar] [CrossRef]
- Urrestizala-Arenaza, N.; Cerchio, S.; Cavaliere, F.; Magliaro, C. Limitations of human brain organoids to study neurodegenerative diseases: A manual to survive. Front Cell Neurosci. 2024, 18, 1419526. [Google Scholar] [CrossRef] [PubMed]
- Maggi, G.; Giacobbe, C.; Iannotta, F.; Santangelo, G.; Vitale, C. Prevalence and clinical aspects of obstructive sleep apnea in Parkinson disease: A meta-analysis. Eur. J. Neurol. 2024, 31, e16109. [Google Scholar] [CrossRef] [PubMed]
- Bargiotas, P.; Bargiotas, I.; Debove, I.; Lachenmayer, M.L.; Vayatis, N.; Schuepbach, W.M.; Bassetti, C.L. Sleep apnea syndrome and subthalamic stimulation in Parkinson’s disease. Sleep Med. 2021, 86, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Benedetti, A.; Lafontaine, A.-L.; Mery, V.; Robinson, A.R.; Kimoff, J.; Gros, P.; Kaminska, M. Obstructive sleep apnea, CPAP therapy and Parkinson’s disease motor function: A longitudinal study. Park. Relat. Disord. 2020, 70, 45–50. [Google Scholar] [CrossRef]
- Sobreira-Neto, M.A.; Pena-Pereira, M.A.; Sobreira, E.S.T.; Chagas, M.H.N.; de Almeida, C.M.O.; Fernandes, R.M.F.; Tumas, V.; Eckeli, A.L. Factors related to excessive sleepiness in patients with Parkinson’s disease. Neurol. Res. 2019, 41, 227–233. [Google Scholar] [CrossRef]
- Mery, V.P.; Gros, P.; Lafontaine, A.-L.; Robinson, A.; Benedetti, A.; Kimoff, R.J.; Kaminska, M. Reduced cognitive function in patients with Parkinson disease and obstructive sleep apnea. Neurology 2017, 88, 1120–1128. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, J.D.J.; Chua, N.Y.M.; Chan, L.-L.; Tan, E.-K. Obstructive Sleep Apnea and Parkinson’s Disease: Bidirectional Clinical and Pathophysiologic Links. Int. J. Mol. Sci. 2025, 26, 3762. https://doi.org/10.3390/ijms26083762
Wang JDJ, Chua NYM, Chan L-L, Tan E-K. Obstructive Sleep Apnea and Parkinson’s Disease: Bidirectional Clinical and Pathophysiologic Links. International Journal of Molecular Sciences. 2025; 26(8):3762. https://doi.org/10.3390/ijms26083762
Chicago/Turabian StyleWang, Jia Dong James, Nevin Yi Meng Chua, Ling-Ling Chan, and Eng-King Tan. 2025. "Obstructive Sleep Apnea and Parkinson’s Disease: Bidirectional Clinical and Pathophysiologic Links" International Journal of Molecular Sciences 26, no. 8: 3762. https://doi.org/10.3390/ijms26083762
APA StyleWang, J. D. J., Chua, N. Y. M., Chan, L.-L., & Tan, E.-K. (2025). Obstructive Sleep Apnea and Parkinson’s Disease: Bidirectional Clinical and Pathophysiologic Links. International Journal of Molecular Sciences, 26(8), 3762. https://doi.org/10.3390/ijms26083762





