An Objective Methodology for the Selection of a Device for Continuous Mobility Assessment
Abstract
:1. Introduction
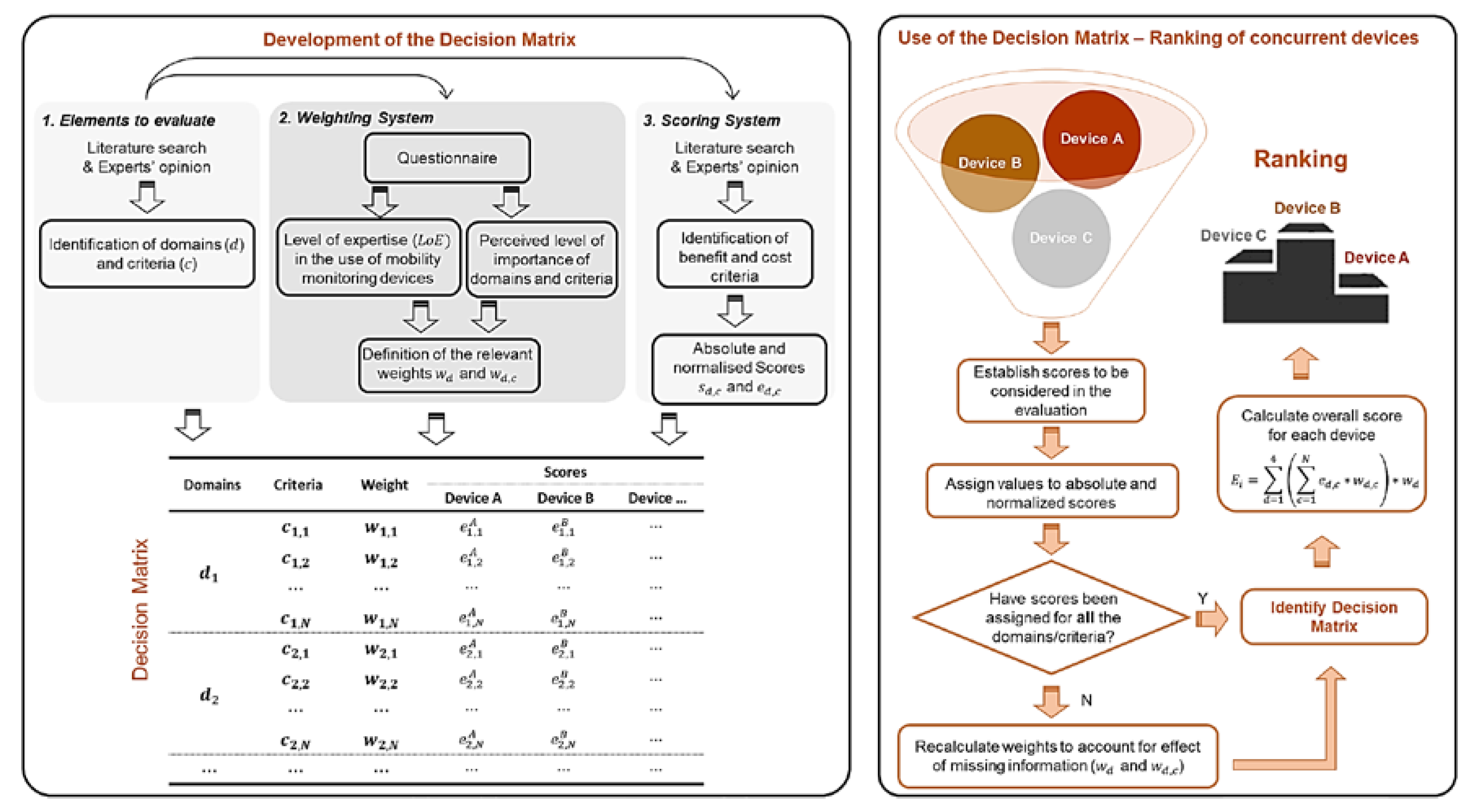
2. Materials and Methods
2.1. Domains and Relevant Criteria
- Concurrent validity–factors related to the validity of the measurements;
- Human factors–factors related to the context of data capture, perception of the user towards the technology, data security and privacy, effect of monitoring outside clinical settings;
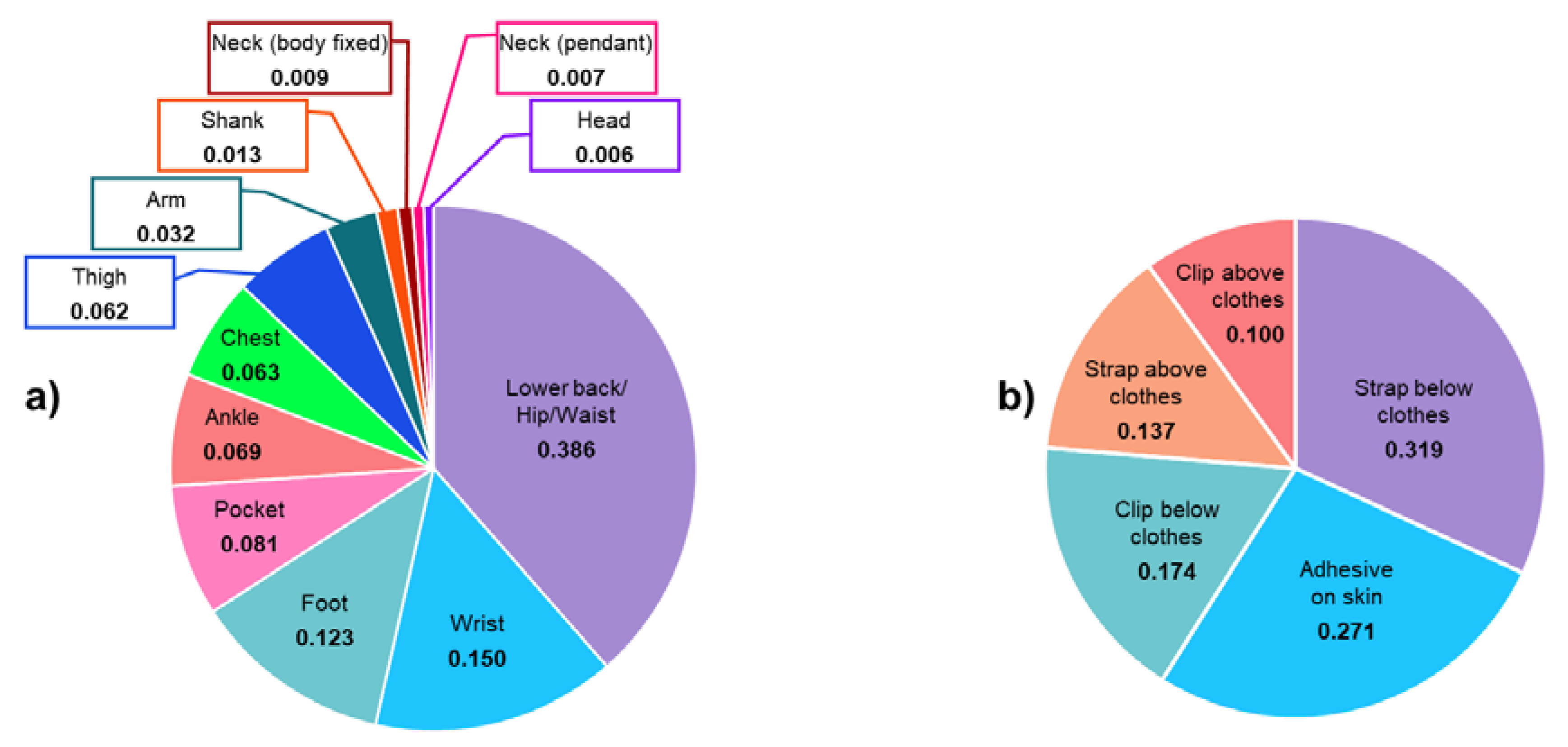
- Wearability & usability for the wearer–e.g., size, location, fixation modality, charging frequency;
- Data capture process–e.g., whether a calibration procedure, device programming, or anthropometric information are required for appropriate data capture.
2.1.1. Concurrent Validity criteria
2.1.2. Human Factors Criteria
2.1.3. Wearability and Usability Criteria
2.1.4. Data Capture Process Criteria
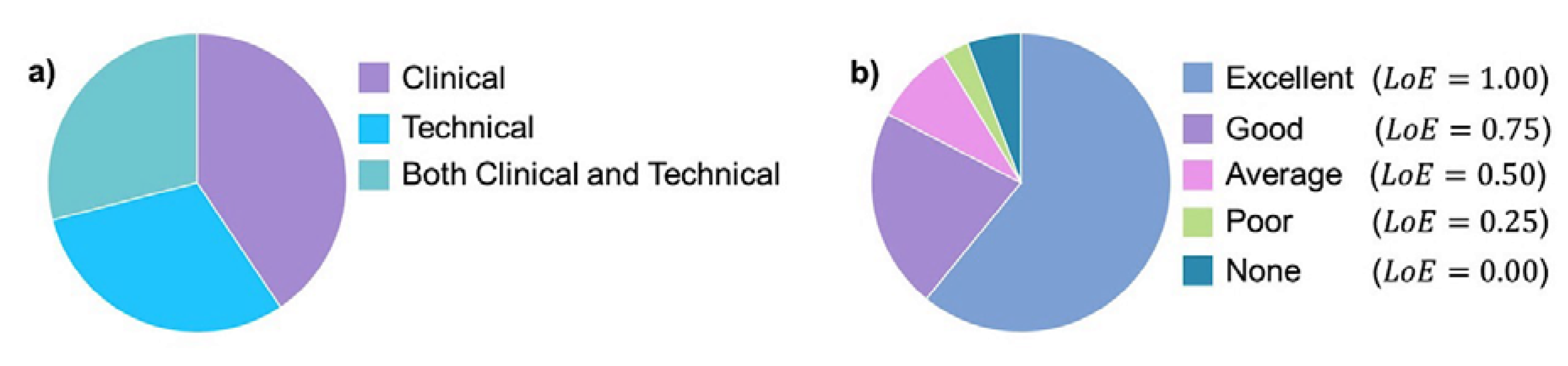
2.2. Weighting System
- Respondents’ background: clinical, technical, or both.
- Respondents’ level of expertise () with the use of wearable devices in clinical practice based on four questions:
- Do you know how a wearable device works and how it is used to identify gait features?
- As a researcher, have you ever used a wearable device?
- Have you ever used wearable devices directly on patients as opposed to healthy individuals?
- Have you ever analysed the information/data extracted from wearable devices to characterise patients’ mobility?
- Each positive response was scored as 0.25, and the total was obtained as a sum of the partial scores. of each participant was then classified as excellent, good, average, poor, or none if total was 1.00, 0.75, 0.50, 0.25, and 0, respectively.
- Respondents’ perceived level of importance of each domain and criterion, based on a 1–5 Likert scale (1 = unimportant; 5 = very important).
- The modal value of the responses of each domain and criterion, and , respectively, calculated as the preferences indicated by each respondent. The latter were multiplied by the relevant , which allowed us to account for the relevant respondents’ level of expertise.
2.3. Scoring System
- Accuracy: closeness of an estimated parameter () to the “true value” measured using a gold standard () and is expressed in percentage as:
- Robustness to changes in the device positioning, quantified as .
- Reliability between different trials, quantified as .
- ICC: the agreement between and in different trials.
- Sensitivity (%): describes the true positive () events, i.e., the number of gait events (GEs–defined as initial and final foot-to-ground contacts and used to identify strides, steps, as well as gait cycle phases [18], expressed as unitless numbers) and Walking Bouts (WBs) correctly identified with a device/algorithm solution () as compared to the values from a gold standard ():
- Specificity (%): number of true negative () events relative to the actual events assessed with a gold standard:
- Positive predictive value (%): events over the total amount of identified GEs, including falsely detected GEs ():
2.4. Comparison of Concurrent Solutions
2.5. Application of the Decision Matrix
- Example 2. An evaluation of four (Movemonitor, Mc Roberts, The Hague, The Netherlands; Up, Jawbone, San Francisco, USA; One, Fitbit, San Francisco, USA; ActivPAL, PAL Technologies Ltd., Glasgow, UK) of the seven wearable devices placed in different locations as explored in Storm et al. [28].
3. Results
3.1. Participants
3.2. Weighting System
3.3. Scores
3.4. Use of the Decision Matrix
3.4.1. Example 1
3.4.2. Example 2
4. Discussion
5. Conclusions
Author Contributions
Funding

Acknowledgments
Conflicts of Interest
References
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Nevitt, M. Gait speed and survival in older adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cesari, M.; Kritchevsky, S.B.; Penninx, B.W.; Nicklas, B.J.; Simonsick, E.M.; Newman, A.B.; Visser, M. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J. Am. Geriatr. Soc. 2005, 53, 1675–1680. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perera, S.; Patel, K.V.; Rosano, C.; Rubin, S.M.; Satterfield, S.; Harris, T.; Newman, A.B. Gait speed predicts incident disability: A pooled analysis. J. Gerontol. Ser. A Biomed. Sci. Med Sci. 2016, 71, 63–71. [Google Scholar] [CrossRef]
- Galperin, I.; Hillel, I.; Del Din, S.; Bekkers, E.M.; Nieuwboer, A.; Abbruzzese, G.; Avanzino, L.; Nieuwhof, F.; Bloem, B.R.; Rochester, L.; et al. Associations between daily-living physical activity and laboratory-based assessments of motor severity in patients with falls and Parkinson’s disease. Parkinsonism Relat. Disord. 2019, 62, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Del Din, S.; Godfrey, A.; Mazzà, C.; Lord, S.; Rochester, L. Free-living monitoring of Parkinson’s disease: Lessons from the field. Mov. Disord. 2016, 31, 1293–1313. [Google Scholar] [CrossRef] [PubMed]
- Aminian, K.; Najafi, B.; Büla, C.; Leyvraz, P.F.; Robert, P. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. J. Biomech. 2002, 35, 689–699. [Google Scholar] [CrossRef]
- Bugané, F.; Benedetti, M.G.; Casadio, G.; Attala, S.; Biagi, F.; Manca, M.; Leardini, A. Estimation of spatial-temporal gait parameters in level walking based on a single accelerometer: Validation on normal subjects by standard gait analysis. Comput. Methods Programs Biomed. 2012, 108, 129–137. [Google Scholar] [CrossRef]
- Catalfamo, P.; Ghoussayni, S.; Ewins, D. Gait event detection on level ground and incline walking using a rate gyroscope. Sensors 2010, 10, 5683–5702. [Google Scholar] [CrossRef] [Green Version]
- Ferrari, A.; Ginis, P.; Hardegger, M.; Casamassima, F.; Rocchi, L.; Chiari, L. A mobile Kalman-filter based solution for the real-time estimation of spatio-temporal gait parameters. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 24, 764–773. [Google Scholar] [CrossRef] [Green Version]
- González, R.C.; López, A.M.; Rodriguez-Uría, J.; Alvarez, D.; Alvarez, J.C. Real-time gait event detection for normal subjects from lower trunk accelerations. Gait Posture 2010, 31, 322–325. [Google Scholar] [CrossRef]
- Lee, H.K.; Hwang, S.J.; Cho, S.P.; Lee, D.R.; You, S.H.; Lee, K.J.; Choi, H.S. Novel algorithm for the hemiplegic gait evaluation using a single 3-axis accelerometer. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 3964–3966. [Google Scholar]
- Lee, J.A.; Cho, S.H.; Lee, Y.J.; Yang, H.K.; Lee, J.W. Portable activity monitoring system for temporal parameters of gait cycles. J. Med Syst. 2010, 34, 959–966. [Google Scholar] [CrossRef] [PubMed]
- Khandelwal, S.; Wickström, N. Identification of gait events using expert knowledge and continuous wavelet transform analysis. In Proceedings of the 7th International Conference on Bio-inspired Systems and Signal Processing (BIOSIGNALS 2014), Angers, France, 3–6 March 2014; pp. 197–204. [Google Scholar]
- Köse, A.; Cereatti, A.; Della Croce, U. Bilateral step length estimation using a single inertial measurement unit attached to the pelvis. J. Neuroeng. Rehabil. 2012, 9, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mariani, B.; Jiménez, M.C.; Vingerhoets, F.J.; Aminian, K. On-shoe wearable sensors for gait and turning assessment of patients with Parkinson’s disease. IEEE Trans. Biomed. Eng. 2012, 60, 155–158. [Google Scholar] [CrossRef] [PubMed]
- McCamley, J.; Donati, M.; Grimpampi, E.; Mazza, C. An enhanced estimate of initial contact and final contact instants of time using lower trunk inertial sensor data. Gait Posture 2012, 36, 316–318. [Google Scholar] [CrossRef]
- Sabatini, A.M.; Martelloni, C.; Scapellato, S.; Cavallo, F. Assessment of walking features from foot inertial sensing. IEEE Trans. Biomed. Eng. 2005, 52, 486–494. [Google Scholar] [CrossRef] [Green Version]
- Salarian, A.; Russmann, H.; Vingerhoets, F.J.; Dehollain, C.; Blanc, Y.; Burkhard, P.R.; Aminian, K. Gait assessment in Parkinson’s disease: Toward an ambulatory system for long-term monitoring. IEEE Trans. Biomed. Eng. 2004, 51, 1434–1443. [Google Scholar] [CrossRef]
- Shin, S.H.; Park, C.G. Adaptive step length estimation algorithm using optimal parameters and movement status awareness. Med. Eng. Phys. 2011, 33, 1064–1071. [Google Scholar] [CrossRef]
- Trojaniello, D.; Cereatti, A.; Pelosin, E.; Avanzino, L.; Mirelman, A.; Hausdorff, J.M.; Della Croce, U. Estimation of step-by-step spatio-temporal parameters of normal and impaired gait using shank-mounted magneto-inertial sensors: Application to elderly, hemiparetic, parkinsonian and choreic gait. J. Neuroeng. Rehabil. 2014, 11, 152. [Google Scholar] [CrossRef] [Green Version]
- Zijlstra, W.; Hof, A.L. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Sahoo, S.; Saboo, M.; Pratihar, D.K.; Mukhopadhyay, S. Real-Time Detection of Actual and Early Gait Events During Level-Ground and Ramp Walking. IEEE Sens. J. 2020. [Google Scholar] [CrossRef]
- Bongartz, M.; Kiss, R.; Lacroix, A.; Eckert, T.; Ullrich, P.; Jansen, C.P.; Feißt, M.; Mellone, S.; Chiari, L.; Becker, C.; et al. Validity, reliability, and feasibility of the uSense activity monitor to register physical activity and gait performance in habitual settings of geriatric patients. Physiol. Meas. 2019, 40, 095005. [Google Scholar] [CrossRef] [PubMed]
- Jasiewicz, J.M.; Allum, J.H.; Middleton, J.W.; Barriskill, A.; Condie, P.; Purcell, B.; Li, R.C.T. Gait event detection using linear accelerometers or angular velocity transducers in able-bodied and spinal-cord injured individuals. Gait Posture 2006, 24, 502–509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khandelwal, S.; Wickström, N. Evaluation of the performance of accelerometer-based gait event detection algorithms in different real-world scenarios using the MAREA gait database. Gait Posture 2017, 51, 84–90. [Google Scholar] [CrossRef]
- Mansour, K.B.; Rezzoug, N.; Gorce, P. Analysis of several methods and inertial sensors locations to assess gait parameters in able-bodied subjects. Gait Posture 2015, 42, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Panebianco, G.P.; Bisi, M.C.; Stagni, R.; Fantozzi, S. Analysis of the performance of 17 algorithms from a systematic review: Influence of sensor position, analysed variable and computational approach in gait timing estimation from IMU measurements. Gait Posture 2018, 66, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Storm, F.A.; Heller, B.W.; Mazzà, C. Step detection and activity recognition accuracy of seven physical activity monitors. PLoS ONE 2015, 10, e0118723. [Google Scholar] [CrossRef]
- Storm, F.A.; Buckley, C.J.; Mazzà, C. Gait event detection in laboratory and real life settings: Accuracy of ankle and waist sensor based methods. Gait Posture 2016, 50, 42–46. [Google Scholar] [CrossRef] [Green Version]
- Storm, F.A.; Nair, K.P.S.; Clarke, A.J.; Van der Meulen, J.M.; Mazza, C. Free-living and laboratory gait characteristics in patients with multiple sclerosis. PLoS ONE 2018, 13, e0196463. [Google Scholar] [CrossRef] [Green Version]
- Trojaniello, D.; Cereatti, A.; Della Croce, U. Accuracy, sensitivity and robustness of five different methods for the estimation of gait temporal parameters using a single inertial sensor mounted on the lower trunk. Gait Posture 2014, 40, 487–492. [Google Scholar] [CrossRef]
- Nguyen, M.D.; Mun, K.R.; Jung, D.; Han, J.; Park, M.; Kim, J.; Kim, J. IMU-based Spectrogram Approach with Deep Convolutional Neural Networks for Gait Classification. In Proceedings of the 2020 IEEE International Conference on Consumer Electronics (ICCE), Las Vegas, NV, USA, 4–6 January 2020; pp. 1–6. [Google Scholar]
- Wang, X.; White, L.; Chen, X.; Gao, Y.; Li, H.; Luo, Y. An empirical study of wearable technology acceptance in healthcare. Ind. Manag. Data Syst. 2015, 115, 1704–1723. [Google Scholar]
- Jia, Y.; Wang, W.; Wen, D.; Liang, L.; Gao, L.; Lei, J. Perceived user preferences and usability evaluation of mainstream wearable devices for health monitoring. PeerJ 2018, 6, e5350. [Google Scholar] [CrossRef] [PubMed]
- Puri, A.; Kim, B.; Nguyen, O.; Stolee, P.; Tung, J.; Lee, J. User acceptance of wrist-worn activity trackers among community-dwelling older adults: Mixed method study. JMIR Mhealth Uhealth 2017, 5, e173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keogh, A.; Dorn, J.F.; Walsh, L.; Calvo, F.; Caulfield, B. Comparing the Usability and Acceptability of Wearable Sensors Among Older Irish Adults in a Real-World Context: Observational Study. JMIR Mhealth Uhealth 2020, 8, e15704. [Google Scholar] [PubMed]
- McMahon, S.K.; Lewis, B.; Oakes, M.; Guan, W.; Wyman, J.F.; Rothman, A.J. Older adults’ experiences using a commercially available monitor to self-track their physical activity. JMIR Mhealth Uhealth 2016, 4, e35. [Google Scholar] [CrossRef]
- Rabinovich, R.A.; Louvaris, Z.; Raste, Y.; Langer, D.; Van Remoortel, H.; Giavedoni, S.; Burtin, C.; Regueiro, E.M.; Vogiatzis, I.; Hopkinson, N.S.; et al. Validity of physical activity monitors during daily life in patients with COPD. Eur. Respir. J. 2013, 42, 1205–1215. [Google Scholar] [CrossRef] [Green Version]
- Vooijs, M.; Alpay, L.L.; Snoeck-Stroband, J.B.; Beerthuizen, T.; Siemonsma, P.C.; Abbink, J.J.; Rövekamp, T.A. Validity and usability of low-cost accelerometers for internet-based self-monitoring of physical activity in patients with chronic obstructive pulmonary disease. Interact. J. Med Res. 2014, 3, e14. [Google Scholar] [CrossRef]
- Mercer, K.; Giangregorio, L.; Schneider, E.; Chilana, P.; Li, M.; Grindrod, K. Acceptance of commercially available wearable activity trackers among adults aged over 50 and with chronic illness: A mixed-methods evaluation. JMIR Mhealth Uhealth 2016, 4, e7. [Google Scholar] [CrossRef]
- Welk, G.J.; Blair, S.N.; Wood, K.; Jones, S.; Thompson, R.W. A comparative evaluation of three accelerometry-based physical activity monitors. Med. Sci. Sports Exerc. 2000, 32, S489–S497. [Google Scholar] [CrossRef]
- Carver, S.J. Integrating multi-criteria evaluation with geographical information systems. Int. J. Geogr. Inf. Syst. 1991, 5, 321–339. [Google Scholar] [CrossRef] [Green Version]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef] [Green Version]
- Caramia, C.; Torricelli, D.; Schmid, M.; Muñoz-Gonzalez, A.; Gonzalez-Vargas, J.; Grandas, F.; Pons, J.L. IMU-Based Classification of Parkinson’s Disease From Gait: A Sensitivity Analysis on Sensor Location and Feature Selection. IEEE J. Biomed. Health Inform. 2018, 22, 1765–1774. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Lach, J.; Lo, B.; Yang, G.Z. Toward pervasive gait analysis with wearable sensors: A systematic review. IEEE J. Biomed. Health Inform. 2016, 20, 1521–1537. [Google Scholar] [CrossRef] [PubMed]
- Greene, B.R.; McGrath, D.; O’Neill, R.; O’Donovan, K.J.; Burns, A.; Caulfield, B. An adaptive gyroscope-based algorithm for temporal gait analysis. Med. Biol. Eng. Comput. 2010, 48, 1251–1260. [Google Scholar] [CrossRef] [PubMed]
- Awais, M.; Palmerini, L.; Chiari, L. Physical activity classification using body-worn inertial sensors in a multi-sensor setup. In Proceedings of the 2016 IEEE 2nd International Forum on Research and Technologies for Society and Industry Leveraging a better tomorrow (RTSI), Bologna, Italy, 7–9 September 2016; pp. 1–4. [Google Scholar]
- Howcroft, J.; Kofman, J.; Lemaire, E.D. Review of fall risk assessment in geriatric populations using inertial sensors. J. Neuroeng. Rehabil. 2013, 10, 91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Summa, A.; Vannozzi, G.; Bergamini, E.; Iosa, M.; Morelli, D.; Cappozzo, A. Multilevel upper body movement control during gait in children with cerebral palsy. PLoS ONE 2016, 11, e0151792. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Fischer, E.; Tunca, C.; Brahms, C.M.; Ersoy, C.; Granacher, U.; Arnrich, B. How We Found Our IMU: Guidelines to IMU Selection and a Comparison of Seven IMUs for Pervasive Healthcare Applications. Sensors 2020, 20, 4090. [Google Scholar] [CrossRef] [PubMed]
- Manta, C.; Patrick-Lake, B.; Goldsack, J.C. Digital Measures That Matter to Patients: A Framework to Guide the Selection and Development of Digital Measures of Health. Digit. Biomark. 2020, 4, 69–77. [Google Scholar] [CrossRef]



| Domain | Criterion | Benefit | Cost | Score |
|---|---|---|---|---|
| Concurrent Validity | Walking speed accuracy | ✓ | Scores based on the relevant technical definitions | |
| Walking speed robustness | ✓ | |||
| Walking speed reliability | ✓ | |||
| Walking speed–Interclass coefficient | ✓ | |||
| Walking bout detection sensitivity | ✓ | |||
| Walking bout detection specificity | ✓ | |||
| Walking bout detection accuracy | ✓ | |||
| Walking bout detection robustness | ✓ | |||
| Walking bout detection reliability | ✓ | |||
| Gait event sensitivity | ✓ | |||
| Gait events identification | ✓ | |||
| Human Factors | Use of technology in healthcare * | ✓ | – | |
| Data security | ✓ | Yes(1)/No(0) | ||
| Adherence to data capture | ✓ | Yes(1)/No(0) | ||
| Burden of data capture * | ✓ | – | ||
| Impact of monitoring | ✓ | Yes(1)/No(0) | ||
| Trust in the device | ✓ | Commercial: Yes(1)/No(0) | ||
| Wearability and usability | Comfort * | ✓ | – | |
| Location | ✓ | 1 | ||
| Ease of use | ✓ | Interaction: Yes(1)/No(0) | ||
| Frequency of recharging | ✓ | Battery Life 2 | ||
| Perceived usefulness * | ✓ | NA | ||
| Whether it provides feedback | ✓ | Yes(1)/No(0) | ||
| Size | ✓ | width x height x depth x mass | ||
| Fixation modality | ✓ | 1 | ||
| Data Capture Process | Calibration procedure | ✓ | Yes(1)/No(0) | |
| Required static/functional movements | ✓ | Yes(1)/No(0) | ||
| Required device programming | ✓ | Yes(1)/No(0) | ||
| Questionnaires/Anthropometric measures | ✓ | Yes(1)/No(0) |
| Domains | Criteria | ||
|---|---|---|---|
| Weight | Weight | ||
| Concurrent Validity | 0.368 | Walking speed accuracy | 0.133 |
| Walking speed reliability | 0.130 | ||
| Walking speed robustness | 0.107 | ||
| Walking speed–Interclass coefficient | 0.107 | ||
| Walking bout detection specificity | 0.097 | ||
| Walking bout detection reliability | 0.095 | ||
| Walking bout detection accuracy | 0.087 | ||
| Walking bout detection sensitivity | 0.064 | ||
| Walking bout detection robustness | 0.062 | ||
| Gait event sensitivity | 0.059 | ||
| Gait events identification (PPV) | 0.057 | ||
| Human Factors | 0.175 | Trust in the device | 0.193 |
| Burden of data capture | 0.193 | ||
| Data security | 0.181 | ||
| Impact of monitoring | 0.163 | ||
| Adherence to data capture | 0.136 | ||
| Use of technology in healthcare | 0.134 | ||
| Wearability and usability | 0.296 | Ease of use | 0.185 |
| Comfort | 0.168 | ||
| Fixation modality | 0.141 | ||
| Size | 0.119 | ||
| Location | 0.116 | ||
| Perceived usefulness | 0.096 | ||
| Frequency of recharging | 0.092 | ||
| Whether it provides feedback | 0.083 | ||
| Data Capture Process | 0.161 | Calibration procedure | 0.326 |
| Required static/functional movements | 0.286 | ||
| Required device programming | 0.197 | ||
| Questionnaires/Anthropometric measures | 0.192 | ||
| Domains | Criteria | |||||
|---|---|---|---|---|---|---|
| Weight | Weight | T1 | T2 | T3 | ||
| Concurrent Validity | 0.368 | Walking bout detection accuracy 1 | 0.328 | 8 | 4 | 2 |
| 0.00 | 0.67 | 1.00 | ||||
| Walking bout detection robustness 1 | 0.234 | 9 | 4 | 2 | ||
| 0.00 | 0.71 | 1.00 | ||||
| Gait event identification (PPV) | 0.215 | 100 | 97 | 100 | ||
| 1.00 | 0.00 | 1.00 | ||||
| Gait events sensitivity | 0.223 | 97 | 82 | 100 | ||
| 0.83 | 0.00 | 1.00 | ||||
| Human Factors | 0.175 | Trust in the device | 0.516 | 1 | 1 | 1 |
| 1 | 1 | 1 | ||||
| Data security | 0.484 | 1 | 1 | 1 | ||
| 1 | 1 | 1 | ||||
| Wearability & usability | 0.296 | Fixation modality | 0.301 | 0.137 | 0.137 | 0.137 |
| 1.00 | 1.00 | 1.00 | ||||
| Size | 0.254 | 525.76 | 525.76 | 525.76 | ||
| 1.00 | 1.00 | 1.00 | ||||
| Location | 0.248 | 0.386 | 0.386 | 0.386 | ||
| 1.00 | 1.00 | 1.00 | ||||
| Frequency of recharging | 0.197 | 1 | 1 | 1 | ||
| 1.00 | 1.00 | 1.00 | ||||
| Data Capture Process | 0.161 | Calibration procedure | 0.326 | 0 | 0 | 0 |
| 1.00 | 1.00 | 1.00 | ||||
| Required static/functional movements | 0.286 | 1 | 1 | 1 | ||
| 0.00 | 0.00 | 0.00 | ||||
| Required device programming | 0.197 | 0 | 0 | 0 | ||
| 1.00 | 1.00 | 1.00 | ||||
| Questionnaires/Anthropometric measures | 0.192 | 1 | 0 | 0 | ||
| 0.00 | 1.00 | 1.00 | ||||
| Overall score | 0.70 | 0.73 | 0.95 |
| Domains | Criteria | ||||||
|---|---|---|---|---|---|---|---|
| Weight | Weight | S1 | S2 | S3 | S4 | ||
| Concurrent Validity | 0.368 | Step detection accuracy | 1.000 | 1.483 | 4.897 | 1.567 | 2.493 |
| 1.00 | 0.00 | 0.98 | 0.70 | ||||
| Human Factors | 0.175 | Trust in the device | 0.516 | 1 | 1 | 1 | 1 |
| 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Data security | 0.484 | 1 | 1 | 1 | 1 | ||
| 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Wearability & usability | 0.296 | Fixation modality | 0.301 | 0.319 | 0.174 | 0.174 | 0.271 |
| 1.00 | 0.00 | 0.00 | 0.67 | ||||
| Size | 0.254 | 3910.62 | 23.17 | 79.01 | 259.70 | ||
| 0.00 | 1.00 | 0.99 | 0.94 | ||||
| Location | 0.248 | 0.386 | 0.15 | 0.386 | 0.013 | ||
| 1.00 | 0.37 | 1.00 | 0.00 | ||||
| Frequency of recharging | 0.197 | 0.2 | 0.2 | 0.2 | 0.2 | ||
| 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Data Capture Process | 0.161 | Calibration procedure | 0.326 | 0 | 0 | 0 | 0 |
| 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Required static/functional movements | 0.286 | 0 | 0 | 0 | 0 | ||
| 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Required device programming | 0.197 | 1 | 0 | 0 | 0 | ||
| 0.00 | 1.00 | 1.00 | 1.00 | ||||
| Questionnaires/Anthropometric measures | 0.192 | 0 | 0 | 0 | 0 | ||
| 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Overall score | 0.89 | 0.41 | 0.81 | 0.78 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonci, T.; Keogh, A.; Del Din, S.; Scott, K.; Mazzà, C.; on behalf of the Mobilise-D consortium. An Objective Methodology for the Selection of a Device for Continuous Mobility Assessment. Sensors 2020, 20, 6509. https://doi.org/10.3390/s20226509
Bonci T, Keogh A, Del Din S, Scott K, Mazzà C, on behalf of the Mobilise-D consortium. An Objective Methodology for the Selection of a Device for Continuous Mobility Assessment. Sensors. 2020; 20(22):6509. https://doi.org/10.3390/s20226509
Chicago/Turabian StyleBonci, Tecla, Alison Keogh, Silvia Del Din, Kirsty Scott, Claudia Mazzà, and on behalf of the Mobilise-D consortium. 2020. "An Objective Methodology for the Selection of a Device for Continuous Mobility Assessment" Sensors 20, no. 22: 6509. https://doi.org/10.3390/s20226509
APA StyleBonci, T., Keogh, A., Del Din, S., Scott, K., Mazzà, C., & on behalf of the Mobilise-D consortium. (2020). An Objective Methodology for the Selection of a Device for Continuous Mobility Assessment. Sensors, 20(22), 6509. https://doi.org/10.3390/s20226509







